Examination and testing for soft tissue damage to the knee
Physical examination of the injured knee (Levy 2001)
• The patient is supine on a treatment table, having already been observed standing and during demonstration of gait (see Chapter 3). The patient should be encouraged to relax as much as possible during palpation and other assessments of the dysfunctional knee joint.
• Both lower extremities are exposed from the groin to the toes and the symptomatic knee is compared with the contralateral knee.
• The uninjured knee should be examined first to provide baseline ‘normal’ values and for the patient to appreciate what examination of the injured knee involves.
• The knee should be observed and examined for edema, ecchymosis, erythema, effusion, patella location and size, and muscle mass, as well as evidence of local injury, such as contusions or lacerations.
• A normal knee should demonstrate a hollow on either side of the patella and should be slightly indented just above the patella. If there is swelling, these gaps will be filled in.
• With more severe effusion the region superior to the patella will swell as this is where the joint cavity is most spacious.
• The position of the patella should be confirmed. If the patella is superiorly displaced this may result from damage to the patellar ligament. If the patella is inferiorly displaced this may be a result of damage to the quadriceps tendon.
• The Q-angle should be measured, as described previously, by drawing a line from the tibial tubercle through, and extending past, the center of the patella and then from the center of the patella to the ASIS (Fig. 13.23). If the angle exceeds 10°–15° the patella is likely to be more vulnerable to subluxation or dislocation, or to excessive wear on its posterior surfaces. It has been suggested that women are likely to have a higher Q-angle due to a wider pelvis and other structural differences. However, it remains debatable that any gender differences add to this problem. Likewise, a normal Q-angle will not ensure an absence of problems. (Levangie & Norkin 2005)
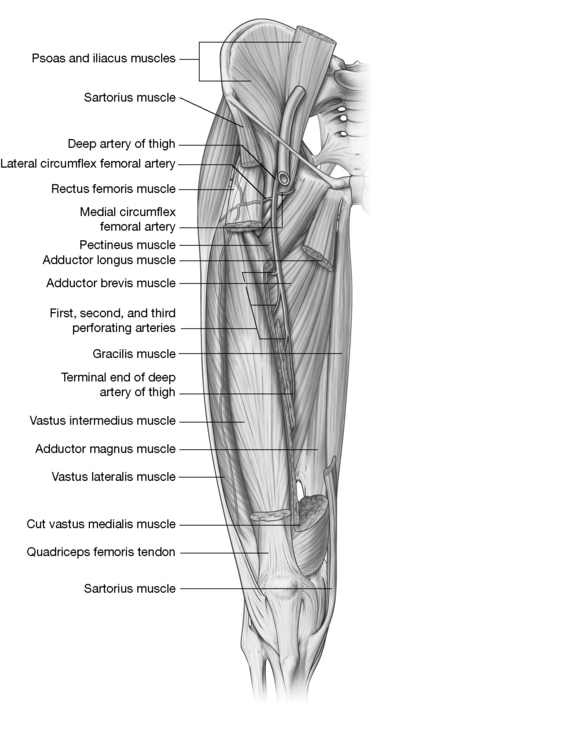
• The quadriceps should be evaluated for atrophy, which, if present, suggests a long-standing or preexisting disorder.
• Atrophy of the vastus medialis muscle may be the result of previous surgery to the knee.
• The patient should move into a prone position and the popliteal fossa should be inspected and palpated. Only the popliteal artery should be palpable. Any abnormal bulges in the artery may involve an aneurysm or thrombophlebitis.
• Cyriax (1982) noted that if the knee joint capsule is damaged there will be gross limitation of flexion, with only slight extension limitation, and that in the early stages, rotation movements remain painless and full.
Palpation of the injured knee
• With the patient supine, the knee should be palpated in slight flexion (with a small pillow under the popliteal fossa).
• Tenderness localized to the joint line suggests a meniscal tear.
• In the case of a torn medial meniscus there will be very localized sensitivity along the medial aspect of the joint, which increases when the tibia is internally rotated and extended.
• If the MCL is damaged, tenderness may be noted along its entire course, from its origin on the medial femoral condyle to its tibial insertion.
• Palpation of MCL is easier if the knee of the supine patient is slightly flexed.
• If there is only localized tenderness at the MCL origin or insertion, an avulsion-type fracture may be the cause.
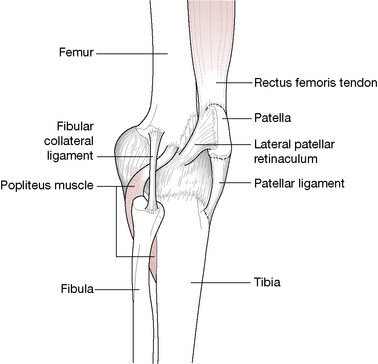
• If the LCL is injured tenderness may be noted from its attachment on the lateral femoral epicondyle to its insertion on the fibular head.
• The anterior aspects of both thighs should be examined and palpated, particularly noting any muscle wasting. If, just proximal to the tibia, there is a transverse tract that is more pliable than the surrounding musculature this may indicate a ruptured quadriceps.
• Inflammation resulting in tenderness, edema and warmth should be palpated for, including the clinically significant prepatellar, infrapatellar and pes anserine bursae, which are situated on the anterior aspect of the knee joint.
• Osgood–Schlatter syndrome is characterized by tenderness and edema at the site where the patellar ligament inserts into the tibial tubercle.
Range of motion testing
• The knee should be evaluated for active flexion and extension.
• If there is difficulty extending the knee there is probably dysfunction associated with the extensor mechanism. However, it should be noted that if there is evidence of significant effusion, this may be preventing normal extension of the knee joint. Hypertonic posterior musculature (hamstrings and popliteus, in particular) can also reduce extension range and quadriceps can reduce flexion range.
• Petty (2006) offers guidelines for evaluating active and passive ranges of movement, suggesting that the following features should be noted: quality, range, pain behavior, resistance during performance of the movement, as well as any provocation of muscle spasm that may occur.
Effusion ‘tap’ test
Toghill (1991) describes assessment for the presence of effusion within the joint capsule, which may not be obvious if it is only slight.
• Normally there is a hollow on the anteromedial aspect of the knee, behind the patella and anterior to the femoral condyle.
• An effusion will commonly fill this space but a slight swelling may not be obvious.
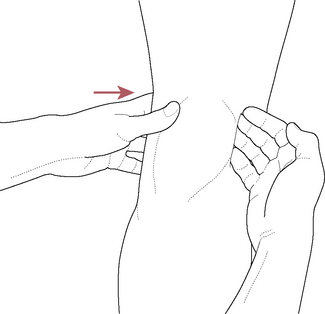
• Light massage is applied to the area to drain any fluid into the synovial cavity and a smart ‘tap’ (‘slap’) is then applied with the flat of the fingers, to the lateral aspect of the knee.
• If there is effusion the hollow on the medial aspect of the joint will rapidly fill.
Active physiological movement (including overpressure)
• With the patient supine both sides are tested for flexion, extension, hyperextension, medial and lateral rotation.
• In each case the patient initiates the movements and the practitioner takes the movement slightly beyond the endpoint of each movement to assess end-feel as well as any symptoms that may emerge (see Box 13.8).
• As with all joint assessments, active movements are likely to yield more accurate ‘real-life’ information if they approximate the sorts of activities involved in daily living. For this reason movements should be repeated a number of times and the speed with which they are performed should be modified (slowly, quickly, very slowly, etc.). Compound movements should be attempted, say involving a joint flexing, extending and rotating in sequence, and end-of-range movements should be sustained to evaluate the effects of fatigue, and differentiation tests should be used where possible.
• Differentiation tests attempt to screen out the component elements of a compound movement. Petty (2006) offer examples. ‘When knee flexion in prone reproduces the patient’s posterior knee pain, differentiation between knee joint, anterior thigh muscles and neural tissues may be required. Adding a compression force through the leg will stress the knee joint, without particularly altering the muscle length or neural tissue. If the symptoms are increased, this would suggest that the knee joint (patellofemoral or tibiofemoral joints) may be the source of symptoms’.
Passive physiological movement
The identical movements tested actively should also be assessed passively. Additional movements, which cannot be self-performed and which should be evaluated passively, include flexion and abduction/adduction of the tibia (producing, respectively, valgus and varus strains), extension.
As Cyriax (1982) notes, passive testing also offers the opportunity to differentiate between problems that largely involve contractile or non-contractile tissues.
• If there is pain or restriction on both active and passive movements in the same direction (e.g. active and passive flexion), the condition involves non-contractile tissues.
• If there is pain or restriction when active and passive movements in opposite directions are performed (e.g. active flexion and passive extension), the condition involves contractile tissues.
Stress testing of the knee joint
CAUTION: Stress forces should involve gentle, firm pressure, rather than sudden forces, which may cause reflexive contraction of associated muscles.
When assessing the joint itself:
• excessive joint motion (laxity) suggests an injury
• a soft endpoint as compared with a healthy, firmer endpoint suggests ligament damage.
• the quality of translation (glide, joint play), when the injured knee is compared to the unaffected side, can be significant, with differences in the feel of side-to-side movement being of greater significance than the actual degree of motion.
The MCL and the LCL are assessed by applying valgus and varus stress to the knee in 30° of flexion and in full extension.
Note: Following the testing procedures below, as pressure is released a ‘clunking’ sensation may be noted, especially if laxity is a feature, and the patient should be forewarned.
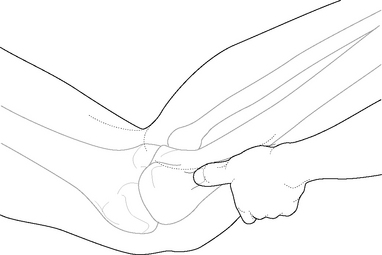
Assessing for MCL damage (abduction stress test)
• The patient lies supine with the leg to be tested lying at the edge of the table.
• The lower extremity is abducted so that the leg is eased off the edge of the table, with the knee placed in 30° of flexion and the foot supported by the practitioner.
• Valgus stress is applied by pressing medially on the lateral aspect of the knee with the thumb of one hand, while the fingers of the same hand palpate the medial aspect of the joint. The second hand directs the ankle laterally, effectively ‘opening’ the medial aspect of the knee joint.
• If a significant degree of gapping of the medial aspect of the knee joint occurs this suggests impairment of the MCL (Levy 2001).
• Comparison of the degree of gapping should be made between the affected and non-affected knees.
• If the knee is placed in extension and there is increased medial joint laxity when an abduction (valgus) force is applied to the leg, there may be additional (to MCL damage) involvement of posterior structures, such as the posterior joint capsule, posterior oblique ligament, posteromedial capsule and/or the PCL (Fig. 13.24).

Figure 13.24 Abduction stress test. The left hand stabilizes the thigh while the right hand applies the abduction force
(adapted from Petty & Moore 1998).
• Mennell (1964) points out that if the knee is in full extension, it is impossible to tilt the joint open medially, when the medial collateral ligament is intact.
• Equally, if the vastus medialis muscle is weakened for some reason, the quadriceps mechanism that locks the joint is impaired and an abnormal degree of side tilting medially may occur.
• Mennell further suggests just ‘two or three degrees of flexion’ for testing regular joint play, when ligament status is not specifically being evaluated (See Box 13.9).
Box 13.9 Joint play for assessment and treatment of the knee
Mennell (1964) and Kaltenborn (1985) pioneered the concept of evaluating and working with those aspects of joint movement that are outside voluntary control-joint play. The various stress tests and drawer tests as described in this chapter all utilize joint play in their methodology, since none of the movements that take place in these tests is under voluntary control.
As Mennell (1964) states:
The movements of joint play are known to all in that they are used to test the ligamentous and muscular stability of the joint. But if the joint is unstable, the movements are exaggerated. The importance of the normal degree of movement in each test remains unrecognized.
This statement may be challenged since his and Kaltenborn’s work has created a generation of therapists and practitioners who do now recognize the importance of ‘normal degrees of movement’ when assessing joints. There remains a concern that, since most of the individuals seen and handled by practitioners have joints that are to some extent ‘dysfunctional’, the opportunity to evaluate normal healthy tissues and joints is far exceeded by the opportunity to evaluate dysfunctional tissues and joints. Without something with which to compare what is being evaluated, a decision as to what is ‘normal’ and what is other than ‘normal’ may be inaccurate. Even provision of normal ranges of motion with which to compare a patient’s range may be inappropriate. Body type and size, age and inborn degrees of flexibility or inflexibility may all confound and confuse a comparison with ‘normal ranges’ of any given movement pattern.
Mennell (1964) describes assessment of the rotational range of joint play in the knee, in which the range of play of the tibial condyles on the stabilized femoral condyles is examined.
• The supine patient’s hip and knee are flexed to 90° and ‘the examiner grasps the thigh anteriorly over the femoral condyles with one hand, and with the other grasps the calcaneus, from beneath the heel, keeping the forearm in line with the lower leg. The practitioner then alternately supinates and pronates the forearm, rotating the tibial condyles clockwise and anticlockwise’.
• Mennell notes that maximal joint play rotation occurs in mid-flexion (as described above) and that ‘there is no rotation of the tibial condyles with the knee in full extension because of the locking mechanism of the quadriceps’.
• Rotation elicited in full extension might mean impairment of quadriceps function, or intraarticular or ligamentous dysfunction.
Lewit (1999) uses joint play therapeutically, as well as for assessment, and suggests that:
The knee joint can be treated first by joint (dis)traction techniques. The simplest is to lay the patient prone on a mat on the floor, the knee bent at right angles. The therapist (standing) puts one foot [having removed the shoe] on the thigh just above the knee and grasps the leg with both hands round the ankle, pulling it in a vertical direction.
As in most joint play methods this is performed slowly and depends on an accurate removal of the soft tissue slack, so that minute degrees of joint play movement can be introduced, encouraging the surfaces of the joints to glide on each other.
The advantage of such distraction methods is that joint play is likely to be increased markedly and with it, active ranges of movement as well.
No pain should be engendered by this approach, either during or after its performance.
Assessing for LCL damage (adduction stress test)
• In order to test for lateral knee joint stability the hand positions should be reversed.
• Varus stress is applied by pressing on the medial aspect of the knee joint (while it is in 30° of flexion) with one hand, while directing the leg (held in slight external rotation) medially with the other, effectively opening the lateral aspect of the knee joint.
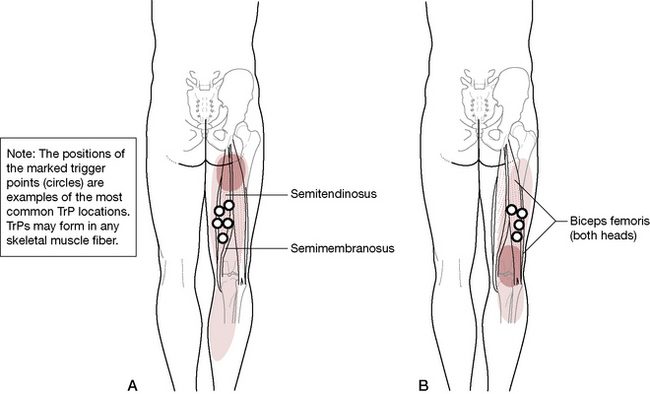
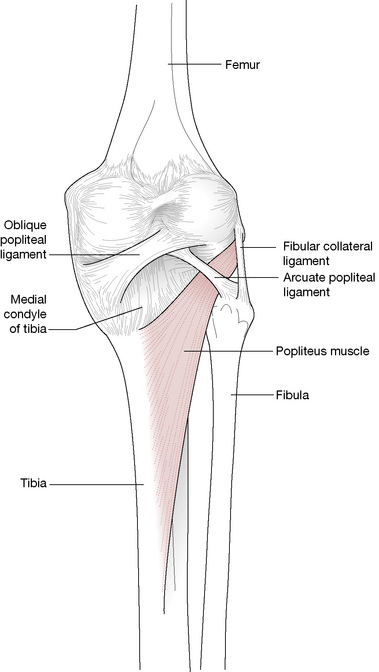
• If a significant degree of gapping of the lateral aspect of the knee joint occurs this suggests impairment of the LCL and possibly also the arcuate-popliteus complex, the posterolateral joint capsule, the iliotibial band and the biceps femoris tendon (Petty 2006).
• Comparison of the degree of gapping should be made between the affected and non-affected knees.
• Mennell (1964) points out that if the knee is in full extension, it is impossible to tilt the joint open laterally if the lateral collateral ligament is intact.
• Mennell further suggests using just ‘two or three degrees of flexion’ for testing regular joint play when ligament status is not specifically being evaluated. ‘Because the knee joint is unlocked by minimal flexion, this tilting open of the lateral joint space is the extent of normal [joint play] movement and has nothing to do with determination of the integrity of the LCL.’
The Lachman maneuver (to confirm ACL integrity)
• The patient lies supine with the knee flexed to 20–30°, draped over the practitioner’s knee (which has been placed onto the table).
• Posteriorly directed pressure on the patient’s femur should be applied with one hand, while the other hand attempts to move the proximal tibia anteriorly, testing the degree of joint play.
• An excessive degree of forward motion of the tibia, without a firm endpoint (i.e. soft end-feel), suggests ACL damage (compare both knees).
• This test also assesses the arcuate-popliteus complex and the posterior oblique ligament.
Anterior drawer test (to evaluate soundness of ACL)
• The patient lies supine with the hip flexed to 45° and the knee to 90°, so that the patient’s foot rests firmly on the examination table.
• The practitioner sits on the dorsum of the foot, placing both hands behind the knee and onto the proximal leg. The thumbs rest over the anterior surface of the joint line to palpate for movement.
• Once the hamstrings seem to be relaxed, a gentle force is applied to ease the proximal leg anteriorly, evaluating joint play between the tibial condyles and the femoral condyles.
• A ‘mushy’ or soft end feel, pain, and/or anterior movement of the tibia is considered positive. False negatives are common, usually due to hamstring spasms, which can prevent the forward translation of the proximal tibia (Lowe 2006)
• This ‘anterior drawer test’ is said to be less sensitive for ACL damage than the Lachman maneuver (Levy 2001). As in that test, an excessive degree of forward motion of the tibia, without a firm endpoint, suggests ACL damage (compare both knees).
• Additionally this test evaluates the posterolateral joint capsule, the MCL and the IT band.
Posterior drawer test (to evaluate soundness of PCL)
• The patient lies supine with the hip flexed to 45° and the knee to 90°, so that the patient’s foot rests firmly on the examination table (Fig. 13.25).

Figure 13.25 Posterior drawer test. The practitioner stabilizes the patient’s foot by sitting lightly on it. An anteroposterior force is applied to the tibia
(adapted from Petty & Moore 1998).
• The practitioner sits (lightly) on the dorsum of the foot and places both hands behind the knee, with thumbs wrapping to the front of the tibia.
• Once the hamstrings seem to be relaxed, a gentle force is applied to ease the proximal leg posteriorly, evaluating joint play between the tibial condyles and the femoral condyles.
• Instability arising from PCL injury manifests as an abnormal increase in posterior tibial translation.
• If there is confusion when trying to distinguish whether abnormal translation of the tibia on the femur originates from excessive ACL or PCL laxity, the tibial sag test should be utilized.
Tibial sag test (to confirm PCL instability)
• The supine patient’s hips and knees are both flexed to 90° and the patient’s heels are supported by the practitioner.
• In this position, the PCL impaired knee will clearly sag backward (tibia ‘falls’ toward the floor in this position) from the effects of gravity (also known as the Godfrey sign) (Levy 2001).
Pivot shift test (to confirm posterolateral capsular damage and/or injury to the ACL, arcuate-popliteus complex and IT band)
• If the ACL is impaired, the tibia tends to subluxate anteriorly during knee extension.
• The supine patient is lying with knee extended. In order to create a valgus stress a moderate degree of pressure should be applied on the lateral aspect of the knee, directed medially, while the knee is being actively flexed (with the leg held in medial rotation).
• As the knee joint approaches 20–40° of flexion, a sudden jerking movement will occur if the ACL is impaired (Fig. 13.26).
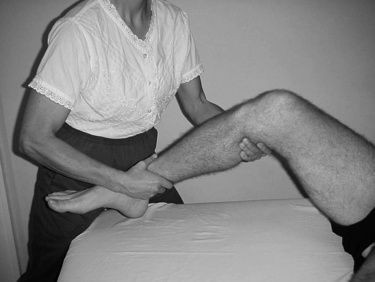
Figure 13.26 Lateral pivot shift. The practitioner applies abduction stress to the leg while moving the knee from extension to flexion while the leg is maintained in medial rotation
(adapted from Petty & Moore 1998).
McMurray tests (to confirm meniscal disorders)
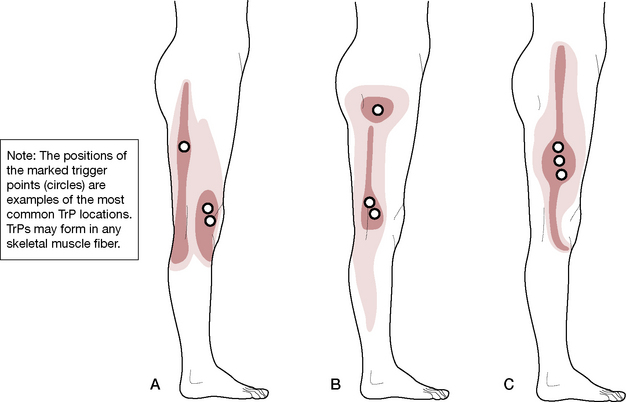
Medial meniscus (Fig. 13.27)
• The patient lies supine with the affected knee in maximum flexion.
• The posteromedial margin is palpated with one hand while the foot is supported by the other hand.
• The leg is externally (laterally) rotated as far as possible, while at the same time the tibia is abducted, thereby creating a valgus strain. While holding these positions, the knee joint is slowly extended.
• In the case of a tear involving the medial meniscus, ‘an audible, palpable, and painful movement’ occurs at the moment that the femur passes over the damaged portion of the meniscus (Levy 2001).
Lateral meniscus
• In order to evaluate the lateral meniscus, a similar method is repeated but this time, as the leg is supported at the foot by one hand, the other hand should be placed over the posterolateral aspect of the knee joint, at which time maximal pain-free internal rotation of the leg should be introduced.
• The tibia is then placed into adduction, creating a varus strain, as the leg is slowly extended.
• In the case of a tear involving the lateral meniscus, ‘an audible, palpable, and painful movement’ occurs at the moment that the femur passes over the damaged portion of the meniscus.
• Levy (2001) warns: ‘Clicks unassociated with pain or joint-line tenderness, especially during lateral meniscus testing, may represent a normal variant and should not be interpreted as evidence of a meniscal tear’.
Further tests for meniscal and ligamentous damage include:
• Apley’s compression test, during which the prone patient’s knee is taken to 90° of flexion. The practitioner stabilizes the thigh and at the same time applies compression to the menisci through the long axis of the femur, via pressure on the heel. The tibia is slowly rotated medially and laterally while compression is maintained. Pain noted during rotation of the tibia, either medially or laterally, implicates the meniscus on that side
• Apley’s compression test, during which precisely the same positioning is maintained, with distraction rather than compression being introduced, as medial and lateral tibial rotation is applied. Pain resulting from this procedure suggests medial or lateral ligamentous dysfunction.
Compression mobilization in rehabilitation after knee surgery
Noel et al (2000) suggest that because cyclical loading of the knee joint, during normal use, stimulates ‘bio-synthetic activity of the chondrocytes’, addition of compression to joint mobilization after surgery should assist in joint repair.
In order to assess the validity of this approach, half of a group of 30 patients were treated, as part of standard rehabilitation physical therapy after intraarticular reconstructive surgery of the ACL, by the addition of compressive force during movement of the knee from end of range of motion (flexion) into the range of motion. This was performed in four series of approximately 20 repetitions daily. Initially, the flexion range of motion (FROM) was measured using a goniometer. The group who received compression with range of motion exercise achieved a FROM of 130° within an average of six treatments, compared with 11 treatments for those who did not have compression added.
• The patient lies prone with a small pad/sandbag under the knee, proximal to the patella.
• The practitioner takes the knee into flexion, carefully establishing the pain-free end of range.
• The practitioner then progressively exerts long axis compression from the calcaneum toward the knee.
• The degree of pressure exerted is the maximum possible without causing pain.
• Maintaining this degree of compression, the practitioner passively eases the knee toward extension over a range of 10–15°.
• The compression is released and the range reassessed and held at the maximal limit of pain-free flexion, as the procedure is repeated.
• In between each series of 20 repetitions, several slow passive movements of the knee through its entire range are performed.
CAUTION: The researchers report: ‘All patients receiving mobilizations with compression described the first session as “very unpleasant” or even painful. When pain was experienced, it was located in the knee fold and/or around the incision at the ligamentum patella. The pain was felt in the extreme flexion position only, and disappeared as soon as mobilization toward extension was started, indicating that the pain was not due to compression…. The unpleasant sensation decreased at the end of each session and from session to session.’
The researchers report thatVan Wingerden (1995)‘relates the pain to a decrease of the gliding properties of the femur on the menisci following the alteration of lubrication after a surgical procedure’.
This caution emphasizes the need to avoid taking the flexed knee beyond a tolerable end range and to advise the patient to anticipate discomfort, which will most probably rapidly diminish and which is not a result of damage to the knee but rather of the distressed and unlubricated tissues being taken into a slight stretch.
Patellar apprehension test
The supine patient’s leg is held and supported in 30° of flexion at the knee. A firm, laterally directed force is applied against the medial aspect of the patella. The test is positive if there is excessive patella movement and/or if the patient displays anxiety (apprehension) and attempts to protect the knee from this pressure. This suggests a patellar subluxation or dislocation.
Additionally it is necessary, as in all other joint areas, to examine the muscular component.
• The relative strength of the phasic muscles should be tested, for example the quadriceps (apart from rectus femoris) and particularly VMO.
• Shortness should be tested for in the regions of postural muscles, for example hamstrings, rectus femoris and TFL/iliotibial band (Liebenson 1996).
See individual muscles for details of appropriate strength or shortness tests, which are described where appropriate.
Positional release methods for knee damage and injury involving ligaments and tendons
PRT for patellar tendon dysfunction
• Tender points related to dysfunction involving the patellar tendon are located close to the apex of the patella, on one or both sides, or in the center of the tendon.
• Digital pressure, applied medially or laterally, or by means of compression between finger and thumb helps to localize the most sensitive area on the tendon.
• The discomfort created in the most sensitive point is registered by the patient as a pain score of ‘10’.
• The patient lies supine with the leg to be treated straight, as the practitioner, standing the alongside the knee, maintains direct pressure onto the tender point with her caudad hand.
• The knee should be in extension with the lower calf supported on a small cushion or rolled-up towel, to create slight hyperextension of the knee.
• The patient reports on changes in perceived discomfort as the practitioner places her cephalad hand just proximal to the patella, easing the patella caudad while at the same time creating medial rotation of the leg. The combination of mild hyperextension of the knee, medial rotation of the tibia and caudad depression of the patella should reduce the perceived discomfort to a score of ‘3’ or less (without additional pain elsewhere).
• This final position of ease (for the tendon) is held for 90 seconds before slowly releasing.
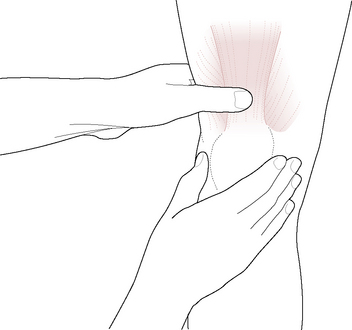
PRT for MCL dysfunction (Fig. 13.28)
• The tender point relating to MCL dysfunction is found on the medial surface of the knee, usually on the anterior aspect of the ligament.
• The patient is supine with the affected leg at the edge of the table.
• The practitioner stands or sits alongside facing the table, cephalad hand enfolding the posterior aspect of the knee, so that the index or middle finger presses onto the tender point on the medial knee.
• The practitioner’s caudad hand supports the foot as the lower extremity is abducted off the table and flexed at the knee to approximately 40° or until some reduction is reported in the tenderness in the palpated point.
• The flexed knee is held in place as, using the caudad hand, fine tuning is introduced involving internal rotation, as well as slight adduction, of the tibia (a varus force).
• Additional ease of discomfort may be achieved by means of mild long-axis compression, from the foot toward the knee.
• Once reported discomfort in the tender point has reduced from ‘10’ to ‘3’, or less (without additional pain elsewhere), the final position of ease is held for at least 90 seconds before a slow return to neutral.
PRT for LCL dysfunction
• The tender point relating to LCL dysfunction is found on the lateral surface of the knee, usually on the anterior aspect of the ligament.
• The patient is supine with the affected leg at the edge of the table.
• The practitioner stands or sits alongside facing the table, cephalad hand enfolding the posterior aspect of the knee, so that the thumb presses onto the tender point on the lateral knee.
• The practitioner’s caudad hand supports the foot as the lower extremity is abducted off the table and flexed at the knee to approximately 40° or until some reduction is reported in the tenderness in the palpated point.
• The flexed knee of the abducted lower extremity is held in place as, using the caudad hand, fine tuning is introduced, involving external (rarely internal) rotation of the tibia, as well as slight abduction of the tibia (a valgus force).
• Very rarely ease may be enhanced by an adduction rather than an abduction of the tibia.
• Additional ease of discomfort may be achieved by means of mild long-axis compression, from the foot toward the knee.
• Once reported discomfort in the tender point has reduced from ‘10’ to ‘3’, or less (without additional pain elsewhere), the final position of ease is held for at least 90 seconds before a slow return to neutral.
PRT for PCL dysfunction
• The tender point for PCL dysfunction is located at the very center of the popliteal space. Care should be taken to avoid compressing the popliteal artery.
• The patient lies supine and the practitioner stands ipsilaterally facing cephalad, with the index or middle finger of her non-tableside hand in contact with the tender point.
• A rolled towel is placed just distal to the popliteal space, supporting the proximal tibia. This placement should reduce reported tender point discomfort slightly.
• Using her tableside hand, the practitioner introduces internal rotation of the tibia, until a further reduction in tenderness in the palpated point is reported. The leg is left in the degree of internal rotation of the tibia that provides the greatest reduction in reported pain.
• The practitioner then places her hand on the distal thigh, just superior to the patella, and introduces a posteriorly directed force (slightly hyperextending the knee) as the patient reports on changes in perceived pain in the tender point.
• Once reported discomfort in the tender point has reduced from ‘10’ to ‘3’, or less (without additional pain elsewhere), the final position of ease is held for at least 90 seconds before a slow return to neutral.
PRT for ACL dysfunction (Fig. 13.29)
• There are ACL tender points on both the anterior and posterior surfaces of the knee.
• The posterior points will be used and treated in this description. These lie in the medial and lateral quadrants of the superior popliteal space.
• The patient lies supine and the practitioner stands ipsilaterally facing cephalad, with the index or middle finger of her non-tableside hand in contact with one of the ACL tender points in the superior popliteal space.
• A rolled towel is placed just proximal to the popliteal space, supporting the distal femur. This placement should reduce reported tender point discomfort slightly.
• Using her tableside hand the practitioner introduces internal rotation of the tibia, until a further reduction in tenderness in the palpated point is reported. The leg is left in the degree of internal rotation of the tibia that provides the greatest reduction in reported pain.
• The practitioner then places her hand on the proximal tibia, just inferior to the patella, and introduces a posteriorly directed force (slightly hyperextending the knee) as the patient reports on changes in perceived pain in the tender point.
• Once reported discomfort in the tender point has reduced from ‘10’ to ‘3’, or less (without additional pain elsewhere), the final position of ease is held for at least 90 seconds before a slow return to neutral.