Nonneoplastic Diseases of Bone
After studying this chapter, the student will be able to:
1 Define benign fibro-osseous lesions.
2 Define dysplasia as it relates to bone diseases and differentiate the term from epithelial dysplasia.
3 List the benign fibro-osseous lesions that occur in the jawbones.
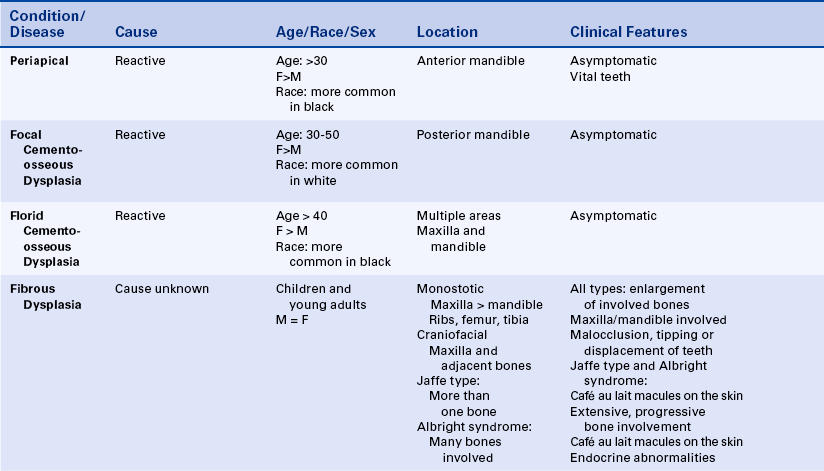
4 Describe the clinical, radiographic, and microscopic features of periapical cemento-osseous dysplasia, focal cemento-osseous dysplasia, and florid cemento-osseous dysplasia.
5 Compare and contrast periapical cemento-osseous dysplasia, focal cemento-osseous dysplasia, and florid cemento-osseous dysplasia.
6 Compare and contrast monostotic fibrous dysplasia with polyostotic fibrous dysplasia.
7 Compare and contrast the radiographic appearance, histologic appearance, and treatment of fibrous dysplasia of the jaws with those of ossifying fibroma of the jaws.
8 Compare and contrast the three types of polyostotic fibrous dysplasia.
9 Describe the histologic appearance of Paget disease of bone and describe its clinical and radiographic appearance when the maxilla or mandible is involved.
10 Describe the clinical, radiographic and microscopic features of the central giant cell granuloma.
Nonneoplastic diseases of bone that affect the maxilla and mandible fall into multiple categories. Inherited diseases that affect bone are discussed in Chapter 6, and benign and malignant neoplasms of bone, including central and peripheral cementifying and ossifying fibromas, are discussed in Chapter 7. Central and peripheral giant cell granulomas are included in Chapter 2, and aneurysmal bone cyst is included in Chapter 5. The purpose of this chapter is to delineate several other nonneoplastic diseases of bone that are important for a dental hygienist to understand but are not covered elsewhere in this text. These include three forms of cemento-osseous dysplasia: (1) periapical, (2) focal, and (3) florid. In addition, the dental hygienist should also be familiar with the various types of fibrous dysplasia and the clinical and radiographic features of Paget disease and osteomalacia.
The term dysplasia as used in this chapter in the context of the cemento-osseous dysplasias and fibrous dysplasia refers to the disordered production of cementum and bone. This term in this context should not be confused with dysplasia as used in the context of epithelial dysplasia. Epithelial dysplasia connotes a premalignant condition affecting squamous epithelium.
BENIGN FIBRO-OSSEOUS LESIONS
Benign fibro-osseous lesions that affect the maxilla and mandible include central and peripheral cementifying and ossifying fibromas (see Chapter 7), periapical cemento-osseous dysplasia, focal cemento-osseous dysplasia, florid cemento-osseous dysplasia, and fibrous dysplasia (Box 8-1).
PERIAPICAL CEMENTO-OSSEOUS DYSPLASIA
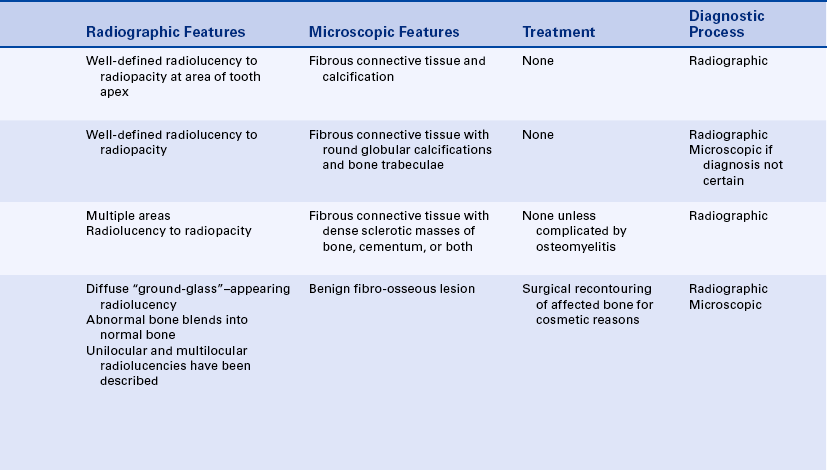
Periapical cemento-osseous dysplasia is a relatively common disease of unknown cause that affects periapical bone (Figure 8-1, A and B). The term cementoma is often used for this disease. However, because the disease does not represent a neoplasm, this term is inappropriate and should be avoided.
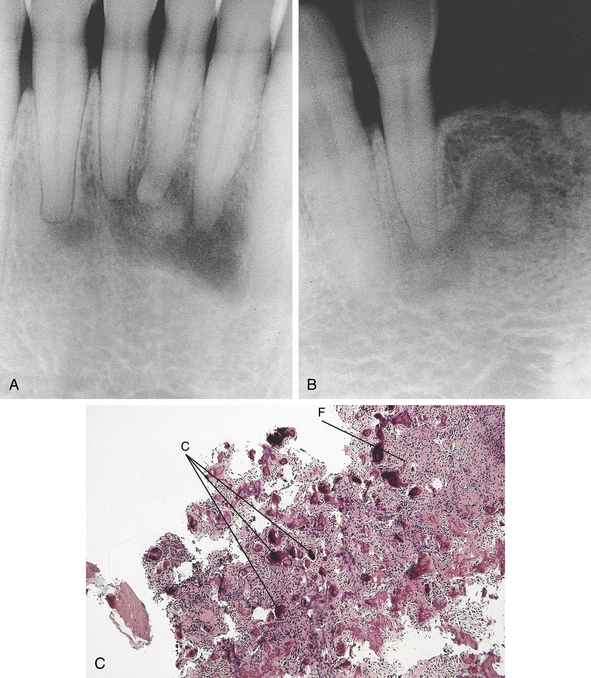
FIGURE 8-1 A and B, Radiographs of periapical cemento-osseous dysplasia. C, Microscopic appearance of periapical cemento-osseous dysplasia shows a combination of cellular fibrous connective tissue (F) and calcified tissue (C).
The lesion is asymptomatic and is discovered on routine radiographic examination. It occurs most commonly in the anterior mandible of patients older than 30 years of age. It is more common in women than men. Many studies have shown a predilection for this disease in black women. Early lesions are well circumscribed and radiolucent and may mimic periapical disease. Teeth in the affected area are vital unless they are coincidentally carious or have been traumatized. With time the lesions become increasingly calcified; therefore older lesions are radiolucent with central opacifications.
The diagnosis of periapical cemento-osseous dysplasia is usually established on the basis of observation of its characteristic clinical and radiographic features. A biopsy may be necessary in cases in which the characteristic radiographic features are not evident. Histologic examination reveals a fibro-osseous lesion. Like other fibro-osseous lesions, periapical cemento-osseous dysplasia is composed of a combination of fibrous tissue and calcifications. The calcifications in this lesion may resemble bone, cementum, or both. Early lesions consist mainly of fibrous tissue, whereas older lesions contain fibrous connective tissue interspersed with numerous calcifications (Figure 8-1, C). If a patient demonstrates radiographic changes characteristic of an early lesion, close follow-up examinations may be necessary to ensure that a correct diagnosis was established. Once the condition is recognized, no treatment is necessary. The lesion remains asymptomatic and localized.
FOCAL CEMENTO-OSSEOUS DYSPLASIA
Focal cemento-osseous dysplasia is an asymptomatic fibro-osseous lesion that shares similar histologic features with periapical cemento-osseous dysplasia and florid cemento-osseous dysplasia. However, it differs from these two lesions in that it has unique clinical and radiographic features.
Focal cemento-osseous dysplasia usually occurs in women between 30 and 50 years of age; and, unlike periapical and florid cemento-osseous dysplasia, it is reported to be more common in white than black individuals. It typically arises in the posterior mandible and appears as an isolated, well-delineated radiolucent-to-radiopaque lesion that is less than 1.5 cm in size.
Biopsy and histologic examination usually are necessary to establish a diagnosis of focal cemento-osseous dysplasia. A characteristic surgical feature of focal cemento-osseous dysplasia is that it is composed of numerous gritty pieces of soft and hard tissue. This finding is distinctly different from the characteristic surgical features of a central cementifying or ossifying fibroma. These latter tumors present as a circular mass of hard tissue that separates easily from the adjacent normal bone. The gritty tissue removed from focal cemento-osseous dysplasia represents fibrous connective tissue interspersed with bone trabeculae and cementum-like material. Once a definitive diagnosis has been established, no further treatment is necessary. The prognosis for focal cemento-osseous dysplasia is excellent. Occasionally this lesion has progressed to florid cemento-osseous dysplasia.
FLORID CEMENTO-OSSEOUS DYSPLASIA
Florid cemento-osseous dysplasia is another fibro-osseous lesion characterized by disordered cementum and bone development. This lesion characteristically involves multiple quadrants in the maxilla and mandible.
Florid cemento-osseous dysplasia occurs most often in black women older than 40 years of age. The cause of this disease is unknown. Radiographically it differs from periapical cemento-osseous dysplasia in that it typically affects more than one quadrant of the maxilla and mandible, often in the posterior areas. Occasionally an early radiolucent phase similar to that seen in periapical cemento-osseous dysplasia may be identified. However, the majority of cases are composed of masses of irregular opacification. (Figure 8-2).
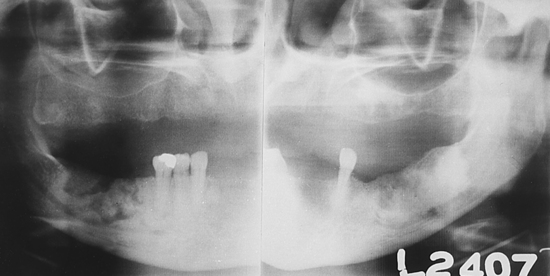
FIGURE 8-2 Florid cemento-osseous dysplasia. Pantomographic radiograph shows irregular radiopaque masses in both the left and right mandible.
Florid cemento-osseous dysplasia is often diagnosed on the basis of its characteristic clinical presentation and radiographic appearance. Because of these findings, treatment is often unnecessary. However, in an edentulous patient the sclerotic masses may perforate the mucosa, resulting in a communication between the oral environment and the underlying bone. This complication may lead to the development of an osteomyelitis, necessitating antibiotic therapy and surgical intervention.
FIBROUS DYSPLASIA
Fibrous dysplasia is a disease that is characterized by the replacement of bone with abnormal fibrous connective tissue interspersed with varying amounts of calcification. Although the cause is unknown, several theories have been proposed. One of the most widely accepted theories is that the unusual fibrous proliferation is the result of abnormal mesenchymal cell function. Several types of fibrous dysplasia exist; each type shares similar microscopic features, but the clinical presentation and associated systemic signs and symptoms differ. Histologically fibrous dysplasia is classified as a benign fibro-osseous lesion. It is composed of vascularized, cellular fibrous connective tissue interspersed with irregular trabeculae of bone emerging from the connective tissue.
Types of Fibrous Dysplasia
Monostotic fibrous dysplasia, the most common type of fibrous dysplasia, is characterized by involvement of a single bone. The mandible and maxilla are commonly affected, and the maxilla is more frequently involved than the mandible. Other bones may be affected, including the ribs, femur, and tibia. Monostotic fibrous dysplasia is most commonly diagnosed in children and young adults; no sex predilection is seen. Clinical examination reveals a painless swelling or bulging of the buccal plate of the maxilla or mandible. The expanding nature of the lesion may lead to malocclusion, tipping, or displacement of adjacent teeth. However, the teeth are rarely mobile.
Polyostotic Fibrous Dysplasia
Polyostotic fibrous dysplasia is characterized by involvement of more than one bone. It typically occurs in children, and a definite female gender predilection is seen. The skull, clavicles, and long bones are often affected; and most cases are asymptomatic. When the long bones are involved, they may exhibit bowing and an associated dull aching pain. Patients with polyostotic fibrous dysplasia often demonstrate skin lesions. These lesions appear as light-brown macules called café au lait spots. Several forms of polyostotic fibrous dysplasia exist. Craniofacial fibrous dysplasia is the term used for polyostotic fibrous dysplasia that involves the maxilla with extension into the sinuses and adjacent zygoma, sphenoid, and occipital bones. Another form of polyostotic fibrous dysplasia is called the Jaffe type (or Jaffe-Lichtenstein type). It involves multiple bones along with associated café au lait macules on the skin. The most severe form of polyostotic fibrous dysplasia is called Albright syndrome (or McCune-Albright syndrome). This condition is characterized by endocrine abnormalities, including precocious puberty in females, and stunting or deformity of skeletal growth in both sexes as a result of early epiphyseal plate closure. Precocious puberty is exhibited by menses, pubic hair, and breast development in children as young as 2 years of age. Other complications of Albright syndrome include diabetes mellitus and hyperthyroidism. Café au lait skin macules may occur in this form of polyostotic fibrous dysplasia.
Clinical examination reveals a painless enlargement of the affected bone or bones. Jaw involvement typically appears as a painless, progressive, unilateral enlargement of the maxilla or mandible. When fibrous dysplasia involves the maxilla, the disease usually extends into the maxillary sinuses. Involvement of the jaws may occur in any type of fibrous dysplasia. The classic radiographic appearance of fibrous dysplasia is a diffuse radiopacity that is described as “looking like ground glass” (Figure 8-3, A). The abnormal bone blends into the adjacent normal bone, making it difficult to determine the periphery of the lesion. A unilocular or multilocular radiolucency, a patchy radiolucency with central opacifications, and a dense radiopacity have also been observed in fibrous dysplasia. The radiolucent or radiopaque appearance of fibrous dysplasia depends on the degree of calcification present in the lesion. Lesions that are primarily radiolucent contain an abundance of fibrous connective tissue with few calcifications, whereas more radiopaque lesions are composed predominantly of calcified tissue and a scant amount of fibrous connective tissue.
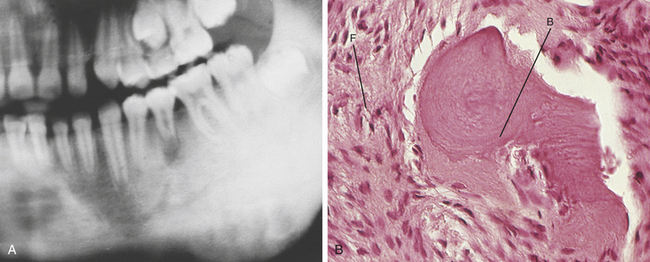
FIGURE 8-3 Fibrous dysplasia. A, Radiograph of fibrous dysplasia demonstrating indistinct borders that blend into the adjacent normal bone. B, Microscopic appearance (high power) of fibrous dysplasia shows cellular fibrous connective tissue (F) and irregular trabeculae of bone (B). (A courtesy Drs. Paul Freedman and Stanley Kerpel.)
The diagnosis of fibrous dysplasia is established by correlating the microscopic findings along with the characteristic clinical features and radiographic appearance. Histologic examination reveals a benign fibro-osseous lesion (Figure 8-3, B). The microscopic appearance is characterized by cellular fibrous connective tissue interspersed with irregularly shaped bone trabeculae. Fibrous dysplasia of the maxilla or mandible is distinguished from a central cementifying or ossifying fibroma on the basis of review of the radiographic findings. In fibrous dysplasia the radiographic changes blend into the surrounding normal bone. In a central cementifying or ossifying fibroma, a tumor that can demonstrate microscopic features similar to fibrous dysplasia, the radiographic findings consist of a well-delineated lesion that is easily delineated from the surrounding normal bone. Likewise other fibro-osseous lesions such as periapical cemento-osseous dysplasia and florid cemento-osseous dysplasia can be distinguished from fibrous dysplasia on the basis of an examination of their distinct clinical and radiographic features. Fibrous dysplasia is treated surgically by recontouring the affected bone for cosmetic reasons. No treatment exists for severe and progressive polyostotic fibrous dysplasia. Radiation treatment of fibrous dysplasia is contraindicated because it has been associated with malignant transformation.
PAGET DISEASE OF BONE
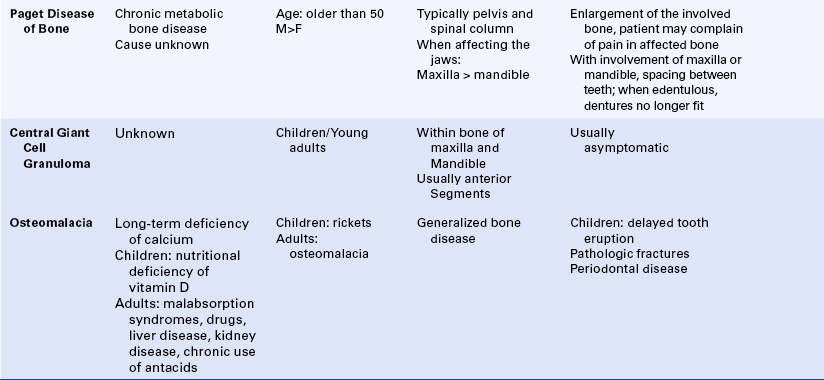
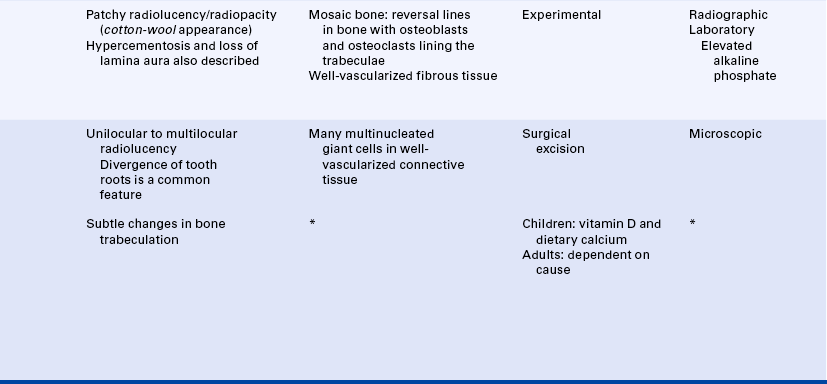
Paget disease of bone, also called osteitis deformans and leontiasis ossea, is a chronic metabolic bone disease. It is characterized by resorption, osteoblastic repair, and remineralization of the involved bone. The cause is unknown. Several theories have been proposed, and a viral cause is suspected. The disease occurs most commonly in men over the age of 50. It typically involves the pelvis and spinal column. When found in the jawbones, the maxilla is more commonly affected than the mandible.
The clinical manifestations of Paget disease depend on the bone involved. Enlargement of the affected bone is common, and the patient often complains of pain. When the maxilla or mandible is involved, spacing between the teeth increases as the bone enlarges (Figure 8-4, A). Edentulous patients may complain that their dentures no longer fit. When other bones of the skull are involved, clinical manifestations include severe headache, dizziness, and deafness. These symptoms occur because the enlarging bone impinges on cranial nerves as they exit the skull. The classic radiographic appearance is a patchy radiolucency and radiopacity that has been referred to as a cotton-wool appearance (Figure 8-4, B). However, this only occurs in the later stages of Paget disease. In earlier stages the radiographic appearance is not as unique. Hypercementosis, loss of the lamina dura, and obliteration of the periodontal ligament may also occur.

FIGURE 8-4 Paget disease. A, Enlargement of the maxilla with spaces between the teeth. B, Radiograph demonstrating irregular opacification that is also referred to as a cotton-wool appearance. In areas, the lamina dura is obliterated. C, Microscopic appearance of Paget disease shows bone trabeculae surfaced by numerous osteoclasts and osteoblasts. The prominent reversal lines (arrows) seen here characterize the mosaic bone pattern of bone.
Laboratory evaluation is important in establishing the diagnosis of Paget disease. The serum alkaline phosphatase level is significantly elevated in active disease. Two different measurements are used to evaluate the serum alkaline phosphatase level. In Bodansky units the normal serum alkaline phosphatase value is 1.5 to 5.0. In Paget disease the serum alkaline phosphatase value can be as high as 250 Bodansky units. Another measurement used for evaluating the serum alkaline phosphatase level is the King-Armstrong unit (KAU). Normal values are 5 to 10 KAU. In patients with Paget disease KAU values may be as high as 200. Histologic examination reveals bone trabeculae surfaced by numerous osteoclasts and osteoblasts (Figure 8-4, C). The involved bone demonstrates prominent reversal lines that result from the resorption and deposition of bone; this pattern has been described as mosaic bone. The connective tissue between the bone trabeculae is so well vascularized that the overlying skin may feel warm when touched. Treatment of Paget disease is experimental. The disease is slowly progressive. Complications include fracture of the involved bone and development of malignant tumors, particularly osteosarcoma. Heart disease is a rare complication of Paget disease.
CENTRAL GIANT CELL GRANULOMA (CENTRAL GIANT CELL LESION)
The giant cell granuloma is a non-neoplastic lesion of unclear pathogenesis. It has also been called a giant cell reparative granuloma; however, evidence that this lesion represents a reparative response is lacking. The giant cell granuloma is composed of well vascularized connective tissue containing many multinucleated giant cells. Red blood cells and chronic inflammatory cells are also seen in this lesion. The giant cell granuloma occurs in both peripheral (gingival or alveolar mucosa) and central (located within the bone of the maxilla or mandible) locations. The peripheral giant cell granuloma is described in Chapter 2.
The central giant cell granuloma occurs within the bone of the maxilla or mandible, primarily in children and young adults. Studies have reported its occurrence more commonly in females than in males. These lesions are common in the anterior segments of the maxilla and mandible and are uncommon in the ramus of the mandible. Patients with central giant cell granulomas may complain of discomfort from the lesions, but pain is not a common feature. Most central giant cell granulomas are discovered on routine radiographs. The lesion is slow growing and destructive and produces a radiolucency in the bone. The borders of the radiolucency may be either sclerotic or ill defined, and they may be unilocular or multilocular (Figure 8-5). Divergence of the roots of teeth adjacent to the lesion is a common feature of central giant cell granuloma. Lesions are treated by surgical removal and occasionally recur.
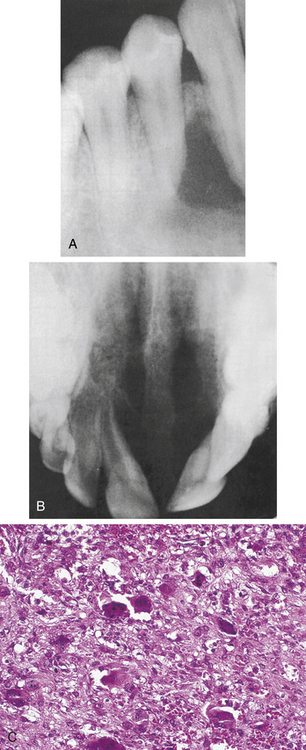
FIGURE 8-5 Radiographs of central giant cell granulomas showing multilocular radiolucencies in the mandible (A) and maxilla (B). C, Microscopic appearance of a central giant cell granuloma showing the same features as a peripheral giant cell granuloma except for the absence of surface mucosa.
A lesion of bone identical to the central giant cell granuloma (often called brown tumor) occurs in patients with hyperparathyroidism (discussed in Chapter 9). They are not surgically removed because they resolve when the underlying disease is successfully treated.
OSTEOMALACIA
Osteomalacia is a disease of bone that develops over a long period of time as the result of calcium deficiency. When this disease occurs in young children, it is usually caused by a nutritional deficiency of vitamin D, and the associated disease is termed rickets. An inherited form of vitamin D deficiency called hypophosphatemic vitamin D–resistant rickets is included in Chapter 6. In adults the disease may be related to various problems such as a malabsorption syndrome, drugs, liver and kidney disease, and the chronic use of antacids. Osteomalacia may also be induced by certain tumors.
Delayed tooth eruption and periodontal disease have been associated with osteomalacia. Changes in bone trabeculation that occur in patients with osteomalacia may be subtle and difficult to detect. Pathologic fractures may also occur.
Treatment is based on identification of the cause of the vitamin D deficiency and includes nutritional supplementation with vitamin D and dietary calcium.
Neville, B.W., et al. Oral and maxillofacial pathology, ed 3. St. Louis: Saunders; 2009.
Regezi, J.A., Sciubba, J.J., Jordan, R.C.K. Oral pathology: clinical-pathologic correlations,, ed 5. St Louis: Saunders; 2008.
Bessho, K., et al. Monostotic fibrous dysplasia with involvement of the mandibular canal. Oral Surg Oral Med Oral Pathol. 1989;68:396.
Collins, M.T. Spectrum and natural history of fibrous dysplasia of bone. J Bone Miner Res. 2006;21(Suppl 2):99.
Hadjipavlou, A.G., Gaitanis, I.N., Kontakis, G.M. Paget disease of the bone and its management. J Bone Joint Surg. 2002;84:160.
MacDonald-Jankowski, D.S. Fibro-osseous lesions of the face and jaws. Clin Radiol. 2004;59:11.
Regezi, J.A. Odontogenic cysts, odontogenic tumors, fibro-osseous, and giant cell lesions of the jaws. Mod Pathol. 2002;15:331.
Singer, S.R., et al. Florid cemento-osseous dysplasia and chronic diffuse osteomyelitis: report of a simultaneous presentation and review of the literature. J Am Dent Assoc. 2005;136:927.
Siris, E.S. Paget disease of bone. J Bone Miner Res. 1998;13:1061.
Summerlin, Don-John, Tomich, C.E. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol. 1994;78:611.
Whyte, M.P. Clinical practice: Paget disease of bone. New Engl J Med. 2006;355:593.
Zacharin, M. The spectrum of McCune Albright syndrome. Pediatr Endocrinol Rev. 2007;4(suppl):412.
REVIEW QUESTIONS
1. A 48-year-old black woman has multiple asymptomatic, radiopaque masses in the mandible and maxilla. No expansion of bone is noted. The most likely diagnosis is:
A Central cementifying fibromas.
B Periapical cemento-osseous dysplasia.
2. All of the following are examples of benign fibro-osseous lesions except:
3. Which of the following is characterized by precocious puberty in females?
4. Periapical cemento-osseous dysplasia is characteristically located in the:
5. Periapical cemento-osseous dysplasia is also known as a(n):
6. Which of the following diseases are associated with café au lait spots?
7. What is the name of the type of fibrous dysplasia that involves the maxilla and adjacent bones?
8. Bone resorption, osteoblastic repair, loss of the lamina dura, hypercementosis, and cotton-wool radiopacities are characteristics of:
9. The most characteristic radiographic appearance of fibrous dysplasia is described as a:
10. All of the following are histologic features seen in Paget disease except one. Which one is the exception?
11. Which of the following is diagnosed on the basis of a characteristic radiographic appearance?
12. In patients with fibrous dysplasia, which of the following is the only recommended treatment modality?
13. Which of the following is helpful in the diagnosis of Paget disease?
14. Osteomalacia is usually caused by a deficiency of:
15. Osteomalacia in children is called:
16. Which of the following diseases may be associated with malignant transformation into an osteosarcoma?
17. Which of the following diseases demonstrates multiple fragments of gritty material when it is removed from the jaws?
A Periapical cemento-osseous dysplasia
B Focal cemento-osseous dysplasia
18. Leontiasis ossea or osteitis deformans are two other names for: