Chapter 12 The hip
Mennell (1964) describes the hip joint as ‘probably the most nearly perfect joint in the body …close to being a perfect ball-and-socket joint’. In erect bilateral stance each hip joint carries approximately one-third of the body’s weight (with the remaining one-third being found in the lower extremities), sufficient force to produce an actual bending between the femoral neck and the shaft of the femur (Lee 2004) (see also Box 12.1). One-legged standing, as well as the compounded force of hopping or landing on one leg, exaggerate these forces dramatically. It is the trabecular systems of the pelvis and femur which in particular resist this bending, shearing force (Levangie & Norkin 2005). Because of its vital role in locomotion and the interaction between the trunk and the lower extremities (especially the lumbo-pelvic-hip region), an optimal combination of osseous, joint, muscular and ligamentous function, as well as integral postural alignment, is required to maintain the hip joint in good working order.
Box 12.1 Compressive forces of the hip joint
Levangie & Norkin (2005) provide a thorough discussion of weight distribution in both bilateral and unilateral stance. They point to factors other than weight (such as torque created by the distance of the joint from the center of gravity of the body) to highlight that compression considerations are more complex than solely weight distribution. Regarding bilateral stance, they note that total hip joint compression, through each hip, should be one-third of body weight. However, they go on to report:
Bergmann and colleagues [1997] showed in several subjects with an instrumented pressure sensitive hip prosthesis that the joint compression across each hip in bilateral stance was 80% to 100% of body weight, rather than one-third (33%) of body weight, as commonly proposed. When they added a symmetrically distributed load to the subject’s trunk, the hip joint forces both hip joints increased by the full weight of the load, rather than by half of the superimposed load, as might be expected. Although the mechanics of someone standing who has a prosthetic hip may not fully represent normal hip joint forces, the findings of Bergmann and colleagues call into question the simplistic view of hip joint forces in bilateral stance.
In unilateral stance, the muscular contractions necessary for torque and countertorque add a tremendous muscular compressive force, much greater than the weight compressive force on the hip joint (Levangie & Norkin 2005).
Lee (2004) summarizes:
The form closure factors which contribute to stability at the hip include the anatomical configuration of the joint as well as the orientation of the trabeculae, and the orientation of the capsule and the ligaments during habitual movements.
Dysfunction therefore requires investigation of all these elements.
Influences are multidirectional, not just downward, from the trunk to the hip. For example, in discussing ‘other’ causes of low back pain, Waddell (1998) makes the pertinent observation:
You should usually be able to distinguish gastrointestinal, genitourinary, hip and vascular disease, if you think about them. We miss them when we do not think, but rather assume that every patient with a back pain must have a spinal problem.
If considering broadly, as Waddell suggests, it becomes evident that the pain could also be due to hip imbalances or from more distal structures of the lower extremity. As Greenman (1996) points out: ‘Dysfunction of the lower extremity [including the hip] alters the functional capacity of the rest of the body, particularly the pelvic girdle’. This is one reason why, when assessment is performed, it is useful to carry out the process from proximal to distal, with any indication of pelvic dysfunction (for example) demanding assessment of the structures distal to it, including the hip joint, knee joint and foot complex.
• The polyaxial articulation at the ball-and-socket hip joint is made up of the head of the femur, ‘the longest and heaviest bone in the body’ (Kuchera & Goodridge 1997), and its articulation with the cup-shaped acetabulum of the innominate bone. (See Fig. 11.1 B and 11.2 B for details of the acetabulum and Figs. 13.1 A and B for details of the femur)
• The articular surfaces are curved to accommodate each other reciprocally. Gray’s anatomy (2005) suggests that evidence favors there being spheroid and slightly ovoid surfaces, which become almost spherical with advancing age.
• Apart from a rough area where the ligament of the head attaches, the femoral head is covered by articular cartilage that, anteriorly, extends laterally over part of the femoral neck.
• The acetabular articular surface is moon shaped (lunate), so forming an incomplete ring, which is broadest above (where body weight is carried when upright) and narrowest in the pubic region.
• The acetabular fossa contains fibroelastic fat, mainly covered by synovial membrane. A fibrocartilaginous acetabular labrum increases acetabular depth.
• Ligaments include the iliofemoral, ischiofemoral, pubofemoral and the ligament of the head of the femur.
• The neck of the femur inclines toward the acetabulum, from the shaft of the femur, at angles that range from less than 120° (coxa varus) to over 135° (coxa valgus), with normal lying between these extremes (i.e. 120–135°) (Fig. 12.1).
• Dislocations occur more easily in a coxa valgus hip, particularly when the femur is adducted. It will be more stable, however, in abduction of the femur (wide-based stance).
• The hip joint displays a precise convex surface (femoral head) articulating symmetrically with the concave one (acetabulum) to provide an ‘outstanding example of a congruous joint’ (Cailliet 1996).
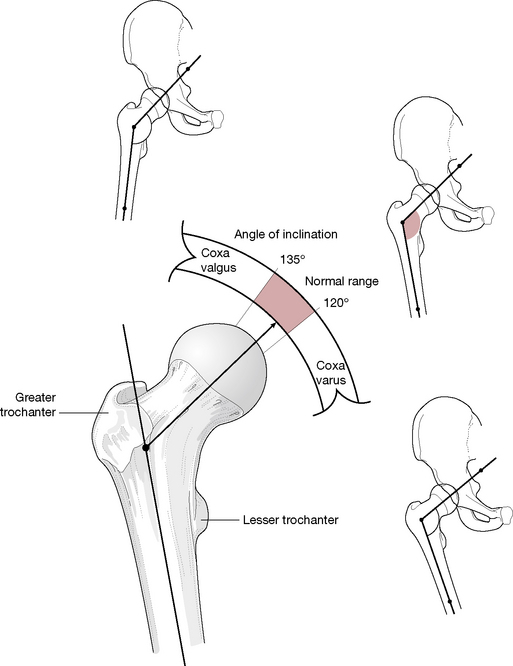
Figure 12.1 The hip joint showing the angle of inclination between the shaft and the neck of the femur in coxa varus and valgus
(adapted from Kuchera & Goodridge 1997).
Capsule, ligaments and membranes
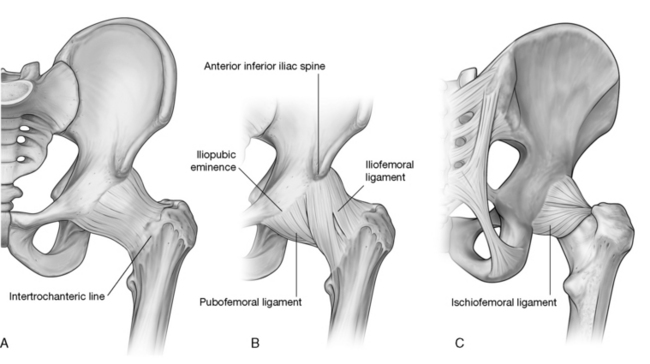
The hip’s fibrous capsule
This powerful structure attaches superiorly to the acetabular margin, just beyond the labrum, and anteriorly to the outer labrum and, close to the acetabular notch, to its transverse acetabular ligament and the rim of the obturator foramen. The capsule, which is shaped like a cylindrical sleeve, enfolds the neck of the femur, attaching to it anteriorly at the intertrochanteric line, superior to the base of the femoral neck. Posteriorly, the capsule attaches to the femur approximately 1 cm above the intertrochanteric crest and below to the femoral neck itself, close to the lesser trochanter.
Anteriorly, a longitudinal retinaculum runs superiorly along the neck, containing blood vessels that supply the femoral head and neck. Postural and functional stress, in the standing position in particular, falls anterosuperiorly and this is where the capsule is thickest. The capsule is composed of circular and longitudinal fibers.
• A collar around the neck of the femur is formed internally by circular fibers, known as the zona orbicularis, which merge with the pubofemoral and ischiofemoral ligaments.
• Longitudinal fibers lie externally, particularly anterosuperiorly, where they are reinforced by the iliofemoral ligament.
• The capsule also receives support from the pubofemoral and ischiofemoral ligaments.
• The capsule is covered by a bursa that separates it from psoas major and iliacus.
• Toe-out stance directs the head of the femur forward (out of the socket). The iliofemoral ligament would be too far forward to prevent subluxation and support would then need to be derived from the iliopsoas tendon.
Synovial membrane
Regarding the synovial membrane, Gray’s anatomy (2005) summarizes:
Starting from the femoral articular margin, it covers the intracapsular part of the femoral neck, then passes to the internal surface of the capsule to cover the acetabular labrum, ligamentum teres and fat in the acetabular fossa. …The hip joint may communicate with the subtendinous iliac (psoas) bursa by a circular aperture between the pubofemoral ligament and the vertical band of the iliofemoral ligament.
Iliofemoral ligament
This powerful triangular structure (commonly referred to as the Y-shaped ligament) lies anterior to the capsule with which it blends. It is a major stabilizing force for the anterior joint. The apex of the triangle attaches between the anterior inferior iliac spine and the acetabular rim, while the base of the triangle attaches to the intertrochanteric line. The ligament has been noted (Gray’s anatomy 2005) as having a less powerful central segment (greater iliofemoral ligament) lying between denser lateral and medial iliofemoral ligaments, both of which attach to the intertrochanteric line, at the superolateral and the inferomedial ends respectively (Fig. 12.2).
Pubofemoral ligament
This is another triangular-shaped structure with its base attaching at the iliopubic eminence, superior pubic ramus, obturator crest and membrane. The ligament merges with the joint capsule distally as well as with the medial iliofemoral ligament.
Ischiofemoral ligament
The posterior aspect of the capsule is supported by the ischiofemoral ligament, which comprises different elements.
• A central part runs from the ischium, posteroinferiorly to the acetabulum.
• ‘The superior ischiofemoral ligament spirals superolaterally behind the femoral neck, some fibers blending with the zona orbicularis, to attach to the greater trochanter deep to the iliofemoral ligament.
• Lateral and medial inferior ischiofemoral ligaments embrace the posterior circumference of the femoral neck.’ (Gray’s anatomy 2005)
Ligamentum teres (Fig. 12.3)
This ligament, also called the ‘ligament of the head of the femur’, is a ‘triangular flat band, its apex is attached anterosuperiorly in the pit on the femoral head; its base is principally attached on both sides of the acetabular notch, between which it blends with the transverse ligament’ (Gray’s anatomy 2005). The ligament is encased by a synovial membrane, ensuring that it does not communicate with the synovial cavity of the hip joint. The ligamentum teres becomes taut when the thigh is adducted and partially flexed. It releases on abduction.
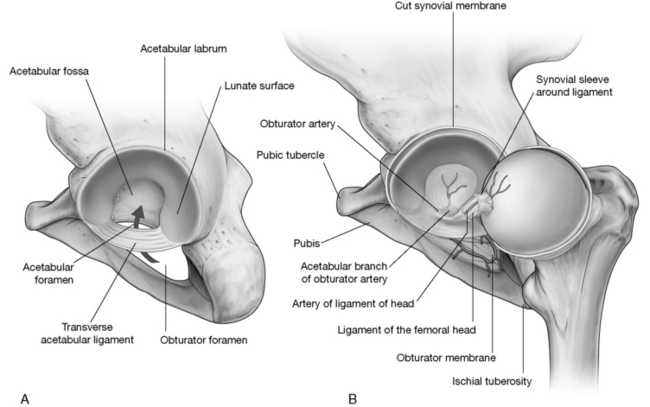
Figure 12.3 A: Acetabulum of hip joint. B: Ligamentum teres provides vascular supply to the head of the femur.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Kapandji (1987) notes: The ligamentum teres plays only a trivial mechanical role though it is extremely strong (breaking force equivalent to 45 kg weight [about 100 lbs]). However, it contributes to the vascular supply of the femoral head. (Kapandji’s emphasis). His illustration depicts the artery of the ligamentum teres coursing through the ligament to supply the proximal end of the femoral head. This secondary blood supply is important to both the child and the adult for different reasons. In the developing child, blood from the retinacular vessels cannot travel through the avascular cartilaginous epiphysis so the head of the femur is supplied through the artery of the ligamentum teres. For the adult this secondary supply might become especially important in preventing avascular necrosis of the femoral head if the primary supply from the retinacular vessels were injured in femoral neck fractures.
Transverse acetabular ligament
This ligament’s strong, flat fibers cross the notch and form a foramen through which vessels and nerves enter the joint (see Fig. 12.3).
Stability
The hip joint’s design provides for excellent stability, unlike that of the shoulder, which is designed more for mobility. When comparing the two joints, it is obvious that the articular surface of the humeral head is greater than that of the glenoid cavity, with the capsule (of the shoulder) offering little restraint. In contrast, in the hip there is a closer fit of the head of the femur to the acetabulum with the labrum providing an encompassing attachment to hold it in place, thereby qualifying the hip as a true ball-and-socket joint (Kapandji 1987), with powerful ligaments providing stabilizing support anteriorly and muscles dominating the support posteriorly.
In the erect position, stability of the hip is also assisted by the interaction of ground forces and gravity. The femoral head is pressed upward by ground forces matching the weight of the body applied by the overhanging ‘roof’ of the acetabulum (Kapandji 1987). Atmospheric pressure as well as appropriate position of the femoral head will also assist in maintaining apposition of the articular surfaces.
The hip ligaments are under moderate tension when the body is in an erect posture and become more taut as the leg moves into extension. Anteriorly, significant stability derives from the ligamentous support, as Gray’s anatomy (2005) explains: The thick capsule is reinforced by three ligaments, of which the iliofemoral is the strongest, and is progressively tightened when the femur extends to the line of the trunk. The pubofemoral and ischiofemoral ligaments also tighten and, as the joint approaches close-packing, resistance to an extending torque rapidly increases. This also implies that the iliofemoral ligament prevents excessive posterior tilt of the pelvis, which constitutes extension of the hip joint.
Despite the considerable power of some of these ligamentous structures (Kuchera & Goodridge (1997) state that the iliofemoral ligament is the most powerful ligament in the body), it is the enormous muscles of the area, including gluteus maximus and the hamstrings, which dominate in providing stability for the posterior portion of the hip joint. As Kuchera & Goodridge (1997) explain:
Flexion of the hip is limited more by the muscles and soft tissues than by ligaments [all hip ligaments are relaxed during flexion]. Straight leg raising at the hip around a transverse axis is limited by the hamstring muscles to 85–90°. If the knee is bent to remove hamstring influence, the thigh can normally be flexed to 135° at the hip.
Angles
Angle of inclination
The angle formed by the shaft and the neck of the femur is termed the angle of inclination (collodiaphysial angle). This angle in the normal adult averages about 125° (though less in women than men) and is greater in the newborn (150°) and less in the elderly (120°) (see Fig. 12.1).
A pathologically decreased angle of inclination (producing coxa vara) affects the strength and stability of the head and neck of the femur (Platzer 2004), as do the trabeculae (Fig. 12.4). The smaller the angle of inclination, the greater the shearing force on the natural ‘zone of weakness’ of the neck of the femur. This decreased angle of inclination will also affect the positioning of the knee and knee mechanics as the weight-bearing line will then run through the medial femoral condyle and produce genu varum of the knee (bow legs).
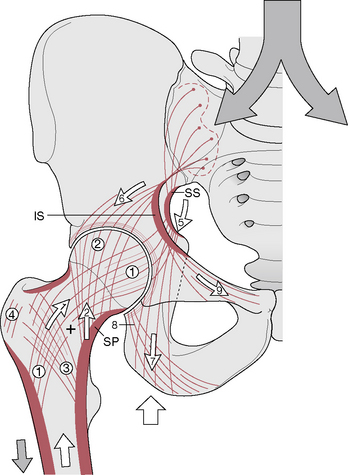
Figure 12.4 The trabecular systems transmit vertical forces from the vertebral column to the hip joints and help prevent damage by shearing forces at the femur’s natural ‘zone of weakness’. The + indicates zone of weakness where fracture commonly occurs
(reproduced with permission from Kapandji 1987).
A pathological increase in the angle of inclination (producing coxa valga) will likewise affect both hip and knee function as can pelvic dysfunction (Box. 12.2). The hip will have a greater tendency to dislocate while the altered weight bearing on the knee joint will be placed primarily on the lateral condyle and result in genu valgum (knock knees) (Platzer 2004). These effects on weight bearing on the knee joint will also produce abnormal loading on the meniscus, often resulting in deterioration of the knee joint.
Box 12.2 Motions of the pelvis at the hip joint
Though movements of the femur are usually used to describe the range of motion of the hip joint, it is far more common for the weight-bearing femur to be relatively fixed and movement to be produced by the pelvis. Several motions of the pelvis at the hip can be considered when the femur is fixed; however, it should also be remembered that during gait both the femur and the pelvis can be moving simultaneously.
Levangie & Norkin (2005) discuss three movements of the hip on the femur and note that regardless of which segment is moving (femur or pelvis), the range of motion of the joint remains the same.
Anterior/posterior tilt of the pelvis (see Fig. 2.16)
In the normal pelvis, the anterior superior iliac spines (ASIS) and the posterior superior iliac spines (PSIS) lie on the same horizontal plane while the ASIS lies on a vertical plane with the symphysis pubis. Anterior tilting of the pelvis (bilaterally) produces flexion of both hips while posterior tilting produces extension of both hips. If the sacrum moves with the innominates, extension and flexion of the spine will also occur (respectively).
Lateral pelvic tilt (see Fig. 12.6)
In the normal pelvis, the ASISs are in horizontal alignment. When they are not horizontally aligned, lateral tilt of the pelvis has occurred. One side of the hip is ‘hiked’ or ‘dropped’ in relation to the other whether in unilateral or bilateral stance (Fig. 12.6). These movements, involving abduction and adduction of the femur, are functionally critical in gait, where weak abductors can create a Trendelenburg sign (see pp. 400 and 426). A key element in assessing lateral tilt is to follow the crest of the non-fixed leg. Levangie & Norkin note that ‘osteokinematic descriptions reference the motion of the end of the lever farthest from the joint axis’.
Pelvic rotation
This motion of the entire pelvis around a vertical axis is best seen from above (see Fig. 3.10). This movement is most common during the single limb support in the gait cycle, although it may be seen in bilateral stance. These motions involve medial and lateral rotation of the femur and are described regarding the movement of the side of the pelvis contralateral to the fixed limb. It should be noted that the terms ‘forward rotation’ or ‘backward rotation’ of the pelvis describe this motion around the vertical axis and should be distinguished from anterior and posterior movements of the individual innominate (or pelvis) around a horizontal axis as these describe the condition noted above as anterior or posterior tilt.
Coordinated activities
Although these three motions of the pelvis may occur individually, they are most dynamically depicted during gait, when they should occur in a magnificently coordinated manner that results in a fluid pattern of movement, not only of the pelvis but also involving many of the joints that lie above and below the pelvis. Interruption of this vibrant kinetic cycle can be produced by a number of dysfunctional patterns, including tight or weak hip musculature, inappropriate firing sequences of muscles, joint dysfunction or pathology as well as dysfunctions within other regions of the body, particularly the foot.
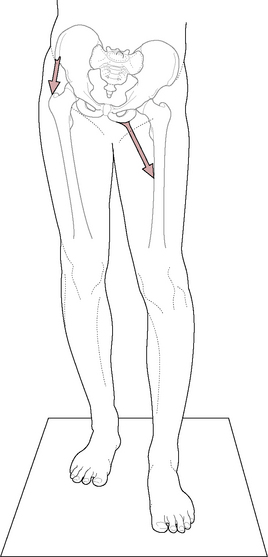
Figure 12.6 Lateral tilt of the pelvis in bilateral stance. Here the right abductors and left adductors will need to work synergistically to shift the weight back to center
(adapted from Levangie & Norkin 2001).
The angle of torsion (also called the angle of anteversion) of the femur expresses the relationship between an axis through the femoral condyles and the axis of the head and neck of the femur (Fig. 12.5). This angle can be observed when looking down the length of the femur from above the femoral head toward the knee. With the femoral condyles lying appropriately in the frontal plane, the axis through the head and neck of the femur normally forms an angle of 10–15° with the frontal plane (although it may vary from 7° to 30°). Levangie & Norkin (2005) point out that a pathological increase of this angle (anteversion), or decrease of the angle (retroversion) as well as abnormal angles of inclination, can:
cause compensatory hip changes and can substantially alter hip joint stability, the weightbearing biomechanics of the hip joint, and muscle biomechanics. …Each structural deviation warrants careful consideration as to the impact on hip joint function and function of the joints both proximal and distal to the hip joint.
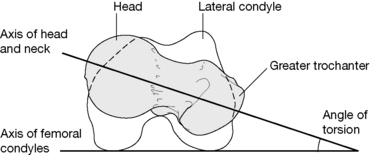
Figure 12.5 The angle of torsion, 15°in the normal adult, depicts the degree to which the femoral head and neck are twisted with respect to the femoral condyles
(adapted from Levangie & Norkin 2001).
If compensations arising from such inborn idiosyncratic variations in the ‘normal’ angle of the femur can produce altered distal and proximal joint changes as well as muscular modifications, the importance of this angle becomes clear. Structural and functional features that might be considered abnormal if the angle of the femur is within normal range might be considered acceptable adaptations when the angle is excessive or reduced. Manual practitioners, who treat patients without the aid of X-ray or other tools such as a clinical goniometer, which identify structural idiosyncrasies, often assess for and recognize apparently ‘dysfunctional’ features, such as lateral rotation of the femur or a wide stance. Such patterns of so-called ‘dysfunction’ may be adaptive compensations for structural abnormalities that are not visually perceivable. In other words, what is abnormal for the normal body might be a natural compensation for the abnormal structure and whether that structure is normal or abnormal may be beyond easy perception. Application of therapy to ‘fix’ or modify the postural positioning, in the case of abnormal structural development, might result in undesirable consequences.
Movement potential
The potential motions of the hip joint include flexion-extension, adduction-abduction, medial and lateral rotation (which are accompanied by glide or spin), as well as circumduction (which is a compound movement resulting from a combination of these six). Gray’s anatomy (2005) implies that there are no accessory movements available, except for very slight separation when strong traction is applied.
Gray’s anatomy (2005) further suggests that ‘circumduction, [can be] conveniently considered as rotations around three orthogonal axes’. It continues:
When the thigh is flexed or extended, the femoral head ‘spins’ in the acetabulum on an approximately transverse axis. Conversely, the acetabula rotate around similar axes in flexion and extension of the trunk on stationary femoral heads. With the foot stationary on the ground, medial and lateral femoral rotation have a vertical axis through the centre of the femoral head and medial condyle. Such axial medial rotation is the inevitable conjunct rotation accompanying terminal extension of the knee and is often referred to as ‘screw home’. The reverse occurs in initial flexion at the knee joint…
In discussion of accessory movements available at the hip later in this chapter (pp. 404–405), it will be seen that there is no general agreement on this topic.
When the knee is in neutral (not bent), active hip flexion to 90–100° from the vertical is possible; however, active extension of the hip beyond the vertical is limited to between 10° and 20°. These movements are enhanced by modifications of the spine and pelvis and/or by flexion of the knee and associated medial or lateral rotation of the hip. Gray’s anatomy (2005) offers an example:
For example, knee flexion (lessening tension in the posterior femoral muscles) increases hip flexion to 120°; the thigh can be drawn passively to the trunk, though with some spinal flexion. Extension in walking and running is increased by forward inclination of the body, pelvic tilting and rotation and lateral hip rotation. Abduction and adduction can be similarly increased.
Passive assistance of hip flexion will increase its range to 145° while passive assistance of extension can increase its range to 30°.
Lee (2004) has graphically detailed the multiple ligamentous involvements in all hip movements. For example:
Extension of the femur winds all of the extraarticular ligaments around the femoral neck and renders them taut. The inferior band of the iliofemoral ligament is under the greatest tension in extension. Flexion of the femur unwinds the ligaments, and when combined with slight adduction, predisposes the femoral head to posterior dislocation if sufficient force is applied to the distal end of the femur (e.g. dashboard impact).
Visualizing the coiling and uncoiling of ligaments as they wrap and unwrap around the neck of the femur, in varying positions of extension and flexion, offers a potent image. More details regarding the muscles responsible for the various ranges of movement can be found in the techniques portion of this chapter where the muscles are grouped according to primary function.
Muscles producing movement (Gray’s anatomy 2005)
• Flexion of the hip with the knee extended is generally about 90° and with the knee flexed reaches about 120°. Hip flexion is produced primarily by psoas major and iliacus, assisted by rectus femoris, sartorius, pectineus, and tensor fasciae latae. The adductors, particularly adductor longus and gracilis, also take part, particularly in early flexion from a fully extended position. The anterior fibers of gluteus medius and minimus also offer weak assistance.
• Extension range is usually considered to be about 10–20° and is primarily produced by gluteus maximus and the hamstrings and assisted by posterior fibers of gluteus medius and minimus and adductor magnus.
• Abduction to about 45–50° is produced by gluteus medius and minimus, assisted by tensor fasciae latae (especially when the hip is flexed), upper fibers of gluteus maximus, sartorius, piriformis (especially when hip is flexed to 90°) and possibly other hip rotators when the hip is flexed.
• Adduction of 20–30° from neutral is performed by adductors longus, brevis and magnus, assisted by pectineus, gracilis, gluteus maximus, the hamstrings, quadratus femoris and obturators internus and externus.
• Medial rotation (with the hip joint in flexion to 90°) offers about 30–35° and is primarily produced by tensor fasciae latae and the anterior fibers of gluteus minimus and medius, although no muscle has this action as its primary function (Levangie & Norkin 2005). Gray’s anatomy (2005) informs us that: ‘Electromyographic data suggests that the adductors usually assist in medial rather than lateral rotation but this is, of course, dependent on the primary position [of the femur]’. Travell & Simons (1992) note that piriformis appears to rotate the thigh medially when the hip is fully flexed.
• Lateral rotation of 50–60° is produced by gluteus maximus, posterior fibers of gluteus medius and minimus, piriformis, obturator externus and internus, gemelli superior and inferior, quadratus femoris, portions of adductor magnus and, in some positions, sartorius.
Disturbances of any of these ranges of movement might therefore call for diligent investigation of the strength of the prime and accessory movers (agonists), shortness of the antagonists, as well as the active presence of myofascial trigger points in any of the agonists or antagonists.
Muscular imbalances in which postural muscles shorten and phasic muscles become inhibited, and possibly lengthen, may play a major part in the evolution of hip dysfunction, encouraging aberrant movement patterns and resulting in adaptational – and ultimately degenerative – changes in the hip, pelvic and spinal joints (Janda 1986). The issues and concepts associated with varying responses to overuse or misuse, by different categories of muscles, are discussed fully in Volume 1, Chapter 5, and are summarized in the Essential Information chapter at the start of this book.
Relations
The muscles and other structures associated with the joint capsule are as follows.
• Anteriorly, the lateral fibers of pectineus separate its most medial part from the femoral vein.
• The tendon of psoas major, with iliacus lateral to it, descends across the capsule with the femoral artery lying anterior to the tendon.
• The femoral nerve lies in a furrow between the tendon and iliacus muscle.
• The straight head of rectus femoris crosses the joint laterally together with a deep layer of the iliotibial tract, which merges with the capsule beneath the lateral border of rectus femoris.
• The head of rectus femoris contacts the capsule superomedially and gluteus minimus covers it laterally.
• Inferiorly, the lateral fibers of pectineus lie alongside the capsule, while obturator externus is located posteriorly. The tendon of obturator externus covers the lower capsule posteriorly, dividing it from quadratus femoris.
• Superior to this the obturator internus tendon and the gemelli pass close to the joint, separating it from the sciatic nerve.
• The nerve supply for quadratus femoris lies beneath the obturator internus tendon.
• Superior to this piriformis crosses the posterior surface of the joint.
Vessels and nerve supply to joint
Articular arteries are branches from the obturator, medial circumflex femoral, and superior and inferior gluteal arteries. Nerves are from the femoral or its muscular branches, the obturator, accessory obturator, the nerve to quadratus femoris and the superior gluteal nerves. (Gray’s anatomy 2005)
Assessment of the hip joint
Is the hip joint behaving normally?
Symptoms of hip joint dysfunction usually include:
• pain aggravated by walking (especially on hard surfaces)
• pain when standing for anything but a short period
• relief of pain when lying down unless lying on the painful side
• painful distribution includes low back and the hip, into the groin and toward the knee.
• a positive Patrick’s (F-AB-ER-E) sign (see p. 407)
• tenderness at the head of the femur when palpated in the groin
Additionally, there is likely to be sensitivity close to the iliac crest and greater trochanter, where the abductors attach.
Lewit (1985) reports that limitation of adduction at the hip might be due to spasm initiated by trigger point activity located at an attachment at the pes anserinus (knee pain may also be reported).
A postural modification occurs over time, leading to prominence of the ipsilateral buttock and compensatory hyperlordosis of the lumbar spine.
Arthritic hip changes are discussed later in this chapter and discussion of hip joint reconstruction surgery is to be found in Box 12.7.
Box 12.7 Total hip replacement
Gray’s anatomy (1995) states: ‘Total hip replacement has, over the last 25 years, become one of the most successful surgical operations, with over 35 000 performed annually in the United Kingdom alone’. Hip replacement is now so widespread that it is important for practitioners to be aware of the variations in surgical procedure and what is and what is not appropriate in terms of adjunctive therapeutic intervention.
Those most likely to undergo replacement are patients with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, avascular necrosis, trauma and tumors affecting the hip. Symptoms preceding the operation are likely to have included pain (mainly over trochanter area, groin and anterior thigh), stiffness, deformity, limb shortening and, therefore, a consequent limp. See the discussion regarding possible trigger point input to arthritic hip pain on p. 411.
The most common current hip replacement comprises a polyethylene hemispherical socket cemented into the acetabulum plus a spherical metallic head and stem (made of titanium alloy, stainless steel or chrome cobalt alloy).
Depending on the type of procedure used, surgical access to the joint can involve:
• a lateral approach in which there is dissection of tensor fasciae latae (Charnley method)
• a posterior approach involving division of the short external rotator muscles (piriformis and the gemelli)
• an anterolateral approach involving separation of the junction between gluteus medius and tensor fasciae latae. The operation scar is a useful clue as to which approach has been used and, therefore, which muscles have been most traumatized.
Despite total hip replacement being ‘mechanically crude’ (Gray’s anatomy 1995), there is more than 90% possibility of the joint remaining fully functional for at least 10 years. Failure usually relates to infection, dislocation or, more commonly, from a loosening of the prosthesis, often through inadequate cementing procedures.
Dalstra (1997) offers other explanations as to why the reconstructed joint may become unstable.
At the femoral side, a metal stem is inserted into the medullary canal. Owing to the high stiffness of this stem compared with that of the bone shaft, the surrounding cortex will become stress-shielded (it does not transfer as much load as it did preoperatively). This phenomenon carries the potential danger of a local reduction of bone mass (Wolff’s law: changes in the function of bone lead to changes in its architecture) which may eventually lead to a loosening of the implant due to lack of supporting bone stock.
Dalstra additionally notes that on the acetabular side of the reconstruction, problems may arise. He reports that a variety of methods of creating a cup may be used, ranging from cemented to non-cemented, hemispherical or conical, with or without metal backing, which ‘also creates an unnatural situation, but its consequences are not as directly apparent as on the femoral side’.
Stress distribution
With hip replacement (reconstruction) the stress loads imposed on aspects of the hip joint alter noticeably (Dalstra 1997). In a normal joint the greatest stress is borne by the subchondral bone in the anterosuperior quadrant, whereas in a reconstructed hip the stresses reduce markedly and are passed to the edges of the joint (Fig. 12.15). This is due to alterations in the rigidity of the pelvic structures, because of new materials, and also to absorption of stress within the cup itself (‘load diverting’), rather than in the bone. The results of these changes can involve bone resorption (Wolff’s law again) as well as problems at the interface of the prosthesis and bone, possibly causing it to fail. As Dalstra reports, ‘effects, such as wear particles, play an important role in the failure mechanism of acetabular implants’.
For the future, ceramic heads coupled with polyethylene sockets, ceramic on ceramic and metal on metal bearing surfaces are all being evaluated, as are innovative cementing strategies.

Figure 12.15 Comparison between the stress intensity in the subchondral bone layer of a normal pelvic bone (left) and a reconstructed pelvic bone (right) during one-legged stance
(reproduced with permission from Vleeming et al 1997).
Is the source of pain a joint or the soft tissues associated with the joint?
When a joint is restricted or painful it is useful to know what degree of contractile soft tissue involvement there is in the dysfunction. Obviously, it is possible (and not uncommon) for the problem to involve both intra- and extraarticular tissues; however, at times it will be one or the other. Active and passive movement of the joint offers a guide (Petty 2006).
• If both active and passive movements of a joint are painful and/or restricted, during movement in the same direction, the source of dysfunction involves non-contractile structures such as the ligaments.
• If both active and passive movements of a joint are painful and/or restricted, during movement in opposite directions, the source of dysfunction involves contractile structures, the musculature.
Differentiation
Lee (2004) suggests that, when confronted by hip symptoms, it is necessary to have in mind those hip conditions that emerge during different periods of growth and development, as well as two broad classifications: articular and non-articular, relating to restriction (hypomobility) of the joint with or without pain, and pain that is present without evidence of restriction, respectively. Lee has provided summaries that help to keep these clinical distinctions in reasonable order (See Boxes 12.3 and 12.4).
Box 12.3 Classification of hip disorders according to age group (Cyriax 1954)
(reproduced with permission from Lee 2004)
Box 12.4 Articular versus non-articular disorders of the hip
(reproduced with permission from Lee 2004)
Ultimately, all assessments and tests have one aim, Lee (1999) asserts: ‘to identify the system (i.e. articular vs. myofascial) which is aberrantly altering the osteokinematic function of the femur during functional movement, so that treatment can be directed accordingly’.
Once established, joint degeneration will clearly involve both articular and soft tissues but in the early stages, where symptoms are mild (stiffness, mild generalized discomfort), establishing a primary focus for therapeutic attention is vital if the insidious progression to major dysfunction is to be halted.
It is also important to recall that, as hip dysfunction evolves, many compensating adaptations will occur, involving the soft tissues of the region, as well as the lumbar spine, SI joints, knees and feet, with patterns of pain and discomfort possibly involving the hip area itself, the buttock, groin, anterior thigh, knee and lower leg.
One of the first aspects of function to be affected when hip disorders emerge will be gait, which is fully discussed in Chapter 3. The earliest indications of hip dysfunction may be demonstrated by a reduced stance phase, with a ‘dot and carry’ limp. As compensations gradually occur muscular imbalances will become pronounced, reducing the force closure potential of the SI joint (see Chapter 11) and the patient’s center of gravity will deviate toward the affected side, resulting in the compensated Trendelenburg sign (Fig. 12.7A).
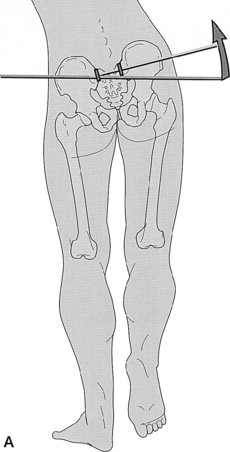
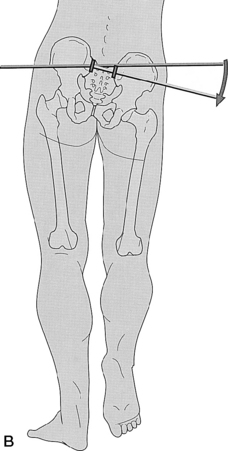
Figure 12.7 A: Compensated Trendelenburg (reproduced with permission from Lee 1999). B: True Trendelenburg
(reproduced with permission from Lee 1999).
Lee explains: ‘In a fully compensated gait, the patient transfers their weight laterally over the involved limb (compensated Trendelenburg), thus reducing the vertical shear forces through the SIJ. In a non-compensated gait pattern, the patient tends to demonstrate a true Trendelenburg [sign]’ (Fig. 12.7B).
Muscular involvement: general assessments
The functional tests suggested by Janda (1983) offer a rapid screening of major movement patterns and the behavior of key hip joint muscles.
• Prone hip extension test (see Chapter 10, p. 291, for description of this test and also see Fig. 10.65) demonstrates relative imbalance between the hip extensors themselves (gluteus maximus, the hamstrings and the erector spinae muscles) as well as between the hip extensors and the hip flexors (iliopsoas, quadriceps).
• Sidelying hip abduction test (see Chapter 11, p. 320, and also Fig. 11.17 for description of this test) demonstrates relative imbalance between the hip abductors themselves (gluteus medius, quadratus lumborum and tensor fasciae latae) as well as between the hip abductors and adductors.
• Postural changes relative to such imbalances may be demonstrated by simple observation of the lower crossed syndrome pattern, as discussed and illustrated in Volume 1, Chapter 5, and in Chapter 11 of this volume.
Liebenson (2007) reports that altered hip extension (see hip extension test described in Chapter 11) commonly involves a weak gluteus maximus, together with overactive (or substituting) and probably shortened:
Trigger point activity is probable in gluteus maximus, iliopsoas, erector spinae and the contralateral upper trapezius and levator scapula. There is likely to be an anterior pelvic tilt, forward drawn posture, increased lumbar lordosis and altered firing sequence of these muscles.
Liebenson further reports that altered hip abduction (see hip abduction test, relating to QL assessment, described in Chapter 11) commonly involves weak gluteus medius, together with overactive (or substituting) and probably shortened:
Trigger point activity is probable in gluteus medius and minimus, piriformis, TFL and QL. There is likely to be a blocked SI joint and altered firing sequence of these muscles.
Once an overall picture, of possible muscular weakness and shortness changes, has been obtained by observational and functional assessment, specific degrees of shortness and/or weakness should be established by focused testing of each muscle. A number of suggestions for such assessment have been provided, muscle by muscle, in the various clinical applications chapters of this volume, much of it based on the work of Janda (1983), Lewit (1999) and Liebenson (2007).
The next stage of evaluation calls for establishing the presence and status of localized myofascial disturbances (trigger points) within the muscles of the region, using NMT or other appropriate palpation methods. These methods are fully described in each clinical applications chapter (see discussion of technique application in Chapter 9).
Signs of serious pathology (other than osteoarthritis – OA)
Lee (2004) reminds us that early evidence of serious hip pathology (such as septic bursitis, osteomyelitis, neoplasm of the upper femur, fractured sacrum) may be obtained by means of signs which, as Cyriax (1954) put it, ‘draw immediate attention to the buttock’. Cyriax suggested that if there is pain or limitation when the hip is passively flexed, with the knee extended, or if there is limitation and greater pain on passive flexion of the hip but this time while the knee is slightly flexed, ‘Further examination [should] reveals a non-capsular pattern of limitation of movement at the hip joint’. Lee (2004) suggests that the end-feel of such restrictions will be ‘empty’, unlike restriction resulting from articular (OA) or myofascial causes, which are likely to produce ‘hard’ and ‘soft’ end-feels respectively, although clinically, ‘the two are usually seen in combination’. An ‘empty’ end-feel, Lee cautions, requires that serious pathology be ruled out before any treatment is started that could potentially aggravate the problem.
False alarms and other options
A number of physical medicine experts have provided examples that highlight the difficulty all practitioners face when attempting to localize the source of pain in the pelvic and hip areas. (See Box 12.5)
• A patient may report the hip feeling ‘out of place’, with the whole leg feeling heavy. The problem, Maitland (2001) suggests, is likely to be an ipsilateral sacroiliac joint strain or sprain. The pain from SI joint problems frequently overlaps with pain deriving from neural structures, the spine or the hip itself.
• Maitland also reports that Schwartzer (1995) consistently proved (using anesthetic block and MRI scans) that groin pain was usually associated with SI joint disorders.
• Lewit (1985) reports on 59 cases of early-stage arthritis of the hip with little (16 patients) or no (43 patients) evidence of degenerative change shown on X-ray, where low back pain was the most severe and frequent complaint.
• Pain in the hip region may be a result of neural impingement, i.e. adverse neurodynamic tension. Specific evaluation techniques, such as the slump test with seated straight leg raising, is helpful in picking up radicular pain. Sensitizing and relieving maneuvers with the slump test can help to differentiate hamstring tightness from adverse neurodynamic tension. Similarly, the sidelying femoral nerve stretch test uses sensitizing and relieving maneuvers that can help to differentiate quadriceps tightness from adverse neurodynamic tension in the distribution of the femoral nerve. (See Figs 12.8A-D)
• Hreljac (1999) looked at anatomic and biomechanical factors that are associated with running injury affecting the hip and lower extremity. An important characteristic in a group of runners that ran for 10 years injury-free was a moderate rate of rear foot pronation - a clear indication that functional kinetic changes at the foot and ankle impact the injury rates on the whole functional kinetic chain.
• Geraci & Brown (2005) insist that the first step in treating muscle imbalance of the hip, regardless of the affected tissue, is to correct biomechanical deficits of the foot and ankle that are commonly the source of altered gait mechanics. In addition, improving the mobility of the scapula and thoracic spine facilitates eccentric stimulation of the abdominals and enhances their role as pelvic stabilizers.
• Lewit (1999) also describes pseudoradicular pain, which appears in most ways to produce the same symptoms as pain emerging from disc compression, or other radicular causes, but which actually results from a joint blockage of, say, L4, L5 or S1. Lewit continues: ‘The pseudoradicular syndrome [involving] L4 is caused by a lesion either in the mobile segment L3/4, or in the hip joint, and for this reason it may be difficult to distinguish a painful hip without clear coxarthrosis from an L3/4 lesion’. Indeed, he points out that both conditions (hip joint and spinal joint dysfunction) may co-exist. And to complicate matters: ‘Since pain radiates toward the knee, and spasm of the adductors (Patrick’s sign) also produces pain in the attachment point – i.e. the pes anserinus on the tibia – pain at the knee is also common’. Additional pseudoradicular pain involving the hip may arise from coccygeal dysfunction: ‘There may be a positive Patrick’s sign and straight leg raising test, spasm of the iliacus or the piriformis, and pain may even simulate hip pain’.
• Lewit cautions that underlying spinal pathology, such as a disc lesion, may make remedial therapy ‘impossible’ because of muscular spasm. Hypertonus, spasm, joint blockage (spinal and sacroiliac)… ’may all be connected with disc lesions, complicating them. Blockage at the segment of a disc lesion being the rule rather than the exception…Obviously, in principle, a disturbance of function is more likely to be remedied by adequate therapy than a structural lesion, such as a disc protrusion. On the other hand, pain originating in the disc or severe blockage may make remedial exercise or static correction impossible because of muscle spasm’. Lewit suggests that in such cases the blockage or spasm should be addressed first, utilizing the gentlest techniques. His formula for this includes ‘muscle energy techniques’… ‘improvement of muscular imbalance and faulty statics [posture] and to treat residual pain (hyperalgesic zones, pain points) by the best methods to suit the case’. In this prescription Lewit very much echoes the approach taken by the authors of this book in their recommended protocols.
Box 12.5 Thoughts on localizing dysfunction
NMT as described in this text offers an opportunity for detailed palpation assessment of tissues when applied systematically and sequentially. Targeting particular structures for specific testing can be achieved in other ways as well. In earlier chapters, and in Volume 1, a formula is described by means of which suspicious dysfunctional areas and joints may be localized for further, more detailed evaluation.
The acronym ARTT (sometimes altered to TART) provides the clue to its constituent parts. A refinement on the basics of this approach of seeking Asymmetry, Range of movement alteration, Tissue texture change and Tenderness includes the following thoughts, as offered by Greenman (1996). He suggests that once suspicion has been raised regarding a particular joint, whether using observation or other screening methods, including ARTT and motion palpation, local dysfunction involving specific tissues may be sought manually. More definitive evaluation of soft tissue can be accomplished with active and passive light and deep touch. Thumbs and fingers can be used as pressure probes searching for areas of tenderness, or more specific evidence of tissue texture change. He calls for ‘multiple variations of motion scanning’ to be introduced by the probing digits as they seek altered range, symmetry and quality of movement. This approach suggests palpating suspect tissues as the individual introduces controlled movement into the area. This approach offers evidence that may be hard to obtain when the patient is totally passive. Additionally, the quality of the feel of specific tissues may be evaluated while movement of distant areas is introduced, perhaps involving an arm or leg movement, while a proximal or distal structure is being palpated at depth; or the response of the tissues under investigation may be evaluated while the patient consciously inhales or exhales.
Practitioners using NMT may recognize that they already do something similar to Greenman’s suggestions or these ideas may stimulate the introduction of controlled patient activity during palpation, adding a further dimension to the palpation process.
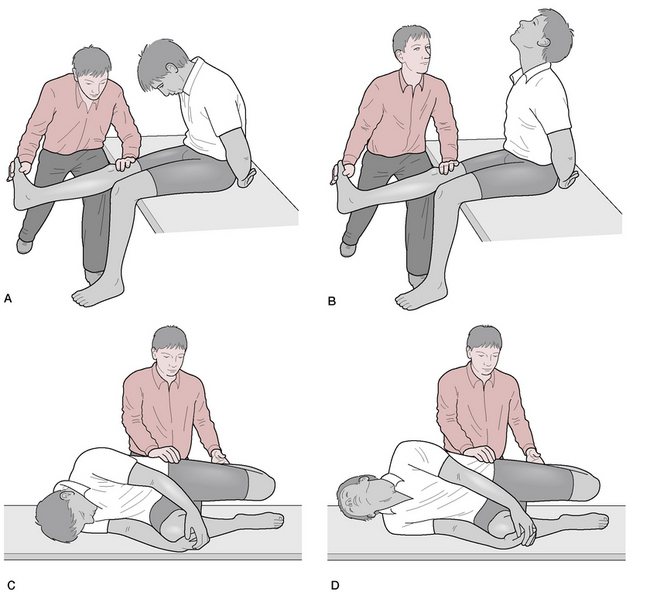
Figure 12.8 A: The slump test with seated straight leg raising, is helpful in picking up radicular pain.
B: If pain is relieved by maneuvers, such as head/neck extension, this differentiates hamstring tightness from adverse neurodynamic tension, i.e. if pain eases in position 12.12B, the pain is neural. C: The side-lying femoral nerve stretch test uses sensitizing and relieving maneuvers that help to differentiate adverse neurodynamic tension in the distribution of the femoral nerve, from quadriceps tightness. D: If pain is relieved by maneuvers such head and neck extension, as illustrated in Fig. 12.12D, the pain is neural.
Risk of hip fracture
Hip fractures are commonly thought of as a complication of osteoporosis with bone mineral density (BMD) being a marker to watch. While BMD is certainly an indicator of fracture risk, Kanis et al (2009) consider a number of other factors that contribute to risk in addition to BMD. These include:
– age, with the risk growing significantly higher with increasing age
– gender, with female surpassing male after the sixth decade with a significant and continuing rise in percentages with age
– body mass index (BMI) with low BMI being a significant risk (which should not be interpreted to mean that BMI is protective)
– personal history of fragility fracture, particularly of the hip, the risk being approximately double when there has been a prior fracture
– family history of hip fractures
– use of glucocorticoids or chemotherapy
– alcohol intake of three or more units per day
– other secondary causes of osteoporosis
– a number of organ related pathologies, include type II diabetes, thyroid disorders, chronic obstructive pulmonary disease, and organ transplant
Kanis et all suggest that awareness of these factors, in association with BMD, can improve accuracy of prediction of fracture risk and be used to develop strategies for prevention.
Ingestion of vitamin D along with calcium supplementation has been shown to reduce risk of hip fracture. Holick (2007) estimates that one billion people worldwide are deficient or insufficient in vitamin D and links deficiency not only with risk of hip fracture and to falling due to a vitamin D-related muscle weakness, but also the development of numerous pathologies, including cancer, schizophrenia, depression, autoimmune disease and other conditions.
Vitamin D supplementation has been shown to decrease the risk of falling in elderly (Kulie et al 2009). Holick (2007) cites several studies of significance, including a compilation of five randomized clinical trials (with a total of 1237 subjects), which showed a 22% reduction in falls with increased vitamin D intake (as compared with only calcium or placebo) and suggested that 800 IU of vitamin D3 per day plus calcium reduced the risk of falls while 400 IU of vitamin D3 per day was ineffective (Bischoff-Ferrari et al 2006). In another study conducted over a 5-month period, nursing home residents showed a 72% reduction in the risk of falls when receiving 800 IU of vitamin D2 per day plus calcium as compared with the placebo group. (Broe et al 2007)
In an analysis published in the British Medical Journal, Järvinen et al (2008) point out that the single biggest factor in fracture risk is not osteoporosis, but, instead, is falling.
Despite this fact, few general practitioners will have assessed the risk of falling among their elderly patients or even know how to do it. Risk of falling is also completely overlooked in many important publications on preventing fractures. We argue that a change of approach is needed. [our italics]
Stating that preventing the fall is a more logical approach, they discuss methods, such as exercise and balance training and supplementation of vitamin D with calcium, alongside identifying and dealing with risk factors (as listed above). ‘In summary, it is time to shift the focus in fracture prevention from osteoporosis to falls. Falling is an under-recognized risk factor for fracture, it is preventable, and prevention provides additional health benefits beyond avoiding fractures.’ The authors of this text agree and point to a number of options within this text (particularly in Chapter 3) and its companion text (regarding cervical issues), as well as Tai Chi and other movement and balance trainings, that can be cautiously applied to those at greatest risk of falling – the elderly population.
Testing for hip dysfunction (including OA)
Evaluation of the hip for biomechanical dysfunction involves application of a variety of test procedures that require precise focus of forces. Tests relating to normal movements as well as accessory movements (outside voluntary control) are required. Out of the complex of information gathered through observation, assessment and palpation, a picture should emerge as to what the pattern of dysfunction entails and possibly of what is actually producing the reported symptoms.
CAUTION: If the patient reports that hip or pelvic pain has appeared for no obvious reason or following only a slight injury, and if the patient:
• has a history of an eating disorder
• has followed an extreme dietary regime (vegan, for example)
• was immobilized, bed-bound, for a period of weeks before onset of hip symptoms
• has recently lost significant amount of weight for no apparent reason
• has a history of cancer or TB
• has a history of thyrotoxicosis or Cushing’s syndrome
• has a history of chronic liver disease or inflammatory bowel disease (malabsorption)
it would be prudent to consider the possibility of bone fracture or pathology and to ask for this to be ruled out (X-ray, scan, etc.) before initiating assessment methods that might exacerbate the situation.
Joint play (accessory movements) in assessment and treatment of hip dysfunction
Joint play involves those aspects of movement at a synovial joint that are outside voluntary muscular control (Kaltenborn 1980).
Petty (2006) explains why joint play (gliding, sliding, translation) movements are so important: ‘Accessory movements are important to examine because they occur during all physiological movements, and, very often, if there is a limitation of the accessory range of movement, this will affect the range of physiological movement available’. (See also Box 12.6). Petty reminds us of Jull’s (1994) summary of the value of joint play evaluation, which can lead to a number of clinical findings, including:
• identification and localization of a dysfunctional joint
• definition of the nature of joint motion abnormality
• assistance in selection of treatment protocols for the joint dysfunction.
Box 12.6 Hints on performing an accessory movement
• Have the patient comfortably positioned.
• Examine the joint movement on the unaffected side first and compare this to the affected side.
• Initially examine the accessory movement without obtaining feedback from the patient about symptom reproduction. This helps to facilitate the process of learning to feel joint movement.
• Have as large an area of skin contact as possible for maximum patient comfort.
• The force is applied using the body weight of the clinician and not the intrinsic muscles of the hand, which can be uncomfortable for both the patient and the clinician.
• Where possible, the clinician’s forearm should lie in the direction of the applied force.
• Apply the force smoothly and slowly through the range, with or without oscillations.
• At the end of the available movement, apply small oscillations to feel the resistance at the end of the range.
• Use just enough force to feel the movement – the harder one presses, the less one feels.
(reproduced with permission from Petty 2006)
Greenman (1996) highlights the importance of the work of the great pioneer of manual medicine John Mennell, who strongly advocated assessment methods (see below) involving joint play (Mennell 1964). Mennell’s definition of joint dysfunction was based on loss of joint play movement that cannot be recovered by voluntary muscular action. As Greenman reminds us: ‘Normal joint-play movement allows for easy, painless performance of voluntary movement. The amount of joint-play is usually less than one-eighth of an inch in any one plane within a synovial joint’
Interestingly, Mennell subscribed to the view that ‘there is only one movement of joint-play at the hip, namely, long axis extension [distraction]’. This is contradicted by Greenman (1996), who describes mobilization methods (see below) that involve different directions of joint play including long-axis distraction, as well as medial and lateral glide.
Kuchera & Goodridge (1997) suggest that the involuntary movement potential at the hip joint (which they term ‘minor movements’) is a little more complex: ‘Anterior glide occurring with external rotation [of the head of the femur] and posterior glide occurring with internal rotation’.
Greenman’s assessment methods involving joint play
Greenman’s mobilization method for the hip involving joint play has been modified (below) for use as an assessment approach, without active mobilization (Fig. 12.9).
• The patient is supine and the practitioner stands at hip level facing the head of the table.
• The patient’s hip and knee are flexed to 90° and the knee is draped over the practitioner’s tableside shoulder and she interlaces her hands to grasp the thigh just inferior to the neck of the femur.
• The practitioner applies caudad traction to remove all soft tissue slack from the joint at which time slight movement cephalad and caudad offers a sense of joint play in those directions.
• The practitioner modifies her position so that she faces the hip and drapes the flexed knee over the back of her neck, enfolding the proximal thigh by interlocking her fingers on the medial thigh (Fig. 12.10). From this position laterally directed traction may be introduced to remove all soft tissue slack at which time a medial and lateral joint-play assessment may be made.

Figure 12.9 Assessment for distraction/compression joint play at the hip
(adapted from Greenman 1996).
Mennell’s hip distraction method (‘long-axis extension’)
Mennell’s long-axis (joint play) distraction assessment for the hip is performed as follows.
• The patient is supine and the practitioner stands at the foot of the table holding the heel and dorsum of the foot in order to exert traction through the long axis of the leg.
• ‘The examiner grasps at arm’s length the subject’s lower leg around the ankle, and positions the leg in its neutral rest position in a few degrees of abduction and external rotation…and then exerts a pull downward in the long axis.’
• If dysfunction exists there will be a noticeable lack of ‘give’ on traction following removal of soft tissue slack. A harsh end-feel will be noted, lacking a sense of joint play.
• This traction clearly involves removal of ‘slack’ at ankle, knee and hip joints but when restriction at the hip is present it is relatively easy to evaluate.
• A series of normal and dysfunctional hip joints should be tested in this way until the feel of dysfunction, and loss of joint play, become clearer. See below for Petty’s (2006) version of this assessment in which she utilizes longitudinal distraction applied from a thigh contact.
• Treatment of joint play restriction is via repetition of the evaluation, which effectively mobilizes the joint to some extent.
• A sharply applied ‘tug’ of the joint can be a useful approach in restoration of joint play, if this lies within the practitioner’s scope of practice (this is effectively a high-velocity mobilization technique) and if the joint is not inflamed.
• Mennell (1964) offers several clinically useful pointers, the first of which is that any additional mobilization attempts focused on the hip should be postponed until joint play has been restored.
• He strongly cautions against any such procedure if pain is produced during the process or if the joint (or any of the lower limb joints) is inflamed.
Lee’s assessment methods involving joint play
Lee describes a variety of supine assessment/treatment methods, using a very similar approach to that described by Greenman (above).
• The patient is supine and the practitioner stands at hip level facing the head of the table.
• The patient’s hip and knee are flexed to 90° and the knee is draped over the practitioner’s tableside shoulder and she interlaces her hands to grasp the thigh just inferior to the neck of the femur.
• Distolateral translation parallel with the neck of the femur or distraction in an inferolateral direction parallel with the long axis of the femur or anteroposterior gliding is introduced, parallel to the plane of the acetabular fossa.
• Lee suggests that these movements be ‘graded according to the irritability of the joint’. Initially gentle grades are indicated, keeping well within the range of pain and reactive muscle spasm. These methods are not introduced during the early inflammatory phase of hip dysfunction following injury but rather are part of the process of normalization during the fibroblastic phases.
• Should capsular adhesions have developed, however, the same maneuvers are indicated but with more force being applied as ‘the joint is taken strongly and specifically to the physiological limit of range’.
Petty’s accessory movement tests (Fig. 12.11)
Various accessory movements are assessed (see below) in which the quality and range of movement, the degree of resistance through and at the end of range, and pain behavior are all evaluated. Petty reminds us that following assessment of joint play (accessory movements), any movements reported by the patient to provoke symptoms and any assessment methods that provoked pain or that reproduced the patient’s symptoms should be reevaluated.
• Anteroposterior glide requires the patient to be side-lying, with a pillow between the legs. The practitioner stands in front of the patient and with her cephalad hand stabilizes the pelvis at the iliac crest, while the heel of the caudad hand introduces anteroposterior pressure at the greater trochanter to evaluate the degree of glide potential (see Fig. 12.11A).
• Posteroanterior glide requires the patient to be side-lying with a pillow between the legs, practitioner standing behind. The practitioner’s cephalad hand stabilizes the pelvis at the ASIS as the caudad hand applies posteroanterior pressure to the posterior aspect of the greater trochanter to evaluate the degree of glide potential (see Fig. 12.11B).
• Longitudinal caudad glide has the patient supine, thigh supported by a cushion, with the practitioner grasping the lateral and medial epicondyles, as the femur is eased caudally to remove slack from the soft tissues surrounding the hip joint, allowing the minute degree of distraction of the femoral head to be assessed (see Fig. 12.11C).
• Lateral transverse joint play at the hip joint requires the supine patient’s hip to be flexed, with a towel wrapped around the upper thigh (for comfort). The practitioner stands facing the lateral aspect of the flexed thigh and clasps her hands together on the medial aspect of the thigh. The knee should rest against one of the practitioner’s anterior shoulders so that medial pressure at that contact allows lateral force applied by the hands to ease the thigh laterally (see Fig. 12.11D).




Figure 12.11 Hip joint accessory movements. A: Anteroposterior. B: Posteroanterior.C: Longitudinal caudad. D: Lateral transverse
(adapted from Petty 2006).
Note: Assessment involving use of joint play is also described in the discussion of occipito-atlantal evaluation presented in Volume 1, Chapter 11 (see Fig. 11.24) and also for general cervical joint restrictions (see Fig. 11.25 A/B). In both of those assessments, translation, which is impossible to introduce actively between individual segments of the spine, is used as a guide to dysfunction.
Hip assessment tests involving movement under voluntary control
Patrick’s test
• The patient is supine and the practitioner stands on the side of the table opposite that being tested.
• The hip is sequentially Flexed, ABducted, Externally Rotated and Extended (F-AB-ER-E).
• This should be a painless procedure with full degree of mobility in the hip being apparent.
• The process also stresses the anterior aspect of the SI joint and is regarded as positive if there is pain reported in the back, buttock or groin.
• Pain noted on any of the elements of the sequence suggest a dysfunctional state of the joint (Fig. 12.12).
Patriquin’s differential assessment method (Patriquin 1972)
If a patient presents with inguinal and anterior thigh pain, with or without pain in the lateral hip, the following differential assessment may be useful.
• The patient is supine, legs in neutral anatomical position with no knee flexion.
• The practitioner stands at the foot of the table holding both heels, one in each of her hands.
• One leg is taken into abduction with the other leg being held in its anatomical position.
• The practitioner observes the degree of abduction of one leg and then the other, at the end of their range of comfortable abduction.
• If the excursion into abduction is less than 45° on the symptomatic side then early osteoarthritic changes may be suspected.
• If abduction is not restricted, Patriquin suggests that a sacral dysfunction may be responsible for the symptoms reported.
Mennell’s hip extension method (Fig. 12.13)
• Mennell notes that extension of the hip is one of the earliest normal movements lost in cases of hip dysfunction.
• Caution: Mennell cautions that joint play should be restored to the hip before the mobilization element of this maneuver is performed.
• Assessment/treatment of hip extension involves the patient lying supine, practitioner standing, facing cephalad at hip level, on the side contralateral to the hip being assessed.
• The non-tested side hip and knee should be fully flexed and if there is limitation of extension potential on the affected side, that thigh will rise from the table surface, as the hip flexes slightly.
• In order to gently mobilize the joint the degree of hip flexion on the unaffected side should be reduced until the thigh once again rests on the table.
• The practitioner applies direct pressure just proximal to the knee, holding the thigh firmly to the table and introduces greater flexion at the hip on the unaffected side, so rotating the pelvis on the immobile head of the affected femur.
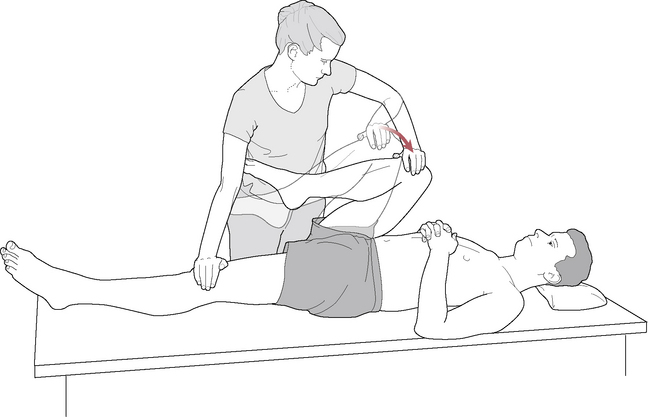
Figure 12.13 Mobilization of the left hip joint into extension. Note that by fixing the left leg to the table and carefully increasing flexion in the right, extension range of motion may be increased on the left
(adapted from Mennell 1964).
Petty’s suggested active and passive assessment guidelines
Petty (2006) emphasizes the importance of testing each active range of hip movement (flexion, extension, abduction, adduction, medial and lateral rotation) several times and also of trying to reproduce normal function by testing combinations of movement, such as flexion with rotation or rotation with flexion. Additionally, movements can be assessed when distraction or compression is passively added to the joint and movements can be performed slowly or quickly.
Passive tests include Patrick’s test (above) and also Maitland’s (1991) quadrant test (Fig. 12.14).
• The patient is supine, hip flexed, with the thigh on the side to be tested ‘sandwiched’ by the practitioner’s forearms, hands folded over the knee and clasped together.
• The leg is adducted at the hip by the practitioner who takes the flexed hip from less than 90° starting position to full flexion, while noting the range and quality of movement and any pain reported.
• In this position, medial rotation and other forces such as long-axis compression can be applied to evaluate the feel and response.

Figure 12.14 Flexion/adduction (or quadrant) test. Practitioner fully supports the thigh with her arms and trunk and with the forearm, which rests along the inner thigh. Longitudinal force can be added with the hands at the knee and medial rotation added
(adapted from Petty 2006).
A surgeon’s view of hip pain, including osteoarthritis
Waddell (1998), an orthopedic surgeon, suggests that problems relating to the hip joint are relatively straightforward to treat, as compared with the low back.
In back pain we often cannot find the cause or even the exact source of the pain…in contrast, with arthritis [of the hip] the problem is clear to both patient and surgeon and both can see it on X-ray. Treatment of arthritis [of the hip] is logical…Treatment for back pain is empiric, and has a high failure rate.
Hip replacement is Waddell’s treatment of choice, where indicated, and some of the issues regarding this form of care are discussed in Box 12.7
A different view
Baldry (2005), a renowned medical acupuncturist, has also evaluated the problems associated with pain relating to arthritis of the hip and arrives at some important conclusions regarding the source of pain in this condition.
• Osteoarthritis of the hip is usually a local phenomenon, unlike generalized arthritic conditions that involve multiple joints.
• OA of the hip (unlike generalized OA) is more common in men and usually has a slow persistent onset (sometimes rapid), with the intensity of symptoms (stiffness, pain) gradually increasing.
• While commonly considered to be the result of bio-mechanical stress (‘wear and tear’), Baldry insists that this concept is ‘no longer tenable’. He suggests that although mechanical features, as well as other factors such as age, gender, obesity and race, are involved as part of the etiology, ‘there are now good reasons for believing that biochemical factors, yet to be identified, must also contribute’.
• Baldry reports that what appears to happen is that a primary degenerative process occurs, involving the joint cartilage, which ‘is ultimately destroyed… and fragments of this floating in the joint space are known to cause an inflammatory reaction in the synovium’.
• Additional encouragement of inflammation may derive from the presence of chemical substances such as pyrophosphates, crystals of which have been found in osteoarthritic joints.
• The pain of OA hip has in the past been considered to result from the damage to the articular cartilaginous surface, resulting in narrowing of the joint space, which encourages damage to underlying bone, involving microfractures, remodeling and osteophyte development.
• Baldry, however, insists that there is evidence (Wyke 1985) that, since there are ‘no receptor nerve endings in the articular cartilage, synovium, or the menisci. Pain … cannot arise directly from the cartilage itself’.
• The apparent mystery as to the source of pain in OA hip conditions seems to deepen as Baldry points out that, although subchondral bone is well supplied with nerves and could generate pain, this seems not to be the case, citing evidence of osteophytes and bony cysts being equally present in patients reporting pain as in those reporting no pain at all.
• Indeed, cases have been recorded of extensive osteo-arthritic joint changes, joint space loss, cysts, sclerosis, osteophytes… all easily seen on X-ray, without pain being a feature (Danielsson 1964).
• Baldry offers the following explanation: ‘The synovium itself …is devoid of nociceptive receptors but when it becomes inflamed, and because of the effect this has on other tissues, pain occurs as a result of stimulation of nerve endings in the synovial blood vessels, the joint capsule, the fat pads, the collateral ligaments, and the adjacent muscles.’
• A combination of the stretching of the wall of the synovial sac, due to inflammation and congestion, and the presence of inflammatory biochemical substances, such as histamine, prostaglandins and polypeptide kinins, then causes the nociceptive receptors to fire.
• Additionally, fibrosis, which results in the capsule and possibly in associated muscles due to such inflammatory processes, leads to contractions and ultimately to irritation of sensory and pain receptors on movement of the joint.
• The adaptive processes then spread to include associated ligaments and tendons (particularly at their attachments) as well as the muscles of the joint and those at a distance, if posture and use patterns change.
• Trigger points evolve in a number of sites associated with these structures, particularly in the articular fat pads, capsule and the periarticular structures.
• This model, explained by Baldry in greater detail than this summary demonstrates, suggests that the pain of an arthritic hip joint therefore arises in the soft tissues of the joint.
• Baldry believes that pain develops in an OA joint primarily due to changes in soft tissues and periarticular structures. ‘This explains why pain in osteoarthritis does not necessarily correlate with the extent of the radiological changes. The one exception to this is osteoarthritis of the hip where generally the pain is proportional to the extent of the joint damage seen on a radiograph (Kellgren 1961).’ We largely agree with this position that radiographs are important to demonstrate the degree of pathology and degeneration, as well as to rule out other more sinister sources of pain.
Note: There is no suggestion intended that hip replacement surgery is undesirable. Indeed, the restoration of function that can be achieved by this procedure is remarkable; however, in management of the pain associated with OA hip conditions, both before and after surgery, the importance of attention to the soft tissues deserves strong emphasis. As Baldry has demonstrated, pain may not be associated with obvious joint damage, but it will almost always be present if soft tissue changes, including trigger point development, have occurred.
Regarding trigger points that can produce hip pain, Travell & Simons (1992) chart several muscles that lie outside the hip region that can produce hip and buttock pain. These include quadratus lumborum, iliocostalis lumborum, longissimus thoracis, semitendinosus, semimembranosus, rectus abdominis and soleus. They note that most of the muscles that lie within the hip and the upper thigh area are associated with pain and dysfunction of this region. In addition to the pain associated with referred patterns of trigger points, thought should also be given to the dysfunctional mechanics that the taut bands affiliated with the trigger points place on the associated joints and also to inhibition or excitation of the muscles located within the target zones of referral.
Muscles of the hip
The muscles of the hip region can usefully be classified by innervation (dorsal or ventral divisions), by location (anterior, posterior, etc.), points of insertion or by function. In the following discussion, grouping them by function has also resulted in a logical order of protocol with the person placed first in supine, then sidelying, then prone position. Many of these muscles have been rightfully addressed in the other technique chapters of this text as well as in several locations in this chapter due to the tremendous overlap of function and influence that abounds in the lower body. When these muscles are discussed in more than one clinical applications chapter, details and influences pertinent to that particular region are highlighted and the discussions found in other chapters are cross-referenced.
In each of the following sections, all muscles that affect the joint in a particular movement will be mentioned but only those that primarily provide that movement will be discussed in detail.
Hip flexion
The muscles that cross the anterior hip in the frontal plane include primarily iliopsoas, rectus femoris, pectineus, tensor fasciae latae, sartorius, gluteus minimus and medius, gracilis and the adductors. These muscles can influence flexion of the hip; however, some of them function in this capacity (or perform more strongly) dependent upon the position of the thigh.
Iliopsoas, rectus femoris (from the quadriceps femoris group) and sartorius are discussed here as the primary flexors of the hip while the others are discussed elsewhere, depending upon the primary function they serve. For instance, although the adductors may play a role in hip flexion, their primary role is adduction and they are therefore discussed in the adductor section.
Iliopsoas (see Figs. 10.62, 12.17)
Attachments: Psoas major: from the lateral borders of vertebral bodies, their intervertebral discs or T12–L5 and the transverse processes of the lumbar vertebrae to merge with the tendon of iliacus and attach to the lesser trochanter of the femur
Innervation: Psoas: lumbar plexus (L1–3)
Muscle type: Postural (type 1), prone to shortening under chronic stress
Function: Iliopsoas flexes the thigh at the hip and assists lateral rotation (especially in the young), assists minimally with abduction of the thigh, assists with sitting up from a supine position. Psoas major also extends the lumbar spine when standing with normal lordosis, (perhaps) flexes the spine when the person is bending forward, and compresses the lumbar vertebral column
Synergists: For hip flexion: rectus femoris, pectineus, adductors brevis, longus and magnus, sartorius, gracilis, tensor fasciae latae
Antagonists: To hip flexion: gluteus maximus, the hamstring group and adductor magnus
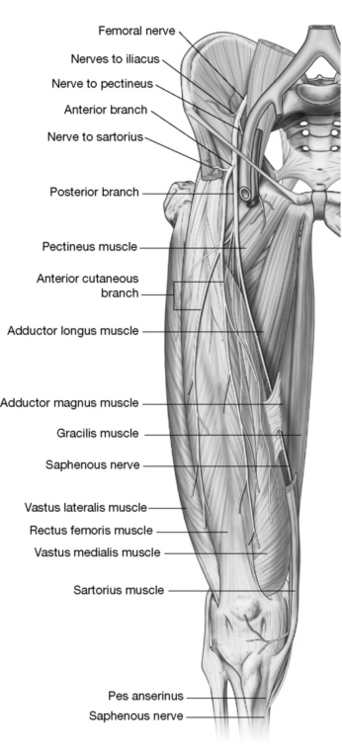
Figure 12.17 The bipennate orientation of the rectus femoris is illustrated as well as the adjacent vasti (medialis and lateralis). Removal of sartorius exposes underlying structures.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Indications for treatment
• Pain in the front of the thigh
• Difficulty rising from seated position
• Inability to perform a sit-up
• Loss of full extension of the hip
• ‘Pseudo-appendicitis’ when appendix is normal
• Difficulty climbing stairs (where hip flexion must be significant)
• Lewit (1999) reports iliacus spasm may result from lesions of the L5-S1 segment producing pseudo-gynecological symptoms
Controversy exists as to the extent of various functions of the psoas but all sources agree that it (along with iliacus) is a powerful flexor of the hip joint. During gait, psoas is only active shortly preceding and during the early swing phase while iliacus is continuously active during walking. Psoas laterally rotates the thigh and is inactive in medial rotation of the thigh, flexes the trunk forward against resistance (as in coming to a sitting position from a recumbent one) and is active in balancing the trunk while sitting (Gray’s anatomy 2005). It is slightly involved in lateral flexion of the torso (Platzer 2004). The iliacus is active during sit-ups, sometimes throughout the entire sit-up; however, it is noted by some authors to be active only after the first 30° (Travell & Simons 1992). Iliacus probably influences anterior tilting of the pelvis directly (Levangie & Norkin 2005) while psoas influences pelvic positioning by increasing lumbar lordosis and therefore the position of the sacrum.
Levangie & Norkin (2005) note the critical importance of iliopsoas in hip flexion from a sitting position (as needed when rising from sitting). They cite Smith et al (1996) who ‘proposed that the hip cannot be flexed beyond 90° when the iliopsoas is paralyzed because the other hip flexor muscles are effectively actively insufficient in that position’.
Travell & Simons (1992) cite Basmajian & Deluca’s (1985) conclusion that: ‘From a functional point of view, the question of whether the iliopsoas rotates the thigh is not worth pursuing…the iliopsoas does not play a significant role in rotation of the normal femur because its tendon is aligned with the axis of rotation in most cases’. While we agree with this conclusion regarding psoas active participation in lateral rotation, we also often find psoas to be tight in the patient presenting with lateral rotation of the femur. Insights as to why this might occur are found in the deeply placed mechanics of the hip, as noted by Cailliet (1996), who describes the following.
In the erect stance, the center of gravity passes behind the center of rotation of the hip joint. The pelvis is angled so that the femoral head is seated directly into the acetabulum. The anterior portion of the capsule is thickened to form the iliofemoral ligament, which permits static stance to exist on a ligamentous support without supporting muscular activity.
Hence when the pelvis and femur are properly positioned, standing should require little muscular support. Cailliet then further notes that toe-out stance directs the head of the femur forward (out of the socket). The iliofemoral ligament is then inappropriately placed to prevent subluxation of the joint and support for the femoral head will be dependent upon the iliopsoas tendon. Therefore, where the patient presents with lateral rotation, the psoas would have the persistent task of stabilizing the hip joint in weight-bearing positions, as well as having its tendon being imposed upon (and potentially irritated by) the femur head.
Travell & Simons (1992) observe that the optimal stretch position of psoas requires that the leg should be in extension and that the thigh should be in neutral (regarding abduction/adduction and rotation) or placed into medial rotation. They note specifically that lateral rotation of the thigh as well as abduction should be avoided when elongating psoas.
A large subtendinous bursa separates the iliopsoas tendon from the pubis and the joint capsule. Inguinal lymph nodes can be palpated in the region of the iliopsoas tendon and, when found to be larger than normal, may indicate disease or injury involving the lower extremity or conditions involving the genital region or lower abdomen or lymphatic system pathologies, such as lymphoma. The pathway of the lymphatic system for the lower extremity is shown in Figure 12.16.
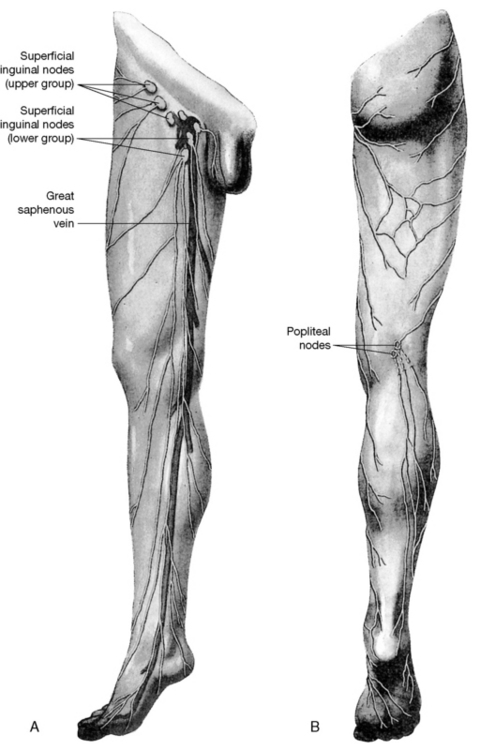
Figure 12.16 A, B:The lymphatic drainage of the superficial tissues of the lower extremity
(reproduced with permission from Gray’s anatomy, 1995).
Methods for the assessment and treatment of psoas are described in Chapter 10 on p. 290 along with a more extensive discussion of its role in influencing the lumbar region. The iliacus muscle is discussed and its treatment described on p. 348 and pp. 412–413 where the pelvis is the focused region. Its tendon may be seen in Fig. 10.62, where the adductor attachments are also illustrated.
Rectus femoris (Fig. 12.17)
Attachments: From the anterior inferior iliac spine (straight head) and the supra-acetabular groove and capsule of hip joint (reflected head) to insert into the patella and continue distal to the patella (as the patellar ligament) to attach to the tibial tuberosity (see Chapter 13)
Innervation: Femoral nerve (L2–4)
Muscle type: Postural (type 1), prone to shortening under stress
Function: Flexion of the thigh at the hip (or pelvis on the thigh depending upon which segment is fixed) and extension of the lower leg at the knee
Synergists: For hip flexion: iliopsoas, pectineus, sartorius, gracilis, tensor fasciae latae and (sometimes) adductors brevis, longus and magnus
Antagonists: To hip flexion: gluteus maximus, the hamstring group and adductor magnus
Special notes
Rectus femoris is the only one of the four heads of the quadriceps femoris muscle group that crosses two joints. The hip flexor function of rectus femoris is considered here while the knee extension tasks are considered on p. 485 with the entire group.
Greenman (1997) observes that when rectus femoris is dysfunctional, it becomes:
facilitated, short and tight [while] the other three components of the quadriceps group… [the vasti]… when dysfunctional, become weak. Shortness and tightness of the rectus femoris is frequently associated with tightness of the psoas muscle and can restrict the anterior capsule of the hip joint…a major problem in the gait results from tightness of the psoas and rectus femoris anteriorly and weakness of the glutei posteriorly.
Travell & Simons (1992) note that when the foot is in a fixed position, the pull of the quadriceps femoris is focused on the proximal end to control the influences of body weight at the pelvis. Though it is not active in quiet standing, the quadriceps femoris is active in backward bending, sitting down from standing position, descending stairs and in squatting. They also point out that its activity increases ‘when heavy loads are carried on the back, when walking speed is increased, and when one wears high heels’. They note the activity of rectus femoris to be more prominent than the remaining vasti portions in high-speed movements.
The rectus femoris can make its most powerful contribution to hip flexion when the knee is flexed. When the hip is flexed and the knee is simultaneously extended, the muscle is considerably shortened and would lose power (Levangie & Norkin 2005).
Trigger points may develop in rectus femoris as a result of prolonged sitting with a weight on the lap (as in holding a child), associated with degenerative hip disease, or during recovery from hip surgery (Travell & Simons 1992). The most common trigger point in rectus femoris is near the pelvic attachment; however, it refers ‘a deep aching pain at night over the thigh above the knee anteriorly’ (Travell & Simons 1992). Since this trigger point target zone lies a significant distance from the location of its associated trigger point, it can easily be overlooked as a source of knee pain. This pattern is illustrated in Chapter 13 (see Fig. 13.35). Additional trigger points in rectus femoris near the knee may be a source of deep knee pain.
The treatment of quadriceps femoris group is discussed in Chapter 13 with the knee, where its position of stretch is also discussed. The following isolated NMT treatment of rectus femoris (following the notes on sartorius) is intended to highlight its involvement in the pelvic region. However, NMT treatment of all the heads of quadriceps femoris is suggested in order to normalize local dysfunction and to locate and deactivate trigger points. Specific MET treatment of rectus femoris is called for if the muscle has shortened.
Assessment for shortness of rectus femoris
• This test reproduces much of the methodology utilized in psoas testing (Chapter 10), but is able to identify rectus femoris shortness specifically.
• The patient lies supine with buttocks (coccyx) as close to the end of the table as possible and with the non-tested leg in full flexion at hip and knee, held there by the patient or by having the sole of the foot of the non-tested side placed against the lateral chest wall of the practitioner. Full flexion of the non-tested side hip helps to maintain the pelvis in full posterior rotation with the lumbar spine flat, which is essential if the test is to be meaningful and stress on the spine is to be avoided.
• If the unsupported thigh of the tested leg fails to lie in a horizontal position in which it is (a) parallel to the floor/table and (b) capable of a movement into hip extension to approximately 10° without more than light pressure from the practitioner’s hand, then the indication is that iliopsoas or rectus femoris is short. The knee is allowed to flex in this portion of the test.
• If rectus femoris is suspected as the cause of reduced range, the tested leg is then held straight by the practitioner and the entire leg again lowered toward the floor for evaluation.
• If the thigh is now able to achieve 10° of hip extension, the responsible tissue is rectus femoris, whose tension on the hip joint was released when the knee (a joint it also crosses) was held in neutral.
MET treatment of rectus femoris (Fig. 12.18)
• The patient lies prone with a cushion under the abdomen to help avoid hyperlordosis.
• The practitioner stands at the side of the table so that she can stabilize the patient’s pelvis (cephalad hand covering sacral area) during the treatment.
• The affected leg is flexed at the knee.
• The practitioner holds the leg at the ankle and introduces flexion of the knee to the first indication of a barrier, perceived either as increasing effort or as palpated ‘bind’.
• If rectus femoris is short then the patient’s heel will not easily be able to touch the buttock.
• Once the restriction barrier has been established, an appropriate degree of resisted isometric effort is introduced (using 15–20% of maximum voluntary contraction potential) as the patient tries to both straighten the leg and to take the thigh toward the table (so activating both ends of rectus).
• Upon the patient’s exhalation, the contraction is followed, by taking the muscle to (if acute) or stretching through (if chronic) the new barrier, by taking the heel toward the buttock with the patient’s help.
• Slight hip extension is increased before the next contraction (using a cushion to support the thigh) as this removes slack from the cephalad end of rectus femoris.
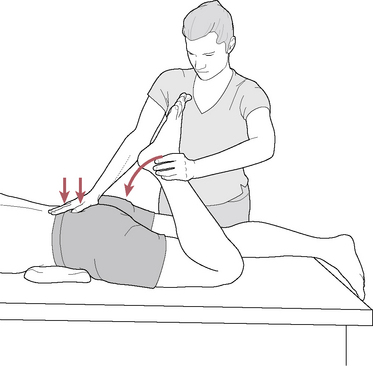
Figure 12.18 MET treatment of left rectus femoris muscle. Note the practitioner’s right hand stabilizes the sacrum and pelvis to prevent undue stress during the stretching phase of the treatment
(adapted from Chaitow 2001).
Sartorius (see Fig. 10.62)
Attachments: Anterior superior iliac spine (ASIS) to the medial proximal anterior tibia just below the condyle (as one of the pes anserinus muscles)
Innervation: Femoral nerve (L2–3)
Muscle type: Phasic (type 2), prone to weakness and lengthening if chronically stressed
Function: Flexes the hip joint and knee during gait; flexes, abducts and laterally rotates the femur
Synergists: For hip flexion during gait: iliacus and tensor fasciae latae
Antagonists: To thigh flexion: gluteus maximus and hamstring group
Special notes
The sartorius, the longest muscle in the body, is one of several muscles that have tendinous inscriptions, a tendinous partition running across a muscle that acts to shorten its length by allowing a long strand to act as two shorter ones. Since central trigger points are known to form at myoneural junctions (Simons et al 1999), this description is important to recall when looking for potential trigger points, which may be relatively scattered. Travell & Simons (1992) note:
The microscopic inscriptions of the sartorius are not aligned and do not form clearly defined bands across the muscle, as do the inscriptions of the rectus abdominis and semitendinosus. Therefore, sartorius myoneural junctions are also exceptional in their distribution throughout the length of the muscle.
The muscle courses from the medial knee to the ASIS, which causes it to directly overlie the femoral neurovascular structures in the middle third of the thigh between the vastus medialis and adductor muscles. The sartorius converts this area into a ‘channel’ (Hunter’s canal), with sartorius being the ‘ceiling’ of this passageway for the femoral vessels and saphenous nerve. This passage ends at the adductor hiatus as the vessels course through the adductor magnus to the posterior thigh.
Sartorius is one of three muscles (with gracilis and semitendinosus) that form the ‘pes anserinus’, a merging of these three tendons at the medial proximal tibia. This region is often tender and is specifically addressed in Chapter 13.
Sartorius has been noted to cause entrapment of the lateral femoral cutaneous nerve, which can affect sensory distribution on the lateral thigh. Travell & Simons (1992) extensively discuss the condition of meralgia paresthetica, symptoms of which are burning pain and paresthesias in the distribution of this nerve. They point to several potential entrapment sites, including the psoas muscles, against the internal pelvis, at the iliac crest (by tight clothing), at the inguinal ligament and by the sartorius muscle, and suggest several courses of action, noting that it usually responds to conservative treatment, including weight loss, avoidance of excessive hip extension or constricting garments around the hips, correction of lower limb length inequality, nerve injection and inactivation of trigger points, particularly in sartorius.
Sartorius assists flexion of both the hip and the knee and is a lateral rotator of the thigh at the hip and a medial rotator of the knee when the knee is in a flexed position. Levangie & Norkin (2005) note that its function is most important when the hip and knee need to be simultaneously flexed, as in stair climbing. Travell & Simons (1992) note that it ‘earned its name as the muscle that assists the hip movements necessary to assume the position of a cross-legged tailor (sartor, a tailor)’. Its trigger point pattern primarily runs along the course of the muscle.
NMT for rectus femoris and sartorius
Lubricated gliding strokes are applied repeatedly to the rectus femoris from the patella toward the AIIS. The thumbs, palm or forearm may be used. As the gliding thumbs examine the superficial bipennate fibers of rectus femoris, fiber direction may be distinguished as coursing diagonally and upward toward the mid-line of the muscle while the vastus lateralis and medialis fibers course in the opposite direction (upward and away from the mid-line of the thigh) (see Fig. 12.17). Increased pressure, if appropriate, will address the deeper fibers of rectus femoris, which course directly to the knee, and vastus intermedius, which lies deep to rectus femoris.
When the thumbs are placed more medially, they will encounter the vastus medialis, which is discussed on p. 486 with the quadriceps femoris.
The course of sartorius runs from the medial knee to the ASIS and separates the quadriceps group from the adductor group. Gliding strokes can be applied with the thumbs along the sartorius with the leg either lying flat on the table (as described with the quadriceps group on p. 486) or with the knee flexed and the leg resting against the practitioner (as described with the adductors on p. 419).
The pelvic attachments of rectus femoris and sartorius can be isolated by placing the thigh in a flexed position. The practitioner stands lateral to the hip region and palpates the ASIS/AIIS area with her cephalad hand. Her caudad hand is placed on the anterior lower thigh and resists flexion of the hip to activate the hip flexors in order to make their tendons more distinct. With activation of the tendons, the practitioner is usually able to feel the diagonally oriented sartorius (medial), the more vertically oriented tensor fasciae latae (lateral) and the rectus femoris, which lies between and slightly lower than the other two (Fig. 12.19).
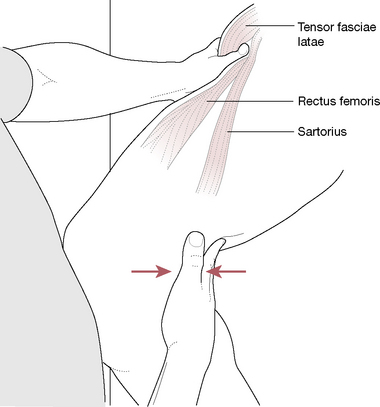
Figure 12.19 Muscles attaching on or near the ASIS can produce anterior pelvic tilt. Sartorius attaches to ASIS, rectus femoris to AIIS and above the brim of the acetabulum, and the tensor fasciae latae to the outer aspect of the ASIS and outer lip of the crest of the ilium. Muscle testing to find tensor fasciae latae is medial rotation resisted by the hand placed on the medial knee region.
Each of these three tendons can be assessed for tenderness, taut fibers and for the presence of trigger points. Short gliding strokes, transverse friction or static compression can be used to release these tissues. The sartorius muscle is further discussed on p. 416, tensor fasciae latae on p. 423 and rectus femoris on p. 414. The distal attachment of the quadriceps femoris is discussed in detail in Chapter 13.