Common disorders of the leg
Circulatory issues including intermittent claudication, restless legs and cramp
Intermittent claudication (IC) refers to cramp-like leg pains, usually affecting the calf muscles. The symptoms are caused by poor arterial circulation (peripheral arterial disease, or PAD) to the leg muscles during exercise, often limiting the individual’s ability to walk more than a short distance. The symptoms are usually relieved by rest.
Cycling and IC (Callaghan 2005)
Aggravating factors related to cycling that may contribute to IC include a mixture of prolonged, repetitive hip flexion, possibly causing trauma to the external iliac artery flow to the lower limbs. There may also be an element of anatomical variation such as extra arterial branches, excessive arterial lengthening, a hypertrophic psoas muscle or associated metabolic disorders such as diabetes mellitus (Schep et al 2002).
Restless leg, cramp & pregnancy (Hensley 2009)
Sleep disturbance is common during the third trimester of pregnancy.
Two under diagnosed sleep disorders commonly experienced by women in the third trimester include leg cramps (LCs) and restless legs syndrome (RLS). LCs may be experienced by up to 30% of pregnant women and RLS by up to 26%. Both usually occur at night, may be described as a ‘cramping’ sensation in the lower leg, which is usually relieved by movement. Leg cramps are most often relieved by dorsiflexion of the foot of the affected leg. RLS is most often relieved by walking.
Although the evidence is weak, the best treatment for LCs during pregnancy appears to be taking supplemental magnesium before bed (Young & Jewell 2002). No evidence exists as to benefits from supplemental calcium, or nighttime leg stretching exercises.
Medical treatment of PAD/IC (Martinez et al 2009)
• lifestyle modification – including smoking cessation
• medications such as aspirin (anti-platelet therapy) and statins (lipid-lowering agents)
• anti-hypertension and diabetic therapy
• surgical procedures (bypass, percutaneous transluminal angioplasty, and iliac and femoral artery stents)
• exercises such as walking, as well as resistance training.
Adjunctive approaches: stretching and exercise
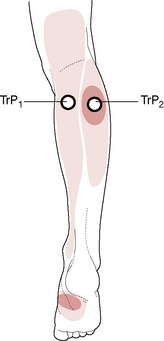
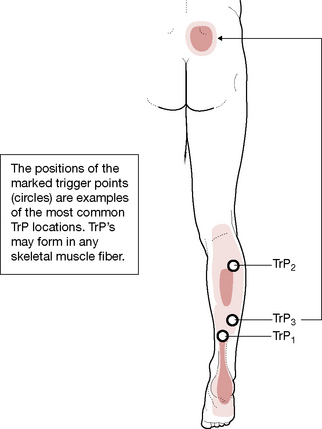
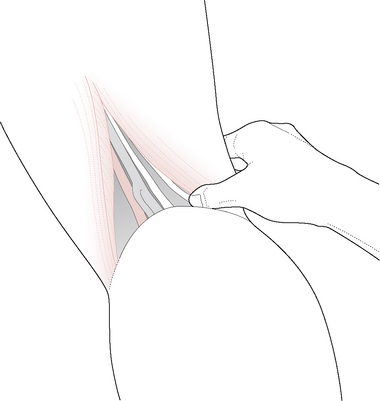
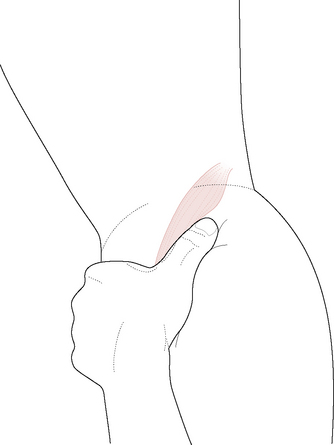
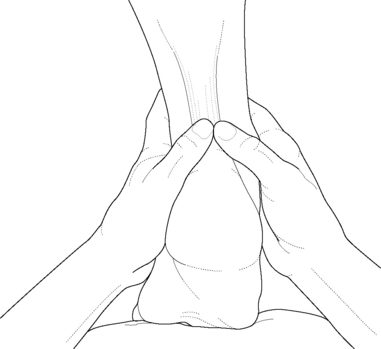
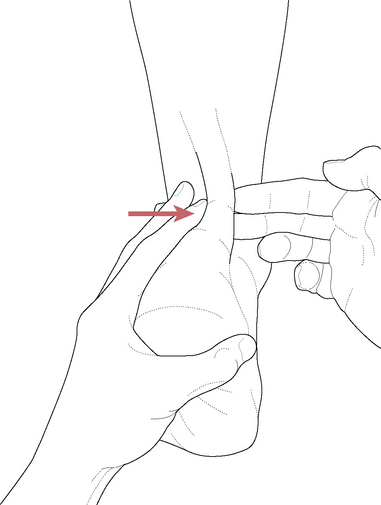
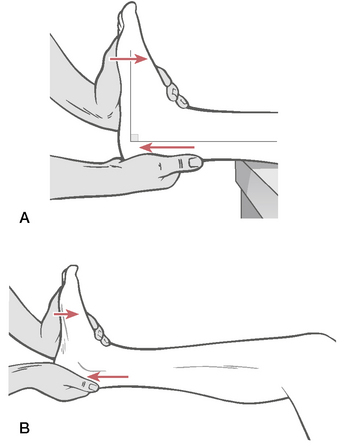
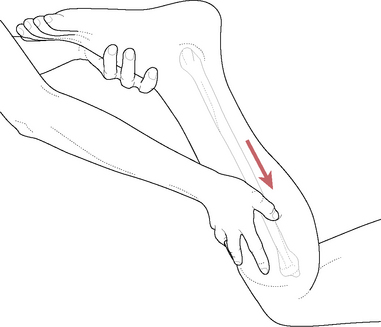
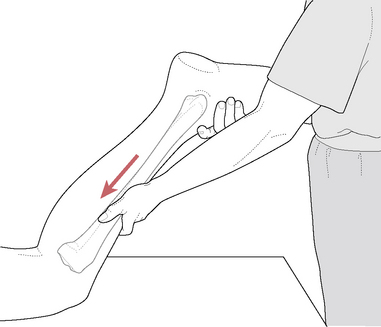
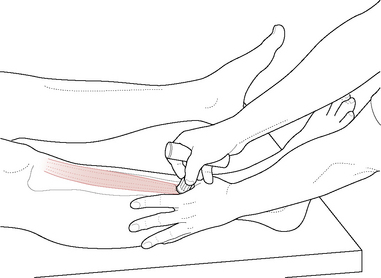
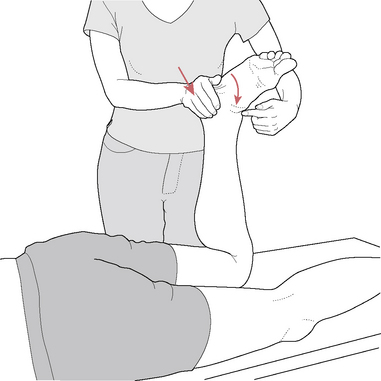
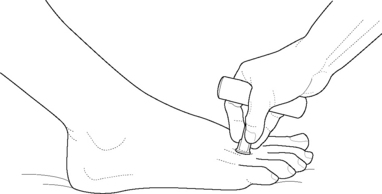
Therapeutic stretches, such as those involving MET, applied to gastrocnemius and soleus (see Figure 14.38) are suggested as part of the warm-up, before regular exercise therapy for IC (Martinez et al 2009).
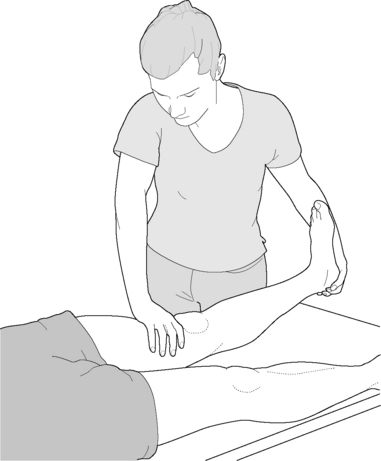
Figure 14.38 Alternative position for treatment of gastrocnemius and/or soleus (if knee is flexed to disengage gastrocnemius)
(adapted from Chaitow 2001).
Regular walking exercise (treadmill or in everyday life) is the most commonly recommended rehabilitation exercise to help in improving peripheral circulatory problems related to PAD/IC (Stewart et al 2008).
Soft tissue approaches
Osteopathic soft tissue methods were successfully applied to patients with PAD/IC (Lombardini et al 2009). A controlled study investigated whether osteopathic manipulative therapy (OMT) mainly involving soft tissue methods that have been incorporated into NMT, as described in this book, could be of benefit to patients with intermittent claudication, alongside standard care.
Compared to a control group (no additional manual treatment), the OMT group achieved a significant increase in blood flow and improvement of subjective symptoms, by the end of the study, and at 6 months follow-up.
Salamon et al (2004) suggest that physical manipulation may promote a rapid release of nitric oxide (NO) that might explain the therapeutic vascular effects of OMT. Apparently NO release promotes vasodilation, inhibits platelet aggregation, white blood cell adhesion and smooth muscle cell proliferation, all of which may contribute to profound physiological benefits (Stefano et al 2000).
Other benefits deriving from the OMT approaches, listed below, might relate to a combination of biomechanical, reflexive and circulatory effects, achieved during treatment.
Treatment protocol:
Following a structural examination of each patient to identify areas of somatic dysfunction, defined as ‘impaired or altered function of related components body framework system: skeletal, arthrodial, and myofascial structures; and related vascular, lymphatic and neural elements’ – OMT was applied.
The OMT treatment methods included myofascial release, strain/counterstrain (positional release), muscle energy soft tissue techniques, high-velocity low amplitude [HVLA] manipulation (thoracolumbar region, typically T10–L1), lymphatic pump and craniosacral manipulation. Most of these methods (apart from HVLA) are described in Chapter 9, and elsewhere throughout this book, and its companion: Clinical Applications of Neuromuscular Techniques. Volume 1: Upper Body (2nd edn., 2008).
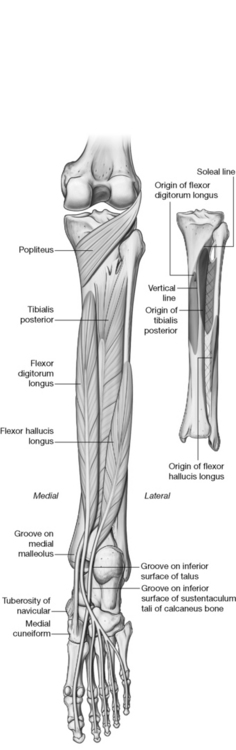
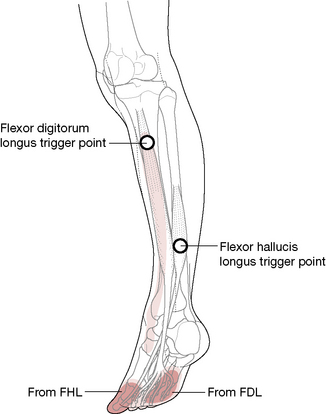
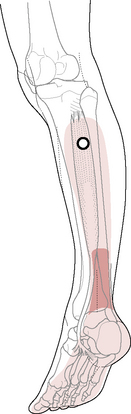
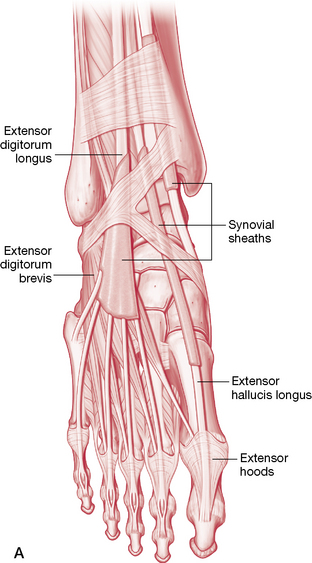
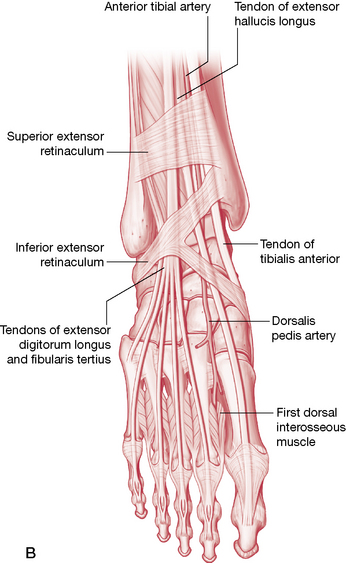
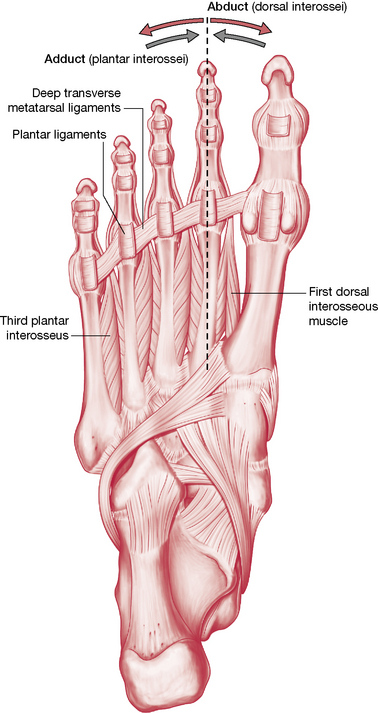
Classifying the muscles of the leg and foot
The muscles of the leg and foot can be functionally classified into those that primarily flex, extend, invert and evert the ankle and subtalar joint and those that act upon the toes. Many of these muscles perform several functions and would appear in several categories. They could certainly be classified as being extrinsic (those arising outside the foot to act upon it) or intrinsic (those arising within the foot structure itself), which has merit when organizing a treatment approach. They could also be classified by innervation as to dorsal and ventral divisions of the plexus. However, the best way to classify the muscles of the leg and foot is by location (Platzer 2004) since the leg is divided into compartments and the foot into dorsal and plantar surfaces.
In the next section, the extrinsic muscles (those arising in the leg) will be considered first, followed by the dorsal and plantar intrinsic muscles of the foot.
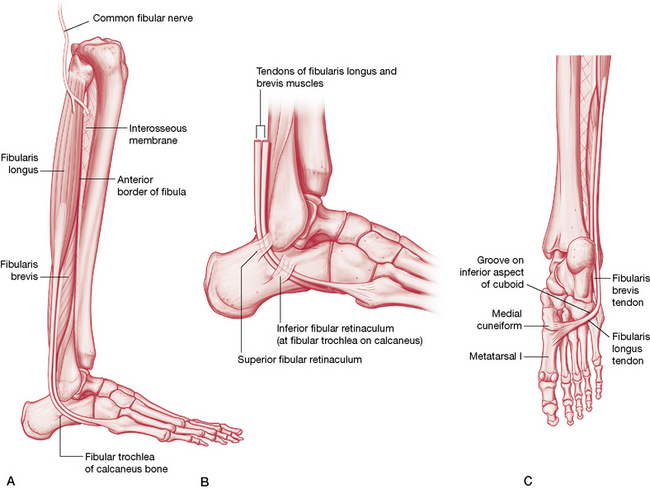
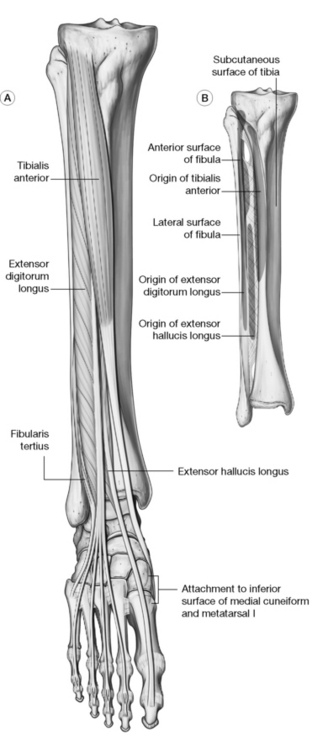
The leg can be conveniently divided into three compartments – anterior, posterior and lateral – although some authors offer only anterior and posterior by including the fibularis muscles in the posterior compartment (Fig. 14.24).
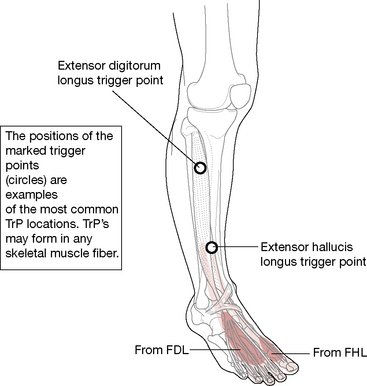
• The anterior compartment contains the dorsiflexors: tibialis anterior, extensor hallucis longus, extensor digitorum longus and fibularis (peroneus) tertius.
• The lateral compartment contains fibularis (peroneus) longus and brevis.
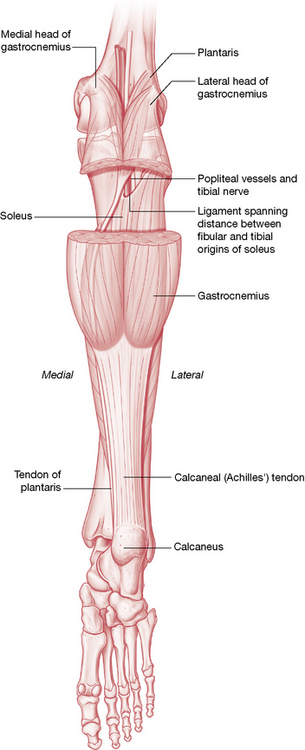
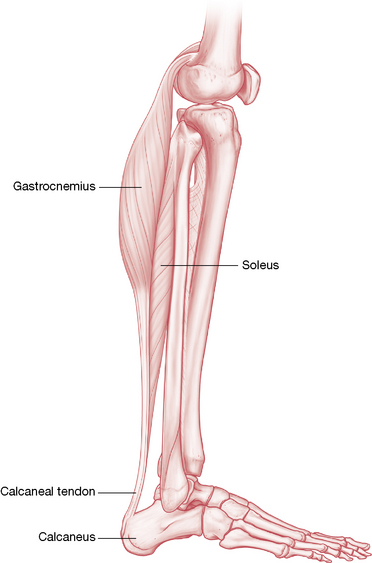
• The posterior compartment can be subdivided into two layers: superficial layer, which includes the triceps surae (gastrocnemius and soleus) and plantaris; and the deep layer, which includes tibialis posterior, flexor hallucis longus and flexor digitorum longus. Although popliteus could certainly be included in the deep layer of the leg, since it does not act upon the foot directly, it is rightfully grouped with the knee on p. 496.
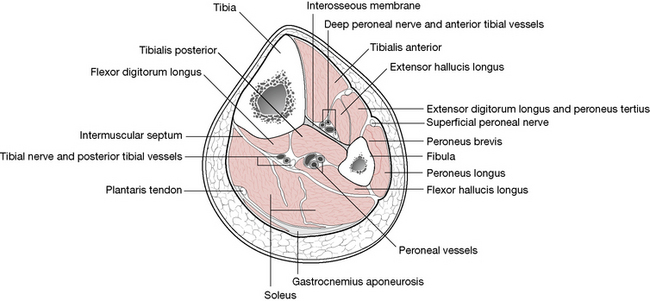
Figure 14.24 Transverse section of the right leg
(adapted with permission from Travell & Simons 1992).
The extrinsic muscles are discussed first in the following section, organized by their compartmental location. The intrinsic muscles are then discussed more briefly and organized as to dorsal or plantar location. Although the discussion of the intrinsic muscles may be brief, this in no way diminishes the tremendously important role they play in maintaining the integrity of the foot.