CHAPTER 60 Resective Osseous Surgery
The damage resulting from periodontal disease manifests in variable destruction of the tooth-supporting bone. Generally, bony deformities are not uniform; they are not indicative of the alveolar housing of the tooth before the disease process and do not reflect the overlying gingival architecture. Bone loss has been classified as either “horizontal” or “vertical,” but in fact, bone loss is most often a combination of horizontal and vertical loss. Horizontal bone loss generally results in a relative thickening of the marginal alveolar bone because bone tapers as it approaches its most coronal margin.
The effects of this thickening and the development of vertical defects leave the alveolar bone with countless combinations of bony shapes. If these various topographic changes are to be altered to provide a more physiologic bone pattern, a method for osseous recontouring must be followed.
Osseous surgery may be defined as the procedure by which changes in the alveolar bone can be accomplished to rid it of deformities induced by the periodontal disease process or other related factors such as exostosis and tooth supraeruption.
Osseous surgery can be either additive or subtractive in nature. Additive osseous surgery includes procedures directed at restoring the alveolar bone to its original level, whereas subtractive osseous surgery is designed to restore the form of preexisting alveolar bone to the level present at the time of surgery or slightly more apical to this level (Figure 60-1).
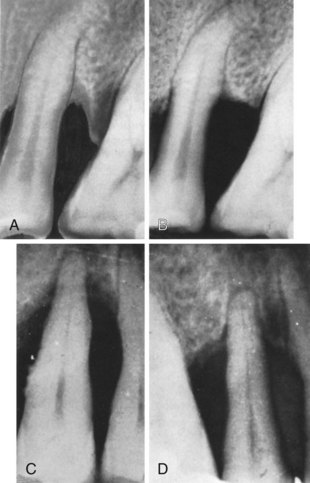
Figure 60-1 Additive and subtractive osseous surgery. A, Before, and B, immediately after subtractive osseous surgery; the osseous wall of the two adjoining infrabony pockets has been removed. C, Before, and D, 1 year after additive osseous surgery; the area has been flapped and thoroughly instrumented, resulting in reconstruction of the interdental and periapical bone.
(Courtesy Drs. E.A. Albano and B.O. Barletta, Buenos Aires, Argentina.)
Additive osseous surgery brings about the ideal result of periodontal therapy; it implies regeneration of lost bone and reestablishment of the periodontal ligament, gingival fibers, and junctional epithelium at a more coronal level. This type of osseous surgery is discussed in Chapter 61.
Subtractive osseous surgery procedures provide an alternative to additive methods and should be used when additive procedures are not feasible. These subtractive procedures are discussed in this chapter.
Selection of Treatment Technique
The morphology of the osseous defect largely determines the treatment technique to be used. One-wall angular defects usually need to be recontoured surgically. Three-wall defects, particularly if they are narrow and deep, can be successfully treated with techniques that strive for new attachment and bone reconstruction. Two-wall angular defects can be treated with either method, depending on their depth, width, and general configuration. Therefore, except for one-wall defects and wide, shallow two-wall defects, along with interdental craters, osseous defects are treated with the objective of obtaining optimal repair by natural healing processes.
Rationale
Osseous resective surgery necessitates following a series of strict guidelines for proper contouring of alveolar bone and subsequent management of the overlying gingival soft tissues. The specifics of these techniques are discussed later in this chapter. The techniques discussed here for osseous resective surgery have limited applicability in deep intrabony or hemiseptal defects, which could be treated with a different surgical approach (see Chapter 61). Osseous surgery provides the purest and surest method for reducing pockets with bony discrepancies that are not overly vertical and also remains one of the principal periodontal modalities because of its long-term success and predictability.
Osseous resective surgery is the most predictable pocket reduction technique.10-12 However, more than any other surgical technique, osseous resective surgery is performed at the expense of bony tissue and attachment level.1,2,8 Thus its value as a surgical approach is limited by the presence, quantity, and shape of the bony tissues and by the amount of attachment loss that is acceptable.
The major rationale for osseous resective surgery is based on the tenet that discrepancies in level and shapes of the bone and gingiva predispose patients to the recurrence of pocket depth postsurgically.6 Although this concept is not universally accepted3,5 and the procedure induces loss of radicular bone in the healing phase, recontouring of bone is the only logical treatment choice in some cases. The goal of osseous resective therapy is to reshape the marginal bone to resemble that of the alveolar process undamaged by periodontal disease. The technique is performed in combination with apically positioned flaps, and the procedure eliminates periodontal pocket depth and improves tissue contour to provide a more easily maintainable environment. The relative merits of pocket reduction procedures are discussed in Chapters 52 and 59; this chapter discusses the osseous resective technique and how and where it may be accomplished.
It is proposed that the conversion of the periodontal pocket to a shallow gingival sulcus enhances the patient’s ability to remove plaque and oral debris from the dentition. Likewise, the ability of dental professionals to maintain the periodontium in a state free of gingivitis and periodontitis is more predictable in the presence of shallow sulci. The more effective the periodontal maintenance therapy, the greater is the longitudinal stability of the surgical result. The efficacy of osseous surgery therefore depends on its ability to affect pocket depth and to promote periodontal maintenance.11,22,23 The merits of resection versus other treatment procedures are discussed in Chapter 52.
Normal Alveolar Bone Morphology
Knowledge of the morphology of the bony periodontium in a state of health is required to perform resective osseous surgery correctly (Figure 60-2). The characteristics of a normal bony form are as follows:
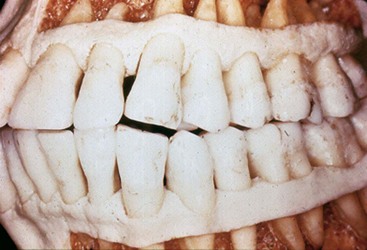
Figure 60-2 Photograph of a healthy bony periodontium in a skull. Although a slight amount of attachment may have been lost, this skull demonstrates the characteristics of normal form.
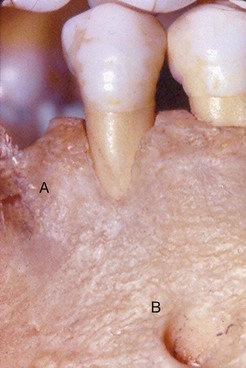
Figure 60-3 Effects of tooth position on facial bony contours. A, Bony fenestration. B, Bony dehiscence. These deformities can and should be detected by palpation, probing, and sounding before flap surgery.
Although these general observations apply to all patients, the bony architecture may vary from patient to patient in the extent of contour, configuration, and thickness. These variations may be both normal and healthy.
Terminology
Numerous terms have been developed to describe the topography of the alveolar housing, the procedure for its removal, and the resulting correction. These terms should be clearly defined.
Procedures used to correct osseous defects have been classified in two groups: osteoplasty and ostectomy.7 Osteoplasty refers to reshaping the bone without removing tooth-supporting bone. Ostectomy, or osteoectomy, includes the removal of tooth-supporting bone. One or both of these procedures may be necessary to produce the desired result.
Terms that describe the bone form after reshaping can refer to morphologic features or to the thoroughness of the reshaping performed. Examples of morphologically descriptive terms include negative, positive, flat, and ideal. These terms all relate to a preconceived standard of ideal osseous form.
Positive architecture and negative architecture refer to the relative position of interdental bone to radicular bone (Figure 60-4). The architecture is “positive” if the radicular bone is apical to the interdental bone. The bone has “negative” architecture if the interdental bone is more apical than the radicular bone. Flat architecture is the reduction of the interdental bone to the same height as the radicular bone.
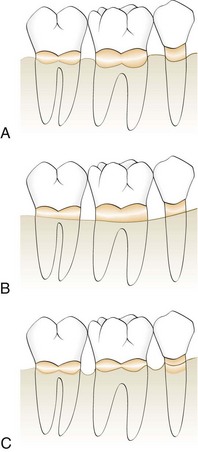
Figure 60-4 Diagram of types of bony architecture. A, Positive bony architecture. B, Flat bony architecture. C, Reversed, or negative, bony form.
Osseous form is considered to be “ideal” when the bone is consistently more coronal on the interproximal surfaces than on the facial and lingual surfaces. The ideal form of the marginal bone has similar interdental height, with gradual, curved slopes between interdental peaks (Figure 60-5).

Figure 60-5 Skull photograph of healthy periodontium. Note the shape of the alveolar bone housing. This bone is considered to have ideal form. It is more coronal in the interproximal areas, with a gradual slope around and away from the tooth.
Terms that relate to the thoroughness of the osseous reshaping techniques include “definitive” and “compromise.” Definitive osseous reshaping implies that further osseous reshaping would not improve the overall result. Compromise osseous reshaping indicates a bone pattern that cannot be improved without significant osseous removal that would be detrimental to the overall result. References to compromise and definitive osseous architecture can be useful to the clinician, not as description of a morphologic feature, but as terms that express the expected therapeutic result.
Factors in Selection of Resective Osseous Surgery
The relationship between the depth and configuration of the bony lesion(s) to root morphology and the adjacent teeth determines the extent that bone and attachment is removed during resection. Bony lesions have been classified according to their configuration and number of bony walls.9 The technique of ostectomy is best applied to patients with early to moderate bone loss (2 to 3 mm) with moderate-length root trunks18 that have bony defects with one or two walls. These shallow-to-moderate bony defects can be effectively managed by osteoplasty and osteoectomy. Patients with advanced attachment loss and deep intrabony defects are not candidates for resection to produce a positive contour. To simulate a normal architectural form, so much bone would have to be removed that the survival of the teeth could be compromised.
Two-walled defects, or craters, occur at the expense of the interseptal bone. As a result, they have buccal and lingual/palatal walls that extend from one tooth to the adjacent tooth. The interdental loss of bone exposes the proximal aspects of both adjacent teeth. The buccal-lingual interproximal contour that results is opposite to the contour of the cementoenamel junction of the teeth (Figure 60-6, A and B). Two-walled defects (craters) are the most common bony defects found in patients with periodontitis.14,20 If the facial and lingual plates of this bone are resected, the resultant interproximal contour would become more flattened or ovate (Figure 60-6, C and D). However, confining resection only to ledges and the interproximal lesion results in a facial and lingual bone form in which the interproximal bone is located more apically than the bone on the facial or lingual aspects of the tooth. This resulting anatomic form is reversed, or negative, architecture17,18,22 (Figure 60-6, C and D).
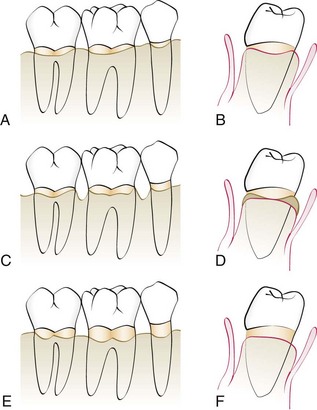
Figure 60-6 Effect of correction of craters. A and B, Diagram of facial and interproximal bony contours after flap reflection. Note the loss of some interproximal bone and cratering. C and D, Line angles; this is only osteoplasty and has resulted in a reversed architecture. E and F, Ostectomy on the facial and lingual bone and the removal of the residual widow’s peaks to produce a positive bony architecture.
Although the production of a reversed architecture minimizes the amount of ostectomy that is performed, it is not without consequences.5 Peaks of bone typically remain at the facial and lingual/palatal line angles of the teeth (widow’s peaks). During healing, the soft tissue tends to bridge the embrasure from the most coronal height of the bone on one tooth to the most coronal heights on the adjacent teeth. The result is therefore the tendency to replicate the attachment contour on the tooth. The interproximal soft tissues invest these peaks of bone, which may subsequently resorb with a tendency to rebound without gain in attachment over time. Interproximal pocket depth can recur.22,24
Ostectomy to a positive architecture requires the removal of the line-angle inconsistencies (widow’s peaks), as well as some of the facial, lingual, and palatal and interproximal bone. The result is a loss of some attachment on the facial and lingual root surfaces but a topography that more closely resembles normal bone form before disease (Figure 60-6, E and F). Proponents of osseous resection to create a positive contour believe that this architecture, devoid of sharp angles and spines, is conducive to the formation of a more uniform and reduced soft tissue dimension postoperatively.17,21 The therapeutic result is less pocket depth and increased ease of periodontal maintenance by the patient, dental hygienist, or dentist.
The amount of attachment lost from the use of ostectomy varies with the depth and configuration of the treated osseous defects. Osseous resection applied to two-wall intrabony defects (craters), the most common osseous defects, results in attachment loss at the proximal line angles and the facial and lingual aspects of the affected teeth without affecting the base of the pocket. The extent of attachment loss during resection to a positive architecture has been measured. When the technique is properly applied to appropriate patients, the mean reduction in attachment circumferentially around the tooth has been determined to be 0.6 mm at six probing sites.22 In practical terms, this means that the technique is best applied to interproximal lesions 1 to 3 mm deep in patients with moderate-to-long root trunks.17 Patients with deep, multiwalled defects are not candidates for resective osseous surgery. They are better treated with regenerative therapies or by combining osteoplasty to reduce bony ledges and to facilitate flap closure with new attachment and regeneration procedures.
Examination and Treatment Planning
The potential for the use of resective osseous surgery is usually identified during a comprehensive periodontal examination. Suitable patients display the signs and symptoms of periodontitis (see Chapter 30). The gingiva may be inflamed, and deposits of plaque, calculus, and oral debris may be present. An increased flow of crevicular fluid may be detected, and bleeding on probing and exudation are often observed.
Periodontal probing and exploration are key aspects of the examination. Careful probing reveals the presence of (1) pocket depth greater than that of a normal gingival sulcus, (2) the location of the base of the pocket relative to the mucogingival junction and attachment level on adjacent teeth, (3) the number of bony walls, and (4) the presence of furcation defects. Transgingival probing, or sounding, under local anesthesia confirms the extent and configuration of the intrabony component of the pocket and of furcation defects.6,16
Routine dental radiographs do not identify the presence of periodontitis and do not accurately document the extent of bony defects. Radiographs cannot accurately document the number of bony walls and the presence or extent of bony lesions on the facial/buccal or lingual/palatal walls. Well-made radiographs provide useful information about the extent of interproximal bone loss, the presence of angular bone loss, caries, root trunk length, and root morphology. Films also facilitate the identification of other dental pathoses that require treatment. In addition, a radiographic survey serves as a means of evaluating the success of therapy and documenting the patient’s longitudinal stability.19
Treatment planning should provide solutions for active periodontal diseases and correction of deformities that result from periodontitis. Planning should also facilitate the performance of other dental procedures included in a comprehensive dental treatment plan. The extent of periodontal involvement can vary significantly from tooth to tooth in the same patient. The response to therapy from patient to patient may also vary, as may the treatment objectives for the patients. Therefore a treatment plan may encompass a number of steps and combinations of procedures in the same surgical area.
After oral hygiene instruction and scaling and root planing, along with other disease control procedures, the response of the patient to these treatment procedures is evaluated by reexamination and recording the changes in the periodontium. Because the extent of periodontal involvement can vary significantly from tooth to tooth in the same patient, the local response to therapy is also variable. The resolution of inflammation and decrease in edema and swelling may have resulted in a return to normal depth and configuration of some pockets, and additional therapy beyond periodic maintenance may not be required.
The patient with moderate-to-advanced periodontitis and bony defects, although the overt signs of periodontitis may be reduced, may display a persistence of pocket depth bleeding on probing and suppuration. These signs may indicate the presence of residual plaque and calculus, attributable to the difficulty of achieving instrumentation in these deep pockets or the patient’s inability or unwillingness to perform adequate oral hygiene in these sites. Patients with inadequate oral hygiene are not good candidates for periodontal surgery. If the supragingival plaque control is good and the residual pocket depths are 5 mm or more, patients with such areas may be candidates for periodontal surgery.13
Resective osseous surgery is also used to facilitate certain restorative and prosthetic dental procedures. Dental caries can be exposed for restoration; fractured roots of abutment teeth can be exposed for removal; and bony exostoses and ridge deformities can be altered in contour to improve the performance of removable or fixed prostheses (Figure 60-7). Severely decayed teeth or teeth with short anatomic crowns can be lengthened by resection or by a combination of orthodontic tooth extrusion and osseous resection. Such procedures allow the therapist to expose more tooth for restoration, prevent an invasion of the biologic width of attachment, and create a periodontal attachment of normal dimension.8,15 Resection can also provide a means of producing optimal crown length for cosmetic purposes.
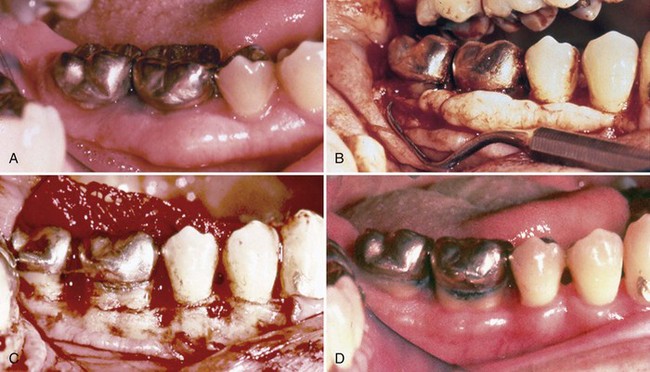
Figure 60-7 Reduction of bony ledges and exposure of caries by osteoplasty. A, Buccal preoperative photograph showing two crowns, exostoses, and caries. B, Flap reflected to reveal caries on both molars at the restoration margins, interdental cratering, and a facial exostosis. C, After osseous surgery; the bulk of the bony removal was by osteoplasty, with minor ostectomy between the two molars. The caries is now exposed, and the crowns are lengthened for restoration. D, Postoperative photograph at 6 weeks. The plaque control is deficient, but the teeth should be readily restorable at this time.
(Courtesy Dr. Joseph Schwartz, Portland, OR.)
Methods of Resective Osseous Surgery
The reshaping process is fundamentally an attempt to gradualize the bone sufficiently to allow soft tissue structures to follow the contour of the bone. The soft tissue predictably attaches to the bone within certain specific dimensions. The length and quality of connective tissue and junctional epithelium that reform in the surgical site depend on numerous factors, including the health of the tissue, condition and topography of the root surface, and proximity of the bone surrounding the tooth. Each of these factors must be controlled to the best of the clinician’s ability to obtain the optimal result, making osseous resective surgery an extremely precise technique.
It is assumed in this chapter that the gingival tissue has been reflected by the apically positioned flap described in Chapter 57. Reshaping of the bone may necessitate selective changes in gingival height. These changes must be calculated and accounted for in the initial flap design. For this reason, it is important for the clinician to know about the underlying bone tissue before flap reflection. The clinician must gain as much indirect knowledge as possible from soft tissue palpation, radiographic assessment, and transgingival probing (sounding).
Radiographic examination can reveal the existence of angular bone loss in the interdental spaces; these areas usually coincide with intrabony pockets. The radiograph does not show the number of bony walls of the defect or document with any accuracy the presence of angular cone defects on facial or lingual surfaces. Clinical examination and probing are used to determine the presence and depth of periodontal pockets on any surface of any tooth and can also provide a general sense of the bony topography, although intrabony pockets can go undetected by probing. Both clinical and radiographic examinations can indicate the presence of intrabony pockets when the clinician finds (1) angular bone loss, (2) irregular bone loss, or (3) pockets of irregular depth in adjacent areas of the same tooth or adjacent teeth.
The experienced clinician can use transgingival probing to predict many features of the underlying bony topography. The information thus obtained can change the treatment plan. For example, an area that had been selected for osseous resective surgery may be found to have a narrow defect that was unnoticed in the initial probing and radiographic assessment and is ideal for augmentation procedures. Such findings can and do change the flap design, osseous procedure, and results expected from the surgical intervention. Transgingival probing is extremely useful just before flap reflection. It is necessary to anesthetize the tissue locally before inserting the probe. The probe should be “walked” along the tissue-tooth interface so that the operator can feel the bony topography. The probe may also be passed horizontally through the tissue to provide three-dimensional information regarding bony contours (i.e., thickness, height, and shape of the underlying base). It must be remembered, however, that this information is still “blind,” and although it is undoubtedly better than probing alone, it has significant limitations. Nevertheless, this step is recommended immediately before the surgical intervention.
The situations that can be encountered after periodontal flap reflection vary greatly. When all soft tissue is removed around the teeth, there may be larger exostoses, ledges, troughs, craters, vertical defects, or combinations of these defects. Therefore each osseous situation presents uniquely challenging problems, especially if reshaping to the optimal level is contemplated.
Osseous Resection Technique
Instrumentation
A number of hand and rotary instruments have been used for osseous resective surgery. Some excellent clinicians use only hand instruments and rongeurs, whereas others prefer a combination of hand and rotary instruments. Rotary instruments are useful for the osteoplastic steps outlined previously, whereas hand instruments provide the most precise and safe results with ostectomy procedures.
Recently piezoelectric surgical techniques, described in Chapter 75, have also been used with success for osseous surgical resective techniques25,26 (Figure 60-8, A). Regardless of instrumentation used, care and precision are required for each step of the procedure to prevent excessive bone removal or root damage, both of which are irreversible. Figure 60-8 illustrates some of the instruments commonly used for osseous resection techniques.

Figure 60-8 Instruments often used in osseous surgery. A, Currently, the piezoelectric surgical instrument has been used successfully in osseous resective surgery. B, Rongeurs: Friedman (top) and 90-degree Blumenthal (bottom). C, Carbide round burs. Left to right, Friction grip, surgical-length friction grip, and slow-speed handpiece. D, Diamond burs. E, Interproximal files: Schluger and Sugarman. F, Back-action chisels. G, Ochsenbein chisels.
To address the many clinical situations, the following sequential steps are suggested for resective osseous surgery (Figure 60-9, A to D):
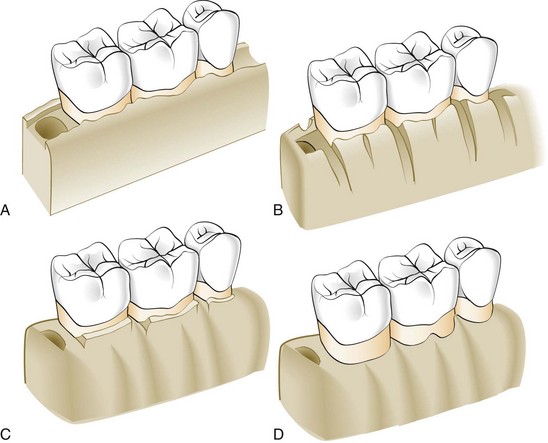
Figure 60-9 A, Drawing of bony topography in moderate periodontitis with interdental craters. B, Vertical grooving, the first step in correction by osseous reshaping. C, Radicular blending and flattening of interproximal bone. D, Gradualizing the marginal bone. Note the area of the furcation on the first molar where the bone is preserved.
Not all steps are necessary in every case, but the sequencing of the steps in the order given is necessary to expedite the reshaping procedure, as well as to minimize the unnecessary removal of bone. Figure 60-10 illustrates bone reshaping in flap surgery for specific anatomic defects.
Vertical Grooving
Vertical grooving is designed to reduce the thickness of the alveolar housing and to provide relative prominence to the radicular aspects of the teeth (see Figure 60-9, B). It also provides continuity from the interproximal surface onto the radicular surface. It is the first step of the resective process because it can define the general thickness and subsequent form of the alveolar housing. This step is usually performed with rotary instruments, such as round carbide burs or diamonds. The advantages of vertical grooving are most apparent with thick bony margins, shallow crater formations, or other areas that require maximal osteoplasty and minimal ostectomy. Vertical grooving is contraindicated in areas with close roots or thin alveolar housing.
Radicular Blending
Radicular blending, the second step of the osseous reshaping technique, is an extension of vertical grooving (see Figure 60-9, C). Conceptually, it is an attempt to gradualize the bone over the entire radicular surface to provide the best results from vertical grooving. This provides a smooth, blended surface for good flap adaptation. The indications are the same as for vertical grooving (i.e., thick ledges of bone on the radicular surface, where selective surgical resection is desired). Naturally, this step is not necessary if vertical grooving is very minor or if the radicular bone is thin or fenestrated. Both vertical grooving and radicular blending are purely osteoplastic techniques that do not remove supporting bone. In most situations, these two procedures compose the bulk of resective osseous surgery. Classically, shallow crater formations, thick osseous ledges of bone on the radicular surfaces, and Class I and early Class II furcation involvements are treated almost entirely with these two steps.
Flattening Interproximal Bone
Flattening of the interdental bone requires the removal of very small amounts of supporting bone (Figure 60-11). It is indicated when interproximal bone levels vary horizontally. By definition, most of the indications for this step are one-walled interproximal defects or hemiseptal defects. The omission of flattening in such cases results in increased pocket depth on the most apical side of the bone loss. This step is typically not necessary with interproximal crater formations or flat interproximal defects. It is best used in defects that have a coronally placed, one-walled edge of a predominantly three-walled angular defect, and it can be helpful in obtaining good flap closure and improved healing in the three-walled defect. The limitation of this step, as with resective osseous surgical therapy in general, is in the treatment of advanced lesions. Large hemiseptal defects would require removal of inordinate amounts of bone to provide a flattened architecture, and the procedure would be too costly in terms of bony support. Compromised osseous architecture is the only logical solution (Figure 60-12).
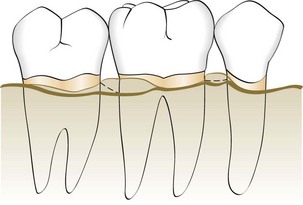
Figure 60-11 Diagrammatic representation of bone irregularities in periodontal disease. The thick line is the proposed correction of the defect. Note the flattening of the interproximal bone between the molars and the protection of the furcal bone on the first molar. Facial crest height is reduced in both interproximal areas to the depth of the defect.

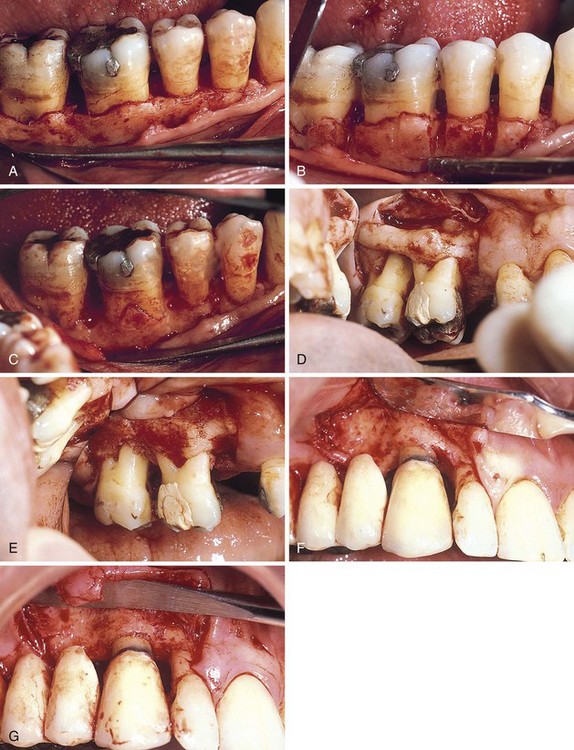
Figure 60-12 Compromise osseous surgery. A and B, Preoperative views of the buccal and lingual surfaces. C and D, Preoperative and postoperative views of the buccal osseous recontouring of Class I buccal furcation defects, a moderate crater between the two molars, and a deep 1-2-3–walled defect at the mesial of the first involvements. D, Buccal aspects of these lesions were corrected with osteoplasty and a small amount of ostectomy. E and F, Preoperative and postoperative views of the lingual osseous management. In E, note the combination 1-2-3–walled defect between the second bicuspid and first molar, as well as the irregular pattern of bone loss with ledging. F, These defects were corrected by osteoplasty and ostectomy, except for the deep defect at the mesial surface of the molar. This area was resected until the residual defect was of two and three walls only and left to repair. G and H, Buccal and lingual 5-year postoperative views of tissue configuration. Note the residual soft tissue defect between the bicuspid and first molar.
Gradualizing Marginal Bone
The final step in the osseous resection technique is also an ostectomy process. Bone removal is minimal but necessary to provide a sound, regular base for the gingival tissue to follow. Failure to remove small bony discrepancies on the gingival line angles (widow’s peaks) allows the tissue to rise to a higher level than the base of the bone loss in the interdental area (see Figure 60-9, C and D). This may make the process of selective recession and subsequent pocket reduction incomplete. This step of the procedure also requires gradualization and blending on the radicular surface (see Figures 60-10, C, and 60-11). The two ostectomy steps should be performed with great care so as not to produce nicks or grooves on the roots. When the radicular bone is thin, it is extremely easy to overdo this step, to the detriment of the entire surgical effort. For this reason, various hand instruments, such as chisels and curettes, are preferable to rotary instruments for gradualizing marginal bone.
Flap Placement and Closure
After performing resection, the clinician positions and sutures the flaps. Flaps may be replaced to their original position, to cover the new bony margin, or they may be apically positioned. Replacing the flap in areas that previously had deep pockets may result initially in greater postoperative pocket depth, although a selective recession may diminish the depth over time. Positioning the flap apically to expose marginal bone is one method of altering the width of the gingiva (denudation). However, such flap placement results in more postsurgical resorption of bone and patient discomfort than if the newly created bony margin were covered by the flap. Positioning the flap to cover the new margin minimizes postoperative complications and results in optimal postsurgical pocket depths (Figure 60-13).

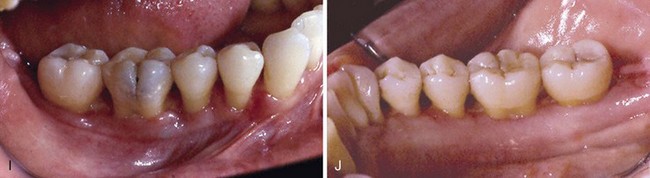
Figure 60-13 Ostectomy and osteoplasty to a positive contour with flap placement at the newly created bony crest for minimal pocket depth. A and B, Buccal and lingual preoperative views. C and D, Buccal preoperative view and postoperative correction. Osteoplasty and ostectomy were used to produce a positive contour. Note the osteoplasty into the buccal furcation of the first molar. This is about the extent of craters that can be corrected to a positive contour in teeth with moderate root trunk length. E and F, Lingual preoperative view and postoperative correction. Osteoplasty and ostectomy were done to produce a positive contour. Note the lingual ledge, which was reduced. Such ledges are common in this area. G and H, Buccal and lingual flaps sutured with continuous sling sutures to allow placement of the flaps to cover the bony margins. Ostectomy and osteoplasty performed to a positive contour, with flap placement at the newly created bony crest for minimal pocket depth. Ostectomy and osteoplasty to a positive contour with flap placement at the newly created bony crest for minimal pocket depth. I and J, Buccal and lingual postoperative views at 1 week. Soft tissue thickness is minimal, and the interdental areas are granulating in over the positive bony form. Minimal pocket depth results from such management.
Suturing may be accomplished using a variety of different suture materials and suture knots4 (see Chapter 57). The sutures should be placed with minimal tension to coapt the flaps, prevent their separation, and maintain the position of the flaps. Sutures placed with excessive tension rapidly pull through the tissues.
Postoperative Maintenance
Sutures may be removed at various times after placement. Nonresorbable sutures such as silk are usually removed after 1 week of healing, although some of the newer synthetic materials may be left for up to 3 weeks or longer without adverse consequences. Resorbable sutures maintain wound approximation for varying periods of 1 to 3 weeks or more, depending on the type of suture material. At the suture removal appointment the periodontal dressing, if present, is removed, and the surgical site is gently cleansed of debris with a cotton pellet dampened with saline. Nonresorbable sutures are then cut and removed. If sutures of a resorbable material were used, the area should be inspected carefully to ensure that no suture fragments remain. Suture removal should be accomplished without dragging contaminated portions of the suture through the periodontal tissues. This may be accomplished by lightly compressing the soft tissue immediately adjacent to the suture. This exposes (extrudes) a portion of the suture that was previously under the gingival tissues and less likely to be contaminated by plaque. The suture is then cut at the gingival surface. Removal of the pressure from the site results in the cut surface being slightly submerged in the tissue. The sutures are then removed with cotton pliers by pulling the suture from its contaminated end.
After suture removal the surgical site is examined carefully, and any excessive granulation tissue is removed with a sharp curette. The patient is provided with postsurgical maintenance instructions and the instruments needed to maintain the surgical site in a plaque-free state. These instruments should not produce additional trauma to the healing tissues. Many therapists find the use of a plaque-suppressive agent such as chlorhexidine digluconate to be a valuable adjunct to postsurgical maintenance. A second postoperative visit is often performed at the second or third week, and the surgical site is lightly debrided for optimal results. Professional prophylaxis for complete plaque removal should be done every 2 weeks until healing is complete or the patient is maintaining appropriate levels of plaque control.
Healing should proceed uneventfully, with the attachment of the flap to the underlying bone completed in 14 to 21 days. Maturation and remodeling can continue for up to 6 months. It is usually advisable to wait at least 6 weeks after completion of healing of the last surgical area before beginning dental restorations. For those patients with a major cosmetic concern, it is wise to wait as long as possible to achieve a postoperative soft tissue position and a stable sulcus.
Specific Osseous Reshaping Situations
The osseous corrective procedure previously described is classically applied to shallow craters with heavy faciolingual ledges (Figure 60-14). The correction of other osseous defects is also possible; however, careful case selection for definitive osseous surgery is extremely important.
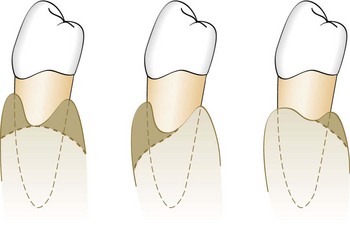
Figure 60-14 Interproximal craters. The shaded areas illustrate different techniques for the management of such defects. The technique that reduces the least amount of supporting bone is preferable.
Correction of one-walled hemiseptal defects requires that the bone be reduced to the level of the most apical portion of the defect. Therefore, great care should be taken to select the appropriate case. If one-walled defects occur next to an edentulous space, the edentulous ridge is reduced to the level of the osseous defect (Figure 60-15).
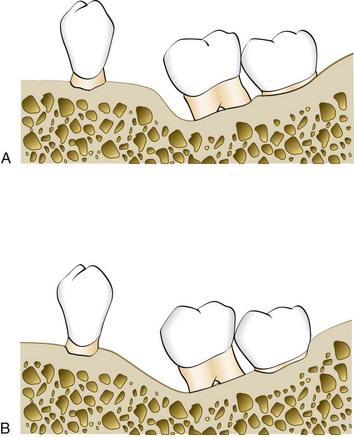
Figure 60-15 Reduction of a one-wall angular defect. A, Angular bone defect mesial to the tilted molar. B, Defect reduced by “ramping” angular bone.
Other situations that complicate osseous correction are exostoses (see Figure 60-10, D and E), malpositioned teeth, and supraerupted teeth. Following the four steps previously outlined best controls each of these situations. In most situations the unique feature of the bony profile is well managed by prudently applying the same principles (see Figure 60-10). However, some situations require deviation from the definitive osseous reshaping technique; examples include dilacerated roots, root proximity, and furcations that would be compromised by osseous surgery.
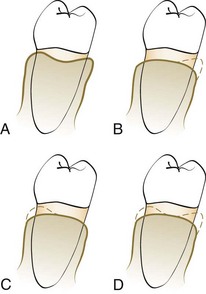
Figure 60-16 Diagram of crater reduction patterns. A, Preoperative bony form after flap reflection. B, Reduction of craters to the lingual wall. C, Reduction of craters to the facial wall. D, Reduction of craters to both the buccal and the lingual wall.
In the absence of ledges or exostoses, the elimination of the bony lesion begins with reduction of the interdental walls of craters, the one-walled component of angular defects, and wells (moats) and grooving into sites of early involvement.10 The walls of the crater may be reduced at the expense of the buccal, lingual, or both walls (Figure 60-16). The reduction should be made to remove the least amount of alveolar bone required to (1) produce a satisfactory form, (2) prevent the therapeutic invasion of furcations, and (3) blend the contours with the adjacent teeth. The selective reduction of bony defects by “ramping” the bone to the palatal or lingual to avoid involvement of the furcations has been advocated by Ochsenbein and Bohannan18 and Tibbetts et al23 (Figure 60-17).
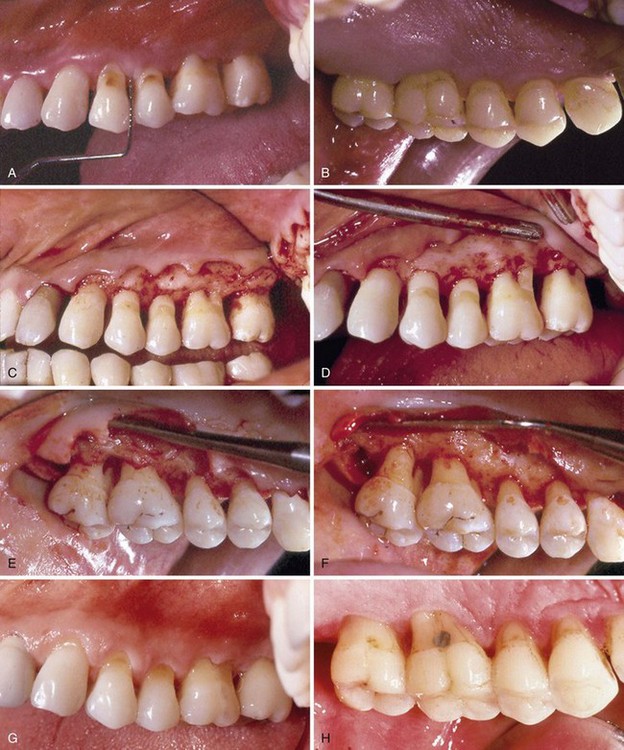
Figure 60-17 Correction of osseous defects largely to the palatal wall. A and B, Buccal and palatal preoperative views, 6 weeks after completion of scaling and root planing. C and D, Buccal preoperative and postoperative views. In C, note the ledging on the facial wall of molars and the one-wall defects on both molars. D, Postoperative view shows the elimination of these defects by osteoplasty on the ledges and ostectomy of the one-wall defects to produce a positive buccal architecture. E and F, Palatal preoperative and postoperative views. In E, note the pattern of bony loss, which is more severe on the palatal wall. In addition to the facial one-wall defects, there is an incipient furcation defect at the mesial wall of the first molar and a Class II furcation at the mesial wall of the second molar. F, configuration of the defects was such that ostectomy was performed on the palatal roots of both molars to produce a compromise architecture. G and H, Ten-year postoperative views of the buccal and palatal areas showing the pattern of soft tissue adaptation to the surgically produced bony form.
In the presence of heavy ledges of bone, it is usually wise to do osteoplasty first to eliminate any exostoses or reduce the buccal/lingual bulk of the bone (Figure 60-18). It is common practice to incorporate a degree of vertical grooving during the reduction of bony ledges, because this facilitates the process of blending the radicular bone into the interproximal areas at the next step.
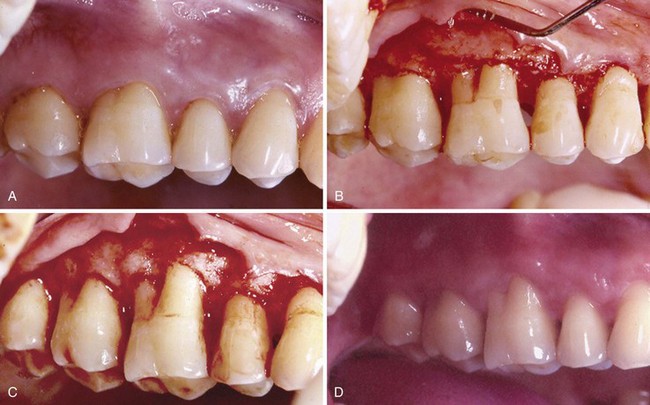
Figure 60-18 Reduction of bony ledges by osteoplasty before correction of interdental defects. A, Buccal preoperative view. B, Buccal flap reflection. Note the buccal ledge and the Class II buccal furcation. C, Buccal correction largely by osteoplasty with minor ostectomy over the root prominence to produce a positive architecture. D, 10-year postoperative view of soft tissue form. Minimal pocket depth is present.
One-walled or hemiseptal defects usually require the removal of some bone from the tooth with the greatest coronal bony height. This removal of bone may result in a significant reduction in attachment on relatively unaffected adjacent teeth to eliminate the defect. However, if a tooth in the surgical field has one-walled defects on both its mesial and its distal surface and this is recognized during examination, the severely affected tooth may be extruded by orthodontic therapy during disease control treatment to minimize or eliminate the need for resection of bone from the adjacent teeth.
Summary
Although osseous surgical techniques cannot be applied to every bony abnormality or topographic modification, it has been clearly demonstrated that properly used osseous surgery can eliminate and modify defects, as well as gradualize excessive bony ledges, irregular alveolar bone, early furcation involvement, excessive bony exostosis, and circumferential defects. When properly performed, resective osseous surgery achieves a physiologic architecture of marginal alveolar bone conducive to gingival flap adaptation with minimal probing depth. The advantages of this surgical modality include a predictable amount of pocket reduction that can enhance oral hygiene and periodic maintenance. It also preserves the width of the attached tissue while removing granulomatous tissue and providing access for debridement of the radicular surfaces. In addition, the osseous resection technique permits recontouring of bony abnormalities, including hemiseptal defects, tori, and ledges. Its substantial benefits include proper assessment for restorative procedures (e.g., crown lengthening) and assessment of restorative overhangs and tooth abnormalities (e.g., enamel projections, enamel pearls, perforations, fractures). Therefore resective osseous surgery can be an important technique in the armamentarium necessary to provide a maintainable periodontium for periodontal patients.
![]() Science Transfer
Science Transfer
Osseous surgery is an effective treatment for patients with moderate bone loss and craters up to 3 mm deep and/or early furcation defects, as well as for bone contour irregularities such as exostoses and ledges. It results in some attachment loss, but by developing bone contours that parallel healthy gingival margin shapes, it gives a stable, new periodontium that can be maintained for years.
The most important determinant for successful periodontal surgical therapy is adequate plaque control, thus all patients must demonstrate satisfactory oral hygiene levels before and after resective osseous surgery. If a patient is unable to achieve 80% or more plaque-free surfaces, surgical therapy is contraindicated and nonsurgical approaches and maintenance are the endpoints of treatment until plaque scores are improved. In areas of esthetic concern, resective osseous surgery can result in increased gingival recession and should not be used in these patients. Patients with advanced bone loss are better treated with regenerative surgical techniques, but in many cases, it is possible to combine resective osseous surgery and regenerative techniques for different periodontal defects treated during the same flap surgery.
1 Black GV. Surgical treatment of pockets. In Black AD, editor: Special dental pathology, ed 3, Chicago: Medico Dental, 1917.
2 Carranza FA, Carranza FAJr. The management of the alveolar bone in the treatment of the periodontal pocket. J Periodontol. 1956;27:29.
3 Caton J, Nyman S. Histometric evaluation of periodontal surgery. III. The effect of bone resection on the connective tissue attachment level. J Periodontol. 1981;52:405.
4 Dahlberg WH. Incisions and suturing: some basic considerations about each in periodontal surgery. Dent Clin North Am. 1969;13:149.
5 Donnenfeld OW, Hoag PM, Weissman DP. A clinical study of the effects of osteoplasty. J Periodontol. 1961;32:131.
6 Easley J. Methods of determining alveolar osseous form. J Periodontol. 1967;38:112.
7 Friedman N. Periodontal osseous surgery: osteoplasty and osteoectomy. J periodontol. 1955;26:257.
8 Garguilo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261.
9 Goldman HM, Cohen DW. The infrabony pocket: classification and treatment. J Periodontol. 1958;29:272.
10 Kaldahl WB, Kalkwarf KL, Patil KD, et al. Evaluation of four modalities of periodontal therapy: mean probing depth, probing attachment level and recession changes. J Periodontol. 1988;59:783.
11 Kaldahl WB, Kalkwarf KL, Patil KD, et al. Long-term evaluation of periodontal therapy. I. Response to four therapeutic modalities. J Periodontol. 1996;67:93.
12 Knowles J, Burgett F, Nissle R, et al. Results of periodontal treatment related to pocket depth and attachment level: eight years. J Periodontol. 1979;50:225.
13 Lindhe J, Socransky S, Nyman S, et al. Critical probing depths in periodontal therapy. J Clin Periodontol. 1982;9:323.
14 Manson JD, Nicholson K. The distribution of bone defects in chronic periodontitis. J Periodontol. 1974;45:88.
15 Maynard JG, Wilson RD. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol. 1979;50:170.
16 Mealey BL, Beybayer MF, Butzin CA, et al. Use of furcal bone sounding to improve the accuracy of furcation diagnosis. J Periodontol. 1994;65:649.
17 Ochsenbein C. A primer for osseous surgery. Int J Periodont Restor Dent. 1986;6:9.
18 Ochsenbein C, Bohannan HM. The palatal approach to osseous surgery. II. Clinical application. J Periodontol. 1964;35:54.
19 Prichard JF. The roentgenographic depiction of periodontal disease. Periodontics. 3(2), 1973.
20 Schluger S. Osseous resection: a basic principle in periodontal surgery. Oral Surg Oral Med Oral Pathol. 1949;2:316.
21 Schluger S, Yuodelis RA, Page RC, et al. Resective periodontal surgery in pocket elimination. In: Periodontal diseases. Philadelphia: Lea & Febiger; 1990.
22 Selipsky HS. Osseous surgery: how much need we compromise? Dent Clin North Am. 1976;20:79.
23 Tibbetts L, Ochsenbein C, Loughlin D. The lingual approach to osseous surgery. J Periodontol. 1976;20:61.
24 Townsend-Olsen C, Ammons WF, Van Belle C. A longitudinal study comparing apically repositioned flaps, with and without osseous surgery. Int J Periodont Restor Dent. 1985;5:11.
25 Vercellotti T, Nevins ML, Kim DM, et al. Osseous response following resective therapy with piezosurgery. Int J Periodontics Restorative Dent. 2005 Dec;25(6):543-549.
26 Vercellotti T, Pollack AS. A new bone surgery device: sinus grafting and periodontal surgery. Compend Contin Educ Dent. 2006 May;27(5):319-325.