Chapter Fifteen Musculoskeletal system
INTRODUCTION
The musculoskeletal system is a vast organ system that provides locomotion, and an upright posture and protection for the body. It is composed of various forms of connective tissue which include bones, skeletal muscle, cartilage, ligaments, tendons and joints. In order to appreciate the impact of disease and trauma to this complex and dynamic system you are advised to first review the structure and function of bones, skeletal muscle, cartilage, ligaments, tendons and joints.
STRUCTURE AND FUNCTION
The musculoskeletal system has both structural and metabolic functions. Its structural function is essential for locomotion, respiration and the protection of internal organs and the central nervous system. The marrow within bones contains critical components of the haematopoietic and immune system. The bone marrow produces B cells, granulocytes and immature thymocytes, in addition to red blood cells and platelets.
Its metabolic function is as a storehouse for calcium, phosphorus and carbonate, and as a buffering system in hydrogen ion concentration. Bone plays a major role in conjunction with the renal system in blood calcium level regulation (Barnato and Sprague, 2009). The enormous mineral surface of the skeleton can also bind toxins and heavy metals, minimising their ability to cause cellular damage.
COMPONENTS OF THE MUSCULOSKELETAL SYSTEM
Bone
Bone is a mineralised connective tissue consisting of cells embedded in a protein matrix of collagen, alkaline phosphatase and osteopontin. This dynamic tissue responds to mechanical stresses through a complex process of remodelling. The remodelling process involves the resorption of micro-damaged bone by osteoclast cells followed by a phase of bone formation by osteoblast cells. In healthy adults this process is coupled to ensure bone density remains stable. Gonadal steroid hormones, parathyroid hormone and various growth factors have been shown to affect this process, indicating a central regulatory mechanism (Karsenty, 2000). When this process becomes uncoupled, normal bone density is altered, leading to a change in the normal architecture of bone seen in diseases such as osteoporosis (Seeman et al, 2006), and Paget’s disease (Matthews and Cundy, 2009).
Cartilage
This connective tissue is a firm gel-like substance characterised by resilience and the ability to absorb mechanical forces. The human body contains three major types of cartilage: hyaline cartilage, elastic cartilage and fibrocartilage. Hyaline cartilage is the most common type of cartilage found in parts of the respiratory tract and on joint surfaces. Within joints, articular cartilage protects the joint by distributing applied loads, and by providing a low-friction-bearing surface to maximise movement. Fibrocartilage is found in the intervertebral discs, menisci of the knee joint and the symphysis pubis. Its structure provides resistance to the compression and shearing forces within these joints. All types of cartilage are avascular and aneural, therefore tears in cartilage cannot heal.
Ligaments and tendons
Ligaments and tendons are connective tissues with complex biomechanical properties. Ligaments connect bone to bone and tendons connect muscles to bone. Injury to a ligament or tendon results in a drastic change in structure, resulting in the formation of scar tissue that is biomechanically inferior. For example, repair of the anterior cruciate ligament (ACL) in the knee requires a new piece of tissue graft from a hamstring muscle. The resultant graft does not possess the same qualities of strength and stability as the original ACL.
Muscles
There are three types of muscle in the human body: smooth, cardiac and skeletal muscle. Skeletal muscles are innervated by the motor nerve fibres of peripheral nerves. Conscious and subconscious contractions of muscles affect posture and locomotion and also generate reflexes. The human body contains over 400 skeletal muscles representing 40–50% of total body weight. A whole skeletal muscle is considered an organ of the muscular system. Skeletal muscle fibres have an abundant blood and nerve supply and are bundled together in a compartment wrapped in a tough fibrous connective tissue called fascia.
Diseases and disorders of the muscular system are diverse and include infections, hormonal, genetic and autoimmune disorders and malignancies. Minor traumatic injuries are the most common disorders of the muscular skeletal system. When major injury to muscles occurs as in limb trauma, intracompartmental tissue pressure can quickly rise. A rise in intracompartmental tissue pressure is known as compartment syndrome. This syndrome is characterised by muscle necrosis called rhabdomyolysis. Rhabdomyolysis ultimately leads to the release of cellular contents—including myoglobin into the circulatory system. This may result in potential life-threatening complications including myoglobinuric acute renal failure, hyperkalaemia and cardiac arrest (Malik et al, 2009; Rupert, 2002).
Joints
Joints are the functional units of the skeleton. Individual joints are described and classified by two qualities—the structure of the joint and the range of movement permitted by the joint.
Classification of joints by structure
Fibrous (synarthrotic) joints. The articulating bones are joined by fibrous connective tissue; for example, the joints (sutures) of the skull bones.
Cartilaginous (amphiarthrotic) joints. The articulating bones are joined by cartilage; for example, the pubic symphysis.
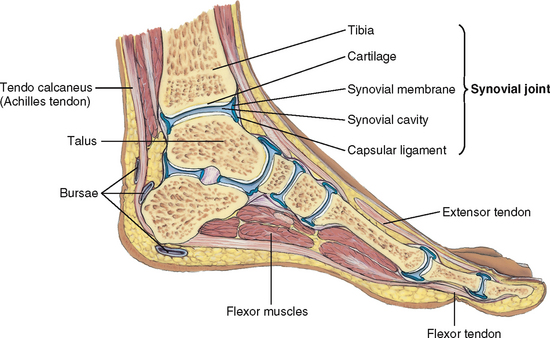
Synovial (diarthrotic) joints. These are freely mobile joints characterised by a joint cavity lined with synovial tissue and supported by ligaments, tendons and bursae (Fig 15.1). Synovial joints may be also sub-classified according to the type of movement that they permit; for example, the ball and socket joint of the hip and hinge joint of the knee.
Each joint reflects a compromise between stability and range of motion. The bones of the skull, for example, are stable but immobile, whereas the shoulder joint allows for a full range of motion but is a relatively unstable joint.
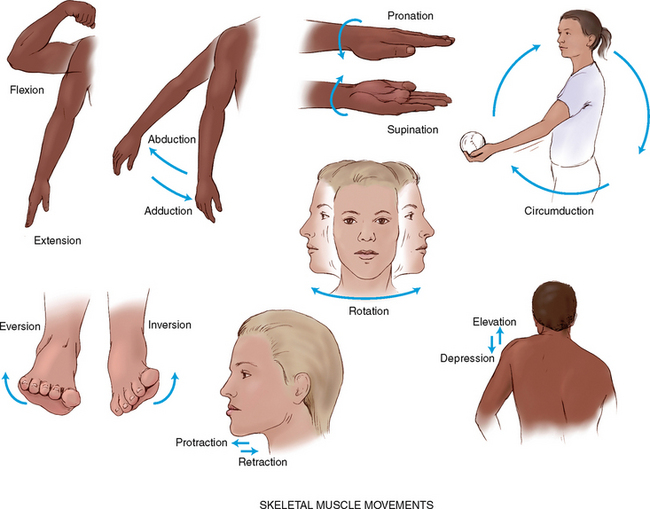
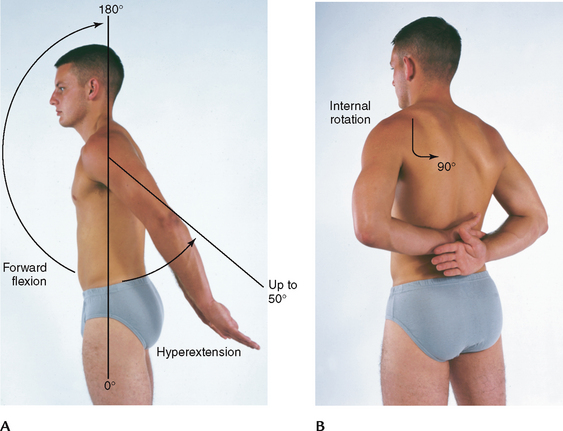
Movement of joints involving muscle contraction produces the following patterns of motion (Fig 15.2):
1. Flexion—bending a limb at a joint
2. Extension—straightening a limb at a joint
3. Abduction—moving a limb away from the midline of the body
4. Adduction—moving a limb towards the midline of the body
5. Pronation—turning the forearm so that the palm is down
6. Supination—turning the forearm so that the palm is up
7. Circumduction—moving the arm in a circle around the shoulder
8. Inversion—moving the sole of the foot inwards at the ankle
9. Eversion—moving the sole of the foot outwards at the ankle
10. Rotation—moving the head around a central axis
11. Protraction—moving a body part forwards and parallel to the ground
12. Retraction—moving a body part backwards and parallel to the ground
Joint anatomy
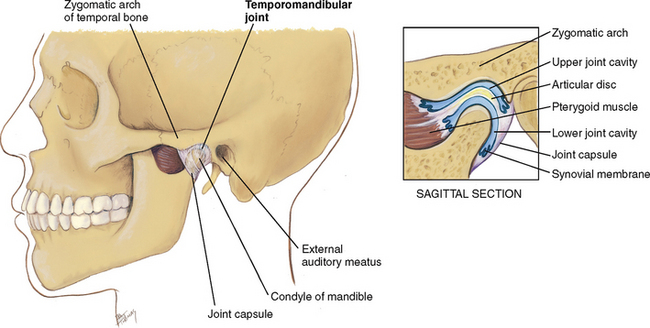
Temporomandibular joint.
The temporomandibular joint (TMJ) is the articulation of the mandible and the temporal bone (Fig 15.3). The TMJ permits jaw function for speaking and chewing. The joint allows three motions: (1) hinge action to open and close the jaws, (2) gliding action for protrusion and retraction and (3) gliding for side-to-side movement of the lower jaw.
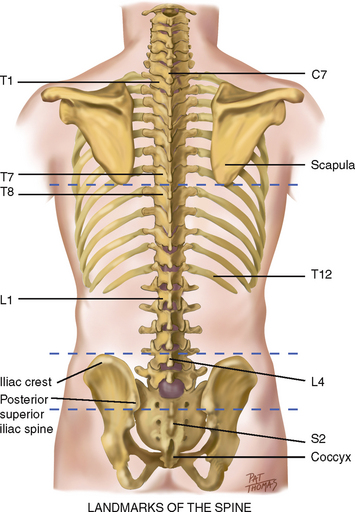
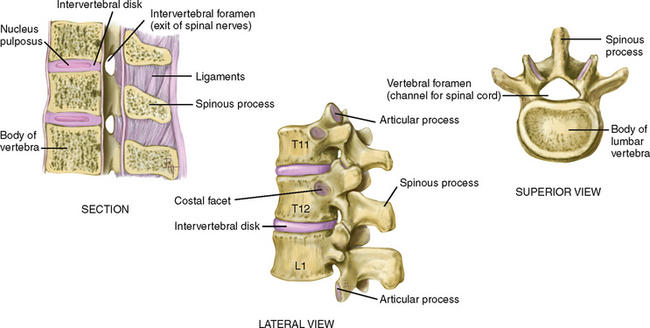
Spinal column.
The vertebrae are 33 connecting bones stacked in a vertical column (Fig 15.4). The spinous processes can be palpated as a furrow down the midline of the back. The furrow has paravertebral muscles mounded on either side down to the sacrum, where it flattens. Humans have 7 cervical, 12 thoracic, 5 lumbar, 5 sacral and 3 or 4 coccygeal vertebrae. The following surface landmarks will orient you to their levels:
• The spinous processes of C7 and T1 are prominent at the base of the neck.
• The inferior angle of the scapula normally is at the level of the interspace between T7 and T8.
• An imaginary line connecting the highest point on each iliac crest crosses L4.
• An imaginary line joining the two symmetric dimples that overlie the posterior superior iliac spines crosses the sacrum.
A lateral view shows that the vertebral column has four curves (a double-S shape) (Fig 15.5). The cervical and lumbar curves are concave (inwards or anterior), and the thoracic and sacrococcygeal curves are convex (outwards or posterior). The balanced or compensatory nature of these curves, together with the resilient intervertebral discs, allows the spine to absorb a great deal of shock.
The intervertebral discs are fibrocartilaginous plates that constitute one-quarter of the length of the column (Fig 15.6). Each disc is made up of three basic structures: the nucleus pulposus, the annulus fibrosus and the vertebral end plates. The inner nucleus pulposus is the semi-fluid gel centre, and has the consistency of toothpaste in the young adult. The main function of the intervertebral discs is to transfer the compression forces from one vertebra to another as loads are put on the spinal column during daily activities. As the spine moves, the elasticity of the discs allows compression on one side, with compensatory expansion on the other. If compression forces are too great, a disc can rupture and the nucleus pulposus can herniate out of the vertebral column, compressing the spinal nerves and causing pain.
The unique structure of the spine enables both upright posture and flexibility for motion. The motions of the vertebral column are flexion (bending forwards), extension (bending back), abduction (to either side) and rotation.
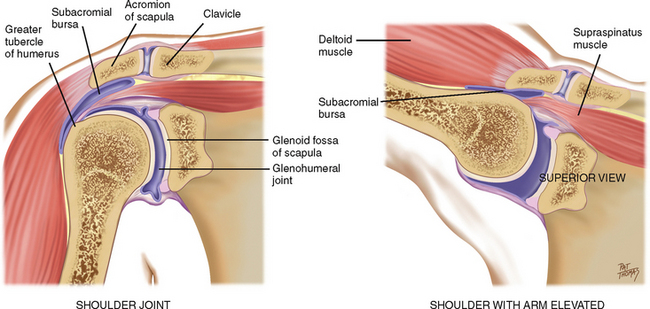
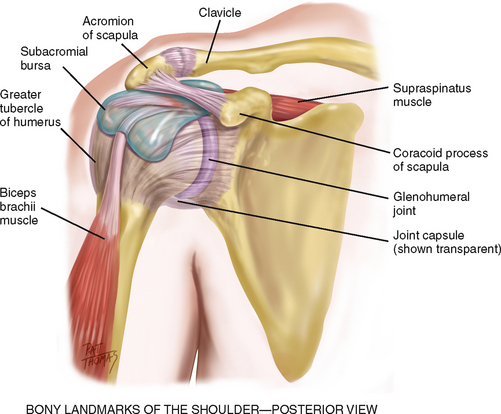
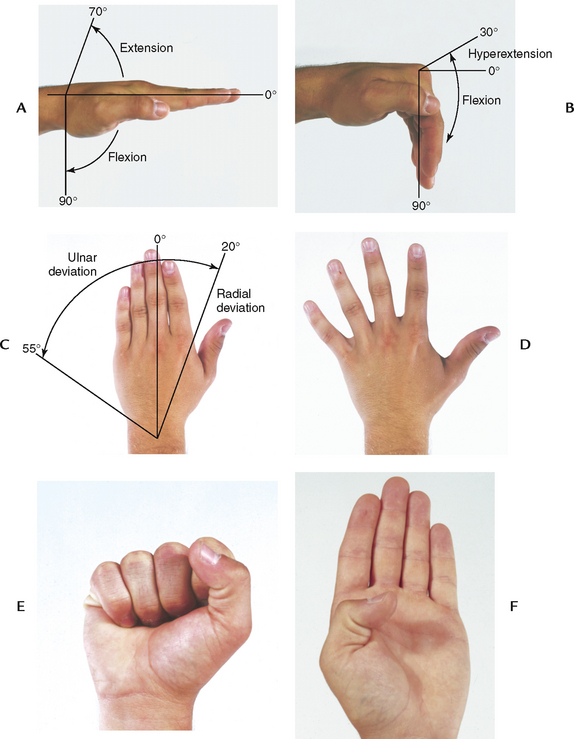
Shoulder.
The glenohumeral joint is the articulation of the humerus with the glenoid fossa of the scapula (Fig 15.7). Its ball-and-socket action allows great mobility of the arm on many axes. The joint is enclosed by a group of four powerful muscles and tendons that support and stabilise it. Together these are called the rotator cuff of the shoulder. The large subacromial bursa helps during abduction of the arm, so that the greater tubercle of the humerus moves easily under the acromion process of the scapula.
The bones of the shoulder have palpable landmarks to guide your examination (Fig 15.8). The scapula and the clavicle connect to form the shoulder girdle. You can palpate the bump of the scapula’s acromion process at the very top of the shoulder. Move your fingers in a small circle outwards, down and around. The next bump is the greater tubercle of the humerus a few centimetres down and laterally, and from that the coracoid process of the scapula is a few centimetres medially. These surround the deeply situated joint.
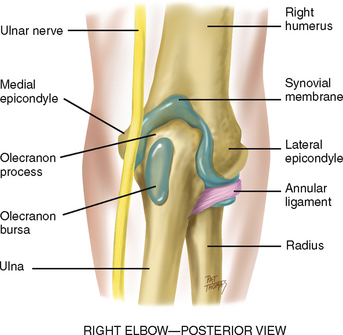
Elbow.
The elbow joint contains the three bony articulations of the humerus, radius and ulna of the forearm (Fig 15.9). Its hinge action moves the forearm (radius and ulna) on one plane, allowing flexion and extension. The olecranon bursa lies between the olecranon process and the skin.
Palpable landmarks are the medial and lateral epicondyles of the humerus and the large olecranon process of the ulna in between them. The sensitive ulnar nerve runs between the olecranon process and the medial epicondyle.
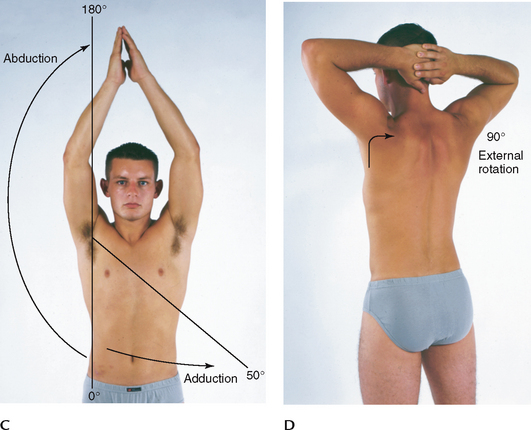
The radius and ulna articulate with each other at two radioulnar joints, one at the elbow and one at the wrist. These move together to permit pronation and supination of the hand and forearm.
Wrist and carpals.
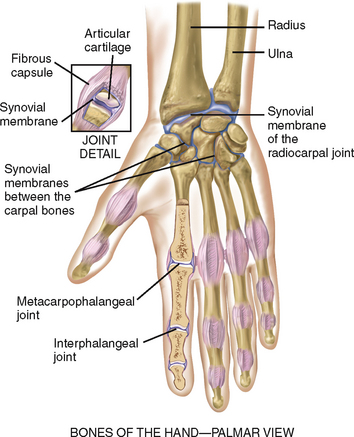
Of the body’s 206 bones, over half are in the hands and feet. The wrist or radiocarpal joint is the articulation of the radius (on the thumb side) and a row of carpal bones (Fig 15.10). Its condyloid action permits movement in two planes at right angles: flexion and extension, and side-to-side deviation. The groove of this joint can be palpated on the dorsum of the wrist.
The midcarpal joint is the articulation between the two parallel rows of carpal bones. It allows flexion, extension and some rotation. The metacarpophalangeal and the interphalangeal joints permit finger flexion and extension. The flexor tendons of the wrist and hand are enclosed in synovial sheaths.
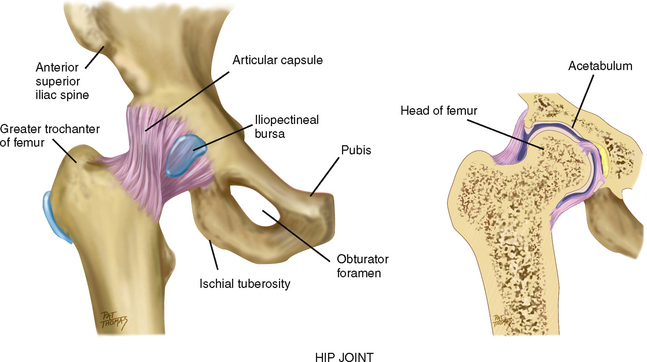
Hip.
The hip joint is the articulation between the acetabulum and the head of the femur (Fig 15.11). As in the shoulder, ball-and-socket action permits a wide range of motion on many axes. The hip has somewhat less range of motion (ROM) than the shoulder, but it has more stability as befits its weight-bearing function. Hip stability is due to powerful muscles that spread over the joint, a strong fibrous articular capsule and the very deep insertion of the head of the femur. Three bursae facilitate movement.
Palpation of these bony landmarks will guide your examination. You can feel the entire iliac crest, from the anterior superior iliac spine to the posterior. The ischial tuberosity lies under the gluteus maximus muscle and is palpable when the hip is flexed. The greater trochanter of the femur is normally the width of the person’s palm below the iliac crest and halfway between the anterior superior iliac spine and the ischial tuberosity. This landmark is best palpated when the person is standing, in a flat depression on the upper lateral side of the thigh.
Knee.
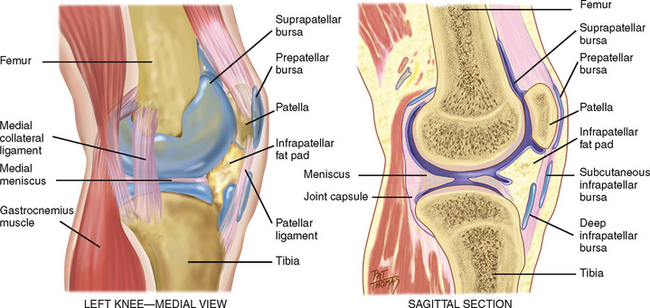
The knee joint is the articulation of three bones—the femur, the tibia and the patella (kneecap)—in one common articular cavity (Fig 15.12). It is the largest joint in the body and is complex. It is a hinge joint, permitting flexion and extension of the lower leg as well as a slight medial and lateral rotation.
The knee’s synovial membrane is the largest in the body. It forms a sac at the superior border of the patella, called the suprapatellar pouch, which extends up as much as 6 cm behind the quadriceps muscle. Two wedge-shaped cartilages, called the medial and lateral menisci, cushion the tibia and femur. The joint is stabilised by two sets of ligaments. The cruciate ligaments (not shown) crisscross within the knee; they give anterior and posterior stability and help control rotation. The collateral ligaments connect the joint at both sides; they give medial and lateral stability and prevent dislocation. Numerous bursae prevent friction. One, the prepatellar bursa, lies between the patella and the skin. The infrapatellar fat pad is a small, triangular fat pad below the patella behind the patellar ligament.
Landmarks of the knee joint start with the large quadriceps muscle, which is palpated on the anterior and lateral thigh (Fig 15.13). The muscle’s four heads merge into a common tendon that continues down to enclose the round bony patella. Then the tendon inserts down on the tibial tuberosity, which is palpated as a bony prominence in the midline. Move to the sides and superiorly and note the lateral and medial condyles of the tibia. Superior to these on either side of the patella are the medial and lateral epicondyles of the femur.
Ankle and foot.
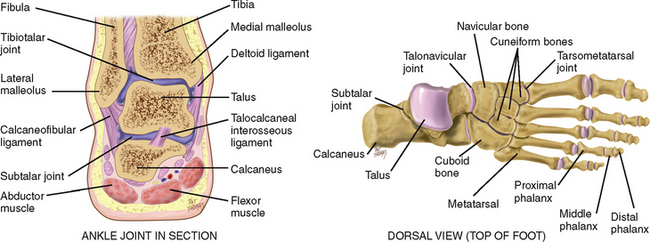
The ankle or tibiotalar joint is the articulation of the tibia, fibula and talus (Fig 15.14). It is a hinge joint, limited to flexion (dorsiflexion) and extension (plantar flexion) on one plane. Landmarks are two bony prominences on either side—the medial malleolus and the lateral malleolus. Strong, tight medial and lateral ligaments extend from each malleolus onto the foot. These help the lateral stability of the ankle joint, although they may be torn in eversion or inversion sprains of the ankle.
Joints distal to the ankle give additional mobility to the foot. The subtalar joint permits inversion and eversion of the foot. The foot has a longitudinal arch, with weight-bearing distributed between the parts that touch the ground—the heads of the metatarsals and the calcaneus (heel).
DEVELOPMENTAL CONSIDERATIONS
Infants and children
By 3 months gestation, the fetus has formed a ‘scale model’ of the skeleton that is made up of cartilage. During succeeding months in utero, the cartilage ossifies into true bone and starts to grow. Bone growth continues after birth—rapidly during infancy and then steadily during childhood—until adolescence, when both boys and girls undergo a rapid growth spurt.
Long bones grow in two dimensions. They increase in width or diameter by deposition of new bony tissue around the shafts. Lengthening occurs at the epiphyses, or growth plates. These specialised growth centres are transverse discs located at the ends of long bone. Any trauma or infection at this location puts the growing child at risk for bone deformity. This longitudinal growth continues until closure of the epiphyses; the last closure occurs at about age 20 years.
Skeletal contour changes are apparent at the vertebral column. At birth the spine has a single C-shaped curve. At 3 to 4 months, raising the baby’s head from prone position develops the anterior curve in the cervical neck region. From 1 year to 18 months, standing erect develops the anterior curve in the lumbar region.
Musculoskeletal conditions seen in the neonatal period include developmental dysplasia of the hip (DDH), talipes equinovarus (clubfoot) and upper and lower limb development deformities.
The term developmental dysplasia of the hip (DDH) describes a wide range of hip abnormalities found within the neonatal period in which the femoral head has an abnormal relationship to the acetabulum. Variances in these disorders range from stable hips with acetabular dysplasia to complete displacement of the femoral head out of an abnormal acetabulum. The prevalence of DDH varies due to diagnostic criteria, examiner skills and disorder progress. Minor hip dysplasia often resolves spontaneously (Hart et al, 2006). The incidence in Australia is cited as ≥19 per 1000 births (Goss, 2002). Successful clinical DDH screening programs within Australia using midwives, maternal child heath nurses and primary care clinicians have been created since the 1960s in order to eliminate ‘late diagnosed’ DDH. Untreated DDH has the potential to prevent long-term hip dysplasia and arthritis. Ultrasound imaging can be a valuable adjunct to the physical examination and a means of monitoring treatment in those high-risk infants—breech presentation, familial history of DDH, structural foot deformity or infants suffering a neuromuscular disease (Green and Oddie, 2008).
Musculoskeletal conditions, however, are evident throughout childhood, affecting up to 30% of children and adolescents. The majority are self-limiting, and often trauma related. These conditions also include life-threatening disorders such as malignant disease and infection (Foster and Kimura, 2009). Chronic musculoskeletal conditions include a spectrum of autoimmune/inflammatory joint and muscle disorders. An estimated 4600 Australian children in 2004–05 had arthritis (AIHW, 2008a). Juvenile arthritis affects the child’s growth and musculoskeletal development. The associated disability and chronic pain symptoms impacts on all aspects of the child’s life and family dynamics.
The pregnant female
It has been reported that almost all women experience some degree of musculoskeletal discomfort during pregnancy and 25% have at least temporarily disabling symptoms with low back pain cited as the most common complaint (Borg-Stein and Dugan, 2007).
Increased levels of circulating hormones (oestrogen, relaxin from the corpus luteum and corticosteroids) cause increased mobility in the joints. Increased mobility in the sacroiliac, sacrococcygeal and symphysis pubis joints in the pelvis contributes to the noticeable changes in maternal posture. The most characteristic change is progressive lordosis, which compensates for the enlarging fetus; otherwise, the centre of balance would shift forwards. Lordosis compensates by shifting the weight further back on the lower extremities. This shift in balance in turn creates strain on the low back muscles, which in some women is felt as low back pain during late pregnancy.
Anterior flexion of the neck and slumping of the shoulder girdle are other postural changes that compensate for the lordosis. These upper back changes may put pressure on the ulnar and median nerves during the third trimester. Carpal tunnel syndrome, for example, has a reported incidence of up to 25%. It is more common in older pregnant women with generalised oedema. Carpal tunnel syndrome found in association with pregnancy almost always resolves within 4 weeks of delivery (Van Slobbe et al, 2004).
Effects of pregnancy on preexisting musculoskeletal conditions
Pregnancy and the associated changes in circulating hormones and postural changes impact on a diverse range of preexisting musculoskeletal conditions. Examples include remission rates up to 75% of women with preexisting rheumatoid arthritis who become pregnant. The remission often continues until approximately 6 weeks postpartum, commonly followed by an exacerbation of symptoms. The exact aetiology of this remission is unknown (De Man et al, 2008). Knowledge of the effects of pregnancy on the musculoskeletal system is vital to ensure patients with preexisting conditions receive effective counselling and support during pregnancy.
Late adulthood (65+ years)
With ageing, loss of bone matrix (resorption) occurs more rapidly than new bone growth (deposition). The net effect is a loss of bone density, or osteoporosis. While the age-adjusted incidence of osteoporotic hip fracture in Australia appears to have decreased over recent years, the actual number of cases has increased in both sexes when population growth and the proportion of older people are taken into account. 2.2 million Australians have an osteoporosis related condition—this will become 3 million by 2021 with 1.65 million women and 0.51 million men affected (AIHW, 2008b). (See also ‘Promoting a healthy lifestyle: osteoporosis—“the silent disease”’ below.)
Postural changes are evident with ageing, and decreased height is the most noticeable. Long bones do not shorten with age. Decreased height is due to shortening of the vertebral column. This is caused by the gradual loss of water and associated thinning of the intervertebral discs. Both men and women can expect a progressive decrease in height beginning at age 40 years in males and age 43 years in females, although this decrease is not significant until age 60 years. A greater decrease occurs in the 70s and 80s as a result of osteoporotic collapse of the vertebrae. The result is a shortening of the trunk and comparatively long extremities. Other postural changes are kyphosis, and a backwards head tilt to compensate for the kyphosis, and a slight flexion of hips and knees.
The distribution of subcutaneous fat changes through life. Usually, men and women gain weight in their 40s and 50s. The contour is different, even if the weight is the same as when younger. They begin to lose fat in the face and deposit it in the abdomen and hips. In the 80s and 90s, fat further decreases in the periphery, which is especially noticeable in the forearms and apparent over the abdomen and hips. Loss of subcutaneous fat leaves bony prominences more marked (e.g. tips of vertebrae, ribs, iliac crests) and body hollows deeper, for example, cheeks and axillae.
An absolute loss in muscle mass occurs; some muscles decrease in size, and some atrophy, producing weakness. The contour of muscles becomes more prominent, and muscle bundles and tendons feel more distinct.
It has become more apparent that lifestyle affects musculoskeletal changes. A sedentary lifestyle hastens the musculoskeletal changes of ageing. High-impact exercise may increase bone strength and reduce hip fragility fractures, but research indicates that exercise needs to be performed frequently for an optimal response (Bailey and Brooke-Wavell, 2010).
The musculoskeletal changes and the associated musculoskeletal degenerative diseases have a major impact on the older person’s safety. Gait pattern changes include slowing down and shorter stride length (Moc et al, 2007). Every year, approximately 30% of Australians over 65 years old fall, with 10% of these falls leading to injury (ACSQHC, 2009). Falls-related injury is one of the leading causes of morbidity and mortality in older Australians. More than 80% of injury-related hospital admissions in people aged 65 years and over are due to falls and falls related injuries (ACSQHC, 2009). Falls are also associated with an increased incidence of death in people over 65 (Bradley and Pointer, 2008). The impact of a fall may lead to a fear of falling which spirals into self-imposed restriction of activity, and general functional decline, reducing both physical and social activities (Zijlstra et al, 2007). Falls prevention programs are thus widespread at both State and Commonwealth level within Australia (DOHA, 2007).
CULTURAL AND SOCIAL CONSIDERATIONS
Musculoskeletal conditions affect over one-third of the Australian population and represent some of the most common causes of pain and disability (ABS, 2006; AIHW, 2008a). The most common musculoskeletal conditions affecting Australians include arthritis, back pain and osteoporosis (ABS, 2006). Since 2002, arthritis and related musculoskeletal conditions have been an Australian National Health Priority Area (ABS, 2006).
This situation is evident globally with musculoskeletal conditions identified as being among the world’s leading causes of long-term pain and disability. The impact of musculoskeletal conditions includes chronic pain, deformity, mobility restriction and functional impairment, as well as affecting mental health and quality of life (Lidgren, 2003). Musculoskeletal conditions impact on families, and society in general, through reduced social interaction, role restrictions, lost productivity and the significant cost of ongoing management and treatment (WHO, 2004).
Road trauma represents a leading cause of traumatic musculoskeletal injury worldwide. In 2001, 495 300 Australians reported a long-term condition caused by a road trauma (ABS, 2003). Over 60% of road trauma victims were adults under 40 years of age (DoITRD, 2009). Sequelae include not only physical and functional impairments such as chronic pain and joint disorders, but also a range of psychological and social problems (Donaldson et al, 2009).
Indigenous Australian males are twice as likely to have a hip fracture as other Australian males, whereas Indigenous females are 26% more likely to have a hip fracture than other Australian females. Indigenous Australians are on average much younger than other Australians at the time of their hip fracture, aged 65 years (compared with 81 years) for males and 74 years (compared with 83 years) for females (AIHW, 2010b). Chronic musculoskeletal diseases and trauma statistics for Indigenous Australians are incomplete. However, higher incidence of smoking, excessive alcohol consumption, poor diet and obesity combined with major deficits in preventative healthcare programs would suggest a likely increased incidence of hip fracture in the future (AHMAC, 2006). (Refer to Ch 4 for further discussion of cultural considerations in health assessment.)
SUBJECTIVE DATA
General principles
As noted previously, musculoskeletal disorders cause pain, stiffness and impairment to activities of daily living.
A comprehensive musculoskeletal assessment should be integrated into a patient’s health assessment as numerous general health issues and prescribed medications affect this system. For example, chronic heart and lung disease impacts on mobility. Visual deficits, Vitamin B12 deficiency and incontinence all increase falls risks.
Musculoskeletal assessment is a systematic process involving application of knowledge of functional anatomy, and the mechanisms of injury and disease across the life span. As nursing roles expand within Australia it is often the nurse who has the first point of contact with the person in both community and hospital settings.
This assessment process involves initially allowing the patient to tell their story, through history taking, of the impact of their joint dysfunction and pain on their lives. Due to the often chronic nature of musculoskeletal disorders it is important to ask about previous complementary therapies, non-prescription medications and remedies. A thorough history will assist in identifying the nature of the musculoskeletal problems; for example, acute injury, degenerative, inflammatory, infective or malignant disorders.
A current medical history including medications is an essential part of musculoskeletal assessment. A variety of endocrine/metabolic disorders, nutritional conditions and medications can impact on bone health. Diseases such as hyperthyroidism, diabetes, renal disease, malabsorption syndromes and glucocorticoids, loop diuretics and aluminium are the most common risk factors (Hansberger, 2006). There is also a strong genetic link associated with musculoskeletal health so the patient should be asked to discuss any family history of fractures or arthritis (Giangregorio and Leslie, 2010).
As the musculoskeletal system is closely linked with the neurological system, it is suggested you refer to Chapter 22. As acute and chronic pain is also often associated with musculoskeletal disorders it is suggested you refer to Chapter 10.
Assessment components
1. Gait, arms, legs and spine (GALS) screening assessment
Trauma (fractures, sprains, dislocations)
5. Functional assessment (activities of daily living (ADLs))
| Assessment guidelines | Clinical significance and clinical alerts |
|---|---|
A screening musculoskeletal examination can rapidly identify those people who require comprehensive musculoskeletal assessment. The Gait Arms Legs and Spine (GALS) screening assessment is a highly sensitive, specific and well-validated screening assessment for the detection of joint abnormalities (ARC, 2005; Doherty, 1992; Lillicrap et al, 2003). Subjective data from this screening assessment involves 3 core questions. Positive responses indicate a detailed history should be taken. A paediatric-specific GALS assessment has also proved highly sensitive, specific and well-validated (ARC, 2005; Foster et al, 2006). |
|
| • Any problems with your joints? Tell me about your pain? | Joint pain and loss of function are the most common musculoskeletal concerns that prompt a person to seek care. |
| • Location: Which joints? On one side or both sides? | Rheumatoid arthritis (RA) involves symmetrical joints; other musculoskeletal illnesses and trauma involve isolated or unilateral joints. |
| • Quality: What does the pain feel like: aching, stiff, sharp or dull, shooting? Severity: How strong is the pain? | Exquisitely tender felt with acute inflammation. |
| • Onset: When did this pain start? | Chronic pain is often associated with degenerative musculoskeletal disorders. |
| • Timing: What time of day does the pain occur? How long does it last? How often does it occur? | RA pain is worse in morning when arising; osteoarthritis is worse later in the day; tendinitis is worse in morning, improves during the day. |
| • Is the pain aggravated by movement, rest, position, weather? Is the pain relieved by rest, medications, application of heat or ice? | Most joint pain is mechanical except in RA, when deformities restrict movement. Many patients have tried prescribed medications, homeopathic remedies, over-the-counter (OTC) medications or combination formulations. These need to be identified and included in your assessment. |
| • Is the pain associated with chills, fever, recent sore throat, trauma and repetitive activity? | Joint pain 10 to 14 days after an untreated strep throat suggests rheumatic fever. Joint injury occurs from trauma or repetitive motion. |
| • Any stiffness in your joints? | RA stiffness occurs in morning and after rest periods. |
| • Any swelling, heat, redness in the joints? | Suggests acute inflammation. |
| Decreased ROM may be due to joint disease or to muscle contracture. | |
| • Any problems in the muscles, such as any pain or cramping? Which muscles? | Myalgia is usually felt as cramping or aching. |
| • If in calf muscles: Is the pain with walking? Does it go away with rest? | Suggests intermittent claudication (Ch 11). |
| • Are your muscle aches associated with fever, chills, the ‘flu’? | Viral illness often includes myalgia. |
| • Any weakness in muscles? | Weakness may involve peripheral |
| • Location: Where is the weakness? How long have you noticed weakness? | vascular system or neurological systems (Chs 11 and 22). |
| • Do the muscles look different there? | Smaller muscles indicate atrophy. Swelling may indicate haematoma or tumour. |
| • When did this occur? What treatment was given? Any problems or limitations now as a result? | Previous joint trauma increases risk of degenerative arthritis. |
| Many patients with back pain have sought treatments provided by physiotherapists, chiropractors, osteopaths or acupuncturists. | |
| The aetiology is diverse, i.e. degenerative or traumatic conditions of the spine, fibrositis, inflammatory spondyloarthrop-athy and metabolic bone conditions are also cited as causes. | |
| • Any numbness and tingling? Any limping? | Spinal nerve-root dysfunction is associated with altered sensory and motor function. See Chapter 22. |
| Functional assessment screens the safety of independent living, the need for community supports and quality of life. | |
| • Bathing—getting in and out of the shower/bath, turning on taps? Can you wash your back, legs, feet, hair? | Degenerative lower limb joint dysfunction affects mobility and steppage and increases risk of falls. Upper limb nerve compression affects precision and grip, e.g. carpal tunnel syndrome. |
| • Toileting–urinating, moving bowels, able to get self on/off toilet, wipe self? | Altered bowel and bladder function may be an indication of cauda equina syndrome. |
| • Dressing–doing buttons, zipper, fasten opening behind neck, pulling dress or sweater over head, pulling up pants. Tying shoelaces, getting shoes that fit? | |
| • Grooming–shaving, brushing teeth, brushing or fixing hair, applying make-up? | Indicates upper limb dysfunction or psychosocial issues. |
| • Eating–preparing meals, pouring liquids, cutting up foods, bringing food to mouth, drinking? | Indicates upper limb dysfunction or psychosocial issues. |
| • Mobility–walking, walking up or down stairs, getting in/out of bed, getting out of house? | When the person is found to have significant impairment of mobility a falls risk screening must be conducted. |
| • Communicating–talking, using phone, writing? | Indicates upper limb/hand dysfunction. |
| Chronic diseases can cause social isolation and depression. | |
| • Tell me about your exercise program. Describe the type of exercise, frequency, the warm-up program. | |
| • Any pain during exercise? How do you treat it? | |
| • Has your weight changed recently? Please describe your usual daily diet. (Note the person’s usual caloric intake, all four food groups, daily amount of protein, calcium.) | |
| • Are you taking any medications for musculoskeletal system: aspirin, anti-inflammatory muscle relaxant, pain reliever? Are you taking any herbal supplements, vitamins or other ‘natural remedies’? | Over-the-counter medications are common first-line treatments for joint pain, e.g. glucosamine. |
| Chronic pain sufferers often use mul tiple analgesia. Herbal medications have iatrogenic effects. The potential interactions of herbal medicines with allopathic medicines have been well documented (Moses and McGuire, 2010). | |
| Assess for | |
| Additional history for infants and children | |
| Children with musculoskeletal problems often present to primary care services with traumatic or non-traumatic injuries. The majority of problems are self-limiting; however, the presentation of life-threatening illnesses such as malignancy or septic arthritis will require urgent referrals to specialty services. Chronic illnesses such as juvenile arthritis and the muscular dystrophies also require urgent referrals to improve care outcomes. Delays in access to care are well reported in childhood musculoskeletal illnesses (Dang-Tan and Franco, 2007; Foster et al, 2009; Mohamed et al, 2000). | Children with growing pains do not limp or experience morning stiffness. Non-accidental injury (NAI) can present as unexplained fracture patterns or bruising with incongruity between child’s and the carer’s/parent’s history. Ensuring the child’s safety and completing detailed documentation are priorities. Refer to your local State and Territory legislation on non-accidental injury and your local hospital/community guidelines for assessment and treatment plans. The nurse within the emergency department and primary setting requires a comprehensive knowledge of growth and development patterns from neonate to adolescent and the associated disease and injury profiles at different stages. Effective pain management is also essential if a comprehensive and targeted history is to be obtained. |
| Ask the parent the following questions: | Traumatic delivery increases risk for fractures (e.g. humerus, clavicle) and hip dysplasia. |
| Period of anoxia may result in hypoto-nia of muscles. | |
| Pain, joint dysfunction, malaise and fever all impact on activity and learning capacity, hence milestones may be affected. For example, toddler may stop walking, develop enuresis or have sleep disturbances. | |
| Recent fever with pain and/or swelling of one joint or bone may indicate an infective or inflammatory process. | |
| Fractures of the epiphyseal plate may lead to deformity. | |
| Immediate pain and swelling following traumatic injury and mechanical dysfunction may indicate a musculoskeletal condition. | |
| Gait changes can indicate normal development or undiagnosed hip problems, e.g. DDH, Perthes and slipped upper femoral epiphysis (SUFE). | |
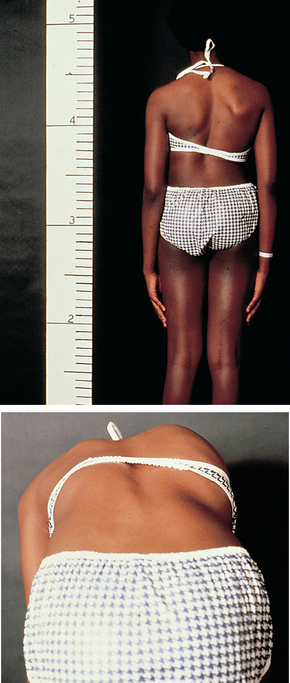
| Spinal problems may present as asymmetrical ribs or waist and head tilting. | |
| Additional history for adolescents | |
| 40% of bone mass accumulates during adolescence. This is achieved through exercise and a healthy diet. | |
| Assess use of safety equipment (e.g. mouth guards, helmets) and safe sporting practices. | |
| Use of safety equipment and presence of adult supervision decreases risk of sports injuries. | |
| Lack of adequate warm-up increases risk of sports injury. | |
| Students may not report injury or pain for fear of limiting participation in sport. | |
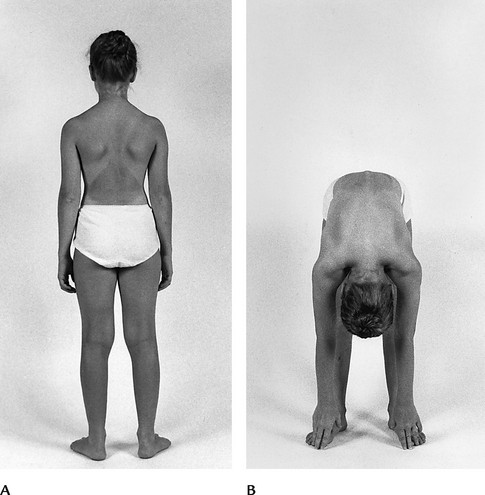
| Adolescents with scoliosis may report unilateral changes in shoulders, rib cage, hip levels and an uneven waist. | |
| Additional history for the adult over 65 years | |
| The questions you should ask the adult should be focused on functional abilities. The aim is to elicit any loss of function, self-care deficit, or safety risk that may occur as a process of ageing or musculoskeletal illness. | |
| Pain/joint dysfunction impacts on activity and increases weakness and lethargy. | |
| It is essential to focus on exploring all falls risks in a positive manner. | |
| All gait aids should be supplied as part of a comprehensive mobility assessment performed by a physiotherapist. |
OBJECTIVE DATA
The purpose of the musculoskeletal examination is to assess patterns of pain, joint abnormalities, and the impact these have on the person’s activities of daily living (ADLs) and psychosocial functioning. Note additional ADL information as the person goes through the motions necessary for an examination: gait, posture, how the person sits in a chair, rises from chair, takes off jacket, manipulates a small object such as a pen and rises from the supine position. It is essential to identify painful joints during the history to ensure these are examined last.
The subjective data will assist in targeting your objective assessment and referral criteria. Musculoskeletal assessment can be challenging for the nurse and the person. It often involves asking intimate questions as well as requiring the person to be partially undressed and therefore vulnerable. You need to ensure the privacy and comfort of the person during musculoskeletal assessment (Ch 6).
All forms of musculoskeletal assessment require a systematic approach:
Expect symmetry of structure and function and normal parameters for that joint.
In addition, a neurovascular assessment of upper and lower limbs is a mandatory component for all musculoskeletal assessments (see Chs 11 and 22 for details of vascular and neurological assessment).
As you approach this examination, focus on the principles of ‘look, feel, then move’.
Look (inspect)—asymmetry of joints, joint swelling, deformity, abnormalities of muscle and soft tissue bulk, erythema, ecchymosis, lesions and rashes, general health of the patient
Feel (palpate)—soft tissue swelling, bony or crystal nodules, tenderness, joint warmth and pain
Move—active movement first followed by passive movement. Perform painful movements last.
| Procedures and normal findings | Abnormal findings and clinical alerts | |
|---|---|---|
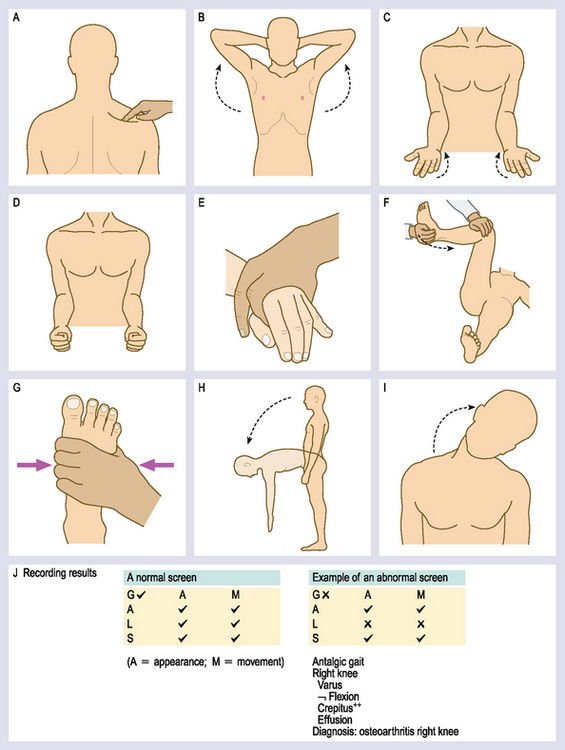
| GALS SCREENING ASSESSMENT | ||
| Arms | ||
Shoulder movements (Figs 15.15, A and B) Ask the patient to place their hands behind their head, with their elbows back. This movement assesses abduction, external rotation of the shoulder and elbow Palpate each shoulder for rotator cuff problems. Ask the patient to extend their arms fully and turn their hands over so palms are down (Fig 15.15, C). Following this ask the patient to turn their hands over. Observe the elbow and hands for any joint/tissue swelling or deformities. Grip strength (Figs 15.15, D and E) Ask the patient to make a fist. Observe the hand and finger movements. Ask the patient to grip your fingers and assess the degree of grip strength. Squeeze across the second to fifth metacarpal. Observe for pain. |
||
| Legs | ||
Patient is lying down with upper torso covered. Hold the knee and hip flexed to 90 degrees. Assess the degree of internal rotation in each hip (Fig 15.15, F). Observe for any reduced muscle bulk especially in quadriceps. Assess: ask patient to flex and extend both knees. Palpate the knee for crepitus and warmth. Inspect the feet for any swelling, deformity or any callosities (Fig 15.15, G). |
||
| Spine | ||
Inspect the spinal column for any abnormalities including kyphosis, scoliosis Observe for symmetry of legs and pelvis. Ask the patient to bring their ear towards their shoulder—assesses lateral cervical flexion (Fig 15.15, I). Hold the patient’s pelvis from behind and ask them to turn from side to side— assesses thoracolumbar rotation. Ask the patient to touch their toes. Palpate for the range of lumbar movement (Fig 15.15, H). Place two fingers over the lumbar vertebrae. Your fingers should move apart as the patient bends forwards—assesses lumbar spine movement. Record results using the framework of Figure 15.15, J. When abnormal results are obtained on the screening GALS assessment proceed to a more detailed physical examination. |
||
| FURTHER OBJECTIVE ASSESSMENT FOR ADVANCED PRACTICE | ||
| The assessments that are described in the following sections require advanced skill and scope of practice. A complete musculoskeletal examination, as described in the following section, is appropriate for persons with a positive musculoskeletal screening assessment. | ||
| Inspection | ||
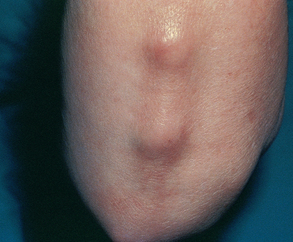
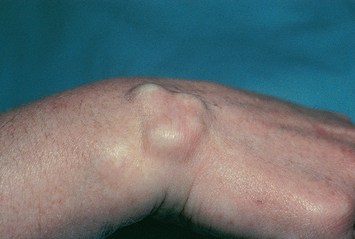
| Note the size and contour of the joint. Inspect the skin and tissues over the joints for colour, swelling and any masses or deformity. Presence of swelling is significant and signals joint irritation. | Swelling may be excess joint fluid (effusion), thickening of the synovial lining, inflammation of surrounding soft tissue (bursae, tendons) or bony enlargement. | |
| Deformities include dislocation (one or more bones in a joint being out of position), subluxation (partial dislocation of a joint), contracture (shortening of a muscle leading to limited ROM of joint) or ankylosis (stiffness or fixation of a joint). | ||
| Palpation | ||
| Palpate each joint, including its skin for temperature, its muscles, bony articulations and area of joint capsule. Notice any heat, tenderness, swelling or masses. Joints are not normally tender to palpation. If any tenderness does occur, try to localise it to specific anatomical structures (e.g. skin, muscles, bursae, ligaments, tendons, fat pads or joint capsule). | ||
| The synovial membrane is not normally palpable. When thickened, it feels ‘doughy’ or ‘boggy’. A small amount of fluid is present in the normal joint, but it is not palpable. | Palpable fluid is abnormal. Because fluid is contained in an enclosed sac, if you push on one side of the sac, the fluid will shift and cause a visible bulging on another side. | |
| Range of motion (ROM) | ||
| Ask for active ROM while stabilising the body area proximal to that being moved. Familiarise yourself with the type of each joint and its normal ROM so that you can recognise limitations. If you see a limitation, gently attempt passive motion. Anchor the joint with one hand while your other hand slowly moves it to its limit. The normal ranges of active and passive motion should be the same. | ||
| If any limitation or any increase in ROM occurs, use a goniometer to measure the angles precisely (Fig 15.16). First extend the joint to neutral or 0 degrees. Center the 0 point of the goniometer on the joint. Keep the fixed arm of the gonio meter on the 0 line and use the movable arm to measure; then flex the joint and measure through the goniometer to determine the angle of greatest flexion. | ||
| Joint motion normally causes no tenderness, pain or crepitation. Do not confuse crepitation with the normal discrete ‘crack’ heard as a tendon or ligament slips over bone during motion, such as when you do a knee bend. | Crepitation is an audible and palpable crunching or grating that accompanies movement. It occurs when the articular surfaces in the joints are roughened, as with rheumatoid arthritis (see Table 15.1). | |
| Muscle testing | ||
| Test the strength of the prime mover muscle groups for each joint. Repeat the motions you elicited for active ROM. Now ask the person to flex and hold as you apply opposing force. Muscle strength should be equal bilaterally and should fully resist your opposing force. (Note: Muscle status and joint status are interdependent and should be interpreted together. Ch 22 discusses the examination of muscles for size and development, tone and presence of tenderness.) | ||
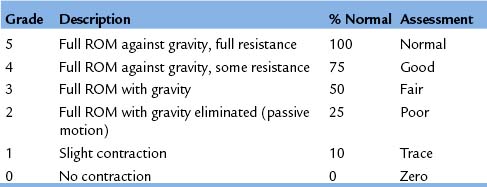
| A wide variability of strength exists among people. You may wish to use a grading system from no voluntary movement to full strength, as shown. | ||
| TEMPOROMANDIBULAR JOINT | ||
| With the person seated, inspect the area just anterior to the ear. Place the tips of your first two fingers in front of each ear and ask the person to open and close the mouth. Drop your fingers into the depressed area over the joint, and note smooth motion of the mandible. An audible and palpable snap or click occurs in many healthy people as the mouth opens (Fig 15.17). Then ask the person to: | ||
| Instructions to person | Motion and expected range | Lateral motion may be lost earlier and more significantly than vertical. |
| Vertical motion. You can measure the space between the upper and lower incisors. Normal is 3 to 6 cm, or three fingers inserted sideways. | ||
| Lateral motion. Normal extent is 1 to 2 cm (Fig 15.18). | ||
| Protrude without deviation. | ||
Palpate the contracted temporalis and masseter muscles as the person clenches the teeth. Compare right and left sides for size,. rmness and strength. Ask the person to move the jaw forwards and laterally against your resistance, and to open mouth against your resistance. This also tests the integrity of cranial nerve V (trigeminal). |
||
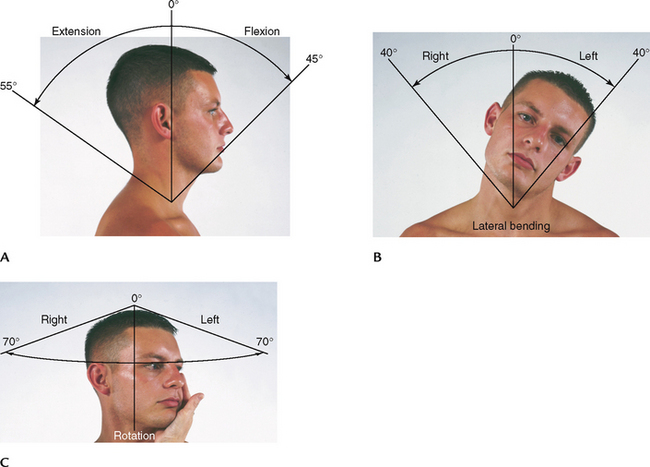
| CERVICAL SPINE | ||
| Inspect the alignment of head and neck. The spine should be straight and the head erect. Palpate the spinous processes and the sternomastoid, trapezius and paravertebral muscles. They should feel. rm, with no muscle spasm or tenderness. | ||
| Ask the person to follow these motions (Fig 15.19): | ||
| Instructions to person | Motion and expected range | Practice alert—do not examine neck movement where there is any suspicion of neck trauma. |
| Flexion of 45 degrees (Fig 15.19, A). | ||
| Hyperextension of 55 degrees. | ||
| Lateral bending of 40 degrees (Fig 15.19, B) | ||
| Rotation of 70 degrees (Fig 15.19, C). | ||
| Repeat the motions while applying opposing force. The person normally can maintain flexion against your full resistance. This also tests integrity of cranial nerve XI (spinal). | The person cannot hold flexion. | |
| UPPER EXTREMITY | ||
| Shoulder | ||
| Inspect and compare both shoulders posteriorly and anteriorly. Check the size and contour of the joint and compare shoulders for equality of bony landmarks. Normally, no redness, muscular atrophy, deformity or swelling is present. Check the anterior aspect of the joint capsule and the subacromial bursa for abnormal swelling. | ||
| Swelling from excess fluid is best seen anteriorly. Considerable fluid must be present to cause a visible distension because the capsule normally is so loose (see Table 15.2). | ||
| If the person reports any shoulder pain, ask that they point to the spot with the hand of the unaffected side. | Swelling of subacromial bursa is localised under deltoid muscle and may be accentuated when the person tries to abduct the arm. | |
| Be aware that shoulder pain may be from local causes or it may be referred pain from a hiatus hernia or a cardiac or pleural condition, which could be potentially serious. Pain from a local cause is reproducible during the examination by palpation or motion. | ||
| While standing in front of the person, palpate both shoulders, noting any muscular spasm or atrophy, swelling, heat or tenderness. Start at the clavicle and methodically explore the acromioclavicular joint, scapula, greater tubercle of the humerus, area of the subacromial bursa, the biceps groove and the anterior aspect of the glenohumeral joint. Palpate the pyramid-shaped axilla; no adenopathy or masses should be present. | ||
| Test ROM by asking the person to perform four motions (Fig 15.20). Cup one hand over the shoulder during ROM to note any crepitation; normally none is present. | ||
| Instructions to person | Motion and expected range | Limited ROM. |
Forward flexion of 180 degrees. Hyperextension up to 50 degrees (Fig 15.20, A). Internal rotation of 90 degrees (Fig 15.20, B). |
||
| Abduction of 180 degrees. Adduction of 50 degrees (Fig 15.20, C). | ||
| External rotation of 90 degrees (Fig 15.20, D). | ||
| Test the strength of the shoulder muscles by asking the person to shrug the shoulders, flex forwards and up and abduct against your resistance. The shoulder shrug also tests the integrity of cranial nerve XI, the spinal accessory. | ||
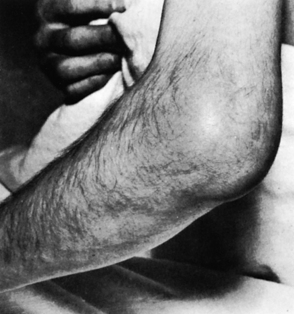
| Elbow | ||
| Inspect the size and contour of the elbow in both flexed and extended positions. Look for any deformity, redness or swelling. Check the olecranon bursa and the normally present hollows on either side of the olecranon process for abnormal swelling. | ||
| Effusion or synovial thickening shows first as a bulge or fullness in groove on either side of the olecranon process, and it occurs with gouty arthritis. | ||
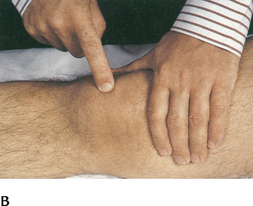
| Palpate with the elbow flexed about 70 degrees and as relaxed as possible (Fig 15.21). Use your left hand to support the person’s left forearm and palpate the extensor surface of the elbow–the olecranon process and the medial and lateral epicondyles of humerus–with your right thumb and fingers. | ||
| With your thumb in the lateral groove and your index and middle fingers in the medial groove, palpate either side of the olecranon process using varying pressure. Normally, present tissues and fat pads feel fairly solid. Check for any synovial thickening, swelling, nodules or tenderness. | ||
| Palpate the area of the olecranon bursa for heat, swelling, tenderness, consistency or nodules. | Subcutaneous nodules are raised, firm and nontender and overlying skin moves freely. Common sites are in the olecranon bursa and along extensor surface of the ulna. These nodules occur with RA (see Table 15.3). | |
| Test ROM by asking the person to: | ||
| Instructions to person | Motion and expected range | |
| While testing muscle strength, stabilise the person’s arm with one hand (Fig 15.24). Have the person flex the elbow against your resistance applied just proximal to the wrist. Then ask the person to extend the elbow against your resistance. | ||
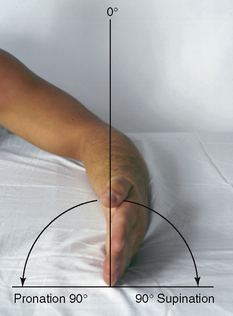
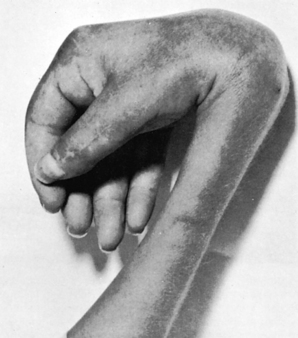
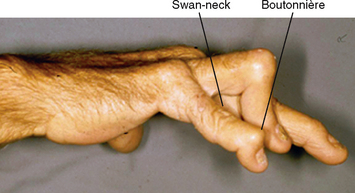
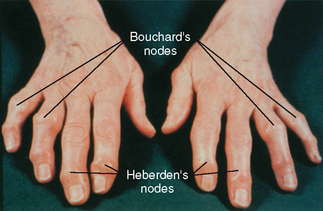
| Wrist and hand | ||
| Inspect the hands and wrists on the dorsal and palmar sides, noting position, contour and shape. The normal functional position of the hand shows the wrist in slight extension. This way the fingers can flex efficiently, and the thumb can oppose them for grip and manipulation. The fingers lie straight in the same axis as the forearm. Normally, no swelling or redness, deformity or nodules are present. | ||
| The skin looks smooth with knuckle wrinkles present and no swelling or lesions. Muscles are full, with the palm showing a rounded mound proximal to the thumb (the thenar eminence) and a smaller rounded mound proximal to the little finger. | Swan-neck or boutonnière deformity in fingers. Atrophy of the thenar eminence (see Table 15.4). |
|
| Palpate each joint in the wrist and hands. Facing the person, support the hand with your fingers under it and palpate the wrist firmly with both your thumbs on its dorsum (Fig 15.25). Make sure the person’s wrist is relaxed and in straight alignment. Move your palpating thumbs side to side to identify the normal depressed areas that overlie the joint space. Use gentle but firm pressure. Normally the joint surfaces feel smooth, with no swelling, bogginess, nodules or tenderness. | Ganglion in wrist. Synovial swelling on dorsum. Generalised swelling. Tenderness. | |
| Palpate the metacarpophalangeal joints with your thumbs, just distal to and on either side of the knuckle (Fig 15.26). | ||
| Use your thumb and index. nger in a pinching motion to palpate the sides of the interphalangeal joints (Fig 15.27). Normally, no synovial thickening, tenderness, warmth or nodules are present. | Heberden’s and Bouchard’s nodules are hard and nontender and occur with osteoarthritis (see Table 15.4). | |
| Test ROM (Fig 15.28) by asking the person to: | Loss of ROM here is the most common and most significant functional loss of the wrist. | |
| Instructions to person | Motion and expected range | |
Hyperextension of 70 degrees (Fig 15.28, A). Palmar flexion of 90 degrees. Flexion of 90 degrees. Hyperextension of 30 degrees (Fig 15.28, B). Ulnar deviation of 50–60 degrees and radial deviation of 20 degrees (Fig 15.28, C). Abduction of 20 degrees; fist tight. The responses should be equal bilaterally (Fig 15.28, D, E). The person is able to perform, and the responses are equal bilaterally (Fig 15.28, F). |
||
| For muscle testing, position the person’s forearm supinated (palm up) and resting on a table (Fig 15.29). Stabilise by holding your hand at the person’s midforearm. Ask the person to flex the wrist against your resistance at the palm. | ||
| Phalen’s test. Ask the person to hold both hands back to back while flexing the wrists 90 degrees. Acute flexion of the wrist for 60 seconds produces no symptoms in the normal hand (Fig 15.30). | Phalen’s test reproduces numbness and burning in a person with carpal tunnel syndrome (see Table 15.4). | |
| Tinel’s sign. Direct percussion of the produces no symptoms in the normal location of the median nerve at the wrist hand (Fig 15.31). | In carpal tunnel syndrome, percussion of the median nerve produces burning and tingling along its distribution, which is a positive Tinel’s sign. | |
| LOWER EXTREMITY | ||
| Hip | ||
| Wait to inspect the hip joint together with the spine a bit later in the examination as the person stands. At that time, note symmetrical levels of iliac crests, gluteal folds and equally sized buttocks. A smooth, even gait reflects equal leg lengths and functional hip motion. | ||
| Help the person into a supine position and palpate the hip joints. The joints should feel stable and symmetrical, with no tenderness or crepitance. | Pain with palpation. Crepitation. | |
| Assess ROM (Fig 15.32) by asking the person to: | ||
| Instructions to person | Hip flexion of 90 degrees (Fig 15.32, A). Hip flexion of 120 degrees. The opposite thigh should remain on the table (Fig 15.32, B). |
|
| Internal rotation of 40 degrees. External rotation of 45 degrees (Fig 15.32, C). | Limited internal rotation of hip is an early and reliable sign of hip disease. | |
| Abduction of 40 to 45 degrees. Adduction of 20 to 30 degrees (Fig 15.32, D). | Limitation of abduction of the hip while supine is the most common motion dysfunction found in hip disease. | |
| Hyperextension of 15 degrees when stabilised. | ||
Shiny and atrophic skin. Swelling or inflammation (see Table 15.5). |
||
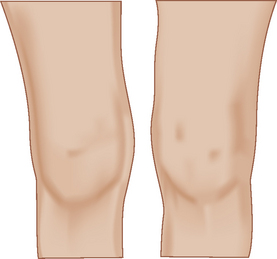
| Inspect lower leg alignment. The lower leg should extend in the same axis as the thigh. | Angulation deformity: | |
| Inspect the knee’s shape and contour. Normally, distinct concavities, or hollows, are present on either side of the patella. Check them for any sign of fullness or swelling. Note other locations, such as the prepatellar bursa and the suprapatellar pouch, for any abnormal swelling. | Hollows disappear; then they may bulge with synovial thickening or effusion. | |
| Check the quadriceps muscle in the anterior thigh for any atrophy. Because it is the prime mover of knee extension, this muscle is important for joint stability during weight bearing. | Atrophy occurs with disuse or chronic disorders. First, it appears in the medial part of the muscle, although it is difficult to note because the vastus medialis is relatively small. | |
| Enhance palpation with the knee in the supine position with complete relaxation of the quadriceps muscle. Start high on the anterior thigh, about 10 cm above the patella. Palpate with your left thumb and fingers in a grasping fashion (Fig 15.33). Proceed down towards the knee, exploring the region of the suprapatellar pouch. Note the consistency of the tissues. The muscles and soft tissues should feel solid, and the joint should feel smooth, with no warmth, tenderness, thickening or nodularity. | Feels fluctuant or boggy with synovitis of suprapatellar pouch. | |
| When swelling occurs, you need to distinguish whether it is due to soft tissue swelling or increased fluid in the joint. The tests for the bulge sign and ballottement of the patella aid this assessment. | ||
| Bulge sign. For swelling in the suprapatellar pouch, the bulge sign confirms the presence of small amounts of fluid as you try to move the fluid from one side of the joint to the other. Firmly stroke up on the medial aspect of the knee two or three times to displace any fluid (Fig 15.34, A). Tap the lateral aspect (Fig 15.34, B). Watch the medial side in the hollow for a distinct bulge from a fluid wave. Normally, none is present. | The bulge sign occurs with very small amounts of effusion, 4 to 8 mL, from fluid flowing across the joint (Fig 15.34, C). | |
| Ballottement of the patella. This test is reliable when larger amounts of fluid are present. Use your left hand to compress the suprapatellar pouch to move any fluid into the knee joint. With your right hand, push the patella sharply against the femur. If no fluid is present, the patella is already snug against the femur (Fig 15.35, A). | If fluid has collected, your tap on the patella moves it through the fluid, and you will hear a tap as the patella bumps up on the femoral condyles (Fig 15.35, B). | |
| A | ||
| Continue palpation and explore the tibiofemoral joint (Fig 15.36). Note smooth joint margins and absence of pain. Palpate the infrapatellar fat pad and the patella. Check for crepitus by holding your hand on the patella as the knee is flexed and extended. Some crepitus in an otherwise asymptomatic knee is not uncommon. | ||
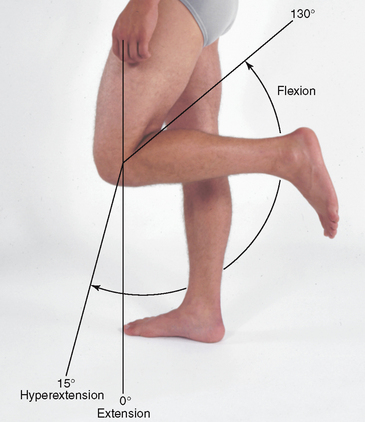
| Check ROM (Fig 15.37) by asking the person to: | Limited ROM. | |
| Instructions to person | Motion and expected range | |
| Check muscle strength by asking the person to maintain knee flexion while you oppose by trying to pull the leg forwards. Muscle extension is demonstrated by the person’s success in rising from a seated position in a low chair or by rising from a squat without using the hands for support. | ||
Special test for meniscal tears McMurray’s test. Perform this test when the person has reported a history of trauma followed by locking, giving way or local pain in the knee. Position the person supine as you stand on the affected side. Hold the heel and flex the knee and hip. Place your other hand on the knee with fingers on the medial side. Rotate the leg in and out to loosen the joint. Externally rotate the leg and push a valgus (inwards) stress on the knee. Then slowly extend the knee. Normally the leg extends smoothly with no pain. |
If you hear or feel a ‘click’, McMurray’s test is positive for a torn meniscus. | |
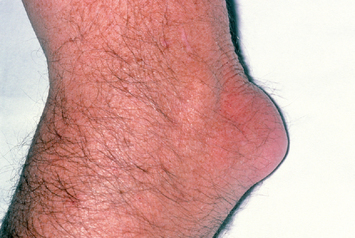
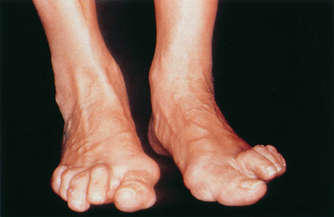
| Ankle and foot | ||
| Inspect while the person is in a sitting, non–weight-bearing position, as well as when standing and walking. Compare both feet, noting position of feet and toes, contour of joints and skin characteristics. The foot should align with the long axis of the lower leg; an imaginary line would fall from midpatella to between the. rst and second toes. | ||
Weight-bearing should fall on the middle of the foot, from the heel, along the midfoot, to between the second and third toes. Most feet have a longitudinal arch, although that can vary normally from ‘flat feet’ to a high instep. The toes point straight forwards and lie flat. The ankles (malleoli) are smooth bony prominences. Normally the skin is smooth, with even colouring and no lesions. Note the locations of any calluses or bursal reactions because they reveal areas of abnormal friction. Examining well-worn shoes helps assess areas of wear and accommodation. |
Hallux valgus (see Table 15.6). Hammertoes. Claw toes. Swelling or inflammation. Calluses. Ulcers. | |
| Support the ankle by grasping the heel with your fingers while palpating with your thumbs (Fig 15.38). Explore the joint spaces. They should feel smooth and depressed, with no fullness, swelling or tenderness. | Swelling or inflammation. Tenderness. | |
| Palpate the metatarsophalangeal joints between your thumb on the dorsum and your fingers on the plantar surface (Fig 15.39). | Swelling or inflammation; tenderness. | |
| Using a pinching motion of your thumb and forefinger, palpate the interphalangeal joints on the medial and lateral sides of the toes. | ||
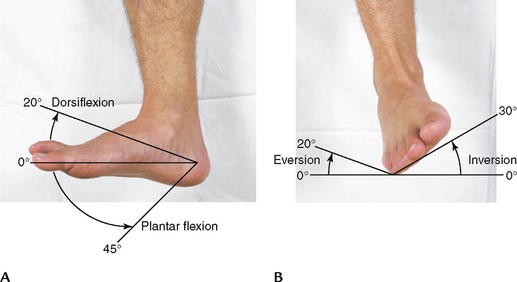
| Test ROM (Fig 15.40) by asking the person to: | Limited ROM. | |
| Instructions to person | Motion and expected range | Pain with motion. |
| Plantar flexion of 45 degrees. Dorsiflexion of 20 degrees (Fig 15.40, A). Eversion of 20 degrees. (Stabilise the ankle with one hand, hold heel with the other to test the subtalar joint.) Inversion of 30 degrees (Fig 15.40, B). | ||
| Assess muscle strength by asking the person to maintain dorsiflexion and plantar flexion against your resistance. | Unable to hold flexion. | |
| SPINE | ||
| The person should be standing, draped in a gown open at the back. Place yourself far enough back so that you can see the entire back. Inspect and note whether the spine is straight by following an imaginary vertical line from the head through the spinous processes and down through the gluteal cleft, and by noting equal horizontal positions for the shoulders, scapulae, iliac crests and gluteal folds, and equal spaces between arm and lateral thorax on the two sides (Fig 15.41, A). The person’s knees and feet should be aligned with the trunk and should be pointing forwards. | A difference in shoulder elevation and in level of scapulae and iliac crests occur with scoliosis (see Table 15.7). | |
| From the side, note the normal convex thoracic curve and concave lumbar curve (Fig 15.41, B). An enhanced thoracic curve, or kyphosis, is common in people over 65 years. A pronounced lumbar curve, or lordosis, is common in obese people. | Lateral tilting and forward bending occur with a herniated nucleus pulposus (see Table 15.8). | |
| Palpate the spinous processes. Normally they are straight and not tender. Palpate the paravertebral muscles; they should feel firm with no tenderness or spasm. | ||
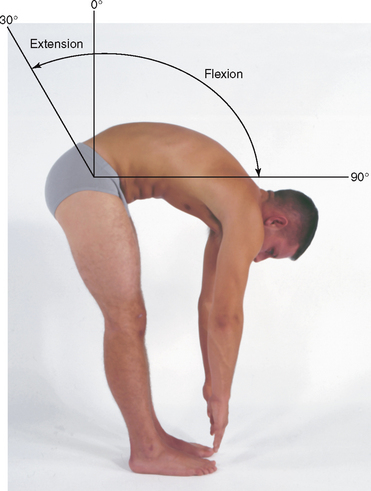
| Check ROM of the spine by asking the person to bend forwards and touch the toes (Fig 15.42). Look for flexion of 75 to 90 degrees and smoothness and symmetry of movement. Note that the concave lumbar curve should disappear with this motion, and the back should have a single convex C-shaped curve. | ||
| If you suspect a spinal curvature during inspection, this may be more clearly seen when the person touches the toes. While the person is bending over, mark a dot on each spinous process. When the person resumes standing, the dots should form a straight vertical line. | If the dots form a slight S-shape when the person stands, a spinal curve is present. | |
| Stabilise the pelvis with your hands. Check ROM (Fig 15.43) by asking the person to: | ||
| Instructions to person motion and expected range | ||
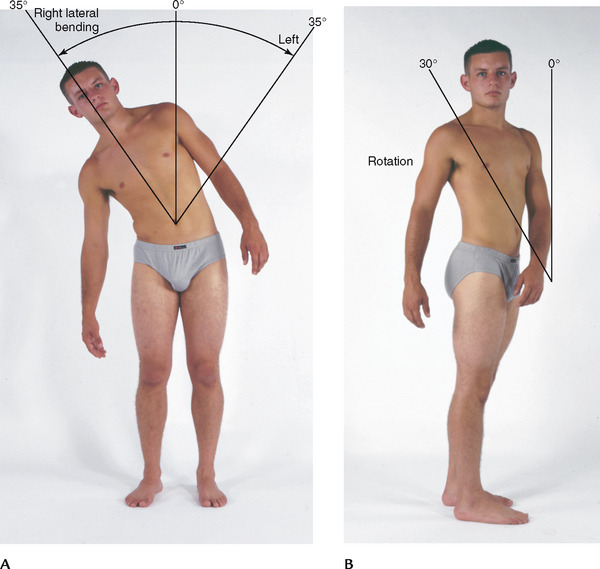
| Lateral bending of 35 degrees (Fig 15.43, A). | ||
| Hyperextension of 30 degrees. | ||
| Rotation of 30 degrees, bilaterally (Fig 15.43, B). | ||
| These manoeuvres reveal only gross restriction. Movement is still possible even if some spinal fusion has occurred. | ||
| Finally, ask the person to walk on their toes for a few steps; then return walking on the heels. | ||
Straight leg raising or LaSegue’s test. These manoeuvres reproduce back and leg pain and help confirm the presence of a herniated nucleus pulposus. Straight leg raising while keeping the knee extended normally produces no pain. Raise the affected leg just short of the point where it produces pain. Then dorsiflex the foot (Fig 15.44). Raise the unaffected leg while leaving the other leg flat. Inquire about the involved side. |
||
| Measure leg length discrepancy. Perform this measurement if you need to determine whether one leg is shorter than the other. For true leg length, measure between fixed points, from the anterior iliac spine to the medial malleolus, crossing the medial side of the knee (Fig 15.45). Normally these measurements are equal or within 1 cm, indicating no true bone discrepancy. | Unequal leg lengths. | |
| Sometimes the true leg length is equal, but the legs still look unequal. For apparent leg length, measure from a nonfixed point (the umbilicus) to a fixed point (medial malleolus) on each leg. | True leg lengths are equal, but apparent leg lengths unequal–this condition occurs with pelvic obliquity or adduction or flexion deformity in the hip. | |
| DEVELOPMENTAL CONSIDERATIONS | ||
Review the developmental milestones discussed in Chapter 3. Keep handy a concise chart of the usual sequence of motor development so that you can refer to expected findings for the age of each child you are examining. Use the Denver II test to screen the fine and gross motor skills for the child’s age. Because some overlap exists between the musculoskeletal and neurological examinations, assessment of muscle tone, resting posture and motor activity are discussed in Chapter 22. |
||
| Infants | ||
| Examine the infant fully undressed and lying on the back. Take care to place the newborn on a warming table to maintain body temperature. | ||
| Feet and legs. Start with the feet and work your way up the extremities. Note any positional deformities, a residual of fetal positioning. Often the newborn’s feet are not held straight but in a varus (apart) or valgus (together) position. It is important to distinguish whether this position is flexible (and thus usually self-correctable) or fixed. Scratch the outside of the bottom of the foot. If the deformity is self-correctable, the foot assumes a normal right angle to the lower leg. Or immobilise the heel with one hand and gently push the forefoot to the neutral position with the other hand. If you can move it to neutral position, it is flexible. | A true deformity is fixed and assumes a right angle only with forced manipulation or not at all. | |
| Note the relationship of the forefoot to the hindfoot. Commonly, the hindfoot is in alignment with the lower leg and just the forefoot angles inwards. This forefoot adduction is metatarsus adductus. It is usually present at birth and usually resolves spontaneously by age 3 years. | Metatarsus varus–adduction and inversion of forefoot. Talipes equinovarus (see Table 15.8). |
|
| Check for tibial torsion, a twisting of the tibia. Place both feet flat on the table, and push to flex up the knees. With the patella and the tibial tubercle in a straight line, place your fingers on the malleoli. In an infant, note that a line connecting the four malleoli is parallel to the table. | More than 20 degrees of deviation; or if lateral malleolus is anterior to medial malleolus indicates tibial torsion. | |
| Tibial torsion may originate from intrauterine positioning and then may be exacerbated at a later age by continuous sitting in a reverse tailor position, the ‘TV squat’. This is sitting with the buttocks on the floor and the lower legs splayed back and out on either side. | ||
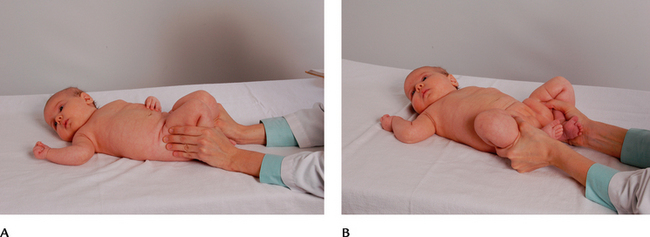
| Hips. Check the hips for developmental hip dysplasia (DDH). The most reliable method is Ortolani’s manoeuvre, which should be done at every professional visit until the infant is 1 year old. With the infant supine, flex the knees holding your thumbs on the inner mid-thighs, and your fingers outside on the hips touching the greater trochanters. Adduct the legs until your thumbs touch (Fig 15.46, A). Then gently lift and abduct, moving the knees apart and down so their lateral aspects touch the table (Fig 15.46, B). This normally feels smooth and has no sound. | ||
| The Allis test is also used to check for hip dislocation by comparing leg lengths (Fig 15.47). Place the baby’s feet flat on the table and flex the knees up. Scan the tops of the knees; normally they are at the same elevation. | This test is usually performed by experienced midwives and maternal and child health nurses–not generalist nurses. | |
| Finding one knee significantly lower than the other is a positive indication of Allis’ sign and suggests hip dislocation. | ||
| Note the gluteal folds. Normally they are equal on both sides. However, some asymmetry may occur in healthy children. | Unequal gluteal folds may accompany hip dislocation after 2 to 3 months of age. | |
| Hands and arms. Inspect the hands, noting shape, number and position of fingers and palmar creases. | Polydactyly is the presence of extra fingers or toes. Syndactyly is webbing between adjacent fingers or toes (see Table 15.4). | |
| A simian crease is a single palmar crease that occurs with Down syndrome, accompanied by short broad fingers, incurving of little fingers and low-set thumbs. | ||
| Palpate the length of the clavicles because the clavicle is the bone most frequently fractured during birth. The clavicles should feel smooth, regular and without crepitus. Also note equal ROM of arms during Moro’s reflex. | Fractured clavicle: Note irregularity at the fracture site, crepitus and angulation. The site has rapid callus formation with a palpable lump within a few weeks. Observe limited arm ROM and unilateral response to Moro’s reflex. | |
| Back. Lift up the infant and examine the back. Note the normal single C curve of the newborn’s spine (Fig 15.48). By 2 months of age, the infant can lift the head while prone. This builds the concave cervical spinal curve and indicates normal forearm strength. Inspect the length of the spine for any tuft of hair, dimple in midline, cyst or mass. Normally, none are present. | A tuft of hair over a dimple in the midline may indicate spina bifida. | |
| A small dimple in the midline–anywhere from the head to the coccyx–suggests dermoid sinus. | ||
| Mass, such as meningocele. | ||
| Observe ROM through spontaneous movement of extremities. | ||
| Test muscle strength by lifting up the infant with your hands under the axillae (Fig 15.49). A baby with normal muscle strength wedges securely between your hands. | A baby who starts to ‘slip’ between your hands shows weakness of the shoulder muscles. | |
| Preschool- and school-age children | ||
| Once the infant learns to crawl and then to walk, the waking hours show perpetual motion. This is convenient for your musculoskeletal assessment; you can observe the muscles and joints during spontaneous play before a table-top examination. Most young children enjoy showing off their physical accomplishments. For specific motions, coax the toddler: ‘Show me how you can walk to Mummy’ or ‘Climb these steps’. Ask the preschooler to hop on one foot or to jump. | ||
| Back. While the child is standing, note the posture. From behind, you should note a ‘plumb line’ from the back of the head, along the spine, to the middle of the sacrum. Shoulders are level within 1 cm, and scapulae are symmetric. From the side, lordosis is common throughout childhood, appearing more pronounced in children with a protuberant abdomen. | Lordosis is marked with muscular dystrophy and rickets. | |
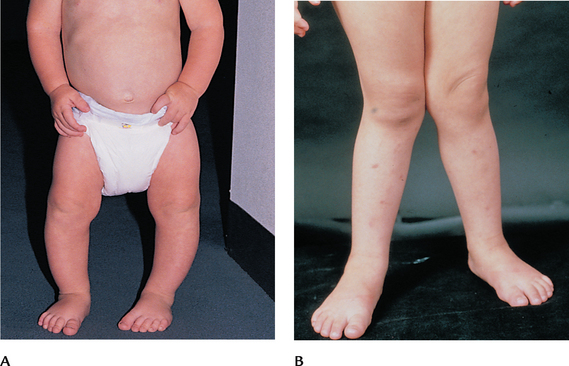
| Legs and feet. Anteriorly, note the leg position. A ‘bowlegged’ stance (genu varum) is a lateral bowing of the legs (Fig 15.50, A). It is present when you measure a persistent space of more than 2.5 cm between the knees when the medial malleoli are together. Genu varum is normal for 1 year after the child begins walking. The child may walk with a waddling gait. This resolves with growth; no treatment is indicated. | Genu varum also occurs with rickets. | |
| ‘Knock knees’ (genu valgum) are present when there is more than 2.5 cm between the medial malleoli when the knees are together (Fig 15.50, B). It occurs normally between 2 and 3½ years of age. Also, treatment is not indicated. (Note: To remember the two conditions, remember to link the r’s and g’s: genu varum–knees apart; genu valgum–knees together.) | Genu valgum also occurs with rickets, poliomyelitis and syphilis. | |
Often, parents tell you they are concerned about the child’s foot development. The most common questions are about ‘flatfeet’ and ‘pigeon toes’. Flatfoot (pes planus) is pronation, or turning in, of the medial side of the foot. The young child may look flatfooted because the normal longitudinal arch is concealed by a fat pad until age 3 years. When standing begins, the child takes a broad-based stance, which causes pronation. Thus pronation is common between 12 and 30 months. You can see it best from behind the child, where the medial side of the foot drops down and in. |
Pronation beyond 30 months. | |
| Pigeon toes, or toeing in, are demonstrated when the child tends to walk on the lateral side of the foot, and the longitudinal arch looks higher than normal. It often starts as a forefoot adduction, which usually corrects spontaneously by age 3 years, as long as the foot is flexible. | Toeing in from forefoot adduction that is fixed, or lasts beyond age 3 years. Toeing in from tibial torsion. | |
| Check the child’s gait while walking away from and returning to you. Let the child wear socks, because a cold tile floor will distort the usual gait. From 1 to 2 years of age, expect a broad-based gait, with arms out for balance. Weight-bearing falls on the inside of the foot. From 3 years of age, the base narrows and the arms are closer to the sides. Inspect the shoes for spots of greatest wear to aid your judgment of the gait. Normally the shoes wear more on the outside of the heel and the inside of the toe. | ||
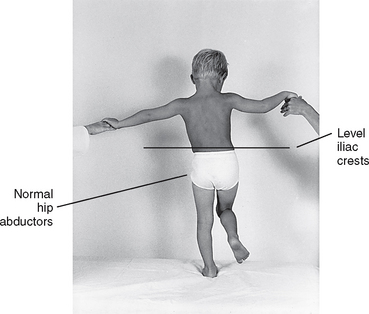
| Check the Trendelenburg’s sign to screen progressive subluxation of the hip (Fig 15.51). Watching from behind, ask the child to stand on one leg, then the other. Watch the iliac crests; they should stay level when weight is shifted. | The sign occurs with severe subluxation of one hip. When the child stands on the good leg, the pelvis looks level. When the child stands on the affected leg, the pelvis drops towards the ‘good’ side. | |
| The child may sit for the remainder of the examination. Start with the feet and hands of the child from 2 to 6 years of age because the child is happy to show these off, and proceed through the examination described earlier. | ||
| Particularly, check the arm for full ROM and presence of pain. Look for subluxation of the elbow (head of the radius). This occurs most often between 2 and 4 years of age as a result of forceful removal of clothing or dangling while adults suspend the child by the hands. | Inability to supinate the hand while the arm is flexed, together with pain in elbow, indicates subluxation of the head of the radius. | |
| Palpate the bones, joints and muscles of the extremities as described in the adult examination. | Pain or tenderness in extremities is usually caused by trauma or infection. | |
| Fractures are usually due to trauma and are exhibited as an inability to use the area, a deformity or an excess of motion in the involved bone with pain and crepitation. | ||
| Enlargement of the tibial tubercles with tenderness suggests Osgood-Schlatter disease (see Table 15.5). | ||
| Adolescents | ||
Proceed with the musculoskeletal examination you provide for the adult, except pay special note to spinal posture. Kyphosis is common during adolescence because of chronic poor posture. Be aware of the risk of sports-related injuries with the adolescent, because sports participation and competition often peak with this age-group. In late 1990s the Spine Society of Australia, with the support of the Royal Australian College of General Practitioners, introduced the National Self-Detection Program for Scoliosis. This program entails the distribution of a brochure for the target age group (Girls 11–13 years of age) in which the physical signs of scoliosis are described. Patients are advised to consult with their family doctor if they have any concerns. The program is endorsed by the Paediatrics and Child Health Division of the Royal Australasian College of Physicians (Scoliosis Australia, nd). |
Scoliosis is most apparent during the preadolescent growth spurt. Asymmetry suggests scoliosis–ribs hump up on one side as child bends forwards, and with unequal landmark elevation (see Table 15.7). | |
| Screen for scoliosis with the forward bend test (Fig 15.52). Seat yourself behind the standing child, and ask the child to stand with the feet shoulder width apart and bend forwards slowly to touch the toes. Expect a straight vertical spine while standing and also while bending forwards. Posterior ribs should be symmetrical, with equal elevation of shoulders, scapulae and iliac crests. You may wish to mark each spinous process with a felt marker. The lineup of ink dots highlights even a subtle curve. | ||
Proceed through the examination described in the adult section. Expected postural changes in pregnancy include progressive lordosis and, towards the third trimester, anterior cervical flexion, kyphosis and slumped shoulders (Fig 15.53, A). When the pregnancy is at term, the protuberant abdomen and the relaxed mobility in the joints create the characteristic ‘waddling’ gait (Fig 15.53, B). |
||
| The adult over 65 years | ||
| Postural changes include a decrease in height, more apparent in the eighth and ninth decades. ‘Lengthening of the arm-trunk axis’ describes this shortening of the trunk with comparatively long extremities. Kyphosis is common, with a backwards head tilt to compensate. This creates the outline of a figure 3 when you view this older adult from the left side. Slight flexion of hips and knees is also common. | ||
| Contour changes include a decrease of fat in the body periphery and fat deposition over the abdomen and hips. The bony prominences become more marked. | ||
| For most adults over 65, ROM testing proceeds as described earlier. ROM and muscle strength are much the same as with the younger adult, provided no musculoskeletal illnesses or arthritic changes are present. | ||
| Functional assessment. For those with advanced ageing changes, arthritic changes or musculoskeletal disability, perform a functional assessment for ADLs. This applies the ROM and muscle strength assessments to the accomplishment of specific activities. You need to determine adequate and safe per form ance of functions essential for independent home life. | ||
| Instructions to person | Common adaptation for ageing changes | |
| Shuffling pattern; swaying; arms out to help balance; broader base of support; person may watch feet. | ||
| Person holds hand rail; may haul body up with it; may lead with favoured (stronger) leg. | ||
| Holds hand rail, sometimes with both hands. | ||
| If the person is weak, they may descend sideways, lowering the weaker leg first. If the person is unsteady, they may watch feet. | ||
| Person often bends at waist instead of bending knees; holds furniture to support while bending and straightening. | ||
| Person uses arms to push off chair arms, upper trunk leans forwards before body straightens, feet planted wide in broad base of support. | ||
| May roll to one side, push with arms to lift up torso, grab bedside table to increase leverage. | ||

Figure 15.21 Epicondyles, head of radius and tendons are common sites of inflammation and local tenderness, or ‘tennis elbow’.
TABLE 15.1 Abnormalities affecting multiple joints
| INFLAMMATORY CONDITIONS |
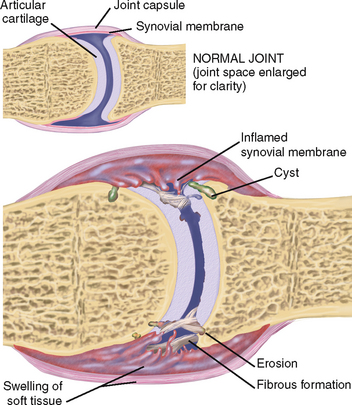 |
| Rheumatoid arthritis (RA) |
| This is a chronic, systemic inflammatory disease of joints and surrounding connective tissue. Inflammation of synovial membrane leads to thickening; then to fibrosis, which limits motion, and finally to bony ankylosis. The disorder is symmetrical and bilateral and is characterised by heat, redness, swelling and painful motion of the affected joints. RA is associated with fatigue, weakness, anorexia, weight loss, low-grade fever and lymphadenopathy. Associated signs are described in the following tables, especially Table 15.4. |
| Ankylosing spondylitis (not illustrated) |
| Chronic progressive inflammation of spine, sacroiliac and larger joints of the extremities, leading to bony ankylosis and deformity. A form of RA, this affects primarily men by a 10:1 ratio, in late adolescence or early adulthood. Spasm of paraspinal muscles pulls spine into forward flexion, obliterating cervical and lumbar curves. Thoracic curve exaggerated into single kyphotic rounding. Also includes flexion deformities of hips and knees. |
| DEGENERATIVE CONDITIONS |
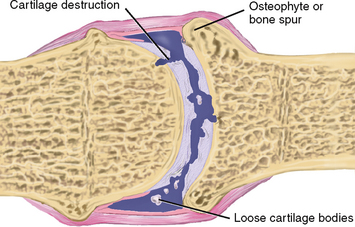 |
| Osteoarthritis (degenerative joint disease) |
| Noninflammatory, localised, progressive disorder involving deterioration of articular cartilages and subchondral bone and formation of new bone (osteophytes) at joint surfaces. Ageing increases incidence; nearly all adults over 60 years old have some radiographic signs of osteoarthritis. Asymmetrical joint involvement commonly affects hands, knees, hips and lumbar and cervical segments of the spine. Affected joints have stiffness, swelling with hard, bony protuberances, pain with motion and limitation of motion (see Table 15.4). |
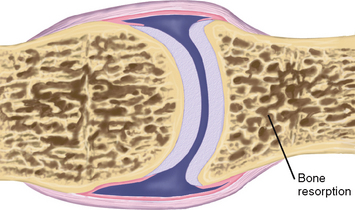 |
| Osteoporosis |
| Decrease in skeletal bone mass occurring when rate of bone resorption is greater than that of bone formation. The weakened bone state increases risk for stress fractures, especially at wrist, hip and vertebrae. Occurs primarily in postmenopausal women. Osteoporosis risk also is associated with smaller height and weight, younger age at menopause, lack of physical activity and lack of oestrogen replacement therapy. |
TABLE 15.2 Abnormalities of the shoulder
 |
| Atrophy |
 |
| Dislocated shoulder |
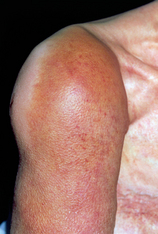 |
| Joint effusion |
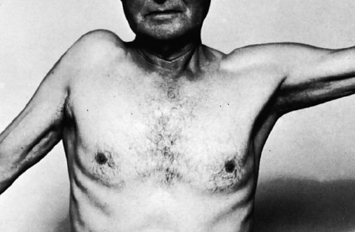 |
| Tear of rotator cuff |
| Characteristic ‘hunched’ position and limited abduction of arm. Occurs from traumatic adduction while arm is held in abduction, or from fall on shoulder, throwing or heavy lifting. Positive drop arm test: If the arm is passively abducted at the shoulder, the person is unable to sustain the position and the arm falls to the side. |
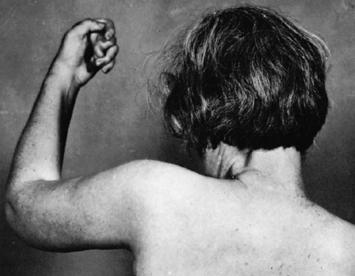 |
| Frozen shoulder–adhesive capsulitis |
| Fibrous tissues form in the joint capsule, causing stiffness, progressive limitation of motion and pain. Motion limited in abduction and external rotation; unable to reach overhead. It may lead to atrophy of shoulder girdle muscles. Gradual onset; unknown cause. It is associated with prolonged bed rest or shoulder immobility. May resolve spontaneously. |
| Subacromial bursitis (not illustrated) |
| Inflammation and swelling of subacromial bursa over the shoulder cause limited ROM and pain with motion. Localised swelling under deltoid muscle may increase by partial passive abduction of the arm. Caused by direct trauma, strain during sports, local or systemic inflammatory process or repetitive motion with injury. |
TABLE 15.3 Abnormalities of the elbow
TABLE 15.4 Abnormalities of the wrist and hand
TABLE 15.5 Abnormalities of the knee
TABLE 15.6 Abnormalities of the ankle and foot
TABLE 15.7 Abnormalities of the spine
TABLE 15.8 Common congenital or paediatric abnormalities
Promoting a healthy lifestyle Osteoporosis–‘the silent disease’
Bone is a dynamic tissue which responds to mechanical stresses through a complex process of remodelling. The remodelling process involves the resorption of micro damaged bone by osteoclast cells followed by a phase of bone formation by osteoblast cells. In healthy adults this process is coupled to ensure bone density remains stable. This process commences in childhood with peak bone mass reached by the end of the second decade of life. Studies suggest that more than 95% of the adult skeleton is formed by the end of adolescence (Rizzoli et al, 2010). There is also a direct link between total body fat in children and reduced bone health, emphasising the value of a healthy lifestyle from childhood through to adulthood (Hrafnkelsson, 2010).
When this bone remodelling process becomes uncoupled, normal bone density is altered leading to a change in the normal architecture of bone seen in diseases such as osteoporosis (Seeman et al, 2006). Osteoporosis is defined as a disease characterised by low bone mass and micro-architectural deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk (WHO, 1994). The loss of bone occurs ‘silently’ and progressively. Often there are no symptoms until the first fracture occurs. Fractures associated with osteoporosis are termed low trauma or fragility fractures and occur most frequently in the neck of femur, vertebrae and distal radius.
The impact of osteoporosis and the resultant low trauma fractures are devastating: 1 in 2 women and 1 in 3 men over 60 years in Australia will suffer an osteoporotic fracture (Osteoporosis Australia, 2010b).
In Australia every day, more than 40 Australians break their hip. Most are aged 65 years or over, and more than half are aged 85 or over. Virtually all of these people will be admitted to hospital, and most will have some kind of surgery. Two people will die in the hospital, and at least four will need to go into a residential aged care facility, either while they recover or permanently. A year later, less than half of those original 40 people will be able to walk as well as they did before the fracture, and another six or seven will have died (AIHW, 2010b: 2).
Risk factors for osteoporosis and fractures include both intrinsic and lifestyle factors.
• Maternal family history of osteoporotic fracture
• Previous low trauma fracture particularly of the hip, spine or wrist
• Early menopause, late menarche (women)
• Absence or suppression of menstrual periods (amenorrhoea) >1 year
• Comorbidity and medical treatments
• Malabsorption syndromes, including coeliac disease and inflammatory bowel disease
• Chronic renal and liver diseases
• Inadequate dietary calcium intake
• Vitamin D deficiency and/or lack of sunlight
• Physical inactivity/sedentary lifestyle over many years
• Regular, excessive alcohol use
• Poor muscle strength and balance
(Osteoporosis Australia, 2006)
In men the most identifiable risk factors also include hypogonadism, excess alcohol, hyperthyroidism and primary hyperparathyroidism (Osteoporosis Australia, 2010a; Thomas-John et al, 2009).
Within Australia it is estimated that more than half of all vertebral fractures do not receive any interventions, although nearly all are associated with disability and pain. It is also estimated that up to 80% of people with osteoporotic fractures remain undiagnosed and untreated. In addition, those people who sustain a low trauma fracture are at substantially greater (2–4-fold) risk of sustaining another fracture of a different type. This is called ‘the cascade effect’, as the risk of additional fractures increases exponentially with each new fracture (Langsetmo et al, 2009).
Nurses have therefore a pivotal role providing advice on osteoporosis risk modification following completion of an osteoporosis risk assessment. The focus of this advice relates to the positive benefits of a diet high in calcium (1000–1500 mg/day) and vitamin D, adequate levels of physical activity and sunlight exposure, smoking cessation and limited alcohol.
Within their daily practice it is crucial for nurses to support patients on the highly successful pharmaceutical treatments for osteoporosis. A recent study by Weycker (2006) concluded that approximately 50–75% of women who start any type of anti-osteoporosis drug therapy (bisphosphonates, calcitonin, selective oestrogen receptor modulators) are no longer using it 12 months later. Osteoporosis is a chronic and ‘silent’ condition requiring long-term therapy. Patients may have difficulty understanding the value of dual energy x-ray absorptiometry (DEXA) scans or biochemical bone markers and may not perceive any clinical benefit from these medications.
Osteoporosis is a preventable disease in many cases. The key message for the nurse to share with their patients is that bone density and quality can significantly improve with lifestyle changes and long-term medications; for example, bisphosphonates can reduce fracture risks by up to 46%.
Osteoporosis Australia has centres in each state and territory offering a wide range of resources for both patients and health professionals.
| www.arthritisaustralia.com.au | Arthritis Australia |
| www.osteoporosis.org.au | Osteoporosis Australia |
| http://www.bones.org.nz/ | Osteoporosis New Zealand |
| www.arthritisnsw.org.au | Arthritis New South Wales |
| www.arthritis.org.au | Arthritis Queensland |
| www.arthritissa.org.au | Arthritis South Australia |
| www.arthritistasmania.com.au | Arthritis Tasmania |
| www.arthritisvic.org.au | Arthritis Victoria |
| www.arthritiswa.org.au | Arthritis Western Australia |
| www.aont.org.au | Arthritis Northern Territory |
| www.health.act.gov.au/c/health | ACT Government Health |
| Information: ACT Health |
DOCUMENTATION AND CRITICAL THINKING
FOCUSED ASSESSMENT: CLINICAL CASE STUDY
MT is a 45-year-old female office worker with a diagnosis of rheumatoid arthritis 3 years ago, who seeks care now for ‘swelling and burning pain in my hands’ for 1 day. She has not been assessed by a rheumatologist since diagnosis and is subsequently not on an effective disease-modifying treatment program.
Subjective
MT was diagnosed as having rheumatoid arthritis at age 41 years by a rheumatologist. Since that time, her ‘flare-ups’ seem to come every 6 to 8 months. Acute episodes involve hand joints and are treated with aspirin, which gives relief. Typically experiences morning stiffness, lasting ½ to 1 hour. Joints feel warm, swollen and tender. Has had weight loss of 4 kg over last 4 years and feels fatigued much of the time. States should rest more, but ‘I can’t take the time’. Daily exercises have been prescribed but doesn’t do them regularly. Takes aspirin for acute flare-ups, feels better in a few days, decreases dose by herself.
Objective
Body joints within normal limits with exception of joints of wrist and hands. Radiocarpal, metacarpophalangeal and proximal interphalangeal joints are red, swollen and tender to palpation. Spindle-shaped swelling of proximal interphalangeal joints of third digit right hand and second digit left hand; ulnar deviation of metacarpophalangeal joints.
Arthritis Research Campaign (ARC). 2005: Clinical assessment of the musculoskeletal system. Available at http://www.arthritis researchuk.org/PDF/Medical Student Handbook 6321.pdf.
Australian Bureau of Statistics (ABS). National health survey: injuries, Australia, 2001. ABS cat. no. 4384.0. Canberra. Available at http://www.abs.gov.au/ausstats/abs@.nsf/mf/4384.0, 2003.
Australian Bureau of Statistics (ABS). 2004–05 National health survey: summary of results, Australia, ABS cat. no. 4364.0. Canberra, 2006, ABS. Available at http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0/.
Australian Commission on Safety and Quality in Health Care (ACSQH). Preventing falls and harm from falls in older people—best practice guidelines for Australian hospitals. Available at http://www.safetyandquality.gov.au/internet/safety/publishing.nsf/Content/FallsGuidelines-AustHospitals.
Australian Health Ministers Advisory Council (AHMAC), Aboriginal and Torres Strait Islander health performance framework report 2006. AHMAC, AHMAC, Canberra, 2006. Available at http://www.health.gov.au/internet/main/publishing.nsf/Content/A218D9F5F5A751DBCA25751400165873/$File/framereport.pdf.
Australian Institute of Health and Welfare (AIHW), 2008a. Arthritis and osteoporosis in Australia—arthritis in children, pp 41–64. Available at http://www.aihw.gov.au/publications/phe/aoa08/aoa08.pdf.
Australian Institute of Health and Welfare (AIHW), 2008b. Arthritis and osteoporosis in Australia. Available at http://www.aihw.gov.au/publications/phe/aoa08/aoa08.pdf.
Australian Institute of Health and Welfare (AIHW), 2010a. Osteoporosis and fractures, pp 89–111. Available at http://www.aihw.gov.au/publications/phe/aoa08/aoa08.pdf.
Australian Institute of Health and Welfare (AIHW). The problem of osteoporotic hip fracture in Australia. Bulletin no. 76. Cat. no. AUS 121. Canberra, AIHW. Available at www.aihw.gov.au/publications/aus/bulletin76/10695.rtf, 2010.
Bailey CA, Brooke-Wavell K. Optimum frequency of exercise for bone health: randomised controlled trial of a high-impact unilateral intervention. Bone. 2010;46(4):1043–1049.
Barnato S, Sprague S. Advances in renal bone disease: osteoporosis and chronic kidney disease. Current Rheumatology Reports. 2009;11:185–190.
Borg-Stein J, Dugan S. Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys Med Rehabil Clin N Am. 2007;18(3):459–476.
Bradley C, Pointer S, for AIHW. 2008: Hospitalisations due to falls by older people. Available at http://www.aihw.gov.au/publications/inj/hdtfbopa05-06/hdtfbopa05-06.pdf.
Buckwalter J. Arthralgia in women: strategies for early diagnosis. J Musculoskel Med. 2006;23:802–808.
Burton S, Lloyd M. An overview of rheumatoid arthritis. Nurs Stand. 2006;20:46–49.
Council of Australian Governments (COAG). 2008: Council of Australian Governments’ Meeting 29 November 2008, Indigenous reform. Available at http://www.coag.gov.au/coag_meeting_outcomes/2008-11-29/#indigenous.
Council of Australian Governments. National Indigenous Reform Agreement (Closing the gap). Available at http://www.coag.gov.au/coag_meeting_outcomes/2009-07-02/docs/NIRA_closing_the_gap.pdf, 2008.
D’Arcy Y. Treatment strategies for low back pain relief. Nurse Pract. 2006;31:16–27.
Dang-Tan T, Franco EL. Diagnosis delays in childhood cancer: a review. Cancer. 2007;110:703–713.
De Man YA, Dolhain RJ, Van de Geijn FE, et al. Disease activity of rheumatoid arthritis during pregnancy: results from a nationwide prospective study. Arthritis Rheum. 2008;59(9):1241–1248.
Department of Health and Ageing (DOHA) National Health Priority Action Council (NHPAC). 2006: Improvement framework for osteoarthritis, rheumatoid arthritis and osteoporosis. Available at http://152.91.25.226/internet/main/publishing.nsf/Content/0C3F942CC20D06CFCA2571410075841F/$File/arthcov.pdf.
Department of Health and Ageing (DOHA), National Health Priority Action Council (NHPAC). Don’t fall for it. Falls can be prevented! A guide to preventing falls for older people, Commonwealth of Australia. Available at http://www.health.gov.au/internet/main/publishing.nsf/Content/phd-pub-injury-dontfall-cnt.htm, 2007.
Department of Infrastructure, Transport, Regional Development and Local Government (DoITRD). 2009: Road deaths Australia 2008 statistical summary. Available at http://www.infrastructure.gov.au/roads/safety/publications/2009/pdf/rsr_04.pdf.
Doherty M, Dacre J, Dieppe P, et al. The ‘GALS’ locomotor screen. Ann Rheum Dis. 1992;51:1165–1169.
Donaldson L, Brooke K, Faux S. Orthopaedic trauma from road crashes: is enough being done? Australian Health Review. 2009;33(1):72–83.
Douglas G, Nicol F, Robertson C. MacLeod’s clinical examination, 12th edn., Edinburgh: Churchill Livingstone/Elsevier, 2009.
Foster H, Eltringham MS, Kay LJ, et al. Delay in access to appropriate care for children presenting with musculoskeletal symptoms and ultimately diagnosed with juvenile idiopathic arthritis. Arthritis Care Res. 2007;57:921–927.
Foster H, Kay L, Friswell M, Coady D, et al. Musculoskeletal screening examination (pGALS) for school-age children based on the adult GALS screen. Arthritis & Rheumatism (Arthritis Care & Research). 2006;55(5):709–716.
Foster H, Kimura Y. Ensuring that all paediatricians and rheumatologists recognise significant rheumatic diseases. Best Practice & Research Clinical Rheumatology. 2009;23:625–642.
Giangregorio L, Leslie W. Time since prior fracture is a risk modifier for ten year osteoporotic fractures. J Bone Miner Res. 2010;25:1400–1405.
Goss PW. Successful screening for neonatal hip instability in Australia. J Paediatr Child Health. 2002;38:469–474.
Green K, Oddie S. The value of the postnatal examination in improving child health. Arch Dis Child Fetal Neonatal Ed. 2008;93:389–393.
Hansberger J. Osteoporosis: review of disease, diagnosis, and treatments for the advanced practice nurse. Internet Journal of Advanced Nursing Practice. 2006;8(1):25–31.
Hart E, Maurice B, Albright M. Developmental dysplasia of the hip—nursing implications and anticipatory guidance for parents. Orthopaedic Nursing. 2006;25(2):100–111.
Hrafnkelsson H, Sigrudsson G, Magnusson KT, et al. Factors associated with bone mineral density and content in 7-year-old children. Bone. 2010;46(4):1058–1062.
Karsenty G. The central regulation of bone remodeling. Trends in Endocrinology and Metabolism. 2000;11(10):437–439.
Langsetmo L, Goltzman D, Kovacs C, et althe CaMos Research Group. Repeat low-trauma fractures occur frequently among men and women who have osteopenic BMD. Journal of Bone and Mineral Research. 2009;24(9):1515–1522.
Lidgren L. The Bone and Joint Decade 2000–2010. Bulletin of the World Health Organization. 2003;81:629.
Lillicrap MS, Byrne E, Speed CA. Musculoskeletal assessment of general medical in-patients—joints still crying for attention. Rheumatology. 2002;42:951–954.
Malik A, Khan W, Chaudhry A, et al. Acute compartment syndrome—a life and limb threatening surgical emergency. Journal of Perioperative Practice. 2009;19(5):137–141.
Manners PJ. Delay in diagnosing juvenile arthritis. Med J Aust. 1999;171:367–369.
Matthews B, Cundy T. Mechanisms of disease—Paget’s disease of bone. Expert Review of Endocrinology & Metabolism. 2009;4(6):651–668.
Moc R, Lim MD, et al. Evaluation of the elderly patient with an abnormal gait. J Am Acad Orthop Surg. 2007;15(2):107–117.
Mohamed K, Appleton R, Nicolaides P. Delayed diagnosis of Duchenne muscular dystrophy. Eur J Paediatr Neurol. 2000;4:219–223.
Moses GM, McGuire T. Drug interactions with complementary medicines. Aust Prescr. 2010;33:177–180.
Osteoporosis Australia, 2006: Prevent the next fracture—guide for nurses. Available at http://www.osteoporosis.org.au/files/internal/oa_fracture_nurse.pdf.
Osteoporosis Australia. Osteoporosis for GPs fact sheet. Available at http://www.osteoporosis.org.au/files/internal/men_osteo_gp-resource.pdf, 2010.
Osteoporosis Australia. Prevent the next fracture—health professional guide. Available at http://www.osteoporosis.org.au/files/internal/oa_fracture_hp.pdf, 2010.
Pink B, Allbon P. The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples, ABS and AIHW, 2008, AIHW cat. no. IHW 21; ABS cat. no. 4704.0. Available at http://www.aihw.gov.au/publications/ihw/hwaatsip08/hwaatsip08.pdf.
Read KM, Kufera JA, Dischinger PC, et al. Life altering outcomes after lower extremity injury sustained in motor vehicle crashes. J Trauma Inj Infect Crit Care. 2004;57:815–823.
Rizzoli R, Bianchi M, Garabédian M, et al. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46:294–305.
Rosendahl K. Ultrasound in the diagnosis of developmental dysplasia of the hip (DDH). Acta Radiology. 2004;45(2):227–235.
Rupert SA. Pathogenesis and treatment of rhabdomyolysis. J Am Acad Nurs Pract. 2002;14(2):82–87.
Scoliosis Australia (nd): The national self detection program for scoliosis. Available at http://www.scoliosis-australia.org/scoliosis/self_detection_prog.html.
Seeman E, Delmas PD. Bone quality—the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354:2250.
Thomas-John M, Codd MB, Manne S, et al. Risk factors for the development of osteoporosis and osteoporotic fractures among older men. J Rheumatol. 2009;36(9):1947–1952.
Transport Accident Commission. The cost of road trauma 2008. Available at http://www.tacsafety.com.au/upload/TAC-civics-task-part-four.pdf, 2008.
Van Slobbe AM, Bohnen AM, Bernsen RM, et al. Incidence rates and determinants in meralgia paresthetica in general practice. J Neurology. 2004;251:294–297.
Weycker D, Macarios D, Edelsberg J, et al. Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int. 2006;17(11):1645–1652.
World Health Organization (WHO). Revised global burden of disease (GBD) 2002 estimates. Years lost due to disability (YLD). Geneva: WHO, 2004. 2004 Available at http://www.who.int/healthinfo/bodgbd2002revised/en/index.html
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group. Geneva: WHO, 1994. (Technical Report Series 843).
Zijlstra G, Van Haastregt J, Van Rossum E, et al. Interventions to reduce fear of falling in community-living older people: a systematic review, Progress in Geriatrics. Journal of Geriatric Society (JAGS). 2007;55:603–615.