Nausea and vomiting
Nausea and vomiting
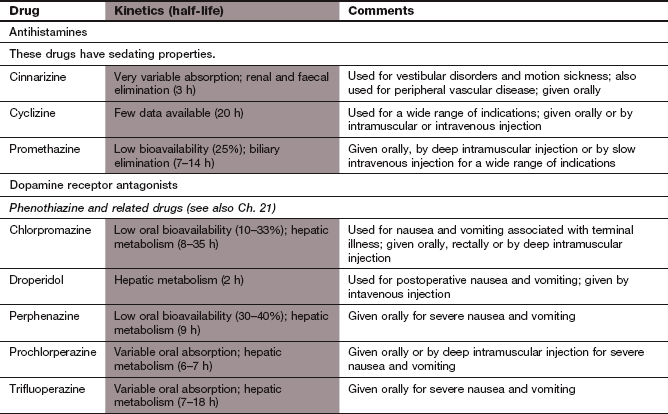
Nausea, retching and vomiting (emesis) are part of the body's defence against ingested toxins. Vomiting is a reflex that is integrated by a loose neuronal network known as the ‘vomiting centre’ in the medulla oblongata of the brainstem. The exact location of the vomiting centre is unclear. It is composed of a series of nuclei in the nucleus tractus solitarius and the dorsal motor nucleus of the vagus. The afferent input to the vomiting centre comes from several sources (Fig. 32.1).
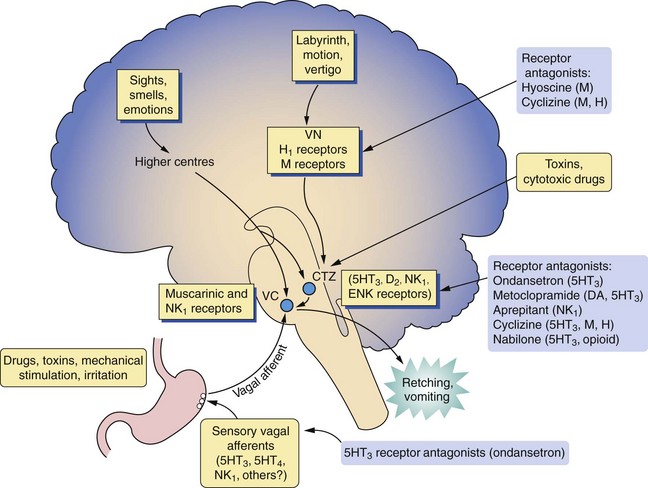
Fig. 32.1 Neuronal pathways and receptors involved in the control of nausea and vomiting.
The pathways and neurotransmitter receptors involved in nausea and vomiting are complex and only those underpinning the mechanisms of action of the anti-emetic drugs are shown. The chemoreceptor trigger zone (CTZ) has neuronal connections to the vomiting centre (VC), which is a collection of nuclei including the dorsal motor nucleus of the vagus and the nucleus tractus solitarius. 5HT3, 5-Hydroxytryptamine type 3 receptor; DA, dopamine receptor; ENK receptor, enkephalin (opioid) receptor; H1, histamine type 1 receptor; M, muscarinic receptor (possibly M2); NK1, neurokinin 1 receptor; VN, vestibular nuclei. Other mediators such as glutamate may also be involved.
 Abdominal and cardiac vagal afferents are activated by mechano- or chemosensory receptors. Chemosensory receptors respond to several agonists such as acetylcholine, dopamine, serotonin, histamine and neurokinins. Some drugs induce vomiting by an effect on gastric chemosensory receptors.
Abdominal and cardiac vagal afferents are activated by mechano- or chemosensory receptors. Chemosensory receptors respond to several agonists such as acetylcholine, dopamine, serotonin, histamine and neurokinins. Some drugs induce vomiting by an effect on gastric chemosensory receptors.
 The area postrema in the floor of the fourth ventricle is the location of the chemoreceptor trigger zone (CTZ). This lies outside the blood–brain barrier and responds to stimuli from the cerebrospinal fluid and the systemic circulation. The CTZ has many receptors for neurotransmitters (such as dopamine, serotonin and substance P) and hormones and it has numerous afferent and efferent connections with the underlying nucleus tractus solitarius.
The area postrema in the floor of the fourth ventricle is the location of the chemoreceptor trigger zone (CTZ). This lies outside the blood–brain barrier and responds to stimuli from the cerebrospinal fluid and the systemic circulation. The CTZ has many receptors for neurotransmitters (such as dopamine, serotonin and substance P) and hormones and it has numerous afferent and efferent connections with the underlying nucleus tractus solitarius.
Other sources include:
 the vestibular nuclei, which are involved in the emetic response to motion,
the vestibular nuclei, which are involved in the emetic response to motion,
 other brainstem structures, such as the amygdala,
other brainstem structures, such as the amygdala,
 higher centres of the cortex and intracranial pressure receptors.
higher centres of the cortex and intracranial pressure receptors.
Several neurotransmitter receptors are involved in direct activation of the vomiting centre including those for dopamine (D2), serotonin, acetylcholine (muscarinic), histamine (H1) and substance P (neurokinin 1, NK1) (Fig. 32.1).
The roles of these multiple receptors in the triggering of nausea and vomiting are complex. For example, 5-HT3 receptor antagonists will provide protection against nausea and vomiting induced by cytotoxic drugs and radiation but not by motion or by apomorphine. Vomiting can result from the summation of several sub-emetic stimuli, for example in the genesis of postoperative nausea and vomiting.
Efferent connections from the vomiting centre include the vagus and phrenic nerves. When stimulated these nerves relax the fundus and body of the stomach and the lower oesophageal sphincter, and retrograde giant contractions occur in the small intestine. Diaphragmatic and abdominal muscle contractions compress the stomach, and together these factors produce vomiting.
Many drugs produce vomiting by stimulating the CTZ and they do not have to cross the blood–brain barrier for this action (Box 32.1).
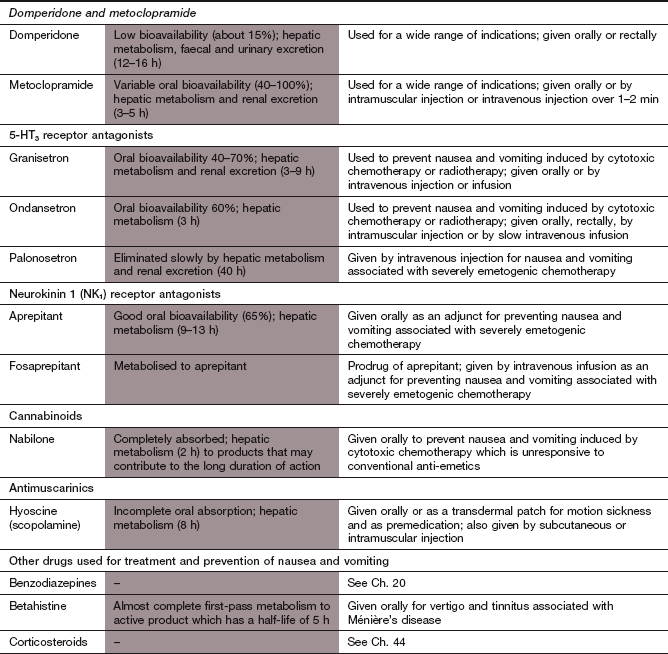
Anti-emetic agents
Mechanism of action and clinical use: Antihistamines prevent and treat vomiting by their antagonist action at histamine H1 receptors (Ch. 39), and many also have antimuscarinic effects. Promethazine also blocks some 5-HT receptor subtypes. Antihistamines are effective against most causes of vomiting but, apart from the use of cyclizine for drug-induced vomiting, they are rarely treatments of choice. Promethazine is used to treat vomiting in pregnancy since it appears to be free from teratogenic effects.
Pharmacokinetics: These drugs are well absorbed orally; both promethazine and cyclizine can also be given by intramuscular or intravenous injection. After oral dosing, promethazine undergoes extensive first-pass metabolism.
 Sedation (particularly with promethazine) and headache.
Sedation (particularly with promethazine) and headache.
 Antimuscarinic effects (Ch. 4), especially dry mouth, urinary retention and blurred vision.
Antimuscarinic effects (Ch. 4), especially dry mouth, urinary retention and blurred vision.
Antimuscarinic agent
Mechanism of action and clinical use: Muscarinic receptors are involved in the visceral afferent input from the gut to the vomiting centre and in the tract that the eighth cranial nerve takes from the labyrinth to the CTZ via the vestibular nucleus. Hyoscine (known as scopolamine in the USA) is used for the treatment of motion sickness and postoperative vomiting. Some antihistamines such as promethazine and cyclizine (see above), and dopamine receptor antagonists such as prochlorperazine (see below), also have antimuscarinic activity.
Pharmacokinetics: Hyoscine is available for oral, parenteral or transdermal use. Oral absorption is good. The adhesive patch for transdermal delivery can be placed behind the ear and delivers a therapeutic dose for 72 h.
 Typical antimuscarinic actions such as dry mouth, urinary retention and blurred vision (Ch. 4).
Typical antimuscarinic actions such as dry mouth, urinary retention and blurred vision (Ch. 4).
Dopamine receptor antagonists
Mechanism of action and clinical use: Domperidone, metoclopramide and the antipsychotic drugs are antagonists at dopamine D2 receptors and inhibit dopaminergic stimulation of the CTZ (Fig. 32.1).
Anti-emetic doses of antipsychotic drugs are generally less than one-third of those used to treat psychoses. The pharmacology of the antipsychotic drugs is discussed in Chapter 21.
Domperidone acts solely by dopamine receptor blockade. Metoclopramide is a dopamine antagonist at usual oral doses, but it also acts as a 5-HT3 receptor antagonist at higher doses. This enhanced efficacy is utilised by intravenous administration of high doses of metoclopramide to treat the vomiting induced by cytotoxic agents such as cisplatin.
Metoclopramide also has prokinetic actions on the gut including increased tone of the gastro-oesophageal sphincter and enhanced gastric emptying and small intestinal motility. These effects arise from agonist activity at the 5-HT4 receptor subtype in the enteric nervous system, which leads indirectly to cholinergic stimulation.
Dopamine receptor antagonists are mainly used to reduce vomiting induced by drugs and surgery. Pure dopamine receptor antagonists are ineffective in motion sickness. Antipsychotic drugs such as prochlorperazine are effective for vestibular disorders and motion sickness as a result of their antimuscarinic activity.
Pharmacokinetics: Metoclopramide and domperidone are well absorbed orally, but have limited bioavailability due to extensive first-pass metabolism in the liver. Metoclopramide is also available for intravenous or intramuscular use, while domperidone can be given rectally by suppository. Metoclopramide has a shorter half-life (3–5 h) than domperidone (12–16 h).
Unwanted effects: Central nervous system (CNS) unwanted effects are produced by metoclopramide and the antipsychotics, but to a lesser extent by domperidone as a result of its lower CNS penetration.
 Acute and chronic extrapyramidal effects from dopamine receptor blockade in the basal ganglia can lead to acute dystonias (especially in children and young adults), akathisia and a parkinsonian-like syndrome. Tardive dyskinesias can develop with prolonged use (see also Ch. 24).
Acute and chronic extrapyramidal effects from dopamine receptor blockade in the basal ganglia can lead to acute dystonias (especially in children and young adults), akathisia and a parkinsonian-like syndrome. Tardive dyskinesias can develop with prolonged use (see also Ch. 24).
 Galactorrhoea and amenorrhoea caused by hyperprolactinaemia from pituitary dopamine receptor blockade.
Galactorrhoea and amenorrhoea caused by hyperprolactinaemia from pituitary dopamine receptor blockade.
5-HT3 receptor antagonists
Mechanism of action and clinical use: The 5-HT3 receptor antagonists block the 5-HT3 receptors in the CTZ and in the gut (Fig. 32.1). They are particularly effective against the acute vomiting induced by highly emetogenic chemotherapeutic agents used for treating cancer (e.g. cisplatin; Ch. 52) and for postoperative vomiting that is resistant to other agents. They are also used for prophylaxis when the consequences of retching and vomiting could be particularly deleterious, for example after eye surgery.
Neurokinin 1 receptor antagonists
Mechanism of action: Aprepitant and its prodrug fosaprepitant are antagonists at NK1 receptors in the CNS, inhibiting the action of substance P. They augment the effects of 5-HT3 receptor antagonists and corticosteroids in preventing the acute and delayed emetic response to the cancer chemotherapeutic agent cisplatin.
Cannabinoids
Mechanism of action and clinical use: Nabilone, a synthetic derivative of tetrahydrocannabinol (a psychoactive substance in cannabis; Ch. 54), is effective in combating vomiting induced by cytotoxic drugs, providing it is given before chemotherapy is started. The mechanism is uncertain, but it may involve inhibition of cortical activity and anxiolysis. Cannabinoid CB1 receptors are found in several areas of the CNS and the action of nabilone at these receptors may inhibit neuronal serotonin release in the dorsal vagal nucleus.
Corticosteroids
Dexamethasone and methylprednisolone are weak anti-emetics. However, they produce additive effects when given with high-dose metoclopramide or with a 5-HT3 receptor antagonist such as ondansetron. High doses of dexamethasone can be given intravenously before cancer chemotherapy, with subsequent oral doses to prevent delayed emesis. The mechanism of action is unknown but may involve reduction of prostaglandin synthesis or release of endorphins. The pharmacology of corticosteroids is discussed in Chapter 44.
Benzodiazepines
Benzodiazepines, such as lorazepam, have no intrinsic anti-emetic activity. They are given orally or intravenously before cancer chemotherapy to sedate and produce amnesia. They are especially useful if there has previously been vomiting with a cytotoxic treatment, since anticipatory nausea and vomiting are then common with subsequent courses. Benzodiazepines are discussed in Chapter 20.
Management of nausea and vomiting
Anti-emetics are used in a number of situations where nausea and vomiting can be troublesome. Some specific clinical uses are considered in more detail (Table 32.1).
Table 32.1
Common indications for various anti-emetic agents
| Cause of vomiting | Treatment |
| Motion sickness | Hyoscine, cyclizine, promethazine |
| Postoperative vomiting | Hyoscine, metoclopramide, domperidone, prochlorperazine, ondansetron (reserved for resistant vomiting) |
| Drug-induced vomiting | Prochlorperazine, metoclopramide, cyclizine (particularly for opioid-induced vomiting) |
| Cytotoxic drug-induced vomiting | Prochlorperazine, metoclopramide, nabilone, ondansetron, aprepitant Adjunctive treatment, e.g. dexamethasone, benzodiazepines |
| Pregnancy-induced vomiting | Promethazine, metoclopramide, pyridoxine |
Drug-induced vomiting
It is sometimes necessary to use drugs that carry a high risk of inducing nausea and vomiting (Box 32.1). Cyclizine, prochlorperazine and metoclopramide are often effective for prevention of opioid-induced vomiting.
More problematic are the highly emetogenic agents used for cancer treatment. Cancer chemotherapy is accompanied by an increase in serotonin release in the gut and the brainstem. Serotonin in the gut probably stimulates vomiting via vagal afferent nerve fibres. For treatments that carry a low risk of vomiting, routine prophylaxis is not needed. For moderately emetogenic treatments, a 5-HT3 receptor antagonist such as ondansetron, possibly combined with a corticosteroid (such as dexamethasone), is usually recommended. For highly emetogenic chemotherapy, a 5-HT3 receptor antagonist combined with dexamethasone and aprepitant can achieve control in up to 80% of cases. Prochlorperazine, domperidone and nabilone can be used when there is intolerance of 5-HT3 receptor antagonists or corticosteroids.
Delayed emesis, occurring at least 16 h after the chemotherapy, may be mediated by CNS 5-HT3 and NK1 receptors. Dexamethasone combined with aprepitant is recommended for control of delayed emesis, with a 5-HT3 receptor antagonist being an alternative to aprepitant.
Anticipatory vomiting prior to cycles of chemotherapy usually occurs if previous cycles have been accompanied by nausea and vomiting. It is most effectively prevented by including a benzodiazepine such as lorazepam with the chemotherapy regimen from the start of treatment, to produce amnesia.
Postoperative vomiting
Postoperative nausea and vomiting frequently occur in the first 24 h after anaesthesia and surgery. They are more common in women, in non-smokers and after a previous episode of postoperative nausea and vomiting. They are provoked by inhalational rather than intravenous anaesthesia, more often by abdominal, ophthalmic or ear, nose and throat procedures, by the use of opioid analgesics, and by postoperative pain, hypotension and gastric stasis.
Dexamethasone, prochlorperazine, hyoscine (using a transdermal patch), promethazine and haloperidol are all effective for preventing postoperative vomiting. Antihistamines may be effective in emesis associated with surgery to the middle ear. If vomiting is severe, or if it carries high risk for the individual (e.g. after eye surgery), then a 5-HT3 receptor antagonist such as ondansetron is particularly effective.
Motion sickness
Motion sickness arises from a mismatch between sensory inputs from the visual and vestibular systems. Behavioural treatments such as habituation or coping strategies involving distraction can be effective. If a drug is needed an antimuscarinic such as hyoscine or an antihistamine such as cyclizine are effective, with promethazine as an alternative. Antimuscarinic unwanted effects or drowsiness may be troublesome with each of these agents.
Vomiting in pregnancy
Nausea is common in pregnancy. High doses of pyridoxine (vitamin B6) or of ground ginger may be effective, and counselling or hypnotism can also be tried.
Hyperemesis gravidarum, severe morning sickness which begins in the first trimester, can lead to marked maternal weight loss, dehydration, electrolyte disturbances and vitamin deficiencies. There is a natural desire to avoid drugs whenever possible if vomiting arises in pregnancy. However, for more severe vomiting, in addition to rehydration and nutritional supplementation, drugs will be necessary. Cyclizine and metoclopramide are the drugs of choice, with prochlorperazine, domperidone, ondansetron or a corticosteroid as second-line options. All these drugs appear to be safe in early pregnancy.
Vertigo
Vertigo is an hallucination of motion, usually perceived as spinning, which is generated in the vestibular system of the inner ear. It is frequently accompanied by nausea and vomiting. There are several causes of vertigo (Box 32.2). The mechanisms of vertigo are poorly understood. Treatment is empirical and involves modulation of neurotransmitters and receptors involved in the vestibular sensory pathway to the oculomotor nucleus. The neurochemistry of vertigo overlaps with that of vomiting, and involves:
 glutamate: excitatory, acting through N-methyl-D-aspartate (NMDA) receptors on both peripheral and central neurons,
glutamate: excitatory, acting through N-methyl-D-aspartate (NMDA) receptors on both peripheral and central neurons,
 acetylcholine: excitatory, acting through muscarinic M2 receptors on peripheral and central neurons,
acetylcholine: excitatory, acting through muscarinic M2 receptors on peripheral and central neurons,
 gamma-aminobutyric acid (GABA): inhibitory, acting through GABAA and GABAB receptors on central neurons,
gamma-aminobutyric acid (GABA): inhibitory, acting through GABAA and GABAB receptors on central neurons,
 histamine: excitatory, acting through H1 and H2 receptors on central neurons,
histamine: excitatory, acting through H1 and H2 receptors on central neurons,
 noradrenaline: involved in central modulation of vestibular sensory transmission,
noradrenaline: involved in central modulation of vestibular sensory transmission,
Ménière's disease is one of the causes of vertigo for which the pathogenesis is better understood. It usually presents with episodic vertigo and associated signs of vagal overactivity such as pallor, sweating, nausea and vomiting. Tinnitus and eventually sensorineural deafness are common. The basic defect is an excess of endolymph in the membranous labyrinth of the middle ear. There may be a genetic predisposition, while anatomical abnormalities in the middle ear and various immunological, vascular or viral precipitating insults may be involved.
Drugs for treatment of vertigo
 Antihistamines (histamine H1 receptor blockers), e.g. cyclizine, promethazine. These are the most widely used drugs for vertigo.
Antihistamines (histamine H1 receptor blockers), e.g. cyclizine, promethazine. These are the most widely used drugs for vertigo.
 Antimuscarinic agents. Vestibular suppression can be achieved with hyoscine, and the mechanism of action may be similar to that involved in the treatment of motion sickness.
Antimuscarinic agents. Vestibular suppression can be achieved with hyoscine, and the mechanism of action may be similar to that involved in the treatment of motion sickness.
 Benzodiazepines. The use of these agents for short periods may help in severe attacks of vertigo.
Benzodiazepines. The use of these agents for short periods may help in severe attacks of vertigo.
 Cimetidine. This drug probably produces symptom relief by blockade of histamine H2 receptors in the CNS (Ch. 33).
Cimetidine. This drug probably produces symptom relief by blockade of histamine H2 receptors in the CNS (Ch. 33).
 Histamine receptor agonists. The use of betahistine to treat Ménière's disease illustrates a paradox that both histaminergic and antihistaminic drugs have been advocated for treatment of this condition. Betahistine is an analogue of L-histidine, the metabolic precursor of histamine. It is a partial agonist at postsynaptic histamine H1 receptors and an antagonist at presynaptic H3 receptors, an action that facilitates central histaminergic neurotransmission. Betahistine also increases blood flow to the inner ear. It is metabolised to an active derivative in the liver. The main unwanted effects are headache and nausea.
Histamine receptor agonists. The use of betahistine to treat Ménière's disease illustrates a paradox that both histaminergic and antihistaminic drugs have been advocated for treatment of this condition. Betahistine is an analogue of L-histidine, the metabolic precursor of histamine. It is a partial agonist at postsynaptic histamine H1 receptors and an antagonist at presynaptic H3 receptors, an action that facilitates central histaminergic neurotransmission. Betahistine also increases blood flow to the inner ear. It is metabolised to an active derivative in the liver. The main unwanted effects are headache and nausea.
 Dopamine receptor antagonists. Several antipsychotic drugs such as prochlorperazine are used in vertigo, mainly to treat the associated nausea. Their use for treatment of dizziness in the elderly is not recommended because of the risk of extrapyramidal effects.
Dopamine receptor antagonists. Several antipsychotic drugs such as prochlorperazine are used in vertigo, mainly to treat the associated nausea. Their use for treatment of dizziness in the elderly is not recommended because of the risk of extrapyramidal effects.
Management of vertigo
Many forms of vertigo are brief and self-limiting. Acute vertigo, such as that caused by vestibular neuronitis, is often treated with anti-emetic agents until vestibular compensation occurs, which is usually encouraged by maintaining activity. The anti-emetic drug should usually be withdrawn as soon as the acute symptoms subside.
Benign paroxysmal positional vertigo responds poorly to drugs and is most effectively treated by vestibular exercises. Drug therapy should be avoided if possible, since it can blunt the effectiveness of the exercises by inhibiting vestibular compensation.
Ménière's disease is often treated initially with lifestyle changes, such as avoidance of excess caffeine, chocolate, alcohol and salt. Modification of the endolymph production in the inner ear with diuretics such as bendroflumethiazide (Ch. 14) is often attempted for persistent symptoms, although clear evidence of efficacy is lacking. Betahistine is often co-prescribed with a diuretic, again with little evidence of benefit. Oral or intratympanic injection of corticosteroid is an alternative to a diuretic. Sedative anti-emetic drugs such as promethazine, cinnarizine or prochlorperazine should only be used for very short periods since they impair vestibular rehabilitation. For refractory symptoms, the vestibular apparatus can be ablated, for example using local delivery of gentamicin (Ch. 51), which is toxic to the inner ear. Surgical treatment is also used for refractory disease.
Several drugs can cause dizziness or a sensation similar to vertigo and recent changes in drug therapy should be considered when a person presents with a new onset of dizziness. Examples of drugs that commonly cause dizziness are antihypertensive agents, vasodilators and antiparkinsonian agents. A more serious degree of vestibular toxicity can be produced by aminoglycosides such as gentamicin (Ch. 51) and high doses of loop diuretics such as furosemide (Ch. 14). This type of vestibular toxicity can be reversible, but is often permanent.
True/false questions
One-best-answer (OBA) question
Which statement concerning nausea and vomiting is the most accurate?
A Afferents from the stomach to the vomiting centre inhibit vomiting when stimulated.
B Selective 5-HT3 receptor antagonists are effective against motion sickness.
C Nabilone is derived from a psychoactive component of cannabis.
D Stimulation of neurokinin 1 (NK1) receptors in the CTZ inhibits nausea.
Case-based questions
A 35-year-old man was diagnosed with non-Hodgkin's lymphoma requiring many sessions of treatment with combined cytotoxic therapy, including cyclophosphamide and vincristine.
A Why was this man likely to experience nausea and vomiting?
Nausea and vomiting started several hours after each course of treatment and continued for 4–5 days.
B What planned anti-emetic treatment prior to the first course of chemotherapy could be beneficial?
C How do the treatments you have chosen work?
This man became very distressed by the severity of the nausea and vomiting and developed intense nausea and vomiting prior to the administration of the chemotherapeutic agents.
D What treatment could be given to reduce the anticipatory nausea and vomiting?
1. False. The CTZ (area postrema) is outside the blood–brain barrier. Some toxins can also cause vomiting by stimulating vagal afferents in the stomach.
2. True. Common antihistamines like promethazine have antimuscarinic activity and inhibit activity in the vomiting centre and in the vestibular nuclei. It is not certain whether the antihistamine component plays a role.
3. True. Dopamine antagonists used as anti-emetics are given at lower doses than in antipsychotic treatment, but they carry a risk of extrapyramidal movement disorders, particularly in the elderly.
4. False. Metoclopramide increases stomach and intestinal motility (prokinetic activity), which can add to its anti-emetic effects.
5. True. Aminoglycosides (such as gentamicin) and loop diuretics (furosemide) may cause vestibular damage, leading to vertigo.
OBA answer
A Incorrect. The vagal afferents from the stomach respond to toxins and are emetogenic.
B Incorrect. Selective 5-HT3 receptor antagonists are not effective against motion sickness, for which a drug with antimuscarinic actions, e.g. hyoscine or promethazine, should be used.
C Correct. Nabilone is a derivative of tetrahydrocannabinol and an agonist at cannabinoid CB1 receptors.
D Incorrect. The effect of stimulating NK1 receptors in the CTZ is to cause vomiting.
Case-based answers
A Cyclophosphamide induces nausea and vomiting in almost all people, but vincristine is much less emetogenic. The vomiting arises from stimulation of the CTZ.
B A selective 5-HT3 receptor antagonist such as ondansetron, alone or together with a corticosteroid, would be beneficial.
C Ondansetron inhibits 5-HT3 receptors in the CTZ and also in the stomach. In the stomach, some cancer chemotherapeutic agents can cause damage and release of serotonin, which stimulates vagal afferents to the vomiting centre. It is uncertain how corticosteroids work, but they have an anti-emetic effect which is additive with ondansetron.
D Anticipatory nausea and vomiting is poorly treated with anti-emetic drugs. Treatment with benzodiazepine anxiolytic drugs prior to the course of chemotherapy can be helpful.
Baloh, RW. Vestibular neuritis. N Engl J Med. 2003;348:1027–1032.
Gan, TJ, Meyer, T, Apfel, CC, et al. Consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71.
Hain, TC, Uddin, M. Pharmacological treatment of vertigo. CNS Drugs. 2003;17:85–100.
Hesketh, PJ. Drug therapy-chemotherapy-induced nausea and vomiting. N Engl J Med. 2008;358:2482–2494.
Jarvis, S, Nelson-Piercy, C. Management of nausea and vomiting in pregnancy. BMJ. 2011;342:d3606.
Jordan, K, Sippel, C, Schmoll, HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007;12:1143–1150.
Nurdin, L, Golding, J, Bronstein, A. Managing motion sickness. BMJ. 2011;343:d7430.
Niebyl, JR. Nausea and vomiting in pregnancy. N Engl J Med. 2011;363:1544–1550.
Sajjadi, H, Paparella, MM. Ménière's disease. Lancet. 2008;372:406–414.
Wilhelm, SM, Dehoorne-Smith, ML, Kale-Pradhan, PB. Prevention of postoperative nausea and vomiting. Ann Pharmacother. 2007;41:68–78.