Chapter 61 NURSING ASSESSMENT: musculoskeletal system
1. Describe the gross anatomical and microscopic composition of bone.
2. Explain the classification system of joints and movements at synovial joints.
3. Describe the types and structure of muscle tissue.
4. Describe the functions of cartilage, muscles, ligaments, tendons, fascia and bursae.
5. Describe age-related changes in the musculoskeletal system and differences in assessment findings.
6. Identify the significant subjective and objective data related to the musculoskeletal system that should be obtained from a patient during assessment.
7. Describe the appropriate techniques used in the physical assessment of the musculoskeletal system.
8. Differentiate between normal and abnormal findings in a physical assessment of the musculoskeletal system.
9. Describe the purpose and significance of results and nursing responsibilities related to diagnostic studies of the musculoskeletal system.
Structures and functions of the musculoskeletal system
The unique structures of the musculoskeletal system allow human beings to complete complex movements in their interactions with the environment. The dexterity of the upper extremities enables an individual to perform complicated technical tasks, while stronger lower extremities allow mobility for varied activities. The musculoskeletal system is composed of voluntary muscle and five types of connective tissue: bones, cartilage, ligaments, tendons and fascia.1
Resilient bone and cartilage absorb energy from any impact, minimising the risk of injury to other body structures. However, this characteristic ability makes the musculoskeletal system itself particularly vulnerable to injury from external forces. Any damage to bone and related soft tissues can cause functional disruption for an individual. Deformity, alteration in body image, alteration in mobility, pain or permanent disability may result from musculoskeletal injury.
BONE
Function
The main functions of bone are support, protection of internal organs, voluntary movement, blood cell production and mineral storage.2 Bones provide the supporting framework that keeps the body from collapsing and they allow the body to bear weight. Bones also protect underlying vital organs and tissues. For example, the skull encloses the brain, the vertebrae surround the spinal cord, and the rib cage contains the lungs and heart. Bones serve as a point of attachment for muscles, which are connected to bones by tendons. Bones act as a lever for muscles, and movement occurs as a result of muscle contractions applied to these levers. Bones contain haematopoietic tissue for the production of red and white blood cells. Bones also serve as a site for storage of inorganic minerals, such as calcium and phosphorus.
Bone was previously thought to be a static, inert substance. It is now known that it is a dynamic tissue that continually changes form and composition. It contains both organic material (collagen) and inorganic material (calcium, phosphate). The internal and external growth and remodelling of bone are ongoing processes. Bone is classified according to structure as cortical (compact and dense) or cancellous (spongy).
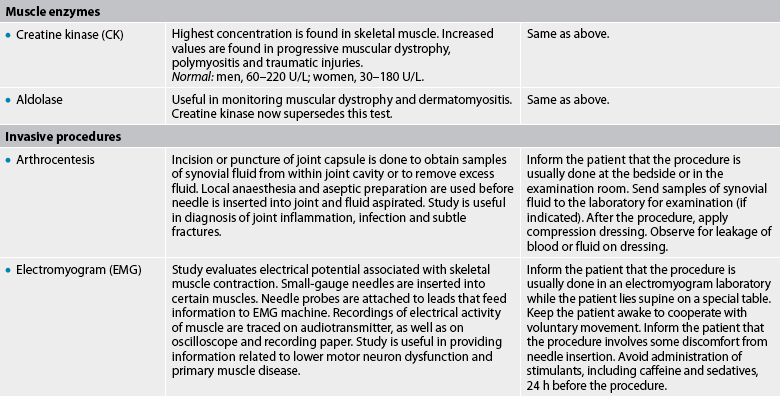
Microscopic structure
Cylindrical structural units (haversian systems) fit closely together in compact bone, creating a dense bone structure (see Fig 61-1, A). Within the systems, the haversian canals run parallel to the bone’s long axis and contain the blood vessels that travel to the bone’s interior from the external covering, the periosteum. Surrounding the haversian canals are concentric rings known as lamellae, which characterise mature bone. Smaller canals (canaliculi) extend from the haversian canals to the lacunae, where mature bone cells are embedded. Cancellous bone lacks the organised structure of cortical (compact) bone. The lamellae are not arranged in concentric rings but rather along the lines of maximum stress placed on the bone. Networks of bone tissue are filled with red or yellow marrow, and blood reaches the bone cells by passing through spaces in the marrow.
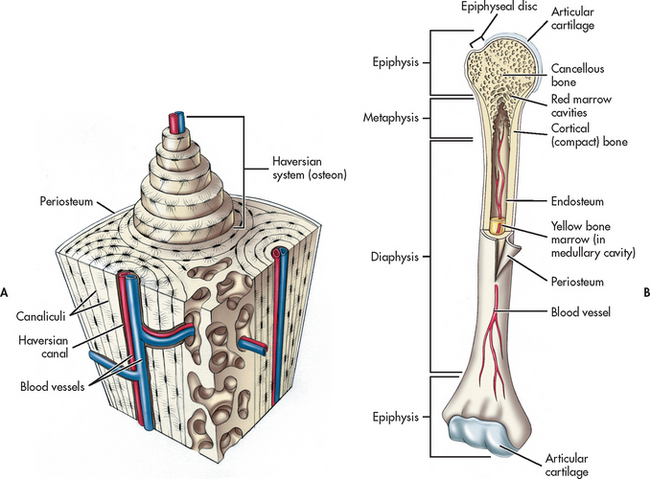
Figure 61-1 Bone structure. A, Cortical (compact) bone showing haversian system. B, Anatomy of a long bone (humerus).
There are three types of bone cells: osteoblasts, osteocytes and osteoclasts. Osteoblasts synthesise organic bone matrix (collagen) and are the basic bone-forming cells. Osteocytes are the mature bone cells. Osteoclasts participate in bone remodelling by assisting in the breakdown of bone tissue. Bone remodelling is the removal of old bone by osteoclasts (resorption) and the deposition of new bone by osteoblasts (ossification). The inner layer of bone is primarily made up of osteoblasts with a few osteoclasts.
Gross structure
The anatomical structure of bone is best represented by a typical long bone such as the humerus (see Fig 61-1, B). Each long bone consists of the epiphysis, the diaphysis and the metaphysis. The epiphysis, the widened area found at each end of a long bone, is composed primarily of cancellous bone. The wide epiphysis allows for greater weight distribution and provides stability for the joint. The epiphysis is also the location of muscle attachment. Articular cartilage covers the ends of the epiphysis to provide a smooth surface for joint movement. The diaphysis is the main shaft of the bone. It provides structural support and is composed of compact bone. The tubular structure of the diaphysis allows it to withstand bending and twisting forces more easily. The metaphysis is the flared area between the epiphysis and the diaphysis. Like the epiphysis, it is composed of cancellous bone. The epiphyseal plate, or growth zone, is the cartilaginous area between the epiphysis and the metaphysis. It actively produces bone to allow longitudinal growth in children. Injury to the epiphyseal plate in a growing child can lead to a shorter extremity that can cause significant functional problems. In the adult, the metaphysis and epiphysis become joined as this plate hardens to mature bone.
The periosteum is composed of fibrous connective tissue that covers the bone. Tiny blood vessels penetrate the periosteum to provide nutrition to the underlying bone. Musculotendinous fibres anchor to the outer layer of the periosteum. The inner layer of the periosteum is attached to the bone by bundles of collagen. No periosteum exists on the articular surfaces of long bones. The bone ends are covered by articular cartilage.
The medullary (marrow) cavity is in the centre of the diaphysis and contains either red or yellow bone marrow.3 In the growing child, red bone marrow is actively involved in haematopoiesis. In the adult, the medullary cavity of long bones contains yellow bone marrow, which is mainly adipose tissue. Yellow marrow is involved in haematopoiesis only in times of extra blood cell need. Blood cell production in the adult normally occurs in the red bone marrow of the skull, ribs, sternum, pelvis, vertebrae and shoulders.
Types
The skeleton consists of 206 bones, which are classified according to shape as long, short, flat or irregular.
• Long bones are characterised by a central shaft (diaphysis) and two widened ends (epiphyses) (see Fig 61-1, B). Examples include the femur, humerus and radius.
• Short bones are composed of cancellous bone covered by a thin layer of compact bone. Examples include the carpals in the hand and the tarsals in the foot.
• Flat bones have two layers of compact bone separated by a layer of cancellous bone. Examples include the ribs, skull, scapula and sternum. The spaces in the cancellous bone contain bone marrow.
• Irregular bones appear in a variety of shapes and sizes. Examples include the vertebrae, sacrum and mandible.
JOINTS
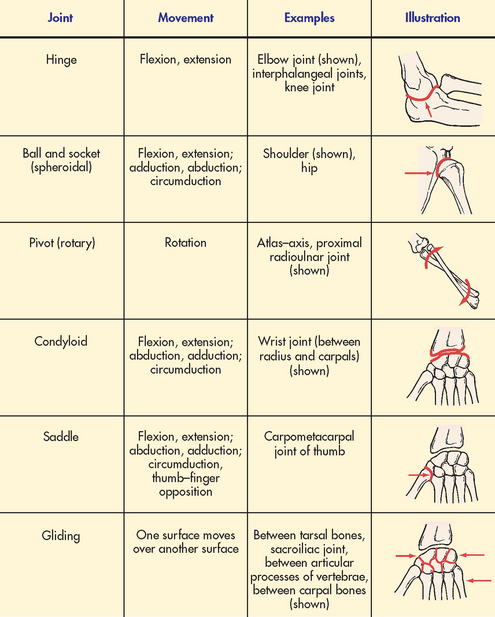
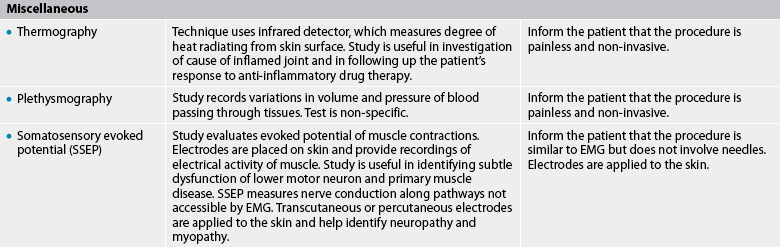
A joint (articulation) is a place where the ends of two bones are in proximity and move in relation to each other. Joints are classified according to the degree of movement that they allow (see Fig 61-2).
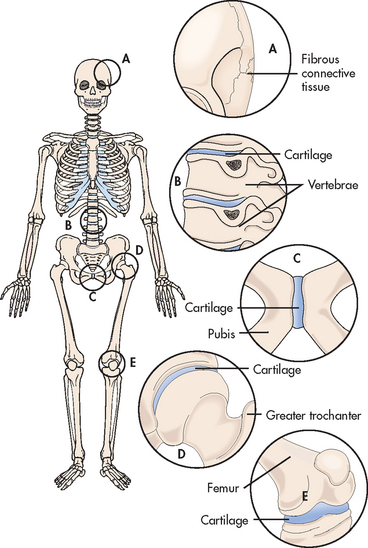
Figure 61-2 Classification of joints. A, B, and C, Synarthrotic (immovable) and amphiarthrotic (slightly movable) joints. D and E, Diarthrodial (freely movable) joints.
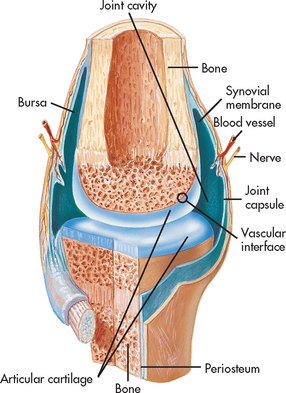
The most common joint is the freely movable diarthrodial (synovial) type. Each joint is enclosed in a capsule of fibrous connective tissue, which joins the two bones together to form a cavity (see Fig 61-3). The capsule is lined by a synovial membrane, which secretes a thick synovial fluid to lubricate the joint and reduce friction, allowing the opposing surfaces to slide freely over each other. The end of each bone is covered with articular (hyaline) cartilage. Supporting structures (e.g. ligaments and tendons) reinforce the joint capsule and provide limits to joint movement.4 Types of diarthrodial joints are shown in Figure 61-4.
CARTILAGE
Cartilage is a rigid connective tissue that serves as a support for soft tissue and provides the articular surface for joint movement. It protects underlying tissues. The cartilage in the epiphyseal plate is also involved in the growth of long bones before physical maturity is reached. Because articular cartilage is relatively avascular, it must receive nourishment by the diffusion of material from the synovial fluid. The lack of a direct blood supply contributes to the slow metabolism of cartilage cells and explains why cartilage tissue heals slowly.
The three types of cartilage tissue are hyaline, elastic and fibrous. Hyaline cartilage, the most common, contains a moderate amount of collagen fibre. It is found in the trachea, bronchi, nose, epiphyseal plate and articular surfaces of bones. Elastic cartilage, which contains both collagen and elastic fibres, is more flexible than hyaline cartilage. It is found in the ear, epiglottis and larynx. Fibrous cartilage (fibrocartilage) consists mostly of collagen fibres and is a tough tissue that often functions as a shock absorber. It is found between the vertebral discs and also forms a protective cushion between the bones of the pelvic girdle, knee and shoulder.
MUSCLE
Types
The three types of muscle tissue are cardiac (striated, involuntary), smooth (non-striated, involuntary) and skeletal (striated, voluntary) muscle. Cardiac muscle is found in the heart. Its spontaneous contractions propel blood through the circulatory system. Smooth muscle occurs in the walls of hollow structures, such as airways, arteries, gastrointestinal (GI) tract, urinary bladder and uterus. Smooth muscle contraction is modulated by neuronal and hormonal influences. Skeletal muscle, which requires neuronal stimulation for contraction, accounts for about half of a human being’s body weight. It is the focus of the following discussion.
Structure
The structural unit of muscle is the muscle cell or muscle fibre, which is highly specialised for contraction. Skeletal muscle fibres are long, multinucleated cylinders that contain many mitochondria to support their high metabolic activity. Muscle fibres are composed of myofibrils, which in turn are made up of protein contractile filaments. The sarcomere is the contractile unit of the myofibrils.5 Each sarcomere consists of myosin (thick) filaments and actin (thin) filaments. The arrangement of the thin and thick filaments accounts for the characteristic banding of muscle when it is seen under a microscope. Muscle contraction occurs as thick and thin filaments slide past each other, causing the sarcomeres to shorten.
Contractions
Skeletal muscle contractions allow posture maintenance, movement and facial expressions. Isometric contractions increase the tension within a muscle but do not produce movement. Repeated isometric contractions make muscles grow larger and stronger. Isotonic contractions shorten a muscle to produce movement. Most contractions are a combination of tension generation (isometric) and shortening (isotonic). Muscle is normally in a state of partial contraction, known as normal muscle tone, the tension between the point of origin and insertion of a muscle.5 Muscular atrophy (decrease in size) occurs with the absence of contraction that results from immobility, whereas increased muscular activity leads to hypertrophy (increase in size).
Skeletal muscle fibres are divided into two groups based on the type of activity they demonstrate. Slow-twitch muscle fibres support prolonged muscle activity, such as marathon running. Because they also support the body against gravity, they assist in maintaining posture. Fast-twitch muscle fibres are used for rapid muscle contraction required for activities such as blinking the eye, jumping or sprinting and tire more readily than slow-twitch muscle fibres.
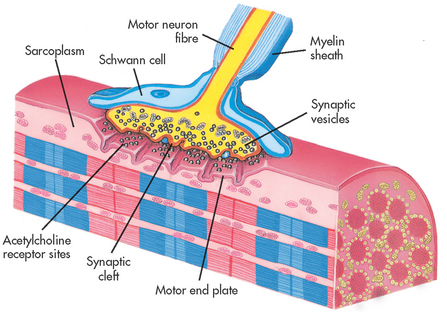
Neuromuscular junction
Skeletal muscle fibres require a nerve impulse in order to contract. A nerve fibre and the skeletal muscle fibres it stimulates are called a motor end plate. The junction between the axon of the nerve cell and the adjacent muscle cell is called the myoneural or neuromuscular junction (see Fig 61-5).
Acetylcholine is released from the motor end plate of the neuron and diffuses across the neuromuscular junction to bind with receptors on the muscle fibre. This stimulates the sarcoplasmic reticulum to release calcium ions into the cytoplasm, which triggers contraction in the myofibrils. A condition known as tetany can occur in the presence of decreased calcium levels.
Energy source
The direct energy source for muscle fibre contractions is adenosine triphosphate (ATP), which is synthesised by cellular oxidative metabolism in numerous mitochondria located close to the myofibrils. It is rapidly depleted through conversion to adenosine diphosphate (ADP) and must be rephosphorylated. Phosphocreatine provides a rapid source for the resynthesis of ATP but it is, in turn, converted to creatine and must be recharged. Glycolysis can serve as a source of ATP when the oxygen supply is inadequate for the metabolic needs of the muscle tissue. Glucose is broken down to pyruvic acid, which can be further converted to lactic acid to make more oxygen available. An accumulation of lactic acid in tissues leads to fatigue and pain—for example, during or following prolonged or strenuous unaccustomed exercise.
LIGAMENTS AND TENDONS
Ligaments and tendons are both composed of dense, fibrous connective tissue that contains bundles of closely packed collagen fibres arranged in the same plane for additional strength. Tendons attach muscles to bones as an extension of the muscle sheath that adheres to the periosteum. Ligaments connect bones to bones (e.g. tibia to femur at knee joint). They have higher elastic content than tendons.6 Ligaments provide stability while permitting controlled movement at the joint. Ligaments and tendons have a relatively poor blood supply, usually making tissue repair a slow process after injury. For example, the stretching or tearing of ligaments that occurs with a sprain may require a long time to mend.
FASCIA
Gerontological considerations: effects of ageing on the musculoskeletal system
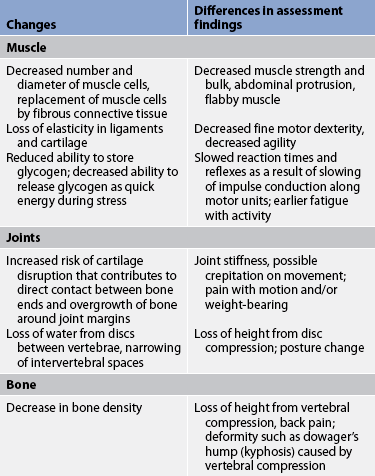
Many of the functional problems experienced by the ageing adult are related to changes of the musculoskeletal system.7 Although some changes begin in early adulthood, obvious signs of musculoskeletal impairment may not appear until later adult years. Alterations may affect the older adult’s ability to complete self-care tasks and pursue other customary activities. Effects of musculoskeletal changes may range from mild discomfort and decreased ability to perform activities of daily living to severe, chronic pain and immobility. The risk of falls also increases in the older adult. Hospital data indicate that 49% of unintentional fall injuries are reported as occurring in older adults.8
The bone remodelling process is altered in the ageing adult. Increased bone resorption and decreased bone formation cause a loss of bone density, contributing to the development of osteopenia and osteoporosis (see Ch 64). Muscle mass and strength also decrease with age. Almost 30% of muscle mass is lost by the eighth decade of life.9 A loss of motor neurons can cause additional problems with skeletal muscle movement. Tendons and ligaments become less flexible and movement becomes more rigid. Joints in the ageing adult are also more likely to be affected by osteoarthritis (see Ch 64).
In addition to the usual musculoskeletal assessment with a particular emphasis on exercise practices, the nurse should determine the impact of age-related changes of the musculoskeletal system on the functional status of the older adult, including those that place the person at an increased risk of falling (see Table 61-1). Functional limitations that are accepted by older adults as a normal part of ageing, and risk of falls, can often be halted or reversed with appropriate preventative strategies.
Diseases such as osteoarthritis and osteoporosis are not the normal consequences of ageing. The nurse should carefully differentiate between expected changes and the effects of disease in the ageing adult. Symptoms of disease can be treated in many cases, helping the older adult to return to a higher functional level. Age-related changes in the musculoskeletal system and differences in assessment findings are presented in Table 61-1.
Fascia refers to layers of connective tissue with intermeshed fibres that can withstand limited stretching. Superficial fascia lies immediately under the skin. Deep fascia is a dense, fibrous tissue that surrounds the muscle bundles, nerves and blood vessels. It also encloses individual muscles, allowing them to act independently and to glide over each other during contraction. In addition, fascia provides strength to muscle tissues.
BURSAE
Bursae are small sacs of connective tissue lined with synovial membrane and containing synovial fluid. They are typically located at bony prominences or joints to relieve pressure and prevent friction between moving parts. For example, bursae are found between the patella and the skin (prepatellar bursa), between the olecranon process of the elbow and the skin (olecranon bursa), between the head of the humerus and the acromion process of the scapula (subacromial bursa), and between the greater trochanter of the proximal femur and the skin (trochanteric bursa). Bursitis is an inflammation of a bursa.
Assessment of the musculoskeletal system
Correct diagnosis of any complaint depends on a complete patient history and thorough physical examination. Musculoskeletal assessment can focus on a specific body part or it can be done as part of a general physical examination or as an examination in itself. The nurse uses the patient’s complaint as a guide in selecting all or part of the components of the musculoskeletal history and physical examination. For example, accidents may result in multisystem trauma. Because serious or life-threatening injuries do not usually involve the musculoskeletal system, critical information about the patient’s condition is obtained to support immediate treatment, and a complete assessment of the musculoskeletal system may be deferred until the patient is stabilised.
The most common symptoms of musculoskeletal impairment include pain, weakness, deformity, limitation of movement, stiffness and joint crepitation.10 Information should also be sought about changes in sensation or in the size of a muscle.
SUBJECTIVE DATA
Important health information
Appropriate questions to ask during a musculoskeletal assessment are included in Table 61-2.
TABLE 61-2 Musculoskeletal system
• Describe your usual daily activities.
• Do you experience any difficulties performing these activities?* Describe what you do if you experience difficulty in dressing, preparing meals and feeding yourself, performing basic hygiene or maintaining your home.
• Do you use any mechanical assistive devices?*
• Do you have to lift heavy objects? Describe any specialised equipment you use or wear when you work or exercise that helps protect you from injury.
• What other safety precautions do you take?
• Do you take any drugs or herbal products to manage your musculoskeletal problem? If so, what is the name of the drug(s) and what are the expected effects?
• When did you have your last tetanus and polio immunisations? When were you last tested for tuberculosis?
• What dietary supplements do you take? (Ask specifically about calcium, vitamin D supplements and herbal products.)
• What is your weight? Describe any recent weight loss or gain. Were your musculoskeletal symptoms affected by the change in your weight?*
• Does your musculoskeletal problem make it difficult for you to reach the toilet in time?*
• Do you need any assistive devices or equipment to achieve satisfactory toileting?*
• Do you experience constipation related to decreased mobility or to drugs taken for your musculoskeletal problem?*
• Do you require assistance in completing your usual daily activities because of a musculoskeletal problem?*
• Describe your usual exercise pattern. Do you experience musculoskeletal symptoms before, during or after exercising?*
• Are you able to move all your joints comfortably through full range of motion? Describe any limitations in mobility.
• Do you use any prosthetic or orthotic devices?*
• Do you experience any difficulty sleeping because of a musculoskeletal problem?* Do you require frequent position changes at night?*
• Do you wake up at night because of musculoskeletal pain?*
• Describe any musculoskeletal pain you experience. How do you manage your pain? (Ask specifically about adjunctive therapies, such as heat and cold, or alternative therapies, such as acupuncture.)
• Describe how changes in your musculoskeletal system (posture, walking, muscle strength) and decreased ability to do certain things have affected how you feel about yourself. How have these changes affected your lifestyle?
• Describe how family members or others assist you with your musculoskeletal problem.
• Describe the effect of your musculoskeletal problem on your work and on your social relationships.
• Describe how you deal with problems such as pain or immobility that have resulted from your musculoskeletal problem.
Past health history
Because certain illnesses are known to affect the musculoskeletal system either directly or indirectly, the nurse should question the patient carefully about past medical problems. These include tuberculosis, poliomyelitis, diabetes mellitus, parathyroid problems, haemophilia, rickets, scurvy, soft-tissue infection and neuromuscular disabilities. In addition, past or developing musculoskeletal problems can affect the patient’s overall health. Trauma to the musculoskeletal system is a common reason for seeking medical assistance. Questions should also focus on symptoms of arthritic and connective tissue diseases (e.g. gout, psoriatic arthritis, systemic lupus erythematosus), osteomalacia, osteomyelitis and fungal infection of the bones or joints. The patient should be asked about possible sources of a secondary bacterial infection, such as the ears, tonsils, teeth, sinuses or genitourinary tract. These infections can enter the bones, resulting in osteomyelitis. A detailed account of the course and treatment of any of these problems should be obtained.
Medications
The nurse needs to carefully question the patient about prescription and over-the-counter drugs, herbal products and nutritional supplements. Detailed information should be obtained about each treatment, including its name, the dose and frequency, the length of time it was taken, its effects and any possible side effects. Specific inquiry should be made about skeletal muscle relaxants, opioids, non-steroidal anti-inflammatory drugs, and systemic and topical corticosteroids. The patient who has taken anti-inflammatory drugs should be questioned about gastrointestinal discomfort or signs of bleeding.
In addition to drugs taken for treatment of a musculoskeletal problem, the patient should be questioned about drugs that can have detrimental effects on this system. These drugs and their potential side effects include antiseizure drugs (osteomalacia), phenothiazines (gait disturbances), corticosteroids (avascular necrosis, decreased bone and muscle mass) and potassium-depleting diuretics (muscle cramps and weakness). Women should be questioned about their menstrual history. Episodes of amenorrhoea can contribute to early development of osteoporosis. Questions about the use of hormone replacement therapy and calcium and vitamin D supplements are important for postmenopausal women. Older men and women should be asked about any known family history of osteoporosis.
Surgery or other treatment
Information should be obtained about past treatment or hospitalisations for musculoskeletal problems. The nurse must carefully document the reason for hospitalisation, the date and duration and the treatment. Details of emergency treatment for musculoskeletal injuries should also be sought. Specific information should be obtained regarding any surgical procedure, the postoperative course and any complications. If the patient experienced a period of prolonged immobilisation, the development of osteoporosis and muscle atrophy should be considered.
Functional health patterns
The use of functional health patterns assists the nurse in organising the data and formulating diagnoses based on information collected about the musculoskeletal system. Table 61-2 summarises specific questions to ask in relation to functional health patterns.
Health perception–health management pattern
The nurse should ask about the patient’s health practices related to the musculoskeletal system, such as maintenance of a normal body weight, avoidance of excessive stress on muscles and joints, and the use of proper body mechanics when lifting objects.11 The patient should be specifically questioned about tetanus and polio immunisations and tuberculin skin test status.
Food or contact allergies have little direct relationship to musculoskeletal problems but the general malaise often associated with allergic reactions may manifest in musculoskeletal stiffness and lethargy. Allergic reactions to drugs used to treat musculoskeletal problems can be significant if they interfere with therapy.
The patient who is a good historian will be able to recount numerous minor and major injuries of the musculoskeletal system. Information should be recorded chronologically and should include the following:
1. mechanism of the injury (e.g. twist, crush, stretch)
2. circumstances related to the injury
A family history should be obtained related to rheumatoid arthritis, sickle cell disease, osteoarthritis, gout, osteoporosis and scoliosis because there is a genetic predisposition for these disorders.
Safety practices can affect the patient’s predisposition for certain injuries and illnesses. Therefore, the nurse should ask the patient about safety practices as they relate to the work environment, recreation and exercise. For example, if the patient works at a computer for long periods of time, the nurse should ask about ergonomic adaptations in the office that decrease the risk of carpal tunnel syndrome or low back pain. Identifying problems in this area will direct the plan for patient teaching.
Nutritional–metabolic pattern
The patient’s description of a typical day’s diet provides clues to areas of nutritional concern that can affect the musculoskeletal system. Adequate amounts of vitamins C and D, calcium and protein are essential for a healthy, intact musculoskeletal system. Abnormal nutritional patterns or lack of skin exposure to sunlight can predispose individuals to problems such as osteomalacia, osteoporosis and rickets. In addition, maintenance of normal weight is an important nutritional goal. Obesity places additional stress on weight-bearing joints, such as the knees, hips and spine, and predisposes individuals to ligamentous instability.
Elimination pattern
Questions about the patient’s mobility may reveal difficulty with ambulating to the toilet. The patient should be asked whether they need an assistive device, such as an elevated toilet seat or a grab bar, to accomplish toileting. Decreased mobility secondary to a musculoskeletal problem can lead to constipation. In addition, musculoskeletal problems can contribute to bowel or bladder incontinence.
Activity–exercise pattern
The nurse should obtain a detailed account of the type, duration and frequency of exercise and recreational activities. Daily, weekend and seasonal patterns should be compared because occasional or sporadic exercise can be more problematic than regular exercise. Many musculoskeletal problems can affect the patient’s activity–exercise pattern. The nurse should question the patient about limitations of movement, pain, weakness, clumsiness, crepitus or any change in the bones or joints that interferes with daily activities.
Extremes of activity related to occupation can also affect the musculoskeletal system. A sedentary occupation can negatively impact on muscle flexibility and strength. Jobs that require extreme effort through heavy lifting or pushing can lead to damage of joints and supporting structures. The nurse should question the patient specifically about work-related injuries to the musculoskeletal system, including treatment and time lost from work.
Sleep–rest pattern
The discomfort caused by musculoskeletal disorders can interfere with a normal sleep pattern. The patient should be questioned about possible alterations in sleep patterns. If the patient describes sleep interference related to a musculoskeletal problem, the nurse should inquire about the type of bedding and pillows used, bedtime routine, sleeping partner and sleeping positions.
Cognitive–perceptual pattern
Any pain that the patient experiences as a result of a musculoskeletal problem should be fully explored and documented. To provide a baseline for later reassessment, the patient should be asked to describe the intensity of the pain on a scale from 1 to 10 (where 0 = no pain and 10 = the most severe pain imaginable). Reassessments over time will assist in determining the effectiveness of any treatment plan. The patient should also be questioned about measures used at home for pain management and about related problems such as joint swelling or muscle weakness. Where there is a history of chronic pain, a more detailed assessment using a tool such as the McGill Pain Inventory may be indicated. (Pain is discussed in Ch 8.)
Self-perception–self-concept pattern
Many chronic musculoskeletal problems lead to deformities that can have a serious negative impact on the patient’s body image and sense of personal worth. The nurse should address the patient’s feelings about each of these changes.
Role–relationship pattern
Impaired mobility and chronic pain from musculoskeletal problems can negatively affect the patient’s ability to perform the roles of spouse, parent or employee. The ability to pursue and maintain meaningful social and personal relationships can also be affected by musculoskeletal problems. The nurse should carefully question the patient about role performance and relationships.
If the patient lives alone, the current musculoskeletal problem and its rehabilitation may make it difficult or impossible to continue this arrangement. The degree of assistance available from family, friends and organised carers should be determined.
Sexuality–reproductive pattern
The pain of musculoskeletal problems can greatly affect the patient’s ability to obtain sexual satisfaction. The nurse should explore this area sensitively, helping the patient to feel comfortable in discussing any sexual problems related to pain, movement and positioning.
OBJECTIVE DATA
Physical examination
Examination involves observation, palpation, motion and muscular assessment.10 Although a general overview will be conducted, data obtained in a careful health history will guide the nurse in choosing areas in which to concentrate the local examination. Specific measurements may be taken as indicated by the local examination.
Inspection
Inspection begins during the nurse’s initial contact with the patient. The patient’s use of an assistive device, such as a walking frame or cane, should be noted. The nurse also observes the patient’s general body build, muscle configuration and symmetry of joint movement. If the patient is able to move independently, the nurse should assess posture and gait by watching the patient walk, stand and sit. Musculoskeletal and neurological problems can result in changes from a normal gait.
A systematic inspection is performed starting at the head and neck and proceeding to the upper extremities, the lower extremities and the trunk. A regular use of a systematic approach is important to avoid missing important aspects of the examination. The skin is inspected for general colour, scars or other overt signs of previous injury or surgery. Any swelling, deformity, nodules or masses and discrepancies in limb length or muscle size should be noted. The patient’s opposite body part is used for comparison when an abnormality is suspected.
Palpation
Any area that has aroused concern because of a subjective complaint or appears abnormal on inspection should be carefully palpated. As with inspection, palpation usually proceeds from head to toe to examine the neck, shoulders, elbows, wrists, hands, back, hips, knees, ankles and feet. Superficial and deep palpation are usually performed consecutively.
The nurse’s hands should be warm to prevent muscle spasm, which can interfere with the identification of essential landmarks or soft-tissue structures. Palpation of both muscles and joints allows for evaluation of skin temperature, local tenderness, swelling and crepitation. The nurse must establish the relationship of adjacent structures and evaluate the general contour, abnormal prominences and local landmarks.
Motion
When assessing the patient’s joint mobility, the nurse must carefully evaluate both passive and active range of motion; measurements should be similar for both manoeuvres. Active range of motion means the patient takes their own joints through all movements without assistance. Passive range of motion occurs when someone else moves the patient’s joints without their participation. The nurse should be cautious in performing passive range of motion because of the risk of injury to underlying structures. Manipulation must cease immediately if pain or resistance is encountered. If deficits in active or passive range of motion are noted, the nurse must assess functional range of motion to determine whether performance of activities of daily living has been affected by joint changes. This is done by asking the patient whether activities such as eating and bathing must be performed with assistance or cannot be done at all.
Range of motion is most accurately assessed with a goniometer, which measures the angle of the joint (see Fig 61-6). Specific degrees of range of motion of all joints are usually not measured unless a musculoskeletal problem has been identified. A less exact but valuable assessment method is to compare the range of motion of one extremity with the range of motion on the opposite side. The most common movements that occur at the synovial joints are described in Table 61-3.
TABLE 61-3 Movement at synovial joints
| Movement | Description |
|---|---|
| Abduction | Movement of part away from midline of body |
| Adduction | Movement of part towards midline of body |
| Circumduction | Combination of flexion, extension, abduction and adduction resulting in circular motion of a body part |
| Eversion | Turning of sole outwards away from midline of body |
| Extension | Straightening of joint that increases angle between two bones |
| External rotation | Movement along longitudinal axis away from midline of body |
| Flexion | Bending of joint as a result of muscle contraction that results in decreased angle between two bones |
| Hyperextension | Extension in which angle exceeds 180° |
| Internal rotation | Movement along longitudinal axis towards midline of body |
| Inversion | Turning of sole inwards towards midline of body |
| Pronation | Turning of palm downwards |
| Supination | Turning of palm upwards |
Muscle strength testing
The nurse grades the strength of individual muscles or groups of muscles during contraction as described in Table 61-4. The patient should be instructed to apply resistance to the force exerted by the nurse—for example, the nurse tries to pull the patient’s bent arm down while the patient tries to raise it. If there is involuntary increased or abnormal resistance, excessive force should not be used during the test. Muscle strength should also be compared with the strength of the opposite extremity. Subtle variations in muscle strength may be noted when comparing the patient’s dominant side with the non-dominant side.
TABLE 61-4 Muscle strength scale
| 0 | No detection of muscular contraction |
|---|---|
| 1 | A barely detectable flicker or trace of contraction with observation or palpation |
| 2 | Active movement of body part with elimination of gravity |
| 3 | Active movement against gravity only and not against resistance |
| 4 | Active movement against gravity and some resistance |
| 5 | Active movement against full resistance without evident fatigue (normal muscle strength) |
Measurement
When length discrepancies or subjective problems are noted, the nurse will often obtain limb length and circumferential muscle mass measurements. For example, leg length should be measured when gait disorders are observed. The affected limb is measured between two bony prominences and compared with the similar measurement of the opposite extremity. Muscle mass is measured circumferentially at the largest area of the muscle. When recording measurements, the nurse should document the exact location at which the measurements were obtained (e.g. the quadriceps muscle is measured 15 cm above the patella). This informs the next examiner of the exact area to be measured and ensures consistency during reassessment.
Other
Assessment of reflexes is discussed in Chapter 55. Box 61-1 is an example of how to record a normal physical assessment of the musculoskeletal system. Common abnormal assessment findings of the musculoskeletal system are presented in Table 61-5.
TABLE 61-5 Musculoskeletal system
COMMON ASSESSMENT ABNORMALITIES
| Finding | Description | Possible aetiology and significance |
|---|---|---|
| Ankylosis | Scarring within a joint leading to stiffness or fixation | Chronic joint inflammation |
| Atrophy | Wasting of muscle, characterised by decreased circumference and flabby appearance leading to decreased function and tone | Muscle denervation, contracture, prolonged disuse as a result of immobilisation |
| Contracture | Resistance of movement of muscle or joint as a result of fibrosis of supporting soft tissues | Shortening of muscle or ligaments, tightness of soft tissue, incorrect positioning of immobilised extremity |
| Crepitation (crepitus) | Crackling sound or grating sensation as a result of friction or broken bone or cartilage bits in joint | Fracture, dislocation, chronic inflammation, osteoarthritis |
| Effusion | Fluid in joint possibly with swelling and pain | Trauma, especially to knees; inflammation |
| Ganglion | Small fluid-filled synovial cyst usually on dorsal surface of wrist or foot | Degeneration of connective tissue close to tendons and joints leading to formation of small cysts |
| Hypertrophy | Increase in size of muscle as a result of enlargement of existing cells | Exercise or other increased stimulation, increased androgens |
| Kyphosis (dowager’s hump) | Anteroposterior or forward bending of thoracic spine with convexity of curve in posterior direction | Poor posture, tuberculosis, arthritis, osteoporosis, growth disturbance of vertebral epiphyses |
| Lordosis | Lumbar spinal deformity resulting in anteroposterior curvature with concavity in posterior direction | Secondary to other spinal deformities, muscular dystrophy, obesity, flexion contracture of hip, congenital dislocation of hip |
| Pes planus | Flatfoot | Congenital condition, muscle paralysis, mild cerebral palsy, early muscular dystrophy |
| Scoliosis | Deformity resulting in lateral curvature of thoracic spine (see Fig 61-7) | Idiopathic or congenital condition, fracture or dislocation, osteomalacia |
| Subluxation | Partial dislocation of joint | Instability of joint capsule and supporting ligaments (e.g. from trauma, arthritis) |
| Valgus (bow legs) | Angulation of bone away from midline | Alteration in gait, pain, arthritis |
| Varus (knock-knees) | Angulation of bone towards midline | Alteration in gait, pain, arthritis |
Scoliosis is a lateral S-shaped curvature of the thoracic and lumbar spine.11 Unequal shoulder and scapula height is usually noted (see Fig 61-7). If the deformity is greater than 45°, lung and cardiac function is generally impaired.
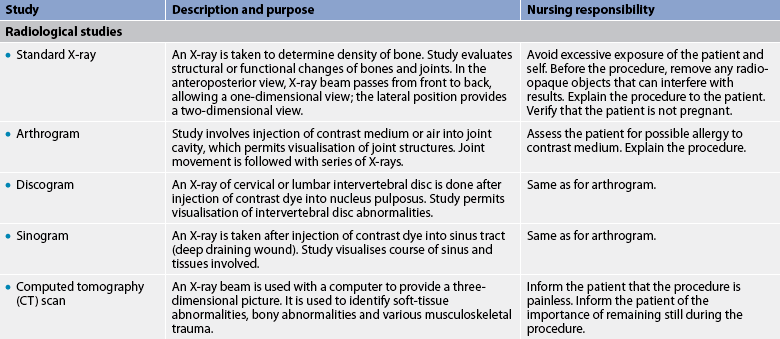
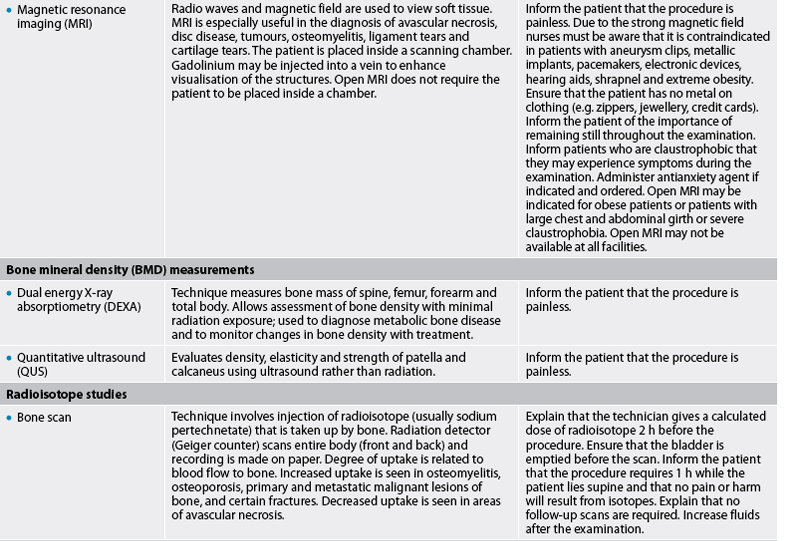
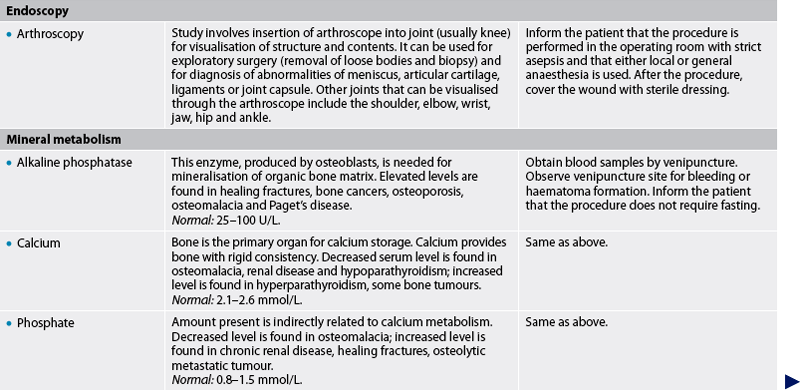
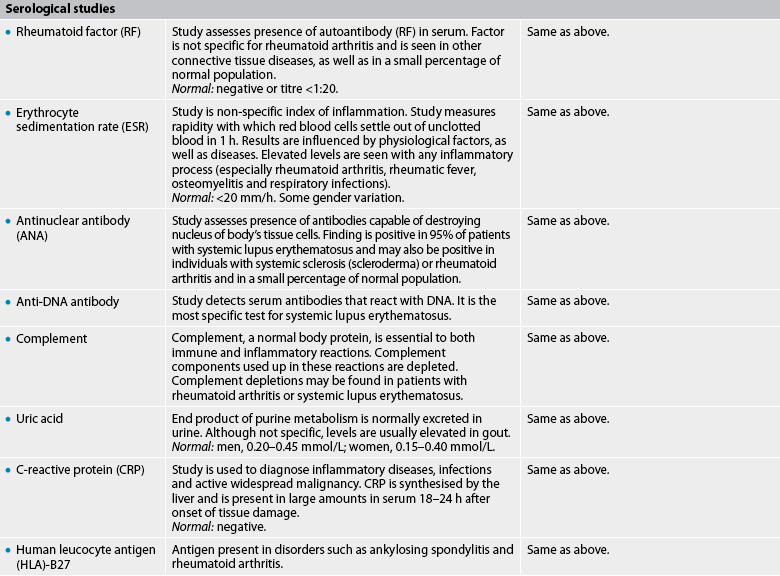
Diagnostic studies of the musculoskeletal system
Diagnostic studies provide important objective data that aid the nurse in monitoring the patient’s condition and planning appropriate interventions. Table 61-6 contains diagnostic studies common to the musculoskeletal system. Magnetic resonance imaging (MRI) has revolutionised diagnosis of musculoskeletal system disorders.12 Tests must be chosen carefully to enhance or clarify information gained from the patient’s history and physical examination. Common diagnostic tests are X-ray, MRI, arthroscopy and measurements of blood chemistry for specific factors related to disease processes of the musculoskeletal system.
X-RAY
The X-ray is the most common diagnostic study used to assess musculoskeletal problems and to monitor the effectiveness of treatment. Because bones are denser than other tissues, X-rays do not penetrate them. Dense areas show as white on the standard X-ray. X-rays provide information about bone deformity, joint congruity, bone density and calcification in soft tissue. Fracture diagnosis and management are the primary indications for X-ray but it is also useful in the evaluation of hereditary, developmental, infectious, inflammatory, neoplastic, metabolic and degenerative disorders.
The anteroposterior and lateral views are the most commonly used standard X-ray perspectives. Additional views in combination with other studies can aid in differential diagnosis. More specific radiological investigations are described in Table 61-6.
MAGNETIC RESONANCE IMAGING
MRI is a diagnostic study that shows the hydrogen density of tissues within the body. The body is composed primarily of hydrogen, and hydrogen possesses magnetic properties that make it appropriate as the basis for MRI. In MRI, radio waves and magnetic fields are used to construct images of soft tissue and bone. The study is particularly advantageous in identifying soft-tissue disorders, including cartilage or ligament tears and herniated discs, but it can also be helpful in diagnosing bone disorders, such as avascular necrosis, tumours and multiple myeloma. An MRI scanner works by creating a very strong magnetic field, so the nurse must make sure that the patient has no metal on their clothing or any implants that could be affected (e.g. pacemaker).
ARTHROSCOPY
A small fibreoptic tube called an arthroscope is used to examine the interior of a joint cavity in a procedure known as arthroscopy. Arthroscopy is performed under sterile conditions. After anaesthesia has been administered, a large-bore needle is inserted into the joint and the joint is distended with fluid or air (see Fig 61-8). When the arthroscope is inserted, the surgeon is able to perform extensive, accurate visualisation of the joint cavity.
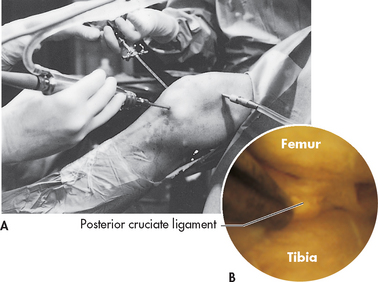
Figure 61-8 Arthroscopy of a knee. A, Insertion of a fibreoptic light source into the joint. B, Internal view of the joint.
Photographs or videotapes can be made through the scope and a biopsy of the synovium or cartilage can be obtained. Torn tissue can be repaired through arthroscopic surgery, eliminating the need for a larger incision and greatly decreasing the recovery time. Typically performed as an outpatient or day procedure, arthroscopy is a highly cost-effective diagnostic test that is usually done on an ambulatory basis.
ARTHROCENTESIS AND SYNOVIAL FLUID ANALYSIS
An arthrocentesis or joint aspiration is usually performed for a synovial fluid analysis. It may also be used to instil medications for the patient with septic arthritis or to remove fluid from joints to relieve pain. After the skin has been cleaned, a local anaesthetic is instilled. An 18-gauge or larger needle is inserted into the joint and fluid is withdrawn. The appropriate sterile container should be readily available to receive the aspirated fluid, which must be transported immediately to the laboratory. The fluid will be examined grossly for volume, colour, clarity, viscosity and mucin clot formation. Normal synovial fluid is transparent and colourless or straw-coloured. It should be scant in amount and of low viscosity. Fluid from an infected joint may be purulent and thick or grey and thin. In gout the fluid may be whitish yellow. Blood may be aspirated if there is haemarthrosis because of injury or a bleeding disorder. The mucin clot test indicates the character of the protein portion of the synovial fluid. Normally a white, rope-like mucin clot is formed. In the presence of an inflammatory process, the clot breaks apart easily and fragments. The fluid is examined grossly for floating fat globules, which indicate bone injury.
The fluid is examined microscopically for cell count and identification. The normal white blood cell (WBC) count is less than 0.2 × 109/L, with fewer than 25% neutrophils and no bacteria. Infection would be suspected if the WBC count reveals more than 25 × 109/L and more than 25% polymorphonuclear cells. Protein content is elevated and glucose is considerably decreased in septic arthritis. The presence of uric acid crystals suggests a diagnosis of gout. A Gram stain and culture may also be done of the aspirated fluid.
MUSCLE ENZYMES
Some tissue cells contain characteristic enzymes that enter the blood only when the cells to which they are confined are damaged or destroyed. The presence in the serum (blood) of significant quantities of these enzymes indicates the probable site of tissue damage. Muscle enzymes are released from injured or dead muscle cells (see Table 61-6). Determinations of muscle enzyme values are used to distinguish between muscle weakness that is due to nerve innervation problems and dystrophic disease of the muscle itself. Aldolase is an enzyme found in heart and skeletal muscle; if it is found in large quantities in the blood, it may be indicative of muscular dystrophy. Creatine kinase, another enzyme released by both damaged cardiac and skeletal muscle, provides information about acute muscular damage (see Ch 33 for information about damage to the heart muscle). Damage to muscles can also cause release of myoglobin.5 Myoglobin is excreted from the body via the urine (called myoglobinuria or rhabdomyolysis) and causes brown pigmentation. Myoglobin is toxic to the tubules of the kidney and can cause acute kidney injury (see Ch 46).
SEROLOGICAL STUDIES
Approximately 80% of people with rheumatoid arthritis and related diseases have an autoantibody known as rheumatoid factor (RF) in their serum. RF is an autoantibody directed against the immunoglobulin IgG. RF titres are higher during periods of increased disease activity. Elevated erythrocyte sedimentation rate and C-reactive protein are non-specific indicators of active inflammation (see Table 61-6).
1. The bone cells that function in the formation of bone tissue are called:
2. While performing passive range of motion for a patient, the nurse puts a hinge joint through the movements of:
3. The nurse teaches a patient with a leg immobilised in traction to prevent muscle atrophy in the affected leg by performing:
4. A patient with bursitis of the shoulder asks the nurse what the bursa does. The nurse’s response is based on the knowledge that bursae:
5. The decreased agility found during assessment of the older adult is caused by the age-related change of:
6. While obtaining subjective assessment data related to the musculoskeletal system, it is particularly important for the nurse to ask about family history in the patient with:
7. When grading muscle strength, the nurse records a score of 2, indicating:
8. A normal assessment finding of the musculoskeletal system is:
9. A patient is scheduled for an electromyogram. The nurse explains that this diagnostic test involves:
1 Roberts D. The musculoskeletal system. In Craven H, ed.: Core curriculum for medical-surgical nursing, 4th edn., Pitman, NJ: Academy of Medical-Surgical Nurses, 2009.
2 Altizer L. Anatomy and physiology. NAON: core curriculum for orthopaedic nursing. 6th edn. Boston: Pearson Custom Publishing; 2007.
3 Thibodeau GA, Patton KT. Structure and function of the human body, 13th edn. St Louis: Mosby, 2008.
4 Brinker M, et al. Basic science and injury of muscle, tendon, and ligament. In DeLee J, Drez D, Miller M, eds.: DeLee and Drez’s orthopaedic sports medicine, 3rd edn., Philadelphia: Saunders, 2009.
5 Craft J, Gordon C, Tiziani A. Understanding pathophysiology. Sydney: Elsevier, 2011.
6 McCance KL, Huether SE. Pathophysiology: the biologic basis for disease in adults and children, 7th edn. St Louis: Mosby, 2010.
7 Pinn VW. Past and future: sex and gender in health research, the aging experience, and implications for musculoskeletal health. Orthop Clin North Am. 2006;37(4):513–521.
8 Australian Institute of Health & Welfare (AIHW). Hospital separations due to injury and poisoning: Australia, 2007–2008. Canberra: AIHW, 2010.
9 Lash R, et al. Diagnosis and management of osteoporosis. Prim Care. 2009;36:1.
10 Swartz MH. Textbook of physical diagnosis, 5th edn. Philadelphia: Elsevier, 2006.
11 Jarvis C. Physical examination and health assessment, 6th edn. Philadelphia: WB Saunders, 2008.
12 Chernecky C, Berger B. Laboratory tests and diagnostic procedures, 5th edn. St Louis: Saunders, 2008.