Neoplasia
After studying this chapter, the student will be able to:
1 Define each of the words in the vocabulary list for this chapter.
2 Explain the difference between a benign tumor and a malignant tumor.
3 Define leukoplakia and erythroplakia.
4 Describe the clinical and histologic features of the calcifying odontogenic cyst and compare and contrast this lesion to the ameloblastoma.
5 Define the following neoplasms, describe the clinical features of each, and explain how they are treated: papilloma, squamous cell carcinoma, verrucous carcinoma, basal cell carcinoma, pleomorphic adenoma, monomorphic adenoma, adenoid cystic carcinoma, mucoepidermoid carcinoma, ameloblastoma, calcifying epithelial odontogenic tumor, adenomatoid odontogenic tumor (AOT), odontogenic myxoma, central cementifying and ossifying fibromas, benign cementoblastoma, ameloblastic fibroma, ameloblastic fibro-odontoma, odontoma, peripheral ossifying fibroma, lipoma, neurofibroma and schwannoma, granular cell tumor, congenital epulis, rhabdomyosarcoma, hemangioma, lymphangioma, Kaposi sarcoma, melanocytic nevi, malignant melanoma, torus, exostosis, osteoma, osteosarcoma, chondrosarcoma, leukemia, lymphoma, multiple myeloma, and metastatic jaw tumors.
(an′ĕplas′tik) Characterized by a loss of differentiation of cells and their orientation to one another; a characteristic of malignant tumors.
(be-nīn′) A condition that, if untreated or with symptomatic therapy, will not become life threatening.
(be-nīn′ too′mor) A tumor that is not malignant and favorable for treatment and recovery.
(kar”si-no′mah) Malignant tumor of epithelium.
(sen′tral) Occurring within bone.
(dis-pla′ze-ah) Disordered growth; alteration in size, shape, and organization of adult cells.
(en-kap′su-lt-ed) Surrounded by a capsule of fibrous connective tissue.
(ē-nū′klē- ′shŭn) Surgical removal without cutting into the lesion
′shŭn) Surgical removal without cutting into the lesion
(eksizh′ən) Surgical removal
(hi”per-kro-mat′ ik) Staining more intensely than normal.
ik) Staining more intensely than normal.
(hi”per-pla′zĕ-ah) Abnormal increase in the number of cells in an organ or tissue.
(im′yĕnō-gläb′yĕlin) A protein, also called an antibody, synthesized by plasma cells in response to a specific antigen.
(in sĭtoo) Confined to the site of origin without invasion of neighboring tissues.
(in-va′zhun) Infiltration and active destruction of surrounding tissues.
(loo-kō-pl ′kē-ah) Clinical term used to identify a white, plaquelike lesion of the oral mucosa that cannot be wiped off or diagnosed as any other disease.
′kē-ah) Clinical term used to identify a white, plaquelike lesion of the oral mucosa that cannot be wiped off or diagnosed as any other disease.
(mah-lig′nant) Resistant to treatment; able to metastasize and kill the host; describing cancer.
(mah-lig′nant too′mor) Cancer; a tumor that is resistant to treatment and may cause death; a tumor that has the potential for uncontrolled growth and dissemination or recurrence, or both.
(mă-tas′tah-sis) (plural, metastases [mĕ-tas′tah-sēz]) Transport of neoplastic cells to parts of the body remote from the primary tumor and the establishment of new tumors at those sites.
(met”ah-stat′ik too′mor) Tumor formed by cells that have been transported from the primary tumor to sites not connected with the original tumor.
(mi-tot′ik fig′ur) (mitosis [mi-to′sis]) Dividing cells caught in the process of mitosis.
(ne”o-pla′ze-ah) New growth; the formation of tumors by the uncontrolled proliferation of cells.
(nē”ō-plas′tik) Pertaining to the formation of tumors by the uncontrolled proliferation of cells.
(ne′o-plazm) Tumor; a new growth of tissue in which growth is uncontrolled and progressive.
(ne′vus) (plural, nevi [ne′vi]) Circumscribed malformation of the skin or oral mucosa presumed to be of hereditary origin; also, a benign tumor of melanocytes (nevus cells).
(o-don”to-jen′ik) Tooth forming.
(ong-kol′o-je) Study of tumors or neoplasms.
(pidungk′yēl ′tid) Attached by a stalk.
′tid) Attached by a stalk.
(pĕ-rif′er-al) Occurring outside of bone.
(ple”o-mor′fik) Occurring in various forms.
(pri′mer-e too′mor) Original tumor; the source of metastasis.
(sar-ko′mah) Malignant tumor of connective tissue.
(ses′il) Attached by a base.
(too′mor) Neoplasm; also, a swelling or enlargement.
(un-difĕr-en′shē- t′ed) Absence of normal differentiation; anaplasia; a characteristic of some malignant tumors.
t′ed) Absence of normal differentiation; anaplasia; a characteristic of some malignant tumors.
DESCRIPTION OF NEOPLASIA
Neoplasia means new growth. It is a process in which cells exhibit uncontrolled proliferation. A neoplasm is a mass of such cells. Although the word tumor means swelling, it is commonly used as a synonym for neoplasm. The study of tumors is called oncology. Onco in Greek means swelling or mass.
For neoplasia to occur, an irreversible change must take place in the cells, and this change must be passed on to new cells, resulting in uncontrolled cell multiplication. In most cases the initial stimulus that triggers the process of cell change is not known. Regulatory processes maintain the size of normal tissues. The regulatory processes that maintain the size of normal tissues do not function correctly in a neoplasm; therefore it exhibits unlimited and unregulated growth.
Like hyperplasia, which is described in Chapter 2, neoplasia is an abnormal process. With hyperplasia, normal cells proliferate in a normal arrangement in response to tissue damage, and the proliferation stops when the stimulus is removed. Although the size of the tissue may be greater than normal, the growth of the tissue is still under control. Reactive lesions such as the irritation fibroma, denture-related hyperplasia (epulis fissuratum), and the pyogenic granuloma described in Chapter 2 are examples of hyperplasia. In contrast, neoplasia is a completely abnormal process; the cells are abnormal, and the proliferation of these cells is uncontrolled and unlimited.
CAUSES OF NEOPLASIA
Many agents—principally chemicals, viruses, and radiation—have been shown to cause neoplastic transformation of cells in the laboratory. Hundreds of chemicals have been shown to cause cancer in animals. In addition, certain chemicals, viruses, and radiation have been shown to cause certain cancers in humans. Neoplastic transformation may also occur spontaneously secondary to a genetic mutation. Viruses that cause tumors are called oncogenic viruses. Radiation from sunlight, x-rays, nuclear fission, or other sources is well established as a cancer-producing agent in humans.
CLASSIFICATION OF TUMORS
Tumors are divided into two categories: benign and malignant. A benign tumor or neoplasm remains localized. It may be encapsulated, which means that it is walled off by surrounding fibrous connective tissue. Sometimes a benign tumor can invade adjacent structures, but it does not have the ability to spread to distant sites. In contrast, a malignant tumor both invades and destroys surrounding tissue and has the ability to spread throughout the body. Cancer is synonymous with malignancy.
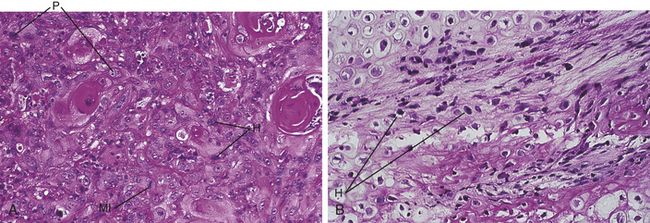
Benign tumors almost always resemble normal cells, whereas malignant tumors vary in their histologic appearance. Malignant tumors composed of neoplastic cells that resemble normal cells are called well-differentiated tumors. Malignant tumors may also be poorly differentiated. The cells of these tumors have only some of the characteristics of the tissue from which they were derived. Still others may be undifferentiated or anaplastic and do not resemble at all the tissue from which they were derived. Malignant tumors are often composed of cells that vary in size and shape (pleomorphic) (Figure 7-1). The nuclei of these cells are darker than those of normal cells (hyperchromatic) and exhibit an increased nuclear cytoplasmic ratio (see Figure 7-1). Normal and abnormal mitotic figures are seen in the nucleus of the neoplastic cells (see Figure 7-1, A). Abnormal mitotic figures are those that are not dividing normally; therefore the shape of the dividing nucleus does not follow the shape of a normal mitotic figure. Table 7-1 compares benign and malignant tumors.
Table 7-1
Comparison of Benign and Malignant Tumors
| Benign | Malignant |
| Usually well differentiated | Well differentiated to anaplastic |
| Usually slow growth | Slow-to-rapid growth |
| Mitotic figures are rare | Mitotic figures may be numerous |
| Usually encapsulated | Invasive and unencapsulated |
| No metastasis | Metastasis likely |
NAMES OF TUMORS
The prefix of the name of a tumor is determined by the tissue or cell of origin. The suffix oma is used to indicate a tumor. For example, a benign tumor of fat is called a lipoma, and a benign tumor of bone is called an osteoma. Malignant tumors are named in a similar fashion. Malignant tumors of epithelium are called carcinomas, and malignant tumors of connective tissue are called sarcomas. The prefix of the name of a malignant tumor is also determined by the tissue or cell of origin. Therefore a malignant tumor of squamous epithelium is called a squamous cell carcinoma or an epidermoid carcinoma, and a malignant tumor of bone is called an osteosarcoma (osteogenic sarcoma). Carcinomas are about 10 times more common than sarcomas. Table 7-2 lists tumors according to their tissue or cell of origin.
Table 7-2
| Tissue of Origin | Benign Tumor | Malignant Tumor |
| Epithelium | ||
| Squamous cells | Papilloma | Squamous cell or epidermoid carcinoma |
| Basal cells | Basal cell carcinoma | |
| Glands or ducts | Adenoma | Adenocarcinoma |
| Neuroectoderm | ||
| Melanocytes | Nevus | Melanoma |
| Connective Tissue | ||
| Fibrous | Fibroma | Fibrosarcoma |
| Cartilage | Chondroma | Chondrosarcoma |
| Bone | Osteoma | Osteosarcoma |
| Fat | Lipoma | Liposarcoma |
| Endothelium | ||
| Blood vessels | Hemangioma | Angiosarcoma |
| Lymphatic vessels | Lymphangioma | Lymphangiosarcoma |
| Muscle | ||
| Smooth muscle | Leiomyoma | Leiomyosarcoma |
| Striated muscle | Rhabdomyoma | Rhabdomyosarcoma |
TREATMENT OF TUMORS
Benign tumors generally are treated by surgical excision, which can be accomplished through wide local excision or enucleation. Malignant tumors are treated by surgery, chemotherapy, or radiation therapy; a combination is often used.
Because many different types of tissues are present in the oral cavity, many different types of tumors can arise in this location. These neoplasms can be either benign or malignant. In this chapter the neoplasms are classified according to their tissue of origin. Benign tumors are described first, followed by their malignant counterparts.
EPITHELIAL TUMORS
Three different types of epithelial tumors occur in the oral cavity: (1) tumors derived from squamous epithelium, (2) tumors derived from salivary gland epithelium, and (3) tumors derived from odontogenic epithelium. A few of the lesions included in this section are not true tumors. The reasons for their inclusion are explained in their descriptions.
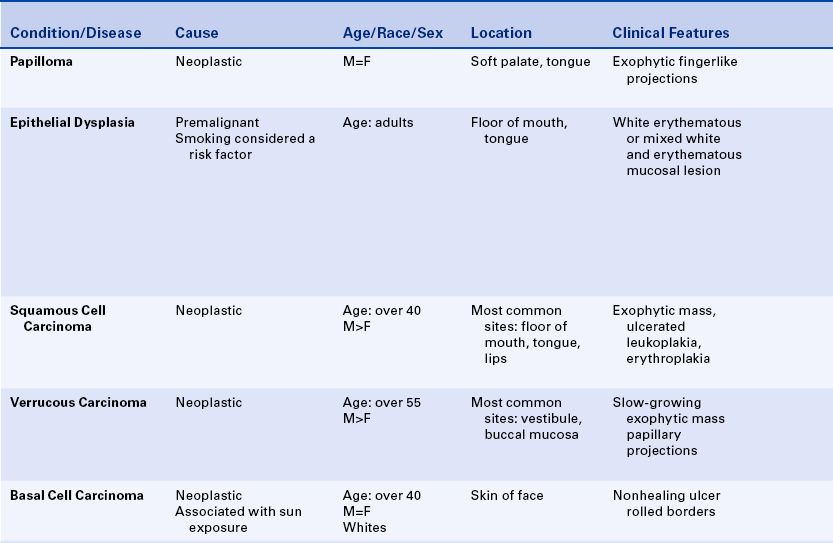
PAPILLOMA
The papilloma is a benign tumor of squamous epithelium that presents as a small, exophytic, pedunculated or sessile growth. These tumors are composed of numerous papillary projections that may be either white or the color of normal mucosa (Figure 7-2). They are often described as cauliflower-like in appearance. Most cases arise on the soft palate or tongue. A papilloma may occur at any age, and an equal sex predilection is noted. Microscopic examination demonstrates numerous fingerlike or papillary projections composed of normal stratified squamous epithelium surfaced by a thickened layer of keratin. A central core of fibrous connective tissue supports each papillary projection. The color of the lesion depends on the amount of surface keratin; the more keratin, the whiter the lesion appears clinically.
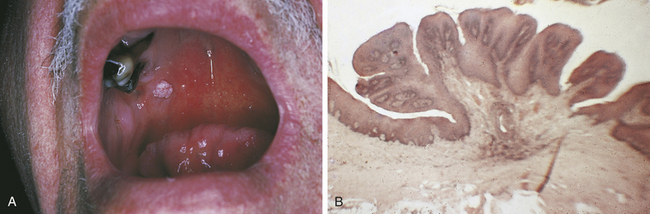
FIGURE 7-2 A, Clinical appearance of a papilloma of the oral mucosa shows a cauliflower-like appearance and rough surface resulting from fingerlike projections. B, Microscopic appearance of a papilloma shows fingerlike projections surfaced by squamous epithelium and supported by thin cores of fibrous connective tissue.
Other oral lesions that may resemble a papilloma clinically are a verruca vulgaris (common wart) and condyloma acuminatum (venereal wart). These two lesions are caused by human papillomaviruses and are described in Chapter 4. They are differentiated from the papilloma by microscopic examination. Special staining procedures can be used to identify viral particles within these lesions.
The papilloma is treated by surgical excision, which must include the base of the growth. With adequate excision, the papilloma usually does not recur.
PREMALIGNANT LESIONS
In any discussion of premalignant lesions of the oral mucosa, it is important to define the term leukoplakia. Leukoplakia is a clinical term and does not refer to a specific histologic appearance. It is defined as a white plaquelike lesion of the oral mucosa that cannot be rubbed off and cannot be diagnosed as a specific disease (Figure 7-3).
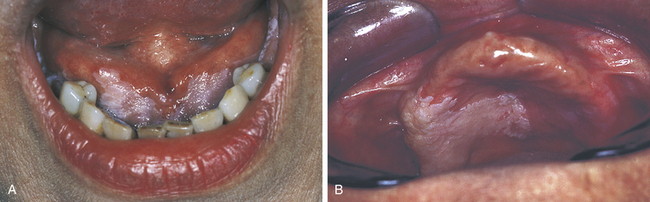
FIGURE 7-3 Clinical appearance of leukoplakia. A, Floor of the mouth. B, Maxillary alveolar mucosa and palate. The cause of these lesions could not be identified.
Leukoplakia is sometimes referred to as idiopathic leukoplakia to emphasize that the specific cause of the lesion is not known. The white lesion illustrated in Figure 7-4 is more accurately called tobacco pouch keratosis rather than a leukoplakia because the direct cause of the lesion is known.

FIGURE 7-4 Clinical appearance of a white lesion that was associated with tobacco chewing (tobacco pouch keratosis). This lesion developed on the lower labial mucosa at the site where the tobacco was held.
The microscopic appearance of leukoplakia varies; therefore a biopsy is essential to establish a definitive diagnosis. Most leukoplakias are the result of hyperkeratosis (thickening of the keratin layer) or a combination of epithelial hyperplasia (thickening of the prickle cell or spinous layer) and hyperkeratosis. When examined microscopically, a leukoplakia may also show epithelial dysplasia, a premalignant condition, or even squamous cell carcinoma, a malignant tumor of squamous epithelium. Depending on the study, approximately 5% to 25% of leukoplakias examined microscopically demonstrated epithelial dysplasia. Studies have also revealed that leukoplakia found on the floor of the mouth, ventrolateral tongue, and lip is more likely to represent epithelial dysplasia or squamous cell carcinoma than leukoplakia occurring in other areas of the oral cavity.
When a white lesion is identified in the oral cavity, the first goal is to identify the cause. Any associated irritation should be removed. If the lesion does not resolve, a biopsy and histologic examination of the tissue must be performed. Any white lesion that is diagnosed as epithelial dysplasia or that cannot be diagnosed as a specific disease should be removed completely. When leukoplakia is found on the floor of the mouth, ventrolateral tongue, or lip, the lesion should be removed regardless of the histologic appearance since there is an increased risk of squamous cell carcinoma developing in these areas.
The treatment of leukoplakia depends on the histologic diagnosis. The treatment of epithelial dysplasia and squamous cell carcinoma is discussed in the sections that follow.
Erythroplakia
Erythroplakia is a clinical term used to describe an oral mucosal lesion that appears as a smooth red patch or a granular red and velvety patch. A lesion that shows a mixture of red and white areas is generally called speckled leukoplakia rather than erythroplakia. Most cases of erythroplakia occur in the floor of the mouth, tongue, and soft palate. Erythroplakia is much less common than leukoplakia. In one study 60 cases of leukoplakia were seen for every one case of erythroplakia. When examined microscopically, 90% of cases of erythroplakia demonstrate epithelial dysplasia or squamous cell carcinoma. Because of these microscopic findings, erythroplakia is considered a more serious clinical finding than leukoplakia (a biopsy must be performed to establish a definitive diagnosis).
Treatment of erythroplakia depends on the histologic diagnosis.
Epithelial Dysplasia
Epithelial dysplasia is a histologic diagnosis that indicates disordered growth. It is considered a premalignant condition. Lesions that microscopically exhibit epithelial dysplasia frequently precede squamous cell carcinoma. Unlike squamous cell carcinoma, the cellular changes in epithelial dysplasia may revert to normal if the stimulus such as tobacco smoking is removed. Epithelial dysplasia may present clinically as an erythematous lesion (erythroplakia), a white lesion (leukoplakia), or a mixed erythematous and white lesion (speckled leukoplakia). Lesions often arise in the floor of the mouth or tongue. The term dysplasia may also be used to describe lesions that occur in tissues other than epithelium.
Dysplasia in other tissues (such as bone) is not considered a premalignant process. Microscopic examination of epithelial dysplasia demonstrates abnormal maturation of epithelial cells with disorganization of the epithelial layers; hyperplasia of the basal cells; and epithelial cells with enlarged and hyperchromatic nuclei, increased nuclear cytoplasmic ratios, abnormal keratinization, and increased numbers of normal and abnormal mitotic figures (Figure 7-5). Microscopically epithelial dysplasia differs from squamous cell carcinoma in that there is no invasion of the abnormal epithelial cells through the basement membrane into the underlying tissue. Severe dysplasia involving the full thickness of the epithelium is called carcinoma in situ.
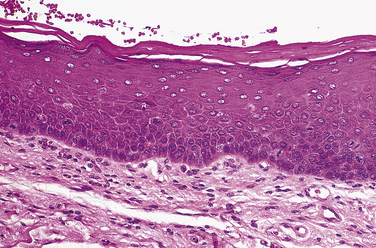
FIGURE 7-5 Microscopic appearance of epithelial dysplasia. Loss of the normal stratification of the epithelium, hyperplasia of the basal cells, and enlarged and hyperchromatic nuclei are seen.
All dysplastic lesions should be excised surgically. Close long-term follow-up examinations are indicated because of the potential for recurrence.
SQUAMOUS CELL CARCINOMA
Squamous cell carcinoma, or epidermoid carcinoma, is a malignant tumor of squamous epithelium. It is the most common primary malignancy of the oral cavity and, like other malignant tumors, can infiltrate adjacent tissues and metastasize to distant sites. Squamous cell carcinoma usually metastasizes to lymph nodes of the neck and then to more distant sites such as the lungs and liver. Clinically squamous cell carcinoma usually presents as an exophytic ulcerative mass (Figure 7-6), but early tumors may be erythematous and plaquelike (erythroplakia), white and plaquelike (leukoplakia), or a mixture of erythematous and white areas (speckled leukoplakia). Squamous cell carcinoma can infiltrate and destroy bone (see Figure 7-6, D).
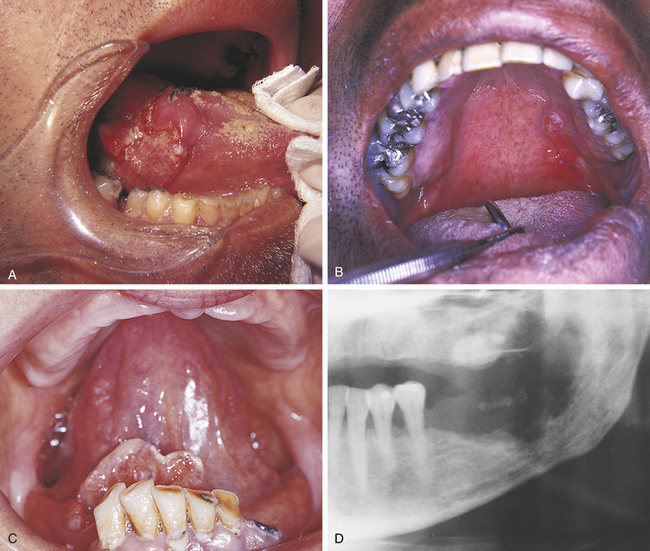
FIGURE 7-6 A, Clinical appearance of a squamous cell carcinoma of the posterolateral tongue shows an exophytic, ulcerated mass. B, Clinical appearance of a squamous cell carcinoma on the left side of the soft palate and fauces. C, Clinical appearance of a squamous cell carcinoma on the floor of the mouth. D, Left side of a panoramic radiograph shows destruction of the mandible by a squamous cell carcinoma. (C courtesy Dr. Edward V. Zegarelli.)
The essential microscopic feature of a squamous cell carcinoma is the invasion of tumor cells through the epithelial basement membrane into the underlying connective tissue (Figure 7-7, A). Invasive sheets and nests of neoplastic squamous cells characterize this tumor. Although squamous cell carcinoma is a malignant tumor, it exhibits features that allow the cells to be recognized as squamous epithelial cells. In well-differentiated tumors these features are easily recognized; however, they may not be easily seen in a poorly differentiated squamous cell carcinoma. Because keratin is a product of squamous epithelium, well-differentiated tumors show keratin formation. In addition to normal surface keratin, the keratin may be seen in individual cells within the tumor and as structures called keratin pearls (Figure 7-7, B). The neoplastic cells are not normal cells. They contain large hyperchromatic nuclei and numerous mitotic figures. Some of the mitotic figures appear normal, whereas others are bizarre (see Figure 7-7, B).
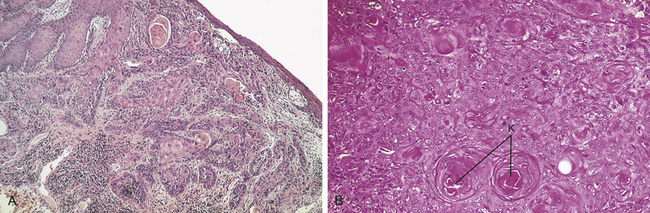
FIGURE 7-7 A, Microscopic appearance (low power) of a squamous cell carcinoma shows infiltration of the tumor into the connective tissue. B, High-power photomicrograph shows abnormal keratinization (K).
Squamous cell carcinomas may occur anywhere in the oral cavity, but most tumors arise on the floor of the mouth, ventrolateral tongue, soft palate, tonsillar pillar, and retromolar areas. The clinical appearance of squamous cell carcinoma occurring in several different locations is seen in Figure 7-6.
Squamous cell carcinomas may occur on the vermilion border of the lips and skin of the face (Figure 7-8). In this location they are associated with sun exposure (actinic cheilitis and actinic keratosis) and tend to be more common in individuals with fair skin. The prognosis for squamous cell carcinoma of the lips and skin is much better than that for squamous cell carcinoma of the oral mucosa. Sun exposure causes recognizable changes of the vermilion border of the lips. The color changes from dark and uniform to mottled grayish-pink. The interface of the vermilion border and the skin becomes blurred, and linear fissures are seen at right angles to the line of the interface. Histologically damage from sun exposure is seen as changes that range from degeneration of the collagen under the epithelium to a condition called solar or actinic cheilitis, in which mild-to-severe epithelial dysplasia occurs. Fair-skinned individuals should be advised either to avoid the sun or to use a sun block.
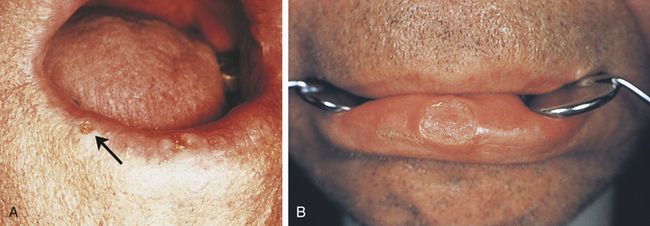
FIGURE 7-8 Clinical appearance of squamous cell carcinoma of the lower lip (arrow). The reader should also note actinic (solar) cheilitis in A. (Courtesy Dr. Edward V. Zegarelli.)
The majority of squamous cell carcinomas occur in patients over 40 years of age. In the past men have outnumbered women; however, in the last 30 years there has been an increased incidence of squamous cell carcinoma in women. This is most likely a result of the increased number of women who smoke and the fact that women outnumber men in older age-groups.
Risk Factors
Several risk factors have been associated with the development of squamous cell carcinoma. The most significant is tobacco—including cigar, pipe, and cigarette smoking; snuff dipping; and tobacco chewing. Alcohol consumption appears to add to the risk of oral squamous cell carcinoma, especially in individuals who also use tobacco products. There is no evidence that chronic irritation is an initiating factor in the development of oral cancer.
Treatment and Prognosis
Squamous cell carcinoma generally is treated by surgical excision. Radiation therapy or chemotherapy may be used in combination with surgery. Occasionally radiation therapy is used alone. The prognosis of squamous cell carcinoma is related to the size and location of the tumor and the presence or absence of metastases. The smaller the tumor at the time of treatment, the better the prognosis. For oral squamous cell carcinoma, determining the size of the tumor and the presence or absence of cervical lymph node involvement and distant metastasis is important in predicting the patient's prognosis. These are assessed using a system called the TNM staging system; the higher the stage, the worse the prognosis (Box 7-1 and Table 7-3). Metastasis to cervical lymph nodes is associated with a much poorer prognosis, as is the presence of distant metastasis. Therefore it is important to identify asymptomatic areas of leukoplakia and erythroplakia while they are small and remove all potentially premalignant lesions.
Table 7-3
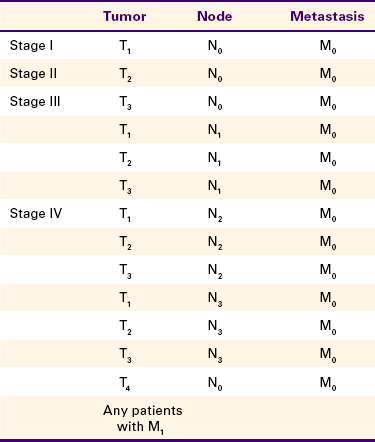
Adapted from Sobin LH, Wittekind C, editors: International union against cancer TNM classification of malignant tumours, ed 6, New York, 2002, Wiley-Liss.
Patients who have undergone radiation therapy for malignant tumors of the head and neck often experience severe xerostomia (dry mouth) as a result of radiation damage to the salivary gland tissue. These patients require preventive dental care consisting of nutritional counseling, topical fluoride application, and meticulous home care. Oral manifestations of therapy for oral cancer is included in Chapter 9.
VERRUCOUS CARCINOMA
Verrucous carcinoma is a specific type of squamous cell carcinoma that is separated from other squamous cell carcinomas because it has a much better prognosis. Clinically it appears as a slow-growing exophytic tumor with a pebbly white and red surface (Figure 7-9). Most cases occur in men over 55 years of age and involve the vestibule and buccal mucosa. Verrucous carcinoma occurs most often in individuals who use smokeless tobacco products. Microscopic examination demonstrates a tumor composed of numerous papillary epithelial proliferations. The spaces between these papillary projections are filled with keratin. The epithelium is well differentiated, does not contain atypical cells, and exhibits broad-based rete pegs that penetrate deeply into the connective tissue. The epithelial basement membrane is intact, and the tumor does not show invasion of tumor cells through the basement membrane, as is seen in squamous cell carcinoma.
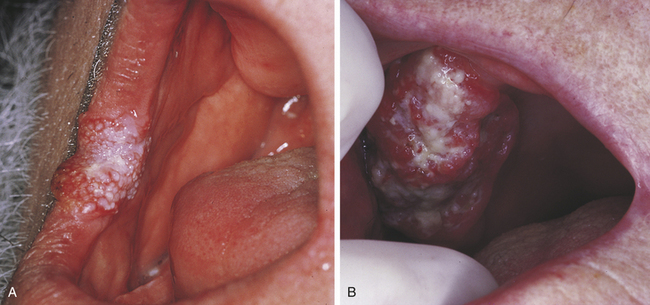
FIGURE 7-9 A, Clinical appearance of a verrucous carcinoma occurring on the commissure and anterior buccal mucosa. B, Maxillary alveolar ridge.
Verrucous carcinoma is treated by surgical excision. Although it is a carcinoma, it usually does not metastasize; therefore the prognosis is better for verrucous carcinoma than for squamous cell carcinoma. If it is not treated, it can cause extensive local damage. Close long-term follow-up is necessary for patients with this condition.
BASAL CELL CARCINOMA
Basal cell carcinoma is a malignant skin tumor associated with excessive sun exposure. This particular neoplasm does not occur in the oral cavity. Basal cell carcinoma frequently arises on the skin of the face and appears as a nonhealing ulcer with characteristic rolled borders (Figure 7-10). Most cases arise in white adults, and no sex predilection is seen.
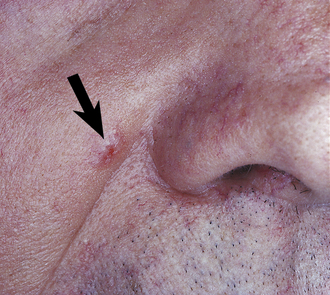
FIGURE 7-10 Clinical appearance of a basal cell carcinoma (arrow) illustrating the characteristic “rolled” borders.
A basal cell carcinoma is composed of a proliferation of basal cells derived from the surface stratified squamous epithelium. Microscopic examination demonstrates nests and islands of basal epithelial cells in the underlying connective tissue. In most cases the tumor cells are well differentiated.
Basal cell carcinoma is a locally invasive tumor that can become quite large and disfiguring if it is not removed. Surgical excision is the treatment of choice, and radiation therapy may be used to treat large lesions. Only rarely does a basal cell carcinoma metastasize. As a general rule, a patient should be referred to an oral and maxillofacial surgeon or dermatologist to have a biopsy performed on any nonhealing ulcer of the skin or lips that has been present for more than 10 days.
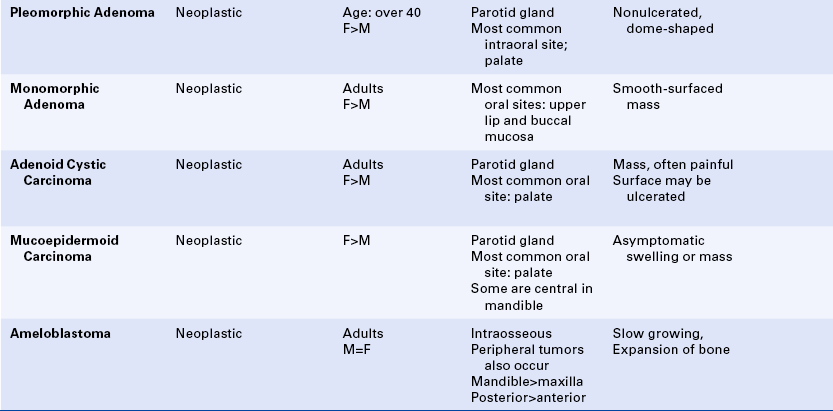
SALIVARY GLAND TUMORS
Benign and malignant tumors may arise in either the major or the minor salivary glands. Tumors may occur within the parotid, submandibular, or sublingual glands; or they may involve any of the minor salivary glands located throughout the oral cavity. Intraorally minor salivary gland tumors are located most commonly at the junction of the hard and soft palates. They can also occur on the labial and buccal mucosa, the retromolar area, the floor of the mouth, and rarely the tongue (Figure 7-11). Tumors of minor salivary gland origin are much more common in the upper lip than in the lower lip.

FIGURE 7-11 A, Benign salivary gland tumor of the palate (pleomorphic adenoma). B, Malignant salivary gland tumor of the palate (adenoid cystic carcinoma). Biopsy site should be noted. C, Benign salivary gland tumor of the upper lip (pleomorphic adenoma). D, Malignant salivary gland tumor of the buccal mucosa (mucoepidermoid carcinoma). E, Malignant salivary gland tumor of the tongue (adenoid cystic carcinoma).
Because the origin of these tumors is glandular epithelium, benign tumors of salivary gland origin are called adenomas. Although some malignant salivary gland tumors are called adenocarcinomas, most have more specific names such as adenoid cystic carcinoma and mucoepidermoid carcinoma. All salivary gland tumors are diagnosed on the basis of their microscopic appearance. A biopsy and microscopic examination of the tissue are required to establish a specific diagnosis.
PLEOMORPHIC ADENOMA (BENIGN MIXED TUMOR)
The pleomorphic adenoma is a benign salivary gland tumor. It is the most common salivary gland neoplasm and accounts for about 90% of all benign salivary gland tumors. Microscopic examination reveals an encapsulated tumor composed of tissue that appears to be a mixture of both epithelium and connective tissue (Figure 7-12). For this reason the tumor is often called the benign mixed tumor. The connective tissue–like part can vary from loose and dense fibrous connective tissue to cartilage. The tissue that looks like connective tissue is derived from a salivary gland cell called a myoepithelial cell.
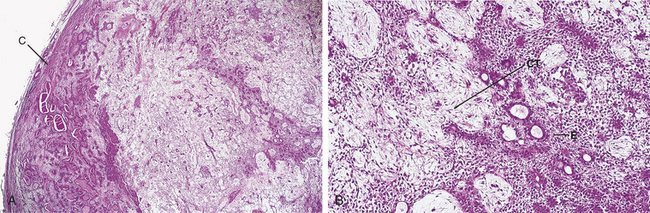
FIGURE 7-12 Microscopic appearance of a pleomorphic adenoma. A, Low-power photomicrograph shows a capsule (C). B, High-power photomicrograph shows a mixture of epithelium (E) and connective tissue (CT).
The most common extraoral location for the pleomorphic adenoma is the parotid gland. The most common intraoral site is the palate. However, these tumors can occur wherever salivary gland tissue is present. Clinically the pleomorphic adenoma appears as a slowly enlarging, nonulcerated, painless, dome-shaped mass (see Figure 7-11, A and C). The surface can be ulcerated if traumatized. Its size can range from a few to several centimeters. Most pleomorphic adenomas occur in individuals over 40 years of age, and a female predilection has been noted. Pleomorphic adenomas have also been reported in children.
The pleomorphic adenoma is treated by surgical excision. The extent of the surgery depends on the location of the tumor. Clinicians treat parotid gland tumors by removing the part of the parotid gland containing the tumor (partial parotidectomy), whereas minor salivary gland tumors are treated by more conservative surgical excision. The pleomorphic adenoma grows by extension of projections of tumor into the surrounding tissue. Therefore some tumors are difficult to remove completely. Recurrence rates vary and are related to the adequacy of the initial surgical removal. Pleomorphic adenomas have been known to undergo malignant transformation; this occurrence is known as a carcinoma arising in a pleomorphic adenoma.
MONOMORPHIC ADENOMA
The monomorphic adenoma is a benign encapsulated salivary gland tumor that occurs less frequently than the pleomorphic adenoma. It is composed of a uniform pattern of epithelial cells (Figure 7-13). These tumors do not have the connective tissue–like component seen in a pleomorphic adenoma. They occur most commonly in adult women, with a predilection for the upper lip and buccal mucosa. Several specific types of monomorphic adenoma based on their histologic patterns have been identified. The papillary cystadenoma lymphomatosum is a unique type of monomorphic adenoma. It is also called Warthin's tumor. Microscopic examination of this particular variant demonstrates an encapsulated tumor composed of two types of tissue: epithelial and lymphoid (Figure 7-14). The epithelial component is neoplastic. It lines papillary projections that protrude from cystic structures. Sheets of lymphocytes surround the cystic structures. In some cases the lymphoid component demonstrates germinal center formation. Warthin's tumor presents as a painless, soft, and compressible or fluctuant mass, usually located in the parotid gland. Intraoral examples are very rare. This tumor often develops bilaterally and occurs predominantly in adult men.
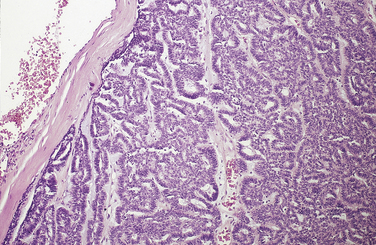
FIGURE 7-13 Microscopic appearance (low power) of a monomorphic adenoma shows a capsule and a uniform pattern of epithelial cells.
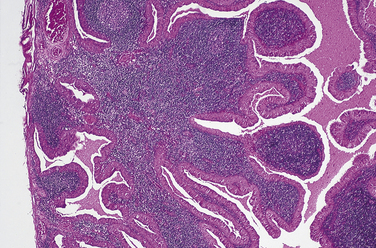
FIGURE 7-14 Microscopic appearance of a papillary cystadenoma lymphomatosum (Warthin's tumor) shows spaces lined by epithelium and surrounded by lymphocytes.
All monomorphic adenomas are treated by surgical excision. Recurrence is rare.
ADENOID CYSTIC CARCINOMA (CYLINDROMA)
The adenoid cystic carcinoma (see Figure 7-11, E) is a malignant tumor of salivary gland origin that can originate from either major or minor salivary gland tissue. It is unencapsulated and infiltrates surrounding tissue. This tumor is composed of small, deeply staining, uniform epithelial cells arranged in perforated round-to-oval islands. The microscopic appearance of adenoid cystic carcinoma has been likened to that of Swiss cheese (Figure 7-15). These round and oval islands represent cylinders of tumor; therefore this tumor has also been called a cylindroma. Although it is malignant, pleomorphic cells and mitotic figures are rarely seen. Malignancy is recognized on the basis of the unique microscopic features. The adenoid cystic carcinoma is a slow-growing malignant tumor.
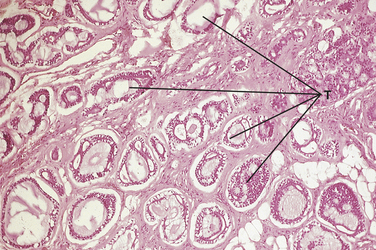
FIGURE 7-15 Microscopic appearance of an adenoid cystic carcinoma shows perforated islands of uniform cells. Tumor (T) is seen infiltrating the adjacent adipose tissue.
The most common extraoral site for an adenoid cystic carcinoma is the parotid gland. The most common intraoral site is the palate. Most tumors appear as slowly growing masses that can exhibit surface ulceration (see Figure 7-11, B and E). Pain is often present because of the tendency of these tumors to surround nerves. Adenoid cystic carcinoma is more common in women than in men and is a tumor of adults; the majority of cases are diagnosed in the fifth and sixth decades of life.
The treatment of choice for adenoid cystic carcinoma is complete surgical excision. Radiation treatment has been attempted and has been shown to be of benefit in some cases. However, recurrence and persistent local invasion are common. Metastasis occurs late in the course of the disease. About 30% of patients experience cervical lymph node involvement. Distant metastases, most often involving the lungs, may occur after many years. In these cases the prognosis is poor.
MUCOEPIDERMOID CARCINOMA
Mucoepidermoid carcinoma is a malignant salivary gland tumor. It is an unencapsulated, infiltrating tumor composed of a combination of mucous cells interspersed with squamouslike epithelial cells called epidermoid cells (Figure 7-16).
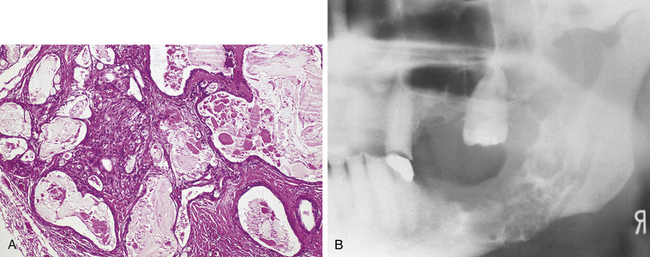
FIGURE 7-16 A, Microscopic appearance (low power) of a mucoepidermoid carcinoma shows cystic structures, mucous cells, and epidermoid cells. B, Radiograph of a central mucoepidermoid carcinoma shows a multilocular radiolucency.
Mucoepidermoid carcinomas involving the major glands occur most often in the parotid gland, whereas minor gland tumors are most common on the palate. They appear clinically as slowly enlarging masses (see Figure 7-11, D). Occasionally a mucoepidermoid carcinoma may arise centrally within bone (see Figure 7-16, B), usually in the mandibular premolar and molar region. In this location it appears as either a unilocular or a multilocular radiolucency (see Figure 7-16, B). A central mucoepidermoid carcinoma is derived from either salivary gland tissue trapped within bone or the transformed epithelial lining of a dentigerous cyst (a developmental odontogenic cyst that forms around the crown of an unerupted or impacted tooth; see Chapter 5).
A mucoepidermoid carcinoma may occur over a wide age range. Although it usually occurs in adults after middle age, this tumor is the most common malignant salivary gland tumor in children. A female predilection is noted.
Treatment of the mucoepidermoid carcinoma consists of complete surgical excision, with close long-term follow-up for signs of recurrence and metastasis. The behavior of any one tumor is difficult to predict and is related to the histologic appearance of the tumor. Low-grade tumors have a 92% 5-year survival rate after initial treatment. For high-grade (more malignant) tumors, only 49% of patients survive 5 years after the initial treatment.
OTHER MALIGNANT SALIVARY GLAND TUMORS
In addition to the adenoid cystic and the mucoepidermoid carcinomas, several other malignant salivary gland tumors exist, including polymorphous low-grade adenocarcinoma (lobular carcinoma), acinic cell adenocarcinoma, and other adenocarcinomas.
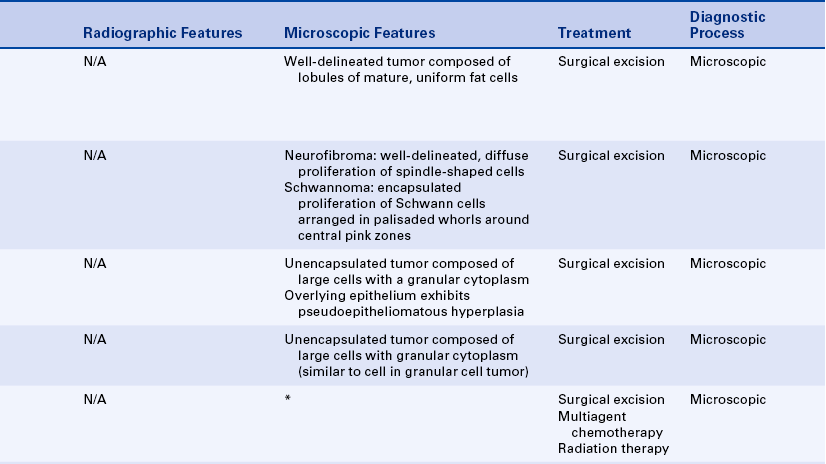
ODONTOGENIC TUMORS
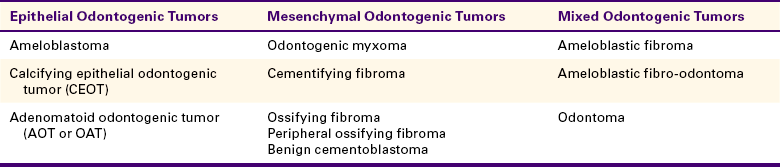
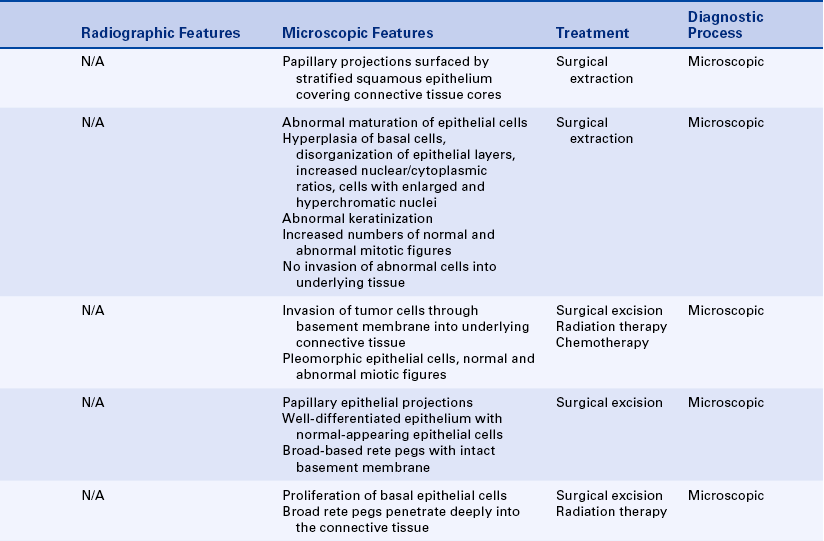
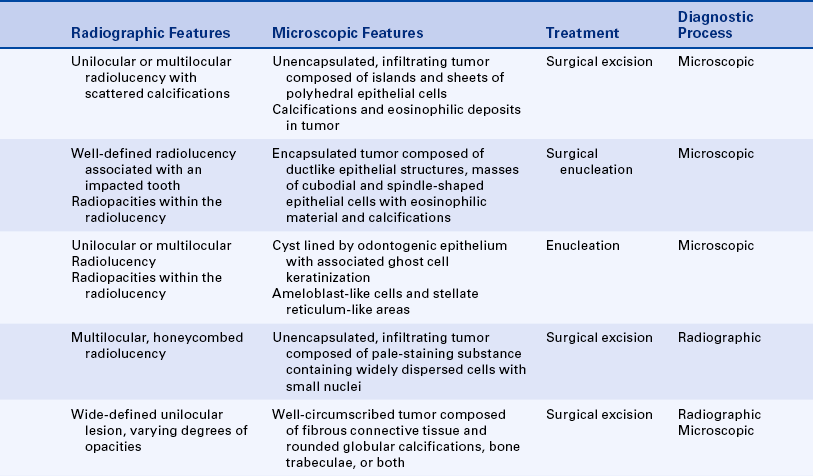
Odontogenic tumors are derived from tooth-forming tissues. Tooth formation results from an interaction between odontogenic epithelium and odontogenic mesenchyme. Some odontogenic tumors are composed of epithelium only, some are composed of mesenchyme only, and others are composed of a mixture of both elements. Most odontogenic tumors are benign. Malignant odontogenic tumors occur but are rare. Table 7-4 presents a classification scheme for odontogenic tumors based on the derivation of the odontogenic tissue.
In addition to the odontogenic tumors described in this text, other uncommon odontogenic tumors such as the squamous odontogenic tumor and the central odontogenic fibroma exist. (See the references at the end of this chapter for more detailed information on these tumors.)
EPITHELIAL ODONTOGENIC TUMORS
The ameloblastoma is a benign, slow-growing but locally aggressive epithelial odontogenic tumor that may arise in either the maxilla or the mandible. It is an unencapsulated tumor that infiltrates into surrounding tissue and can cause extensive destruction. When it occurs in the maxilla, death can result from direct extension into the brain and adjacent vital structures. An ameloblastoma is composed of ameloblast-like epithelial cells that surround areas resembling stellate reticulum. These cells are arranged in either dental follicle-like islands or interconnecting strands (Figure 7-17).
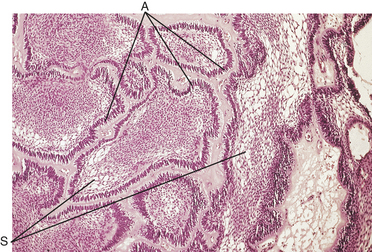
FIGURE 7-17 Microscopic appearance (low-power) of a follicular ameloblastoma shows dental follicle-like islands composed of epithelial cells consisting of peripheral ameloblast-like cells (A) and stellate reticulum-like areas (S).
The classic radiographic appearance of an ameloblastoma is a multilocular soap bubble–like or honeycombed radiolucency (Figure 7-18). In smaller tumors the radiolucency may be unilocular. An ameloblastoma may arise anywhere in the jaws and can occur in association with a dentigerous cyst (Figure 7-19). However, 80% of ameloblastomas arise in the mandible, most often in the molar and ramus area. The molar area is also the most common location when they occur in the maxilla. The tumor may cause expansion of bone. The initial presentation is usually a slowly developing, asymptomatic swelling of the affected bone. The age range of individuals affected is broad, but most ameloblastomas occur in adults. No sex predilection is noted.
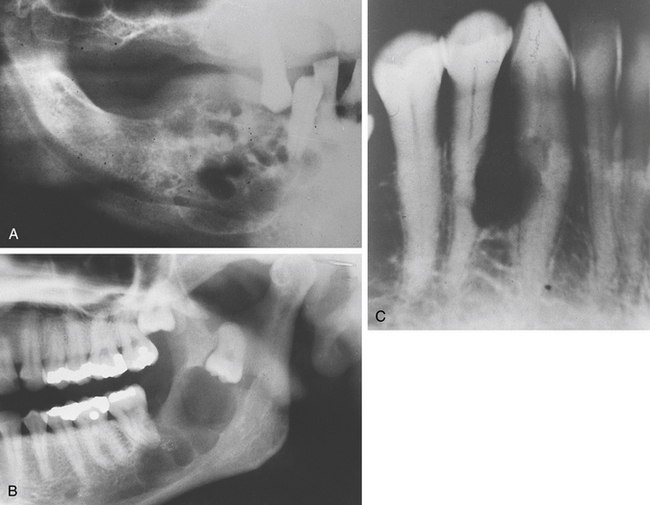
FIGURE 7-18 A, Radiograph of an ameloblastoma shows multilocular radiolucency in the molar area of the mandible. B, Radiograph of an ameloblastoma shows a multilocular radiolucency in the molar area of the mandible. C, Radiograph of an ameloblastoma shows a small but multilocular radiolucency in the mandibular cuspid and bicuspid region.
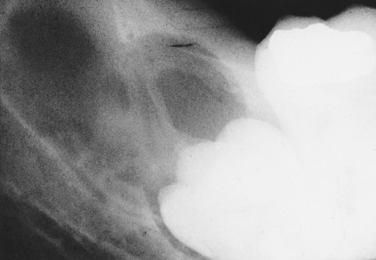
FIGURE 7-19 Radiograph of an ameloblastoma that formed in association with an impacted tooth and dentigerous cyst.
Ameloblastomas are treated by complete surgical removal. Recurrence is common. Occasionally these tumors occur in the gingiva and do not involve bone, in which case they are called peripheral ameloblastomas. These are also treated by surgical excision and differ from the central ameloblastomas in that they generally do not recur.
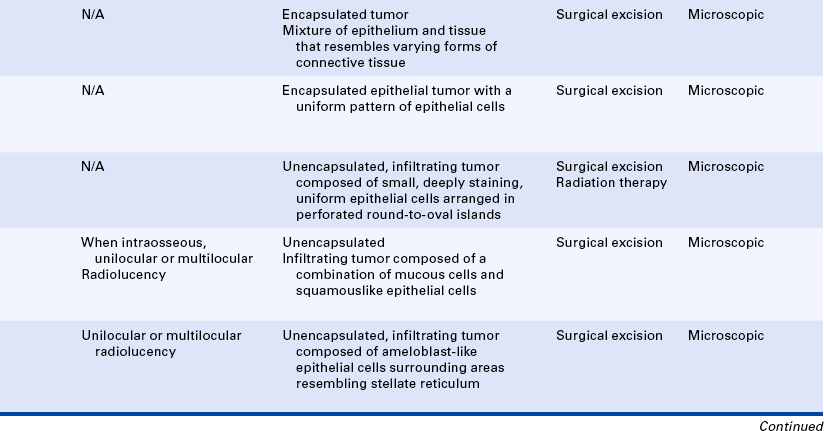
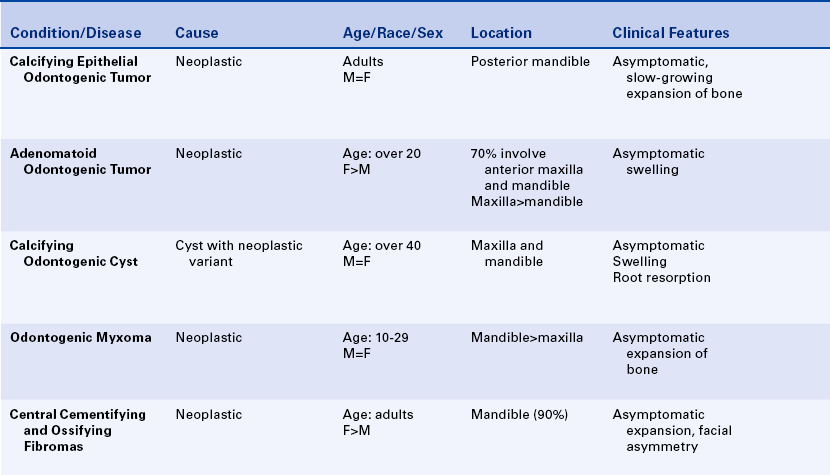
Calcifying Epithelial Odontogenic Tumor
The calcifying epithelial odontogenic tumor, also known as a Pindborg tumor, is a benign epithelial odontogenic tumor that occurs much less frequently than the ameloblastoma. It is a unique odontogenic tumor because the proliferating cells do not resemble odontogenic epithelium. The tumor is composed of islands and sheets of polyhedral (multisided) epithelial cells. Deposits similar to amyloid are seen in the tumor, and calcifications are seen within these deposits. The amyloid-like material is thought to represent a form of abnormal enamel protein (Figure 7-20, A). Radiographically the calcifying epithelial odontogenic tumor appears as a unilocular or multilocular radiolucency (Figure 7-20, B). Calcifications that form within the tumor appear as radiopacities within the radiolucency.
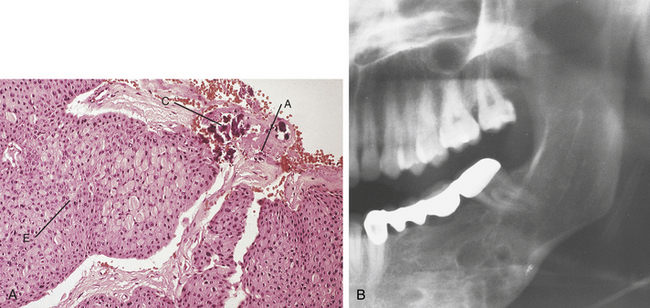
FIGURE 7-20 Calcifying epithelial odontogenic tumor. A, Microscopic appearance (low power) of a calcifying epithelial odontogenic tumor shows sheets of epithelial cells (E), amorphous material (A), and calcifications (C). B, Radiograph of a calcifying epithelial odontogenic tumor shows a multilocular radiolucency.
The majority of patients affected with this tumor are adults. However, the calcifying epithelial odontogenic tumor affects a broad age range that extends from young adults to elderly individuals. No sex predilection is noted. Reports of this tumor occurring in the mandible are twice as common as reports of it occurring in the maxilla. Although it can occur anywhere in the maxilla or mandible, the bicuspid and molar areas are the most common locations. Many neoplasms are associated with impacted teeth.
Treatment of the calcifying epithelial odontogenic tumor depends on the size and location of the tumor and involves complete surgical excision. Recurrence has been reported, but the recurrence rate is lower than that for an ameloblastoma.
Adenomatoid Odontogenic Tumor
The adenomatoid odontogenic tumor (AOT), also known as an odontogenic adenomatoid tumor, is an encapsulated, benign epithelial odontogenic tumor that has a distinctive age, sex, and site distribution. It also differs from other epithelial odontogenic tumors in that it does not recur. Approximately 70% of AOTs occur in females under 20 years of age, and 70% involve the anterior part of the jaws. The maxilla is more commonly involved than the mandible. Many AOTs are associated with impacted teeth. Although a localized swelling may be present, most are asymptomatic and are discovered on routine radiographic examination.
Radiographically the AOT appears as a well-circumscribed radiolucency (Figure 7-21, B). Because of the frequent association with an impacted tooth, an adenomatoid odontogenic tumor often simulates a dentigerous cyst. However, unlike the dentigerous cyst (see Chapter 5), the adenomatoid odontogenic tumor extends beyond the cementoenamel junction and can involve 50% to 60% of the root. As calcifications form within the tumor, radiopaque areas of varying size are visible on radiographs. Histologic examination reveals a dense, fibrous connective tissue capsule surrounding ductlike structures, whorls, and large masses of cuboidal and spindle-shaped epithelial cells (Figure 7-21, A). The ductlike structures are one of the distinctive features of this tumor and are the reason for the name adenomatoid, or glandlike.
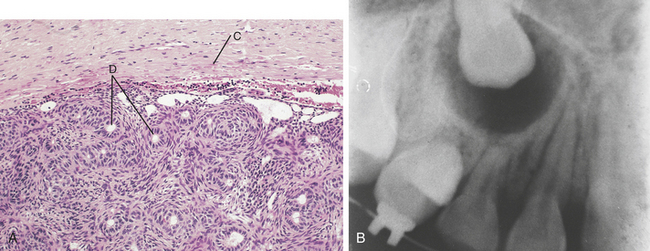
FIGURE 7-21 Adenomatoid odontogenic tumor. A, Microscopic appearance of an adenomatoid odontogenic tumor shows the capsule (C), epithelial cells, and ductlike structures (D). B, Radiograph of an adenomatoid odontogenic tumor shows a unilocular radiolucency surrounding the crown of an unerupted maxillary cuspid.
These structures are not ducts but actually ameloblast-like cells that resemble ducts because of their circular arrangement. Eosinophilic material is seen in the centers of these structures, and calcifications also form in this tumor.
The clinician should treat an adenomatoid odontogenic tumor conservatively by enucleation. The tumor is removed in its entirety since it is easily separated from the surrounding bone. Recurrence is rare.
Calcifying Odontogenic Cyst
The calcifying odontogenic cyst is a nonaggressive cystic lesion that affects a broad age range but is most commonly seen in individuals younger than 40 years of age. No sex predilection has been noted. A solid variant of the calcifying odontogenic cyst has been reported and has been suggested to represent a neoplasm rather than a cyst.
Histologic examination reveals a cystic structure lined by odontogenic epithelium with an associated and characteristic ghost cell keratinization (Figure 7-22, A). The epithelium resembles that seen in an ameloblastoma, consisting of ameloblast-like cells and stellate reticulum-like areas. The ghost cells that are characteristic of this lesion exhibit a clear central area. They are thought to represent degenerating epithelial cells. The calcifying odontogenic cyst is usually a radiographically well-defined lesion that can present as either a unilocular or a multilocular radiolucency (Figure 7-22, B). Calcifications can occur and are seen as radiopaque areas.
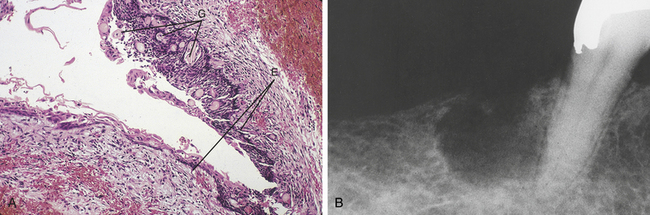
FIGURE 7-22 Calcifying odontogenic cyst. A, Microscopic appearance of a calcifying odontogenic cyst shows a cystic structure lined by odontogenic epithelium (E) with associated ghost cells (G). B, Radiograph of a calcifying odontogenic cyst shows a unilocular radiolucency of the mandible.
The calcifying odontogenic cyst generally is treated by surgical enucleation. Although a few recurrences have been reported, it usually does not recur. The solid variant may exhibit more aggressive behavior and may be treated with a more extensive surgical procedure.
MESENCHYMAL ODONTOGENIC TUMORS
The odontogenic myxoma is a benign mesenchymal odontogenic tumor that occurs most often in young individuals between 10 and 29 years of age. No sex predilection is noted.
The odontogenic myxoma exhibits a multilocular, honeycombed radiolucency with poorly defined margins (Figure 7-23, B). The tumor may become quite large and cause tooth displacement. Although most cases occur in the posterior mandible, the odontogenic myxoma may arise anywhere in the maxilla or mandible. Histologic examination reveals a nonencapsulated infiltrating tumor composed of a pale-staining mucopolysaccharide ground substance that contains dispersed cells with long cytoplasmic processes (Figure 7-23, A). This tissue closely resembles tissue seen in the dental papilla, the mesenchymal component of tooth-forming tissue.
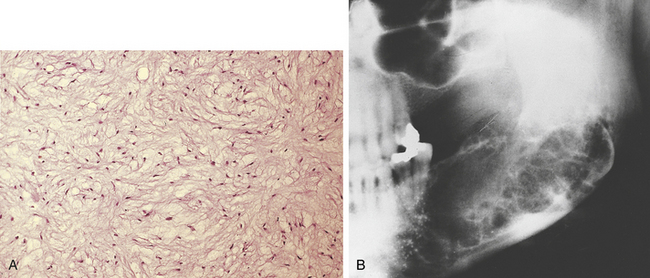
FIGURE 7-23 A, Photomicrograph of an odontogenic myxoma shows background substance containing widely dispersed cells with long cytoplasmic processes. B, Radiograph of an odontogenic myxoma shows a multilocular, honeycombed radiolucency.
The odontogenic myxoma is treated by complete surgical excision. The extent of the surgery depends on the size of the tumor. The recurrence rate is approximately 25%, and most recurrences take place within 2 years following treatment.
Central Cementifying and Central Ossifying Fibromas
The central cementifying fibroma and central ossifying fibroma are benign well-circumscribed tumors classified as fibro-osseous lesions. They are considered variants of the same neoplasm since they are both composed of fibrous connective tissue and calcifications. In the central cementifying fibroma the calcifications are rounded and globular, resembling cementum (Figure 7-24, A), whereas in the central ossifying fibroma the calcifications more closely resemble bone trabeculae. Some tumors have a mixture of globular calcifications resembling cementum and bone trabeculae. These tumors are called central cemento-ossifying fibromas. This particular variant results from the potential of periodontal ligament cells to produce either cementum or bone.
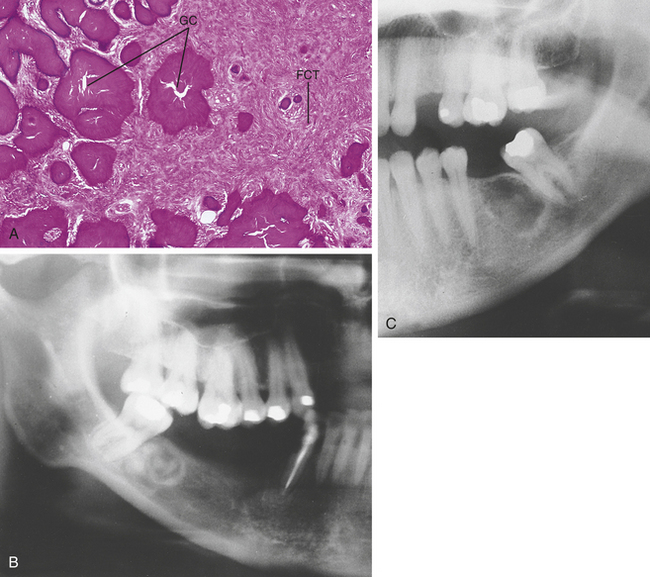
FIGURE 7-24 A, Photomicrograph of a central cementifying fibroma shows rounded, globular calcifications (GC) and cellular fibrous connective tissue (FCT). B, Radiograph of a central cementifying fibroma shows a well-circumscribed radiolucent lesion. C, Radiograph of a central cementifying fibroma shows a radiolucent and radiopaque lesion.
The tumor usually occurs in adults in the third and fourth decades of life. Women are affected more often than men. Affected patients may be asymptomatic or demonstrate bone expansion or facial asymmetry. Radiographically the central cementifying and central ossifying fibroma are well-defined and demonstrate a radiolucent-to-radiopaque appearance, depending on the amount of calcified tissue present (Figure 7-24, B and C). The majority of cases occur in the mandible.
Other benign fibro-osseous lesions such as periapical cemento-osseous dysplasia and fibrous dysplasia (discussed in Chapter 8) may be histologically identical to the central cementifying and central ossifying fibroma. The radiographic appearance of each of these individual lesions is important in distinguishing them from one another.
The central cementifying and central ossifying fibromas are treated by surgical excision. Because these lesions are well delineated, they separate easily from the surrounding bone. Recurrence is rare.
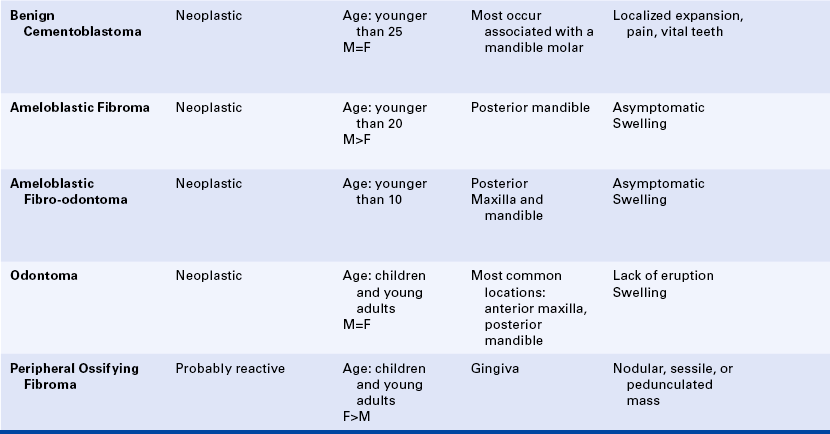
Benign Cementoblastoma
The benign cementoblastoma is a cementum-producing lesion that is fused to the root or roots of a vital tooth. The tumor typically occurs in young adults. Unlike other odontogenic tumors, pain is a frequent symptom. The radiographic appearance is distinctive and consists of a well-defined radiopaque mass with a surrounding radiolucent halo (Figure 7-25). However, early in its development this lesion may be radiolucent and mimic inflammatory periapical disease The radiolucent halo represents the periodontal ligament. The neoplasm is usually seen in continuity with the root or roots of a mandibular molar or premolar tooth. Obliteration of the apex of the affected tooth is common. Occasional cases may cause localized bone expansion. Microscopic examination reveals a proliferation of cellular cementum fused to the root or roots of the affected tooth.

FIGURE 7-25 Radiograph of a benign cementoblastoma shows a well-circumscribed radiopaque mass surrounded by a radiolucent halo and attached to the roots of a mandibular first molar.
Treatment of the benign cementoblastoma consists of enucleation of the tumor and removal of the involved tooth. It does not recur.
MIXED ODONTOGENIC TUMORS
The ameloblastic fibroma is a benign, mixed odontogenic tumor that occurs in young children and adults. Most cases occur in individuals younger than 20 years of age. A male sex predilection is noted. The most common location is the mandibular bicuspid and molar region. Most patients are asymptomatic, but bone expansion or swelling may be noted. Radiographically the ameloblastic fibroma appears as either a well-defined or a poorly defined unilocular or multilocular radiolucency (Figure 7-26, B).
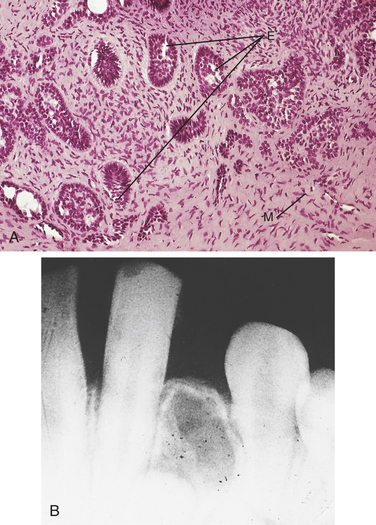
FIGURE 7-26 A, Microscopic appearance of an ameloblastic fibroma shows a combination of odontogenic epithelium (E) and mesenchymal tissue (M). B, Radiograph of an ameloblastic fibroma shows a poorly defined radiolucency.
Histologic examination demonstrates a nonencapsulated odontogenic tumor composed of strands and small islands of ameloblast-like epithelial cells and tissue that resembles the dental papilla (Figure 7-26 A).
The ameloblastic fibroma is treated by surgical excision, and recurrence rate is low.
Ameloblastic Fibro-odontoma
The ameloblastic fibro-odontoma is a benign odontogenic tumor that has features of both an ameloblastic fibroma and an odontoma. Most cases occur in young adults, with an average age of 10 years. No sex predilection is noted. The ameloblastic fibro-odontoma typically arises in the posterior jaws and is often asymptomatic. However, some patients may experience swelling of the affected area.
Radiographic examination reveals a well-delineated radiolucent lesion that may be unilocular or multilocular. Calcifications of various size and shape are noted within the radiolucency. These calcifications represent tooth formation.
Microscopic examination demonstrates features similar to those described in the ameloblastic fibroma combined with structures that resemble teeth. Therefore various amounts of enamel, dentin, cementum, and pulp tissue are produced.
The ameloblastic fibro-odontoma is a well-circumscribed lesion that usually separates easily from the surrounding bone. It is treated by conservation surgical excision, and recurrence is unusual.
Odontoma
The odontoma is an odontogenic tumor composed of mature enamel, dentin, cementum, and pulp tissue. The odontoma is the most common of the odontogenic tumors. The two types of odontomas are compound and complex. A compound odontoma consists of a collection of numerous small teeth. Although compound odontomas may consist of many small teeth, they do not exhibit unlimited growth potential and therefore are more accurately developmental lesions than true tumors. A complex odontoma consists of a mass of enamel, dentin, cementum, and pulp that does not resemble a normal tooth.
Most odontomas are detected in adolescents and young adults. No sex predilection is noted. The compound odontoma is usually located in the anterior maxilla, and the complex odontoma most commonly occurs in the posterior mandible. The most common clinical manifestation of an odontoma is the failure of a permanent tooth to erupt. Most odontomas are small, but large lesions can cause swelling and displacement of erupted teeth. Odontomas can be associated with impacted or unerupted teeth and odontogenic cysts and tumors.
Radiographically compound odontomas appear as a cluster of numerous miniature teeth surrounded by a radiolucent halo (Figure 7-27). A complex odontoma appears as a radiopaque mass surrounded by a thin radiolucent halo (Figure 7-28).

FIGURE 7-27 Radiograph of a compound odontoma shows a collection of numerous, small, toothlike radiopacities surrounded by a radiolucent halo.

FIGURE 7-28 Radiograph of a complex odontoma shows a radiopaque mass surrounded by a radiolucent halo.
Treatment of an odontoma consists of surgical excision. They generally do not recur.
PERIPHERAL ODONTOGENIC TUMORS
The peripheral ossifying fibroma is usually a well-demarcated sessile or pedunculated lesion that appears to originate from the gingival interdental papilla and is most likely derived from cells of the periodontal ligament (Figure 7-29, A). It is more common in females than in males and often occurs in young individuals. It has been reported in children and adults.
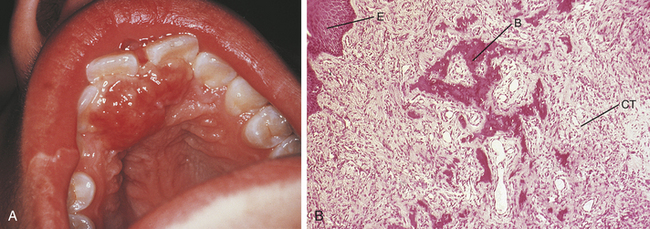
FIGURE 7-29 A, Clinical appearance of a peripheral ossifying fibroma shows an exophytic lesion involving the palatal gingiva of the maxillary anterior teeth. B, Photomicrograph of a peripheral ossifying fibroma shows bonelike calcifications (B) in cellular fibrous connective tissue (CT). A small amount of surface epithelium (E) is also visible.
It is composed of cellular fibrous connective tissue interspersed with scattered bone and cementum-like calcifications (Figure 7-29, B). Microscopically the peripheral ossifying fibroma is similar to the central cementifying fibroma and central ossifying fibroma.
Treatment of the peripheral ossifying fibroma consists of surgical excision with thorough scaling of the adjacent teeth to remove any irritants that can induce regrowth of the lesion. The recurrence rate for the peripheral ossifying fibroma is about 16%.
Other Peripheral Odontogenic Tumors
Several other odontogenic tumors have been reported to occur in the gingiva without underlying bone involvement. Although rare, these lesions are important to the dental hygienist because of their gingival location. The peripheral ameloblastoma (described earlier in this chapter) and the peripheral calcifying epithelial odontogenic tumor have been reported to occur in this location.
Treatment for the tumors described previously is surgical excision. After appropriate treatment recurrence is rare.
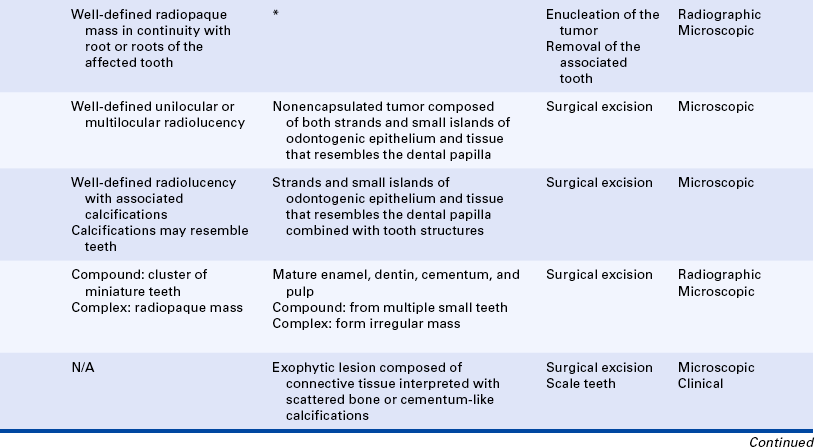
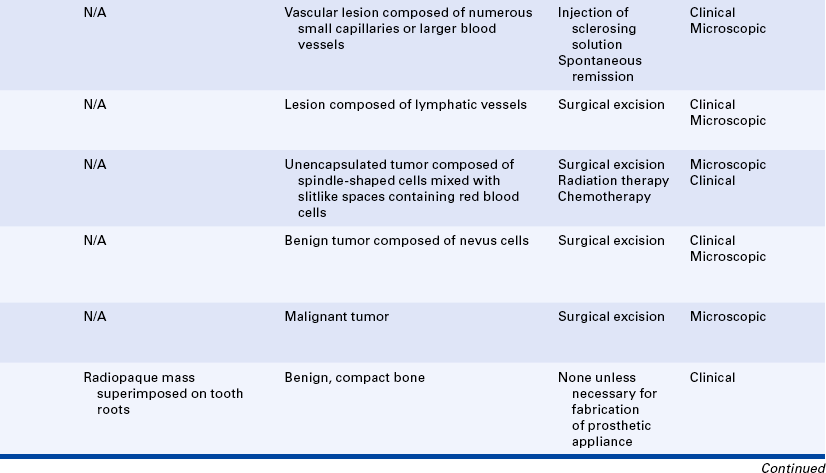
TUMORS OF SOFT TISSUE
Tumors of soft tissue include benign and malignant tumors of adipose tissue (fat), nerve, muscle, blood, and lymphatic vessels.
LIPOMA
The lipoma is a benign tumor of mature fat cells. Clinically it appears as a yellowish mass that is surfaced by a thin layer of epithelium (Figure 7-30, A). Because of this thin epithelium, a delicate pattern of blood vessels is usually seen on its surface. The majority of lipomas occur in individuals over 40 years of age, and no sex predilection is noted. The most common intraoral locations are the buccal mucosa and the vestibule. Microscopic examination reveals a well-delineated tumor composed of lobules of mature fat cells that are uniform in size and shape (Figure 7-30, B).
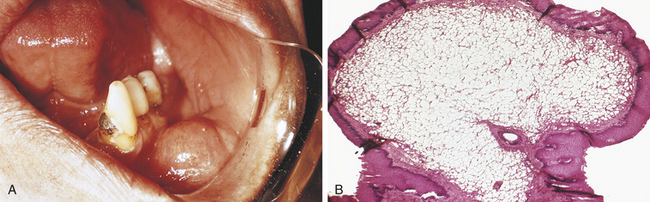
FIGURE 7-30 A, Clinical appearance of a lipoma. B, Photomicrograph of a lipoma shows mature fat cells. (A courtesy Dr. Edward V. Zegarelli.)
The lipoma is treated by surgical excision and generally does not recur.
TUMORS OF NERVE TISSUE
The neurofibroma (Figure 7-31, A) and the schwannoma are benign tumors derived from nerve tissue. The schwannoma is also called a neurilemmoma. The schwannoma is derived from Schwann cells, and the neurofibroma is derived from Schwann cells and perineural fibroblasts. Both of these cells are components of the connective tissue surrounding a nerve. Although the neurofibroma and schwannoma are distinct tumors microscopically, they are quite similar in their clinical presentation and behavior and therefore are discussed together. The tongue is the most common intraoral location. Neurofibromas and schwannomas may occur at any age, and no sex predilection is noted. Microscopic examination of a neurofibroma reveals a fairly well-delineated but unencapsulated, proliferation of spindle-shaped Schwann cells and perineural fibroblasts (Figure 7-31, B). A schwannoma is composed of spindle-shaped Schwann cells arranged in palisaded whorls around a central pink zone. A connective tissue capsule surrounds the schwannoma.
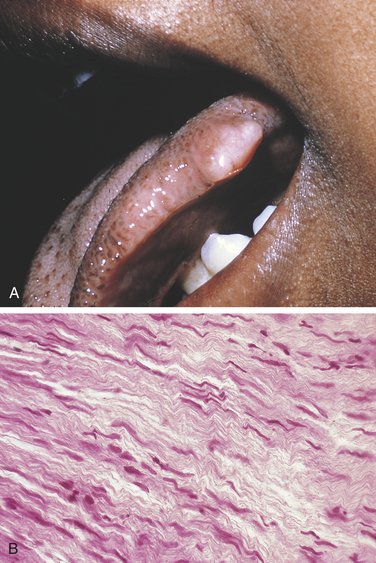
FIGURE 7-31 A, Clinical appearance of a neurofibroma shows a nonulcerated mass on the lateral border of the tongue. B, Photomicrograph of a neurofibroma.
A neurofibroma and a schwannoma are both treated by surgical excision. They generally do not recur. Malignant tumors of nerve tissue occur but are extremely rare.
Multiple neurofibromas occur in a genetically inherited disorder known as neurofibromatosis of von Recklinghausen or von Recklinghausen's disease. Patients with this syndrome have numerous neurofibromas on the skin and other sites in addition to other abnormalities. This syndrome is genetically inherited and is described in detail in Chapter 6.
Granular Cell Tumor
The granular cell tumor is a benign tumor composed of large cells with a granular cytoplasm. It most likely arises from a neural or primitive mesenchymal cell. The granular cell tumor most often occurs on the tongue, followed by the buccal mucosa. It appears as a painless, nonulcerated nodule (Figure 7-32, A). Most cases occur in adults, and a female sex predilection is noted. Microscopic examination reveals large oval-shaped cells with a granular cytoplasm. The granular cells are found in the connective tissue and between striated muscle fibers (Figure 7-32, B). The overlying surface epithelium may exhibit pseudoepitheliomatous hyperplasia, which is a benign proliferation of epithelium into the connective tissue (Figure 7-32, C).
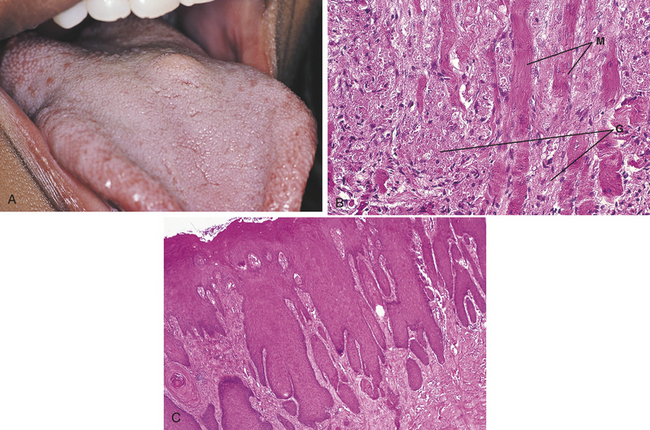
FIGURE 7-32 A, Clinical appearance of a granular cell tumor of the tongue shows a nonulcerated mass. B, Photomicrograph of a granular cell tumor showing granular cell(s) (G) between striated muscle fiber(s) (M). C, Photomicroscope of a granular cell tumor showing overlying pseudoepitheliomatous hyperplasia. (A courtesy Dr. Sidney Eisig.)
This tumor is treated by surgical excision and does not recur.
Congenital Epulis
The congenital epulis, or congenital epulis of the newborn, is a benign neoplasm composed of cells that closely resemble those seen in the granular cell tumor. The neoplasm most likely arises from a primitive mesenchymal cell. This tumor is present at birth and appears as a sessile or pedunculated mass on the gingiva. It usually occurs on the anterior maxillary gingiva and almost always occurs in girls.
The congenital epulis is treated by surgical excision and does not recur. Occasional examples have regressed without treatment.
TUMORS OF MUSCLE
Tumors of muscle are extremely uncommon in the oral cavity. The rhabdomyoma, a benign tumor of striated muscle, has been reported to occur on the tongue. The leiomyoma, a benign tumor of smooth muscle, may occur in association with blood vessels. These tumors are called vascular leiomyomas and occasionally occur in the oral cavity.
The rhabdomyosarcoma, a malignant tumor of striated muscle, is the most common malignant soft tissue tumor of the head and neck in children. It typically occurs in individuals under 10 years of age and has a male sex predilection. It is a rapidly growing, destructive tumor. The rhabdomyosarcoma is an aggressive malignant tumor that is best treated by a combination of multidrug chemotherapy, radiation therapy, and surgery. Despite treatment, the prognosis is poor.
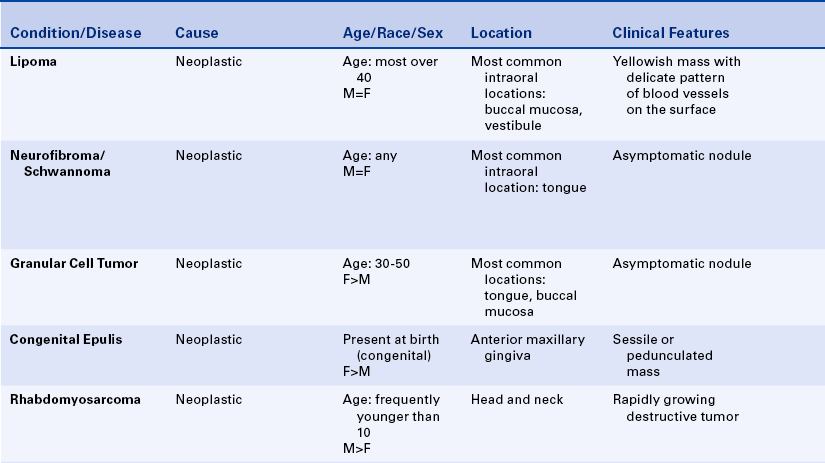
VASCULAR TUMORS
The hemangioma is a benign proliferation of capillaries (Figure 7-33, A and B). It is a common vascular lesion considered by many to represent a developmental lesion rather than a tumor because hemangiomas generally do not exhibit an unlimited growth potential. Some contain numerous small capillaries and are called capillary hemangiomas. Others contain larger blood vessels and are called cavernous hemangiomas (Figure 7-33, C).
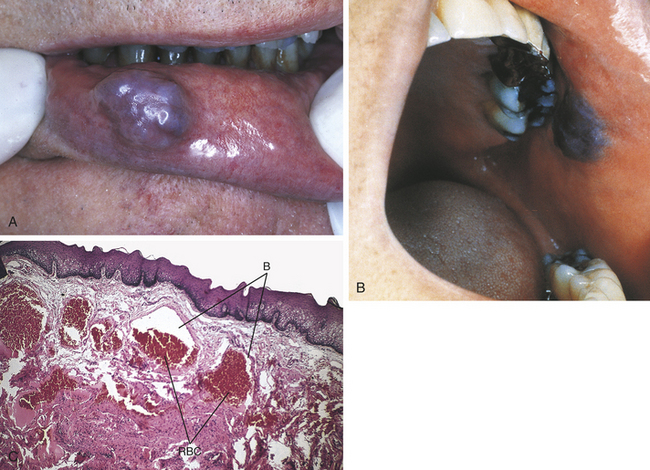
FIGURE 7-33 Clinical appearance of a hemangioma of the lower lip (A) and of the buccal mucosa (B). C, Microscopic appearance of a cavernous hemangioma showing large dilated blood vessels (B) filled with red blood cells (RBC).
Most are present at birth or arise shortly thereafter. More than half of the hemangiomas that occur in the body occur in the head and neck area. The tongue is the most common intraoral location. Involvement of the tongue often leads to marked enlargement (macroglossia). Hemangiomas are more common in girls than in boys. They also occur in adults as a response to trauma and represent an abnormal proliferation of blood vessels during the healing process. They appear as variably sized, deep-red or blue lesions that frequently blanch when pressure is applied.
Many hemangiomas undergo spontaneous remission. Others can enlarge rapidly because of hemorrhage, thrombosis, or inflammation. Treatment is variable and includes surgery or the injection of a sclerosing solution into the lesion, which causes it to resolve.
Lymphangioma
The lymphangioma is a benign tumor of lymphatic vessels. It is less common than the hemangioma. Most lymphangiomas are present at birth, and half arise in the head and neck area. No sex predilection is noted. The most common intraoral location is the tongue, where the lymphangioma presents as an ill-defined mass with a pebbly surface. Involvement of the tongue may lead to macroglossia. A cystic lymphangioma in the neck is called a cystic hygroma. It is usually present at birth or develops shortly thereafter.
Lymphangiomas generally are treated by surgical excision and tend to recur.
Malignant Vascular Tumors
Malignant vascular tumors such as angiosarcoma may occur in the oral cavity but are rare. Kaposi sarcoma is a malignant vascular tumor and may arise in multiple sites, including the skin and oral mucosa. Classic Kaposi sarcoma occurs as multiple purplish tumors of the lower extremities in older men. The condition in these patients progresses slowly, usually resolves with low doses of radiation, and rarely causes death. With the advent of the human immunodeficiency virus (HIV) epidemic in the 1980s, Kaposi sarcoma has appeared in a much more aggressive form. In HIV-positive patients these lesions are often seen in the oral cavity, where they present as purple macules, plaques, or exophytic tumors. The hard palate and gingiva are the most common intraoral sites. Kaposi sarcoma associated with HIV infection is described in Chapter 4. It may also occur in patients with other forms of immunodeficiency, specifically patients who have received immunosuppressive drug therapy as a result of organ transplantation.
Kaposi sarcoma is caused by a human herpesvirus (HHV) that is called both human herpesvirus type 8 and Kaposi sarcoma–associated herpesvirus. Men are affected more often than women. Microscopic examination reveals a neoplasm composed of spindle-shaped cells mixed with slitlike spaces containing red blood cells.
Kaposi sarcoma is treated by surgical excision, radiation therapy, chemotherapy, or a combination of these therapies. In HIV-positive patients recurrence is common, and the disease may progress rapidly.
MELANOCYTIC NEVI
The word nevus (plural, nevi) has two meanings. Here the word is used to mean a benign tumor of melanocytes (melanin-producing cells), which are called nevus cells. Nevus also refers to a pigmented congenital lesion (a lesion present at birth). A hemangioma present at birth is an example of this second type of nevus.
Melanocytic nevi can arise on the skin or the oral mucosa. Intraoral tumors consist of tan-to-brown macules or papules that occur most often on the hard palate. The buccal mucosa is the second most common intraoral location (Figure 7-34). They occur twice as often in women as in men and are usually first identified in individuals between 20 and 50 years of age. Basal cell carcinomas are a component of the inherited nevoid basal cell carcinoma syndrome described in Chapter 6.
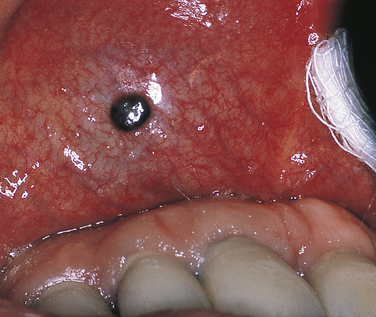
FIGURE 7-34 Clinical appearance of a melanocytic nevus shows a well-defined pigmented lesion on the labial mucosa.
Most pigmented lesions that occur in the oral cavity are benign. Pigmented lesions that exhibit ulceration, an increase in size, or a change in color may be malignant.
A biopsy followed by microscopic examination is indicated for pigmented lesions of unknown cause, unknown duration, or recent onset. Surgical excision is the treatment of choice for intraoral melanocytic nevi. Recurrence is rare.
MALIGNANT MELANOMA
Malignant melanoma is a malignant tumor of melanocytes (Figure 7-35). Although the name malignant melanoma suggests that a benign counterpart exists, all melanomas are malignant. Most malignant melanomas arise on the skin as a result of prolonged exposure to sunlight. Primary malignant melanoma of the oral cavity is rare. However, malignant melanomas that arise on the skin may metastasize to the oral cavity.
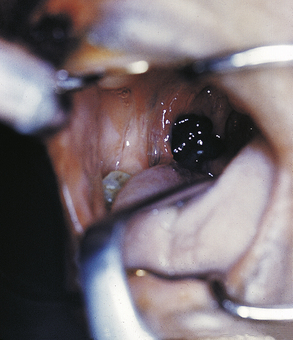
FIGURE 7-35 Clinical appearance of a malignant melanoma shows a darkly pigmented lesion in the area of the fauces. (Courtesy Dr. Edward V. Zegarelli.)
Malignant melanoma usually presents as a rapidly enlarging blue-to-black mass. Malignant melanoma is a very aggressive tumor that exhibits an unpredictable behavior and early metastasis. The most common intraoral locations are the palate and maxillary gingiva. These neoplasms usually occur in adults older than 40 years of age.
Malignant melanomas are treated by surgical excision. Chemotherapy may be used in conjunction with surgery. The prognosis for oral malignant melanoma is poor.
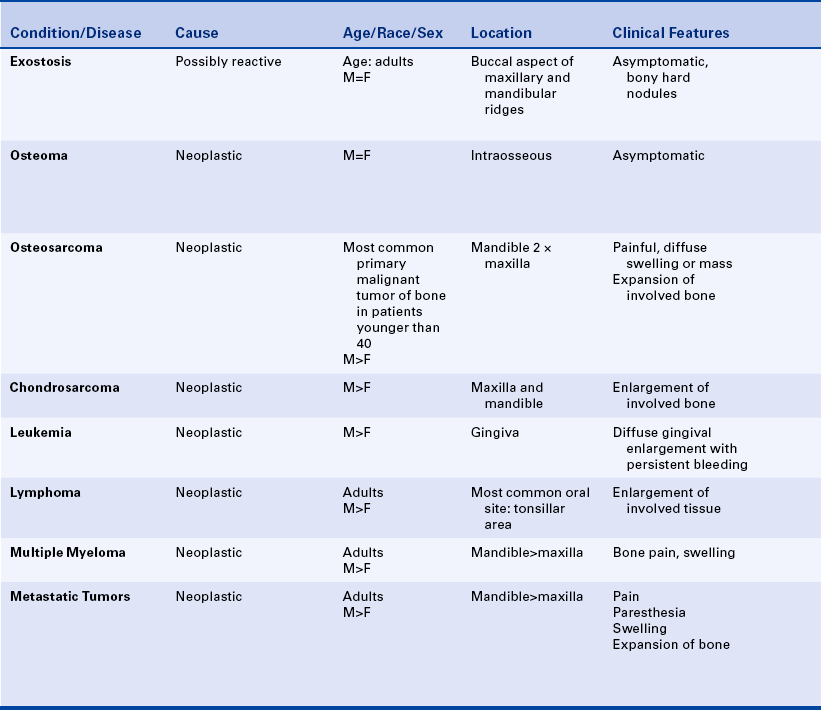
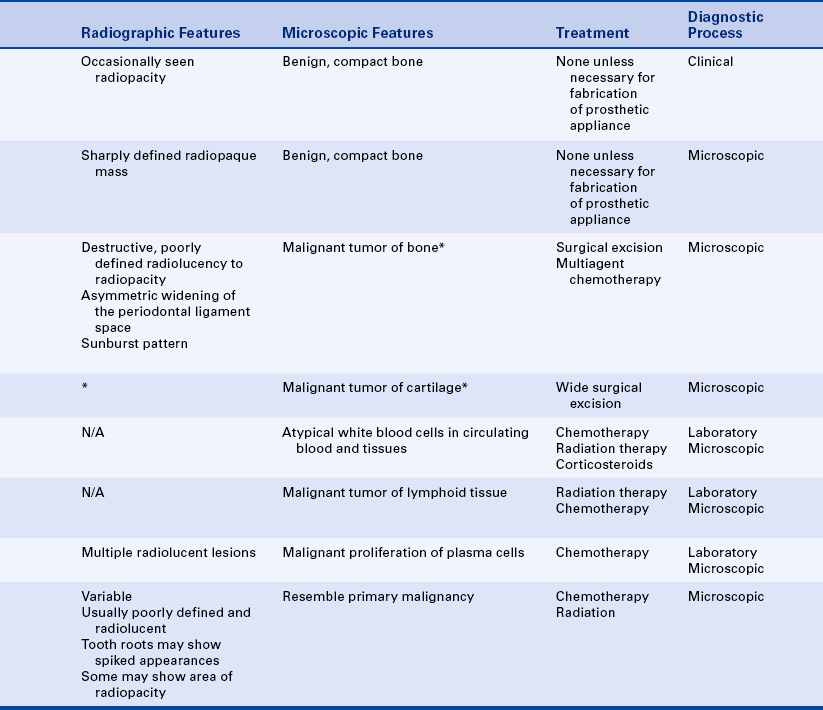
TORUS
A torus (plural, tori) is a benign lesion composed of normal compact bone. Tori are located in the midline of the palate (torus palatinus or palatal torus) or the lingual aspect of the mandible in the area of the premolars (torus mandibularis or mandibular torus) (Figure 7-36, A and B). Tori are not true tumors. Because they have a hereditary basis, they are also discussed in Chapter 6. They are described in this chapter because of their resemblance to an osteoma. Tori occur in adults and are more common in women than in men. They present as an asymptomatic, bony hard, lobulated mass covered by epithelium with very little underlying fibrous connective tissue. Surface ulceration may occur if a torus is traumatized. Palatal or mandibular tori may result in radiopaque areas superimposed on tooth roots. The diagnosis is confirmed by the presence of a torus on clinical examination.
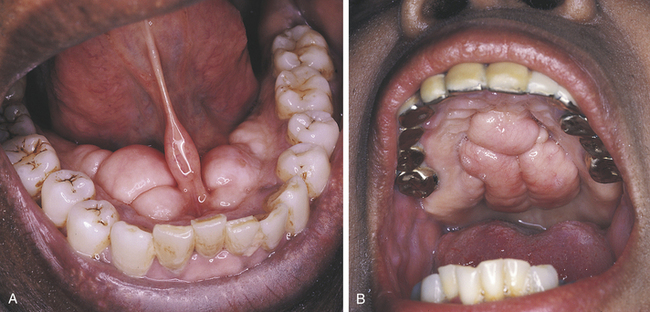
FIGURE 7-36 A, Clinical appearance of bilateral lobulated mandibular tori. B, Clinical appearance of a lobulated torus palatinus.
No treatment is necessary unless they interfere with the fabrication of a prosthetic appliance. If a prosthetic appliance needs to be constructed, a torus should be excised surgically.
EXOSTOSIS
An exostosis (plural, exostoses) is a small nodular excrescence of normal compact bone (Figure 7-37). Exostoses present as asymptomatic, bony hard nodules on the buccal aspect of the maxillary or mandibular alveolar ridges. Most cases occur in adults, and no sex predilection is noted. An increased incidence is noted in individuals who have a grinding or bruxing habit.

FIGURE 7-37 Clinical appearance of exostoses on the labial and buccal aspect of the maxilla. Less prominent exostoses are noted on the labial and buccal aspect of the mandible.
No treatment is indicated unless they interfere with the fabrication of a prosthetic appliance. If a prosthetic appliance needs to be constructed, an exostosis should be excised surgically.
OSTEOMA
An osteoma is an asymptomatic benign tumor composed of normal compact bone. It is a slow-growing tumor that appears radiographically as either a sharply defined radiopaque mass within bone or a delineated mass attached to the outer surface of the bone (Figure 7-38). A large osteoma within bone may cause expansion of the involved bone. No sex predilection is noted. The most common location within the jaws is the posterior mandible. Osteomas are a component of Gardner syndrome that is transmitted genetically and described in Chapter 6.
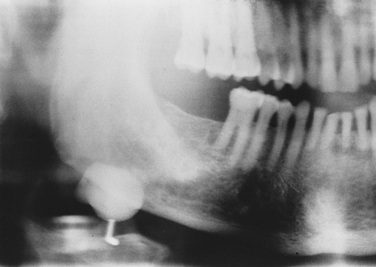
FIGURE 7-38 Radiograph of an osteoma shows a radiopacity of the posterior mandible. (Courtesy Dr. Sidney Eisig.)
Osteomas are treated by surgical excision and generally do not recur.
OSTEOSARCOMA
Osteosarcoma (osteogenic sarcoma) is a malignant tumor of bone-forming tissue. It is the most common primary malignant tumor of bone in patients under 40 years of age. Tumors that involve the long bones occur at an average age of 27 years, whereas the average age of occurrence for tumors that involve the jaws is about 37 years of age. These tumors occur in the mandible twice as frequently as in the maxilla and are more common in men than in women. Patients may experience a diffuse swelling or mass that is often painful (Figure 7-39, A). Some patients present initially with a toothache or exhibit tooth mobility. Paresthesia of the lip is common in tumors involving the mandible.
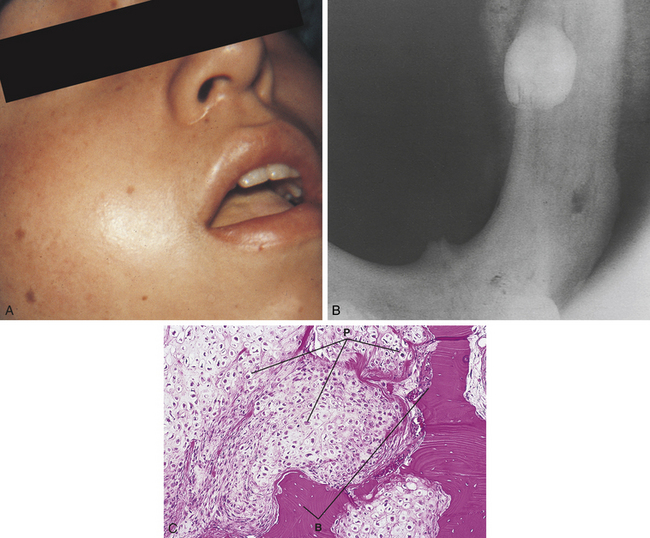
FIGURE 7-39 A, Clinical appearance of an osteogenic sarcoma shows swelling. B, Radiograph of an osteogenic sarcoma in the left molar area shows a poorly defined radiopaque lesion. C, Microscopic appearance of an osteogenic sarcoma shows pleomorphic (P) and hyperchromatic cells and bone formation (B).
The radiographic appearance of an osteosarcoma varies from radiolucent to radiopaque (Figure 7-39, B). It is usually a destructive, poorly defined lesion and may or may not involve the adjacent soft tissue. Asymmetric widening of the periodontal ligament space and a sunburst pattern may be seen radiographically in some cases. Microscopic examination of this tumor shows pleomorphic and hyperchromatic cells and abnormal bone formation. Abnormal cartilage formation may also be present (Figure 7-39, C).
Currently osteosarcomas are treated with preoperative multiagent chemotherapy followed by surgery. Jaw tumors frequently recur after treatment. Only about 20% of patients with osteosarcoma of the jaws survive 5 years.
TUMORS OF CARTILAGE
Cartilaginous tumors of the jawbones are extremely rare and are more likely to be malignant than benign. A chondroma is a benign tumor of cartilage. A chondrosarcoma is a malignant tumor of cartilage (Figure 7-40). A chondrosarcoma may occur in either the maxilla or the mandible and is more common in men than in women. Most patients have enlargement of the affected bone.
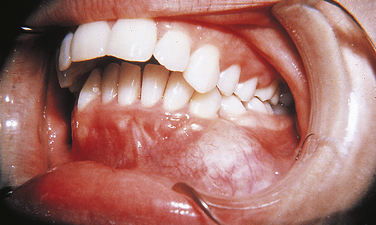
FIGURE 7-40 Clinical appearance of a chondrosarcoma shows an exophytic mass in the anterior mandible.
Chondrosarcomas are treated by wide surgical excision. Radiation therapy and chemotherapy are not effective. The prognosis is poor. Only about 30% of patients with chondrosarcoma involving the jaws survive 5 years after the diagnosis.
LEUKEMIA
Leukemia comprises a broad group of disorders characterized by an overproduction of atypical white blood cells. The atypical white blood cells proliferate in the bone marrow and then spill into the circulating blood and tissues. Several types of leukemia are classified according to the kind of cells that are proliferating: myelocytes, lymphocytes, or monocytes.
Leukemias are divided into two forms: acute and chronic. Acute leukemia is most common in children and young adults and is characterized by a proliferation of immature white blood cells (blasts). Chronic leukemia is characterized by an excess proliferation of mature white blood cells and most frequently occurs in middle-age adults. Leukemia occurs more often in men than in women.
Although oral involvement may occur in any type of leukemia, the monocytic variant most often exhibits oral lesions. A common oral manifestation of monocytic leukemia is diffuse gingival enlargement with persistent bleeding (Figure 7-41). (Leukemia is further described in Chapter 9.)

FIGURE 7-41 Clinical appearance of a patient with leukemic infiltration of the gingiva resulting in diffuse enlargement. (Courtesy Dr. Edward V. Zegarelli.)
The treatment of leukemia consists of chemotherapy, radiation therapy, and corticosteroids. The prognosis depends on the type of leukemia and the extent of disease.
LYMPHOMA (NON-HODGKIN'S LYMPHOMA)
Lymphoma is a malignant tumor of lymphoid tissue. Numerous types of lymphoma exist, each of which is differentiated on the basis of microscopic findings. The characteristic clinical presentation is gradual enlargement of involved lymph nodes. Rarely a lymphoma may present as a primary lesion in the oral soft tissues or bone. However, most lymphomas involve either lymph nodes or aggregates of lymphoid tissue that are located in the digestive tract from the oral cavity to the anus. In the oral cavity lymphoid tissue is located at the base of the tongue, soft palate, and pharynx (Waldeyer's ring). The most common location for intraoral lymphoma is the tonsillar area. Lymphomas usually occur in adults and are more common in men than in women.
Lymphoma is treated by radiotherapy, surgery, chemotherapy, or a combination of these therapies. The prognosis depends on the type of lymphoma and the extent of involvement.
MULTIPLE MYELOMA
Multiple myeloma is a systemic, malignant proliferation of plasma cells that causes destructive lesions in bone. The neoplastic plasma cells produce large amounts of immunoglobulin. Most patients are older than 40 years of age, and the disease occurs most commonly in the seventh decade of life. Men are affected more often than women. Patients usually experience bone pain and swelling. Pathologic fracture of an involved bone is common and typically occurs in bones weakened as a result of their destruction by the proliferation of neoplastic plasma cells (Figure 7-42, A).
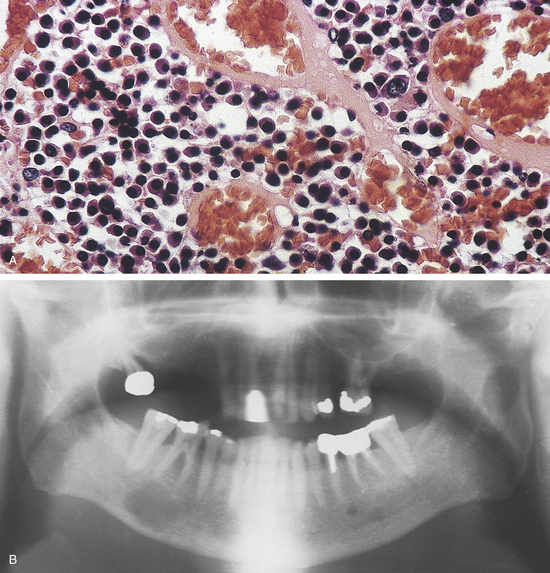
FIGURE 7-42 Multiple myeloma. A, Microscopic appearance of multiple myeloma shows a proliferation of plasma cells. B, Radiograph shows multiple radiolucent lesions of the mandible in a patient with multiple myeloma.
Radiographically the involved bones show multiple radiolucent lesions. The disease can involve the skull, spine, ribs, pelvis, long bones, and jaws. The mandible is affected more often than the maxilla (Figure 7-42, B). Most patients have an elevation of a single type of immunoglobulin, which is detected by a process called immunoelectrophoresis. This elevation is called a monoclonal spike. Patients may have fragments of immunoglobulins in the urine. These fragments are called Bence Jones proteins.
The tumors are composed of sheets of well- to–poorly differentiated plasma cells.
A localized tumor of plasma cells in soft tissue is called an extramedullary plasmacytoma. Although these are rare tumors, they are more common in the head and neck region than anywhere else in the body. Many patients with extramedullary plasmacytoma will eventually develop multiple myeloma. Therefore patients with a single tumor of plasma cells must be evaluated to determine if the lesion is solitary or part of multiple myeloma.
Patients with multiple myeloma are treated with chemotherapy and radiation. The prognosis is poor. The most common cause of death is infection followed by renal failure. Only 18% of patients survive 5 years after the diagnosis.
METASTATIC TUMORS OF THE JAWS
Metastatic tumors of the jaws from primary sites elsewhere in the body are rare. Most of these tumors arise from the thyroid, breast, lungs, prostate gland, and kidneys. The most frequent intraoral site for metastatic tumors of the jaws is the mandible. Patients display various signs and symptoms, including pain, paresthesia or anesthesia of the lip, swelling, expansion of the affected bone, and loosening of the teeth in the involved area. Metastatic lesions usually appear several years after the primary lesion is discovered. Occasionally the oral metastatic tumor is the first manifestation of a primary tumor elsewhere. Most patients are adults, and men are affected more often than women.
The radiographic appearance of metastatic tumors varies (Figure 7-43). Lesions are usually poorly defined and radiolucent. The roots of the involved teeth may show a spiked appearance. Metastatic tumors from the breast, prostate gland, and lungs may form bone and therefore may show areas of radiopacity.
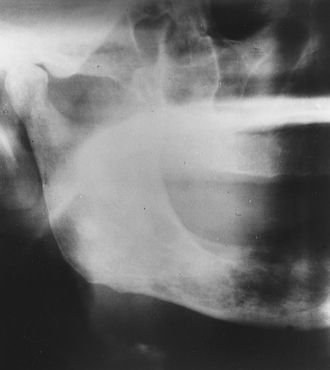
FIGURE 7-43 Radiograph shows diffuse radiolucent and radiopaque changes resulting from metastatic carcinoma of the prostate gland.
Histologically the metastatic tumor resembles the primary malignancy. Most metastatic tumors in the jaws are epithelial in origin, and most are adenocarcinomas.
Chemotherapy and radiation therapy are used to alleviate the discomfort of metastatic tumors in the jaws. The prognosis for patients with tumors that have metastasized to the jaws is poor.
Neville, B.W., et al. Oral and maxillofacial pathology, ed 3. St Louis: Saunders; 2009.
Regezi, J.A., Sciubba, J.J., Jordan, R.C.K. Oral pathology: clinical-pathologic correlations, ed 5. St Louis: Saunders; 2008.
Kumar, V., Cotran, R.S., Robbins, S.L. Robbins basic pathology, ed 8. Philadelphia: Saunders; 2007.
Abbey, L.M., Page, D.G., Sawyer, D.R. The clinical and histopathologic features of a series of 464 oral squamous cell papillomas. Oral Surg Oral Med Oral Pathol. 1980;49:419.
Damm, D.D., et al. Leukoplakia of the maxillary vestibule—an association with Viadent? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:61.
Fantasia, J.E., Damm, D.D. Oral Diagnosis: exophytic lesion of palatal mucosa: papilloma. Gen Dent. 2004;181:183.
Freitas, M.D., et al. Clinicopathologic aspects of oral leukoplakia in smokers and nonsmokers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:199.
Kaugars, G.E., et al. Actinic cheilitis: a review of 152 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:181.
Krutchkoff, D.F., et al. Oral cancer: a survey of 566 cases from the University of Connecticut Oral Pathology Biopsy Service 1975-1986. Oral Surg Oral Med Oral Pathol. 1990;70:192.
Medina, J.E., Dichtel, W., Luna, M.A. Verrucous-squamous carcinomas of the oral cavity: a clinicopathologic study of 104 cases. Arch Otolaryngol. 1984;110:437.
Padayachee, A., Van Wyk, C.W. Human papillomavirus (HPV) in oral squamous cell papillomas. J Oral Pathol. 1987;16:353.
Shibuya, H., et al. Multiple primary cancer risk in patients with squamous cell carcinoma of the oral cavity. Cancer. 1987;60:3083.
Warnakulasuriya, K.A.A.S., Ralhan, R. Clinical, pathological, cellular and molecular lesions caused by oral smokeless tobacco—a review. J Oral Pathol Med. 2007;36:63.
Shafer, W.G., Waldron, C.A. Erythroplakia of the oral cavity. Cancer. 1975;36:1021.
Silverman, S., Jr., Gorsky, M., Lozada, F. Oral leukoplakia and malignant transformation: a follow-up study of 257 patients. Cancer. 1984;53:563.
Waldron, C.A., Shafer, W.G. Leukoplakia revisited: a clinicopathologic study of 3256 oral leukoplakias. Cancer. 1975;36:1386.
Eveson, J.W., Cawson, R.A. Tumours of the minor (oropharyngeal) salivary glands: a demographic study of 336 cases. J Oral Pathol. 1985;14:500.
Pires, F.R., et al. Intra-oral minor salivary gland tumors: a clinicopathological study of 546 cases. Oral Oncol. 2007;43:463.
Waldron, C.A., El-Mofty, S.K., Gnepp, D.R. Tumors of the intraoral minor salivary glands: a demographic and histologic study of 426 cases. Oral Surg Oral Med Oral Pathol. 1988;66:323.
Ai-Ru, L., Zhen, L., Jian, S. Calcifying epithelial odontogenic tumors: a clinicopathologic study of 9 cases. J Oral Pathol. 1982;11:399.
Buchner, A., Ficarra, G., Hansen, L.S. Peripheral odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1987;64:432.
Courtney, R.M., Kerr, D.A. The odontogenic adenomatoid tumor: a comprehensive study of 20 new cases. Oral Surg Oral Med Oral Pathol. 1975;39:424.
Daley, T.D., Wysocki, G.P. Peripheral odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994;78:329.
Kaugars, G.E., Miller, M.E., Abbey, L.M. Odontomas. Oral Surg Oral Med Oral Pathol. 1989;67:172.
Shamaskin, R.G., Svirsky, J.A., Kaugars, G.E. Intraosseous and extraosseous calcifying odontogenic cyst (Gorlin cyst). J Oral Maxillofac Surg. 1989;47:562.
Ulmansky, M., et al. Benign cementoblastoma. Oral Surg Oral Med Oral Pathol. 1994;77:48.
Waldron, C.A., El-Mofty, S.K. A histopathologic study of 116 ameloblastomas with special reference to the desmoplastic variant. Oral Surg Oral Med Oral Pathol. 1987;63:441.
Furlong, M.A., Fanburg-Smith, J.C., Childers, E.L.B. Lipoma of the oral and maxillofacial region: site and subclassification of 125 cases. Oral Surg Oral Med Oral Pathol. 2004;98:441.
Cunha, K.S., et al. Neurofibromatosis type I with periodontal manifestations: a case report and literature review. Br Dent J. 2004;196:457.
Hernandez, G.A., et al. Aneurysmal bone cyst versus hemangioma of the mandible. Oral Surg Oral Med Oral Pathol. 1993;76:790.
Tumors of Melanin-Producing Cells
Kaugars, G.E., et al. Oral melanotic macules. Oral Surg Oral Med Oral Pathol. 1993;76:59.
Meleti, M., et al. Oral malignant melanoma: the Amsterdam experience. J Oral Maxillofac Surg. 2007;65:2181.
Canadian Society of Otolaryngology—Head and Neck Surgery Oncology Study Group. Osteogenic sarcoma of the mandible and maxilla: a Canadian review (1980-2000). J Otolaryngol. 2004;33:139.
Forteza, G., Colmenero, A., Lopez-Barea, F. Osteogenic sarcoma of the maxilla and mandible. Oral Surg Oral Med Oral Pathol. 1986;62:179.
Tumors of Blood-Forming Tissues
Lambertenghi-Deliliers, G., et al. Incidence of jaw lesions in 193 patients with multiple myeloma. Oral Surg Oral Med Oral Pathol. 1988;65:533.
Raubenheimer, E.J., Dauth, J., van Wilpe, E. Multiple myeloma: a study of 10 cases. J Oral Pathol. 1987;16:383.
Hasimoto, N., et al. Pathological characteristics of metastatic carcinoma in the human mandible. J Oral Pathol. 1987;16:362.
REVIEW QUESTIONS
1. Which of the following are associated with the neoplastic transformation of cells?
A Abnormal proliferation of cells in response to tissue damage.
B Controlled proliferation of cells.
C Normal arrangement of proliferating cells.
D Irreversible change that results in an uncontrolled multiplication of cells.
3. Which of the following statements concerning leukoplakia is true?
A Most cases represent examples of epithelial dysplasia.
B Sites that are at high risk for epithelial dysplasia include the palate and gingiva.
4. Which of the following is a characteristic of benign tumors?
5. A small white exophytic lesion on the palate is a benign lesion composed of squamous epithelium. Papillary projections are arranged in a cauliflower-like appearance. It is most likely a:
6. Which of the following is not a histologic characteristic of squamous cell carcinoma?
7. Which of the following are the most common locations for intraoral squamous cell carcinoma?
A Upper labial mucosa, buccal mucosa, and hard palate
B Lower labial mucosa, maxillary gingiva, and buccal mucosa
8. A patient with squamous cell carcinoma of the lateral tongue exhibits metastatic disease in the lungs. What clinical stage correlates with these findings?
9. Which of the following represents the earliest clinical example of squamous cell carcinoma?
10. The most appropriate treatment for epithelial dysplasia is:
11. Verrucous carcinoma is differentiated from squamous cell carcinoma because it:
12. The most common intraoral location for salivary gland tumors is the:
13. Which of the following is an example of a malignant salivary gland tumor?
14. Which of the following statements concerning an ameloblastoma is true?
15. The odontogenic tumor that characteristically appears as a well-circumscribed radiolucency located in the anterior maxilla of an adolescent girl is an:
16. Which odontogenic tumor most closely resembles the mesenchyme of the dental follicle?
17. A benign cementoblastoma may be recognized radiographically because:
A It is a well-circumscribed radiopaque lesion with a radiolucent halo attached to the root of a tooth.
B It has a radiolucent multilocular appearance.
C It is a radiolucent lesion surrounding the crown of an impacted tooth.
D It is an ill-defined radiolucent lesion containing scattered opacifications.
18. Which of the following lesions characteristically occurs on the alveolar mucosa?
19. Human herpesvirus 8 is associated with:
20. A compound odontoma differs from a complex odontoma in that a compound odontoma:
A Is composed of toothlike structures.
B Has unlimited growth potential.
21. Peripheral odontogenic tumors are located on the:
22. A benign tumor of adipose tissue is called a:
23. The most common malignant soft tissue tumor of the head and neck in children is:
24. Malignant melanoma of the oral cavity is rare; however, the most common intraoral location is the:
25. Which of the following neoplasms often occurs in the buccal mucosa or vestibule?
26. A malignant tumor of bone-forming tissue is called:
27. An overproduction of atypical white blood cells in the circulating blood is called:
28. Which of the following is a malignant tumor of lymphocytes?
29. The cell involved in multiple myeloma is the:
30. The most frequent intraoral site for metastatic tumors is the:
31. Which of the following tumors is associated with von Recklinghausen's disease?
32. Which of the following is the most common odontogenic tumor?
33. Which of the following salivary gland tumors often occurs in adult men?
34. A benign tumor composed of a proliferation of capillaries is called a:
35. A white plaquelike lesion that cannot be rubbed off or diagnosed clinically as a specific disease is called:
36. All of the following are benign lesions that histologically contain bone or bonelike material except a(n):
37. Which of the following malignant tumors may present as diffuse gingival enlargement with persistent bleeding?
38. Which of the following malignancies is characterized by a monoclonal spike on immunoelectrophoresis?
39. Which of the following malignant tumors has been reported to show a characteristic sunburst pattern on radiographic examination?
40. All of the following neoplasms arise from squamous epithelium except a(n):
41. All of the following are true concerning solar cheilitis except one. Which one is the exception?
A Mottled grayish-pink discoloration of lower lip
B Distinct demarcation between vermilion border and skin
42. Which of the following has the best long-term prognosis?
43. Which of the following does not arise in the oral cavity?
44. Which of the following may undergo malignant transformation?
45. Which of the following neoplasms occurs most often in males?
46. Pain is most often a clinical features of a(n):
47. Central involvement of the jaws may occur with a:
48. Syndrome involvement may occur with a(n):
49. Which of the following neoplasms is least likely to occur in the jaws?
50. Which of the following neoplasms has the worst long-term prognosis?