Soft Tissue Calcification and Ossification
The deposition of calcium salts, primarily calcium phosphate, usually occurs in the skeleton. When it occurs in an unorganized fashion in soft tissue, it is referred to as heterotopic calcification. This soft tissue mineralization may develop in a wide variety of unrelated disorders and degenerative processes. Heterotopic calcifications may be divided into three categories:
Dystrophic calcification refers to calcification that forms in degenerating, diseased, and dead tissue despite normal serum calcium and phosphate levels. The soft tissue may be damaged by blunt trauma, inflammation, injections, the presence of parasites, soft tissue changes arising from disease, and many other causes. This calcification usually is localized to the site of injury. Idiopathic calcification (or calcinosis) results from deposition of calcium in normal tissue despite normal serum calcium and phosphate levels. Examples include chondrocalcinosis and phleboliths. Metastatic calcification results when minerals precipitate into normal tissue as a result of higher than normal serum levels of calcium (e.g., hyperparathyroidism, hypercalcemia, of malignancy) or phosphate (e.g., chronic renal failure). Metastatic calcification usually occurs bilaterally and symmetrically.
When the mineral is deposited in soft tissue as organized, well-formed bone, the process is known as heterotopic ossification. The term heterotopic indicates that bone has formed in an abnormal (extraskeletal) location. The heterotopic bone may be all compact bone, or it may show some trabeculae and fatty marrow. The deposits may range from 1 mm to several centimeters in diameter, and one or more may be present. The causes range from posttraumatic ossification, bone produced by tumors, and ossification caused by diseases such as progressive myositis ossificans and ankylosing spondylitis.
Clinical Features
Sites of heterotopic calcification or ossification may not cause significant signs or symptoms; they most often are detected as incidental findings during radiographic examination.
Radiographic Features
Soft tissue opacities are fairly common, present on about 4% of panoramic radiographs. In most cases the goal is to identify the calcification correctly to determine whether treatment or further investigation is required. Some soft tissue calcifications require no intervention or long-term surveillance, whereas others may be life threatening and the underlying cause requires treatment. When the soft tissue calcification is adjacent to bone, it sometimes is difficult to determine whether the calcification is within bone or soft tissue. Another radiographic view at right angles is useful. The important criteria to consider in arriving at the correct interpretation are the anatomic location, number, distribution, and shape of the calcifications. Analysis of the location requires knowledge of soft tissue anatomy, such as the position of lymph nodes, stylohyoid ligaments, blood vessels, laryngeal cartilages, and the major ducts of the salivary glands.
GENERAL DYSTROPHIC CALCIFICATION OF THE ORAL REGIONS
Dystrophic calcification is the precipitation of calcium salts into primary sites of chronic inflammation or dead and dying tissue. This process is usually associated with a high local concentration of phosphatase, as in normal bone calcification, an increase in local alkalinity, and anoxic conditions within the inactive or devitalized tissue. A long-standing chronically inflamed cyst is a common location of dystrophic calcification.
Clinical Features
Common soft tissue sites include the gingiva, tongue, lymph nodes, and cheek. Dystrophic calcifications may produce no signs or symptoms, although occasionally enlargement and ulceration of overlying soft tissues may occur, and a solid mass of calcium salts sometimes can be palpated.
Radiographic Features
The radiographic appearance of dystrophic calcification varies from barely perceptible, fine grains of radiopacities to larger, irregular radiopaque particles that rarely exceed 0.5 cm in diameter. One or more of these radiopacities may be seen, and the calcification may be homogeneous or may contain punctate areas. The outline of the calcified area usually is irregular or indistinct. Common sites are long-standing chronically inflamed cysts (Fig. 28-1) and polyps (Fig. 28-2).
CALCIFIED LYMPH NODES
Dystrophic calcification occurs in lymph nodes that have been chronically inflamed because of various diseases, frequently granulomatous disorders. The lymphoid tissue becomes replaced by hydroxyapatite-like calcium salts, nearly effacing all of nodal architecture. The presence of calcifications in lymph nodes implies disease, either active or the result of previously treated pathosis. In the past, tuberculosis was the most common disease causing calcified lymph nodes (scrofula or cervical tuberculous adenitis). Other well-known causes of lymph node calcification include bacille Calmette-Guérin vaccination, sarcoidosis, cat-scratch disease, rheumatoid arthritis and systemic sclerosis, lymphoma previously treated with radiation therapy, fungal infections, and metastases from distant calcifying neoplasms, most notably metastatic thyroid carcinoma.
Clinical Features
Calcified lymph nodes are generally asymptomatic, and these nodes are first discovered as an incidental finding on a panoramic radiograph. The most commonly involved nodes are the submandibular and superficial and deep cervical nodes and, less commonly, the preauricular and submental nodes. When these nodes can be palpated, they are hard, lumpy, round to oblong masses.
Radiographic Features
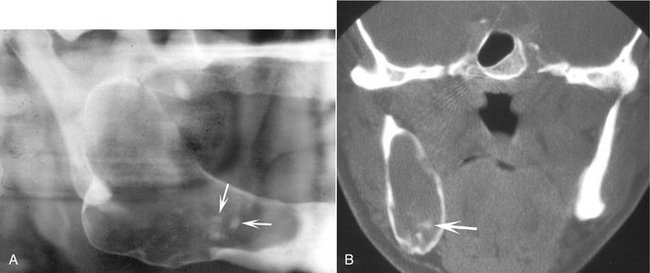
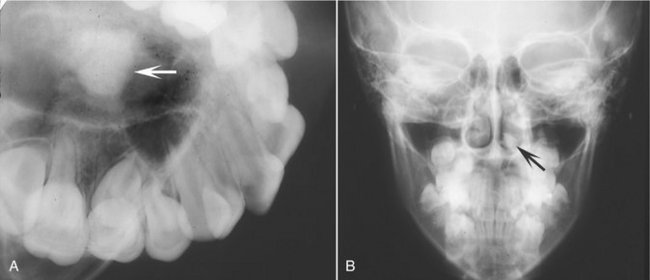
Location.: The most common location is the submandibular region, either at or below the inferior border of the mandible near the angle, or between the posterior border of the ramus and cervical spine. The image of the calcified node sometimes overlaps the inferior aspect of the ramus. Lymph node calcifications may affect a single node or a linear series of nodes in a phenomenon known as lymph node “chaining” (Fig. 28-3).

FIG. 28-3 Examples of dystrophic calcification in the lymph nodes. A, Two large examples positioned behind the ramus with a cauliflower-like shape and two smaller examples in a more superior position (arrows). B, Several smaller examples positioned below the lower border of the mandible. C, A larger example.
Periphery.: The periphery is well defined and usually irregular, occasionally having a lobulated appearance similar to the outer shape of cauliflower. This irregularity of shape is of great significance in distinguishing node calcifications from other potential soft tissue calcifications in the area.
Internal Structure.: The internal aspect is without pattern but may vary in the degree of radiopacity, giving the impression of a collection of spherical or irregular masses. Occasionally the lesion has a laminated appearance, or the radiopacity may appear only on the surface of the node (eggshell calcification).The pattern of nodal calcification does not reliably distinguish between benign and malignant disease.
Differential Diagnosis
Differentiation between a single calcified lymph node and a sialolith in the hilar region of the submandibular gland may be difficult because both may appear near or adjacent to the inferior cortex of the mandible just anterior to the angle. Usually a sialolith has a smooth outline, whereas a calcified lymph node is usually irregular and sometimes lobulated. The differentiation can be made if the patient has symptoms related to the submandibular salivary gland (see Chapter 31). Occasionally sialography may be necessary to make the differentiation. Another calcification that may have a similar appearance in this region is a phlebolith; however, phleboliths are usually smaller and multiple, with concentric radiopaque and radiolucent rings, and their shape may mimic a portion of a blood vessel.
Management
Calcified lymph nodes usually do not require treatment; however, the underlying cause should be established in case treatment is required, such as in the case of active disease.
Definition
Tonsillar calculi are formed when repeated bouts of inflammation enlarge the tonsillar crypts. Incomplete resolution of organic debris (dead bacteria and pus, epithelial cells, and food) can serve as the nidus for dystrophic calcification.
Clinical Features
Tonsilloliths usually present as hard, round, white or yellow objects projecting from the tonsillar crypts, usually of the palatine tonsil. Small calcifications usually produce no clinical signs or symptoms. However, pain, swelling, fetor oris, dysphagia, or a foreign body sensation on swallowing has been reported with larger calcifications. Giant tonsilloliths stretching lymphoid tissue resulting in ulceration and extrusion are much less common. These calcifications have been reported to occur between 20 and 68 years of age; they are found more often in older age groups.
Radiographic Features
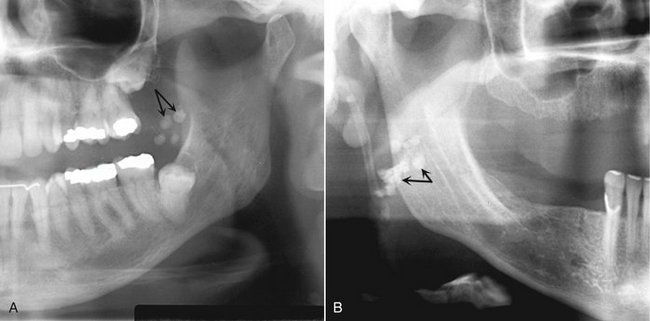
Location.: In the panoramic film, tonsilloliths appear as single or multiple radiopacities that overlap the mid portion of the mandibular ramus in the region where the image of the dorsal surface of the tongue crosses the ramus in the oropharyngeal air spaces. Tonsilloliths frequently appear on the panoramic radiograph immediately inferior to the mandibular canal (Fig. 28-4).
Differential Diagnosis
The clinical differential diagnosis includes calcified granulomatous disease, syphilis, mycosis, or lymphoma, which may produce a firm tonsillar mass. The essential radiographic differential diagnosis is a radiopaque lesion within the mandibular ramus, such as a dense bone island. When in doubt, a right-angle view such as a posteroanterior skull view or an open Towne’s view may show that the calcification lies to the medial aspect of the ramus. Three-dimensional imaging such as computed tomography (CT) or cone beam CT may be necessary for precise localization.
Treatment
No treatment is required for most tonsillar calcifications. In symptomatic patients, tonsilloliths may be expressed manually, possibly with the patient under sedation to suppress the gag reflex. However, large calcifications with associated symptoms are removed surgically. Treatment of asymptomatic tonsilloliths may be considered in elderly patients with mechanical deglutition disorders and the immunocompromised because of the risk for aspiration pneumonia.
CYSTICERCOSIS
When humans ingest eggs or gravid proglottids from the parasite Taenia solium (pork tapeworm), the covering of the eggs is digested in the stomach and the larval form (Cysticercus cellulosae) of the parasite is hatched. The larvae penetrate the mucosa, enter the blood vessels and lymphatics, and are distributed in the tissues all over the body but preferentially locate to brain, muscle, skin, liver, lungs, and heart. They are also found in the oral and perioral tissues, especially the muscles of mastication. In tissues other than the intestinal mucosa, the larvae eventually die and are treated as foreign bodies, causing granuloma formation, scarring, and calcification approximately 3 months later. These areas in the tissues are called cysticerci. There is currently an increased incidence of cysticercosis in the American Southwest and urban Northeast, especially among Koreans and Hispanics. The problem is much worse in developing countries of Central and South America, Asia, and Africa, where there is fecal contamination of agricultural soil and pork is a valued food.
Clinical Features
Mild cases of cysticercosis are completely asymptomatic. More severe cases have symptoms that range from mild to severe gastrointestinal upset with epigastric pain and severe nausea and vomiting. Invasion of the brain may result in seizures, headache, visual disturbances, acute obstructive hydrocephalus, irritability, loss of consciousness, and death. Examination of the oral mucosa may disclose palpable, well-circumscribed soft fluctuant swellings, which resemble a mucocele or benign mesenchymal neoplasm. Multiple small nodules may be felt in the region of the masseter and suprahyoid muscles and in the tongue, buccal mucosa, or lip.
Radiographic Features
While alive, larvae are not visible radiographically. Death of the parasites and development of calcifications in subcutaneous and muscular sites occurs approximately 5 years after the initial infection.
Location.: The locations of calcified cysticerci include the muscles of mastication and facial expression, the suprahyoid muscle, and the postcervical musculature, as well as in the tongue, buccal mucosa, or lip.
Differential Diagnosis
Cysticercus may appear similar to a sialolith. However, the small size of the calcified nodules of cysticerci and their widespread dissemination, particularly in brain and muscles, are highly suggestive of the diagnosis.
Management
Although basic sanitation (proper preparation of pork and avoiding fecal contamination of water supplies and vegetables) is needed to extinguish this source of infection, the symptoms that accompany the initial infestation are best treated by a physician using an antihelminthic such as praziquantel. After the larvae have settled and calcified in the oral tissues, however, they are harmless. However, it is important to carry out a detailed investigation in each patient to rule out the presence of the parasite in other locations.
Arterial Calcifications
Two distinct patterns of arterial calcification can be identified both radiographically and histologically, Monckeberg’s medial calcinosis and calcified atherosclerotic plaque.
MONCKEBERG’S MEDIAL CALCINOSIS (ARTERIOSCLEROSIS)
The hallmark of arteriosclerosis is the fragmentation, degeneration, and eventual loss of elastic fibers followed by the deposition of calcium within the medial coat of the vessel.
Clinical Features
Most patients are asymptomatic initially, although late in the course of the disease may have clinical pathosis such as cutaneous gangrene, peripheral vascular disease, and myositis as a result of vascular insufficiency. Patients with Sturge-Weber syndrome also develop intracranial arterial calcifications.
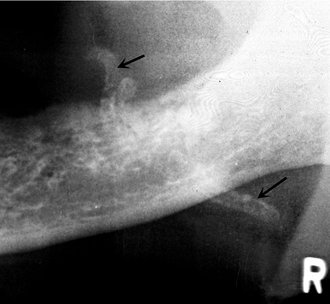
Radiographic Features
Location.: Medial calcinosis involving the facial artery or, less commonly, the carotid artery, may be viewed on panoramic radiographs.
Periphery and Shape.: The calcific deposits in the wall of the artery outline an image of the artery. From the side, the calcified vessel appears as a parallel pair of thin, radiopaque lines (Fig. 28-5) that may have a straight course or a tortuous path and is described as a “pipe stem” or “tram-track” appearance. In cross-section, involved vessels will display a circular or ringlike pattern.
CALCIFIED ATHEROSCLEROTIC PLAQUE
Atheromatous plaque in the extracranial carotid vasculature is the major contributing source of cerebrovascular embolic and occlusive disease. Dystrophic calcification can occur in the evolution of plaque within the intima of the involved vessel.
Radiographic Findings
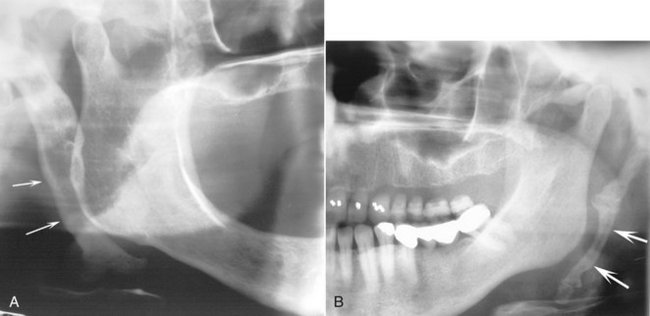
Location.: Atherosclerosis first develops at arterial bifurcations as a result of increased endothelial damage from shear forces at these sites. When calcification has occurred, these lesions may be visible in the panoramic radiograph in the soft tissues of the neck either superior or inferior to the greater cornu of the hyoid bone (where the common carotid artery splits into the external and internal carotid arteries) and adjacent to the cervical vertebrae C3, C4, or the intervertebral space between them (Fig. 28-6).
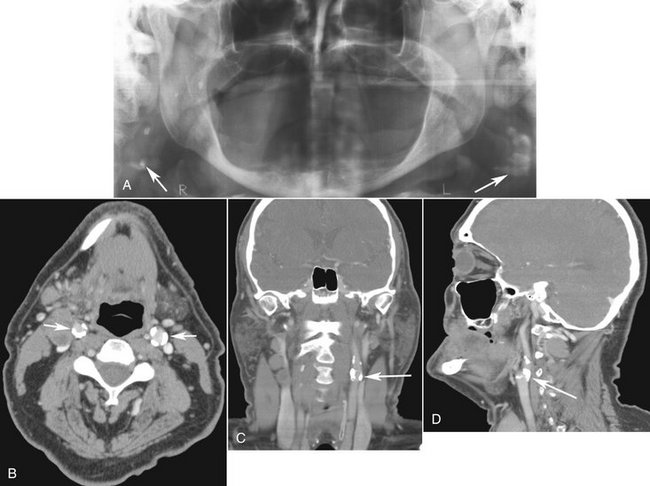
FIG. 28-6 A, Panoramic image with bilateral examples of calcifications associated with the carotid arteries (arrows). B, Axial CT image of the same case with soft tissue algorithm showing bilateral calcification with the walls of the carotid arteries (arrows). C and D, Coronal and sagittal CT images of the same case demonstrating the carotid calcifications (arrows).
Differential Diagnosis
Calcified triticeous cartilage may be mistaken for atheromatous plaque, although the uniform size, shape, and location of calcified triticeous cartilage in the laryngeal cartilage skeleton identify this innocuous condition.
Management
Many published case reports and case series report individual instances of patients with calcified carotid atheromata on panoramic radiographs who were found to have clinically significant stenoses with a heightened risk for a cerebrovascular accident. However, further research needs to be conducted with case-control or cohort studies with a control group to determine whether calcified carotid atheromas represent an independent risk factor for stroke. In the meantime, patients with calcified carotid atheromata, especially those with established risk factors for cerebrovascular and cardiovascular disease, should be referred to their physicians for further investigation.
SIALOLITH
Sialoliths are stones found within the ducts of salivary glands (also see Chapter 31). Mechanical conditions contributing to a slow flow rate and physiochemical characteristics of the gland secretion both contribute to the formation of a nidus and subsequent precipitation of calcium and phosphate salts.
Clinical Features
Sialoliths are most common in the submandibular glands of men in their middle and later years. They usually occur singly (70% to 80%) but may be multiple, especially in the parotid gland. Patients with salivary stones may be asymptomatic, but they usually have a history of pain and swelling in the floor of the mouth and in the involved submandibular gland or in the cheek in the case of parotid sialoliths. This discomfort may intensify at mealtimes, when salivary flow is stimulated. Because the stone usually does not block the flow of saliva completely, the pain and swelling gradually subside. As many as 9% of patients have recurrent sialolithiasis, and about 10% of patients with sialolithiasis also have nephrolithiasis.
Radiographic Features
Location.: The submandibular gland is involved more often (83% to 94% of cases) than the parotid gland (4% to 10%) or the sublingual gland (1% to 7%), probably because the submandibular gland has a longer and more tortuous duct, an uphill flow in the proximal portion, and more viscous saliva with a higher mineral content. About half of submandibular stones lie in the distal portion of Wharton’s duct, 20% in the proximal portion, and 30% in the gland itself.
Periphery and Shape.: Sialoliths located in the duct of the submandibular gland usually are cylindric and very smooth in their outlines. Stones that form in the hilus of a submandibular gland tend to be larger and more irregularly shaped (Fig. 28-7).
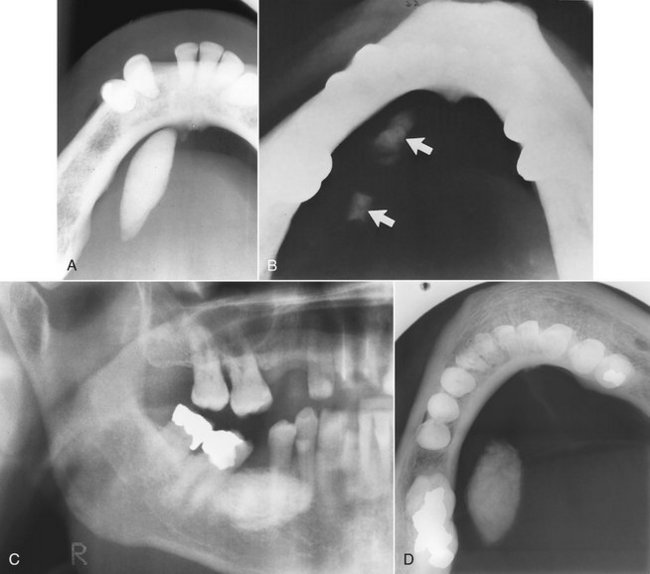
FIG. 28-7 A and B, Standard occlusal projections of single and multiple examples of calcified sialoliths (arrows) in the duct of a submandibular gland. Exposure times have been reduced to better demonstrate these calcifications, which are less calcified than the mandible. In another example (C), the image of the sialolith is superimposed over the mandibular alveolar process in this cropped panoramic image. D, Occlusal view of the same case.
Internal Structure.: Some stones are homogeneously radiopaque, and others show evidence of multiple layers of calcification (Fig. 28-8, A). Less than 20% of submandibular gland sialoliths and 40% of those in the parotid gland are radiolucent because of the low mineral content of the parotid secretions.
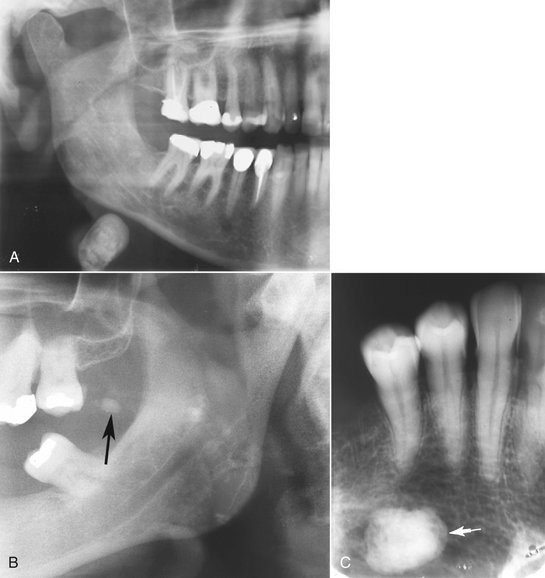
FIG. 28-8 A, Cropped panoramic image of a submandibular gland sialolith; note the position and also the hint at a laminated internal pattern. B, Cropped panoramic image of a sialolith (arrow) involving the parotid gland. C, Intraoral periapical image of superimposed submandibular sialolith that could be difficult to differentiate from a dense bone island without an occlusal film. (B courtesy Drs. John Lovas and Nick Hogg, Dalhousie University.)
Applied Radiology
Salivary stones occasionally are seen on periapical views superimposed over the mandibular premolar and molar apices (Fig. 28-8, C). The best view for visualizing stones in the distal portion of Wharton’s duct is a standard mandibular occlusal view using half the usual exposure time, which displays the floor of the mouth without overlap from the mandible. Stones in a more posterior location are best visualized on lateral oblique views of the mandible or on a panoramic film. To demonstrate stones in the parotid gland duct, the clinician places a periapical film in the buccal vestibule, reduces the exposure time, and orients x-ray beam through the cheek. Also, stones in the parotid duct can be seen if the patient “blows out” the cheek as an anteroposterior skull view is exposed. An open-mouth lateral skull projection can be used or sometimes visible in a panoramic view (Fig. 28-8, B). When radiographs to detect sialoliths are produced, the exposure time should be reduced to about half of normal. This helps in detecting stones that are lightly calcified. If a noncalcified stone is suspected, sialography is used (see Chapter 31).
Differential Diagnosis
Sialoliths can be distinguished from other soft tissue calcifications because they usually are associated with pain or swelling of the involved salivary gland. Other calcifications (e.g., lymph nodes) are asymptomatic. If the diagnosis is unclear, the clinician can prescribe a sialogram.
Management
Small stones often may be “milked out” through the duct orifice by bimanual palpation. If the stone is too large or located in the proximal duct, nonsurgical or minimally invasive sialolithotomy using intracorporeal lithotriptors is becoming a popular treatment modality. In cases of exceedingly large sialoliths, surgical removal of the stone or gland may be required.
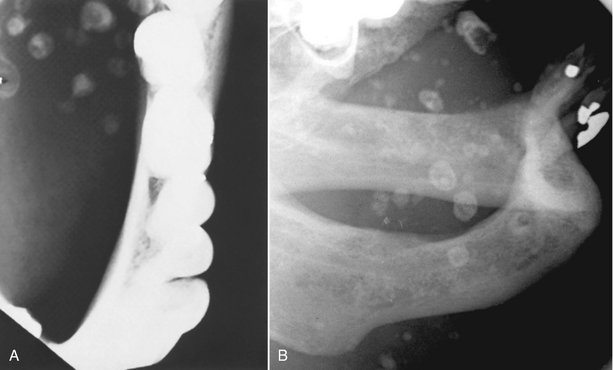
PHLEBOLITHS
Intravascular thrombi, which arise from venous stagnation, sometimes become organized or even mineralized. Such mineralization begins in the core of the thrombus and consists of crystals of apatite with calcium phosphate and calcium carbonate. Phleboliths are calcified thrombi found in veins, venulae, or the sinusoidal vessels of hemangiomas (especially the cavernous type).
Clinical Features
In the head and neck, phleboliths nearly always signal the presence of a hemangioma. In an adult, phleboliths may be the sole residua of a childhood hemangioma that has long since regressed. The involved soft tissue may be swollen, throbbing, or discolored by the presence of veins or a soft tissue hemangioma. Hemangiomas often fluctuate in size, associated with changes in body position or during a Valsalva maneuver. Applying pressure to the involved tissue should cause a blanching or change in color if the lesion is vascular in nature. Auscultation may reveal a bruit in cases of cavernous hemangioma but not in the capillary type.
Radiographic Features
Location.: Phleboliths most commonly are found in hemangiomas (see Chapter 22).
Periphery and Shape.: In cross-section the shape is round or oval, up to 6 mm in diameter with a smooth periphery. If the involved blood vessel is viewed from the side, the phlebolith may resemble a straight or slightly curved sausage.
Internal Structure.: The internal aspect may be homogeneously radiopaque but more commonly has the appearance of laminations, giving phleboliths a bull’s-eye or “target” appearance. A radiolucent center may be seen, which may represent the remaining patent portion of the vessel (Fig. 28-9).
Differential Diagnosis
A phlebolith may have a shape similar to that of a sialolith. Sialoliths usually occur singly; if more than one is present, they usually are oriented in a single line, whereas phleboliths are usually multiple and have a more random, clustered distribution. The importance of correctly identifying phleboliths lies in the identification of a possible vascular lesion such as a hemangioma. This is critical if surgical procedures are contemplated.
LARYNGEAL CARTILAGE CALCIFICATIONS
The small, paired triticeous cartilages are found within the lateral thyrohyoid ligaments. Both the thyroid and triticeous cartilages consist of hyaline cartilage, which has a tendency to calcify or ossify with advancing age.
Clinical Features
Calcification of tracheal cartilages is an incidental radiographic finding with no clinical features.
Radiographic Features
Location.: The calcified triticeous cartilage is located on a lateral skull or panoramic radiograph within the soft tissues of the pharynx inferior to the greater cornu of the hyoid bone and adjacent to the superior border of C4. The superior cornu of a calcified thyroid cartilage appears medial to C4 and is superimposed on the prevertebral soft tissue (Fig. 28-10).
Periphery and Shape.: The word triticeous means “grain of wheat,” and the cartilage measures 7 to 9 mm in length and 2 to 4 mm in width. The periphery of the calcified triticeous cartilage is well defined and smooth, and the geometry is exceedingly regular. Usually only the top 2 to 3 mm of a calcified thyroid cartilage will be visible at the lower edge of a panoramic radiograph with 6-inch systems.
RHINOLITH/ANTROLITH
Calcareous concretions that occur in the nose (rhinoliths) or the antrum of the maxillary sinus (antroliths) arise from the deposition of nasal, lacrimal, and inflammatory mineral salts such as calcium phosphate, calcium carbonate, and magnesium by accretion around a nidus. In cases of rhinolith, the nidus is usually an exogenous foreign body (coins, beads, etc.), especially in the pediatric population. The route of entry is usually anterior, but some may enter the choana posteriorly during sneezing, coughing, or emesis. The nidus for an antrolith is usually endogenous (root tip, bone fragment, blood clot, inspissated mucus, etc.), especially in the adult population.
Clinical Features
The patient may be asymptomatic for extended periods of time, but the expanding mass may impinge on the mucosa, producing pain, congestion, and ulceration. The patient may have a unilateral purulent rhinorrhea, sinusitis, headache, epistaxis, anosmia, fetor, and fever.
Radiographic Features
Location.: Rhinoliths develop in the nose (Fig. 28-11), whereas antroliths develop in the antrum of the maxillary sinus (see Fig. 27-10).
Metastatic Calcification
Calcification of the soft tissues in the oral region caused by conditions involving elevated serum calcium and phosphate levels, such as hyperparathyroidism (see Chapter 25) or hypercalcemia of malignancy, are extremely rare.
OSSIFICATION OF THE STYLOHYOID LIGAMENT
Embryologically, the styloid process arises from the second branchial arch (Reichert cartilage), which consists of four sections that give rise to the stylohyoid complex. Ossification of the stylohyoid ligament usually extends downward from the base of the skull and commonly occurs bilaterally. However, in rare cases the ossification begins at the lesser horn of the hyoid and in fewer still in a central area of the ligament.
Clinical Features
The ossified ligament usually can be detected by palpation over the tonsil as a hard, pointed structure. Only a minority of patients have symptoms and there is very little correlation between the extent of ossification and the intensity of the accompanying symptoms. Symptoms related to this ossified ligament are termed Eagle syndrome, which is expressed as one of two subtypes: classic Eagle syndrome resulting from cranial nerve impingement, and the carotid artery syndrome, resulting from impingement on the carotid vessels. When this entity is associated with discomfort and the patient has a recent history of neck trauma (typically tonsillectomy), the condition is called classic Eagle syndrome. The ossified stylohyoid complex and local scar tissue are thought to cause symptoms by impinging on cranial nerves V, VII, IX, X, or XII, all of which pass in close proximity to the styloid process. Symptoms may include vague, nagging to intense pain in the pharynx on swallowing, turning the head, or opening the mouth, especially on yawning, and tinnitus or otalgia. Clinical findings without a history of neck trauma constitute carotid artery syndrome. The patient may describe referred pain along the distribution of the external (ECA) or internal carotid artery (ICA). This is the result of mechanical impingement of the involved artery and stimulation of its sympathetic nerve plexus. When the ECA is impinged and stimulated, the patient may feel suborbital facial pain. Symptoms when the ICA is affected may include eye pain, temporal or parietal headache, aphasia, visual symptoms, weakness, and transient hemispheric ischemia with vertigo or syncope, notably on turning the head to the ipsilateral side. In these patients, pain is produced by mechanical irritation of sympathetic nerve tissue in the arterial wall, producing regional carotidynia. This may occur even in the absence of ossification of the stylohyoid complex. Only deviation of the styloid process, usually medially, is required for the tip of the process to impinge an artery. These individuals usually are older than 40 years. This condition is more prevalent than classic Eagle syndrome.
Radiographic Features
Ossification of the stylohyoid ligament is detected fairly commonly as an incidental feature on panoramic radiographs. In one study, approximately 18% of a population examined showed ossification of more than 30 mm of the stylohyoid ligament. The ligament may have at least some calcification in individuals of any age.
Location.: In a panoramic image the linear ossification extends forward from the region of the mastoid process and crosses the posteroinferior aspect of the ramus toward the hyoid bone. The hyoid bone is positioned roughly parallel to or superimposed on the posterior aspect of the inferior cortex of the mandible.
Shape.: The styloid process appears as a long, tapering, thin, radiopaque process that is thicker at its base and projects downward and forward (Fig. 28-12). It normally varies from about 0.5 to 2.5 cm in length. The ossified ligament has roughly a straight outline, but in some cases some irregularity may be seen in the outer surface. The farther the radiopaque ossified ligament extends toward the hyoid bone, the more likely it is that it will be interrupted by radiolucent, jointlike junctions (pseudoarticulations).
Differential Diagnosis
The symptoms accompanying stylohyoid ligament ossification and Eagle syndrome or stylohyoid syndrome generally are vague; however, when they occur with the distinctive radiographic evidence of ligament ossification, little chance exists that the complaint will be confused with another entity. Occasionally, though, the symptoms may be similar to those seen in temporomandibular joint dysfunction.
Management
Most patients with ossification of the stylohyoid ligament are asymptomatic, and no treatment is required. For patients with vague symptoms, a conservative approach of reassurance and steroid or lidocaine injections into the tonsillar fossa would be recommended initially. However, for patients with persistent or intense symptoms, the recommended treatment is amputation of the stylohyoid process (stylohyoidectomy).
OSTEOMA CUTIS
Osteoma cutis is a rare soft tissue ossification in the skin. Approximately 85% of cases occur as a result of acne of long duration, developing in a scar or chronic inflammatory dermatosis. Histologically these lesions are areas of dense viable bone in the dermis or subcutaneous tissue. They occasionally are found in diffuse scleroderma, replacing the altered collagen in the dermis and subcutaneous septa.
Clinical Features
Osteoma cutis can occur anywhere, but the face is the most common site. The tongue is the most common intraoral site (osteoma mucosae or osseous choristoma). Osteoma cutis does not cause any visible change in the overlying skin other than an occasional color change that may appear yellowish white. If the lesion is large, the individual osteoma may be palpated. A needle inserted into one of the papules is met with stonelike resistance. Some patients have numerous (dozens to hundreds) of lesions, usually on the face in females and on the scalp or chest in males. This form is known as multiple miliary osteoma cutis.
Radiographic Features
Location.: Radiographically, osteoma cutis most commonly appears in the cheek and lip regions (Fig. 28-13). In this location the image can be superimposed over a tooth root or alveolar process, giving the appearance of an area of dense bone. Accurate localization can be achieved by placing an intraoral film between the cheek and alveolar process to image the cheek alone. As an alternative, a posteroanterior skull view with the cheek blown outward by use of a soft tissue technique of 60 peak kilovolts helps localize osteomas in the skin.
Periphery and Shape.: Osteoma cutis appears as smoothly outlined, radiopaque, washer-shaped images. These single or multiple radiopacities usually are very small, although the size can range from 0.1 to 5 cm.
Internal Structure.: The internal aspect may be homogeneously radiopaque but usually has a radiolucent center that represents normal fatty marrow, giving the lesion a donut appearance radiographically. Trabeculae occasionally develop in the marrow cavity of larger osteomas. Individual lesions of calcified cystic acne resemble a snowflakelike radiopacity, which corresponds to the clinical location of the scar.
Differential Diagnosis
The differential diagnosis should include myositis ossificans, calcinosis cutis, and osteoma mucosae. If the blown-out cheek technique is used, the lesions of osteoma cutis appear much more superficial than mucosal lesions. Myositis ossificans is of greater proportions, in some cases causing noticeable deformity of the facial contour.
Management
No treatment is required, but these osteomas occasionally are removed for cosmetic reasons. Resurfacing of the skin with the erbium:yttrium-aluminum-garnet laser with tretinoin cream has been successful in treating multiple miliary osteoma cutis. More recently, good cosmetic results have been reported with a needle microincision-extirpation technique in patients with multiple miliary osteoma cutis.
MYOSITIS OSSIFICANS
In myositis ossificans; fibrous tissue and heterotopic bone form within the interstitial tissue of muscle and associated tendons and ligaments. Secondary destruction and atrophy of the muscle occur as this fibrous tissue and bone interdigitate and separate the muscle fibers. There are two principal forms: localized and progressive.
Definition
Localized myositis ossificans results from acute or chronic trauma or from heavy muscular strain caused by certain occupations and sports. Muscle injury from multiple injections (occasionally from dental anesthetic) also may be a cause. Skeletal muscle has limited capacity for regeneration after significant physical trauma. The injury leads to considerable hemorrhage into the muscle or associated tendons/fascia. It has been proposed that exuberant proliferation of vascular granulation tissue subsequently undergoes metaplasia to cartilage and bone during the healing process. The term myositis is misleading because no inflammation is involved. The fibrous tissue and bone form within the interstitial tissue of the muscle; no actual ossification of the muscle fibers occurs.
Clinical Features
Localized myositis ossificans can develop at any age in either sex, but it occurs most often in young men who engage in vigorous activity. The site of the precipitating trauma remains swollen, tender, and painful much longer than expected. The overlying skin may be red and inflamed, and when the lesion involves a muscle of mastication, opening the jaws may be difficult. After about 2 or 3 weeks, the area of ossification becomes apparent in the tissues; a firm intramuscular mass can be palpated. The localized lesion may enlarge slowly, but eventually it stops growing. The lesion may appear fixed, or it may be freely movable on palpation.
Radiographic Features
Location.: The most commonly involved muscles of the head and neck are the masseter and sternocleidomastoid. However, other muscles of mastication may be involved, such as the medial and lateral pterygoid and the temporalis muscles. The anterior attachments of the temporalis as well as the medial pterygoid muscles are at risk of injury on administration of mandibular block anesthesia. Usually a radiolucent band can be seen between the area of ossification and adjacent bone, and the heterotopic bone may lie along the long axis of the muscle (Fig. 28-14).
Periphery and Shape.: The periphery commonly is more radiopaque than the internal structure. There is a variation in shape from irregular oval to linear streaks (pseudotrabeculae) running in the same direction as the normal muscle fibers. These pseudotrabeculae are characteristic of myositis ossificans and strongly imply a diagnosis.
Internal Structure.: The internal structure varies with time. Within the third or fourth week after injury, the radiographic appearance is a faintly homogeneous radiopacity. This organizes further, and by 2 months a delicate lacy or feathery radiopaque internal structure develops. These changes indicate the formation of bone; however, this bone does not have a normal-appearing trabecular pattern. Gradually the image becomes denser and better defined, maturing fully in about 5 to 6 months. After this period the lesion may shrink.
Differential Diagnosis
The differential diagnosis of localized myositis ossificans includes ossification of the stylohyoid ligament and other soft tissue calcifications. However, both the form and location of myositis ossificans often are enough to make the differential diagnosis. Other lesions to consider are bone-forming tumors. Although tumors such as osteogenic sarcoma can form a linear bone pattern (see Chapter 23), the tumor is contiguous with the adjacent bone, and signs of bone destruction often are present.
Management
Rest and limitation of use are recommended to diminish the extent of the calcific deposit. Surgical excision of the entire calcified mass with intensive physiotherapy to minimize postsurgical scarring is the recommended treatment.
Definition
Progressive myositis ossificans is a rare hereditary disease with autosomal dominant transmission, but less commonly it arises as a result of spontaneous mutation. It is more common in males and causes symptoms from early infancy. Progressive formation of heterotopic bone occurs within the interstitial tissue of muscles, tendons, ligaments, and fascia, and the involved muscles atrophy.
Clinical Features
In most cases the heterotopic ossification starts in the muscles of the neck and upper back and moves to the extremities. The disease commences with soft tissue swelling that is tender and painful and may show redness and heat, indicating the presence of inflammation. The acute symptoms subside, and a firm mass remains in the tissues. This condition may affect any of the striated muscles, including the heart and diaphragm. In some cases the spread of ossification is limited; in others it becomes extensive, affecting almost all the large muscles of the body. Stiffness and limitation of motion of the neck, chest, back, and extremities (especially the shoulders) gradually increase. Functional deficits are progressive and handicapping. Advanced stages of the disease result in the “petrified man” condition. During the third decade the process may spontaneously arrest; however, most patients die during the third or fourth decades. Premature death usually results from respiratory embarrassment or from inanition through the involvement of the muscles of mastication.
Radiographic Features
The radiographic appearance of progressive myositis ossificans is similar to that described for the limited form. The heterotopic bone more commonly is oriented along the long axis of the involved muscle (Fig. 28-15). Osseous malformation of the regions of muscle attachment, such as the mandibular condyles, also may be seen.
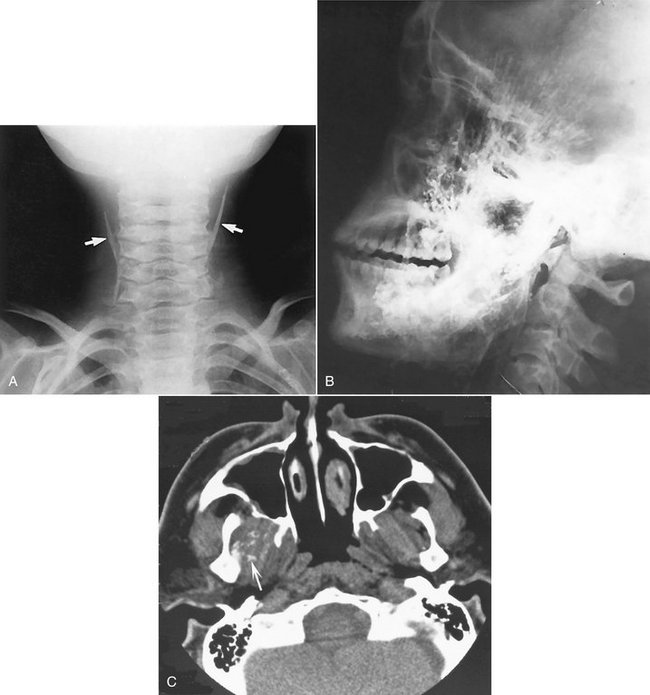
FIG. 28-15 A, Myositis ossificans, seen as bilateral linear calcifications (arrows) of the sternohyoid muscle. B, Extensive ossification of the masseter and temporalis muscles. C, An axial CT scan with soft tissue algorithm demonstrating calcifications in the lateral pterygoid muscle (arrow). (A courtesy Dr. H. Worth, Vancouver, British Columbia; B from Shawkat AH: Myositis ossificans: report of a case, Oral Surg 23:751-754, 1967.)
Differential Diagnosis
In the initial stages of the disease, distinguishing between progressive myositis ossificans and rheumatoid arthritis may be difficult. However, the presence of specific anomalies suggests the diagnosis. In the case of calcinosis, the deposits of amorphous calcium salts frequently resorb, but in progressive myositis ossificans, the bone never disappears.
Banks, K, Bui-Mansfield, L, Chew, F, et al. A compartmental approach to the radiographic evaluation of soft-tissue calcifications. Semin Roentgenol. 2005;40:391–407.
Carter, L. Clinical indications as a basis for ordering extraoral imaging studies. Compendium. 2004;25:95–102.
Keberle, M, Robinson, S. Physiologic and pathologic calcifications and ossifications in the face and neck. Eur Radiol. 2007;17:2103–2111.
Monsour, PA, Romaniuk, K, Hutchings, RD. Soft tissue calcifications in the differential diagnosis of opacities superimposed over the mandible by dental panoramic radiography. Aust Dent J. 1991;36:94–101.
Worth, HM. Principles and practice of oral radiologic interpretation. St. Louis: Mosby; 1963.
Eisenkraft, B, Som, P. The spectrum of benign and malignant etiologies of cervical node calcification. AJR Am J Roentgenol. 1999;172:1433–1437.
Paquette, M, Terezhalmy, G, Moore, W. Calcified lymph nodes. Quint Int. 2003;34:562–563.
DYSTROPHIC CALCIFICATION IN THE TONSILS
Ansai, T, Takehara, T. Tonsillolith as a halitosis-inducing factor. Br Dent J. 2005;198:263–264.
Dal Rio, A, Franchi-Teixeira, A, Nicola, E. Relationship between the presence of tonsilloliths and halitosis in patients with chronic caseous tonsillitis. Br Dent J. 2007. Published on-line November 23
Mandel, L. Multiple bilateral tonsilloliths: case report. J Oral Maxillofac Surg. 2008;66:148–150.
Delgado-Azañero, WA, Mosqueda-Taylor, A, Carlos-Bregni, R, et al. Oral cysticercosis: a collaborative study of 16 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:528–533.
Ribeiro, A, Luvizotto, M, Soubhia, A, et al. Oral cysticercosis: case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e56–e58.
Almog, DM, Horev, T, Illig, K, et al. Correlating carotid artery stenosis detected by panoramic radiography with clinically relevant carotid artery stenosis determined by duplex ultrasound. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:768–773.
Carter, LC, Tsimidis, K, Fabiano, J. Carotid calcifications on panoramic radiography identify an asymptomatic male patient at risk for stroke: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:119–122.
Friedlander, AH, Altman, L. Carotid artery atheromas in postmenopausal women: their prevalence on panoramic radiographs and their relationship to atherogenic risk. J Am Dent Assoc. 2001;132:1130–1136.
Mupparapu, M, Kim, I. Calcified carotid artery atheroma and stroke. J Am Dent Assoc. 2007;138:483–492.
Güneri, P, Kaya, A, Caliskan, M. Antroliths: survey of the literature and report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:517–521.
Kaushik, V, Bhalla, R, Pahade, A. Rhinolithiasis. ENT Ear Nose Throat J. 2004;83:512. 514
Munoz, A, Pedrosa, I, Villafruela, M. “Eraseroma” as a cause of rhinolith: CT and MRI in a child. Neuroradiology. 1997;39:824–826.
Orhan, K, Kocyigit, D, Kisnisci, R, et al. Rhinolithiasis: an uncommon entity of the nasal cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;101:e28–e32.
Pinto, LS, Campagnoli, EB, de Souza Azevedo, R, et al. Rhinoliths causing palatal perforation: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e42–e46.
Ho, V, Currie, WJ, Walker, A. Sialolithiasis of minor salivary glands. Br J Oral Maxillofac Surg. 1992;30:273–275.
McGurk, M, Escudier, M, Thomas, B, et al. A revolution in the management of obstructive salivary gland disease. Dent Update. 2006;33:28–30.
Nahlieli, O, Nakar, L, Nazarian, Y, et al. Sialoendoscopy: a new approach to salivary gland obstructive pathology. J Am Dent Assoc. 2006;137:1394–1400.
Nakayama, E, Okamura, K, Mitsuyasu, T, et al. A newly developed interventional sialendoscope for a completely nonsurgical sialolithectomy using intracorporeal electrohydraulic lithotripsy. J Oral Maxillofac Surg. 2007;65:1402–1405.
Williams, MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32:819–834.
Altug, H, Büyüksoy, V, Okçu, K, Dogan, N. Hemangiomas of the head and neck with phleboliths: clinical features, diagnostic imaging, and treatment of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e60–e64.
Chuang C-C, Lin H-C, Huang, C-W. Submandibular cavernous hemangiomas with multiple phleboliths masquerading as sialolithiasis. J Chin Med Assoc. 2005;68:441–443.
Kakimoto, N, Tanimoto, K, Nishiyama, H, et al. CT and MR imaging features of oral and maxillofacial hemangioma and vascular malformation. Eur J Radiol. 2005;55:108–112.
Ahmad, M, Madden, R, Perez, L. Triticeous cartilage: prevalence on panoramic radiographs and diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:225–230.
Carter, L. Discrimination between calcified triticeous cartilage and calcified carotid atheroma on panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:108–110.
Mupparrapu, M, Vuppalapati, A. Ossification of laryngeal cartilages on lateral cephalometric radiographs. Angle Orthod. 2005;75:196–201.
Bafaqeeh, SA. Eagle syndrome: classic and carotid artery types. J Otolaryngol. 2000;29:88–94.
Balbuena, L, Hayes, D, Ramirez, SG, et al. Eagle’s syndrome (elongated styloid process). South Med J. 1997;90:331–334.
Chuang, WC, Short, JH, McKinney, AM, et al. Reversible left hemispheric ischemia secondary to carotid compression in Eagle syndrome: surgical and CT angiographic correlation. AJNR Am J Neuroradiol. 2007;28:143–145.
Eagle, WW. Elongated styloid process, symptoms and treatment. AMA Arch Otolaryngol. 1958;67:172–176.
Baskan, EB, Turan, H, Tunali, S, et al. Miliary osteoma cutis of the face: treatment with the needle microincision-extirpation method. J Dermatol Treat. 2007;18:252–254.
Farhood, V, Steed, DL, Krolls, SO. Osteoma cutis: cutaneous ossification with oral manifestations. Oral Surg. 1978;45:98–103.
Hughes, PS. Multiple miliary osteomas of the face ablated with the erbium:YAG laser. Arch Dermatol. 1999;135:378–380.
Shigehara, H, Honda, Y, Kishi, K, et al. Radiographic and morphologic studies of multiple miliary osteomas of cadaver skin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:121–125.
Thielen, AM, Stucki, L, Braun, RP, et al. Multiple cutaneous osteomas of the face associated with chronic inflammatory acne. J Eur Acad Dermatol Venereol. 2006;20:321–326.
Kaplan, FS, McCluskey, W, Hahn, G, et al. Genetic transmission of fibrodysplasia ossificans progressive: report of a family. J Bone Joint Surg Am. 1993;75:1214–1220.
Sarac, S, Sennaroglu, L, Hosal, AS, et al. Myositis ossificans in the neck. Eur Arch Otorhinolaryngol. 1999;256:199–201.
Spinazze, R, Heffez, L, Bays, R. Chronic progressive limitation of mouth opening. J Oral Maxillofac Surg. 1998;56:1178–1186.
St.-Hilaire, H, Weber, W, Ramer, M, et al. Clinicopatholgic conference: trismus following dental treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:261–266.