CHAPTER 67
Therapist’s Management of the Stiff Hand
JUDY C. COLDITZ, OTR/L, CHT, FAOTA*
CRITICAL POINTS
▪ Effective rehabilitation of the stiff hand requires that the effects of immobilization be minimized while not overloading healing tissue.
▪ Interosseous muscle tightness frequently contributes to limited finger flexion. One should assume that interosseous muscle tightness contributes to the limited motion until it can be proven otherwise.
▪ In the chronically stiff hand, tissue adherence and stiffness, chronic edema, and maladapted cortical patterning are interdependent problems. To be successful regaining mobility of the stiff hand, all three problems must be altered simultaneously.
The Challenge of the Stiff Hand
Clinical experience confirms certain risk factors for stiffness in the hand. The more tissue traumatized, the greater the likelihood of stiffness.1 Severe trauma injuring bone and multiple soft tissue layers usually requires longer periods of immobilization because of the need to regain skeletal stability. The decrease in tissue elasticity that accompanies increasing age creates less tolerance for the insult of trauma.2 Infection that extends the wound beyond its mechanically created boundary creates adherence between multiple remote tissue planes. Although we know these basic facts, many questions about stiffness in the hand remain unanswered: Why do some patients have great difficulty regaining motion long after others have returned to normal function? How can we identify what amount of motion, at what frequency, and with what duration will maximize individual patient results? We do know, as did Sir Charles Bell in 1883, that “the mechanical properties of the living frame, like the endowments of the mind, must not lie idle, or they will suffer deterioration.”3 Prolonged immobilization is the greatest enemy of hand mobility. Our challenge is to devise a treatment program that provides balanced stimuli to elicit a positive response.
Definition of Stiffness
The term stiff is used commonly when describing the hand lacking full mobility. The word stiff is usually reserved to describe the physical property of matter whose close molecular structure makes it rigid, resisting deformation when an external force is applied. Stiffness of the hand is not an increased rigidity of the tissues themselves4 but a constraint created by crosslinking of the previously elastic configuration of the collagen fibers.5
Collagen provides most of the tensile strength of the tissue in the hand. Collagen fibers themselves are inelastic, but movement between the collagen fibers imparts elasticity to the tissue. Normal hand motion occurs when these strong, dense connective tissue structures glide relative to one another.6 Stiffness is caused by the fixation of the tissue layers so that the usual elastic relational motion is restricted by crosslinks binding the collagen fibers together.5,7-11
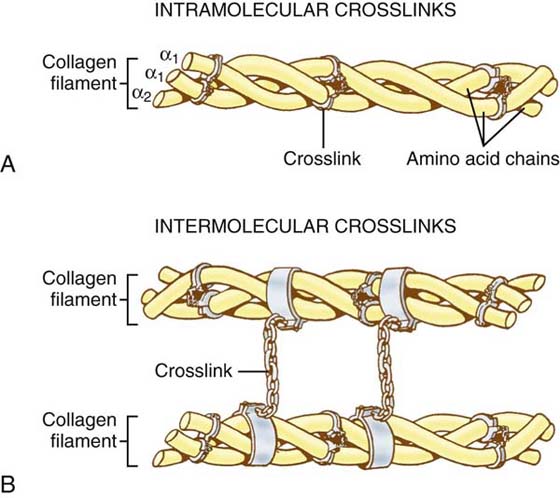
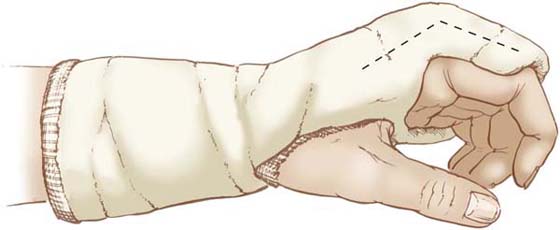
Peacock and Cohen11,12 provide an excellent analogy for the concomitant strength and elasticity of normal collagen. They compare collagen fibers to the strength of the relatively inelastic nylon thread used to make women’s nylon stockings. Significant elasticity of the stocking fabric is created by the way in which the nylon threads are knitted together. Collagen crosslinking does not change the collagen fibers themselves (analogous to the nylon thread), but it restricts the movement of one fiber (thread) in relation to another (Fig. 67-1).
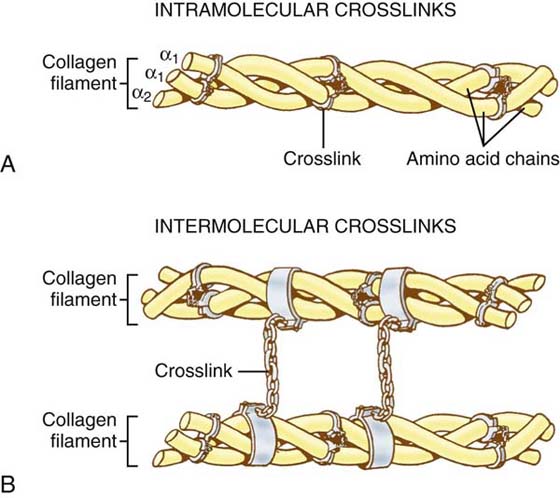
Figure 67-1 A, Collagen crosslinking occurs between amino acid chains within one collagen filament (weak crosslinks) and (B) between collagen filaments, locking them to one another (strong crosslinks). (From Hardy MA. The biology of scar formation. Phys Ther. 1989;69:1020.)
Stiffness and the Stages of Wound Healing
Tissue injury creates a relatively extended period of heightened collagen synthesis, degradation, and deposition within a wound as compared with the rate of this process within normal uninjured tissue.12 Healing tissue progresses through three stages: inflammatory, fibroplasia, and remodeling (or maturation).13 Although these are chronologic stages, they do not follow a precise timeline unless the wound has no complications.
During the inflammatory stage the wound prepares to heal, during the fibroplastic stage the tissue structure is rebuilt, and during the remodeling stage the final tissue configuration develops.14 In the ideal circumstance a healing wound progresses through these stages in an orderly and timely manner. Wounds with massive tissue injury, infection, absence of wound closure, or delayed healing, or wounds requiring repeated surgery or lacking proper wound hygiene, have extended stages of healing far beyond the ideal time frame. Therapists treating complex injuries cannot follow the chronology of a wound and assume a certain stage; instead they must be able to evaluate the characteristics of the wound or healing scar and determine the appropriate stage to devise appropriate therapy.
In the uncomplicated wound, the initial inflammatory phase of wound healing is completed within a few days. Randomly oriented, matted collagen fibrils unite the injured structures during this early phase of healing, although fibers cannot be visualized through the light microscope until the fourth or fifth day after injury. Because the intercellular forces are weak, wounds may be disrupted with ease during this stage.6 Most surgical wounds are protected with immobilization until the wound healing has begun.
In the uncomplicated wound the fibroplasia stage begins at the end of the first week of healing, when the fibroblast begins replacing the macrophage as the most common cell type. About 2 days later fibroblasts begin the process of collagen synthesis and outnumber the granulocytes and macrophages in the wound. The fibroblasts evolve into myofibroblasts and are responsible for collagen fiber synthesis and concurrent contraction of the wound edges. Capillaries reestablish within the wound, forming a dense network. Collagen fibers are laid down between the capillaries, forming the scar needed to keep the wound closed. By the end of the second week, the wound is filled with newly synthesized but disorganized collagen fibers invading all areas of the wound.6,15,16 Although the strength of the wound remains diminished (at 3 weeks an incised and sutured wound has less than 15% of its ultimate tensile strength),6 the random orientation of the collagen fibers limits their movement relative to one another. At this stage the scar is not strong and cannot tolerate excessive stress. If wound circumstances are ideal, the fibroplastic stage (also called the proliferative stage) occurs within the first week after the wound is created. However, in complex wounds or wounds with complications, this period is greatly extended.
Joint stiffness and tissue adherence palpated during this stage can be described by a soft end-feel at the limitation of passive motion. This tissue responsiveness occurs because the crosslinking of the collagen fibers is weak and stress causes the collagen fibers to align themselves with the direction of stress. The fluctuant end-feel of the passive joint limitation results primarily from edema filling the interstitial spaces and thus limiting full passive mobility. Because of the diminished strength of the healing tissue, excessive force can tear the fibrils, causing more injury and reviving the inflammatory process. Any force must be applied slowly and gently, and be sustained for a brief period of time. During fibroplasia, intermittent active motion is the ideal means of applying stress to the disorganized collagen to encourage realignment. More resistive motions can be coaxed by the application of a gentle sustained force applied using orthotic mobilization. Young scars can be altered morphologically by conditions of stress that are ineffective in older scars.17
In the uncomplicated wound the maturation stage usually begins between 3 and 6 weeks after surgery or injury. In the hand with delayed healing, infection, multiple tissue trauma, or multiple surgeries, the beginning of the maturation phase may be prolonged many weeks or months. As the cell population decreases, the number of scar collagen fibers increases.6 The total collagen accumulation then stabilizes and remains constant. At this stage collagen deposition is accompanied by collagen degradation, creating equilibrium. Alteration in the architecture of scar collagen fibers occurs as the scar matures. The tissue continues to respond to applied stress, but the response is greatly diminished as compared with the earlier stages. Physical changes are caused by changes in the number of covalent bonds between collagen molecules (see Fig. 67-1). Scars remain metabolically active for years, slowly changing in size, shape, color, texture, and strength,6 and ultimately begin to resemble normal tissue.
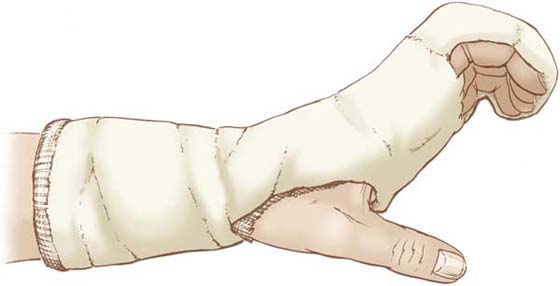
Wounds that are well into the maturation stage exhibit a hard end-feel when passive joint motion is applied. The joint motion does not yield to gentle force and stops abruptly. This response to palpation requires more consistent application of force to effect change. In the early part of the maturation stage, intermittent serial static or static progressive use of an orthosis can effectively mobilize the stiff hand. More complex injuries and more resistive chronically stiff hands require a more consistent application of gentle force, requiring a different approach. A nonremovable cast is recommended to consistently direct active force across stiff joints. This technique, casting motion to mobilize stiffness (CMMS), is discussed later (see “Evaluation and Treatment of the Chronically Stiff Hand”).
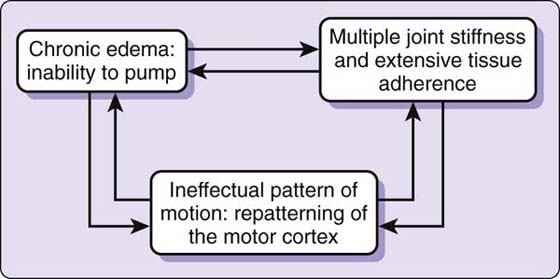
Evaluation and Treatment of Early Stiffness
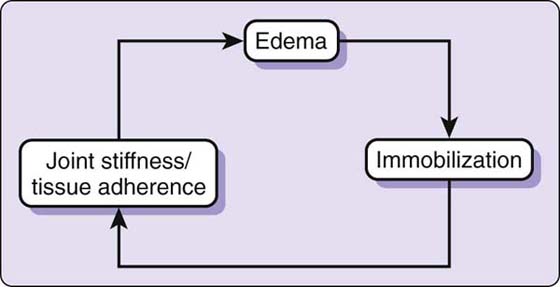
The demarcation line between the early stiff hand and the chronically stiff hand is difficult to pinpoint. In the following sections the early stiff hand is discussed separately from the chronically stiff hand, because the treatment approaches suggested differ greatly. Regardless of the stage of stiffness, manual examination is required to determine exactly which anatomic structures are limiting motion. The early stiff hand that is past the acute stage of healing but continues with edema, joint stiffness, and/or tissue adherence remains relatively immobile. This immobility may result from lack of functional use, pain, fear, or continued protection of healing tissue. A cycle is established in which inactivity leads to stiffness and adherence. This leads to continuing edema, which leads to continued inactivity (Fig. 67-2). In most postsurgical hand patients, changing one of these three factors readily breaks this cycle. For example, reducing edema allows greater potential for movement, which decreases inactivity and in turn decreases stiffness and tissue adherence. As the therapist and patient work together on each of the three factors, the other factors are directly influenced and the mobility of the hand returns.
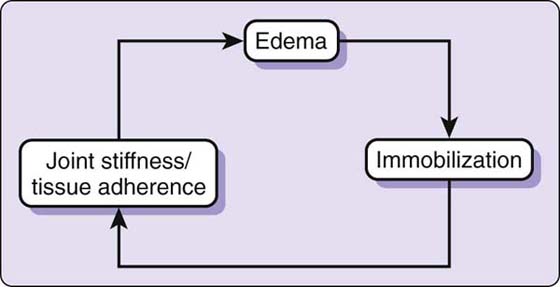
Figure 67-2 In the early stiff hand, three factors interplay to create stiffness: edema, immobilization, and joint stiffness–tissue adherence. Changing any one factor alters the cycle of stiffness.
Edema
Treatment of the stiff hand cannot begin without a thorough understanding of the causes of edema and the factors that influence it. Because its presence is a primary cause for immobility of the injured hand, edema reduction to create potential for motion is always a primary component of treating the stiff hand.
The reader is encouraged to review the other chapters about the lymphatic system and treatment for edema in this text (see Chapters 63 and 65). Key points are briefly reviewed here to support edema reduction recommendations made later in this chapter. These recommendations may differ from some long-held treatment beliefs.
Edema is excess fluid in the interstitium (the spaces between cells).18-21 Because one-sixth of the body consists of spaces between cells,20 there is significant room for expansion when the spaces are filled with edema. The injured hand normally develops edema as a result of increased capillary permeability, which allows leakage of fluid and protein into the tissue spaces.20 The presence of mild postoperative edema actually facilitates wound healing by causing a moderate increase in the strength of the healing wound and an increase in macrophages and fibroblasts.18,22 Greater amounts of edema destroy the continuity of the wound, breaking the fibrin seal and the integrity of the sutures.18
The lymphatic system is an intricate network of lymphatic conduits that drain excess fluid and other substances, including cells, proteins, lipids, microorganisms, and debris from the tissues to maintain homeostasis.20,21
Following an injury, the lymphatic system is often overwhelmed by the rate of capillary filtration and cannot carry the volume of fluid as fast as it is produced. This results in the development of edema. This normal edema production in response to injury is to be clearly differentiated from lymphedema, caused by lymphatic obstruction that causes protein to accumulate in the tissue spaces, which gives rise to osmosis of the fluid out of the capillaries.
Movement of lymph fluid through the lymphatic system is aided greatly by external forces—adjacent muscle contraction, tissue compression (e.g., gentle massage, bandaging), and general stimulation (e.g., arterial pulsations, body movement)—because the lymphatic system itself has no active pump. If wound healing progresses without complication, edema begins to subside and motion is regained. However, injured hands that develop significant stiffness do not follow this path, and inflammation and edema persist.
Pitting versus Nonpitting Edema
Before the development of externally visible pitting edema, the interstitial spaces must first become filled with fluid. This filling of the interstitium with lymphatic fluid increases the internal pressure, eliminating the ease of movement before edema is visible externally. Although this interstitial edema cannot be visually appreciated or measured as easily as pitting edema, it plays a significant role in preventing full motion of the hand.
Most of the interstitial fluid is trapped within the interstitial tissue gel. When edema exists in pockets of free fluid outside the interstitial spaces, it “pits” with pressure. These pockets of free fluid can hold more than half of the volume of the interstitial fluid.20 One common location of pitting edema is on the dorsum of the hand, where the loose dorsal skin pocket provides ample space for pockets of free fluid to accumulate. Manual pressure placed on the dorsal pocket causes the fluid to move, leaving an indentation (or pit)—thus the term pitting edema (Fig. 67-3).

Figure 67-3 Pitting edema is best observed on the dorsum of the hand after sustained pressure with the thumb.
Evaluation of Edema
External pitting edema can be measured accurately via water displacement.23,24 Measurement of pressure created by interstitial edema is impossible to accurately measure. A precise observational examination is far more useful in appreciating the level of interstitial edema.
Careful inspection of both hands (Fig. 67-4), comparing the general appearance, gives an insightful view of the presence of interstitial edema. Loss or diminution of normal small skin wrinkles, tautness or obliteration of the dorsal finger joint creases, and obscurity of metacarpal head definition and of the dorsal finger extensor tendons are recordable observations of the presence of interstitial edema.

Figure 67-4 Visual comparison of the injured and uninjured hands shows differences in skin wrinkles and creases, metacarpal head definition, and prominence of dorsal extensor tendons.
The presence of interstitial edema can be felt if the examiner palpates both hands simultaneously with eyes closed. Comparable fullness of the tissues is palpable, creating diminished tissue mobility in the injured hand. (In contrast, pitting edema is felt as fluctuant.) Active and passive joint motion is limited by a tangible fullness of the space, creating a soft feel to the end-range of joint motion. An experienced clinician can discern by palpation whether edema is the primary cause for limited passive joint motion.
Unfortunately, such palpation does not allow objective, quantifiable measurement, so that accurate comparison examinations and documentation of edema reduction are impossible. Some therapists use circumferential measurements of a digit, palm, or wrist, but the lack of reliability makes such measurements useful only as an approximate indicator of progress. If such measurements are used, the anatomic location of the measuring tape must be recorded and a repeatable amount of force applied to the measuring tape at each examination.
Edema Control Techniques
Minimizing the negative effects of immobilization caused by edema is the most useful initial treatment for the injured hand. Elevation, active muscle contraction, external pressure from various sources, and stimulation via gentle light massage can prevent the accumulation of excessive edema. Understanding which edema reduction technique to use when and the optimal type of force or pressure to use throughout the stages of healing is key to successful prevention of the stiff hand. Readers are urged to review the chapters on edema in this book (Chapters 63 and 65).
Elevation. Immediately following injury and/or surgery, immobilization of the tissues is usually necessary to allow completion of the inflammatory phase of healing without disrupting the healing wound.
Interstitial fluids tend to accumulate in dependent parts because the increased intravascular pressure increases capillary filtration.19,25 Even a normal hand can develop edema if it is immobile and dependent.26 Thus, elevation of the immobilized hand minimizes edema. The postcapillary blood pressure that facilitates venous return is less than 15 mm Hg of hydrostatic pressure. If the hand is in a dependent position, the pressure opposing the venous return is approximately 35 mm Hg of hydrostatic pressure.20
Elevation of the extremity, i.e., hand above the elbow, elbow above the heart, is the single most useful postoperative instruction to decrease the hydrostatic pressure in the vessels.25 Patients must be instructed carefully on the precise definition of elevation. The concept of a drop of water being able to run downhill to the heart without ever encountering an uphill run helps patients visualize adequate elevation.
Maintaining the arm in a sling is not adequate elevation and encourages the extremity to become quiescent. It is far more productive to instruct the patient to maintain elevation during the day by using pillows or books and reserve the use of a sling for brief periods of ambulation. During this time, intermittent active motion of the proximal joints should be encouraged to ensure that joint motion is maintained and large proximal muscle groups are recruited to assist venous and lymphatic flow.
When the surgical dressing is removed and intermittent active motion of the injured part is begun, intermittent elevation is still necessary to assist edema reduction. There is often a practical quandary. The hand is edematous and active motion is encouraged, but the patient is also instructed to elevate the hand, which is in an inactive position for the extremity. A balance can be achieved by instructing the patient to do active pumping exercises intermittently with the hand and arm elevated and to elevate the hand when not using it actively. Prolonged periods of using the hand in a dependent position with minimal active motion are to be avoided at this stage because of the difficulty maintaining the pumping balance.
Active Motion: Pumping versus Gliding Motion. Active muscle pumping near the site of edema is the single most important stimulus for increasing lymphatic flow. However, active motion across the site of injury immediately after surgery may disrupt healing and often cannot be immediately employed. Because there are no muscles within the digits, skin movement and tissue compression from active flexion is the stimulus required for increased lymphatic flow in the digits. When digital motion must be limited to protect healing structures, gentle pressure to the digit, elevation, and active muscle contraction in adjacent uninjured areas must substitute for active motion of the digit itself. With many digital injuries, the metacarpophalangeal (MCP) joint may safely be allowed full motion. This permits the patient to perform pumping exercises of digital adduction and abduction, and MCP joint flexion and extension, which contracts the adjacent proximal intrinsic muscles. Conversely, blocking the MCP joints in extension assures active flexion forces are directed to the interphalangeal (IP) joints to effectively mobilize the digital edema. If a well-conformed orthosis is applied to stabilize the MCP joints in extension, the molded volar orthosis surface provides appropriate pressure to the dense lymphatic network in the palm. This palmar pressure further assists in the reduction of digital edema.
In a randomized study of patients who started shoulder range of motion (ROM) immediately versus 7 days after axillary dissection for cancer, those waiting 7 days had less wound drainage, fewer days of drainage, and earlier postoperative discharge than patients who started immediately following surgery. There was no difference in the outcome of ROM in the two groups.27 This study suggests that active motion should appropriately be delayed when tissue injury or surgical dissection is extensive.
The muscles proximal to the wrist are larger than the intrinsic muscles of the hand and thus more effective stimulators of the lymphatic system. As long as the vascular status of the hand is stable, intermittent active motion of proximal muscles is begun as early as possible following surgery. Waste products that are evacuated from the injured hand are more effectively moved through the lymphatic system with this intermittent active motion. Passive ROM does not stimulate muscle contraction and, for that reason, cannot be substituted for active motion to reduce edema.28
When active motion of the injured part is allowed, elevation and proximal pumping must be continued until enough motion is present at the injury site to allow local pumping sufficient for adequate lymphatic flow. Patients who exercise the injured part of the hand while elevated see a dramatic edema reduction as they gain motion at the site of injury.
Compression. In addition to active muscle contraction providing intermittent internal compression to the lymphatic conduits, gentle external pressure also aids in lymphatic flow. Excessive pressure restricts lymphatic flow. For this reason, large compressive bandages are applied postoperatively to maintain gentle pressure to the hand. As one would expect, the use of external pressure alone, in the absence of active pumping, provides little long-term change. However, the use of external pressure as an adjunct to active motion often can interrupt the edema cycle, allowing potential for full active motion.
External wraps or elastic garments, external orthoses or bandages, or gentle external massage provide external pressure treatment. In the past, recommendations have been made for firm retrograde pressure to “push” the edema out of the hand. This concept should be abandoned and a concept of gentle external pressure should be adopted to facilitate lymphatic flow. See Chapters 63 and 65 on edema treatment for additional treatment suggestions.
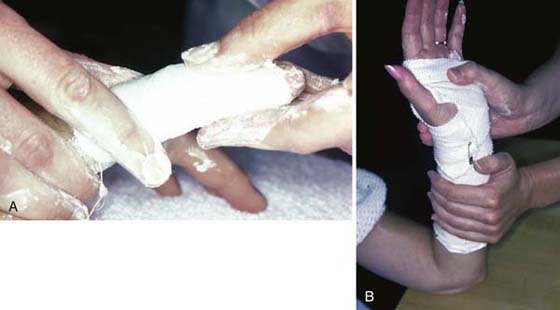
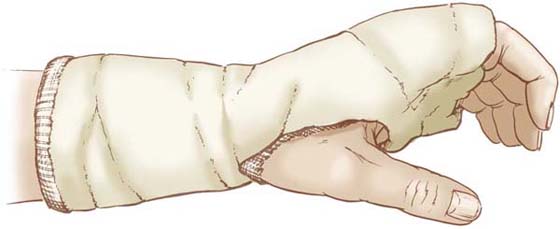
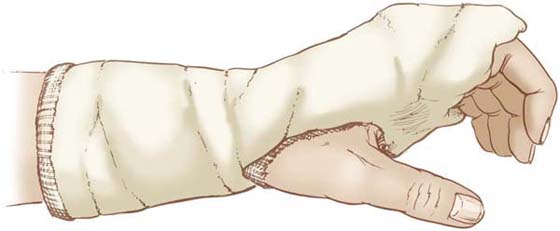
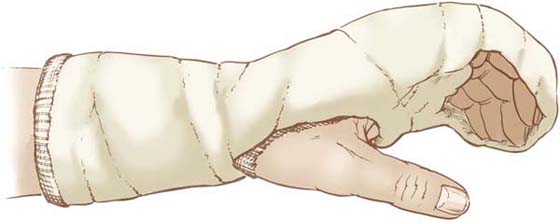
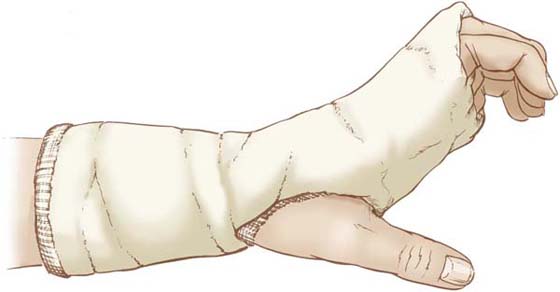
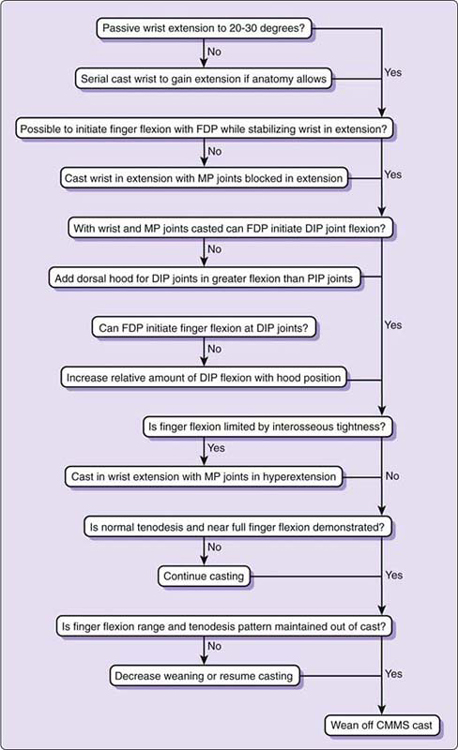
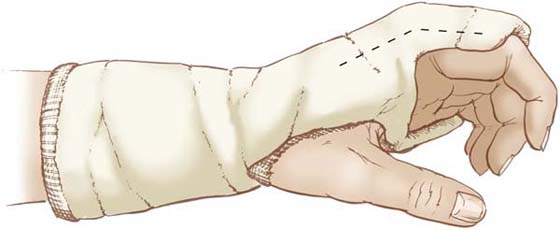
Compressive Bandage. Surgical dressings and other forms of immobilization are used to provide necessary rest so newly injured tissues are protected from external forces and can begin the healing process. When a wound has delayed healing, some form of bandaging that continues to supply gentle compression is advisable. When a patient presents with significant pitting edema (regardless of the stage of healing), the quantity of edema present in the tissues is so great that mobilization of the joints is futile until the edema is reduced. Although the foremost goal is mobilization of the hand, a brief period of partial immobilization in a bulky compressive dressing that distributes pressure to all tissues is a wise initial treatment (Fig. 67-5). The fingers are gently wrapped with a self-adherent elastic bandage before multiple layers of fluffed gauze squares are placed between the digits and also applied dorsally and volarly. A gauze wrap around the hand and wrist compresses the fluffed gauze squares. The fingers are left free to flex and extend at the IP joints, but the motion of the MCP joints is limited temporarily by the bandage. Elastic bandages and/or plaster of Paris slabs may be added to the exterior of the dressing for more specific support and compression. In significant pitting edema, the consistency of pressure provided by such a nonremovable overnight dressing can assist in dramatic edema reduction.

Figure 67-5 A bulky dressing may be used overnight or for a few days to provide prolonged but gentle compression for effective edema reduction.
If edema is a result of excessive manipulation of the hand causing a prolonged inflammatory response, a short period of rest and immobilization in a compressive bandage reduces both edema and inflammation. This approach allows a better starting point for upgrading motion and the use of other gentle edema reduction techniques. It may seem contradictory to immobilize a stiff swollen hand. The immobilization is necessary, because it is the most effective way to provide conformed pressure that will reduce the edema to a level at which productive active motion is possible.
Orthoses Immobilization decreases initial edema, reduces pain, and permits tissue repair without the stress of external forces. The use of immobilization orthoses during the acute stages of wound healing can provide effective rest and compression in addition to accurate positioning to protect healing structures or to maintain a balanced position. If orthoses are applied with straps, the lymphatic vessels can be occluded by the pressure of the strap.29 Pitting edema distal or proximal to a strap is a sign that strap pressure is impeding lymphatic flow. A safer alternative is the use of a wide elastic wrap or a molded thermoplastic piece that covers both dorsally and volarly. This distributes pressure rather than localizing it to a strap. When applying a hand-resting orthosis to an edematous hand, it is best to hold it in place by wrapping a wide elastic bandage at an angle along the full length of the orthosis. Later, when the edema has subsided, straps may be applied. This application technique is also effective for orthotic fabrications on the edematous elbow.
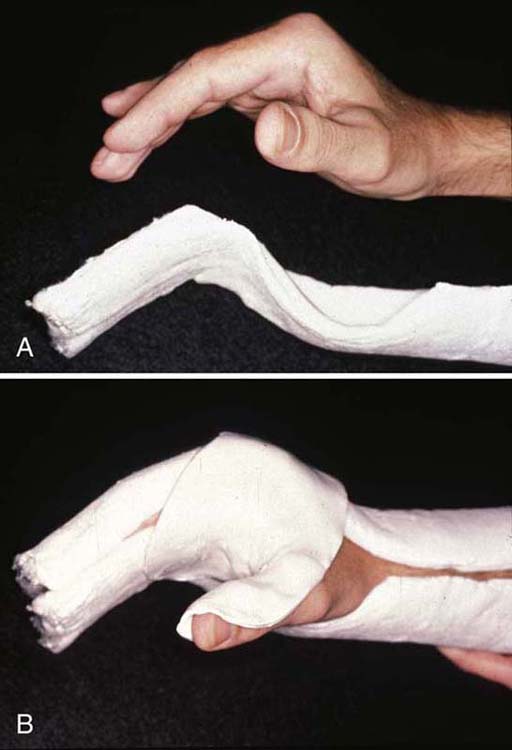
A removable immobilization orthosis made from dorsal and volar plaster of Paris slabs provides the most precise positioning, intimate fit, and even distribution of pressure possible30 (Fig. 67-6). As edema subsides, this plaster of Paris splint is serially changed to safely gain new joint positions. Either a plaster of Paris or thermoplastic immobilization orthosis can assist in optimal positioning and provide gentle distributed pressure while still protecting healing tissues from stress.
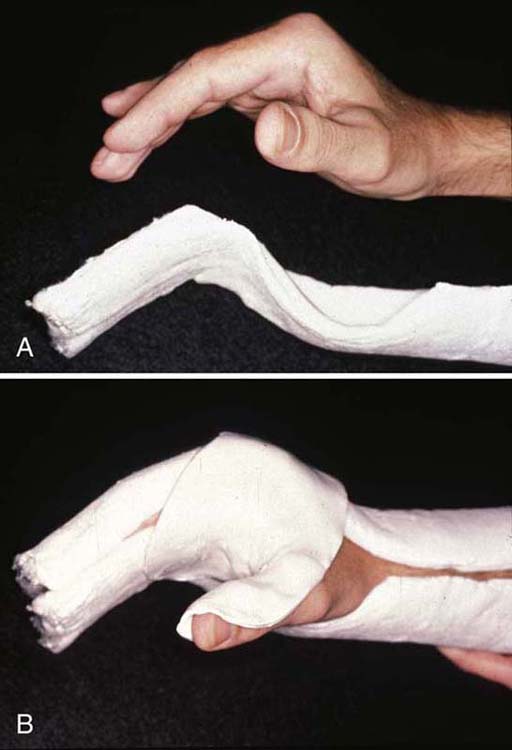
Figure 67-6 A, Volar plaster slab positions the hand. B, The hand is held precisely in position by the addition of a dorsal slab and an (optional) smaller slab to position the thumb.
External Wraps. Self-adherent elastic wraps are commonly used to control edema in the hand and especially in the digits. Any self-adherent elastic wrap must be applied lightly with particular caution so that it does not constrict blood flow or restrict active motion. It is the consistency of light pressure, not the intensity of pressure that is important. It is particularly important to explain this concept to patients and have them demonstrate independent light application of the self-adherent elastic wrap before leaving the clinic.
A single layer of the self-adherent elastic wrap can be applied by wrapping either a 3- or 4-inch width around the digit and gently pinching it together on the dorsum of the finger and trimming to a narrow seam (Fig. 67-7). This application allows easier adjustment of the tension with the one hand the patient has available than does the wrapping of multiple overlapping layers. One or two layers of tubular stockinette sized to fit the finger and applied underneath the self-adherent elastic wrap will offer a more gentle contact with the skin during movement of the digit.

Figure 67-7 A and B, Self-adherent elastic wrap is applied to the injured digit by pinching the material together on the dorsum of the finger. C, The material is trimmed to make a small unobtrusive seam.
Gloves. Elastic gloves are a convenient and inexpensive means of providing external pressure. Since one glove does not fit all patients and there is a lack of direct contact of the glove in the palm, the fit of the glove should be carefully assessed. The glove should fit like a loose second skin, providing a very gentle traction to the skin when the hand is moved within it. U.S. suppliers now market various brands of inexpensive edema gloves that are appropriate for use with the edematous hand. Tight constrictive gloves should be avoided.
Gentle External Massage. All hand therapists should become thoroughly familiar with the gentle-massage approach of manual lymphatic therapy techniques (see Chapter 63, Chapter 64 and Chapter 65). Originally developed as a means of facilitating lymphatic flow in patients with chronic lymphedema, this gentle facilitatory massage can be helpful with many hand trauma patients, most of whom have normal lymphatic anatomy.
After the acute healing phase has subsided, patients with isolated injuries may require only a short period of gentle massage. Patients with extensive crush injuries or large wound areas where the lymphatic anatomy is altered are ideal candidates for longer-term manual edema mobilization techniques (see Chapter 63, Chapter 64 and Chapter 65) to facilitate lymphatic flow around injury areas to reestablish lymphatic flow. Above all else, vigorous, forceful massage as recommended by many in the past should be abandoned. Superficial lymphatic vessels are thin, fragile structures that may be further destroyed by vigorous therapy.31
Mobilizing the Early Stiff Hand
Although many treatment techniques have been developed to mobilize the stiff hand, no basic research supports any particular exercise treatment regimen to regain mobility.9,10 Two basic principles for postoperative rehabilitation are imperative: The effects of immobilization must be minimized, and healing tissue must not be overloaded.32
Benefits of Early Motion
After injury, limited early movement reestablishes tissue homeostasis, increases venous and lymphatic flow, increases tensile strength of the wound, and directs the alignment and orientation of collagen fibers.7,15,20,33-35
In the early postoperative period, the beneficial effects of motion can be provided either by active or continuous passive motion (CPM), but active motion must quickly assume the dominant role if the patient is to resume functional use. The challenge is to allow enough motion to nullify the negative effects of immobilization but prevent excessive motion that will impede normal healing.
Beginning with Arem and Madden,17 many studies have validated the concept of controlled stress to promote favorable collagen orientation and to increase tensile strength of the healing tissue. Unknown, however, is how much, how many repetitions, how often, how long, and to what extent motion should be carried out for optimal stress application to influence tissue. If we knew how to precisely apply stress, postoperative therapy would be more efficient and productive.6 At this time, the guideline for the parameters of stress application must be the observation of a positive influence on the tissue and the absence of a renewed inflammatory response.
Early active motion should be precise, preventing substitution motions of the uninjured looser joints. For active motion to be productive in the stiff hand, it is usually necessary to block the looser joints. Active motion should be to the easy maximum end-range and should be repeated intermittently throughout the day. Frequent repetitions during each exercise period or extremely frequent exercise periods are not indicated early in rehabilitation. As a general guideline, the more acute the injury and the more inflamed the tissues, the more intermittent the active motion should be. As edema subsides and active motion is tolerated without an increasing inflammatory response, more frequent motion is indicated. The schedule for the balance between rest and motion depends on the tolerance of the tissue for increased frequency of motion, which can be determined only by a gentle trial-and-error method.
Importance of Preventing or Resolving Interosseous Muscle Tightness
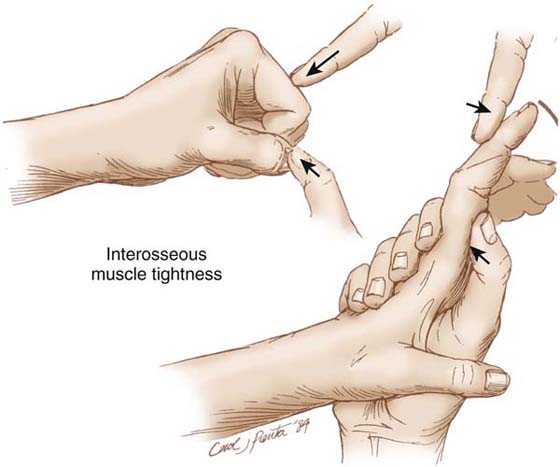
A discussion of the stiff hand is incomplete without a focus on the most frequent cause of finger stiffness: Interosseous muscle tightness (commonly, but incorrectly, called “intrinsic tightness”). The interosseous muscles reside within a tight fascial compartment between the metacarpal bones. These small interosseous muscles have limited excursion, making them relatively intolerant to the adaptive shortening that occurs as a result of immobilization. Direct trauma to the metacarpal area may also create injury or ischemia to these muscles, causing potential for an even greater severity of interosseous muscle tightness.
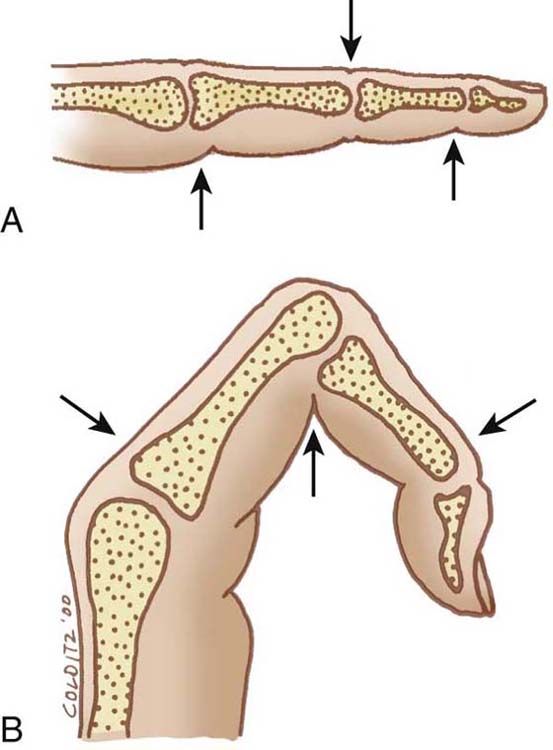
Full finger flexion demands elongation of the interosseous muscles. If the interosseous muscles are tight, full finger flexion is limited by the tightness. Since the line of pull of the interosseous muscles is volar to the MCP joint and dorsal to the IP joints, interosseous muscle tightness is determined by defining the amount of passive proximal interphalangeal (PIP) joint flexion when the MCP joint is flexed and then determining if this amount of PIP joint flexion is less when the MCP joint is simultaneously brought into passive hyperextension. This is the position of maximum elongation of the interosseous muscles.
Lack of full finger flexion is often assumed to be caused only by joint stiffness and/or lack of full glide of the extrinsic flexor tendons, and testing for interosseous muscle tightness is overlooked. Since interosseous muscle tightness from either direct injury or adaptive shortening frequently contributes to limited finger flexion, one should always assume this is contributing to the limited motion until it can be proven otherwise.
Instead of working on active and passive end-range composite finger flexion, the most appropriate approach to resolving stiffness of the fingers may be to block the MCP joints in extension while allowing full IP joint flexion. An exercise orthosis that blocks the MCP joints in extension is appropriate for the newly injured hand. For more severe and long standing interosseous muscle tightness a nonremovable cast may be required. (See “Dominant Interosseous Flexion Pattern”.)
The complex subject of interosseous muscle tightness versus lumbrical muscle tightness, and methods for testing, quantifying, and resolving interosseous muscle tightness are beyond the scope of this chapter, and the reader is referred to other sources.36
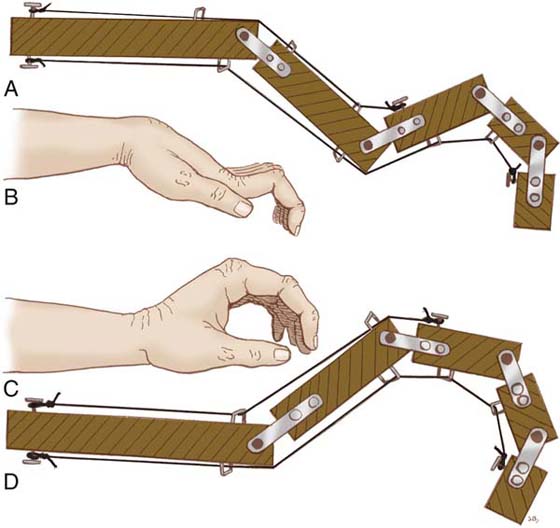
Blocking Motions
Unlike most of the large joints in the body, the small joints of the hand are moved by muscles crossing multiple joints. Because muscle pull results in the movement of the joints with the least resistance, muscle excursion will affect proximal mobile joints before affecting stiffer distal joints. Manual blocking transfers the muscle force to the targeted stiff joint, enabling the patient to experience glide at the site of restriction. For example, when the MCP joint is blocked during finger flexion, extrinsic flexor glide is directed across the IP joints rather than allowing MCP flexion directed by the interosseous muscles (Fig. 67-8). If blocking is an early part of treatment, many patients require only intermittent manual blocking exercises to regain balanced motion. If joint stiffness and/or tissue adherence is persistent, a blocking orthosis offers a longer period of sustained redirected active motion across the stiff joints to regain balanced motion (see Fig. 67-8).

Figure 67-8 A, Ulnar-volar view of an orthosis to allow active elongation of both the interosseous and lumbrical muscles. Note overlapping ulnar-sided closure, intimate contour of orthotic material in palm, and block over proximal phalanx allowing full PIP joint flexion. B, Dorsal view of orthosis shows intimate contour and well-distributed pressure over all MCP joints. C, Radial-lateral view shows position of MCP joint hyperextension. In the stiff hand, MCP joint hyperextension may have to be serially regained.(Copyright Judy C. Colditz, 2008.)
Balance of Exercise and Rest
The primary guideline for exercise progression should be the status of the hand after exercise. If edema, pain, and stiffness increase after exercise (or any treatment), the hand is not yet ready for that level of stress. Conversely, if the patient experiences sustained increased comfort and mobility, the amount of exercise is appropriate for the stage of recovery and may be slowly upgraded. Most patients can sense a positive tissue response versus a negative one and modify their exercise regimen accordingly to maintain the positive response.
Proprioceptive Feedback
When working to regain finger flexion, proprioceptive feedback is essential. Providing resistance to finger flexion to increase the patient’s proprioceptive sense of digital motion is beneficial. This is particularly critical in the presence of diminished sensibility. This type of feedback can be accomplished by the patient holding an object slightly smaller than the available range of finger flexion. Use of a padded handle that demands some effort to be held firmly will allow use of the hand for eating and self-care activities while demanding slightly more finger flexion than is readily available. The size of the handle is decreased as the patient gains flexion range.
Muscle Isolation and Pattern of Motion
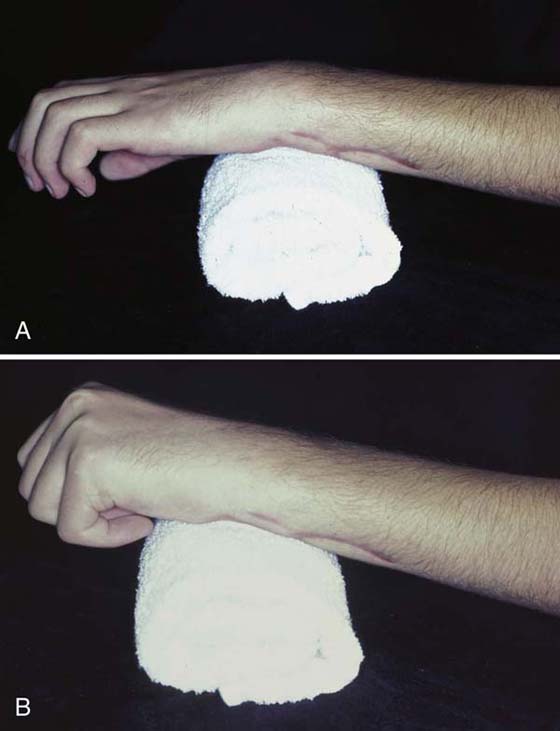
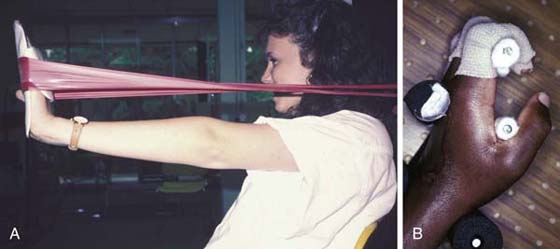
Patients who experience stiffness of the hand following injury invariably feel that a strong muscle pull is required to overcome the stiffness. Unfortunately, this excessive effort recruits the strongest muscles and overpowers the weaker muscles (Fig. 67-9). Co-contraction of muscles is a common result of excessive effort. The patient must first be taught that a gentle pull isolates the desired muscle and that exercise for strengthening comes later in therapy. The patient learns a clear difference between a strong global pull that is ineffectual and a gentle but sustained precise pull that reestablishes muscle balance. Understanding this difference between the “right” and the “wrong” way to exercise ensures that the patient repeats the exercise correctly at home. It may be helpful to have the patient pull intensely and let the stronger muscles overpower to appreciate the contrast with the gentler isolation exercises.
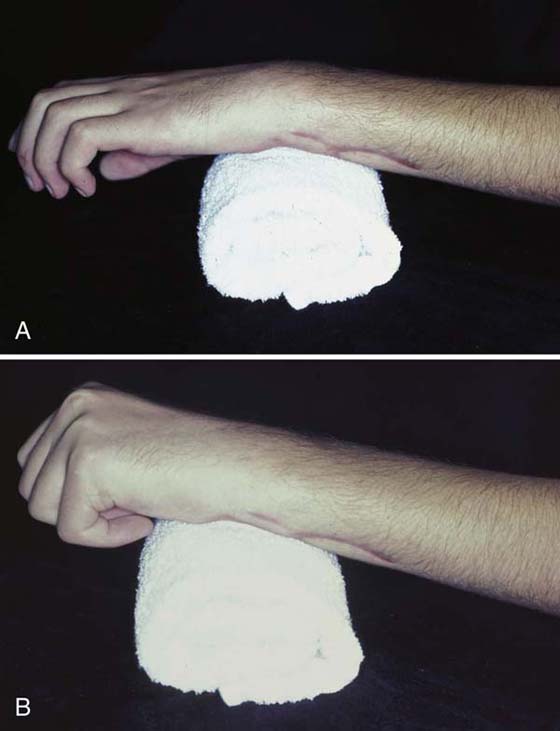
Figure 67-9 A, After Colles’ fracture, a patient attempts wrist extension but uses extrinsic finger extensors instead of wrist extensor muscles. B, When the patient maintains full finger flexion, he or she can isolate the wrist extensor muscles.
Patients whose limbs have been immobilized in a cast following a distal radius fracture provide a practical example. The weakened wrist extensor muscles cannot adequately stabilize the wrist in extension to allow the finger flexor muscles to flex the digits. When the patient is asked to extend the wrist, the finger extensor muscles substitute for the wrist extensor muscles because they have been unrestrained in the cast and are stronger (see Fig. 67-9). If edema and finger stiffness are accompanying complications, little progress can be made with finger motion until the patient can stabilize the wrist with the wrist extensor muscles.
Low-Load, Prolonged Stress
It is often stated that therapy should apply a low-load, prolonged stress to accomplish plastic deformation of the tissues.37-39 Early in the fibroplasia stage of healing, before collagen crosslinking is well established, intermittent active motion is usually enough stress to favorably alter the crosslinking. Later in healing, when excess collagen crosslinking limits motion, low-load, prolonged stress favorably modifies the crosslinks and the collagen fibrils slip over each other.40 This slippage is accomplished by active exercises that provide a concentrated force application to achieve maximum joint motion and soft tissue glide, which allows slippage of the crosslinks. This may be gained in a number of ways. If the tissues do not mobilize in response to blocked active exercise, orthotic mobilization that provides a gentle force for a longer period may be indicated. If the stiffness is persistent, a nonremovable cast promotes cyclic motion directed to the stiffer joints. This concentration of active force across stiff joints can mobilize even the most resistant of joints. (See “Evaluation and Treatment of the Chronically Stiff Hand” section.)
Passive Range of Motion
Although joint motion can be maintained by either active or passive motion,41 passive motion provides limited glide of the tissue planes other than the periarticular structures. Increasing passive motion does not necessarily increase active motion.
As with other therapeutic techniques, there are no research data to dictate the ideal force, speed, and duration of passive motion.5 Although passive joint motion often is prescribed to overcome post-traumatic joint stiffness, no research supports the efficacy of either intermittent passive motion or CPM to reduce joint stiffness.9 Aggressive passive motion of the hand is detrimental and should be avoided.8,28
Passive motion in the injured hand should be defined as the gentle encouragement of tissues to reach a maximum available length. The amount of force should respect the resistance of the tissues, and the position should be increased only when the tissues relax and decreased resistance is felt. When edema is diminished, any gentle passive joint motion should be done with accompanying gentle traction to the joint to allow room for one joint surface to glide over the other without compression. One gentle, prolonged hold will allow the motion to be repeated actively more effectively than many repeated quick sudden passive stretches. Quick, forceful stretches result in tissue damage and should be avoided at all times.
In the hand with more mature stiffness caused by increased collagen crosslinking, the brief intermittent nature of passive motion is ineffective and should be avoided. This seems contradictory, because one assumes that the stiffer the joint the more force is required to mobilize it. Rather than increased force, it is the increased duration of a low-level force that best creates change. When patients with significantly stiff hand joints undergo passive ROM during a therapy session, there is an immediate response of tissue mobilization. However, when the patient returns, the progress gained in the previous session has not been retained. A study of stiffness in rabbits after tibia fracture compared ankle stiffness between joints undergoing CPM and joints that remained immobile in a cast. The ankles receiving CPM demonstrated immediate reduced stiffness, but over time the stiffness in the CPM group was progressively and significantly greater than the group immobilized.9 This study suggests that further investigation is warranted regarding the long-term effects of passive ROM on stiff joints.
Active Range of Motion
Active ROM has multiple advantages over passive ROM. Active motion stimulates the lymphatic system, diminishing edema, and more quickly returns the hand to a state of homeostasis. Active motion also requires normal reciprocal glide of soft tissue structures such as tendons and ligaments. Another advantage of active motion is the continued association of the motor cortex to the active muscle contraction. Patients sustaining injury who are unable to use normal muscle recruitment patterns move in maladapted patterns. If maladapted movement continues, the motor cortex learns the maladapted motion and defines it as normal. A period of only 9 weeks will alter the motor cortex patterning.42 The earlier the patient is able to recruit the appropriate muscle pattern, the greater the patient’s potential to recapture full mobility.
Joint Mobilization
Although manual joint mobilization is advocated by many for the treatment of stiff joints of the hand, manual mobilization of the small joints of the hand is best reserved for specific capsular tightness with no accompanying inflammation. When motion is limited as a result of edema, manual joint mobilization may be ineffective and can lead to an increased inflammatory response. Joint mobilization without accompanying edema reduction does not increase the available room for movement. There are no published data on the effectiveness of joint mobilization in reducing joint stiffness. Nor are there any data that suggest harm.
Benefits of CPM
Because joint motion is needed to preserve joint lubrication,7,40 CPM often is used postoperatively to treat joint pathology. Neither laboratory nor clinical studies have shown that CPM is useful for treating joint stiffness once it has occurred.10,43 Therefore, CPM is appropriately reserved for the immediate postoperative period to prevent complications rather than to resolve stiffness. Readers are referred to the archives on the companion Website for the chapter Continuous Passive Motion for the Upper Extremity: Why, When, and How by LaStayo and Cass from the 5th edition.
Pathologic Patterns of Motion in the Early Stiff Hand
Loss of Wrist Tenodesis Pattern
The exquisite balance of muscle forces crossing the wrist and fingers creates a reciprocal motion called tenodesis. Finger extension occurs with wrist flexion as a result of the increased tension on the extrinsic extensor muscles when the wrist flexes. Conversely, when the wrist extends, tension is increased in the extrinsic flexor muscles that flex the fingers. This reciprocal action establishes the normal grasp and release pattern of the hand.
With stiffness, the tenodesis balance in the hand is frequently affected. In a minor injury, tenodesis is regained as motion at the injury site improves. In more severe injuries requiring long periods of immobilization, many joints may become stiff and the muscles crossing them become weak, altering the reciprocal balanced motion.
The wrist is the key joint to reestablishing the tenodesis balance in the hand. Without the ability to stabilize the wrist in extension, the finger flexor muscles cannot transfer enough power to regain finger flexion. Usually the primary goal is to regain digital flexion for grasp and manipulation of objects. However, when the fingers and the wrist all have limited motion, active finger flexion is not possible without first gaining some wrist extension (Fig. 67-10).
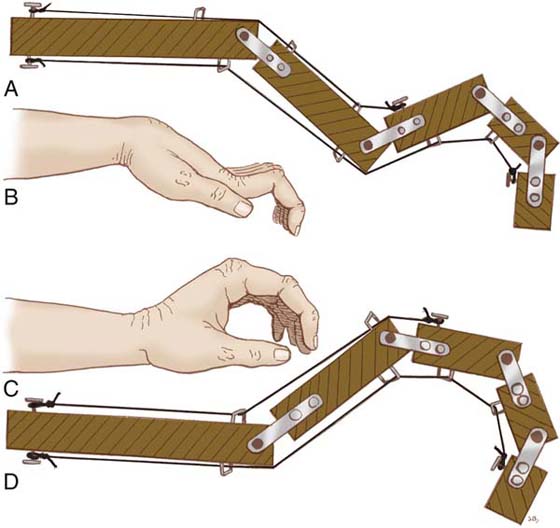
Figure 67-10 A and B, Loss of wrist extension creates tension on the extrinsic extensor muscles, and finger flexion is lost. C and D, With the wrist in extension, the tension on the finger flexors facilitates digital flexion. (From Bunnell S. Surgery of the Hand, 2nd ed. Philadelphia: JB Lippincott, 1948: p. 84)
Intrinsic-Plus Pattern
During normal finger flexion, IP joint flexion dominates before significant MCP joint flexion begins.41 If the hand is edematous and extrinsic flexor glide is limited (commonly seen after immobilization of wrist fractures or flexor tendon repair), the patient will initiate finger flexion with MCP joint flexion, and little IP joint flexion occurs. In this pattern of motion the interosseous and lumbrical muscles are never elongated to their maximum length, and they adaptively shorten, making the mobilization of the IP joints even more difficult.
Early treatment—consisting of activities, exercises, and/or orthoses that block MCP joint flexion and require IP joint flexion (unless contraindicated by surgical repairs)—can convert global finger flexion into specific glide across the IP joints (see Fig. 67-8). In the chronically stiff hand, longer periods of intervention may be necessary to change the pattern of motion. (See section on “Evaluation and Treatment of the Chronically Stiff Hand.”)
Intrinsic-Minus Pattern
When the intrinsic muscles are not actively participating in digital flexion, isolated MCP joint flexion is absent. Flexion occurs first at the IP joints, and only after full IP joint flexion do the extrinsic flexors pull the MCP joint into flexion. This may result from denervation of the intrinsic muscles, but in the stiff hand it is more commonly a result of isolated capsular tightness of the MCP joints or the restraint created by adherence of the extensor tendons on the dorsum of the hand. Blocking the wrist so that flexion forces from the extrinsic flexors can be directed to the MCP joints is required to actively mobilize the MCP joints. Without MCP joint flexion the intrinsic hand muscles cannot participate in the digital flexion.
Evaluation and Treatment of Joint Stiffness and Decreased Tissue Glide
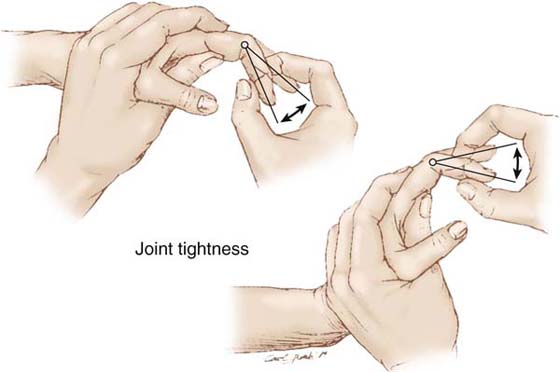
Joint Tightness
Joint tightness is identified by manually examining the passive ROM of a joint to determine whether the passive ROM changes as proximal and distal joint positions are altered. If the joint ROM does not change, isolated joint tightness is present (Fig. 67-11).
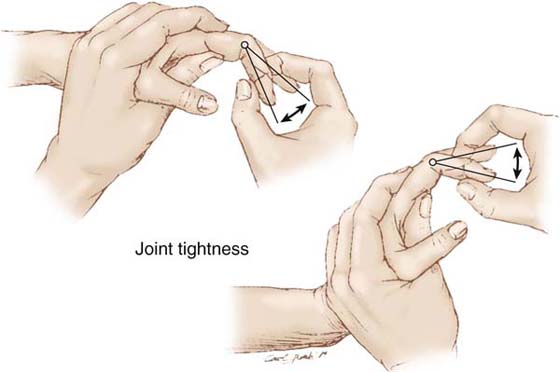
Figure 67-11 Joint capsular tightness is defined when the range of passive joint motion is the same regardless of the position of proximal and distal joints.
Clinical reality usually provides a combination of joint tightness and other external constraints, such as muscle–tendon unit tightness or tendon adherence. An experienced therapist can determine the balance and mix of the many tissues that are limiting motion. Accurate appraisal may be limited until certain joint motions have been regained. For example, PIP joint flexion must be gained before the full extent of interosseous muscle tightness can be determined.
Accurate, repeated ROM measurements must be the means of monitoring improvement.44 If there is a large discrepancy between the active and passive ROM, the emphasis should lie on active pull-through. If the active and passive ROM are equal, it may be appropriate to gain passive motion via mobilization orthotic positioning. Increased passive motion can also be achieved by blocking the more flexible joints, allowing active motion to reduce joint stiffness, which in turn increases passive ROM.
Manual Treatment. The degree of trauma to the joint capsule and the stage of healing determine whether the palpated resistance to full-joint motion is the expected amount of joint stiffness. When joint tightness is evaluated, a distinction should be made between a joint with a soft end-feel and one with a hard end-feel. A soft end-feel refers to a joint whose stiffness is characterized by a soft and springy end to the passive joint motion. This soft end-feel joint tightness results from edema within the joint capsule and the early stages of collagen crosslinking. With active motion and an intermittent low-load stress, the capsular joint structures can regain independent glide. Hard end-feel joint tightness has less edema present and is primarily a result of more mature collagen crosslinking. When moved to its maximum ROM, there is an abrupt and well-defined end point to the passive test. The hard end-feel joint requires more prolonged periods of mobilization in an orthosis to gain motion or more sustained periods of cyclical active motion. (See the section on “Evaluation and Treatment of the Chronically Stiff Hand”.)
It is appropriate to apply manual gentle passive ROM to joints with a soft end-feel. If the joint edema is minimal, gentle prolonged passive stretching to soft end-feel joints can allow more active motion to be transmitted across the stiff joint. In many cases this is enough influence to resolve joint stiffness. In the joint sustaining minor trauma, early intermittent gentle passive motion may produce full active motion without further intervention.
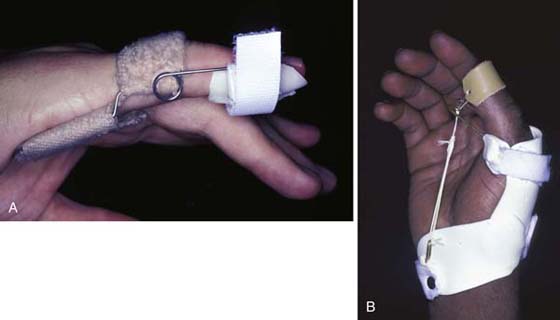
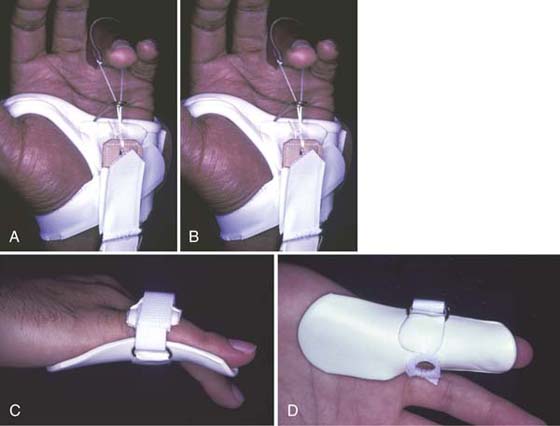
Joint Mobilization via Use of an Orthosis. If active and passive mobilization techniques are not successful or if the joint resistance is significant when initially evaluated, mobilization orthotic positioning to regain capsular length in one direction may be essential to regain joint motion. The motion with the greatest resistance is the least likely motion to be regained with only active and intermittent passive stretching, and this motion should be the target of mobilization via use of an orthosis. Wrist joint extension, MCP joint flexion, and IP joint extension are often the most resistant joint motions, and must be given orthotic priority to balance the strength of the more powerful opposing muscles.
Mobilizing orthoses directed toward isolated joint tightness requires that only the involved joint be included in the orthosis (Fig. 67-12A). Orthoses may be applied that provide a dynamic, serial static, or static progressive force. Dynamic force applied by rubber band or spring traction is a soft application of force appropriate for joints with a soft end-feel. If joint edema is present, serial static orthoses can gain joint motion concurrent to providing edema reduction via gentle joint compression. Joints with greater resistance respond favorably to prolonged application of serial static orthoses, or may respond to static progressive orthoses. Serial static or static progressive orthoses should be reserved for extension mobilization positioning, since compression of the joint in the maximally flexed position is poorly tolerated. A dynamic force may be more comfortable for the patient at the end-range of joint flexion than an unyielding static progressive force, because flexion dramatically increases intra-articular pressure45 (Fig. 67-12B). (See Chapters 123 through 125 for further discussion regarding use of orthoses for mobilization of joints.)
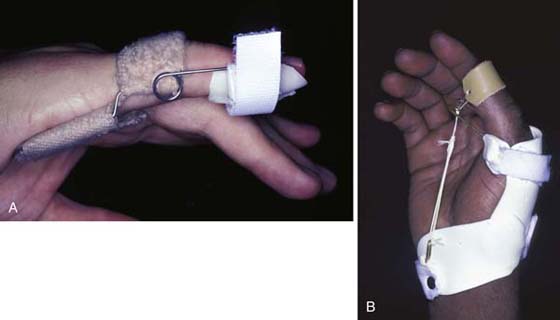
Figure 67-12 A, A dynamic PIP extension-mobilization orthosis effectively gains PIP joint extension without including other joints. B, An orthosis stabilizes the MCP joint of the thumb while dynamically mobilizing the IP joint into flexion.
Muscle–Tendon Unit Tightness
Muscle–tendon unit tightness is shortening of the muscle–tendon unit from origin to insertion, limiting full simultaneous motion of all joints crossed by the muscle–tendon unit. The muscle is the elastic part of this unit, which shortens with disuse. This tightness commonly occurs as a result of immobilization or restricted motion following injury or surgery. If a muscle–tendon unit is left in a short position in the presence of tissue inflammation, the tendon will also become adherent along its entire path, even if there is no direct trauma to the tendon or tendon bed. Specific trauma to the tendon or tendon bed, however, creates distinct adherence at the site of injury. Tendon adherence thus may be isolated to the point of trauma or extend over a larger area of more extensive trauma or immobilization in the presence of inflammation. Tendon adherence affects movement only of the joint(s) distal to the point of adherence. Although both muscle–tendon unit tightness and tendon adherence may have similar clinical presentations, careful examination identifies the exact location of the problem.
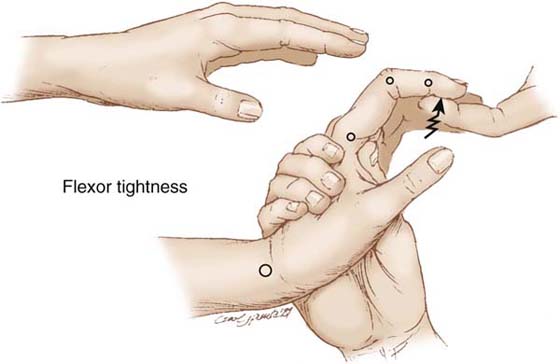
Evaluation. Both tendon adherence and muscle–tendon unit tightness are demonstrated by a distinct difference between the passive distal joint motion when the proximal joints are positioned in flexion versus extension (Fig. 67-13).
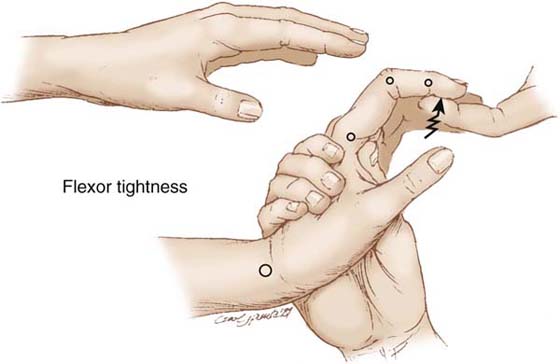
Figure 67-13 Tightness of the extrinsic flexor muscles is seen when finger extension is limited when the wrist is extended but unimpeded when the wrist is in a neutral position or in flexion.
The most proximal joint crossed by the muscle–tendon unit is the key to appraising tightness. For example, with tightness of the extrinsic extensor muscles, the fingers will be unable to flex as far with the wrist in flexion as when the wrist is in extension. The opposite is true for extrinsic flexor muscle tightness; with wrist extension, finger extension is limited by the shortness of the extrinsic flexor muscle–tendon unit(s). But when the wrist is flexed, the fingers can extend. To achieve an effective stretch of the extrinsic flexor muscles, the wrist must be held in extension while the fingers are also gently but firmly held in maximum extension (Fig. 67-14A).
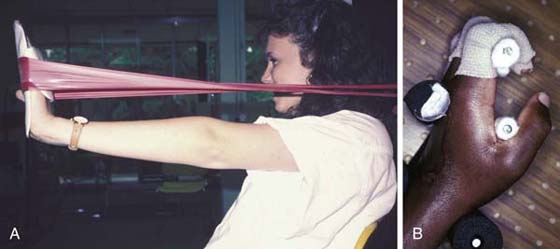
Figure 67-14 A, Stretching long-flexor tightness may combine an orthosis to hold the fingers in extension while elastic stretches the wrist into extension. B, A pegboard stabilizes various joints to allow the patient to apply prolonged active stretch for IP joint tightness and intrinsic muscle tightness.
The same principle holds for the interosseous muscles in the hand, with the MCP joint key to evaluating interosseous muscle tightness. Because the interosseous muscle–tendon units run volar to the axis of the MCP joint and dorsal to the axis of the PIP joints, the maximum stretch of this muscle–tendon unit occurs when the MCP joint is held in maximum extension (e.g., hyperextension) and the PIP joint is passively flexed. If the range of passive PIP joint flexion is less when the MCP joint is held in full extension, the interosseous muscles are tight (Fig. 67-15). Examining the patient’s contralateral uninjured finger for interosseous muscle provides a baseline for that individual’s normal interosseous muscle–tendon unit length.36 This varies considerably among normal individuals.
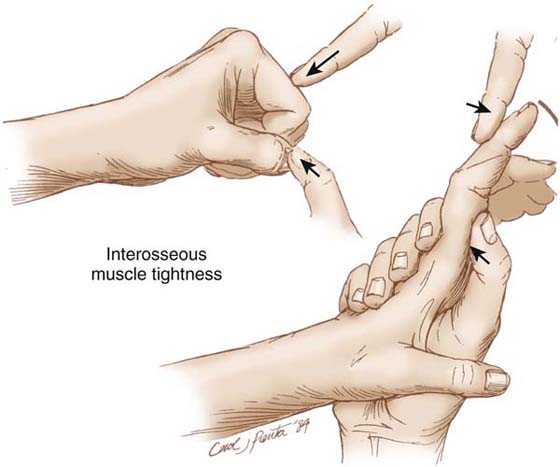
Figure 67-15 Interosseous muscle tightness is noted when PIP joint passive flexion is less when the MCP joint is extended (or hyperextended) than when it is flexed.
Treatment.Tightness Because muscle–tendon unit tightness usually results from immobility of the hand, intermittent passive stretching following by active blocked motion often alleviates mild muscle–tendon unit tightness. This is true especially when stretching is started early after the injury or surgery. The stretch must be prolonged46 and followed by active use of the muscle through the stretched range.
Tendon adherence seen early usually can be eliminated by a prolonged stretch to glide the tendon through its maximum range. Such stretching must be delayed if the tendon has been repaired. If, when stretching tendon adherence, the therapist feels a palpable release of the adherence, the stretched position should be maintained and then slowly incrementally positioned until the response subsides. This sudden slipping of the tissue layers can be felt as the gentle force is sustained through the increasing range. It should be strongly emphasized that this prolonged manual stretching is a slowly applied force and is continued based only on a positive tissue response. The therapist can palpate the diminished resistance in the tissues. The patient should be comfortable throughout this procedure, feeling pulling and perhaps slight discomfort, but never pain. Patients with early tendon adherence may experience a dramatic improvement in motion after such a prolonged stretch. More commonly, one does not see this sudden dramatic response but instead sees slow improvement over a longer time with repeated stretching.
Both passive mobilization via an orthosis and active exercise can elongate muscle–tendon tightness (see Figs. 67-12 and 67-14). Orthoses to diminish muscle–tendon unit tightness require that all joints crossed by the tightness be included in the orthosis. Orthoses for muscle–tendon unit tightness should be easily adjustable or replaceable as gains are made. Mobilization via orthoses is discussed more fully later in this chapter.
Adherence. A tendon may be adherent anywhere along its path. Motion to decrease the adherence is accomplished only by joint motion distal to the adherence. This can be active motion of the joints distal to the adherence that actively pulls on the adherent tendon, or it can be passive motion of the joints distal to the adherence, which are moved in the direction opposite to the active motion (i.e., passive extension if a flexor tendon is adherent). This insight allows correct positioning for exercise and determines the joint(s) to be included in any orthosis. Mobilization via orthoses to decrease tendon adherence is effective only in regaining distal glide of an adherent flexor or extensor tendon. To gain proximal glide, the patient must isolate and strengthen the correct muscle to regain full excursion of the adherent muscle–tendon unit.
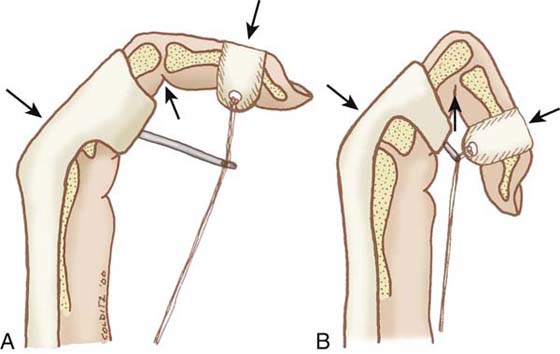
Adherence after flexor tendon repair provides an example of the type of active motion necessary to gain proximal glide of an adherent tendon. Commonly, after flexor tendon repair the patient flexes strongly with the unimpeded interosseous muscles, and minimally glides the extrinsic flexor tendons, especially if the injury has been within the flexor sheath (zone II). Commonly the MCP joint fully flexes before the IP joints reach full flexion. When tendon healing permits, blocking the MCP joint in extension to demand flexor tendon excursion across the distal joints is mandatory (see Fig. 67-8A and Fig. 67-14B). Tendon-gliding exercises47,48 that require independent glide of the profundus and superficialis tendons relative to one another and of the profundus tendon relative to the underlying bone must be included. Early gentle resistance provides helpful feedback to ensure correct motion and begins to strengthen the weakest muscle unit. When tendon healing is complete, neuromuscular electrical stimulation may be used if a feedback effect is desired and muscle fiber recruitment is inadequate.
Mobilization via an Orthosis. Use of an orthosis to decrease tendon adherence need include only the joints distal to the site of adherence. An example would be dorsal adherence of an extensor tendon over a healed metacarpal fracture. Orthotic positioning of all finger joints in flexion to glide the tendon distally would not require inclusion of the wrist, because the adherence is distal to the wrist. In contrast, if the problem is tightness of the extrinsic extensor muscles, the wrist must be positioned in some flexion within the orthosis to effectively stretch the muscle–tendon unit.
Skin and Scar Tightness and Adherence
All wounds heal with internal and external scar. Depending on the size, location, and extent of scar, external scars (especially linear scars) may limit joint motion. Even if the scar is not adherent to the underlying joint(s), the length of the scar may not allow multiple joints to move in the same direction simultaneously. For example, a split-thickness skin graft on the dorsum of the hand can tether the skin so that either IP joint flexion or MCP joint flexion is possible, but simultaneous MCP and IP joint flexion is not possible.
Evaluation. Skin tightness is assessed by positioning joints so that the limiting scar must elongate to a maximum length. Blanching, palpable tightness, or immobility of the scar or skin displays the extent of tightness (Fig. 67-16). If skin tightness is limiting joint motion, placing the skin in its shortest position allows increased joint motion proximally or distally. This motion is diminished as either joint is positioned to elongate the involved skin. This limitation may be difficult to determine in a severe injury that creates both skin tightness and joint tightness.

Figure 67-16 Blanching of the skin at the MCP joint demonstrates scar adherence and tightness.
Manual Treatment. External scars are visually evident but must be palpated to determine their mobility and character. All new external scars will be adherent to the underlying bed and will have decreased oil and sweat production. In large scars, the lack of lubrication and adherence causes the scar to be dry and intolerant to frictional forces. As the scar reaches maturity and can tolerate friction, gentle direct massage with an appropriate lubricant is the treatment of choice.
Orthotic Mobilization for Skin Tightness. Unlike other tightness often alleviated by intermittent stretch, skin tightness usually requires prolonged holding of the skin at its maximum length. Use of an orthosis is mandatory to accomplish this. Prolonged serial static orthotic positioning with a positive-pressure interface mold provides the best force to realign the collagen fibers. Any orthosis to elongate skin and scar tightness must also position the joints at the proximal and distal ends of the tightness to allow full elongation of the tissue.
In the hand such prolonged positioning with the skin in the longest position is difficult to achieve. The need for increased mobility and strengthening of the hand must be balanced with the need for prolonged scar elongation. At a minimum, such mobilization positioning orthoses should be worn during sleep. In the initial stages of wound contraction the orthosis may be required 23 of 24 hours if the graft or scar covers a large area and/or multiple joints. As tissue matures, the duration of orthosis wear may be slowly decreased to nighttime only. The rigid effect of an orthosis counteracts myofibroblast pull49 and decreases scar proliferation and contraction.
General Principles of Passive Orthotic Mobilization of the Early Stiff Hand
Therapists must have a wide spectrum of treatment skills to mobilize stiffness in the hand. If the patient is seen early after a simple injury, often no passive mobilization with an orthosis is required. However, patients with greater tissue damage commonly require orthotic positioning to optimize functional motion. It must be emphasized that use of an orthosis alone is not adequate treatment but must always be in conjunction with an individualized exercise program. Because scar can be modified by stress application,17 passive orthotic mobilization may be an important part of regaining mobility of the severely injured hand. Unfortunately, all orthoses, even those applying passive mobilization, impose immobilization and constriction, and the good of the orthosis must outweigh the negative effects of restriction and immobilization.8 Orthotic mobilization applied early postinjury that repositions joints with serial application is the safest early means of mobilizing healing tissue.
Each orthosis applied to the injured hand must be designed based on the mobilization goals for that hand.50 Therapists must possess analytic skills, manual construction skills, and biomechanical knowledge to apply well-fitting and well-designed orthoses. Adequate discussion of orthotic fabrication far exceeds the scope of this chapter, but important points are discussed in the following sections.
Tissue Response to Orthotic Mobilization
Human tissue responds to the application of mechanical force. Because collagen tissue is elastic by virtue of the weave configuration of the larger subunits,11 short-duration force applied to collagen fibers elongates the tissue but provides no alteration of the collagen fiber construct. This is the elastic response.37,51 If the force is applied over a prolonged period, the plastic response occurs. The tissue retains all or part of the elongated position. The amount of temporary versus long-term change of tissues depends on the intensity and duration of the applied load.33,38
Optimal deformation is with the application of an intermittent low-load stress for defined periods of time.33,37,46,52 One can understand this principle by thinking how a rubber band, when quickly stretched, returns to its original length; a rubber band held stretched does not return to its original length as quickly or as completely.
The dilemma is that prolonged positioning imposes immobilization. The challenge is to balance periods of passive orthotic mobilization with periods of active movement to ensure the maintenance of passive gains. Passive orthotic mobilization must apply a low magnitude of force to avoid stimulation of the inflammatory response that increases edema and fibrosis.
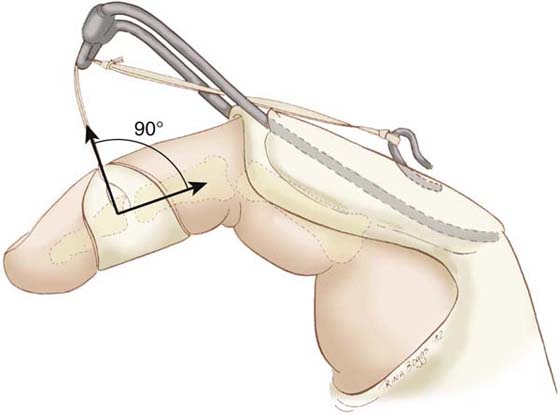
Force Application in Orthotic Mobilization
Although it is possible to measure the amount of force being applied with an orthosis, there is currently no way of measuring either the optimal amount of stress needed or the optimal application time of the stress to bring about the most rapid agreeable scar modification. The critical question is not the amount of force we are applying but the pressure exerted on the skin where the force is applied.8 This point-of-force application becomes the limiting factor. Although one can measure how much pressure can be tolerated before skin necrosis occurs, this is of indirect value because mobilization orthoses are applied intermittently. Pressure becomes relatively unimportant in the presence of intermittent application.8,53 Fess has demonstrated that experienced therapists consistently choose greater amounts of force for application to more mature scar.54 Flowers and LaStayo have introduced the idea of total end-range time (the amount of time a restricted joint is held at maximum length), suggesting that future orthosis prescriptions will specify both the amount and duration of force application.38 Glasgow et al. demonstrated a statistically significant greater effect of longer versus shorter applications of total end-range time in resolving joint contractures in a prospective randomized trial.55 Until we have a means of measuring the amount of resistance in the tissues and developing a rationale for the maximum desirable force, the patient’s tissue response to the force application remains the primary guideline to force application.
The patient must understand that the goal is not to tolerate increasing amounts of tension but rather to tolerate low tension for longer periods. After an initial adjustment period, a patient’s tissues should comfortably increase tolerance to the prolonged passive-mobilization force. The patient should be aware of the sensation of stretching while wearing the orthosis but should not experience pain. A motivated patient will eagerly wear an effective, well-fitting orthosis.
Types of Mobilization Orthoses
A therapist can choose from three types of passive mobilization orthoses (serial static, dynamic, and static progressive) or can choose a splint that provides active redirection. In the early stiff hand, active redirection can be accomplished by a removable exercise orthosis (see Fig. 67-8), and more chronic stiffness requires a nonremovable cast. Understanding the mechanical effect of each type of orthosis allows the therapist to choose the most effective means of regaining motion while facilitating healing.
Serial Static Mobilization Orthoses. A serial static orthosis immobilizes joints in a stationary position. The orthosis is applied with the tissue at its maximum length and is worn for long periods of time to allow the tissue to adapt8,56 (Fig. 67-17). After a period of tissue accommodation, either a new orthosis is applied or the old orthosis is remolded to hold the tissue at a new maximum length. Although the orthosis is stationary, the repeated repositioning of the joint(s) increases the length of the tissues.
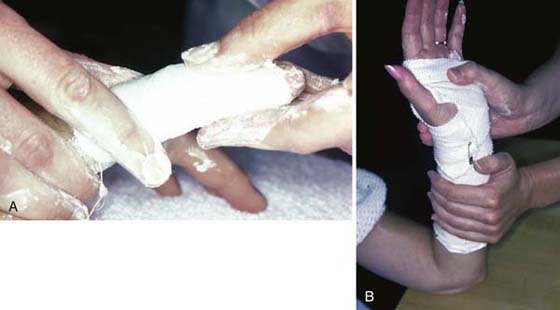
Figure 67-17 A, A stiff PIP joint with a flexion contracture can be resolved effectively by serial extension mobilization casts to the finger. B, Wrist extension is regained by serial application of dorsal and volar plaster slabs.
Dynamic Mobilization Orthoses. A dynamic orthosis applies force to a specific joint or joints. A stretched rubber band, spring, or wire coil generates the continuous force (see Fig. 67-12). As joint motion changes, the force of the orthosis continues. Although the force is constantly pulling while the orthosis is applied, the application of force is intermittent because the orthosis is periodically removed.57 In the early stiff hand where collagen crosslinking is immature, intermittent dynamic force application effectively restores tissue mobility. In the hand with more mature stiffness, the intermittent nature of the force application is often inadequate to effect desired change.
For dynamic force application to mobilize the tightest structures, the hand must at times be positioned awkwardly in the orthosis. The intermittent nature of dynamic force application allows such awkward positions to be tolerated, because active therapy combines with the orthotic positioning program to regain balanced motion. Use of a dynamic orthosis is the technique of choice when passive motion of the joints is responsive to manual stretch and inflammation has subsided.51,58
A period of therapy to regain active tendon pull-through and edema reduction while increasing the tolerance to stress readies the hand for dynamic mobilization in an orthosis. If the dynamic orthosis is applied too early or with too much force, it can escalate the inflammatory response.
Static Progressive Mobilization Orthoses. Static progressive mobilization orthoses may appear identical to dynamic mobilization orthoses, but the applied force is not dynamic (Fig. 67-18). Instead of the constant pull of a rubber band or spring, the tension on the joint is an adjustable static force. The force may be applied via hook-and-loop fastener or with commercially available components that adjust in small increments. When tension is applied, the joint is positioned at its maximum end-range. The force is adjusted when the tissue response allows repositioning to a new length.
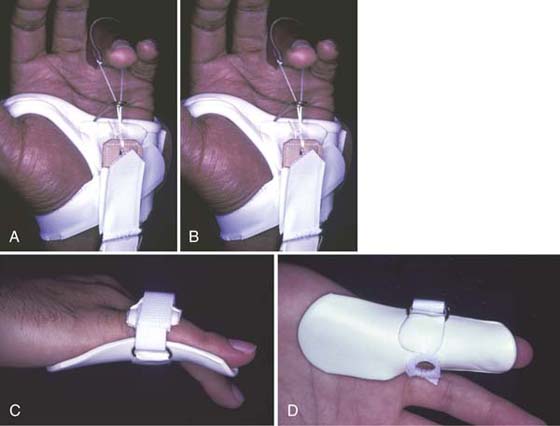
Figure 67-18 A and B, Static progressive orthosis applies flexion force to gain MCP joint flexion. C and D, Serial static orthosis gains end-range proximal IP joint extension, because volar piece is molded in a position of greater extension than is available to the joint. (From Colditz JC. Efficient mechanics of PIP mobilisation splinting. Br J Hand Ther. 2000;5:65. Copyright 2000.)
Static progressive orthoses are effective for joints with limited motion when there is significant resistance at the end of the passive stretch. Static progressive orthoses are especially recommended when positioning to regain end-range joint extension of the small joints of the hand (see Fig. 67-18C and D). As with other passive mobilization orthoses, the patient removes the orthosis and works on active glide or may use another orthosis to gain another direction of motion. Prolonged stretch at the end of the ROM is what gives the joint its full easy motion in both directions. The earlier the hand is ready for static progressive positioning, the shorter the time required to regain motion. The longer after injury that positioning is initiated, the longer the orthosis will have to be worn to regain the motion.
Choosing Mobilization Orthoses Based on the Stage of Healing
The stress appropriate to mobilize tissues differs in each clinical stage of healing. Static immobilization splints rest inflamed tissues during initial healing to provide protection and to allow inflammation to subside. If the desired position of immobilization cannot be obtained initially, serial static mobilization orthoses can safely reposition joints of the hand without providing undue stress to healing tissues. When injury is extensive and inflammation is prolonged, the rest provided by the orthosis is of continuing value. The process of tissue healing and maturation proceeds at variable rates in individuals, and many patients may have a prolonged inflammatory response.58 After the initial inflammation subsides, the injured tissues begin the proliferative stage of healing. Cells are multiplying at a rate higher than normal. During this stage, correctly applied stress has its optimal benefit in determining the length, orientation, and relationship of the collagen fibers. If patients do not respond sufficiently to gentle manual passive stretching and active exercise, the gentle force of a dynamic orthosis is usually all that is required. If there is any indication of a continuing inflammatory response (e.g., fluctuant edema, reddened joints, pain with joint motion), a serial static orthosis should be chosen to provide a balance of rest while also repositioning joints.
As the tissue matures and joint motion has significant resistance with a hard end-feel, the prolonged force of serial static or static progressive orthotic positioning is necessary. A truly resistive joint is best treated with a serial static orthosis that is not removed by the patient. Although the static progressive orthosis also provides prolonged positioning at the maximum passive length, its periodic removal allows the tissue to resume the original resting length. These recommendations are based on clinical experience and not on empirical research results. A recent study comparing dynamic to static progressive elbow mobilization via orthotic positioning demonstrated no difference between these two methods.59
A new technique of mobilizing stiffness, casting motion to mobilize stiffness (CMMS), is appropriate for the chronically stiff hand unresponsive to traditional therapy techniques. This is discussed in a subsequent section.
Basic Principles of Orthotic Mobilization
Because passive orthotic mobilization is often an integral part of effective therapy for the stiff hand, the basic principles of mobilization by orthosis are discussed in this section. The reader is directed to more in-depth information on this topic available from numerous sources.57,60-71
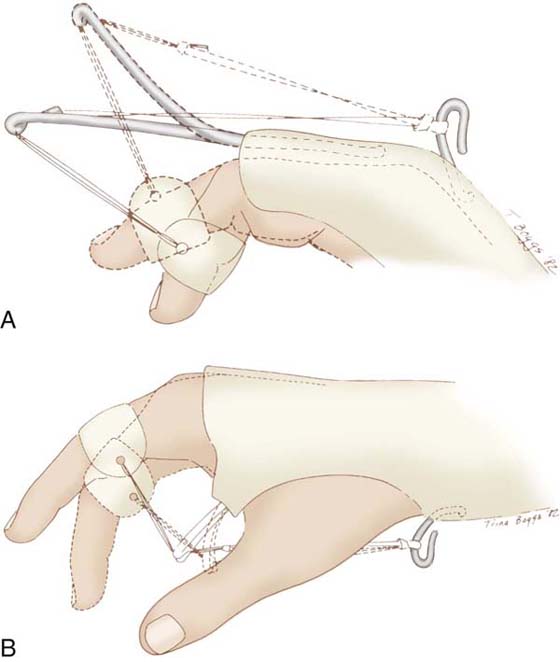
The effectiveness of any mobilization orthosis is limited by the accuracy of the design, fit, and force application. Every orthosis that immobilizes or mobilizes a joint must use three points of pressure for each joint.62 The middle force is applied directly at the axis of the joint. Without crossing another joint, the two opposite forces are placed as far away from the middle force as possible for maximum efficiency (Fig. 67-19).
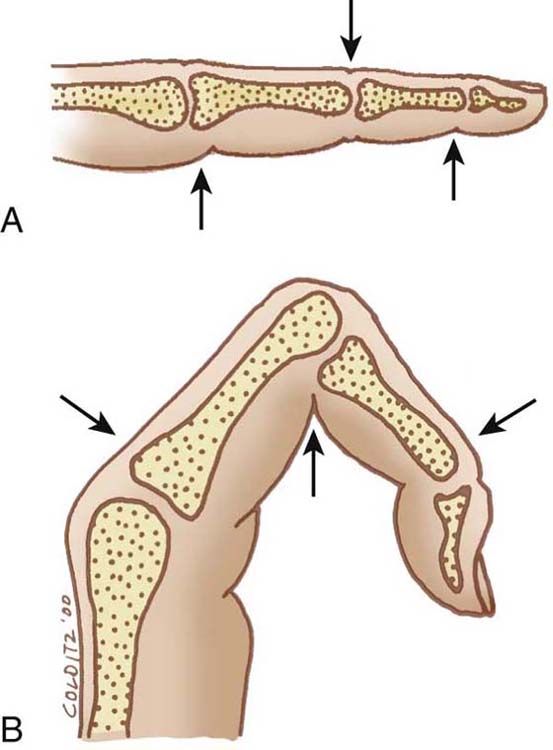
Figure 67-19 A, The three points of force for PIP joint extension orthotic positioning places the middle point of force directly on the extensor surface of the joint and the two opposite forces palmarly—as far from the joint as possible. B, The three points of force for PIP joint flexion orthotic positioning are in the same location, but on opposite surfaces to those for extension. (From Colditz JC. Efficient mechanics of PIP mobilisation splinting. Br J Hand Ther. 2000;5:65-71. Copyright 2000.)
Orthotic fabrication for extension mobilization or immobilization places the middle force over the dorsum of the joint axis, and the opposing forces are placed on the volar surface as far away as possible without crossing over another mobile joint (see Fig. 67-19A). Because there is little natural padding on the dorsum of the hand, pressure over the joint must be carefully placed and be well molded to be comfortable.
The three points of pressure for flexion mobilization orthotic fabrication are the reverse of those used for extension: Volarly over the axis of the joint with the two opposing forces applying pressure dorsally as far away from the joint as practical (see Fig. 67-19B). The difficulty in flexion mobilization orthotic fabrication is the impossibility of applying force directly over the volar aspect of a joint while also allowing room for the joint to fully flex.
Unlike extension mobilization orthoses, where the forces are almost in direct opposition, the forces may be almost at right angles in flexion mobilization orthoses. This is especially true when flexing the joints of the hand (Fig. 67-20). If the forces are at a right angle, the orthosis base shifts distally before the stiff joint moves unless the orthosis base is adequately secured.
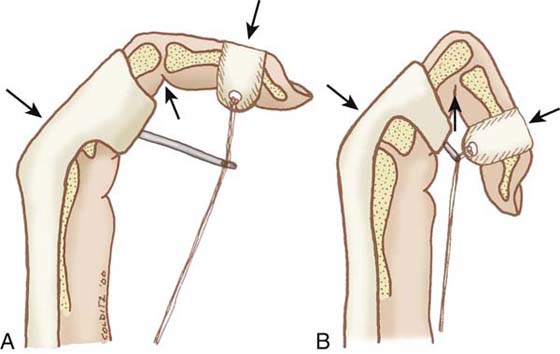
Figure 67-20 A and B, The line of force application for PIP joint flexion mobilization changes based on the angle of maximum passive flexion of the joint. (From Colditz JC. Efficient mechanics of PIP mobilisation splinting. Br J Hand Ther. 2000;5:65-71. Copyright 2000.)
Distributing Pressure Evenly. The palmar surface of the hand, with its thicker and more adherent skin and with the presence of the thenar and hypothenar muscles, can tolerate pressure more easily than the dorsum of the hand. The skin on the dorsum of the hand is thin and highly mobile. The dorsum of the hand also has multiple bony prominences that tolerate pressure poorly. For example, in low-profile dynamic or static progressive PIP joint extension mobilization designs, the orthosis is molded contiguously over the MCP joints to distribute pressure over as much of the dorsal surface as possible. The leading edge of the block ends exactly at the joint axis so that all the force is specifically directed to the precise anatomic location.62 Well-distributed pressure over the dorsal hand tissues is better tolerated than the concentrated pressure of a strap. Pressure on the neurovascular bundles of fingers can be minimized by constructing finger loops of a firm material and attaching string to both sides.64
Another example of effective pressure distribution is the use of dorsal and volar plaster slabs for serial repositioning of the wrist (or wrist and fingers). The molded volar and dorsal pieces distribute pressure over both surfaces. The three points of pressure needed to immobilize the wrist (two volarly that are proximal and distal to the wrist and one dorsally over the wrist) are widely distributed by the molded contours (see Fig. 67-17B). This is in contrast to the use of a volar slab with a strap concentrating the force over the dorsal wrist area.
Providing Constant Tension. Even distribution of pressure is the primary factor to ensure comfort with force application. Avoiding sharp edges or ill-fitting molded shapes will enhance comfortable prolonged wear. Attention to construction detail coupled with listening to the patient and modifying the orthosis readily in response to the patient’s comments will ensure maximum wear and comfort.
The tolerance to the force of dynamic or static progressive mobilization orthoses usually relates to the amount of force application. Using the minimum force the patient can tolerate for increasing amounts of time is preferable to using increasing amounts of force. The patient’s goal should be increased wearing time before force is increased. Conversely, if the patient cannot comfortably wear the orthosis beyond a few minutes and the orthosis fits well, the force should be decreased.
Ease of Adjustment. Any passive mobilization orthosis must be easy to remold, inexpensive to replace, and quick to adjust. Because the goal is increased motion, the orthosis must be adaptable to the anticipated change. Low-temperature thermoplastic materials with memory allow quick remolding and adjustments to adapt to new positions, decreased edema, or to relieve unwanted pressure. Unfortunately, thermoplastic materials with memory also limit the intimate conformity of the material to the small shapes of the hand. The use of plaster of Paris for specific clinical applications allows quick construction of a new orthosis with minimal materials cost and provides the ultimate shape conformity.72
Brass rods used as outriggers for dynamic or static progressive mobilization orthoses allow quick adjustments by bending the wire (Fig. 67-21). For example, as finger joint flexion increases, the line of pull of the finger loop must be directed closer toward the palm. Alternatively, as finger extension improves, the dorsal outrigger must be shortened and placed more proximally.
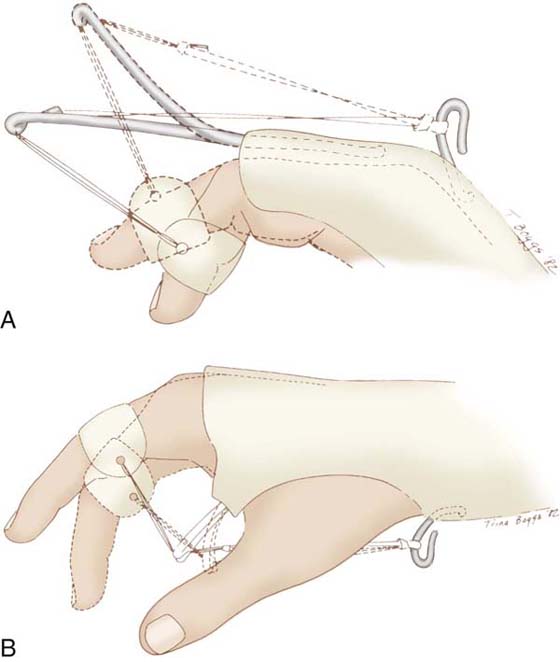
Figure 67-21 Ease of adjustment of low-profile wire outrigger system is accomplished by bending the wire outrigger. This allows maintenance of a 90-degree line of pull when either extension (A) or flexion (B) is gained. (From Colditz JC. The biomechanics of a thumb carpometacarpal immobilization splint: design and fitting. Am J Occup Ther. 1983;37:182-188. Reprinted with the permission of the American Occupational Therapy Association, Inc. Copyright 1983.)
Providing a Force Perpendicular to the Long-Bone Axis. The construction of a dynamic or static progressive mobilization orthosis requires attention to a few additional mechanical principles. To mobilize a joint, one must provide a pull at a 90-degree angle to the axis of the long bone that is the distal articulation of the joint in question64 (Fig. 67-22). The outrigger is positioned as close to the point of force application as possible. The outrigger redirects the line of pull and keeps the line close to, and parallel with, the orthosis base. This system is of value only if a secure orthosis base has been applied that is intimately conformed, has well-distributed pressure, and accurately stabilizes the proximal joints.
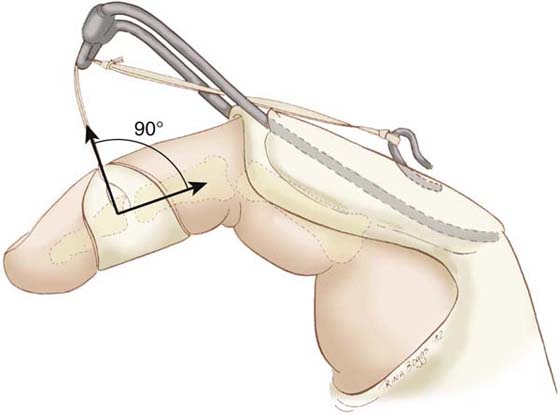
Figure 67-22 To extend the PIP joint, a low-profile dynamic (or static progressive) orthosis provides a line of pull at a 90-degree angle to the distal end of the middle phalanx. (From Colditz JC. The biomechanics of a thumb carpometacarpal immobilization splint: design and fitting. Am J Occup Ther. 1983;37:182-188. Reprinted with the permission of the American Occupational Therapy Association, Inc. Copyright 1983.)
The outrigger will deform before the tissue elongates if either the outrigger or its attachment to the orthosis base is unstable. Outrigger stability is directly correlated to length of the outrigger and the manner of attachment to the base. Attaching the outrigger over a large area of the orthosis base and to the distal edge of the orthosis contributes to maximum outrigger attachment stability.
Wearing Tolerance. When applying a passive mobilization orthosis, one must observe two areas of progress. First, the patient must be able to tolerate the orthosis comfortably for increasing periods of time. If this does not occur, the orthosis either needs adjustment or is the wrong type. Intolerance also may suggest that the orthosis has been applied at the wrong time in the healing process. Second, precise goniometric measurements must be taken before application of the orthosis. If there are no measurable gains for a few weeks after application, the orthosis is not effective. Reevaluation of the type of orthosis, the fit, and the patient’s tolerance is merited.
Many patients are encouraged by the rapid gains of motion in response to orthosis application. They become discouraged when they remove the force of the orthosis and the deformity recurs. Patients should be instructed that to maintain gains of motion made while wearing the orthosis, its prolonged use as well as concomitant active exercises will be required. (See Chapters 123 through 125 for further discussion regarding use of orthoses for mobilization of joints.)
Evaluation and Treatment of the Chronically Stiff Hand
Clinical experience and review of the literature suggests three factors that interplay to perpetuate stiffness in the chronically stiff hand (Fig. 67-23). First, there is stiffness limiting movement in multiple joints, often including uninjured joints. Adherence of multiple soft tissue layers is palpable, adding constraints to limited passive joint motion. Intermittent manual mobilization or use of a mobilization orthosis provides only a temporary reduction of the stiffness. Second, the lack of active motion has diminished the pumping ability of the lymphatic system, and chronic edema permeates all tissue planes, even sites remote from the original injury. Edema reduction efforts prove temporary, because the stiffness limits active motion and lymphatic pumping cannot be maintained. Third, because the joint stiffness and tissue adherence have caused long-term repetition of an awkward and ineffectual pattern of movement, the ineffectual pattern has become the dominant motion in the motor cortex. Even if the patient wants to move in a balanced, normal pattern, the resistance from tissue adherence and the chronic edema makes it mechanically impossible to do so. The patient continually repeats the ineffectual pattern of movement, and it remains dominant.
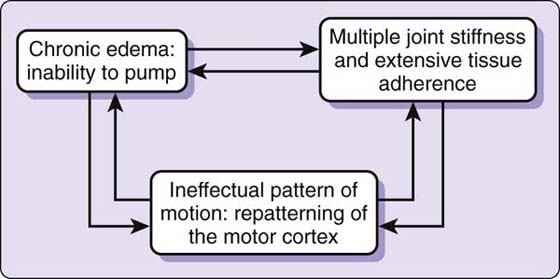
Figure 67-23 In the chronically stiff hand, three factors are interdependent, and effective mobilization requires that all factors are addressed simultaneously.
In the chronically stiff hand, these three factors of tissue adherence and stiffness, chronic edema, and motor cortex patterning are interdependent. Changing one factor alone does not change the other factors. If mobility of the stiff hand is to be regained, all three factors must be altered simultaneously (see Fig. 67-23). Such chronic stiffness can be dramatically reduced using a technique called CMMS, developed by the author.72,73 The CMMS technique is appropriate for the chronically stiff hand unresponsive to traditional therapy techniques.
Casting Motion to Mobilize Stiffness
CMMS is the use of plaster of Paris casting to selectively immobilize proximal joints in a desired position while constraining distal joints so that they move within a productive direction and range.72,73 Unlike more traditional treatment methods, the CMMS technique simultaneously mobilizes stiff joints, reduces edema, and generates a new pattern of motion to revive the cortical representation of normal motion. Traditional manual mobilization techniques and mobilization orthoses are less effective in the chronically stiff hand than in the newly stiff hand, because these techniques are intermittent and address only one problem at a time.
The CMMS technique contradicts traditional treatment theory in several ways. First and most dramatically, active motion regains both active and passive joint motion. No passive motion, modality, or manual treatment is applied. Because the cast immobilizes proximal joints and allows only the stiff joints to move in the range and direction needed, motion is isolated and part of the hand is immobilized. Typically, therapists believe that immobilization of any joint is to be avoided and motion in all directions should be gained concurrently. CMMS focuses on gaining the motion that is needed most, which may temporarily cause loss of motion in the other direction or loss of motion in the immobilized joints. This approach also contradicts the common assumption that one should never allow gains in one direction of motion at the expense of the other direction. In the chronically stiff hand, the balance of motion is overwhelmingly in favor of the stiff pattern. The constrained motion within the cast allows the opposite pattern of motion to become dominant, while simultaneously mobilizing adherent tissues and evacuating the stagnant edema. Reeducation of a more normal pattern of motion is facilitated by the restraints imposed by the cast and, when the patient is weaned from it, the motions temporarily lost while in the cast return (unless there is some specific anatomic injury preventing such return). In cases of altered anatomy following injury the therapist must be convinced that the reconstructed anatomy has the potential to return to the balanced motion before applying the CMMS technique. The same concern is not applicable to stiffness of uninjured joints resulting from immobilization.
CMMS can successfully mobilize severe stiffness that is unresponsive to traditional treatment.74 Because the patient is mobilizing only with active motion, treatment is not painful. Therapy sessions consist of reevaluation, cast changes, and home instructions, creating a cost-effective treatment approach that is overwhelming for neither the therapist nor the patient. As functional motion is regained, a very slow weaning from the cast wear is begun and the functional use of the hand continues the progression of mobilization.
To accurately convey the appropriate application of the CMMS technique, the rationale of the technique is discussed, followed by discussion of the clinical application of the technique.
Joint Stiffness and Tissue Adherence
Unlike other therapy approaches to reduce joint stiffness, CMMS uses only active motion to mobilize stiff joints. Therapists do not expect active motion alone to have the ability to mobilize a stiff joint that has an abrupt hard end to passive motion. Perhaps this disbelief arises from the assumption that, if active motion could resolve joint tightness and tissue adherence, it would have already done so. However, without the constraint of the cast directing movement to the stiffest joints, the patient will unavoidably move the more mobile joint(s) first, leaving the stiff joint with the least power and excursion during active motion. The fact that frequent cyclic active movement alone mobilizes significant joint stiffness is the most persuasive aspect of the CMMS technique.
The relative immobility of the chronically stiff hand allows development of the well-known negative effects of immobilization (see Fig. 67-23). In particular, the lack of normal stress to the tissues allows excessive crosslink formation within the collagen matrix, creating increased mechanical resistance to motion. When the hand is positioned within the cast, cyclic active motion across the stiff joints applies positive stress to the tissues, altering the crosslinking, and tissue resistance diminishes.16,35,75 Because the only motion occurring at the joint is motion within the range needed, all active movement reinforces gains in ROM. In the acutely injured hand, intermittent blocking exercises are enough to accomplish this, but in the chronically stiff hand the nonremovable cast provides the consistency needed for active motion to successfully mobilize stiff joints.
Mobilization orthoses applied to the chronically stiff hand apply an intermittent force at the end of the joint motion in one direction only. Unfortunately, the mobilization orthosis also imposes immobilization during this time, because no active tissue gliding is occurring. When the orthosis is removed, the patient reverts to the ineffectual pattern of motion, nullifying the gains of passive motion made while wearing the orthosis. The negative aspects of orthotic mobilization in the chronically stiff hand are compared with the positive aspects of the CMMS technique in Table 67-1.
Table 67-1 A Comparison of the Disadvantages of Mobilization Orthotic Positioning with the Advantages of the CMMS Technique in the Chronically Stiff Hand
Disadvantages of Mobilization Orthotic Positioning |
Advantages of CMMS |
Mobilization of Stiff Joints |
1. Immobilizes stiff joint(s) at end range. |
1. Active motion mobilizes joint at end of range. |
2. Applies force in one direction only. |
2. Active motion is possible in two opposite directions. |
3. Prevents active excursion of the soft tissues and tendon(s) across the joint. |
3. Active motion allows repeated excursion. |
Reduction of Chronic Edema |
1. Applies localized constrictive force. |
1. Applies well-distributed, light, sustained pressure and provides pseudo-massage. |
2. Can apply excessive passive force. |
2. Cannot apply excessive force. |
3. Active lymphatic pumping is lacking. |
3. Active motion facilitates lymphatic pumping. |
4. Inflammatory response may be prolonged. |
4. Diminished tissue inflammation is observable. |
Repatterning of Motor Cortex |
1. Allows no active motion. |
1. Desired active motion occurs. |
2. Intermittent use allows pathologic motion to recur when orthosis is removed. |
2. Nonremovable cast allows adequate time and repetitions for cortical repatterning. |
3. No effort is directed toward regaining normal tenodesis motion. |
3. Weaning proceeds only as patient can maintain normal tenodesis motion. |
As discussed previously, CPM has proven the effectiveness of long-term cyclic loading applied acutely after injury to prevent joint stiffness,43,45,76 but its usefulness for reducing stiffness has not been demonstrated.10,43 Undoubtedly, this is because the patient with a stiff hand reverts to the nonfunctional pattern of movement upon discontinuation of the CPM, providing no reinforcement to improved joint mobility. Intermittent blocked motion has long been used by therapists to achieve precise tendon glide across joints. The CMMS technique simply provides a sustained blocking exercise rather than an intermittent one. The CMMS technique combines stiffness reduction with simultaneous cortical repatterning of the active motion.
Because of its intermittent nature, manual passive ROM is ineffective in changing joint stiffness in the chronically stiff hand. Although there may be an immediate positive response to manual application of passive ROM in patients with chronic stiffness, they do not maintain passive gains made in a previous therapy session. Although the effects of stress deprivation on connective tissues can be prevented by both passive and active joint motion,5 there is no proven correlation between the application of passive motion and increased active motion in the chronically stiff hand. In the chronically stiff hand, because of the lack of differential reciprocal tissue glide during passive motion, passive ROM does not result in increased active ROM. If applied repeatedly and forcefully, passive ROM prolongs the inflammatory response in the chronically stiff hand.
To regain passive motion, it has been assumed that stiff joints must be held at length by applying a low-load, prolonged stress with a mobilization orthosis.8 A positive relationship between the total time a joint is held at end-range and decreased tissue resistance to passive motion has been demonstrated.38,55 However, a positive relationship between active motion and increased total end-range time has not been proven. End-range active cyclic loading77 across stiff joints provided by the CMMS technique provides an effective low-load and more prolonged force, though cyclic in nature. Not only does motion occur in the range needed, but the constraint of the cast restricts the joints from returning to the position of adaptive shortening.
The principle of using a cast to limit motion in one direction to increase active motion in the other direction has been used only in the larger joints of patients with spastic muscles. King78 reports the use of a drop-out elbow cast for spastic elbow contracture of 90 degrees of flexion. In 12 days the contracture was reduced to 12 degrees of flexion. Others report similar improvement in motion and also report a calming effect on the spasticity as a result of cast application.79-81
Edema
The chronically stiff hand is characterized by atrophic, shiny skin with diminished or absent joint creases, mild pitting (or nonpitting) edema, and firmness to palpation of the tissues throughout the hand as compared with the contralateral uninjured hand (Fig. 67-24). Edema within the joint capsule limits joint motion. When inflammation persists, pain with motion encourages patients to hold joints immobile in the most comfortable position.14,18,82,83

Figure 67-24 A chronically stiff hand shows an absence of a normal tenodesis pattern and the resulting ineffectual pattern of motion when finger flexion is attempted.
Prolonged edema continues because limited active motion restricts the pumping ability of the lymphatic system. Additionally, severe hand trauma may include direct injury to the lymphatic system. With prolonged edema, excess fibrosis from the lingering presence of high-protein edema further impedes the flow of fluid and proteins through the tissue channels to the initial lymphatics,18,21,84 resulting in a low-grade chronic inflammation.20 Although patients who have sustained trauma to the hand may have injury to the local lymphatic system, the proximal lymphatic system is normal. Lack of motion in the hand reduces the distal-to-proximal pumping that moves the lymphatic fluid to the more proximal lymphatic vessels. The CMMS technique resembles the effects of bandaging and gentle superficial massage used in manual lymphatic therapy techniques to evacuate the lymphatic fluid to more proximal areas.85
Active motion is the single most effective stimulator of the lymphatic system.20,28 The CMMS technique reduces edema by redirecting active motion to the stiffest area, which is usually the more distal joints. The absence of muscles in the digits requires that skin motion and tissue compression produced by digital flexion provide physical stimulation of the superficial lymphatics. The concurrent contraction of the intrinsic hand muscles helps move the lymphatic fluid proximally. Active movement of unconstrained proximal joints that are not in the cast continues the distal-to-proximal lymphatic pumping.
In addition to active motion of the distal joints, consistent light compression of the tissues by the cast and movement of the skin relative to the cast padding stimulates lymphatic flow.31,86 The intimately molded contour of the plaster of Paris cast provides constant light tissue pressure to facilitate lymphatic fluid movement in the delicate initial lymphatics of the skin. Gilbert87 describes the lymphatic network of the palm and fingers as much more abundant than its dorsal counterpart. The firmness of the plaster of Paris in the palm during active finger flexion may provide a more effective means of lymphatic stimulation to the hand than other treatment approaches.
Movement of the hand within the cast provides a pseudo-massage of the skin as the hand moves against the soft padded, but unyielding, contour of the cast. Because the initial lymphatics are thin, fragile structures, they are collapsed easily by vigorous massage,18,31 and such gentle but frequent facilitatory movement provides the appropriate amount of stimulation while eliminating the possibility of overly vigorous and destructive edema reduction techniques. The fact that the cast is nonremovable provides constant stimulation during cyclic active motion.
Additionally, the insulating quality of the cast provides neutral warmth, retaining body heat.78,81 Because a direct relationship exists between ambient temperature and the permeability of the initial lymphatics,88,89 this factor may also assist in increasing lymphatic flow. In addition, neutral warmth may assist in general tissue relaxation and/or facilitate tissue elongation.78,81,90 During the weaning phase, patients usually elect to wear the bivalved cast, stating that the warmth, comfort, and ability to move correctly within the cast is a comforting experience.
Because the accumulation of plasma proteins is a cause of chronic inflammation,91 stimulation of the lymphatic system by the movement within the cast reduces the observable redness and the pain associated with joint motion. The reduced pain encourages active joint motion, which in turn becomes more comfortable.
Change in the Pattern of Motion
Perhaps the most significant but least appreciated difference between the recently injured hand and the chronically stiff hand is the change in the pattern of active motion of the hand (Fig. 67-25). Local tissue adherence and/or joint tightness prevent normal synergistic motion. In chronic stiffness this maladapted pattern has been repeated long enough that the definition of movement in the cerebral motor cortex has been altered. In the chronically stiff hand this altered pattern of motion restricts both motor and sensory feedback input. Limited use of the hand creates feedback deprivation similar to rigid immobilization.92,93

Figure 67-25 A, Chronically stiff hand 7 months after flexor tendon and nerve injury at the volar wrist shows limited passive motion and poor ability to stabilize wrist in extension. B, Cast provides optimal position for active mobilization of fingers into flexion. C, Resulting range and pattern of flexion (note tenodesis is present) after a few weeks of cast wear.
Neuroscience literature has proven that animals and humans trained in movement combinations magnify the cortical representations of the motor areas predominantly used, and that lack of use decreases the cortical area.94-97 For example, squirrel monkeys given a repetitive fine motor task increase cortical representation of the small muscles of the hand while simultaneously decreasing the representation of the larger proximal muscles.98 The first dorsal interosseous muscle in the reading hand of Braille readers has a larger cortical representation than in the nondominant hand of the same person or in the hands of control subjects who do not read Braille or are not blind.99
It is therefore logical that the altered pattern of motion created by tissue adherence in the chronically stiff hand provides the opportunity for diminished cortical representation of the previous normal pattern of active motion. At the same time, the cortical area controlling the newly dominant muscle(s) enlarges. The constrained motion within the CMMS cast demands repetition of correct muscle activation, providing prolonged active movement necessary to repattern the somatosensory cortex. Although cortical representation changes rapidly based on use, for repatterning to become an ingrained automatic dominant motion, the motion must be repeated for long periods during the day and over many days or weeks.98,100-104 Repatterning is enhanced by conscious, close attention to the desired active motion.105 Unattended repetitive motion and passive motion result in little or no significant plasticity changes in the cortex,106,107 explaining why passive motion may be ineffectual in the chronically stiff hand. In the absence of permanent peripheral injury (i.e., amputation or denervation), the altered pattern can be quickly retrained to the original “normal” because the original cortical connection patterns persist and can easily be reactivated.103
Because of the long standing feedback deprivation that has caused abnormal movement pattern changes in the somatosensory cortex, regaining motion is both a complex mechanical and a cerebral issue. All too often hand therapists assume that the problem is only mechanical or related to the peripheral tissues, and are frustrated when traditional mobilization techniques are not successful.
The same dysfunctional patterns of motion are seen in the chronically stiff hand as in the newly injured hand. A wrist tenodesis pattern often is absent or altered. Wrist flexion is commonly observed when finger flexion is attempted. The key to directing normal digital movement with the CMMS cast is stabilization of the wrist in slight (20–30 degrees) extension. Even when the stiffness is localized to a single PIP joint, the wrist must be included in the cast to direct the force and tendon excursion to the stiff joint. Because the wrist is the largest joint crossed by the extrinsic muscles, its position is critical to directing excursion to the smaller joints. Positioning the wrist in slight extension takes stretch off the weakened wrist extensors56 and positions them so that they can fire synergistically with the finger flexors. If passive wrist extension is limited, a period of serial casting to bring the wrist into slight extension is required before application of the CMMS cast.
The mechanical problems of joint stiffness and tissue adherence are well described in the previous section on evaluation and treatment of early stiffness, and are described here only in relation to the desired design of the CMMS cast.
Dominant Interosseous Flexion Pattern
Normal finger flexion is initiated by the extrinsic flexor muscles, specifically the flexor digitorum profundus (FDP). The IP joints flex considerably far before significant MCP joint flexion is included.41,108 One of the most common pathologic patterns of motion typically observed in the stiff hand is digital flexion dominated by the interosseous muscles where finger flexion is initiated at the MCP joint(s) instead of at the distal interphalangeal (DIP) joint(s). If the patient has difficulty gliding the FDP tendons across the stiff IP joints, this reinforces the interosseous muscle dominance. Because the normal arc of finger flexion exhibits significant IP joint flexion before MCP joint flexion, patients demonstrating a pathologic pattern of dominant MCP joint flexion have their casts applied with the MCP joints blocked in extension.
A position of MCP joint extension reinforces extrinsic flexor tendon glide and provides maximum active tension on the flexor tendons.109 Blocking the MCP joints in extension recreates the correct initial phase of digital flexion by isolating the FDP muscle, facilitating profundus glide within the digit for IP joint motion, and preventing dominant interosseous muscle (MCP joint flexion) pattern (Fig. 67-26).
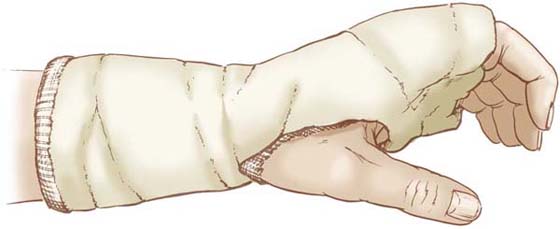
Figure 67-26 Initial cast to facilitate long-flexor glide and to mobilize IP joints includes the MCP joints, maintaining them in extension.(Copyright Judy C. Colditz, 2008.)
In the severely stiff hand with limited passive joint motion, diminished flexor tendon glide, and severe interosseous muscle tightness, it is difficult to mobilize all of these structures simultaneously. In such a circumstance, the initial cast should block the MCP joints in slight flexion (Fig. 67-27). If initially the MCP joints are positioned in full hyperextension, it is more difficult for the patient to pull against the interosseous muscle and joint tightness, and initiate motion with the extrinsic flexor muscles. Blocking the MCP joint in slight flexion allows the FDP tendon to increase its glide and mobilize the stiff IP joints before also being required to pull against the interosseous muscle–tendon unit tightness. It is simply mechanically overwhelming in the severely stiff hand to start with the MCP joints in hyperextension.
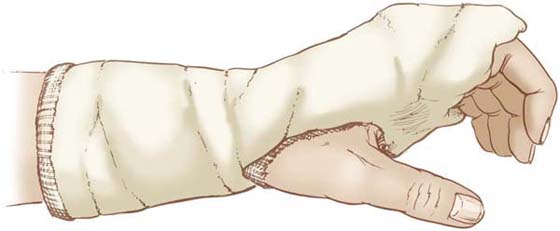
Figure 67-27 A cast positioning the MCP joints in slight flexion is desirable as a starting position if interosseous muscles are extremely tight and/or IP joint tightness is severe. This same cast position with slight MCP flexion is desirable when wanting to gain both flexion and extension of a stiff proximal IP joint.(Copyright Judy C. Colditz, 2008.)
Some patients cannot actively initiate IP flexion with the profundus muscles when the MCP joints are stabilized in extension. Although these patients are few, they have the most severe stiffness. To help the patient isolate and gain glide of the FDP tendon(s), a dorsal hood is placed over the IP joints (Fig. 67-28). This hood simply positions the DIP joints in relatively greater flexion than the PIP joints, so when the patient pulls away from the dorsal hood, the motion is initiated first with the FDP muscle(s). The patient is instructed to flex the IP joints by first moving the fingernails away from the hood.
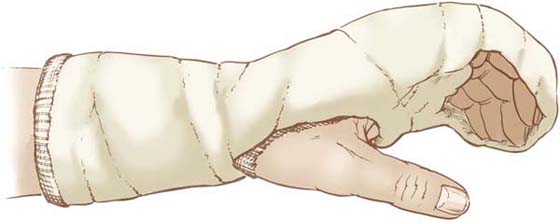
Figure 67-28 A dorsal hood made of plaster of Paris is positioned over the fingers so the DIP joints are in a starting position of relatively greater flexion than the PIP joints. This positioning facilitates initiation of finger flexion at the DIP joint(s).(Copyright Judy C. Colditz, 2008.)
The purpose of the dorsal hood is not to serially push the joints into more flexion but instead to capture the normal relative starting position of active IP joint motion. The hood positions the IP joints in the ideal relationship to one another to assure that finger flexion is instigated by the FDP muscles. Once IP joint motion is partially regained and excursion of the extrinsic flexors is reestablished within the finger, positioning the MCP joints in full extension (hyperextension) in the cast is necessary to elongate the interosseous and lumbrical muscles (Fig. 67-29). A stepwise treatment approach is the most effective; allow the FDP tendon to increase its glide and mobilize the stiff IP joints before also being required to pull against the interosseous muscle–tendon unit tightness.
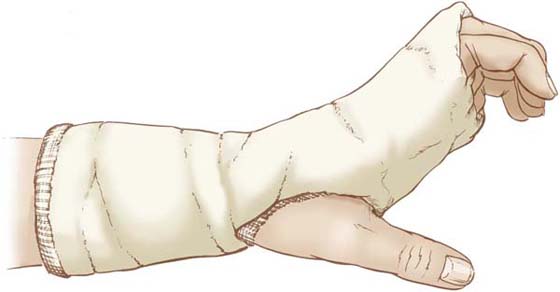
Figure 67-29 After FDP tendon glide and IP joint mobility are regained, the hand is positioned in the cast with the MCP joints in full extension (hyperextension) to allow cyclic active motion to reduce tightness of both the interosseous and lumbrical muscles.(Copyright Judy C. Colditz, 2008.)
When full IP flexion is possible while the MCP joints are held hyperextended, the MCP joint immobilization may be slowly discontinued (see later comments on weaning) and full composite finger flexion allowed. This should be considered only when the patient is able to spontaneously initiate flexion with the FDP muscles.
Some patients may however present initially with reasonable IP joint ROM and FDP tendon glide. These patients do not need to wear a cast with the MCP joints blocked in slight flexion but can immediately begin using the “intrinsic muscle stretch” cast in Figure 67-29.
In the severely stiff hand the range of finger flexion may dramatically improve when the MCP joints are blocked in the initial cast. This dramatic mechanical mobilization may tempt the therapist to begin early weaning and to think that a cast with the MCP joints held in hyperextension is unnecessary. This treatment route will be a disservice to the patient, as it is impossible to have severe chronic limited finger flexion without developing secondary interosseous muscle tightness.
Limited digital motion present in all chronically stiff hands will cause the interosseous muscles to adaptively shorten. After the patient has regained digital flexion using the profundus muscle(s), or if finger flexion is present but not full, a cast to position the MCP joints in maximum extension (hyperextension) but to allow full IP joint flexion is applied so cyclic active digital flexion elongates both the interosseus and lumbrical muscles (see Fig. 67-29). The lumbrical muscle is in its longest position when the profundus muscle is actively contracting (as a result of the proximal movement of the origin of the lumbrical muscle on the profundus tendon) while the MCP joints are in extension and the IP joints are flexed. Thus, the active hook position elongates both of these intrinsic hand muscles. If the intrinsic finger muscles are extremely tight or the patient had great difficulty in regaining profundus glide, a dorsal hood may also be attached to this cast design (Fig. 67-30). The hood is infrequently needed at this stage. Although this cast position of MCP joint hyperextension does not support functional use of the hand, its use is mandatory to reach the ultimate goal of normal ROM and functional use of the hand.
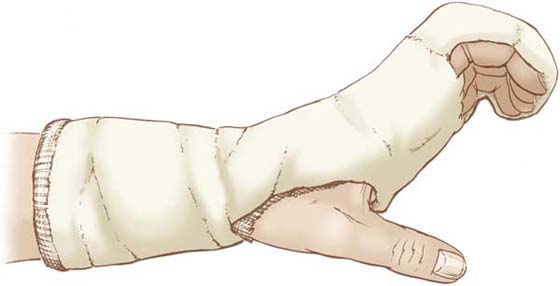
Figure 67-30 If the patient has had great difficulty isolating the extrinsic flexor muscles and regaining active IP joint flexion, it may be desirable to continue the hood as part of the cast used to elongate the intrinsic muscles.(Copyright Judy C. Colditz, 2008.)
Almost all surgical and therapy texts stress the importance of positioning the MCP joints in flexion to maintain the maximum length of the collateral ligaments. Inclusion of the extended MCP joints in the cast is contradictory to this traditional teaching. It is the increased IP active motion resulting from this position that reduces edema and demands glide of the tendons of the intrinsic muscles across the MCP joint, two factors that outweigh the temporary immobilization of these joints. Much of the cause of limited MP joint flexion is probably edema within the joint capsule, which is loose in extension but compressed in flexion. By blocking the MCP joint in full extension with the cast providing a contoured palmar pressure, edema within the MCP joints is reduced while the intrinsic muscle tendons are gliding past the MCP joint. Active IP joint flexion with the MCP joints blocked in extension demands elongation of the interosseous and lumbrical muscles. Active IP extension with the MCP joint in full extension also demands maximum muscle contraction of the interosseous muscles. Blocking the MP joints in full extension while allowing active IP joint flexion and extension thus elongates and tones the interosseous muscles. Since the interosseous muscles are the prime MCP joint flexor muscle(s), when casting is discontinued, MCP joint flexion can be regained without further specific intervention toward mobilizing the MCP joints into flexion. The only exception is if there is the presence of specific dorsal adherence resulting from dorsal trauma.
The inability to initiate finger flexion with the profundus muscles is commonly seen in the stiff hand following immobilization for a distal radius fracture or other trauma. In the initial CMMS cast, the desired relational position of DIP and PIP joint flexion may not be attainable because of joint stiffness, especially the DIP joint. After a few days in the cast the patient will gain digital flexion, but it is usually with the flexor digitorum superficialis (FDS) muscles rather than with the FDP muscles. If this occurs, the addition of a small piece of plaster of Paris or thermoplastic material over the distal edge of the dorsal hood (just over the distal phalanx) will aid in greater DIP joint flexion as the patient moves cyclically. It is important that each time the patient actively flexes, the fingernails move away from the dorsal hood before the PIP joint moves. The patient must look at and think about initiating this active motion to regain glide of the FDP tendon(s).
The complex decision-making process of applying the CMMS technique for the most common problem of regaining digital flexion in the chronically stiff hand is illustrated in Figure 67-31. This illustration only applies to stiff hands lacking full finger flexion.
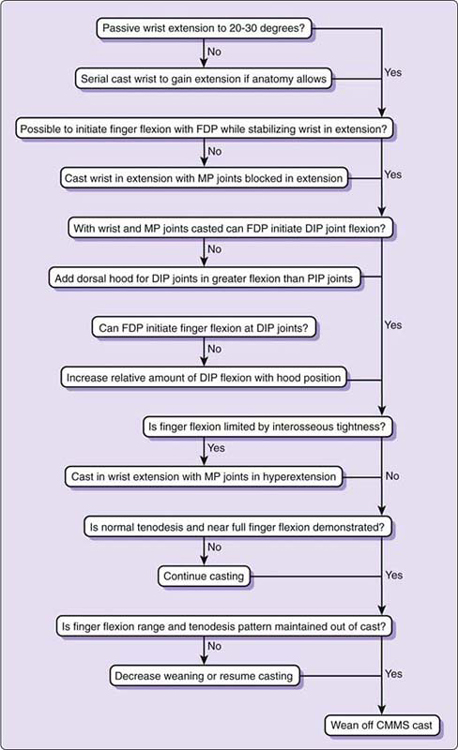
Figure 67-31 Algorithm outlining the decision-making process for the application of the CMMS technique to regain finger flexion in the chronically stiff hand.(Copyright: Judy C. Colditz, 2008.)
Dominant Extrinsic Flexion Pattern (or Intrinsic Minus)
Although the dominant intrinsic flexion pattern discussed above is the most common pattern of stiffness seen in the hand, other patterns of stiffness present that require other cast designs to effect change.
When MCP joint flexion is limited either by capsular tightness or by adherence of the extrinsic extensor system, the intrinsic muscle power to the IP joints is eliminated, explaining the term “intrinsic-minus pattern.” The intrinsic muscles cannot get into position to provide force for digital control, and the extrinsic muscles dominate the pattern of motion.
To regain MCP joint flexion, the wrist cast is applied in slight extension and a dorsal hood is placed only over the proximal phalanges, positioning them at their easy available maximum passive flexion range (Fig. 67-32). Care must be taken to assure the cast does not extend too far distally on the palmar surface, thus blocking MCP joint flexion. The patient works to actively pull the proximal phalanx away from the dorsal hood while flexing only the PIP joint with the superficialis muscle. The patient is instructed to place the fingertips on the cast and to “slide” the fingertips proximally. This exercise isolates the interosseous muscles, and cyclic loading increases the range of MCP joint flexion.
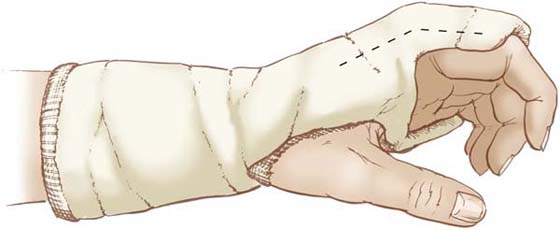
Figure 67-32 MCP joint flexion is regained by allowing cyclic active MCP joint flexion away from a dorsal block.(Copyright Judy C. Colditz, 2008.)
As MCP joint flexion increases, the cast may be changed to create a starting position of somewhat greater MCP joint flexion (Fig. 67-33). A small pad can also be inserted between the proximal phalanx and the dorsal block to position the MCP joints in slightly more flexion. The purpose is not to serially position the MCP joints in maximum flexion and hold them there, but instead to position the MCP joints in slightly greater flexion so active MCP joint flexion is within the end-range. The cast never holds the MCP joint immobile, because there is always room for the movement into and away from end-range flexion.
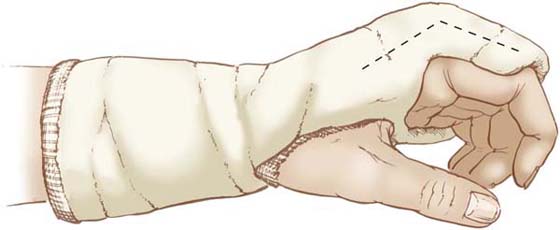
Figure 67-33 When the initial range of MCP joint flexion is regained, the MCP joints are positioned in somewhat greater flexion so they can be exercised in the available end-range of flexion.(Copyright Judy C. Colditz, 2008.)
Dominant Isolated Interphalangeal Joint Tightness
When injury is at or near a joint, isolated capsular tightness can prevent or restrict joint movement. The muscle–tendon units that normally move the joint shift their power to the adjacent unrestricted joints, diminishing the force available to mobilize the stiff joint(s). In such a circumstance the CMMS cast is applied to block all proximal joint movement (see Fig. 67-27). The wrist and all digits are included, so the overflow from the adjacent digital movement helps the patient initiate the joint motion needed. In extreme cases (seen primarily in children), the distal joints may also have to be constrained. If the patient has difficulty initiating active motion because of the severity of the joint stiffness, a dorsal hood may be needed to direct the desired range and direction of motion (see Fig. 67-28). This is only rarely required.
Traditional treatment for capsular tightness usually focuses on gaining one direction of motion at a time. Gains in one direction often create a loss of motion in the opposite direction. Energy is then directed toward resolving the lost motion, which in turn cancels out the initial gains, making the entire process minimally successful. The greatest advantage of the CMMS approach is the ability to simultaneously gain both flexion and extension in a stiff distal joint. This gain of reciprocal motion reestablishes the two-way differential glide of the tissues, and both active and passive joint motion is reestablished.
Clinical Application of CMMS
General Principles
Because the extrinsic flexors and the extrinsic extensor muscles strongly influence digital motion, the wrist must always be included in the cast and positioned in slight extension so the extrinsic muscle power is directed toward the digits. It is this position that facilitates the most effective transmission of force to the joints of the hand to mobilize them into flexion. Even if the stiffness is limited to only one digit, the other digits should be included in the cast to allow the cortical representation of the uninjured digits to assist with accurate motion.103 The only exception to this may be to allow slightly greater freedom of motion in the index finger if the stiffness is isolated to the ulnar digits.
It is important to use plaster of Paris for the CMMS technique because of its inherent intimate molding ability.72 Other synthetic casting materials are more rigid and have sharp edges. Thermoplastic splinting materials should not be substituted for the plaster of Paris, because they are readily removed and allow for poor skin tolerance to prolonged wear. Only in cases in which the stiffness is not yet chronic and shorter periods of exercise are effective can the principles of the CMMS technique be applied with thermoplastic materials.
To regain joint mobility, significant time is required. In Noyes’ study of immobilization of monkey knees, it took one year to fully resolve the flexion contracture.35 The most challenging principle for hand therapists is the amount of time in a cast required to result in permanent change in active motion for the chronically stiff hand. Although the mechanical change is usually relatively rapid, the cortical change needed for the motion to be permanently retained requires a prolonged period of repeated constrained motion. Patients with chronic stiffness may wear the cast for many weeks or a few months with few or no cast changes. When more acute injuries are being treated, tissue responds rapidly to intervention. In the chronically stiff hand, effective change takes much longer.
Treatment Guidelines
It is difficult to relay detailed treatment protocols for the CMMS technique, but general guidelines are given in the following sections. Each treatment sequence is based on the patient’s individual diagnosis, specific causes of tightness and/or lack of glide, pathologic pattern of motion, and response to the CMMS treatment. The therapist must be able to critically evaluate the stiff hand and determine the exact anatomic structures limiting motion. This knowledge determines the specific position needed to harness productive active motion within a cast. The algorithm flow chart (see Fig. 67-31) is an example of the thought process applicable to a stiff hand with limited finger flexion and interosseous muscles tightness.
Cast Design. The design of the CMMS cast is determined by the pattern of motion and locus of tightness (see Figs. 67-26 through 67-30, 67-32, and 67-33). The position for immobilizing proximal joints is not arbitrary. For example, if the PIP joint of the little finger is primarily lacking extension, one might choose to immobilize the MCP joint in significant flexion to facilitate proximal excursion of the dorsal apparatus across the joint and invite greater participation of the extensor digitorum communis. If the PIP joint of the little finger primarily lacks flexion, placing the MCP joint in full extension (or even hyperextension) drives more extrinsic flexor force across the joint toward flexion. If both flexion and extension are equally limited in the little finger PIP joint, a position of about 45 degrees of MCP joint flexion would give the best mechanical advantage for mobility of the PIP joint in both directions.
An arbitrary time period for cast wear is initially chosen. The cast is then removed to reevaluate the active pattern of motion. Observation of the new, altered, active pattern of motion determines the desired position of the proximal joints and the position of any dorsal blocks in the next cast. When the next cast is applied, usually only the position of the MCP and IP joints is changed, and the new wrist cast is applied in the same slightly extended position. The exception to this would be if there is an element of extrinsic flexor or extensor muscle tightness that requires a change of wrist position.
Time in the Cast. The most challenging aspect of the CMMS treatment for therapists is the amount of time required in the cast to repattern the motor cortex. Initial mechanical gains will be rapid, and the therapist will be tempted to immediately begin the weaning process. Experience has proven that this approach is fruitless, because the patient immediately reverts to the old maladapted pattern of motion that has remained dominant in the motor cortex. Stiffness returns.
It is important to take into account the duration of time the hand has moved in the stiff altered pattern. The longer this nonproductive pattern has been present, the longer the time required in the cast for the cortical change to be enduring. Most patients require a minimum of 2 to 4 weeks of full-time casting, although the design of the cast may be changed during this time. Patients with prolonged chronic stiffness may require 6, 8, or more weeks of full-time casting. Although this seems like a protracted period for the therapist, one must keep in mind that it is really a short period relative to the time the stiffness has been present.
Weaning Process. After a prolonged period of full-time cast wear, a period of slow weaning must occur to ensure that the patient can retain the active motion gained. Because of weakness from the chronic stiffness and from partial immobilization in the cast, the patient will quickly fatigue and revert to the previous maladaptive pattern of movement. Initially, time out of the cast should be short. The frequency of short time periods out of the cast should be increased before each time period is increased.
When the patient can display the desired ROM out of the cast while also demonstrating a spontaneous tenodesis pattern, slow weaning can begin. The cast is sawn on the radial and ulnar aspects, but the underneath padding and stockinette are cut only on the radial side. The edges of the sawn cast are covered with adhesive tape to secure the padding and stockinette and to cover the raw edges of the plaster of Paris. Circumferential hook-and-loop straps are then applied. The cast can then be removed and reapplied to allow weaning to slowly begin (Fig. 67-34).

Figure 67-34 When the patient is ready to begin weaning from the CMMS cast, the cast can be made removable by bivalving it and applying hook-and-loop straps to secure it when reapplied.
The weaning process starts with brief (about 15-minute) periods out of the cast a few times a day. The patient works actively on nonresistive tasks that use the tenodesis pattern and concentrates on moving in the correct active pattern. After 1 or 2 weeks of slightly increasing the number of times out of the cast, functional activities are added that purposefully use the desired motion but do not provide excessive resistance. The patient learns to identify when the pattern of motion is disintegrating, and returns to the cast. Awareness of how the hand should be used ensures that all motions out of the cast reinforce the gains made while in the cast.
Therapists are cautioned at this time to avoid focusing on regaining motion in the opposite direction. Contractures of the PIP or other joints will probably be present as a result of the time in the cast. If efforts are immediately directed toward eliminating the joint contractures as the weaning begins, that effort will cancel the effectiveness of the time in the cast. Only when the desired motion has been regained and the patient can maintain the motion out of the cast is any effort directed toward regaining motion in the opposite direction. In most cases the motion will slowly return with normal hand use. Therapists also should be cautioned that it is futile during the weaning period to revert to manual treatment techniques. The focus should remain on functional active motion.
Invariably, patients who are weaned too quickly will require a period of repeat casting. The treatment principles of the CMMS technique are so contradictory to traditional teaching that it will require a dramatic change in thinking to become comfortable with this treatment technique.
Contraindications
The CMMS technique should not be used unless the therapist has skill in the application of a safe and comfortable plaster of Paris cast and its safe removal. The cast must be applied perfectly, with well-distributed pressure affording perfect comfort. Precision is required to adequately block the small joints of the hand while allowing full motion of the adjacent joints. Excessive exothermic reaction of the hardening plaster of Paris must be avoided.110-113 Claustrophobic patients may not be able to tolerate the confines of the cast, and the technique should be applied judiciously to this population. The circumferential cast should never be applied to acute injuries, especially if vascular instability is present. It may be used in select postsurgical cases such as flexor tenolysis to facilitate correct tendon glide, but only after a few days in the postoperative compressive dressing.
This technique should not be indiscriminately applied to all patients with chronic stiffness. In the cases of severe trauma, the anatomic changes from an injury may eliminate the potential for regaining balanced motion, and the loss of motion created by the CMMS casting may not be regained. Elderly patients with significant osteoarthritis may have some residual extension loss of the IP joints, and they should be treated with more caution.
Historically, a great deal of time, effort, and pain endurance has been required to restore motion to the chronically stiff hand.8 In the era of increasing cost-benefit analysis, the amount of motion regained relative to the time and energy expended on treatment must be an efficient return. The CMMS treatment method simplifies the treatment approach, and even a severely stiff hand can be mobilized with only a few therapy visits and cast changes extended over a number of months. It is important to note that the CMMS treatment method was developed by the author and although there is sound theoretical basis and the author’s clinical experience supporting this technique, its use warrants prospective clinical research studies to demonstrate its effectiveness.
Summary
Understanding the causes of stiffness in the hand and choosing the type and timing of intervention is fundamental to successful mobilization of the stiff hand. A gentle approach to the tissues of the hand aimed at reducing edema and avoiding stimulation of the inflammatory response is required. The ability to influence and improve motion of the hand is the result of appropriate responses to the processes occurring in the hand. Gentle manual stretching, active motion, and use of the hand in conjunction with timely mobilizing orthoses can effectively transform the newly stiff hand into a mobile one. When the stiffness is prolonged and chronic joint tightness and tissue adherence limit motion, when chronic edema prolongs the inflammatory effect, and when the stiffness allows only a nonfunctional pattern of motion, these complex interrelated problems can be addressed with the newer technique of CMMS.
The delicate balance between tissue glide and freedom of motion can be restored, even after severe hand injuries, if the therapist provides a program of treatment based on a sound understanding of, and respect for, tissue response and the healing continuum.
REFERENCES
1. Duncan RW, Freeland AE, Jaseley MR, Maydreck EF. Open hand fractures: an analysis of the recovery of active motion and of complications. J Hand Surg [Am]. 1993;18A:387-394.
2. Weinzweig N, Weinzweig J. Basic principles and techniques in plastic surgery. Vol. I In: Cohen M, Goldwyn RM, eds. Mastery of Plastic and Reconstructive Surgery. Boston: Little, Brown; 1994.
3. Bell C. The Hand: Its Mechanisms and Vital Endowments as Evincing Design. The Bridgewater Treatise. London: Wm Pickering; 1833.
4. Watson N. What is stiffness? J Hand Ther. 1994;7(3):147-149.
5. Frank C, Akeson WH, Woo SLY, et al. Physiology and therapeutic value of passive joint motion. Clin Orthop Rel Res. 1984;185:113-125.
6. Madden JW. Wound healing: the biological basis of hand surgery. Clin Plast Surg. 1976;3(1):3-11.
7. Akeson WH, Amiel D, Abel MF, et al. Effects of immobilization on joints. Clin Orthop Rel Res. 1987;219:28-37.
8. Brand PW, Hollister AM. Clinical Mechanics of the Hand. 3rd ed St. Louis: Mosby; 1999.
9. Grauer D, Kabo JM, Dorey FJ, Meals RA. The effects of intermittent passive exercise on joint stiffness following periarticular fracture in rabbits. Clin Orthop. 1987;220:259-265.
10. Meals RA. Posttraumatic limb swelling and joint stiffness are not causally related experimental observations in rabbits. Clin Orthop. 1993;287:292-303.
11. Peacock EEJ. Some biochemical and biophysical aspects of joint stiffness: role of collagen synthesis as opposed to altered molecular bonding. Ann Surg. 1966;164(1):1-12.
12. Peacock EEJ, Cohen IK. Wound healing. In: McCarthy JG, ed. Plastic Surgery. Philadelphia: W.B. Saunders; 1990:161-185.
13. Campos AC, Groth AK, Branco AB. Assessment and nutritional aspects of wound healing. Curr Opin Clin Nutr Metab Care. 2008;11(3):281-288.
14. Hardy MA. The biology of scar formation. Hand Manage Phys Ther. 1989.(12):1014-1024.
15. Akeson WH, Amiel D, Mechanic GL, et al. Collagen cross-linking alterations in joint contractures: changes in the reducible cross-links in periarticular connective tissue collagen after nine weeks of immobilization. Connect Tiss Res. 1977;5:15-19.
16. Akeson WH, Amiel D, Woo SLY. Immobility effects on synovial joints—the pathomechanics of joint contracture. Biorheology. 1980;17:95-110.
17. Arem AJ, Madden JW. Effects of stress on healing wounds: I. intermittent noncyclical tension. J Surg Res. 1976;20:93-102.
18. Casley-Smith JR, Casley-Smith JR. High-protein oedemas and the Benzo-pyrones. Sydney: J. B. Lippincott; 1986.
19. Ganong WH. Review of Medical Physiology. 18th ed Stamford, Conne: Appleton & Lange; 1997.
20. Guyton AC, Hall J. Human Physiology and Mechanisms of Disease. 6th ed Philadelphia: WB Saunders; 1996.
21. Mortimer PS. Therapy approches for lymphedema. Angiology. 1997;48(1):87-91.
22. Asboe-Hansen G, Dyrbye M, Moltke E, Wegelius O. Tissue edema—A stimulus of connective tissue regeneration. J Invest Dermatol. 1959;32:505-507.
23. Brand PW, Wood H. Hand Volumeter Instruction Sheet. Carville, LA: United States Public Health Service. [pamphlet]
24. Waylett-Rendall J, Seibly D. A study of the accuracy of a commercially available volumeter. J Hand Ther. 1991;4:10-13.
25. Vasudevan SV, Melvin JL. Upper extremity edema control: rationale of the techniques. Am J Occup Ther. 1979;33(8):520-523.
26. Simons P, Smith PC, Lees WR, McGrouther DA. Venous pumps of the hand. Jour Hand Surg [Br]. 1996;21B(5):595-599.
27. Lotz M, Duncan M, Gerber L. Early versus delayed shoulder motion following axillary dissection. Ann Surg. 1981;193(3):288-295.
28. Namba RS, Kabo JM, Dorey FJ, Meals RA. Continuous passive motion versus immobilization. Clin Orthop Related Res. 1991;267:218-223.
29. Sorenson MK. The edematous hand. Phys Ther. 1989;69(12):1059-1064.
30. Taams KO, Ash GJ, Johannes S. Maintaining the safe position in a palmar splint: The “double-T” plaster splint. J Hand Surg [Br]. 1996;21B(3):396-399.
31. Ryan TJ, Mortimer PS, Jones RL. Lymphatics of the skin. Int J Dermatol. 1986;25(7):411-419.
32. Kasperczyk WJ, Bosch U, Oestern HJ, Tschcerne H. Influence of immobilization on autograft healing in the knee joint. A preliminary study in a sheep knee PCL model. Arch Orthop Trauma Surg. 1991;110(3):158-161.
33. Cyr L, Ross R. How controlled stress affects healing tissue. J Hand Ther. 1998;11(2):125-130.
34. Gelberman RH, Amifl D, Gonsalves M, et al. The influence of protected passive mobilization on the healing of flexor tendons. J Hand Surg [Am]. 1982;7:170-175.
35. Noyes FR. Functional properties of knee ligaments and alterations induced by immobilization. Clin Orthop Related Res. 1977;123:210-241.
36. Colditz JC. Digital Dynamics [DVD & CD]. Raleigh, NC: HandLab, a division of RHRC, Inc.; 2010.
37. Bonutti PM, Windau JE, Ables BA, Miller BG. Static progressive stretch to reestablish elbow range of motion. Clin Orthop Rel Res. 1994;303:128-134.
38. Flowers KR, LaStayo P. Effect of total end range time on improving passive range of motion. J Hand Ther. 1994;7(3):150-157.
39. Light KE, Nuzik S, Personius W, Barstrom A. Low-load prolonged stretch vs. high-load brief stretch in treating knee contractures. Phys Ther. 1984;64(3):330-333.
40. Woo SL-Y, Matthews P, Akeson WH, et al. Connective tissue response to immobility: correlative study of biomechanical measurements of normal and immobilized rabbit knees. Arth Rheum. 1975;18(3):257-264.
41. Arbuckle JD, McGrouther DA. Measurement of the arc of digital flexion and joint movement ranges. J Hand Surg [Br]. 1995;20B(6):836-840.
42. Kleim JA, Barbay S, Nudo RJ. Functional reorganization of the rat motor cortex following motor skill learning. J Neurophysiol. 1998;80(6):3321-3325.
43. Salter RB. The biologic concept of continuous passive motion of synovial joints: the first 18 years of basic research and its clinical application. Clin Orthop Related Res. 1989;242:12-25.
44. American Academy of Orthopaedic Surgeons. The Clinical Measurement of Joint Motion. Rosemont: IL; 1994.
45. O’Driscoll SW, Kumar A, Salter RB. The effect of the volume of effusion, joint position and continuous passive motion on intraarticular pressure in the rabbit knee. J Rheumatol. 1983;10(3):360-363.
46. Kottke FJ, Pauley DL, Ptak RA. The rationale for prolonged stretching for correction of shortening of connective tissue. Arch Phys Med Rehabil. 1966;47:345-352.
47. Wehbe MA, Hunter JM. Flexor tendon gliding in the hand. Part I: in vivo excursions. J Hand Surg [Am]. 1985;10A(4):570-574.
48. Wehbe MA, Hunter JM. Flexor tendon gliding in the hand. Part II: differential gliding. J Hand Surg [Am]. 1985;10(4):575-579.
49. Rudolph R. Contraction and the control of contraction. World J Surg. 1980;4:279-287.
50. Barr N. The Hand, Principles and Techniques of Simple Splintmaking in Rehabilitation. Sevenoaks, Kent, GB: Butterworths; 1975.
51. Bunch WH, Keagy RD. Principles of Orthotic Treatment. St. Louis: C.V. Mosby; 1976.
52. McClure PW, Blackburn LG, Dusold C. The use of splints in the treatment of joint stiffness: biologic rationale and an algorithm for making clinical decisions. Phys Ther. 1994;74(12):1101-1107.
53. Brand PW. The forces of dynamic splinting: ten questions before applying a dynamic splint to the hand. In: Mackin EJ, Callahan A, Skirven TM, eds., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed St. Louis: Mosby; 2002.
54. Fess EE. Rubber band traction: Physical properties, splint design and identification of force magnitude. J Hand Surg. 1984;9A:610. [Proceedings]
55. Glasgow C, Wilton J, Tooth L. Optimal daily total end range time for contracture: resolution in splinting. J Hand Ther. 2003;16(3):207-218.
56. Gossman M, Sahrmann S. Review of the length-associated changes in muscles: experimental evidence and clinical implications. Phys Ther. 1982;62:1799-1808.
57. Colditz JC. Principles of splints and splint prescription. In: Peimer CA, ed. Surgery of the Hand and Upper Extremity. New York: McGraw-Hill; 1996.
58. Bryant W. Wound healing. Clin Symp. 1977;29:3.
59. Lindenhovius A, Doornberg J, Jupiter J, et al. A prospective randomized controlled trial of dynamic vs. static progressive elbow splinting for post-traumatic elbow stiffness. Seattle, Washington: Annual Meeting American Society for Surgery of the Hand; 2007.
60. Callahan AD, McEntee P. Splinting proximal interphalangeal joint contractures: a new design. J Hand Ther. 1986;40(6):408-413.
61. Cannon NM, Foltz RW, Koepfer JM, et al. Manual of Hand Splinting. New York: Churchill Livingstone; 1985.
62. Colditz JC. Efficient mechanics of PIP mobilisation splinting. Brit J Hand Ther. 2000;5(3):65-71.
63. Colditz JC. Splinting the hand with a peripheral nerve injury. In: Mackin EJ, Callahan A, Skirven T, eds., et al. Rehabilitation of the Hand. 5th ed St. Louis: Mosby; 2002.
64. Colditz JC. Low profile dynamic splinting. Am J Occup Ther. 1983;37(3):182-188.
65. Coppard BM, Lohman H. Introduction to Splinting—A Clinical-Reasoning & Problem-solving Approach. 2nd ed St. Louis: Mosby; 2001.
66. Fess EE, Gettle KS, Philips CA, Janson JR. Hand and Upper Extremity Splinting, Principles and Methods. 3rd ed St. Louis, MO: Elsevier Mosby; 2005.
67. Jacobs ML, Austin N. Splinting the Hand and Upper Extremity: Principles and Process. Baltimore: Lippincott Williams & Wilkins; 2003.
68. McKee P, Morgan L. Orthotics in Rehabilitation. Philadelphia: F.A. Davis; 1998.
69. Van Lede P, Van Veldhoven G. Therapeutic Hand Splints—A Rational Approach. Volume I: Mechanical and Biomechanical Considerations. Antwerp, Belgium: Provan bvba; 1998.
70. Van Lede P, Van Veldhoven G. Therapeutic Hand Splints—A Rational Approach. Volume II: Practical Applications. Knokke-Heist, Belgium: Provan bvba; 2002.
71. Wilton J. Hand Splinting. London: W.B. Saunders.; 1997.
72. Colditz JC. Plaster of Paris: the forgotten splinting material. J Hand Ther. 2002;15:144-157.
73. Colditz JC. Preliminary report of a new technique for casting motion to mobilize stiffness. J Hand Ther. 2000;13(1). [Abstract]
74. Rose RL. The use of CMMS (casting motion to mobilize stiffness) to regain digital flexion following Dupuytren’s fasciectomy. Proceedings of the 10th congress of the International Federation of Societies for Surgery of the Hand and the 7th Congress of the International Federation of Societies for Hand Therapy; Medimond; Mar 2007.
75. Donatelli R, Owens-Burkhart H. Effects of immobilization on the extensibility of periarticular connective tissue. J Orthop Sports Phys Ther. 1981;3(2):67-72.
76. Van Royen BJ, O’Driscoll SW, Dhert WJA, Salter RB. A comparison of the effects of immobilization and continuous passive motion on surgical wound healing in mature rabbits. Plastic Reconst Surg. 1986;78(3):360-366.
77. Weisman G, Pope MH, John RJ. Cyclic loading in knee ligaments. Am J Sports Med. 1980;8(1):24-30.
78. King TI. Plaster splinting as a means of reducing elbow flexor spasticity: a case study. Am J Occup Ther. 1982;36(10):671-673.
79. Goya-Eppenstein P, Hill J, Philips CA, et al. Casting Protocols for the Upper and Lower Extremities. Gaithersburg, MD: Aspen Publishers; 1999.
80. Lannin NA, Novak I, Cusick A. A systematic review of upper extremity casting for children and adults with central nervous system motor disorders. Clin Rehabil. 2007;21:963-967.
81. Law M, Cadman D, Rosenbaum P, et al. Neurodevelopmental therapy and upper-extremity inhibitive casting for children with cerebral palsy. Dev Med Child Neurol. 1991;33(5):379-387.
82. deAndrade J, Grant C, Dixon A. Joint distension and reflex muscle inhibition in the knee. J Bone Joint Surg [Am]. 1965;47:313-322.
83. Young A, Stokes M, Iles JF. Effects of joint pathology on muscle. Clin Orthop Related Res. 1987;219:21-27.
84. Gaffney RM, Casley-Smith JR. Excess plasma proteins as a cause of chronic inflammation and lymphoedema: biochemical estimations. J Patholog. 1981;133:229-242.
85. Consensus Document of the International Society of Lymphology Executive Committee. The diagnosis and treatment of peripheral lymphedema. Lymphology. 1995;28:113-117.
86. Leduc O, Peeters A, Bourgeious P. Bandages: scintigraphic demonstration of its efficacy on colloidal protein reabsorption during muscle activity. Prog Lymphol. 1990;XII:421-423.
87. Gilbert A. Anatomy of the lymphatics of the upper limb. Vol. 1 In: Tubiana R, ed. The Hand. Philadelphia: W.B. Saunders; 1981.
88. Ohkuma M. Skin and lymphatic system. Prog Lymphol. 1990;X-II:45-50.
89. Xujian S. Effect of massage and temperature on the permeability of initial lymphatics. Lymphology. 1990;23:48-50.
90. Newton MJ, Lehmkuhl D. Muscle spindle response to body heating and localized muscle cooling: implications for relief of spasticity. Phys Ther. 1972;52:725-735.
91. Casley-Smith JR, Gaffney RM. Excess plasma proteins as a cause of chronic inflammation and lymphoedma: quantitative electron microscopy. J Pathol. 1981;133(3):243-272.
92. Dehne E, Torp RP. Treatment of joint injuries by immediate mobilization. Clin Orthop Rel Res. 1971;77:218-232.
93. Liepert J, Bauder H, Miltner WHR, Taub E, Weiller C. Treatment-induced cortical reorganization after stroke in humans. Stroke. 2000;31(6):1210-1216.
94. Blake DT, Byl N, Merzenich M. Representation of the hand in the cerebral cortex. Behav Brain Res. 2002;135(1-2):179-184.
95. Classen J, Liepert J, Wise S, et al. Modulation of associative human motor cortical plasticity by attention. J Neurophysiol. 1998;79(2):1117-1123.
96. Taub E. New discoevery equals change in clinical practice. J Rehabil Res Devel. 1999;36(3):237-251.
97. Taub E, Uswatte G. Constraint-induced movement therapy: a new family of techniques with broad application. J Rehabil Res Dev. 1999;36(3):vii-viii.
98. Nudo RJ, Milliken GW, Jenkins WM, Merzenich MM. Use-dependent alterations of movement representations in primary motor cortex of adult squirrel monkeys. J Neurosci. 1996 15;16(2):785-807.
99. Pascual-Leone A, Cammarota A, Wassermann EM, et al. Modulation of motor cortical outputs to the reading hand of Braille readers. Ann Neurol. 1993;34:33-37.
100. Bonaiuti D, Rebasti L, Sioli P. The Constraint Induced Movement Therapy: a systematic review of randomised controlled trials on the adult stroke patients. Eur Medicophys. 2007;43(2):139-146.
101. Szaflarski JP, Page SJ, Kissela BM, et al. Cortical reorganization following modified constraint-induced movement therapy: a study of 4 patients with chronic stroke. Arch Phys Med Rehabil. 2006;87(8):1052-1058.
102. Hoare B, Imms C, Carey L, Wasiak J. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: a Cochrane systematic review. Clin Rehabil. 2007;21(8):675-685.
103. Kaas JH. Plasticity of sensory and motor maps in adult mammals. Annu Rev Neurosci. 1991;14:137-167.
104. Merzenich M, Kaas J, Wall J, et al. Progression of change following median nerve section in the cortical representation of the hand in areas 3b and 1 in adult owl and squirrel monkeys. Neuroscience. 1983;10:639-665.
105. Page S, Levine P, Hill V. Mental practice as a “gateway” to modified constraint-induced therapy: A promising combination to improve function. Am J Occup Ther. 2007;61(3):321-327.
106. Byl NN, Merzenich M, Jenkins WM. A primate genesis model of focal dystonia and repetitive strain injury: I. Learning-induced dedifferentiation of the representation of the hand in the primary somatosensory cortex in adult monkeys. Neurology. 1996;47:508-520.
107. Merzenich M, Jenkins WM. Reorganization of cortical representation of the hand following alterations of skin inputs induced by nerve injury, skin island transfer and experience. J Hand Ther. 1993;6:89-94.
108. Somia N, Rash GS, Wachowiak M, Gupta A. The initiation and sequence of digital joint motion. J Hand Surg. 1998;23B(6):792-795.
109. Savage R. The influence of wrist position on the minimum force required for active movement of the interphalangeal joints. J Hand Surg [Am]. 1988;13-B(3):262-268.
110. Becker DJ. Danger of burns from fresh plaster splints surrounded by too much cotton. Plast Reconstr Surg. 1978;62:436-437.
111. Gannaway JK, Hunter JR. Thermal effects of casting materials. Clin Orthop. 1983;181:191-195.
112. Hedeboe J, Larsen FM, Lucht U, Christensen ST. Heat generation in plaster-of-Paris and resulting hand burns. Burns Incl Therm Inj. 1982;9(1):46-48.
113. Woo K. Techniques in Surgical Casting and Splinting. Philadelphia: Lea & Febiger; 1987.