8 MEDIASTINUM: ANATOMY, MASSES AND AIR
The mediastinum is situated between the pleurae covering the medial aspects of the right and left lungs. Its borders are the thoracic inlet (superiorly), the diaphragm (inferiorly), the parietal pleurae (laterally), the vertebral column (posteriorly) and the sternum (anteriorly).
At the root of each lung the lateral parietal pleural boundary is absent.
ANATOMICAL COMPARTMENTS
Anatomists and surgeons use various classifications to define the mediastinal compartments. Felson1 and Zylak2 have pointed out that, in terms of CXR diagnosis, a simple longitudinal division is most relevant.
We like Felson’s description1. He divided the mediastinum into three compartments—anterior, middle and posterior—there being no need to refer to a superior compartment.
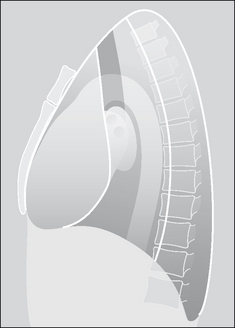
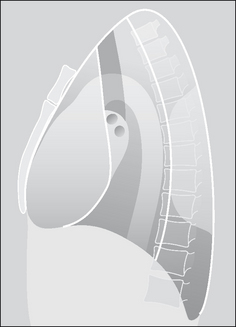
The anatomical compartments are best understood with reference to the lateral CXR (Figs 8.1 and 8.2).
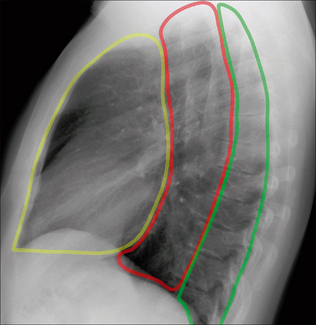
Figure 8.1 The anterior, middle and posterior compartments of the mediastinum are easy to identify on the lateral CXR.
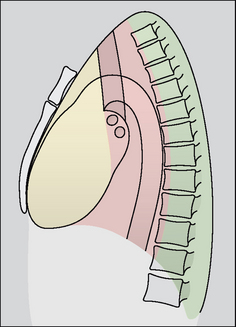
Figure 8.2 The three anatomical compartments: anterior, middle and posterior—as described by Felson1.
Table 8.1 Mediastinal boundaries.
| Compartment | Anteriorly | Posteriorly |
|---|---|---|
| Anterior | Sternum | Anterior aspect of trachea and posterior margin of heart |
| Middle | Anterior aspect of trachea and posterior margin of heart | A vertical line drawn along the thoracic vertebrae 1 cm behind their anterior margins |
| Posterior | Vertical line drawn along the thoracic vertebrae 1 cm behind their anterior margins | Costovertebral junctions |
Table 8.2 Mediastinal contents.
| Compartment | Main structures/tissues |
|---|---|
| Anterior | Fat, lymph nodes, thymus/thymic remnant, heart, ascending aorta |
| Middle | Trachea, bronchi, lymph nodes, oesophagus, descending aorta |
| Posterior | Paravertebral soft tissues |
CXR APPEARANCES—NORMAL
FRONTAL CXR
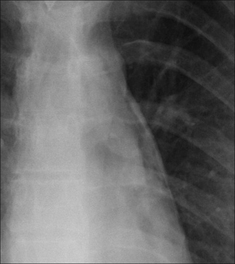
In adults the normal mediastinal shadow is in effect the cardiac outline, the thoracic aorta, the superior vena cava, and the vessels arising from the aortic arch.
In young adults neither the aortic arch nor its vessels are prominent and they contribute very little to the outline of the mediastinum. In middle age unfolding of the aortic arch occurs. As we get even older, other vessels become tortuous and the mediastinal contour continues to widen and alter (Fig. 8.3).
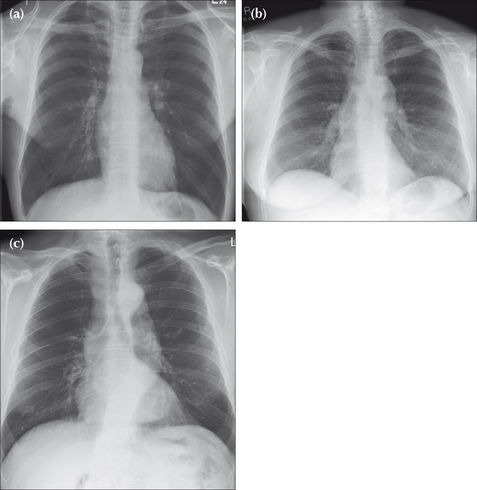
Figure 8.3 The normal mediastinal outline can change with age. In particular, the ascending and descending aorta unfolds and becomes more prominent from middle age onwards. (a) Age 30. (b) Another patient, age 50. (c) An elderly patient, age 80.
Some normal mediastinal appearances on the frontal CXR may be confusing or puzzling; particularly fat collections (Figs 8.4 and 8.5) and various interface lines (Figs 8.6-8.13).
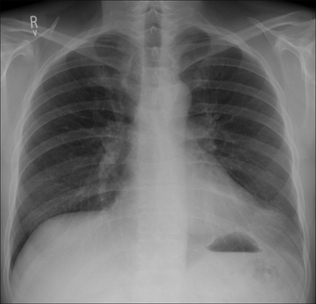
Figure 8.4 The media-stinum often contains small or large collections of fat. In this patient a large fat collection (or pad) is situated at the left cardiophrenic angle.
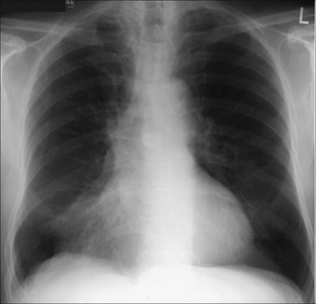
Figure 8.5 A prominent fat pad blurs part of the right cardiac border. Sometimes this blurring is mistaken for middle lobe disease (see pp. 49 and 238).
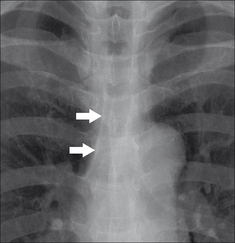
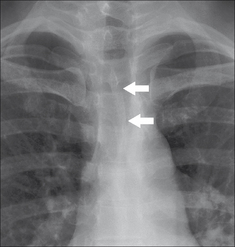
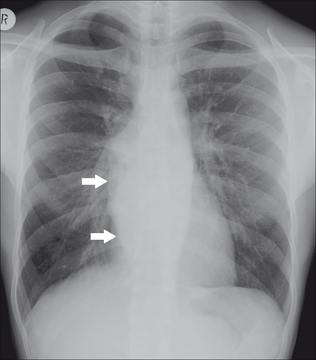
Figure 8.6 A normal right paratracheal stripe (arrows). The stripe represents the right wall of the trachea outlined by the air in the trachea and the air in the adjacent right lung. The thickness of this stripe should not exceed2.5 mm (see data on p. 242).
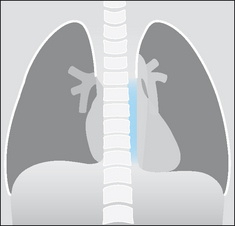
Figure 8.7 Normal left paravertebral stripe (blue). Compare this with the CXR appearance in Fig. 8.9.
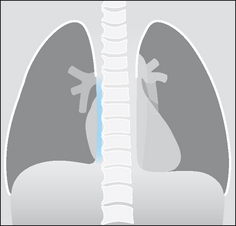
Figure 8.8 A right paravertebral stripe (blue) is rarely seen on a normal frontal CXR—unless age related osteophytes are present.
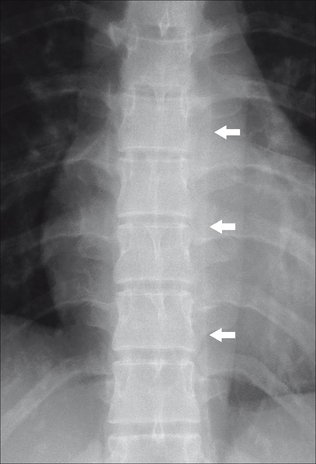
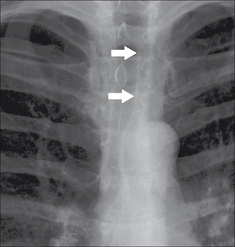
Figure 8.9 Normal left paravertebral stripe (arrows). This is the interface between the lung and the paravertebral soft tissues. Note that a right paravertebral stripe is not evident.
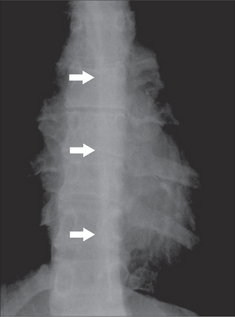
Figure 8.10 Normal azygo-oesophageal line (arrows). This lung–soft tissue interface is visible on many CXRs.
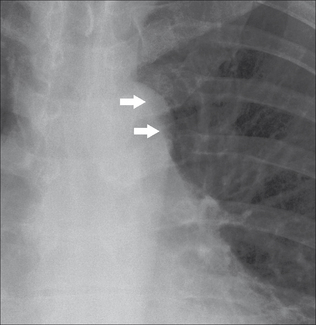
Figure 8.13 The aorto-pulmonary stripe (arrows). A normal, but uncommon, appearance. It alters the usual configuration seen between the main pulmonary artery and the arch of the aorta. This normal variant (a pleural reflection) may cause confusion.
Fat collections3
Visible pads of fat are present at the right and/or left cardiophrenic angles in approximately 50% of patients aged 50 or older (see Chapter 16, p. 239). If a large fat collection is present it may:
Interface lines and stripes
The air in the lung abuts various mediastinal structures. Where the interface is long and vertical it results in a longitudinal or slightly angled line on the CXR. These normal shadows can baffle the novice. Their occurrence on a CXR varies from individual to individual.
There are six mediastinal lines (stripes) that are regularly seen on normal CXRs. Two of these stripes can be helpful in detecting an abnormality. Specifically:
NB: the left side of the trachea does not interface with the lung, so there is no matching stripe on the left side.
 The paravertebral stripes4,5:
The paravertebral stripes4,5:
 The left paravertebral stripe is visualised on almost all well-penetrated CXRs. This is because the descending aorta displaces the adjacent lung laterally. This displacement causes the pleural surface and lung edge to be seen tangentially as they pass lateral to the paravertebral soft tissues from front to back.
The left paravertebral stripe is visualised on almost all well-penetrated CXRs. This is because the descending aorta displaces the adjacent lung laterally. This displacement causes the pleural surface and lung edge to be seen tangentially as they pass lateral to the paravertebral soft tissues from front to back. A right paravertebral stripe is not visualised until middle age, when age related osteophytes are often present and may displace the adjacent pleura laterally (Fig. 8.8).
A right paravertebral stripe is not visualised until middle age, when age related osteophytes are often present and may displace the adjacent pleura laterally (Fig. 8.8).Four other lines or stripes also occur.
 Posterior junction line:
Posterior junction line:
 Formed where the two lungs abut each other posteriorly. It extends from above the clavicles to the level of the arch of the aorta (Fig. 8.12).
Formed where the two lungs abut each other posteriorly. It extends from above the clavicles to the level of the arch of the aorta (Fig. 8.12). Aorto-pulmonary stripe:
Aorto-pulmonary stripe:
 In some people a segment of mediastinal pleura does not blend with the outline of the mediastinum but is reflected as a straight line between the main pulmonary artery and the aortic arch (Fig. 8.13).
In some people a segment of mediastinal pleura does not blend with the outline of the mediastinum but is reflected as a straight line between the main pulmonary artery and the aortic arch (Fig. 8.13).LATERAL CXR
Mediastinal shadows show age related differences due to progressive unfolding of the ascending and descending thoracic aorta (see Chapter 2, Figs 2.32 and 2.33).
Fat collections and the cardiac incisura
Fat at the cardiophrenic angles (often a feature of middle-aged prosperity) are superimposed over each other on the lateral CXR. In addition, the apex of the heart intrudes onto and displaces part of the left lung. This combination of epicardial fat and the cardiac apex (the latter creating the cardiac incisura) sometimes produces a fairly dense shadow situated anteriorly (see Chapter 2, Figs 2.33 and 2.34).
Lines and stripes
Two stripes are visible on most lateral CXRs.
 The posterior tracheal stripe. This is produced by the interface between the posterior wall of the trachea and the adjacent lung (Fig. 8.14).
The posterior tracheal stripe. This is produced by the interface between the posterior wall of the trachea and the adjacent lung (Fig. 8.14). The retrosternal soft tissue margin (or stripe). A small amount of fat and connective tissue lies between the parietal pleura and the sternum. On the lateral CXR this narrow soft tissue interface (it is only occasionally referred to as a stripe or a line) is readily visualised (Fig. 8.14).
The retrosternal soft tissue margin (or stripe). A small amount of fat and connective tissue lies between the parietal pleura and the sternum. On the lateral CXR this narrow soft tissue interface (it is only occasionally referred to as a stripe or a line) is readily visualised (Fig. 8.14).MEDIASTINAL MASSES
MASSES—OFTEN OBVIOUS…SOMETIMES SUBTLE
Obvious
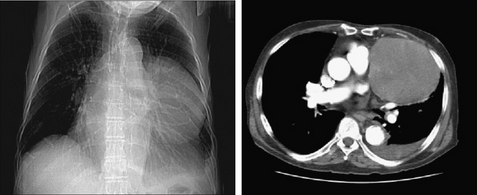
Many mediastinal masses are large. Most of these will be readily apparent on the frontal CXR (Fig. 8.15). You should attempt to place the mass within a particular mediastinal compartment in order to create a helpful differential diagnosis. The key to doing this is to decide which particular structure(s) the mass lies against (see below).
Subtle
Small mediastinal masses may be difficult to detect. This occurs when the mass barely projects or does not project beyond the mediastinal boundaries—i.e. the normal mediastinal silhouette remains superficially or truly unaltered.
Three key features can help you to detect such a mass.
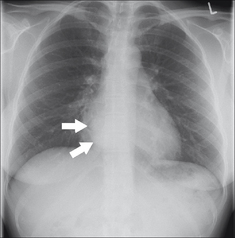
Figure 8.16 Density alteration. Increased density (arrows) over the right side of the heart adds to the suggestion of a mediastinal mass. Bronchogenic cyst.
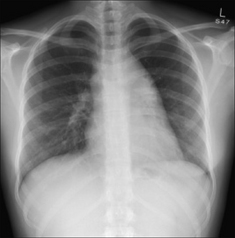
Figure 8.17 Contour alteration. Widening of the mediastinum to the right and left sides is evident. Lymphoma. (Incidentally, this is a good example of the hilum overlay sign1, described in Chapter 16, p. 233).
CREATING A DIFFERENTIAL DIAGNOSIS
| Compartment | Common causes | Notes |
|---|---|---|
| Anterior | The Four Ts: | |
| Middle | ||
| Posterior |
In order to create a helpful differential diagnosis, you should attempt to place the mass in a particular compartment. This can often be done reasonably accurately using the frontal CXR alone. The lateral CXR will almost always reinforce your frontal view assessment.
On the frontal CXR
The silhouette sign (p. 45) is the key.
 An anterior mediastinal mass lies adjacent to the heart. It may efface a heart border or the margin of the ascending aorta. It will not efface the hila nor widen a paraspinal line (Fig. 8.19).
An anterior mediastinal mass lies adjacent to the heart. It may efface a heart border or the margin of the ascending aorta. It will not efface the hila nor widen a paraspinal line (Fig. 8.19). A middle mediastinal mass may splay the carina or efface a normal hilar shadow. It will not efface a heart border nor widen a paraspinal line (Fig. 8.20).
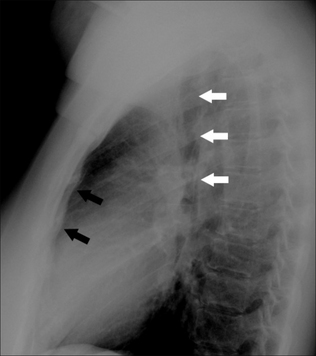
A middle mediastinal mass may splay the carina or efface a normal hilar shadow. It will not efface a heart border nor widen a paraspinal line (Fig. 8.20). A posterior mediastinal mass will displace either or both of the paravertebral stripes laterally. It may also widen the space between adjacent ribs and may destroy or erode a vertebra or a rib. It will not efface a heart border or a hilar shadow (Fig. 8.21).
A posterior mediastinal mass will displace either or both of the paravertebral stripes laterally. It may also widen the space between adjacent ribs and may destroy or erode a vertebra or a rib. It will not efface a heart border or a hilar shadow (Fig. 8.21).
Figure 8.19 The region of the right heart border is abnormal. The border is very prominent and it has a most unusual shape for an enlarged right atrium. Anterior mediastinal mass.
On the lateral CXR
The lateral CXR will help to confirm or to modify the assessment that you have made from the frontal view. Trace Felson’s mediastinal boundaries (Fig. 8.2) and place the main bulk of the mass in the appropriate compartment.
Figure 8.22 An abrupt change in density is evident across the cardiac shadow. Anterior mediastinal mass.
Some helpful hints—frontal and lateral CXRs
 The most common anterior mediastinal mass is an enlarged retrosternal thyroid. This mass will almost always displace or narrow the trachea. Its well-defined margins will fade out above the clavicles (the cervicothoracic sign—see Chapter 16, pp. 234–235).
The most common anterior mediastinal mass is an enlarged retrosternal thyroid. This mass will almost always displace or narrow the trachea. Its well-defined margins will fade out above the clavicles (the cervicothoracic sign—see Chapter 16, pp. 234–235). Linear calcification is often seen in vascular masses (e.g. an aneurysm). Occasionally a thymoma or a teratoma will also calcify.
Linear calcification is often seen in vascular masses (e.g. an aneurysm). Occasionally a thymoma or a teratoma will also calcify. Lymphadenopathy can be seen in any compartment but is particularly common at or around the hila. Enlarged nodes tend to produce a lumpy, bumpy contour.
Lymphadenopathy can be seen in any compartment but is particularly common at or around the hila. Enlarged nodes tend to produce a lumpy, bumpy contour. An aortic aneurysm will follow the course of the aorta. Often a normal aortic knuckle will not be identified.
An aortic aneurysm will follow the course of the aorta. Often a normal aortic knuckle will not be identified. A fixed hiatus hernia (middle mediastinum in position) can often be diagnosed from the frontal CXR. It shows an increased density overlying the heart. Usually it extends to the left of the midline. Classically, it will contain gas. An air–fluid level is often visible. See p. 320.
A fixed hiatus hernia (middle mediastinum in position) can often be diagnosed from the frontal CXR. It shows an increased density overlying the heart. Usually it extends to the left of the midline. Classically, it will contain gas. An air–fluid level is often visible. See p. 320.GAS IN THE MEDIASTINUM—PNEUMOMEDIASTINUM
Some aspects of pneumomediastinum are included on pp. 104–105 in Chapter 7; in particular, the causes for a co-existing pneumothorax and pneumomediastinum are explained.
The mediastinum communicates with extrathoracic sites via numerous fascial planes. Air in the mediastinum can dissect along these planes and may be seen in various positions outside the thorax. These extrathoracic sites include the:
PNEUMOMEDIASTINUM: CAUSES
The most common cause is rupture of an alveolus. There are other causes(Table 8.4). When an alveolus ruptures, the air dissects along vascular bundles within the lung to reach the root of the lung. From the lung root the air enters the mediastinal soft tissues (Fig. 8.25).
Table 8.4 Causes of pneumomediastinum.
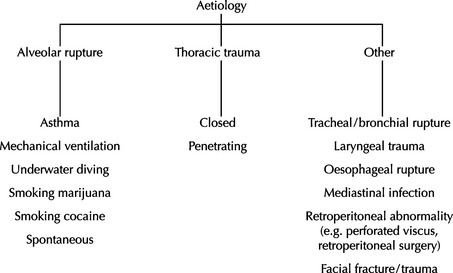 |
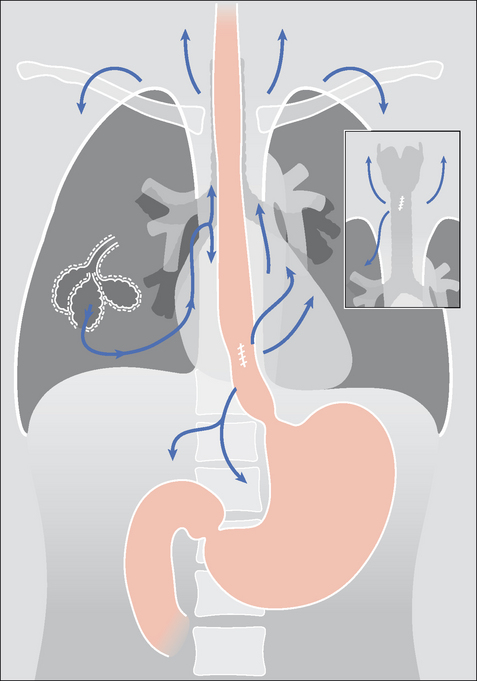
Figure 8.25 Air or gas can enter the mediastinum as a result of different pathological processes. These include rupture of an alveolus, tracheal or bronchial rupture, or a tear in the wall of the oesophagus. The air commonly extends into the neck. Very occasionally the mediastinal air dissects inferiorly into the retroperitoneum.
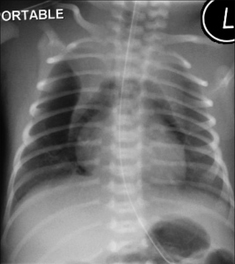
PNEUMOMEDIASTINUM: CXR APPEARANCES2,6-9
One, some, or all of these findings may be present:
 The “continuous diaphragm sign”. Normally the central part of the diaphragm is not visualised on a frontal CXR because it is not in contact with lung. Mediastinal gas can dissect along this tissue plane. Consequently the entire surface of the diaphragm may be visible (Fig. 8.26).
The “continuous diaphragm sign”. Normally the central part of the diaphragm is not visualised on a frontal CXR because it is not in contact with lung. Mediastinal gas can dissect along this tissue plane. Consequently the entire surface of the diaphragm may be visible (Fig. 8.26). A lucent (black) halo surrounding the heart. This is air. It may elevate the mediastinal pleura away from the heart (Fig. 8.26).
A lucent (black) halo surrounding the heart. This is air. It may elevate the mediastinal pleura away from the heart (Fig. 8.26). Air around the arteries arising from the aortic arch. Appearing as black rings and often referred to as the “ring around the artery sign”, or the “tubular artery sign”.
Air around the arteries arising from the aortic arch. Appearing as black rings and often referred to as the “ring around the artery sign”, or the “tubular artery sign”.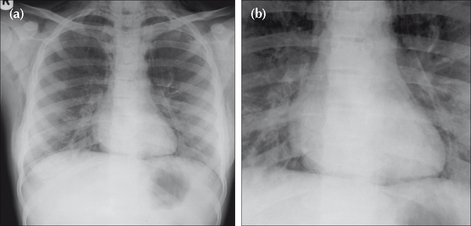
Figure 8.26 Acute asthma (a). Very small bilateral pneumothoraces were evident. Air has also dissected into the mediastinum and resulted in surgical emphysema extending into the neck and the anterior chest wall. The blown-up image (b) shows: (1) the continuous diaphragm sign; and (2) a halo of air surrounding the heart.
PNEUMOMEDIASTINUM VERSUS OTHER GAS COLLECTIONS
Pneumomediastinum versus pneumopericardium
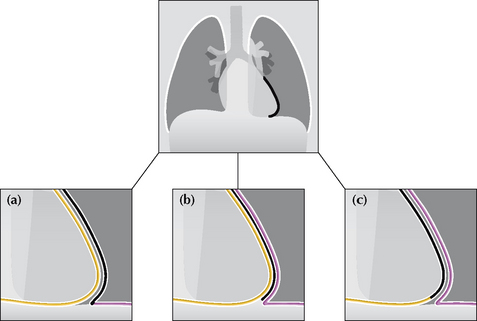
Figure 8.29 A sharp black line around the cardiac margin may be due to: (a) air in the pleural space adjacent to the heart (pneumothorax); or (b) air in the mediastinal soft tissues (pneumomediastinum); or (c) air in the pericardial sac (pneumopericardium). Occasionally, this appearance is mimicked by a Mach effect (see p. 128).
 A pneumopericardium can mimic a pneumomediastinum. It usually results from penetrating trauma or immediately following thoracic surgery.
A pneumopericardium can mimic a pneumomediastinum. It usually results from penetrating trauma or immediately following thoracic surgery.Pneumomediastinum versus pneumothorax
Sometimes air in the medial pleural space (pneumothorax) will outline the lateral margin of the heart and can be mistaken for a pneumomediastinum.
If you are in doubt as to where the air is situated—obtain a lateraldecubitus CXR (see p. 231).
POTENTIAL PITFALL: THE MACH EFFECT10
Sometimes a normal CXR will show a thin, well-defined, black line around one or both lateral margins of the heart. This is an optical illusion resulting from overlap of superimposed normal structures. This illusion is known as a Mach band or Mach effect.
Whenever a sharp black line is seen adjacent to a heart border the possibility of a pneumomediastium or a pneumothorax must be considered. Nevertheless, an unimportant Mach band must be kept in mind. Invariably, the clinical features will make a Mach band likely or unlikely. If uncertainty persists then a lateral decubitus CXR will clarify (see Chapter 16, p. 231).
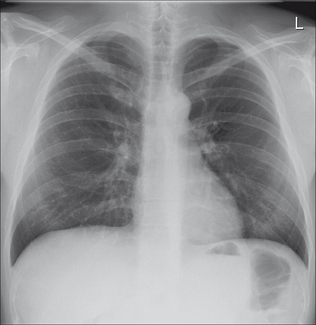
Figure 8.30 A Mach effect10 is responsible for the sharp black line adjacent to the left heart border. An occasional normal appearance which can be misinterpreted as a pneumomediastinum. In practice, the clinical features will usually distinguish between a Mach effect and air in the soft tissues.
PNEUMOMEDIASTINUM IN AN INFANT
See Chapter 15, pp. 208–210.
AN INTERESTING CONDITION—SPONTANEOUS PNEUMOMEDIASTINUM
Aetiology/pathology
Alveolar rupture. Thought to be linked to Valsalva’s manoeuvre (e.g. athletic activity, defaecation, parturition, marijuana smoking, use of cocaine).
1. Felson B. Chest Roentgenology. Philadelphia, PA: WB Saunders, 1973.
2. Zylak CM, Standen JR, Barnes GR, et al. Pneumomediastinum revisited. Radiographics. 2000;20:1043-1057.
3. Price JE, Rigler LG. Widening of the mediastinum resulting from fat accumulation. Radiology. 1970;96:497-500.
4. Genereux GP. The posterior pleural reflections. AJR. 1983;141:141-149.
5. Donnelly LF, Frush DP, Zheng JY, et al. Differentiating normal from abnormal inferior thoracic paravertebral soft tissues on chest radiography in children. AJR. 2000;175:477-483.
6. Rohlfing BM, Webb WR, Schlobohm RM. Ventilator related extra-alveolar air in adults. Radiology. 1976;121:25-31.
7. Westcott JL, Cole SR. Interstitial pulmonary emphysema in children and adults; roentgenographic features. Radiology. 1974;111:367-378.
8. Bejvan SM, Godwin JD. Pneumomediastinum: old signs and new signs. AJR. 1996;166:1041-1048.
9. Han SY, McElvein RB, Aldrete JS, et al. Perforation of the oesophagus: correlation of site and cause with plain film findings. AJR. 1985;145:537-540.
10. Chasen MH. Practical applications of Mach band theory in thoracic analysis. Radiology. 2001;219:596-610.