Chapter 43 NURSING MANAGEMENT: liver, pancreas and biliary tract problems
1. Define jaundice and describe the signs and symptoms that may occur with the different types of jaundice.
2. Differentiate between the types of viral hepatitis, including their aetiology, pathophysiology, clinical manifestations, complications and multidisciplinary care.
3. Apply knowledge of nursing to the patient with viral hepatitis.
4. Explain the aetiology, pathophysiology, clinical manifestations, complications and multidisciplinary care of the patient with cirrhosis of the liver.
5. Analyse the nursing management of the patient with cirrhosis of the liver.
6. Evaluate the clinical manifestations and management of liver cancer.
7. Describe the pathophysiology, clinical manifestations, complications and multidisciplinary care of acute and chronic pancreatitis.
8. Describe the nursing management of the patient with pancreatitis.
9. Explain the clinical manifestations and multidisciplinary care of the patient with pancreatic cancer.
10. Explore the pathophysiology, clinical manifestations, complications and multidisciplinary care, including surgical therapy, of gall bladder disorders.
11. Describe the nursing management of the patient undergoing conservative or surgical treatment of cholecystitis and cholelithiasis.
Jaundice
Jaundice, a yellowish discolouration of body tissues, results from an alteration in either normal bilirubin metabolism or the flow of bile into the hepatic or biliary duct systems. It is a symptom rather than a disease. Jaundice results when the concentration of bilirubin in the blood becomes abnormally increased. The bilirubin level has to be approximately three times the normal levels (<20 μmol/L) for jaundice to occur. Jaundice can usually first be detected in the sclera and skin (see Fig 43-1).
Most of the body’s bilirubin is formed from the breakdown of haemoglobin (from erythrocytes) by macrophages (see Fig 38-6). This unconjugated (indirect) bilirubin is released into the circulation bound to albumin and is not water-soluble. Because it is not water-soluble and cannot be filtered in the kidneys, unconjugated bilirubin is not excreted in the urine. In the liver the unconjugated bilirubin is conjugated with glucuronic acid to form conjugated (direct) bilirubin, which is water-soluble. Conjugated bilirubin is secreted into bile, which flows through the hepatic and biliary duct system into the small intestine. In the large intestine, bilirubin is converted to stercobilinogen and urobilinogen by bacterial action. Stercobilinogen gives the characteristic brown colour to faeces. Some urobilinogen is reabsorbed into the portal circulation and returned to the liver. Normally a very small amount of urobilinogen is excreted in urine.
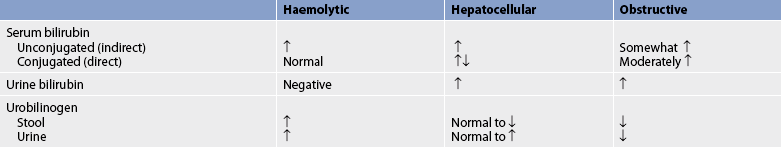
The three types of jaundice are classified as haemolytic, hepatocellular and obstructive. Diagnostic findings associated with these types of jaundice are shown in Table 43-1.
HAEMOLYTIC JAUNDICE
Haemolytic (prehepatic) jaundice is due to an increased breakdown of red blood cells (RBCs), which produces an increased amount of unconjugated bilirubin in the blood (see Table 43-1). The liver is unable to handle this increased load. Causes of haemolytic jaundice include blood transfusion reactions, sickle cell crisis and haemolytic anaemia.
HEPATOCELLULAR JAUNDICE
Hepatocellular (hepatic) jaundice results from the liver’s altered ability to take up bilirubin from the blood or to conjugate or excrete it. Initially both unconjugated and conjugated bilirubin serum levels are increased (see Table 43-1). In hepatocellular disease the hepatocytes are damaged and leak bilirubin, thus increasing levels of conjugated bilirubin. In severe disease, both unconjugated and conjugated bilirubin are elevated as a result of both the inability of hepatocytes to conjugate bilirubin and the continued cell leaking of conjugated bilirubin. As the number of unhealthy hepatocytes increases, the ability to conjugate bilirubin will eventually decrease. Because conjugated bilirubin is water-soluble, it is excreted in the urine. The most common causes of hepatocellular jaundice are hepatitis, cirrhosis and hepatic carcinoma.
OBSTRUCTIVE JAUNDICE
Obstructive (posthepatic) jaundice is due to impeded or obstructed flow of bile through the liver or biliary duct system. The obstruction may be intrahepatic or extrahepatic. Intrahepatic obstructions are due to swelling or fibrosis of the liver’s canaliculi and bile ducts. This can be caused by damage from liver tumours, hepatitis or cirrhosis. Causes of extrahepatic obstruction include common bile duct obstruction by a stone, sclerosing cholangitis and carcinoma of the head of the pancreas. Laboratory findings show an elevation of both unconjugated and conjugated bilirubin and urine bilirubin (see Table 43-1). Because bilirubin does not enter the intestines, there is decreased to no faecal or urinary urobilinogen. With complete obstruction, the stools are clay-coloured.
Hepatitis
Hepatitis is inflammation of the liver. Acute viral hepatitis is the most common form of hepatitis.1 The types of viral hepatitis are A, B, C, D, E and G. Hepatitis may also be caused by drugs (including alcohol), chemicals (see Box 38-1) and autoimmune diseases and metabolic abnormalities. Rarely, hepatitis is caused by bacteria, such as streptococci, salmonellae and Escherichia coli.
Viral hepatitis is a major public health concern. Approximately 1.4 million cases of hepatitis A occur annually worldwide1 and it is almost universal during childhood in some developing countries.
About 2 billion people worldwide have been infected with the hepatitis B virus (HBV). Of these, approximately 50–75% (nearly 400 million people) have active viral replication or chronic active infection. An estimated 600,000 people die each year due to the acute or chronic consequences of hepatitis B.2 There are an estimated 165,000 people living with chronic hepatitis B in Australia3 and approximately 90,000 in New Zealand.4 The incidence of hepatitis B has decreased in many countries due to the widespread use of the HBV vaccine.
Worldwide, approximately 200 million people are infected with the hepatitis C virus (HCV). In Australia, it is estimated that 202,400 people are chronically infected with hepatitis C,5 and in New Zealand the number is estimated to be 50,000.6 Symptoms of early disease are mild, so consequently hepatitis C often is not recognised until the chronic stages, when it has caused severe liver disease. It is thought that approximately 20% of patients with chronic HCV will progress to cirrhosis of the liver within 20–40 years. The introduction of testing of transfusion blood and blood products, along with safer needle-using practices by injecting drug users, has resulted in a drop in new cases since the late 1980s. However, because of the 15–20-year delay between infection and the clinical appearance of liver damage, it is likely that the long-term effects of HCV infection will pose important healthcare challenges for the next 20 years. Chronic HBV and HCV account for 80% of hepatocellular cancer cases today.
Co-infection of HCV and human immunodeficiency virus (HIV) is increasing. Approximately 40% of HIV-infected patients also have HCV. This high rate of co-infection is primarily related to intravenous drug use. The presence of both HIV and HCV places the sufferer at greater risk of end-stage liver disease. (HIV is discussed in Ch 14.)
AETIOLOGY
Viral hepatitis can be caused by one of six major viruses: A, B, C, D, E and G. Other viruses known to produce liver inflammation and damage include cytomegalovirus, Epstein-Barr virus, herpes virus, coxsackievirus and rubella virus.
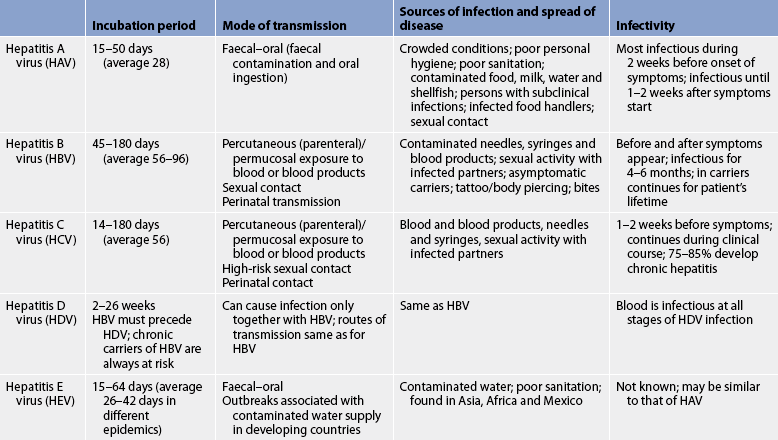
The only definitive way to distinguish among the various forms of viral hepatitis is by the presence of viral antigens and the subsequent development of antibodies to them. Outbreaks of hepatitis are generally caused by hepatitis A virus (HAV). Infection with each virus provides immunity to that virus (homologous immunity). However, the patient can still develop another type of viral hepatitis. An individual infected with hepatitis C can be reinfected with another strain of hepatitis C. The characteristics of hepatitis viruses are summarised in Table 43-2.
Hepatitis A virus
HAV is a ribonucleic acid (RNA) virus family that is transmitted primarily through the faecal–oral route (mainly by ingestion of food or liquid infected with the virus). Poor hygiene, crowded situations and poor sanitary conditions are all factors related to hepatitis A transmission. Transmission occurs between family members, institutionalised individuals, children in day-care centres and from common-source outbreaks. The disease occurs more frequently in developing countries. Food-borne hepatitis A outbreaks are usually due to contamination of food during preparation by an infected food handler.
It frequently occurs in small outbreaks caused by faecal contamination of food or drinking water. It is found in faeces 2 or more weeks before the onset of symptoms and up to 1 week after the onset of jaundice (see Fig 43-2). It is present in the blood only briefly. Anti-HAV (antibody to HAV) immunoglobulin M (IgM) appears in the serum as the stool becomes negative for the virus. Detection of anti-HAV IgM indicates acute hepatitis, and anti-HAV immunoglobulin G (IgG) is an indicator of past infection. The presence of IgG antibody provides lifelong immunity.
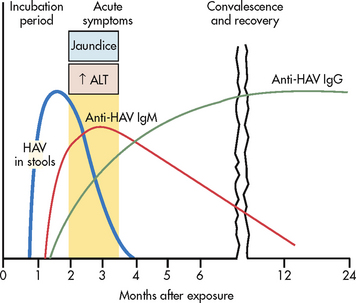
Figure 43-2 The course of infection with hepatitis A virus (HAV). ALT, alanine aminotransferase; IgG, immunoglobulin G; IgM, immunoglobulin M.
There is no chronic carrier state for HAV. The virus is present in faeces during the incubation period so it can be carried and transmitted by persons who have undetectable, subclinical infections. The greatest risk of transmission occurs before clinical symptoms are apparent. It can also be transmitted by patients with anicteric (non-jaundice) hepatitis A.
Hepatitis B virus
HBV is a deoxyribonucleic acid (DNA) virus that is transmitted percutaneously (e.g. injecting drug use, accidental needle-stick punctures); by mucosal exposure to infectious blood, blood products or other body fluids (e.g. semen, vaginal secretions, saliva); or perinatally by mothers infected with HBV. Transmission occurs when infected blood or other body fluids enter the body of a person who is not immune to the virus. Hepatitis B has also been transmitted through organ and tissue transplantation. In the Asia–Pacific region perinatal transmission from mother to infant is the usual source. Approximately 90% of infants infected at birth go on to develop chronic hepatitis B.7 In persons who have HBV, hepatitis B surface antigen (HBsAg) has been detected in almost every body fluid. Infected semen and saliva contain much lower concentrations of HBV than blood but the virus can be transmitted via these secretions. If gastrointestinal (GI) bleeding occurs, faeces can be contaminated with the virus from the blood. There is no evidence that urine, faeces (without GI bleeding), breast milk, tears and sweat are infective. In 20–30% of patients with acute hepatitis B, there are no readily identifiable risk factors.7
Hepatitis B may also be acquired through sexual contact, either heterosexual or male homosexual sex. Although there is a much lower risk of transmission, kissing and sharing of food items may spread the virus via saliva. Other at-risk individuals include those who have household contact with chronically infected persons, haemodialysis patients, and healthcare and public safety workers. The HBV can live on a dry surface for at least 7 days. HBV is much more infectious than HIV.
HBV is a complex structure with three distinct antigens: the surface antigen (HBsAg), the core antigen (HBcAg) and the e antigen (HBeAg). The persistence of HBsAg in the serum for 6–12 months or longer after infection with the virus indicates chronic hepatitis B infection. Each antigen has a corresponding antibody that may develop in response to hepatitis B infection. These antibodies can be detected in the serum of persons with prior exposure to the antigenic virus (see Fig 43-3). The presence of hepatitis B surface antibody (anti-HBs or HBsAB) indicates immunity from the HBV vaccine or from past HBV infection.
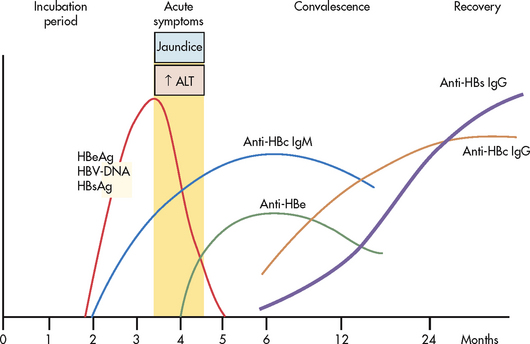
Figure 43-3 The course of infection with hepatitis B virus (HBV). ALT, alanine aminotransferase; anti-HBc, antibody to hepatitis B core antigen; anti-HBe, antibody to HBeAg; anti-HBs, antibody to HBsAg; DNA, deoxyribonucleic acid; HBeAg, hepatitis B e antigen; HBsAg, hepatitis B surface antigen; IgG, immunoglobulin G; IgM, immunoglobulin M.
Approximately 6% of those infected over the age of 5 develop chronic HBV. They become chronic HBV carriers and may transmit the virus.7 The HBsAg level remains detectable in chronic carriers (HBsAg positive on at least two occasions at least 6 months apart). With chronic infection, liver enzyme values may be normal or elevated. Patients with chronic HBV may have a normal liver, low-grade disease or severe liver disease. They are also at higher risk of developing hepatocellular carcinoma. Approximately 15–25% of chronically infected persons die from chronic liver disease.7
Hepatitis C virus
HCV is an RNA virus that is primarily transmitted percutaneously. The most common mode of HCV transmission is the sharing of contaminated needles and equipment among IV drug users. Transmission during blood transfusion has been eliminated. The proportion of cases attributed to high-risk sexual behaviour (e.g. unprotected sex, multiple partners) has increased in recent years to 20%. In Australia, 90% of new infections result from the sharing or reuse of drug-injecting equipment contaminated with infected blood and 10% result from other risk-taking behaviours that involve blood-to-blood contact (e.g. unsterile tattooing, body piercing and skin penetration procedures), needle-stick injuries and vertical transmission from mother to baby (passage of a pathogen from a mother directly to her baby during the perinatal period). Genotyping is used in determining treatment schedules and drugs.8 A reliable antibody test for HCV was not widely available before 1992, so any patients given blood or blood products before then are at risk of chronic HCV infection and should be tested.
Hepatitis D virus
Hepatitis D virus (HDV), also called delta virus, is a defective single-stranded RNA virus that cannot survive on its own. HDV requires HBV to replicate. It can be acquired at the same time as HBV or a person with HBV can be infected with HDV at a later time. The importance of HDV relates to its clinical virulence. Patients with HBV–HDV co-infection may have more severe acute disease and a greater risk of fulminant hepatitis (2–20%) compared with those infected with HBV alone.7 HDV is transmitted percutaneously, similar to HBV. There is no vaccine for HDV; however, vaccination against HBV reduces the risk of co-infection.
Hepatitis E virus
Hepatitis E virus (HEV) is an RNA virus that is transmitted by the faecal–oral route. The most common mode of transmission is drinking contaminated water. Hepatitis E occurs primarily in developing countries, with epidemics reported in India, Asia, Mexico and Africa. Most cases reported in Western countries are in people who have recently travelled to HEV-endemic areas. Currently, no serologic tests to diagnose HEV infection are commercially available. Acute disease is identified by the presence of anti-HEV IgM antibodies in the serum and should be considered if a person has symptoms and has recently travelled to HEV-endemic areas.7
Hepatitis G virus
Hepatitis G virus (HGV) is a poorly characterised parenterally and sexually transmitted virus. HGV often coexists with other viral infections, such as HBV and HCV, and HIV, but does not appear to cause liver damage by itself.9 It has been found in some blood donors and can be transmitted by blood transfusion.
PATHOPHYSIOLOGY
Liver
The pathophysiological changes in the various types of viral hepatitis are similar. Hepatitis involves widespread inflammation of liver tissue. During acute infection, liver damage is mediated by cytotoxic cytokines and natural killer cells that cause lysis of infected hepatocytes. Liver cell damage results in hepatic cell necrosis. There is proliferation and enlargement of the Kupffer cells. Inflammation of the periportal areas may interrupt bile flow (cholestasis). With time, liver cells can regenerate in an orderly manner and, if no complications occur, they should resume their normal appearance and function.
Systemic effects
The antigen–antibody complexes between the virus and its corresponding antibody form a circulating immune complex in the early phases of hepatitis. The circulating immune complex activates the complement system (see Ch 13). The clinical manifestations of this activation are rash, angio-oedema, arthritis, fever and malaise. Cryoglobulinaemia (abnormal proteins found in the blood), glomerulonephritis and vasculitis have also been found secondary to immune complex activation.
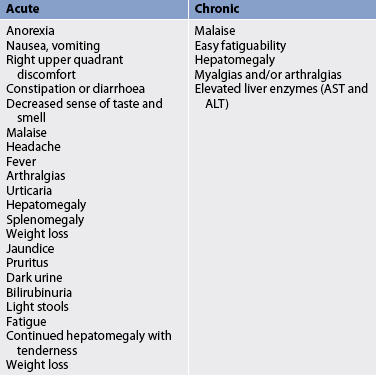
CLINICAL MANIFESTATIONS
A large number of patients have no symptoms. For example, 30% of patients with acute HBV infection and 80% of patients with acute HCV infection will be asymptomatic. The clinical manifestations of viral hepatitis may be classified into acute and chronic phases (see Table 43-3).
The acute phase usually lasts from 1 to 4 months. During the incubation period, symptoms may include malaise, anorexia, fatigue, nausea, occasional vomiting and abdominal (right upper quadrant) discomfort. The anorexia is sometimes severe and may be due to cytokines or other chemicals produced by the infected liver. Weight loss may occur. The patient may find food repugnant and, if a smoker, may have a distaste for cigarettes. There is also a decreased sense of smell. Other symptoms may include headache, low-grade fever, arthralgias and skin rashes. Physical examination may reveal hepatomegaly, lymphadenopathy and sometimes splenomegaly. The acute phase is the period of maximal infectivity.
The acute phase may be icteric (symptomatic, including jaundice) or anicteric. Jaundice results when bilirubin diffuses into the tissues. The urine may darken because of excess bilirubin being excreted by the kidneys. If conjugated bilirubin cannot flow out of the liver because of obstruction or inflammation of the bile ducts, the stools will be light or clay-coloured. Pruritus sometimes accompanies the jaundice, especially if cholestasis is present. The pruritus occurs as a result of the accumulation of bile salts beneath the skin.
When jaundice occurs, the fever usually subsides. The GI symptoms usually remain and some fatigue may continue. The liver is usually enlarged and tender. The convalescent phase following the acute phase begins as jaundice is disappearing and lasts weeks to months, with an average of 2–4 months. During this period the patient’s major complaint is malaise and easy fatiguability. Hepatomegaly remains for several weeks, but splenomegaly subsides during this period. Relapses may occur.
Almost all cases of acute hepatitis A resolve, although a small number may have a viral relapse in the first 2–3 months after the infection. The disappearance of jaundice does not mean the patient has totally recovered. Many HBV infections and the majority of HCV infections result in chronic (life-long) viral infection. Some patients may be asymptomatic. Others, however, may have intermittent or ongoing malaise, fatigue, myalgias, arthralgias and hepatomegaly.
General considerations
Not all patients with viral hepatitis have jaundice. This is termed anicteric hepatitis. A high percentage of persons with HAV are anicteric and do not have symptoms.
There is some slight variation in manifestations between the types of hepatitis. In hepatitis A the onset is more acute and the symptoms are usually mild and flu-like. In hepatitis B the onset is more insidious and the symptoms are usually more severe. In hepatitis C the majority of cases are asymptomatic or mild. However, HCV has a high rate of persistence and in the majority of people leads to chronic liver disease.
COMPLICATIONS
Most patients with acute viral hepatitis recover completely with no complications. The overall mortality rate for acute hepatitis is less than 1%. The mortality rate is higher in older adults and those with underlying debilitating illnesses (including chronic liver disease). Complications that can occur include fulminant hepatic failure, chronic hepatitis, cirrhosis of the liver and hepatocellular carcinoma.
HBV can cause fulminant hepatic failure and results in chronic infection in approximately 10% of those infected as adults but in 90% of those infected in early childhood. Chronic hepatitis B is a risk factor for the development of hepatocellular carcinoma with or without evidence of cirrhosis.
It is not known what factors contribute to the persistence of the virus in some patients. Chronic HBV infection is more likely to develop in infants born to infected mothers and those who acquire the infection as children (e.g. before the age of 5) compared with those who acquire the virus after the age of 5.7 Alterations in the patient’s cellular immune response may be important in the development of the chronic HBsAg carrier state and the progression from acute hepatitis B to chronic hepatitis. These immune system alterations may explain why the patient with chronic renal failure who is undergoing dialysis when hepatitis B develops is more at risk of chronic hepatitis.10 (Persons with chronic renal failure are known to have a depressed cellular immune response.)
There is a greater risk of HCV infection becoming chronic compared with HBV. Approximately 75–85% of patients who acquire HCV will go on to develop chronic infection.7 Approximately 60–70% of patients with HCV will develop chronic liver disease and 5–50% will develop cirrhosis over 20–30 years; of these, 1–5% will die of cirrhosis or hepatocellular cancer.11 HCV infection rarely causes fulminant hepatic failure. Risk factors for progression to cirrhosis include male gender, heavy alcohol consumption and excess iron deposition in the liver. Elevated cholesterol or triglycerides, obesity and diabetes mellitus are also risk factors for the progression of HCV to cirrhosis. Patients who have cirrhosis caused by HCV are at risk of hepatocellular carcinoma. The prognosis of chronic HCV has greatly increased the demand for liver transplants.
Fulminant viral hepatitis
Fulminant viral hepatitis develops in a small percentage of patients and results in severe impairment or necrosis of liver cells and potential liver failure.2,3 The disorder may occur as a complication of hepatitis B, particularly when co-infection with HDV is present. It occurs much less frequently with HCV and rarely occurs with HAV. Toxic reactions to drugs and congenital metabolic disorders may also cause fulminant viral hepatitis and liver failure. Hepatocellular failure with death usually occurs unless urgent liver transplantation is performed.
DIAGNOSTIC STUDIES
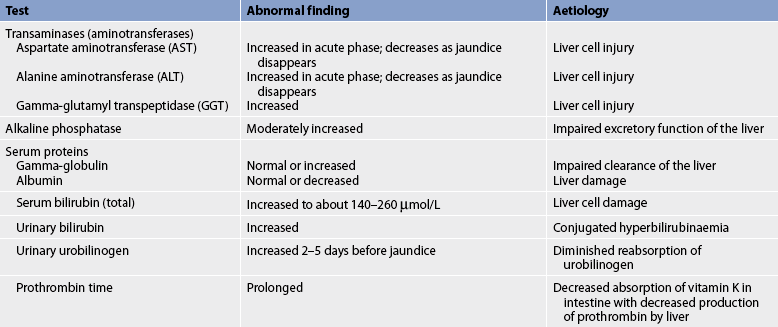
Tests for the different types of viral hepatitis are presented in Table 43-4. In viral hepatitis, many of the liver function tests show significant abnormalities. The common abnormalities are identified in Table 43-5.
TABLE 43-4 Tests for viral hepatitis
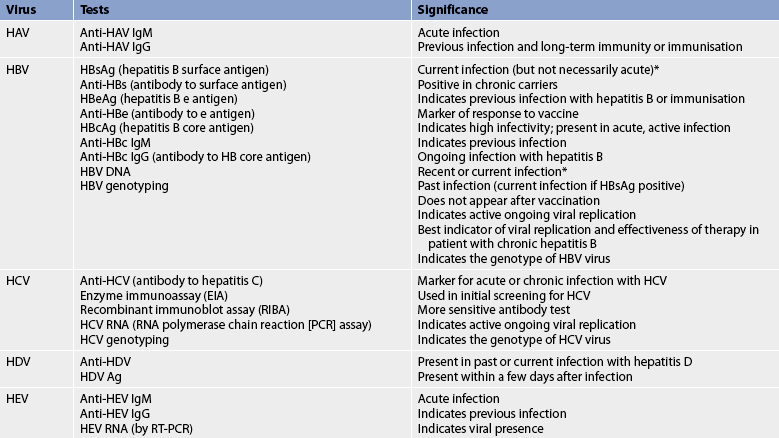
DNA, deoxyribonucleic acid; HAV, hepatitis A virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HDV, hepatitis D virus; HEV, hepatitis E virus; RNA, ribonucleic acid; RT, reverse transcriptase.
* If positive HBsAg and anti-HBc IgM, it indicates the presence of acute infection.
Several tests are available to determine the presence of HCV. Unlike HAV and HBV, antibodies to HCV are not protective and may be an indicator of chronic disease. For the patient who has a positive anti-HCV test by enzyme immunoassay, confirmatory testing is required. To detect active disease (the presence of circulating HCV), HCV-RNA testing is performed. This may be particularly helpful in the immunocompromised patient (e.g. the patient with HIV) whose antibody production is very low (below the detection level of the antibody tests). In addition, this test may be helpful in identifying the presence of the virus in exposed individuals (e.g. healthcare workers) before the development of antibodies. Initial testing for HCV includes HCV antibody testing followed by HCV-RNA testing to document viraemia if antibody positive. A small number of patients may have a false positive HCV antibody test.
For those patients who test positive for HCV, genotyping of the virus should be determined before drug therapy is started. Genotyping has been found to have an important role in managing infection. It is one of the strongest predictors of response to therapy and influences the duration of treatment.5 There are six genotypes of HCV and more than 50 subtypes. In Australia, the predominant genotypes are genotype 1 and genotype 3, while in New Zealand genotype 1 is more prevalent.5 Genotype 1 is more resistant to treatment than other HCV genotypes.8
Chronic HBV is identified by the persistence of HBsAg for longer than 6 months. Patients with chronic HBV are evaluated by assessment of liver function tests, HBV-DNA (which measures the level of circulating HBV) and the presence of HBeAg and anti-HBe. There are several known genotypes of HBV (e.g. A, B, C). In some centres, HBV genotyping is performed prior to starting treatment. HBV genotyping may be useful in predicting disease and treatment outcomes.12
Physical assessment may reveal hepatic tenderness, hepatomegaly and splenomegaly. The liver is palpable. A liver biopsy is not indicated in acute hepatitis unless the diagnosis is in doubt. In chronic hepatitis a liver biopsy may be performed for histological examination of liver cells and characterisation of the degree of inflammation, fibrosis or cirrhosis that may be present. A patient who has a bleeding disorder may not be an appropriate candidate for biopsy because of the risk of bleeding. In these patients a transjugular biopsy may be an option. Newer techniques (sonograms [Fibro scan]) provide information about the degree of liver scarring, which is sometimes referred to as ‘stiffness’ of the liver.
MULTIDISCIPLINARY CARE
There is no specific treatment or therapy for acute viral hepatitis. Most patients can be managed at home. The emphasis is on measures to rest the body and assist the liver in regenerating (see Box 43-1). Adequate nutrients and rest seem to be most beneficial for healing and liver cell regeneration. Emphasis is placed on a well-balanced diet that the patient can tolerate. Rest reduces the metabolic demands on the liver and promotes cell regeneration. Bed rest may be indicated while the patient is symptomatic. The degree of rest ordered depends on the severity of symptoms, but usually alternating periods of activity and rest are adequate. Counselling should include the importance of avoiding alcohol and notification of possible contacts for testing and prophylaxis, if indicated.
Drug therapy
There are no specific drug therapies for the treatment of acute viral hepatitis. Supportive drug therapy may include antiemetics, such as dimenhydrinate. Phenothiazines should not be used because of their possible cholestatic and hepatotoxic effects. If the patient requires a sedative or hypnotic drug, diphenhydramine (Benadryl) or chloral hydrate may be used.
Chronic hepatitis B
Drug therapy for chronic HBV is focused on decreasing the viral load, decreasing the rate of disease progression and decreasing the rate of drug-resistant HBV. Long-term goals are the prevention of cirrhosis, hepatic failure and liver cancer. Current drug therapies for chronic HBV do not eradicate the virus and have limited long-term efficacy.13
α-interferon has multiple effects on the viral replication cycle. After binding to receptors on host cell membranes, the drug blocks viral entry into cells, synthesis of viral proteins, and viral assembly and release. There are two forms of α-interferon: conventional (Intron A) and pegylated. Conventional α-interferon has a short half-life necessitating frequent subcutaneous administration (three times per week). In contrast, the long-acting preparations (pegylated interferons) are administered subcutaneously less frequently (just once per week) making them more convenient. In addition, with the long-acting preparations, blood levels remain high between doses and therefore clinical responses are better.
The long-acting preparations are made by conjugating a conventional interferon with polyethylene glycol (PEG), in a process known as pegylation. Therapeutic effects of pegylated products (Pegasys and PEG-Intron) are due solely to its interferon component. The PEG component serves only to delay elimination of the drug. Because of their convenience and superior efficacy, these products are preferred to conventional interferon and are used in both hepatitis C and hepatitis B.
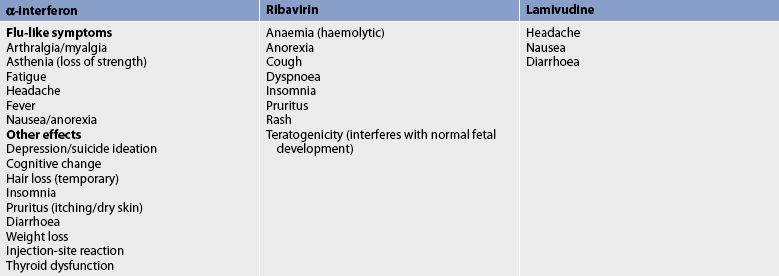
In patients with HBV receiving α-interferon, one-third will have a significant reduction of serum HBV DNA levels, normalisation of ALT levels and loss of HBeAg. The response to treatment may vary based on viral genotype. α-interferon treatment is associated with a number of side effects (see Table 43-6). These side effects are dose related and tend to decrease in severity with continued treatment. Patients receiving α-interferon should have blood counts and a liver function test performed every 4–6 weeks.
Lamivudine, adefovir, entecavir, telbivudine and tenofovir are oral medications used in the treatment of chronic HBV when there is evidence of active viral replication. These drugs suppress HBV replication by inhibiting viral DNA synthesis. They have beneficial effects in terms of reducing viral load, decreasing liver damage and decreasing liver enzymes. Most patients with HBV will require long-term treatment with these medications. If seroconversion (loss of HBeAg) occurs, some patients may be able to discontinue therapy. Seroconversion occurs in 5–20% of HBV patients treated with these oral medications. When these drugs are stopped, the majority of patients (except those who have seroconverted) have HBV DNA and liver inflammation levels that return to pretreatment levels. There have been problems with resistance to lamivudine and adefovir during long-term treatment. A combination of lamivudine and adefovir may be recommended.4 The patient taking adefovir should be monitored for potential nephrotoxicity. Resistance to tenofovir and entecavir is far less than that observed with lamivudine.13 None of the HBV drugs should be used in pregnant women.
Lactic acidosis and severe hepatomegaly with steatosis have been reported with the use of oral medications. Acute, severe exacerbations of hepatitis B have developed following discontinuation of drugs. If these drugs are discontinued, liver function should be monitored closely for several months.
Chronic hepatitis C
Drug therapy is directed at clearing the virus, reducing the viral load and decreasing progression of the disease. Standard treatment for HCV is the combination of ribavirin and pegylated α-interferon.6 Pegylated α-interferon is injected once a week and ribavirin is taken orally twice daily. Treatment of chronic hepatitis C is individualised and based on the severity of liver disease, the potential for side effects, the presence of comorbid conditions, the patient’s readiness for treatment and the presence of other health problems (e.g. HIV).14
Ribavirin, given in combination with α-interferon, has a synergistic effect and reduces the rate of relapse following α-interferon therapy for HCV. Patients who have advanced fibrosis or cirrhosis can be treated with drug therapy as long as liver decompensation (e.g. ascites, oesophageal haemorrhage, jaundice, wasting and encephalopathy) is not present. Ribavirin has a number of side effects, as shown in Table 43-6.
Many patients with HIV also have HCV. Patients who have stable HIV infection and relatively intact immune systems (>200 CD4+ T cells/μL) are treated for HCV with the goal of eradicating HCV and reducing the risk of progression to cirrhosis. However, for those with advanced liver disease, the goal of HCV treatment is to delay disease progression.
The drug treatment of HIV in patients with coexisting HCV requires close attention to liver function, in particular lymphocyte and white and red blood cell counts. HCV treatment with ribavirin and α-interferon may reduce CD4+ counts, increase leucopenia and increase the patient’s risk of anaemia (ribavirin effects).15 Drug interactions may also occur in patients being treated for both HIV and HCV. Depending on the degree of liver damage associated with HCV, drug therapy for HIV may need to be altered because of the potential for drug interactions between some HIV medications and ribavirin.
Depression or mood changes can be common in patients receiving treatment for HCV. Pretreatment with antidepressants such as escitalopram reduces the development of treatment-related depression in patients receiving treatment for HCV.
Nutritional therapy
An important measure in assisting hepatocytes to regenerate is adequate nutrition. No special diet is required in the treatment of viral hepatitis. However, a diet high in carbohydrates and proteins with low fat content is usually recommended. Adequate kilojoules are important because the patient usually loses weight. If fat content is poorly tolerated because of decreased bile production, it should be reduced. Basically, the specific foods in the diet are dictated by the patient. Vitamin supplements, particularly B-complex vitamins and vitamin K, are frequently used. If anorexia, nausea and vomiting are severe, intravenous (IV) solutions of glucose or supplemental enteral feedings may be used. Fluid and electrolyte balance must be maintained.
Prevention
Hepatitis A
Both hepatitis A vaccine and normal human immunoglobulin (NHIG) are used for the prevention of hepatitis A.1 The vaccine is used for pre-exposure prophylaxis, and NHIG can be used either before or after exposure. NHIG provides temporary (6–8 weeks) passive immunity and is effective in preventing hepatitis A if given within 1–2 weeks of exposure. It is recommended for persons who do not have anti-HAV antibodies and are exposed to hepatitis A from close contact with others (e.g. household, day-care centre) who have HAV or food-borne exposure. It may also be used as a prophylactic measure for travellers to countries that have a high incidence of hepatitis A if hepatitis A vaccine cannot be administered more than 2 weeks prior to travel. These people should also receive concomitant administration of the vaccine. In addition to travellers to HAV-endemic areas, the vaccination is recommended for people working in rural and remote Indigenous communities, child care and preschool personnel, people with intellectual disabilities and their carers, healthcare workers who are at risk of exposure, sewage workers, men who have sex with men, injecting drug users, military personnel and patients with chronic liver disease or haemophilia.
There are currently several forms of the hepatitis A vaccine and active immunisation is an important and effective means of controlling hepatitis A from a public health perspective. Primary immunisation consists of a single dose administered intramuscularly in the deltoid muscle. A booster is recommended any time between 6 and 12 months after the primary dose to ensure adequate antibody titres and long-term protection. However, primary immunisation provides immunity within 30 days after a single dose. The vaccine may be administered concomitantly with NHIG, although the ultimate antibody titre obtained is likely to be lower than if the vaccine is given alone.
Twinrix, a combined HAV and HBV vaccine, is available for those over the age of 18 years.1 The primary immunisation consists of three doses, given on a 0-, 1- and 6-month schedule, the same schedule as that used for the single HBV vaccine. Twinrix may be given to individuals at risk of acquiring both infections, which includes expatriates and long-term visitors to developing countries, medical and nursing undergraduate students, men who have sex with men, injecting drug users, patients with chronic liver disease, people with intellectual disabilities and their carers, and people with haemophilia. The side effects of the vaccine are mild and are usually limited to soreness and redness at the injection site.
Hepatitis B
Immunisation with hepatitis B vaccine is the most effective method of preventing HBV infection. In addition to immunising newborns and adolescents, it is important to vaccinate adults in the major risk groups. These include injecting drug users, haemodialysis and liver transplant patients, patients with clotting disorders, individuals with chronic liver disease, HIV/HCV and other immunosuppressed adults, inmates of long-term correctional facilities, residents and staff of facilities for people with intellectual disabilities, healthcare workers, sex workers, men who have sex with men, sexual partners of patients with acute hepatitis B or of asymptomatic carriers, and household members living with a hepatitis B carrier. It is hoped that universal vaccination will lead to eventual prevention and control of hepatitis B.
Hepatitis B vaccine is produced through recombinant DNA technology (see Ch 13). The vaccines are H-B-Vax II and Engerix-B. The vaccine is given in a series of three intramuscular injections in the deltoid muscle. The second dose is administered within 1 month of the first, and the third within 6 months of the first. The vaccine is greater than 95% effective. Successful vaccination should result in anti-HBs titres of 10 mIU/mL or greater. However, it has not been definitely determined what level of antibody is required to provide protection; this means that the frequency of boosters (additional doses) is yet to be determined. Only minor adverse reactions have been reported with vaccination, including transient fever and soreness at the injection site. The vaccine is not contraindicated in pregnancy.
For post-exposure prophylaxis, the vaccine and hepatitis B immune globulin (HBIG) are used. HBIG contains antibodies to HBV and confers temporary passive immunity. HBIG is prepared from the plasma of donors with high titres of anti-HBs and is expensive. HBIG is recommended for post-exposure prophylaxis in cases of needle-stick injury, mucous membrane contact or sexual exposure, and for infants born to mothers who are positive for HBsAg. It should be given after exposure, preferably within 24 hours. The vaccine series should also be started.16
Hepatitis C
Currently there are no vaccines to prevent HCV, although several are in development. Vaccination against hepatitis A and hepatitis B is available and is recommended for people with hepatitis C. There have been cases documented where co-infection with hepatitis A and/or B in people with hepatitis C has resulted in severe liver disease, liver failure and a more rapid and severe course of disease progression.5
 NURSING MANAGEMENT: HEPATITIS
NURSING MANAGEMENT: HEPATITIS
 Nursing assessment
Nursing assessment
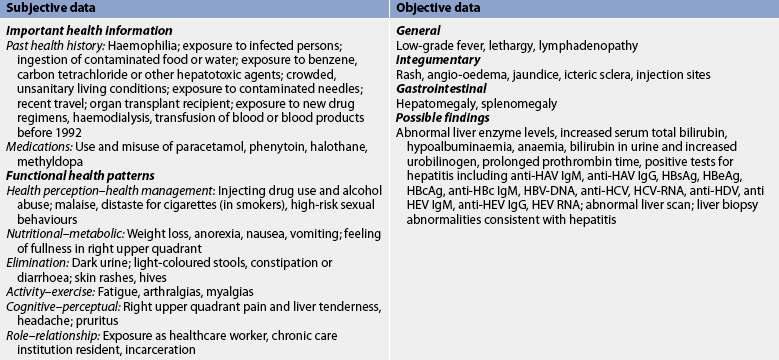
Subjective and objective data that should be obtained from a person with hepatitis are presented in Table 43-7.
 Nursing diagnoses
Nursing diagnoses
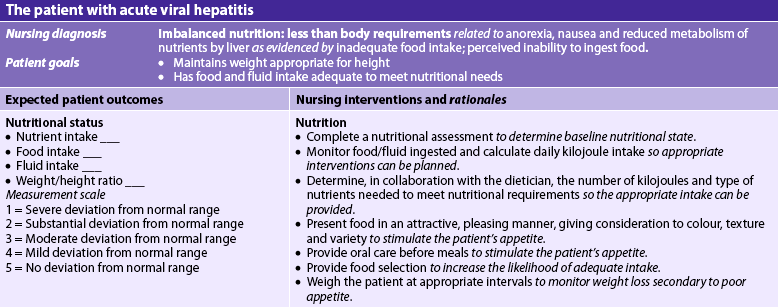
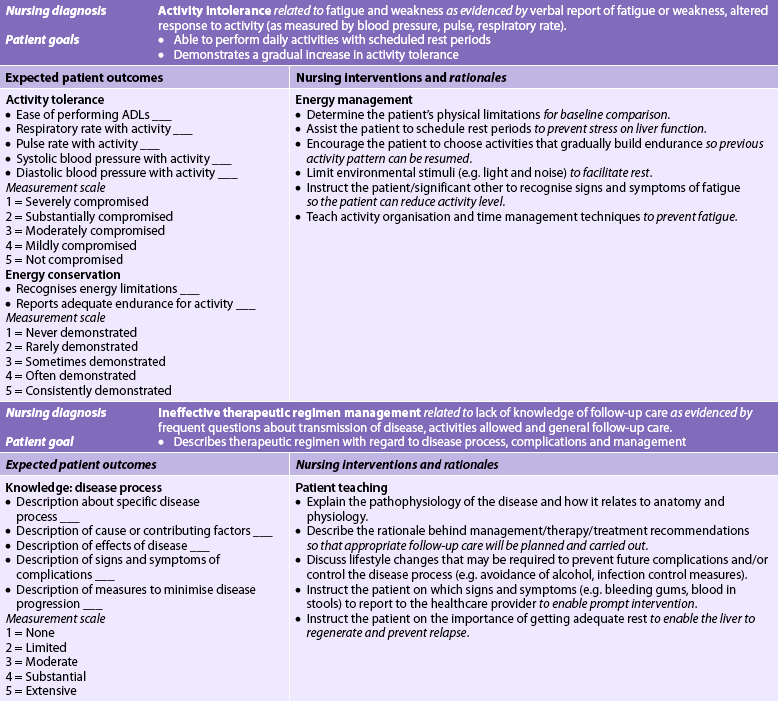
Nursing diagnoses for the patient with hepatitis may include, but are not limited to, those presented in NCP 43-1.
 Planning
Planning
The overall goals are that the patient with viral hepatitis will: (1) have relief of discomfort; (2) be able to resume normal activities; and (3) return to normal liver function without complications.
 Nursing implementation
Nursing implementation
 Health promotion
Health promotion
Viral hepatitis is a community health problem. The nurse must assume a significant role in the control and prevention of this disease. It is helpful to first understand the epidemiology of the different types of viral hepatitis before considering appropriate control measures.
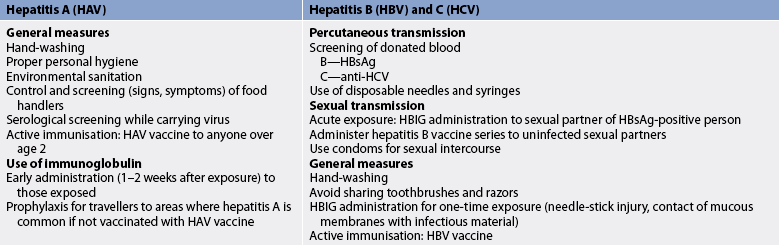
 Hepatitis A
Hepatitis A
Vaccination is the best protection against HAV. Outbreaks of viral hepatitis are usually due to HAV. Preventative measures include personal and environmental hygiene and health education to promote good sanitation (see Table 43-8). Hand-washing is essential and is probably the most important precaution. Health teaching should include careful hand-washing after bowel movements and before eating. When hepatitis A occurs in a food handler, NHIG should be administered to all other food handlers at the establishment. Patrons may also need to be given NHIG.
Isolation is not required for hepatitis A. For a patient with hepatitis A, standard infection control precautions should be used. A private room is indicated if the patient is incontinent of stool or has poor personal hygiene.
 Hepatitis B
Hepatitis B
The use of the hepatitis B vaccine is the best means of protection. Control and prevention of hepatitis B also focus on the identification of possible exposure via percutaneous and sexual transmission (see Table 43-8). The nurse must be aware of the individuals at high risk of contracting hepatitis B and teach methods to reduce risks.
Good hygienic practices, including hand-washing and the use of gloves when expecting contact with blood, are important. A condom is advised for sexual intercourse, and the partner should be vaccinated. Razors, toothbrushes and other personal items should not be shared. Close contacts of the patient with hepatitis B who are HBsAg negative and antibody negative should be vaccinated.
According to infection control guidelines in Australia and New Zealand,16 standard infection control precautions should be followed for the patient with hepatitis B. This includes the use of disposable needles and syringes, which should be disposed of in puncture-resistant disposal units without recapping, bending or breaking.
 Hepatitis C
Hepatitis C
There is no hepatitis C vaccine currently available. The primary measures to prevent HCV transmission are screening of blood, organ and tissue donors; use of infection control precautions; and modification of high-risk behaviour. As in HBV prevention, the nurse should identify individuals at high risk of contracting HCV and teach methods to reduce risks. Infection with HCV often coexists with HIV infection.
The use of gloves when expecting contact with blood is important. A condom may be advised for sexual intercourse with an individual with HCV. Razors, toothbrushes and other personal items should not be shared. Preventative and control measures for hepatitis A, B and C are summarised in Table 43-8.
 Acute intervention
Acute intervention
 Jaundice
Jaundice
The nurse should assess for the degree of jaundice. In light-skinned people the jaundice is usually observed first in the sclera of the eyes and later in the skin. In dark-skinned people, jaundice is observed in the hard palate of the mouth and inner canthus of the eyes. Ictotest reagent tablets may be used to detect urinary bilirubin. The urine may have a dark-brown or brownish-red colour because of the presence of bilirubin. Comfort measures to relieve pruritus (if present), headache and arthralgias are helpful (see NCP 43-1).
Ensuring that the patient receives adequate nutrition is not always easy. The anorexia and distaste for food cause nutritional problems. Dietary assessment must be considered. The nurse should try to determine whether some foods appeal to the patient in spite of the anorexia. Small, frequent meals may be preferable to three large ones and may also help prevent nausea. Often, a patient with hepatitis finds that anorexia is not as severe in the morning, so it is easier to eat a good breakfast than a large dinner. Measures to stimulate the appetite, such as mouth care, antiemetics and attractively served meals in pleasant surroundings, should be included in the nursing care plan. Other measures that may be tried to counteract the anorexia are carbonated beverages and the avoidance of very hot or very cold foods. Adequate fluid intake (2500–3000 mL per day) is important.
 Rest
Rest
Rest is essential and is an important factor in promoting liver cell regeneration. The nurse must assess the patient’s response to the rest and activity plan and modify it accordingly. If the patient is on bed rest, measures to prevent skin, respiratory and circulatory complications should be initiated. Assessment of the liver function tests and symptoms should continue as a guide to activity.
Psychological and emotional rest is as essential as physical rest. Bed rest may produce anxiety and extreme restlessness in some patients and may be more damaging than reasonable ambulation. Diversional activities, such as reading and hobbies (e.g. knitting, stamp collecting), may help the patient.
 Ambulatory and home care
Ambulatory and home care
Most patients with viral hepatitis will be cared for at home so the nurse must assess the patient’s knowledge of nutrition and provide the necessary dietary teaching. Rest and adequate nutrition are especially important until studies show that liver function has returned to normal. The patient must be cautioned about overexertion and the need to follow the doctor’s advice about when it is safe to return to work. The nurse must also teach the patient and family about preventative measures and how to prevent transmission to other family members. The patient should know what symptoms should be reported to the healthcare provider.
The patient should be assessed for any manifestations indicative of complications. Bleeding tendencies with increasing prothrombin time values, symptoms of encephalopathy or abnormal liver function tests indicate problems, and the patient should be assessed and treated promptly.
The patient should be instructed to have regular follow-up for at least 1 year after the diagnosis of hepatitis. Because relapses are fairly common with hepatitis B and C, the patient should be advised about the symptoms of recurrence and the need for follow-up evaluations. All patients with chronic HBV or HCV should avoid alcohol as it is well established that alcohol can make the liver disease worse (progression is accelerated).
A patient who remains positive for HBsAg is a chronic carrier and should never be a blood donor. A patient who tests positive for the HCV antibody should also not donate blood. Due to the shortage of livers available for transplantation, the use of liver tissues from individuals who are HBcAb positive is now being considered for select (HBV naive) recipients.
The patient with HBV or HCV should be instructed to use a condom when engaging in sexual intercourse. The patient who is receiving α-interferon for the treatment of hepatitis B or C requires education about the drug. α-interferon is administered subcutaneously and thus the patient or family member needs to be taught how to administer the drug. There are numerous side effects with the therapy, including flu-like symptoms (e.g. fever, malaise, fatigue, chills). The nurse or doctor may recommend that paracetamol be administered 30–60 minutes before injection to reduce these symptoms. Other significant side effects include thrombocytopenia, neutropenia, psychiatric disturbances (e.g. mood swings, depression), serious thyroid dysfunction and limited alopecia (see Table 43-6). (Additional information on α-interferon is presented in Chs 13 and 15.)
CONTROL OF HEPATITIS IN HEALTHCARE PERSONNEL
Hepatitis A
Hepatitis A is rarely transmitted from patients to healthcare personnel. When this does occur, it is associated with patients with undiagnosed hepatitis A who are treated for other problems. Usually these patients are incontinent of faeces. The use of standard infection control precautions should prevent transmission of HAV to healthcare personnel.
Hepatitis B
Healthcare workers may be exposed to HBV from needle-stick injuries or blood contamination to mucous membranes or non-intact skin. If a healthcare worker is exposed to HBV through a needle-stick injury and does not receive the vaccine, there is a 6–30% chance of infection with hepatitis B.17 Vaccination is the most effective method to prevent HBV in healthcare workers. The principal mode of transmission of HBV for healthcare personnel is parenteral (e.g. needle-stick injuries). Other forms of transmission include contamination of fresh cutaneous scratches or abrasions, burns and contamination of mucosal surfaces with infective blood, blood products, saliva or semen.
Hepatitis C
Transmission is usually due to percutaneous needle exposure or other blood exposure and undetected parenteral transmission. Measures to prevent transmission of the viruses from patients to healthcare personnel are presented in Table 43-9. Very rarely are patients infected by healthcare workers.
Toxic and drug-induced hepatitis
Liver injury and death may occur after the inhalation, parenteral injection or ingestion of certain chemical substances (see Box 38-1). The two major types of chemical hepatotoxicity are toxic and drug-induced hepatitis. Agents producing toxic hepatitis are generally systemic poisons (e.g. carbon tetrachloride, gold compounds) or are converted in the liver to toxic metabolites (e.g. paracetamol). Liver necrosis generally occurs within 2–3 days of acute exposure to a toxic substance.
Idiosyncratic drug reactions produce drug-induced hepatitis. Such agents as halothane, isoniazid, flucloxacillin, methotrexate and methyldopa may produce idiosyncratic reactions because of patient susceptibility (metabolic reactivity) to these agents or immunologically mediated hypersensitivity responses. Some herbal medications have caused liver injury severe enough to require liver transplantation. Liver injury may occur at any time during or shortly after exposure. However, some responses are delayed, occurring 2–5 weeks after exposure.
Older patients are particularly vulnerable to drug-induced hepatitis. This is due to several factors, including increased use of prescription and over-the-counter drugs, which can lead to drug interactions and potential drug toxicity. Age-related decreases in liver function caused by decreased liver blood flow and enzyme activity result in decreased drug metabolism. In addition, with ageing there is a decrease in the ability of the liver to recover from drug-induced injury.
Toxic and drug-induced hepatitis are similar to viral hepatitis in the pathophysiological changes in the liver and the clinical manifestations they cause. The usual presenting clinical findings are anorexia, nausea, vomiting, hepatomegaly, splenomegaly and abnormal liver function studies. Treatment is largely supportive as in acute viral hepatitis. Recovery may be rapid if the hepatotoxin is identified and removed. Liver transplantation may be necessary in cases of severe liver damage.
Autoimmune/metabolic/genetic liver diseases
AUTOIMMUNE HEPATITIS
Autoimmune hepatitis is a chronic inflammatory disorder of the liver of unknown cause, although it may be related to both genetic and environmental factors. Prior viral infections may be the initiating factor and then progressive cytotoxic T-cell-mediated injury of hepatocytes occurs. The disease is characterised by the presence of autoantibodies, high levels of serum immunoglobulins and frequent association with other autoimmune diseases. Circulating autoantibodies, including antinuclear antibodies (ANA) and anti-DNA antibodies, are present in most patients with autoimmune hepatitis. The presenting signs and symptoms are variable and similar to those of viral hepatitis. Laboratory tests (elevation of liver enzymes) reveal liver inflammation without evidence of viral antigens. The majority (70–80%) of patients who are diagnosed with autoimmune hepatitis are women. The course of the disease is also variable, with the majority of the patients exhibiting chronic active hepatitis. Liver cancer develops in approximately 6% of patients.
Unlike viral hepatitis, autoimmune hepatitis (in which there is evidence of necrosis and cirrhosis) is treated with corticosteroids or other immunosuppressive agents. Daily treatment with methylprednisolone alone or in combination with azathioprine will induce remission in approximately 80% of patients. If these drugs do not work, other immunosuppressive therapies (e.g. cyclosporin, tacrolimus or mycophenolate mofetil) are initiated. Liver transplant is indicated for liver failure.
WILSON’S DISEASE
Wilson’s disease is an autosomal recessive disorder of copper metabolism. The reduced excretion of copper in bile and the resulting accumulation of copper leads to liver disease, progressive neurological disorders and psychiatric illnesses as well as renal dysfunction. The hallmark sign of Wilson’s disease is corneal Kayser-Fleischer rings. These are brownish-reddish coloured rings that can be seen in the cornea near the limbus on eye examination. The recommended initial treatment of symptomatic patients or those with active disease is with chelating agents, such as D-penicillamine, which promote the excretion of urinary copper. Liver transplantation is indicated for patients presenting with fulminant hepatic failure and for progressive hepatic dysfunction who are not responding to chelation with D-penicillamine. Wilson’s disease is cured by transplantation.
HAEMOCHROMATOSIS
Hereditary haemochromatosis (HH) is one of the most common inherited disorders in Caucasians. Most patients are homozygous for the C282Y mutation and genetic testing. The disease is characterised by inappropriate intestinal absorption of iron, with progressive deposition in the parenchymal cells of the liver and other organs (heart, pancreas, endocrine, skin, joints). The degree of iron overload has a direct impact on the life expectancy of the individual with HH. Liver transplantation is indicated for advanced decompensated cirrhosis or the presence of non-resectable hepatocellular carcinoma detected on screening a cirrhotic liver. The major causes of death are decompensated cirrhosis, hepatocellular carcinoma, diabetes mellitus and cardiomyopathy.
PRIMARY BILIARY CIRRHOSIS
Primary biliary cirrhosis (PBC) is a chronic inflammatory condition of the liver. It is characterised by generalised pruritus, hepatomegaly and hyperpigmentation of the skin. While the aetiology of PBC is not completely understood, it appears that both genetic and environmental factors, such as chemical exposure and infection, may play a role. In PBC there is a T-cell mediated attack of the small bile duct epithelial cells resulting in a loss of bile ducts and ultimately cholestasis (blockage of bile flow). Over time this leads to liver necrosis and cirrhosis. Patients with PBC are at increased risk of hepatocellular cancer.
Approximately 95% of patients diagnosed with PBC are women. The incidence of PBC in many Western countries is increasing. Women in mid-life, aged between 30 and 60, are most frequently affected. The disease is associated with other autoimmune disorders, such as rheumatoid arthritis, Sjögren’s syndrome and scleroderma (discussed in Ch 64).
In the early stages patients may be asymptomatic. Patients may present to their healthcare provider with symptoms of fatigue and pruritus. Bleeding associated with hypoprothrombinaemia may also be present. Jaundice is a late sign. Osteoporosis is also found in a significant number of patients. In addition, patients may present with signs of fat malabsorption, including low levels of fat-soluble vitamins, which occurs due to decreased bile secretion. Serum alkaline phosphatase levels, antimitochrondrial antibodies (AMA), ANAs and serum lipid levels are also elevated. Histological evidence of damage is found on liver biopsy.
The goals of treatment are the suppression of ongoing liver damage, the prevention of complications, and symptom management. Management of complications and symptoms includes a focus on malabsorption, skin disorders, including pruritus and xanthomas (cholesterol deposits in the skin), hyperlipidaemia, vitamin deficiencies, anaemia and fatigue. Cholestyramine is used to manage pruritus. Patients are monitored for progression to cirrhosis, which is variable across patients. Liver transplantation is a treatment option for end-stage liver disease in patients with PBC.
NON-ALCOHOLIC FATTY LIVER DISEASE AND NON-ALCOHOLIC STEATOHEPATITIS
Non-alcoholic fatty liver disease (NAFLD) is a group of disorders that is characterised by hepatic steatosis (accumulation of fat in the liver) that is not associated with other causes such as hepatitis, autoimmune disease or alcohol. Histologically, cell changes include the presence of fatty changes in the hepatocytes. This accumulation of fat can lead to inflammation and scarring, which is called non-alcoholic steatohepatitis (NASH). People with NASH can develop advanced scarring (cirrhosis) with an increased risk for developing hepatocellular cancer and liver failure.
Currently, NAFLD affects between 12% and 24% of the population in the Asia–Pacific region.18 The risk of developing NAFLD is directly related to body weight and is a major complication of obesity. NAFLD should be considered in patients with risk factors such as obesity, diabetes mellitus, hypertriglyceridaemia, severe weight loss (especially in those whose weight loss was recent) and syndromes associated with insulin resistance. Poor diet and conditions such as tuberculosis, intestinal bypass and medications (e.g. corticosteroids) can also lead to NAFLD. NAFLD should also be considered in patients who have persistently elevated ALT levels and for whom no other cause can be found. NAFLD can progress to liver fibrosis and cirrhosis.
Clinical manifestations and diagnostic studies
Most patients with NAFLD are asymptomatic. NAFLD is usually diagnosed during the evaluation of other health problems, such as hypertension, diabetes mellitus or obesity. For example, in some asymptomatic patients an elevated ALT level is found when liver function tests are performed during the course of monitoring antihyperlipidaemic drug therapy. Only a small number of patients exhibit signs of serious liver disease (e.g. ascites, variceal haemorrhage). Jaundice occurs late in NAFLD and indicates advanced liver disease.
Elevations in liver function tests (ALT, AST) two to four times higher than normal values are often the first signs of NAFLD. However, elevations may be associated with a number of other liver disorders. With progression of the disease the serum albumin level is reduced and the serum bilirubin level and prothrombin time are elevated. Definitive diagnosis is by liver biopsy and histological examination of hepatocytes. Ultrasound and computed tomography (CT) scans are also used to diagnose NAFLD.
Multidisciplinary care
Those who are older, obese or have diabetes mellitus are at risk of advanced liver disease. There is no definitive treatment and therefore therapy is directed at reducing risk factors. This includes treating diabetes mellitus, reducing body weight and eliminating harmful medications.
For those who are overweight, weight reduction is important. Weight loss will improve insulin sensitivity and reduce liver enzyme levels. There is no specific dietary therapy that is recommended. However, a heart-healthy diet based on the Healthy Living Pyramid (see Fig 39-1) is appropriate. Patients should have liver function monitored during weight loss because too rapid a loss of weight is associated with liver failure. Dietary changes to induce weight loss are more likely to succeed if behaviour-modification therapy is employed. In some cases, NAFLD may progress to liver failure and liver transplantation may be required.
Cirrhosis of the liver
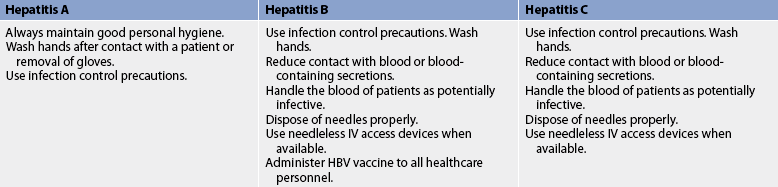
Cirrhosis is a chronic progressive disease of the liver characterised by extensive degeneration and destruction of the liver parenchymal cells (see Fig 43-4). The liver cells attempt to regenerate but the regenerative process is disorganised, resulting in abnormal blood vessel and bile duct architecture. The overgrowth of new and fibrous connective tissue distorts the liver’s normal lobular structure, resulting in lobules of irregular size and shape with impeded vascular flow. Cirrhosis may have an insidious, prolonged course.

Figure 43-4 Cirrhosis that developed secondary to alcoholism. The characteristic diffuse nodularity of the surface is due to the combination of regeneration and scarring of the liver.
Cirrhosis has a prevalence of 70 per 100,000 males and 50 per 100,000 females, with the highest incidence occurring between the ages of 40 and 60. Excessive alcohol ingestion is the single most common cause of cirrhosis.
AETIOLOGY AND PATHOPHYSIOLOGY
Any chronic (long-term) liver disease, including excessive alcohol intake and NAFLD, can cause cirrhosis. The specific cause of cirrhosis may not be determined in all patients. Excessive alcohol ingestion is the single most common cause because alcohol has a direct hepatotoxic effect. Some controversy exists as to whether the cause is the alcohol or the malnutrition that often coexists with chronic alcoholism. A common problem in alcoholics is protein malnutrition. There have been cases of nutrition-related cirrhosis resulting from extreme dieting, malabsorption and obesity. Environmental factors, as well as a genetic predisposition, may also lead to the development of cirrhosis, regardless of dietary or alcohol intake.
Approximately 20% of patients with chronic hepatitis C and 10–20% of those with chronic hepatitis B will develop cirrhosis. Chronic inflammation and cell necrosis result in fibrosis and, ultimately, cirrhosis. Chronic hepatitis combined with alcohol ingestion is synergistic with accelerating liver damage.
Biliary causes of cirrhosis include primary biliary cirrhosis (described earlier in this chapter) and primary sclerosing cholangitis. Primary sclerosing cholangitis is a chronic inflammatory condition affecting the liver and bile ducts. It is most frequently found in men. The aetiology of primary sclerosing cholangitis is unknown. However, it is strongly associated with ulcerative colitis. The chronic inflammation can ultimately progress to cirrhosis and end-stage liver disease.
Cardiac cirrhosis includes a spectrum of hepatic derangements that result from long-standing severe right-sided heart failure. The treatment is aimed at managing the patient’s underlying heart failure.
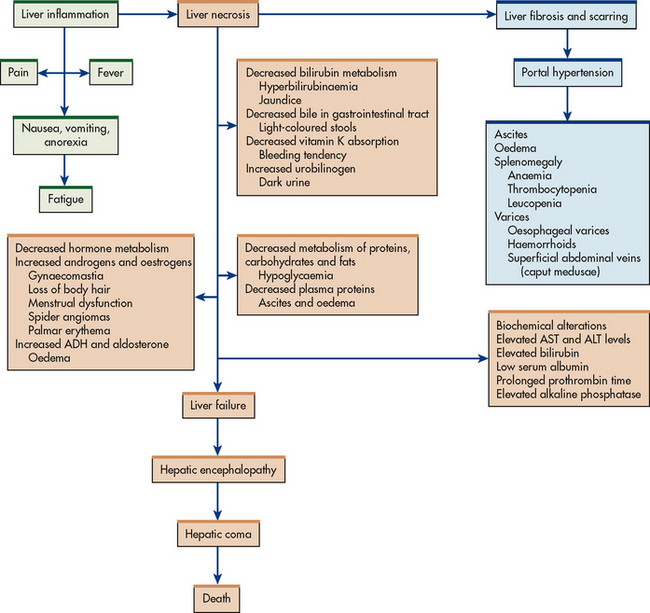
CLINICAL MANIFESTATIONS
The onset of cirrhosis is usually insidious. Occasionally there is an abrupt onset of symptoms. GI disturbances are common early symptoms and include anorexia, dyspepsia, flatulence, nausea and vomiting, and change in bowel habits (diarrhoea or constipation). These symptoms occur as a result of the liver’s altered metabolism of carbohydrates, fats and proteins. The patient may complain of abdominal pain described as a dull, heavy feeling in the right upper quadrant or epigastrium. The pain may be due to swelling and stretching of the liver capsule, spasm of the biliary ducts and intermittent vascular spasm. Other early manifestations are fever, lassitude, slight weight loss and enlargement of the liver and spleen. The liver is palpable in many patients with cirrhosis.
Later symptoms may be severe and result from liver failure and portal hypertension. Jaundice, peripheral oedema and ascites develop gradually. Other late symptoms include skin lesions, haematological disorders, endocrine disturbances and peripheral neuropathies (see Fig 43-5). In the advanced stages the liver becomes small and nodular.
• Jaundice. Jaundice results from the functional derangement of liver cells and compression of the bile ducts by connective tissue overgrowth. Jaundice occurs as a result of the decreased ability to conjugate and excrete bilirubin (hepatocellular jaundice). The jaundice may be minimal or severe depending on the degree of liver damage. If obstruction of the biliary tract occurs, obstructive jaundice may also occur and is usually accompanied by pruritus. The pruritus is due to an accumulation of bile salts underneath the skin.
• Skin lesions. Various skin manifestations are commonly seen in cirrhosis. Spider angiomas (telangiectasia or spider naevi) are small, dilated blood vessels with bright-red centre points and spider-like branches. They occur on the nose, cheeks, upper trunk, neck and shoulders. Palmar erythema (a red area that blanches with pressure) is located on the palms of the hands. Both of these types of lesions are attributed to an increase in circulating oestrogen as a result of the damaged liver’s inability to metabolise steroid hormones.
• Haematological problems. Haematological problems include thrombocytopenia, leucopenia, anaemia and coagulation disorders. Thrombocytopenia, leucopenia and anaemia are probably caused by the splenomegaly. Splenomegaly results from the back-up of blood from the portal vein into the spleen (portal hypertension). Overactivity of the enlarged spleen results in an increased removal of blood cells from the circulation. The anaemia is also due to inadequate RBC production and survival. Other factors involved in the anaemia relate to poor diet, poor absorption of folic acid and bleeding from varices. Coagulation problems result from the liver’s inability to produce prothrombin and other factors essential for blood clotting. Coagulation problems are manifested by haemorrhagic phenomena or bleeding tendencies (e.g. epistaxis, purpura, petechiae, easy bruising, gingival bleeding, heavy menstrual bleeding).
• Endocrine disturbances. Several signs and symptoms relating to the metabolism and inactivation of adrenocortical hormones, oestrogen and testosterone occur in cirrhosis. Normally the liver metabolises these hormones. When the damaged liver is unable to do this, various manifestations occur. In men, gynaecomastia, loss of axillary and pubic hair, testicular atrophy and impotence with loss of libido may occur as a result of oestrogen accumulation. In younger women amenorrhoea may occur and in older females there may be vaginal bleeding. The liver fails to metabolise aldosterone adequately, resulting in hyperaldosteronism with subsequent sodium and water retention and potassium loss.
• Peripheral neuropathy. Peripheral neuropathy is a common finding in alcoholic cirrhosis. It is probably due to a dietary deficiency of thiamine, folic acid and vitamin B12. The neuropathy usually results in mixed nervous system symptoms but sensory symptoms may predominate. Clinical manifestations of cirrhosis of the liver are numerous and may eventually involve the total body (see Fig 43-6).
COMPLICATIONS
Major complications of cirrhosis are portal hypertension with resultant oesophageal/gastric varices, peripheral oedema and ascites, hepatic encephalopathy (coma) and hepatorenal syndrome.
Portal hypertension and oesophageal/gastric varices
Because of the structural changes in the liver from the cirrhotic process, there is compression and destruction of the portal and hepatic veins and sinusoids. These changes result in obstruction to the normal flow of blood through the portal system, resulting in portal hypertension. Portal hypertension is characterised by increased venous pressure in the portal circulation, as well as splenomegaly, large collateral veins, ascites, systemic hypertension and varices. Many pathophysiological changes result from portal hypertension. Collateral circulation develops in an attempt to reduce this high portal pressure and also to reduce the increased plasma volume and lymphatic flow. The common areas where the collateral channels form are in the lower oesophagus (the anastomosis of the left gastric vein and the azygos veins), the anterior abdominal wall, the parietal peritoneum and the rectum. Varicosities may develop in areas where the collateral and systemic circulations communicate, resulting in oesophageal, gastric and duodenal varices, caput medusae (ring of varices around the umbilicus) and haemorrhoids. Even though bleeding can occur from all luminal varices, it is those in the oesophagus and stomach that commonly rupture.
Oesophageal varices are a complex of tortuous veins at the lower end of the oesophagus, enlarged and swollen as a result of portal hypertension. Gastric varices are located in the upper portion (cardia, fundus) of the stomach. They occur alone or in combination with oesophageal varices. Varices are a common complication of cirrhosis, occurring in two-thirds to three-quarters of patients with cirrhosis. These collateral vessels contain little elastic tissue and are quite fragile. They tolerate the high blood pressure poorly and the result is distended veins that bleed easily. Large varices are more likely to bleed. Oesophageal varices are responsible for approximately 80% of variceal haemorrhages. The remaining 20% of varices are due to gastric varices.
Bleeding varices are the most life-threatening complication of cirrhosis. The varices rupture and bleed in response to ulceration and irritation. Factors producing ulceration and irritation include alcohol ingestion, swallowing of poorly masticated food, ingestion of coarse food, acid regurgitation from the stomach and increased intraabdominal pressure caused by nausea, vomiting, straining at stool, coughing, sneezing or lifting heavy objects. The patient may have melaena or haematemesis. There may be slow oozing or massive haemorrhage, which is a medical emergency.
Portal hypertension may also result in a condition termed portal hypertensive gastropathy (PHG). In this condition, the endoscopic appearance of the gastric mucosa is a characteristic mosaic-like pattern with or without red spots. Histologically, these lesions correspond to dilated vessels in the mucosa and submucosa in the absence of erosions or inflammation. Venous congestion related with raised portal pressure and increased gastric blood flow are crucial factors for the development of PHG. It is an important condition, as approximately 8% of upper GI bleeding in cirrhotic patients is secondary to PHG. Endoscopic therapies do not have a role in treatment; a reduction in portal pressure through propranolol, portosystemic shunts or liver transplantation is effective.
Peripheral oedema and ascites
Peripheral oedema sometimes precedes ascites but in some patients its development coincides with or occurs after ascites. Oedema results from decreased colloidal oncotic pressure as a result of impaired liver synthesis of albumin and increased portocaval pressure due to portal hypertension. Peripheral oedema occurs as ankle and presacral oedema.
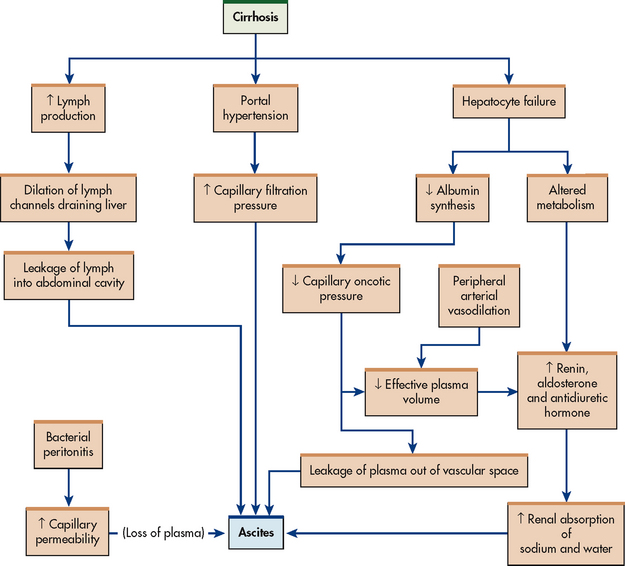
Ascites is the accumulation of serous fluid in the peritoneal or abdominal cavity. It is a common manifestation of cirrhosis. When the blood pressure is elevated in the liver, as occurs in cirrhosis, proteins move from the blood vessels via the larger pores of the sinusoids (capillaries) into the lymph space (see Fig 43-7). When the lymphatic system is unable to carry off the excess proteins and water, they leak through the liver capsule into the peritoneal cavity. The osmotic pressure of the proteins pulls additional fluid into the peritoneal cavity (see Table 43-10).
TABLE 43-10 Factors involved in the development of ascites
| Factor | Mechanism |
|---|---|
| Portal hypertension | Increase in resistance of blood flow through liver |
| Increased flow of hepatic lymph | Weeping of protein-rich lymph from surface of cirrhotic liver, intrahepatic blockage of lymph channels |
| Decreased serum colloidal oncotic pressure | Impairment of liver synthesis of albumin, loss of albumin into peritoneal cavity |
| Hyperaldosteronism | Increase in aldosterone secretion stimulated by decreased renal blood flow; impairment of liver metabolism of aldosterone |
| Impaired water excretion | Reduction in renal vascular flow and excessive serum levels of antidiuretic |
A second mechanism of ascites formation is hypoalbuminaemia resulting from the inability of the liver to synthesise albumin. The hypoalbuminaemia results in decreased colloidal oncotic pressure. A third mechanism is hyperaldosteronism, which occurs when aldosterone is not metabolised by damaged hepatocytes. The increased level of aldosterone causes increased sodium reabsorption by the renal tubules. This retention of sodium, as well as an increase in antidiuretic hormone, causes additional water retention in these patients. Because of oedema formation there is decreased intravascular volume and, subsequently, decreased renal blood flow and glomerular filtration.
Ascites is manifested by abdominal distension with weight gain (see Fig 43-8). If the ascites is severe, the umbilicus may be everted. Abdominal striae with distended abdominal wall veins may be present. The patient has signs of dehydration (e.g. dry tongue and skin, sunken eyeballs, muscle weakness). There is also a decrease in urinary output. Hypokalaemia is common and is due to an excessive loss of potassium because of the effects of increased aldosterone. Low potassium levels can also result from diuretic therapy used to treat the ascites.

Figure 43-8 Ascites and gynaecomastia associated with cirrhosis of the liver. This photograph was taken after a paracentesis was performed.
Because of alterations in immune function associated with cirrhosis, patients with ascites are at risk of spontaneous bacterial peritonitis. This occurs in approximately 8–30% of hospitalised patients with cirrhosis and ascites and is particularly common after variceal haemorrhage. The bacteria most frequently found are Gram-negative enteric pathogens, such as E. coli.
Hepatic encephalopathy
Hepatic encephalopathy is a neuropsychiatric manifestation of liver damage. It is considered a terminal complication in liver disease. Hepatic encephalopathy can occur in any condition in which liver damage causes ammonia to enter the systemic circulation without liver detoxification.19
Hepatic encephalopathy is a metabolic encephalopathy that is associated with variable levels of cerebral oedema. The pathogenesis of hepatic encephalopathy is multifactorial and includes the neurotoxic effects of ammonia, abnormal neurotransmission, astrocyte swelling and inflammatory cytokines. Hepatic encephalopathy is associated with rising levels of ammonia. However, the exact mechanism of action of ammonia remains to be determined. A major source of ammonia is the bacterial and enzymatic deamination of amino acids in the intestines. The ammonia that results from this deamination process normally goes to the liver via the portal circulation and is converted to urea, which is then excreted by the kidneys. When the blood is shunted past the liver via the collateral anastomoses or when the liver is unable to convert ammonia to urea, large quantities of ammonia remain in the systemic circulation. The ammonia crosses the blood–brain barrier and produces neurological toxic manifestations. A number of factors may precipitate hepatic encephalopathy, mostly because they increase the amount of circulating ammonia (see Table 43-11). Hepatic encephalopathy is also a complication of surgical shunt procedures and transjugular intrahepatic portosystemic shunt (TIPS), which are used to reduce portal hypertension.20
TABLE 43-11 Factors precipitating hepatic encephalopathy
| Factor | Mechanism |
|---|---|
| GI haemorrhage | Increase in ammonia in GI tract |
| Constipation | Increase in ammonia from bacterial action on faeces |
| Hypokalaemia | Potassium ions are needed by brain to metabolise ammonia |
| Hypovolaemia | Increase in blood ammonia by causing hepatic hypoxia; impairment of cerebral, hepatic and renal function because of decreased blood flow |
| Infection | Increase in catabolism, increase in cerebral sensitivity to toxins |
| Cerebral depressants (e.g. opioids) | Decrease in detoxification by liver, causing increase in cerebral depression |
| Metabolic alkalosis | Facilitation of transport of ammonia across blood–brain barrier, increase in renal production of ammonia |
| Paracentesis | Loss of sodium and potassium ions, decrease in blood volume |
| Dehydration | Potentiation of ammonia toxicity |
| Increased metabolism | Increase in workload of liver |
| Uraemia (renal failure) | Retention of nitrogenous metabolites |
GI, gastrointestinal.
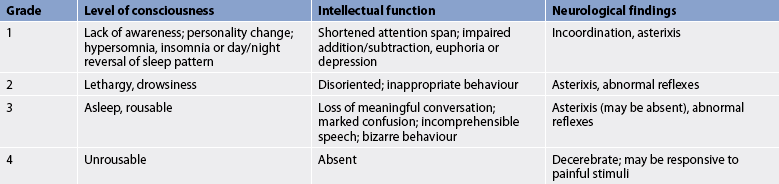
Clinical manifestations of encephalopathy are changes in neurological and mental responsiveness, ranging from sleep disturbances to deep coma. Changes may occur suddenly because of an increase in ammonia in response to bleeding varices, or gradually as blood ammonia levels slowly increase. A grading system is often used to classify the stages of hepatic encephalopathy (see Table 43-12). In the early stages (stages 0 and 1), manifestations include euphoria, depression, apathy, irritability, memory loss, confusion, yawning, drowsiness, insomnia and agitation. Later stages (stages 2 and 3) are characterised by slow and slurred speech, emotional lability, impaired judgement, hiccups, slow and deep respirations, hyperactive reflexes and a positive Babinski’s reflex. Clinical manifestations of impending coma (stage 4) include disorientation as to time, place or person.
A characteristic manifestation of hepatic encephalopathy is asterixis, or flapping tremors (liver flap). This may take several forms, the most common involving the arms and hands. When asked to hold the arms and hands stretched out, the patient is unable to hold this position and there will be a series of rapid flexion and extension movements of the hands. Other signs of asterixis are rhythmic movements of the legs, with dorsiflexion of the foot, and rhythmic movements in the face, with strong closure of the eyelids. Impairments in writing involve difficulty in moving the pen or pencil from left to right and apraxia (the inability to construct simple figures). Other signs include hyperventilation, hypothermia, and grimacing and grasping reflexes.
Fetor hepaticus—a musty, sweet odour of the patient’s breath—occurs in some patients with encephalopathy. This odour is from the accumulation of digestive by-products that the liver is unable to degrade.
Hepatorenal syndrome
Hepatorenal syndrome is a serious complication of cirrhosis. It is characterised by functional renal failure with advancing azotaemia, oliguria and intractable ascites. There is no structural abnormality of the kidneys. The aetiology is complex but the final common pathway is likely to be that portal hypertension along with liver decompensation results in splanchnic and systemic vasodilation and decreased arterial blood volume. As a result, renal vasoconstriction occurs and renal failure follows. This renal failure can be reversed by liver transplantation. In the patient with cirrhosis, hepatorenal syndrome frequently follows diuretic therapy, GI haemorrhage or paracentesis.21
DIAGNOSTIC STUDIES
In cirrhosis there are abnormalities in most of the liver function studies. Enzyme levels, including alkaline phosphatase, AST, ALT and gamma-glutamyltransferase (GGT), are initially elevated because of the release of these enzymes from damaged liver cells. However, in compensated or end-stage liver disease, AST and ALT levels may be normal. Protein metabolism tests show decreased total protein, decreased albumin, increased serum bilirubin and increased globulin levels. The liver does not synthesise gamma-globulins but does synthesise albumin. Gamma-globulins (antibodies) are produced by B lymphocytes. The globulin level often increases in cirrhosis and indicates increased synthesis or decreased removal. Fat metabolism abnormalities are reflected by decreased cholesterol levels. The prothrombin time is prolonged and bilirubin metabolism is altered (see hepatocellular jaundice in Table 43-1). Liver biopsy may be performed to identify liver cell changes and alterations in the lobular structure. Differential analysis of ascitic fluid may be helpful in establishing a diagnosis.
MULTIDISCIPLINARY CARE
Rest
Although there is no specific therapy for cirrhosis, certain measures can be taken to promote liver cell regeneration and prevent or treat complications (see Box 43-2). Rest is significant in reducing the metabolic demands of the liver and allowing recovery of liver cells. At various times during the progress of cirrhosis, the rest may have to take the form of complete bed rest.
BOX 43-2 Cirrhosis of the liver
MULTIDISCIPLINARY CARE