Female reproduction
Physiology of the menstrual cycle
Mechanisms of hormonal contraception
The ‘combined’ hormonal contraceptive
Progestogen-only contraceptives
Efficacy of hormonal contraception
Pharmacokinetics of contraceptive steroids
Physiology of the menstrual cycle
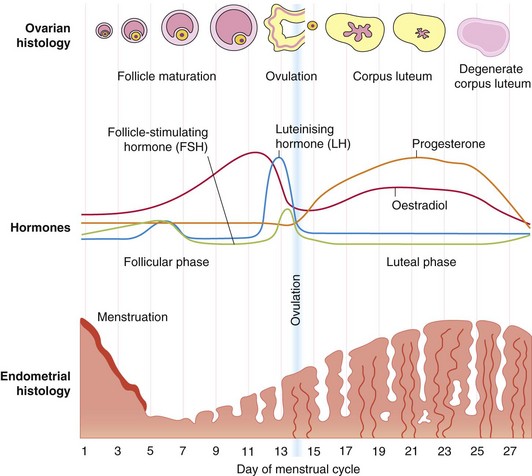
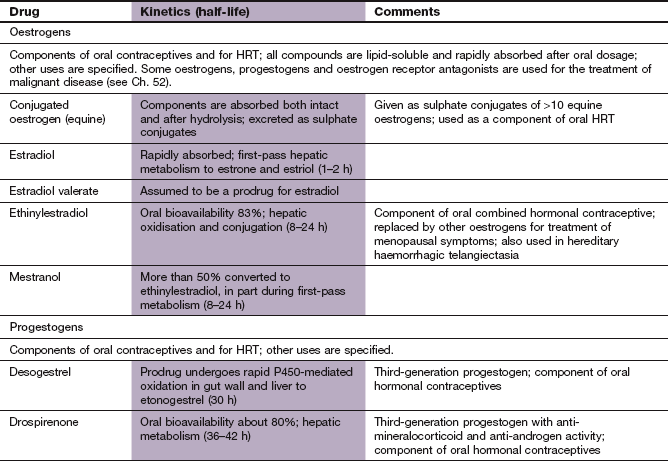
The endocrine function of the hypothalamo–pituitary–ovarian axis acts through a series of feedback loops to control the reproductive processes of the menstrual cycle (Fig. 45.1). The menstrual cycle begins with the uterus shedding its lining (menstrual phase: usually days 1 to 3–5 of the menstrual cycle). Following the shedding of the endometrium, a group of five to seven follicles in the ovary that have been growing for up to a year start to mature. This occurs under the influence of the gonadotropic hormone follicle-stimulating hormone (FSH) secreted from the anterior pituitary (follicular phase: approximately days 5–13 of the menstrual cycle). The secretion of FSH starts during the menstrual phase and continues during the early follicular phase, and is a result of the low circulating concentration of oestrogen. Release of the gonadotropic hormones FSH and luteinizing hormone (LH) is controlled by pulsatile secretion of gonadotropin-releasing hormone (GnRH) from the hypothalamus (see also Ch. 43). The small follicles produce gonadotropin surge-attenuating factor (GnSAF) that acts on the hypothalamus to inhibit GnRH release and prevent a rise in LH. The follicles also produce inhibin, which reduces FSH release. A single dominant ovarian follicle (or occasionally two) is selected and matures in preparation for ovulation at the expense of the remaining follicles. Regression of the other follicles is probably due to a lack of receptors for FSH.
FSH drives the developing ovarian follicle to convert androgens produced by its thecal cells into oestradiol (Fig. 44.2) within its granulosa cells. Oestradiol secretion from the follicle slowly rises as the follicle matures. In the window of time between the early to mid-follicular phase of the menstrual cycle the modest amount of oestrogen secreted by the follicle exerts negative feedback on both the hypothalamus and pituitary to keep gonadotropin secretion low (Fig. 43.1). The low plasma concentration of progesterone also weakly suppresses gonadotropin secretion in the early follicular phase.
In the late follicular phase a cohort of granulosa cells in the maturing ovarian follicle differentiates under the influence of FSH and starts to express LH receptors. These granulosa cells can then be stimulated by LH to secrete progesterone and are destined to become the corpus luteum after ovulation. In the mid- to late follicular phase the circulating oestradiol concentration rises dramatically as the follicle secretes more of the hormone under the influence of FSH. Eventually the plasma oestradiol reaches a critical concentration of about 200 pg · mL−1 for 48 h. The rapid rise and sustained high concentration of oestradiol triggers a switch from negative feedback to positive feedback of oestradiol upon the pituitary and hypothalamus, causing pulsatile release of GnRH. As a result there is an acute mid-cycle surge of LH for about 48 h, which is essential for ovulation. Ovulation involves release of the secondary oocyte from the follicle, which rapidly matures into an ovum.
Following ovulation (about day 14 of the menstrual cycle) the residual follicle transforms into the corpus luteum under the influence of the pituitary gonadotropins. The plasma LH concentration falls rapidly and remains low throughout the secretory (luteal) phase (days 15–26 of the menstrual cycle). The reason for this is that granulosa cells expressing LH receptors proliferate in the corpus luteum and produce increasing amounts of progesterone. Progesterone suppresses LH and FSH production by negative feedback on the hypothalamus and pituitary. If implantation of a fertilised ovum does not occur the corpus luteum regresses after about 10 days, since it requires gonadotropins to maintain itself.
From day 5 to late in the menstrual cycle the gradually increasing plasma concentrations of oestrogens, and subsequently progesterone, which are produced as the menstrual cycle progresses, result in proliferation and vascularisation of endometrial cells that are able to secrete a variety of fluids and nutrients aimed at making the endometrium receptive for implantation. The temporal precision of the change in receptivity is critical if successful implantation of a fertilised oocyte is to occur. Oestrogen and progesterone cause the endometrium to become oedematous, and its glands secrete increasing quantities of amino acids, sugars and glycoproteins in a viscous liquid. At the end of the menstrual cycle the circulating concentrations of progesterone and oestrogen eventually fall to levels that no longer support the endometrium. Deprived of hormonal support, the endometrial spiral arteries go into spasm and the endometrial cells die, producing digestive enzymes (ischaemic phase: days 27–28 of the menstrual cycle). As a consequence of this and other changes the endometrium is shed during menstruation.
The cervical mucus is also influenced by oestrogen and progesterone concentrations. Under the dominant influence of progesterone cervical mucus is viscid and less penetrable by sperm, whereas at ovulation the high plasma oestradiol concentration results in thinner and more elastic mucus that is easily penetrable by sperm. Progesterone also inhibits the motility of the fallopian tube, altering the transport of sperm, and the fertilised or unfertilised oocyte. Excess progesterone may alter the chance of fertilisation occurring or the embryo may reach the uterine cavity when the endometrium is not receptive to implantation. Oestrogens have the opposite action, increasing tubal motility, and may accelerate the transport of the ovum into the uterine cavity.
Physiology of pregnancy
Pregnancy is accompanied by considerable hormonal changes. When a fertilised ovum implants in the uterine lining the corpus luteum becomes essential for the production of progesterone and maintenance of pregnancy during the first 6–8 weeks. After this placental production of hormones takes over and the combined feto-placental unit produces progressively greater quantities of oestrogen and progesterone which reach the maternal circulation. The dividing cells of the implanted ovum start to secrete human chorionic gonadotropin (HCG) from about 9 days after fertilisation (Ch. 43). HCG stimulates the corpus luteum to continue to secrete progesterone. Eventually, the placenta takes over the production of HCG, progesterone and oestrogen. The placenta also produces human placental lactogen as pregnancy advances, resulting in the development of duct and milk-secreting cells in the mother's breasts. The precise balance of sex steroids also contributes to quiescence of the uterus during pregnancy and the onset of labour at term.
Mechanism of action of oestrogens and progestogens
In common with other steroid hormones, both oestrogens and progestogens act by influencing gene transcription (see also Ch. 44). They passively diffuse into the cell and bind to specific receptors in either the cytoplasm or cell nucleus (see Fig. 1.8). The receptors are associated with heat-shock protein (HSP) when in their unbound state in the cytosol. HSP dissociates when the hormone binds to the receptor, and the receptor forms dimers that are translocated by active transport to the cell nucleus. The steroid–receptor complex associates with hormone-response elements of numerous oestrogen- or progesterone-responsive genes. This leads to recruitment of co-activator molecules to the complex, and produces gene transcription (co-activation). Oestrogen binds to two specific cytoplasmic receptors (ERα and ERβ), which have different tissue distributions. Progesterone also has two specific receptors (PR-A and PR-B) that regulate progesterone-responsive genes. Oestrogen increases and progesterone decreases the expression of the progesterone receptors.
Steroidal contraceptives
Oral hormonal contraceptives (‘the pill’) are the most widely used form of contraception and contain either a combination of a synthetic oestrogen with a synthetic progestogen (a C19 synthetic progesterone derivative) or a progestogen alone.
Mechanisms of hormonal contraception
Elevated circulating concentrations of synthetic oestrogen and progestogen prevent the precise cyclic pattern of hormone-related events seen in the normal menstrual cycle (Fig. 45.2), and can be used for contraception.
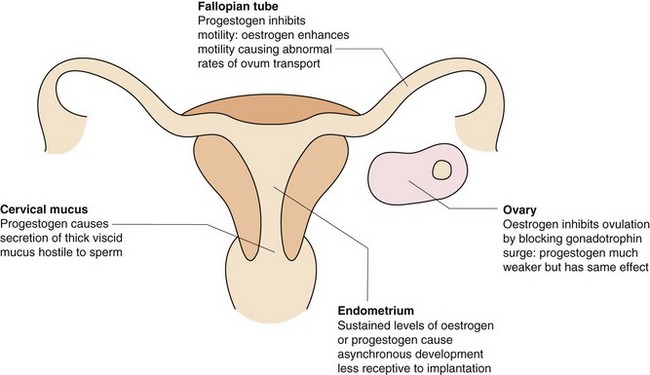
Fig. 45.2 The main contraceptive actions of the synthetic oestrogens and progestogens in the combined hormonal contraceptive pill.
FSH, follicle-stimulating hormone; LH, luteinizing hormone.
 The combination of oestrogen and progestogen exerts its contraceptive effect mainly through suppression of FSH release, which prevents development of the follicles in the ovary. The lack of a dominant follicle means that production of oestradiol is impaired. The failure of plasma oestradiol to rise, combined with negative feedback from the progestogen, prevents the mid-cycle LH surge that is essential for ovulation to occur.
The combination of oestrogen and progestogen exerts its contraceptive effect mainly through suppression of FSH release, which prevents development of the follicles in the ovary. The lack of a dominant follicle means that production of oestradiol is impaired. The failure of plasma oestradiol to rise, combined with negative feedback from the progestogen, prevents the mid-cycle LH surge that is essential for ovulation to occur.
 Progestogen produces asynchronous development of the endometrium with stromal thinning, which makes it less receptive to implantation of the fertilised ovum. Fallopian tube motility is increased by oestrogens and decreased by progestogens; this may affect fertility by altering the rate of transport of the ovum.
Progestogen produces asynchronous development of the endometrium with stromal thinning, which makes it less receptive to implantation of the fertilised ovum. Fallopian tube motility is increased by oestrogens and decreased by progestogens; this may affect fertility by altering the rate of transport of the ovum.
 Progestogen alters cervical mucus, making it thicker and less copious, thereby creating an environment more hostile to sperm penetration.
Progestogen alters cervical mucus, making it thicker and less copious, thereby creating an environment more hostile to sperm penetration.
Progestogens can be used alone for contraception, when the mechanism depends on the dose of progestogen. Low-dose progestogen inhibits ovulation in only about 50% of cycles, and contraception relies upon the other actions of the hormone. With higher doses, inhibition of follicular development and ovulation becomes more important.
The ‘combined’ hormonal contraceptive
Combined hormonal contraceptives (often called the combined oral contraceptive pill, or COCP) contain both a synthetic oestrogen and progestogen. The oestrogen component is usually ethinylestradiol (an oestrogen that is alkylated at C17 to slow its metabolism) but in some combinations is mestranol, a compound that is metabolised in the liver to ethinylestradiol. Over the years since the combined oral hormonal contraceptive was introduced, the dose of the oestrogen component has been reduced to minimise unwanted effects. ‘Second-generation’ combined hormonal contraceptives have a lower oestrogen concentration than ‘first-generation’ combined hormonal contraceptives, which are no longer used. The lowest dose of oestrogen that gives good menstrual cycle control (absence of breakthrough bleeding; see below) is preferred.
The progestogen component of the second-generation combined oral hormonal contraceptives is either levonorgestrel (the active isomer of norgestrel) or norethisterone; these compounds are testosterone analogues that also possess residual androgenic activity. ‘Third-generation’ oral combined hormonal contraceptives contain modified progestogens that have less androgenic activity – desogestrel, gestodene, norgestimate (which are all derivatives of norgestrel) – or anti-androgenic activity – dienogest, drospirenone (a derivative of the aldosterone antagonist spironolactone with some anti-mineralocorticoid activity). Modified progestogens are used if there are unacceptable unwanted effects with the second-generation progestogens.
Other differences and similarities between second- and third-generation combined hormonal contraceptives are discussed below.
Monophasic preparations
Monophasic preparations contain fixed amounts of oestrogen and progestogen. They are taken daily for the first 21 days of the menstrual cycle followed by seven contraceptive-free days with tablets containing an inactive substance, such as lactose. The oestrogen concentration should be the lowest that maintains good cycle control and produces minimal unwanted effects. There is a choice of:
 low-strength preparations that contain 20 µg ethinylestradiol,
low-strength preparations that contain 20 µg ethinylestradiol,
 standard-strength preparations that contain 30 or 35 µg ethinylestradiol, or 50 µg mestranol.
standard-strength preparations that contain 30 or 35 µg ethinylestradiol, or 50 µg mestranol.
The monophasic oral combined hormonal contraceptive contains one of several progestogens. In some women it may be necessary to change the formulation to reduce minor unwanted effects, such as breakthrough bleeding or weight gain during the menstrual cycle. The degree of androgenic activity possessed by different progestogens (see combined hormonal contraceptive section above) may influence the suitability of an individual preparation for a particular woman.
A transdermal patch formulation of low-strength ethinylestradiol with the third-generation progestogen norelgestromin is also available; this is applied weekly for 3 weeks followed by a 7-day patch-free interval. There is also a vaginal contraceptive ring that contains ethinylestradiol with the progestogen etonorgestrel.
Biphasic and triphasic preparations
Biphasic and triphasic preparations are designed to mimic more closely the changes in sex hormone concentrations that occur during the natural menstrual cycle. The total sex hormone intake through the cycle is no less than with monophasic preparations. Several preparations are available, all of which contain ethinylestradiol in combination with levonorgestrel, norethisterone or gestodene. The dose of ethinylestradiol is either kept constant throughout, as in the monophasic pills, or increased during days 7–12. Progestogen doses are increased once (biphasic) or twice (triphasic) as the menstrual cycle proceeds.
Progestogen-only contraceptives
Oral progestogen-only contraceptives
The oral progestogen-only contraceptive (‘progestogen-only pill’, or POP) is particularly useful for women in whom the administration of oestrogen is considered to be undesirable, for example if there is a history of thromboembolic disorders (see below). Pregnancy rates are slightly higher than with a low-dose combined oral hormonal contraceptive. Various progestogens are used, such as desogestrel, etynodiol diacetate, gestodene, levonorgestrel or norethisterone. The progestogen-only contraceptive must be taken daily, without a break, and within 3 h of the usual time every day (see efficacy below). Because the dose of progestogen is low, bleeding does occur at monthly intervals but may be irregular. Breakthrough bleeding occurs in up to 40% of women; this is much higher than with the combined hormonal contraceptive. Some women become amenorrhoeic while using progestogen-only contraception.
Parenteral progestogen-only contraceptives
Intramuscular injection of a progestogen, either medroxyprogesterone acetate or norethisterone, can provide contraception for up to 8–12 weeks. The higher dose of progestogen compared with the oral preparations reliably inhibits ovulation, and therefore there is a low incidence of ectopic pregnancy. The contraceptive effect is fully reversible, but there is a high incidence of amenorrhoea when its effect wears off. Prolonged use of medroxyprogesterone acetate can reduce bone mineral density and cause osteoporosis. The loss of bone mineral density occurs over the first 2–3 years of use and then stabilises. Prolonged use of medroxyprogesterone acetate beyond 2 years, or its use in adolescents or people with other risk factors for osteoporosis, is discouraged.
A subcutaneous implant of etonogestrel provides contraception for up to 3 years, after which time it should be replaced. The progestogen is released from a flexible rod inserted subdermally on the lower surface of the upper arm. Local irritation is experienced by some women. The implants are radio-opaque so they can be easily located by radiography. Unwanted effects are similar to those experienced with the oral progestogen-only contraceptive, but lower doses of progestogen are needed because first-pass metabolism in the gut and liver is avoided.
Intra-uterine progestogen-only device
A plastic intra-uterine contraceptive system (IUS) with a levonorgestrel-releasing system from a silicone reservoir provides effective contraception with reduced menstrual blood loss compared with copper intra-uterine contraceptive devices (IUCDs) that do not contain a progestogen, and carries less risk of pelvic inflammatory disease. The progestogen is released from the device for a period of 5 years. The device is also used to control menstrual bleeding in women with primary menorrhagia by preventing endometrial proliferation.
Efficacy of hormonal contraception
When taken according to the recommended schedule, the failure rate for the combined hormonal contraceptive is 0.2%. With the combined oral hormonal preparations, contraceptive protection is reduced if there is a delay of more than 24 h in taking the daily dose. In such circumstances the missed dose should be taken as soon as possible. If two doses are missed then additional contraceptive measures should be used for 7 days.
Failure of the progestogen-only oral contraceptive is age-related and is up to 5% in young women, falling with decreasing fertility to about 0.3% at the age of 40 years. With the oral progestogen-only contraceptive, other contraceptive precautions should be taken for 2 days if there is a delay of only 3 h or more after the normal time of taking the daily dose.
Emergency contraception
This can be carried out with the progestogen levonorgestrel, the progesterone receptor modulator ulipristal acetate, or a copper-containing IUCD. A single large dose of levonorgestrel is taken within 72 h after unprotected intercourse, and preferably within 12 h. Levonorgestrel inhibits ovulation, but only if taken before the LH surge. The treatment is successful in up to 99% of cases, but the efficacy is greatly reduced if used between 72 and 120 h after unprotected intercourse. Nausea is a frequent unwanted effect, occurring in up to 22% of women, and an anti-emetic (e.g. domperidone; Ch. 32) may be needed. Absorption takes 2 h and vomiting after this time will not affect the efficacy of treatment. A larger dose may be required if drugs that induce drug-metabolising enzymes in the liver are being taken. In the UK, levonorgestrel can be purchased without prescription by women over the age of 16 years.
The progesterone receptor modulator ulipristal acetate suppresses the mature follicle up to and including the time of the LH surge, so can be effective when taken up to 120 h after unprotected intercourse. Insertion of a copper IUCD up to 5 days after unprotected sexual intercourse is more effective as emergency contraception than levonorgestrel, but it is not known whether it is more effective than ulipristal acetate.
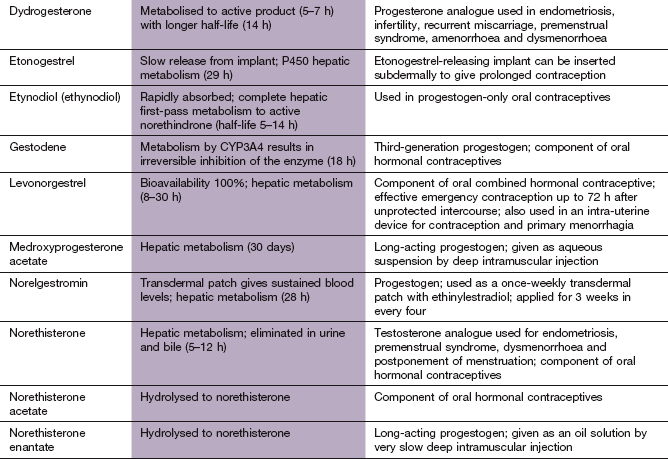
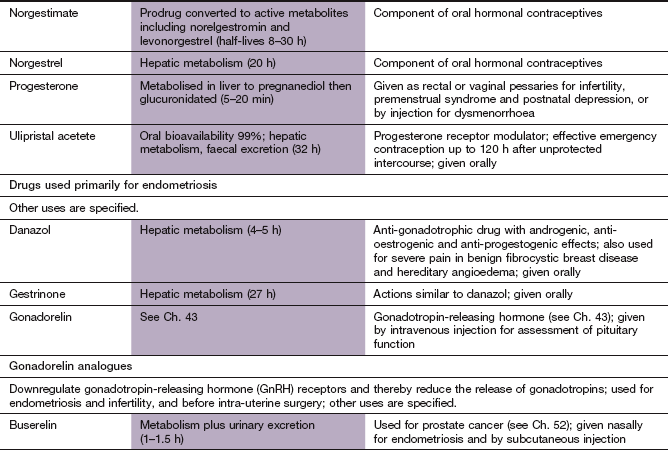
Pharmacokinetics of contraceptive steroids
The synthetic oestrogens, like the naturally occurring oestradiol-17β (oestradiol), and progestogens are highly lipid-soluble molecules that are rapidly and completely absorbed from the gut lumen after oral administration. Synthetic drugs are metabolised more slowly, including less first-pass metabolism, than the natural hormones oestradiol (half-life 1–2 h) and progesterone (half-life 5–20 min), so they have greater oral bioavailability and longer half-lives. For example, ethinylestradiol undergoes some first-pass metabolism (about 20%) but this is low compared with oestradiol (90–95%), and its half-life is longer (8–24 h). Some synthetic drugs are prodrugs that undergo first-pass metabolism to the active entity. Oestrogens and progestogens are eliminated by hepatic metabolism, often involving CYP3A4-mediated oxidation and/or conjugation with glucuronic acid and/or sulphate. The conjugates may undergo enterohepatic cycling. Enterohepatic cycling of ethinylestradiol is responsible for maintaining effective plasma concentrations with low-dose formulations. There is considerable inter-individual variation in plasma levels of oestrogens and progestogens after ingestion of the combined hormonal contraceptive.
The kinetics of oestrogens and progestogens can be affected by the administration of other drugs. Contraceptive failure may occur if there is concomitant treatment with drugs that induce liver cytochrome P450 enzymes (Table 2.7), such as anticonvulsants (e.g. barbiturates, carbamazepine or phenytoin), antiretroviral drugs (e.g. nelfinavir, nevirapine or ritonavir) or antibacterials (e.g. rifampicin and rifabutin) (Ch. 51). A higher dose of ethinylestradiol (using multiple tablets) should be used during and for 4 weeks after stopping these drugs. Alternatively, a form of contraception unaffected by enzyme-inducing drugs should be used (such as an IUCD or parenteral progestogen).
The pharmacokinetics of individual synthetic oestrogens and progestogens vary widely and details are given in the drug compendium at the end of this chapter.
Beneficial and unwanted effects of contraceptive steroids
 Cancer: there is a 40% reduction in the risk of ovarian cancer after 5 years of use and persisting for up to 15 years after stopping. Endometrial cancer is reduced by 50%, with a similar duration of protection.
Cancer: there is a 40% reduction in the risk of ovarian cancer after 5 years of use and persisting for up to 15 years after stopping. Endometrial cancer is reduced by 50%, with a similar duration of protection.
 Acne can be treated with combined oral hormonal contraceptives, since they reduce the concentration of free testosterone (Ch. 49). A combination of ethinylestradiol with cyproterone acetate, a weak progestogen with antiandrogenic activity (Ch. 46), is sometimes used for this purpose.
Acne can be treated with combined oral hormonal contraceptives, since they reduce the concentration of free testosterone (Ch. 49). A combination of ethinylestradiol with cyproterone acetate, a weak progestogen with antiandrogenic activity (Ch. 46), is sometimes used for this purpose.
 Dysfunctional uterine bleeding, for example menorrhagia, is reduced by the combined oral hormonal contraceptive or an intra-uterine progestogen-only device.
Dysfunctional uterine bleeding, for example menorrhagia, is reduced by the combined oral hormonal contraceptive or an intra-uterine progestogen-only device.
Unwanted effects
Both oestrogens and progestogens have a number of minor and major unwanted effects, but the incidence of the major effects, although important, is relatively low.
 Thromboembolism: the incidence of venous thromboembolic disease is increased in some subgroups of women taking the combined hormonal contraceptive. The mechanisms are complex but include procoagulant activity from increased production of clotting factors X and II and decreased production of anticoagulant anti-thrombin (Ch. 11). Fibrinolysis is impaired, while reduced prostacyclin generation enhances platelet aggregation (Ch. 11). The risk of thromboembolism increases with age, and is greater in women who smoke (because smoking increases the risk of thrombogenesis) or who are obese and in those with a thrombophilic tendency, such as deficiency of protein C or protein S or the presence of factor V Leiden. The baseline risk of venous thromboembolism in women of reproductive age not taking the combined oral hormonal contraceptive is about 5 per 100 000 per year. The risk in women taking second-generation preparations (containing levonorgestrel) is about 15 per 100 000 per year and in those taking third-generation preparations containing desogestrel or gestodene (and possibly drospirenone) is about 25 per 100 000 per year. It is important that these risks are put into context; for example the risk of venous thromboembolism in pregnancy is 60 per 100 000 pregnancies.
Thromboembolism: the incidence of venous thromboembolic disease is increased in some subgroups of women taking the combined hormonal contraceptive. The mechanisms are complex but include procoagulant activity from increased production of clotting factors X and II and decreased production of anticoagulant anti-thrombin (Ch. 11). Fibrinolysis is impaired, while reduced prostacyclin generation enhances platelet aggregation (Ch. 11). The risk of thromboembolism increases with age, and is greater in women who smoke (because smoking increases the risk of thrombogenesis) or who are obese and in those with a thrombophilic tendency, such as deficiency of protein C or protein S or the presence of factor V Leiden. The baseline risk of venous thromboembolism in women of reproductive age not taking the combined oral hormonal contraceptive is about 5 per 100 000 per year. The risk in women taking second-generation preparations (containing levonorgestrel) is about 15 per 100 000 per year and in those taking third-generation preparations containing desogestrel or gestodene (and possibly drospirenone) is about 25 per 100 000 per year. It is important that these risks are put into context; for example the risk of venous thromboembolism in pregnancy is 60 per 100 000 pregnancies.
 Ischaemic heart disease and ischaemic stroke: there is an increased risk of myocardial infarction and stroke in women taking the combined hormonal contraceptive who smoke or who are hypertensive, particularly in those over the age of 35 years. The added risk in those over 40 years is 20 per 100 000 for smokers and 29 per 100 000 for women with hypertension. It has been suggested that enhanced thrombogenesis rather than premature atherogenesis is responsible for the excess cardiovascular risk with the combined hormonal contraceptive. The lowest possible dose of oestrogen should be given to older women who use the combined hormonal contraceptive.
Ischaemic heart disease and ischaemic stroke: there is an increased risk of myocardial infarction and stroke in women taking the combined hormonal contraceptive who smoke or who are hypertensive, particularly in those over the age of 35 years. The added risk in those over 40 years is 20 per 100 000 for smokers and 29 per 100 000 for women with hypertension. It has been suggested that enhanced thrombogenesis rather than premature atherogenesis is responsible for the excess cardiovascular risk with the combined hormonal contraceptive. The lowest possible dose of oestrogen should be given to older women who use the combined hormonal contraceptive.
 Increase in blood pressure: a small increase in blood pressure, typically 5/3 mmHg, is common during use of the combined hormonal contraceptive, but not of progestogen-only contraceptives. A significant rise can occur in about 5% of women with previously normal blood pressure and in up to 15% of women with pre-existing hypertension. The mechanism is probably an increase in plasma renin substrate (Ch. 6) produced by oestrogen and, to a lesser extent, progestogen. Blood pressure may remain elevated for some months after the combined hormonal contraceptive has been stopped. Regular monitoring of blood pressure is advisable during use of the combined hormonal contraceptive, and it should be stopped if the blood pressure rises above 160 mmHg systolic or 95 mmHg diastolic.
Increase in blood pressure: a small increase in blood pressure, typically 5/3 mmHg, is common during use of the combined hormonal contraceptive, but not of progestogen-only contraceptives. A significant rise can occur in about 5% of women with previously normal blood pressure and in up to 15% of women with pre-existing hypertension. The mechanism is probably an increase in plasma renin substrate (Ch. 6) produced by oestrogen and, to a lesser extent, progestogen. Blood pressure may remain elevated for some months after the combined hormonal contraceptive has been stopped. Regular monitoring of blood pressure is advisable during use of the combined hormonal contraceptive, and it should be stopped if the blood pressure rises above 160 mmHg systolic or 95 mmHg diastolic.
 Cancer: there is a small excess risk of breast cancer, but it is uncertain whether this relates to earlier diagnosis. The rate of diagnosis remains higher for 10 years after the combined hormonal contraceptive is stopped. The incidence of cervical cancer is slightly increased by combined hormonal contraceptives after 5 years of use.
Cancer: there is a small excess risk of breast cancer, but it is uncertain whether this relates to earlier diagnosis. The rate of diagnosis remains higher for 10 years after the combined hormonal contraceptive is stopped. The incidence of cervical cancer is slightly increased by combined hormonal contraceptives after 5 years of use.
 Nausea, mastalgia, depression, headache, weight gain and provocation of migraine may be minimised by prescribing preparations with low oestrogen content, or by changing the progestogen to desogestrel, drospirenone or gestodene. Women who have migraine with aura are at increased risk of stroke if they take a combined hormonal contraceptive.
Nausea, mastalgia, depression, headache, weight gain and provocation of migraine may be minimised by prescribing preparations with low oestrogen content, or by changing the progestogen to desogestrel, drospirenone or gestodene. Women who have migraine with aura are at increased risk of stroke if they take a combined hormonal contraceptive.
 Breakthrough bleeding occurs frequently in some women, whereas in others withdrawal bleeding fails to occur. Gestodene-containing pills or triphasic preparations probably give the best cycle control. Amenorrhoea after stopping the combined hormonal contraceptive can last beyond a few months in about 5% of women, and a small number can experience amenorrhoea for more than a year. A history of irregular periods before taking the combined hormonal contraceptive increases the chance of prolonged amenorrhoea.
Breakthrough bleeding occurs frequently in some women, whereas in others withdrawal bleeding fails to occur. Gestodene-containing pills or triphasic preparations probably give the best cycle control. Amenorrhoea after stopping the combined hormonal contraceptive can last beyond a few months in about 5% of women, and a small number can experience amenorrhoea for more than a year. A history of irregular periods before taking the combined hormonal contraceptive increases the chance of prolonged amenorrhoea.
 Metabolic effects: oestrogens alone increase protective plasma high-density lipoprotein (HDL) cholesterol, decrease low-density lipoprotein (LDL) cholesterol and increase plasma triglycerides (see also Ch. 48). When used in combination with the second-generation progestogens, HDL cholesterol is reduced. Oestrogens increase vascular prostacyclin and nitric oxide synthesis, inhibit platelet adhesion and suppress smooth muscle cell proliferation. Some progestogens such as norethisterone and medroxyprogesterone acetate may oppose the beneficial effects of oestrogens on the arterial wall. The third-generation combined hormonal contraceptives containing gestodene and desogestrel increase plasma triglycerides but, unlike the progestogens in the second-generation pills, they increase HDL cholesterol. The clinical relevance of these small changes is uncertain.
Metabolic effects: oestrogens alone increase protective plasma high-density lipoprotein (HDL) cholesterol, decrease low-density lipoprotein (LDL) cholesterol and increase plasma triglycerides (see also Ch. 48). When used in combination with the second-generation progestogens, HDL cholesterol is reduced. Oestrogens increase vascular prostacyclin and nitric oxide synthesis, inhibit platelet adhesion and suppress smooth muscle cell proliferation. Some progestogens such as norethisterone and medroxyprogesterone acetate may oppose the beneficial effects of oestrogens on the arterial wall. The third-generation combined hormonal contraceptives containing gestodene and desogestrel increase plasma triglycerides but, unlike the progestogens in the second-generation pills, they increase HDL cholesterol. The clinical relevance of these small changes is uncertain.
 Increased skin pigmentation can occur in some women who take oestrogens. The androgenic progestogens can sometimes cause or aggravate hirsutism and acne or produce weight gain. In women with hyperandrogenaemia (such as occurs with polycystic ovary syndrome) a third-generation combined hormonal contraceptive would be preferred, as gestodene and desogestrel have little androgenic activity.
Increased skin pigmentation can occur in some women who take oestrogens. The androgenic progestogens can sometimes cause or aggravate hirsutism and acne or produce weight gain. In women with hyperandrogenaemia (such as occurs with polycystic ovary syndrome) a third-generation combined hormonal contraceptive would be preferred, as gestodene and desogestrel have little androgenic activity.
 Effects on the liver are occasionally seen. Cholestatic jaundice can be produced by progestogens, and oestrogens increase the risk of gallstones.
Effects on the liver are occasionally seen. Cholestatic jaundice can be produced by progestogens, and oestrogens increase the risk of gallstones.
 Drug interactions: drugs that increase the metabolism of oestrogen may cause a reduction in the efficacy of the combined hormonal contraceptive, which may result in breakthrough bleeding and contraceptive failure (see above).
Drug interactions: drugs that increase the metabolism of oestrogen may cause a reduction in the efficacy of the combined hormonal contraceptive, which may result in breakthrough bleeding and contraceptive failure (see above).
Non-contraceptive uses of steroidal contraceptives
The combined hormonal contraceptive can be used:
 to reduce excessive blood loss from menorrhagia,
to reduce excessive blood loss from menorrhagia,
 to reduce the pain of dysmenorrhoea,
to reduce the pain of dysmenorrhoea,
Menorrhagia
Excessive menstrual blood loss is a common gynaecological problem. Menstrual loss can be reduced to a variable extent by non-steroidal anti-inflammatory drugs (NSAIDs; Ch. 29), and numerous different NSAIDs have been used. They are taken only during the time of menstruation. The combined hormonal contraceptives and the progestogen-only contraceptives can also reduce excessive menstrual loss. To be useful the progestogen-only contraceptive has to be taken for 3 weeks at a fairly high dose. A more effective way of giving the progestogen is from an intra-uterine progestogen system (IUS), which reduces blood loss by up to 90%.
The antifibrinolytic agent tranexamic acid (Ch. 11) can also reduce menstrual blood loss by up to 50%. Its effect is rapid in onset and therapy is only required during the time of menstruation.
Dysmenorrhoea
The cause of primary dysmenorrhoea (pain associated with menstruation) is unknown. Many explanations have been proposed, including uterine hyperactivity, excessive prostaglandin or leukotriene generation and excessive production of vasopressin. Various NSAIDs (Ch. 29) have been used for the relief of dysmenorrhoea, with approximately 70% of women being relieved of their symptoms. There are differences in efficacy among the NSAIDs that are poorly understood and do not seem to be simply related to their analgesic or anti-inflammatory activity. NSAIDs with a licence for this indication in the UK include ibuprofen, mefenamic acid and naproxen.
The combined hormonal contraceptive and the progestogen-only contraceptive are effective in reducing symptoms of dysmenorrhoea.
Premenstrual disorders
Many women experience a variety of symptoms precipitated by ovulation that may continue up to the end of menstruation. The term premenstrual syndrome is used to describe the symptom complex if a woman has at least one week free of symptoms every cycle. Physical symptoms include joint and muscle pains, breast tenderness, abdominal bloating, headaches, weight gain and oedema of the hands or feet. These are often accompanied by increased appetite, fatigue, mood swings, irritability and sleep disturbance. Second-generation combined hormonal contraceptives can produce similar symptoms to premenstrual syndrome.
Treatment is varied, and includes cognitive behavioural therapy and aerobic exercise. If symptoms are more severe, the diuretic spironolactone (Ch. 14) can reduce abdominal bloating, breast discomfort and mood disturbance. Selective serotonin reuptake inhibitors, such as citalopram (Ch. 22), are effective when used for 2 weeks prior to menstruation at lower doses than required to treat depression. A combined hormonal contraceptive containing drospirenone is helpful if fertility is not an issue, or ovulation can be suppressed with a gonadorelin agonist analogue such as goserelin (Ch. 43) or use of the ‘impeded’ androgen danazol (Ch. 46) in the luteal phase.
Endometriosis
Endometriosis is the presence and proliferation of endometrial tissue outside the uterine cavity. It may arise from retrograde menstrual flow through the fallopian tubes. The main consequences are pelvic pain, dysmenorrhoea, dyspareunia and infertility. Treatment is either medical or surgical.
Medical treatment can be given to suppress ovarian activity and create a hypo-oestrogenic anovulatory state, but does not restore fertility. Symptoms often improve in pregnancy, and the combined hormonal contraceptive or a progestogen-only contraceptive are often effective treatments. Alternative strategies include induction of a pseudo-postmenopausal state with the use of danazol (Ch. 46) or gonadotropin-releasing hormone (GnRH) analogues (Ch. 43). Treatment is usually necessary for at least 6 months, but up to 50% of women have recurrence of painful symptoms in the 2 years after it is stopped.
If fertility is the major problem, then treatment involves surgery or in vitro fertilisation techniques (Ch. 43).
Hormone-replacement therapy
The menopausal transition from regular periods to amenorrhoea begins at a median age of 51 years and takes place over about 4 years. It arises because there is a natural depletion of ovarian follicles and as a result the plasma oestrogen concentration falls, with a consequent rise in plasma FSH. After the menopause, the ovaries do not produce oestrogen or progesterone, but continue to produce testosterone. Some oestrogen is still produced by conversion of adrenal corticosteroids to oestradiol in peripheral adipose tissue. The consequences of oestrogen deficiency during and after the menopause include the following.
 Symptoms such as vasomotor instability (hot flushes and night sweats), and altered sexual and urinary function. Vasomotor instability results from resetting of the hypothalamic temperature set-point so that it perceives that the body is warmer than it is. Vasodilation and sweating represent an attempt to disperse heat. The mechanism is uncertain but may be due to either reduced oestrogen or increased FSH leading to a reduction in noradrenergic or serotonergic neurotransmission in the hypothalamus. Loss of connective tissue in the vagina and trigone of the bladder, and a less acidic vaginal pH underlie many of the other problems. These include vaginal dryness, discomfort and itching, dyspareunia, and urinary urgency, frequency and incontinence. Breast atrophy and thinning of the skin also occur. Other postmenopausal symptoms such as irritability and depression are less clearly related to oestrogen deficiency.
Symptoms such as vasomotor instability (hot flushes and night sweats), and altered sexual and urinary function. Vasomotor instability results from resetting of the hypothalamic temperature set-point so that it perceives that the body is warmer than it is. Vasodilation and sweating represent an attempt to disperse heat. The mechanism is uncertain but may be due to either reduced oestrogen or increased FSH leading to a reduction in noradrenergic or serotonergic neurotransmission in the hypothalamus. Loss of connective tissue in the vagina and trigone of the bladder, and a less acidic vaginal pH underlie many of the other problems. These include vaginal dryness, discomfort and itching, dyspareunia, and urinary urgency, frequency and incontinence. Breast atrophy and thinning of the skin also occur. Other postmenopausal symptoms such as irritability and depression are less clearly related to oestrogen deficiency.
 Bone loss leading to osteoporosis (Ch. 42) and an increased susceptibility to fragility fracture occur after the menopause. The ERβ receptor is present in higher concentrations in developing cancellous bone (such as vertebrae), and the ERα receptor in developing cortical bone (such as the hip). Oestrogen deficiency increases bone turnover, with bone resorption increasing more than formation.
Bone loss leading to osteoporosis (Ch. 42) and an increased susceptibility to fragility fracture occur after the menopause. The ERβ receptor is present in higher concentrations in developing cancellous bone (such as vertebrae), and the ERα receptor in developing cortical bone (such as the hip). Oestrogen deficiency increases bone turnover, with bone resorption increasing more than formation.
 Cardiovascular disease and cerebrovascular disease are more common. The cause is uncertain. Unfavourable changes in lipids may be part of the explanation, due to a reduced HDL2 cholesterol subfraction and increased LDL cholesterol (see Ch. 48). However, an independent effect of oestrogen in reducing plasma fibrinogen (a factor in thrombogenesis) may be more important. Oestrogen receptors are found on the cells of the arterial wall, and stimulation decreases arterial resistance and increases vessel compliance, which may also be relevant.
Cardiovascular disease and cerebrovascular disease are more common. The cause is uncertain. Unfavourable changes in lipids may be part of the explanation, due to a reduced HDL2 cholesterol subfraction and increased LDL cholesterol (see Ch. 48). However, an independent effect of oestrogen in reducing plasma fibrinogen (a factor in thrombogenesis) may be more important. Oestrogen receptors are found on the cells of the arterial wall, and stimulation decreases arterial resistance and increases vessel compliance, which may also be relevant.
Treatment with oestrogens during the peri- and postmenopausal period is often advocated to try to reverse the effects of oestrogen deficiency, but recent evidence of both lack of efficacy and potential harm has limited their use (see benefits and risks below).
Oral hormone-replacement therapy and other drugs used for postmenopausal conditions
Oral oestrogens and progestogens
For hormone-replacement therapy (HRT), oestrogens are given at much lower doses than are used for contraception. However, if oestrogen is given alone for more than a few weeks to a woman who has a uterus then cystic hyperplasia of the endometrium can occur. Progestogen is given concurrently to avoid this, and is used for 12 days each calendar month or continuously if withdrawal bleeding is to be avoided. Oestrogen can be used alone if the woman has had a hysterectomy.
The majority of oral HRT preparations contain the natural estradiol as the oestrogen, although preparations with conjugated equine oestrogens are also available. Synthetic progestogens are used: dydrogesterone, medroxyprogesterone, norethisterone, levonorgestrel or drospirenone.
Oral oestrogen replacement will reduce the symptoms of postmenopausal oestrogen deficiency, although relief may take up to 3 months. Treatment for symptom relief probably should be given for at least 6 months to perimenopausal women, after which withdrawal can be attempted to see whether symptoms have resolved spontaneously.
Tibolone
Tibolone is a synthetic compound with combined weak oestrogenic, progestogenic and androgenic properties. Its effects are predominantly oestrogenic, although in breast tissue it inhibits the enzyme responsible for activation of its metabolites, giving a low incidence of breast tenderness. In the endometrium it activates progesterone and androgen receptors, and the effects are mainly progestogenic, without stimulation of the endometrium or producing bleeding. Tibolone reduces postmenopausal symptoms and prevents postmenopausal bone loss. Vaginal bleeding can occur in women who still produce some endogenous oestrogen, and therefore tibolone is not usually given to women who are within 12 months of their last period.
Raloxifene
Raloxifene is a selective oestrogen receptor modulator which has oestrogenic effects on bone but anti-oestrogenic actions on breast and uterine receptors. It increases bone mineral density in postmenopausal osteoporosis, but does not treat menopausal symptoms. More details on raloxifene and osteoporosis are given in Chapter 42.
Vaginal oestrogen
Oestrogen cream (usually estradiol) or pessaries can be used to treat vaginal atrophy and dyspareunia and can relieve perimenopausal urinary symptoms such as frequency and dysuria. Considerable systemic absorption occurs with some formulations, and an oral progestogen may be needed to prevent endometrial hyperplasia. Creams or pessaries are used daily for 2–3 weeks initially and then applied twice weekly for as long as required.
Subcutaneous oestrogen implants
Estradiol can be implanted surgically as pellets that release drug for up to 6 months. The major use for this option is when tolerance of oral oestrogen is poor, perhaps because of nausea. Oral progestogen must also be taken for 10–12 days each month if the woman has a uterus, and continued for up to 2 years after stopping oestrogen, to prevent vaginal bleeding from persistently high oestrogen levels.
Transdermal oestrogen with progestogen
A variety of transdermal patches that deliver sex steroids are available. In some preparations, oestrogen alone is delivered by patches applied twice weekly for 2 weeks, followed by patches delivering oestrogen plus progestogen for 2 weeks. In other regimens, progestogen is taken orally for at least 12 days of the cycle while continuing with the patch-delivered oestrogen. Patches delivering continuous oestrogen plus progestogen (levonorgestrel or norethisterone) are also available. A lower dose of progestogen can be used because the transdermal route avoids first-pass metabolism, and this might reduce unwanted effects. Estradiol gels applied twice daily are also available and require co-administration of oral progestogen for 12 days per month in women with a uterus. It is recommended that patches are applied below the waistline, and not close to the breasts.
Benefits and risks of hormone-replacement therapy
The benefits and risks of oestrogen-based HRT are highly individual for the patient. For most women it is recommended that HRT is reserved for short-term alleviation of menopausal symptoms. Any treatment should be reviewed at least annually. Tibolone (see above) or alternative approaches to the treatment of menopausal symptoms (see below) should be considered. Atrophic vaginitis may respond to a short course of topical oestrogen.
HRT reduces the risk of vertebral and non-vertebral osteoporotic fractures. However, because of the potential risks of treatment, HRT is not considered to be first-line treatment except for women with early natural or surgical menopause before the age of 45 years, in whom it is not recommended that treatment should continue beyond the age of 50 years.
Unwanted effects of hormone-replacement therapy
 Breakthrough bleeding can be troublesome, and regular withdrawal bleeds during the cycle are common unless continuous progestogen is used. These may be preceded by symptoms of premenstrual tension.
Breakthrough bleeding can be troublesome, and regular withdrawal bleeds during the cycle are common unless continuous progestogen is used. These may be preceded by symptoms of premenstrual tension.
 Breast pain and abdominal or leg cramps.
Breast pain and abdominal or leg cramps.
 Depression, irritability, loss of energy and poor concentration due to progestogen.
Depression, irritability, loss of energy and poor concentration due to progestogen.
 Transdermal delivery can cause contact sensitisation.
Transdermal delivery can cause contact sensitisation.
 Increased risk of venous thromboembolism, especially in the first year and in those with other risk factors (obesity, smoking, immobility, previous thromboembolic disease). The risk after 5 years of use is increased by about 40% for combined HRT (added risk is 4 cases per 1000 for combined HRT, and 1 case per 1000 for oestrogen-only HRT over 5 years if aged 50–59 years; the excess risk is more than doubled between 60 and 69 years). Transdermal oestrogen replacement may not increase the risk of venous thromboembolism.
Increased risk of venous thromboembolism, especially in the first year and in those with other risk factors (obesity, smoking, immobility, previous thromboembolic disease). The risk after 5 years of use is increased by about 40% for combined HRT (added risk is 4 cases per 1000 for combined HRT, and 1 case per 1000 for oestrogen-only HRT over 5 years if aged 50–59 years; the excess risk is more than doubled between 60 and 69 years). Transdermal oestrogen replacement may not increase the risk of venous thromboembolism.
 Increased risk of stroke (excess risk is 1 case per 1000 for combined HRT and 2 cases per 1000 for oestrogen-only HRT over 5 years if aged 50–59 years; this excess risk is tripled between 60 and 69 years).
Increased risk of stroke (excess risk is 1 case per 1000 for combined HRT and 2 cases per 1000 for oestrogen-only HRT over 5 years if aged 50–59 years; this excess risk is tripled between 60 and 69 years).
 HRT does not prevent coronary heart disease, and may increase the risk in the first year of treatment.
HRT does not prevent coronary heart disease, and may increase the risk in the first year of treatment.
 Increased risk of breast cancer within 1–2 years of starting use, increasing further with duration of use. The excess risk is lost 5 years after stopping HRT. Taking combined HRT for 10 years leads to a 40% increase in the risk of developing breast cancer in women aged 50–64 years (excess risk is 6 cases per 1000). Oestrogen-only HRT carries about one-quarter of this excess risk.
Increased risk of breast cancer within 1–2 years of starting use, increasing further with duration of use. The excess risk is lost 5 years after stopping HRT. Taking combined HRT for 10 years leads to a 40% increase in the risk of developing breast cancer in women aged 50–64 years (excess risk is 6 cases per 1000). Oestrogen-only HRT carries about one-quarter of this excess risk.
 The risk of endometrial cancer is increased by oestrogen-only HRT, which should be avoided in women who have a uterus.
The risk of endometrial cancer is increased by oestrogen-only HRT, which should be avoided in women who have a uterus.
 The risk of cholecystitis is increased by oral but not transdermal oestrogen.
The risk of cholecystitis is increased by oral but not transdermal oestrogen.
Alternative treatments for menopausal symptoms
Oestrogens are by far the most effective treatment for menopausal symptoms. Vasomotor symptoms may be alleviated by the use of high doses of progestogens but unwanted effects are common. There is limited evidence for the use of antidepressants that modulate monoaminergic neurotransmission, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) (Ch. 22). The anticonvulsant gabapentin (Ch. 23) is effective for treating hot flushes.
The onset and induction of labour
The aetiology of the induction of labour is still uncertain (Fig. 45.3). The actual onset may be multifactorial in nature and it is probable that prostaglandins, oxytocin, progesterone, oestrogen and corticosteroids are among the agents involved. Lack of knowledge about the mechanisms that underpin the onset of labour is directly reflected in a poor ability to prevent preterm labour, where at best parturition can be delayed for only short periods of time (see below).
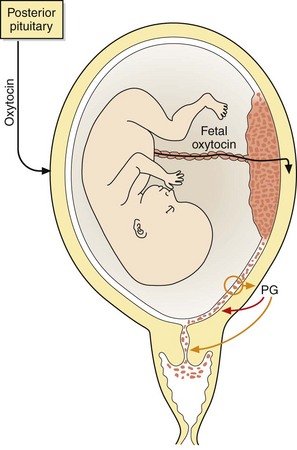
Fig. 45.3 Induction of labour.
The mechanisms involved in the onset of labour in humans are uncertain but likely to be multifactorial. Prostaglandins (PG) are synthesised by the amnion and decidua and they stimulate the uterus and soften the cervix. Fetal and maternal oxytocin and prostaglandins may be involved in the processes of labour; their role in the initiation of labour is uncertain.
Corticotropin-releasing hormone
The critical factor in the timing of birth in humans is development of the placenta, and particularly expression of the gene for corticotropin-releasing hormone (CRH; also known as corticotropin-releasing factor) by the placenta. Placental CRH production increases dramatically at the end of pregnancy. Prior to this, its production is suppressed by progesterone, but it is stimulated by a rise in glucocorticoid production and catecholamine release prior to parturition. The increase in CRH drives the fetal hypothalamo–pituitary–adrenal axis to produce corticosteroids and dehydroepiandrosterone (Ch. 43). In the fetus, CRH and cortisol stimulate the fetal lung to produce surfactant protein A (Ch. 13), which enters amniotic fluid and then the amnion, where it stimulates synthesis of prostaglandin E2 (PGE2). In the mother, the formation of myometrial PGF2α is also increased.
Prostaglandins
PGF2α and PGE2 are synthesised by the cells of the amnion and decidua and have many actions that could contribute to labour. Uterine contractile sensitivity to prostaglandins is approximately 10-fold higher at term than in earlier pregnancy. The contractility of the uterus during labour commences at the utero-tubular junction and progresses through the body of the uterus to the cervix, thus promoting efficient labour. This type of synchronous contractile pattern, which does not occur in early pregnancy, is caused by prostaglandins and oestrogens promoting the synthesis of ‘contraction-associated proteins’ and increasing connectivity between myometrial cells. Gap junctions are specialised connections between the smooth muscle cells that allow excitatory impulses to pass between cells. The type of uterine contractions that result in efficient progress of labour can only occur in uterine muscle cells that are rich in gap junctions. The progesterone-dominated uterus has few gap junctions. Prostaglandins also increase the release of Ca2+ from intracellular stores in myometrial cells, which promotes muscle contraction.
PGE2 softens the cervix, an essential prerequisite for the smooth passage of labour. Prostaglandins also increase the synthesis of oxytocin from the posterior pituitary.
Oxytocin
Oxytocin is a peptide produced by the posterior pituitary (Ch. 43). There is a marked increase in the expression of uterine oxytocin receptors from about 35 weeks of pregnancy onwards, so that oxytocin has a marked uterotonic action at term but is much less effective earlier in pregnancy. Oxytocin acts synergistically with prostaglandins to release Ca2+ from intracellular stores in the myometrial cells and promote muscle contraction. The oxytocin concentration in the maternal circulation does not increase until the second stage of labour.
Sex steroid hormones
Oestrogens and progesterone both increase during pregnancy. Overall, the actions of oestradiol promote uterine contractility while progesterone decreases contractility. Production of dehydroepiandrosterone is also increased just before parturition.
 Progesterone: decreases gap junctions, diminishes uterine pacemaker activity and decreases the sensitivity of the uterus to oxytocin and prostaglandins. At the onset of labour there is reduced responsiveness of progesterone receptors which blocks the cellular action of the hormone.
Progesterone: decreases gap junctions, diminishes uterine pacemaker activity and decreases the sensitivity of the uterus to oxytocin and prostaglandins. At the onset of labour there is reduced responsiveness of progesterone receptors which blocks the cellular action of the hormone.
 Oestradiol: increases the number of uterine oxytocin receptors and increases oxytocin release from the posterior pituitary. It increases gap junctions, and fundal dominance of uterine contractility is increased by an effect on the functional pacemaker at the utero-tubular junction. Oestradiol increases the synthesis of prostaglandins and increases the sensitivity of the uterus to their effects and has a softening effect on the cervix.
Oestradiol: increases the number of uterine oxytocin receptors and increases oxytocin release from the posterior pituitary. It increases gap junctions, and fundal dominance of uterine contractility is increased by an effect on the functional pacemaker at the utero-tubular junction. Oestradiol increases the synthesis of prostaglandins and increases the sensitivity of the uterus to their effects and has a softening effect on the cervix.
 Dehydroepiandrosterone: this has high activity at oestrogen ERβ receptors that contributes to fetal lung maturation. It also enhances the production of oestrogen by the placenta, which may be important in the timing of the onset of labour.
Dehydroepiandrosterone: this has high activity at oestrogen ERβ receptors that contributes to fetal lung maturation. It also enhances the production of oestrogen by the placenta, which may be important in the timing of the onset of labour.
Drugs used for inducing labour
Oxytocin and prostaglandins are the only drugs currently used to induce labour.
Oxytocin
Oxytocin is given by slow intravenous infusion for the induction of labour and to augment contractions in inadequate labour. The concentration given depends upon the response: the aim is to produce regular coordinated contractions at intervals of approximately 1.5–2 min with complete relaxation between contractions. Oxytocin is an effective uterine stimulant in women at term, and labour will usually proceed well if the cervix is partially dilated and softened prior to its use. Inappropriately high concentrations of oxytocin can cause uterine hypertonus, in which the uterus does not relax between contractions, and fetal distress can occur. As labour progresses and the woman's ‘endogenous’ induction mechanisms come into play, the concentration of oxytocin may need to be reduced. Following delivery, oxytocin can also be useful to reduce postpartum haemorrhage (see below). Oxytocin, unlike prostaglandins, does not soften the cervix and is now often used after intravaginal prostaglandin (usually dinoprostone) has been given for this purpose (see below). Oxytocin in high doses has a weak antidiuretic activity as it is related to vasopressin and large doses can cause fluid retention (Ch. 43).
Dinoprostone
Dinoprostone (the name for exogenous PGE2) causes contractions of both the non-pregnant and the pregnant uterus. The sensitivity of the uterus to prostaglandins is higher than to oxytocin prior to term. Like oxytocin, correct doses of prostaglandins can produce contractions that are indistinguishable from spontaneous labour. Prostaglandins have the added advantage of softening (‘ripening’) the cervix, so they can be used for induction of labour before term. Dinoprostone is given as vaginal tablets, pessaries or gels for induction of labour or for priming of the uterus prior to rupture of membranes and induction by oxytocin. In some women dinoprostone will result only in ripening of the cervix, whereas others will go into labour. Dinoprostone is rarely used intravenously for the induction of labour, as it produces more unwanted effects.
Induction of abortion
Prostaglandins are widely used for the induction of abortion. In the second trimester their use results in fewer complications than surgical abortion. Gemeprost (a PGE1 analogue), given as an intravaginal pessary, is used for the medical induction of first- or second-trimester therapeutic abortion or management of intra-uterine death. Misoprostol is an alternative that can be given orally or vaginally. Both drugs produce prolonged uterine contraction. Mifepristone pretreatment (see below) is used before vaginal administration of a prostaglandin.
Gemeprost is also given as a pessary to ripen and soften the cervix prior to early surgical abortion.
Mifepristone
Mechanism of action and uses: Mifepristone is a potent progesterone receptor antagonist. It is given orally and sensitises the uterus to prostaglandin-induced contractions and softens the cervix. For medical termination of pregnancy up to 24 weeks' gestation or following spontaneous fetal death, mifepristone is given as a single oral dose followed 36 h later by either oral gemeprost, or oral or vaginal misoprostol (Ch. 33). It can also be given alone to soften the cervix 36 h before surgical termination of early pregnancy.
Postpartum haemorrhage
Bleeding can arise after incomplete abortion or after a normal delivery. In the latter situation, preventative treatment is routinely given to avoid excessive blood loss.
Ergometrine maleate
Ergometrine causes hypertonic contractions of the uterus and is therefore not used for induction of labour as it would result in fetal distress and poor progress in labour. After placental separation, uterine hypertonus produced by ergometrine squeezes the uterine blood vessels and reduces blood loss. It also causes vasoconstriction by α-adrenoceptor stimulation (see ergotamine Ch. 26), which further limits haemorrhage.
Management of postpartum haemorrhage
To minimise bleeding after delivery, ergometrine should be given together with oxytocin by intramuscular injection on delivery of the anterior shoulder. Following delivery of the baby, postpartum haemorrhage can also be reduced by increasing the concentrations of intravenous oxytocin being administered. This causes hypertonic contraction of the uterus and compresses intra-uterine blood vessels. If bleeding continues, the prostaglandin carboprost (15-methyl-PGF2α, a compound related to dinoprostone) is given by intramuscular injection.
Myometrial relaxants (tocolytics) and preterm labour
Preterm birth is a delivery that occurs before 37 weeks of gestation, and affects more than 10% of pregnancies. It is possible that preterm labour has multifactorial origins, such as myometrial and fetal membrane overdistension (as may occur with multiple fetuses), early fetal endocrine activation, decidual haemorrhage and intra-uterine infection or inflammation.
Prematurity is the largest cause of neonatal morbidity and mortality, but relatively poor pharmacological tools are available currently to prevent it. Therapeutic strategies have concentrated on inhibition of myometrial contractions (tocolysis) between 24 and 33 weeks gestation. Tocolytics have not been shown to improve fetal morbidity or mortality, but they provide a limited time for treatment with a corticosteroid to enhance lung maturation (Ch. 13), or for transfer of the mother to a specialist unit. Prophylactic treatment with antibacterials may improve outcome in particular at-risk groups but has not been widely adopted.
Atosiban
Mechanism of action: Atosiban is a peptide analogue of oxytocin that is an antagonist at oxytocin receptors in the decidua and myometrium, reducing the release of intracellular Ca2+.
Beta2-adrenoceptor agonists
β2-Adrenoceptor agonists inhibit uterine contractility by increasing the intracellular concentration of cAMP. Salbutamol and terbutaline are given intravenously or orally for up to 48 h following the start of preterm labour, after which the risks to the mother increase with no benefit to the fetus. Unwanted effects include nausea, vomiting, flushing and maternal and fetal tachycardia with hypotension (see also Ch. 12).
Calcium channel blockers
Nifedipine (Ch. 5) is used orally and is as effective as other tocolytics, with fewer unwanted effects than β2-adrenoceptor agonists. The use of nifedipine may improve fetal outcome.
Other agents for preterm labour
Magnesium sulphate has been widely used in the USA for treating women in preterm labour. Recent evidence indicates that it may be no better than placebo, and may be associated with worse fetal outcomes. Intravenous or transdermal glyceryl trinitrate (Ch. 5) may be effective through nitric oxide generation in smooth muscle, but is not widely used.
The NSAID indometacin (Ch. 29) can be successful for delaying delivery, but there are concerns about transient neonatal renal impairment and premature closure of the ductus arteriosus.
True/false questions
1. Oestrogen has a negative feedback effect on luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion from the anterior pituitary throughout the follicular phase of the menstrual cycle.
2. In the luteal phase, the elevated level of progesterone is controlled by gonadotropins.
3. Progesterone causes cervical mucus to be viscous and hostile to the passage of sperm.
4. The oral progestogen-only contraceptive reliably inhibits ovulation.
5. Both oestrogen and progesterone inhibit the motility of the fallopian tube.
6. The functioning corpus luteum maintains pregnancy for the first 6–8 weeks after implantation.
7. Progestogens used in combined hormonal contraceptives do not differ in their androgenic activity.
8. Biphasic and triphasic formulations of combined hormonal contraceptives result in lower overall dosages of oestrogen and progestogen than monophasic formulations.
9. Effective protection is lost if there is a delay of more than 3 h in taking the daily oral dose of an oral combined hormonal contraceptive.
10. Emergency contraception with ulipristal acetate is effective taken up to 120 h after unprotected intercourse.
11. An etonogestrel implant beneath the skin of the upper arm provides effective contraception for 5 years.
12. Antiepileptic drugs such as carbamazepine can reduce the plasma concentrations of oestrogens and progestogens.
13. Mortality from venous thromboembolism is increased in women using the oral combined hormonal contraceptive who smoke, particularly those over the age of 35 years.
14. The combined hormonal contraceptive significantly increases blood pressure in most women.
15. Oestrogen used on its own as hormone-replacement therapy (HRT) may cause endometrial hyperplasia.
16. Postmenopausal women taking continuous HRT with both oestrogen and progestogens do not experience breakthrough bleeding.
17. Oestrogens and progestogens can be given transdermally.
18. Raloxifene blocks oestrogen receptors in bone.
19. Tibolone reduces bone loss in postmenopausal women.
20. Oxytocin is preferred to prostaglandins for the induction of labour at 34 weeks of gestation.
21. Progesterone increases the number of gap junctions in the uterus.
22. Ergometrine can be used for the induction of labour.
23. Atosiban is a tocolytic drug that acts by blocking oxytocin receptors.
24. Non-steroidal anti-inflammatory drugs (NSAIDs) are used in treating dysmenorrhoea.
One-best-answer (OBA) questions
1. Identify the incorrect statement below concerning drugs used during labour and abortion.
A Mifepristone is a progesterone receptor antagonist used to induce abortion.
B Prostaglandin E2 (PGE2) is preferred to oxytocin for induction of labour at 35 weeks of gestation.
C Oxytocin is less likely than prostaglandins to cause uterine hypertonus.
D β2-Adrenoceptor agonists do not reduce mortality in children born preterm.
E Ergometrine reduces postpartum haemorrhage by constricting uterine blood vessels.
2. Identify the most accurate statement below concerning the contraceptive options for a 35-year-old woman who smokes 40 cigarettes a day, but who, despite treatment, has not been able to stop smoking.
A The oral combined hormonal contraceptive would be suitable for her contraception.
B The oral combined hormonal contraceptive would increase her risk of endometrial cancer.
C The oral combined hormonal contraceptive would have a lower failure rate than an intra-uterine contraceptive device (IUCD).
D The oral progestogen-only contraceptive would provide adequate contraception without increasing the risk of venous thromboembolism.
E An intramuscular injection of medroxyprogesterone acetate would give contraceptive protection for at least 6 months.
1. False. The negative feedback in the early part of the follicular phase switches to positive feedback at an oestradiol level of approximately 200 pg⋅mL−1, resulting in the mid-cycle surge in LH and FSH.
2. True. The LH levels fall precipitously after the mid-cycle surge, but they are high enough to support the secretion of progesterone in the luteal phase.
3. True. The effect on cervical mucus is an important action of the oral progestogen-only contraceptive.
4. False. Ovulation occurs in up to 50% of women with the oral progestogen-only contraceptive, as other effects are responsible for its contraceptive action. Ovulation is reliably inhibited in women using parenteral progestogens.
5. False. Progesterone inhibits fallopian tube motility, and oestrogens enhance it. An imbalance may alter oocyte transport and the probability of fertilisation and implantation.
6. True. After 6–8 weeks of pregnancy maintained by the corpus luteum, the placenta takes over production of sex steroids under the influence of HCG.
7. False. Progestogens in second-generation combined hormonal contraceptives (such as levonorgestrel and norethisterone) have variable androgenic activity, but gestodene and desogestrel used in third-generation combined contraceptives have little or no androgenic activity.
8. False. Biphasic and triphasic formulations mimic more closely the steroidal changes in the menstrual cycle, but they do not reduce the overall administered load of sex steroids.
9. False. Protection is reduced if there is a delay of more than 12 h in taking a daily dose of the combined hormonal contraceptive, but this can occur with a delay of only 3 h in taking oral progesterone-only contraceptives.
10. True. The progesterone receptor modulator ulipristal acetate suppresses the follicle until the time of the LH surge and is effective up to 120 h after unprotected intercourse.
11. False. Etonogestrel implants must be replaced every 3 years.
12. True. By inducing liver microsomal enzymes, the effective concentrations of oestrogens and progestogens may be reduced as their metabolism is enhanced.
13. True. The excess risk of thromboembolic disease in women taking the combined hormonal contraceptive is significantly greater in smokers over the age of 35 years.
14. False. A small increase in blood pressure is commonly seen with the combined contraceptive, but a significant rise occurs in only 5% of previously normotensive women.
15. True. The risk of endometrial hyperplasia with oestrogen is reduced by giving progestogens concurrently; oestrogens can be used alone in women who have had a hysterectomy.
16. False. Breakthrough bleeding frequently occurs, particularly in the first 6 months of treatment.
17. True. Both oestrogens and progestogens undergo first-pass metabolism and this can be avoided by transdermal absorption from patches.
18. False. Raloxifene is a selective oestrogen receptor modulator; it stimulates oestrogen receptors in bone but not in breast or uterine tissue.
19. True. Tibolone has weak oestrogenic and progestogenic activity and reduces bone loss.
20. False. Oxytocin is less effective in earlier pregnancy compared with full term. An intravaginal pessary of prostaglandin would increase uterine contractility and also soften the cervix.
21. False. Oestrogens increase uterine gap junctions in the uterus, facilitating uterine contractility, while progesterone opposes this action of oestrogens.
22. False. Ergometrine is given alone or together with oxytocin at the time of delivery and produces hypertonic uterine activity to reduce postpartum haemorrhage; it should not be given for labour induction.
23. True. Antagonism of oxytocin receptors by atosiban reduces uterine contractility in preterm labour; other tocolytic drugs include β2-adrenoceptor agonists and calcium channel blockers.
24. True. NSAIDs relieve dysmenorrhoea in approximately 70% of women; the combined and progestogen-only hormonal contraceptives may also be effective.
OBA answers
1. Answer C is the incorrect statement.
A Correct. Blockade of the actions of progesterone by mifepristone results in abortion, although the precise mechanisms are uncertain.
B Correct. Women should be given intravaginal prostaglandins to soften the cervix prior to rupture of the membranes, and then intravenous oxytocin if required.
C Incorrect. Both oxytocin and prostaglandins can cause uterine hypertonus and fetal distress if given in inappropriate amounts.
D Correct. β2-Adrenoceptor agonists may delay labour for 48 h, but they have not been shown to decrease morbidity or mortality in the preterm newborn child.
E Correct. Ergometrine constricts uterine blood vessels via α1-adrenoceptors and uterine hypertonus further compresses blood vessels, reducing postpartum blood loss.
2. Answer D is the most accurate statement.
A Incorrect. In a 35-year-old woman who smokes, the oral combined hormonal contraceptive is not a good choice due to an increased risk of cardiovascular complications.
B Incorrect. The oral combined hormonal contraceptive reduces the risk of endometrial cancer.
C Incorrect. The IUCD is as effective as the combined hormonal contraceptive.
D Correct. The risk of thromboembolic complications is related to the oestrogen content of the combined hormonal contraceptive.
E Incorrect. Intramuscular medroxyprogesterone acetate is effective for 8–12 weeks.
Boulvain, M, Kelly, A, Irion, O. Intracervical prostaglandins for induction of labour. Cochrane Database Syst Rev. (1):2008.
Farquhar, C. Endometriosis. BMJ. 2007;334:249–253.
Grady, D. Management of the menopause. N Engl J Med. 2006;355:2338–2347.
Gruber, CJ, Tschuggel, W, Schneeberger, C, et al. Production and actions of estrogens. N Engl J Med. 2002;346:340–352.
Hickey, M, Davis, SR, Sturdee, DW. Treatment of menopausal symptoms: what shall we do now? Lancet. 2005;366:409–421.
Hickey, M, Elliott, J, Davison, SL. Hormone replacement therapy. BMJ. 2012;344:e763.
Kaunitz, AM. Hormonal contraception in women of older reproductive age. N Engl J Med. 2008;358:1262–1270.
Norwitz, ER, Robinson, JN, Shallis, JRG. The control of labor. N Engl J Med. 1999;341:660–666.
O'Brien, S, Rapkin, A, Dennerstein, L, et al. Diagnosis and management of premenstrual disorders. BMJ. 2011;342:d2994.
Peterson, HB, Curtis, KM. Long-acting methods of contraception. N Engl J Med. 2005;353:2169–2175.
Petitti, DB. Combination estrogen–progestin oral contraceptives. N Engl J Med. 2003;349:1443–1450.
Prabakar, I, Webb, A. Emergency contraception. BMJ. 2012;344:e1492.
Prentice, A. Medical management of menorrhagia. BMJ. 1999;319:1343–1345.
Riggs, BL, Hartmann, LC. Selective estrogen-receptor modulators. Mechanisms of action and application to clinical practice. N Engl J Med. 2003;348:618–629.
Sanchez-Ramos, L. Induction of labor. Obstet Gynecol Clin North Am. 2005;32:181–200.
Simhan, HN, Caritis, SN. Prevention of preterm delivery. N Engl J Med. 2007;357:477–487.
Stearns, V, Ullmer, L, Lopez, JF, et al. Hot flushes. Lancet. 2002;360:1851–1861.
Stubblefield, PG, Carr-Ellis, S, Borgatta, L. Methods for induced abortion. Obstet Gynecol. 2004;104:174–185.