Nutrition and Bone Health
Sections of this chapter were written by John J.B. Anderson, PhD for the previous edition of this text.
Adequate nutrition is essential for the development and maintenance of the skeleton (i.e., bone health). Although diseases of the bone such as osteoporosis and osteomalacia (a condition of impaired mineralization caused by vitamin D and calcium deficiency) have complex causes, the development of these diseases can be minimized by providing adequate amounts of nutrients throughout the life cycle. Of these diseases, osteoporosis is the most common and destructive of productivity and quality of life.
The number of people older than 65 years in the United States is projected to reach almost 25% of the population by 2020. The average life expectancy in the United States is almost 81 years for women and 74 for men. As a result of the increasing numbers of older adults, osteoporosis with resulting hip fractures has become more significant in cost, morbidity, and mortality in the United States. Although the use of bone-building nutrients is necessary after the onset of osteoporosis, the benefits of adequate intakes (AIs) of bone-building nutrients during adolescence and adulthood are significant.
Bone Structure and Bone Physiology
Bone is a term used to mean both an organ, such as the femur, and a tissue, such as trabecular bone tissue. Each bone contains bone tissues of two major types, trabecular and cortical. These tissues undergo bone modeling during growth (height gain) and bone remodeling after growth ceases.
Composition of Bone
Bone consists of an organic matrix or osteoid, primarily collagen fibers, in which salts of calcium and phosphate are deposited in combination with hydroxyl ions in crystals of hydroxyapatite. The cablelike tensile strength of collagen and the hardness of hydroxyapatite combine to give bone its great strength. Other components of the bone matrix include osteocalcin, osteopontin, and several other matrix proteins.
Types of Bone Tissue
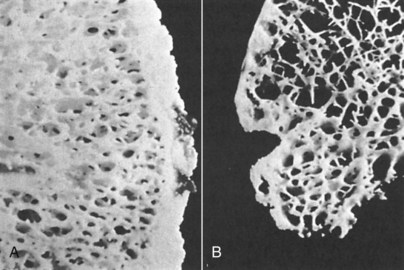
Approximately 80% of the skeleton consists of compact or cortical bone tissue. Shafts of the long bones contain primarily cortical bone, which consists of osteons or Haversian systems that undergo continuous but slow remodeling, and both contain an outer periosteal layer of compact circumferential lamellae and an inner endosteal layer of trabecular tissue. The remaining 20% of the skeleton is trabecular or cancellous bone tissue, which exists in the knobby ends of the long bones, the iliac crest of the pelvis, the wrists, scapulas, vertebrae, and the regions of bones that line the marrow. Trabecular bone is less dense than cortical bone as a result of an open structure of interconnecting bony spicules that resemble a sponge in appearance; thus trabecular bone is also called spongy bone or spongiosa.
The elaborate interconnecting components (columns and struts) of trabecular bone tissue add support to the cortical bone shell of the long bones and provide a large surface area that is exposed to circulating fluids from the marrow, and is lined by a disproportionately larger number of cells than cortical bone tissue. Therefore trabecular bone tissue is much more responsive to estrogens or the lack of estrogens than cortical bone tissue (Figure 25-1). The loss of trabecular bone tissue late in life is largely responsible for the occurrence of fractures, especially those of the spine.
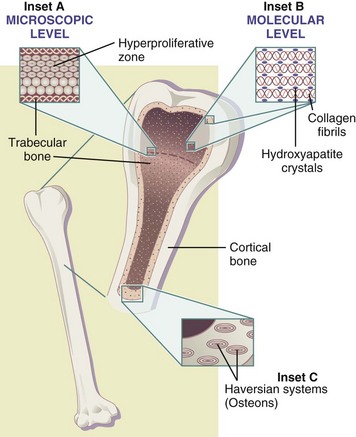
FIGURE 25-1 Schematic diagram of the structure of a long bone (hemisection of a long bone, such as the tibia). The ends of the long bones contain high percentages of trabecular (cancellous) bone tissue, whereas the shaft contains predominately cortical bone tissue. Inset A includes an enlarged section (approximately 100-fold) of the growth plate (epiphysis) and the subjacent hyperproliferative zone containing cartilage cells stacked like coins. Inset B includes a section of collagen molecules (triple helices) surrounded by mineralized deposits (dark spheroids) at a magnification of approximately 1,000,000-fold. These collagen-mineral complexes exist in both trabecular and cortical bone tissues. Inset C shows the cross-section of half of the mid-shaft of a long bone (magnification 10-fold). This section of cortical bone tissue contains vertical Haversian systems (osteons) that run parallel with the shaft axis; many are required to extend this system from one end of the shaft to the other. At the center of each osteon is a canal that contains an artery that supplies bone tissues with nutrients and oxygen, a vein for removing wastes, and a nerve for returning afferent relays to the brain. (Copyright John J. B. Anderson and Sanford C. Garner.)
Bone Cells
Osteoblasts are responsible for the formation or production of bone tissue, and osteoclasts govern the resorption or breakdown of bone (also see “Bone Modeling and Bone Remodeling” later in this chapter). The functions of these two cell types are listed in Table 25-1.
TABLE 25-1
Functions of Osteoblasts and Osteoclasts
| Osteoblasts | Osteoclasts |
| Bone Formation | Bone Resorption |
| Synthesis of matrix proteins: Collagen type 1 (90%); Osteocalcin and others (10%) |
Degradation of bone tissue via enzymes and acid (H+) secretion |
| Mineralization | |
| Communication: Secretion of cytokines that act on osteoblasts | Communication: Secretion of enzymes that act on osteoclasts |
Two other important cell types also exist in bone tissue, osteocytes and bone-lining cells (inactive osteoblasts), both of which are derived from osteoblasts. The origin of the osteoblasts and osteoclasts is from primitive precursor cells found in bone marrow, now known to be stimulated by hormones and growth factors as part of their differentiation to become mature, functional bone cells.
Cartilage
In the embryo, cartilage forms the first temporary skeleton, until it develops into a mature bone matrix. In the adult, cartilage is found as flexible supports in areas such as the nose and ear. Cartilage is not bone, and is neither vascularized nor calcified.
Calcium Homeostasis
Bone tissue serves as a reservoir of calcium and other minerals that are used by other tissues of the body. Calcium homeostasis is the process of maintenance of a constant serum calcium concentration. The body is almost totally reliant on this bone tissue source of calcium when the diet is inadequate. Bone tissue is also dynamic, because it undergoes bone turnover via both modeling early in life and remodeling after skeletal growth (height gain) ceases.
Although 99% of the body calcium is found in the skeleton, the remaining 1% is critical to a great variety of indispensable life processes. The concentration of calcium in blood and other extracellular fluids is regulated by complex mechanisms that balance calcium intake and excretion with bodily needs. When calcium intake is not adequate, homeostasis is maintained by drawing on mineral from the bone to keep the serum calcium ion concentration at its set level (approximately 10 mg/dL). Depending on the amount of calcium required, homeostasis can be accomplished by drawing from two major skeletal sources: readily mobilizable calcium ions in the bone fluid, or through osteoclastic resorption from the bone tissue itself. The daily turnover of skeletal calcium ions (transfers in and out of bone) is surprisingly high, which supports the dynamic activity of bone tissue in calcium homeostasis.
Blood calcium concentration is regulated by two calcium-regulating hormones -parathyroid hormone (PTH) and 1,25 dihydroxy vitamin D3 (calcitriol). Through direct actions on the skeleton and kidney and indirect actions in the gut, PTH contributes to overall calcium homeostasis. Intermittent parathyroid hormone (PTH) therapy contributes to bone formation by prolonging the life of osteoblasts. However, high continuous levels of PTH contribute to bone loss (Kousteni and Bilezikian, 2008).
Active vitamin D, as calcitriol, also plays a role by increasing the efficiency of intestinal calcium absorption in the upper half of the small bowel. Vitamin D works in concert with PTH, enhancing bone release of calcium to maintain blood values. Vitamin D primarily is obtained from sunlight’s interaction with precursors in the skin and secondarily from the diet. Calcitriol also has a direct effect on osteoblasts to increase the formation of several bone matrix proteins and other local factors needed for new bone formation and the suppression of bone degradation. The optimal intake and blood values for vitamin D remain under study. (see Chapter 3 and Chapter 8).
Bone Modeling
Bone modeling is the term applied to the growth of the skeleton until mature height is achieved. For example, during bone modeling long bones elongate and widen by undergoing great internal changes as well as external expansions in their structures. In modeling, the formation of new bone tissue occurs first and is followed by the resorption of old tissue. In long bones growth occurs both at terminal epiphyses (growth plates that undergo hyperproliferation) and circumferentially in lamellae; at each location cells undergo division and contribute to the formation of new bone tissue (see Figure 25-1).
Bone modeling is typically completed in females by ages 16 to 18 and in males by ages 18 to 20. After growth (height gain) ceases, gains in bone tissue may continue by the process known as bone consolidation. The major event of the skeleton in early life is growth, whereas there is an inevitable decline of bone mass in later stages of life (Figure 25-2).

FIGURE 25-2 The early gain and later loss of bone in females. Peak bone mineral density (BMD) is typically achieved by age 30. Menopause occurs at approximately age 50 or within a few years. Postmenopausal women typically enter the fracture risk range after age 60. Men have a more gradual decline in BMD, which starts at 50 years. (Copyright John J. B. Anderson and Sanford C. Garner.)
Bone Remodeling
After skeletal growth is completed, bone continuously undergoes change in response to strains on the skeleton. Bone adapts to changes in lifestyle factors and dietary intakes, maintains calcium concentration in extracellular fluids, and repairs microscopic fractures that occur over time. Bone remodeling is a process in which bone is continuously resorbed through the action of the osteoclasts and reformed through the action of the osteoblasts. A greater proportion occurs in the trabecular bone, especially at those sites located in areas subject to the greatest weight-bearing strains. In normal young adults the resorption and formation phases are tightly coupled, and bone mass is maintained at zero balance. In seniors bone loss involves an uncoupling of the phases of bone remodeling with an increase of resorption over formation and thus bone loss. Trabecular bone declines the most following menopause because of unopposed osteoclastic activity.
The remodeling process is initiated by the activation of preosteoclastic cells in the bone marrow. Interleukin (IL)-1 and other cytokines released from bone-lining cells act as the triggers in the activation of precursor stem cells in bone marrow. The preosteoclast cells from the bone marrow migrate to the surfaces of bone while differentiating into mature osteoclasts. The osteoclasts then cover a specific area of trabecular or cortical bone tissue. Acids and proteolytic enzymes released by the osteoclasts form small cavities on bone surfaces and resorb both bone mineral and matrix on the surface of trabecular bone or cortical bone. The resorptive process is rapid, and it is completed within a few days, whereas the refilling of these cavities by osteoblasts is slow (i.e., on the order of 3 to 6 months or even as long as a year or more in older adults).
The rebuilding or formation stage involves secretion of collagen and other matrix proteins by the osteoblasts, also derived from precursor stem cells in bone marrow. Collagen polymerizes to form mature triple-stranded fibers, and other matrix proteins are secreted. Within a few days salts of calcium and phosphate begin to precipitate on the collagen fibers, developing into crystals of hydroxyapatite. Approximately 4% of the total bone surface is involved in remodeling at any given time as new bone is renewed continually throughout the skeleton. Even in the mature skeleton, bone remains a dynamic tissue. Normal bone turnover is illustrated in Figure 25-3.
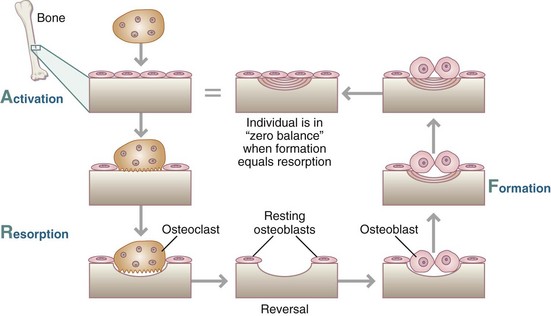
FIGURE 25-3 Normal bone turnover in healthy adults. (Copyright John J. B. Anderson and Sanford C. Garner.)
When the resorption and formation phases are in balance, the same amount of bone tissue exists at the completion of the formation phase as at the beginning of the resorption phase. The benefit to the skeleton of this remodeling is the renewal of bone without any microfractures. However, when dietary calcium is low, osteoclastic resorption becomes relatively greater than formation by osteoblasts because of a persistently elevated PTH concentration in blood (Figure 25-4). Then large amounts of bone tissue are removed and typically not fully replaced. The net result is a decrease in both bone mineral content (BMC) and bone mineral density (BMD).
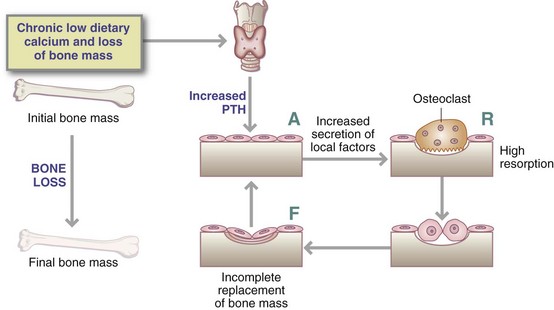
FIGURE 25-4 Effects of persistently elevated serum concentration of parathyroid hormone (PTH) on bone mass; this incorporates the effect of estradiol, counteracting the effect of PTH. (Copyright John J. B. Anderson and Sanford C. Garner.)
The action of PTH in promoting activity of the osteoclasts is countered by estrogen, which reduces the response of osteoblasts to PTH. PTH acts directly on osteoblasts, which increase the production of IL-6 and other cytokines that in turn stimulate osteoclasts to resorb bone. Estrogen helps to block the production of PTH-stimulated cytokines. See Fig. 25-5. Calcitonin, a vestigial hormone, may directly inhibit osteoclast activity (resorption), but the significance of its physiologic role in human subjects is not clear.
Osteocalcin and Bone Markers
Osteocalcin is a protein derived from osteoblasts. In bone matrix, osteocalcin assists in the mineralization process, perhaps acting to stop the formation of crystals and to prevent overmineralization. Interpretation of its level in blood is complicated by the fact that it is involved in both formation and resorption, which typically occur simultaneously at several different skeletal sites. There is difficulty in using it as a marker for predicting future fracture risk. Some osteocalcin is secreted by osteoblasts directly into the circulating blood, with a reciprocal relationship between bones and energy metabolism. Leptin influences osteoblast functions and, in turn, osteocalcin influences energy metabolism through increased insulin secretion and sensitivity, increased energy expenditure, and fat mass reduction (Hinoi et al., 2009).
Bone markers are used for research and for monitoring the effectiveness of medication on bone turnover. Plasma bone-specific alkaline phosphatase is a marker of bone formation, although total plasma alkaline phosphatase may also be used. Other markers of bone resorption include plasma crosslinked collagen telopeptides, urinary N-telopeptides, and plasma tartrate-resistant acid phosphatase.
Bone Mass
Bone mass is a generic term that refers to BMC but not to BMD. Bone mineral content (BMC) is more appropriately used in assessing the amount of bone accumulated before the cessation of growth (height gain), whereas bone mineral density (BMD) is better used to describe bone after the developmental period is completed. These measurements are often used interchangeably, but BMD is more useful for monitoring bone changes in adults. However, neither BMC nor BMD provides information on the microarchitectural (three-dimensional) structural quality of bone tissue (i.e., index of risk of fracture).
Accumulation of Bone Mass
During the growth periods of childhood, puberty, and early adulthood, formation exceeds the resorption of bone. Peak bone mass (PBM) is reached by 30 years of age or so (see Figure 25-2). The long bones stop growing in length by approximately age 18 in females and age 20 in males, but bone mass continues to accumulate for a few more years by a process known as consolidation (i.e., filling-in of osteons in the shafts of long bones). The age when BMD acquisition ceases varies, depending not only on diet but also on physical activity.
Peak Bone Mass
PBM is greater in men than in women because of men’s larger frame size. BMC, but not necessarily BMD, is typically lower in women. Both the lean and fat components of body composition contribute to these differences in bone mass. BMD is also greater in blacks and Hispanics than in whites and Asians, related to larger muscle mass, differences in body weight, lifestyle factors, and dietary intake (Pothiwala et al., 2006). Hereditary factors also contribute to the extent of accumulation of PBM.
PBM is related to appropriate intake of calories, protein, calcium, phosphorus, and vitamins D and K. Because bone formation begins in the embryo, more attention is being focused on maternal nutrition and health as a predictor of the child’s future PBM (Prentice et al., 2011). Physical activity also plays a role. Children’s activities should include ground-force reactions, such as running, skipping, or jumping, as these activities are site-specific to the bone. The importance of strengthening exercise continues to be investigated. The optimal time to begin physical activity to enhance PBM is not exact.
Body weight is positively associated with BMD, probably attributable to both adipose and lean mass (Reid, 2008). PBM is diminished in cases of anorexia nervosa (Misra and Klibanski, 2006), as well as in chronic diseases.
Loss of Bone Mass
Age is an important determinant of BMD. At approximately age 40, BMD begins to diminish gradually in both sexes, but bone loss increases greatly in women after age 50 or after menopause. A continuous loss thereafter in postmenopausal women occurs at rate of 1% to 2% per year during the next decade. Men continue to have bone loss, but at a much lower rate than women of the same age until age 70, when the loss rates are about the same for both genders. Loss of bone mass is the result of changes in the hormone-directed mechanisms that govern bone remodeling.
Cortical bone tissue and trabecular bone tissue undergo different patterns of aging. Loss of cortical bone eventually plateaus and may even cease late in life. Trabecular bone loss begins in both sexes as early as 40 years of age. Premenopausal loss of trabecular bone in women is much greater than that of cortical bone. Loss of both kinds of bone accelerates in women after menopause, although trabecular bone is also lost at a much higher rate than cortical bone. Differences between normal and osteoporotic bone—both trabecular and cortical tissues—are shown in Figure 25-6.
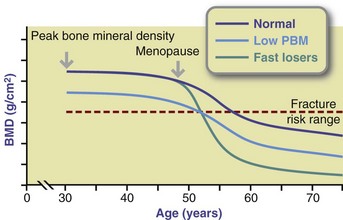
FIGURE 25-6 Variable patterns of bone loss of women following the onset of menopause at approximately 50 years of age. The rapid loss of bone mineral density (BMD) in some women referred to as fast losers is contrasted to the loss of slow losers. Women who develop low peak BMD have less bone mass than women with normal BMD, but they also can lose BMD either as slow or fast losers. (Copyright John J. B. Anderson and Sanford C. Garner.)
The accelerated bone loss rate of 2% to 3% per year continues for between 5 and 10 years after menopause, and then the rate declines gradually to 0.5% to 1% per year thereafter. Some postmenopausal women lose bone at an even faster rate (Figure 25-7). If the age of a woman is known, her vertebral bone mass may be predicted (see Clinical Insight: Postmenopausal Women at High Risk for Hip Fracture).
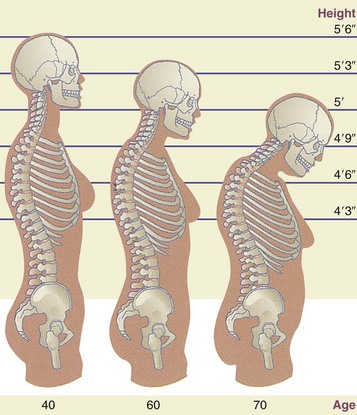
FIGURE 25-7 Normal spine at age 40 and osteoporotic changes at ages 60 and 70. These changes can cause a loss of as much as 6 to 9 inches in height and result in the dowager’s hump (far right) in the upper thoracic vertebrae. (From Ignatavicius D, Workman M: Medical-surgical nursing: critical thinking for collaborative care, ed 5, Philadelphia, 2006, Saunders.)
The normal bone loss that occurs with aging in both sexes is related to the decline of osteoblastic function such as the reduced production of collagen, osteocalcin, osteopontin, and other matrix proteins. As a result of the uncoupling of the remodeling process, osteoclastic resorption exceeds formation with an increasing differential. Bone loss in men accelerates in later years, typically in ages 60 through 79. The reason for bone loss in men is very similar to that in women, being either age-related, idiopathic, or secondary to an underlying disease or medication. The prevalence of low bone mass and osteoporosis in men is increasing as more men are being screened or diagnosed using dual-energy x-ray absorptiometry (DEXA). It has been estimated that 39% of osteoporotic fractures are in men (Khosla, 2010.)
Measurement of Bone Mineral Content and Bone Mineral Density
Bone densitometry measures bone mass on the basis of tissue absorption of photons produced by one or two monoenergetic x-ray tubes. DEXA (see Chapter 6 and Fig. 6-10) is available in most hospitals and many clinics for the measurement of the total body and regional skeletal sites such as the lumbar vertebrae and the proximal femur (hip). Results of DEXA measurements are commonly expressed as T-scores.
Ultrasound Measurements of Bone
Quantitative ultrasound measurements of the heel bone (calcaneus) and the kneecap are becoming popular. Ultrasound instruments measure the velocity of sound waves transmitted through bone and broadband ultrasound attenuation (BUA). Measurements at the calcaneus correlate well with BMD measurements at this same skeletal site, meaning that low values by DEXA are typically mirrored by low values of BUA. However, ultrasound measurements are considered screening tools, whereas DEXA measurements are considered diagnostic.
Fracture Risk Assessment
The World Health Organization (WHO) developed an algorithm to predict fracture by using femoral head BMD and clinical indicators of low bone mass. This uses economic modeling to guide the most cost-effective instances to begin medications. Vertebral fractures that are confirmed by x-rays are a strong predictor of future vertebral fractures, as well as fractures at other sites (National Osteoporosis Foundation [NOF], 2010). DEXA scans can also identify vertebral fractures.
Nutrition and Bone
Calcium, phosphate, and vitamin D are essential for normal bone structure and function. Protein, calories, and other micronutrients also help develop and maintain bone (Tucker, 2009).
Protein
Both protein and calcium are important components of PBM, especially before puberty (Rizzoli, 2008). Adequate protein intake, with adequate calcium intake, is needed for optimal bone health. A meta-analysis of studies concerned with protein intake and indicators of bone health found a slight positive effect on BMD, but it did not influence the risk of fracture over the long-term for total protein, animal protein, or vegetable protein (Darling et al., 2009;) unfortunately, this analysis did not consider calcium intake.
The negative effects of either too high or too low an intake of protein is more pronounced with inadequate calcium intake, especially in seniors (Tucker, 2009). The theory that higher protein intakes produce a higher acidic load, which increases calcium urinary excretion, has not been verified.
Very low protein intake may theoretically negatively affect bone turnover and development. In cases of negative nitrogen balance, such as with fracture or surgery, higher protein intake may be advised.
Minerals
Calcium intake in the primary prevention of osteoporosis has received much attention. The Institute of Medicine Dietary Reference Intakes (DRIs) for calcium and vitamin D, are given as RDAs. The RDA for calcium from preadolescence (age 9 years) through adolescence (up to 19 years) was increased to 1300 mg/day for both genders (IOM, 2011). The RDAs for calcium adults, pregnant and lactating women and children, are listed on the inside front cover).
People older than 11 years, particularly females, typically do not receive the recommended amount of calcium. According to the National Health and Nutrition Examination Survey (2007), teen and adult women consume considerably less than the current RDAs. Males are more likely to consume somewhat greater amounts than females, but after 50 years of age they also do not meet the recommended levels. These deficits translate, on average, into the need for an additional 500 mg/day for teenage girls and adult women.
Food sources are recommended first for supplying calcium needs because of the coingestion of other essential nutrients. In the United States, the primary source of calcium is dairy foods, and this intake is higher in white than in black women (Plawecki et al., 2009). However, calcium fortification of nondairy foods such as nondairy milks and other beverages, juices, breakfast cereals, bread, and some crackers is common.
Calcium bioavailability from foods is generally good, and the amount of calcium in the food is more important than its bioavailability. However, the order of concern relative to calcium absorption efficiency is first the individual’s need for calcium, second the amount consumed because absorption efficiency is inversely related to amount consumed, and third the intake of absorption enhancers or inhibitors. For example, absorption from foods high in oxalic and phytic acid (certain vegetables and legumes) is lower than from dairy products.
The amount of calcium in foods varies with the brand, serving size, and whether it has been fortified. Read the Nutrition Facts label to determine the amount of calcium per serving. Multiply the daily value (DV) percentage by 10 to determine the milligrams of calcium. For example, a 20% DV equals 200 mg of calcium (see Chapter 12). Labeling for “excellent” (>200 mg/serving) and “good” (100-200 mg/serving) sources of calcium are regulated by the Food and Drug Administration (FDA).
Calcium from Supplements
Reaching RDA levels of calcium from foods should be the first goal, but if insufficient amounts of calcium from foods are consumed, supplements of calcium should then be ingested to reach the age-specific RDA. The upper limit of safety for calcium intake is 2500 mg for everyone older than 1 year except for youth age 9-18 years and pregnant or lactating women when it is 3000 mg/day. Box 25-1 lists the potential risks associated with excessive calcium intake.
An increasing percentage of the population is taking calcium supplements. Persons who should take supplements include those not meeting the RDA on most days, those taking corticosteroids, those with low bone mass or osteoporosis, women who are perimenopausal or postmenopausal, and those who are lactose intolerant. Calcium carbonate is the most common form of calcium supplement. It should be taken with food because an acidic environment enhances absorption. For those with achlorhydria, which often occurs in seniors, calcium citrate may be more appropriate because it does not require an acidic environment for absorption and does not further reduce the acidity of the stomach (Straub, 2007).
Calcium supplementation absorption is optimal when taken as individual doses of 500 mg or less. Many formulations include vitamin D, because the likelihood of needing vitamin D is high if calcium supplementation is needed. Choosing a supplement that has the United States Pharmacopeia designation increases the likelihood that the supplement quantity is consistent with the label, and that good manufacturing practices are used.
Phosphate
Phosphate salts are available in practically all foods either naturally or because of processing. In healthy adults, the urinary phosphorus excretion approximately equals intake. The regulation of phosphorus levels in the blood is tightly controlled by an interaction between vitamin D from the kidney, PTH from the parathyroid glands, and fibroblast growth factor 23 from bone. Both calcium and phosphate ions in a ratio of approximately 1 : 1 are needed for the mineralization of bone.
Excessive phosphorus intake as phosphates can greatly alter the calcium/phosphate ratio, especially if calcium intakes are low. Too much phosphate compared with calcium lowers the serum calcium ion concentration, which then stimulates PTH; if this pattern of intake becomes chronic, bone loss is thought to follow.
Soft drinks are poor in nutrient value but high in phosphate content. However, studies have found that the soft drink primarily displaces milk as a beverage, so the negative effect is from lower calcium intake rather than higher phosphate intake. Some studies have found a negative correlation between soft drink intake and BMD in women but not in men. Those at high risk and those who have osteoporosis may want to avoid these beverages because an effect is theoretically possible (Tucker, 2009).
Magnesium
Magnesium dietary deficits seem to have little effect on bone tissue, but one report suggests that meeting the RDIs for magnesium improve BMD (Ryder et al., 2005). However, diets deficient in magnesium are likely deficient in other nutrients that are needed for healthy bone growth and maintenance. Nevertheless, magnesium deficiency may affect the quality of bone by decreasing bone formation, preventing the optimal crystal formation, and having a negative effect on PTH (Rude et al., 2009).
Trace Minerals
Few studies are available about the effects of trace elements on bone. Iron, zinc, copper, manganese, and boron may function in bone cells, but their specific roles in preventing bone loss are not well established. In one study, supplementation of copper, fluoride, manganese, and zinc along with calcium for 1 year resulted in a reduced loss of lumbar BMD compared with the greater loss in a group receiving only calcium supplementation (Nieves, 2005).
Boron
Boron is used by osteoblasts for bone formation. It is required to convert estrogen to its most active form, 17-beta-estradiol, and estrogen is involved in bone metabolism. However, it is not known whether, or how much boron is required for optimal bone health. (Hakki et al., 2010; Nielsen, 2008).
Copper
Copper is needed for the enzyme that increases the crosslinking of collagen and elastin molecules, and it may have roles in other enzymes of bone cells. Because of the changes induced in the two matrix proteins by low copper intakes, bone mineralization may also be reduced, especially in seniors.
Fluoride
Fluoride ions enter the hydroxyapatite crystals of bone as substitutes for hydroxyl ions. Water containing 1 ppm of fluoride does not help bone in the same way that it helps tooth surfaces. Within narrow limits of safety (less than 2 ppm), fluoride ions have little effect on increasing the hardness of bone mineral. At intakes of 2 ppm or greater, fluoride may produce bone that is subject to increased microfractures because of the change in the properties of the hydroxyapatite crystals.
Iron
Iron serves as a catalytic cofactor for the vitamin C–dependent hydroxylations of proline and lysine in collagen maturation. Iron also has other roles in osteoblasts and osteoclasts in mitochondrial oxidative-phosphorylation, as well as in other heme- and nonheme-containing enzymes, similar to the needs of other cells in the body.
Vitamins
An individual’s vitamin D status depends mostly on sunlight exposure, and secondarily on dietary intake of vitamin D. The synthesis of vitamin D by skin exposed to sunlight varies considerably as a result of many factors, including skin tone, sunscreen use, environmental latitude, and age (McCarty, 2008). The skin of older individuals is less efficient at producing vitamin D following exposure to ultraviolet (UV) light because the skin is thinner and it contains fewer cells that can synthesize vitamin D. In addition, older adults living in nursing homes and similar institutions typically have little exposure to sunlight. Those who live at northern latitudes in the United States and Canada are at increased risk of osteoporosis because of limited UV light during winter months.
The few foods that naturally contain vitamin D are egg yolks, fatty fish such as salmon, mackerel, catfish, tuna, and sardines, cod liver oil, and mushrooms (see Appendix 51). The vitamin D content of fish varies, as does the content in UV-exposed mushrooms. Fluid milk in the United States is fortified with vitamin D at a standardized level of 400 IU per quart, whereas other foods, including juices, cereals, yogurt, and margarines, may be fortified in varying amounts. The RDAs for vitamin D across the life cycle are shown inside the front cover. The upper limit is 100 µg (4000 IU) for everyone older than 8 years, and lower levels for younger children (see inside front cover). From any source, vitamin D must be hydroxylated in the kidney before becoming the physiologically active calcitriol.
To prevent rickets, the American Academy of Pediatrics recommends that all infants who are exclusively breastfed be supplemented with 400 IU of vitamin D. Infants who are both formula and breastfed should also be supplemented until they are consistently taking 1 liter (1 quart) of formula a day. They further recommend continuing the supplementation until 1 year of age, when children begin drinking vitamin D–fortified milk (Wagner and Greer, 2008).
The older adult is at increased risk for vitamin D deficiency. Risks are from decreased synthesis of vitamin D by the skin because of changes in the skin and decreased exposure to sunlight; increased body fat; decreased renal function that decreases the hydroxylation of vitamin D to its active form; and decreased levels of insulin-like growth factor 1, calcitonin, and estrogen, which affect hydroxylase activity. In general, seniors may benefit from daily vitamin D supplementation of 10-20 mcg (400 IU-800 IU) to reach serum 25-hydroxy vitamin D (calcidiol) levels of at least 30 ng/mL (75 nmol/L). Older adults who are frail or institutionalized may need up to 50 mcg (2000 IU)/day. Mobility, skin tone, body weight, and dietary habits may modify these recommendations (Oudshoorn et al., 2009). The most common blood test for vitamin D status is serum 25-hydroxyvitamin D level, although other tests may also be used.
Vitamin K
Vitamin K is an essential micronutrient for bone health. Its role in posttranslational modification of several matrix proteins, including osteocalcin, is well established. Following bone resorption, osteocalcin is released and enters the blood. In this way, osteocalcin serves as a serum bone marker for predicting the risk of a fracture (see Appendix 30). Many older adults have inadequate intakes of vitamin K, primarily because their consumption of dark-green leafy vegetables is so low. Most of the vitamin K intake in the United States is from green leafy vegetables, with about one third from fats and oils. Although menaquinones, a form of vitamin K, are formed in the gut by bacteria, the influence of this source on vitamin K status appears to be weak. It is important to consider the vitamin K intake in older persons who may also be taking blood-thinning medications (vitamin K antagonists). Rather than having these patients avoid vitamin K in foods and thus jeopardize their bone status, it is better to have the vitamin K daily intake be consistent and regulate the vitamin K antagonist medication. In fact, it has been shown that therapeutic international normalized ratio (INR) ranges from blood thinning medication can be achieved with vitamin K in low-dose supplementation, and when fluctuations are few (Ford and Moll, 2008).
Vitamin A (Retinol)
Vitamin A consumption is generally considered to be beneficial to bone growth and maintenance. Lycopene may be protective against oxidative stress; more research is suggested (MacKinnon et al, 2011).
Excessive retinol intake (but not carotenoids) may contribute to risk for hip fractures. However, there is not complete understanding, and many still question the effect on bone of excessive retinol intake (Ribaya-Mercado and Blumberg, 2007). Nevertheless, concern remains that the combined intakes of supplemental vitamin A and vitamin A from fortified foods may be too high in the United States, especially in health-conscious postmenopausal white women. The window of safe consumption of vitamin A is fairly narrow, but it may be even narrower for seniors.
Other Dietary Components
Several other dietary factors have been associated with bone health but their relative quantitative importance is not clear.
Alcohol
Moderate consumption of wine and beer may be beneficial to bone in men and postmenopausal women. Non-alcoholic constituents, such as silicon in beer, need further investigation.
In men, high liquor intakes (>2 drinks/d) are associated with significantly lower BMD (Kanis et al., 2005; Tucker et al, 2009). Heavy alcohol consumption also may be accompanied by poor dietary intake, cigarette smoking, poor balance, and an increased risk of falls.
Caffeine and Soft Drinks
The relationship of moderate consumption of caffeine to osteoporosis has not been clearly established. Excessive caffeine intake may have a deleterious effect on BMD (Ruffing et al., 2006). Intake of colas is also associated with lower BMD. Although the primary issue may be displacement of dairy beverages, there is also a potential direct effect (Tucker, 2009). Rapid metabolizers of caffeine may be a high risk group for bone loss (Hallström et al, 2010.)
Dietary Fiber
Excessive dietary fiber intake may interfere with calcium absorption, but any interference is considered extremely small in the typical low-fiber diet. Vegans who may consume as much as 50 g of fiber a day are most likely to have a significant depression in intestinal calcium absorption, but this is often offset by adequate calcium intake.
Isoflavones
The isoflavones in soybeans function both as estrogen agonists and antioxidants in bone cells. They inhibit bone resorption in female animal models without ovaries, but not in young adult females with normal estrogen status. Some but not all studies show modest skeletal benefits.
Potassium bicarbonate
The skeleton serves as a buffer to help regulate acid-base balance, and a high-acid diet may contribute to the progressive decline in bone mass and osteoporosis (Sebastian, 2005).
In postmenopausal women, an oral dose of potassium bicarbonate sufficient to neutralize endogenous acid improves calcium balance and bone. Decreased bone resorption and an increased rate of bone formation can result. See Clinical Insight: Urine pH—How Does Diet Affect It? in Chapter 36.
Sodium
A high sodium intake may contribute to osteoporosis because of increased calcium excretion (Massey, 2005). While the calciuric effect of sodium has been speculated, there seem to be no adverse effects with adequate calcium and vitamin D intake (Ilich et al, 2010).
Vegetarian Diets
Though research is inconclusive, vegetarian diets may be more beneficial for bone than animal-based diets. They may provide less calcium than animal diets but animal proteins contribute to urine acidity. In general, fruits and vegetables in the diet promote an alkaline urine and less need for neutralizing calcium. In addition they are high in potassium, which is considered a bone-protective nutrient. See Clinical Insight: Urine pH—How Does Diet Affect It? in Chapter 36. Polyphenols and other antioxidants in plant foods support optimal functioning and health of bone cells and provide many bone-healthy nutrients.
Osteopenia and Osteoporosis
Osteoporosis may have its origin in early life during the period of skeletal growth and PBM accumulation. The WHO defines osteoporosis in terms of decline in BMD.
Definitions
When BMD falls sufficiently below healthy values (1 standard deviation [SD] according to WHO standards) low bone mass or osteopenia exists. Osteoporosis occurs when the BMD becomes so low (greater than 2.5 SDs below healthy values) that the skeleton is unable to sustain ordinary strains. However, the National Osteoporosis Foundation (2010) states that the WHO BMD diagnostic classification should not be applied to premenopausal women, men younger than 50 years of age, or children. Clinical assessment and ethnically adjusted Z-scores are thought to be more reflective of the norms in other groups.
Prevalence
It is estimated that 8 million women and 2 million men in the United States are classified as osteoporotic. More than 2 million osteoporotic fractures were estimated to occur in 2005, which represents a cost of billions of dollars in health care and rehabilitation services. One fourth of these osteoporosis-related fractures involve the vertebrae; 297,000 are fractures of the hip, which typically result in incapacitation, long-term nursing care, and significant mortality.
Types of Osteoporosis
Osteoporosis is considered to have a broad spectrum of variant forms. There are two types of primary osteoporosis, distinguished in general by sex, the age at which fractures occur, and the kinds of bone involved. Secondary osteoporosis results when an identifiable drug or disease process causes loss of bone tissue (Box 25-2).
Estrogen-androgen deficient osteoporosis occurs in women within a few years of menopause from loss of trabecular bone tissue and cessation of ovarian production of estrogens. BMC and BMD measurements of the lumbar spine of women with postmenopausal osteoporosis may be as much as 25% to 40% lower than in age-matched nonosteoporotic control women of the same age range. Other bone sites with a preponderance of trabecular bone such as the pelvis, ribs, and proximal femur also display low BMD. Rarely, men may develop androgen-deficient osteoporosis if they have a significant decline in androgen production. This osteoporosis is characterized by fractures of the distal radius (Colles fractures) and “crush” fractures of the lumbar vertebrae that are often painful and deforming.
Age-related primary osteoporosis occurs at approximately age 70 and beyond. Both cortical and trabecular bone tissues undergo remodeling, but more remodeling occurs in trabecular tissue. In seniors, the processes of bone resorption and bone formation become uncoupled. Many women lose several inches in height between 50 and 80 years of age. Although age-associated osteoporosis affects both sexes, women are more severely affected because they have a smaller skeletal mass than men and they live longer.
Fractures may occur during ordinary activities, such as lifting a sack of groceries or stepping over a shower opening, but more hip fractures result from a fall. Hip fractures affect nearly 20% of postmenopausal women up to age 80 and almost 50% of those beyond that age, and the hip fracture numbers are steadily increasing in men. A dramatic increase in hip fractures occurs late in life, and almost all women beyond 80 years of age are at risk of hip fracture. Although fractures of the hips characterize this osteoporosis, vertebral fractures also increase with age. Wedge fractures of vertebrae typically lead to back pain, loss of height, spinal deformity, and kyphosis or “dowager’s hump.”
Causes and Risk Factors
Osteoporosis is a complex heterogeneous disorder and many risk factors contribute during a lifetime. Low BMD is common to all types of osteoporosis, but an imbalance between bone resorption and formation results from an array of factors characteristic of each form of this disease. Loss of bone mass to a degree that produces fractures can result from (1) an excessive acceleration of resorption, especially after menopause; or (2) a suboptimal peak bone mass that results in bone after menopause (or later in life in men) that becomes fragile and susceptible to fracture. Risk factors for osteoporosis include age, race, gender, and factors noted in Box 25-3.
Alcohol and Cigarettes
Cigarette smoking and excessive alcohol consumption are risk factors for developing osteoporosis, probably because of toxic effects on osteoblasts. Moderate alcohol intake has no detrimental effect on bone, and some studies show a modest positive effect in postmenopausal women. Three or more drinks per day is associated with increased risk of falling and may pose other threats to bone health. The risk appears significant even after adjusting for BMD when comparing smokers versus nonsmokers (North America Menopause Society, 2010). Excessive consumption (more than three drinks a day) for an extended period may result in bone loss. The combination of smoking and alcohol, common among young women and men, places them at increased risk for osteoporosis.
Body Weight
Body weight is a principal determinant of bone density and fracture risk; adipose tissue mass is a major contributor (Reid, 2010). The greater the body mass, the greater the BMD. Fat and bone are linked by pathways involving adiponectin; insulin, amylin, and preptin; and leptin and adipocytic estrogens, which ultimately serve the function of providing a skeleton appropriate to the mass of adipose tissue it is carrying (Reid, 2010).
The lower the body mass, the lower the BMD. Young girls who are typically premenarcheal may incur fractures with minimum trauma because of low BMC and BMD related to rapid growth in height that is not accompanied with a proportionate increase in weight (Goulding et al., 2005). Young, overweight males with low bone mass may also suffer fractures (Goulding et al., 2005). Weight loss from dieting, bariatric surgery, or sarcopenia are also associated with bone loss. Thus being overweight is protective against osteoporosis and underweight is a risk factor for fractures (Reid, 2010).
Ethnicity
Whites and Asians suffer more osteoporotic fractures than blacks and Hispanics, who usually have a greater bone density. However, hypovitaminosis D with secondary hyperparathyroidism occurs more often in the black population. Thin women, particularly of northern European ancestry, have the highest risk of osteoporosis.
Lactation
A striking but transient bone loss occurs in women who breast-feed for 6 months or longer, especially from the femoral neck and lumbar spine. Sufficient calcium and vitamin D intake are essential during this time for the mother to replete her own serum and storage levels, but repletion typically does not occur until several months after peak lactation. Several successive pregnancies and lactations over a relatively few years may contribute to significant bone loss by the end of the period of childbearing if nutrition is inadequate.
Limited Weight-Bearing Exercise
Maintenance of healthy bone requires exposure to weight-bearing pressures. A good diet plus exercise from roughly ages 10 to 20 years is particularly important for skeletal growth, accrual of bone mass, and increased femoral bone dimensions (Iuliano-Burns et al., 2005). Physical activity, especially upper body activities, is thought to contribute to an increase in bone mass or density (Chubak et al., 2006). Lack of exercise and a sedentary mode of living may also contribute to bone loss, although the most important influence is probably an inadequate accumulation of bone mass.
Exercise is beneficial for reducing skeletal inflammatory markers in frail older individuals (Lambert et al., 2008). Stresses from muscle contraction and maintaining the body in an upright position against the pull of gravity stimulate osteoblast function. Bones not subjected to normal use rapidly lose mass.
Immobility in varying degrees is well recognized as a cause of bone loss. Invalids confined to bed or persons unable to move freely are commonly affected. Astronauts living in conditions of zero gravity for only a few days experience bone loss, especially in the lower extremities; appropriate exercise is a feature of their daily routines.
Loss of Menses
Loss of menses at any age is a major determinant of osteoporosis risk in women. Acceleration of bone loss coincides with menopause, either natural or surgical, at which time the ovaries stop producing estrogen. Estrogen replacement therapies have been shown to conserve BMD and reduce fracture risk within the first few years following menopause, at least in short-term studies.
Any interruption of menstruation for an extended period results in bone loss. The amenorrhea that accompanies excessive weight loss seen in patients with anorexia nervosa or in individuals who participate in high-intensity sports, dance, or other forms of exercise has the same adverse effect on bones as menopause. BMD in amenorrheic athletes has been measured at levels 25% to 40% below normal. Young women with the “female athlete triad” of disordered eating, amenorrhea, and low BMD are at increased risk for having fractures. These young women may benefit from the use of oral contraceptive agents plus calcium and vitamin D supplements.
Nutrients
Many nutrients and several nonnutrients have been implicated as causal risk factors for osteoporosis and have been discussed in previous paragraphs. Frank vitamin D deficiency has been widely reported at northerly latitudes in North America and Europe. Vitamin D insufficiency is now considered more common at latitudes closer to the equator than previously thought because of reduced exposure to sunlight during the year (Hypponen and Power, 2007).
Medications
A number of medications contribute adversely to osteoporosis, either by interfering with calcium absorption or by actively promoting calcium loss from bone (Box 25-4). For example, corticosteroids affect vitamin D metabolism and can lead to bone loss. Excessive amounts of exogenous thyroid hormone can promote loss of bone mass over time.
Prevention of Osteoporosis and Fractures
The increasing longevity of the population emphasizes the need for prevention of osteoporosis. Universal guidelines apply to everyone. Consuming adequate amounts of calcium and vitamin D, lifelong muscle strengthening and weight-bearing exercise, avoidance of tobacco, moderate or no intake of alcohol, and steps to avoid falls are all part of the holistic approach to a lifestyle that promotes bone health (NAMS, 2010).
Exercise
To preserve bone health through adulthood, the American Academy of Sports Medicine recommends weight-bearing activity three to five times per week and resistance exercise two to three times per week with moderate to high bone-loading force for a combination of 30 to 60 minutes per week. Regular walking and swimming appear to have minor benefits in older individuals. More active participation (such as weight-bearing exercises and intensive walking) has positive effects on BMD.
Medical Nutrition Therapy
Calcium (1000 mg/day) and vitamin D (800 to 1000 units/day) are typically recommended as supplements for patients being treated with one of the bone drugs, either antiresorptive or anabolic. These amounts are considered both safe and sufficient for bone formation. The efficacy of calcium or calcium plus vitamin D supplementation continues to be investigated. Several studies report a reduction in fracture risk for postmenopausal women when supplements with calcium and vitamin D are used (Stránský and Rysavá, 2009). In a meta-analysis of 15 publications of nursing home residents, supplementation with calcium (1200 mg) and vitamin D (800 IU) reduced fracture risk and improved BMD (Parikh et al., 2009). Several studies also report the efficacy of calcium and vitamin D supplementation in older adults who live at home.
Interventions with children also show the benefits of calcium supplementation on PBM (Lanham-New, 2008). Reports are not consistent, however, possibly because of the variation in calcium and vitamin D status or environmental factors. Thus, because of the range of nutrients involved in bone health, a healthy diet emphasizing the key nutrients seems most promising in achieving an intake for optimal bone health (Tucker, 2009).
FDA-Approved Drug Treatments
Estrogen replacement therapy (ERT) is hormone-replacement therapy approved by the FDA as treatment for the prevention of osteoporosis. Because of potential side effects, nonestrogen treatment for prevention is recommended, especially if menopausal symptom relief is not a goal.
Bisphosphonates act as antiresorbers on osteoclasts to reduce their bone-degradative activities. They have been shown to be effective in reducing the incidence of new fractures (Epstein, 2006). The bisphosphonates act by inhibiting osteoclast-mediated bone resorption. Examples include alendronate, risedronate, ibandronate, and zoledronic acid. Side effects include gastrointestinal problems and rare cases of jaw necrosis.
Calcitonin, the hormone, is used to inhibit osteoclastic bone resorption by blocking the stimulatory effects of PTH on these cells. Calcitonin can be administered by nasal spray. It improves BMD, especially of the lumbar spine, and it may reduce the recurrence of fractures in patients with osteoporosis. Calcitonin is approved by the FDA for postmenopausal treatment of osteoporosis, but it is recommended that the women be at least five years’ postmenopausal.
PTH therapy is approved by the FDA for the treatment of postmenopausal women and men at high risk for fracture, and for those on long-term glucocorticoid therapy. PTH works by increasing osteoblast number and function (Kousteni and Bilezikian, 2008). PTH increases spine, hip, and total body BMD. PTH is often prescribed first, followed by bisphosphonates, so that an increase in bone mass is followed by antiresorptive therapy (Cosman, 2008).
Selective estrogen receptor modulators (SERMs) are able to stimulate estrogen receptors (ER) in bone tissue and yet have very little effect on the ERs of the breast or uterus. Another term for SERMs is estrogen agonist or antagonist because they act as weak estrogen agonists at times and as weak estrogen antagonists at others. Two examples of these drugs are tamoxifen and raloxifene. The most common side effect is hot flashes.
Drug Treatments Not Yet Approved By the FDA
Calcitriol is 1,25-dihyroxy vitamin D3, and has had little use in the treatment of osteoporosis because of its potential toxicity. Calcium plus calcitriol may be useful, however, in patients who are taking high-dose corticosteroid therapy, during which vertebral fractures are common.
Growth hormone and insulin-like growth factors may improve bone through anabolic effects, but more research is needed.
Osteoprotegerin (OPG) is a natural cytokine secreted by osteoblasts as well as other cell types. OPG can be detected in human serum and inactivates another cytokine that affects osteoclasts, thereby inhibiting osteoclast activation and bone resorption. Final results from clinical trials are anticipated.
PTH 1-84 is an intact human recombinant form of PTH undergoing clinical trials.
Sodium fluoride treatment increases bone mass, especially in trabecular bone. However, the quality of the bone typically is not normal. Fluoride ions become incorporated at the surfaces of hydroxyapatite crystals; the size and structure of the crystals become so altered that the mechanical competence of the bone declines. Fluoride therapy is not likely ever to be approved by the FDA.
Strontium ranelate is the mechanism supporting the reduction in spine and nonspine fractures; yet, the use of strontium is not clear.
Prevention of Falls
Fractures of the humerus, wrist, pelvis, and hip are often age related, resulting from a combination of osteoporosis and falling. Although only a small percentage of falls result in fractures, preventing falls through education and attention to the living environment of older adults is an important measure. Wearing girdles with built-in pads to protect the hips during a fall has been demonstrated in some, but not all, studies to significantly reduce the rate of fractures in a well-controlled investigation. A physical therapist can often evaluate the home to provide advice on reducing the likelihood of falls.
Center for Disease Control and Prevention
http://www.cdc.gov/nutrition/everyone/basics/vitamins/calcium.html
National Institutes of Health—Bone Health
http://www.nichd.nih.gov/health/topics/bone_health.cfm
References
Chubak, J, et al. Effect of exercise on bone mineral density and lean mass in postmenopausal women. Med Sci Sports Exerc. 2006;38:1236.
Cosman, F. Parathyroid hormone treatment for osteoporosis. Cur Opin Endocrin Diab Obes. 2008;15:495.
Darling, AL, et al. Dietary protein and bone health: a systematic review and meta-analysis. Am J Clin Nutr. 2009;90:1674.
Epstein, S. Update of current therapeutic options for the treatment of postmenopausal osteoporosis. Clin Ther. 2006;28:151.
Ford, SK, Moll, S. Vitamin K supplementation to decrease variability of international normalized ratio in patients on vitamin K antagonists: a literature review. Curr Opin Hematol. 2008;15(5):504.
Goulding, A, et al. Bone and body composition of children and adolescents with repeated forearm fractures. J Bone Miner Res. 2005;20:2090.
Hakki, SS, et al. Boron regulates mineralized tissue-associated proteins in osteoblasts (MC3T3-E1). J Trace Elem Med Biol. 2010;24(4):243.
Hallström, H, et al. Coffee consumption and CYP1A2 genotype in relation to bone mineral density of the proximal femur in elderly men and women: a cohort study. Nutr Metab (Lond). 2010;7:12.
Hinoi, E, et al. An osteoblast-dependent mechanism contributes to the leptin regulation of insulin secretion. Ann N Y Acad Sci. 2009;1173:E20.
Hypponen, E, Power, C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007;85:860.
Ilich, JZ, et al. Higher habitual sodium intake is not detrimental for bones in older women with adequate calcium intake. Eur J Appl Physiol. 2010;109:745.
Institute of Medicine (IOM), Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board: Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academy Press; 2011. Accessed at. www.nap.edu
Iuliano-Burns, S, et al. Diet and exercise during growth have site-specific skeletal effects: a co-twin study. Osteoporos Int. 2005;16:1225.
Kanis, JA, et al. Alcohol intake as a risk factor for fracture. Osteopros Int. 2005;16:737.
Khosla, S. Update in male osteoporosis. J Clin Endocrinol Metab. 2010;95:3.
Kousteni, S, Bilezikian, JP. The cell biology of parathyroid hormone in osteoblasts. Curr Osteoporos Rep. 2008;6:72.
Lambert, CP, et al. Exercise but not diet-induced weight loss decreases skeletal muscle inflammatory gene expression in frail obese elderly persons. J Appl Physiol. 2008;105:473.
Lanham-New, SA. Importance of calcium, vitamin D and vitamin K for osteoporosis prevention and treatment. Proc Nutr Soc. 2008;67:163.
MacKinnon, AS, et al. Dietary restriction of lycopene for a period of one month resulted in significantly increased biomarkers of oxidative stress and bone resorption in postmenopausal women. J Nutr Health Aging. 2011;15:133.
Massey, LK. Effect of dietary salt intake on circadian calcium metabolism, bone turnover, and calcium oxalate kidney stone risk in postmenopausal women. Nutr Res. 2005;25:891.
McCarty, CA. Sunlight exposure assessment: can we accurately assess vitamin D exposure from sunlight questionnaires? Am J Clin Nutr. 2008;87:1097.
Misra, M, Klibanski, A. Anorexia nervosa and osteoporosis. Rev Endocr Metab Disord. 2006;7:91.
National Health and Nutrition Examination Survey (NHANES). NHANES home. Accessed 2 April 2010 from www.cdc.gov/nchs/nhanes.htm.
National Osteoporosis Foundation [NOF.]. Website http://www.nof.org/. [Accessed 7/13/10].
Nielsen, FH. Is boron nutritionally relevant? Nutr Rev. 2008;66:183.
Nieves, JW. Osteoporosis: the role of micronutrients. Am J Clin Nutr. 2005;81:1232S.
North America Menopause Society (NAMS). Management of osteoporosis in post-menopausal women: 2010 position statement of the North America Menopause Society. Menopause. 2010;17:25.
Oudshoorn, C, et al. Ageing and vitamin D deficiency: effects on calcium homeostasis and considerations for vitamin D supplementation. Br J Nutr. 2009;101:1597.
Parikh, S, et al. Pharmacological management of osteoporosis in nursing home populations: a systematic review. J Am Geriatr Soc. 2009;57:327.
Plawecki, KL, et al. Assessing calcium intake in postmenopausal women. Prev Chronic Dis. 2009;6:124.
Pothiwala, P, et al. Ethnic variation in risk for osteoporosis among women: a review of biological and behavioral factors. J Womens Health. 2006;15:709.
Prentice, A. Milk intake, calcium and vitamin d in pregnancy and lactation: effects on maternal, fetal and infant bone in low- and high-income countries. Nestle Nutr Workshop Ser Pediatr Program. 2011;67:1.
Reid, IR. Fat and bone. Arch Biochem Biophys. 2010;503(1):20.
Reid, IR. Relationships between fat and bone. Osteoporos Int. 2008;19:595.
Ribaya-Mercado, JD, Blumberg, JB. Vitamin A: is it a risk factor for osteoporosis and bone fracture? Nutr Rev. 2007;65:425.
Rizzoli, R. Nutrition: its role in bone health. Best Pract Res Clin Endocrinol Metab. 2008;22:813.
Rude, RK, et al. Skeletal and hormonal effects of magnesium deficiency. J Am Coll Nutr. 2009;28:131.
Ruffing, J, et al. Determinants of bone mass and bone size in a large cohort of physically active young adult men. Nutr Metabol. 2006;3:14.
Ryder, KM, et al. Magnesium intake from food and supplements is associated with bone mineral density in healthy older white subjects. J Am Geriatr Soc. 2005;53:1875.
Sebastian, A. Dietary protein content and the diet’s net acid load: opposing effects on bone health. Am J Clin Nutr. 2005;82:921.
Stránský, M, Rysavá, L. Nutrition as prevention and treatment of osteoporosis. Physiol Res. 2009;58:S7.
Straub, DA. Calcium supplementation in clinical practice: a review of forms, doses, and indications. Nutr Clin Pract. 2007;22:286.
Tucker, KL. Osteoporosis prevention and nutrition. Curr Osteoporos Rep. 2009;7:111.
Tucker, KL, et al. Effects of beer, wine, and liquor intakes on bone mineral density in older men and women. Am J Clin Nutr. 2009;89:1188.
Wagner, CL, Greer, FR. American Academy of Pediatrics Section on Breastfeeding, American Academy of Pediatrics Committee on Nutrition: Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122:1142.