Chapter 13 The knee
The knee, the intermediate joint of the lower limb, is formed by two joints, the knee joint (often referred to as femorotibial or tibiofemoral joint) and the patellofemoral, with the first being the weight-bearing component and the second serving to reduce friction of the quadriceps tendon on the femoral condyles and acting as an ‘anatomic pulley for the quadriceps muscle’ (Levangie & Norkin 2005). Kapandji (1987) expresses the paradoxical ‘mutually exclusive’ requirements of the knee joint as having to provide ‘great stability in complete extension, when the knee is subjected to severe stresses resulting from body weight and the length of the lever arms involved’ as well as great mobility, essential when running or gait on uneven ground, which is achieved only with a certain degree of flexion. ‘The knee resolves this problem by highly ingenious mechanical devices but the poor degree of interlocking of the surfaces – essential for great mobility – renders it liable to sprains and dislocations.’
The knee is not well protected by fat or muscle mass, making it relatively susceptible to trauma. Additionally, it is often subjected to maximal stress (being located at the intersection of two long levers) and is ‘probably the most vulnerable of all structures of the body to soft tissue injury with attendant pain and impairment’ (Cailliet 1996). The knee is unstable during flexion, making its ligaments and menisci most susceptible to injury; however, fractures of the articular surfaces and ruptures of the ligaments are more likely during extension injuries (Kapandji 1987). Due to its easily palpable contours and features, coupled with potential use of arthroscopic examination, if needed, the diagnostic process for the knee is fortunately far easier than for many other joints of the body (Hoppenfeld 1976).
In writing this chapter, we have included many quotes from the skilled writings of Pamela Levangie and Cynthia Norkin (2005) (and their contributing authors), who have described this complex joint and its complicated movements in their book, Joint structure and function: a comprehensive analysis. Their dedication to clarity and accuracy of information is particularly obvious in such a difficult subject as the knee joint.
The knee joint is discussed first in this chapter, with the patellofemoral joint, whose function is distinctly different, following it. The discussions in this chapter start from the inside with the bony surfaces and then progress outwardly, through the menisci, ligaments, joint capsule and, finally, the muscular elements. The proximal tibiofibular joint, which relates functionally to the ankle joint (Levangie & Norkin 2005), is not enclosed within the joint capsule of the knee and is therefore not discussed in this chapter. Details regarding the tibiofibular joints are to be found in Chapter 14 with the ankle and foot complex.
Regarding terminology of the region of the knee, the common use of both tibiofemoral joint and femorotibial joint appears in textbooks as well as journal articles. Gray’s anatomy (2005) uses only tibiofemoral joint, however, Gray’s Anatomy for Students (Drake et al 2010) does not. Terminologia anatomica (FCAT 1998), an international standard on human anatomical terminology developed by the Federative Committee on Anatomical Terminology (FCAT) and the International Federation of Associations of Anatomists (IFAA), suggests that the appropriate name is the knee joint. We have adopted that term throughout this chapter except in direct quotes from other authors, which show terms used by them.
The knee joint
The knee joint, the largest and most complicated joint in the body, is a special type of hinge joint. While hinge joints normally allow one degree of movement, this trochoginglymus joint allows flexion/extension of the joint, produced by a combination of rolling and gliding, and, when in a flexed position, also allows a small degree of rotation (Platzer 2004). Because it must perform its movement while also bearing most of the body’s weight (at times well over five-sixths of the entire weight of the body), it seems as though stability of this joint should be a primary feature when, in fact, the joint design itself engenders relative instability. The following summations by no means explain the detailed architecture of the knee joint but they are intended to give a simplistic yet encompassing view of the knee on which basic assessment skills may be built. Readers interested in a deeper understanding of the mechanics of this joint (and others) are referred to Volume 2 of three volumes titled The physiology of the joints, which were beautifully mastered and illustrated by I. A. Kapandji.
Regarding the relationship of the femur and tibia, Gray’s anatomy (2005) notes:
In standing, the femoral shafts converge downwards and medially to the knees and almost touch: they lie below the hip joints. Since the tibia and fibula descend vertically from the knees, the ankles are also in the line of body weight in standing or walking. Femoral obliquity varies, but is greater in women, reflecting the relatively greater pelvic breadth and shorter femora.
It is interesting that despite this obliquity, in the normal knee, body weight is evenly distributed onto the medial and lateral femoral condyles. Abnormal femoral positioning, resulting in valgus or varus positions of the knee, can significantly alter this weight distribution as well as affect foot position and the mechanics of both the knee and foot.
The incongruence of the convex femoral condyles and the concave tibial condyles is significant, so much so that interposed menisci are needed to achieve a degree of stability. However, it is the ligamentous and muscular components – not joint congruency – that primarily support this joint (Cailliet 1996). Because an understanding of the bony and cartilaginous features is complicated, yet essential, they are deserving of detailed discussion.
The femur
The femur is the longest and strongest bone in the human body, its strength evident by its weight and its power obvious by its muscular forces (Gray’s anatomy 2005). It is composed of:
• a head at the proximal end – projected by its short neck to meet the acetabulum (see Chapter 12)
• a shaft that is almost cylindrical. It displays three surfaces (anterior, lateral and medial) and their associated borders, bows forward and has a degree of torsion around its vertical anatomical axis. This anatomical axis courses downward and medially at an oblique angle to meet the vertically oriented tibia, providing the knee joint with a normal valgus angle of 5–10°
• double condyles on the distal end are separated by an intracondylar notch or fossa, with the medial condyle extending further distally as well as being longer than the lateral condyle.
Because weight-bearing forces follow a mechanical rather than anatomical axis, the angulation of the femur assists in placing the femoral condyles under the head of the femur so that, in a normally positioned leg, the weight-bearing line passes through the center of the knee joint (between the condylar tubercles) and then through the center of the talus. Levangie & Norkin (2005) note:
This line represents the mechanical axis, or weightbearing line, of the lower extremity, and in a normally aligned knee, it will pass through the center of the joint between the intercondular tubercles. The weight-bearing line can be used as a simplification of the ground reaction force as it travels up the lower extremity. In bilateral stance, the weight-bearing stresses on the knee joint are, therefore, equally distributed between the medial and alteral condyles (or medial and alteral compartments).
They note, however, that in unilateral stance or once dynamic forces are introduced to the joint, deviation in normal force distribution may occur.
• an anterior surface that is smooth and gently convex
• a lateral surface, which has as a posterior boundary the linea aspera, that displays itself as a crest with lateral and medial edges, diverging proximally (to form the gluteal tuberosity) and distally toward the condyles, to form the medial and lateral supracondylar lines
• a medial surface, which has the linea aspera as its posterior border.
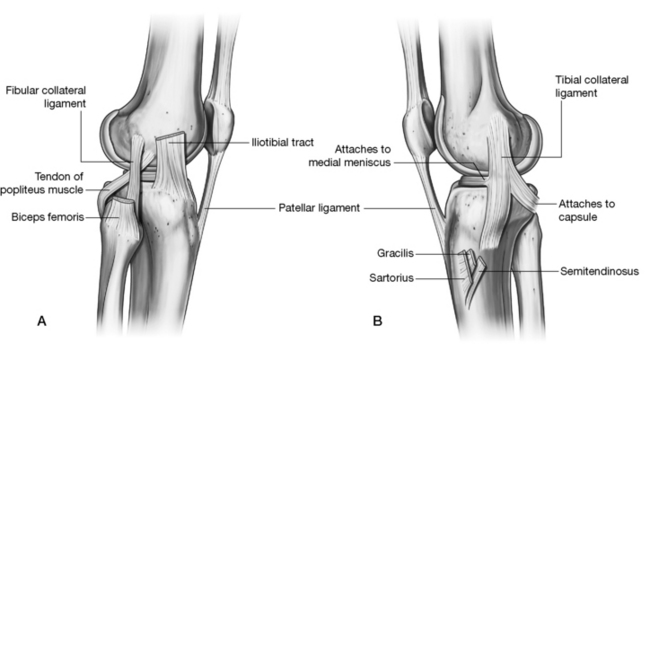
• The femoral shaft lies within a muscular envelope. The following attachments are shown in Figure 13.1.
• Vastus intermedius (VI) attaches anteriorly and laterally on its upper three quarters.
• Articularis genus attaches on the anterior surface just distal to the end of the VI.
• The most distal anterior surface is covered by a suprapatellar bursa.
• The medial surface, devoid of attachments, is covered by vastus medialis.
• At the proximal anterior surface can be seen a small attachment of vastus lateralis and vastus medialis.
• At the greater trochanter the gluteus minimus and medius, piriformis and the remaining deep hip rotators attach.
• At the lesser trochanter, the iliopsoas is the only attachment, with iliacus extending down the shaft a short distance.
• Gluteus maximus attaches posteriorly to the gluteal tuberosity, which is continuous with
• the linea aspera, which provides attachments for the adductor group, vastus medialis, vastus lateralis and short head of biceps femoris as well as the intermuscular septa.
• Distally, on the posterior and lateral aspects of the femur, the gastrocnemius, plantaris and popliteus attach as well as the adductor magnus, which attaches to the adductor tubercle.
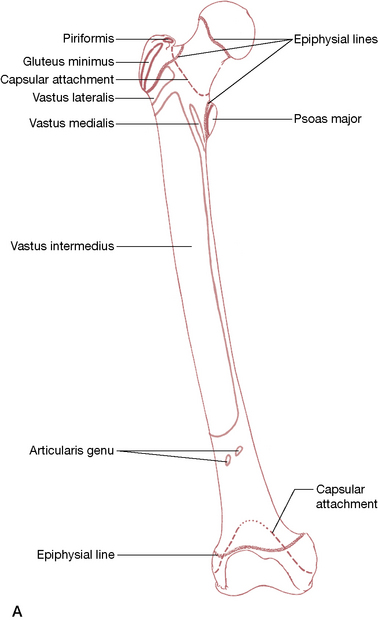
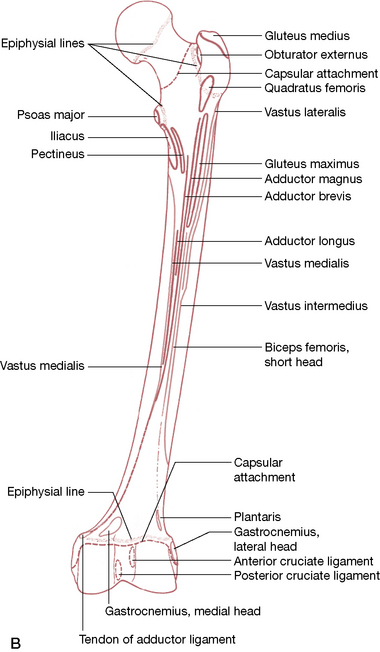
Figure 13.1 A: Anterior aspect of the right femur with lines showing the muscular attachments. B: Posterior aspect of the right femur with lines showing the muscular attachments.
Both A and B are reproduced with permission from Gray’s anatomy 1995.
Femoral condyles
The distal end of the femur is constructed for the transmission of weight to the tibia (Fig. 13.2), with two formidable condyles. These condyles are convex in both a frontal and sagittal plane and are bordered through their length by a saddle-shaped groove, which unites them anteriorly (as the patellar groove or surface) and which separates them posteriorly (as the intercondylar notch or fossa). Anteriorly, these condyles merge with the shaft, united by, and continuous with, the patellar surface (as described with the patellofemoral joint on p. 462). They do not articulate with the proximal end of the fibula (Fig. 13.3), which articulates only with the lateral proximal tibia.
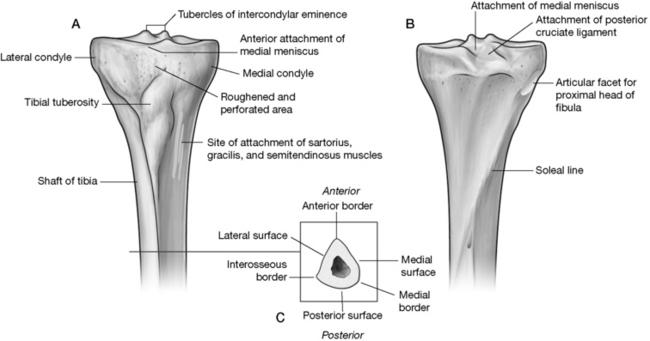
Figure 13.2 The proximal tibia. A: Anterior view; B: Posterior view; C: Crossection
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
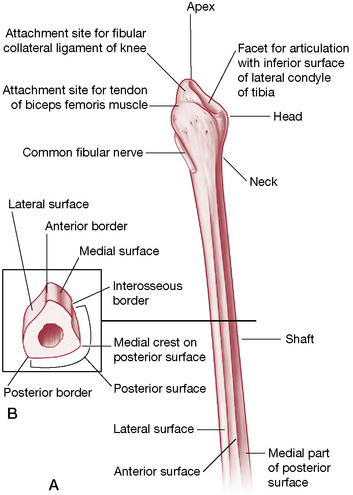
Figure 13.3 The proximal fibula. Note facet that articulates with the lateral tibia.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
The medial and lateral femoral condyles, which diverge distally and posteriorly, can be compared. They offer the following features (Platzer 2004) (Figs 13.4A, 13.5, 13.6). Both femoral condyles are covered with articular cartilage.
• The medial condyle is uniform in width while the lateral condyle is narrower in the back than in the front.
• The medial condyle extends more distally, which counters the oblique position of the femoral shaft, placing the condyles ‘in the same horizontal plane despite their different sizes’ (Platzer 2004).
• The two condyles are almost equally (and only slightly) curved in a transverse plane about the sagittal axis.
• In the sagittal plane, the curvature increases posteriorly, resulting in a decreased radius posteriorly, placing the mid-points of the curve on a spiral line and resulting in ‘not one but innumerable transverse axes, which permits the typical flexion of the knee joint that consists of sliding and rolling motion’ (Platzer 2004).
• An additional vertical curvature on the medial condyle (as seen from below) allows for a rotational feature during flexion.
• The articulating surface of the lateral femoral condyle (excluding the patellar surface) is shorter than the articular surface of the medial femoral condyle.
• Proximal to the medial condyle lies the medial epicondyle, which receives the tibial (medial) collateral ligament and, on its upper edge, the adductor magnus attaches to its adductor tubercle.
• The fibular (lateral) collateral ligament attaches to the lateral epicondyle (above the lateral condyle) and the lateral head of gastrocnemius attaches posterosuperior to this.
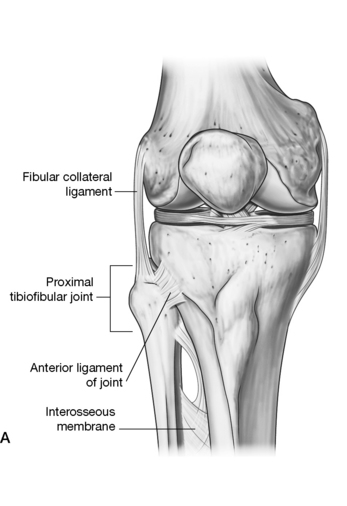
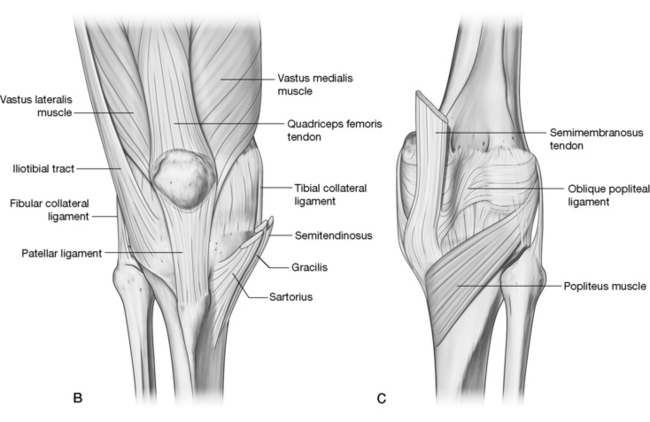
Figure 13.4 A: The knee joint is a highly incongruent joint that has a complex ligamentous system that affords stability to this moderately unstable joint. B/C: The muscles and ligaments, along with the patella and menisci, work together as vastly complex mechanisms that provide stability as one rises, steps and even runs on this unstable surface. (All are reproduced with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
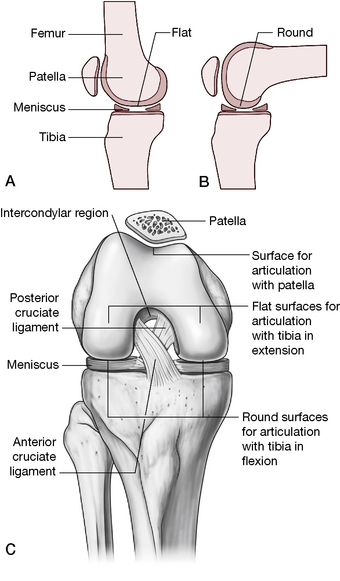
Figure 13.5 A: The flat surface of the femur rests on the menisci during extension. B: During flexion, the femoral condyles roll and slide until the round posterior aspect rests on the tibia. C: With the anterior knee flexed, the cruciate ligaments are partially visible.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Intercondylar fossa
The two condyles are separated distally by the intercondylar fossa, a significant groove lying between the two condyles. This fossa is limited anteriorly by the distal border of the patellar surface and posteriorly by the intercondylar line, which separates it from the popliteal surface of the femur. The capsular ligament, oblique popliteal ligament and the infrapatellar synovial fold all attach to the intercondylar line on the posterior femur. The intercondylar fossa lies within the joint capsule but due to the arrangement of the synovial membrane, is largely extrasynovial and extraarticular, as are the cruciate ligaments, which lie in this region (see ligamentous discussion following this section).
• On the medial surface of the lateral condyle, which makes up the lateral wall of the fossa, is the smooth proximal attachment site for the anterior cruciate ligament.
• On the lateral surface of the medial condyle, which makes up the fossa’s medial wall, is the smooth proximal attachment site for the posterior cruciate ligament.
• The popliteal surface of the femur is a triangular surface delimited by the medial and lateral supracondylar lines and, distally, by the intercondylar line (upper edge of intercondylar fossa).
Regarding the popliteal region:
• the medial head of gastrocnemius attaches a little above the medial condyle
• various arteries lie close by, including the popliteal artery, which arches above the condyle as it branches from the superior medial genicular artery
• plantaris attaches to the distal part of the lateral supracondylar line, separating the lateral genicular artery from bone
• the medial supracondylar line provides the attachment for vastus medialis and the tendon of adductor magnus. The line is crossed by femoral vessels, which enter the popliteal fossa from the adductor canal
• this triangular area is the upper half of the diamond-shaped ‘popliteal fossa’, a region that requires caution during palpation due to the course of relatively exposed neurovascular structures
The proximal tibia
The vertically oriented tibia (Fig. 13.2) lies medial to, and is stronger than, the accompanying fibula. (Fig. 13.3) The tibia’s proximal end, the tibial plateau, provides a surface for articulation with the femur, thereby allowing transmission of the body’s weight as well as ground reaction forces (13.4A). When both forces are transmitted strongly, as in jumping from an elevated position, the knee joint and its internal elements are at increased risk for injury. Additionally, when the angulation of the femur and tibia is other than normal (genu valgum, genu varum), significant changes take place in the weight-bearing pressures on the menisci and cartilage (see Box 13.1).
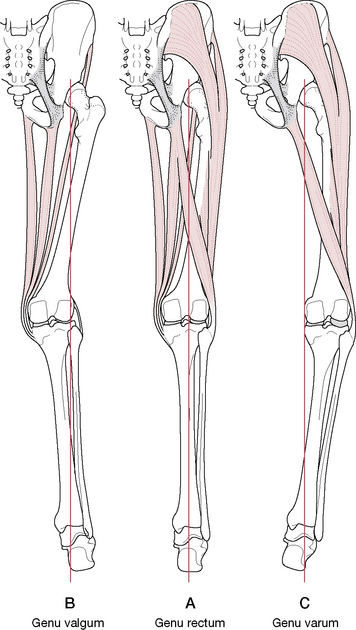
Figure 13.7 Normal alignment of lower limb is middle figure. A: Genu rectum. B: Genu valgum. C: Genu varum. Vertical line indicates weight-bearing line
(adapted from Platzer 2004).
Box 13.1 Weight-bearing forces and knee joint alignment (Platzer 2004)
The mechanical axis of the lower limb lies on a straight line drawn through the center of three joints: the hip, the knee and the ankle (Fig. 13.7A). This mechanical axis coincides with the anatomical axis of the tibia, but the anatomical axis of the femur is diagonally inclined, which forms a 6° acute angle with the mechanical axis and gives the knee joint a normally slightly valgus position.
In genu valgum (knock knees), the weight-bearing line is displaced laterally and courses through the lateral femoral condyle and head of the fibula, overstretching the medial collateral ligament and placing excessive stress on the lateral meniscus and the cartilaginous joint surfaces of the lateral tibial and fibular condyles (Fig. 13.7B).
In genu varus (bow legs), the weight-bearing line is displaced medially and courses through the medial femoral condyle or medial to it, overstretching the lateral collateral ligament and placing excessive stress on the medial meniscus and the cartilaginous joint surfaces of the medial tibial and fibular condyles (Fig. 13.7C).
A high degree of incongruity exists between the convex femoral condyles and the concave surfaces of the tibial condyles, requiring accessory joint structures to be interposed to provide stability while retaining mobility. This is accomplished to some degree by the menisci (described with the tibial plateaus below) and substantially supported by the cruciate and collateral ligaments of the knee. These elements are designed to provide stable movement in flexion and extension, with a degree of rotation. However, they are at increased risk of injury, particularly when the weight-bearing, fully extended knee is placed under a shearing or rotational force (as when the body rotates above it on the extended knee, planted foot) or when the knee joint is forcefully taken through an adduction or abduction movement (as when impacted from the side during sporting events).
Below the articular surface of the tibia, ledges project outwardly both medially and laterally, the latter offering a facet that is directed distolaterally to receive the head of the fibula. Anteriorly, near the proximal end of tibia, is the tibial tuberosity, being the truncated apex of a triangular area that lies distal to the anterior aspect of the condylar surfaces. It has a smooth upper portion (over which the patellar ligament lies) and a rough distal region (where the patellar ligament attaches).
Tibial plateaus (superior articular facets) (Figs 13.8, 13.9)
The proximal articular surface of the tibia is composed of two massive condyles and an intercondylar eminence, the latter featuring the medial and lateral intercondylar tubercles.
• During knee flexion the intercondylar eminence slides in the intercondylar groove of the femur as well as becoming a fulcrum around which rotation can take place when the knee is flexed. The complexity of these concepts is well illustrated and described by Kapandji (1987) as a mechanical model.
• At full extension, the eminence becomes lodged in the intercondylar notch of the femur and the tibia then rotates about it in the final stage of extension (Levangie & Norkin 2005). This ‘screw home’ locking mechanism results in an automatic (terminal) rotation of the knee joint that brings the joint into a close-packed position and ‘locks’ it in extension. It must then be ‘unlocked’ before flexion can occur or else damage may result.
• In front of the intercondylar eminence lies the anterior intercondylar area to which the anterior cruciate ligament attaches and, anterior to this, the anterior horn of the medial meniscus attaches. The anterior horn of the lateral meniscus attaches lateral to the anterior cruciate ligament (see Fig. 13.9).
• Behind the eminence lies the attachment of the posterior cruciate ligament in the posterior intercondylar area. Between the attachments of the two cruciate ligaments lie the attachments of the posterior horns of both menisci (see Fig. 13.9).
• The articulating surface of the lateral condyle is half the size of that of the medial condyle and its articular cartilage is one-third as thick as that of the medial condyle.
• The articular surfaces of the tibial plateau are concave centrally but flatten peripherally. The menisci rest, one on each condyle, on the flattened portion of the surface and increase the concavity of each tibial condyle (Gray’s anatomy 2005) (see description of the menisci below).
• From a frontal perspective, both tibial condyles are concave yet shallow; however, the two condyles differ in anteroposterior profile. The medial condyle is concave while the lateral condyle is convex, adding to the instability of the joint, as the lateral femoral condyle must ride up and over this slope during joint movements (Fig. 13.10).
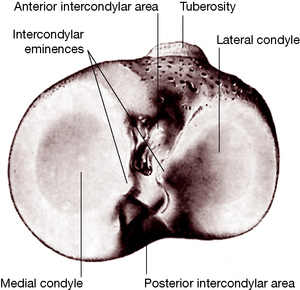
Figure 13.8 The proximal articular surface of the right tibia
(reproduced with permission from Gray’s anatomy 1995).
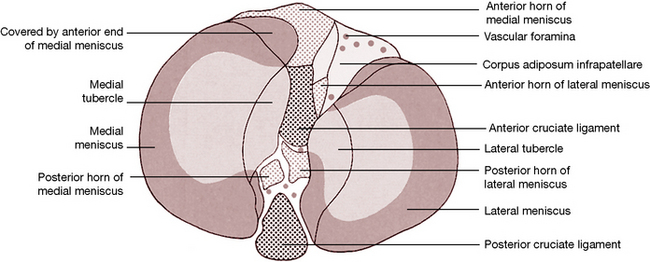
Figure 13.9 Surface features of the proximal aspect of the right tibia
(reproduced with permission from Gray’s anatomy 1995).
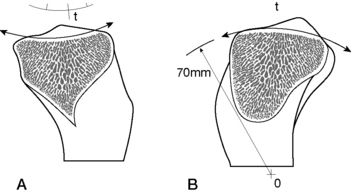
Figure 13.10 A: Section of the medial condyle shows its concavity superiorly. B: Section of the lateral condyle shows its convexity superiorly
(reproduced with permission from Kapandji 1987).
Kapandji (1987) notes:
Therefore, while the medial condyle is biconcave superiorly, the lateral condyle is concave in the frontal plane and convex in the sagittal plane (as seen in the fresh specimen). As a result, the medial femoral condyle is relatively stable inside the concave medial tibial condyle, while the lateral femoral condyle is unstable as it rides on the convex surface of the lateral tibial condyle. Its stability during movements depends on the integrity of the anterior cruciate ligament.
The anterior and posterior cruciate ligaments are discussed further below.
Menisci (Fig. 13.11)
Due to the high degree of incongruence in the knee joint, accessory joint structures are necessary to enhance stability while still allowing mobility within the joint. The semilunar cartilages, or menisci (moon shaped), create a deepened hollowed surface that covers approximately two-thirds of the tibial articulating surface. They not only increase congruence of the articular surfaces, they also serve as shock absorbers, distribute weight-bearing forces and assist in reducing friction during joint movement. There are structural differences between the two menisci (medial and lateral), which, therefore, result in functional diversity. Additionally, the medial two-thirds of each meniscus and its peripheral aspects are different, warranting a discussion of the structure of individual menisci, before a comparison of the two.
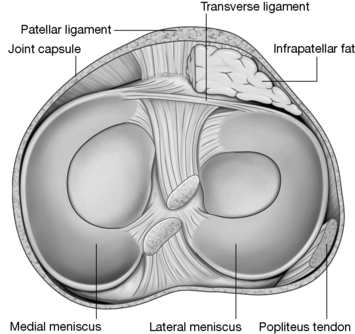
Figure 13.11 Superior aspect of the right tibia showing the menisci and the tibial attachments of the cruciate ligaments.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Each meniscus is an incomplete ring-shaped structure composed of connective tissue with extensive collagen components. Though similar to a disc (which is complete through its center), a meniscus is open centrally. In this case, the meniscus is an incomplete ring, with its two ends firmly attached in the intercondylar region, resulting in each being open toward the center of the knee. Each crescent-shaped structure displays an anterior and posterior horn with the ends of the lateral meniscus attaching near each other to form almost a complete circle (O-shaped) while the medial meniscus, by having its ends attached further apart, is more similar to a half-moon (C-shaped).
Each meniscus is thicker at its outer margin, giving it a wedged shape that tapers toward the center and provides concavity to its tibial condyle. Its blood supply uniquely enters the periphery of the meniscus through a tortuous route to amply supply:
• the entire meniscus in the infant
• only the outer third of the meniscus, while the middle and inner thirds remain avascular, in the adult
Levangie & Norkin (2005) comment on the effects of this decreasing blood supply.
The process of fluid diffusion to support nutrition requires intermittent loading of the meniscus by either weight-bearing or muscular contractions. Subsequently, during prolonged periods of immobilization or conditions of non-weight-bearing, the meniscus may not receive appropriate nutrition. The avascular nature of the central portion of the meniscus reduces the potential for healing after an injury. In adults, only the peripheral vascularized region of the meniscal body is capable of inflammation, repair, and remodeling following a tearing injury.
The nerve supply to the menisci is substantial; free nerve endings supply nociceptive information while mechanoreception is offered by Ruffini corpuscles, Pacinian corpuscles and Golgi tendon organs (Levangie & Norkin 2005), indicating that the menisci are a source of information about joint position, direction of movement and velocity of movement as well as information about tissue deformation.
Dysfunctional joint mechanics, ligamentous injuries and arthritic changes, as examples, can severely disrupt the proprioceptive function of the knees (Koralewicz & Engh 2000) (see Box 13.6).
Box 13.6 Proprioception and the arthritic knee
Koralewicz & Engh (2000) compared proprioception in arthritic and age-matched normal knees. They note that proprioception: ‘the ability to sense joint position and joint motion – is affected by factors such as age, muscle fatigue, and osteoarthritis’. The purpose of their study was to determine whether there was a difference in proprioception between arthritic knees and nonarthritic, age-matched, normal knees. Additionally they sought to evaluate whether, when proprioception is reduced in an arthritic knee, it also was reduced in the opposite knee irrespective of the presence of arthritis. One hundred and seventeen patients who were scheduled for total knee arthroplasty due to severe arthritis (mean age 67.9 years) were compared with a control group of 40 patients who were recruited from a hospital-based cardiac rehabilitation program and did not have knee arthritis (mean age 68.3 years).
• middle-aged and elderly persons with advanced knee arthritis were significantly less sensitive to the detection of passive motion of the knee than middle-aged and elderly persons without knee arthritis.
• the ability to detect passive motion was reduced in both knees when arthritis was present in only one knee.
The researchers raise the question as to whether the loss of proprioception is a precursor, and possibly a contributor, to the development of the arthritic changes in the knee. Such loss of proprioception is independent of the severity of knee arthritis and may foretell the development of arthritis.
The collagen fibers of each meniscus are arranged in two directions.
• The medial two-thirds comprise radially organized collagen bundles, lined by thinner collagen bundles parallel to the surface. This suggests a biomechanical compression coping function.
• The peripheral third comprises larger circumferentially arranged bundles, suggesting biomechanical tension coping functions.
• The peripheral circumferential fibers are strongly anchored to the intercondylar bone, preventing outward displacement of the menisci.
The wedge-shaped menisci each provide three surfaces: the superior surface (1) which articulates with the femur, the peripheral surface (2) with its overall cylindrical shape, which is in contact with and adherent to the deep surface of the joint capsule, and the inferior surface, which rests on the tibial condyle (Fig. 13.12).
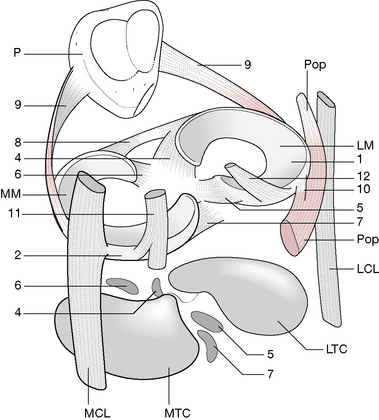
Figure 13.12 The menisci have been lifted off the tibial condyles and the femoral condyles removed to illustrate the intrajoint elements
(reproduced with permission from Kapandji 1987).
Kapandji (1987) describes the attachments of the menisci and notes that the meniscal attachments between the femoral and tibial surfaces are important from the functional point of view.
• They attach to the deep surface of the capsule; the medial meniscus firmly attaches while the lateral meniscus has very loose connections.
• Each horn anchors to the tibial condyle in the anterior and posterior intercondylar fossae, respectively.
• Lateral meniscus: the anterior horn (4) attaches just in front of the lateral intercondylar tubercle while the posterior horn (5) attaches just posterior to the same tubercle.
• Medial meniscus: the anterior horn (6) inserts in the anteromedial angle of the anterior intercondylar fossa while the posterior horn (7) attaches in the posteromedial angle of the posterior intercondylar fossa.
• The transverse ligament of the knee (8) links the two anterior horns and (rarely) may attach to the tibial plateau (de Abreu et al 2007). It is found in approximately 73.5% of knee joints (de Abreu et al 2007), being absent in the remainder (de Abreu et al 2007, Gray’s anatomy 2005, Platzer 2004).
• The meniscopatellar fibers (9) run from the lateral edges of the patella (P) to the lateral borders of each meniscus.
• The medial (tibial) collateral ligament (MCL) is attached to the internal border of the medial meniscus.
• The lateral (fibular) collateral ligament (LCL) is separated from its corresponding meniscus by the tendon of the popliteus (Pop), which itself attaches (10) to the posterior border of the lateral meniscus (LM).
• The semimembranosus tendon (11) attaches by fibrous expansion to the posterior edge of the medial meniscus (MM).
• The menisco-femoral ligament (fibers from the posterior cruciate ligament) are inserted into the posterior horn of the lateral meniscus (12). A few fibers of the anterior cruciate ligament insert into the anterior horn of the medial meniscus as well.
The two menisci differ from each other not only in their shape but also in their mobility. During movements of flexion, extension and rotation of the tibia, both menisci follow the displacements of the femoral condyles. Due to its loose attachments the lateral meniscus rotates more freely about its central attachments and is less prone to mechanical entrapment. The medial meniscus, however, is more firmly attached and displays only half the movement of the lateral meniscus and is therefore more frequently injured during knee motions (see joint movement details below).
The ability to resist both the compression and tension forces is especially important in the knee joint, as described by Levangie & Norkin (2005).
Although compressive forces in the dynamic knee joint ordinarily may reach one to two times body weight during gait and stair climbing and three to four times body weight during running, the menisci assume 50% to 70% of the imposed load. Removal of the menisci nearly doubles the articular cartilage stress on the femur and multiplies the forces by six or seven times on the tibial plateau. … For this reason, meniscectomies are rarely performed after a meniscal tear; instead, care is taken to preserve as much of the meniscus as possible, either through debridement (removal of damaged tissue) or repair.
The ability of the menisci to resist these forces diminishes with age and with meniscal degeneration.
Gray’s anatomy (1995) reports that menisci ‘spread load by increasing the congruity of the articulation, give stability by their physical presence and as providers of proprioceptive feedback, probably assist lubrication, and may cushion extremes of flexion and extension.’ In adults, the peripheral zone is vascularized; however, the inner regions, where most tears occur, are avascular. Hence, peripheral tears have repair possibility, whereas with central tears resection may be the best choice.
Fibrous capsule and synovial membrane
The fibrous capsule is complex and so is the synovial lining. Many of the bursae are continuous with the joint capsule, being invaginations of the synovium and able to fill or void as needed and, in fact, doing so in response to pressures applied to them during flexion and extension.
• The posterior, vertical fibers attach proximally to the posterior margins of the femoral condyles and inter-condylar fossa; distally to the posterior margins of the tibial condyles and intercondylar area; proximally on each side with gastrocnemius attachments, strengthened centrally by the oblique popliteal ligament (derived from the tendon of semimembranosus), which thickens it.
• Medial capsular fibers attach to the femoral and tibial condyles where the capsule blends with the medial (tibial) collateral ligament.
• Lateral capsular fibers attach to the femur above popliteus and follow its tendon to the tibial condyle and fibular head. It is interrupted where popliteus emerges. A prolongation of the iliotibial tract fills in between the oblique popliteal and lateral (fibular) collateral ligament and partially covers the latter.
• Anteriorly, the capsule blends with expansions from the vasti medialis and lateralis, which attach to the patellar margins and patellar ligament, from where fibers extend posteriorly to the collateral ligaments and tibial condyles. Medial and lateral patellar retinacula are formed with the lateral being augmented by the iliotibial tract. An absence of capsule proximal to the patella allows for continuity of the suprapatellar bursa with the joint.
• The capsule attaches internally to the meniscal rims, which affords them a connection to the tibia by short coronary ligaments.
Regarding the synovial lining, Levangie & Norkin (2005) note: The synovial lining of the joint capsule is quite complex and is among the most extensive and involved in the body’. They describe the ensheathing, infolding synovial lining in detail, noting its adherence to the fibrous layer of the capsule except posteriorly where ‘the synovium breaks away from the inner wall and invaginates anteriorly between the femoral condyles’. It adheres to the sides and anterior portion of the anterior and posterior cruciate ligaments, resulting in these ligaments, while contained within the knee joint capsule, being excluded from the synovial sleeve.
Gray’s anatomy (2005) notes that:
The synovial membrane of the knee is the most extensive and complex in the body. It forms a large suprapatellar bursa between quadriceps femoris and the lower femoral shaft. The bursa is an extension of the joint cavity and is sustained by articularis genu, which is attached to it. Alongside the patella the membrane extends beneath the aponeurosis of the vasti, especially under vastus medialis. …Distal to the patella, the synovial membrane is separated from the patellar tendon by an infrapatellar fat pad . … the membrane projects into the joint as two fringes, alar folds, which bear villi. … At the sides of the joint the synovial membrane descends from the femur and lines the capsule as far as the menisci, whose surfaces have no synovial covering.
Kapandji (1987) offers a detailed description of the variable plicae (recesses, pleats) of the synovial lining as well as the infrapatellar pad, a considerable pad of adipose tissue located between the patella and the anterior inter-condylar fossa. Regarding the plicae, Levangie & Norkin (2005) state:
Because size, shape, and frequency of these plicae vary among individuals, descriptions also vary among authors. The most frequent locations for the plicae, in descending order of incidence, are inferior (infrapatellar plica), superior (suprapatellar plica), and medial (mediopatellar plica). …Synovial plicae, when they exist, are generally composed of loose, pliant, and elastic fibrous connective tissue that easily passes back and forth over the femoral condyles as the knee flexes and extends. On occasion, a plica may become irritated and inflamed, which leads to pain, effusion, and change in joint structure and function, called plica syndrome.
Bursae
There are many bursae in the region of the knee, some of which are continuous with the joint capsule. (Fig. 13.13)
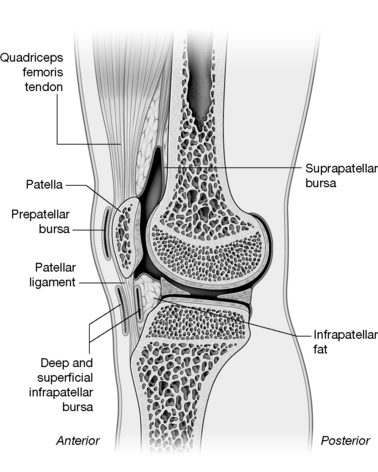
Figure 13.13 Several of the bursae of the knee can be seen in this crossection. Articularis genus is visible deep to the quadriceps tendon.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
The most important include the following:
• subcutaneous prepatellar bursa between the lower patella and skin allows movement of the skin over the patella during flexion and extension
• infrapatellar bursa between the tibia and patellar ligament reduces friction between these two surfaces
• subcutaneous infrapatellar bursa between the distal part of the tibial tuberosity and skin may become irritated by kneeling or by direct trauma
• suprapatellar bursa between the femur and quadriceps femoris is continuous with the joint capsule.
• between the lateral collateral ligament and the tendon of biceps femoris
• between the lateral collateral ligament and the tendon of popliteus
• between the tendon of popliteus and the lateral femoral condyle, usually an extension from the joint.
• between the medial head of gastrocnemius and fibrous capsule
• between the medial collateral ligament and the tendons of sartorius, gracilis and semitendinosus
• various bursae deep to the medial collateral ligament between the capsule, femur, medial meniscus, tibia or tendon of semimembranosus
• between the tendon of semimembranosus and the medial tibial condyle.
Regarding the bursae that communicate with the joint capsule, Levangie & Norkin (2005) note:
The three bursae that are connected to the synovial lining of the joint capsule allow the lubricating synovial fluid to move from recess to recess during flexion and extension of the knee. In extension, the posterior capsule and ligaments are taut and the gastrocnemius and subpopliteal bursae are compressed. This shifts the synovial fluid anteriorly (Rauschining 1980). [Fig. 13.14A] In flexion, the suprapatellar bursa is compressed anteriorly and the fluid is forced posteriorly. [Fig. 13.14B] When the joint is in the semiflexed position, the synovial fluid is under the least amount of pressure. Clinically, when there is an excess of fluid within the joint cavity, as a result of injury or disease (termed joint effusion), the semiflexed knee position helps to relieve tension in the capsule and, therefore, minimizes discomfort.
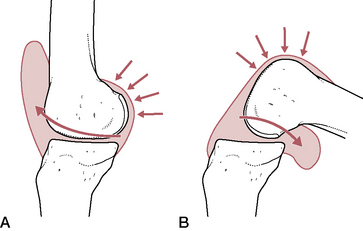
Figure 13.14 A: In extension the fluid of the knee moves anteriorly due to tension of the gastrocnemius while (B) in flexion it is pressed posteriorly by the quadriceps tendon, ensuring that the articulating surfaces are constantly bathed in the nourishing and lubricating synovial fluid
(reproduced with permission from Kapandji 1987).
Ligaments of the knee joint
The health of the ligaments and capsule of the knee joint is critical to knee stability and in maintaining integrity, and also in knee joint mobility (Levangie & Norkin 2005). The various ligaments play critical roles in preventing excessive knee extension, controlling varus and valgus stresses at the knee, preventing excessive anterior and posterior displacement as well as medial and lateral rotation of the tibia beneath the femur and modulating various combinations of displacement and rotation, collectively known as rotatory stabilization (Levangie & Norkin 2005). The most important of the knee ligaments include:
• patellar ligament (ligamentum (tendo) patellae) (discussed later)
• anterior and posterior cruciate ligaments
• medial (tibial) and lateral (fibular) collateral ligaments
• arcuate popliteal and posterior oblique ligaments
Cruciate ligaments (Fig. 13.15)
The anterior and posterior cruciate ligaments are very powerful structures that cross each other (hence their name) as they run anteriorly and posteriorly from their tibial attachments to their femoral attachments. Although located centrally within the joint capsule, they lie outside the synovial membrane, which invaginates around them to their anterior surface. These two ligaments are considered to be significantly responsible for ensuring stability of the knee and, when damaged, contribute to considerable impairment and disability. Cailliet (1992) interestingly notes, however, that ‘…there are several reported cases of congenital absence of cruciate ligaments with apparent normal knee function (Johansson & Aparisi 1982, Noble 1976, Tolo 1981), which brings into question why traumatic impairment of the ACL causes such disability’.
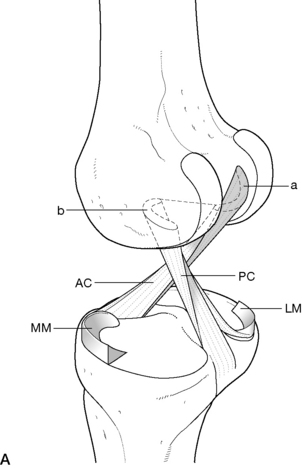
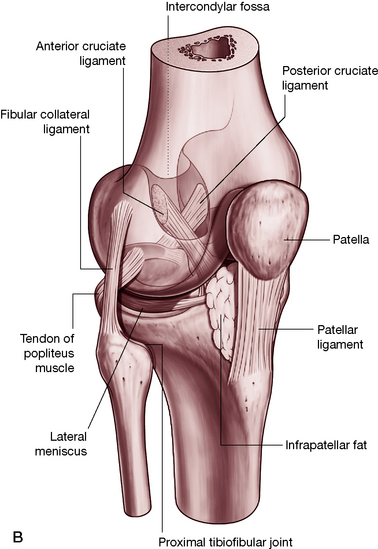
Figure 13.15 A: The cruciate ligaments. a: Attachment of anterior cruciate ligament (AC) b: Attachment of posterior cruciate ligament (PC); medial meniscus (MM); lateral meniscus (LM). (reproduced with permission from Kapandji 1987); B: The complexities of the knee joint are made ‘visible’ in this transparency graphic. (Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
Much confusion between these two ligaments can be avoided once it is realized that they are named for the location of their tibial attachment; that is, the anterior cruciate ligament (ACL) attaches to the anterior aspect of the tibial plateau and the posterior cruciate (PCL) to the posterior aspect. Staying with the tibia as the base of understanding, it is then easy to remember that the ACL forbids excessive anterior displacement of the tibia, while the PCL forbids excessive posterior displacement. However, sometimes descriptions are given as to excessive movement of the femur on the fixed tibia, which are also movements that these ligaments restrain. By recalling the relationship between the tibia and the femur when the femur is moving anteriorly, it is easier to understand which ligament prevents the movement and is therefore more vulnerable to injury in that particular case. That is, when the femur is moving anteriorly on the tibia, the tibia is posteriorly related to it, hence the posterior ligament will check that movement.
Both cruciate ligaments are composed of type I collagen separated by type III collagen fibrils, as well as abundant fibroblasts. Levangie & Norkin (2005) note:
Ligamentous injuries may occur as a result of a force that causes the joint to exceed its normal ROM, usually the translational ROM. Although excessive forces may cause ligamentous tears, lower-level forces may similarly cause disruption in ligaments weakened by aging, disease, immobilization, steroids, or vascular insufficiency. …A weakened ligament may take 10 months or more to return to normal stiffness once the underlying problem has been resolved. After a ligament injury or reconstruction, the new or damaged tissue must be protected to minimize excessive stress through the healing tissue. Absence of tissue stress, however, is also detrimental, because the new tissue will not adapt and become stronger under unloaded conditions
Therefore, prolonged disuse of the knee joint may weaken the ligaments, as noted by Cailliet (1992): ‘Failure occurs more rapidly after any significant immobilization in which the ligaments are not being repeatedly stretched to their physiological limits (Noyes et al 1974)’. Rehabilitation becomes a balancing act between too much applied stress and not enough.
In addition to restraining excessive tibial displacement, these two ligaments also limit excessive tibial rotation on the femur and, to a small degree, limit valgus and varus stresses upon the knee joint. Additionally, when placed under tension, each ligament, by its angulation of attachment, causes rotation of the tibia and hence plays an important role in functional joint movements.
Anterior cruciate ligament
The ACL attaches medially to the anterior intercondylar area of the tibia and partially blends with the anterior horn of the lateral meniscus (Gray’s anatomy 2005). It ascends superiorly and postero-laterally, to attach to the posteromedial aspect of the lateral femoral condyle while twisting upon itself en route, lying, as a whole, primarily anterolateral to the posterior cruciate (Gray’s anatomy 2005).
The ACL is considered to be the primary restraint that forbids excessive forward translation of the tibia under the femoral condyles. Details of the functions of its various bands when placed at different degrees of flexion are beyond the scope of this text but it is interesting to note that the posterolateral band checks excessive hyper-extension of the knee, while the anteromedial band is more involved with the flexed knee, although tautness is maintained in a portion of the fibers in all positions (Cailliet 1992, Levangie & Norkin 2005). It is likely that the ACL also makes minor contributions to restraining both varus and valgus stresses.
Regarding the ACL’s role during rotation of the tibia, Levangie & Norkin (2005) state:
Although the ACL may not make an important contribution to limiting medial rotation of the tibia, medial rotation of the tibia on the femur increases the strain on the [anteromedial band] of the ACL, with the peak strain occurring between 10° and 15°. … Regardless of the rotational effect on the ACL’s loading pattern, injury to the ACL appears to occur most commonly when the knee is slightly flexed and the tibia is rotated in either direction in weight-bearing. In flexion and medial rotation, the ACL is tensed as it winds around the PCL. In flexion and lateral rotation, the ACL is tensed as it is stretched over the lateral femoral condyle.
Posterior cruciate ligament
The stronger, less oblique and somewhat shorter fibers of the PCL are attached to the posterior intercondylar area and posterior horn of the lateral meniscus, blending with the posterior capsule and ascending anteromedially to the lateral surface of the medial femoral condyle (Gray’s anatomy 2005). It is twice as strong as the ACL, resulting in much less frequent injury.
The PCL is considered the primary restraint that prevents excessive posterior translation of the tibia under the femoral condyles. It, too, can be divided into various bands – the anteriomedial band (AMB) and the posterolateral band (PLB) (Levangie & Norkin 2005). It is likely that the PCL also makes minor contributions to restraining both varus and valgus stresses. As a knee stabilizer, it is taut when the weight-bearing tibia is extended and it restrains hyperextension of the knee.
Like the ACL, the PCL plays a role in restraining as well as producing rotation of the tibia. That is, when posterior translational forces are placed on the tibia and the PCL is taken into tension, a consistent concomitant lateral rotation of the tibia (medial rotation of the femur) is produced. Levangie & Norkin (2005) suggest that: ‘Increasing tension in the knee joint ligaments … may also contribute to the obligatory rotational motion … The tibial tubercles become lodged in the intercondylar notch, the menisci are tightly interposed between the tibial and femoral condyles, and the ligaments are taut’. This ‘screw home’ locking mechanism results in an automatic (terminal) rotation of the knee joint, which brings the joint into a close-packed position and ‘locks’ it in extension, where further rotation is disallowed.
The collateral and capsular ligaments (see Figs 13.4A, 13.5, 13.14)
The collateral and capsular ligaments of the knee reinforce the rather thin fibrous membrane of the joint capsule. The collateral ligaments are of substantial importance since they not only restrict varus and valgus forces on the knee joint but also stabilize the knee by guiding it during movements. Therefore, the collateral ligaments, like the cruciate ligaments previously discussed, are important in facilitating functional movements of the knee joint as well as stabilizing it.
Medial (tibial) collateral ligament (MCL)
This broad flat band at the medial aspect of the joint extends from the medial femoral epicondyle, sloping anteriorly to descend to the medial margin and posterior medial surface of the tibial shaft. Some fibers blend with the joint capsule while others extend medially to fuse with the medial meniscus, resulting in less mobility of the medial meniscus than the lateral. It is separated from the tendons of sartorius, gracilis and semitendinosus, which cross it, by bursae and it covers the anterior part of the semimembranosus tendon. Posteriorly it blends with the back of the capsule and attaches to the medial tibial condyle.
The primary and obvious function of the MCL is to resist valgus stresses at the knee joint, especially when the knee is extended. However, Levangie & Norkin (2005) note: ‘When the knee is flexed, the MCL plays a more critical role in resisting valgus stress despite the permitted joint gapping.’ They also state that the MCL checks lateral rotation of the tibia contributes to restraint when anterior displacement of the tibia is not adequately prevented by the ACL. The MCL is richly supplied with blood and has the capacity to heal when damaged or ruptured. ‘An isolated injury, therefore, does not often necessitate surgical stabilization, but is often left to heal on its own, although this remodeling process can take up to a year.’
Lateral (fibular) collateral ligament (LCL)
The LCL attaches to the lateral femoral epicondyle, proximal to the popliteal groove, from where it runs to the head of the fibula anterior to its apex. The tendon of biceps femoris overlaps and merges with it, while beneath it lie the popliteal tendon, the inferior lateral genicular vessels and nerve.
This ligament resists varus stresses and limits lateral rotation of the tibia. Like its medial counterpart, it plays a role in resisting excessive displacement of the tibia, in this case posterior displacement when combined with lateral rotation. It does not attach to the lateral meniscus, which therefore remains freer to move with the condyles, resulting in less frequent injury (20%) than tends to occur in the medial meniscus (80%) (Cailliet 2004).
Popliteal ligaments
Oblique popliteal ligament
The tendon of semimembranosus expands to form the oblique popliteal ligament, which partially merges with the capsule from where it directs laterally to the intercondylar line and lateral femoral condyle. It reinforces the posteromedial aspect of the joint capsule.
Arcuate popliteal ligament
The arcuate popliteal ligament reinforces the posterolateral aspect of the joint capsule coursing from the apex of the fibular head, crossing the tendon of popliteus, and merging into the joint capsule (Gray’s anatomy 2005).
Meniscofemoral ligaments
The anterior and posterior meniscofemoral ligaments extend from the posterior horn of the lateral meniscus to attach to the medial femoral condyle. They vary as to their presence and, according to Cailliet (1992), ‘apparently work in concert with the popliteus muscle to maintain stability (by making the lateral meniscus congruent with the lateral femoral condyles)’. When the femur externally rotates, these ligaments assist popliteus in pulling the meniscus posterolaterally to avoid entrapment.
Iliotibial band
The iliotibial (IT) band is a fibrous reinforcement of the fascia lata of the thigh, into which tensor fasciae latae and gluteus maximus muscles introduce proximally oriented tension that stabilizes the lateral knee. The IT band attaches to the lateral tubercle of the tibia, the lateral femoral condyle and the linea aspera of the femur. The tendinous fibers of the anterior portion of the tensor fasciae latae (a muscle that contributes to the IT band) also merge into the lateral patellar retinaculum and deep fascia of the leg. While the band is not actually a ligament, at the knee it is considered to be a passive joint structure serving to stabilize the knee since contraction of the muscles contributing to it does not create movement of it at the knee level. Levangie & Norkin (2005) note: ‘The IT band moves anterior to the knee joint axis as the knee is extended, and posteriorly over the lateral femoral condyle as the knee is flexed. The IT band, therefore, remains consistently taut regardless of position of the hip or knee’s position.’ The treatment of the iliotibial band is further discussed on p. 424.
Relations
Regarding the structures that overlie the joint, Gray’s anatomy (2005) mentions the following muscular and neurovascular relationships.
Anteriorly are the tendon of quadriceps femoris (which encloses and is attached to the non-articular surfaces of the patella), the patellar tendon, tendinous expansions from vastus medialis and lateralis which extend over the anteromedial and anterolateral aspects of the capsule respectively), and the patellar retinacula. Posteromedial is sartorius, and the tendon of gracilis which lies along its posterior border, both descending across the joint. Posterolaterally the biceps tendon and the common peroneal nerve which lies medial to it are in contact with the capsule, separating it from popliteus. Posteriorly the popliteal artery and associated lymph nodes lie on the oblique popliteal ligament: the popliteal vein is posteromedial or medial, and the tibial nerve posterior to both. The nerve and vessels are overlapped by both heads of gastrocnemius and laterally by plantaris. Gastrocnemius contacts the capsules either side of the vessels. Semimembranosus lies between the capsule and semitendinosus, medial to the medial head of gastrocnemius.
Movements of the knee joint
The movements of the knee joint are limited to flexion/extension with some axial rotation. In addition to these functional movements of the joint, anterior and posterior displacement of the tibia or femur, as well as some abduction and adduction of the tibia, are possible. ‘The small amounts of anteroposterior and medial lateral displacements that occur in the normal knee are the result of joint incongruence and variations in ligamentous elasticity. Although these translations may be seen as undesirable, they are necessary for normal joint motions to occur.’ (Levangie & Norkin 2005). Excessive movements of this type generally indicate laxity of the ligamentous elements.
The position of reference from which one can measure the range of motion of the knee joint is established by the axis of the leg being in line with the axis of the thigh and is usually termed a position of ‘full extension’. The following ranges of motion for movements of the knee use the position of reference as their starting point and are considered normal ranges (Kapandji 1987).
Flexion is movement of the posterior leg toward the posterior thigh from the position of reference, from which it is able to achieve (if the hip is simultaneously extended) about 120° of pure active flexion (a little more if follow-through is included), 140° if the hip is flexed and up to 160° if the knee is being passively flexed (heel touches buttocks).
In the position of reference, the leg is fully extended, so making active extension 0°. However, it is possible to achieve 5–10° of passive extension (sometimes erroneously called ‘hyperextension’). Relative extension brings the knee toward the position of reference from any position of flexion.
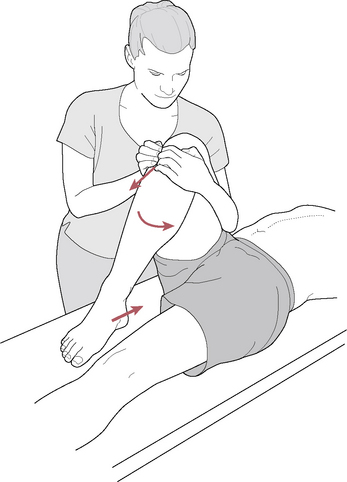
Axial rotation of the knee joint is maximal when the knee is at 90° of flexion. It is important that the patient is placed in a position that also prevents hip rotation, such as sitting on the table with legs hanging at 90° over the table edge. In this position of flexion, a normal range of active medial rotation of the tibia is around 30° with lateral rotation being around 40°. Passive rotation adds 5° in medial rotation and up to 10° in lateral rotation (Fig. 13.16).
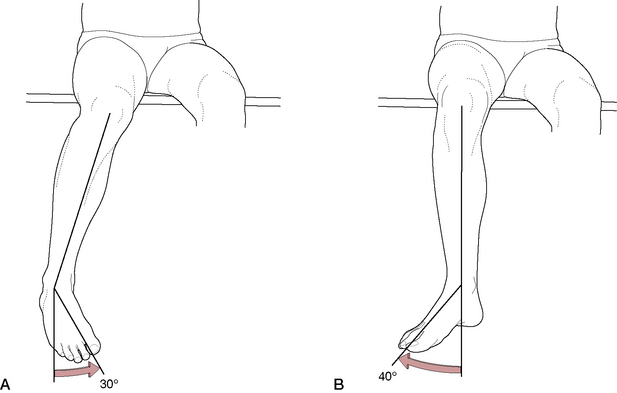
Figure 13.16 A: Active medial rotation of the knee. B: Active lateral rotation of the knee. Passive rotation will yield an additional 5–10°
(reproduced with permission from Kapandji 1987).
The contrast between what is observed as simple flexion and extension of the knee and what is actually occurring internally, involving as it does a complex coordination of numerous subsystems within the joint, is quite amazing. The movements are every bit as complex as the joint design itself, with each of the previously discussed structures playing an intricate role in functional movements of the knee.
Arthrokinematics of the knee joint
Though the roundedness of the femoral condyles suggests that they roll over the tibial condyles, this is only partially true. As compared to the relatively small tibial condyles, the large femoral condyles would in fact quickly use up the amount of ‘runway’ available and spill over and fall off the tibial plateau, thereby dislocating the joint (Kapandji 1987). In fact, the length of the tibial condyle is only half that needed for the femoral condyle to roll across it. In order for the condyle to fully engage itself on the short tibial condyle, a degree of sliding (gliding) is necessary. During flexion of the weight-bearing knee, the femur rolls onto the posterior aspect of its condyles, which (after a certain degree of pure rolling) simultaneously slide posteriorly on the tibial plateau. After initial movement begins, the menisci must move with the condyles in order to avoid being damaged, each being pushed around the tibial surface by its respective femoral condyle, as the condyle engages the sloping edge of its meniscus.
To highlight the complexity of this situation, it is important to note that the asymmetry of size of the medial and lateral condyles also adds its component to joint movement. For instance, as the joint extends, the lateral condyle completes its rolling-gliding motion at about 30° of remaining flexion, while the longer medial condyle still has more condylar surface to roll upon. At this point, the lateral condyle is somewhat ‘fixed’ and becomes a pivotal point around which the medial condyle completes its motion. Distortion of the menisci (not just movement on it or of it) becomes an important component of functional joint movement, as the medial femoral condyle pushes the medial meniscus posteriorly. Levangie & Norkin (2005) approach it similarly from a tibial aspect:
This continued anterior motion of the medial tibial condyle results in lateral rotation of the tibia on the femur, with the motion most evident in the final 5° of extension.
While the condyles distort the menisci passively, ligamentous and muscular elements actively play a role.
The resultant movement of the medial condyle around the lateral condyle is also influenced by the cruciate and collateral ligaments, which, when reaching maximum length, mandate resultant axial spin of the tibia or femur. In extension, the condylar movement coupled with ligamentous tension creates ‘automatic’ or ‘terminal’ rotation of the knee joint, commonly also referred to as a ‘screw home mechanism’, which locks the joint in full extension. The tibial tubercles are thereby lodged into the intercondylar notch, the menisci distorted and tightly embedded between the femoral and tibial condyles and the ligaments are pulled taut. Though the cruciate ligaments are not a true pivotal point, they are a central link, strategically placed so that as tension is exerted on them, they influence (increase) the rotational component, thereby close-packing and locking the joint to create tremendous stability of the fully extended knee.
A reverse of this movement is necessary to unlock the joint and allow flexion to once again take place. Levangie & Norkin (2001) note:
The laterally rotated tibia cannot imply flex but must medially rotate concomitantly as flexion is initiated. A flexion force will automatically result in medial rotation of the tibia because the longer medial side will move before the shorter lateral side.
During flexion, pure rolling (without glide) occurs only during the first 10–15° for the medial condyle and goes on to about 20° for the lateral condyle (Fig. 13.5A/B). Kapandji (1987) insightfully states that while the degree of rolling and sliding varies from condyle to condyle, and also varies in flexion and extension, ‘the 15–20° of initial rolling corresponds to the normal range of the movements of flexion and extension during ordinary walking’. Distortion of the menisci is then reserved for greater degrees of movement, including axial rotation.
Kapandji (1987) explains the important role the menisci play as ‘elastic coupling which transmits any compression forces between the femur and the tibia’. In extension, the greatest degree of condylar contact is needed to insure stability, while mobility (due to lessened contact) is needed during flexion. This is possible with the help of the active mechanisms.
…during extension the menisci are pulled forward by the meniscopatellar fibers, which are stretched by the anterior movement of the patella, and this draws the transverse ligament forward [while the condyles are moving posteriorly]. In addition, the posterior horn of the lateral meniscus is pulled anteriorly by the tension developed in the meniscofemoral ligament, as the posterior cruciate ligament becomes taut; during flexion, the medial meniscus is drawn posteriorly by the semimembranous expansion which is attached to its posterior edge, while the anterior horn is pulled anteriorly by the fibres of the anterior cruciate ligament attached to it; the lateral meniscus is drawn posteriorly by the popliteus expansion.
This tugging of the menisci into various positions most ideally allows the condyles to roll, slide/glide or cease movement, as needed, without entrapping and thereby damaging the interposed meniscal tissue.
Levangie & Norkin (2005) describe the arthro-kinematics (intraarticular movements) of the knee joint.
The large articular surface of the femur and the relatively small tibial condyle create a potential problem as the femur begins to flex on the fixed tibia. If the femoral condyles were permitted to roll posteriorly on the tibial plateau, the femur would run out of tibia and limit the flexion excursion. … The wedge shape of the menisci posteriorly forces the femoral condyle to roll ‘uphill’ as the knee flexes.
As the oblique forces of the condyles and menisci interact, the menisci are virtually pushed around by the femoral condyles and travel with them as they move about the tibial plateau. ‘The oblique contact force of the menisci on the femur helps guide the femur anteriorly during flexion while the reaction force of the femur on the menisci deforms the menisci posteriorly on the tibial plateau’. Because of the loose attachments of the lateral meniscus as well as the fact that its two horns attach relatively near each other, it is far more mobile than the medial one, leading to greater incidence of injury to the less mobile medial meniscus.
The patellofemoral joint
The role of the patella, the body’s largest sesamoid bone, is to protect the quadriceps tendon from friction against the femur and to act as an anatomic eccentric pulley as the small bone, and its associated tendon, slide up and down the patellar surface of the femur and the intercondylar notch. It is by means of the shape and movement of the patella that the laterally oblique force of the quadriceps muscles is transformed into a vertical force (Kapandji 1987).
A detailed discussion of the mechanics of patellar movement and the resultant dysfunctions that can result from poor mechanics is beyond the scope of this text. However, a brief review of surface anatomy and functional movements of the patellofemoral joint will assist the clinician in assessing involvement of these elements. Further details regarding this joint are found in the texts cited in this section.
Patellar surface of the femur
The proximal border of the patella surface of the femur runs distally and medially, separated from the tibial surfaces by two faint grooves, which cross the condyles obliquely. The lateral groove runs laterally and slightly forward, resting on the anterior edge of the lateral meniscus with the knee fully extended. The medial groove rests on the anterior edge of the medial meniscus in full extension. The patellar surface continues back to the lateral part of the medial condyle as a semilunar area, which articulates with the patella’s medial vertical facet in full flexion (Fig. 13.17).
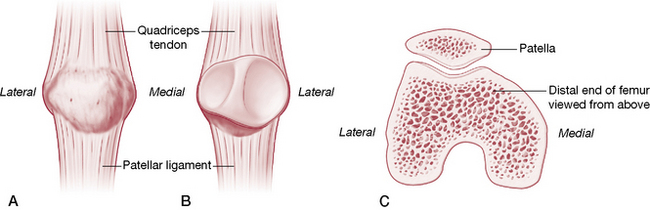
Figure 13.17 A/B: Anterior and posterior aspects of the right patella; C: Transverse section of distal end of femur (viewed from below).
(reproduced with permission from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone).
Gray’s anatomy (2005) describes the anterior surface of the distal femur.
The articular surface is a broad area, like an inverted U, for the patella [above] and the tibia [below]. The patellar surface extends anteriorly on both condyles, especially the lateral. It is transversely concave, vertically convex and grooved for the posterior patellar surface. The tibial surface is divided by the intercondylar fossa but is anteriorly continuous with the patellar surface…
A vertically oriented ridge divides the patella’s posterior surface into medial and lateral facets, which articulates with the femur. Covered with articular cartilage, these facets are adapted to the femoral surface, allowing the patella to ride smoothly up and down the femoral sulcus. An additional ridge on some patellae separates the medial facet from the extreme medial edge, denoting an additional surface known as the odd facet.
The patella
The patella lies within the quadriceps femoris tendon, anterior to the knee joint. Its shape is flat, triangular and curved. When standing, the distal apex of the patella lies slightly proximal to the level of the knee joint. The patella’s articular surface is much smaller than the femoral surface and its contact surface varies considerably during its movements, owing to the fact that it is one of the least congruent joints in the body (Levangie & Norkin 2005).
The thick superior patella border is an attachment for quadriceps femoris (rectus femoris and vastus intermedius). The medial and lateral borders respectively provide attachments for the tendons of vastus medialis and lateralis (known as the medial and lateral patellar retinacula). The lateral retinaculum also has attachments from the iliotibial tract.
The convex anterior surface allows passage for blood vessels and is separated from the skin by a prepatellar bursa, as well as being covered by fibers from the quadriceps tendon. This subsequently blends distally with superficial fibers of the patellar ligament, which is more accurately a continuation of the quadriceps tendon.
The oval, posterior articular surface of the patella is smooth and is crossed by a vertical ridge, which divides the patellar articular area into medial and lateral (the larger) facets. Approximately 30% of patellae will also have a second vertical ridge separating the medial facet from the third ‘odd’ facet, the extreme medial edge of the patella, which contacts the medial femoral condyle in extreme flexion. These facets, as well as the ridges, are well covered by articular cartilage. The patellar ligament attaches distally to a roughened apex and the infrapatellar pad of fat covers the area between the roughened apex and articular surface.
The distal surface of the patella is the attachment site for the patellar ligament (ligamentum (tendo) patella). The ligament derives from the tendon of quadriceps femoris, which continues on from the patella to attach to the superior aspect of the tibial tuberosity. It merges into the fibrous capsule as the medial and lateral patellar retinacula. The ligament is separated from the synovial membrane by a fat pad and from the tibia by a bursa.
• the descending genicular branches of the femoral artery
• superior, middle and inferior genicular branches of the popliteal artery
• anterior and posterior recurrent branches of anterior tibial artery
• the circumflex fibular artery
• the descending branch of the lateral circumflex femoral artery.
Movements of the patella
The patella is capable of several motions due primarily to its small articular surface (as compared to its associated femoral surface), its lack of congruence, and the several directions of tension available through the quadricep fibers. When the knee is fully extended, the patella is suspended in front of the femur with little or no contact of the articular surfaces. As the knee joint flexes, the patella is seated between the femoral condyles and slides down the femur (patellar flexion), ending in full flexion by presenting its articular surface superiorly (facing the distal end of the femur). During this course of sliding distally, it may experience medial and lateral patellar tilting (rotation about a vertical axis) (Fig. 13.18) the degree of which depends upon the shape of the femoral condyles, which it must conform to en route. The patella may also be shifted medially or laterally (primarily by quadriceps tension), thereby creating more drag on the corresponding articular facets. When the tibia is medially or laterally rotated, the patella may also exhibit medial and lateral rotation about an anterior/posterior axis, being pulled into rotation by the tibia via the patellar ligament (Fig. 13.19).
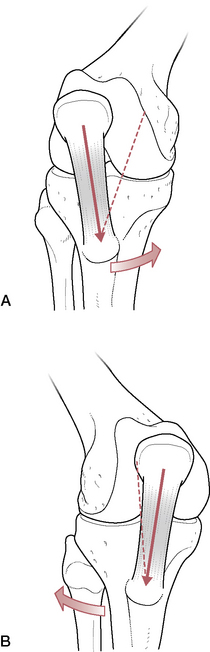
Figure 13.19 A: Medial and B: lateral patellar rotation with arrows indicating rotation of the tibia
(reproduced with permission from Kapandji 1987).
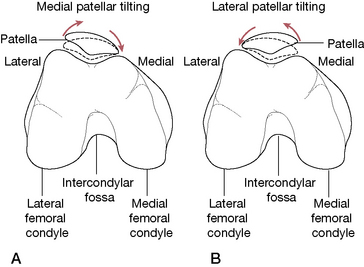
Figure 13.18 A: Medial and (B) lateral patellar tilting as viewed from the distal end of the femur. The dotted line shows normal position while superior and inferior tilting are not illustrated
(adapted from Levangie & Norkin 2001).
Levangie & Norkin (2005) note, ‘Failure of the patella to slide, tilt, rotate, or shift appropriately can lead to restrictions in knee joint ROM, to instability of the patellofemoral joint, or to pain caused by erosion of the patellofemoral articular surfaces’. Additionally, as the knee flexes and extends, the quadriceps pull the patella superiorly while the patellar tendon (ligament) pulls it inferiorly, which actually results in posterior compression force onto the femur. ‘During the stance phase of walking, when peak knee flexion is only approximately 20°, the patellofemoral compressive force is approximately 25% to 50% of body weight (Heino Breacher & Powers 2002). With greater knee flexion and greater quadriceps activity, as during running, patellofemoral compressive forces have been estimated to reach between five and six times body weight. (Flynn & Soutas-Little 1995)’
A major contributing force in pulling the patella out of its normal track, which thereby influences excessive pressures on particular aspects of the facet surfaces, is that of imbalanced pull of the quadriceps muscles. The effect of the alignment of the quadriceps and patellar ligament as they pull the patella across the femoral condyles can be assessed using a measurement called the Q-angle (the quadriceps angle, see Fig. 13.23). The angle, measured with the knee in extension or slightly flexed, is formed by the intersection of a line running from the ASIS to the mid-patella and a line connecting the tibial tuberosity to the mid-patella. An angle of 10° to 15° is considered normal. When the Q-angle is excessive (due to the pull of lateral forces), the vastus medialis oblique is responsible for horizontally aligning the patella and preventing lateral excursion. If this portion of the quadriceps is weak, or if hypertrophy of the vastus lateralis exists, especially in the presence of a high Q-angle, this will likely produce imbalanced patellar tracking as well as increased compressive forces, including those onto the lateral lip of the femoral sulcus (Levangie & Norkin 2005) (see p. 475 for further discussion).
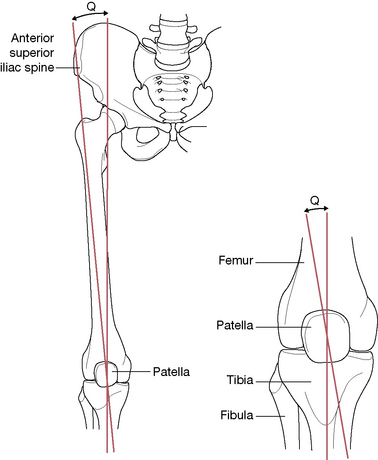
Figure 13.23 The Q-angle is formed by a line drawn from the ASIS to the middle of the patella and another line drawn from the tibial tuberosity extending through the patella. An angle of 10–15° is considered normal
(adapted from Cailliet 1996).
Soft tissue and joint dysfunction and assessment protocols
Throughout the body all cartilage is avascular, alymphatic, and aneural. Since cartilage is devoid of innervation, any injury to it will not be appreciated until there is a synovial reaction. Since the synovium is innervated it transmits nociception. Pain can also be experienced when the cartilage has undergone sufficient degeneration to expose the underlying bone, which is also innervated and transmits pain. Structural damage to cartilage can therefore occur even though the patient is totally oblivious of the injury (Cailliet 1992).
Some key causes of soft tissue damage to the knee include the following.
• Direct impact trauma, for example, involving contact sports or blows to the knee during motor vehicle accidents (MVAs).
• Levy (2001) suggests that most soft tissue wounds sustained by the knee derive from actions producing excessive torque on the knee joint, ‘especially those activities involving twisting, rapid deceleration, or landing from a jump’.
• Injuries to ligaments are inevitable if tensile forces placed on the knee exceed the intrinsic tone of the ligaments.
• Reversible injuries may result when low-intensity forces (lateral to medial) are involved. However, when heavy loads are applied, irreversible rupture of the ligament fibers may take place.
• Valgus-directed blows are common and most damaging when the knee joint is already in full external rotation, since this position places various ligaments on stretch. Resulting injuries (where forces are directed medially from the lateral aspect of the knee) may include tears of the MCL, damage to the posterior medial capsule and to the ACL (known as the O’Donahue triad) (Levy 2001).
• Varus knee injuries can result in a variety of problems, depending on the knee position at the time.
• If the knee is in a neutral position at the time of a laterally directed force (to the medial aspect of the knee), the LCL, the iliotibial band and/or the biceps femoris are likely to be damaged.
• If, however, the knee is extended and stressed by attempted internal rotation at the time of a strong varus strain the LCL, ACL, PCL and the lateral posterior capsule may be damaged.
• Varus stress to the flexed knee that is also being stressed by (inappropriate) internal rotation tends to produce LCL injury, as well as the ‘lateral posterior capsule and/or lateral meniscus and, if extreme, impairment of the PCL’ (Levy 2001).
• Traumas involving rotational movements are likely to cause tears in the menisci.
• The cruciate ligaments may be damaged when extreme hyperextension forces are applied.
• With regard to blows that rupture the cruciate ligaments, which ligament is injured will depend upon which bone is thrust in a posterior or anterior direction. ACL rupture, which is one of the most common and most serious of knee injuries, can result from a number of causes: for example, posteriorly directed blows to the femur that hyperextend the knee and thrust the femur posteriorly upon the fixed tibial plateau; excessive degrees of non-forceful hyperextension of the knee, as well as intense deceleration forces applied to the femur while the tibia is still moving forward. ACL damage may occur in isolation or together with other knee injuries, particularly tears of the menisci or MCL.
• PCL tears commonly result after falls onto a flexed knee that impacts the tibia and thrusts it posteriorly or, after sustaining a direct blow to the anterior aspect of the tibia (e.g. as in a MVA). PCL injuries are seldom isolated and are likely to involve other structures of the knee.
• Surgical intervention, knee replacement for example, results in major trauma to the soft tissues of the knee, sometimes demanding manipulation under anesthetic (see Box 13.5).
Box 13.5 Knee manipulation following total knee arthroplasty (Lombardi et al 1991) (see also box 13.4 on knee replacement)
Box 13.4 Total knee replacement: arthroplasty
When degenerative damage to the knee joint is advanced, most commonly due to osteoarthritis or rheumatoid disease, total surgical replacement or reconstruction (knee arthroplasty), is an option.
Cemented total knee replacement is regarded as the ideal approach for total knee arthroplasty (there are also partial variations), but use of uncemented designs, with bioactive surfaces (e.g. hydroxyapatite) also show promising results (Meneghini & Hanssen 2008)
Satisfactory knee function is usually restored following total knee arthroplasty, and the majority of patients are able to return to normal functionality, often including low-impact sporting activity. (Healy et al 2008)
Babazadeh et al (2009) report that the arthritic process, leading to a total knee replacement, can cause irreversible ligament shortening on one side and elongated ligaments on the opposite side. During surgery, ligament-balancing methods may attempt to counter these changes. This is achieved usually by removing osteophytes, and lengthening and dissecting tight ligaments in sequence.
Long-term studies show a 91–96% prosthesis survival rate at 14–15 years of follow-up. No difference appears to exist between posterior cruciate ligament-retaining and posterior cruciate ligament-substituting designs. Cementless designs do not have the same length of follow-up, but studies at 10–12 years report a 95% prosthesis survival rate. (March et al 2004)
Lombardi et al (1991) compared variables in 60 osteoarthritic patients with 94 posterior stabilized knee arthroplasties, who required manipulation. These were compared to 28 osteoarthritic patients with 41 posterior stabilized knee arthroplasties, who did not require manipulation.
Overall knee alignment, joint line elevation, anterior to posterior (AP) dimension of the knee, AP placement of the tibial component, patella height, obesity, age, preoperative flexion, time of manipulation, single versus bilateral, final flexion, final Hospital for Special Surgery (HSS) score and the development of heterotopic ossification were compared in both groups.
An increase in the AP knee dimension by 12% or greater significantly predisposed patients requiring manipulation. Quadriceps adhesions also led to manipulation and rupturing of these adhesions led to an increase in heterotopic ossification.
This evidence suggests that effusion (which increases knee dimensions) and the causes of effusion, as well as the presence of adhesions associated with quadriceps attachments, and scar sites, should be minimized if at all possible.
Manual therapy that incorporated manual lymphatic drainage, normalization (as far as possible) of traumatized quadriceps tissues utilizing MFR, MET, NMT and deep tissue massage methods, rehabilitation exercising and hydrotherapy should all assist in this.
• If there is marked effusion, severe pain and/or muscle spasm, underlying knee joint instability may be masked.
• All patients with knee injuries should be tested for active knee extension. Levy (2001) reports that about half of patients with a quadriceps tendon rupture initially are misdiagnosed and that ‘delayed diagnosis of extensor apparatus disruption may lead to contracture of the affected muscles, impairing the ability for later surgical repair of the lesion’.
• If a meniscal tear is not diagnosed, this may lead to chronic osteoarthritis in the knee joint.
• A torn lateral collateral ligament, if not sutured, is likely to produce massive scar formation during healing, which may affect its functional properties (Cailliet 1996).
CAUTION: It is important to note that while major injuries to the knee often make weight bearing impossible, being able to walk does not rule out the possibility of serious internal knee derangement. Similarly, the absence of joint effusion does not exclude the possibility of serious internal damage.
Sprains and strains of the knee
A sprain involves the stretching or tearing of noncontractile segments, such as ligaments or the joint capsule. In the knee joint, collateral ligament sprains are relatively common.
A strain of a ligament occurs when the imposed physical force on the ligamentous tissue exceeds that of normal stress and possibly surpasses the normal resilience of the tissue, but does not cause deformation or damage to the ligament. It also usually involves stretching or severing along the course of muscles or tendons, which may be injured by the force. Strain may also be caused by too much effort, or by excessive use, and may occur in bone as well as soft tissues.
Levy (2001), Cailliet (2004), and others classify ligamentous (sprains) according to the degree of impairment, as follows.
• Grade I sprain: in which stretching but no or only minor tearing of the ligament with most of the fibers intact has occurred, leaving local tenderness, minimal edema and no gross instability during stress testing. (Cailliet 2004) Motion tests demonstrate a firm endpoint. Treatment is by means of the RICE protocol, although some may benefit from a hinged knee brace (Cailliet 2004). (Bonica (1990) offers a slightly different description. ‘“Strain” is the term used for a condition in which a physical force imposed on the ligamentous tissue possibly exceeds that produced by normal stress but does not cause deformation or damage to the ligament, and physiologic recovery usually follows.’)
• Grade II sprain: in which moderate partial tears of the ligaments or nearly complete ruptures, but with an intact capsule (Cailliet 2004), have occurred, leaving moderate local tenderness, extensive swelling, and instability with stress testing, and moderate incapacity. There remains a firm endpoint at the end of range. Initial care demands some form of brace, cast or support to protect the joint, followed by conservative manual therapy and rehabilitation protocols.
• Grade III sprain: involving a complete tear, with discomfort on passive manipulation and a variable amount of edema (ranging from negligible to marked). There is likely to be clear instability with stress testing (and a soft endpoint). Grade III sprains almost always also involve tears of the posterior capsule and often the oblique popliteal ligament. Surgical intervention is often necessary followed by several months of support using a brace as well as manual therapy and rehabilitation. (Cailliet 2004)
Prognosis for sprains:
• The majority of grade I and grade II collateral ligament sprains heal over a 4–6-week period involving conservative rehabilitation therapy. Recurrence remains likely and chronic discomfort or pain is not unusual.
• Grade III collateral sprains require 3 or more months of support (brace) and manual therapy.
• If immobilization is necessary for any level of strain/sprain, rehabilitation exercises are required. Cailliet (2004) suggests ‘…immobilization of the knee for as short as a week leads to marked atrophy of the quadriceps muscle group, which requires rehabilitation exercises for strengthening and endurance as well as proprioception balance training’.
Characteristic pain signs
• If anterior knee pain starts abruptly, accompanied by inability to bear weight, this suggests damage to the extensor mechanism.
• If pain is acute and is localized to the medial or lateral regions of the knee joint, ligamentous and/or meniscal damage may be suspected.
• Pain of recent origin located at the posteromedial corner of the knee suggests a tear of the medial meniscus or an expanding or ruptured Baker’s cyst.
• Chronic pain that is worse at night may result from a tumor.
• Bursitis/tendinitis is likely to produce discomfort that is chronic worse on rising or walking after sitting, and provoked by prolonged use.
• Bearing in mind the evidence presented by Travell & Simons (1992), consideration should be given to what degree of knee pain (or any other pain conditions) derive from, or are exacerbated by, active myofascial trigger point activity.
Gross swelling/effusion (Fig. 13.20)
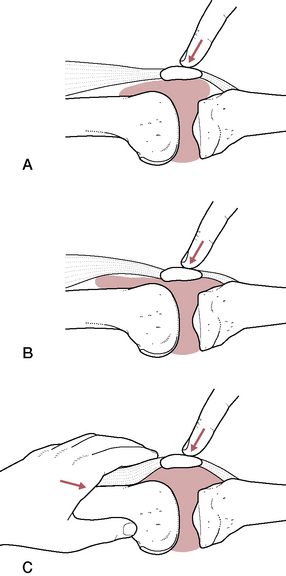
Figure 13.20 Ballotement test for effusion. A: Direct pressure causes no ballotement although fluid may not be obvious. B: With only a small amount of fluid, it may disperse superiorly and inferiorly, resulting in a negative test. C: Pressure applied proximal to the patella disperses the fluid laterally and medially, resulting in a positive ballotement test for presence of fluid or blood
(adapted with permission from Cailliet 1996).
• If effusion commences within 6 hours of an injury, suspicion points to a cruciate ligament tear, an articular fracture or knee dislocation.
• If effusion is delayed, meniscal injury is possible.
• Levy (2001) reports that ‘nearly one half of patients who sustain an acute ligament rupture experience localized edema at the site of injury’.
• Confusingly, complete ligamentous or capsular tears may result in only a small amount of swelling.
• Localized swellings may be noted with prepatellar bursitis, meniscal cystic changes, Baker’s cyst or a popliteal artery aneurysm.
Aspiration of fluid from the knee
• The knee joint provides one of the easiest sites for aspiration of fluid.
• Aspiration may be used to confirm a diagnosis, for example of sepsis or inflammatory arthritis, as well as for relieving pain due to swelling.
• The knee may contain 50 cc or more of fluid.
• If blood is aspirated this suggests a ligamentous tear (ACL, PCL), osteochondral fracture, peripheral meniscus tear, capsular tear or patellar dislocation.
• If fat globules are present in the aspirant this strongly suggests an intraarticular fracture.
• Although unusual, infection and hemarthrosis are known complications following aspiration.
Common (named) disorders of the knee
Patellofemoral pain syndrome (PFPS): tracking problems
A number of symptoms may develop in regards to the cartilage of the patella, including crepitation, pain and decreased range of motion of flexion and extension. Whether in an acute inflammatory stage or with moderate deterioration, patellofemoral pain syndrome (PFPS), also known as patella tracking disorder, is usually associated with weak quadriceps, weak hamstrings, abnormal femoral condyle movement, or internal or external rotation of the femur, any of which could contribute to abnormal patellofemoral contact (Cailliet 2004). Teng et al (2007) suggest that the fatigue rate of vastus medialis oblique as compare to vastus lateralis is an important factor and have presented research evidence demonstrating that individuals with PFPS had greater fatigability in the VMO than the VL.
Pedrelli et al (2009) note that patellar tendinopathy occurs frequently in athletes who perform multiple jumps – for example – in basketball, volleyball, and beach-volley. Patellar tendinopathy is also reported following frequent stair climbing, hiking and squatting. (Morelli & Rowe 2004). A feature in the etiology seems to be repetitive movements, as well as excessive strength training of the extensor compartment (quadriceps). Minor traumas and strains that result contribute significantly to this overuse syndrome. Symptoms, at first characterized by pain during strain, can evolve into inflammation (tendinitis) (Warden & Brukner 2003) with pain at rest, and eventually tissue changes and, in some cases, even tendon rupture.
In the discussion in Box 13.3 of taping procedures for treatment of PFPS, it is suggested that inappropriate patella tracking is a common mechanism in the evolution of knee pain.
Liebenson (1996) contends that in conditions involving quadriceps or patellofemoral dysfunction (‘runner’s knee’) or patellar tendinitis (‘jumper’s knee’), tracking disorders are commonly involved. He suggests that most tracking disorders ‘result from an imbalance between the quadriceps and the hamstrings…[and]…may also be attributed to lateral tracking of the patella caused by overactive TFL substituting for a weak gluteus medius’.
Liebenson reports that other common muscular problems associated with this type of knee dysfunction include: tightness of TFL, hip flexors, gastrocnemius and soleus, hamstrings, adductors and piriformis, as well as weakness of the hamstrings and gluteus medius (see discussion of postural and phasic muscles in Chapter 1). He suggests evaluation of possible foot dysfunction, as well as assessments such as the hip abduction test (Fig. 11.17, p. 320). This test evaluates (among other things) the relative efficiency of gluteus medius, which, if weak, will cause an increased role for TFL, which in turn will reduce the efficiency of patella tracking, with knee pain a probable end-result.
‘The key is not to wait until cartilage or meniscus damage occurs, or for the surgeons to practice their lateral release procedures.’ Instead, rehabilitation programs are recommended involving closed chain exercises, such as squats and lunges, but only if painless (Tipper 1992). If performance of these proves painful (probably because of the patella tracking problems), ‘Stretch out the tight muscles, start propriosensory balance training and facilitate gluteus medius’ and then, when squats and lunges can be performed painlessly, these should be started ‘and [then] gradually increase the depth of knee flexion’.
The authors concur with this approach, with additional need for evaluation (and treatment, if appropriate) of global postural patterns that may be involved, as well as myofascial trigger points that might produce TFL tightness and gluteus medius weakness.
Self-treatment for patellofemoral dysfunction
Baycroft (1990) observes that conditions such as PFPS, ‘runner’s knee’, ‘movie goer’s knee’ or chondromalacia patellae are most likely ‘the result of repeated microtrauma to the articular cartilage of the patellofemoral joint, in the presence of biomechanical influences which predispose to misalignment of the patella’.
As noted in Box 13.3 (taping), a distinction is now made between chondromalacia patellae and PFPS, with the former involving a degree of degeneration of the cartilage beneath the patella (Lowe 1999). PFPS is of unknown etiology or pathogenesis (Baquie & Brukner 1997) and it may or may not incorporate true chondromalacia patellae (Lowe 2006).
Baycroft describes a sequence for self-care, which requires that the practitioner instruct and coach the patient as follows.
• The patient sits on a chair with the leg to be treated extended at the knee, but relaxed.
• The practitioner shows the patient how the patella can be easily and gently (and painlessly!) glided proximally, distally, medially and laterally. It should be kept in mind that the knee must be fully yet passively extended in order for movement of the patella to occur.
• Some directions of glide are likely to be more resistant than others, most probably gliding distally as well as medially.
• Once the patient has learned to perform these passive gliding movements, the practitioner places the patient’s ipsilateral hand proximal to the upper pole of the patella, so that the patella is held by the first webspace, without compressing the patellofemoral joint.
• The patient is then asked to gently contract the quadriceps, drawing the patella proximally, so that it is engaged and resisted by the webbing of the hand. This should be completely painless. If pain is noted, the contraction and movement of the patella should be minimized. ‘If the maneuver is continued too far, or too vigorously, into the painful range, the condition will be aggravated rather than relieved’.
• The patient is asked to perform the procedure (involving proximal, distal, medial and lateral glides, as well as resisted quadriceps contractions (with complete relaxation between contractions), to the pain-free barrier for 5–10 repetitions, 3–6 times daily.
• The patient should gradually increase the range (degree of contraction and therefore amount of movement of the patella) but always remaining within a pain-free zone and always performing the translation movements, as well as the contractions.
Baycroft continues: ‘Once the patient has achieved a full range of painless active [and ideally symmetrical] patellar gliding, compression is added by altering the grip so that the upper pole of the patella is held in the palm of the hand. The sequence [of gliding and contractions] is repeated with increasing compression until the patient is asymptomatic’. Note: Medial and distal glides are particularly important in restoring balanced tracking.
Baycroft suggests that the passive stretching of shortened structures (achieved by medial and distal glides, mainly) as well as the toning of the quadriceps, especially vastus medialis obliquus, mobilizes and balances the patella and therefore minimizes joint irritation and rapidly removes symptoms.
The authors suggest that this protocol might well accompany other home care methods (such as Liebenson’s suggested squats and lunges, or the stretching of any shortened muscles, such as TFL, for example) as part of a comprehensive approach to such dysfunctional knee conditions as PFPS.
Patellar tendon tendinitis
Accompanying PFPS, there may be active inflammation of the patellar tendon, where quadriceps attaches to the patella. Schiowitz (1991) notes that ‘pain may be at the proximal, or more often, distal pole of the patella’. Pain will be very localized and aggravated by activity, but there is unlikely to be any associated swelling. Beneficial strategies may include:
• reducing stress on the tendon by means of releasing excessive tone in quadriceps (rectus femoris primarily) by utilizing myofascial release, NMT, PRT, MET and/or trigger point deactivation, as well as generally applying the principles of normalizing imbalances between agonists, antagonists and synergists
• normalizing foot function as well as postural and gait habits
• nutritional and hydrotherapeutic approaches designed to help modulate inflammation (see Volume 1 Chapter 7).
Fascial manipulation for patellar tendinitis
Fascial Manipulation® aims to map local fascial areas that, when treated appropriately, allows restoration of tensional balance. The selection of appropriate ‘points’ for treatment in any dysfunctional condition involves an analysis of the motor units responsible for moving a joint in a specific direction (e.g. sagittal, frontal, horizontal).
In this way, so-called centers of coordination (CC) are identified that, if dysfunctional (‘dense’), will negatively influence the functionality of corresponding soft-tissues (particularly fascia) and joints. In patellar tendinopathy, the monoarticular muscular fibers of vastus medialis, intermedius and lateralis, the biarticular muscular fibers of rectus femoris, and the associated fascial structures are considered to be implicated. In this instance, the CC is situated over the vastus intermedius muscle, overlapping with the acupuncture point ST32 (Bossy et al 1980), and with one of the major trigger points of the quadriceps group, as described by Simons et al (1999). Using this approach, Pedrelli et al (2009) treated 18 patients suffering from patellar tendon pain (mean duration of symptoms 8.6 months).
In this example of Fascial Manipulation® the treatment was performed with the patient supine and the therapist standing on the side to be treated. The therapist applied elbow pressure over the muscular fascia in the area between vastus lateralis and rectus femoris muscles (Figure 13.22), applying pressure toward vastus intermedius. Static pressure was applied, followed by deep friction or mobilization of the fascial tissues.
Intermittent friction was repeated for about 5 minutes, until the fascia was able to glide more freely and the patient reported that pain had decreased significantly. Results demonstrated a substantial decrease in pain immediately after treatment (p<0.0001), which was maintained at 1 month follow-up. See Fig. 13.22.
Osgood–Schlatter disease
This condition involves inflammation of the tibial tubercle resulting from traction tendinitis caused by excessive traction from the patellar tendon. It is relieved by rest and by reduction in traction stress applied to the tubercle. As in patellar tendinitis (above) beneficial strategies may include:
• reducing stress on the tendon by means of releasing excessive tone in quadriceps (rectus femoris primarily) utilizing NMT, MFR, PRT, MET and/or trigger point deactivation, as well as generally applying the principles of normalizing imbalances between agonists, antagonists and synergists
• normalizing foot function as well as postural and gait habits
• nutritional and hydrotherapeutic approaches designed to help modulate inflammation (see Volume 1, Chapter 7).
Chondromalacia patellae
If the scenario described in the notes on PFPS relating to unbalanced tracking of the patella during flexion and extension of the knee is a regular, chronic event, an excessive degree of friction is likely between the inner patella surface and the condylar surfaces. This in turn leads to irritation and, ultimately, pathological degenerative changes to the cartilage, broadly termed chondromalacia. Ultimately, this can result in arthritic changes. Knee pain during flexion and extension of the knee (much as in PFPS) is the likely presenting symptom. Symptoms are likely to be aggravated by use of stairs. A degree of noisy crepitus is likely and the patient may feel that the knee gives way at times, associated with increasing weakness of the quadriceps in general and VMO in particular. This weakness is likely to be accompanied by measurable degrees of atrophy, with the circumference of the thigh reducing appreciably and fairly rapidly (a matter of weeks can see a marked change). Assessment by means of arthroscopy (see Box 13.2) can offer definitive evidence of the cartilaginous changes. The patellofemoral compression test is a useful, simple assessment tool that can identify the condition with reasonable accuracy.
Arthroscopy is the most commonly performed type of orthopedic surgery and the knee is by far the most common joint on which it is performed. It involves use of an arthroscope, a very small instrument (part of which is a fiberoptic camera), that can be inserted into a joint through a tiny incision (often no more than 4mm, 1/8th of an inch, long), in order to examine (and sometimes treat) the interior of a joint.
Although a number of uncontrolled, retrospective case series have reported substantial pain relief after arthroscopic lavage, or arthroscopic debridement, for osteoarthritis of the knee (Baumgaertner 1990, Owings & Kozak 1998) more recent research studies have questioned the efficacy of knee arthroscopy to repair damaged tissues (‘key-hole surgery’) (Kirkley et al 2008).
In regards to the knee, arthroscopy is commonly used to visualize tissues for the purpose of diagnosis, as well as to possibly treat meniscus injuries. Englund et al (2008) have noted, however, that imaging methods (such as MRI) have made such interventions less common for diagnosis. They also suggest that their research demonstrated no long-term benefit for chronic pain symptoms in middle-aged and elderly patients following arthroscopic treatment, above that achieved by medication and physical therapy.
Moseley et al (2002) have reported that the fact that approximately 60% of damaged menisci cause no pain, and are frequently found in asymptomatic subjects, which calls into question the rationale for arthrosocopy. In their study, 180 military veterans with osteoarthritis of the knee were randomly assigned to receive arthroscopic debridement with lavage, or arthroscopic lavage alone without debridement (a procedure that imitated the surgical debridement, where superficial incisions to the skin were made to give the appearance that the debridement procedure had been performed). Moseley et al noted that, over a period of 2 years post-surgery, ‘In this controlled trial, involving patients with osteoarthritis of the knee, the outcomes after arthroscopic lavage or arthroscopic debridement were no better than those after a placebo procedure.’ (See also Box 13.12)
Levy (2001) reports that in most patients sustaining severe ligamentous or meniscal damage, plain film findings are normal. Fewer than 15% of knee radiographs reveal clinically significant findings.
Plain film radiographs are suggested for the following individuals with an acute knee injury:
• if experiencing tenderness over the fibular head
• reporting discomfort confined to the patella upon palpation
• if unable to flex the knee to 90°
• if incapable of bearing weight, immediately and for at least four steps.
Although plain radiography is not very helpful in diagnosis of soft tissue injuries, certain findings are suggestive of ligamentous, meniscal or tendon damage. Crucially, however, a 45° flexion, weight-bearing radiograph can show joint space loss and point to early osteoarthritic changes.
CT scans offer effective imaging to corroborate the presence of knee fractures. Ultrasound assessment may be able to help in differentiation of a Baker’s cyst, popliteal artery aneurysm and thrombophlebitis.
MRI is currently the method of choice for evaluating soft tissue injuries of the knee, especially if surgery is contemplated.
The patellofemoral compression test
• The patient is seated on the edge of the treatment table with knees flexed.
• The practitioner (or the patient) places a hand covering the patella with light compression and asks the patient to straighten the knee.
• If pain and/or grating crepitus is obvious, this is strongly suggestive of degenerative changes of the cartilage and possibly suggests chondromalacia patellae.
Bursitis
Pes anserine bursitis features include swelling at the medial aspect of the knee, inferior to the joint space, with severe localized tenderness. This is aggravated by contractions of sartorius, gracilis and semitendinosus.
Therapeutic attention should be given to dysfunction (shortness, weakness, trigger point activity) involving all muscular attachments to the knee, particularly those attaching medially. Antiinflammatory strategies should be employed, particularly hydrotherapy.
PRT methods may offer rapid first aid relief (see Box 7.2, p. 163).
Infrapatellar bursitis (aka ‘housemaid’s knee’)
• The infrapatellar bursa, between the tibia and the patellar ligament, will be swollen, usually as a result of localized trauma or habitual kneeling pressure.
• Pain is usually not a feature.
• This bursa is outside the joint capsule and the swelling therefore does not interfere with normal function.
• Therapeutic attention should be given to reducing pressure (kneeling) onto the area and lymphatic drainage.
Baker’s (or popliteal) cyst (commonly associated with semimembranosus tendon bursa)
• This effusion may relate to rheumatoid arthritis activity. If so, it may extend into the calf.
• The cyst may harmlessly rupture, causing pain and tenderness that mimics deep vein thrombosis (Toghill 1991).
• The swelling is usually painless and is not significant unless it interferes (through size) with normal joint motion.
Positional release first aid for the painful patella
Irrespective of the cause(s) of the pain noted in the patellar region, it is usually possible to offer (often only short-term) relief, by means of safe positional release interventions, which can be safely taught to patients for home use. This approach does not deal with the underlying causes of the condition, but can provide symptomatic relief.
• The periphery of the patella is carefully palpated using light pressure directed toward the center of the patella, to discover any localized areas of specific tenderness.
• With the knee in light extension digital pressure is applied onto the tender point to be treated, sufficient to warrant a score of ‘10’, to represent the level of discomfort.
• The patella should then be lightly eased toward the palpated pain point until a reduction in reported pain is noted.
• Further reductions are gained by easing the patella clockwise or anticlockwise, until the score is ‘3’ or less.
• This is held for 90 seconds before releasing, repalpating and possibly treating another tender point in the same manner.
Osteoarthritis (OA) of the knee
Women are affected with osteoarthritic knees more often than men and an estimated 25–30% of people between 45 and 64 and 60% of people older than 65 have radio-graphically detectable OA (Buckwalter & Lane 1996), although many are asymptomatic. Dowdy et al (1998) suggest that in injured knees, meniscus and cartilage transplants may prevent the development or progression of osteoarthritis.
The most common symptoms associated with OA knee are difficulty using stairs and difficulty in squatting. The symptoms are usually activity related, being worse by the end of the day. Pain may be localized to one compartment of the knee (i.e. medial, lateral or patellofemoral) or it can be more widespread, and may be associated with intermittent or constant swelling. If symptoms include a complaint of locking, either a meniscus tear or a loose body may be suspected. If the knee ‘gives way’ it should be established whether this is because of pain or because of actual mechanical instability.
Physical examination
• If the patient with OA demonstrates genu varum, medial compartment involvement is likely, while genu valgum suggests lateral arthritic changes in the knee joint (see Box 13.1).
• The range of flexion is limited as compared with a normal maximum flexion of approximately 120°. Crepitus of the patellofemoral joint is common.
• Knee stability in the coronal (i.e. varus/valgus) and sagittal (anteroposterior) planes should be determined (see p. 477, stress tests involving joint play).
• DeJour et al (1994) suggest that patients with OA knee may have increased tibial translation on Lachman’s test and anterior drawer testing (see below) indicating chronic ACL insufficiency, a possible precursor to OA.
• Tight hamstrings are very common in patients who have OA knees and they exacerbate the knee pain.
• It is important for the hip and back to be examined to rule out any contribution to the patient’s symptoms.
Activity modification and exercise
High-impact activities that include running and jumping are undesirable for anyone with OA knee. Low-impact activities such as swimming and cycling are usually safe and beneficial for the arthritic knee. If there is also evidence of patellofemoral chondrosis, activities that load the patellofemoral joint, such as squatting or use of stairs, should be limited.
Maintaining a healthy body weight is extremely important with OA knee problems and along with attention to diet, patients should maintain a regular exercise program to maximize aerobic conditioning.
Manual therapy
• The goals of conservative manual therapy are to increase range of motion, flexibility (especially in the hamstrings) and stability via enhanced quadriceps and hamstring strength.
• Hamstring stretching, quadriceps rehabilitation and isometric strengthening (e.g. straight leg raises) are all usually indicated, but their use should be determined by assessment.
• Additionally, closed kinetic chain strengthening of the quadriceps and hamstrings should be initiated, involving co-contraction of the hamstrings and quadriceps.
• As with all painful conditions, the contribution to the symptoms of active myofascial trigger points should be evaluated and these should be deactivated as appropriate.
• The use of supporting ‘knee sleeves’ during exercising may help active patients regain a sense of stability, possibly by enhancing their awareness of the knee joint (proprioception).
Note: Aspiration may be required to alleviate fluid buildup. Total or partial knee replacement should be considered in active patients only when all other options have been exhausted.
Soft tissue manipulation and joints
If soft tissue manipulation is used to treat a restricted joint, this implies that the treatment methods used do not actively manipulate the joint but rather the soft tissues associated with the joint dysfunction. Methods that fall into the broad definition of ‘soft tissue manipulation’ include all traditional massage methods, NMT, MET, PRT, MFR, mobilization with movement (MWM), as well as a variety of methods to encourage lengthening of shortened structures, toning of weakened ones and the normalization of localized or reflexogenic dysfunction (such as trigger points).
Employment of these approaches does not necessarily preclude the need for active joint manipulation in correcting restriction (although it frequently does), but can lessen the need to utilize high-velocity thrusts or long lever techniques, and to make their employment simpler and far less likely to traumatize the local tissues or the patient (See Boxes 13.10 and 13.11).
Box 13.11 Mobilization with movement (MWM) techniques for the knee (see Chapter 9)
Mulligan (1999), who developed MWM methods, suggests, ‘MWMs should always be tried when there is loss of movement that is obviously not the result of serious trauma’. MWM utilizes joint play, gliding, as a primary tool, after which the patient actively attempts to perform the movement that was previously restricted. If restriction is painlessly reduced as the joint is held in a glide or translation, it is performed again several times, after which it is tested without the addition of translation and should have improved.
Mulligan suggests: ‘Medial glide with medial knee pain and lateral glide with lateral knee pain’ and that flexion loss (as might occur in collateral ligament strain) is usually likely to be more assisted by MWMs than extension loss.
Many of the MWM applications to the knee require the use of a strap/seatbelt type device, to assist in production of stabilization and sustained glide. These are not described in this text since they require instruction in their usage, which should be acquired via normal physical therapy training procedures or through advanced workshops.
MWM for flexion pain and/or restriction of the knee (Fig. 13.30)
• The patient is supine, with the knee flexed to just short of the position where pain or restriction would be noted.
• The practitioner stands ipsilaterally, at waist level, facing the foot of the table, with both her hands enfolding the proximal tibia so that her fingers lie on the anterior tibial shaft, with the thenar eminence of the non-tableside hand resting posterior to the head of the fibula.
• The tibia is internally rotated by the practitioner’s hands and at the same time slight ventral (anteriorly directed) glide is introduced to the fibula.
• While these light forces are maintained, the patient is asked to actively increase the range of flexion, without passing any point where pain is noted.
• Light overpressure may be added by the practitioner when the patient reaches the end of the (new) range. (See Box 13.8 on overpressure.)
Box 13.8 Overpressure and end-feel
Overpressure refers to the practitioner adding force to an active movement, at the end of the physiological range as achieved by the patient. This is avoided if symptoms are not obvious at the end of range.
Petty (2006) provides the following guidelines for its use.
• The patient should be comfortable and supported.
• The practitioner should be in a comfortable position.
• Transference of body weight to initiate force for overpressure is preferred to application of intrinsic strength from the practitioner’s hands.
• The practitioner’s contacts need to be positioned ‘in line with the directions of force’, which should be applied slowly and smoothly, at the end of range achieved by the patient.
• At the end of the range the practitioner ‘applies small oscillatory movements to feel the resistance at this position’.
• The information gathered as overpressure is applied includes the following.
• The quality of the movement (Is it, as it should be, pain free, smooth and free of resistance?)
• Any additional range gained by overpressure (Is it to a normal endpoint, or is it an excessive degree of movement?)
• The resistance toward, and at the end of, the range of movement (Is it soft, empty, firm, hard, springy, abrupt?)
• Any pain (or other symptoms) noted at the end of range when overpressure is used (Is pain local, sharp, dull, referring?)
When end-feel is anything but normal (too early or too late), the questions the practitioner needs to ask relate to what is causing this difference. Is the obstacle an articular surface; a limitation due to loss of extensibility of muscle, ligament, tendon; a protective spasm; an increased degree of laxity due to mechanical or neurological features?
As Petty (2006) explains:
The pain may increase, decrease or stay the same when overpressure is applied. This is valuable information as it can confirm the severity of the patient’s pain and can help to determine the firmness with which manual treatment techniques can be applied. A patient whose pain is eased or remains the same with overpressure could be treated more firmly than a patient whose pain is increased.
MWM self-treatment
• The patient stands and places his right foot (in this example) flat onto the seat of a chair.
• He places his hands around the proximal leg, so that fingers meet anteriorly and the thenar eminence of his right hand rests posterior to the fibula head.
• With his hands he internally rotates the tibia while simultaneously easing the fibula anteriorly.
• Maintaining these forces of tibial rotation and anterior fibula glide, the patient increases the previously restricted, or painful, range of knee flexion, provided there is no pain on flexion.
• Mulligan reports: ‘I have my patients with OA knees do this on a regular basis as a home treatment. When …[this]…is successful, tape the tibia in internal rotation on the femur’. Mulligan suggests that taping with the leg in internal rotation is frequently useful for patellofemoral problems where tracking of the patella is faulty. (See Box 13.3 on taping procedures.)
Box 13.3 Supportive and proprioceptive taping for the knee
Taping is a widely used treatment modality that research has shown to improve function of injured knees, with benefits lasting well after removal of the tape (Perlau et al 1995). Following the success in taping ankles for increased stability and taping knees to improve patellofemoral function (Ernst et al 1999, Gerrard 1998, Refshauge et al 2000), use of taping has been extended to treatment and rehabilitation of shoulder and spinal dysfunction. Morrissey (2001) states:
Taping can be used to affect pain directly by offloading irritable myofascial and/or neural tissues. Taping can also be indirectly used to alter the pain associated with identified faulty movement patterns. These effects are essentially proprioceptively mediated. …The management of patello-femoral pain by means of taping has also been increasingly investigated in the literature and described elsewhere (McConnell 1996) with evidence for both mechanical and motor control effects of taping on patello-femoral movement and symptoms.
Various theories have been expounded to explain the clinical results obtained by taping.
Possible mechanisms
Proprioceptive response
According to Kneeshaw (2002): ‘Tape is said to stimulate neuromuscular pathways via increased afferent feedback from cutaneous receptors which with expert retraining can facilitate a more appropriate neuromuscular response (Parkhurst & Burnett 1994, Perlau et al 1995, McNair et al 1995)’. For example, Morrissey (2001) reports that: ‘Recent research suggests that, in a normal ankle joint, facilitation of proprioceptive cutaneous input by means of taping is effective in improving reaction speed and position awareness (Robbins 1995, Lohrer 1999). There is also some evidence that taping the patella can influence the relative onset of activity of the vastus lateralis and vastus medialis obliquus during quadriceps activation (Gilleard 1998). This may be cutaneously mediated.’
‘Biofeedback’ response
Morrissey (2001) suggests that:
Tape is applied in such a way that there is little or no tension while the body part is held or moved in the desired direction or plane. The tissues will therefore develop more tension when movement occurs outside of these parameters. This tension will be sensed consciously thus giving a stimulus to the patient to correct the movement pattern. Over time and with sufficient repetition and feedback, these patterns can become learned components of the motor engrams for given movements. This process therefore represents cutaneously mediated proprioceptive biofeedback.
Biomechanical response
The mechanical effects involve relocation of joints in such a way as to enhance stability or to alter length-tension relationships in order to approximate an ideal musculoskeletal posture or improved motor pattern (Gerrard 1998, Kibler 1998, Kneeshaw 2002).
• If taping is applied to hold an inhibited (underactive, ‘weak’) muscle in a shortened position, there will be a shift of the length–tension curve to the left, allowing greater force development in the inner range through optimized actin-myosin overlap during the cross-bridge cycle. This will encourage enhanced strength in previously inhibited muscles.
• Morrissey (2001) states: ‘Similarly, if taping can be applied in such a fashion that a relatively short, overactive, muscle is held in a lengthened position, there will be a shift of the length tension curve to the right, and lesser force development through decreased actin-myosin overlap during the cross-bridge cycle at the point in joint range at which the muscle is required to work’. This will encourage reduced activity in overactive postural muscles and will enhance tone in inhibited antagonists (Chaitow 2006) (Figs 13.21, 13.22).

Figure 13.22 Treatment position with pressure being applied to the centre of coordination - according to Fascial Manipulation® technique methodology.
(Borrowed from Pedrelli et al Journal of Bodywork and Movement Therapies 2009;13(1):73-80

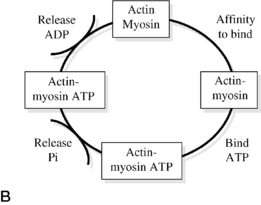
Figure 13.21 A: Length-tension curves. Although lengthening muscle has the capability to generate more force, postural muscles frequently need to generate most force in inner range positions in which case it is often desirable that they are relatively short (reproduced with permission from Morrissey Journal of Bodywork and Movement Therapies 2000; 4(3):190). B: The cross-bridge cycle. The primary motor proteins of muscle, actin and myosin, have a natural affinity and hydrolyze their fuel ATP (adenosine-triphosphate), first releasing inorganic phosphate (Pi) then adenosine diphosphate (ADP). Each of the stages of the cross-bridge cycle is in an equilibrium and can move in either direction dependent on a number of factors. The force generated is dependent on a number of factors including the stage of protein action, the degree of overlap of actin and myosin chains (hence the number of binding sites available) and the amount of motor units recruited and coordinated
(reproduced with permission from Morrissey Journal of Bodywork and Movement Therapies 2000; 4(3):190).
Additionally, there is probably a placebo effect (Hume & Gerrard 1998).
Taping as a form of positional release?
Despite these often attractive hypotheses there remains disagreement in the literature (see below) as to how taping actually contributes to patient improvement (Alt et al 1995, Ernst et al 1999, McNair et al 1995, Powers et al 1997, Refshauge et al 2000). There is also a suggestion that the therapeutic principles involved in positional release techniques (see Chapter 9 this volume and Volume 1, Chapter 10) may account for at least part of the success of this approach, since the tissues are, for a period of time, ‘unloaded’ – effectively being placed into their ‘comfort’ or ‘ease’ positions (Chaitow 2007, Morrissey 2001, 2007).
Clinical observations
Since there are a variety of taping possibilities in treatment of knee problems, an essential first step is to have a correct diagnosis, including if possible the pertinent causative factors. If the chosen taping application initially provides a beneficial result it should be reapplied in conjunction with relevant treatment and exercise until the symptoms disappear or the desired motor pattern has been achieved free of tape (Morrissey 2000).
Patellar taping in treatment of PFPS
Crossley et al (2000) have described patellar taping in treatment of PFPS, a common condition both in sporting settings and among the general population, of unknown etiology or pathogenesis (Baquie & Brukner 1997). This condition may or may not involve true chondromalacia patellae, which leads to degeneration of cartilage on the underside of the patella (Lowe 2006, Lowe 1999). (Note: Chondromalacia patellae is discussed elsewhere in this chapter.)
The symptoms of PFPS involve pain in the region of the anterior knee and/or surrounding the patella, commonly provoked or increased by sitting for a lengthy period, by stair climbing or squatting activities.
Among the etiological factors that have been suggested as leading to excessive stress being placed on the patellofemoral joint are (Merchant 1988):
• lateral displacement of the patella, possibly resulting from poor VMO function
• excessive tone or shortness of lateral soft tissue structures (iliotibial tract, vastus lateralis)
A variety of treatment approaches have been used to enhance the alignment of the patella in treating PFPS, including:
• specific VMO and general quadriceps retraining
• identification and stretching of shortened soft tissue structures
• focus on possible etiological input from the foot with appropriate orthotic support.
The original taping protocols for PFPS were developed by McConnell (1986) and her methods have subsequently been widely used (and modified), particularly in Australia.
A variety of taping applications may be required to achieve pain relief in PFPS, to modify patellar misalignments, including excessive lateral glide, lateral tilt, posterior tilt of the inferior pole and/or excessive rotation (McConnell 1996). Apart from attempting to correct such misalignments, taping may also be used to unload painful structures or to inhibit vastus lateralis overactivity. According to Crossley et al (2000):
The choice of taping techniques is based partly on the assessment of patellar alignment, and partly on the attainment of pain reduction. Appropriate taping combinations should decrease the patient’s pain by at least 50% during provocative activities and this may require a number of taping components.
The ideal result is one in which the patient can perform rehabilitation exercises (particularly aimed at enhanced quadriceps function), as well as everyday activities, in a relatively pain-free manner. ‘Ideally, tape is worn all day every day, especially in the early stages of treatment, and is continued until the patient is pain free. Patients are advised to remove the tape and reapply it if the pain from PFPS reoccurs’ (Crossley et al 2000).
Despite the undoubted success achieved clinically using taping methods in treatment of PFPS, the comprehensive review conducted by Crossley et al (2000) has failed to identify the mechanisms by which improvements are achieved. They conclude:
Patellar taping may affect the alignment of the patella, function of the quadriceps or the ability of the patellofemoral joint to withstand joint reaction forces but it is unknown whether these effects are causes or consequences of PFPS pain … [and] … while research is required to identify the mechanisms to explain the effects of patellar tape, it can be used with confidence as a safe and inexpensive adjunct to a rehabilitation program in the management of PFPS.
Taping guidelines (adapted from Morrissey 2001)
It is essential to be clear about the aims of taping in order to ensure optimal results. Which tissues need to be ‘unloaded’? Which tissues need to be moved? Which tissues need to be inhibited?
• The skin should be prepared by removal of surface oils and body hair.
• The tissues (such as the patella) should be placed in the desired position.
• A hypoallergenic mesh tape should be applied without tension.
• A strong zinc oxide tape should then be applied with a little tension to unload distressed tissues or to reposition structures, after which movement should be reassessed to evaluate the effect of the intervention.
• Further tapes may then be applied as necessary.
• The taping is maintained in position until the patient has learned to actively control movement in the desired fashion; or rehabilitation exercises have achieved the desired end of retraining functions or re-toning weakened musculature; or the effects on symptoms (such as pain reduction) are maintained when it is not worn, which may be a matter of hours or days. Morrissey (2001) suggests removal after 48 hours and reapplication if necessary.
Skin reactions
If a skin reaction develops this can be due to an allergic reaction, a ‘heat rash’ or because the tape is concentrating too much tension in one area. Heat rashes tend to be localized to the area under the tape and rapidly reduce. Allergic reactions are more irritating and widespread and should be treated with great caution as reapplication is likely to lead to a more severe reaction due to immune sensitization.
Box 13.10 Articulation/Mobilization of the Knee (Schiowitz 1991)
CAUTION: These articulation methods derive from osteopathic techniques and might be construed as manipulation in some states. Practitioners should ensure that their licensure allows them to perform these essentially safe mobilization techniques.
Schiowitz (1991) has detailed mobilization methods that derive from osteopathic joint mobilization methodology. He describes them as ‘myofascial ligament release techniques’ for treatment of somatic dysfunction of joints such as the knee, hip or ankle. They are essentially the same as many of the assessment methods described earlier in this chapter (and others), involving repetition and slightly greater force than would be used in assessment.
While largely ‘knee focused’, the first of the methods described involves the knee and the hip, as the movements used are compound. Schiowitz points out that:
Any of these methods can be modified by introducing isometric resistance to create myofascial relaxation. The joint is placed at its barrier of motion, then the patient actively attempts to reverse the motion against the isometric resistance supplied by the practitioner.
See Chapter 9 of this volume and Volume 1, Chapter 10 for descriptions of muscle energy techniques (MET).
CAUTION: None of these methods should be continued if pain is created by their performance, and none is meant to be used in the presence of acute dysfunction, active arthritic conditions, inflammation or where tissue damage (tears, etc.) is suspected.
Hip and knee mobilization
Specifically indicated if lateral knee structures are chronically shortened (e.g. IT band).
• The patient is supine and the practitioner stands ipsilaterally and facing the table.
• The patient’s knee and hip are flexed to 90° and the hip is abducted and externally rotated to a comfortable, painless, end-of-range position.
• The practitioner maintains the knee in its position by placing her cephalad hand onto its medial surface while at the same time, with the other (caudad) hand, she holds the distal tibial shaft, which she externally rotates to its pain-free end of range.
• These positions, in which hip and knee are held at their external rotation barriers, is held for 3–4 seconds before, ‘while maintaining pressure with both hands, the practitioner slowly returns the patient’s hip and knee to full extension on the table, releasing the pressure of both hands only at the last 5° of full extension’.
Knee mobilization
For enhancing flexion and extension of the knee utilizing anteroposterior glide. Ideal for knee restrictions that are not accompanied by any ligamentous laxity or internal damage.
• The patient is supine with hip and knee flexed to 90° and the practitioner stands ipsilaterally at the side of the table, facing the head.
• The patient’s ankle is tucked into, and held firmly by, the practitioner’s tableside axilla, while both her hands enfold the proximal tibia so that thumbs lie anteriorly and the fingers interlock in the popliteal space.
• The practitioner rocks forward slightly, increasing the degree of knee flexion slightly, while simultaneously gliding the tibia posteriorly with her thumbs.
• After a few seconds the practitioner rocks backward while simultaneously gliding the tibia anteriorly.
• The to and fro rocking motion is repeated three to four times, increasing the anterior and posterior slide motions each time’ (Schiowitz 1991).
Knee mobilization
For enhancing internal and external rotation of the knee. Ideal for knee restrictions that are not accompanied by any ligamentous laxity or internal damage.
• The patient lies supine with a pillow beneath the knee to create approximately 15° of flexion.
• The practitioner sits on the table ipsilaterally and distal to the knee, facing the head.
• The practitioner holds the patient’s ankle/lower shin firmly.
• The practitioner’s hands enfold the patient’s proximal tibia so that thumbs lie anteriorly and the fingers interlock in the popliteal space.
• The practitioner introduces anterior translation (glide) of the tibia on the femur and leans backward to apply traction.
• After a few seconds the traction and glide are slowly released as the practitioner rocks forward.
• The practitioner then introduces posterior glide of the tibia on the femur and again applies traction by leaning backward.
• This is released after a few seconds as the practitioner rocks forward.
• The practitioner introduces internal rotation of the tibia on the femur together with traction, then releases this and introduces external rotation of the tibia on the femur with traction and releases this.
• This sequence of anterior glide, posterior glide, internal and then external rotation, each accompanied by traction, is then repeated.
If there is a wish to add MET methodology to any of these mobilization sequences, the patient should be instructed to actively attempt to reverse the movement that the practitioner has introduced, utilizing no more than 20% of available strength, for 5–7 seconds, against resistance from the practitioner, after which the mobilization continues as described.
Lewit (1999) describes the ‘no man’s land’, which lies between neurology, orthopedics and rheumatology, which, he says, is the home of the vast majority of patients with pain derived from the locomotor system and in whom no definite pathomorphological changes are found. He makes the suggestion that these be termed cases of ‘functional pathology of the locomotor system’. These include most of the patients attending osteopathic, chiropractic, physiotherapy, and massage practitioners. The most frequent symptom of these individuals is pain, which may be reflected clinically by reflex changes, such as muscle spasm, myofascial trigger points, hyperalgesic skin zones, periosteal pain points or a wide variety of other sensitive areas that have no obvious pathological origin.
Moule (1991), describing his use of the European (Lief’s) version of NMT, suggests that:
A principle of NMT is that it is of prime importance to treat connective tissue lesions and abnormalities, prior to any manipulative treatment of the bony structures. If more orthodox and less penetrating soft tissue techniques are used, whilst the bony abnormality may be corrected by the application of a specific adjustment, because the soft tissues remain in a similar state to that existing prior to the manipulation, there is a strong likelihood of a recurrence of the lesion. NMT tends to dispense with specific [joint] adjustment, for, subsequent to using these specialised soft tissue measures [NMT], a generalised mobilisation will allow the muscular and connective tissues to encourage the bony structures to return to their normal alignment. This may take a little longer to produce relief from discomfort, but in the long run it means that the correction is more permanent, and there is less danger of any damage to the muscular and connective tissues from forceful manipulation.
Moule, who has successfully treated many of Europe’s leading sporting figures, continues:
One of the most common injuries one encounters is hamstring problems. These are particularly prevalent amongst footballers [soccer players], who in many cases develop the injury through overdevelopment of the quadriceps, without adequate attention to the maintenance and mobility (i.e. lengthening and stretching) of the hamstrings at the same time. The normal treatment of hamstring injuries is ultra-sonic and massage. [Results from] these techniques are not particularly rapid and the resultant loss of overall muscle tone, due to the inability of the leg to be used normally, retards a return to normal function. With NMT a lesion can be accurately and rapidly detected and, by the use of deep thumb manipulation, the soft tissue lesion can be dealt with rapidly and effectively. Where there is muscular fibre damage this can be felt and literally ‘ironed out’. The effect of the technique is to stimulate circulation in the area thus encouraging healing. Where there is inflammation and swelling the technique promotes drainage and the restoration of normal tone.…NMT is also beneficial in the treatment of knee lesions, particularly ligamentous problems and the subsequent inflammation in the joint itself. Correct application of NMT to these lesions will improve drainage from the knee and encourages healing to take place far more rapidly than through orthodox techniques. Where there is knee misalignments or dislocation, reduction of spasm is most important as a prerequisite to satisfactory manipulation of the joint. In many cases injury occurs when the legs become anchored due to studs in the boots. If rotation of the trunk is superimposed onto this static lower limb situation the stress imposed on the knee joint is enormous. The application of NMT prior to attempting correction not only makes this less painful, but ensures that the result is [likely to be] lasting.
NMT is also beneficial in the treatment of prepatellar bursitis, and synovial inflammatory problems.
The authors suggest that the same principles apply to the appropriate use of most soft tissue manipulation methods in treatment of joint dysfunction. The restoration of soft tissue integrity and balance should be a primary objective, whatever the etiology. (See Box 13.7 for details regarding fall-related injuries.)
Box 13.7 Fall-related injuries: age and severity
Falls are the leading cause of injury-related visits to emergency rooms in the United States and the primary etiology of accidental deaths in persons over the age of 65 years. The mortality rate for falls increases dramatically with age in both sexes and in all racial and ethnic groups, with falls accounting for 70% of accidental deaths in persons 75 years of age and older.
Falls can be markers of poor health and declining function, and they are often associated with significant morbidity. More than 90% of hip fractures occur as a result of falls, with most of these fractures occurring in persons over 70 years of age. One third of community-dwelling elderly persons and 60% of nursing home residents fall each year. Risk factors for falls in the elderly include increasing age, medication use, cognitive impairment and sensory deficits (Fuller 2000).
Orces (2009) reports that fall-related injuries among older adults are a major public health problem associated with considerable morbidity, mortality, and health care costs. 30% of people older than 65 years who live in the community fall each year; this proportion increases to 50% at 80 years of age. Although not all falls lead to injury, about 10% of falls result in a serious injury, such as a hip fracture, other serious soft-tissue injury, or head injury. Falls account for 10% of visits to the emergency rooms and 6% of urgent hospitalizations among older adults.
The CDC [http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html] has reported that:
• Women are 67% more likely than men to have a nonfatal fall injury.
• Rates of fall-related fractures among older adults are more than twice as high for women as for men (Stevens & Sogolow 2005).
• In 2003, about 72% of older adults admitted to the hospital for hip fractures were women.
• The risk of being seriously injured in a fall increases with age. In 2001, the rates of fall injuries for adults 85 and older were four to five times that of adults 65 to 74 (Stevens & Sogolow 2005).
• Nearly 85% of deaths from falls in 2004 were among people 75 and older.
• People 75 and older who fall are four to five times more likely to be admitted to a long-term care facility for a year or longer (Donald et al. 1999).
• After age 75, white men have the highest fatality rates, followed by white women, black men, and black women.
• White women have significantly higher rates of fall–related hip fractures than black women (Stevens & Sogolow 2005).
Prevention
A fact-sheet published by the Centers for Disease Control & Prevention [http://www.cdc.gov/HomeandRecreationalSafety/Falls/index.html] suggests that older adults can take several steps to protect their independence and reduce their risk of falling. They should – for example:
• Exercise regularly; exercise programs like Tai Chi that increase strength and improve balance are especially good.
• Ask their doctor or pharmacist to review their medicines – both prescription and over-the counter – to reduce side effects and interactions.
• Have their eyes checked by an eye doctor at least once a year.