Chapter 10 The lumbar spine
The spine functions to support the upright body as well as any load it carries, to allow movement and to protect the central nervous system (cord) and the nerve roots which emerge from it. The vertebral column is designed to simultaneously accomplish the seemingly contradictory tasks of providing stability so that upright posture can be maintained while, at the same time, providing plasticity for an extremely wide range of movements.
Spinal design involves relatively small structures that are superimposed upon one another, held together (and upright) by the tensile forces of the musculature. Excessive movement of the spine’s many joints is restrained by an array of ligaments, the intervertebral discs and, to a degree, by the arrangement of the articular surfaces. Discussions regarding the spinal column as a whole, the intervertebral discs and functional curvatures of the spine, as well as specific details of the cervical and thoracic spinal regions, are offered in Volume 1 of this text. In this volume, details of the lumbar spine, sacrum and pelvis are presented which usefully combine with discussions from the companion text to offer a more complete picture of spinal structure and associated spinal dysfunctions.
Functions of the lumbar spine
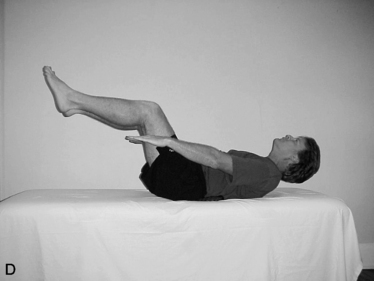
Movements of the lumbar vertebrae include flexion, extension, some bilateral sideflexion, a small amount of axial rotation, distraction, compression, anterior/posterior translation and medial/lateral translation (Fig. 10.1).
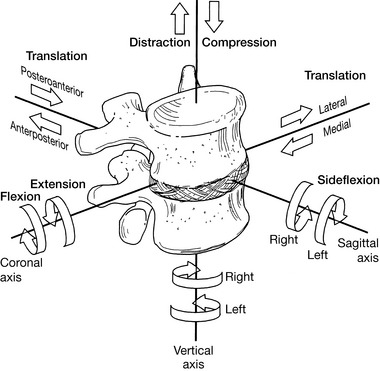
Figure 10.1 In mechanical terms, there is the potential for 12 degrees of motion of the lumbar vertebrae
(reproduced with permission from Lee (2004)).
Coupling
Under normal conditions these spinal movements are usually combined (coupling); for example, the combination of sagittal rotation and translation occurring during flexion and extension (Bogduk 2005). Rasch & Burke (1978) created a generally accepted, extremely simple definition of coupling: ‘Lateral flexion of the spine is always accompanied by some rotation.’
It is rare for a single movement to take place rather than these common combinations, that appear to be dependent on the structural features that regulate and constrain them, notably the spine itself, the intervertebral discs, the facet joints, the ligaments and the myofascial network, which both supports and moves all the other structures (Waddell 1998). Zhao et al (2008) used stereophotogrammetry techniques to record movements of the spine in 3D, during the gait cycle. They observed that the lateral and transverse rotations of the lumbar segments have the largest range of motion in the spine, reinforcing the notion that this region plays a crucial role in modulating upper body positioning, while maintaining body stability. All the subjects tested demonstrated that adjacent regions of the thoracic, lumbar spines and pelvic segments, exhibited coupled rotations during gait – in both the transverse and frontal planes. However, these patterns of rotation varied considerably from one subject to the next – indicating that they are individual, and not universally predictable. It is suggested that these individual patterns may be due to variable muscular features, which differ significantly between individuals.
Dysfunction, by definition, always involves deviation from normal function. It is also axiomatic that deviations from the norm require awareness of normality as a base, so that the degree of dysfunction can be identified, compared and monitored. How short, strong, weak or restricted a structure is (as examples) requires appraisal of the degree of functional efficiency, compared with what is regarded as normal. In other words, dysfunction is always relative to a commonly held perception of what is ‘normal’. ‘Normal’ (how tight, strong, weak, etc. something is) itself requires a reasonable range, a ‘zone’ of normality that is often genetically determined and/or associated with particular body types and shapes, in order to allow for the vast degree of individuality which exists in pain-free, structurally sound, functional humans.
In many instances, structural modifications associated with functional changes will also be visibly or palpably identifiable. Of course, this structure-function continuum also applies to the normal physiological functions of structures, based on the intrinsic architectural design of the area. For example, in the thoracic spine functional movements (such as extension) are limited by the structural features of the vertebrae, which effectively prevent backward bending. Sideflexion as well as flexion potential in the thoracic spine is also limited by the inter- and supraspinal ligaments and by the ribs, especially in the upper thoracic region. The flexion potential of thoracic vertebrae, therefore, exists mainly in the lower thoracic segments, in which rib fixation is less of a factor. Rotation potential for the thoracic region is freer, however, with the axis of rotation being in the mid-thoracic area. As Lewit (1985) explains:
Function and its disturbances are of particular significance at the thoracolumbar junction. This may be because in this region movement changes from one type to another within a single segment, as can be deduced from the shape of the apophyseal joints: on a single vertebrae the upper articular processes may be in the coronal plane and the lower mostly in the sagittal plane. Whereas in the lowest thoracic segments axial rotation is the most prominent function, it suddenly ceases between T12 and L1.
Lumbar vertebral structure (Bogduk 2005, Gray’s anatomy 2005, Lee 2004, Ward 1997)
A healthy representative lumbar vertebra consists of a number of distinctive parts (Fig. 10.2).
• Vertebral body, which is level along its superior and inferior surfaces, with slightly concave anterior and lateral surfaces. The body is constructed of cancellous bone (structured for strength and lightness) as a honeycomb of struts or rods, known as trabeculae, running vertically as well as transversely. Additional hydraulic strength is created within the vertebral body by the presence of blood. Waddell (1998) elaborates: ‘We tend to think of bone as rigid but that is not strictly true. Vertebrae are six times stiffer and three times thicker than the discs and only allow half the deformation, but they do have some elasticity’. Bogduk (2005) paints a vivid picture of the interior of the vertebral body: ‘When filled with blood, the trabeculated cavity of the vertebral body appears like a sponge, and for this reason it is sometimes referred to as the vertebral spongiosa’.
• The sponge-like honeycomb of the body is surrounded by a raised rim of smoother bone known as the ring apophysis.
• From the posterior surface of the vertebral body two strong projections emerge, the pedicles, which are part of the neural arch that surrounds and protects the spinal cord.
• The remainder of this neural arch comprises the laminae, which project from each pedicle before curving toward the mid-line where they merge into each other and become the spinous process.
• The function of the hollow, thick-walled, cylindrical pedicles is to transmit bending and tension forces between the potentially highly mobile body of the vertebra (anterior element) and the posterior element, with its muscular attachments and projecting leverage arms (transverse, spinous processes, etc.).
• Bogduk (2005) notes that it is significant that all the muscles acting directly on the lumbar vertebrae pull inferiorly obliging forces to be transmitted to the vertebral body through the pedicles.
• Projecting laterally from the junction of the pedicles and the laminae are the transverse processes and projecting from the inferior surface of each transverse process, close to the pedicle, is the accessory process. Superior and medial to the accessory process, separated from it by a notch, lies the mamillary (‘breast-like’) process.
• Projecting posteriorly from the junction of the laminae is the spinous process. The laminae seem to act as stabilizing structures that absorb or transfer forces imposed on the spinous and inferior articular processes.
• Between the superior and inferior articular processes lies the pars interarticularis, that part of the laminae which copes with the transfer of horizontally and vertically oriented stresses. If this is not adequate to the stresses imposed on it, stress fractures can occur.
• The transverse, spinous and various accessory processes all provide anchorage for muscular attachments. The larger and longer the process involved, the greater the degree of leverage potential the attaching muscle will have on the posterior elements of the spine. Some psoas fibers and the crura of the diaphragm are the only significant muscular attachments to the bodies of the vertebrae. These are not thought to exert any primary action on the segments to which they attach by some (Bogduk 2005) while others (Kapandji 1974, Platzer 2004, Rothstein et al 1991, Travell & Simons 1992) vary in opinion as to lumbar spinal movement (see discussion of psoas on p. 287).
• Inferior and lateral to the laminae are specialized hook-like structures known as the inferior articular processes, which articulate with the superior articular processes of the vertebra below, which project superiorly from the junction of the pedicles and the laminae. The synovial joints thus formed provide an excellent locking mechanism, which helps to prevent excessive rotation, as well as anterior translation (glide) movement of one segment on another.
• Smooth surfaces, covered with cartilage, exist on the medial surfaces of the two superior articular processes, as well as on the lateral surfaces of the two inferior articular processes. These are the articular facets of these articular processes, which make up the zygapophysial (‘facet’) joints.
• The architectural design of the vertebral bodies is such that they can slide in all directions in relation to each other’s endplate surfaces. As Bogduk (2005) expresses it: ‘There are no hooks, bumps or ridges on the vertebral bodies that prevent gliding or twisting movements between them. Lacking such features, the vertebral bodies are totally dependent on other structures for stability in the horizontal plane, and foremost among these are the posterior elements of the vertebrae’– namely the laminae, the articular and spinous processes and, to a lesser degree, the annular fibers of the disc and the ligaments of each segment.
• The posterior elements collectively comprise an uneven mass of bone characterized by a variety of projections which manage the multiple forces imposed on the vertebrae.
• Some key characteristics of the five lumbar vertebrae include the following (Bogduk 2005, Gray’s anatomy 2005, Lee 2004, Ward 1997).
• Lumbar vertebrae are relatively large in size compared with thoracic vertebrae.
• The vertebral body of L5 is wide transversely and vertically deep anteriorly (so contributing to the sacrovertebral angle).
• There is an absence of costal facets and transverse foramina, which are present in the vertebrae above the lumbar region.
• Transverse processes protrude virtually horizontally.
• The superior articular facets are angled posteromedially
• The inferior articular facets are angled anterolaterally
• The 5th lumbar vertebrae, which is itself very large, has ‘more substantial’ transverse processes (Gray’s anatomy 2005), compared with other lumbar vertebrae in which transverse processes are long and thin.
• The lumbar transverse processes increase in length from the first to the third and then shorten.
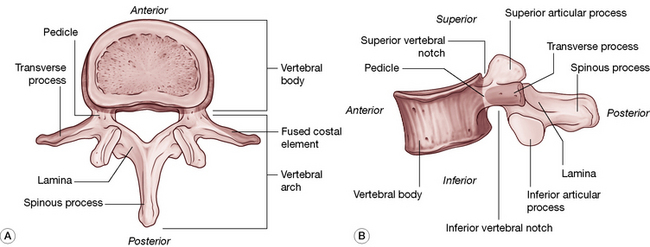
Figure 10.2 The parts of a typical lumbar vertebra. A: Superior view. B: Lateral view.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
The intervertebral disc joint (see also Volume 1, Figs 11.2 & 11.5)
• The three features of the intervertebral disc are the peripheral annulus fibrosus, the core nucleus pulposus and the vertebral endplates that lie superiorly and inferiorly and which attach the disc to the vertebrae above and below. Bogduk (2005) suggests that the endplates are regarded as part of the intervertebral disc rather than part of the vertebral body, since they are strongly bound to the disc and only weakly attached to the vertebral body.
• The annulus and the nucleus pulposus meld and merge into one another rather than having distinct boundaries.
• The annulus fibrosus is a superbly configured collagen construction, made up of 10–20 spiral and inter-digitated layers, the lamellae, capable of restraining movements and stabilizing the joint (Cailliet 1995) (see Volume 1, Fig. 11.2). Each fiber is a trihelix chain of numerous amino acids, which gives it an element of elasticity, making each annulus fibrosus, in all but name, a ligamentous structure. As Bogduk (2005) puts it, ‘The anuli fibrosi can be construed as the principal ligaments of the vertebral bodies. [It] functions as a ligament in resisting distraction, bending, sliding and twisting movements of the intervertebral joint … It is only during weightbearing that it functions in concert with the nucleus pulposus’.
• The annular fibers course on a diagonal to connect adjacent vertebral endplates. Each layer of fibers lies in the opposite direction to the previous layer so that when one layer is stretched by rotation or shearing forces, the adjacent layer is relaxed (see Volume 1, Fig. 11.2).
• The disc fibers may be stretched to their physiological length and will recoil when the force is released. If stretched beyond their physiological length, the amino acid chains may be damaged and will no longer recoil.
• The vertebral endplates comprise a layer of cartilage that covers the superior or inferior surface of the body of the vertebra and is encircled by the ring apophysis. The endplate attaches the body to the disc itself, completely covering the nucleus pulposus and, to a large extent, the annulus. The attachment of the endplate to the vertebral body is far weaker than is its attachment to the disc.
• The nucleus, when in a young and healthy state, is an incompressible but deformable paste-like, semi-fluid proteoglycan gel (approximately 80% of which is water) which is designed to conduct and tolerate pressure, relating mainly to weight bearing. With age it dessicates and loses many of its valuable protective properties.
• Though the discs have a vascular supply in the early stages of life, by the third decade the disc is avascular and nutrition to the disc is thereafter in part supplied through imbibition, where alternating compression and relaxation create a sponge-like induction of fluids.
• As long as the container remains elastic, the gel cannot be compressed but can merely deform in response to any external pressure applied to it.
• Since the nucleus conforms to the laws of fluids under pressure, when the disc is at rest, external pressure applied to the disc will be transmitted in all directions, according to Pascal’s law. When external forces compress the disc, the nucleus deforms and the annular fibers, while remaining taut, bulge.
• While the design offers optimal conditions of hydraulic support as well as numerous combinations of movements, postural distortions brought on by overuse, strain and trauma can lead to degenerative changes in the disc, usually accompanied by muscular dysfunction and often associated with chronic pain.
• The permeability of the endplates and the disc is enhanced by exercise and lessens with age.
• There is an approximately 20% reduction in disc volume and height through the day, due to gravity and activity. In health, the disc volume is restored after rest (lying down) through osmotic forces (imbibition).
The zygapophysial (facet) joints
• The zygapophysial (facet) joints (see discussion on p. 221 as to terminology) carry approximately a quarter of the weight of the trunk under normal conditions, although Waddell (1998) reports: ‘This may rise to 70% when the discs narrow with degenerative changes’.
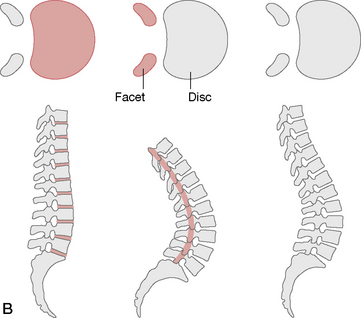
• The oval-shaped facet joints provide stability and facilitate movements such as rotation and translation (shunt, glide, shift) and are exposed to shearing and compression forces (Figs 10.3, 10.4). Figure 10.3 depicts moderate differences between the cervical, thoracic and lumbar joints, which ultimately affects the range and degree of motion of each vertebra as well as that of the spinal region.
• The degree to which a pair of facet joints achieves its influence on rotation and displacement depends on the relative curved or flat nature of the surfaces involved (Fig. 10.5).
• The articular surface of each facet joint is cartilaginous and is surrounded on its dorsal, superior and inferior margins by a collagen-based capsule. Anteriorly, the ligamentum flavum borders the facet joint capsule.
• The facet joint structure houses fat as well as meniscoid structures, composed of connective tissue, adipose tissue and fibroadipose tissue. These are interpreted (there is no consensus – Bogduk 2005) as acting as shock absorbers or protective surfaces.
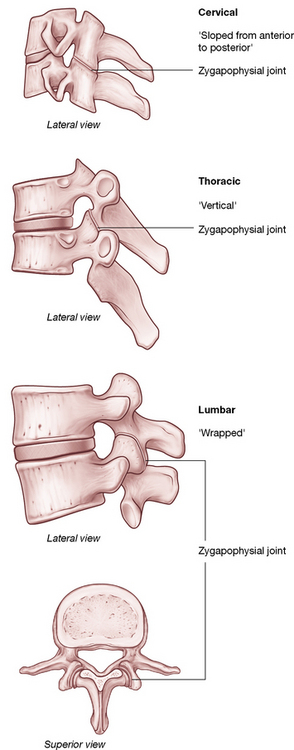
Figure 10.3 Significant differences exist between cervical, thoracic and lumbar vertebrae. Note the differences in angulation of the zygapophysial joints, which determine the type of movements available at each segment.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
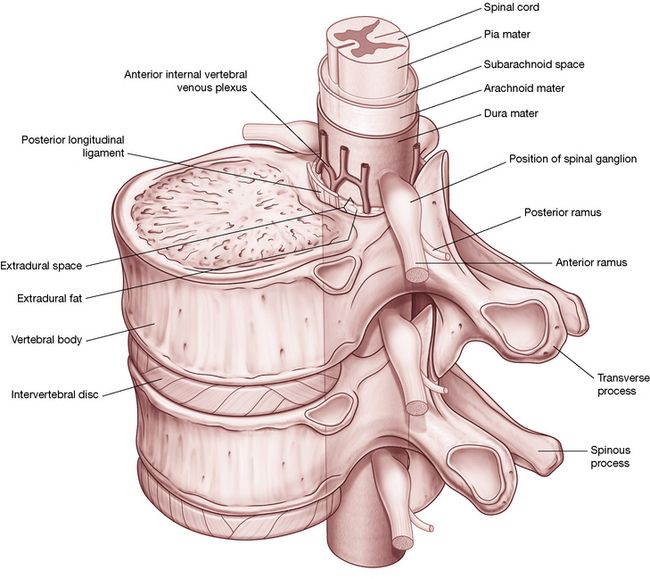
Figure 10.4 If an intervertebral joint is compressed (1), the inferior articular processes of the upper vertebra impact the laminae below (2), allowing weight to be transmitted through the inferior articular processes (3). Note the almost vertical angle of the facet joint, a factor of particular importance in application of SNAGs, as described in Box 10.3.
Box 10.3 Sustained natural apophyseal glides (snags) for the lumbar spine
Note: This text discusses multidisciplinary approaches to treatment protocols. The practitioner must determine which techniques lie within the scope of her professional license and skills and is cautioned to practice within that scope.
As explained in Volume 1, SNAGs relates to the painless gliding (or translating) of the superior of a pair of vertebrae that display any pain or restriction on movement. If that dysfunction involves the facets, the patient should be able to perform the previously restricted or painful movement during the ‘glide’ and the after-effect should be a removal or reduction of the previous symptoms. The process, known as SNAGs, involves the spinous process or articular pillar of the superior vertebra of a restricted segment being held in an anterior translation direction that follows the angle of the facet joint, while the patient slowly performs the previously restricted or painful movement.
If the pain is eliminated and/or the range increased during the procedure, this process is then repeated several times. When SNAGs ‘works’, this process will frequently completely release a previously blocked facet restriction resulting in pain-free and increased range of motion.
If no improvement is noted during application of SNAGs, or if the pain is increased during its application, then the condition is not suitable for this approach and other tactics should be used.
For SNAGs to be applicable, the presentation of the patient should include a particular movement that is usually painful or restricted. This approach is not suitable for conditions where the pain is noted at rest or where it is not exacerbated by movement. If the painful/restricted movement occurs when standing, the treatment should be applied in standing. Likewise, if pain and/or restriction only appears in the seated position, the treatment should be with the patient seated.
Mulligan (1999), who developed the SNAGs approach, writes the following in discussing the various theories on the origin of low back pain.
We read of facet theories, disc theories, muscle theories and so on. …up till now one thing has always puzzled me about the disc theory. This being the fact that a simple facet manipulation can sometimes bring great relief to the patient that we ‘know’ has a minor disc lesion.
Mulligan goes on to describe his view that, under normal circumstances, as the spine flexes and the ventral aspects of the vertebral bodies approximate, the disc content shifts posteriorly and in order to accommodate this the facet joints have to be sufficiently mobile. If there exists uni- or bilateral facet blockage or restriction, the vertebral bodies will be unable to separate dorsally and the posterior bulge of the disc may produce symptoms. ‘What I am implying is that most back pain comes from the disc which is producing symptoms due in no small measure to the facets.’
Whether Mulligan’s theory is correct or not is largely irrelevant. It offers a perspective and a ‘story line’ that makes some physiological sense. This allows the practitioner to experiment with a method that is safe, painless and superbly efficient, when it works! It should be kept in mind that much that is done manually (and much that is done in mainstream medicine) has no proof as to why and how particular methods are efficient therapeutically. If a method is shown to be effective and safe, then explanations may have to wait. Were this not so, high-velocity thrust methods, ischemic compression methods or almost all manual therapy techniques would not be in beneficial use. This is not to say that understanding how a method achieves its results is unimportant. Rather, if something is safe and helpful, and there is a reasonable facsimile of a modus operandi, it is fine to incorporate it into clinical use, while others struggle to explain its mechanisms.
SNAGs application method
Note: The segment to be treated using SNAGs, which is restricted or painful on movement, should previously have been identified by motion palpation and/or direct manual palpation. Also note that the application of SNAGs in the lumbar region calls for a stabilization ‘strap’/belt which links the practitioner and the patient (see Fig. 10.15). Straps of this sort (seatbelt width and materials) are widely used in physical and manual therapy and can be obtained from suppliers to the physical therapy profession.
The patient is seated on a treatment table with legs over the side (Fig. 10.15A) or stands alongside the table (Fig. 10.15B). If seated, a strap/belt is placed around the patient’s lower abdomen, below the anterior iliac spines, and loops around the practitioner’s upper thighs (ideally below the hip joints) (Fig. 10.15A). If the patient is standing a similar strap connection should be established (see Fig. 10.15B) and the patient should ensure that he maintains the knees in slight flexion throughout the procedure in order to minimize hamstring or neural tension influences.
The practitioner makes contact with the ulnar border of her dominant hand, slightly inferior to the spinous process of the superior of the two vertebrae in the segment to be treated. The practitioner’s other hand should be placed on the treatment table to assist in maintaining stability.
The patient should be asked to perform the movement that is either restricted or painful (in this example, flexion). Once the first sign of pain or restriction is noted, the patient should be asked to ease very slightly back from this barrier/point. (‘I would like you to bend forward slowly until you feel the very first sign of pain, or where you feel it difficult to bend further. Once you have identified that degree of bend, ease slightly back.’) The practitioner should now apply a light degree of pressure onto the spinous process in the direction of the facet plane, painlessly easing (translating, gliding) the superior vertebra superoanteriorly. The patient’s stability is maintained by applying backward pressure via the strap looping around both the practitioner and the patient.
While holding this translation the patient should be asked to perform the previously painful or limited movement and if flexion (in this example) is now further, easier, painless, the position of flexion should be held for a few seconds before a slow return to the start position with the translation force maintained throughout, until the start position has been reached.
If the maneuver was successful the process is repeated at least twice more. If there was no gain in range or reduction of pain, the same procedure is attempted again with an altered angle of translation or on a different segment. Note: When translation pressure is applied along the facet plane at the correct angle there will be a slight sense of ‘give’ or yielding, whereas when the angle is incorrect a blocked, hard feel will be noted.
Mulligan (1999) suggests that at times the ulnar border contact of the treatment hand should be made unilaterally, rather than centrally as described above.
If the central SNAG is not helpful a unilateral glide should be tried… in the case of an L4/5 segmental lesion…place the ulnar border of your right hand (just distal to the pisiform) under the transverse process of L4 on the right, and as the patient flexes push along the facet plane. If unsuccessful try a unilateral SNAG on the opposite side.
Mulligan reports that over time he has gradually come to use the unilateral rather than the central SNAG method more commonly.
When treating the lumbosacral segment (L5 on the sacrum) Mulligan (1999) suggests:
As with the cervical spine [see Volume 1] one thumb reinforces the other, which is placed over the superior facet. The thumbs glide the superior L5 facet up on the sacral facet as flexion takes place. NB: it is impossible to use your thumbs above the lumbosacral segment as the inferior facet projects posteriorly further than its partner making correct thumb placement impossible.
These ‘mobilization with movement’ methods are not considered to be manipulation of joints and are unlikely to infringe most licensing guidelines. The area is being held in a direction that approximates its normal movement and the patient performs the movement, which, if painless, allows the facet restriction to normalize. The authors consider this approach to be an extension of positional release (PRT) methods and active joint range of motion. However, if the practitioner deems this to be outside her scope of practice, adherence to individual licensing guidelines is advised.
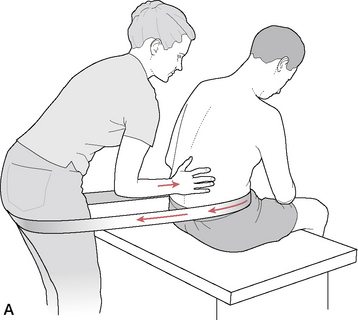
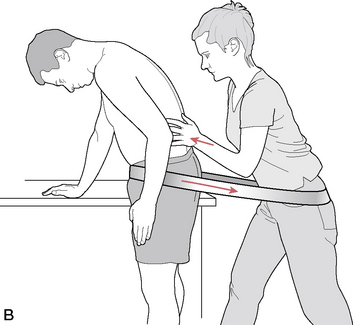
Figure 10.15 A: SNAGs for lumbar flexion restriction, patient seated. B: SNAGs for lumbar flexion restriction, patient standing
(adapted from Mulligan (1999)).
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
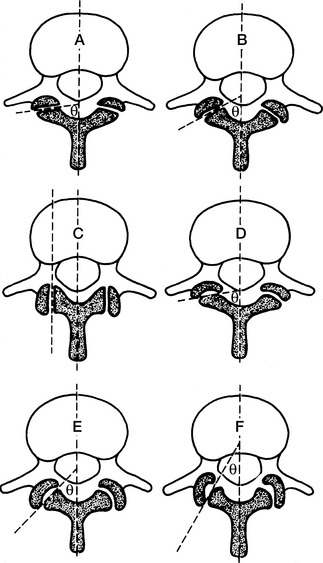
Figure 10.5 The variations of orientation and curvature of the lumbar zygapophysial joint. A: Flat joints orientated close to 90° to the sagittal plane. B: Flat joints orientated at 60° to the sagittal plane. C: Flat joints orientated parallel (0°) to the sagittal plane. D: Slightly curved joints with an average orientation close to 90° to the sagittal plane. E: ‘C’-shaped joints orientated at 45° to the sagittal plane. F: ‘J’-shaped joints orientated at 30° to the sagittal plane
(reproduced with permission from Bogduk (1997)).
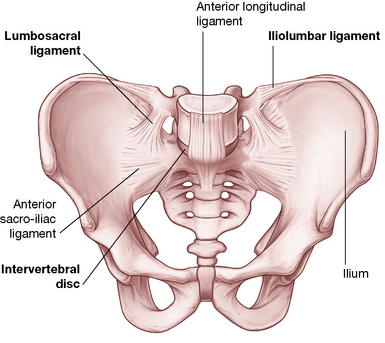
Ligaments
• A major function of viscoelastic structures such as ligaments is to establish limits to movement while providing stability.
• Ligaments are also sensory organs and have significant input to sensation and reflexive/synergistic activation of muscles. In some joints, such as the intervertebral joints of the spine, the role of the muscles as restraints is amplified (Solomonow 2009).
• The two major ligaments of the spine are the extremely powerful anterior and posterior longitudinal ligaments.
• The anterior longitudinal ligament extends from the sacrum to the cervical spine, with some fibers extending from one segment to the next and others extending for up to five segments.
• The attachment of the fibers of the anterior longitudinal ligament is into bone, mainly the anterior margin of the lumbar vertebral bodies and also, via collagen fibers, to the concave anterior surface of the bodies.
• The anterior longitudinal ligament is distinct from the annulus fibrosus, which attaches mainly to the vertebral endplates. It also merges with the crura of the diaphragm on the anterior surfaces of (at least) the first three lumbar vertebrae.
• Bogduk (2005) suggests: ‘… detailed examination of the crura and their attachments suggests that many of the tendinous fibers of the crura [of the diaphragm] are prolonged caudally beyond the upper three lumbar vertebrae… [and that]… these tendons constitute much of what has otherwise been interpreted as the lumbar anterior longitudinal ligament. Thus it may be that [this] is, to a greater or lesser extent, not strictly a ligament but more a prolonged tendon attachment’.
• The posterior longitudinal ligament contains fibers of different lengths, some of which span two discs while others span up to five discs, attaching from the superior margin of one vertebrae to insert into bone on the inferior margin several segments above. As with the anterior longitudinal ligament, the posterior one protects against undue separation forces and offers protection to the deeper structures.
• As indicated previously, the annuli fibrosi should also be regarded as ligamentous, due to their task of connecting adjacent vertebrae and restricting their excessive movements. Since the annulus fibrosus resists vertical distraction and other movements of the intervertebral joint, it is in effect acting as a ligament during all spinal movements, as well as offering structural protection to the nucleus.
• The ligamentum flavum, the most elastic of the spinal ligaments, connects the laminae of one vertebra to the laminae of the vertebra below it, while laterally it forms the anterior capsule of the facet joint. The precise purpose of the elastic nature of this ligament remains to be established but Bogduk (2005) points out that its location near the neural structures is likely associated with its high degree of elastic properties. He notes that were it more collagenous in nature, it would buckle upon relaxation and could encroach upon neural structures. With its higher elastic properties, it will simply retract to its normal thickness without buckling, thereby reducing the likelihood of neural compression (Fig. 10.6).
• The largely collagen (i.e. inelastic) based interspinous ligaments attach neighboring spinous processes to each other. There are ventral, middle and dorsal aspects to the ligament, with the latter merging to a great extent with the supraspinous ligament (Fig. 10.7).
• The supraspinous ligament attaches to and joins adjacent spinous processes, crossing the interspinous space. The reality of its claim to be a ligament is challenged, since much of it comprises tendinous fibers that derive from the thoracolumbar fascia and back muscles, such as the multifidi and the aponeurosis of longissimus thoracis.
• The iliolumbar ligaments occur bilaterally and link the transverse processes of L5 to the ilium, preventing anterior drift of L5 on the sacrum. The iliolumbar ligaments, which are apparently not present in infants where the tissue is muscular, gradually become ligamentous during adult life and later in life degenerate into fatty tissue. Parts of the superior aspects of the iliolumbar ligament arise from fascia surrounding quadratus lumborum (Thompson 2001). See further discussion of this ligament on p. 220 (Fig. 10.8).
• The intertransverse ligaments comprise sheets of connective tissue that extend from one transverse process to the next. Bogduk (2005) notes that they are more membranous than ligamentous, fulfilling a role of separating and defining particular prevertebral compartments that divide the anterior and posterior lumbar musculature.
• Approximately 50% of individuals have transforaminal ligaments, which span various aspects of the intervertebral foramina. As with the intertransverse ligaments, these are more fascial than ligamentous.
• The so-called ‘mamillo-accessory’ ligament is a tendon-like collagen structure, running from the mamillary process to the ipsilateral accessory process. Thus, because it links parts of the same bone, it is not a true ligament. It frequently ossifies in later life with no apparent negative effects.
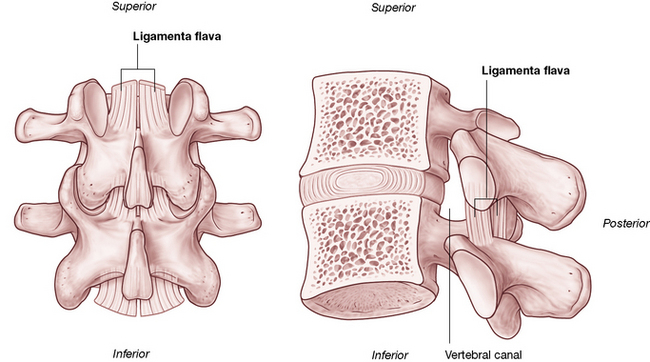
Figure 10.6 The ligamentum flavum. A: Posterior view. B: Lateral review. (note proximity to the spinal canal.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
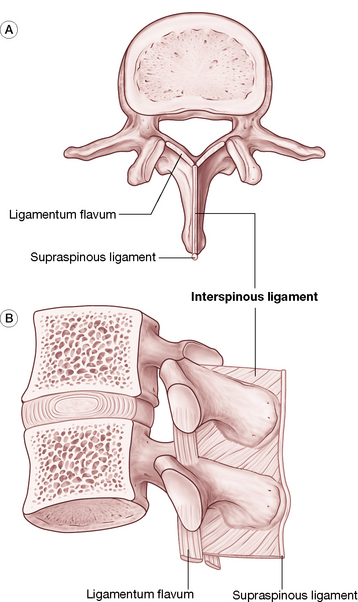
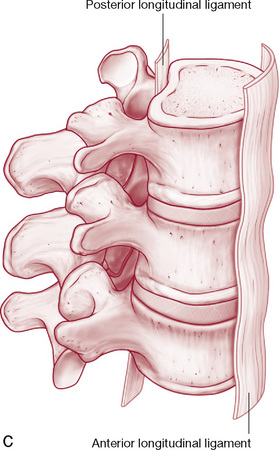
Figure 10.7 Various ligaments of the lumbar spine ligaments. Relationship of supraspinous and interspinous ligaments with ligamentum flavum viewed from (A) above and (B) laterally. (C) Anterior longitudinal ligament and posterior longitudinal ligament.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Additional notes on associated spinal structures
Lumbar biomechanics are discussed at length by Bogduk (2005) and are well illustrated by Kapandji (1974). The biomechanics of the cervical region and thoracic region, as well as the structure of the disc components, are discussed at length in Volume 1 of this text. Some points of particular interest to the lumbar region are listed here.
• It is virtually automatic for sidebending of a vertebral segment to be accompanied by rotation and, in the lumbar spine, this is primarily (but not always) to the opposite side (type 1) (Zhao et al 2008) (Fig. 10.9).
• L5, however, sidebends to the same side during flexion and rotation (type 2) and the ‘L4–5 joint exhibits no particular bias; in some subjects the coupling is ipsilateral while in others it is contralateral’ (Bogduk 2005).
• Descending through the 1st lumbar vertebral foramen is the conus medullaris of the spinal cord.
• The lower lumbar foramina house the cauda equina and the spinal meninges.
• The cord may be traumatized in numerous ways and may also become ischemic due to spinal stenosis, a narrowing of the neural canal, which may be exacerbated by osteophyte formation.
• Other factors that might cause impingement or irritation of the cord include disc protrusion, as well as excessive laxity allowing an undue degree of vertebral translation anteroposteriorly and from side to side.
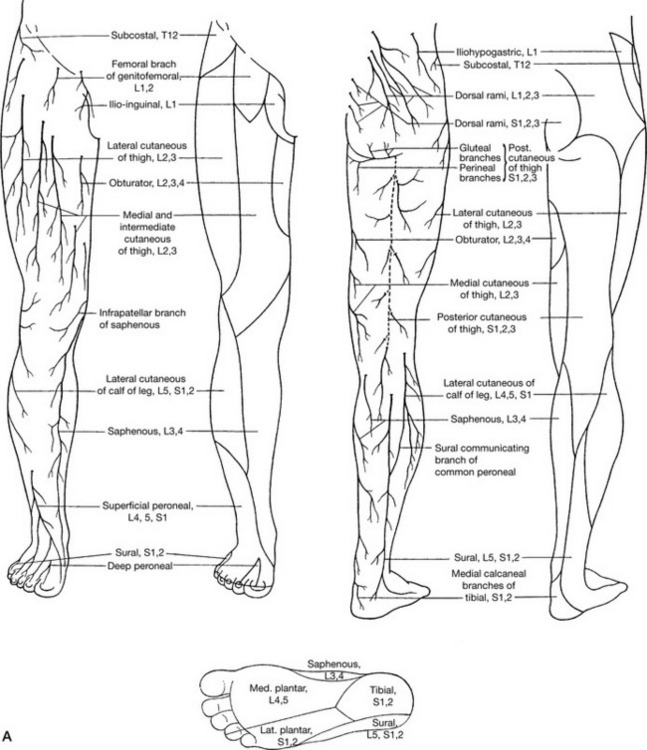
• The nerve plexus that supplies the lower extremity derives from the cord at the lumbar and sacral levels, which means that any nerve root impingement (disc protrusion, osteophyte pressure, etc.) of the lumbar intervertebral foramina could produce both local symptoms as well as neurological symptoms involving the lower extremity.
• Postural dysfunction, once established, tends to lead to biomechanical adaptation and a self-perpetuating, habitual pattern of use in which dysfunction begets ever greater dysfunction.
• It is important to consider global posture rather than local factors alone when assessing biomechanical dysfunction, together with awareness of previous compensation patterns. While some compensatory patterns can be seen as common, almost ‘normal’, how the body adapts when traumas (even minor ones) and/or new postural strains are imposed will be strongly influenced by existing compensatory patterns. In other words, there is a degree of unpredictability where compensations are concerned, especially when recent demands are overlaid onto existing adaptation patterns.
• Structural compensations can involve a variety of influences, for example as the body attempts to maintain the eyes and ears in an ideally level position. Such adaptations will almost always involve the cervical region and may involve lumbar compensations. These adaptations will be superimposed on whatever additional compensatory changes have already occurred in that region. The practitioner, therefore, has to keep in mind that what is presented and observed may represent acute problems evolving out of chronic adaptive patterns. ‘Unpeeling’ the layers of the problem to reveal core, treatable obstacles to recovery of normal function involves patience and skill.
• Chapter 2 examines posture and postural compensations in more depth, as do the remaining technique chapters where the pelvis and feet, the very foundations of the body’s structural support, are discussed.
• The following muscular attachments are of particular importance in the lumbar region.
• The crura of the diaphragm attaches to the 2nd and 3rd lumbar vertebral bodies, lateral to the anterior ligament.
• Psoas major attaches posterolaterally to the upper and lower margins of all the lumbar vertebral bodies (Gray’s anatomy 2005).
• The spinal processes serve as attachments for the posterior lamellae of the thoracolumbar fascia, erector spinae, spinalis thoracis, multifidi, interspinal muscles and ligaments and the supraspinous ligaments (Fig. 10.10).
• There is a vertical ridge on all the lumbar transverse processes, close to the tip, to which the anterior layer of the thoracolumbar fascia attaches and which separates a medial area, to which psoas major attaches, from a lateral area for quadratus lumborum attachment.
• The medial and lateral arcuate ligaments attach to the transverse processes of L1, while the iliolumbar ligament attaches to the transverse processes of L5 (and sometimes weakly to L4).
• The posterior aspects of the lumbar transverse processes are covered by deep dorsal muscles, with attachments from longissimus thoracis.
• The lateral intertransverse muscles attach to the upper and lower borders of adjacent transverse processes.
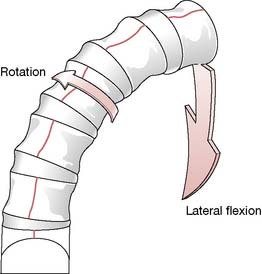
Figure 10.9 Sidebending of a vertebral segment of the lumbar spine is usually, but not always (Zhao G et al 2008), accompanied by contralateral rotation (type 1)
(reproduced with permission from Kapandji (1974)).
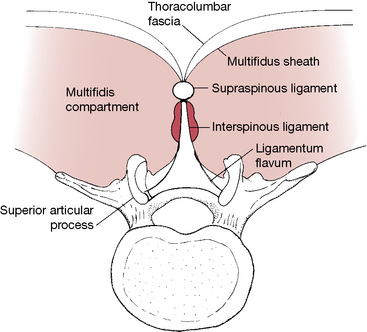
Figure 10.10 A horizontal view of a lumbar vertebra illustrating the interspinous-supraspinous-thoracolumbar (IST) ligamentous complex. By anchoring the thoracolumbar fascia and multifidus sheath to the facet joint capsules, the IST complex becomes the central support system for the lumbar spine
(reproduced with permission from Vleeming et al (1997)).
Transitional areas
Adaptive compensation forces (involving joints, ligaments, muscles and fascia), feeding upwards from the pelvic region or downwards from the upper trunk, commonly localize at the level of transition between the relatively inflexible thoracic spine and the relatively flexible lumbar spine: the thoracolumbar junction. The T12-L1 coupling is an important transitional segment as it is where free rotation is abruptly forbidden and where flexion and extension are suddenly and significantly allowed. As Waddell (1998) puts it: The transitional regions between fixed and flexible parts of the spine have greater functional demands, which might explain why these are the areas of most symptoms.
And as suggested above, any functional changes that occur are always accompanied by structural features, such as palpable shortening, fibrosis, or asymmetrical features affecting joint range of motion.
Spinal equilibrium and stability are subordinate to the integrity of the basic structures of the spine that comprise:
• the spinal column itself (vertebrae, zygapophysial joints, discs and ligaments), which Panjabi (1992) calls the ‘passive system’
The spinal column: its structure and function
As noted, the integrated structure of the spine, together with its nerve supply and muscles, serves various functions that offer stability, mobility and defense. Each of these functions imposes different demands on the way the structure is constructed. A need to offer support alone might have resulted in a more rigid structure, while if protective functions were the dominant requirement, greater mass might have developed. A compromise has evolved, combining mobility with relative rigidity and bulk. As Vleeming et al (1997) put it: ‘The demands of support and those of mobility are always in conflict, and achieving balance between them requires good control mechanisms’. The relative flexibility and support offered by discs, ligaments and muscles are, therefore, key elements in allowing efficient delivery of the various functions that the spine demands.
Braggins (2000) asserts that the two seemingly opposing functions of the vertebral column, rigidity and mobility, have resulted in the development of tough bones that offer strength as well as protection for the soft tissues within and around them, while at the same time there are many small jointed bones that offer flexibility.
In the properly positioned spinal column, the vertebral bodies and the intervertebral discs carry most of the load of the structures above them (and anything being carried). When healthy, the discs themselves are sufficiently flexible to allow flexion, extension, sideflexion, translation (glide) and varying degrees of rotation. The ability of the spine to absorb mechanical stress, therefore, depends to a large extent on the integrity of the spinal discs as well as on the spinal curves. (See Volume 1, Chapter 11 and Chapter 14 for details regarding the cervical and thoracic spine, respectively.)
Posteriorly, the zygapophysial joints emerge from the spine to form a ring of bone to protect the cord and emerging nerves and to offer (on each side) an articulatory connection, as the superior articular process of one vertebra meets the inferior articular process of the vertebra above. The term facet joints, so commonly used to describe these zygapophysial joints, fails to accurately identify the nature of these structures. Its common usage and popularity, however, are supported by its inclusion in most texts.
As Bogduk (2005) explains:
The term ‘zygapophysial’* is derived from the Greek words apophysis, meaning outgrowth, and zygos, meaning yoke or bridge. The term …. therefore means a ‘bridging outgrowth’, and refers to any articular process…other names that are used for the zygapophysial joints are ‘apophysial’ joints and ‘facet’ joints… ‘Facet’ joint is a lazy and deplorable term.
Bogduk’s obvious irritation at the use of this term arises from the fact that every joint in the body that has an articular facet is a ‘facet’ joint (for example, in the thoracic spine where each segment has facet articulations with ribs at the costovertebral and costotransverse joints). The descriptor ‘facet joint’ has, however, through common usage come to mean, in clinical shorthand, the zygapophysial joint and in this text the common usage of the term ‘facet joint’ may accompany or even at times replace ‘zygapophysial joint’ despite the fact that Bogduk’s objection is undoubtedly technically and semantically accurate.
Flexible stability
Flexibility and stability are the key words to define the needs of most joints and regions of the body. There would, for example, be little physiological benefit in a spinal region being stable but inflexible or in being flexible though unstable.
Achieving a combination of flexible stability is the focus of the therapeutic intent of most manual therapy disciplines through whatever means they employ.
• Stability clearly derives from a balanced degree of muscular tone in agonists and antagonists, rather than an imbalance such as is evident in lower crossed syndrome patterns where hypertonic extensors commonly overwhelm abdominal flexors (Janda 1996) (see Volume 1, Fig. 5.2).
• Flexibility relates to balanced tone as well as to healthy muscular, ligamentous and joint status and function (optimal strength, elasticity, etc.).
The lumbar spine, in particular, requires maximum stability and flexibility if back pain and dysfunction are to be avoided. As Liebenson (2000a) points out:
Spinal injury occurs when stress on a tissue exceeds the tissue’s tolerance. It is not so much excessive load as too much motion which is the primary mechanism of injury. Spinal injury and recovery depends on a number of factors such as avoiding repetitive motion, end-range loading, and early morning spinal stress. Also important is improving muscular endurance.
Adaptability = tolerance
The previous statement by Liebenson focuses attention on those essential elements that can be applied to understanding almost all musculoskeletal (and general health) breakdown: realization that the adaptive capacity of an organism as a whole, or of local tissues and structures in particular, has been exceeded. Liebenson’s use of the word ‘tolerance’ suggests several possible reasons for breakdown. The tissues could have been too weak to adapt to the demands or too inflexible, or both, or there could have been poor coordination between muscle groups. Restoration of reasonable function requires approaches that both ‘lighten the [adaptive] load and/or enhance function’. The solution to much local dysfunction is, therefore, to be found by encouragement of greater adaptability (e.g. increased flexibility, stability, strength and endurance) as well as aiming to reduce the adaptive demands being made on the tissues in question.
Identification of imbalances: essential first step
Successful therapeutic and rehabilitation approaches which meet these requirements for the recovery from musculoskeletal distress demand initial identification of underlying dysfunction, whether this involves hyper- or hypotonicity, hyper- or hypomobility, shortness, weakness, the presence of fibrosis, local myofascial trigger points and/or other evidence of chronic compensation, or indeed decompensation, where adaptive mechanisms break down and pathology ensues. Therapeutic attention needs to focus on the current dysfunctional pattern (which may have emerged as a result of overuse, misuse, disuse or abuse of already compromised structures) as well as on the underlying predisposing features. These issues are described in greater detail in Volume 1, Chapter 4.
Stress factors and homeostasis
It is worth emphasizing that repetitive minor stress has a cumulative effect equivalent to that of a single major stress event. Liebenson (2000a) informs us:
Most low back injuries are not the result of a single exposure to high magnitude load, but instead a cumulative trauma from sub-failure magnitude loads…in particular low back injury has been shown to result from repetitive motion at end range.
McGill (1998) confirms that low back injury is usually the result ‘of a history of excessive loading which gradually, but progressively, reduces the tissue failure tolerance’. These views are amplified by those of Paris (1997), as discussed later in this chapter.
In 1974 Selye discussed the ways in which multiple minor stress factors impact on the organism. As Shealy (1984) has explained:
Selye has emphasized that any systemic stress elicits an essentially generalized reaction…in addition to any specific damage each stressor might cause. During the stage of resistance (adaptation) a given stressor may trigger less of an alarm; however, Selye insists that adaptation to one [stress] agent is acquired at the expense of resistance to other agents. That is, as one accommodates to a given stressor, other stressors may require lower thresholds for eliciting an alarm reaction. Of considerable importance is Selye’s observation that concomitant exposure to several stressors elicits an alarm reaction at stress levels which individually are sub-threshold. (our italics) (Fig. 10.11).
The clinical importance of this cumulative impact cannot be overemphasized. In a given situation it may be possible to identify behaviors in a patient that individually are minor and seemingly innocuous, but which cumulatively impose sufficient adaptive demands to become significant. ‘Lightening the stress load’ may, in such a setting, therefore require only minor behavioral modifications in order to achieve clinical benefit and symptomatic improvement.
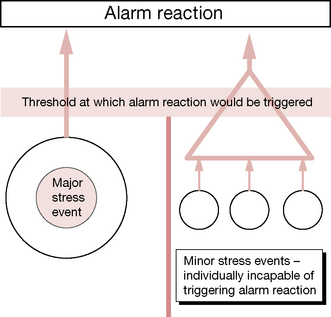
Figure 10.11 A combination of minor stresses, each incapable of triggering an alarm reaction in the general adaptation syndrome, can, when combined or sustained, produce sufficient adaptive demand to initiate the alarm
(reproduced with permission from Chaitow & DeLany (2008)).
For example, Lewit (1985) has shown that when the thoracolumbar junction region is painfully restricted, an array of local musculature might be shown to be involved, frequently including quadratus lumborum, the erector spinae, psoas and even tensor fascia latae. Therapeutic interventions and self-care that begin to normalize dysfunction in those most implicated (based on assessment and palpation findings) can often produce a satisfactory resolution without all the structures needing to be treated. As the process evolves, self-normalization commonly takes over, once key restrictions, weaknesses, shortnesses, etc. are addressed. In other words, once a part of the ‘stress load’ has been eased, or functionality restored, homeostatic mechanisms are usually capable of restoring normal function without everything that is demonstrably dysfunctional having to be treated. This theme of homeostatic self-regulation is discussed at length in Volume 1, Chapter 4 and is reviewed in Chapter 1 of this volume.
It is also important to reemphasize that ‘stressors’ (in the context of our focus on the musculoskeletal system), which can be defined as events and factors that demand adaptive responses (from the body as a whole or from local tissues or structures), are not confined to those of a biomechanical nature. Biochemical and psychologically based stressors interact with biomechanical features so profoundly as to form a triad of influences, all of which need to be taken into account.
Examples of these interactions, and greater discussion of the mechanisms involved, are to be found in Volume 1. The following brief quote from Volume 1, Chapter 9, offers a sense of these interactions and how modification of one can influence the others and the overall status of the individual.
The influences of a biomechanical, biochemical and psychosocial nature do not produce single changes. Their interaction with each other is profound.
• Hyperventilation leads to alkalosis, alters neural reporting (initially hyper and then hypo), creates feelings of anxiety and apprehension, and directly impacts on the thoracic and cervical regions’ structural components, both muscles and joints. (Gilbert 1998).
• Altered chemistry (hypoglycemia, alkalosis, etc.) affects mood directly while altered mood (depression, anxiety) changes blood chemistry, as well as altered muscle tone and, by implication, trigger point evolution (Pongratz et al 2004, Brostoff 1992).
• Altered structure (posture, for example) modifies function (breathing, for example) and therefore impacts on chemistry (e.g. O2: CO2 balance, circulatory efficiency and delivery of nutrients, etc.) which impacts on mood (Gilbert 1998).
Within these categories – biochemical, biomechanical and psychosocial – are to be found most major influences on health, with ‘subdivisions’ (such as ischemia, postural imbalance, trigger point evolution, neural entrapments and compressions, nutritional and emotional factors) being of particular interest in NMT (Chaitow & DeLany 2008).
The contextual environment
The brief discussion that follows relates to the ways in which the lumbar spine performs its myriad tasks and of the efficiency (or otherwise) of the soft tissue structures that support and move it. There is a need to be aware of the mechanical confines under which the lumbar spine operates, the forces it responds to, the structures it interacts with; in other words, its contextual environment.
The lumbar spine does not operate in a vacuum.
• It articulates at the thoracolumbar junction with its superstructure, the thoracic spine, and all that this indirectly attaches to, as well as with the pelvis, at the sacrum.
• It links directly to the upper extremities via latissimus dorsi and to the lower extremities via the psoas muscles
• It is intimately involved in respiratory function via the merging of both psoas and quadratus lumborum with the diaphragm, which also attaches to the lumbar spine.
• It also copes with gravitational demands, as well as a wide range of movement requirements involving flexion, extension, sideflexion, rotation, torsion, shearing forces, compression and elongation.
The unified nature of spinal stabilization (in particular) and spinal function (in general) is discussed by Tunnell (2000), who offers a useful summary of the background to spinal function and dysfunction.
The problem of spinal stabilization is unique. The term ‘axial organ’ has been coined to refer to the spine and highlights the fact that the spine, while composed of many segments, has a unique function as a distinct and unified organ within the motor system. It functions as the structural axis, or core, of the motor system, around which the peripheral trunk and extremities are organized. However, the spine can only function effectively in this capacity with adequate neuromuscular activity and coordination (Gardner-Morse et al 1995). This requires perception/proprioception, planning, timing, coordination, speed, endurance and strength.
Research has demonstrated the feed-forward spinal stabilization response that occurs before intentional movement begins (Cresswell 1994). The CNS must choose a postural set for each activity, whether static or dynamic. Thus effective stabilization of the spine consists firstly of stabilization of the individual spinal segments into a spinal posture which is both safe for the spine, and biomechanically consistent with the task at hand, and secondly of activity of the more peripheral trunk muscles which transfer loads from the trunk to the pelvis and minimizes the loads experienced by the spinal segments (Bergmark 1989).
Gender issues and posture
The complexity of postural influences is evident in a study by Roberts & Arefi-Afshar (2007). They sought to establish whether proprioceptive feedback from body postures operate differently for women and men. Participants received feedback regarding their posture, and results showed that when men received ‘success feedback’ regarding standing upright as opposed to slumping, this enhanced their performance. In contrast, after adopting an upright posture, women went on, after ‘success feedback’, to perform more poorly. The reasons for this disparity in responses remain unclear.
One role of the practitioner is to perform assessment tasks that help to unmask imbalances and dysfunctional features that may be contributing to a failure of the spinal (or other) structures to operate normally. A range of palpation and assessment methods are described throughout this text.
Soft tissue spinal support
The lumbar spine transfers the weight of the upper body to the pelvis and the lower extremities and also provides mobility for the trunk and protection to central neural structures. The stability of the lumbosacral spine depends on a variety of soft tissue supports as well as its own intrinsic architecture. Willard (in Vleeming et al 2007) provides an insight to the cohesive nature of the soft tissue support.
Although typically described as separate entities in most textbooks of anatomy, these fibrous, soft tissue structures actually form a continuous ligamentous stocking in which the lumbar vertebrae and sacrum are positioned. The major muscles representing the prime movers in this region – such as multifidus, gluteus maximus, and biceps femoris – have various attachments to this elongated, ligamentous stocking.
Coordination
Within this integrated musculoligamentous corset, incorporating both spinal and abdominal structures, stability is more probable if a coordinated relationship exists between agonists and synergists. Low back pain has been shown to be more likely and more severe where inco-ordination exists; for example, overactivity in antagonist back muscles during the swing phase of the gait cycle (see Chapter 3) (Arendt-Nielson 1984), as well as delayed activation of transversus abdominis (for spinal stabilization) during arm movement (Hodges & Richardson 1999). Malcoordination of this sort leads to an unstable situation where injury can more easily occur.
Other forms of coordination may involve co-contraction of antagonist muscles as a stabilizing feature. Cholewicki et al (1997) have shown that lumbar stability was enhanced by the coactivation of agonists and antagonists, but that increased levels of such behavior might be an indication that the passive stabilizing systems of the lumbar spine were less than optimal.
Brief moments of co-contraction are, however, seen as being vital in maintaining safe joint stabilization when unexpected loading occurs. One of the most important muscles responsible for creating stability in the lumbar spine when it is in a neutral range (i.e. not end range) is transversus abdominis (Cholewicki et al 1997). Indeed, studies that employed EMG demonstrated that transversus abdominis is the first muscle recruited when a sudden, alarm perturbation requiring stabilization occurs (Cresswell 1994).
Liebenson (2000d) elaborates to the contrary: ‘While the abdominal muscles receive much of the attention for their protective function in the low back, it is the extensors that are perhaps of even more importance. Decreased trunk extensor endurance has been shown to correlate with low back trouble’. See ‘Endurance factors’ on p. 226 and also Box 10.2, which describes aspects of rehabilitation for these vital supporting structures.
Box 10.2 Core stabilization assessment and exercises
There is an ongoing debate among experts as to the relative importance in back stability of the abdominal musculature as against the trunk extensors. In truth, the debate matters little in the broad context, since the functional integrity of both groups is essential for normal healthy spinal function. Indeed, there is much evidence, as explained earlier in this chapter, that co-contraction of opposing musculature in the spinal region is a common event during normal activities, accentuating the need for good tone and status in both anterior and posterior muscular groups (Cholewicki et al 1997, Liebenson 2000b, d). A variety of exercises have been developed to achieve core stability involving the corset of muscles which surround, stabilize and, to an extent, move the lumbar spine.
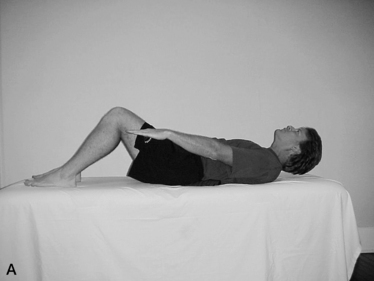
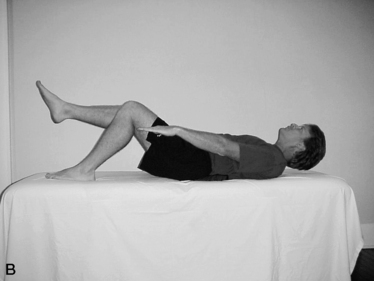
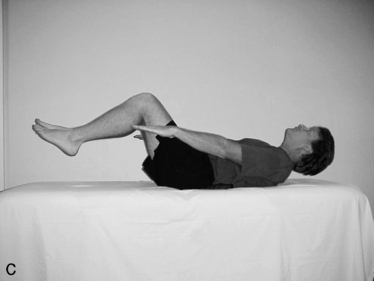
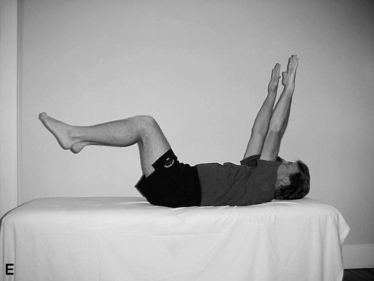
Richardson & Jull (1995) have described a ‘coordination’ test that assists in evaluating the patient’s ability to maintain the lumbar spine in a steady state during different degrees of loading. Norris (2000b) describes this procedure of assessment of spinal stability.
• The patient adopts a supine hook-lying position, with a pressure (bio)feedback pad (inflatable cushion attached to pressure gauge, similar to the unit used to test blood pressure) under the lumbar spine.
• The inflated pad registers the degree of pressure being applied by the lumbar spine toward the floor. The objective is to maintain the pressure throughout the performance of various degrees of activity (see below).
• First the patient is asked to hollow the back, bringing the umbilicus toward the spine/floor, so initiating co-contraction of transverse abdominis and multifidus (Fig. 10.13) and to maintain this position as increasing degrees of load are applied by gradually straightening one leg by sliding the heel along the floor. This causes the hip flexors to work eccentrically and, if this overrides the stability of the pelvis, it will tilt. Therefore, if there is a change (reduction) in pressure on the gauge or if a pelvic tilting/increased lumbar lordosis is observed or palpated before the leg is fully extended, this suggests deep abdominal muscular insufficiency involving transversus abdominis and internal obliques.
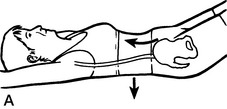
Figure 10.13 A ‘Neutral spine’ coordination test
reproduced with permission from Journal of Bodywork and Movement Therapies 2000;4(2):110)
B When there is greater flexion in the spine, there is greater loading on the disc, while when there is greater extension in the spine the load shifts toward the facets. Maintaining a neutral spine is the best way to load share between the 3 pillars of the tripod mechanism.
Taken from Figure 2, Wallden M 2009 The Neutral Spine Principle. JBMT 13(4):352–361
• Once the basic stabilization exercise of hollowing the abdomen while maintaining pressure to the floor is achievable without holding the breath, more advanced stabilization exercises may be introduced. These involve, in a graduated way, introducing variations on lower limb or trunk loading and are performed while maintaining the lumbar spine pressed toward the floor (confirmed by a relatively constant reading on the pressure gauge or by observation). These graduated stabilization exercises involve the adoption by the patient of positions that progress as illustrated in Fig. 10.14, commencing with upper limb flexion alone (A) to upper and lower limbs being flexed and held (D), followed by the ‘dead bug’ position and eventually trunk curls (F and G). Repetition of these held positions (5–8 seconds) a number of times daily produces a gradual regaining of spinal stability (see also self-help exercise in Chapter 7).
Liebenson (2000b) states: ‘The most important thing to remember about safe back training is ‘that in acute stages the exercises should reduce or centralize the patient’s pain, and in the subacute recovery stage they should improve motor control’.
As well as abdominal tone and stability, it is necessary to encourage extensor function to be optimal and coordinated with abdominal muscle function. To encourage spinal extensor tone and strength in order to encourage spinal stability, simple home exercise protocols can be suggested (see Chapter 7, extensor exercises, p. 165).
Liebenson (2000d) says that: ‘Endurance training of agonist and antagonist co-contraction ability about a joint has been shown to improve joint stability. This does not require a very strong muscular effort. Hoffer & Andreasson (1981) showed that efforts of just 25% of maximum voluntary contraction (MVC) provided maximal joint stiffness. A prolonged tonic holding contraction and a low MVC is ideally suited to selectively recruit and train type 1 [postural] muscle fiber function’ (our emphasis).
Central and peripheral control
Panjabi (1992) suggests that there are three distinct and integrated subsystems, which work together to encourage spinal stability:
• A neural control subsystem (which comprises both peripheral and central control)
• The active muscular subsystem
• The passive osteoligamentous subsystem (including articulating surfaces and periarticular soft tissue structures)
The requirements needed to maintain spinal stability, in any given situation, are assessed by the central neural subsystem, which then signals to the muscular system to produce the appropriate responses. If there is poor central (motor) control, or if the muscular or ligamentous structures are incapable of adequately meeting the stabilization needs, a recipe for dysfunction and pain exists.
Discussing appropriate therapeutic choices where muscular dysfunction is apparent, Bullock-Saxton (2000) says:
An understanding of the deficit in the neural system is essential for treatment. Treatment of the muscle pattern response without this perspective can be misdirected and futile. Effectively the muscles are the reflection of either some peripheral neural change, or some central neural change.
An example of inadequate motor control is offered by Liebenson (2000b): ‘Inappropriate muscle activation sequences during seemingly trivial tasks such as bending to pick up a pencil can compromise spinal stability and potentiate buckling of the passive ligamentous restraints’.
Coordination of muscular activity to provide adequate stabilization when performing even trivial movements demands appropriate neural input and this, in turn, requires coherent data from proprioceptors, mechano-receptors and other neural reporting stations. Efferent transmissions are more likely to be appropriate if based on accurate afferent information, deriving from proprio-ceptive impulses, as well as sensory (e.g. visual) sources.
Why would peripheral information flow be inaccurate or inadequate? Janda (1978, 1986) suggests that normal information flow to the cord and brain can modify due to changes in activity from sensory receptors (neural reporting stations – see Volume 1, Chapter 3, and Chapter 2 in this volume) and also from modifications in the stimulation threshold of spinal cord cells. Examples of ways in which peripheral information can become modified include inflammation, trigger point activity, pain, peripheral injury, and altered joint biomechanics. Apparently pain stimuli ‘are capable of altering the sensitivity to central perception of pain, and other afferent stimuli, as well as altering the efferent response not only at segmental level, but to many levels both ipsilateral and contralateral to the source of the stimuli’ (our emphasis) (Bullock-Saxton 2000). If the CNS is not receiving information accurately, or is not interpreting the information appropriately, the nature of its response is likely to be unsuited to the needs of the tissues it is serving.
Muscles in such areas are therefore likely to be either overactive or inhibited. As Tunnell (2000) explains:
The terms ‘overactive’ and ‘inhibited’ refer to altered neurological states of a muscle. In an ‘overactive’ muscle, the threshold of activation is lowered; and the muscle may be activated earlier and more often than normal and may be included in movements or functions in which it would normally be silent. An inhibited muscle exhibits an elevated threshold for activation and is left out of movements where it would normally be included. The terms ‘weak’ (loss of muscle strength) and ‘tight’ (shortness, loss of extensibility) on the other hand refer to biomechanical properties of the muscle.
Murphy (2000) expands on this theme.
It is common to find inhibition in certain muscles that have an important stabilization role in patients with spinal complaints… It is important to realize that, while most muscles in patients with spinal complaints will have sufficient strength to perform their role in movement and stability, if the central nervous system is not properly activating them, at the right moment, to the correct magnitude, and in harmony with the other muscles involved in the activity, dysfunction and microtrauma may result. From a clinical viewpoint this is far more important than ‘weakness’.
The dysfunctional pattern that would emerge from such a scenario would result in altered muscle-firing sequences, imbalances between agonists and antagonists, a failure of synergists to perform their supportive roles and ultimately pain and dysfunction. The understanding of such patterns requires an awareness of different muscle designation characteristics, relating to whether a muscle offers a supportive, stabilizing role or performs a more active, phasic, mobilizing function (see Volume 1, Chapter 2 as well as functional screening sequence in Volume 1, Chapter 5).
As Norris (2000a) explains:
The combination of muscle laxity and poor holding ability on one hand, with muscle tightness and dominance on the other hand, will alter the equilibrium point of the joint, tending to pull the joint towards the tight muscle. An inability to move actively through the full range due to a combination of tightness with poor inner range control will change the nature of a movement entirely.
Norris was not directing these thoughts specifically to the spine or spinal joints, but the concept of such imbalance leading ultimately to dysfunction is clear in any context.
The neural supply of the lumbar spine’s musculo-ligamentous support system suggests a high density of nociceptors which, if irritated by failure to meet adaptive demands, can initiate a process of neurogenic inflammation that can lead to chronic back pain (Garrett et al 1992, Levine et al 1993). This condition of chronic inflammation may be further aggravated and perpetuated by hormonal imbalance, adrenal exhaustion or other nutritional inadequacies (Lee & Hopkins 1996, Pizzorno & Murray 1990, Werbach 1996).
Choices muscles make
Under challenging aerobic conditions, if muscles such as transversus abdominis have to ‘choose’ between simultaneously enhancing respiratory function and stabilizing spinal structures, the respiratory demands will be selected and met, while the spinal stabilization may be inadequate to the demands on it (Richardson et al 1999, McGill 1995). Under such circumstances, possibly involving repetitive bending and lifting, the spine would become vulnerable. (See Box 10.4 later in this chapter for discussion on lifting.)
Muscle type relates to the density of type 1 and 2 fibers (slow and fast twitch, respectively) and this correlates to a large extent with endurance features (fatigue resistance) (Bogduk 2005). Slow-twitch fibers in some back muscles, such as longissimus, constitute as much as 70% of the total fiber content (55% in multifidus and iliocostalis). Bogduk says there is a strong possibility that: ‘Endurance may be a direct function of the density of slow-twitch fibers in the back muscles, and that lack of resistance to fatigue is a risk factor for back injury, and that conditioning [training] can change the histochemical profile of an individual to overcome this risk’. These observations would seem to equate with common sense, that the stronger and ‘fitter’ the muscles of the back, the less likely they are to fail when demands are placed on them.
The story regarding the lifting of heavy (and sometimes light) weights and back injury is, however, more complicated than that (Fig. 10.16).
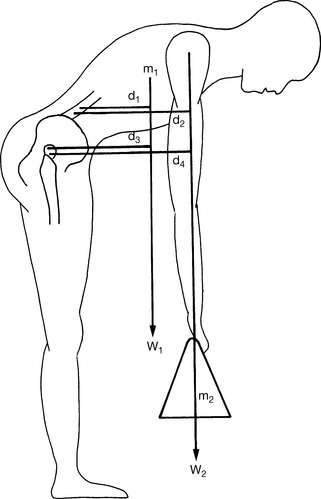
Figure 10.16 The flexion moments exerted on a flexed trunk. Forces generated by the weight of the trunk and the load to be lifted act vertically in front of the lumbar spine and hip joint. The moments they exert on each joint are proportional to the distance between the line of action of each force and the joint in question. The mass of the trunk (m1) exerts a force (W1) that acts a measurable distance in front of the lumbar spine (d1) and the hip joint (d3). The mass to be lifted (m2) exerts a force (W2) that acts a measurable distance from the lumbar spine (d2) and the hip joint (d4). The respective moments acting on the lumbar spine will be W1d1 and W1d3; those on the hip joint will be W2d2 and W2d4
(reproduced with permission from Bogduk (1997)).
The biomechanics of lifting are complicated, as indicated in Fig. 10.16. Bogduk (2005) uses an example of a 70 kg (150 Ib) man lifting a 10 kg (22 Ib) mass when fully stooped. ‘The upper trunk weighs about 40 kg (88 Ib) and acts about 30 cm (12 inches) in front of the lumbar spine, while the arms holding the mass to be lifted lie about 45 cm (18 inches) in front of the lumbar spine.’
Bogduk calculates that this is well within lifting capabilities. However, when the weight is increased to 30 kg (66 Ib) lifting is only possible if the weight is held closer to the spine. And even if this distance is decreased to 15 cm (6 inches) this particular individual’s lifting limit would be approximately 90 kg (198 Ib).
As Bogduk expresses it: ‘The back muscles are simply not strong enough to raise greater loads’. And yet greater loads are lifted, requiring explanations which move beyond the strength and endurance potentials of the back muscles. Theories have included the following.
• Intraabdominal pressure (balloon) theory (Bartelink 1957). This suggested that increased intraabdominal pressure could assist the lumbar spine in resisting flexion during lifting. However, Bogduk shows that there is scant correlation between intraabdominal pressure and the weight being lifted, or intradiscal pressure. Evidence from bioengineering has shown the intraabdominal pressure theory to be severely flawed in a number of respects (Nachemson 1986), with pressure being generated via these means being more likely to obstruct the abdominal aorta than to increase weight-lifting potential. (Farfan & Gracovetsky 1981).
• Gracovetsky et al (1985) note that the orientation of the posterior thoracolumbar fascia was such that during lifting, increased tension on it would automatically exert forces via the abdominal musculature, which would increase lumbar extension. Bogduk (2005) reports, however, that while the theoretical aspects of this model are not inaccurate, in practice (because of the limited degree of spinal attachment from the abdominal muscles to the thoracolumbar fascia), ‘the contribution that abdominal muscles might make to anti-flexion moments is trivial’.
• Gracovetsky et al (1981) propose a quite different model, suggesting that the lumbar spine, when fully flexed, would impose stretch onto the interspinous and supraspinous ligaments, the posterior thoracolumbar fascia and the capsules of the zygapophysial joints, so creating tension between the lumbar spinous processes and the ilia. As Bogduk explains: ‘Under such conditions the active energy for a lift was provided by the powerful hip extensor muscles’… which would rotate the pelvis posteriorly, raising the flexed lumbar spine passively, ‘like a long, rigid arm rotating on the pelvis and raising the external load with it’. Not only did this model not require participation of the back muscles, such participation was seen as undesirable: ‘Any active extension of the lumbar spine would disengage the posterior ligaments and preclude them from transmitting tension’. Once again, however, flaws exist in this model, not least the variable strength of the spinal ligaments. Bogduk again explains: ‘The posterior ligamentous system is not strong enough to replace the back muscles as a mechanism to prevent flexion of the lumbar spine during lifting. Some other mechanism must operate’.
• Other models include a ‘hydraulic amplifier’ hypothesis (Gracovetsky et al 1977), as well as an ‘arch’ theory (Aspden 1989), which has itself been challenged.
• Bogduk (2005) summarizes the current state of the debate.
The exact mechanism of heavy lifting remains unexplained. The back muscles are too weak to extend the lumbar spine against large flexion moments; the intra-abdominal balloon has been refuted; the abdominal mechanism and thoracolumbar fascia have been refuted; and the posterior ligamentous system appears too weak to replace the back muscles. Engineering models of the hydraulic amplifier effect and the arch model are still subject to debate. What remains to be explained is what provides the missing force to sustain heavy loads, and why intraabdominal pressure is so consistently generated during lifts if it is neither to brace the thoracolumbar fascia nor to provide an intraabdominal balloon.
Bogduk supplies further fuel for the debate by noting the following points.
• Researchers have so far ignored the role of the abdominal musculature in controlling axial rotation. The oblique abdominal muscles would come into play if the load being lifted was anything other than perfectly balanced in the mid-line. Resulting contraction of these abdominal muscles to control axial rotation would incidentally raise intraabdominal pressure, making this
• Inadequately explored so far, suggests Bogduk, is the factor of the passive strength of the spinal musculature. He notes that as muscles elongate their maximum contractile potential reduces but at the same time their passive elastic tension increases. Therefore, in an elongated muscle, ‘the total passive and active tension generated is at least equal to the maximum contractile capacity of the muscle at resting lingth’. This means that when the spine is in full flexion and the back muscles are electrically silent, ‘they are still capable of providing passive tension equal to their maximum contractile strength’, so making them capable of supplementing the posterior ligamentous system.
For these reasons, Bogduk suggests, some of the models which have been discarded may in fact have value; for example, if passive muscular tension in the back muscles is considered alongside the posterior ligamentous input to lifting. Norris (2000b) seems to include this concept in his observations.
Richardson et al also state that:
There is evidence that the multifidus muscle is continuously active in upright postures, compared with relaxed recumbent positions. Along with the lumbar longissimus and iliocostalis, the multifidus provides antigravity support to the spine with almost continuous activity. In fact, the multifidus is probably active in all anti-gravity activity.
Somewhat surprisingly, Richardson et al also highlight the importance of the diaphragm in postural control. In a study that measured activity of both the costal diaphragm and the crural portion of the diaphragm, as well as transversus abdominis, it was found that contraction occurred (in all these structures) when spinal stabilization was required (in this instance during shoulder flexion).
The results provide evidence that the diaphragm does contribute to spinal control and may do so by assisting with pressurization and control of displacement of the abdominal contents, allowing transversus abdominis to increase tension in the thoracolumbar fascia or to generate intra-abdominal pressure.
Noting the evidence relating to the role in spinal stabilization of the diaphragm, that Richardson et al (1999) have demonstrated, it is worth considering that anyone with a breathing pattern imbalance (a tendency to upper chest breathing, for example) might develop trigger point activity in the diaphragm itself (Lewit 1999). The repercussions and chains of involvement of this may be widespread. Lewit describes an active diaphragmatic trigger point, located ventrally under the arch of the ribs, which is associated with a trigger point in longissimus thoracis. Liebenson (2000c) explains the so-called Silvertolpe phenomenon (Fig. 10.12) relating to this trigger:
when [the trigger in longissimus thoracis is] perpendicularly palpated [this] causes a twitch response which can travel to the hamstring muscles causing extension of the low back or an anterior pelvic tilt (Silvertolpe 1989).

Figure 10.12 Palpation of the Silvertolpe reflex
(reproduced with permission from Journal of Bodywork and Movement Therapies 2000; 4(3):195).
Lewit (1999) and Liebenson (2000c) both report that the presence of these triggers (longissimus thoracis and diaphragm) may be associated with further points in the buttock at the level of the coccyx and that symptoms presented might include ‘low back pain, coccyx pain, pseudo-visceral pain and dysphonia’ and that therapeutic focus might need to involve treatment of the sacrotuberous ligament, the coccygeus muscle and other structures related to the pelvic and thoracic diaphragms. The importance of this illustrative example is the widespread linkages that can be demonstrated to be active, impacting not only on local structures but on functions such as breathing and speech.
The involvement of the diaphragm in postural stabilization suggests that situations might easily occur when such contradictory demands are evident, where postural stabilizing control is required at the same time as physiological requirements create demands for greater diaphragmatic movement. Richardson et al (1999) state: ‘This is an area of ongoing research, but must involve eccentric/concentric phases of activation of the diaphragm’.
Other muscles are also involved in stabilization and antigravity tasks, but these examples exemplify the complex interactions, which occur constantly whenever the need for core stability occurs. It is also to be kept in mind that here the discussion involves relatively functional muscles needing to make demanding and instantaneous choices. One can only imagine the complications which arise when these contradictory demands are placed on dysfunctional, hyper- or hypotonic tissues or those which are functioning out of the normal firing sequence.
Specific muscle involvement in stabilization
Such are the variety of movements and positions the lower back is called upon to manage that, within the ‘ligamentous stocking’ (Vleeming et al 2007), particular structures may have to handle greater stress loads than others. For example, twisting movements place differentiated stress on the rotatores and the intertransversarii posteriorly, while anteriorly the oblique abdominals help to stabilize the spine during sideflexion and twisting, particularly if the spine is simultaneously being axially compressed (McGill 1991).
Notes on quadratus lumborum
One of the major stabilizing influences on the low back is quadratus lumborum (QL), attaching as it does to spinal transverse processes as well as the pelvis and last rib. Regarding its stabilizing effects, McGill (1998) reports that it acts as a ‘bilateral vertebral buttress’.
QL does far more than sideflex the spine. In studies using EMG to measure activity as increasing degrees of weight were involved (erect normal subjects), it was noted that the greater the weight handled, the more QL activity occurred, without any evidence of sideflexion (McGill et al 1996). It was also noted that the stabilizing support to the lumbar spine from QL, in this setting, was greater than in erector spinae, rectus abdominis, internal obliques and external obliques (multifidi and transversus abdominis were not measured). Noting this study, which demonstrates QL’s stabilizing nature, Murphy (2000) asks: ‘To what extent is the QL active in mobilizing the lumbar spine or pelvis [since] classically QL is thought to contribute to lateral flexion of the lumbar spine, hip hiking, unilateral stance and hip abduction?’.
Norris (2000a) suggests that QL is, in fact, capable of being seen as two distinct entities with quite separate functions. ‘It seems likely that the muscle may act functionally in medial and lateral portions with the medial portion being more active as a stabilizor (sic) of the lumbar spine and the lateral more active as a mobilizor (sic).’ Norris points out that examples of such divisions of labor exist in other muscles, for example (citing a report by Jull 1994), gluteus medius, where the posterior fibers are more posturally involved.
Richardson (2000) supports Norris’ observation regarding QL’s dual role: ‘QL consists of two functionally different parts. Medial fibers are local spinal segmental stabilizers and the lateral fibers global, acting to assist lateral bending’. Tunnell concurs (2000) and says: ‘This example [of QL’s dual role] accents the reality that in the end a muscle’s function depends on the forces it is responding to and the task it is trying to accomplish for the body’.
Travell & Simons (1992) offer a slightly different perspective.
In an upright subject, the quadratus lumborum functions to control or ‘brake’ side bending to the opposite side by a lengthening contraction [i.e. eccentric]. Stabilization of the lumbar spine on the pelvis by the quadratus lumborum is so important that, according to Knapp [1978], complete bilateral paralysis of this muscle makes walking impossible, even with braces.
They also note its proposed role in stabilizing the last rib during inhalation and forced exhalation.
Endurance factors
The degree of endurance possessed by the muscles that support and stabilize the back is apparently a key element in the predisposition of spinal structures to pain and dysfunction. Indeed, if important muscles such as multifidus can be shown to have lost significant levels of their endurance potential, this can predict that recurrence of low back pain is more likely, or that it is likely to occur in previously trouble-free individuals (Biering-Sorensen 1984, Luoto 1995).
Fatigue is the end result of poor endurance to whatever demands are being experienced. Repetitive tasks such as bending and lifting, which are initiated by mechanically efficient squatting activities, have been shown to gradually give way to stooping and decreased postural stability as fatigue increases (Panjabi 1992).
Acute low back pain may be accompanied by evidence of multifidus atrophy, ipsilateral to the pain, and at the same spinal levels as joint dysfunction is noted. The atrophy may remain after recovery from the pain symptoms, unless exercises are undertaken to retrain the muscle (Hides et al 1993).
Localized multifidus changes were observed in individuals with chronic low back pain (CLBP) when both the size (cross-sectional area, CSA) and the ability to voluntarily perform an isometric contraction of the muscle were compared. Ultrasound imaging was used at four vertebral levels, in people with and without chronic CLBP, demonstrating a significantly smaller CSA of the multifidus muscle, at the L5 level, for those with CLBP, compared with those from the healthy group, and a significantly smaller contraction for subjects of the CLBP group at the same vertebral level. These results were not present at other vertebral levels and the clinical relevance of this finding is that rehabilitation efforts may need to be specifically localized in order to target localized impairments in motor control (Wallwork et al 2009).
Liebenson (2000d) describes the importance of the relative endurance potential of the extensors of the spine.
The evidence is extremely strong because it is prospective [predictive]. Biederman et al (1991) reported greater fatiguability in the multifidus than other parts of the erector spinae in chronic low back pain patients vs normals. Of note is the fact that moth-eaten type 1 [i.e. postural] muscle fibers (‘slow-twitch’) in the multifidus of chronic low back pain patients have been reported (Rantanan et al 1993). This signifies degeneration and possibly fatty infiltration of the type 1 – endurance functioning muscle fibers of the multifidus.
Note: Discussion of the distinction between type 1 and type 2 fibers is found in Volume 1, Chapter 2.
Liebenson (2000a) summarizes the need for preventing low back injury as requiring ‘conditioning or adaptation’ (i.e. avoidance of undue stress and acquisition of improved flexibility and stability, which leads to greater tolerance to strain). He suggests that there is evidence that too little (or infrequent) tissue stress can be damaging, as can too much (or too frequent or prolonged) exposure to biomechanical stress. In other words, deconditioning through inactivity provokes dysfunction just as efficiently as does excessive and inappropriate biomechanical stress.
McGill (1998) suggests that a neutral spine should be used in all loading tasks to reduce the chance of injury (see Box 10.2 for more on neutral spine). This suggestion is coupled with a warning to avoid spinal end-of-range motions (stooping to lift, for example). Additional common-sense methods are suggested, including rotation of tasks to vary loads, introduction of frequent short rest breaks and maintaining loads close to the spine (McGill & Norman 1993). There is also evidence that tissues are more vulnerable after rest (for example, early morning) and after sitting for even brief (30 minutes or more) periods (Adams et al 1987).
Impostor symptoms
Grieve (1994) describes conditions that ‘masquerade’ as others, and some of these relating to the lumbar spine are summarized below. Perhaps the most important concept that a manual practitioner can practice is to remain suspicious of visceral pathology – first and foremost – since ignoring these types of conditions can produce the most serious consequences.
Suspicion that a problem is other than musculoskeletal might arise due to:
• misleading symptoms: something not seeming quite right regarding the patient’s story describing the pain or other symptoms. A practitioner’s gut feeling should always cause her to err on the side of caution and refer onward for another opinion
• patterns of activities that aggravate or ease the symptoms seem unusual and give rise to doubts in the mind of the practitioner
• symptoms that arise from sinister causes (neoplasms, for example), that closely mimic musculoskeletal symptoms, or which are present alongside actual musculoskeletal dysfunction. Lack of progress in resolution of symptoms or unusual responses to treatment should cause the practitioner to review the situation.
A number of observations on this topic, by Grieve and others, are summarized in Box 10.1.
Making sense of low backache
When a patient presents with a backache any reasonably well-trained practitioner will be aware of the huge list of possible causes. Diagnosis of the cause(s) of backache is commonly one of exclusion. Once (hopefully) all the life-threatening possibilities have been eliminated, there remain a large number of (mainly) non-critical causative options. A number of excellent clinicians have provided their perspectives on how best to manage the process of evaluation and assessment, which should lead to an understanding of the likeliest cause of the individual’s backache (Braggins 2000, Liebenson 2007, Norris 2000b, Vleeming et al 2007, Waddell 1998).
Waddell (1998) has described a simple diagnostic triage* in which a decision is made based on the history, presenting symptoms and clinical judgment of the practitioner. This initial screening determines subsequent management of the case, involving appropriate investigation, treatment and/or referral. Waddell divides backache into three categories (described in more detail below): ‘simple backache’, nerve root pain and serious pathology. Waddell makes a particularly important observation when he says:
You should be able to distinguish gastrointestinal, genitourinary, hip or vascular disease, if you think about them. We miss them when we do not think, but rather assume that every patient with a back pain must have a spinal problem. (Waddell’s italics)
Norris, who subscribes to Waddell’s process of differential screening using the triage process, advises the following guidelines for reestablishing back stability, using stabilization exercises (see Box 10.2) for the different triage groups.
• Simple backache: begin stability exercises and continue until fully functional.
• Nerve root compression: begin exercise as pain allows but refer to specialist if there has been no improvement within 4 weeks.
• Serious pathology: use back stabilization exercises only after surgical or medical intervention.
Greenough (2009) has listed major red flag features for anyone presenting with low back pain that should alert the practitioner to possible serious pathology, requiring referral and further investigation.
If the patient with back pain:
• Is under 50 years of age, whose back pain has failed to improve
• Has a previous history of cancer
The NMT perspective
The authors of this book suggest that therapists and practitioners, who utilize soft tissue manipulation, for example NMT and MET, should follow roughly the triage and red flag guidelines, as outlined above. Positional release methods may be safely employed in any triage category, at any stage, for short-term symptom relief, since these approaches are completely non-invasive. Deactivation of trigger points, performed extremely carefully, could also be incorporated into settings outside ‘simple backache’, in order to reduce the pain load.
The ‘Simple Backache’ (i.e. biomechanical in origin)
Greenough (2009) has summarized the key features of non-specific/simple/biomechanical low back pain, as follows:
• Affects the low back, buttock, thigh, and sometimes the calf or foot
• Feels stiff on rising – for around 30 minutes
• May result in shuffling gait, and a need to change position
• Sleep is usually sound, after settling
• May cause waking when turning over
• May produce a sense of ‘giving way’ with trivial movement – such as a bend or twist
• Improves gradually over a period of weeks - with or without treatment
One of the criteria for this categorization (‘simple’) is that the patient who presents with what Waddell (1998) terms ‘common non-specific’ backache is otherwise ‘well’. This implies that biomechanical factors are the primary aggravating features and that the symptoms vary with activity. In contrast with non-mechanical backache, simple forms are usually variable in intensity, are relieved by rest, particular positions and movements (such as stretching). The pain of uncomplicated backache may be severe and may spread to the buttocks and thighs but seldom involves dangerous pathology. Waddell is dismissive of attempts to classify ‘non-specific’, or ‘uncomplicated’, low back pain into categories: ‘…at present we have no reliable way of sub-classifying nonspecific low back pain’.
Paris (1997) presents a variety of methods for distinguishing one form of back pain from another and takes a different view as to the common etiology of low back pain, very much in line with that of McGill (1998), as discussed earlier in this chapter. He describes a:
… – paradigm of back pain being caused by a summation of dysfunctions, each contributing to an accumulation of noxious stimuli, which, when the individual’s level for appreciation is reached, will be interpreted by the individual as discomfort and, when sufficiently accumulated, will result in pain even in the stout-hearted, producing one more patient seeking assistance.
The reader is referred to the notes on the general and local adaptation syndromes (GAS and LAS) in Volume 1, Chapter 4, and to a summary of this information in the Essential Information section of this book. It is also useful to remind ourselves of Shealy’s (1984) words, as noted earlier in this chapter, describing one of the key findings of the major researcher into stress influences, Hans Selye. ‘Of considerable importance is Selye’s observation that concomitant exposure to several stressors elicits an alarm reaction at stress levels which individually are sub-threshold…’ In other words, ‘simple’ low back pain seldom emerges as a result of a single event but rather follows a compounding of minor influences, usually overlaid on underlying, predisposing factors (shortness, tightness, altered firing sequences, active trigger points, weakness, restriction, etc.).
Paris (a physical therapist) continues:
In back management, traditional medicine is invaluable for pain relief and little else. Medical diagnosis is unable to find or agree on most causes of low back or, for that matter, shoulder pain. Again, the reason for this is that physicians are trained in disease, not in detecting dysfunctions, and dysfunctions are usually multiple rather than singular.
This message is of great value to those who struggle to help patients with back pain. The need is not to look for ‘a cause’ but for as many signs of dysfunction as can be elicited by observation, palpation and assessment. Out of the amalgam of influences of these factors the back pain will have emerged and, following detailed assessment, the task of the practitioner is twofold: to reduce the burden of adaptation to which the area is being subjected and, at the same time, to enhance the functional integrity of the back so that it can better handle the abuses and misuses to which it is routinely subjected.
It is possible to identify some of the obvious reductionist thinking and conceptual bias associated with different perspectives on low back pain. For example, a great deal of chiropractic thinking focuses on vertebral misalignment and facet dysfunction, while disc dysfunction has received most attention from manual medicine (e.g. Cyriax 1982). Myofascial pain, on the other hand (trigger point-generated back pain), has received the most attention from Travell & Simons (1992) and Simons et al (1999) as well as the more extensive world of physical therapy, massage and neuromuscular therapy. Paris (1997) sums up the need to move away from single-cause thinking: ‘Deciding on which structure is the cause [of back pain] is a waste of time – but trying to decide on which structures are involved is constructive’.
Awareness of the structures involved as well as the habits and/or events that have loaded them with adaptive demands allows for the use of therapeutic and rehabilitation interventions which can lead to the restoration of pain-free function and better patterns of use. On p. 246 a variety of assessment protocols are detailed and the controversial question relating to the accuracy of commonly used tests is discussed.
Where might pain arise from in low back pain problems?
• Fatigued and ischemic musculature (and tendons): established by tests that evaluate unbalanced firing patterns, such as prone hip extension test (p. 291 FIG 10.65) and sidelying hip abduction test (p. 257); muscle shortness, which is usually obviously related to postural imbalances such as the lower crossed syndrome (see Chapter 2, pp. 20–21) and further established by specific muscle shortness evaluations (described for all postural muscles in appropriate segments of each clinical application chapter); fibrosis and other soft tissue changes (established during NMT and other palpation procedures). Treatment protocols will depend on the nature of the dysfunctional pattern, including deep connective tissue work, stretching methods, such as MET and MFR, and rehabilitation exercises.
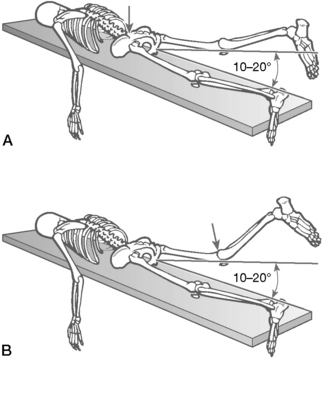
Figure 10.65 A: Abnormal hip extension movement pattern is associated with shortened psoas. B: Leg raising is initiated with an anterior pelvic tilt. If excessive hamstring substitution occurs, the extended knee will flex
(reproduced with permission from Chaitow (2001)).
• Myofascial trigger points: established by NMT and other palpation methods and treated by appropriate deactivation strategies including NMT, INIT, MET, PRT, acupuncture, etc. (see Volume 1, Chapter 6 and Chapter 9).
• Instability involving spinal ligament weakness (and outer annulus of spinal discs): established by history and assessment. Paris (1997) believes that: ‘Ligamentous weakness precedes segmental ligamentous instability, and instability is a precursor of the clinically apparent disc condition perhaps requiring surgery with or without fusion’. Ligamentous weakness pain usually starts as a dull ache, spreading slowly throughout the day to muscles that are assuming the ligament’s role as stabilizers. People who habitually self-manipulate (‘cracking themselves’) obtain short-term relief but actually increase the degree of instability. Suggestive signs of instability may include a visible rotation on standing that vanishes when prone or supine, marked hypertonic state of paraspinal musculature, increased range of movement (‘hypermobile’), periodic acute exacerbations of low back pain. Treatment should include reestablishing optimal muscular balance, core stability exercises, possible HVLA manipulation of the often restricted structures adjacent to the hypermobile segments, and postural reeducation, with avoidance of imposition of stress to the spine and of self-manipulation.
• Degenerative discs: established by signs, symptoms and evaluation strategies, including neurological (see p. 236) such as motor weakness and loss of sensation, as well as by scan evidence, if appropriate. Treatment depends on degree of acuteness/chronicity. Traction might be an initial approach (including self-applied) until the acute phase has passed, although traction is not universally approved (Paris 1997). Bedrest without bathroom privileges is essential in some cases, if acute swelling of soft tissues in the area of disc protrusion has occurred. Subsequent, subacute stage attempts to improve spinal biomechanics might include postural reeducation, mild stretching, core stability protocols, specific exercises (such as extension exercises to reestablish lordosis if this has been lost) and avoidance of spinal loading activities. Surgery should not be a first resort and should only be considered if neurological signs are evident.
• Facet capsules: involvement of zygapophysial facets as a cause of back pain requires careful assessment. The osteopathic diagnostic palpation requires that there be four indicators implied by the acronym ARTT: asymmetry of the segment (A), restricted range of motion (R), tissue texture changes (T) and tenderness/pain on palpation (T). Facet dysfunction might include facet capsule synovitis, facet capsule entrapment, facet blockage due to meniscus or loose body entrapment, or degenerative arthrosis of the facet joint. Treatment of facet joint problems includes rest, positional release methods, easing of excessive muscular guarding using NMT, MET or MFR, active manipulation (HVLA) or (most usefully for facet problems) the use of sustained natural apophyseal glide (SNAGs) methods as described in this chapter (see also Box 10.3 and Volume 1, Chapters 10 and 11).
• SIJ capsules and ligaments: the sacroiliac joint and its ligaments, which are a common source of low back pain, are described fully in Chapter 11.
• Anomalies such as spondylolisthesis are best established by X-ray or scan. Unless there are neurological signs spondylolisthesis is best treated conservatively, encouraging improved posture, rebalancing of the entire low back/pelvic musculature and core stabilization protocols (see p. 229). Psoas shortness will aggravate the condition and careful normalization of these muscles is often called for. If neurological signs accompany a spondylolisthesis, surgery and possibly fusion may be required.
• Stenosis of the spinal canal or lateral foramen: evaluated by means of signs and symptoms (commonly involving neurological symptoms exacerbated by exercise and relieved by forward bending – the pain is usually aggravated by riding a stationary bicycle with the spine in lordosis) and scan evidence. Paris (1997) suggests a variety of possible approaches. For a bilateral problem, he suggests reducing lordosis including loss of (abdominal) weight if this is a factor, deep tissue work and lumbar stretching, HVLA manipulation of lumbar spinal facets if restricted, use of viscoelastic insoles and possible modification of heel height (often lowering these). For a unilateral problem, a heel lift under the contralateral heel may change the local biomechanics sufficiently to reduce pressure at the neural foramen.
• Arthritic changes: signs and symptoms and history as well as X-ray or scan evidence confirm presence of arthritic changes. This category incorporates conditions such as lupus, ankylosing spondylitis, rheumatoid and osteoarthritis. Manual therapy contributions to such conditions are largely peripheral to the wider needs of the individual but may offer carefully modulated treatment suitable to the specific condition and patient, focusing on pain relief, circulatory and drainage enhancement and functional rehabilitation.
• Additionally, low back pain may be a feature of widespread conditions in which pain is a primary feature, such as fibromyalgia, where bodywork plays a role in palliative care, and functional support (for example, breathing function), rather than being able to address the systemic causes of the condition (Chaitow 2009).
• Psychogenic pain and somatization should also be considered where obvious somatic causes are absent.
Nerve root pain (see Box 10.5)
Box 10.5 Neurological examination
Waddell (1998) reminds us that less than 1% of all backache involves serious pathology or major structural problems (such as spondylolisthesis or cauda equina syndrome) and that the presence of such rare conditions needs to be ruled out so that evaluation of more probable causes can be investigated (see Box 10.1).
Box 10.1 Impostor symptoms (differential diagnosis)
Examples of ‘impostor’ symptoms, which replicate or produce low back pain, include the following.
• Almost any abdominal disorder can reflect as pain in the back (peptic ulcer, colon cancer, abdominal arterial disease). Therefore, all other symptoms should be evaluated alongside the musculoskeletal assessment.
• Andriopoulos et al (2007) report that a high proportion of patients with the brucellosis (an infection acquired from infected animals or milk) present with low back pain as a major symptom.
• Low back pain may be a major presenting symptom of carcinoma of the cervix, especially when there are secondary pulmonary tumors. (Storck et al 2004).
• A hiatal hernia is usually associated with bilateral thoracic and shoulder pain.
• Waddell (1998) suggests that cauda equina syndrome (involving a cluster of fine nerves at the terminal end of the spinal cord) and/or widespread neurological disorders should be considered if the patient with low back pain reports difficulty with micturition (desire for, or frequent urination, or inability to urinate at times) and/or fecal incontinence. A saddle formation area of anesthesia may be reported around the anus, perineum or genitals. There may be accompanying motor weakness in the legs, evidenced by gait disturbance (see Chapter 3). Immediate specialist referral is called for with any such symptoms.
• Suspicion of ankylosing spondylitis, or other chronic inflammatory conditions, should be raised if the symptoms of low backache involve an incremental onset prior to 40 years of age (usually in a male) which also involves: a family history; extreme stiffness in the morning; constant stiffness involving all movements of the spine in all directions; peripheral joint pain and restriction; associated colitis, iritis and/or skin problems such as psoriasis.
• Angina pain classically presents with chest, anterior cervical and (usually left) arm pain. Thoracic facet or disc conditions can mimic angina, as can active trigger point activity. Aggravating and ameliorating factors can usually offer clues as to whether the condition is cardiac related or responds to biomechanical influences.
• A dysfunctional gall bladder commonly refers pain to the mid-thoracic area uni- or bilaterally. Aggravating and ameliorating factors can usually offer clues as to whether the condition is related to digestive function or is biomechanically influenced.
• Sacroiliac and right buttock pain may be produced by perforation of the ilium in regional ileitis (Crohn’s disease).
• Pain that closely resembles acute thoracolumbar dysfunction can be the result of urolithiasis (stones in the ureter, ‘renal colic’).
• Pronounced low back pain (possibly referring to the testicles) may be associated with an aneurysm that is about to rupture. Grieve reports that: ‘the onset of dissection of the ascending aorta or aortic arch is characterized by a sudden, tearing chest pain’, which may radiate to the neck, thorax, abdomen and legs. The distinction between such symptoms and an acute musculoskeletal problem may be discerned by the ‘suddenness, severity and spread’ of the pain.
• If a patient has a background of coronary, pulmonary or bronchial disease the vertebral veins may have become varicosed, leading to an ill-defined backache. Grieve discusses the widespread nature of venous drainage from the vertebral column. These veins as well as associated arteries and arterioles are: ‘supplied with a dense plexiform arrangement of unmyelinated nerve fibers which constitute an important part of the vertebral column, and which may be irritated in a variety of ways to give rise to pain’.
• Osteitis deformans (Paget’s disease) may present with a constant aching pain but may be symptomless. Needle biopsy is necessary for confirmation of a diagnosis.
• The filament at the end of the dural tube, the filum terminale, may be involved in a tethering lesion, especially in adolescents during the ‘growth spurt’ years, with symptoms of back pain. Grieve reports: ‘The presence of mild bilateral pes cavus, shortening of the tendocalcaneus and a history of childhood enuresis, without a clear history of any neurological disease, might indicate a meningeal anomaly as the cause’.
• See also Volume 1, Figure 6.5 for common pain referred zones of various organs.
If the cause of low back pain is not ‘serious’, and if the triage approach is being used, the condition then lies within one of two areas: either ‘simple’ mechanical backache or backache involving neurological factors. If the backache involves the neurological system then the source may involve either peripheral or central features or both and it may be a local (e.g. one nerve root) or a widespread, generalized problem which requires expert differential diagnosis.
Within the nervous system, factors involving information input and/or the processing of information and/or the response of central structures might be implicated (Butler 1999).
Kellgren showed as far back as 1939 that it was possible to produce referred pain into the legs by stimulating portions of almost any tissue in the back. Waddell (1998) is clear that much leg pain associated with low back problems has nothing to do with disc impingement of neural structures (although, of course, a disc may be the cause) and reports that approximately 70% of patients with low back pain have some radiating pain in the legs which may derive from the ‘fascia, muscles, ligaments, periosteum, facet joints, disc or epidural structures’.
Petty (2006), who have provided a succinct and clinically useful sequence for musculoskeletal assessment of the patient, suggest that neurological assessment is required if the patient displays symptoms below the level of the buttock crease. The sequence they suggest involves initially using light touch (cotton wool) and pain sensation (pin prick) tests in order to discriminate between the involvement of peripheral nerves and those which derive from the spine, represented by dermatome distribution. This allows the practitioner to discriminate between sensory loss of altered sensation caused by a spinal (root) dysfunction and symptoms deriving from a peripheral nerve problem (entrapment, etc.).
Protocol for assessment of symptoms caused by nerve root or peripheral nerve dysfunction (Fig. 10.17)
Dermatome (skin tests) are performed to establish whether a nerve root or peripheral nerve is involved.
• The patient’s ability to detect (eyes closed) the presence of static cotton wool (cotton balls) placed onto areas of skin is evaluated. The patient is asked to report to the practitioner when he feels the presence of the cotton wool touching the skin.
• If the reported symptoms involve loss of sensation, the process commences by placing cotton wool on the insensitive (i.e. numb) area. Sequential placements are made until the patient reports ‘feeling’ the cotton wool, so allowing a mapping of ‘normal’ and ‘abnormal’ zones of the dermatome.
• If the symptoms involve hypersensitive sensations (tingling, burning, etc.), the cotton wool is placed initially on the sensitive skin and moved around (i.e. lifted and replaced) progressively until areas of normal sensation are reached, so mapping the hypersensitive zones.
• The practitioner utilizes knowledge of the patient’s reported pain patterns (Fig. 10.17C) and cutaneous distribution of the peripheral nerves (Fig. 10.17A) and dermatomes (Fig.10.17B) in order to evaluate the source of the symptoms.
As Petty (2006) explains:
Sensory changes are due to a lesion of the sensory nerves anywhere from the spinal nerve root to its terminal branches in the skin… Knowledge of the cutaneous distribution of nerve roots (dermatomes) and peripheral nerves enables the clinician to distinguish the sensory loss due to a root lesion from that due to a peripheral nerve lesion… It must be remembered, however, that there is a great deal of variability from person to person and an overlap between the cutaneous and the peripheral nerves and dermatome areas.
• Waddell (1998) suggests that nerve irritation should be evaluated by methods that stretch or irritate the nerve to see whether symptoms can be reproduced. Braggins (2000) discusses the normal movement of neural structures. She points out that:
In the course of normal everyday living, movements take place in the neural environment, not only of the meninges and nerve roots within the spinal and radicular canals, but also in the peripheral nerves within their mechanical interface tunnels, throughout the body: bones, muscles, joints, fascia and fibro-osseous tunnels.
In order to evaluate the freedom of movement of neural structures within their mechanical interface, stretching (‘neurodynamic’) tests are used, such as the following.
• Straight leg raising (SLR) test is performed with the patient supine. His leg is lifted upward by the practitioner with the knee maintained in a straight position and should raise to approximately 80–85° without discomfort or pain. If straight leg raising is painful, it must be determined whether this is due to impingement of the sciatic nerve (pain usually extending all the way down the leg) or to hamstring tightness (pain usually only involving the posterior thigh). The results of the straight leg raising test are open to misinterpretation. There is, for example, little significance in limitation of range apart from indicating shortness or spasm of the hamstrings or as an indirect contributor to back pain. However, when limitation of range of SLR with the addition of passive dorsiflexion of the foot at the end of the movement (which stretches the sciatic nerve) reproduces pain in the leg, it is significant and indicates neural irritation. Unfortunately, this test does not pinpoint the cause of that irritation, which could be in the lumbar spine or anywhere along the course of the sciatic nerve (Hoppenfeld 1976). It also could be caused by the stretching of trigger points, particularly if several in different tissues are stretched, thereby producing a pattern from the hip to the foot. Soleus alone could encompass the calf, heel and foot and possibly even the sacral region (Travell & Simons 1992). These patterns combined with hamstring patterns (both of which would be placed on stretch by this test) could duplicate nerve entrapment symptoms.
• Well-leg straight leg raising test is performed with the SLR test above and involves the supine patient raising the leg on his uninvolved side to determine if this causes pain on the involved side. If so, this points to a space-occupying lesion, such as a disc herniation (Hoppenfeld 1976).
• The Valsalva maneuver increases intrathecal pressure and, when positive, suggests probable pathology either causing intrathecal pressure or involving the theca itself. The patient is asked to bear down as if he were trying to open his bowels and if this causes pain in the back or radiating pain down the legs, the test is considered positive.
• Femoral stretch test is used when leg pain associated with back pain suggests that an upper nerve root may be involved. With the patient sidelying or prone, the leg is taken into flexion at the knee to evaluate reproduction of a radiating anterior thigh pain (not just tightness which indicates quadricep shortness). The pelvis should be maintained in neutral position during this test to avoid increasing lumbar lordosis and possible (confusing) radicular pain from lumbar facet surfaces. Trigger points whose patterns duplicate those reported by the patient should be ruled out as the cause.
• The ‘bowstring’ test involves allowing slight knee flexion at the end of its excursion into straight leg raising to where pain is noted and then applying thumb pressure onto the sciatic nerve where it crosses the popliteal fossa. Waddell (1998) notes: ‘With an irritable nerve, you may produce pain or paresthesia radiating up or down the leg. Local pain beneath your thumb is not diagnostic’ (Fig. 10.18).
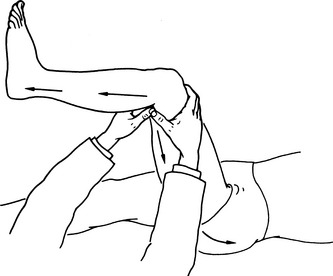
Figure 10.18 The diagnostic feature of the bowstring test is reproduction of the symptomatic root pain or paresthesia
(adapted from Waddell (1998) with permission).
• The Kernig test stretches the spinal cord and its overlying meningeal casing as the supine patient is asked to place both hands behind his head and carefully, but forcibly, flex his neck so that his chin moves toward his chest. A complaint of pain in the cervical spine, low back or down the legs may indicate meningeal irritation, nerve root involvement or irritation from the dural casing. A more broadly spread symptom report may indicate posterior protrusion of a cervical disc into the spinal cord.
• Other positive signs of nerve irritation include pain in both the back and the leg on coughing.
• Hoover’s test helps to determine if the patient’s claim to be unable to lift his leg is genuine. The practitioner cups the heels of both feet and asks the patient to raise the leg on the involved side. If the patient is truly trying to raise the leg, downward pressure from the calcaneus will be felt on the uninvolved side. If this is not felt, malingering is to be suspected.
• The causes of disturbed neural dynamics (previously described as ‘adverse mechanical or neural tension’) include factors that produce musculoskeletal dysfunction that impinge on neural structures, including disc protrusion, stenosis, spondylolisthesis, joint instability, scar tissue, high intramuscular pressure and overuse syndromes (Braggins 2000).
Muscle strength tests are performed to evaluate involvement of particular myotomes and their spinal nerve roots.
• By testing particular joints and thereby the associated muscle groups (see below) it is possible to gain information as to which spinal level may be involved. Myotome strength tests call for a short (2–3 seconds) isometric contraction involving the patient’s effort against the practitioner’s manual resistance. The muscles are placed into a mid-range position and the patient is asked to maintain the position against the effort applied by the practitioner. Additionally, individual muscles can be strength tested, using standard methods, to evaluate peripheral nerve involvement. By comparing the results with knowledge of the distribution of peripheral nerves it should be possible to discriminate between a nerve root dysfunction and a peripheral nerve involvement. Myotome testing for lumbar and sacral nerve root involvement involves the following strength tests (Fig. 10.19).
• Strength test of hip flexion evaluates L2. The patient attempts to maintain hip flexion as the practitioner attempts to overcome this effort (Fig. 10.20A). Strength test of knee extension evaluates L3. Patient attempts to maintain straight leg as practitioner attempts to introduce flexion (Fig. 10.20B).
• Strength test of foot dorsiflexion evaluates L4. Patient attempts to maintain dorsiflexion as practitioner attempts to plantarflex feet (Fig. 10.20C).
• Strength test of great toe extension evaluates L5. Patient attempts to maintain great toe extension as practitioner attempts to flex toes (Fig. 10.20D).
• Strength test of foot eversion evaluates S1. Patient attempts to maintain eversion as practitioner attempts to invert feet (Fig. 10.20E).
• Strength test involving bilateral buttock contraction evaluates S1. Practitioner palpates gluteus maximus to assess comparative
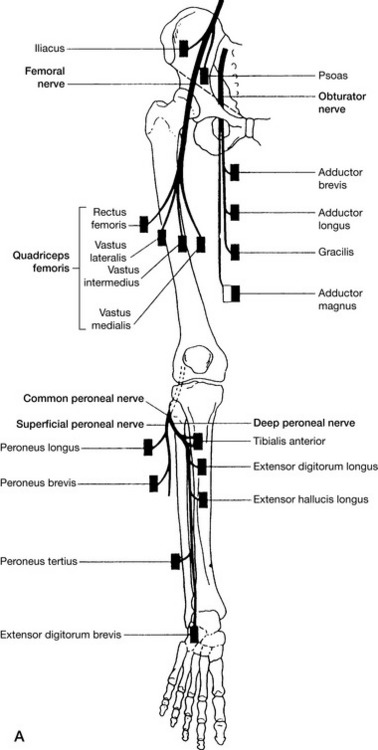
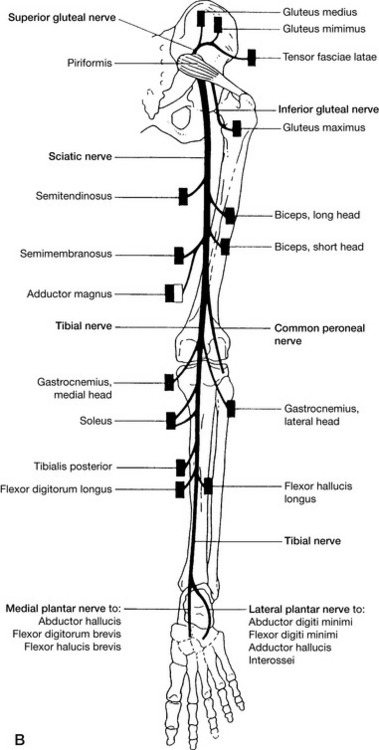
Figure 10.19 Diagrams of the nerves on the anterior (A) and posterior (B) aspects of the lower limb and the muscles that they supply
(adapted from Petty & Moore (1998)).
strength of bilateral contraction as patient tightens buttock muscles strongly (Fig. 10.20F).
• Strength test of knee flexion evaluates S1 and S2. Patient attempts to maintain position as practitioner attempts to straighten flexed knee (Fig. 10.20G).
• Testing standing on toes of one foot evaluates S2. Patient flexes one knee and attempts to maintain toe standing position on one foot and then the other, with practitioner offering light finger-tip support if balance is unsteady (Fig. 10.20H).
• Deep tendon reflexes are evaluated in order to provide possible evidence of upper motor lesion. In the lower extremity, the reflexes tested are knee and ankle jerk. The deep tendon tests involve tapping the tendon several times with a rubber hammer. The standard means of recording the degree of reflex activity following a deep tendon test are:

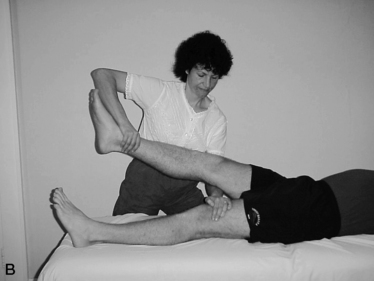

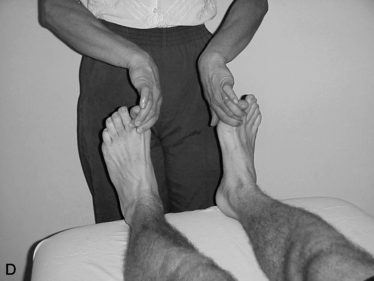

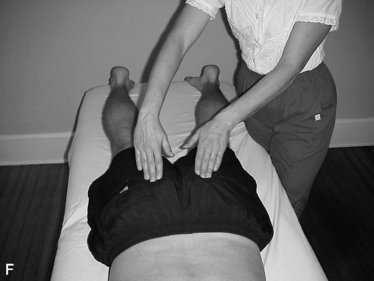

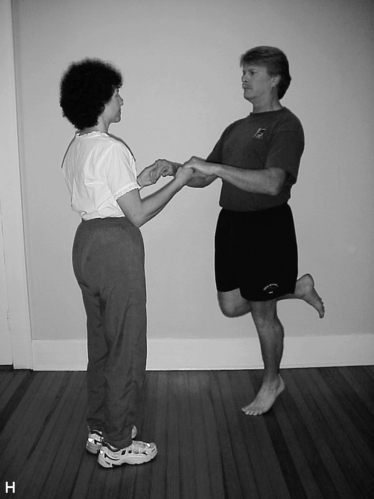
Figure 10.20 Myotome testing for the lumbar and sacral nerve roots. A: L2, hip flexion. B: L3, knee extension. C: L4, foot dorsiflexion. D: L5, extension of the big toe
(adapted from Petty & Moore (1998)). Myotome testing for the lumbar and sacral nerve roots. E: S1, foot eversion. F: S1 contract buttock. G: S1 and S2, knee flexion. H: S2, toe standing (adapted from Petty & Moore (1998)).
+ or 2 = average
• The patella tendon (‘knee jerk’) reflex: the patient is supine.
• The practitioner stands on the side to be tested. The patient’s knee is slightly flexed and supported by the practitioner’s cephalad arm, which rests, palm down, on the patient’s contralateral thigh. The patella tendon is firmly tapped with a reflex hammer to assess the response that, if normal, should involve a moderate extension of the knee.
• The ankle tendon (‘ankle jerk’) reflex: the patient is supine with the leg to be tested flexed at knee and hip and externally rotated at the hip. The practitioner holds the foot in this position to stabilize the leg and a tap is applied (or several taps) to the Achilles tendon with a reflex hammer, approximately 1 inch (2.5 cm) above the insertion into the calcaneus. If pain is noted, or if the normal plantar reflex of the foot does not occur, a rupture of the Achilles tendon should be suspected. If an excessive response is noted an upper motor lesion should be suspected.
Extensor (Babinski) plantar test
In a normal response, when the lateral aspect of the sole of the foot is lightly stroked, the toes will plantarflex. If dorsiflexion of the great toe occurs after the stroke and the other toes spread apart, the test is positive, confirming an upper neuron lesion.
Caution: It should not be assumed that altered reflexes alone confirm spinal root dysfunction. It has been demonstrated that irritation of a (zygapophysial) facet joint (by injection of saline) is capable of altering, and in some instances abolishing, ankle reflexes. The reflex can be restored by injection of steroids.
In order to confirm nerve root involvement, tendon reflex changes as well as sensory and/or motor changes (see tests above) should be present.
Greenough (2009) has summarized the key features of neurological pain deriving from the low back, possibly a result of disc prolapse, or spinal stenosis, as follows:
• There are usually two main symptoms:
• There are usually positive signs from, for example:
• Positive evidence based on imaging is a usual prerequisite (along with the above) before surgery is considered.
It is essential to bear in mind that referred pain from the back is common, and the extent of radiation into the leg is variable. It is quite possible for referred pain to radiate into the calf, the foot and the toes (Figure 10.17C). The common perception that pain below the knee must be secondary to nerve root compression is incorrect, and can lead to inappropriate treatment… If leg pain changes from side to side then it is referred.
Causes of nerve root pain that produces sciatic-type symptoms can include disc prolapse, stenosis of the spine, scar formation or more complex neurological disorders. As a rule, nerve root pain involves pain along the sciatic distribution, down the leg and including the foot (i.e. it is present in definable dermatomes), which is more intense than the accompanying back pain. There is commonly a degree of paresthesia/numbness in the same areas as the pain. Waddell points to a useful distinction that can be made. Most local problems in the lower back affect a single nerve root, with dermatomal numbness or paresthesia, or muscle weakness of a single myotome. If neurological symptoms or signs affect several nerve roots, or both legs, then there may be a more widespread neurological disorder. This may present as unsteadiness or gait disturbance.
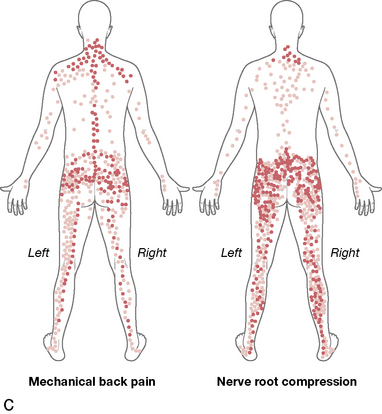
C Composite of body maps of pain, completed by patients with mechanical back pain and with nerve root compression.
Taken from Figure 1 page 302: Greenough C 2009 Degenerative disc and vertebral disease - Clinical Surgery 27 (7):301–305.
(See Box 10.5 for details of a sequence of neurological evaluation.)
One of the clearest signs of neural involvement in low back/sciatic pain is the straight leg raising test (see Box 10.5, p. 238), which aggravates and/or reproduces the painful symptoms.
Distortions and anomalies
If abnormal structural features are noted on examination, such as scoliosis or marked kyphosis, it is important to observe whether this remains evident during prone positioning.
• If it does not remain in prone positioning, i.e. the spinal distortion reduces or normalizes when the patient lies face down, then it represents muscular contraction/spasm. A true scoliosis will remain evident even under anesthetic.
• If it does remain in prone positioning, the cause may be structural or may be muscular, since a long-term, fixated, muscularly induced scoliosis may also remain in non-weightbearing positions.
Serious spinal pathology
A wide range of conditions can produce low back pain as part of their symptomatology. A selection of some of the most important is given in Box 10.1. Waddell (1998) suggests that the patient presenting with low back pain should be a cause for concern if any combination of the following ‘red flag’ features are reported or noted (see Box 10.1).
• The patient is patently unwell and/or reports a loss of weight in association with the back pain. A background history that involves carcinoma, tuberculosis, rheumatological disorders or other systemic diseases, use of steroid medication, drug abuse or a diagnosis of being HIV positive should arouse suspicion when accompanied by a backache.
• The patient reports that there is also thoracic pain present. Waddell (1998) points out that most mechanical problems affecting the back produce symptoms in the low back or neck. ‘Pain in the thoracic spine or between the shoulder blades is less common and, when it does occur, it is more likely to be due to serious pathology (such as an osteoporotic collapse of a vertebra).’*
• The symptoms follow a road traffic accident (see Chapter 4) or any other severe trauma. Detailed assessment should be carried out to establish whether trauma has resulted in fractures or other posttraumatic after-effects.
• There are widespread neurological symptoms, calling for immediate referral to an expert in that field.
• The patient is under 20 or over 55 at presentation or was within these age parameters at the onset of the condition. When low back pain manifests in children or teenagers, caution should be exercised until anomalies such as spondylolisthesis have been ruled out (see Chapter 5 for discussion of sporting influences on spinal dysfunction, especially in regard to overtraining issues). In older patients who present with low back pain, serious conditions such as osteoporosis or metastasis should be considered.
• The back pain is constant or progressively severe and is apparently unrelated to mechanical influences (i.e. still present at rest).
Tests that may be called for include X-ray to rule out, for example, the presence of spondylolisthesis or whether any bone damage such as a vertebral collapse has occurred or whether there is evidence of carcinoma (see Box 10.6). Additionally, it is useful to establish the erythrocyte sedimentation rate (ESR) which, if greater than 25, suggests the presence of an ongoing inflammatory disorder.
Box 10.6 X-ray: usefulness and dangers
According to Paris (1997): ‘X-rays have, in all but a few instances, lost their validity as a diagnostic tool, being used more to prove a bias rather than being a true investigative method. Back pain when relieved rarely if ever changes the X-ray [image].
Waddell (1998) informs us that: ‘Standard X-rays of the lumbar spine involve about 120 times the dose of radiation [required] for chest X-ray’ and should only be used if clear evidence suggests a need. He elaborates further: ‘It is important to remember that serious pathology can exist in the presence of normal X-rays. It takes time for such disease processes to produce bony destruction and false-negative X-rays are common in the early stages of both tumour and infection’. Waddell advises following the Royal College of Radiologists guidelines (see below) when considering use of plain X-rays.
According to the guidelines of the US Department of Health Care Policy and Research (AHCPR 1994), the routine use of X-rays is not recommended unless a red flag is noted because of radiation risks. The instances in which AHCPR do recommend use of X-rays are:
• to rule out fracture in anyone with acute low back pain if there has been recent significant trauma, or recent mild trauma in individuals over the age of 50, or a history of steroid use, or osteoporosis, or in anyone over 70
• plain X-rays are suggested together with complete blood count and erythrocyte sedimentation rate, to rule out tumor or infection for individuals with acute low back pain if any of the following red flags are present: prior cancer or recent infection; fever over 100°F; intravenous drug abuse; prolonged steroid use; low back pain which is worse on resting; unexplained weight loss
• in such cases, if plain X-rays are negative, alternative investigations using bone scan, CT or MRI may be useful (but not during pregnancy).
The British Royal College of Radiologists guidelines are very similar (RCR 1993) and suggest that acute back pain usually results from conditions that are not diagnosable by means of X-ray, with pain correlating poorly with the severity of changes noted on radiology. X-ray investigation is suggested only if symptoms are getting progressively worse or are not resolving or if there are marked neurological signs (sphincter or gait disturbances or motor loss) or a history of trauma.
The stabilizing role of thoracolumbar fascia (Fig. 10.21)
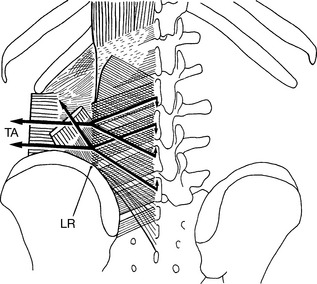
Figure 10.21 The mechanics of the thoracolumbar fascia. From any point in a lateral raphe (LR), lateral tension in the posterior layer of the thoracolumbar fascia is transmitted upward through the deep lamina of the posterior layer and downward through the superficial layer. Because of the obliquity of these lines of tension, a small downward vector is generated at the mid-line attachment of the deep lamina, and a small upward vector is generated at the mid-line attachment of the superficial lamina. These mutually opposite vectors tend to approximate or oppose the separation of the L2 and L4, and L3 and L5 spinous processes. Lateral tension on the fascia can be exerted by the transversus abdominis (TA) and to a lesser extent by the few fibers of the internal oblique when they attach to the lateral raphe
(reproduced with permission from Bogduk (1997)).
Fascia envelops, weaves, supports and provides form to the many tissues of the body, including myofascial, skeletal and organ. In the lumbar region, three layers of thoracolumbar fascia combine to envelop the muscles of the region and to separate them into compartments. The fibers of several lumbar muscles, as well as abdominal muscles, invest into this fascial network to fulfill a strong biomechanical and stabilizing role for the lumbar spine. In describing the three layers of fascia, Bogduk (2005) notes the following characteristics.
Posterior layer
• Covers the muscles of the back from the lumbosacral region through the thoracic region as far as the splenii
• Has a cross-hatched appearance due to two laminae
• Arises from the spinous processes of the lumbar vertebrae
• Wraps around the back to blend with the other layers
• Along the lateral border of iliocostalis lumborum the fascial union is very dense, forming the ‘lateral raphe’
• At sacral levels, extends from the mid-line to the posterior superior iliac spine and the posterior segment of the iliac crest
• Fuses with aponeurosis of both erector spinae and gluteus maximus.
Regarding this important fascia and the role it plays, Cailliet (1995) comments:
The erector spinae muscles…cannot generate sufficient movement to lift objects exceeding 35 kg [approximately 77 lbs]. Thus, in lifting heavy objects, tissues other than the erector spinae muscles must be brought into play. The ligaments or fascia must be considered along with the major muscles groups being involved…Intracompartmental pressure within the fascial sheaths is also considered a factor unloading the spine and explains the value of strong abdominal muscles, especially the obliques, which insert on the fascia of the erector spinae muscles. By their attachment to the fascia, they laterally elongate the fascia, making a stronger extensor component. They also stiffen the fascia, increasing the intracompartmental pressure.
Cailliet has pointed to an efficient system by which the body can employ numerous tissues to perform the task, including distant muscles, via the fascial system. (See Box 10.4 for discussion on lifting.)
When viewed in horizontal section (Fig. 10.22), the tensional elements are readily seen to fall into three groups: the posterior muscles, the deep abdominal muscles and the muscles of the abdominal wall (Kapandji 1974).
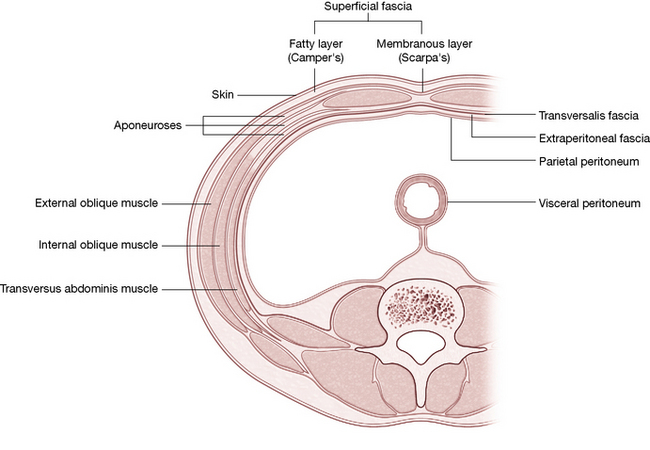
Figure 10.22 The trunk muscles (seen in horizontal section) tensional elements fall into three groups: the posterior muscles, the deep abdominal muscles and the muscles of the abdominal wall.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
• The posterior muscles lie in three planes (layers), which are discussed here (and treated later) from superficial to deep. The superficial plane consists of the latissimus dorsi and its thick accompanying lumbar fascia. The intermediate plane consists of the serratus posterior inferior. The deep plane is composed, from medial to lateral, of multifidus and rotatores (of the transversospinalis muscle group), the longissimus, the spinalis (which lies posterior to the transversospinalis) and, most laterally, the iliocostalis. The deepest layer is collectively called the paravertebral muscle group since their large fleshy mass fills the paravertebral gutters (lamina).
• The deep abdominal muscles consist of the quadratus lumborum, which lies immediately lateral to the spine, and the psoas, which lies anterior to the spine. Among the many tasks that they perform, these muscles serve as powerful stabilizers during upright posture.
• The muscles of the abdominal wall consist of the rectus abdominis anteriorly and, laterally from superficial to deep, the external oblique, internal oblique and transversus abdominis. The rectus abdominis is ensheathed by fascia which arises from the obliquus internus and which joins at the anterior mid-line to form a dense, solid raphe of supporting fascia – the linea alba.
Using assessment protocols
The previous chapter covered the characteristic concepts of NMT and how it is possible (in fact, necessary) to interweave the gathering of information with treatment protocols. As the practitioner becomes more familiar with the treatment steps offered in these technique chapters, the appropriate degree of pressure from the contact digit or hand, as well as the steps to perform to assess and treat each tissue, will become second nature.
The authors suggest that where the tissues being assessed and treated are particularly tense, restricted and/or indurated, the prior use of applied heat (if appropriate), positional release methods, myofascial release, muscle energy techniques or other mobilization and movement therapies (if tolerated) can reduce superficial hypertonicity sufficiently to allow better access for exploring, assessing, localizing and, ultimately, treating the dysfunctional tissues.
Note: Although outside the scope of practice of many practitioners, it is necessary to list HVLA thrust manipulation as also producing a release of excessive tone in all muscles attaching to a manipulated joint (Gibbons & Tehan 2000, Lewit 1985, Liebenson 2007).
This physiological response is commonly used in chiropractic and osteopathic treatment to effect the short-term release of hypertonicity, which a variety of soft tissue approaches achieve via other means. We feel that soft tissue methods are potentially less invasive, as well as being at least as efficient as HVLA thrust techniques in achieving normalization of dysfunction in most instances that involve joint restriction. Clinical experience suggests that where joint blockage exists, soft tissue causes are more frequent than situations where intraarticular restrictions are the primary factor, and where HVLA thrust methods might be presumed to have an advantage.
Sequencing
Sequencing is an important element in bodywork. What should be treated first? Where should treatment begin? How much should be done? To some extent the answer to these questions remains a matter of experience and preference and is based upon what each case particularly requires. However, in many instances, protocols and prescriptions based on clinical experience – and sometimes research – can be of significant value. Several concepts relating to sequencing may usefully be kept in mind when addressing dysfunctions from an NMT perspective. Most of these thoughts are based on the clinical experience of the authors and those with whom they have worked and studied.
• Superficial muscles should be addressed before deeper layers (i.e. the erector spinae should receive therapeutic attention before attempting to treat multifidi).
• The proximal portions of an extremity should be released before the distal portions (i.e. the thigh region would be treated before the lower leg).
• The portion of the spinal column from which innervation to an extremity emerges should receive attention at the same time as the extremity (i.e. the lumbar spine would be treated when the lower extremity is addressed).
• A reclining (prone, supine or sidelying) position for the patient reduces the muscle’s weight-bearing responsibilities and is usually preferred over upright postures (sitting or standing), although upright postures can be used in some instances and are essential when using SNAG (sustained natural apophyseal glide) protocols, as described in this and later chapters (see Box 10.3). Additionally, upright posture is clearly essential in most rehabilitation and reeducation-of-use protocols.
• Alternative body positions, such as sidelying postures, may be substituted when appropriate, although they are not always described in this text.
• If NMT is to be applied to an area that is particularly tense, restricted or sensitive, the practitioner may choose to initially utilize:
• Or these (or other) approaches (all of which are described in appropriate segments of this text and its companion volume) may be used subsequent to or interspersed with NMT evaluation and treatment.
The methods of NMT assessment and treatment, seamlessly merged with a variety of methods, techniques and modalities (ultrasound, hydrotherapy, acupuncture, ice, heat, relaxation methods, etc.), provide the modern clinician with an abundant set of resources with which to handle somatic dysfunction.
Note: The instructions in this text are given for the right side of the body and are simply reversed for the other side. In clinical application, both sides of spinal muscles should always be treated to avoid instability and reflexive splinting, which may occur if only one side is addressed.
Lumbar spine assessment protocols
There is an ongoing debate as to what constitutes ‘normal’ range of joint motion and what influences abnormal behavior of joint movement. The lumbar area is no exception to this tendency, with disagreement expressed as to the mean values of movement and also as to the actual value of such information. Regarding the lumbar spine, Bogduk (2005) notes: ‘Total ranges of motion are not of any diagnostic value, for aberrations of total movement indicate neither the nature of any disease nor its location’. He does, however, acknowledge that there is potential value in comparing movement ranges of various age groups or degenerative conditions and attributes greater potential diagnostic significance to the range of movement of individual lumbar intervertebral joints than to the spine as a whole. There seems to be a wide range of responses in the entire lumbar spine, and at individual segments, to conditions such as non-specific low back pain (normal extension, reduced flexion, increased side-bending and rotation –termed coupling), nerve root tension (reduced flexion and normal coupling) and disc herniation (reduced ranges in all segments but increased coupling in segment above herniation). Bogduk (2005) suggests that such ranges of movement, demonstrated radiographically, are not sufficiently distinctive to allow a diagnosis to be made based on this method of assessment.
Petty (2006) notes that the quality of active movement is of primary importance and suggest that movements be repeated several times to provide a clearer picture of performance than that which single movements can provide. It is also suggested that the speed of movement can be altered, various movements can be combined (flexion then lateral flexion or lateral flexion with flexion, etc.), movements can be sustained and that compression or distraction can be added during the assessment. They advise that for both active and passive physiological joint movement, the clinician should note the following:
• the behavior of pain through the range of movement
• the resistance through the range of movement and at the end of the range of movement
While the precise range of motion of the lumbar spine will remain a matter of debate and a topic of interest, the gathering of information as listed above from a variety of lumbar movements will be invaluable to the practitioner in determining which muscles and/or joint segments may be involved in a particular condition and, therefore, which treatment applications will be most suited for that patient. Among those movements with diagnostic value, Petty lists and illustrate the following to be tested.
• Flexion (both single and repetitive, performed in both standing and supine positions)
• Extension (both single and repetitive, performed in both standing and prone positions)
• Lateral flexion (to the left and to the right)
• Rotation (to the left and to the right) – performed seated
• Left quadrant (combines extension, left rotation and left lateral flexion) – performed seated
• Right quadrant (combines extension, right rotation and right lateral flexion) – performed seated
• Side gliding in standing (both singular and repetitive, performed to each side).
Observation of ‘C’ curve
A broad ‘snapshot’ of current flexion potential in the lumbar spine is achieved by having the patient adopt a standing and then a seated flexion position. A profile view of what should be a ‘C’-shaped curve provides a first view of segments where flexion is absent or deficient. The ideal, ‘normal’ result should demonstrate that a sequential degree of flexion has occurred at each segment, producing a ‘C’ curve with no ‘flat’ areas. Flatness suggests an inability to flex at that segment, due to intrasegmental, intersegmental or soft tissue dysfunction.
The influence of musculature, such as the hamstrings on pelvic and lumbar spinal flexion potential, is noted by comparing the seated and standing flexion ranges. The ability of the pelvis to rotate anteriorly during flexion will be influenced by shortening of the posterior spinal muscles and/or the musculature and fascia of the calf and thigh. Bilaterally shortened hamstrings reduce the potential for the pelvis to rotate anteriorly during seated spinal flexion with legs fully extended, maintaining it in (or encouraging it toward) posterior rotation (and counternutation), together with a tendency for the knees to flex. See a detailed description of the ‘C’ curve evaluation in the discussion of the erector spinae group on p. 262 and Figure 10.36.
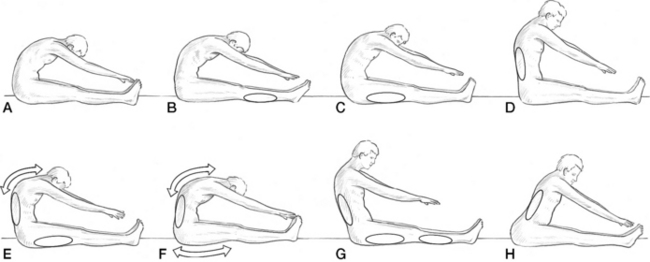
Figure 10.36 Tests for shortness of the erector spinae and associated postural muscles. A: Normal length of erector spinae muscles and posterior thigh muscles. B: Tight gastrocnemius and soleus; the inability to dorsiflex the feet indicates tightness of the plantarflexor group. C: Tight hamstring muscles, which cause the pelvis to tilt posteriorly. D: Tight low back erector spinae muscles. E: Tight hamstrings; slightly tight low back muscles and overstretched upper back muscles. F: Slightly shortened lower back muscles, stretched upper back muscles and slightly stretched hamstrings. G: Tight low back muscles, hamstrings and gastrocnemius/soleus. H: Very tight low back muscles, with the lordosis maintained even in flexion
(reproduced with permission from Chaitow (2010)).
Evidence of rotoscoliosis
When the spine is in seated or standing flexion a perspective can be obtained that views the flexed spine from an anterior or posterior position, providing evidence of any rotoscoliosis that might exist. If this is demonstrated in the standing position it suggests a possibly uneven sacral base. If the spinal rotoscoliosis occurs in the seated position it suggests spinal causes (Fig. 10.23).
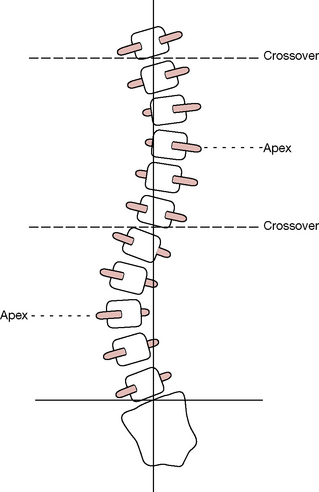
Figure 10.23 Posterior view of spine showing rotoscoliosis involving both rotation and sidebending of the lumbar and thoracic spines, possibly in response to an uneven sacral base (if standing) or intrinsic spinal causes (if seated)
(adapted from Mitchell et al (1979)).
Lumbar spine myofascial elements
As examination of the lower back begins, inspection of the skin and subcutaneous tissue may reveal evidence of a variety of unusual tissue states. Hoppenfeld (1976) notes the following and their possible pathological causes.
• A patch of hair may be evidence of underlying bony pathology.
• Patchy (‘blotchy’), reddened discoloration could indicate infection or improper or excessive use of a heating pad or hot water bottle.
• Soft, doughy lumps in the area of the lower back may be the fatty masses of a lipoma (sometimes associated with spina bifida), which may impinge on spinal cord or nerve roots.
• Skin tags and skin discolorations may be indicative of neurofibromatosis.
• Birth marks and port wine marks may be suggestive of underlying bony pathology, such as spina bifida.
In preparation for palpation and treatment of individual muscles, techniques that soften the superficial fascia as well as offering some assessment potential of underlying conditions can be usefully employed. For instance, bindegewebsmassage (connective tissue massage, skin rolling), can be applied to the dry skin of the lumbar and sacral areas. Areas where the skin appears to be ‘stuck’ to the underlying tissue, and/or which display a sense of ‘drag’ (indicating increased sympathetic activity and consequent increased hydrosis/tissue moisture/sweat) when a single digit is very lightly stroked across it, are all exhibiting evidence of underlying dysfunction, such as a myofascial trigger point or an area of facilitation (Lewit 1999). These practical assessment concepts are fully described in Volume 1, Chapter 6. (See also Fig. 10.24 in this text.)
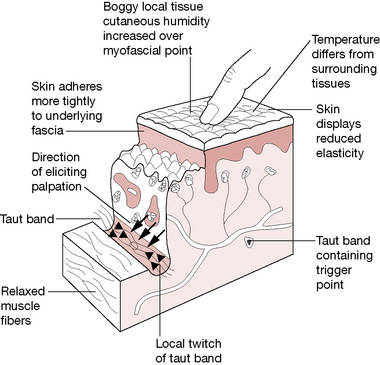
Figure 10.24 Altered physiology of tissues in region of myofascial trigger point
(reproduced with permission from Chaitow & DeLany (2008)).
Repetitive rolling of the skin between the fingers and gentle, sustained skin traction will offer mechanical distress to the fascial content, which usually results in a softening of the fascia and a release of the fascial restriction. Less invasively and far more comfortably, Lewit (1999) has noted that using two finger pads to simply hold apart (to its current elastic barrier for up to 30 seconds) tense skin which overlies dysfunctional tissues (such as a trigger point) produces a slow release, loosening both the skin and underlying fascial component and beginning the deactivation process (a ‘mini-myofascial release’).
Two-handed, crossed-arm myofascial release (MFR) can be applied in vertical, horizontal or diagonal patterns and sustained for several minutes or until the fascia softens and lengthens. MFR techniques are particularly responsive (and the length of application time may be significantly diminished) if MFR is used after applications of skin rolling or other procedures that are thought to provoke the gel state of the ground substance of fascia to return to sol, a more liquid (‘solate’) state. MFR procedures are, however, difficult to employ immediately after heat applications due to prolonged sweating, which causes loss of traction on the skin and slippage of the hands.
Other methods that will produce similar changes in indurated, congested, hypertonic soft tissues include variations of MET, which involve use of isometric and isotonic eccentric contractions as precursors to subsequent stretching/lengthening procedures. Additionally NMT, in its treatment mode, using a variety of massage strokes, ischemic compression and cross-fiber work, can beneficially modify localized restricted structures in a very precise manner (see Volume 1, Chapter 1 for more details on connective tissue).
Lumbar spine NMT treatment protocols
Latissimus dorsi (Fig. 10.25)
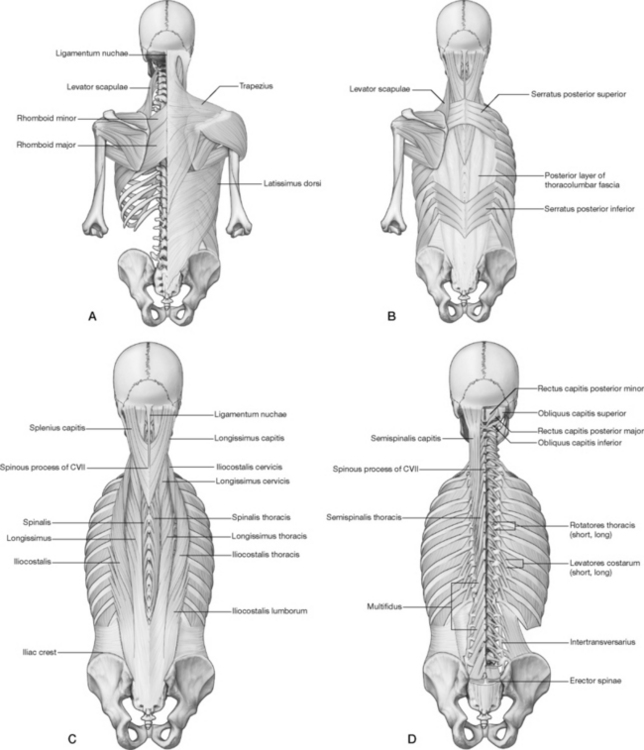
Figure 10.25 Superficial and deeper muscles of the cervical, thoracic and lumbar regions.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Attachments: Spinous processes of T7–12, thoracolumbar fascia (anchoring it to all lumbar vertebrae and sacrum), posterior third of the iliac crest, 9th–12th ribs and (sometimes) inferior angle of scapula to the intertubercular groove of the humerus
Innervation: Thoracodorsal (long subscapular) nerve (C6–8)
Muscle type: Postural (type 1), shortens when chronically stressed
Function: Medial rotation when arm is abducted, extension of the humerus, adduction of the humerus, particularly across the back, humeral depression; influences neck, thoracic and pelvic postures and forced exhalation, such as when coughing (Platzer 2004)
Synergists: Medial rotation: teres major, pectoralis major, subscapularis, biceps brachii
Extension of humerus: teres major and long head of triceps
Adduction of humerus: most anterior and posterior fibers of deltoid, triceps long head, teres major, pectoralis major Depression of shoulder girdle: lower pectoralis major, lower trapezius, possibly serratus anterior and pectoralis minor
Antagonists: To medial rotation: teres minor, infraspinatus, posterior deltoid
To extension of humerus: pectoralis major, biceps brachii, anterior deltoid
To humeral head distraction: stabilized by long head of triceps, coracobrachialis
To depression of shoulder girdle: scalenes (thorax elevation), upper trapezius
Special notes
Portions of the latissimus dorsi attach to the lower ribs on its way to the lower back and pelvic attachments. The latissimus dorsi powerfully depresses the shoulder and therefore can influence shoulder position and neck postures as well as pelvic and trunk postures by its extensive attachments to the lumbar vertebrae, sacrum and iliac crest (Simons et al 1999). Though its primary function is humeral movement, its extensive connection into the lower back and its coverage of the deeper back muscles warrant its consideration with the lumbar region.
Vleeming et al (2007, 1995) support concepts that latissimus dorsi and gluteus maximus contribute significantly to the thoracolumbar fascia and thereby create a ‘posterior sling’. They suggest that both increase tension within that fascia (ipsilaterally and contralaterally) and, by ‘cinching’ the fascia, can stiffen the lumbar spine and offer stability, particularly in regards to translatory movement between vertebrae and for force closure of the SI joint. Conversely, Bogduk et al (1998) clearly suggests that the latissimus dorsi moves the arm and raise the trunk in brachiation. ‘Its possible contribution to extension of the lumbar spine is trivial as is its capacity to brace the sacroiliac joint.’
Simons et al (1999) note that Dittrich (1954) illustrates and discusses conditions of fibrous tissue pathology and tears of the lumbodorsal fascia and subfascial fat, in low back pain patients. Dittrich attributed the damage to excessive tension of latissimus dorsi.
Latissimus dorsi can place tension on the brachial plexus by depressing the entire shoulder girdle and should always be addressed when the patient presents with a very ‘guarded’ cervical pain associated with rotation of the head or shoulder movements (Chaitow & DeLany 2008). This type of pain often feels ‘neurological’ when the tense nerve plexus is further stretched by neck or arm movements. Relief is often immediate and long lasting when the latissimus contractures and myofascial restrictions are released, especially if they were ‘tying down’ the shoulder girdle. If latissimus dorsi is short it tends to ‘crowd’ the axillary region, internally rotating the humerus and impeding normal lymphatic drainage (Schafer 1987).
Contributions from latissimus dorsi are routinely used in breast cancer reconstruction (Vetto et al 2009), for repairs in the shoulder region (Kim et al 2009), and for tissue replacement of burn patients (Danino et al, in press).
Dowling (1991) reports that latissimus dorsi is an accessory breathing muscle and that it ‘may play a role in either expiration or inspiration, depending on the fixed position of the arm’.
Michael Kuchera (1997a) offers a reminder of the vital role of latissimus dorsi in sacroiliac stability (Fig. 10.26).
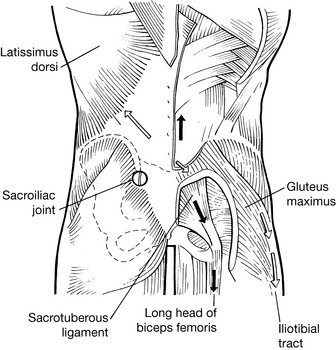
Figure 10.26 Schematic dorsal view of lower back displays continuity of longitudinal muscle-tendon-fascial sling, involving biceps femoris, sacrotuberous ligament and erector spinae, which provide a vertical tensional element. Gluteus maximus, thoracolumbar fascia and contralateral latissimus dorsi provide diagonal tension, which contributes to stabilization of the SI joint
(reproduced with permission from Vleeming et al (2007)).
Posturally induced stress disturbs stability by causing imbalance in the four major muscles involved in force closure [of the SI joint during the gait cycle – see Chapters 3 and 11]: the erector spinae, gluteus maximus, latissimus dorsi and biceps femoris.
Assessment for latissimus dorsi shortness/dysfunction (Fig. 10.27)
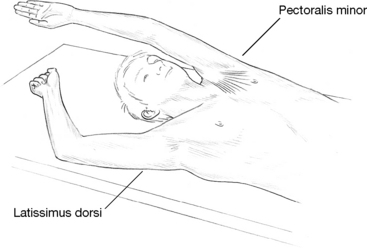
Figure 10.27 The right arm deviation suggests probable latissimus dorsi shortness, although teres major involvement is also possible. The left arm also shows loss of range due to pectoral shortening
(reproduced with permission from Chaitow (2006)).
• The patient lies supine, knees flexed, with the head 1.5 feet (45 cm) from the top edge of the table and extends the arms above the head, resting them on the treatment surface with the palms facing upward.
• If latissimus is normal, the arms should be able to easily lie flat on the table above the shoulder. If the arms are held laterally – elbow(s) pulled away from the body – then latissimus dorsi is probably short on that side.
• The standing patient is asked to flex the torso and allow the arms to hang freely from the shoulders as he holds a half-bent position, trunk parallel with the floor. It is commonly more comfortable for the low back patient to stoop than to stand upright, as noted in positional release methodology (Jones 1981). If, however, this position proves uncomfortable the supine test should be used.
• The arms are allowed to hang freely, palms facing each other. In doing so, if the arms hang other than perpendicular to the floor some muscular restriction can be assumed.
• If this involves latissimus dorsi, the arms will be held closer to the legs than perpendicular (alternatively, if they hang markedly forward of such a position, then trapezius or deltoid shortening is possibly involved).
• To assess for latissimus shortness in this position (one side at a time), the practitioner stands in front of the patient (who remains in this half-bent position). While stabilizing the scapula with one hand, the practitioner grasps the arm, just proximal to the elbow, and gently draws the (straight) arm forward.
• If there is not excessive ‘bind’ in the tissue being tested, the arm should easily reach a level higher than the back of the head.
• If this movement is not possible, the latissimus is probably shortened, although it is possible that teres major and/or pectoralis major could also be implicated.
NMT for latissimus dorsi
• The patient lies in the prone position with the arm at 90° of horizontal abduction, elbow bent and with the humerus in lateral rotation so that the hand rests on the table surface near the head or on the face rest. The position of the arm can be varied to hang off the table and be placed into medial rotation, depending upon tautness of the fibers that will influence the practitioner’s ability to grasp them. (A sidelying position for treating latissimus dorsi is shown in Volume 1, Chapter 13, and a supine position is also possible.)
• The practitioner stands at the head end of the table and uses her ipsilateral hand to grasp the portion of latissimus dorsi that comprises most of the free border of the posterior axillary fold (about mid-scapular level). The practitioner could stand at the side of the table, however, that position tends to place the dorsal surface of the fingers more snugly against the lateral surface of the breast of female patients, which can be avoided by using the cephalad position.
• Pincer compression is used to grasp, compress and/or roll the tissue between the fingers and thumb while examining for taut fibers and dense, nodular tissue.
• Beginning near the posterior axillary fold, the practitioner assesses the latissimus dorsi’s long fibers at hand-width intervals until the rib attachments are met. These outer fibers ‘tie’ the humerus to the lower ribs. Ischemic bands are often found in this portion of the muscle and central trigger points are found at mid-fiber region of this most lateral portion of the muscle, which is approximately halfway between the humerus and rib attachments (Fig. 10.28).

Figure 10.28 Latissimus dorsi shortness can affect lower back, ribs, shoulder position and may affect the cervical region. The long fibers of latissimus dorsi are available in prone (shown here), sidelying or supine positions.
• By repositioning the arm closer to the patient’s head or closer to the torso, the practitioner can place the muscle fibers in a more stretched or more relaxed position, depending upon the patient’s comfort and the tissue’s response to the stretch component. A more relaxed position will allow the fibers to be more easily picked up, manually tractioned or manipulated, whereas a more elongated position will make the taut fibers of a trigger point band more palpable and possibly more responsive to compression treatments due to the applied tension on the actin and myosin components.
• The practitioner’s pincer grasp applied at mid-fiber region can be slid along taut fibers in search of trigger points, which will palpate as more dense, more tender or as nodular tissues. When a trigger point is located, exquisite tenderness and the patient’s report of a referral pattern will indicate the need for treatment.
• Applied compression that matches the tension found in the tissues should provoke a moderate discomfort and should be maintained for approximately 8–12 seconds, during which time the discomfort at the palpation site as well as within the target zone should begin to subside (see Chapter 9 for trigger point treatment descriptions). This compression technique is applied several times with a brief lapse of time in between and is followed by stretching of the latissimus fibers. Passive stretch is repeated several times and can be followed by active range of movement, which should also be given as ‘homework’.
• The attachments onto the spinous processes, ribs, sacrum and iliac crest may be addressed with friction, gliding strokes or static pressure, depending on tenderness level. The beveled pressure bar or finger tips (when more tender) can be used to apply friction or static pressure techniques onto the rib attachments, throughout the lamina groove (Volume 1, Fig. 14.20) and on the sacrum (Fig. 11.73, p. 377) while thumbs are best used along the top of the iliac crest.
• Trigger points found in latissimus dorsi refer to the mid-thoracic region, the inferior angle of the scapula and down the medial aspect of the arm, forearm and hand as well as the anterior shoulder and lateral trunk (Simons et al 1999) (see Volume 1, Fig. 13.51).
MET treatment of latissimus dorsi ‘banana stretch’ (see Volume 1, Fig. 13.56)
• The patient lies supine with the ankles crossed.
• The table should be adjusted so that the patient lies at roughly the height of the practitioner’s upper abdomen.
• With the legs straight, the patient’s feet are placed just off the side of the table to help anchor the lower extremities.
• The practitioner stands at waist level on the side opposite the side to be treated and faces the table.
• The patient slightly sidebends the torso contralaterally (bending toward the practitioner).
• The patient places the ipsilateral arm behind his neck as the practitioner slides her cephalad hand under the patient’s shoulders to hold the axilla on the side being treated. The patient then grasps the practitioner’s arm at the elbow.
• Depending upon the length of the patient’s arms, as well as body shape, it may be possible for the patient to interlink hands with the practitioner’s hand, which is close to the axilla, thereby offering a greater degree of stability in subsequent lifting and stretching procedures.
• The practitioner’s caudad hand is placed lightly on the anterior superior iliac spine on the side to be treated, in order to offer stability to the pelvis during the subsequent contraction and stretching phases.
• The patient is instructed to very lightly take the point of the treatment side elbow toward his sacrum as he also lightly tries to bend backwards and toward the treated side. The practitioner resists this effort with the hand at the axilla, as well as the forearm that lies across the patient’s upper back. This action produces an isometric contraction in latissimus dorsi.
• After 7 seconds the patient is asked to relax completely as the practitioner, utilizing body weight and weight transference from front leg to back, sidebends the patient further and, at the same time, straightens her own trunk and leans caudad, effectively lifting the patient’s thorax from the table surface and so introducing a stretch into latissimus (as well as quadratus lumborum and obliques).
• This stretch is held for 15–20 seconds, which allows a lengthening of shortened musculature in the region.
• These steps are repeated once or twice more for greatest effect (See Volume 1, Fig. 13.56.).
PRT for latissimus dorsi 1 (most suitable for acute problems)
• The patient is supine (although it is possible to produce a similar effect with patient prone) and lies close to the edge of the table. The practitioner is tableside, at waist level, facing cephalad (see Volume 1, Fig. 13.57)
• Using her tableside hand, the practitioner searches for, and locates, an area of marked localized tenderness on the upper medial aspect of the humerus, where latissimus attaches.
• The patient is instructed to grade the applied pressure to this dysfunctional region of the muscle as a ‘10’.
• The practitioner’s non-tableside hand holds the patient’s forearm just above the elbow and eases the humerus into slight extension, ensuring (by ‘fine tuning’ the degree of extension) that the ‘score’ has reduced somewhat.
• The practitioner then internally rotates the humerus, while also applying light traction in such a way as to reduce the pain ‘score’ more.
• When the score is reduced to ‘3’ or less, the position of ‘ease’ is held for 90 seconds before a slow return to neutral.
• For prone application all the mechanics of the procedure are identical.
PRT for latissimus dorsi 2 (more suitable for chronic problems)
• Patient is sidelying with affected side uppermost (or alternatively prone) and an area of marked sensitivity (tender point) is located in the belly of the latissimus dorsi muscle at roughly T10 level, approximately 5 cm (2 inches) lateral to the spine.
• If sidelying, the patient’s ipsilateral pelvic crest is eased into a slight degree of posterior rotation until the patient reports a slight reduction in the palpated tender point pain (Fig. 10.30). If prone, the ipsilateral pelvic posterior rotation is performed and sustained by placement of a small pad/cushion under the ASIS.

Figure 10.30 Positional release of latissimus dorsi in which the practitioner’s right hand is monitoring the tender point, as the left hand ‘fine tunes’ the patient until an ‘ease’ position is reached
(adapted from Deig (2001)).
• Whether the patient is in prone or sidelying, the ipsilateral arm is then brought into slight extension at the shoulder and is adducted and internally rotated until a marked degree of pain reduction (in the palpated tender point) is reported – without creating any pain elsewhere.
• A final degree of ‘crowding’ of latissimus tissues is achieved by means of light inferomedially directed sustained pressure applied to the shoulder, toward the palpating hand on the tender point, which usually reduces the reported pain to ‘3’ or less.
• This final position of ease should be held for at least 90 seconds before a slow return of the arm and trunk to neutral.
Serratus posterior inferior (see Fig. 10.25b)
Attachments: Spinous processes of T11-L3 and the thora-columbar fascia to the inferior borders of the lower four ribs
Innervation: Intercostal nerves (T9–12)
Muscle type: Phasic (type 2), weakens when stressed
Function: Depresses lower four ribs and pulls them (unilaterally) posteriorly, not necessarily in respiration (Gray’s anatomy 2005), to probably rotate the lower thorax (Simons et al 1999) and to extend the lower thorax when bilaterally activated (Simons et al 1999)
Synergists: For expiration: internal intercostals, quadratus lumborum
For rotation: ipsilateral iliocostalis and longissimus thoracis
For extension: bilateral iliocostalis and longissimus thoracis
Special notes
Several texts note serratus posterior inferior as a respiratory muscle and debate abounds regarding whether it is active on inhalation, apparently to stabilize the ribs against the upward pull of the diaphragm (Clemente 1985, Jenkins 1991, Simons et al 1999), or in exhalation, particularly in forced expiration (Kapandji 1974, Rasch & Burke 1978). Simons et al (1999) note that ‘an electromyographic study found no respiratory activity attributable to the muscle’.
Trigger points in this muscle may produce low backache similar to that of renal disease. While its trigger points and attachments should be treated, kidney disease (or possibly other visceral pathologies) should also be ruled out as a source of viscerosomatic referral, especially when the myofascial pain keeps returning after treatment. The quadratus lumborum muscle, located nearby, should also be examined.
CAUTION: The lower two ribs are ‘floating ribs’, varying in length, and are not attached anteriorly by costal cartilage. The distal ends of the ribs may be sharp, which requires that palpation be carried out carefully. Additionally, excessive pressure should be avoided, especially in patients with known or suspected osteoporosis.
NMT for serratus posterior inferior (see Volume 1, Fig. 14.23)
After dry skin applications of myofascial release prepare the region for NMT palpation, the practitioner’s thumb can be used with light lubrication to glide from the spinous processes of T11-L3 to the attachments of serratus posterior inferior on the lower four ribs or to traverse the fibers. The thumbs can also be used to glide laterally along the inferior aspect of each of the lower four ribs (through the latissimus dorsi fibers). The patient will often report tenderness and a ‘burning’ discomfort as the thumb slides laterally. Repetitions of the stroke usually rapidly reduce the discomfort. Spot tenderness associated with a central trigger point may be found but taut fibers are difficult to feel through the overlying muscles (Simons et al 1999).
See also Boxes 10.7 and 10.11 for details of Lief’s NMT approach to intercostal assessment.
Box 10.11 Lief’s abdominal NMT protocol
Lief’s NMT treatment of the abdominal and related areas focuses largely on specific
Lief’s abdominal NMT application (Fig. 10.59)
In treating the abdominal and lower thoracic regions the patient should be supine with the head supported by a medium-sized pillow and the knees flexed, either with a bolster under them or drawn right up so that the feet approximate the buttocks. Lubricant should be applied to the area being treated.
Intercostal treatment
The practitioner is positioned level with the patient’s waist and a series of strokes are applied with the tip of the thumb, or with a finger tip, along the course of the intercostal spaces from the sternum, laterally (see descriptions of Lief’s thumb and finger techniques in Volume 1, Chapter 9).
It is important that the insertions of the internal and external intercostal muscles receive attention. The margins of the ribs, both inferior and superior aspects, should receive firm gliding pressure from the distal phalanx of the thumb or middle or index finger. If there is too little space to allow such a degree of differentiated pressure then a simple stroke along the available intercostal space should be made.
If the thumb cannot be insinuated between the ribs, a finger (side of finger) contact can be used in which the gliding stroke is drawn toward the practitioner (toward mid-line) from the contralateral side.
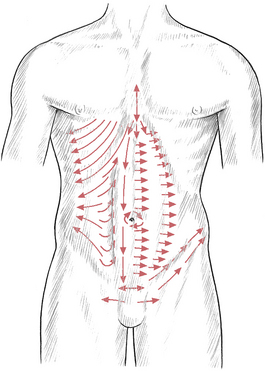
Figure 10.59 Neuromuscular abdominal technique. Suggested lines of application to access primary trigger point attachment sites and interfaces between different muscle groups
(reproduced with permission from Chaitow (2010)).
The intercostals from the 5th rib to the costal margin should receive a series of two or three deep, slow-moving, gliding strokes on each side, with special reference to points of particular congestion or sensitivity. These areas may benefit from up to 30 seconds of firm but not heavy, sustained or variable pressure techniques.
The practitioner should bear in mind the various reflex patterns in the region. Gentle searching of tissues overlying or surrounding the sternum may elicit sensitivity in the rudimentary sternalis muscle, which has been found to house trigger points. It is not necessary for the practitioner to change sides during the treatment of the intercostals unless it is found to be more comfortable to do so.
The practitioner should be facing the patient and be half-turned toward the head with her feet spread apart for an even distribution of weight and with her knees flexed to facilitate the transfer of pressure through the arms. Most of the maneuvers in the intercostal area and on the abdomen itself involve finger and thumb movements of a lighter nature than those applied to the heavy spinal musculature.
Having assessed and, if appropriate, treated the intercostal musculature and connective tissue (including trigger point deactivation, if necessary), the practitioner, using either a deep thumb pressure or a contact with the pads of the finger tips, applies a series of short searching and treating strokes in a combination of oblique lateral and inferior directions from the xyphoid process (see Fig. 10.59).
Lief’s NMT of the rectus sheath
Next, a series of deep slow strokes is applied along and under the costal margins. The costal margin itself, as well as the tissues internal and cephalad to it, require diligent assessment as this is a key attachment location. Whether diaphragmatic attachments can be located is questionable but sustained, firm (but not invasively aggressive) pressure allows gradual access to an area which can reveal trigger points of exquisite sensitivity with virtually unpredictable areas of influence. Many seem to produce sensations internally, while others create sensations in the lower extremities or in the throat, upper chest and shoulders. Deactivation of such triggers needs to be carried out slowly, carefully and with sensitivity.
A series of short strokes (1–2 inches, 2.5–5 cm) with fairly deep but not painful pressure is then applied by the thumb, from the mid-line out to the lateral aspect of the rectus sheath. This series of strokes starts just inferior to the xyphoid and the last lateral stroke concludes at the pubic promontory. This series may be repeated on each side several times depending upon the degree of tension, congestion and sensitivity noted.
A similar pattern of treatment is followed across the lateral border of the rectus sheath. A series of short, deep, slow-moving, laterally oriented thumb strokes is applied from just inferior to the costal margin of the rectus sheath until the inguinal ligament is reached. Both sides are assessed and treated in this way.
A series of similar strokes is then applied first on one side and then the other, laterally from the lateral border of the rectus sheath and onto the oblique abdominal muscles. These strokes follow the contour of the trunk so that the more proximal strokes travel in a slightly inferior curve while passing laterally, while the more distal strokes have a superior inclination that follows the iliac crest, as the hand passes laterally. A total of five or six strokes should complete these movements and this could be repeated before performing the same movements on the contralateral side.
In treating the ipsilateral side, it may be more comfortable to apply the therapeutic stroke via the flexed finger tips which are drawn toward the practitioner, or a thumb stroke may be used. In treating the contralateral side, thumb pressure can more easily be applied, as in spinal technique, with the fingers acting as a fulcrum and the thumb gliding toward them in a series of 2 or 3 inch-long strokes. The sensing of contracted, gangliform areas of dysfunction is more difficult in abdominal work and requires great sensitivity of touch and concentration on the part of the practitioner.
Umbilicus
A series of strokes should then be applied around the umbilicus. Using thumb or flexed finger tips, a number of movements of a stretching nature should be performed in which the non-treating hand stabilizes the tissue at the start of the stroke which firstly runs from approximately 1 inch (2.5 cm) superior and lateral to the umbilicus on the right side, to the same level on the left side. The non-treating hand then stabilizes the tissues at this endpoint of the stroke and a further stretching and probing stroke is applied inferiorly to a point about 1 inch (2.5 cm) inferior and lateral to the umbilicus on the left side. This area is then stabilized and the stroke is applied to a similar point on the right.
The ‘square’ is completed by a further stroke upward to end at the point at which the series began. This series of movements should have a rhythmical pattern so that as the treating hand reaches the end of its stroke, the non-treating hand comes to that point and replaces the contact as a stabilizing pressure while the treating hand begins its next movement. A series of three or four such circuits of the umbilicus is performed.
Linea alba
Additional strokes should be applied along the mid-line, on the linea alba itself, while searching for evidence of contractions, adhesions, fibrotic nodules, edema and sensitivity.
CAUTION: Caution is always required to avoid deep pressure on the linea alba, especially if this muscular interface is weakened by pregnancy, surgery or trauma. It should also be recalled that the linea alba is a place of attachment of the external obliques as well as transversus abdominis (Braggins 2000).
European (Lief’s) NMT for iliac fossa and symphysis pubis
The sheaths of the rectus abdominis muscles (Fig. 10.60), from the costal margins downwards to the pubic bones, are evaluated by finger or thumb strokes. Attention is given to the soft tissue component as well as the insertions into the iliac fossa, the pubic bones and the symphysis pubis, including the inguinal ligament (see Fig. 10.59).
Strokes should be made, commencing at the ASIS, which attempt to evaluate those attachments of internal and external obliques and transversus abdominis that can be contacted.
A deep but not painful stroke, employing the pad of the thumb, should be applied to the superior aspect of the pubic crest. This stroke should start at the symphysis pubis and move laterally, first in one direction and, after repeating it once or twice, then the other direction. A similar series, starting at the center and moving laterally, should then be applied over the anterior aspect of the pubic bone. Great care should be taken not to use undue pressure as the area is sensitive at the best of times and may be acutely so if there is dysfunction associated with the insertions into these structures. A series of deep slow movements is then performed, via the thumb, along the superior and inferior aspects of the inguinal ligament, starting at the pubic bone and running up to the iliac crest.
In this lower abdominal area, close to the ASIS and toward the umbilicus, many of the tender points associated with flexion strains of the lumbar and lower thoracic spine may be located. Positional release methods should be employed to relieve the dysfunctional patterns associated with these (see Volume 1, Chapter 10, as well as specific discussion of PRT in this chapter on p. 286 relating to the abdominal musculature).
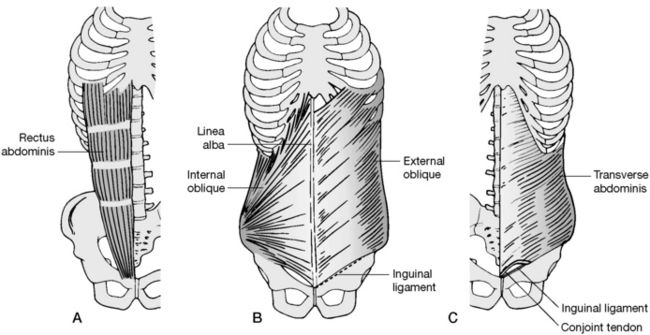
Figure 10.60 A: Rectus abdominis. B: Right internal and left external obliques. C: Left transversus abdominis
(adapted from Braggins (2000) with permission).
The thumbs or fingertips may then be insinuated beneath the lateral rectus abdominis border at its lower margins and deep pressure applied toward the mid-line. The hand or thumb should then slowly move cephalad in short stages while maintaining this medial pressure. This lifts the connective tissue from its underlying attachments and helps to normalize localized contractures and fibrous infiltrations.
A soothing series of massage strokes should complete attention to this vital and sensitive region.