Chapter 11 The pelvis
The pelvis (literally ‘basin’) ‘is massive because its primary function is to withstand compression and other forces due to body weight and powerful musculature…’ (Gray’s anatomy 1995).
Functional adaptations create the structural features of the pelvis, which has locomotion and support as primary purposes in both genders, and that in the female specifically includes parturition. The pelvis of the male and the female are, therefore, distinctly different and provide marked skeletal variations.
A partial list of pelvic differences related to gender includes the following.
• The pelvic cavity is longer and more cone shaped in the male and shorter and more cylindrical in the female.
• The male pelvis has a heavier architecture for attachment of larger muscle groups.
• The male iliac crest is more rugged and more medially inclined anteriorly. The female ilia are more vertically inclined, but do not ascend as far as in the male, making the iliac fossae shallower. This probably accounts for the greater prominence of the hips in females (Gray’s anatomy 2005, p. 1431).
• The female sacral base and sacrum as a whole are broader than in the male.
• The male acetabulum is larger than in the female.
• In females the pubis, which forms the anterior pelvic wall, has a lower height than the male.
Different pelvic types
Gray’s anatomy (2005) suggests that there are four major classifications of pelvic types. Differences are greater at the inferior aperture than at the brim (crest).
• Anthropoid (males only): which is common in males and has a typical deep, fairly narrow, pelvic bowl.
• Android (common in both males and females): which is an intermediate design, somewhere between the anthropoid and gynaecoid.
• Gynaecoid (females only): characterized by a wide and shallow pelvic bowl.
• Platypelloid (rare): which has an even wider and shallower pelvic bowl than the gynaecoid.
Pelvic architecture
The pelvis is composed of two innominate bones (each made up of an ilium, ischium and pubis), with the sacrum wedged between the ilia posteriorly. The ilium, ischium and pubis have cartilaginous connections in the young but fuse to become one bone by adult life. (Fig. 11.1A/B)
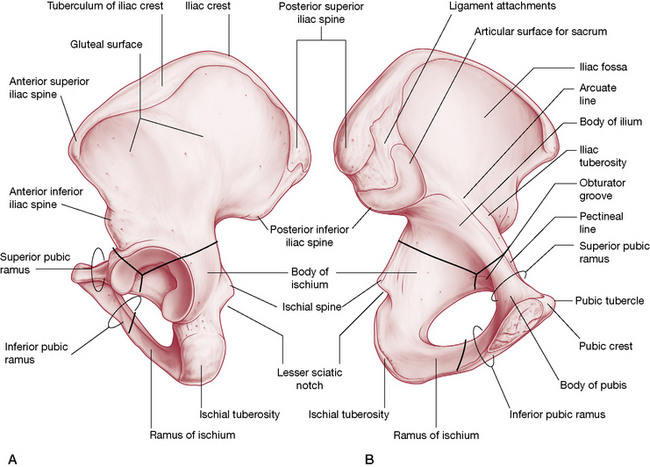
Figure 11.1 A: The medial (internal) view of the left innominate bone. B: The lateral (external) view of the left innominate bone
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Each innominate bone articulates with its pair anteriorly at the symphysis pubis, thereby forming the pelvic girdle. On the lateral surface of each innominate a cup-shaped, deep depression forms the acetabulum for articulation with the femoral head. The acetabulum comprises the junction of the ilium, ischium and the pubic bones and its articulation with the femur constitutes a true ball and socket joint.
The pelvic girdle or ring
• two innominate bones (literal meaning: ‘nameless’), which are formed from the ilia, ischia and pubic bones. These three bones have cartilaginous connections that fuse to become one bone by adult life
• the sacrum, which wedges between the ilia
• the coccyx, which comprises one or two bones and which attaches to the sacrum, is formed from four fused rudimentary vertebrae
• a multitude of ligamentous structures that bind much of the pelvis together
• Lee (2004) includes the two femoral bones as part of the pelvic structure.
The main function of the pelvic girdle is to offer a linkage mechanism between the upper body and the lower limbs for locomotion; however, it also provides support for the abdomen and pelvic organs (Gray’s anatomy 2005, p. 1430). Expandability of the pelvis during gestation and childbirth is augmented by hormonal involvements that allow relaxation of supporting ligaments and therefore gradual and significant structural distortion.
Pregnancy and the pelvis
The ligaments of the pelvis relax during pregnancy, making the joints they serve flexible for expansion and often creating instability in the process. The relaxation of previously stable structures increases the potential for dysfunction and Gray’s anatomy (2005, p. 1439) reports that:
During pregnancy the pelvic joints and ligaments loosen under the influence of the hormone relaxin. Movements in the joints increase. Relaxation renders the sacroiliac locking mechanism less effective, permitting greater rotation and perhaps allowing alterations in pelvic diameters at childbirth, although the effect is probably small. The impaired locking mechanism diverts the strain of weightbearing to the ligaments, with frequent sacroiliac strain after pregnancy.
Note: Form and force closure mechanisms for the SI joint are discussed fully later in this chapter.
Levangie & Norkin (2005) discuss the influences of relaxin, a hormone produced during pregnancy that is thought to activate the collagenolytic system. This system alters the ground substance by increasing its water content and decreasing viscosity and also regulates new collagen formation.
The action of relaxin is to decrease the intrinsic strength and the rigidity of collagen and is thought to be responsible for the softening of the ligaments supporting the [sacroiliac joints] and the symphysis pubis. Consequently, the joints become more mobile and less stable, and the likelihood of injury to these joints is increased. The combination of loosened posterior ligaments and an anterior weight shift caused by a heavy uterus may allow excessive movement of the ilia on the sacrum and result in stretching of the SIJ capsules.
Cyriax (1982) states that relaxin is present for up to 3 months after pregnancy. In the authors’ opinion, this is the ideal time to assess and deal with possible displacement of the pelvic bones that may have occurred as a result of pregnancy and/or labor. If possible, correction of such situations should take place before the depletion of relaxin firms the ligaments with the bones in inappropriate positions.
Lee (2004) reports that:
The morphological changes within the pelvic girdle associated with pregnancy are universal and often occur without symptoms. Occasionally, women present between the 26th and 28th weeks with increasing tenderness over the [sacroiliac joint] and/or pubic symphysis secondary to loss of force closure. … If a woman presents at this time with moderate to severe (7/10 on a visual analog scale) pelvic pain and has asymmetric laxity of the SIJs, then this can be predicative of ongoing pelvic pain into the post-partum period (8 weeks postpartum).
The type of stabilizing belt Lee suggests is worn just above the greater trochanters in order to augment sacroiliac form closure mechanisms ‘until such time as the connective tissue tightens and rehabilitation for force closure mechanisms is instituted’. SI rehabilitation is discussed later in this chapter.
The innominates
As mentioned previously, each innominate is formed from three component bones, the ilium, ischium and pubic bone, and these elements can be described individually (Figs. 11.2 A/B).
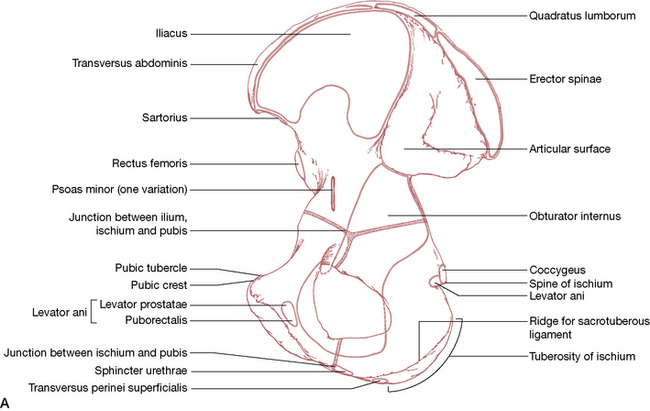
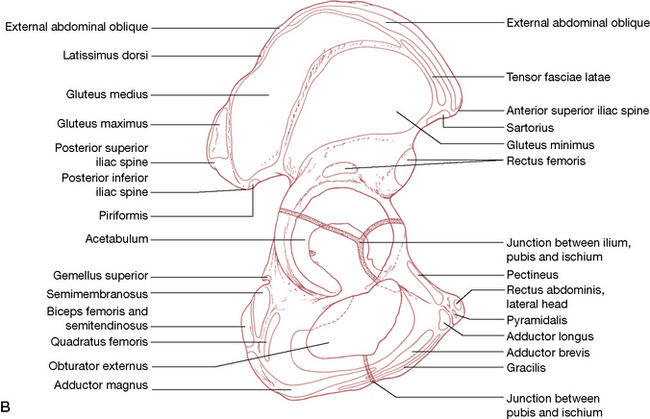
Figure 11.2 Muscle attachments of pelvis A: Medial (internal) view B: Lateral (external) view
(reproduced with permission from Gray’s anatomy 1995).
The ilium (Fig. 11.3)
• A fan-shaped crest is ‘sinuously curved’ (Gray’s anatomy 2005) as it connects the anterior superior iliac spine (ASIS) with the posterior superior iliac spine (PSIS – which is easily palpated beneath the ‘dimpled’ area approximately 4 cm lateral to the second sacral spine) (Fig. 11.4).
• The ASIS is palpable at the lateral end of the inguinal fold.
• The lateral part of the ilium forms the superior aspect of the acetabulum, which hosts the head of the femur.
• Inferior to the PSIS is the posterior inferior iliac spine (PIIS), which lies just posterior to the articular surface of the sacroiliac (SI) joint.
• The articular surface, which forms the ilial portion of the SI joint, is L-shaped and is found on the posterosuperior aspect of the medial surface of each ilium (Fig. 11.5).
• The L-shaped articular surface has a long arm that runs anteroposteriorly and a short arm that runs inferosuperiorly.
• A number of important muscles and ligaments attach to the ilium including quadratus lumborum, erector spinae, iliacus, transversus abdominis, rectus femoris, gluteus minimus, medius and maximus, sartorius, tensor fasciae latae, obliquus abdominis externus and internus, latissimus dorsi and piriformis –see Figs 11.2A/B.
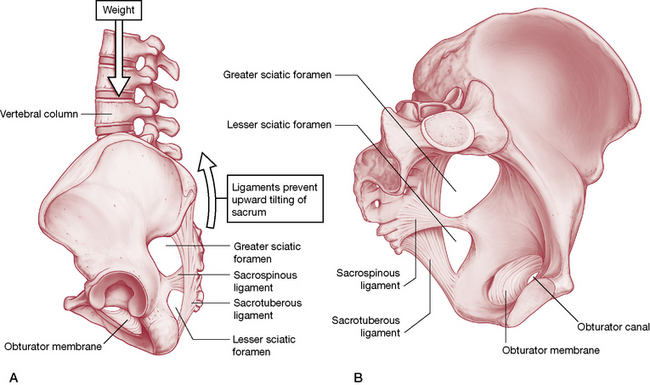
Figure 11.3 Sacrotuberous and sacrospinous ligaments. A: anterior aspect. B: Sacrotuberous ligament helps prevent upward tilting of the sacrum.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
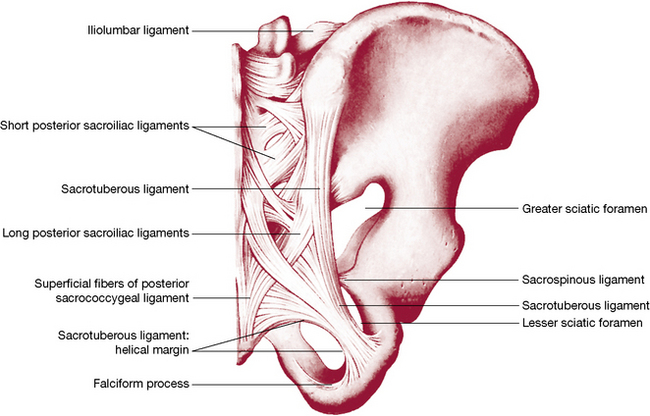
Figure 11.4 Joints and ligaments on the posterior aspect of the right half of the pelvis and 5th lumbar vertebra
(reproduced with permission from Gray’s anatomy 1995).
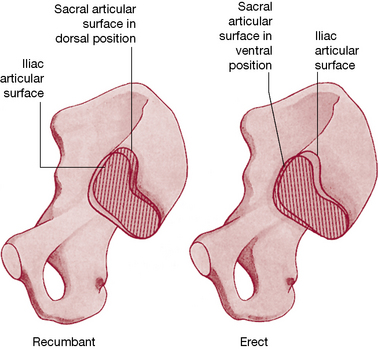
Figure 11.5 The changing relation (rotation) of the auricular surface of the sacrum and that of the ilium when changing from a recumbent to an erect posture
(reproduced with permission from Gray’s anatomy 1995).
The ischium
• Each ischium forms one inferoposterior aspect of its respective innominate.
• Anterior to the border of the ischium is the obturator foramen.
• A tuberosity projecting from the body of the ischium (‘sit bone’) takes the weight of the upper body in sitting.
• The superior part of the body of the ischium forms the floor of the acetabulum as well as a portion of the posterior part of the articular surface of the hip joint.
• A projection (ramus) anteromedially from the lower aspect of the body of the ischium meets the inferior ramus of the pubis.
• There are a number of powerful muscular attachments to the ischium, most notably the hamstrings (biceps femoris, semimembranosus and semitendinosus) as well as quadratus femoris, obturator externus and adductor magnus (see Figs 11.2A/B).
Pubic bones
• The anterior aspect of the pelvis is formed by the junction of the two pubic rami at the symphysis pubis.
• The pubis links to the ilium superiorly by means of the superior pubic ramus, which makes up the anterior portion of the acetabulum.
• The inferior pubic ramus joins the ischium at the obturator foramen’s medial aspect.
• A great many muscular attachments including gracilis, adductors longus and brevis, pectineus and rectus abdominis (lateral head) are connected to the pubis (see 11.2A/B).
The symphysis pubis
• The junction of the two pubic bones is fibrocartilaginous, joined by the superior and the arcuate pubic ligaments.
• An interpubic disc connects the medial surfaces of the pubic bones.
According to Gray’s anatomy (2005): ‘Angulation, rotation and displacement are possible but slight…Some separation is said to occur late in gestation and during childbirth’. Despite Gray’s suggesting that ‘possible but slight’ displacement can occur at the symphysis, osteopathic and chiropractic clinical experience contradicts this apparent minimizing of the potential for pubic dysfunction. Pubic dysfunction patterns, and suggested treatments, are described on p. 334 (Greenman 1996, Ward 1997).
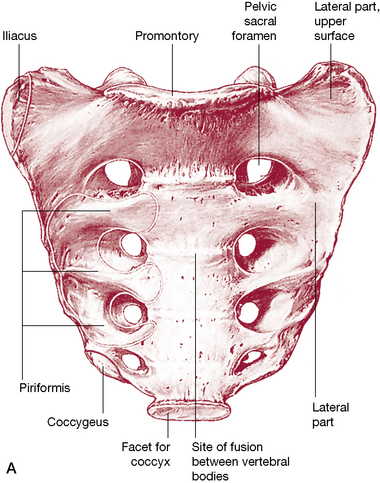
The sacrum (Figs. 11.6 A/B)
• The female sacrum is shorter and wider than the male’s, as a rule (as is the pelvic cavity – see notes on pelvic classifications on p. 301).
• The sacrum, a triangular fusion of five vertebrae, is wedged between the innominate bones to form the posterosuperior wall of the pelvic bowl.
• The caudal end of the sacrum (the apex) articulates with the coccyx while the flat cephalad aspect (the base) articulates with the 5th lumbar vertebrae at the sacrovertebral angle.
• The dorsal surface of the sacrum is convex and the ventral surface concave.
• The sacral base is wide transversely with an anteriorly projecting edge, the sacral promontory.
• The sacral foramen is triangular in shape and caudally is known as the sacral hiatus.
• The superior, concave-shaped, articular processes of the sacrum project cephalad, articulating with the inferior articular processes of the 5th lumbar vertebra.
• Modified transverse processes and costal elements fuse together, and to the rest of the modified vertebral structure, to form the sacral ala or lateral mass.
• The ventral surface of the sacrum is usually vertically and transversely concave.
• The four pairs of sacral foramina have access to the sacral canal via intervertebral foramina, through which the ventral rami of the upper four sacral nerves pass on the ventral surface.
• Lateral to the foramina, costal elements merge and, together with the transverse processes (also known as the costal elements), form the lateral aspect of the sacrum.
• The dorsal surface of the sacrum has a sacral ‘crest’ with either three or four spinal tubercles, formed from fused sacral spines.
• Inferior to the lowest spinal tubercle is the sacral hiatus formed by the failure of the 5th sacral segment’s laminae to meet medially, so exposing the dorsal surface of the 5th sacral vertebral body.
• Fused laminae lie alongside the sacral tubercles and lateral to these are the dorsal sacral foramina (which lead to the sacral canal) through which run the dorsal rami of the sacral spinal nerves.
• Medial to the foramina runs the intermediate sacral crest, composed of fused sacral articular processes, the lowest pair (5th) of which is not fused and projects caudally to form the sacral cornua on each side of the sacral hiatus.
• The sacral cornua links with the coccygeal cornua by means of the intercornual ligaments.
• The lateral surface of the sacrum is formed from fusion of the vertebral transverse processes and costal elements.
• The inferior half of the lateral surface is L-shaped and broad (auricular surface) and articulates with the ilium (see p. 311, sacroiliac joint).
• Posterior to the auricular surface is a rough area where ligamentous attachments occur (see later in this chapter).
• The sacral apex is formed from the inferior aspect of the 5th sacral vertebral body and has an oval facet that articulates with the coccyx.
• The sacral canal, as discussed, forms from fused sacral vertebral foramina, with the upper aspect of its triangular opening pointing cranially when the individual is in a standing position.
• The cauda equina, the filum terminale and the spinal meninges run through the sacral canal.
• The lateral walls of the canal open to the sacral vertebral foramina while inferiorly the canal opens at the sacral hiatus.
• The filum terminale (which attaches to the tip of the coccyx) exits from the sacral hiatus (as do the 5th sacral spinal nerves).
• Attaching to the ventral and dorsal surfaces of the first vertebral sacral body are terminal fibers of anterior and posterior longitudinal ligaments. The lowest pair of ligamentum flava attach to the upper laminar borders.
• The ala or lateral mass is smooth superiorly (covered by psoas major) and laterally rough where the iliolumbar ligament attaches. Iliacus attaches to the anterolateral aspect of this area.
• The sacrum’s pelvic surface provides attachments for piriformis muscles.
• Running anterior to piriformis, having emerged from the pelvic foramina, are the first three sacral ventral rami.
• The sympathetic trunks and the median sacral vessels descend medial to the foramina, directly in contact with bony surfaces.
• Lateral sacral vessels descend lateral to the foramina, also in touch with the bony surface.
• The ventral surface of the upper sacral segments is covered by parietal peritoneum and is crossed by the attachment of the sigmoid mesocolon.
• The rectum is directly in contact with the pelvic surfaces of the 3rd, 4th and 5th sacral vertebrae.
• Erector spinae attach to the dorsal sacral surface, overlying multifidus, which also attaches to the sacrum.
• The upper three sacral spinal dorsal rami penetrate these muscles as they emerge from the dorsal foramina.
• The auricular surface is covered by cartilage and has elevations cranially and caudally. Posterior to the auricular surface are depressions and roughened attachment sites for interosseous sacroiliac ligaments.
• Inferior to the auricular surface are a cluster of attachment sites for gluteus maximus and coccygeus as well as the sacrotuberous and sacrospinous ligaments.
Figure 11.7 Median sagittal section through the sacrum
(reproduced with permission from Gray’s anatomy 1995).
Functions of the sacrum
Bogduk (2005) elegantly demystifies the role of the sacrum.
The sacrum is massive, but not because it bears the load of the vertebral column. After all, the L5 vertebra bears almost as much load as does the sacrum but is considerably smaller. Rather, the sacrum is massive because it must be locked into the pelvis between the two ilia. The bulk of the sacrum lies in the bodies and transverse elements of the upper two segments and the upper part of the third segment. These segments are designed to allow the sacrum to be locked into the pelvic girdle, and to transfer axial forces laterally into the lower limbs (and vice versa).
The sacrum is therefore a glorified wedge, with all the refinement of design required to perform that role, as well as to allow passage through it of neural structures, to offer attachment sites to a variety of ligaments and muscles, and to engage in minute degrees of movement at the articulations between itself and the ilia.
Nutation
The movement of the sacrum between the ilia involves a nodding motion, known as nutation, which creates an anterior motion of the sacral promontory. Counternutation is the return to the neutral start position from a nutated position as well as a posterior motion of the sacral promontory.
Bilateral sacral nutation and counternutation movements occur around a coronal axis within the interosseous ligament. Unilateral sacral nutation takes place when the lower extremity is extended. There is also a constant degree of alternating (muscularly) ‘braced’ nutation in the standing position (Dorman 1997). Some muscular influences on sacroiliac function are discussed later in this chapter.
Figures 11.8 and 11.9 illustrate clearly the way in which the SI joint allows a gliding action of the sacrum to occur inferiorly (caudally) along the short arm and posteriorly along the long arm of the joint during nutation; during counternutation the sacrum glides anteriorly on the long-arm surface and superiorly (cephalad) along the short arm. The total degree of movement that occurs in either nutation or counternutation does not exceed 2 mm, but is palpable (see palpation tests later in this chapter). Snijders et al (1997) report that multifidus and levator ani act as a force couple, to help in control of the sacral nutation/counternutation processes.
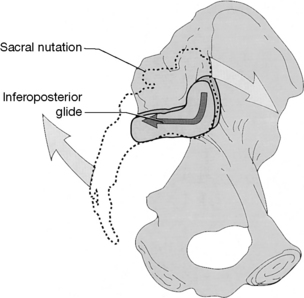
Figure 11.8 When the sacrum nutates, its articular surface glides inferoposteriorly relative to the innominate
(reproduced with permission from Lee 1999).
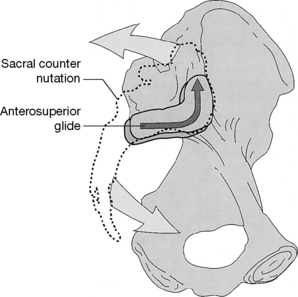
Figure 11.9 When the sacrum counternutates, its articular surface glides anterosuperiorly relative to the innominate
(reproduced with permission from Lee 1999).
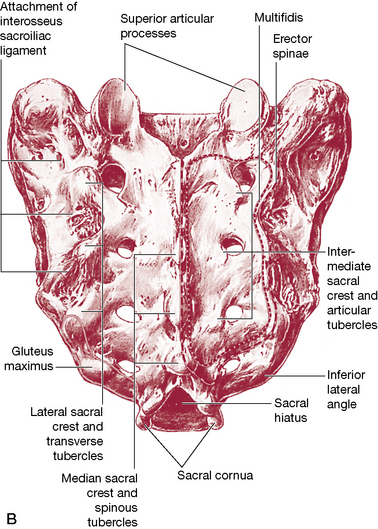
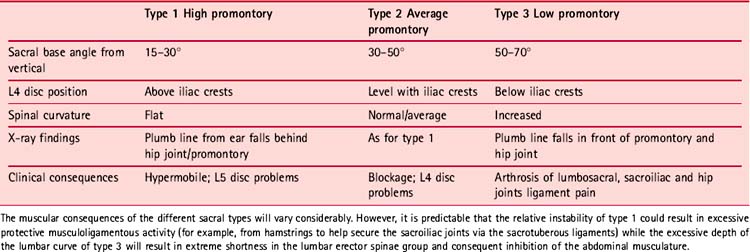
Sacral differences (see Fig. 11.10 and Table 11.1)
Lewit (1985) pays tribute to the early work of Erdmann (1956) and Gutmann (1965) into pelvic biomechanics:
Gutmann and Erdmann distinguish three pelvic [sacral] types with far-reaching differences in function and possible pathology. The first presents a long sacrum and high sacral promontory [i.e the anterior projection of the sacral base, reflecting the angle of the base to the vertical], the second the average or intermediate type, and the third a low promontory and considerable pelvic inclination.
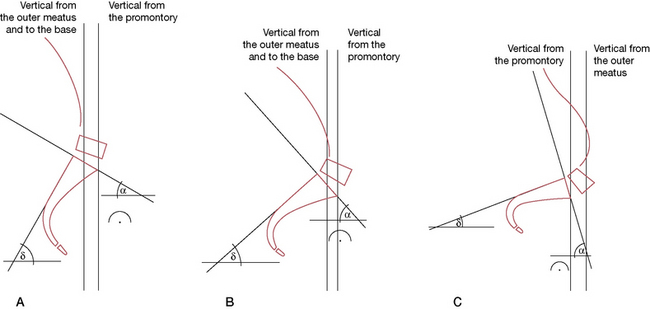
Figure 11.10 Pelvic types showing (A) high promontory, (B) average type, (C) increased pelvic (sacral) inclination
(adapted from Manipulative Therapy in Rehabilitation of the Locomotor System by K Lewit. Reprinted by permission of Elsevier Science Limited).
The greater the angle between the plane of the sacral base and the vertical, the deeper the lumbar curve is likely to be, while the shallower the angle between the plane of the sacral base and the vertical, the flatter the lumbar spine will be. The extreme angle seen with the third pelvic type involves the type of low back and pelvic orientation noted with spondylolisthesis, where L5 virtually slips anteriorly from the sacral base on which it should be supported.
The coccyx
• The coccyx is composed of three, four (most commonly) or five fused, rudimentary vertebrae. The first coccygeal vertebral body forms its upper surface, or base, and articulates via an oval facet with the sacral apex.
• Dorsolaterally to the facet lie two coccygeal cornua, which articulate with the sacral cornua superiorly.
• A thin, fibrocartilagenous disc, somewhat thinner laterally, lies between the surfaces of the coccyx and sacrum.
• Rudimentary transverse processes project superolaterally, which sometimes articulate and sometimes fuse with the inferolateral sacral angle, to complete the 5th sacral foramina.
• The 2nd to 4th coccygeal segments become progressively smaller, described by Gray’s anatomy (2005) as ‘mere fused nodules’.
• The levator ani and coccygeus muscles attach to the pelvic surface laterally.
• The ventral sacrococcygeal ligament attaches ventrally to the 1st and sometimes 2nd coccygeal bodies, as well as to the cornua.
• Between the 5th sacral body and the cornua an intervertebral foramen allows passage of the 5th sacral spinal nerve.
• The dorsal surface of the coccyx has attachments for gluteus maximus, sphincter ani externus (at the very tip) and the deep and superficial dorsal sacrococcygeal ligaments.
• The filum terminale lies between the deep and superficial dorsal sacrococcygeal ligaments, merges with them and to the dorsum of the 1st coccygeal segment. This filament therefore represents a direct attachment of the meninges of the brain, via the spinal dura, to the coccyx. Goodheart (1985) has described a positional release method involving the coccyx and the filum terminale. The objectives include easing spinal and pelvic dysfunctions relating to hypothesized dural restrictions (see Box 11.1).
Box 11.1 Goodheart’s filum terminale (coccygeal) lift technique
Goodheart (1985) has described a method that seems to rely on the crowding, or slackening, of spinal, dural tissues with the coccyx being used as the means of achieving this. Good clinical results in terms of improved function and release of hypertonicity in local areas, as well as those some distance from the point of application, are claimed. Goodheart’s term for this is a ‘filum terminale cephalad lift’.
Goodheart (1985) and Walther (1988) report that there is frequently a dramatic lengthening of the spinal column after application of this coccygeal lift procedure, with Goodheart mentioning specifically that, in good health, there should be no difference greater than about 1 inch in the measured length of the spinal column sitting, standing and lying, using a tapeless measure, which is rolled along the length of the spine.
Goodheart (1984) states:
Tension can be exerted where the foramen magnum is attached to the dura, and also at the 1st, 2nd and 3rd cervicals, which if they are in a state of fixation can limit motion. The dural tube is completely free of any dural attachment all the way down to the 2nd anterior sacral segment where finally the filum terminale attaches to the posterior portion of the 1st coccygeal segment. The release that comes from the coccygeal lift cannot be just a linear longitudinal tension problem. The body is intricately simple and simply intricate and once we understand the closed kinematic chain and the concept of the finite length of the dura, we can see how spinal adjustments can sometimes allow compensations to take place.
Improvements in pelvic, spinal and cervical function have been reported (Goodheart 1985, Walther 1988) following use of the coccygeal lift.
As in all positional release methods, tender areas are used as the means of monitoring the lift of the coccyx designed to produce the effects Goodheart describes. The tender areas employed are located in the neck flexor or extensor muscles.
One of the authors (LC) has found the following version of the coccygeal lift (there are prone position variations) to be effective. Note that the application of this method is contraindicated if there is any inflammatory process in the coccygeal region. The method is unlikely to be successful (and could prove uncomfortable) if there has been a previous fracture of the coccyx, altering its normal contours, to an ‘L’ shape, for example.
Method
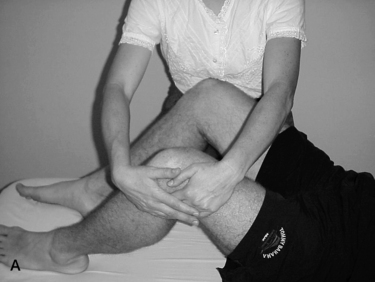
• The patient is sidelying and an area of particular sensitivity to pressure is located in the cervical spinal area.
• The patient uses his own digital pressure to monitor the pain once the practitioner has identified it. A score of ‘10’ is ascribed to the tender point and the objective is for this to reduce by at least 70% during the procedure.
• The practitioner stands at upper thigh level, behind the sidelying patient, facing the side of the table.
• Using the lateral aspect of her cephalad hand (which should be relaxed and not tense throughout the procedure) she achieves contact along the length of the coccyx as she tucks her cephalad elbow against her hip/abdomen area.
• The force required to move the coccyx toward the head is applied by the practitioner leaning into the hand contact, not by any arm or hand effort.
• This application of pressure is not a push on the coccyx but a slowly applied easing of it toward the head and should cause no pain in the coccygeal region if introduced gently but firmly.
• Simultaneously the caudad hand holds the ASIS area in order to stabilize the anterior pelvis and so be able to introduce fine tuning of its position during the ‘lift’, in order to reduce the reported sensitivity score.
• As in positional release methods, the patient reports on the changes in palpated pain levels until a 70% reduction is achieved.
• This position is held for 90 seconds after which reevaluation of dysfunctional structures is performed.
Ligaments of the pelvis
The sacroiliac (SI) joint is supported by ligaments ventrally dorsally and interosseously, as follows.
The ventral (or anterior) SI ligament
This forms from an anteroinferior capsular thickening, which is most developed near the arcuate line and the PIIS, from where it connects the 3rd sacral segment to the lateral surface of the peri-auricular sulcus. Bogduk (2005) suggests that it both helps to bind the ilium to the sacrum and prevents anterior diastasis (slippage, separation) of the joint.
The interosseous SI ligament
This vast connection is the main bonding structure between the sacrum and the ilium, filling much of the space posterosuperior to the joint. Covering it superficially is the dorsal SI ligament (below). Gray’s anatomy (2005, p. 1439) describes this as ‘the major bond between the [sacrum and ilia], filling the irregular space posterior superior to the joint’. It is the largest typical syndesmosis in the body (a syndesmosis is a fibrous articulation in which the bony surfaces are held together by interosseous ligaments). Bogduk (2005) regards this structure as ‘the most important ligament of the sacroiliac joint’, the main function of which is to bind the ilium strongly to the sacrum.
The dorsal (or posterior) SI ligament
This covers the interosseous ligament, with the dorsal rami of the sacral spinal nerves and blood vessels lying between them. There are short and long fibers that link the lateral sacral crests to the PSIS and internal aspect of the iliac crest. The short posterior SI ligament helps to stabilize, as well as to prevent posterior flaring of, the joint. Additionally there are inferior posterior fibers that link the 3rd and 4th sacral segments to the PSIS. The long posterior SI ligament is continuous laterally with the sacrotuberous ligament (see below) and medially with the thoracolumbar fascia. It has an additional role in reducing the degree of backward rocking (counternutation) of the sacrum on the ilium (Bogduk 2005).
The sacrotuberous ligament
The sacrotuberous ligament is really a vertebropelvic ligament although it has, via its connections, profound influence over the SI joint. Both it and the sacrospinous ligament (see below) reduce the opportunity for the sacrum to tilt (nutate), by holding it firmly to the ischium (Bogduk 2005).
The ligament is attached at its cephalad end to the posterior superior iliac spine, blending with the dorsal SI ligaments, the lower sacrum and the coccyx, from where it runs via a thick narrow band, which widens caudally as it attaches to the medial aspect of the ischial tuberosity. From there it spreads toward a merging with the fascial sheath of the internal pudendal nerves and vessels. The posterior surface of the sacrotuberous ligament hosts the attachment of the gluteus maximus, while the superficial lower fibers are joined by the tendon of biceps femoris.
Gray’s (1995, p. 668) notes:
Many fibres of biceps femoris pass into the ligament, an interesting fact, since the sacrum and posterior part of the ilium are primitive mammalian attachments of biceps femoris – the tuberosity being a secondary attachment, the ligament representing, at least in part, remains of primitive tendon.
The ligament is penetrated by the coccygeal branches of the inferior gluteal artery, the perforating cutaneous nerve and filaments of the coccygeal plexus (Gray’s anatomy 2005)
The clinical significance of these attachments warrants emphasis. For example, as Van Wingerden et al (1997) state:
Force from the biceps femoris muscle can lead to increased tension in the sacrotuberous ligament in various ways. Since increased tension in the sacrotuberous ligament diminishes the range of sacroiliac joint motion, the biceps femoris can play a role in stabilization of the SIJ…In this respect, an increase in hamstring tension might well be part of a defensive arthrokinematic reflex mechanism of the body to diminish spinal load.
Such considerations should be kept in mind when SI joint dysfunction or persistent hamstring tightness is noted, as there would be little benefit in interfering with such a protective mechanism by overenthusiastic treatment of a hamstring. Conversely, treatment of the hamstrings should be considered when the lumbar region, SIJ and or sacrotuberous ligament stabilization can be produced but is inefficient.
Also relevant is the knowledge that an active trigger point in biceps femoris may modify its own tone (Simons et al 1999) and thereby influence SI joint stability (i.e. the muscle would have increased tone but may well be weaker than is appropriate, causing imbalances). This highlights the need for a trigger point search in muscles associated with dysfunctional joints. The eventual course of therapeutic action may or may not involve deactivation of a trigger point in such a setting. See the discussion on trigger points and gluteus weakness on p. 365.
The sacrospinous ligament
The sacrospinous ligament is a narrow triangular structure that attaches to the spine of the ischium and the lateral borders of both the sacrum and the coccyx, where it blends with the sacrotuberous ligament.
The sacrospinous ligament has as its anterior component the coccygeus muscle; that is, muscle and ligament are the anterior and posterior aspects of the same structure (Gray’s anatomy 2005).
The sciatic foramina
There are two sciatic foramina, the greater and the lesser on each side. The greater sciatic foramen has as its anterosuperior margin the greater sciatic notch, with the sacrotuberous ligament forming its posterior boundary and the ischial spine and sacrospinous ligament providing its inferior borders. The piriformis muscle passes through it as do the superior gluteal vessels and nerves, which leave the pelvis via this route. Below the piriformis, a number of additional structures exit the pelvis via the greater foramen, including the sciatic nerve (usually), inferior pudendal nerve and vessels, inferior gluteal nerve and vessels, posterior femoral cutaneous nerves and the nerves to obturator internus and quadratus femoris (Heinking et al 1997).
The lesser sciatic foramen has as its boundaries the ischial body anteriorly, the ischial spine and the sacrospinous ligament superiorly and the sacrotuberous ligament posteriorly. The tendon and nerve of obturator internus as well as the pudendal nerve and vessels pass through the foramen.
Note: Piriformis is a postural muscle, which will shorten if stressed (Janda 1983). The effect of shortening is to increase its diameter and, because of its location, this allows for direct pressure to be exerted on the sciatic nerve within the foramen, since they pass through it together. After exiting the foramen, the nerve passes under the piriformis in 85% of people. However, in the other 15% the sciatic nerve (or part of it) passes through the muscle so that contraction, spasm, or contractures could produce direct muscular entrapment of the nerve (Beaton & Anson 1938, Te Poorten 1969, Travell & Simons 1992). A diagnosis of piriformis syndrome might be made for either foraminal or muscular belly entrapment (Fig. 11.11).
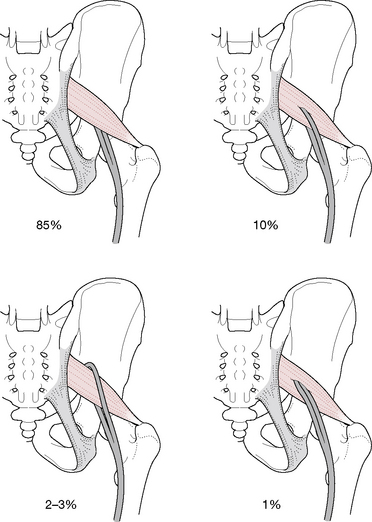
Figure 11.11 Normal and idiosyncratic sciatic nerve positions in relation to the piriformis muscle
(adapted from Ward 1997).
In addition, the pudendal nerve and the blood vessels of the internal iliac artery, as well as common perineal nerves, posterior femoral cutaneous nerve and nerves of the hip rotators, can all be affected in a similar manner (Janda 1996). If the pudendal nerve and blood vessels, which pass through the greater sciatic foramen and reenter the pelvis via the lesser sciatic foramen, are compressed because of piriformis contractures, impaired circulation to the genitalia will occur (in either gender). Since external rotation of the hips is required for coitus by women, pain noted during this act, as well as impotence in men, could relate to impaired circulation induced by piriformis dysfunction within the sciatic foramen.
The next focus of this chapter is the sacroiliac joints – a major source of pain and dysfunction. Before looking at this remarkable structure, we suggest that the subjects of pain in general, and pain as it relates to the pelvis in particular, as discussed in Box 11.2 on p. 317, should be read as the definitions are relevant in the remaining discussions.
Box 11.2 Definitions of pelvic pain
Epidemiology
Female: It is suggested that approximately 15–20% of women, aged 18–50 years, have experienced chronic pelvic pain (CPP) lasting for more than one year (Howard 2003).
Male: A prevalence of 8% chronic prostatitis/chronic pelvic pain syndrome is estimated in the US male population. (Anderson 2008)
Before looking at various pelvic pain definitions, it may be useful to outline a current authoritative view as to what pain is – in the context of the sort of problems that this book is considering.
In 2002 The International Association for the Study of Pain (IASP) proposed the following definition: ‘Pain is an unpleasant sensory and emotional experience associated with either actual or potential tissue damage, or described in terms of such damage.’ (Merskey & Bogduk 2002)
A distinction is made between nociceptive pain associated with tissue damage or inflammation (‘inflammatory pain’), and neuropathic pain that results from changes in the peripheral or central nervous systems. It is also noted that many pains have a mixed neuropathic and nociceptive etiology.
Pelvic girdle pain (PGP)
The pelvic girdle is considered to be the bony ring formed by the hip bones and the sacrum, to which the lower limbs are attached. A definition has been proposed of pelvic girdle pain (and dysfunction), that aims to distinguish this from pelvic pain and dysfunction relating to gynecological or urological disorders. (Vleeming et al 2008)
• ‘Pelvic girdle pain (PGP) generally arises in relation to pregnancy, trauma, arthritis and osteoarthritis.
• Pain is experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the SIJ.
• The pain may radiate in the posterior thigh and can also occur in conjunction with/or separately in the symphysis.
• The endurance capacity for standing, walking, and sitting is diminished.
• The diagnosis of PGP can be reached after exclusion of lumbar causes.
• The pain or functional disturbances in relation to PGP must be reproducible by specific clinical tests.’
In reality, these structural (PGP) and gynecological and/or urological features of pelvic pain frequently overlap, so that the definition above may need to be supplemented by a further definition – that of ‘chronic pelvic pain’ (CPP).
CPP has been defined as follows (Fall et al 2004):
Non-malignant pain, perceived in structures related to the pelvis of either men or women …. [text removed that relates to definition of the word ‘chronic’]. …In all cases, there often are associated negative cognitive, behavioural, sexual and emotional consequences.
It is clear that this broader CPP definition incorporates the features of PGP, without specifying tissues or locations.
The American College of Gynecologists, also in 2004, proposed the following definition of CPP:
Noncyclical pain of at least six months’ duration, involving the pelvis, anterior abdominal wall, lower back, and/or buttocks, serious enough to cause disability or to necessitate medical care. (ACOG 2004)
Therefore, when the term chronic pelvic pain (CPP) is used in this text, unless specifically stated to the contrary, this will refer to pain anywhere in the pelvis, arising from, or being referred to part or all of the region that lies inferior to the lumbar spine (although this will be involved at times) and superior to the gluteal folds (although adductors and hamstrings may contribute to it) – whether involving osseous, neurological, ligamentous, or other soft tissues, including the viscera.
The sacroiliac joint
The surfaces of articulation between the sacrum and the ilium are reciprocally irregular, which restricts movement and provides the joint with considerable strength as it transmits weight from the vertebral column and the trunk to the lower limbs. There is an articular joint capsule that attaches close to both articular margins.
With age, in both genders, fibrous adhesions and other changes gradually obliterate the joint. ‘In old age the joint may be completely fibrosed and occasionally even ossified’ (Gray’s anatomy 2005, p. 1438). Clinically, these changes are important as radiographic research has demonstrated that even before age 50, 6% of joints show evidence of a degenerative process (Cohen et al 1967).
SI joint movement
A very small amount of anteroposterior rotation occurs around a transverse axis when the trunk is flexed or extended, with the degree of movement increasing during pregnancy. According to Gray’s anatomy (1995):
The greatest sacral movement relative to the iliac bones is in rising from a recumbent to a standing position…the sacral promontory advances as much as 5 to 6 mm as body weight impinges on the sacrum…movement is not simple rotation…some translation is associated with it.
Bogduk (2005) explains the essential role of the SI joints.
The joint is placed strategically in the pelvic ring at the site of maximum torsional stress in order to relieve that stress. In teleological terms, a solid ring of bone will not work; it will crack, and the SI joint is there in anticipation of that crack.
Indeed, the evidence is that when the SI joint fuses, as it does in some people due to age or disease (ankylosing spondylitis, for example), the sacrum does literally crack, especially if weakened by osteoporosis (Lourie 1982). Bogduk (2005) reports:
Under these conditions the torsional stresses, normally buffered by the sacroiliac joint, are transferred to the sacrum, which fails by fracture. Conspicuously and strikingly, these fractures run vertically through the ala of the sacrum parallel to the sacroiliac joint.
The current understanding of the SI joint is therefore that it performs stress absorption functions as forces from above or below are transferred into the pelvic mechanism. These forces are partially absorbed into the enormous and powerful ligamentous support which the joint enjoys and partially into the unique mechanical relationship the sacrum has with the ilia, where an osseous locking device allows transfer of forces into the pelvis as a whole. Bogduk (2005) again succinctly summarizes the way in which the functional needs of the SI joint have been accommodated into its design.
For its longitudinal functions, it will exhibit osseous features that lock it into the pelvic ring. For its anti-torsion functions it will exhibit, in a parasagittal plane, a planar surface that can allow gliding movements, but it will be strongly reinforced by ligaments that both retain the locking mechanism and absorb twisting forces.
These functional needs have been superbly incorporated into the SI joint’s design.
Self-locking mechanisms of the SI joint
Two mechanisms lock the joint physiologically and these are known as ‘form closure’ and ‘force closure’ mechanisms.
Form closure is the state of stability that occurs when the very close-fitting joint surfaces of the SI joint approximate, in order to reduce movement opportunities. The efficiency and degree of form closure will vary with the particular characteristics of the structure (size, shape, age) as well as the level of loading involved. Lee (2004) lists three ways that fit (form) of the sacroiliac joint protect it from shear.
1) the sacrum is wedge-shaped vertically and anterioposteriorly, which allows the innominates to stabilize it
2) the articular cartilage is irregular (not smooth), especially on the ilium
3) a frontal dissection of the SIJ reveals bony extensions covered with cartilage that protrude into the joint.
‘All three factors enhance stabilization of the SIJ when compression (force closure) are required to balance the moment of a large external load.’
Force closure refers to the support offered to the SI joint by the ligaments of the area directly, as well as the various sling systems which involve both muscular and ligamentous structures (see discussions within this chapter) (Vleeming et al 2007).
Examples of ‘force closure’ are:
• during anterior rotation of the innominate or during sacral counternutation, the SI joint is stabilized by a tightening of the long dorsal sacroiliac ligament
• during sacral nutation or posterior rotation of the innominate, the SI joint is stabilized by the sacrotuberous and interosseous ligaments.
Motor control and force closure
O’Sullivan & Beales (2007) suggest that the motor control system can become dysfunctional in a variety of ways, leading to maladaptation and pain (see Figure 11.12). Maladaptive changes might then in turn lead to reduced force closure (involving a deficit in motor control) or excessive force closure (involving either a deficit, or an increase in motor activation), resulting in a mechanism for ongoing peripheral pain sensitization and leading to chronic pain that involves the sacroiliac and/or other pelvic structures. Additionally the pelvic floor itself may be involved in such adaptations – with the possibility of chronic pelvic pain (CPP) symptoms emerging (O’Sullivan, 2005).
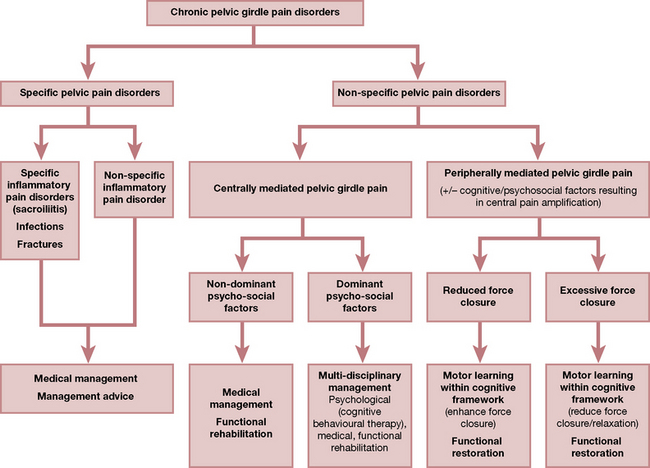
Figure 11.12 The vicious cycle pain from centrally mediated girdle pain.
From O’Sullivan P, Beales D 2007 [pp e4 figure 3] Diagnosis and classification of pelvic girdle pain disorders, Part 2: Illustration of the utility of a classification system via case studies. Manual Therapy 12:e1–e12
Note: See notes toward the end of this chapter on pelvic floor issues.
A summary of muscular involvements in these processes is outlined below.
Innervation of the SI joint
Bogduk (2005) reports that there is little in the way of authoritative evidence to support various contradictory claims as to the precise innervation of the joint. Lee (2004) reports that there is evidence that posteriorly the SI joint is supplied from the posterior rami of the S1 and S2 spinal nerves (Solonen 1957); that the dorsal SI ligaments (and probably the joint) are supplied from lateral divisions of the dorsal rami of L5, S1, S2 and S3 spinal nerves (Bradlay 1985), while the lateral branches of L5, S1 and S2 dorsal rami form a plexus between the interosseous and dorsal sacroiliac ligaments (Grob 1995). There was contradictory research evidence from Solonen and from Grob as to the ventral neural supply to the SI joint, which apparently varied considerably between different individuals. Lee asserts: ‘The wide distribution of innervation is reflected clinically in the variety of pain patterns reported by patients with SI joint dysfunction’.
Muscles and the SI joint
According to Bogduk (2005) there are no muscles that actively move the SI joints; however, a great many muscles attach powerfully on either the sacrum or the ilia and are therefore capable of strongly influencing the functional adequacy of the pelvis as a whole and of SI joints in particular.
Dorman (1997) suggests that: ‘Judging by their attachments, various muscles are probably involved, directly or indirectly, in force closure of the SIJ’. Indirectly muscles can act on ligaments and fascia (see the discussion regarding the influence of the hamstrings on the sacrotuberous ligament on p. 436 and in Chapter 3).
Muscle activity and the SI joint when walking
Dorman (1995) analyzed muscular activity relating to SI function during the gait cycle.
• Erector spinae ‘might be expected to promote nutation’. Dorman (1995) suggests that select subsegments of this group might fire independently when required.
• Gluteus maximus promotes self-locking of the SI joint and controls nutation when the fibers which attach to the sacrotuberous ligament contract. This is clearly a secondary function of gluteus maximus and would only operate in particular postural and nutation positions.
• Gluteus medius has a distinctive role to play in locking the SI joint during the stance phase of the gait cycle. However, Dorman (1997) suggests that it is subject to reflex inhibition when the ilium on the affected side is in an anterior position, at which time tenderness will be noted on deep palpation under the rim of the iliac crest (sidelying).
• Latissimus dorsi joins across the mid-line with the contralateral gluteus maximus via the thoracolumbar fascia and activates during trunk rotation (which occurs during gait). The thoracolumbar fascia can also be tightened by the erector spinae. The effect is to stabilize the SI joint.
• Biceps femoris can change the tension of the sacrotuberous ligament, modulating its tension and influencing the SI joint. This influence varies with body position and the degree of nutation.
Slings, units and systems (Fig. 11.13)
Lee (2004) discusses muscular contributions to the stability of the pelvic structures (as well as the lumbar spine and the hip) and points out that there are two muscular systems involved, a local and a global system.
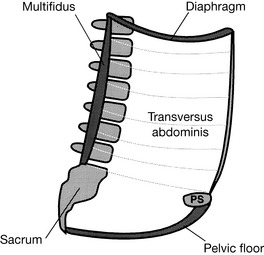
Figure 11.13 The muscles of the inner unit include the multifidus, transversus abdominis, diaphragm and the pelvic floor
(reproduced with permission from Lee 1999).
• the muscles of the pelvic floor (primarily levator ani and coccygeus)
In the past, four slings (then referred to as systems) were described by Lee (1999) as comprising the second muscle system, these being
• Posterior oblique system (latissimus dorsi, gluteus maximus and the lumbodorsal fascia which links them). When latissimus and contralateral gluteus maximus contract there is a force closure of the posterior aspect of the SI joint.
• Deep longitudinal system (erector spinae, deep laminae of the thoracodorsal fascia, sacrotuberous ligament and biceps femoris). When contraction occurs, biceps femoris influences compression of the SI joint and sacral nutation can be controlled (Van Wingerden et al 1993).
• Anterior oblique system (external and internal obliques, the contralateral adductors of the thigh and the intervening abdominal fascia). The obliques take part in most upper and lower limb as well as trunk movements, with transversus abdominis stabilizing. The obliques act almost constantly in unsupported sitting, although cross-legged posture allows them ‘time-out’ (see the discussion of this phenomenon later in this chapter). Snijders et al (1997) suggest that cross-legged sitting offers stabilization for the SI joint, obviating the need for force closure.
• Lateral system (gluteus medius and minimus and contralateral adductors of the thigh).
Lee (2004) has revised these concepts: ‘The global system of muscles is essentially an integrated sling system, comprising several muscles, which produces forces. A muscle may participate in more than one sling and the slings may overlap and interconnect depending on the task being demanded. The hypothesis is that the slings have no beginning or end but rather connect to assist in the transference of forces. It is possible that the slings are all part of one interconnected myofascial system and the particular sling (anterior oblique, posterior oblique, lateral, longitudinal), which is identified during any motion, is merely due to the activation of selective parts of the whole.’
Practitioners might reflect on circumstances that would create imbalances in the force closure mechanisms which so carefully support the SI joint. Anything which inhibits the primary players in this process should be suspect, including:
• excessive tone in antagonists to gluteus maximus, minimus and medius, biceps femoris, lumbar erector spinae, multifidus, adductor and abductors of the thigh as well as the oblique abdominals and transversus abdominis
• inhibition, which may also derive from local or referring trigger points
• other forms of local muscular dysfunction (inflammation, fibrosis, etc.)
Lee (2004) succinctly summarizes that ‘the ability to transfer load through the pelvis effectively is dynamic and depends on:
1. optimal function of the bones, joints and ligaments (form closure or joint congruency) …
2. optimal function of the muscles and fascia (force closure) …
3. appropriate neural function (motor control, emotional state) …’
As these structures weaken or modify, spread of dysfunction to other body parts will also be seen, from the feet to the cranium.
Leg crossing – a muscular benefit?
Dorman (1997) asks: ‘Do any muscles maintain a state of continuous contraction to maintain the state of force closure – bracing – of the SI articulations?’ The answer is somewhat surprising. It was found on EMG testing that during normal standing and sitting there was no firing of either biceps femoris or gluteus maximus but there was an almost constant firing of the internal oblique abdominal muscles (Dorman 1997). Firing of the internal obliques almost ceased, however, when the legs were crossed! It is thought that, because trunk rotation takes place when cross-legged, the fascial tube of the body is placed under some slight tension, thereby maintaining compression on the pelvis and allowing the oblique abdominals to relax. As Dorman points out: ‘When [muscles] do not relax fatigue, spasm and trigger points develop.’
The mechanism of crossing the legs when seated therefore apparently produces temporary release of these overworked muscles (Snijders et al 1995). However, as Dorman elaborates:
[During cross legged sitting] the ischium is subject to increased weight bearing, and the tension measured in the latissimus dorsi of the one side and the gluteus maximus of the other is increased. This balance can be maintained for some time, but creep in the soft tissues is apt to give enough slack after an interval, which will reflexly ‘wake up’ the ‘guardian’ internal oblique muscles. It is now that the sitting subject instinctively reverses, changes over to crossing the other leg, an experience we have all noticed subjectively.
Gait and the pelvis
In Chapter 3 the gait cycle is discussed in all its complexity. In this section the effects of walking (on the pelvis in general and the SI joint in particular) are summarized (Lee 2004, Schafer 1987, Vleeming et al 2007).
Understanding the role that muscles, tendons and fascia play in the act of walking requires awareness of the concept of energy storage by these structures. See Chapter 3 for notes on energy storage.
• During the swing phase of gait, as the right leg moves forward, the superior aspect of the ilium rotates posteriorly while the sacral base inclines anteriorly. (Fig. 11.14).
• As this happens, sacral nutation and ligamentous tension increase on the right and the SI joint is compressed as the joint prepares for heel strike and weight bearing.
• Just before heel strike, activation occurs in the ipsilateral hamstrings, thereby stabilizing the extended knee and tightening the sacrotuberous ligament to further stabilize the SI joint.
• Vleeming et al (2007) have demonstrated that as the foot approaches heel strike there is a downward movement of the fibula, increasing (via biceps femoris) the tension on the sacrotuberous ligament, while simultaneously the tibialis anterior (which attaches to the first metatarsal bone) fires, in order to dorsiflex the foot in preparation for heel strike.
• Tibialis anterior links to peroneus longus under the foot, thus completing the sling mechanism.
• Biceps femoris, tibialis anterior and peroneus longus together form this longitudinal muscle-tendon-fascial sling, which is loaded to create an energy store (loaded elastic element), to be used during the next part of the gait cycle.
• During the brief single support phase of the gait cycle, biceps femoris activity reduces as compression of the SI joint reduces and the ipsilateral innominate bone rotates anteriorly.
• At this stage, as the right heel strikes and the left arm swings forward, gluteus maximus activates to compress and stabilize the SI joint, as well as to provide coupling (via the thoracolumbar fascia) with the contralateral latissimus dorsi, which assists in counterrotation of the trunk on the pelvis.
• This effectively creates an oblique muscle-fascia-tendon sling across the torso, which creates a further energy store for use in the next phase of the cycle.
• Some of the gluteal tension is also transferred into the lower limb via the iliotibial tract.
• Vleeming et al (2007) describe what happens next: ‘In addition, the iliotibial tract can be tensed by expansion of the huge vastus lateralis muscle during its contraction… [and] is active during the single support phase to counteract flexion in the knee.’ They point out that the iliotibial band merges with the outer lateral capsule of the knee, with the fibers running perpendicular to the patella tendon, which attaches to the tibia.
• Protection of the knee from forward shear forces is therefore available during the single support phase by the integrated and combined actions of the thoracolumbar fascia, gluteus maximus and the iliotibial tract.
• As the single support phase ends and the double support phase initiates, there is a lessened loading of the SI joints and gluteus maximus reduces its activity.
• As the next step starts, the leg swings forward and nutation at the SI joint starts again.
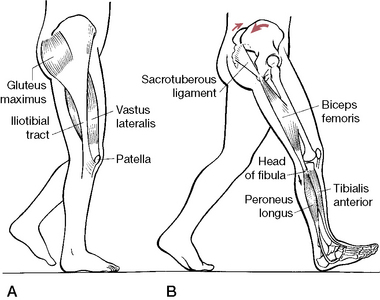
Figure 11.14 A: Lower part of the oblique dorsal muscle-fascia-tendon sling. Relationship between the gluteus maximus, iliotibial tract, vastus lateralis muscle and knee in a single support phase. The iliotibial tract can be tensed by action of the dorsally located gluteus maximus and ventrolaterally located tensor fascia latae muscle. The tract can also be tensed by contraction of the vastus lateralis. B: The longitudinal muscle-tendon-fascia sling. Relationships at the end of the swing phase
(reproduced with permission from Vleeming et al 1997).
Therapeutic considerations
In general terms, when imbalances, distortions and/or functional changes have occurred in the low back and/or pelvis (or elsewhere), restoration of normal function requires that a logical sequence of therapeutic and rehabilitation strategies are employed.
Potential soft tissue and joint restrictions, shortening of myofascial tissue and dysfunctions (e.g. trigger points) need to be assessed and treated appropriately in order to restore an optimal degree of voluntary control.
Appropriate treatment requires lengthening of what is short, strengthening of what is weak, mobilization of what is restricted (‘blocked’), deactivation of trigger points, reintegration of functional patterns of use, etc. In order for this to be achieved, sound evaluation and assessment methods are required. And within this evaluation there is a need to maintain awareness that some apparently dysfunctional states are, in fact, protective and are part of the way the body is best handling its adaptive responses. A more complete evaluation of the underlying causes may therefore be required before the tissues that are actually serving to stabilize and protect can be safely released. Esential Information Section of this Volume for discussion of the role of trigger points as possible protectors of normal function.
Following appropriate therapeutic interventions, when (even partial) voluntary control of an area has been achieved, reflex (automatic) control needs to be encouraged and regained. This protocol involves retraining and rehabilitation strategies that help the individual to alter habitual patterns of use, which may have contributed to the original dysfunctional situation.
The suggested therapeutic sequence therefore involves assessment → local treatment → general treatment → rehabilitation, with an overlap occurring between all these stages. Rehabilitation/self-help strategies should commence early, with general and local therapeutic strategies often taking place during the same session, while assessment is continuous throughout the process.
Homeostatic subtext
The key subtext of the discussion in Box 11.2 is that the body and the local structures/tissues are self-regulating, self-healing and have a propensity for recovery if causative factors are eliminated or eased. Causative factors fall into one of two categories: they are either factors that are loading the adaptive mechanisms of the body (through overuse, misuse, abuse or underuse, for example) or they represent a failure of the adaptive functions. Treatment, of whatever sort, therefore needs to aim at reducing the adaptive load while assisting in enhancing function to better handle the load.
Appropriate treatment therefore encourages self-healing, which is why so many different methods can achieve similar ends. It is the self-regulating (homeostatic) mechanisms that normalize and heal, not the applied treatment. Treatment can only be a catalyst toward that end. A deeper discussion of these concepts is found in Volume 1, Chapter 4.
Pelvic problems and the low back
Almost all problems of the lumbar spine will create stresses involving the pelvis and all pelvic dysfunctions and imbalances place adaptation demands on the lumbar spine, making it essential to consider the lumbar-pelvic mechanisms as a continuum (Schafer 1987).
A common feature of low back and pelvic dysfunction involves an unbalanced pattern known as the ‘lower crossed syndrome’, first described in detail by Janda (1982, 1983). This dysfunctional pattern is the result of a chain of events in which particular muscles shorten and others are inhibited in response to stresses imposed on them.
As Greenman (1996) explains: ‘Muscle imbalance consists of shortening and tightening of muscle groups (usually the tonic [‘postural’] muscles), weakness of certain muscle groups (usually the phasic muscles), and loss of control on integrated muscle function.’ The term ‘pseudoparesis’ is used by Janda (1983) to describe the reciprocal inhibition-related weakness of phasic muscles, as compared with true weakness.
Lower crossed syndrome (Fig. 11.15)
The lower crossed syndrome involves the following basic imbalance pattern: iliopsoas, rectus femoris, TFL, the short adductors of the thigh and the erector spinae group all tighten and shorten, while the abdominal and gluteal muscles all weaken (i.e. are inhibited). The result of this chain reaction is to tilt the pelvis forward on the frontal plane, while flexing the hip joints and exaggerating lumbar lordosis. L5-S1 will have increased likelihood of soft tissue and joint distress, accompanied by pain and irritation. An additional stress feature commonly appears in the sagittal plane in which quadratus lumborum shortens and tightens, while gluteus maximus and medius weaken.
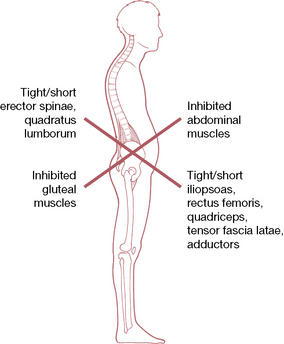
Figure 11.15 Lower crossed syndrome (after Janda)
(reproduced with permission from Chaitow & DeLany 2008).
When this ‘lateral corset’ becomes unstable the pelvis is held in increased elevation, which is accentuated when walking (‘hip hike’) as quadratus fires inappropriately. This instability results in L5-S1 stress in the sagittal plane, which leads to lower back pain. These combined stresses produce instability at the lumbodorsal junction, an unstable transition point at best. The relative weakness/inhibition of gluteus maximus has implications for SI joint stability during the gait cycle, as explained earlier in this chapter.
The piriformis muscles are also commonly involved. Since in approximately 20% of individuals, the right piriformis is penetrated by either the peroneal portion of the sciatic nerve or, rarely, by the whole nerve (the incidence of this is apparently greatly increased in individuals of Asian descent), non-disc related sciatic symptoms may result but are rarely noted beyond the knee when entrapment of the nerve is due to piriformis (Heinking et al 1997, Kuchera & Goodridge 1997).
Treatment sequencing
An almost inevitable consequence of a lower crossed syndrome pattern is that stresses will translate superiorly, thereby triggering or aggravating an upper crossed syndrome pattern (described fully in Volume 1, Chapter 5). We readily see in these examples how the upper and lower body interact with each other, not only functionally but dysfunctionally as well.
The solution for patterns such as the lower crossed syndrome is to identify both the shortened and the weakened structures and to set about normalizing their dysfunctional status. This might involve:
• deactivating trigger points within the dysfunctional (short/weak, etc.) muscles or trigger points that might be influencing them, such as those located in synergists or antagonists
• normalizing the short and/or weak muscles, with the objective of restoring balance. This may involve purely soft tissue approaches or be combined with osseous manipulation and rehabilitation exercises
• reeducating posture and body usage, if results are to be other than short term.
Recognizing inappropriate firing sequences
An additional consequence of muscle dysfunction is a tendency for firing sequences to become unbalanced, so that synergists adopt the role of prime mover in important movement patterns. For example, what happens if the main culprits in disturbed motor patterns are weak muscles, inhibited by overactive antagonists? The threshold of irritation in the weakened muscle is raised and therefore, as a rule, the muscle contracts later than normal or, in some cases, not at all. This alters the order in which muscles contract and leads to poor coordination between prime movers, synergists and antagonists. The most characteristic feature is substitution, which alters the entire pattern. This change is particularly evident if the weak muscle is the agonist in a particular movement sequence (see tests below). For example, when testing for movements such as prone hip extension, if the gluteus maximus has weakened, the hamstrings (which should be assisting gluteus maximus, not dominating it) will be excessively active, as will the ipsilateral erector spinae (which should be bracing the low back and not acting as hip extensors through their action of extending the lumbar spine). If, on the other hand, the neutralizers and/or the fixators are weak, the basic pattern persists but there is accessory motion; if the antagonists are weak, the range of motion is increased (Vasilyeva & Lewit 1996).
Clinical example
Vasilyeva & Lewit (1996) have described an example of the repercussions of a weakened (inhibited) gluteus maximus, in which the hamstrings and erector spinae are overactive. (Fig. 11.16).
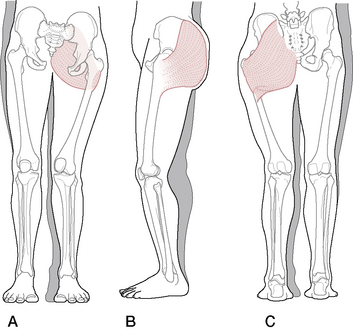
Figure 11.16 Changes in body outline because of weakness of the gluteus maximus. Front view (A), side view (B), back view (C)
(adapted with permission from Liebenson 1996).
Consider the attachments of gluteus maximus, which attach (on the pelvic end) to the ilium behind the posterior gluteal line, lower posterior part of sacrum, lateral aspect of coccyx, sacrotuberous ligament, lumbodorsal aponeurosis and fascia of gluteus medius and (on the femoral end) to the iliotibial band of fascia latae and the gluteal ridge of the femur.
If the muscle is inhibited (weakened reciprocally by overactive antagonists including biceps femoris and the erector spinae group, or by the presence in it, or in functionally related muscles, of active trigger points) (Simons et al 1999), there will be a series of changes including:
• anteversion and external rotation of the innominate
• anteversion and ipsilateral flexion and rotation of the sacrum
• hyperlordosis of the lumbar spine with a tendency to scoliosis toward the ipsilateral side
• contralateral deviation of the lower part of the sacrum and coccyx
• flexion, adduction and internal rotation of the thigh in the acetabulum
• an increase in the transverse diameter of the pelvis and the hip
• the greater trochanter would be displaced superiorly and protruding
• the upper margin of the ilium would be tilted anteriorly with the ASIS low
• the PSIS would be closer to the sacrum than normal
• there would be a valgosity at the knee with the patella medially translated
The patterns of pain and dysfunction that would emerge would be predictable, involving back, pelvic, hip, knee and foot pain, with a transference of stress superiorly as well, throwing the upper body into a compensating pattern of adaptive stress.
Possible trigger point involvement
In what way may trigger points be playing a part in such patterns of dysfunction? Trigger points are activated when the myofascial tissue is overloaded (strained, overused), shortened (especially repetitively, prolonged or abruptly), traumatized, chilled or as a result of low oxygenation of the tissues, systemic biochemical imbalance (e.g. hormonal, nutritional) or febrile illness (fever) (Simons et al 1999).
According to Simons et al (1999), an active trigger point will inhibit the function of a muscle in which it is housed as well as those that lie in its target zone of referral. Therefore, the trigger points may be in the weak muscle or in a muscle that refers into it, or both.
Although weakness is generally characteristic of a muscle with active myofascial trigger points, the magnitude is variable from muscle to muscle, and from subject to subject. EMG studies indicate that, in muscles with active trigger points, the muscle starts out fatigued, it fatigues more rapidly, and it becomes exhausted sooner than normal muscles.
As noted, weakness may also be a reflection of inhibition referred from a trigger point in another muscle. A clinical decision might be made to treat active trigger points as a primary goal of the therapeutic strategy. Alternatively, other dysfunctional features (such as structural imbalances, biochemical (e.g. nutritional) imbalances or breathing dysfunction) might attract primary attention and the trigger point(s) could be monitored to evaluate changes in activity. If a release and balancing of local joint restriction, muscular shortness, weakness and/or coordination features is under way, the aberrant behavior of local trigger points may calm down. On the other hand, trigger point deactivation may be a requirement for that very rebalancing process to proceed. Additional discussion is found in Volume 1, Chapter 4.
Further observation may also alert the practitioner to the presence of a crossed syndrome (see Fig. 11.15), in which the pelvis is tilted anteriorly, the abdomen protrudes and there is increased thoracic kyphosis, with the head thrust forward, with rounded shoulders, etc. How the individual stands and moves offers important observational clues as to underlying patterns of dysfunction, thereby guiding the practitioner toward which structures deserve closer attention, testing and evaluation.
Screening
How is the practitioner to know which muscles, among the many involved in pelvic function and dysfunction, display relative shortness, weakness and/or inappropriate firing sequences? (See Box 11.3)
Box 11.3 Questions regarding therapeutic intervention
In this book, when the reader is confronted by a series of descriptions of therapeutic modalities and procedures it will be all too easy to wonder which should be chosen in relation to treating a particular condition. For example, in the description of sacroiliac dysfunction and pain, a variety of strategies are offered for normalizing the restricted joint. The following queries serve to guide decisions regarding protocols, while still maintaining diverse choices based upon what is found in examination.
Q. Should manipulation/mobilization techniques of the joint be used?
A. Possibly; however, in the experience of the authors, soft tissue imbalances that might be causing or maintaining the problem are usually best dealt with first. Manipulation of the joint may require referral to an appropriately licensed practitioner and usually best follows the creation of a suitable soft tissue environment in which shortness/weakness imbalances have been lessened. The information in this chapter has shown just how complex muscular and ligamentous influences on the SI joint can be. For instance, as described above, during walking there is a ‘bracing’ of the ligamentous support of the SI joint to help stabilize it, involving all or any of the following muscles: latissimus dorsi, gluteus maximus, iliotibial band, peroneus longus, tibialis anterior and more (Dorman 1997). Since any of these muscles could conceivably be involved in maintaining compression/locking of the joint, they should be considered and evaluated (and if necessary, treated) when dysfunction of the joint occurs, prior to manipulation of the joint.
Q. Should muscles attaching to the pelvis be evaluated for shortness/weakness and treated accordingly?
A. Almost certainly, as any obvious shortness or weakness in muscles attaching to the pelvis is likely to be maintaining dysfunctional patterns of use, even if it was not part of the original cause of the SI joint problem. Any muscle that has a working relationship (e.g. antagonist, synergist) with muscles stabilizing the SI joint could therefore be helping to create an imbalance and should be assessed for shortness and/or weakness. However, it should always be kept in mind that what is observed is an adaptive compensation and the underlying causes should be sought and corrected as a primary concern.
Q. Should MET or PRT or MFR or NMT or mobilization or HVT or other tactics be used?
A. Yes, to most of the above! The choice of procedure, however, should depend on the training of the individual, the degree of acuteness/chronicity of the tissues being treated and the tissue’s response when the modality is applied. The more acute the situation, the less direct and invasive the choice of procedure should be, calling for positional release methods initially, for example. HVT should be reserved for joints that are non-responsive to soft tissue approaches and in any case should follow a degree of normalization of the soft tissues of the region, rather than preceding soft tissue work. Occasionally, however, the soft tissues that are not responding may do so beautifully after the joints have been mobilized. All the procedures listed will ‘work’ – if they are appropriate to the needs of the dysfunctional region and if they encourage a restoration of functional integrity.
Q. Should trigger points be located and deactivated and, if so, in which stage of the therapeutic sequence and which treatment approach should be chosen?
A. Trigger points may be major players in the maintenance of dysfunctional soft tissue status. Trigger points in the key muscles associated with the SI joint, or antagonists/synergists of these, could create imbalances that would result in SI joint pain. Trigger points may therefore (and usually do) need to be located and treated early in a therapeutic sequence aimed at restoring normal SI joint function, using methods with which the practitioner is familiar (and licensed to perform), whether this be procaine injections, acupuncture, ultrasound, spray-and-stretch techniques or any suitable manual approach ranging from ischemic compression to positional release and stretching or indeed a combination of these methods. What matters is that the choice of method is logical, non-harmful and effective and that the practitioner has been well trained to use it.
Additionally, there may be times (as discussed elsewhere within this text) when trigger points may be serving a protective or stabilizing role to a more complex compensatory pattern. Their treatment may then be best left until after correction of the adaptational mechanisms that have caused their formation. Indeed, with correction of the primary compensating pattern (forward head position, for instance), the trigger points (in this case, masticatory muscles) may spontaneously deactivate without intervention when the forward head position and possibly resulting SCM trigger points are corrected (Simons et al 1999).
Q. When should postural reeducation and improved use patterns (e.g. sitting posture, work habits, recreational stresses, etc.) be addressed?
A. The process of reeducation and rehabilitation should start early on, through discussion and provision of information, with homework starting just as soon as the condition allows (e.g. it would be damaging to suggest stretching too early after trauma while consolidation of tissue repair was incomplete or to suggest postures that, in the early stages of recovery, caused pain). The more accurately the individual (patient) understands the reasons why homework procedures are being requested, the more likely is a satisfactory degree of compliance.
Q. Should factors other than manual therapies be considered?
A. Absolutely! The need to always keep in mind the multifactorial influences on dysfunction can never be overemphasized. Biochemical and psychosocial factors need to be considered alongside the biomechanical ones. For discussions on this vital topic, see the Essential Information chapter for details of the concepts involved.
Testing and a rapid screening procedure are needed, involving functional tests (below) as well as assessment of length and strength, which can usually identify the precise dysfunctional features of a condition. A number of these tests associated with particular regions and joints are detailed in this text and its companion. Several functional assessments directly relating to the pelvic imbalance, as described above, are of clinical importance and are included in the following section.
Janda’s functional tests
Janda (1996) has developed a series of functional assessments that can be used to show changes which suggest imbalance, by providing evidence of over- or under-activity. Some of these directly related to the lumbar and pelvic area are outlined below. Janda’s concepts and methods are currently widely used within a range of manual therapy professions (Frank et al 2009). Greenman (1996) elaborates on the means whereby these assessments have been validated.
Muscle dysfunction is not only characterized by facilitation and inhibition but also in the manner in which muscles sequentially fire. Altered muscle firing patterns show delay in activation and in the amplitude of electromyographic activity in the dynamic-phasic muscles. Continued exercise in the presence of abnormal muscle firing sequences perpetuates hypertonicity, tightness and shortening of the tonic muscles with continued and progressive inhibition of the phasic muscles.
The evolution of myofascial trigger points, in both the bellies and attachments of muscles stressed in this way, is inevitable (Simons et al 1999).
Altered movement patterns can be tested as part of a screening examination for locomotor dysfunction. In general, observation alone is all that is needed to determine the altered movement pattern. However, light palpation may also be used if observation is difficult due to poor lighting, a visual problem or if the person is not sufficiently disrobed.
Although some of these tests relate directly to the lower back and limb, their relevance to the upper regions of the body should be clear, based on the interconnectedness of body mechanics.
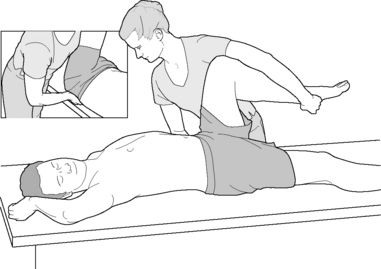
Prone hip extension test (see Volume 1, Fig. 5.5)
• The person lies prone and the practitioner stands to the side at waist level with the cephalad hand spanning the lower lumbar musculature and assessing erector spinae activity.
• The caudal hand is placed so that the heel lies on the gluteal muscle mass with the finger tips on the hamstrings.
• The person is asked to raise his leg into extension as the practitioner assesses the firing sequence.
• The normal activation sequence is (1) gluteus maximus, (2) hamstrings, followed by (3) erector spinae contralateral, then (4) ipsilateral. (Note: not all clinicians agree with this sequence definition; some believe hamstrings fire first or that there should be a simultaneous contraction of hamstrings and gluteus maximus.)
• If the hamstrings and/or erectors take on the role of gluteus maximus as the prime mover, they will become shortened and further inhibit gluteus maximus.
• Janda (1996) says: ‘The poorest pattern occurs when the erector spinae on the ipsilateral side, or even the shoulder girdle muscles, initiate the movement and activation of gluteus maximus is weak and substantially delayed … the leg lift is achieved by pelvic forward tilt and hyperlordosis of the lumbar spine, which undoubtedly stresses this region.’
Variation
• When the hip extension movement is performed the lower limb should be observed to be ‘hinging’ at the hip joint.
• If, instead, the hinge seems to take place in the lumbar spine, the indication is that the lumbar spinal extensors have adopted much of the role of gluteus maximus and that these extensors (and probably hamstrings) will have shortened.
Hip abduction test (Fig. 11.17) (Frank et al 2009)
• The person lies on the side, ideally with his head on a cushion, with the upper leg straight and the lower leg flexed at hip and knee, for balance.
• The practitioner, who is observing not palpating, stands in front of the person and toward the head end of the table.
• The person is asked to slowly raise the leg into abduction.
• Normal is represented by pure hip abduction to 45°. Abnormal is represented by:
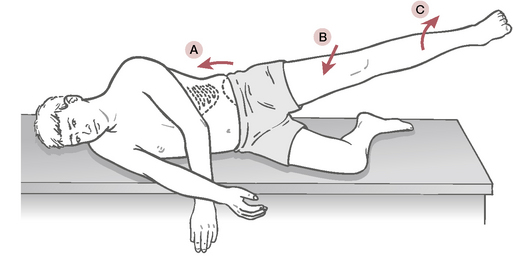
Figure 11.17 Hip abduction test which, if normal, occurs without (a) ‘hip hike’, (b) hip flexion or (c) external rotation
(reproduced with permission from Chaitow & DeLany 2008).
Variation 1
• Before the test is performed the practitioner (standing behind the sidelying patient) lightly places the finger tips of the cephalad hand onto the lateral margin of quadratus lumborum while also placing the caudal hand so that the heel is on gluteus medius and the finger tips on TFL.
• If quadratus lumborum is overactive (and, by implication, shortened), it will fire before gluteus and possibly before TFL.
• The indication would be that quadratus (and possibly TFL) had shortened and that gluteus medius is inhibited.
Variation 2
• When observing the abduction of the hip, there should be a sense of ‘hinging’ occurring at the hip and not at waist level.
• If there is a definite sense of the hinge being in the low back/waist area, the implication is the same as in variation 1 – that quadratus is overactive and shortened, while gluteus medius is inhibited and weak.
Tests for weakness
Simons et al (1999) suggest that weakness needs to be evaluated both statically and dynamically. In static testing, a single muscle is being evaluated as the patient attempts a voluntary contraction and this process is under cortical control. In dynamic testing, which involves muscular effort relative to a normal functional movement and where a degree of coordinated muscular effort is required, there is a greater degree of ‘vulnerability to reflex inhibition’ (Simons et al 1999), for example, involving trigger points. Dynamic activity is under less direct cortical control and often involves coordinated patterns of integrated neural and muscular function that are semi-automatic, largely under cerebellar control. Key differences in these testing methods are as follows.
A muscle that is being statically loaded may suddenly quit because of pain in an associated stabilizer or in the muscle itself. This may relate to a variety of dysfunctional possibilities ranging from inflammation to trigger point activity. The cessation of effort during a static test may occur just prior to the point at which pain would be noted and may be a learned response. Simons et al (1999) suggest that the location and degree of pain associated with this kind of test can ‘help to locate the inhibiting trigger points’. The deactivation of such points is capable of rapidly normalizing strength in such muscles once the inhibiting factor ceases.
In the case of reflexly induced weakness, a degree of reeducation and rehabilitation is usually required to encourage more normal coordinated patterns of use, once causative factors – such as myofascial trigger point activity or joint restriction – have been eliminated. There are clearly different perspectives as to priorities in treating such dysfunction, with one body of thought maintaining that normalization of joint restriction is a priority (a largely chiropractic perspective). For example, Liebenson (2007) suggests that joint mobilization should precede muscle relaxation methods, while others believe that normalization of any muscular/ligamentous features deserves priority (Kuchera 1997). It seems possible that both points of view are correct in different circumstances. The practitioner is best guided by keen observation of the response of the patient’s body when a particular order is applied and should change that order (or the modality choice) when a satisfactory outcome is not fairly consistently achieved.
Strength and stamina testing for gluteus maximus and medius
Lee (1997), Liebenson (2007) and Norris (2000) describe strength (or, more accurately, endurance) tests for gluteus medius and maximus.
Gluteus medius
Method 1
• The patient is sidelying, leg to be tested is uppermost with knee extended.
• The hip is placed and supported in slight extension, abduction and external rotation and the patient is asked to maintain the position of the trunk and leg when support for the leg is released.
• When the support is released and if gluteus medius is weak, there may be posterior pelvic rotation or the spine may be pulled into sideflexion as quadratus lumborum attempts to brace the leg.
• If the patient can maintain the original position for 10 seconds, pressure is then applied to the leg in the direction of hip flexion, adduction and internal rotation, thereby resisting gluteus medius posterior fibers.
• If the posterior fibers of gluteus medius are weak, the patient will be unable to hold the position against pressure.
• If weakness is established, the implications for SI joint instability during the gait cycle are clear. Reasons for the relative weakness should be assessed, which could possibly involve excess tone in antagonists or trigger points in gluteus medius or associated muscles.
• Special attention should be given to searching for trigger points in those muscles that refer into the gluteus medius region, such as quadratus lumborum, gluteus maximus and minimus, iliocostalis lumborum, piriformis, and rectus abdominis.
Method 2 (Norris 2000)
• The patient is sidelying with lower leg straight and upper leg (to be tested) flexed at hip and knee, so that the medial aspect of the foot rests on the table surface just distal to and posterior to the contralateral knee.
• The hip is passively externally rotated so that the foot now rests with the sole on the floor, at which time the patient is asked to maintain that position, involving gluteus medius in a stabilizing task in its inner range.
• Optimal endurance is indicated by an ability to maintain this position for 10–20 seconds.
• If endurance is poor a holding time of less than 10 seconds will be evident and if the limb drops away from the inner range position immediately, a lengthened and very weak gluteus medius is probable.
Method 3
• The Trendelenburg sign evaluates gluteus medius strength.
• The patient stands with weight on both feet, the sacral dimples (which should be level) are observed and their relative height to each other noted so that their behavior during the subsequent test can be accurately monitored. This example will test the right side.
• As the patient lifts the left leg to stand on the right one, the right gluteus medius should contract, thereby abducting the pelvis on the supported side, which results in elevation of the pelvis on the left side (i.e. the left sacral dimple should remain level or move superiorly). If this happens the test is negative (i.e. the muscle is behaving normally).
• If the muscle is inadequate to the task of stabilizing the pelvis (i.e. the left sacral dimple drops), the test is positive and gluteus medius (and minimus) is assumed to be weak or not functioning. A false-negative may occur when the contralateral (left in this case) quadratus lumborum or obliques substitute for weak gluteals.
• The reasons for this dysfunction should be investigated and might include pathologies that bring the attachments close to each other (fractures of the greater trochanter, slipped capital femoral epiphysis), congenital dislocation, poliomyelitis or nerve root lesions (Hoppenfeld 1976).
Method 4 (Liebenson 2007)
• This variation on the previous test evaluates the stamina of gluteus medius rather than its initial strength.
• The standing patient is instructed to shift from two-leg to one-leg support while standing on the leg being tested.
• The pelvis should remain relatively level and not shift more than 1 inch (2.5 cm) toward the weight-bearing side within the first 20 seconds of single-leg standing.
• The position is held for 20 seconds and the following indications of gluteus medius weakness should be evaluated: gluteus medius is weak if greater than 1 inch (2.5 cm) side shift occurs before 20 seconds or if pelvic unleveling occurs before 20 seconds.
Gluteus maximus
Method 1
The patient is prone and is requested to contract the buttocks, squeezing them together, as they are palpated. A strong bilateral contraction should be noted.
Method 2 (Lee 1999)
• The patient is then asked to extend one hip (no greater than 10°) while the ipsilateral knee is flexed to 90°.
• The practitioner offers some counterpressure to the extended thigh to assess its stability.
• If the patient introduces extension of the lumbar spine to assist the stabilization effort, there is an implication of relative gluteus maximus weakness.
• Reasons for the relative weakness should be established, possibly involving excess tone in antagonists, trigger points in associated muscles or nerve root lesions.
Method 3 (Norris 2000)
• To assess stamina of gluteus maximus, the prone patient’s leg, flexed at the knee, is taken into extension to between 5° and 10° and the patient is asked to hold this.
• Optimal endurance is indicated when this full inner range stabilizing task can be maintained for 10–20 seconds.
• If endurance is poor a holding time of less than 10 seconds will be evident and if the limb drops away from the inner range position immediately, a lengthened and very weak gluteus maximus is probable.
Strength testing for piriformis
Travell & Simons (1992) describe the Pace abduction test, which can be used to test for strength of the piriformis. It appears here with minor modifications.
• The patient is seated and the practitioner stands in front of the patient.
• The practitioner’s hands are placed (one on each of) the lateral aspects of the knees and offer resistance as the patient is asked to push the hands apart.
• Weakness, pain and faltering may be observed on the weaker side.
Pelvic tilts and inclinations
There is a great deal of disagreement regarding the best means of assessing the mechanics of pelvic inclinations, as well as what to do clinically about such deviations from the symmetrical norm. There are also a variety of opinions as to the value or otherwise of observation and palpation of the lumbar region, the pelvis in general and the sacrum in particular, since the region of the low back involves so many structural idiosyncrasies.
As Kuchera (1997) explains:
The lumbosacroiliac region is, unfortunately, the site of the greatest number of congenital spinal anomalies, including facet asymmetry. This complicates the interpretation of palpatory findings. For this reason appropriate diagnosis of …low back dysfunction should not be based solely on static anatomic landmarks; asymmetric landmark interpretation should always be coupled with motion testing in the region. (our italics)
The low back and pelvic region has been described as ‘a self-compensating force couple that accommodates, mitigates, balances, stores and redirects forces affecting the pelvis and its principal ligaments’ (Don Tigny 1995). Imbalances can relate to musculoligamentous factors as these structures attempt to stabilize and cope with stresses imposed by gravity as well as the postural, weight-bearing and movement activities of the upper and lower body. Compensations that create a variety of observable asymmetries may emerge from failures of the SI joint’s self-bracing systems and/or be due to congenital imbalances (small hemipelvis, short leg, etc.) or derive from trauma.
The pelvis can be observed in many individuals to be tilted anteriorly or posteriorly or to have a lateral inclination. It is important to note that a great many people, with no symptoms at all, have just such apparently dysfunctional pelvic inclinations. A patient may present with symptoms of pain, or other dysfunction, involving the low back and/or pelvis and may also have a pelvic tilt or lateral inclination; however, this does not mean that the two factors are connected. In other words, there may be no causal link between the symptoms and the tilt or inclination. The descriptions given earlier in this chapter as to the imbalances resulting from biceps femoris shortness, combined with weakness of gluteus maximus, and of the lower crossed syndrome pattern offer a clear indication as to how such patterns evolve. Schafer (1987) states:
Forward tilt of the ilium is essentially the product of weak abdominals, hamstrings, or both, [as well as] hypertonicity of the lumboextensors or hip flexors and contractures of the rectus femoris. This distortion is by far the most common postural fault of muscular origin.
Testing and treating pelvic, sacral, iliac and sacroiliac dysfunctions
Heinking et al (1997) have outlined a logical osteopathic perspective of the tortuous processes required to make sense of pelvic, sacral and sacroiliac biomechanics and dysfunctional states. They assert that three questions require answering at the outset:
The answers to these questions should evolve through a process of assessment as described below. At this juncture it is worth reflecting on the relative inaccuracy, in research studies, of individual assessment tests. See Box 11.4 for a discussion of this. Protocols deriving from the work of various osteopathic, chiropractic, physical therapy and manual medicine clinical experts, including Greenman (1996), Heinking et al (1997), Schafer (1987), Lee (2004), Petty (2006), Lewit (1999) and others, have been modified and added to in the examination and assessment descriptions given below.
Box 11.4 How reliable and accurate are pelvic (and other) assessment methods?
When considering the reliability of the results of assessment protocols, interexaminer (interrater) reliability is an important issue. Reproducible examination is of the utmost importance and the results of interexaminer studies, especially regarding pelvic assessments, are not encouraging.
In particular, researchers such as Bogduk (2005) and Buyruk et al (1997) have criticized the reliability, validity and specificity of biomechanical tests involving the sacroiliac joint. Buyruk et al, for example, state:
Assessment of the stiffness of pelvic joints remains a problem in clinical practice. In clinics, pain provocation tests of SIJ stiffness are done in several ways, such as using Patrick’s F-A-B-ER-E, Gaenslen and pelvic rock tests (Hoppenfeld 1976). However, these methods are unreliable and subjective. The outcome depends entirely on the experience and skills of the observer.
Buyruk et al (1997) suggest that high-tech methods such as color Doppler imaging and Doppler imaging of vibrations offer more accurate, objective means of evaluating SI joint stiffness. Bogduk (2005) goes further and sweepingly dismisses most palpation and manual assessment procedures. ‘Those conditions that have attracted the greatest popularity in clinical practice – muscle pain, ligament pain, trigger points – are associated with the smallest amount of scientific evidence…[and]…no reliable means of diagnosis have been established.’ He continues by suggesting that less popular diagnoses, such as zygapophysial joint pain, sacroiliac joint pain and internal disc disruption, have been more fully researched as sources of pain, but that these all require:
Sophisticated techniques and specialised radiological facilities for their diagnosis. In contrast, the hitherto popular diagnoses [muscular, trigger point pain sources, etc.] are ones that are easy to make, and do not require sophisticated techniques or facilities: they are ‘office’ diagnoses and their treatment are ‘office’ procedures. Yet it is these diagnoses and treatments that are least supported by scientific evidence.
The evidence
The question of reliability of manual tests, palpation and assessments for SI joint dysfunction has been tested many times. The results remain equivocal; in other words, the jury is still out. Although in some studies 100% accuracy was achieved, in others the results were as low as 60% and in some instances no better than chance.
• Slipman et al (1998) investigated the predictive value of SI joint ‘provocation’ tests, as compared with what they describe as the medical ‘gold standard’ approach, of a joint block injection. Fifty patients were selected to be tested by joint block if they tested positive using at least three manual methods. The manual provocation tests always included Patrick’s F-AB-ER-E test, as well as direct palpation for pain in the ipsilateral sacral sulcus, plus one other from the wide range of choices available, such as pain provocation by means of the transverse anterior distraction compression test or transverse posterior distraction test or Gaenslen’s test. The working hypothesis was that if the joint block injections (performed using fluoroscopically guided needling) effectively eliminated SI pain, the manual assessment had been accurate. The results showed that 30 of the 50 patients were relieved of symptoms by 80% or more by means of joint block, whereas 20 achieved less than 80% relief. A 60% degree of accuracy in identifying SI joint syndrome was therefore noted using manual testing, in this study.
• Hestboek & Leboeufe-Yde (2000) have performed a systematic review of peer-reviewed chiropractic and manual medicine literature relating to the accuracy of tests performed for the lumbopelvic spine. In regard to the SI joint in particular, they noted:
The results of reliability testing for motion palpation of SI joints ranged from slight concordance to good agreement. … The two studies of intraexaminer reliability scored greater than the 80% limit (86% and 100%)…. Three studies of interexaminer reliability were included…with two scoring more than 80%.
In their conclusions they state:
Only studies focusing on palpation for pain had consistently acceptable reliability values. Studies testing for motion palpation for the lumbar spine and sacroiliac joints, for leg-length inequality, and most of the sacro-occipital technique tests had mixed findings, whereas visual inspection…had consistently unacceptable agreement.
• It is worth considering that the basic palpation skills of many practitioners may be inadequate to the task of manual assessment. O’Haire & Gibbons (2000) conducted a pilot study to evaluate interexaminer and intraexaminer accuracy for assessing sacroiliac anatomical landmarks using palpation and observation. Since much manual assessment and subsequent treatment choices depend greatly on accurate identification of landmarks, the ability to locate the PSIS (posterior superior iliac spine), SS (sacral sulcus) and the SILA (sacral inferior lateral angle) would seem to be basic to subsequent evaluation. Intraexaminer results yielded a range of less-than-chance to moderate for SILA palpation, with only slight to moderate agreement for PSIS and SS. Interexaminer agreement was slight. The authors of the study conclude:
Information derived from palpation should be consistent within a practitioner and interpreted in a form that is transmissible to other practitioners…further studies are required to determine why agreement on both static and motion palpatory findings remains poor.
It may justifiably be questioned whether such studies negate the value of clinical assessment. The examples given, and Bogduk’s viewpoint described earlier, should certainly be taken seriously. Assessment is not a process that can be skimped or performed other than diligently, if the treatment procedures based on the findings are to be of value to the patient.
Lee (2004) agrees with Bogduk (1997) that ideally a ‘biomechanical diagnosis requires biomechanical criteria’ and that ‘Pain on movement is not that criteria’. However, the fact that there is relatively poor intertester reliability when applying tests does not necessarily negate the value of these tests, merely the efficiency with which they are applied.
The tests for spinal and sacroiliac function (i.e. mobility/stability, not pain) continue to be developed and hopefully will be able to withstand the scrutiny and rigor of scientific research and take their place in a clinical evaluation that follows a biomechanical and not a pain model.
Discussing the value of tests (many of which are the same as those suggested in this text), she notes that while individually, in isolation, some may fail evaluation as to their reliability and validity, when combined into a sequence of numerous evaluation strategies, and especially when ‘a clinical reasoning process is applied to their findings’, they offer a logical biomechanical diagnosis and ‘without apology, they continue to be defended’.
Lee (2002) has elaborated on her viewpoint as expressed above.
Recent research (Van Wingerden et al 2001, Richardson et al 2000) in the pelvic girdle has shown that the stiffness value (directly related to range of motion; Buyruk et al 1995a) of the sacroiliac joint is related to compression within the pelvis. In these two studies, compression was increased by activation of transversus abdominis, multifidus, erector spinae, gluteus maximus and/or biceps femoris. Whenever these muscles were activated (in isolation or combination), the stiffness value (measured with oscillations and the Echodoppler as per the method originally proposed by Buyruk et al 1995b) of the SIJ increased (and thus the range of motion decreased). Unless the specific muscle activation pattern is noted during whatever range of motion test (active or passive) is being evaluated for reliability – there is no way of knowing what amount of compression the SIJ is under (at that moment) and therefore what the available range of motion should be. Hungerford (unpublished study) has shown that normal individuals performing a one leg standing hip flexion test vary their motor control strategy each time they perform the test, implying that different muscles can be used to perform the same osteokinematic motion. This will vary the amount of compression each time they lift the leg and thus vary the range of motion. Unless trials are repeated and motions averaged, reliability is impossible – not because the tester can’t feel what’s happening but because the subject keeps changing from moment to moment.
The authors of this book agree with Lee. Assessment that leads to treatment choices should not be based on single pieces of evidence. A picture should form from a variety of information-gathering strategies and the history of the individual, involving observation and palpation as well as specific tests, and from which the ‘clinical reasoning’ should emerge to help determine which treatment choices are most indicated.
The sequence of examination that is recommended involves evaluation with the patient standing, sitting (with feet on the floor), lying supine and then lying prone. Some of the assessment methods are observational with the patient static, whereas others involve palpation with the patient either active or passive.
The three key biomechanical elements of pelvic evaluation are:
• asymmetry of pelvic and lower extremity landmarks, ascertained by observation and palpation
• altered motion potential in the joints of the pelvis, ascertained by means of seated, standing, supine and prone evaluations
• altered soft tissue status (short, weak, lengthened, etc.) in the muscles and ligaments of the pelvic girdle.
A fourth assessment criterion involves sensitivity, discomfort or pain, noted during any of the other evaluations. The joints being evaluated are:
• pubic (the relationship of the two pubic bones at the symphysis pubis)
• sacroiliac (the relationship of the sacrum between the two ilia)
• iliosacral (the relationship between each ilium and the sacrum).
Thoughts on treatment strategies
Many of the dysfunctional patterns involving the pelvis in general, and the sacrum in particular, are extremely difficult to diagnose, as there exists a great degree of overlap in symptomatic pictures and assessment variables (For an example, see Box 11.5). As DiGiovanna (1991) explains: ‘Specific treatment of specific dysfunction is most effective. However, because of the firm ligamentous attachments of this [SI joint] articulation, nonspecific treatment may be equally effective.’
Box 11.5 Short leg and heel lift considerations
A short leg imbalance may be very well compensated for, without any requirement for intervention. If, however, symptoms exist that can be tracked back to such an imbalance, where ‘short leg syndrome’ is a reality (even if it should really be called a ‘sacral base unbalancing syndrome’) a solution involving a heel, sole or whole shoe lift may sometimes be appropriate (Greenman 1996, Kuchera & Kuchera 1997).
Cooperstein & Lew (2009) have suggested that ‘Across varying methodologies for measuring LLI [leg length inequality] and pelvic torsion, a consistent, dose-related pattern was identified in which the innominate rotates anteriorly on the side of a shorter leg and posteriorly on the side of the longer leg. …Practitioners of manual medicine who derive vectors for intervention based on leg checking procedures should consider the possibility that the direction of pelvic torsion may be variable depending on whether the LLI is of anatomical or functional origin.’
Compensation for a short leg/sacral base unleveling will usually involve a scoliosis with one or more lateral curves. The lumbar scoliosis usually involves sideflexion away from, and rotation toward, the short leg side. Pelvic rotation is automatic and a variety of additional compensation adaptations evolve as the body attempts to maintain reliable coordinated information input from visual, vestibular and proprioceptive sources.
Kuchera & Kuchera (1997) describe characteristic changes:
The innominate typically rotates anteriorly on the side of the apparent short leg to lengthen that extremity relative to the other. The innominate on the side of the apparent long leg may rotate posteriorly to relatively shorten that extremity.
Other changes may include pronation of the foot on the long leg side; increased lumbosacral angle; pelvic rotation and scoliosis as described and, over time, excessive wear and probably osteoarthritis in the hip joint of the long leg side.
Suspicion of this type of imbalance may be raised by an otherwise unexplained history of recurrent pain and dysfunction involving the spine, pelvis and/or myofascial tissues. The soft tissues involved in such dysfunctional patterns may be expected to include: shortening in the concave tissues of the scoliosis (together with lengthening in the convex side soft tissues); tight adductors on one side and abductors on the other; tight hamstrings on one side and quadriceps on the other; pain in the iliolumbar ligament on the side of the convexity of the lumbar scoliosis; pain may be referred from the iliolumbar ligament to the ipsilateral groin and upper medial thigh; SI ligaments on the side of convexity may be stressed and refer pain into the lateral leg; on the long leg side unilateral sciatica and hip pain may be reported; a wide variety of dysfunctional patterns may affect the postural muscles of the region. Greenman (1996) reports that he has found any leg length discrepancy greater than 6 mm (quarter of an inch) to be significant if accompanied by low back or lower extremity pain.
Because compensation efficiency varies so markedly from person to person no single landmark variation can precisely identify the reality of a short leg condition. Kuchera & Kuchera (1997) suggest that the following are all individually inaccurate in identifying the presence of sacral base unleveling or short leg syndrome (Beal 1950, Clarke 1972, Nichols & Bailey 1955).
• Alignment of spinous processes
• ASIS or hip-to-ankle measurements
• Supine measurement /comparison of medial malleolus levels
• Even standing evaluation of greater trochanter heights, while being ‘somewhat more helpful’, may be inaccurate because of the presence of coxa varus or coxa valgus.
Apart from a complex symptom picture, Kuchera & Kuchera assert that a positive standing flexion test, accompanied by a negative seated flexion test (see pp. 331 and 333), should raise suspicion of negative influences on the pelvis from the lower extremity, possibly a short lower extremity. Following mobilization of restrictions revealed by clinical examination of the spine and pelvis, standing X-rays that include data as to iliac crest heights, femoral head heights, sacral base unleveling and scoliotic patterns should be examined in order to establish actual leg length discrepancies. Kuchera & Kuchera (1997) suggest that such X-ray evidence should only be gathered ‘when the spine is as mobile as possible, and any nonphysiological (shear) somatic dysfunctions have been removed.’
Greenman (1996) speaks of not performing X-ray studies until ‘the patient [is] at maximum biomechanical function of the lumbar spine, pelvis and lower extremities.’
The treatment of a short lower extremity by means of heel or sole lifts is highly controversial and experts have presented contrary viewpoints. Some basic guidelines are important if any modification of heel or sole height is considered.
• Avoid heel lifts if the lumbar spine is not flexible as the adaptive forces created by the lift will be transmitted into structures and tissues other than the lumbar spine, creating greater mischief in areas cephalad to it.
• Once a heel lift strategy has been decided on, the objective should be to avoid adding, in total, more than half of the measured discrepancy between the legs.
• Kuchera & Kuchera (1997) suggest that if the spine is reasonably flexible a heel lift of no more than 1/8th of an inch (3 mm) should be introduced initially, with gradual increments of heel height thereafter, at a rate no greater than 1/16th of an inch (1.5 mm) per week, until a half inch is reached. They also suggest that any increment beyond a half inch lift (1.3 cm) should include sole as well as heel.
• Greenman (1996), however, disagrees with such slow increments and suggests starting with an initial 3/8 inch (9 mm) lift, followed, if necessary, by a reduction of 3/8 inch (9 mm) of the heel on the long leg side shoes, 3–6 weeks later. If the total lift required is beyond 3/4 inch (9 mm), Greenman suggests that further increments to the short leg side should involve 3/8 inch (9 mm) lifts of both heel and sole.
• Greenman makes a useful clinical observation regarding tactics for lengthening of the short lower extremity if there is a sacral base angle greater than 42° or if there is a marked lumbar lordosis. In order to avoid increasing the anterior tilt in such circumstances the change in leg length should be applied to the long leg side, with reduction in heel height by the appropriate amount.
Such thoughts have been kept in mind in the following discussions of the region, which involves assessment and treatment of some of the main dysfunctional patterns to be noted in the pelvis, in general, and the SI joint, in particular. The treatment protocols described do not include descriptions of high-velocity low-amplitude (HVLA or ‘thrust’) techniques, which are adequately described elsewhere, with Gibbons & Tehan’s text (2000) recommended for accuracy and clarity. Instead, focus is placed on soft tissue methods, whether this involves deactivation of trigger points, where appropriate, or the toning and facilitation toward normality of weakened, inhibited, structures or the lengthening and stretching of shortened ones or the use of soft tissue features to modify joint mobilization and/or the use of rehabilitation and self-help exercise protocols to reestablish functional integrity and discourage inappropriate use patterns.
Details of many of the methods that can achieve these ends are described throughout the clinical applications portion of this chapter and the remainder of the text.
Hypermobility issues
Hypermobility as a general issue is discussed in Chapter 1 (see Box 1.3). However, there are several important considerations relative to joint laxity that have particular relevance to the low back and sacroiliac joints. It should be obvious that joint structures which have a reduced sense of stability and resilience, or in which the range of motion is clearly excessive, should not receive treatment that is likely to increase these unstable states. As explained more fully in Box 1.3, three broad categorizations of joint laxity exist.
• Particular pathological conditions, most notably Marfan’s syndrome and Ehlers-Danlos syndrome, predispose toward joint laxity that involves histological changes affecting the connective tissues.
• The ectomorph body type displays a physiological hypermobility, often noted in athletes, gymnasts and ballet dancers. In these instances the hypermobility is commonly compensated for by excellent muscle tone.
• Restriction (hypomobility) in one joint may produce a compensatory hypermobility in adjacent or associated structures. In such cases there is a risk that manual therapy focus will be on the hypermobile segments/areas, which are commonly where pain is noted, rather than the hypomobile primary structure(s). Such an approach would almost certainly aggravate the hypermobility if the techniques used encouraged soft tissue lengthening. There exists a potential danger for a hyper-mobile joint to become unstable when inappropriately treated. Instability may call for support, surgery or a form of engineered hypotonicity, such as is produced by sclerosing injections (Greenman 1996). (See Box 11.6)
Box 11.6 Prolotherapy, surgical fusion and fixation of the SI joint
When the SI joint is unstable and contributing to a chronic low back pain condition, a variety of therapeutic intervention possibilities exist, ranging from the conservative (see this and the previous chapter) to the radical. Lippitt (1997) suggests:
Low back pain that has defied diagnosis by conventional means frequently emanates from the SIJ, and pain can be relieved by SIJ stabilization. Stabilization may be achieved by physiotherapy modalities such as muscle strengthening or balancing, by belting, by tightening of the SI ligament complex via proliferant injections, or, if these fail, by SIJ fixation or fusion. Fixation can be accomplished by placing screws across the joint.
Fusion
Keating et al (1997) describe the use of fusion of the SI joint for a very small percentage of patients whose chronic SIJ dysfunction does not resolve via non-operative methods. The procedures used involve ‘a combination of surgical debridement and autogenous bone grafting of the inferior-posterior SIJ, with compression screw fixation of the superior joint’.
The recovery timeline includes:
• first week: crutches with emphasis on weight bearing
• weeks 1–2: full weight bearing and limited walking and cycling exercise
• weeks 2–3: all activities increased and exercises for low back extensors, as well as piriformis and lower body stretching
• weeks 3–4: full rehabilitation program three times weekly
• week 4: full exercise regime and lumbar extension training exercises using machines
• weeks 4–6: return to sedentary work, avoiding lifting greater than 10 kg weights and continuation of full exercise program.
After assessment at 8 weeks all activities increase and by 10–12 weeks postoperatively regular work and sporting activities resume.
Keating et al (1997) note that the most important issue after surgery is early activation of the patient, especially walking and piriformis stretching, which ‘continues for 2 months following surgery’.
Fixation
Lippitt (1997) differentiates intraarticular SIJ problems (pathology including fracture, degenerative joint problems, tumor, infection, inflammatory spondyloarthropathies, etc.) and extraarticular SIJ problems caused by ‘disruption of the ligamentous support system’ in which, although the joint may be inflamed, it remains structurally normal. Criteria for fixation (very similar to those suggested for fusion) include disabling levels of pain localized to the SIJ, unrelieved by normal conservative methods, but relieved short term by a sacroiliac anesthetic joint block. Other major causes of lumbopelvic pain should have been ruled out including disc herniation, arthropathy affecting facet joints, entrapment of nerve roots, spinal stenosis and arthritic changes of the hip. Fixation procedures usually involve a careful positioning of the joint followed by insertion of (usually) titanium screws to fix the joint from the ilium to the sacrum.
All associated conditions would be treated using conventional methods before, or after, the surgical intervention. Lippitt (1997) reports the procedure to be ‘relatively simple, safe, and effective’. … .‘To date, no screw has broken or backed out, and follow-up X-rays have failed to show evidence of fusion despite continued clinical improvement. The procedure has been performed in women of childbearing potential who are willing to undergo caesarean section if necessary. To date none of these patients have become pregnant.’
Prolotherapy
Hackett (1958) pioneered the use of controlled irritation of relaxed ligamentous tissues to achieve proliferation with minimal scarring, with a view to enhancing stability of the weakened structures. The key to success was increased collagen formation, hyperplasia of the ligament tissue – without evidence of histological damage (scarring). Dorman (1997) suggests that prolotherapy (proliferant therapy; ‘intentional provocation of increased connective tissue formation’) achieved by injection into the tissues of various solutions (containing tissue irritants such as phenol, osmotic shock agents such as glucose, inflammatory precursors such as sodium morrhuate, and particulates which sustain local irritation such as pumice flour) enhances ligamentous function, particularly in structures such as the SIJ and knee.
Dorman’s research suggests that SIJ movement has a profound influence on energy storage and transfer during the gait cycle (see Chapter 3) particularly involving the posterior SI ligaments. He maintains that sacroiliac:
ligament relaxation [i.e. laxity] can be responsible for…a series of painful syndromes in and around the human pelvis [and] the transfer of torque through the tensegrity mechanism to other sites in the axial skeleton, particularly the cervical spine and thoracolumbar junction.
When conservative methods of normalization fail or ‘when ligament relaxation, alone or associated with fault propagation at a proximal or remote site, has led to permanent changes in ligaments or fascia, treatment by prolotherapy is restorative’. The injections are commonly into the pelvic stabilizing ligaments, ‘in particular the layers of the posterior SI ligaments, paying particular attention to the deepest and central part’.
Dorman reports that protocols for use of prolotherapy include manipulation (‘modified osteopathic technique’) and ‘a full range of movement exercises, to encourage healing in the natural lines of strain’.
The authors suggest that there is probably a place, in extreme circumstances, for all of these procedures but that conservative methods, such as those described throughout this book, should be attempted initially. In terms of choices, prolotherapy appears less invasive than either of the surgical procedures described and fixation involves less traumatic damage than fusion. Ultimately, the individual patient, having taken professional advice, has to decide on what is most appropriate. However, it is suggested that as wide a range of options as possible should be sought before undertaking an irreversible procedure.
If hypermobility is suspected either as a pathological, physiological or compensatory phenomenon, all methods that involve mobilization, stretching or manipulation should be applied with utmost caution and selectivity, based on specific needs and with the underlying situation of laxity in mind.
Kappler (1997) cautions that: ‘A normal physiological reaction to a painful hypermobile joint is for muscles surrounding the joint to splint the joint, and protect it from excess motion. Physical examination reveals restriction of motion. Underneath the protective muscle splinting is the unstable joint.’ It may be useful to reflect that one way in which the body might maintain excess tone in a muscle offering such protective support would be for it to evolve trigger point activity. These distressed supporting muscles (and their associated trigger points) might be best left untreated until underlying use patterns can be modified. Kappler (1997) suggests: ‘Management [of hypermobile structures] involves modifying patient activity that contributes to instability, mobilizing adjacent hypomobile joints, and prescribing active rehabilitation exercises.’
General tests for hypermobility are described in Chapter 1.
Iliosacral or sacroiliac?
Osteopathic methodology, based on the work of Fred Mitchell (1967), makes a distinction between SI joint problems that primarily involve iliosacral dysfunction (involving both innominate and/or pubic factors) and those which are primarily sacral (as in sacroiliac) in nature.
Iliosacral dysfunctions, which are determined by means of the standing flexion test, the ‘stork’ (Gillet) test and by various palpation methods (see the ensuing discussions), are thought to involve neuromuscular imbalances (possibly involving iliopsoas, hamstring or other muscular or fascial changes), and are frequently amenable to soft tissue treatment methods (including MET), for their normalization.
Confusion is sometimes expressed as to the difference between a sacroiliac and an iliosacral dysfunction. An imperfect but illustrative analogy may be offered by imagining a door within its frame. If a door cannot swing freely open and closed within its frame, the problem may lie in one of a number of areas.
• The door itself may have modified (possibly due to the hinges working loose or actual warping of the material of the door), preventing it from freely swinging within the unchanged door frame.
• The frame may have modified, perhaps becoming warped, so that the door could not move freely within it.
• The level of the floor might have modified, altering both the frame and the door positions.
Whichever of these events had occurred, objectively the problem would be a ‘stuck’ door, unable to open or close correctly. However, the cause and therefore the remedy might possibly lie within the door, the frame, the supporting hinges or the foundations on which the structure rested.
The analogy with the sacrum, its ‘frame’ (the ilia) and the foundation and supporting structures is obvious.
Primary sacral dysfunctions are frequently more complex than innominate problems, in both their etiology and treatment. A particularly useful soft tissue approach for both assessment and treatment of sacral dysfunction, using positional release methodology (strain-counterstrain), is described later in this chapter.
Observation is an important element in pelvic assessment and Lee (2004) makes the case for landmark points of reference being established before mobility tests are performed, ‘When interpreting mobility findings, the position of the bone at the beginning of the test should be correlated with the subsequent mobility, since alterations in joint mobility may merely be a reflection of an altered starting position’.
The authors suggest that evaluation of findings deriving from the assessments described below is more likely to be accurate if they are considered in conjunction with a comprehensive assessment for shortness of associated musculature. For example, shortness in quadratus lumborum, latissimus dorsi, tensor fasciae latae, piriformis, hamstrings, etc. can modify pelvic position markedly and so produce apparently dysfunctional joint patterns, or positional findings which are unrelated to actual joint dysfunction. Mobility (and other) tests should be repeated 3–4 times for a more accurate assessment.
For example, a unilaterally short quadratus lumborum may cause one pelvic crest to appear more cephalad than the other and/or a unilaterally short hamstring may prevent pelvic movement from being symmetrical during spinal flexion. If short muscle assessments are not carried out prior to the pelvic joint assessments described below, there should at the very least be an evaluation of functional integrity of the associated muscles, using Janda’s functional prone hip extension and sidelying hip abduction tests, described on p. 320.
Static innominate positional evaluation
• The patient is prone and the relative positions of the PSISs, ASISs and the ischial tuberosities are evaluated for their relative superiority/inferiority.
• The inferomedial aspect of the sacrotuberous ligament should be palpated as to its relative tension in order to verify the positional assessment. Lee (1999) states: ‘If the innominate is posteriorly rotated, the sacrotuberous ligament should be taut since the points of attachment are attenuated. However, if the innominate is anteriorly rotated the sacrotuberous ligament should be relatively slack.’
Static sacral positional evaluation (Figs 11.18 - 11.20)
• The patient is evaluated first in a seated and fully flexed position, then prone with the spine in neutral and then prone in extension.
• In order to evaluate sacral status, it is necessary to compare the left and right side posteroanterior relationship of (a) the sacral base and (b) the inferior lateral angle (see Fig. 11.20). The positional findings (which are not diagnostic of dysfunction) are evaluated as follows.
• If there is an anterior sacral base on one side (say, right in this example) and a posterior inferior lateral angle (ILA) on the other side (say, left in this example), this is noted as a left rotated sacrum (and vice versa if the sacral base was posterior on the right and the ILA anterior on the other).
• It is usual for such rotations to be accompanied by a sidebending of the sacrum to the opposite side. For example, if there were an anterior sacral base on the right and a posterior inferior sacral angle on the left (i.e. left rotated sacrum), the sacrum will commonly sidebend toward the right and its freer degree of movement would be further in the direction in which it is deviating (i.e. it would be difficult for the sacrum to further rotate right and sidebend left (Ward 1997).

Figure 11.18 Points of anterior palpation for positional testing of the innominate
(reproduced with permission from Lee 1999).
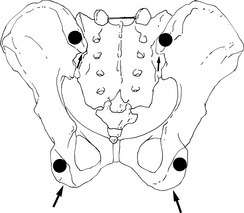
Figure 11.19 Points of posterior palpation (large arrows) for positional testing of the innominate. The inferior aspect (small arrows) of the PSIS and the ischial tuberosity (dots) are palpated bilaterally and the superoinferior/mediolateral relationship noted
(reproduced with permission from Lee 1999).
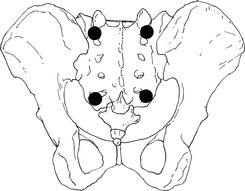
Figure 11.20 Points of palpation for positional testing of the sacrum
(reproduced with permission from Lee 1999).
Sacral torsions
It is not within the scope of this text to describe the highly complex (and somewhat controversial) assessment protocols for so-called sacral torsions, in which rotational motion about an oblique axis occurs at the lumbosacral junction. They are mentioned here merely to highlight the nature of this dysfunctional pattern, which relates to sacral dysfunctions relative to the last lumbar vertebrae, for example where the sacrum has rotated left and L5 has rotated right (Fig. 11.21). For reading on this topic, and to evaluate different perspectives, the following texts are recommended.
• DiGiovanna E, Schiowitz S, Dowling D 2004 An osteopathic approach to diagnosis and treatment, 3rd edn. J B Lippincott, Philadelphia
• Greenman P 2003 Principles of manual medicine, 3rd edn. Lippincott, Williams and Wilkins, Baltimore
• Lee D 2004 The pelvic girdle: an approach to the examination and treatment of the lumbopelvic-hip region, 3rd edn. Churchill Livingstone, Edinburgh
• Heinking K, Jones III J M, Kappler R 1997 Pelvis and sacrum. In: Ward R (ed) American Osteopathic Association: foundations for osteopathic medicine. Williams and Wilkins, Baltimore
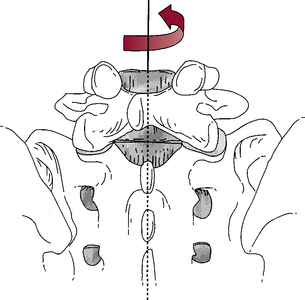
Figure 11.21 Right axial torsion of the L5 vertebra is resisted by osseous impaction of the left zygapophysial joint and capsular distraction of the right zygapophysial joint as well as by the segmental ligaments, the intervertebral disc and the myofascia
(reproduced with permission from Lee 1999).
A discussion of ‘sacral foramen tender points’ is presented later in this chapter for methods that utilize positional release (strain-counterstrain) to treat presumed sacral torsions.
Standing pelvic assessments
Before carrying out other pelvic assessments, the Trendelenburg sign (as described in Method 3 on p. 321.) should be performed to evaluate relative strength of gluteus medius.
The standing patient’s gluteal folds should also be observed. These represent the lower borders of gluteus maximus and their relative symmetry is noted. Observations of asymmetry in crest, PSIS and gluteal fold height may represent the influence of postural imbalances, leg length discrepancy, neurological dysfunction and/or habitual patterns of use. At this stage the differences are noted. They are not diagnostic but represent a snapshot of aspects of current pelvic balance or imbalance. Standing observational evaluation of pelvic tilt should be performed, followed by static evaluation of the relative positions of the innominates and the sacrum.
Note: All findings should be recorded/charted.
Standing pelvic orientation evaluation (‘tilt’)
• The practitioner kneels at the side of the standing patient and places one index finger on the ASIS and the other on the PSIS.
• Normal pelvic orientation is considered to result in the anterior contact appearing level with the posterior contact or no more than half an inch (1 cm) lower.
• If the anterior finger is more than half an inch (1 cm) lower, the pelvis is considered to have tilted anteriorly.
• If the posterior finger is to any degree lower than the anterior finger, there is a posterior pelvic tilt (see Fig. 2.16).
Standing pelvic balance test
• The practitioner squats behind the standing patient, whose weight should be evenly carried on both sides, and places the medial side of her hands on the lateral pelvis below the crests and pushes inwards and upwards until the index fingers lie superior to the crest.
• If these are judged to be level then anatomical leg length discrepancy is unlikely.
• If an inequality of height of the pelvic crests is observed, the heights of the greater trochanters should also be assessed, by direct palpation.
• If both the pelvic crest height and the height of the ipsilateral greater trochanter appear to be greater than the opposite side, an anatomical leg length difference can be presumed (Greenman 1996).
• If the pelvic crest height or the trochanter height is greater on one side than the other, pelvic dysfunction is a possible explanation, commonly involving postural muscle shortening and imbalance (e.g. quadratus lumborum) or actual structural osseous asymmetry may exist.
Standing PSIS symmetry test
The PSIS positions are assessed just below the pelvic dimples.
• Anteriority of one PSIS may involve shortness of the external rotators of the ipsilateral leg (iliopsoas, quadratus femoris, piriformis) or contralateral internal rotators (anterior fibers of gluteus medius, tensor fasciae latae, hamstrings) and involves a rotation of the pelvis or innominate around a vertical axis.
• Inferiority of one PSIS may indicate hamstring shortness or pelvic/pubic dysfunction and involves posterior tilt of that innominate around a horizontal axis.
• Superiority of one PSIS may indicate rectus femoris, TFL, anterior gluteal or iliacus shortness and involves anterior tilt of that innominate around a horizontal axis.
• To determine if one PSIS is superior or the other inferior, each should be compared to its paired ASIS and normal would be indicated by an ASIS and a PSIS, on the same side, being level (or almost level) with each other.
CAUTION: The evidence derived from the standing flexion test as described below is invalid if there is concurrent shortness in the hamstrings, since this will effectively give either:
• a false-negative result ipsilaterally and/or a false-positive sign contralaterally if there exists unilateral hamstring shortness (due to the restraining influence on the side of hamstring shortness, creating a compensating innominate movement on the other side during flexion) or
• false-negative results if there is bilateral hamstring shortness (i.e. there may be iliosacral motion that is masked by the restriction placed on the ilia via hamstring shortness).
The hamstring length test as described in Chapter 12 should therefore be carried out first and if this proves positive these structures should be normalized, if appropriate, prior to use of the assessment methods described here. At the very least, the likelihood of a false-positive standing flexion test should be kept in mind if there are hamstring influences of this sort operating.
Standing flexion (iliosacral or forward bending) test
With the patient standing, any apparent inequality of leg length, as suggested by unequal pelvic crest heights, should be compensated for by insertion of a pad (‘shim’) under the foot on the short side. This helps to avoid errors in judgment as to the endpoint positions, for example when assessing the end of range during the Gillet or standing flexion tests.
• The thumbs are placed firmly (a light contact is useless) on the inferior slope of the PSIS and the patient is asked to go into full flexion while thumb contact is maintained, with the practitioner’s eyes level with the thumbs (Fig. 11.22).
• The patient’s knees should remain extended during this bend.
• The practitioner observes, especially near the end of the excursion of the bend, whether one or other PSIS ‘travels’ more anterosuperiorly than the other.
• If one thumb moves a greater distance anterosuperiorly during flexion it indicates that the ilium is ‘fixed’ to the sacrum on that side (or that the contralateral hamstrings are short or that the ipsilateral quadratus lumborum is short: therefore, all these muscles should have been assessed prior to the standing flexion test).
• If both hamstrings are excessively short this may produce a false-negative test result, with the flexion potential limited by the muscular shortness, preventing an accurate assessment of iliac movement.
• At the end of the flexion excursion, Lee (2004) has the patient come back to upright and bend backward, in order to extend the lumbar spine. ‘The pelvic girdle should posteriorly tilt symmetrically on the femoral heads’. That is, the PSISs should move equally in a caudad (inferior) direction.
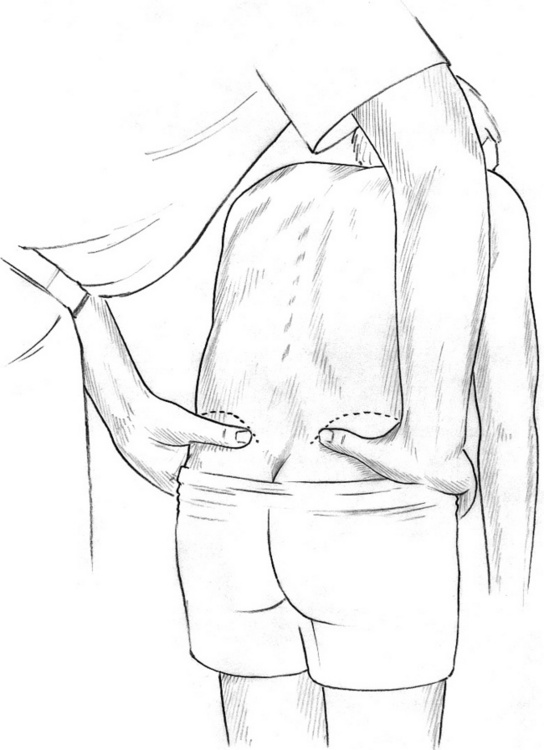
Figure 11.22 Standing flexion test for iliosacral restriction. The dysfunctional side is the side on which the thumb moves on flexion
(reproduced with permission from Chaitow 2006).
Note: Both the standing flexion test (above) and the ‘stork’ test (below) are capable of demonstrating which side of the pelvis is most dysfunctional, restricted or hypomobile. They do not, however, offer evidence as to what type of dysfunction has occurred (i.e. whether it is an anterior or posterior innominate rotation, internal or external innominate flare dysfunction or something else). The nature of the dysfunction needs to be evaluated by other means, including aspects of supine pelvic assessment as described later in this section.
Standing iliosacral ‘stork’ (one-leg standing or Gillet test)
• The practitioner places one thumb on the PSIS and the other thumb on the ipsilateral sacral crest, at the same level.
• The standing patient flexes knee and hip and lifts the tested side knee so that he is standing only on the contralateral leg.
• The normal response would be for the ilium on the tested side to rotate posteriorly as the sacrum rotates toward the side of movement. This would bring the thumb on the PSIS caudad and medial.
• Lee (2004) states that this test (if performed on the right) ‘examines the ability of the low back, pelvis, and hip to transfer load unilaterally (support phase) as well as for the pelvis to allow intrapelvic rotation’.
• If, upon flexion of the knee and hip, the ipsilateral PSIS moves cephalad in relation to the sacrum, this is an indication of ipsilateral pubic symphysis and iliosacral dysfunction. This finding can be used to confirm the findings of the standing flexion test (above). Petty (2006) also suggest that a positive Gillet test indicates ipsilateral sacroiliac dysfunction.
• Lee (1999) reminds us that this test also allows assessment of ‘the patient’s ability to transfer weight through the contralateral limb and to maintain balance’.
Standing hip extension test
• The patient stands with weight on both feet equally.
• The practitioner palpates the PSIS and sacral base as in the stork/Gillet test above.
• The patient extends the leg at the hip on the side to be tested.
• The innominate should rotate anteriorly and the thumb on the PSIS should displace superolaterally relative to the sacrum.
• Failure to do so may indicate a restriction of the innominate’s ability to tilt anteriorly and to glide inferoposteriorly on the sacrum.
Spinal behavior during flexion tests
Greenman (1996) suggests that during both the standing and seated flexion tests attention should be paid to the behavior of the lumbar and thoracic spines, looking for alterations in the free movement of the spine and the appearance of any lateral curves.
If altered vertebral mechanics is more severe during the standing flexion test than seated, major restriction in the lower extremity is suggested. If vertebral dysrhythmia is worse during the seated flexion test, major restriction above the pelvic girdle is suggested.
Confirmation of such imbalances may be obtained by use of the standing and seated spinal rotation observation as described below.
Standing and seated spinal rotoscoliosis tests
• After the standing flexion test and before performing the seated flexion test, the practitioner moves to the front of the fully flexed, standing patient and looks down the spine for evidence of greater ‘fullness’ on one side or the other of the lower thoracic and lumbar spine (and associated ribs), indicating the muscular mounding commonly associated with spinal rotoscoliosis (or possibly due to excessive tension in quadratus lumborum, or hypertrophy of the erector spinae).
• With the (now) seated patient fully flexed, the practitioner stands at the head and looks down the spine for evidence of fullness and mounding in the paravertebral muscles, in the lower thoracic and lumbar area.
• If greater fullness exists in a paraspinal area of the lumbar spine, with the patient standing as opposed to seated, then this is evidence of a compensatory process, involving the postural muscles of the lower extremities and pelvic area, as a primary factor.
• If, however, fullness in the lumbar paraspinal region is the same when seated, or greater when seated, this indicates some primary spinal dysfunction and not a compensation for postural muscle imbalances.
• The focus of treatment and rehabilitation will depend on whether primary factors are considered to relate to pelvic or spinal biomechanics or whether they have more to do with imbalances in the postural musculature of the lower extremity. The assessments described help to isolate causative influences.
Seated pelvic assessments
Seated flexion (sacroiliac) test
• The patient is seated with feet flat on the floor for support.
• The practitioner is behind the patient with thumbs firmly placed on the inferior slopes of the PSISs, fingers placed on the curve of the pelvis, index fingers on the crests, in order to provide stabilizing support for the hands.
• The seated flexion test involves observation of thumb movement, if any, during full slowly introduced flexion (Fig. 11.23).
• Since the weight of the trunk rests on the ischial tuberosities, the ilia cannot easily move and if one PSIS moves more cephalad during flexion, this suggests a sacroiliac restriction on that side.
• A false-positive result may be caused by an ipsilateral shortness in quadratus lumborum (Greenman 1996).
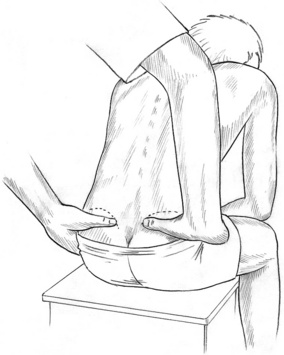
Figure 11.23 Seated flexion test for sacroiliac restriction. The dysfunctional side is the side on which the thumb moves on flexion
(reproduced with permission from Chaitow 2006).
Supine pelvic assessments and treatment protocols
Pelvic alignment in supine prior to assessment
A clinically useful tactic is suggested for establishing a relaxed alignment of the pelvis before assessment, so that minimal deviation is produced by postural muscles.
• The supine patient is asked to flex the knees, maintaining the feet (placed centrally and together) on the table.
• The patient is asked to raise the buttocks off the table slightly and then to lower the buttocks back onto the table and lower the knees.
• Subsequent assessment of landmarks will be more accurate as a result of this simple maneuver (Heinking et al 1997).
Supine shear dysfunction assessment
• If there is an apparent unleveling of the iliac crests in an unloaded situation (patient supine or prone) – having used the supine pelvic alignment protocol described immediately above – a shear dysfunction (‘upslip’ or ‘downslip’) is probable. (See Box 2.6, p. 38, regarding determination of the practitioner’s dominant eye.)
• Heinking et al (1997) suggest that ‘downslip’, or inferior innominate shear, is unusual and will reduce or normalize with walking. The characteristics are of an ASIS, a PSIS and a pubic ramus that are all more caudad than their contralateral components. There are likely to be complaints of pelvic pain and accompanying tissue texture changes at the ipsilateral SI joint and pubic symphysis.
• When an ‘upslip’ or superior innominate shear has occurred the characteristics are of an ASIS, PSIS and pubic ramus that are all more cephalad than their contralateral pair without any evidence of innominate rotation. There are likely to be complaints of pelvic pain and accompanying tissue texture changes at the ipsilateral SI joint and pubic symphysis.
MET of a superior innominate shear (Greenman 1996) (Fig. 11.24)
• The patient is supine with legs straight and supported by the table and with the feet extending off the end of the table.
• For treatment of left side upslip, the practitioner stands at the foot of the table and braces against the contralateral foot to produce stability.
• The ipsilateral foot is held slightly proximal to the ankle.
• The leg is abducted to approximately 15° and is then internally rotated until the end of range is noted.
• The combination of forces (abduction and internal rotation of the extended leg) loose packs the sacroiliac joint and close packs the hip.
• The practitioner introduces long axis traction to take out available slack as the patient introduces a series of isometric muscle energy contractions, such as trying to pull the leg toward the hip or trying to lengthen the leg or attempting to externally rotate and adduct the leg.
• Each such effort, lasting no more than 5–7 seconds, should involve no more than 10–20% of available strength and should be completely resisted by the practitioner.
• Each isometric effort should be accompanied by the patient’s held inhalation.
• After each effort and complete relaxation and resumption of normal breathing, the ‘slack’ is removed, i.e. increased traction, slight abduction and internal rotation to the first barrier of resistance.
• After several efforts the levels of the landmarks (ASIS, PSIS, pubic ramus) should be retested and, if close to balanced, the treatment is complete.
• Greenman (1996) suggests that upslip dysfunction and pubic symphysis dysfunction (described below) should be treated prior to continuation of pelvic assessment. ‘When an innominate shear dysfunction is present, it appears to restrict all other motions within the SI joint. Therefore, it deserves attention early in the [assessment and] treatment process.’

Figure 11.24 Practitioner holds the extended (left) leg in internal rotation, abduction and long axis extension (traction) to close pack the hip joint during the MET procedure to treat left superior innominate shear. Note practitioner’s left thigh braces patient’s right leg to provide counterpressure
(adapted from Greenman 1996).
Pubic dysfunction assessment (Fig. 11.25)
The simplest way to find the bones is to ask the patient to find them on himself after he has been shown a skeletal body chart and offered an explanation as to why the practitioner is going to palpate this area. A male patient is also asked to displace the genitals (if needed) and to ‘protect’ himself during the treatment. It is useful to have the patient void the bladder prior to the test as even light pressure on the lower abdomen may be poorly tolerated if the bladder is full and if there is any anxiety regarding this function. This is especially true for the person who has a tendency toward incontinence.
• The practitioner stands to one side or the other, at upper thigh level, facing cephalad.
• Once the patient has located the bony surface, in order to allow the practitioner to identify the superior margin of the pubic bones without undue difficulty or invasive contact, the palm of the practitioner’s tableside hand is placed palm down on the lower abdomen, finger tips close to the umbilicus.
• The heel of the hand is slid caudally until it comes into contact with the superior aspect of the pubic bone.
• Having located this landmark, the practitioner places both index fingers on the anterior aspect of the symphysis pubis and slides each of these laterally (to opposite sides) approximately 1–2 finger-tip widths in order to simultaneously evaluate the positions of the pubic tubercles.
• Is one tubercle more cephalad or caudad than the other?
• Is there evidence of increased tension on one side or the other at the attachment of the inguinal ligament?
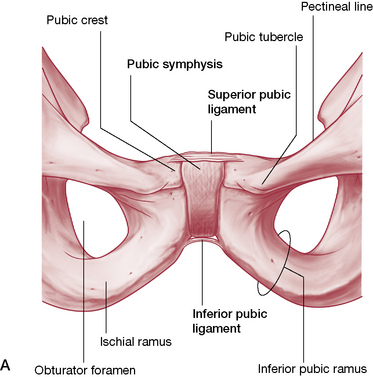
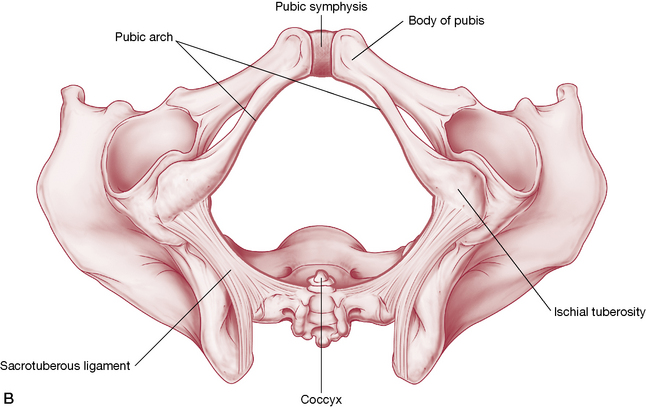
Figure 11.25 A: Anterior view of the pubic symphysis. B: Pubic symphysis as part of the pubic arch.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Greenman (1996) suggests that any such positive finding calls for treatment prior to the assessment proceeding. Treatment would depend on other findings but might include:
• muscle energy ‘shotgun’ approach (described on p. 336)
• normalization of associated musculature. Greenman (1996) points out that: ‘Muscle imbalance between the abdominals above and the adductors below are major contributors to the presence and persistence of this dysfunction. They frequently result from the chronic posture of standing with more load on one leg than the other.’ Consideration should also be given to gluteus medius and minimus since they work in association with the contralateral adductors and may be prevoking a compensation pattern.
• use of PRT, especially if the condition accompanies low back (L5) pain or dysfunction as the symphysis pubis is the location of the Jones tender point associated with such dysfunction. Heinking et al (1997) state: ‘What appears to be a pubic dysfunction may actually be reflexive evidence of L5 dysfunction’ (see positional release notes in Chapter 10 and in Volume 1, Chapter 10).
Note: It is our experience that dysfunction at the symphysis pubis, as demonstrated by positive findings in the test described above, is commonly a compensation for primary iliosacral or sacroiliac dysfunction and will correct spontaneously when these dysfunctions are appropriately normalized. However, as Heinking et al (1997) state: ‘There are times when the ASISs appear to be equal, the PSISs appear to be equal, and yet the pubes are definitely displaced so that one is detectably superior and the other inferior.’ The finding in such a case would be of a primary pubic shear dysfunction.
MET treatment of pubic dysfunction
Two simple methods, which utilize multiple myofascial contractions simultaneously, can frequently normalize pubic dysfunction. Failing this, normalization of coexisting iliosacral dysfunctions (rotations and flares, as described below) will commonly restore pubic relationships at the symphysis to normal. Method 1 is performed and then method 2. Method 1 is repeated and then method 2 is also repeated.
‘Shotgun’ method 2
The practitioner separates the knees and places her forearm between them (palm on inside of one knee and elbow on inside of other knee), as the patient, using full strength (or less if this is uncomfortable) attempts to push the knees together for 3–4 seconds.
‘Shotgun’ method 3 (Liebenson 2007)
The patient’s separated knees are slowly but forcefully adducted against the patient’s resistance to introduce an isotonic eccentric stretch of the external rotator muscles, effectively toning these and producing a release in tone of the internal rotators through reciprocal inhibition. See the discussion of muscle energy procedures in Chapter 9 (Fig. 11.26).
‘Shotgun’ method 4
The practitioner slowly but forcefully separates the patient’s knees, which are being adducted against this resistance, so producing an isotonic eccentric stretch of the soft tissues involved. This fourth variation has been found useful by one author (LC) as a final component of the ‘shotgun’ sequence, after the methods described above are completed.
The muscular and ligamentous forces created by all of these contractions contributes to normalization of imbalances at the symphysis, sometimes audibly. There may also be an audible release in the region of one or other inguinal ligament.
Positional release methods for pubic shear/inguinal dysfunction (or suprapubic pain)
Method 1: Morrison’s ‘inguinal lift’
Morrison (1969) maintained that most women who regularly wear high heels present with a degree of what he termed ‘pelvic slippage’. The use of the approach described below is meant to enable low back adjustments to ‘hold’. He recommended its application when low back problems failed to respond to more usual methods, since he maintained that the pelvic imbalance could act to prevent the normalization of spinal dysfunction.
• The patient lies supine with legs apart and straight.
• The superior (cephalad) margin of the pubis should be palpated, close to the inguinal area by following the previously mentioned methods for palpating the pubic area. Pain will be found on the side of ‘slippage’ (‘upslip’, superior shear).
• This most painful site should be pressed/palpated by the patient who is asked to report a numerical value for the pain.
• The objective, as in all strain-counterstrain positional release methods, is to reduce levels of perceived pain during the procedure, from a starting level of ‘10’, by at least 70% (Chaitow 2007) (see methodology briefly described in Chapter 9 and more fully in Volume 1, Chapter 10).
• The male patient should be asked to displace the genitals toward the non-treated side with one hand while palpating the painful point with the other.
• Whether the patient is male or female, another person should be in the room as a chaperone since both the practitioner and the patient are vulnerable when treating the inguinal area.
• The practitioner stands just below the patient’s waist level on the side to be treated and places the flat caudad hand on the inner thigh so that the web between finger and thumb comes into contact with the tendon of gracilis, at the ischiopubic junction.
• It is important that the contact hand on the gracilis tendon should be relaxed, not rigid.
• Light pressure, superiorly directed (cephalad), is then applied to assess for discomfort. The soft ‘webbing’ contact on the tendon allows the applied force to be increased gradually without discomfort, removing available slack from the tissues of both the hand and the inguinal area. If the pressure on the inguinal area is tolerable, the hemipelvis on the affected side is then ‘lifted’ in the direction of the patient’s ipsilateral shoulder until pain reduces adequately from the point being palpated by the patient. This position is held for 30 seconds.
• The ‘lift’ should be introduced via the practitioner’s whole-body effort rather than by means of pushing with the contact hand, in order to minimize the potential sensitivity of the region.
• One author (LC) has found that introduction of a degree of lift toward the ceiling via the contact hand (sometimes involving support from the other hand) often produces a greater degree of pain reduction at the palpated point.
• Morrison described ‘multiple releases’ of tension in supporting soft tissues as well as a more balanced pelvic mechanism resulting from this method. The authors suggest that this method can be usefully applied to lower abdominal ‘tension’ as well as to pelvic imbalances. By removing the tension from highly stressed ligamentous and other soft tissues in the pelvis, some degree of rebalancing normalization occurs.
Method 2: strain-counterstrain
• The patient is supine and the most sensitive tender point is located on the cephalad aspect of the superior pubic ramus of the dysfunctional side. The most common site is just less than an inch (2 cm) lateral to the symphysis. (D’Ambrogio & Roth 1997).
• The patient (or the practitioner) localizes and presses that point to create a reference pain, which the patient values as ‘10’.
• The practitioner, standing on the dysfunctional side, flexes the patient’s hip and knee on that side to between 90° and 120°, stopping at the position which produces the greatest reduction in reported sensitivity in the tender point. Abduction and rotation are seldom needed.
• The position of ‘ease’ is held for 90 seconds before a slow return to neutral, which is followed by repalpation and assessment of the dysfunction.
Supine iliosacral dysfunction evaluation
These notes are designed to help make sense of the standing flexion test findings and to offer confirmation. Once an iliosacral dysfunction has been identified by virtue of a unilateral cephalad PSIS movement during the standing flexion test and/or during the stork test (see pp. 331–332), it is necessary to define precisely what type of restriction exists. The accuracy of these visual and palpation assessments depends to a large extent upon observation of landmarks and refers back to the results of the standing flexion and the Gillet (stork) tests, and depends on them to guide the practitioner as to which side is (most) dysfunctional.
Iliosacral dysfunction possibilities include:
Rotational dysfunctions
• The patient lies supine, legs flat on the table, and the practitioner approaches the table from the side that allows her dominant eye to be placed directly over the pelvis (see Box 2.6 regarding determination of dominant eye).
• The practitioner locates the inferior slopes of the two ASISs with her thumbs and views these contacts from directly above the pelvis with the dominant eye over the center line (bird’s eye view) (Fig. 11.27).
• Which ASIS is nearer the head and which nearer the feet? In other words, is there a possibility that one innominate has tilted posteriorly or the other anteriorly?
• The answer is determined by which ASIS is superior and which is inferior and by reference back to the result of the standing flexion test or the stork (Gillet) test (see pp. 331–332).
• The side of dysfunction as determined by the standing flexion test and/or the standing hip flexion test (Gillet’s stork test) defines which observed anterior landmark is taken into consideration (Figs 11.28, 11.29).
• If the ASIS appears inferior on the dysfunctional side (compared to its counterpart) it is assumed that the innominate has tilted anteriorly on the sacrum on that side.
• If, however, the ASIS appears superior to its counterpart on the dysfunctional side, then the ilium is assumed to have tilted posteriorly on the sacrum on that side.

Figure 11.27 Practitioner adopts position so that bird’s eye view is possible of palpated ASIS prominences
(reproduced with permission from Chaitow 2006).
Figure 11.28 The ASISs are level, suggesting no rotational dysfunction of the ilia
(reproduced with permission from Chaitow 2006).
Figure 11.29 The right ASIS is higher than the left and if the right thumb had been noted to move during the standing flexion test, this would suggest a posterior right innominate tilt. If the left thumb had moved it would suggest an anterior rotation of the left ilium
(reproduced with permission from Chaitow 2006).
Flare dysfunctions (see also Chapter 2 for supine postural assessment)
• While observing the ASISs, the relative positions of these landmarks are noted in relation to the mid-line of the patient’s abdomen by using either the linea alba or the umbilicus as a guide (see p. 339 regarding umbilicus deviations).
• Is one thumb closer to the umbilicus, or the linea alba, than the other?
• Is the ASIS on the side which is further from the umbilicus outflared or is the ASIS which is closer to the umbilicus indicative of that side being inflared? In other words, which side is dysfunctional and which normal? It is quite possible to have an inflare on one side and an outflare on the other.
• Is there approximately equal distance on both sides from the ASIS to the lateral aspect of the fleshy mass of gluteus medius? An inflared side will appear to have greater distance and an outflared side will appear to have less distance between the ASIS and the most lateral aspect of gluteus medius.
• The side on which the PSIS was observed to move superiorly during the flexion or stork test is the dysfunctional side.
• If the ASIS on that side is closer to the umbilicus it represents an inflare whereas if the ASIS is further from the umbilicus, it represents an outflare on that side and the other innominate is normal.
• Flare dysfunctions are usually treated prior to rotation dysfunctions.
Note: It is stressed that the MET iliosacral treatment methods described below should always be preceded by normalization (as far as possible) of soft tissue influences such as short, tight or weak musculature, including trigger point activity.
MET of iliac inflare (Fig. 11.30)
When performing the following steps, care should be taken not to use the powerful leverage available from the flexed and abducted leg; its own weight and gravity provide adequate leverage and the ‘release’ of tone achieved via isometric contractions will do the rest.
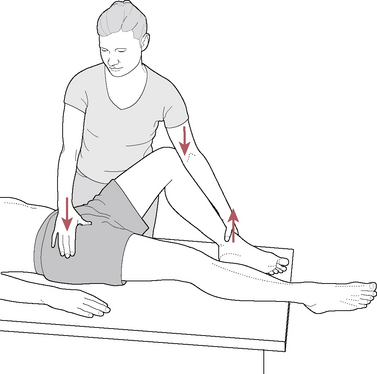
Figure 11.30 MET treatment of iliosacral inflare dysfunction on the left
(reproduced with permission from Chaitow 2006).
CAUTION: It is very easy to turn an inflare into an outflare by overenthusiastic use of force.
• The patient is supine with the ipsilateral hip flexed and abducted while full external rotation is introduced to the hip. The practitioner stands on the dysfunctional side, with her cephalad hand stabilizing the contralateral ASIS. The forearm of her caudad arm is lying along the medial surface of the lower leg with her elbow stabilizing the medial aspect of the patient’s knee. Her caudad hand grasps and holds his ipsilateral ankle, elevated slightly from the table.
• While holding his breath, the patient is asked to lightly adduct and internally rotate the hip against the resistance offered by the restraining arm for 10 seconds.
• On complete relaxation and exhalation, and with the pelvis held stable by the cephalad hand, the flexed leg is allowed to ease into greater abduction and external rotation to its next elastic barrier of resistance, if new ‘slack’ is now available.
• Process is repeated once, at which time the knee is slowly straightened while abduction and external rotation of the hip are maintained by the practitioner’s support.
• Leg is then returned to lie flat on the table in neutral position.
• The degree of flare should be reevaluated and any rotation then treated (see below).
MET treatment of iliac outflare (Fig. 11.31)
• The patient is supine and the practitioner is on the same side as the dysfunctional ilium. The practitioner’s supinated cephalad hand is placed under the patient’s buttocks with her finger tips hooked into the ipsilateral sacral sulcus.
• The shoulder of her caudal arm lies on the lateral aspect of the patient’s flexed knee. That arm wraps over his leg so that her forearm rests along his medial calf/shin area as her hand grasps the medial aspect of his ipsilateral heel.
• With the hip on the treated side fully flexed, adducted and internally rotated, the patient is asked to abduct the hip against resistance offered by the practitioner’s ‘wrapped’ arm, while using up to 50% of his strength. The resistance is maintained for 10 seconds while the patient is holding his breath.
• Following this and complete relaxation, slack is taken out (through adduction and internal rotation) and the exercise is repeated once more.
• As the leg is taken into greater adduction and internal rotation, to take advantage of the release of tone following the isometric contraction, the practitioner’s fingers in the sacral sulcus exert a light but steady traction toward the practitioner, effectively guiding the ilium into a more inflared position.
• After the final contraction, adduction and internal rotation are maintained as the leg is slowly returned to the table to its original neutral position.
• The evaluation for flare dysfunction is then repeated and if relative normality has been restored, any rotational dysfunction is then treated, as per the methods described below.
MET of anterior innominate tilt: prone position (Fig. 11.32)
• The patient is prone and positioned so that the affected leg and hip are flexed and hang over the edge of the table.
• The practitioner stands at lower thigh level on the side to be treated, while guarding against the person falling off the side of the table. The practitioner should not leave the person ‘hanging’ for any reason.
• The tableside hand stabilizes the sacral area, palpating the SI joint, while the other hand supports the flexed knee and, using the knee as a handle on the thigh, guides the hip into greater flexion, thereby inducing posterior innominate tilt, until the restriction barrier is sensed:
• The patient is asked to inhale, to hold the breath and to attempt to move the hip into extension for 10 seconds using no more than 20% of available strength.
• On releasing the breath and the effort, and upon complete relaxation and exhalation, the leg/innominate is guided to its new barrier as hip flexion is increased to take out available slack.
• Subsequent contractions can involve different directions of effort (‘try to push your knee sideways’ or ‘try to move your knee toward your shoulder’, etc.) in order to bring into operation a variety of muscular factors to encourage release of the joint.*

Figure 11.32 MET treatment of an anterior iliosacral restriction
(reproduced with permission from Chaitow 2006).
The standing flexion test (p. 331) should be performed again to establish whether the joint is now free.
MET of anterior innominate tilt: supine position (Fig. 11.33)
• The procedure should only be performed if that particular innominate has been determined to be anteriorly tilted. In a bilateral anteriorly tilted pelvis, both sides should be treated but this procedure should not be performed on an innominate if it is determined to be posteriorly tilted or if it lies in neutral position.
• The procedure should not be performed (or might possibly be performed with extreme caution) if that leg has had hip replacement, or if serious disc herniations, disc fusion or other severe conditions exist, unless the attending physician approves its use.
• It is essential to normalize muscles attaching to the ilia and sacrum in conjunction with this procedure.
• Prior to the procedure and also in between the steps, the apparent functional leg length can be checked by observing the relationship of the medial malleoli. With each successful ‘posterior tilt’ that treated leg should appear ‘shorter’ than before the movement, as judged by its shortened relationship to the opposite malleolus. The treatment should conclude with the malleoli level with each other, even if neutral position of the pelvis has not been achieved.
• The patient is supine with the ipsilateral knee bent and the hip fully flexed. The contralateral leg is lying on the table. Note: The knee on the contralateral side may be bent with the foot flat on the table during the procedure if lower back discomfort exists.
• The practitioner is standing at the level of the hip on the affected side with the thumb of her cephalad hand placed on the inferior slope of the ASIS. Her caudal arm reaches laterally around the hip and under the affected buttock so that her fingers cup the posterior aspect of the ipsilateral ischium, with her thumb tucked into the palm of the hand to avoid intrusion into the genital region. The patient may need to raise that hip slightly in order for the practitioner to more easily place her hand on the ischial tuberosity.
• The patient will assist the procedure by grasping over the ipsilateral knee or under the knee onto the posterior thigh.
• As the patient pulls his knee toward his chest, the practitioner should simultaneously press the ASIS cephalad and pull the ischium toward the ceiling while attempting to posteriorly rotate the innominate to the first barrier of resistance.
• The straight contralateral leg, which is lying flat on the table, will begin to lift at the end range of motion of the treated side and, as it does, the patient attempts to straighten the leg being treated while applying his own resistance (at about 20–30% effort) and while holding his breath. This position is maintained for 10 seconds.
• The practitioner maintains a passive posterior range of motion of the innominate with the patient’s accompanying activation of the adductor magnus and gluteus maximus. A subtle posterior tilt of the innominate may be noticed.
• Upon complete relaxation and restoration of normal breath, the practitioner assists the innominate into a posterior range of motion to the next barrier of resistance.
• The procedure is repeated once more and then performed twice on the contralateral side if anterior tilt was also noted there.
• This entire bilateral procedure can be repeated several times until neutral position is achieved or no further improvement is seen.
• Other variations of this supine procedure exist, including those which use the practitioner’s shoulder to resist the hip extension or which have the leg straight, employing a rope for resistance. While these variations are useful the method described is preferred since it avoids all strain on the practitioner’s body and allows her to focus totally on what is being felt in the motion of the innominate.
MET of posterior innominate tilt: prone position (Fig. 11.34)
• The patient is prone and the practitioner stands on the side opposite the dysfunctional iliosacral joint, at thigh level, facing cephalad. This procedure could be performed from the ipsilateral side but contralateral is preferable because of the angle of force in relation to the SI joint plane.
• The caudad hand supports the anterior aspect of the patient’s bent knee while the other hand rests on the PSIS of the affected side to evaluate bind in the SI joint.
• The hip of the affected side is hyperextended until free movement ceases, as evidenced by the following observations:
• While the practitioner maintains the joint at its restriction barrier, the patient is asked, with no more than 20% of strength, to flex the hip against resistance for 10 seconds while holding his breath. After cessation of the effort with complete relaxation, and with release of the breath and on exhalation, the hip is extended further to its new barrier.
• No force is used at all; the movement after the contraction simply takes advantage of whatever slack is then available.
• Variations in the direction of the contraction are sometimes useful if no appreciable gain is achieved using hip and knee flexion against resistance; abduction or adduction or even attempted extension may prove beneficial.
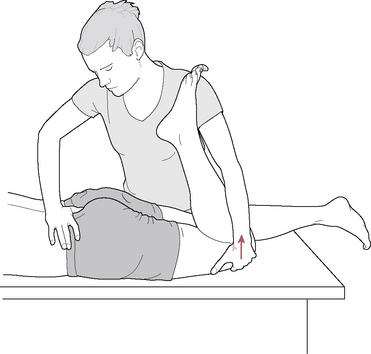
Figure 11.34 MET treatment of posterior innominate tilt
(reproduced with permission from Chaitow 2006).
The standing flexion test should be performed again to establish whether iliosacral movement is now free, once a sense of ‘release’ has been noted following one of the contractions.
Supine active straight leg raising test
(See Figures 11.35ABCD for both supine and prone versions of this test.)
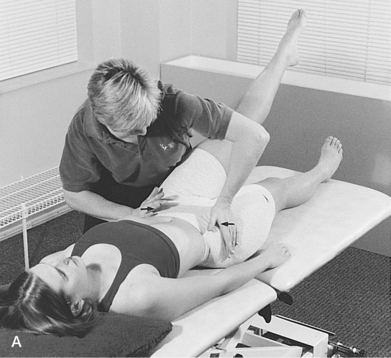
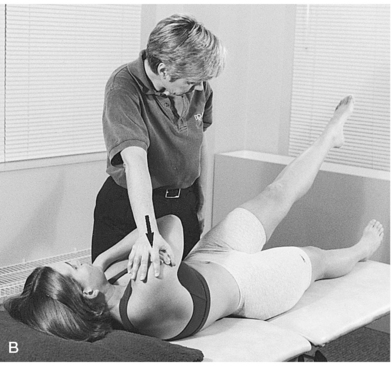


Figure 11.35 Supine active straight leg raise test. A: form closure; B: force closure; Prone active straight leg raise test. C: with form closure augmented. D: with force closure augmented
(adapted from Lee 1999).
Active straight leg raising tests enhance information deriving from the seated flexion test described earlier.
• The patient is supine and is asked to raise one leg.
• If there is evidence of compensating rotation of the pelvis toward the side of the raised leg, and/or if pain or difficulty in raising the leg is reported, during performance of the movement, dysfunction is confirmed.
• The same leg should then be raised as the practitioner imparts compressive medially directed force across the pelvis with a hand on the lateral aspect of each innominate at the level of the ASIS (this augments form closure of the SI joint). If form closure as applied by the practitioner enhances the ability to easily raise the leg this suggests that structural factors within the joint may require externally enhanced support, such as a supporting belt (See Fig. 11.35A).
• To enhance force closure, the same leg is raised with the patient slightly flexing and rotating the trunk toward the side being tested, against the practitioner’s resistance, which is applied to the contralateral shoulder. This activates oblique muscular forces and force-closes the ipsilateral SI joint (which is being assessed). If initial leg raising suggests SI dysfunction and this is reduced by means of force closure, the prognosis is good if the patient engages in appropriate rehabilitation exercise (Lee 1999). A similar prone force closure assessment should also be performed (see below) (See Fig. 11.35B).