Chapter 14 The leg and foot
The leg is composed of the tibia, fibula and the extrinsic muscles that operate the foot. The foot is much more complex, being composed of 26 bones (seven tarsals, five metatarsals and 14 phalanges), 25 component joints, and is divided into three functional segments (forefoot, midfoot, hindfoot). With the two feet containing over a quarter of the bones of the human body, little doubt remains that these mechanically complex structures are designed to be dynamically flexible yet structurally dependable.
Some of the terminology regarding movements of the foot is not universally agreed upon and clarifications are listed in Box 14.1.
Box 14.1 Semantics: clarifying terminology
In considering the terminology used to describe the foot’s position and movements, differences in nomenclature are commonly found, which creates confusion for most readers. This type of confusion is not confined to the lower extremity, nor is it a new situation. Within the medical professions, unclear terminology may result in serious consequences (Greathouse et al 2004). In 1998, the Federative Committee on Anatomical Terminology (FCAT) and the International Federation of Associations of Anatomists (IFAA) updated a previously recognized authoritative work (Nomina Anatomica) and published it under a new title, Terminologia Anatomica. This text contains parallel listing of Latin terms and English equivalents that designate the structures of the human body. Having been developed by an international committee of anatomists, is intended for worldwide use as the definitive nomenclature text (FCAT 1998).
The following points are offered to help clarify the terms adopted with in this NMT text.
Where standard terms exist, consistency with those terms adopted by FCAT ruled. Additional discussion are below and within the text, as appropriate.
• Regarding the lower extremity, the portion that lies between the hip and knee joints is the thigh, while the portion that lies between the knee and ankle joints is the leg. ‘Lower leg’ is that portion of the leg that lies near the ankle.
• What was previously known as peroneal is now fibular, e.g. peroneus longus is fibularis longus and peroneal nerve is fibular nerve. This is more descriptive of the region and it helps to prevent confusion with similar terms, such as the perineum (perineal) or the peritoneum (peritoneal).
• Standard anatomical position describes the foot divided into the tarsus (seven bones), metatarsus (five) and phalanges (14 + two sesamoids) (Gray’s anatomy 2005). However, regarding functionality, the foot can be better divided into three functional segments: the hindfoot (calcaneus and talus), the midfoot (navicular, cuboid and three cuneiforms) and the forefoot (five metatarsals, 14 phalanges and two sesamoids).
• Dorsal and plantar surfaces replace the terms anterior and posterior respectively, while proximal and distal are used in their normal manner.
• ‘Crural’ pertains to the leg.
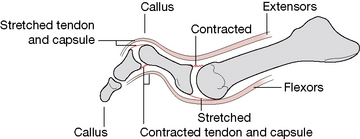
• Flexion of a joint approximates the joint surfaces so as to create a more acute angle. (The reader might reflect on whether this descriptive ‘rule’ is used consistently, for example in relation to normal cervical and lumbar curves where the creation of more acute joint angles occurs when these areas are extended, rather than flexed [i.e. backward bending should really be called ‘flexion of the lumbar spine’!], which might add confusion rather than clarity to texts.) In regard to the foot, moving the dorsal surface of the foot toward the tibia constitutes flexion of the ankle joint. Therefore, movement in the opposite direction constitutes extension of the joint. However, with the foot, these movements are usually termed dorsiflexion and plantarflexion, respectively. While some authors feel the use of the term plantarflexion is inappropriate (Kapandji 1987), it does clarify a movement that might otherwise be even more unclear. Some of the confusion surrounding the use of flexion and extension regarding the ankle is due to the fact that the toe extensors assist in creating ankle flexion while the toe flexors assist in ankle extension. The terms dorsi- and plantarflexion help in this dilemma and are therefore used in this text to define flexion and extension of the ankle, respectively.
• Supination and pronation are often used synonymously with inversion and eversion of the foot. However, one set of terms often relates to movement about a longitudinal axis while the other set defines a simultaneous triplanar movement about the longitudinal, horizontal and vertical axis. It is not surprising that these are confused since definitive texts have no universal alignment regarding their usage. Regarding this terminology issue, Levangie & Norkin (2001) explain:
Although pronation/supination and inversion/eversion are often substituted for each other, there is consensus across the literature in using varus-valgus of the calcaneus to refer to the frontal plane component of subtalar motion. Regardless of how the terms are used, it should be noted that subtalar supination is invariably linked with subtalar inversion and calcaneovarus, whereas subtalar pronation is invariably linked with subtalar eversion and calcaneovalgus…Terms used in research and published literature should carefully be defined to impart the most and clearest information.
• In the subsequent edition of their text, Levangie & Norkin (2005) suggest ‘…some of these terminology differences are not really as problematic as they might initially seem.’ We suggest that, regardless of the term employed to describe it, it is most important to realize that the movement that turns the sole of foot toward the mid-line and elevates its medial aspect (whether called supination or inversion) is a triaxial movement involving rotation about a vertical, longitudinal and horizontal axis.
• Regarding this particular terminology debate, Gray’s anatomy (2005) points out that ‘Pronation and supination are usually better terms than eversion and inversion, as the latter rarely occur in isolation and the former describe the “compound” motion that usually occurs’.
• For simplicity in this text, the term supination is used to describe the lifting of the medial border of the foot and pronation to describe the lifting of the lateral border of the foot. Inversion and eversion are used infrequently in this text (e.g., in direct quotes) to describe the same movements.
The most significant joints of foot mechanics include the talocrural (ankle) joint, the subtalar (talocalcaneal) joint, transverse tarsal (talonavicular and calcaneocuboid) joint, the metatarsophalangeal joints and the interphalangeal joints. Additionally the compound joint, the talocalcaneonavicular joint, plays an important role in directing weight-bearing forces placed on the talus above both toward the heel and into the forefoot. Functional integrity of the plantar vault, or arch, system of the foot is dependent upon the integrity of each of these joints, which are, in turn, dependent upon a functional arch system as well as the function of more proximal joints, such as the knee and hip.
The leg
The tibia, the second longest bone in the body and its companion, the fibula, are vertically oriented and articulate at both their upper and lower ends (Figs 14.1, 14.2).
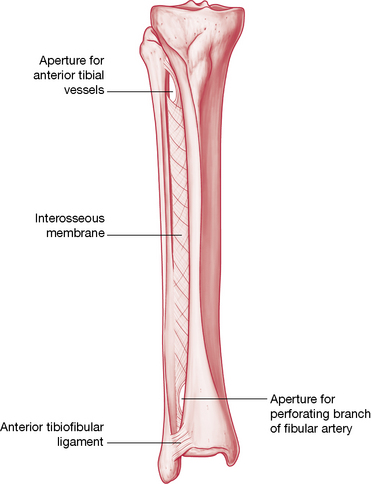
Figure 14.1 Anterior aspect of the right tibia and fibula. Interosseous membrane offers stability while also allowing mobility between the two bones.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
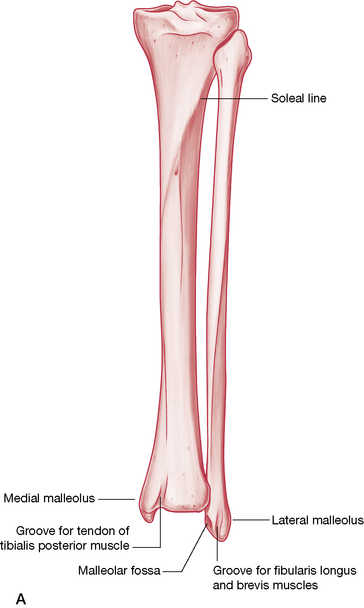
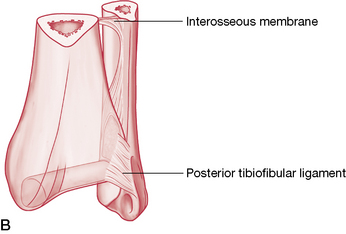
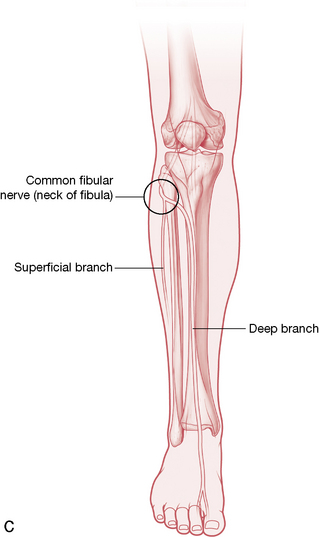
Figure 14.2 A: Anterior aspect of the right tibia and fibula. B: Posterior distal tibiofibular joint. C: Course of common fibular nerve, which is vulnerable at the head and neck of the fibula.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
While the fibula has no articulation at the knee joint itself, it does indeed have a proximal articulation with the tibia on the inferior surface of the tibia’s lateral projection. Both bones are included in the ankle joint, their distal ends forming a mortise, which receives the head of the talus. The two leg bones are also connected through their entire length by the interosseous membrane, a tough, fibrous sheath that strengthens the tibiofibular syndesmosis, offers a broad surface for muscular attachment and provides separation of the anterior and posterior compartments of the leg.
The proximal tibia (described on p. 450) has (on the inferior surface of its lateral projection) a fibular facet, which faces distally and posterolaterally to receive the fibular head. This articulation comprises the proximal tibiofibular joint. While this joint does not provide a high degree of movement, dysfunctions within this joint are an important consideration when the ankle is being assessed due to the potential impact this may have on distal tibiofibular joint function, and, therefore, movements of the ankle joint.
The triangular shaft of the tibia has a medial, lateral and posterior surface, the borders of which are fairly sharply defined. The medial surface is immediately recognizable as the ‘shin’, while the interosseous border is the attachment site for the interosseous membrane. When compared to the proximal end, the distal end of the tibia, where its medial malleolus projects inferomedially, is noted to be rotated laterally (tibial torsion) about 30°, this being significantly more in Africans (Eckhoff et al 1994). The distal surface, which articulates with the talus, is concave sagittally, convex transversely and is continuous with the malleolar articular surface. The medial malleolus lies anterior and proximal to the lateral malleolus. Various ligaments (described below) and the joint capsule attach to it.
The fibula has a proximal head, a long, thin shaft and a distal projection, the lateral malleolus. The head offers a round facet, which articulates with the tibia. Like the tibia, the fibula has three borders and surfaces, the details of both being well described by Gray’s anatomy (2005). Its distal end articulates with the lateral talar surface and is joined to the tibia as a syndesmosis (fibrous union that does not directly contact) to form the ankle mortise.
Both the proximal and distal tibiofibular joints are stabilized by anterior and posterior tibiofibular ligaments. Additionally, the distal end also possesses an inferior transverse ligament and the crural tibiofibular interosseous ligament, which offer support to the distal joint, as does the interosseous membrane.
The proximal tibiofibular joint
The proximal tibiofibular joint is a synovial joint that is not directly connected with the knee joint. When the knee is flexed, this joint plays a part in rotation of the leg, allowing small degrees of supplementary abduction and adduction of the fibula (Lewit 1985) or, as Kuchera & Goodridge (1997) term it, ‘anterolateral and posteromedial glide of the fibular head’.
Greenman (1996) notes that the behavior of the fibular head is strongly influenced by the biceps femoris muscle, which attaches to it, suggesting that any dysfunction of the tibiofibular joint calls for assessment of this muscle, for length, strength and localized dysfunction (trigger points). Schiowitz (1991) notes that: ‘When evaluating or treating a fibular head dysfunction, the [practitioner] should completely examine the distal articulation as well, at the ankle joint’. Kuchera & Goodridge (1997) point out that functional movement of the distal tibiofibular joint is imperative as it allows the ankle mortise to accommodate the increased width of the posterior portion of the talus during dorsiflexion.
Proximal tibiofibular joint play
Lewit (1985) reports joint play at the proximal tibiofibular joint as involving an anteroposterior glide as well as some rotation potential of the fibular head on the tibia.
• When the tibia and ankle are externally rotated, the proximal fibular head elevates and glides (translates) anteriorly, to accommodate this movement (Kuchera & Goodridge 1997) (Fig. 14.3).
• Similarly, when the tibia and ankle are internally rotated, the proximal fibular head depresses and glides (translates) posteriorly, to accommodate this movement.
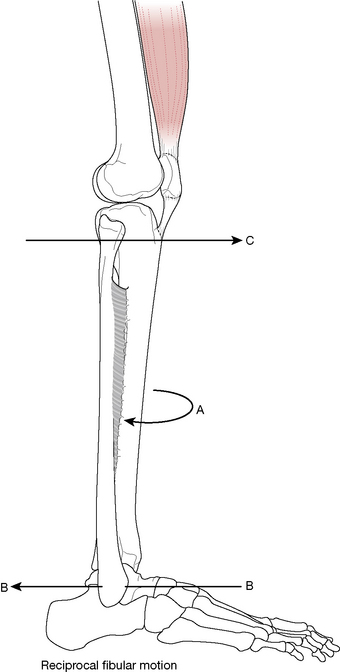
Figure 14.3 External rotation of the tibia (A) moves the distal fibula posteriorly (B) while the fibular head moves anteriorly (C). All these movements are reversed for internal rotation of the tibia (after Ward 1997).
The proximal tibiofibular joint’s role in ankle sprains
Details regarding ankle sprains are discussed on p. 512. In addition to those considerations, Kuchera & Goodridge (1997) suggest that in cases of recurrent ankle sprain, examination for fibular head dysfunction should be carried out, ‘because with trauma the physiologic, reciprocal motion [between the distal and proximal tibiofibular articulations] may not occur’.
Greenman (1996), discussing the problem of recurrent ankle sprain, suggests they ‘are difficult to treat’ and that ‘structural diagnostic findings in this population consistently show dysfunction at the proximal tibiofibular joint and dorsiflexion restrictions of the talus at the talotibial articulation’. Greenman further observes that common findings include loss of subtalar joint play, pronation of the cuboid, and weakness of the lateral compartment muscles and tibialis anterior.
• In cases involving a pronation sprain of the ankle joint, ‘the distal talofibular joint glides posteriorly and the head of the fibula glides anteriorly’.
• In cases of supination ankle sprain, ‘the distal fibula is often found to be anterior and the fibular head is posterior’ (Kuchera & Goodridge 1997).
Testing joint play and mobilizing the proximal tibiofibular joint
• The patient is supine with hip and knee flexed so that the sole of the foot is flat on the table.
• The practitioner sits so that her buttock rests on the patient’s toes, stabilizing the foot to the table.
• The head of the fibula is grasped between thumb and index finger of one hand as the other hand holds the tibia firmly, inferior to the patella.
• Care should be taken to avoid excessive pressure on the posterior aspect of the fibula head as well as its neck, as the common fibular nerve (relatively exposed) wraps around it and is vulnerable to compression (Kuchera & Goodridge 1997) (see Fig. 14.2C).
• The thumb resting on the anterior surface of the fibula should be reinforced by placing the thumb of the other hand over it.
• A movement that takes the fibular head firmly posteriorly and anteriorly, in a slightly curved manner (i.e. not quite a straight backward-and-forward movement, but more back and slightly curving inferiorly, followed by forward and slightly curving superiorly, at an angle of approximately 30° – see Fig. 14.3), determines whether there is freedom of joint glide in each direction.
• If restriction is noted in either direction, repetitive rhythmical springing of the fibula at the end of its range should restore normal joint play.
• It is worth noting that when the fibular head glides anteriorly there is automatic reciprocal movement posteriorly at the distal fibula (lateral malleolus), while posterior glide of the fibula head results in anterior movement of the distal fibula. Restrictions at the distal fibula are, therefore, likely to influence behavior proximally and vice versa.
• Petty (2006) utilizes a similar anteroposterior glide to that described above, but suggests a prone position for the posteroanterior assessment.
• The prone patient’s leg is supported proximal to the ankle on a cushion, so that the knee is in slight flexion.
• The practitioner’s thumbs are applied to the posterior aspect of the fibula head while avoiding the common fibular nerve, with fingers curved around the proximal leg to offer support for the hands as well as to stabilize the leg.
• On-and-off combined thumb pressure is applied to assess anterior glide potential of the head of the fibula.
Entrapment possibility
As observed above, care is required to avoid undue pressure on the posterior aspect of the fibula head due to neural structure proximity. Kuchera & Goodridge (1997) point out additionally that dysfunction that involves the fibular head being locked in a posteriorly translated direction ‘may cause symptoms related to entrapment neuropathy or compression of the common peroneal [fibular] nerve’ (see Box 14.9).
Box 14.9 Neural impingement and neurodynamic testing
Note: See Volume 1, Box 13.11 for additional information regarding the background to neural impingement.
Korr (1970, 1981) demonstrated that nerves transport vital biochemical substances throughout the body, constantly. The rate of axonal transport of such substances varies from 1 mm/day to several hundred mm/day, with ‘different cargoes being carried at different rates’. ‘The motor powers (for the waves of transportation) are provided by the axon itself’. Transportation is a two-way traffic, with retrograde transportation, ‘a fundamental means of communication between neurons and between neurons and non-neuronal cells’.
Korr (1981) believes this process to have an important role in maintenance of ‘the plasticity of the nervous system, serving to keep motor-neurons and muscle cells, or two synapsing neurons, mutually adapted to each other and responsive to each other’s changing circumstances’. The trophic influence of neural structures on the structural and functional characteristics of the soft tissues they supply can be shown to be vulnerable to disturbance. Korr (1981) explains:
Any factor which causes derangement of transport mechanisms in the axon, or that chronically alters the quality or quantity of the axonally transported substances, could cause the trophic influences to become detrimental. This alteration in turn would produce aberrations of structure, function, and metabolism, thereby contributing to dysfunction and disease.
Among the negative influences frequently operating on these transport mechanisms, Korr informs us, are deformations of nerves and roots, such as compression, stretching, angulation and torsion. Nerves are particularly vulnerable in their passage over highly mobile joints, through bony canals, intervertebral foramina, fascial layers and tonically contracted muscles (for example, posterior rami of spinal nerves and spinal extensor muscles).
Neurodynamic testing for and the treatment of ‘tensions’ in neural structures offer a means of dealing with some forms of pain and dysfunction.
Maitland (1986) suggested that assessment and treatment of ‘adverse mechanical tension’ (AMT) in the nervous system should be seen as a form of ‘mobilization’.
Any pathology in the mechanical interface (MI) between nerves and their surrounding tissues can produce abnormalities in nerve movement, resulting in tension on neural structures. Examples of MI dysfunction are nerve impingement by disc protrusion, osteophyte contact or carpal tunnel constriction. These problems may be regarded as mechanical in origin and symptoms will more easily be provoked by movement rather than passive testing.
Chemical or inflammatory causes of neural tension can also occur, resulting in ‘interneural fibrosis’, which leads to reduced elasticity and increased ‘tension’, which would become obvious with tension testing of these structures (see the discussion of Morton’s neuroma on p. 532). The pathophysiological changes resulting from inflammation, or from chemical damage (i.e. toxicity) lead to internal mechanical restrictions of neural structures, which are quite different from externally applied mechanical causes, such as would be produced by a disc lesion, for example.
When a neurodynamic test (see below) is positive (i.e. pain is produced by one or another element of the test – initial position alone or with ‘sensitizing’ additions) it indicates only that AMT exists somewhere in the nervous system and not that this is necessarily at the site of reported pain.
Petty (2006) suggests that in order to ‘ascertain the degree to which neural tissue is responsible for the production of the patient’s [ankle and foot] symptoms’ the tests that should be carried out are passive neck flexion, straight leg raising, passive knee flexion and slump. These tests are described below, with the exception of passive neck flexion, which is self-explanatory.
• A positive tension test is one in which the patient’s symptoms are reproduced by the test procedure and where these symptoms can be altered by variations in what are termed ‘sensitizing maneuvers’, which are used to ‘add weight to’, and confirm, the initial finding of AMT.
• Adding dorsiflexion during SLR is an example of a sensitizing maneuver.
• Precise symptom reproduction may not be possible, but the test is still possibly relevant if other abnormal symptoms are produced during the test and its accompanying sensitizing procedures. Comparison with the test findings on an opposite limb, for example, may indicate an abnormality worth exploring.
• Altered range of movement is another indicator of abnormality, whether this is noted during the initial test position or during sensitizing additions.
Variations of passive motion of the nervous system during examination and treatment
1. An increase in tension can be produced in the interneural component, where tension is being applied from both ends, so to speak, as in the ‘slump’ test (Fig. 14.45).
2. Increased tension can be produced in the extraneural component, which then produces the maximum movement of the nerve in relation to its mechanical interface (such as in straight leg raising) with the likelihood of restrictions showing up at ‘tension points’.
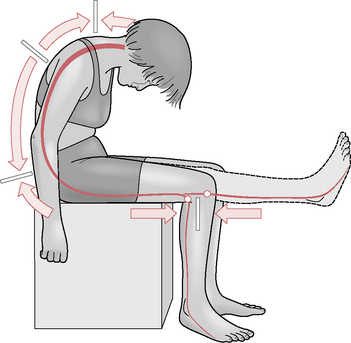
Figure 14.45 The slump test places the entire neural network, from pons to the feet, under tension. Note the movement pattern of nerve roots and dura mater as indicated by the arrows. Also note that as the knee moves from flexion to extension the tibial nerve moves in two directions in relation to the tibia and femur. The fibular tension point is at the head of the fibula. No neural movement occurs behind the knee or at levels C6, T6 or L4
(Butler 1994).
3. Movement of extraneural tissues in another plane can be engineered.
CAUTION: General precautions and contraindications
• Care should be taken of the spine during the ‘slump test’ if disc problems are involved or if the neck is sensitive (or the patient is prone to dizziness).
• If any area is sensitive, care should be taken not to aggravate existing conditions during performance of tests.
• If obvious neurological problems exist, special care should be taken to avoid exacerbation that vigorous or strong stretching might provoke.
• Similar precautions apply to diabetic, MS or recent surgical patients or where the area being tested is affected by circulatory deficit.
• Tests of the sort described below should be avoided if there has been recent onset or worsening of neurological signs or if there is any cauda equina or cord lesion.
Straight leg raising (SLR) test
Note: See text relating to hamstring tests (for shortness) in Chapters 10 and 12. See Figure 12.46 in particular. In Chapter 10 Box 10.5, see discussion under the subheading: Protocol for assessment of symptoms caused by nerve root or peripheral nerve dysfunction (p. 237).
The leg is raised in the sagittal plane, knee extended.
It is suggested that this test should be used in all vertebral disorders, all lower limb disorders (and some upper limb disorders) to establish the possibility of abnormal mechanical tension in the nervous system in the lower back or limb.
Sensitizing additions to SLR
• Ankle dorsiflexion (this stresses the tibial component of the sciatic nerve).
• Ankle plantarflexion plus inversion (this stresses the common fibular nerve, which may be useful with anterior shin and dorsal foot symptoms).
• Increased medial hip rotation.
• Altered spinal position (for example, left SLR may be ‘sensitized’ by lateral flexion to the right of the spine).
The SLR test should be performed with the addition, one at a time, of each sensitizing maneuver, in order to assess changes in symptoms, new symptoms, restrictions, etc.
The question being asked is: ‘Can the leg be raised as far, and as easily, without force, and without symptoms (new or old) appearing, when the sensitizing additions are incorporated?’
Notes on SLR test
• During the SLR test there is caudad movement of the lumbosacral nerve roots in relation to interfacing tissue (which is why there is a ‘positive’ indication of pain and limitation of leg-raising potential when SLR is performed in the presence of a prolapsed intervertebral disc).
• The tibial nerve, proximal to the knee, moves caudad (in relation to the mechanical interface) during SLR, whereas distal to the knee it moves cranially. There is no movement of the tibial nerve behind the knee itself, which is therefore known as a ‘tension point’.
• The common fibular nerve is attached firmly to the head of the fibula (another ‘tension point’).
Prone knee bend test (PKB)
• The patient is prone and the knee is flexed, taking the heel toward the buttock to assess reproduction of existing symptoms, or other abnormal symptoms, or altered range of movement (heel should approximate buttock easily). See Figure 12.18 for positioning in prone position.
• During the test, the knee of the prone patient is flexed while the hip and thigh are stabilized, which moves the nerves and roots from L2, L3, L4 and, particularly, the femoral nerve and its branches.
• If, however, the test is conducted with the patient sidelying, the hip should be maintained in extension during the test (this alternative position is thought more appropriate for identifying entrapped lateral femoral cutaneous nerve problems).
• It is obvious that the PKB test stretches rectus femoris and rotates the pelvis anteriorly, thus extending the lumbar spine, which can confuse interpretation of nerve impingement symptoms. Care should be taken to avoid this by stabilizing the pelvis or by placement of a pillow under the abdomen to support the lumbar spine. A bodyCushion™ would most ideally achieve this goal.
• Sensitizing maneuvers include (in either prone or sidelying use of the test):
The ‘slump test’
Butler (1994) regards this as the most important test in this series. It links neural and connective tissue components from the pons to the feet and requires care in performance and interpretation (Fig. 14.45). The slump test is suggested for all spinal disorders, most lower limb disorders and some upper limb disorders (those that seem to involve the nervous system).
The test involves the seated patient introducing the following sequence of movements:
• thoracic and then lumbar flexion, followed by
• sometimes also hip flexion (produced by either bringing the trunk forward on the hips or by increasing SLR).
Additional sensitizing movements during slump testing are achieved by changes in the terminal positions of joints. Butler (1994) gives examples.
• If the test reproduces (for example) lumbar and radiating thigh pain, a change in head position – say into slight extension – could result in total relief of these symptoms (desensitizing).
• A change in ankle and knee positions could significantly change cervical, thoracic or head pain produced by the test.
• In both instances this would confirm that AMT was operating, although the site would remain obscure.
• Trunk sidebending and rotation or even extension, hip adduction, abduction or rotation and varying neck positions are all sensitizing movements.
Cadaver studies demonstrate that neuromeningeal movement occurs in various directions, with C6, T6 and L4 intervertebral levels being regions of constant state (i.e. no movement, therefore ‘tension points’). Butler (1994) reports that many restrictions identified during the slump test may only be corrected by appropriate spinal manipulation.
It is possible for SLR to be positive (e.g. symptoms are reproduced) and the slump test negative (no symptom reproduction) and vice versa, so both should always be performed.
The following findings have been reported in research using the slump test. Mid-thoracic to T9 are painful on trunk and neck flexion in 50% of ‘normal’ individuals. The following are considered normal responses if they are symmetrical.
• Hamstring and posterior knee pain occurring with trunk and neck flexion, when the knees are extended and increasing further with ankle dorsiflexion.
• Restrictions in ankle dorsiflexion during trunk/neck flexion while the knee is in extension.
• There is a common decrease in pain noted on release of neck flexion and an increase in range of knee extension or ankle dorsiflexion on release of neck flexion.
If the patient’s symptoms are reproduced by the slump position, altered or aggravated by sensitizing movements and can be relieved by desensitizing maneuvers, the test is regarded as positive.
Butler (1994) suggests that in treating adverse mechanical tensions in the nervous system, initial stretching of the tissues associated with neural restrictions should commence well away from the site of pain in sensitive individuals and conditions. It is not within the scope of this text to detail methods for releasing abnormal tensions, except to suggest that the treatment positions are commonly a replication of the test positions (as in shortened musculature, where MET is used).
We suggest that when the protocols outlined throughout the clinical applications segments are diligently carried out, including identifying and releasing tense and shortened musculature, releasing tense, indurated, fibrotic myofascial structures using NMT or other deep tissue methods as well as deactivating trigger points, where appropriate, mobilizing joints, including those aspects of movement that are involuntary (joint play), there will almost always be an improvement in abnormal neural restrictions.
Retesting restricted tissues regularly during treatment is important, in order to see whether gains in range of motion or lessening of pain noted during AMT testing are being achieved.
Mobilization with movement (MWM) to release the fibula head
If knee pain is reported in the posterolateral aspect of the knee joint and no internal knee dysfunction is apparent, joint play of the tibiofibular joint may be restricted.
• The patient is lying or standing.
• The practitioner applies anterior or posterior pressure to the fibula head (with thumb pressure toward the direction of joint play restriction), as the patient actively, slowly, flexes and extends the knee several times.
• If the pain-free range is increased during the exercise, the indication is that the problem is of a mechanical nature at the proximal tibiofibular joint and this procedure may well normalize it (Mulligan 1999, Petty 2006). Due to their reciprocal movements, the distal tibiofibular joints should also be accessed.
MET for releasing restricted proximal tibiofibular joint
For posterior fibular head dysfunction (where anterior glide is restricted)
• The patient sits on the treatment table with legs hanging over the edge.
• The practitioner sits in front of the patient supporting the foot with one ‘supporting’ hand
• The practitioner’s other hand engages the posterior aspect of the fibular head and introduces an anteriorly directed force, while avoiding compression of the fibular nerve.
• At the same time the supporting hand passively inverts, plantarflexes and adducts the foot (creating supination), to the first resistance barriers in these directions.
• When slack has been removed via these movements, the patient is asked to evert, abduct and dorsiflex the foot, using a moderate degree of effort (‘Try to use no more than 25% of your strength, while I resist your effort’).
• This isometric effort is held for 5–7 seconds (Greenman [1996] suggests just 3–5 seconds).
• Following complete relaxation of the muscular effort by the patient, slack is removed by the contacts on the fibular head and also the foot, as a new barrier is engaged (i.e. increased inversion and internal rotation) and the process is repeated once or twice more.
• According to Goodridge & Kuchera (1997) the muscles that are likely to be involved in this resisted isometric effort include extensor digitorum longus and tibialis anterior. The sustained contraction should ‘draw the fibula anteriorly along the tibial articular surface’. Additionally, the isometric action of these muscles should inhibit their antagonists, which may be holding the fibular head posteriorly (see discussion of muscle energy technique in Chapter 9).
For anterior fibular head dysfunction (where posterior glide is restricted)
• The patient sits on the treatment table with legs hanging over the edge.
• The practitioner sits in front of the patient supporting the foot with one hand
• The practitioner’s other hand engages the anterior aspect of the fibular head and introduces a posteriorly directed force.
• At the same time the supporting hand passively inverts and dorsiflexes the foot.
• When slack has been removed via these movements, the patient is asked to evert and plantarflex the foot, using a moderate degree of effort (‘Try to use no more than 25% of your strength, while I resist your effort’).
• This isometric effort is held for 5–7 seconds (Greenman [1996] suggests just 3–5 seconds).
• Following complete relaxation of the muscular effort by the patient, slack is removed by the contacts on the fibular head, and also the foot, as a new barrier is engaged (i.e. increased inversion and dorsiflexion) and the process is repeated once or twice more.
• The muscles that are likely to be involved in this resisted isometric effort include fibularis (peroneus) longus, ‘to draw the fibula laterally from the tibia, making posterior gliding easier’ and soleus, ‘to draw the fibula posteriorly along the tibial articular surface’ (Goodridge & Kuchera 1997). Additionally, the isometric action of these muscles should inhibit their antagonists, which may be holding the fibular head anteriorly (see discussion of MET in Chapter 9).
The ankle joint and hindfoot
The ankle joint composes of the malleoli of the tibia and fibula, the distal surface of the tibia and the body of the talus (see Figs 14.1, 14.2, 14.4). The tibia is weight-bearing onto the head of the talus, while the fibula has very little weight-bearing responsibility, with ‘no more than 10% of the weight that comes through the femur being transmitted through the fibula’ (Levangie & Norkin 2005).
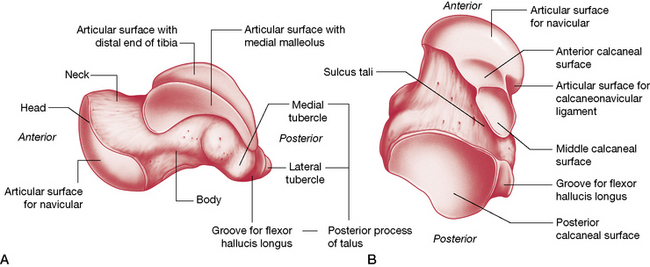
Figure 14.4 The (A) medial and (B) posterior aspects of the talus.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
The tibiofibular component supplies three facets, which together form an almost continuously concave surface, resembling an adjustable mortise (similar to an adjustable wrench). Levangie & Norkin (2005) observe:
The adjustable mortise is more complex than a fixed mortise because it combines mobility and stability functions. The mortise of the ankle is adjustable, relying on the proximal and distal tibiofibular joints to both permit and control the changes in the mortise.
The proximal head of the talus is a wedge-shaped structure, wider anteriorly than posteriorly, that is held in an arch (mortise) created by the medial (tibial) and lateral (fibular) malleoli. Approximately one-third of the medial aspect of the talus is bounded by the tibial malleolus, while the lateral aspect of the talus is entirely bounded by the fibular malleolus, which is more posteriorly situated when compared to the tibial malleolus. The relative oblique axis between the malleoli results in ‘a toeing out (by about 15°) of the free foot…with dorsiflexion and toeing in, with plantarflexion’. We are reminded by Goodridge & Kuchera (1997) that this position of the free foot is important ‘when setting up manipulative techniques addressing this joint’.
The tibia rests on the proximal trochlear surface of the talus. The talus projects a long neck that ends in a rounded distal head for articulation with the navicular bone and the plantar calcaneonavicular ligament, and it offers a facet for each of the malleoli and three articulations with the calcaneus (Fig. 14.4).
The talus has no direct muscular attachments so its ligamentous structure is significant (see below). Its movements are influenced by muscular action on bones that lie above and below it (Greenman 1996). Because of the strong ligaments of the ankle, the shape of the crural concavity and the length of the lateral malleolus on the talus, joint dislocation is extremely unlikely unless accompanied by fracture.
The ankle mortise (also called talocrural, tibiotalar or talotibiofibular joint) is designed to handle enormous degrees of force. (Figs 14.5) Gray’s anatomy (1995) reports that: Compressive forces transmitted across the joint during gait reach five times body weight while tangential shear forces, the result of internally rotating muscle forces and externally rotating inertial forces associated with the body moving over the foot, may reach 80% body weight.
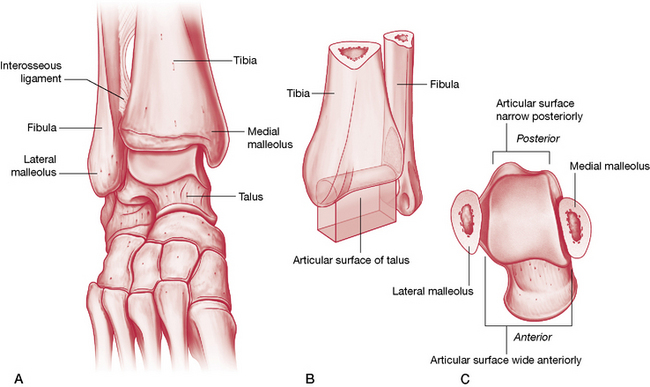
Figure 14.5 The ankle joint. A) The ankle joint functions as a mortise, with the tibia and fibula ‘grasping’ the talus. B) The tibia is weight-bearing while the fibula slides in relation to the tibia. C) The anterior aspect of the head of the talus ‘wedges’ between the tibia and fibula during dorsiflexion.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Gray’s anatomy (2005) describes the ankle joint as follows:
The joint is approximately a uniaxial hinge. The lower end of the tibia and its medial malleolus, together with the lateral malleolus of the fibula and inferior transverse tibiofibular ligament, form a deep recess (‘mortise’) for the body of the talus. Although it appears to be a simple hinge its axis of rotation is dynamic, shifting during dorsi- and plantar flexion.
During dorsiflexion, the fibula and tibia spread away from each other (but only slightly) to accommodate the wider anterior aspects of the head of the talus. This malleolar gap is increased a minor amount by slight lateral rotation of the fibula and a small gliding movement at the proximal tibiofibular joint, which affects the distal joint as well. The close-packed position for this joint is full dorsiflexion where the joint is most congruent and the ligaments are taut. Its least stable position is plantarflexion, where the narrow portion of the talus fits loosely into the mortise.
Levangie & Norkin (2005) artfully describe the mortise:
The function of the ankle (talocrural) joint is dependent on stability of the tibiofibular mortise. The tibia and fibula would be unable to grasp and hold on to the talus if the tibia and fibula were permitted to separate or if one side of the mortise were missing. The analogous mortise of a wrench could not perform its function of grasping a bolt if the two pincer segments moved apart every time a force was applied to the wrench. Conversely, the ankle mortise must have some mobility function to serve; otherwise, a single fused arch would better serve ankle joint function. The mobility role of the mortise belongs primarily to the fibula.
Since movements of the fibula assist the foot in accommodating unstable surfaces, muscular control of the foot when it is not in full dorsiflexion is essential to stability of the structure.
The line of the joint is usually considered to be at the anterior margin of the tibia’s distal end. This can be palpated if the superficial tendons are relaxed. Along with those tendons will be found a variety of structures that are listed here in relation to the malleoli.
Anterior to the malleoli on the dorsum of the talocrural joint:
Posterior to the medial malleolus (Fig. 14.6):
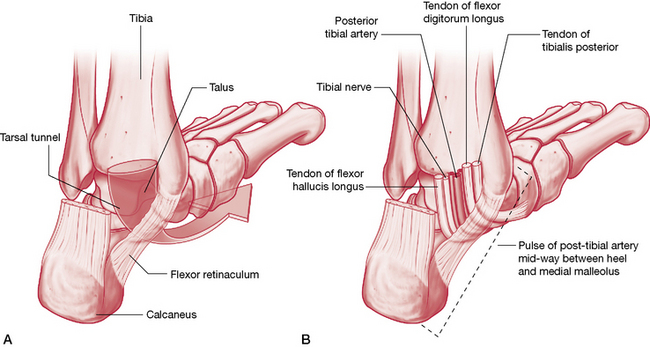
Figure 14.6 The course of the neurovascular structures beneath the medial malleolus
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Posterior to the lateral malleolus (in a groove):
The arterial blood supply to the joint is from the malleolar rami of the anterior tibial and fibular arteries. Nerve supply to the joint derives from the deep fibular and tibial nerves.
The ankle ligaments
The bones that make up the crural arch (the distal tibia and the medial and lateral malleoli) are connected to the talus by the joint capsule and powerful ligaments (Fig. 14.7ABC).
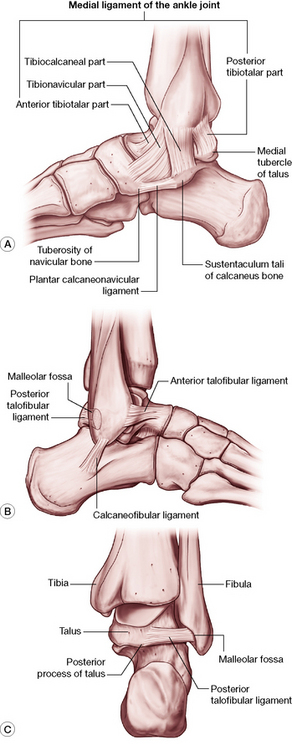
Figure 14.7 The ligaments of the A) medial ankle B) lateral ankle and C) posterior aspect of the ankle joint
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Medial (deltoid) ligament
This extremely powerful, medially located ligament is triangular in shape with its superior attachments on the apex as well as the anterior and posterior borders of the medial malleolus. Inferiorly it has a variety of fibers and attachments, as described by Gray’s anatomy (2005).
…the anterior (tibionavicular [fibers]) pass forwards to the navicular tuberosity and, behind this, blend with the medial margin of the plantar calcaneonavicular ligament; intermediate (tibiocalcaneal) fibers descend almost vertically to the whole length of the sustentaculum tali; posterior fibers (posterior tibiotalar) pass posterolaterally to the medial side of the talus and its medial tubercle. The deep fibers (anterior tibiotalar) pass from the tip of the medial malleolus to the non-articular part of the medial talar surface.
Anterior talofibular ligament
This ligament attaches to the anterior margin of the lateral (fibular) malleolus from which it runs inferiorly, anteriorly and medially to attach at both the lateral articular facet of the talus and the lateral aspect of its neck.
Posterior talofibular ligament
This attaches to the lower aspect of the lateral malleolus from where it runs virtually horizontally to the lateral tubercle of the posterior talar process. Gray’s anatomy (2005) reports that: ‘A “tibial slip” of fibres connects it to the medial malleolus’.
Calcaneofibular ligament
This is ‘a long cord, [that] runs from a depression anterior to the apex of the fibular malleolus [inferiorly] to a tubercle on the lateral calcaneal surface and is crossed by the tendons of peroneus [fibularis] longus and brevis’ (Gray’s anatomy 2005).
Movements of the ankle joint
Kuchera & Goodridge (1997) suggest that the ankle joint is in fact two joints, which should be considered together as a functional unit: the talocrural joint (ankle mortise) and the subtalar joint (described below). They point to the research of Inman (1976) who showed that during the gait cycle, as weight is taken on the foot, there is ‘visible medial rotation of the tibia [that] is greater than can be attributed to movement solely at the talocrural joint’. Inman demonstrated that the increased tibial rotation resulted from ‘relative calcaneal eversion about the subtalar axis’. As the stance phase progresses the tibia then externally (laterally) rotates, at the same time as calcaneal inversion occurs, again about the subtalar axis (see Box 14.1).
The motions of the ankle joint are as follows.
• Plantarflexion (up to 50°, if motion is not isolated and includes subtalar or transverse tarsal joint excursion) achieved by soleus and gastrocnemius, assisted by plantaris, fibularis (peroneus) longus and brevis, tibialis posterior, flexor digitorum longus and flexor hallucis longus.
• Dorsiflexion (10° with knee straight, 30° with knee flexed) achieved largely by tibialis anterior, extensor digitorum longus and fibularis (peroneus) tertius, assisted by extensor hallucis longus (Schiowitz 1991, Travell & Simons 1992).
• Accessory minor motions of anterior glide with plantar flexion and posterior glide with dorsiflexion (Goodridge & Kuchera 1997).
• Additionally, Kuchera & Goodridge (1997) note that: ‘Plantar flexion is accompanied by adduction and supination of the foot….[and]…the proximal fibular head glides posteriorly and inferiorly…[and]…the talus glides anteriorly, placing the narrow position of the talus in the ankle mortise, a less stable position’.
• Although it appears to be simply a hinge, during plantarflexion it is dynamic and can shift (Gray’s anatomy 2005). Platzer (2004) notes that in plantarflexion (open-packed position), some side-to-side movement is possible.
• Stability during symmetrical standing requires continuous action by soleus, which increases during forward leaning (often involving gastrocnemius) and decreases with backward sway. If a backward movement takes the center of gravity posterior to the transverse axes of the ankle joints, the plantarflexors relax and the dorsiflexors contract (Gray’s anatomy 2005).
Dorsiflexion stability
Gray’s anatomy (2005) describes the solidity of the joint during dorsiflexion.
Dorsiflexion is the ‘close-packed’ position, with maximal congruence and ligamentous tension; from this position all major thrusting movements are exerted, in walking, running and jumping. The malleoli embrace the talus, and even in relaxation no appreciable lateral movement can occur without stretch of the inferior tibiofibular syndesmosis and slight bending of the fibula.
During dorsiflexion the widest part of the talus glides posteriorly into the ‘embrace of the malleoli’ and it is this stability that is being exploited when ankle sprains are taped, usually emphasizing dorsiflexion (Goodridge & Kuchera 1997).
Goodridge & Kuchera (1997) note that the distal tibiofibular joint is a syndesmosis (a fibrous joint in which relatively distant opposing surfaces are united by ligaments), which allows the accommodation of the wedge-shaped talus, as it separates the tibia from the fibula during dorsiflexion of the foot. For this reason, ‘Restricted dorsiflexion of the ankle warrants examination and treatment of this syndesmosis’.
The talocalcaneal (subtalar) joint
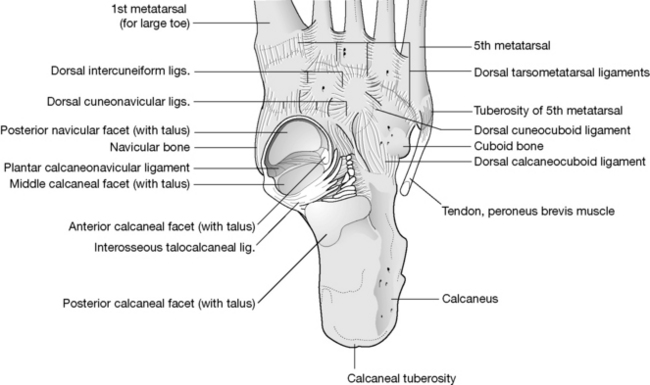
The talocalcaneal (or subtalar) joint is a composite joint formed by the articulation of the talus (Fig 14.4) with the calcaneus (Fig. 14.8) at three surfaces. The largest of these three surfaces lies posterior to the tarsal canal while the anterior and middle facets lie anterior to it. These surfaces are further divided into anterior and posterior independent components by the interosseous talocalcaneal ligament, which lies obliquely between them, separating them into two compartments. The posterior portion has its own synovial cavity while the anterior and middle facets share one. These three articulating surfaces are collectively called the talocalcaneal joint, though it is helpful to consider the two different components of this joint separately. To distinguish them, the posterior component can be called the subtalar joint proper (or posterior subtalar joint) and the anterior component called the talocalcaneonavicular (TCN) joint.
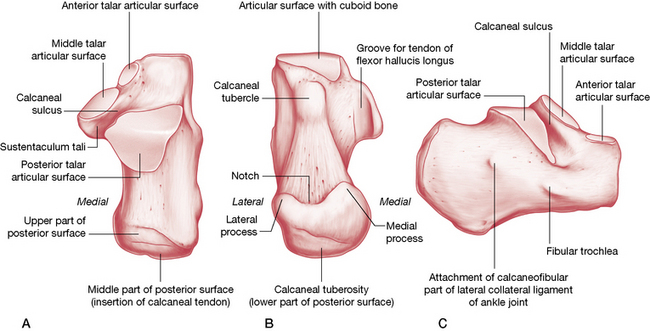
Figure 14.8 The calcaneus: A) superior view; B) posterior view; C) lateral view
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
In collectively describing these surfaces, Cailliet (1997) writes:
Much of the inversion and eversion of the foot occurs at this joint. The entire body and part of the head of the talus rest onf the anterior two thirds of the calcaneus, which is divided into three areas: 1) the posterior third, which is saddle-shaped; 2) the anterior third, which forms a horizontal surface; and 3) the intermediate third, which forms an inclined plane between the other areas.
The calcaneus is the largest tarsal bone, with the muscles of the calf attaching to its projecting posterior surface. In addition to the three articulations with the talus, its anterior surface offers a convex surface for articulation with the cuboid (Fig. 14.5A). The smooth facets contrast with the remaining rough surfaces of the calcaneus, where numerous ligaments and muscles attach. The sustentaculum tali projects medially from it and (dorsally) offers the middle facet, which articulates with the talus, making it also part of the TCN joint.
The posterior saddle-shaped (convex) articular surface of the calcaneus receives the concave talar facet. The middle and anterior articular surfaces include convex talar and concave calcaneal facets, therefore being the reverse of the posterior articulation. Since the talocalcaneal joint is composed of several joints lying in different planes, this unique configuration ‘permits simultaneous movement in different directions’ (Cailliet 1997). Triplanar movement around a single joint axis and functional weight-bearing at this joint are ‘critical for dampening the rotational forces imposed by the body weight while maintaining contact of the foot with the supporting surface’ (Levangie & Norkin 2005).
Levangie & Norkin (2005) explain:
Although the subtalar [talocalcaneal] joint is composed of three articulations, the alternating convex-concave facets limit the potential mobility of the joint. When the talus moves on the posterior facet of the calcaneus, the articular surface of the talus should, theoretically, slide in the same direction as the bone moves – a concave surface moving on a stable convex surface. However, at the middle and anterior joints, the talar surfaces (again, theoretically) should glide in a direction opposite to movement of the bone – a convex surface moving on a stable concave surface. Motion of the talus, therefore, is a complex twisting or screwlike motion that can proceed only as long as the facets can accommodate simultaneous and opposite, motions across the surfaces. The result is a triplanar motion of the talus around a single oblique joint axis, producing the motion of supination/pronation.
Capsule and ligaments of the subtalar joint
The bones of the subtalar joint proper are connected by a fibrous capsule and by lateral, medial, interosseous talocalcaneal and cervical ligaments.
• The fibrous capsule envelops the joint, attaching via short fibers to its articular margins. The joint’s synovial membrane is separate from other tarsal joints (Gray’s anatomy 2005).
• Lateral talocalcaneal ligament: this descends obliquely posteriorly from the lateral talar process to the lateral calcaneal surface. It attaches anterosuperiorly to the calcaneofibular ligament.
• Medial talocalcaneal ligament: this joins the medial talar tubercle to the posterior aspect of the sustentaculum tali and the adjacent medial surface of the calcaneus. Its fibers become continuous with the medial (deltoid) ligament.
• Interosseous talocalcaneal ligament: this descends obliquely and laterally from the sulcus tali to sulcus calcanei.
• Cervical ligament: this is attached to the superior calcaneal surface and ascends medially to an inferolateral tubercle on the talar neck.
Between the posterior and middle articulations lies a deep groove, which forms the obliquely oriented tarsal tunnel (canal). The larger end of this tunnel, the sinus tarsi, lies just anterior to the lateral malleolus, while its smaller end emerges between the medial malleolus and the sustentaculum tali (medially projecting ledge on the calcaneus). Within the tunnel resides the interosseous talocalcaneal ligament, which divides the subtalar from the TCN joint.
The subtalar joint has been described as a ‘shock absorber’ by Kuchera & Kuchera (1994), a designation earned, they say, because ‘in coordination with the inter-tarsal joints, it determines the distribution of forces upon the skeleton and soft tissues of the foot’.
Kapandji (1987) calls the talus ‘an unusual bone’ (due to the fact that it has no muscular attachments) and in view of its role as a ‘distributor’ of loads over the entire foot (Fig. 14.9); also, because ‘it is entirely covered by articular surfaces and ligamentous insertions; hence its name of “relay station”’.
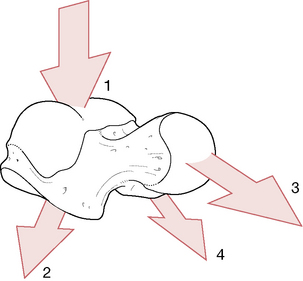
Figure 14.9 The distribution of body weight through the talus
(reproduced with permission from Kapandji 1987).
Mennell (1964) graphically describes this shock-absorbing potential.
Its most important movement is a rocking movement of the talus upon the calcaneus, which is entirely independent of voluntary muscle action. It is this movement which takes up all the stresses and strains of stubbing the toes and that spares the ankle from gross trauma, both on toe-off and at heel-strike, in the normal function of walking and when abnormal stresses …are inflicted on the ankle joint. If it were not for the involuntary rocking motion at the subtalar joint, fracture dislocations would be more commonplace.
Gray’s anatomy (2005) notes that there are anterior and posterior articulations between the calcaneus and talus as described above. However, the subtalar joint, as described in Gray’s anatomy, relates only to the posterior articulation, which has its own joint capsule. The anterior articulation between the talus and calcaneus is then seen to be part of the TCN joint, a viewpoint that has merit and is discussed later in this chapter. As mentioned elsewhere, there is value in considering these joints individually as well as collectively with regard to foot movements.
Schiowitz (1991) describes the major motions of the subtalar joint as:
• calcaneal abduction (valgus), which creates foot eversion (involving fibularis longus and brevis)
• adduction (varus), which creates foot inversion, in relation to the talus (involving tibialis anterior and posterior).
It is worth remembering that these movements cannot occur in isolation but are mandatory simultaneous movements in the three planes of space. The terms used to describe these movements are subject to confusion (see Box 14.1) based on lack of agreement; however, regardless of the term chosen, they move the foot simultaneously in its vertical, horizontal and longitudinal axes. As the medial aspect of the foot is elevated, it is simultaneously adducted and plantarflexed. As the lateral aspect of the foot is elevated, it is simultaneously abducted and dorsiflexed. These movements cannot happen in isolation but instead are triaxial.
Kuchera & Goodridge (1997) describe the joint’s action as being ‘like a mitred hinge’ in which movements of the calcaneus induce rotation of the tibia.
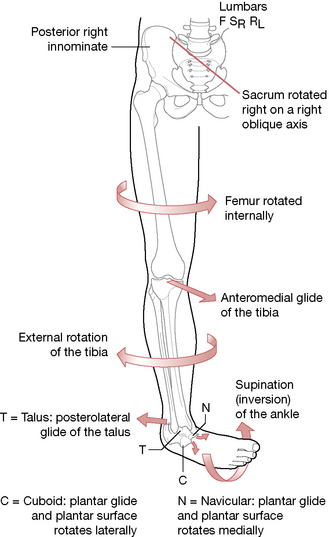
Inversion of the calcaneus produces external rotation of the tibia and the talus glides posterolaterally over the calcaneus. Eversion of the calcaneus produces medial rotation of the tibia and anteromedial glide of the talus on the calcaneus.
Levangie & Norkin (2005) note that:
Although the triplanar motions of pronation/supination can be described by its three componenet (cardinal) motions, these subtalar component motions are coupled and cannot occur independently. The coupled motions must occur simultaneously as the calcaneus (or talus) twists across the subtalar joint’s three articular surfaces.
Ankle sprains
Note: See also the notes in the previous section of this chapter that discuss the relationship between the proximal and distal tibiofibular joints and ankle sprain. See also Box 14.3.
Plantarflexion is the position in which ankle sprains are most likely to occur. Schiowitz (1991) reports that: ‘The most common [ankle] sprain represents an inversion and is usually caused by a combination of plantarflexion, internal rotation and inversion. The lateral ligaments sustain the initial impact’ (Fig. 14.10).
Gray’s anatomy (1995) clarifies the mechanisms of ankle sprain.
So-called sprains of the joint are almost always abduction sprains of subtalar joints, although some medial (deltoid) fibers may also be torn. True sprains are usually due to forcible plantarflexion, resulting in capsular tears in front (most commonly of the anterior talofibular ligament) and bruising by impaction of structures behind the joint.
Merck (2001) report that in ankle sprain, the anterior talofibular ligament (ATL) usually ruptures first after which the fibulocalcaneal ligament (FCL) may separate. Merck suggest that if the ATL is ruptured, examination for associated trauma to the lateral FCL should be carried out. Palpation of the lateral ankle usually rapidly determines the site of the ligamentous injury. If ATL is ruptured during a sprain, anterior displacement of the talus becomes possible. To test this, the patient sits on the side of a table with legs hanging freely. The practitioner places one hand in front of the patient’s leg, while the other hand grasps the patient’s heel posteriorly and attempts to move the talus anteriorly.
Types of ankle sprain
Kuchera & Goodridge (1997) note that:
Instability or loss of neuromuscular control?
Merck (2001) states:
Persons with ligamentous laxity who have extensive subtalar inversion ranges are often prone to inversion injury. Weakness of the peroneal [fibularis] tendons is an occasional predisposing factor that may occur with lumbar disk disease. Forefoot valgus, in which the forefoot tends to evert during the gait cycle, causing the subtalar joint to compensate by inversion, may predispose to ankle sprain. Some persons have an inherited tendency to develop inverted subtalar joints (subtalar varus). [See notes on hypermobility in Chapter 11.]
Richie (2001), who has reviewed the clinical syndrome of functional ankle instability, finds that instability is usually not a result of hypermobility. He asserts that recent evidence has demonstrated that the majority of patients with functional instability of the ankle emphatically do not have mechanical hypermobility of the ankle joint but that functional instability of the ankle results from a loss of neuromuscular control.
The components of neuromuscular control include proprioception, muscle strength, muscle reaction time and postural control. Proprioceptive deficits lead to a delay in peroneal [fibularis] reaction time, which appears to be a peripheral reflex. Proprioception and eversion muscle strength improve with the use of passive supportive devices. Balance and postural control of the ankle appear to be diminished after a lateral ankle sprain and can be restored through training that is mediated through central nervous mechanisms.
Murphy (2000) points out that:
For the nervous system to stabilize the head and neck, it must be aware of the position of the head in space. This requires … knowledge of the head position in relation to the trunk, which, in turn, is dependent on knowledge of the position of the trunk relative to the ground.
Knowledge of trunk position requires that normal afferentation from the foot is forthcoming. However, ‘In the presence of foot dysfunction, the afferentation is compromised and additional responsibility may be placed on the cervical spine for this function’.
O’Connel’s proprioception experiment
Murphy reports on O’Connel’s (1971) experiment in which healthy students were placed on a large swing and were asked, as the swing moved forward, to jump off and land on a large mat. The time taken to achieve erect stance after the jump was noted and postural responses recorded. The test was conducted in three phases.
1. Without visual impedance or altered foot afference (see 2 and 3).
3. Blindfolded and after the feet had been immersed in ice water for 20 minutes (virtually anesthetizing the feet).
The results showed that, with the unimpeded jump, erect stance was achieved in periods ranging from 0.21 to 0.53 seconds. When blindfolded, erect stance was achieved in times ranging from 0.22 to 0.77 seconds. When blindfolded and anesthetized, none of the students was able to achieve erect stance without assistance. The input to the brain from the feet is vital. A simple test offers some evidence for the efficiency of this input.
Test for postural foot reaction
• The patient stands erect and looks straight ahead and is asked to lean the body forward, so that weight is shifted to the forefoot
• A normal reaction is one in which the intrinsic foot muscles contract to produce flexion of the distal interphalangeal joints.
• Abnormal findings (positive test) that suggest poor foot stabilization may include (Murphy 2000):
If the test is positive, Murphy (2000) says, ‘It is important to assess the foot for local dysfunction. This includes examination for joint dysfunction and improper positional relationships’ (see Box 14.2).
Box 14.2 Rehabilitation of disequilibrium/loss of balance
(See Chapter 2 for more detail)
• Adaptive patterns of use such as altered posture and gait, commonly associated with loss of balance, may result from musculoskeletal conditions ranging from ankle sprain to low back pain (Mientjes & Frank 1999, Takala & Korhonen 1998).
• Normalization of balance problems through sensory motor retraining has been shown to lead to reduction in back pain more efficiently than active (manipulative) treatment (Karlberg et al 1995, Liebenson 2001).
• For patients with poor posture involving poor foot reaction to postural stress (see test on p. 514), Murphy (2000) describes balance training in which, initially, the patient performs a ‘marching action’ (marching on the spot), lifting the knees as high as possible, while ensuring that movement is isolated to the hips, i.e. ‘hiking of the iliac crests is avoided’. This action is first performed barefoot and once the pattern of movement is being well performed, wearing balance sandals (which have a hemisphere on the soles, see p. 56–57). Once marching on the spot in balance sandals has been mastered, slow progression of marching (still raising the knees high) while moving slowly forward and then back, or sideways, is performed. Perturbations may also be added (see below).
• Liebenson (2001) describes rehabilitation objectives when loss of equilibrium has manifested. ‘Improving balance and speed of contraction is crucial in spinal stabilization because the activation of stabilizers is necessary to control the neutral zone. The goal of sensorimotor exercise is to integrate peripheral function with central programming. Movements that require conscious and willful activation may be monotonous and prematurely fatiguing to the participant. In contrast, movements that are subcortical and reflexive in nature require less concentration, are faster acting and may be eventually automatized’.
• Mcllroy & Makin (1995) created deliberate ‘perturbation’ in order to challenge the stabilizing mechanisms as a rehabilitation strategy. ‘Unexpected perturbations lead to reactive responses. Expected perturbations lead to anticipatory postural adjustments (APAs). Training can lead to the incorporation of APAs into reactive situations. During a jostle from a stance position the stance leg hip abductors undergo “intense” activation. After APA training the load is decreased.’
• Balance board and wobble board training encourage greater and more rapid strength restoration than isotonic exercises (Balogun & Adesinasi 1992) (see Fig. 2.43).
• Balance sandals encourage hip stabilizer contraction efficiency (Bullock-Saxton et al 1993) (see Fig. 2.44).
• Balance retraining using tactics of standing and walking on thick foam can reduce evidence of ataxia within 2 weeks (Brandt & Krafczyk 1981).
• Tai chi exercises, performed regularly and long term, significantly enhance balance in the elderly (Jancewicz 2001, Wolf 1996, Wolfson & Whipple 1996).
• In order to encourage normal foot function, Janda & Va’vrova (1996) suggest establishing a ‘short foot’. This involves creating a shortened longitudinal arch with no flexion of the toes (accomplished by ‘scrunching’ and raising the arch of the foot without flexing the toes, thereby shortening the arch) (Bullock-Saxton et al 1993, Janda & Va’vrova 1996). This leads to an increased proprioceptive outflow (see Fig. 2.45).
• Lewit (1999) and Liebenson (2001) suggest that with both the feet maintained in a ‘short foot’ state, exercises should proceed from sitting to standing and then on to balance retraining on both stable and labile (such as foam or a rocker board) surfaces.
• In standing, the individual may be encouraged to balance standing on one foot (in a doorway so that support is available if balance is lost!) repetitively, until it is possible to achieve 30 seconds on each foot.
• Additional balance exercises, maintaining ‘short feet’, might involve standing, one leg forward of the other, while maintaining balance in a forward lean (lunge) position.
• With the patient maintaining ‘short feet’, Liebenson (2001) suggests: ‘In order to elicit fast, reflexive responses the patient is “pushed” quickly but gently about the torso and shoulders. This challenges the patient to remain upright and respond to sudden changes in their center of gravity. These pushes are performed in two-leg and in single-leg standing with the eyes open. Closing the eyes while performing these exercises focuses the participant’s awareness on kinesthetic sense and is more challenging to perform’.
• Additional challenges may be introduced when the patient is on an unstable surface (such as a rocker board, on two legs or one) involving a variety of tactics to modify the center of gravity (catching balls, turning the head, etc.). Care should be exercised with elderly or fragile patients to prevent them from falling.
• Tactics similar to the flat surface trainings may be used while both participants are standing in water at about lower chest level, which is especially helpful when working with the elderly to prevent injuries from falling on hard surfaces. These steps may eventually take place in the ocean under calm conditions where mild waves add to the balance challenges.
Box 14.3 Complications associated with ankle sprain (and notes on Arthroscopy)
Meniscoid body
Impingement of a small nodule may occur between the lateral malleolus and the talus, following severe ankle sprains, leading to marked synovitis and possibly chronic fibrotic swelling and induration (Merck 2001). Standard treatment is by means of corticosteroid injections and local anesthetic, introduced between the talus and the lateral malleolus. Adjunctive care should aim at ensuring normal joint play, muscle tone, strength and length, with attention to the gait cycle. Rehabilitation exercises should be introduced to counteract the compensation habits that may have been acquired. When inflammation is active, hydrotherapy and nutritional strategies, as outlined in Chapter 7, may be useful for symptom relief.
Neuralgia of the intermediate dorsal cutaneous nerve
A branch of the superficial fibular nerve crosses over the ATL and this is commonly traumatized during inversion (lateral ligament) sprains of the ankle. Local anesthetic nerve blocks may be helpful. Adjunctive care should include ensuring normal joint play, muscle tone, strength and length, with attention to the gait cycle.
Fibularis tenosynovitis
Chronic eversion of the subtalar joint while walking may lead to swelling below the lateral malleolus resulting from tenosynovitis of the fibularis tendons. When inflammation is active, hydrotherapy and nutritional strategies, as outlined in Chapter 7, may be useful for symptom relief. Attention should be given to the underlying pronation of the subtalar joint by means of orthotics, wedges and/or taping, as well as normalizing joint play and balancing muscle tone, strength and length, with focus on posture and the gait cycle.
Reflex sympathetic dystrophy (Sudeck’s posttraumatic reflex atrophy)
Localized osteoporosis may result from angiospasm, secondary to ankle sprain, leading to a painfully swollen foot. Differential assessment is necessary to screen for ligamentous injury as a cause of the effusion. The reported pain is likely to be out of proportion to the clinical findings in cases of RSD. Merck (2001) suggest: ‘Multiple trigger points of pain moving from one site to another and changes in skin moisture or color are characteristic’. Kappler & Ramey (1997) report that early recognition and treatment are important to prevent permanent disability. RSD may be reversible in its early phases. (See Box 14.4 for discussion of therapeutic approaches for RSD.)
Sinus tarsi syndrome
The precise cause of persistent pain at the sinus tarsi following ankle sprains is unclear, although a partial rupture of the interosseous talocalcaneal ligament or the stem of the inferior cruciate ligament may be to blame (Merck 2001). Misdiagnosis is not uncommon, because if the ATL is tender near the sinus tarsi, patients with persistent pain over the ATL may be misdiagnosed as having sinus tarsi pain. Oloff et al (2001) report that when 29 consecutive patients were examined for sinus tarsi syndrome, using arthroscopy, it was found that there was a history of trauma in 86%, with an inversion sprain being the most common predisposing injury (63%). Twenty-six patients who had additional MRI evaluation all demonstrated chronic synovitis of the subtalar joint and/or fibrosis. Oloff suggests that: ‘Subtalar joint arthroscopy [is] a relatively safe and effective diagnostic and therapeutic technique in the management of sinus tarsi syndrome’. Other standard treatment methods include injection with lidocaine-type drugs.
Ankle arthroscopy
‘Keyhole’ arthroscopic investigation and surgery involves the use of needle-like probes, which may contain minute cameras, lasers or surgical instruments. Use of small instruments and incisions reduces trauma to surrounding tissue and hastens rehabilitation and recovery, so that surgery of this sort may not require a hospital stay.
A variety of procedures can be carried out arthroscopically including diagnosis, biopsy, arthroplasty, fusion (in cases of arthritis, for example), excision of fragments/loose bodies, ligament repair for instability or damage, and cartilage repair or removal.
Box 14.4 Therapeutic considerations for RSD
The etiology of reflex sympathetic dystrophy (RSD) is not yet fully understood. The condition usually involves a distal extremity (commonly hand, wrist, ankle or foot) and is commonly characterized by pain, tenderness and intense burning. Apart from pain, signs may include trophic skin changes, vasomotor instability and demineralization of bone. RSD is most common in people over 50 years of age who have suffered an event such as a stroke, trauma, peripheral neural damage or a myocardial infarction. Excessive sympathetic activity is a feature and this may relate to thoracic spinal dysfunction. Nerve blocks are reported to be effective for a short time but do not appear to offer lasting benefit (Wilson 1991).
The progression of RSD commonly follows three stages:
• In two-thirds of cases, a precipitating event results, within a few weeks, in intense burning pain and warm edema, particularly affecting the joints (whole hand or whole foot usually). Sweating and increased hair growth may be noted in the area.
• Over a period of 3–6 months the overlying skin becomes thinner and shiny and the area cools, although the main symptoms of pain remain.
• Over a further 3–6 months contractures of a potentially irreversible nature appear, as the skin and subcutaneous tissues atrophy.
Kappler & Ramey (1997) note that:
Appropriate mobilization of the patient following a myocardial infarction, stroke or injury may help prevent this condition. Pain should be properly controlled. Exercises are helpful … treatment should focus on reduction of sympathetic tone to the extremity. This includes correcting cervical, upper thoracic and upper rib dysfunctions.
They recommend osteopathic articulation and mobilization methods involving the whole person.
Mense & Simons (2001) summarize the basic science aspects, and clinical aspects, of RSD. In this summary they state:
In the 1950s, the group of symptoms that behaved as though they depended on abnormal sympathetic nervous system activity was included in the generic term ‘reflex sympathetic dystrophy’. By the beginning of the 1990s, it became clear that this term was an oversimplification. It was officially replaced (Merskey & Bogduk 1994) by the noncommittal term ‘complex regional pain syndrome (CRPS)’, which the authors defined as including CRPS type I, which had no known neurological lesion to account for the pain, and CRPS type II, which was associated with partial injury of a nerve.
They suggest that the clinical characteristics include:
1) pain that is intermittent or continuous and often exacerbated by physical or emotional stressors; 2) sensory changes that include hyperesthesia to any modality and allodynia in response to light touch, thermal stimulation (cold or warm), deep pressure, or joint movement; 3) sympathetic dysfunction observed as vasomotor or sudomotor instability in the involved limb; 4) edema of either the pitting or brawny type, that may or may not respond to dependency and elevation of the limb; and 5) motor dysfunctions that may include tremor, dystonia, loss of strength, and loss of endurance of the affected muscle groups.
Since these listed characteristics parallel those produced by trigger points, it would be reasonable to investigate the degree to which trigger points may be involved in perpetuating the condition. Mense & Simons note that clinicians have found that ‘a CRPS seemed to dispose to the development of TrPs in the affected musculature. Frequently, inactivation of the TrPs markedly improved, if not relieved, the symptoms, especially if the intervention occurred within a month or so of onset’. The degree to which trigger points are involved in this and other chronic pain syndromes is in need of focused clinical and scientific research.
Clinical diagnosis of damage due to ankle sprain
• Stress X-rays of the ankle may be useful in determining the extent of ligamentous damage.
• Arthrography of the ankle may help determine the exact site and extent of ligamentous injury (if performed within a few days of the trauma) but this is usually only used if surgical correction of a ruptured ligament is planned.
• MRI can indicate the integrity of the collateral ligaments of the ankle and this assessment method may be used if the patient is allergic to the dye used in arthrography.
Wider implications of ankle sprain injuries
Goodridge & Kuchera (1997) describe the sometimes unpredictable somatic dysfunctions that may occur, in addition to obvious ligamentous stress, during sprain injury of the ankle joint.
• Stretching of lateral compartment (as well as anterior compartment) muscles, encouraging trigger point development.
• The distal fibula may be drawn anteriorly with reciprocal posterior glide of the fibular head, or
• ‘if the anterior talofibular ligament is torn, the distal fibula may move posteriorly with anterior glide of the fibular head’.
• Additionally, the tibia may externally rotate, ‘with an anteromedial glide of the tibial plateau’.
Goodridge & Kuchera (1997) expand on the wider repercussions that may follow such a spread of effects from an ankle sprain.
Myofascial forces then continue upward into the pelvis and spine. Failure to diagnose, and treat or rehabilitate beyond the ankle itself increases recurrence rates, and prolongs the healing and rehabilitation process. It also increases complaints at distant sites due to the patient’s involuntary attempts to compensate for continued dysfunction.
This important warning is one that the authors heartily endorse and that practitioners of all disciplines should heed. The chain reaction of adaptive influences that result from apparently trivial foot and ankle injury or dysfunction do not seem to be well comprehended (by many in the health-care professions as well as the public). In the haste to restore local function following sprains and minor injuries, wider influences resulting from compensation patterns are often ignored or overlooked. An educational effort is needed that encourages the patient to become aware of the vital need for ‘sound foundations’ in general and for the integrity of the structures and proprioceptive functions of the ankles and feet. This is a message that the information in this chapter and of earlier chapters of this text will hopefully reinforce.
Assessment and treatment of the ankle joint and hindfoot
Greenman (1996) strongly suggests that evaluation and treatment of both the proximal and distal tibiofibular joints are necessary before ‘addressing the talotibiofibular mortise articulation’. See discussion and treatment suggestions for tibiofibular joints on pp. 505–506.
Testing joint play and mobilizing the talotibiofibular joint
• As with most paired joints, assessment of the dysfunctional side is helped by comparing it with its normal pair, which requires that the ‘normal’ side be assessed first.
• The patient is supine with the practitioner at the foot of the table holding the leg to be evaluated in her ipsilateral hand (right leg, right hand).
• The patient’s foot should be quite relaxed and not dorsiflexed in any way.
• The patient’s heel should rest in the palm of the hand with the fingers wrapping around the medial aspect.
• The practitioner, using her contralateral thumb and index finger (to the leg being examined), takes hold of the lateral malleolus and glides (translates) it anteriorly and posteriorly while the remainder of the ankle/heel is held firmly in place by the other hand.
• Any restriction in either direction is noted and compared with the other leg.
Assessment of distraction joint play at the talotibiofibular (ankle) and subtalar joints, utilizing long-axis extension (Fig. 14.11)
• The practitioner sits on the edge of the table, approximately halfway along its length, with her back to the supine patient’s torso.
• The patient’s hip (on the side on which the practitioner is seated) is abducted, externally rotated and flexed to not less than 90°.
• Additionally the knee is flexed to 90° and hooked around the practitioner’s torso (see Fig. 14.11).
• The practitioner grasps the leg around the ankle so that the webbing of one hand (if this is the patient’s right leg, it will be her right hand) overlays the dorsum of the foot, close to the talus.
• The webbing of the practitioner’s other hand overlies the Achilles tendon.
• Both of the practitioner’s thumbs rest on the medial aspect of the calcaneus.
• The practitioner leans backward (against the posterior aspect of the patient’s thigh) in order to remove soft tissue slack, easing the foot away from the mortise joint (the foot must remain at right angles throughout).
• A small degree of joint play should be present. If this is absent, repetition of the procedure several times, without force, may mobilize joint play.
• MET procedures may be incorporated, in which, before the attempted long-axis distraction, the patient is asked to introduce a moderately strong isometric contraction of the muscles of the ankle joint, resisted by the practitioner for 5–7 seconds, before the maneuver is attempted.
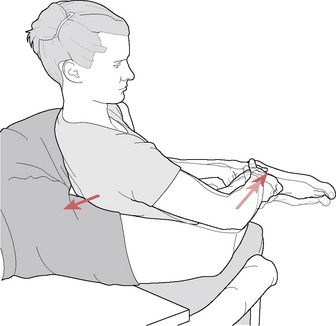
Figure 14.11 Practitioner is seated with back to patient in order to induce long-axis distraction evaluating joint play at the talotibiofibular and subtalar joints
(adapted from Mennell 1964).
Medial and lateral joint play tilt between calcaneus and talus
Additional, subtle joint play movements are possible during long-axis distraction of the joints, as suggested by Mennell (1964).
• ‘Holding the foot and leg with the [joint]…in a position at the limit of long axis extension, the [practitioner] now pushes upward and forward with the hand that is behind the Achilles tendon, thereby rocking the calcaneus forward on the talus.
• Then, the [practitioner] pushes backward and downward with the hand that is on the anterodorsal aspect of the foot to produce the posterior rock of the calcaneus on the talus.
• These movements have nothing to do with plantarflexion and dorsiflexion, which must be avoided (during this procedure)’.
• A degree of joint play involving side tilt (medially and laterally) is also possible when the joints (talotibiofibular and subtalar) are fully distracted.
• In order to assess joint play that tilts the calcaneus in a medial direction, the practitioner’s thumbs, which lie on the medial aspect of the calcaneus, apply ‘pressure laterally upon the calcaneus, tilting the subtalar joint open on its medial aspect. This movement is one of pure tilt of the calcaneus on the talus and is not simple eversion of the foot at the subtalar joint’.
• In order to assess joint play that tilts the calcaneus in a lateral direction, the practitioner’s fingers (of both hands), which lie on the lateral aspect of the calcaneus, apply pressure medially upon the calcaneus, while the thumbs are used as a pivot, so tilting the subtalar joint open on its lateral aspect (i.e. the calcaneus tilts on the talus).
Assessment of the talotibiofibular joint for anteroposterior glide (joint play) (shown for right ankle)
• The patient is supine with the right knee and ankle at 90° and with the heel resting on the table.
• The practitioner stands at the side of the foot of the table, facing the ankle to be assessed, holding the patient’s leg just above the malleoli with her left hand and the dorsum of the foot with the other.
• The right hand is placed on the dorsum of the foot so that the webbing between index finger and thumb spans the anterior talus, stabilizing this throughout the assessment procedure.
• The practitioner’s left hand alternately draws the leg forward and pushes it posteriorly, so inducing anteroposterior glide of the articulating surfaces of the tibia and fibula on the talus (Fig. 14.12).
• There should be a small degree of joint play. If this is absent, repetition of the procedure several times, without force, may mobilize joint play.
• MET procedures may be incorporated in which, before the attempted long-axis distraction, the patient is asked to introduce a moderately strong isometric contraction of the muscles of the ankle joint, resisted by the practitioner for 5–7 seconds, before the maneuver is attempted.
Testing and mobilizing restricted joint play at the distal talocalcaneal (subtalar) joint
• The patient is supine with the practitioner at the foot of the table, holding the anterior ankle area on the side to be evaluated in her ipsilateral hand (right leg, right hand), which is oriented to span the anterior foot so that the webbing between thumb and index finger overlays the neck of the talus, stabilizing it.
• A 90°angle should be maintained between foot and leg as the contralateral hand holds the calcaneus and introduces glide movements of the calcaneus, under the talus, in posterolateral and anteromedial directions.
• The quality of joint play on both sides should be compared.
• If restriction is noted in either direction, repetitive rhythmical springing of the talus at the end of its range should restore normal joint play.
• Alternatively, generalized isometric contractions, involving the patient contracting the muscles of the foot firmly, for 5–7 second periods, followed by repetitive gliding/translating movements, may induce a release.
Differentiating talotibiofibular (ankle) from talocalcaneal (subtalar) dysfunction
Mennell (1964) insisted that it was important to differentiate subtalar (talocalcaneal) problems from those involving the talotibiofibular (or as he termed it ‘mortise joint’) problems.
For the talotibiofibular (ankle) joint, the procedure is as follows.
• The patient is supine, with hip flexed and the knee and ankle (of the side to be tested) both at right angles, with the foot resting on the table surface, on the heel (‘the postero-inferior angle of the calcaneus’), with the sole of the foot unsupported.
• The practitioner is at the foot of the table and, with one hand, holds the anterior aspect of the leg, approximately 15 cm (6 inches) proximal to the ankle joint, while placing the flat of her other hand against the sole of the foot to offer it support and to maintain it in an unchanging plane during the subsequent procedures.
• The hand holding the leg exerts a series of long-axis movements, caudad and cephalad, along the shaft (long-axis) of the tibia, which lightly rocks on the heel support, ‘thereby producing plantarflexion and dorsiflexion of the foot at the mortise joint’ (Fig. 14.13).
• Mennell states that: ‘If these movements are full, free and painless, there is obviously no pathological condition of this [talotibiofibular] joint’.

Figure 14.13 Hand and leg positions for eliciting pure dorsiflexion and plantarflexion of the talotibiofibular joint
(after Mennell 1964).
For the subtalar joint the procedure is as follows.
• All elements of the previous (talotibiofibular) test are maintained. However, in order to assess the subtalar joint, ‘Instead of stopping the plantar-flexion movement at its limit, the [practitioner] now pushes through the limit of this movement, thereby producing a rocking of the talus on the calcaneus’.
• The movement this produces, Mennell states, is not one of hyperflexion (in a plantar direction), which would only assess discomfort in the anterior ligaments of the ankle joint.
• Instead, this test depends for its efficacy on a resistance, or friction, effect between the heel and the table surface, as the caudally directed push is made on the tibia (Fig. 14.14).
• Mennell explains: ‘This friction force is sufficient to stabilize the calcaneus while the talus rocks forward upon it. Pain on the performance of this movement indicates [dysfunction] giving rise to pain at the subtalar joint’.

Figure 14.14 Hand and leg positions for eliciting rocking of the talar on the calcaneus to test for subtalar dysfunction
(adapted from Mennell 1964).
Assessment for plantar and/or dorsiflexion restriction at the talotibiofibular joint
• The patient sits on the edge of the table with both legs hanging freely over the edge.
• The practitioner sits/squats in front of the patient, supporting both feet in her hands.
• The practitioner simultaneously, or separately, assesses and compares plantarflexion.
• Still supporting the feet, the practitioner places her thumbs onto the anterior surface of the neck of the talus, on each foot.
• The practitioner moves the feet posteriorly toward the table, inducing dorsiflexion at the ankle.
• As this occurs the talus should glide posteriorly and the degree and feel of this movement are compared.
• Greenman (1996) notes that there is likely to be tenderness on the side of a palpated talus that fails to adequately move posteriorly on dorsiflexion.
• A muscular cause of restricted dorsiflexion would be shortness of gastrocnemius and/or soleus.
• Dysfunction of the tibiofibluar joints should also be assessed to assure appropriate movement of the fibula during dorsiflexion.
MET treatment of dorsiflexion restriction at the talotibiofibular joint
• The patient sits on the edge of the table with both legs hanging freely over the edge.
• The practitioner sits/squats in front of the patient and supports the plantar surface of the forefoot with one hand, while placing the webbing between index finger and thumb, of the other hand, against the neck of the talus.
• The easy (unforced) dorsiflexion barrier is engaged by a combination of hand efforts that simultaneously dorsiflex the foot and apply posterior force to the neck of the talus.
• The patient is asked to plantarflex against the practitioner’s unyielding resistance, for 5–7 seconds, utilizing no more than 25% of available muscle strength.
• On complete relaxation the practitioner takes out slack and engages a new restriction barrier.
MET treatment of plantarflexion restriction at the talotibiofibular joint
• The patient is supine with the affected leg in neutral
• The practitioner is at the foot of the table, lateral to the leg to be treated.
• The practitioner cups the patient’s heel in her nontableside hand, while placing the palm of her tableside hand over the dorsal surface of the foot.
• The ankle should be plantarflexed to its easy (nonpainful) barrier.
• The patient is asked to dorsiflex the foot (‘Try to flex your ankle by bringing your toes and the top of your foot toward your knee, against the pressure of my hand, using only about a quarter of your strength’).
• The practitioner resists the effort, so inducing an isometric contraction, which should be held for approximately 7 seconds.
• On complete relaxation, the foot should be taken to its new restriction barrier, without force and the process repeated.
PRT treatment of medial (deltoid) ligament dysfunction
• Tender points for dysfunction involving the medial deltoid ligament are located inferior to the medial malleolus. The area should be palpated and the most sensitive ‘point’ identified.
• The patient is sidelying, affected leg uppermost, flexed at hip and knee, with the distal calf supported by a cushion, and the affected ankle extended over the edge of the table.
• The practitioner stands close to the foot facing the side of the table and with the index or middle finger of her caudad hand locates and applies pressure to the previously identified tender point, inferior to the medial malleolus. The patient is asked to register a score of ‘10’ for the discomfort noted at the point of pressure.
• The practitioner holds the patient’s calcaneus with her cephalad hand and with this contact induces an adduction of the calcaneus (inversion of the ankle), folding it over the contact finger on the tender point, which should reduce the reported ‘pain score’.
• Further fine-tuning toward a position of ease for the joint that may involve rotation or compression of the ankle, with score reductions indicating that the directions being produced are helpful (and vice versa).
• The final position of maximum ease, once a 70% reduction in the original pain has been achieved, is held for 90 seconds before returning slowly to neutral.
PRT treatment of anterior talofibular ligament dysfunction
• The tender point for dysfunction involving the anterior talofibular ligament is located approximately 2 cm (0.8 inches) anterior and inferior to the lateral malleolus, in a slight depression on the talus. The point should be located by palpation.
• The patient is sidelying, affected leg on the treatment table, flexed at hip and knee, distal fibula supported by a cushion, with the affected ankle extended over the edge of the table.
• The practitioner stands close to the foot facing the side of the table, and with the index or middle finger of her caudad hand locates and applies pressure to the previously identified tender point, inferior and anterior to the lateral malleolus. The patient is asked to register a score of ‘10’ for the discomfort noted at the point of pressure.
• The practitioner holds the patient’s calcaneus with her cephalad hand and with this contact induces an abduction of the calcaneus (eversion of the ankle).
• The reported pain score should decrease markedly once the correct angle of eversion is achieved.
• Further fine tuning toward a position of ease for the joint may involve rotation or compression of the ankle, with score reductions indicating that the directions being produced are helpful (and vice versa).
• The final position of maximum ease, once a 70% reduction in the original pain has been achieved, is held for 90 seconds before returning slowly to neutral.
MWM treatment of restricted talotibiofibular joint and for postinversion sprain
Mulligan (1999) suggests that this joint may display loss of joint play following inversion (lateral ligament) sprains of the ankle. He describes a slightly different hold, when using MWM, from that outlined in the assessment above, although that hold is also effective.
• The patient is supine and the practitioner is at the foot of the table.
• The practitioner applies her contralateral thenar eminence to the anterior aspect of the lateral malleolus, fingers wrapped loosely around the Achilles tendon.
• The other hand is placed so that the thenar eminence lies posterior to the medial malleolus, with fingers overlapping posteriorly.
• The fibula is painlessly glided posteriorly and slightly superiorly (along the line of the anterior talofibular ligament) while at the same time the patient is asked to slowly invert the foot.
• This movement should be more easily accomplished while the fibula is held in this translation position.
• If the inversion is painless, the patient is asked to repeat this 5–10 times.
• If the fibular glide is uncomfortable the angle of pressure on it should be slightly modified.
• Mulligan suggests that: ‘The repositioning of the fibula should be undertaken as soon as possible after an inversion sprain’. He also suggests that taping be used to hold the fibula in a posterior/superior direction for several days, during the period when RICE protocols are being followed and that within 48 hours MWM should be attempted.
Common disorders of the hindfoot
Calcaneal spur syndrome (and plantar fasciitis)
The calcaneal spur syndrome is characterized by the presence of a benign growth extending away from the bone and often accompanied by extreme heel pain in the area of the inferior calcaneus, caused by the pull of the plantar fascia (and sometimes by the insertion of the Achilles tendon) on the periosteum. There may be no obvious evidence of a heel spur on X-ray (Merck 2001). Note: A negative X-ray for bone spur is not conclusive, as in the early stages visual evidence is often minimal.
Spurs may result from excessive traction on the calcaneal periosteum by the plantar fascia. The stretching may lead to pain along the inner border of the plantar fascia (plantar fasciitis). It is considered that flat feet and contracted heel cords may contribute to the development of spurs through increased plantar fascial tension (Merck 2001).
• If there is no X-ray evidence of a spur, pain in this region may be the result of active trigger points (for example, from quadratus plantae or soleus) (Travell & Simons 1992).
• A bursa may develop and become inflamed (inferior calcaneal bursitis), in which case the heel may start to throb and become warm. Assessment: firm thumb pressure onto the center of the heel will evoke a painful response.
• If pain is reported when firm digital pressure is applied along the inner border of the fascia with the ankle in dorsiflexion, plantar fasciitis is probable. Manual release of triceps surae and plantaris may be helpful.
• Differential diagnosis is necessary to distinguish simple fasciitis and calcaneal spur from ankylosing spondylitis, Reiter’s syndrome, rheumatoid arthritis and gout, any of which might involve moderate-to-severe inflammation and swelling. Differential diagnosis may require scan, X-ray and blood test evidence.
First aid involves the RICE protocol and introducing mild antiinflammatory strategies (see Chapters 6 and 7). Treatment may involve methods that release excessive tension in the plantarflexors and fascia and deactivate associated trigger points. Attention should also focus on achieving normal muscle tone, strength and length, with particular focus on the individual’s gait cycle, with use of rehabilitation exercises to counteract any compensation habits acquired during periods of pain. Orthotic control and strapping may be useful in rehabilitation. Short-term use of NSAID medication and, in extreme circumstances, steroid injections and/or surgery may be called for. Habits of use regarding the feet (such as hooking them on a chair rung when working) should be considered as should overall postural positioning.
Epiphysitis of the calcaneus (Sever’s disease)
This condition involves painful cartilage break in the heel, affecting children.
Usually, before age 16, when ossification of the calcaneus (which develops from two centers of ossification) is incomplete, excessive strain involving vigorous activities may cause a break in the cartilage that connects the two, as yet non-united bones. Diagnosis is based on the patient’s age, the identification of pain along the heel growth centers on the margins of the heel and a history of vigorous activity. Warmth and swelling may occasionally be present. The condition cannot be diagnosed radiographically.
Heel pads may be helpful in reducing the pull of the Achilles tendon on the heel, as might treatment of the triceps surae. Immobilization in a cast is usually required and recovery may take several months. Subsequent attention should focus on achieving normal muscle tone, strength and length, with particular focus on the individual’s gait cycle, with use of rehabilitation exercises to counteract the compensation habits acquired during immobilization.
Posterior Achilles tendon bursitis (Haglund’s deformity)
This condition, which occurs mostly in young women, involves an inflamed bursa overlying the Achilles tendon attachment associated with a prominent bony enlargement of the calcaneus. It commonly results from variations in heel position and function and inappropriate footwear, particularly high heels. Merck (2001) states:
The heel tends to function in an inverted position throughout the gait cycle, excessively compressing the soft tissue between the posterolateral aspect of the calcaneus and the shoe counter (the stiff, formed heel portion). This aspect of the calcaneus becomes prominent, can be palpated easily and often is mistaken for an exostosis.
Early signs include increased redness and induration, often ‘protected’ by adhesive tape to ease shoe pressure. If the inflamed bursa enlarges, a painful red lump develops over the tendon. In time, the bursa may become fibrotic and calcium may further enlarge the process.
Treatment might involve foam rubber or felt heel pads, in order to elevate the heel (as well as padding around the bursa initially), plus ensuring that shoe pressure is minimized. Use of an orthotic to prevent abnormal heel motion may also be helpful. Antiinflammatory medication offers short-term benefit only. Medical treatment might involve infiltration of a soluble corticosteroid to ease inflammation. Excision of the posterolateral aspect of the calcaneus is sometimes suggested by surgeons in severe recurrent cases.
Adjunctive care should include ensuring normal muscle tone, strength and length, with attention to the gait cycle, with use of rehabilitation exercises to counteract the compensation habits that may have been acquired. When inflammation is active, hydrotherapy and nutritional strategies, as outlined in Chapters 6 and 7, may be useful for symptom relief.
Anterior Achilles tendon bursitis (Albert’s disease)
The bursa, which lies anterior to attachment of the Achilles tendon to the calcaneus, may become inflamed due to injury or in association with inflammatory arthritis. It would be aggravated by anything that added strain to the Achilles tendon, including inappropriately high or rigid shoes.
Symptoms may arise suddenly in case of trauma, whereas if the bursa is being irritated by a systemic problem, such as arthritis, a slow evolution is likely. Swelling and heat, together with pain, will be noted in the retrocalcaneal space. Walking and tight shoes are likely to aggravate the symptoms, which over time extend medially and laterally, beyond the area anterior to the tendon.
Differential diagnosis is necessary to distinguish bursitis from a fractured posterolateral tubercle (see below and Box 14.5) or degenerative changes to the calcaneus (as may occur in rheumatoid arthritis). These conditions would be confirmed by X-ray, whereas the bursitis is characterized by warmth and swelling contiguous to the tendon, with pain noted mainly in the soft tissues. Rest and hydrotherapy may offer relief but when inflammation is severe, an intrabursal injection of a soluble corticosteroid is commonly helpful. Subsequent attention should focus on achieving normal muscle tone, strength and length, with particular focus on the individual’s gait cycle, with use of rehabilitation exercises to counteract the compensation habits acquired during immobilization.
Box 14.5 Common fractures of the ankle and foot
Thordarson (1996) reports that some of the most common, and potentially serious, ankle and hindfoot fractures involve the tibial plafond, malleolus, calcaneus and talus (including osteochondral lesions). He suggests that many fractures, such as that of the lateral process of the talus, can be managed conservatively with casts, but that severe or displaced fractures usually require surgery. Standard rehabilitation protocols typically focus on rest as well as strengthening and stretching exercises.
Fractures of the ankle and hindfoot usually occur as the result of a traumatic episode whereas chronic injuries, such as stress fractures, are more likely in the midfoot and forefoot (and the leg). McBryde (1976) reported that 95% of all stress fractures in athletes involve the lower extremity, with the upper third of the tibia (the site of approximately 50% of all stress fractures seen in adolescents), the metatarsals and the fibula also being common sites (see notes on stress fracture in Chapter 5).
Adjunctive rehabilitation following most fractures requires application of the methods outlined in this text: normalization of joint play, range of motion, muscle balance (involving normalizing shortness and/or weakness), deactivation of trigger points and a combination of toning, stretching and general rehabilitation exercises. Additionally, in regards to foot injuries, neurological rehabilitation and restoration of balance mechanisms should also be addressed.
Ankle fractures
An important initial distinction with ankle fractures is whether the malleolus is involved or the more severe tibial plafond (pilon) intraarticular impaction fracture.
Tibial plafond fractures usually result from a high-energy axial load, such as occurs in a fall from a height or an MVA. Pain would be immediate and walking impossible. Assessment demonstrates significant swelling with or without deformity. Thordarson (1996) notes that: ‘These fractures – in contrast to malleolus fractures – involve the weight-bearing surface of the plafond and generally require open reduction and internal fixation. Results are frequently poor despite operative intervention’.
Malleolus fracture
These are relatively common and can involve the lateral or medial malleolus or both. The cause is usually an external rotation injury to the ankle. Accompanying ligament damage is routine, most often of the deltoid ligament and of the anterior and posterior tibiofibular ligaments. There is immediate pain and difficulty in walking. Effusion and bony sensitivity are noted over the fracture site(s), with or without a visible deformity. Malleolus fractures are typically classified by the position of the foot at the time of injury or in relation to the level of the fibular fracture, relative to the ankle joint.
The standard medical treatment for displaced malleolus fractures is closed reduction and casting followed by ice and elevation. However, Thordarson (1996) points to some of the hazards relating to the setting of the reduced fracture.
If an anatomic reduction is obtained, these fractures can be managed with a cast. However, post-reduction radiographs must show that the joint space is symmetric on a mortise view, because even 1 to 2 mm of displacement of the talus within the mortise can cause dramatic changes in the contact area and pressures within the ankle. One study (Ramsey & Hamilton 1976) demonstrated a 40% decrease in contact area with a 1-mm lateral shift of the talus. Because of this potential for change in the contact area and pressure in the ankle with an intraarticular fracture, surgeons recommend open reduction and internal fixation of persistently displaced malleolus fractures to guarantee an anatomic reduction. An added benefit of operative treatment in an athlete is a more aggressive, early rehabilitation. Range-of-motion exercises can be started after wound healing, but compliance with non-weight bearing must be emphasized.
• Most patients with a malleolus fracture require 6 weeks of immobilization.
• Patients with a displaced ankle fracture that has undergone successful closed reduction will typically require 2 to 4 weeks in a long-leg cast and then an additional 2 to 4 weeks in a short-leg nonwalking cast.
• Patients with an initially nondisplaced fracture or who were treated surgically will generally require 4 weeks of non-weight bearing in a short-leg cast or removable walking boot, followed by 2 weeks in a walking cast or boot. The removable boot will allow for earlier range-of-motion exercises.
• In patients treated nonoperatively, follow-up radiographs must be obtained weekly for the first 2 to 3 weeks following injury to rule out fracture displacement.
• Following fracture healing, patients can begin physical therapy for range-of-motion and strengthening exercises. Most patients who sustain a malleolus fracture will miss at least 3 months from most sports, and frequently 6 months or more from impact sports.
Maisonneuve fracture
This serious injury involves an external rotation injury of the ankle with an associated fracture of the proximal third of the fibula. This is often misdiagnosed and can result in long-term disability.
Presentation will involve external rotation of the foot and medial ankle pain. Tenderness on palpation will be noted over the deltoid ligament and the fracture site. Anyone who reports proximal fibular tenderness after a twisting injury to the ankle should be referred for X-rays of the ankle, the tibia and fibula.
If a fibula fracture is found, an open reduction and internal fixation with screws is usual. These are generally removed 8–12 weeks after surgery.
Calcaneus fractures
These occur most commonly after high-energy axial loads, frequently during athletic activity, or in association with an avulsion of the Achilles tendon. About three-quarters of calcaneal fractures extend into the subtalar joint (De Lee 1993).
Thordarson (1996) notes that:
Following a fracture, patients have severe heel pain and cannot walk. They have moderate-to-severe hindfoot swelling and tenderness on exam…any displacement warrants a computed tomography (CT) scan. Initial treatment for displaced and nondisplaced intra-articular fractures includes immobilization in a bulky dressing and splint, with ice and elevation to control edema. Most displaced fractures are managed operatively, but these patients typically experience residual stiffness of their subtalar joint that will adversely affect future athletic performance. For nondisplaced extra-articular calcaneus fractures, patients wear a short-leg cast or walking boot for about 6 weeks.
When the fracture results from avulsion this usually involves a violent contraction of the gastrocnemius and soleus. This form of calcaneal fracture can usually be managed in a plantarflexed short-leg cast for 6 weeks followed by physical therapy involving stretching. However, surgery is needed if displacement is significant.
Talus neck fractures
These are relatively uncommon and result from trauma involving hyperdorsiflexion of the ankle. This might occur in an MVA where the ankle is hyperdorsiflexed by the brake pedal. An extremely serious concern relates to the potential complication of avascular necrosis of the talus. Severe hindfoot pain and moderate-to-severe edema, tenderness and ecchymosis are the presenting features. The body of the talus may be palpable in the posteromedial ankle area.
Thordarson (1996) insists that:
Displaced talar neck fractures are true surgical emergencies. The fracture must be reduced immediately to minimize the risk of avascular necrosis or skin slough. The talus has limited vascularization; most of its blood supply enters the neck via an anastomotic sling and flows posteriorly. A fracture, therefore, disrupts the intraosseous portion of the blood supply, and the greater the displacement, the greater the disruption of the blood supply and likelihood of necrosis. Avascular necrosis may lead to collapse of the body of the talus, resulting in arthritic changes that necessitate ankle fusion. Even without avascular necrosis, many patients develop a significant degree of subtalar arthrosis or arthritis, which leads to residual hindfoot stiffness and pain. Treatment for patients who have a nondisplaced talar neck fracture typically involves a short-leg nonwalking cast for 6 to 8 weeks followed by range-of-motion exercises.
Fracture of the posterolateral talar tubercle
A plantarflexion injury that forces the posterior inferior lip of the tibia against the talar tubercle may result in fracture. This sort of injury may occur following a sudden jump onto the ball of the foot or toes, such as may occur in basketball or tennis, or when stepping backward and down with force, after standing on a chair. Individuals with elongated lateral talar tubercles seem particularly prone to this injury (Merck 2001).
Signs and symptoms include pain and swelling behind the ankle, with difficulty walking downhill or downstairs. There may be unremitting swelling, but obvious inflammation is seldom more than mild. Pain is brought on by the action of plantarflexion, while dorsiflexion of the large toe may also aggravate the pain. The diagnosis is confirmed by means of a lateral X-ray.
Medical treatment, as for most fractures, is by immobilization in a cast for 4–6 weeks, with standard use of antiinflammatory and pain-relieving medication. Rarely, surgery may be necessary. Adjunctive care should include ensuring normal muscle tone, strength and length, with attention to the gait cycle. Rehabilitation exercises should be introduced to counteract the compensation habits that may have been acquired during immobilization. When inflammation is active, hydrotherapy and nutritional strategies, as outlined in Chapters 6 and 7, may be useful for symptom relief.
Fracture of the lateral talar process
The typical mechanism of this trauma involves acute hyperdorsiflexion with inversion. The patient will report lateral ankle pain and effusion and local tenderness will be noted. A lateral X-ray shows a fragment of the lateral process along the inferior aspect of the talus. Surgery may be called for and a short-leg cast for 6 weeks is usual.
Osteochondral injury of the talus dome
Thordarson (1996) notes that:
A more common talus injury in sports is an osteochondral fracture of the dome of the talus that results from an inversion injury. A related, chronic condition probably caused by repetitive trauma is osteochondritis dissecans (OCD). … it is postulated that the corner of the talus fractures as the dome rotates laterally through the mortise … If the fragment displaces, they will experience locking or clicking.
Examination reveals tenderness over the lateral aspect of the talar dome. Radiographs may demonstrate a small flake of bone off the lateral dome of the talus. Patients tend to report a gradual onset of pain that is activity related. If the fragment displaces, locking may occur. Treatment may involve arthroscopy (see Box 13.2 and notes in Box 14.3) or other forms of surgery and the use of a cast for 6 weeks. Patients are cautioned to avoid weight bearing for 6 weeks while fibrocartilage is forming, although range-of-motion exercises should be performed.
Achilles tendinitis and rupture (clement 1984, rolf & movin 1997, teitz et al 1997)
Athletic overuse, change of terrain such as unaccustomed running up hill, a sudden increase in distance covered or the wearing of inappropriate shoes can all cause extreme stress to the Achilles tendon. Tendinitis is characterized by persistent pain and swelling and often by grating or crackling sensations as the ankle is moved into flexion and extension.
There may be clinical evidence of inflammation (redness, swelling, etc.) without histological evidence, in which case the correct term is tendinosis rather than tendinitis. Tendinosis may be related to localized areas of diminished blood supply just above the tendon insertion and may remain subclinical until a rupture occurs. Heel cord contractures may be present. Training errors in adults in their 30s and 40s, most commonly associated with running, are major contributory features.
Antiinflammatory strategies (RICE, etc.) are called for as well as avoiding undue pressure on the tendon. Use of cushioned shoes, and sometimes raising the heel to ease tendon stress, may help. Careful stretching is necessary and diligent warm-up protocols should be followed if active exercise is continued. There remains a risk of tendon rupture. If this occurs pain may be marked and there will be an inability to stand on tiptoe on the injured foot. Surgery or a cast is required. Any massage applied should be careful to avoid actively inflamed tissue but manual lymphatic drainage and gentle massage and stretching of healing tissue (after the first 2 weeks or so) may reduce scar tissue formation.
Posterior tibial nerve neuralgia
The posterior tibial nerve passes through a canal (tarsal tunnel) at the level of the ankle, where it divides into the medial and lateral plantar nerves. Fibroosseous compression of the nerve within the canal (tarsal tunnel syndrome), synovitis involving the flexor tendons of the ankle or inflammatory arthritis creating pressure on the nerve may all induce neuralgia. If swelling accompanies the neuralgia its source should be established (venous, inflammatory, rheumatic, traumatic, etc.).
Symptoms include pain (sometimes of a burning or tingling nature) in and around the ankle, which commonly reaches the toes. The pain is worse on walking (and sometimes on standing) and eased by rest.
When the nerve is irritated, tapping or applying light pressure to the posterior tibial nerve below the medial malleolus, at a site of compression or injury, often produces distal tingling (Tinel’s sign). Confirmation of the diagnosis of posterior tibial nerve neuralgia is by electrodiagnostic testing.
Treatment is commonly by means of strapping the foot into a neutral or slightly inverted position or may involve the wearing of orthotic supports that maintain inversion, so reducing tension on the nerve. If there is no neural compression within the canal, corticosteroid injections or, in severe unremitting cases, surgery may be suggested. Subsequent attention should focus on achieving normal muscle tone, strength and length, with particular focus on the individual’s gait cycle, with use of rehabilitation exercises to counteract the compensation habits acquired during immobilization.
The midfoot
The foot can be divided into three functional segments: the hindfoot (calcaneus and talus), the midfoot (navicular, cuboid and three cuneiforms) and the forefoot (five metatarsals, 14 phalanges and two sesamoids). These segments interact to create a multitude of movement possibilities. The talocrural (ankle) joint and the talocalcaneal (subtalar) joint, constituting the ankle and hindfoot, have been discussed. The complex components of the talocalcaneonavicular joint (TCN) are considered independent of the transverse tarsal (or midtarsal) joint, a compound joint composed of the talonavicular and calcaneocuboid joints. The tarsometatarsal joints and interphalangeal joints, collectively known as the forefoot, along with a multitude of supporting ligaments, add to the elaborate structure of the foot (Figs 14.15, 14.16).
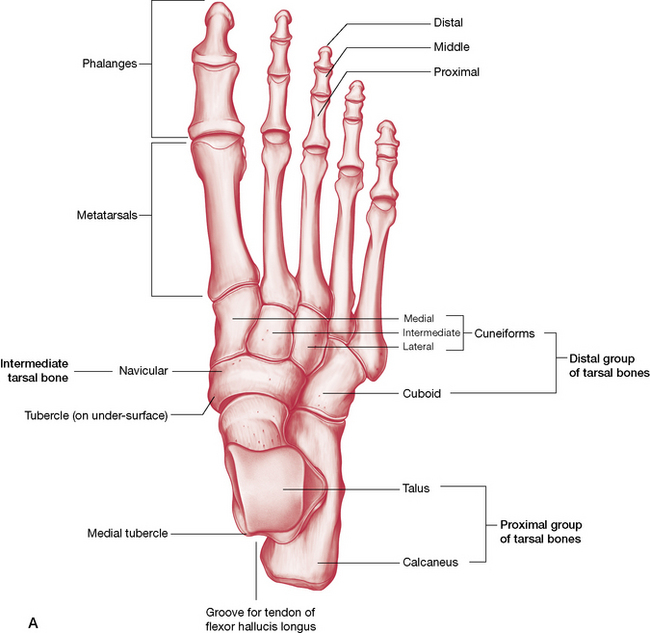
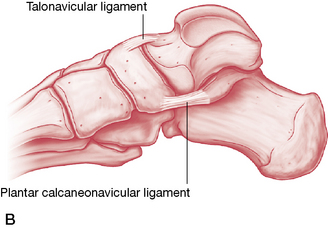
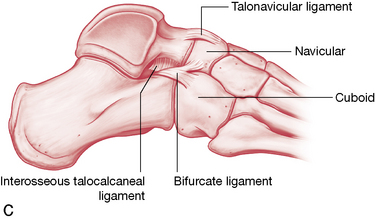
Figure 14.15 Bones of the foot A) dorsal aspect; B) medial aspect; C) lateral aspect.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
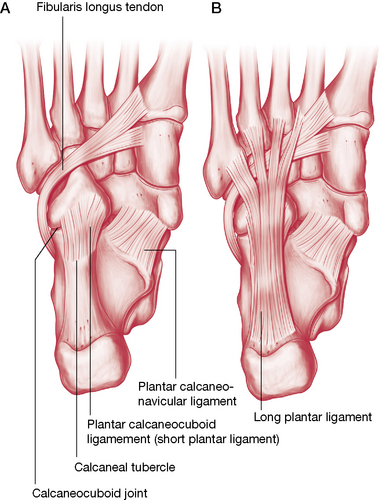
Figure 14.16 Plantar aspect of the bones, ligaments and tendons of the foot
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
The transverse tarsal joint, also known as the midtarsal joint, transects the foot to divide the hindfoot from the midfoot (see Fig. 14.18). This ‘S’-shaped compound joint is one of two common sites of amputation of the foot. Though the talonavicular joint is considered as part of the transverse tarsal joint (see discussion below), it is also helpful to consider it as part of a more complex, multiaxial, compound articulation known as the talocalcaneonavicular joint.
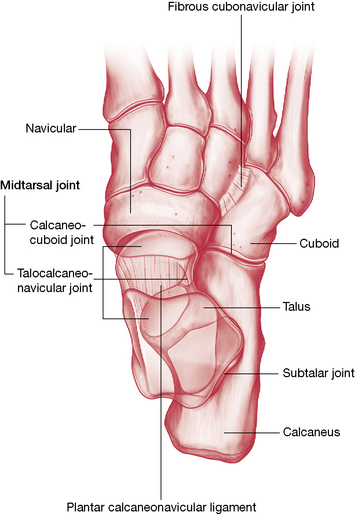
Figure 14.18 The transverse tarsal joint (talonavicular and calcaneocuboid joints) and the metatarsophalangeal joints.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Talocalcaneonavicular (TCN) joint
The talonavicular joint is the most anterior part of a more complex joint, the talocalcaneonavicular (TCN) joint (Fig. 14.17). Like the subtalar joint, it is a triplanar joint producing simultaneous movements across longitudinal, vertical and horizontal axis (supination/pronation, inversion/eversion). Because the TCN joint is a compound joint, having several articular surfaces in different planes, any movement produced by the talus results in mandatory motion at each of these surfaces.
In a previous edition of their work, Levangie & Norkin (2001) described the TCN as the ‘key to foot function’, skillfully illustrating an interesting view with their description of this joint.
The talonavicular articulation is formed proximally by the anterior portion of the head of the talus and distally by the concave posterior navicular. The talar head, however, also articulates inferiorly with the anterior and medial facets of the calcaneus and with the plantar calcaneonavicular [spring] ligament, that spans the gap between the calcaneus and navicular below the talar head. Consequently, we can visualize the TCN as a ball and socket joint where the large convexity of the head of the talus is received by a large ‘socket’ formed by the concavity of the navicular, the concavities of the anterior and medial calcaneal facets, by the plantar calcaneonavicular ligament and by the deltoid ligament medially and the bifurcate ligaments laterally.
All of this is enclosed by a single capsule, hence the description of this complex as being a ‘joint’. The TCN joint capsule is reinforced by ligamentous support from the superomedial portion of the cartilage covered calcaneonavicular ligament (forming a sling for the head of the talus, which articulates with it), the inferior calcaneonavicular ligament, the medial and lateral collateral ligaments, inferior extensor retinacular structures, cervical ligament and the dorsal talocalcaneal and interosseous ligaments. Additionally, it gains support from related ligaments associated with the adjacent calcaneocuboid joint.
In a subsequent edition of their textbook, Levangie and Norkin (2005) put less emphasis on consideration of the TCN structure as a joint. ‘…it might be argued that even this compound term is incomplete. The talus in weight-bearing also can be considered to act as a ballbearing between three joints: (1) the tibiofibular mortise (the ankle joint) superiorly, (2) the calcaneus (the subtalar joint) inferiorly, and (3) the navicular bone (talonavicular joint) anteriorly. In weight-bearing supination/pronation, the talus dorsiflexes and plantarflexes within the mortise, as well as on the calcaneus and the navicular bone. Abduction/adduction of the talus during supination/pronation not only occurs on the calcaneus and the navicular bone but also affects the position of the mortise as the body of the talus laterally and medially rotates.’ It should also be borne in mind that each of these movements translates forces to all surrounding structures that must interact with weight distribution from above (influenced by balance, objects being carried, etc.) and ground reaction forces from below (influenced by terrain, speed, etc.). It is not surprising that anatomical terminology fails miserably in describing the complexities of the foot.
Transverse tarsal joint
The talonavicular and calcaneocuboid joints together form the compound transverse tarsal joint, an ‘S’-shaped joint that divides the hindfoot from the midfoot (Fig. 14.18). Forefoot range of movement in triaxial rotation (supination/pronation) is thereby increased by simultaneous gliding of the talonavicular and calcaneocuboid joints. As the medial edge of the foot is lifted (supinated, inverted) the talar head rotates on the navicular while cuboid glides down the calcaneus in an opposite movement. This transverse tarsal movement adds to the supination/pronation ranges occurring as a result of subtalar movement, and allows ‘the forefoot to remain flat on the ground (relatively immobile) while the hindfoot (talus and calcaneous) pronates or supinates in response to the terrain or the rotations imposed by the leg.’ (Levangie & Norkin 2005).
An important function of this joint is allowing tibial rotation to be absorbed by the hindfoot, without translating these destabilizing forces into the forefoot, a response that is critical to stability of the gait foot. The converse is also true, especially when on rough terrain. That is, if the forefoot must adjust to a rocky surface, the transverse tarsal joint absorbs forefoot rotation, reducing the translation of these forces into the hindfoot and subsequently, through the ankle joint, into the leg, knee and hip.
Talonavicular joint
On the distal end of the anteriorly protruding neck of the talus is a convex facet, which articulates with the concave proximal surface of the navicular bone.The wider talar surface allows for significant gliding, resulting in supination/pronation as the talus moves on the relatively fixed navicular bone. On the navicular’s distal surface are three concave surfaces, which articulate with three cuneiform bones. Weight is transferred through the talus to the navicular, which in turn transfers it to the three cuneiforms.
Calcaneocuboid joint
Lateral to the talonavicular joint lies the calcaneocuboid joint where the cuboid is effectively interposed between the calcaneus proximally and the 4th and 5th metatarsals distally. The fibularis longus crosses the cuboid in a groove on the plantar surface. On the cuboid’s medial surface lies an oval facet for the lateral cuneiform and usually another (proximal medial surface) for the navicular, a smooth vertical ridge separating their shared continuous surface (Gray’s anatomy 2005). Proximally the cuboid and calcaneus form a complex, obliquely set concavoconvex articular facet. Due to the unique joint shape (see below), movement at this joint is more limited than at the talonavicular joint. Their reciprocal action is a key to foot function.
Levangie & Norkin (2005) explain its movements.
The articular surfaces of both the calcaneus and the cuboid are complex, being reciprocally concave/convex both side to side and top to bottom. The reciprocal shape makes available motion at the calcaneocuboid joint more restricted than that of the ball-and-socket-shaped talonavicular joint. As the calcaneus moves at the subtalar joint during weight-bearing, activities it must meet the conflicting intra-articular demands of the opposing saddle-shaped surfaces, which results in a twisting motion
Regarding the longitudinal axis of the foot, Levangie & Norkin (2005) suggest:
Motion around this [longitudinal] axis is triplanar, producing supination/pronation with coupled components similar to those seen at the subtalar joint but now simultaneously including both the talus and calcaneus segments moving on the navicular and cuboid segments. Unlike the axis of the subtalar joint, the longitudinal axis of the transverse tarsal joint approaches a true A-P axis, and so the inversion/eversion components of the transverse tarsal movement predominate.
Full supination results in both TCN and transverse tarsal joints being placed in a locked, close-packed position, while pronation results in both joints being loose packed and mobile.
Tarsometatarsal (TMT) joints
The tarsometatarsal joints, composed of the articulation of the distal surface of the three cuneiforms and cuboid with the bases of the five metatarsals, have varying mobility (least mobile is the second metatarsal) and some shared capsules (2 and 3 share, 4 and 5 share).
In the medial column, the navicular articulates with the three wedge-like cuneiform bones, which in turn articulate with the first three metatarsals. Laterally, the cuboid articulates directly with the last two metatarsal bones. The cuneiform bones wedge together to form a transverse arch (see Box 14.6). Additionally, the medial and lateral cuneiforms project distally beyond the middle one, which forms a recess for the second metatarsal base and stabilizes it against motion.
The plantar vault is a structure that uses concepts of triangular equilibrium, with the anterior aspect of the triangle being a ‘floating’ component, which is bound somewhat at the posterior tarsus. The vault provides a dynamic component to gait while functional arches act as elastic shock absorbers. Unless exercised on actual ground surfaces (beaches, rocky slopes), the ability of the arches to ‘hollow’ and to adapt to ever-changing terrain is often lost to the town dweller, who almost always walks on even, firm ground.
Regarding the plantar vault, Kapandji (1987) eloquently states:
The plantar vault is an architectural structure which blends all the elements of the foot – joints, ligaments and muscles – into a unified system. Thanks to its changes of curvature and its elasticity, the vault can adapt itself to unevenness of the ground, and can transmit to the ground the forces exerted by the weight of the body and its movements. This it achieves with the best mechanical advantage under the most varied conditions. The plantar vault acts as a shock-absorber essential for the flexibility of the gait. Any pathological conditions, which exaggerate or flatten its curvatures, interfere seriously with the support of the body on the ground and necessarily with running, walking and the maintenance of the erect posture.
The plantar aponeurosis, which arises from superficial fascia and sometimes from the plantaris muscle (Cailliet 1997, Gray’s 2005), provides a substantial structural component for the plantar vault of the foot. Levangie & Norkin (2001) simplify this concept.
From the beginning to the end of the stance phase of gait, tension on the platar aponeurosis increases…For this reason, the function of the aponeurosis in supporting the arches has been compared to the function of a tie-rod on a truss. The truss and the tie-rod form a triangle; the two struts of the truss form the sides of the triangle and the tie-rod is the bottom. The talus and calcaneus form the posterior strut, and the remaining tarsal and the metatarsals form the anterior strut. The plantar aponeurosis, as the tie-rod, holds together the anterior and posterior struts when the body weight is loaded onto the triangle. This structural design is efficient for the weight-bearing foot because the struts (bones) are subjected to compression forces, whereas the tie-rod (aponeurosis) is subjected to tension forces. Bending moments to the bone that can cause injury are minimized.
The functional anatomy of the foot is commonly described in terms of its longitudinal and transverse arches, which help compose the ‘vault’ (Fig. 14.19). The longitudinal arch (or curve) can be divided into medial and lateral constituents and is accompanied by a transverse curvature.
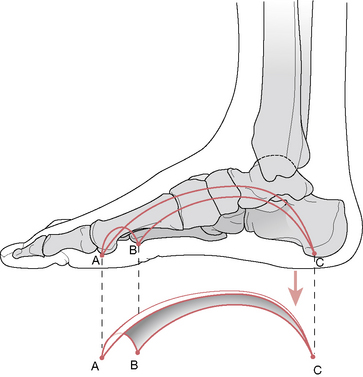
Figure 14.19 The plantar vault from a medial perspective, with its three support points occurring at the calcaneus and the first and fifth metatarsal heads
(reproduced with permission from Kapandji 1987).
The medial longitudinal (‘spring’) arch has bony components (pillars) composed of the calcaneus, talus, navicular, the cuneiforms and the first three metatarsals (Fig. 14.20). This arch is designed to transmit and absorb force. Gray’s anatomy (2005) summarizes:
The bones themselves contribute little to the stability of the arch, whereas the ligaments contribute significantly. The most important ligamentous structure is the plantar aponeurosis, which acts as a tie beam between the supporting pillars. Dorsiflexion, especially of the hallux, draws the two pillars [calcaneous and three metatarsal heads] together, thus heightening the arch.
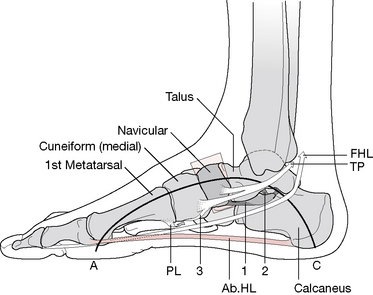
Figure 14.20 The medial longitudinal arch. A: first metatarsal contact; C: calcaneal contact; PL: fibularis (peroneus) longus; TP: tibialis posterior; FHL: flexor hallucis longus; Ab HL: abductor hallucis longus; 1: plantar calcaneonavicular ligament; 2: talocalcanean ligament; 3: tibialis posterior attachment, which blends with plantar ligaments
(reproduced with permission from Kapandji 1987).
The medial longitudinal arch is higher, more mobile and resilient than the lateral and, as it flattens, there is a progressive tightening of the plantar calcaneonavicular ligament and plantar fascia. Active support of the medial arch is primarily supplied by tibialis posterior (the tendon of which has attachments on the navicular, first cuneiform and the bases of the second, third and fourth metatarsals), fibularis (peroneus) longus, flexor hallucis longus, flexor digitorum longus and abductor hallucis.
The lateral longitudinal arch comprises the calcaneus, cuboid and the fourth and fifth metatarsals (Fig. 14.21). This arch is low, has limited mobility and is designed for transmission of force to the walking surface rather than for the absorption of weight and thrust (Gray’s anatomy 2005, Schiowitz 1991). Muscles acting to tighten it include fibularis brevis and longus, and abductor digiti minimi.
The transverse arch is best described as an almost full-length transverse curvature of the tarsals and metatarsals, giving a ‘vaulted’ appearance to the foot. It can be examined at several locations along its length (Fig. 14.22). The flexible anterior aspect includes the metatarsal heads. The fixed metatarsal arch includes the bases of the metatarsals. The fixed posterior aspect includes the cuboid and the cuneiforms, resting on the ground only at the laterally placed cuboid while the neighboring navicular is ‘slung above the ground and overhangs the medial surface of the cuboid’ (Kapandji 1987). The muscular support for the transverse arch includes fibularis longus (which acts on all three components of the arch system), adductor hallucis running transversely and tibialis posterior, which runs (from beneath the medial malleolus) obliquely anterolaterally.
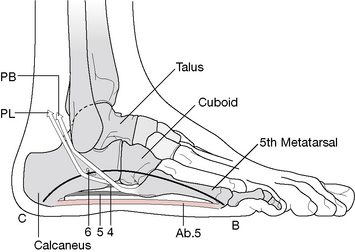
Figure 14.21 The lateral longitudinal arch. B: fifth metatarsal contact; C: calcaneal contact; PL: fibularis (peroneus) longus; PB: fibularis (peroneus) brevis; Ab 5: abductor digiti minimi; 4: long plantar ligament deep; 5: long plantar ligament superficial; 6: peroneal tubercle of calcaneus
(reproduced with permission from Kapandji 1987).
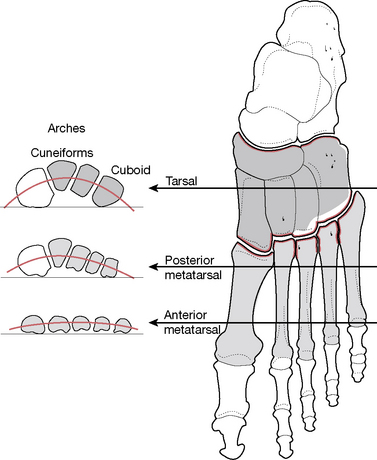
Figure 14.22 The ‘vaulted’ appearance of the foot is in part due to an almost full-length transverse curvature of the tarsals and metatarsals. The degree of transverse arching will vary at different points of the foot, as shown here by considering the metatarsal heads, metatarsal bases and the tarsals
(adapted from Cailliet 1997).
The intrinsic muscles are significant contributors to the muscular support of the arches. Their line of pull lies essentially in the long arch of the foot and perpendicular to the transverse tarsal joints; thus they can exert considerable flexion force on the forefoot and are also the principal stabilizers of the transverse tarsal joint.
Regarding the arches, though there are some shared philosophies, there is little agreement, especially concerning the ‘transverse arch’.
• Schiowitz (1991) suggests that although: ‘many authors describe a number of transverse arches, with the exception of the metatarsal heads, these arches do not transmit force to the ground’.
• Gray’s anatomy (2005), in partial agreement with Schiowitz, states that: ‘Transmission of force occurs at the metatarsal heads, to some degree along the lateral border of the foot, and through subjacent soft tissues.’
• Regarding the anterior metatarsal transverse arch comprising the five metatarsal heads, Greenman (1996) suggests that: ‘The metatarsal arch is not a true arch, but refers to the relation of the heads of the five metatarsals’. He notes that restrictions of the metatarsal heads are usually secondary to dysfunctional patterns involving the other arches of the foot and are likely to be associated with soft tissue changes, especially involving the plantar fascia (see below). Joint play here includes dorsal and plantar glide, as well as rotation (Greenman 1996). If restriction is noted it is commonly between the second and third metatarsals, with associated tenderness in the interosseous musculature.
Gray’s anatomy (1995) observes that:
The human foot, alone among primates, is normally arched in its skeletal basis, usually with visible concavity in the sole. The word ‘arch’ so applied has perhaps become too architectural, imposing rigidity on classical descriptions of curved pedal form and differences of interpretation more linguistic than factual. The word has several meanings and doubtless ‘arches of the foot’ has various implications. As a start, at simplest, the term implies little more than a curved form, concave on the plantar aspect. Such an arch should not be compared with static masonry, with pediments on terra firma and an intermediate keystone structure. The pedal arch is dynamic; muscles and ligaments are functionally inseparable. Moreover, its heel is often off the ground. In this account, therefore, ‘arch’ denotes no more than curved form, just as the back is merely curved when ‘arched’.
It should be borne in mind that the plantar vault, whether considered as a twisted osteoligamentous plate (Gray’s anatomy 2005, Levangie & Norkin 2005) or as an architectural wonder, is an integral component of whole-body health, its influences being felt both locally and throughout the body. The health and integrity of this dynamic system should be a priority component of most therapeutic interventions.
The articular surfaces with adjoining metatarsals allow a little movement between them. Stability is reinforced by numerous ligaments, including the deep transverse metatarsal ligament, which helps prevent excessive movement and splaying (spreading apart) of the metatarsal heads (Levangie & Norkin 2005).
The function of the TMT joints is to continue the movements of the transverse tarsal joint when needed, while retaining ground contact of the forefoot. Levangie & Norkin (2005) note:
As long as the transverse tarsal joint motion is adequate to compensate for the hindfoot position, considerable TMT joint motion is not required. However, when the hindfoot position is at an end point in its available TOM or the transverse tarsal joint is inadequate to provide full compensation, the TMT joints may rotate to provide further adjustment of forefoot position.
As the weight-bearing hindfoot moves in inversion and eversion patterns, the midfoot and forefoot move in the opposite direction to counterrotate the forefoot, in order to maintain plantar contact. This compensation usually occurs first in the transverse tarsal joint and, if necessary, further compensation occurs at the TMT joints, including varying dorsiflexion and plantarflexion of the rays of the foot. For example, if the calcaneus inverts (supinates), the forefoot must produce relative pronation in order to maintain contact with the ground, otherwise the medial aspect would lift from the ground and create instability. Most of the forefoot pronation will occur at the transverse tarsal joint but, if calcaneal movement is extreme, then tarsometatarsal joints must also compensate, which may include dorsi- and plantarflexion as well as rotational movements of the rays about the second toe, commonly referred to as a supination twist (Levangie & Norkin 2005). This rotation about the second ray (longitudinal axis) will increase or decrease the curvature of the anterior arch (Kapandji 1987). The configuration of the forefoot will vary depending upon the surface to which the foot is adjusting.
The arches of the foot
The midfoot region of the foot is usually associated with the arch system. Although the plantar vault truly span over almost the full length of the foot, dysfunction of the medial longitudinal arch is usually most visible in the midfoot region. The plantar vault, with its longitudinal and transverse arches, is more fully discussed in Box 14.6.
Common disorders of the midfoot
Pes planus (flat foot)
If the medial longitudinal arch is lost this is known as pes planus or flat footed, and can be either flexible or rigid. Flexible flat foot, which is marked by the reappearance of the arch when the foot is non-weight-bearing, may be correctable, whereas rigid flat foot does not usually respond to manual therapies or exercise. Mechanically, collapse of this arch may occur because of hyperpronation or from increased eversion of the subtalar joint. This leads to the calcaneus lying in valgus and external rotation relative to the talus. It is most noticeable in the midfoot region where associated sagging or medial excursion of the midfoot occurs when the talus moves anteriorly, medially and inferiorly, the navicular slides inferiorly, and the calcaneus pronates (Levangie & Norkin 2005).
The incidence of pes planus is approximately 20% in adults, the majority of which are flexible. Flat feet are not necessarily uncomfortable, as long as there is no heel cord contracture, but flat feet associated with heel cord contracture may limit function and lead to discomfort when walking. Heel cord contracture is associated with lateral deviation of Achilles when weight bearing (Staheli et al 1987).
Evidence suggests that flat feet protect against metatarsal stress fractures but the feet offer poor shock absorption with regard to the lower back, leading to a higher incidence of low back pain. In contrast, a pes cavus foot (high arch) may actually be somewhat protective of stress-related low back pain (Ogon 1999). Although associated foot dysfunction (hammer toe, claw toe) may result, the consequences of pes cavus are not usually as far-reaching as pes planus.
It is important to distinguish between flexible flat foot and rigid (or spastic) flat foot. Surgical intervention is only called for if there is a rigid flat foot (seldom in flexible flat foot) and only when pain, deformity (midfoot breakdown) or severe contracture are factors. A small number of flexible flat feet do not correct with growth and eventually become rigid due to adaptive changes (Lau & Daniels 1998).
Conservative treatment
Wenger et al (1989) suggest that, since flexible flat foot is generally a benign condition, it rarely requires treatment. If there are problems associated with heel cord shortening, stretching should be the main treatment. It is important when stretching to ensure that the foot is supinated in order to avoid worsening midfoot collapse.
Wenger et al suggest that in most cases orthotics do not change osseous relationships and are ineffective. They go further and indicate that arch supports may actually make the patient’s symptoms worse, unless and until heel cord shortening is relieved.
It is also suggested that in some cases, patients with a calcaneovalgus deformity can normalize their weight-bearing pattern by using a medial heel wedge. This should be distinguished from calcaneovalgus dysfunction for which a heel wedge could be detrimental.
The forefoot
The metatarsophalangeal (MTP) joints and the interphalangeal (IP) joints of the foot are identical to those found in the hand (Kapandji 1987), descriptions of which can be found in Volume 1 of this text. Each MTP joint is composed of a convex metatarsal head articulating with a shallow phalangeal ‘socket’ that allows for flexion, (considerably more) extension and some abduction and adduction.
The metatarsal length has an unusual arrangement, with the 2nd metatarsal being longest, followed by the 3rd, 1st, 4th and 5th. However, due to their arrangement at the proximal end (e.g, 2nd metatarsal being recessed between the cuneiforms), the proximal joints lie on an oblique axis. As a group, the MTP joints allow a hinge-type motion of the foot across this oblique line (termed the metatarsal break) as the heel is raised from the supporting surface by active contraction of the plantarflexors. As these muscles contract, they contribute to supination, which creates a locking of the hindfoot and midfoot. The resulting rigid lever rotates around the oblique metatarsal break (MTP axis) (Fig. 14.23) as the toes are stabilized against the supporting surface. Lavengie & Norkin (2005) explain:
The obliquity of the axis for the metatarsal break allows weight to be distributed across the metatarsal heads and toes more evenly that would occur if the axis were truly coronal. If the body weight passed forward through the foot and the metatarsal break occurred around a coronal MTP axis, an excessive amount of weight would be placed on the first and second metatarsal heads. These two toes would also require a disproportionately large extension range. The obliquity of the axis of the metatarsal break shifts the weight laterally, minimizing the large load on the first two digits.

Figure 14.23 The toes are stabilized against the supporting surface as the resulting rigid lever rotates around the oblique metatarsal break (MTP axis)
(adapted from Levangie & Norkin 2001).
The phalanges are hinge joints and are limited to flexion and extension, with flexion being considerable and extension being limited. These movements are accompanied by slight associated rotation (see Box 14.11 for toe movements).
Box 14.11 Movements of the toes
The tendinous arrangement of the toes is similar to that of the hand as are the digital joints. Like the hand, the tendon of the extensor digitorum longus (EDL) forms a dorsal aponeurosis into which the extensor digitorum brevis, the lumbricals and (sometimes) the interossei merge. The primary functional difference between these associated foot and hand structures is that flexion exceeds extension in metacarpophalangeal joints whereas extension exceeds flexion in the metatarsophalangeal (MTP) joints. In the foot, this difference is extremely important in the final phase of gait when dorsiflexion (extension) of the MTP joints reaches or exceeds 90° (Kapandji 1987). A closer examination of the tendinous arrangement of the toe muscles as well as the mechanics of their movement may assist in understanding the development of dysfunctional deformities, such as hammer toes, claw toes and mallet toes.
The following pertains to the lesser toes, which have a higher occurrence of flexion deformity than the great toe, which only has two phalanges instead of three.
• The lumbricals (L) attach to the base of the proximal phalanx and also merge into the tendon of the EDL on the dorsal surface of the toes. The interossei (Ix) may have a similar attachment into the dorsal aponeurosis of EDL but anatomical variations exist. When EDL is relaxed, contraction of lumbricals and interossei (if they indeed insert into the tendon complex) produces plantarflexion of the MTP joints (Fig. 14.54).
• On the plantar surface, the flexor digitorum brevis (FDB) splits near its distal attachment at the middle phalanx, forming a tunnel through which the flexor digitorum longus (FDL) courses to attach to the distal phalanx. When FDB and FDL simultaneously contract, they plantarflex the interproximal and distal interphalangeal joints, respectively (Fig. 14.55). Assistance from the interossei and lumbricals will result in plantarflexion of all the toe joints, causing a plantarward curling of the toes.
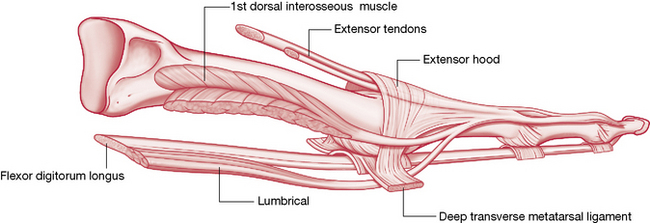
Figure 14.54 Lumbrical and interossei produce plantarflexion of the metatarsophalangeal joints
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
• On the dorsal aspect, extensor digitorum brevis (EDB) merges into the tendons of EDL and serves to extend all three phalanges of the lesser toes except the fifth, which is usually extended by EDL only.
• The tendon complex of EDL forms an elaborate dorsal aponeurosis into which the EDB, the lumbricals and (sometimes) the interossei merge. As mentioned previously, when EDL is relaxed and the flexors contract, the lumbricals and interossei can assist plantarflexion of the MTP joints. However, when EDL contracts and the flexors relax, the lumbricals and (sometimes) interossei will assist extension (dorsiflexion) of the MTP joints instead (Fig. 14.56).
These muscles work together to press the toes into the ground when weight is borne onto the ball of the foot to stabilize the forefoot and to provide rigidity to the toes, while also allowing the forefoot rocker to function. Like so many foot muscles, these muscles adjust the foot to instantaneously changing terrain, ‘grabbing’ the ground as necessary to provide balance to the gait foot. When substitution and muscular imbalance occur, resulting digital contracture can produce deformities of toe position. A common result is the development of hammer toe (Fig. 14.57), which is a fixed-flexion deformity of the interphalangeal joint in which capsules and tendons of the toe shorten and calluses develop in areas that bear excessive pressure or that rub on the shoe. Claw toe or mallet toe can develop in a similar manner, the evolution of which simply depends upon which joints are held in flexion or extension.
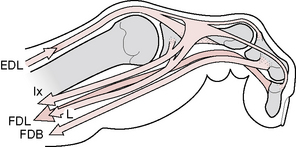
Figure 14.55 Curling of the toes into full plantarflexion relies on long and short toe flexors
(reproduced with permission from Kapandji 1987).
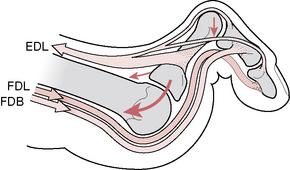
Figure 14.56 Dysfunctional muscular imbalances can produce ‘claw toe’ positioning
(reproduced with permission from Kapandji 1987).
In any of these positional deformities of the toes, evaluation of the toe joints, hypertonicity of musculature, trigger points in these muscles, as well as those whose target zones include these muscles, gait patterning, static postural alignment and the shoes that the patient wears will provide clues as to the possible cause as well as assist in formulating a treatment plan. Treatment might include the manual techniques described within this text, orthoses that assist in correction of structural problems and, when the condition is disabling or severe, surgical correction.
The toes, though capable of grasping, are primarily used to create a smooth transition of weight to the other foot during gait and, during standing, to help maintain pressure against the ground (Levangie & Norkin 2005). While the structure of the toes is very similar to that of the fingers, their functional design is geared more toward the tasks of weight-bearing and gait, rather than grasping.
Sesamoid bones of the lower extremity
Non-articular sesamoid bones or cartilages are frequently found in the lower limb (Gray’s anatomy 2005) and bursal arrangements may also occur at such sites. Those muscles in the lower limb in which these minute bones are commonly found include:
• flexor hallucis brevis (directly beneath the first metatarsal head)
• fibularis (peroneus) longus at the cuboid bone
• tibialis anterior at the medial cuneiform bone
• the tendon of tibialis posterior on the medial side of the talar head
• lateral part of gastrocnemius posterior to the lateral femoral condyle
• tendon of psoas major at its ilial contact