CHAPTER 43 Persons with Diabetes Mellitus
Diabetes mellitus, one of the most widespread diseases, affects approximately 21 million people, about 7% of the population. Of these, approximately 6.2 million are undiagnosed. These numbers are increasing substantially with increasing obesity. As many as one in three people born in 2000 will develop diabetes.1 Individuals with diabetes face shortened life spans and the probability of developing acute and chronic health complications. Only heart disease and cancer kill more Americans than diabetes and its complications.
Diabetes mellitus is actually a group of disorders characterized by hyperglycemia (abnormally increased blood glucose) resulting from defective insulin secretion or defective insulin action or a combination of both. Chronic hyperglycemia damages eyes, kidneys, nerves (neuropathy), heart, and blood vessels (microangiopathy). The dental hygienist plays a key role on managing oral disease in persons with diabetes (Box 43-1).
CLASSIFICATION OF DIABETES (TABLE 43-1 and BOX 43-2)
Four major clinical types of diabetes mellitus are as follows2:
TABLE 43-1 Characteristics of Type 1 and Type 2 Diabetes Mellitus
| Factor | Type 1 | Type 2 |
|---|---|---|
| Age at onset | Usually young, but may occur at any age | Usually in persons older than 40 years of age but may occur at any age |
| Type of onset | Usually abrupt | Insidious |
| Genetic susceptibility | HLA-related DR3, DR4, and others | Frequent genetic background; not HLA-related |
| Environmental factors | Virus, toxins, autoimmune stimulation | Obesity, poor nutrition |
| Islet-cell antibody | Present at outset | Not observed |
| Endogenous insulin | Minimal or absent | Stimulated response is (1) adequate but with delayed secretion, or (2) reduced but not absent |
| Nutritional status | Thin, catabolic state | Obese or may be normal |
| Symptoms | Thirst, polyuria, polyphagia, fatigue | Frequently none, or mild |
| Ketosis | Prone, at onset or during insulin deficiency | Resistant, except during infection or stress |
| Control of diabetes | Often difficult, with wide glucose fluctuation | Variable, helped by dietary adherence |
| Dietary management | Essential | Essential, may suffice for glycemic control |
| Insulin | Required for all | Required for about 40% |
| Sulfonylurea | Not efficacious | Efficacious |
| Vascular and neurologic complications | Seen in majority after 5 or more years of diabetes | Frequent |
HLA, Human leukocyte antigen.
Type 1 (Insulin Deficient)
Type 1 diabetes mellitus, which involves about 5% to 10% of the diabetic population, commonly occurs in childhood and adolescence but can strike at any age. Individuals who develop type 1 diabetes mellitus are rarely obese. An absolute deficiency of insulin secretion is characteristic in this type, and treatment requires regular lifelong administration of insulin by injection to prevent ketosis and sustain health. The disease results from destruction of the beta cells of the pancreas with abrupt symptoms in children and slow onset in adults. Genetic predisposition related to the presence of certain human leukocyte antigens (HLAs) that influence immune activity directed against islet cells is essential for type 1 diabetes. Research studies suggest a genetic origin associated with type 1 and type 2 diabetes. The role of genetics is weaker in type 1 diabetes than in type 2 diabetes. Environmental factors, still poorly defined, are postulated to play a causative role in genetically predisposed individuals. Autoimmune reaction and environmental factors, such as viral infection, have been demonstrated in research. Twin studies reveal that if one twin develops type 1 diabetes, the other twin will develop the disease in approximately 50% of cases.3
Type 2 (Insulin Resistant)
Type 2 diabetes mellitus is recognized as a heterogeneous disorder that results from insulin resistance and insulin secretory defect. Most individuals with type 2 diabetes are obese, and obesity itself causes some degree of insulin resistance. Individuals who are not obese by traditional weight criteria may have an increased percentage of body fat distributed in the abdominal region. People with type 2 diabetes constitute approximately 90% to 95% of the diabetic population. Of the undiagnosed the vast majority have type 2 diabetes. Risk of developing type 2 diabetes increases with obesity, age, lack of physical activity, history of GDM, hypertension, and dyslipidemia (abnormal amounts of blood lipids). Frequency of type 2 diabetes varies with racial and ethnic groups. Ketoacidosis seldom occurs in type 2 diabetes, but when present, it is associated with infection. Type 2 diabetes usually goes undiagnosed for years because hyperglycemia develops gradually without classic symptoms. Nevertheless, risk of developing macrovascular and microvascular complications (problems in the large and small blood vessels) is high. Symptoms may be gradual, and weight loss is uncommon (Table 43-2).
TABLE 43-2 Complications of Diabetes Mellitus
| Affected Area | Complications |
|---|---|
| Eyes | |
| Kidneys | |
| Mouth | |
| Reproductive system | |
| Skin | |
| Vascular system | |
| Peripheral nerves |
Persons with type 2 diabetes often respond to weight reduction, dietary management, exercise, and oral hypoglycemic medications. Persons with type 2 diabetes may require insulin therapy to achieve good control or during illness, which is an important distinction between insulin-dependent and insulin-treated individuals.
Predominantly, type 2 diabetes is genetically inherited and has no association with autoimmune beta-cell destruction. In studies, if one twin develops type 2 diabetes the other twin has a 100% chance of developing the disease.3 Obesity has a major role in the development of type 2 diabetes, but more research is needed.
Gestational Diabetes Mellitus
Gestational diabetes mellitus occurs in 4% of pregnancies in the United States4 and represents 90% of all pregnancies complicated by diabetes. Clinical characteristics include glucose intolerance that has its onset or recognition during pregnancy. Therefore diabetic women who become pregnant are not in the GDM classification. High-risk individuals include women with the following conditions:
Even in the nondiabetic individual, normal pregnancy affects both fetal and maternal metabolism and exerts a diabetogenic effect. GDM generally reverts following birth because the condition is a consequence of the normal anti-insulin effects of pregnancy hormones and diversion of natural glucose to the fetus.
GDM increases risk of perinatal morbidity and mortality. Maternal complications include increased rate of cesarean delivery and chronic hypertension. Furthermore, women with a history of GDM are at increased risk for developing diabetes 5 to 10 years later. Six weeks or more after pregnancy ends, the woman with GDM should be reclassified as having one of the following:
Other Specific Types of Diabetes Mellitus
The category of other specific types of diabetes mellitus is heterogeneous in nature and includes diabetes in which the causative relationship is known, such as diabetes mellitus associated with certain conditions and syndromes (e.g., genetic defects of the beta cells, pancreatic disease, endocrine disease, chemical-induced agents, and genetic syndromes). In other diabetic disorders such as genetic syndromes associated with glucose intolerance, a causative relationship is suspected. Rare and highly specific causes of diabetes and insulin resistance include defects in insulin receptors located on the cell membrane and conditions such as systemic lupus erythematosus in which insulin-receptor antibodies may develop. In addition to the presence of the specific condition or syndrome, diabetes mellitus also is present.
Prediabetes
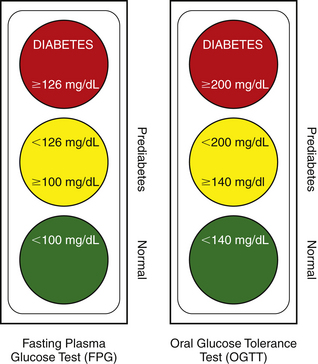
The designations impaired glucose tolerance and impaired fasting glucose (IFG) are metabolic stages intermediate between normal glucose homeostasis and diabetes. IGT and IFG have been officially termed prediabetes and designated as risk factors for future diabetes and cardiovascular disease (CVD). Individuals at high risk for developing diabetes can be given a wide variety of interventions that can delay, and sometimes prevent diabetes onset. IGT can be determined only by an oral glucose tolerance test (OGTT) consisting of a standard glucose challenge followed 2 hours later by measurement of venous plasma glucose concentration. IFG is determined by a fasting plasma glucose test. Disease management includes dietary control of obesity, treatment of hypertension and hyperlipidemia (high amounts of fat in the blood), and elimination of smoking, if the individual smokes (Figure 43-1 and see Box 43-2).
PATHOPHYSIOLOGY OF DIABETES
To use glucose, the body must produce insulin. A person with diabetes produces too little insulin or has an inability to use insulin. Insulin, an anabolic hormone (used to build up the body), stimulates entry of glucose into the cell and enhances fat storage. The presence of insulin, therefore, prevents the body from breaking down fat. Without insulin, glucose remains in the bloodstream (hyperglycemia) rather than being stored or used by cells to produce energy.
Insulin Deprivation
The net effect of insulin deficiency is that blood glucose concentration rises (hyperglycemia). Without insulin, the glucose derived from a meal cannot be used or stored. When the blood glucose level rises >150 mg/dL, the kidney tubules become incapable of resorption. Glucose appears in the urine (glucosuria), taking with it a large amount of fluid, thus raising the volume of urine (polyuria) and necessitating frequent urination. Dehydration follows, leading to excessive thirst (polydipsia). Ketoacidosis may follow hyperglycemia when blood glucose levels rise to >400 mg/dL (Box 43-3). Impaired carbohydrate metabolism, which the body interprets as energy starvation, causes excessive ingestion of food (polyphagia) and necessitates use of fats and proteins (hyperglycemia progressively glycates body proteins) to satisfy energy requirements. Ketoacids and ketone bodies (acetone) are produced as a result of catabolism of fatty acids (lipolysis). Ketones accumulate in the tissues, are excreted in the urine (ketonuria), and circulate in the blood (ketonemia), causing a drop in the pH of the blood and leading to diabetic coma.
Clinical Signs and Symptoms
Diabetes is characterized by hyperglycemia. In type 1 diabetes mellitus, the predominant problem is impaired insulin production, whereas in type 2 diabetes mellitus the predominant problem is the inability to use the insulin produced by the body. A considerable overlap exists, however, in clinical features of the two forms of diabetes. The deficiency of insulin action leads to derangements of the intermediary metabolism of carbohydrates, protein, and lipids. In clinical practice the suspicion of diabetes is gleaned from history and physical findings (Box 43-4).
BOX 43-4 Warning Signs of Diabetes
Adapted from American Diabetes Association: Diabetes symptoms. Available at: http://www.diabetes.org/diabetes-symptoms.jsp. Accessed October 8, 2008.
Type 1 diabetes mellitus is characterized by sudden appearance of the following:
Type 2 diabetes mellitus is characterized by slow onset; includes any of the type 1 symptoms and/or the following:
Indicators of probable diabetes mellitus (cardinal signs of diabetes) are as follows:
Symptoms of marked hyperglycemia also include polyphagia (eating extreme amounts of food) and blurred vision. Impairment of growth and susceptibility to certain infections may also accompany chronic hyperglycemia. A family history of diabetes, obesity, GDM, premature atherosclerosis, and neuropathic disorders also are indications of probable diabetes mellitus (Boxes 43-5, 43-6, and 43-7).
BOX 43-5 Criteria for Testing for Diabetes in Asymptomatic, Adult, Undiagnosed Individuals∗
Testing for diabetes should be considered in the following situations:
∗ May not be correct for all ethnic groups.
BOX 43-6 Testing for Type 2 Diabetes in Children4
Chronic Complications
People with both types of diabetes mellitus show a tendency for severe, multisystem, long-term complications (see Table 43-2), including the following:
 Autonomic neuropathy causing gastrointestinal, genitourinary, and cardiovascular symptoms and sexual dysfunction
Autonomic neuropathy causing gastrointestinal, genitourinary, and cardiovascular symptoms and sexual dysfunctionMechanisms thought to cause tissue damage in diabetics are alterations in the host immunoinflammatory response including altered function of immune cells (including neutrophils, monocytes, and macrophages), elevated levels of tumor necrosis factor-alpha (TNF-α), alterations in connective tissue metabolism, glycation of tissue proteins forming advanced glycation end products (AGEs)5 and AGE-modified collagen.5 Individuals with diabetes have an increased incidence of atherosclerotic, cardiovascular, peripheral vascular, and cerebrovascular disease. Hypertension, abnormalities in lipoprotein metabolism, and periodontal disease are found in people with diabetes. The emotional and social impact of diabetes and the demands of therapy cause significant unmet human needs in individuals with diabetes and their families (Table 43-3). All complications affect clients with both type 1 and type 2 diabetes, although clinical consequences differ greatly. Generally, kidney and eye diseases predominate in type 1 diabetes, atherosclerotic disease predominates in type 2 disease, and neuropathy occurs in both (see Table 43-2).
TABLE 43-3 Some Unmet Human Needs of Persons with Diabetes and the Effect on Outcomes of Self-Monitoring of Blood Glucose
| Unmet Human Need | Client's Feeling | Example: Client's Behavioral Response |
|---|---|---|
| Protection from health risks | I want to be 100% okay. | Seeking perfection; therefore records results as 100% okay. |
| Responsibility for oral health | ||
| Conceptualization and problem solving | ||
| Freedom from fear and stress |
Adapted from Skyler JS, Reeves ML: Intensive treatment of type I diabetes mellitus. In Olefsky JM, Sherwin RS, eds: Diabetes mellitus: management and complications, New York, 1985, Churchill Livingstone.
Diabetes—A Risk Factor for Periodontal Disease
See Chapter 17, section on modifiable risk factors, and Chapter 18.
Periodontal disease is the sixth complication of diabetes. Young adults with diabetes have twice the periodontal disease risk of those without diabetes. One third of individuals with diabetes have severe periodontal disease with attachment loss of 5 mm or greater.6 Level of glycemic control seems to be an important determinant in the relationship.
DIABETIC EMERGENCIES (SEE CHAPTER 8)
Individuals with uncontrolled diabetes increase their risk of the following medical emergencies:
Occurrence of stupor or coma in diabetes may be due to several causes, for example, the diabetic condition may be undiagnosed or the person with type 1 disease may not have followed the required insulin regimen. Stress, infection, and increased level of activity contribute to an emergency situation.
Hypoglycemia (see Box 43-7; Tables 43-4 and 43-5)
Hypoglycemia (blood glucose concentration <50 mg/dL), the most common metabolic emergency in persons with type 1 diabetes mellitus, is a condition resulting from an excess of insulin and a glucose deficiency in the body. (Blood glucose concentration of 80 to 120 mg/dL is normal). Annually, severe episodes occur in one of five individuals; minor episodes occur every 2 weeks on average in each insulin-treated person. In clients with type 2 disease treated with sulfonylurea agents, hypoglycemia is more common than is generally recognized and may be severe, especially in older persons treated with longer-acting agents. Signs and symptoms of hypoglycemia result from a lack of glucose in the brain and compensation by the nervous system for this lack of glucose (see Box 43-7). Main causes of hypoglycemia in persons with type 1 disease are listed in Table 43-4.
TABLE 43-4 Causes of Hypoglycemia in Type 1 Diabetes Mellitus
| Factor | Cause |
|---|---|
| Insulin | |
| Food | |
| Exercise | |
| Other |
TABLE 43-5 Hypoglycemia Compared with Hyperglycemia
| Signs and Symptoms | Hypoglycemia (40-50 mg/dL) | Hyperglycemia (400-600 mg/dL) |
|---|---|---|
| Onset | Rapid (minutes) | Slow (days/weeks) |
| Thirst | Absent | Increased |
| Nausea and vomiting | Absent | Frequent |
| Vision | Double | Dim |
| Respirations | Normal | Difficult, hyperventilation |
| Skin | Moist, pale | Hot, dry, flushed |
| Tremors | Frequent | Absent |
| Blood pressure | Normal | Hypotension |
Individuals with diabetes can manage mild hypoglycemia themselves by ingesting glucose, sweet drinks, or milk. Between 10 and 20 g of glucose (about the amount in an 8-ounce glass of 2% fat milk, a 4-ounce glass of orange juice, three pieces of hard candy, or eight Lifesavers candies) is generally adequate, although many persons take considerably more because they fear prolonged hypoglycemia. More severe hypoglycemia also can be treated by oral ingestion of carbohydrates, but another person may have to administer it. If the victim is unconscious, treatment requires intravenous dextrose solution or an intramuscular injection of 0.5 mg to 1.0 mg glucagon, followed on awakening by oral complex carbohydrate with a protein source (e.g., small meat or cheese sandwich or cottage cheese and fruit).
Hyperglycemic Ketoacidotic Coma (Diabetic Coma) (see Table 43-5)
Although the percentage of all diabetic deaths caused by hyperglycemia ketoacidotic coma has decreased dramatically from more than 60% in preinsulin days to 1% at present, it is still considerable, especially in younger individuals. Prevention is the best treatment; however, emergency treatment requires hospitalization to correct fluid and electrolyte imbalances.
Coma resulting from absolute insulin deficiency is found in persons with acute-onset type 1 diabetes in whom diagnosis was unknown or delayed and in individuals with known diabetes who discontinued or decreased their insulin dose for some reason. Coma from a temporary insulin deficiency may be caused by infection or stressful situations in which there is an increase in secretion of anti-insulin hormones (glucagon, cortisol, and catecholamines) (Box 43-8). Infection is the most common precipitating factor and is present in more than 50% of all persons with diabetic ketoacidotic coma.
A series of biochemical events explains the basis of severe ketoacidosis, and signs and symptoms are presented in Table 43-6. Clear guidelines on maintaining control should be provided to the diabetic client with intercurrent infection to resolve the infection early (Box 43-9).
TABLE 43-6 Features of Severe Diabetic Ketoacidosis
| Features | Possible Causes |
|---|---|
| Symptoms | |
| Signs | |
∗ Indicates speculated or unknown cause.
BOX 43-9 Guidelines for Maintaining Glycemic Control in Persons with Diabetes Mellitus
∗ Alternatively, the total daily dose can be given as four equal-divided doses of short-acting regular insulin with carbohydrate taken after each injection. This allows flexibility for increasing insulin but is necessary only for seriously uncontrolled diabetes with infections.
Treatment of diabetic ketoacidosis requires hospitalization to restore the disturbed metabolic fluid and electrolyte state to normal. Fluid rehydration (salt and water), insulin, potassium, broad-spectrum antibiotic therapy, and treatment of precipitating factors are the main elements of diabetic coma treatment.
DISEASE MANAGEMENT
Glycemic Control: Self-Monitoring of Blood Glucose and A1c
The most important clinical advance in the control of diabetes mellitus is self-monitoring of blood glucose with small, automated devices. Blood glucose levels can be monitored as needed; however, four times per day is generally recommended. Monitoring is done by placing a small drop of blood on a reagent strip, which is then inserted into the meter. The meter measures glucose concentration and displays a value of glucose in millimeters per deciliter (mm/dL) of blood.
The hemoglobin A1c laboratory test (also known as the A1c test) is used by the physician to monitor overall glycemic control. Hemoglobin A is made during the 120-day life span of a red blood cell. Blood glucose attaches to the hemoglobin A and is used as a record of blood glucose levels over the past 3 to 4 months. The normal A1c level is <6%.2 Abnormal A1c levels correlate with glucose intolerance and the development of diabetic complications. Recommendations for A1c levels and blood measurements are presented in Box 43-10.
BOX 43-10 Glycemic Control: Summary of Recommendations for Adults with Diabetes2
| A1c | <7.0%∗ |
| Preprandial capillary plasma glucose | 90 to 130 mg/dL |
| Peak postprandial capillary plasma glucose† | <180 mg/dL |
| Blood pressure | <130/80 mmHg |
| Lipids | |
| Low-density lipoprotein (LDL) | <100 mg/dL |
| Triglycerides | <150 mg/dL |
| High-density lipoprotein (HDL) | >40 mg/dL |
Medical Nutrition Therapy
Diet remains the hallmark of diabetes therapy, despite advances in insulin formulations, insulin delivery systems, and oral medications. Diabetic diets are designed to provide appropriate quantities of food at regular intervals, supply daily caloric requirements to aid in achieving or maintaining desirable body weight, and reduce fat intake to correct an unfavorable lipid profile conducive to atherosclerosis.
In type 2 diabetes, reduction in hyperglycemia is correlated with weight loss. In type 1 diabetes mellitus, nutritional strategies involve monitoring the percentage of carbohydrate (55% to 60% of total calories) to protein (12% to 20% of total calories) intake. Meal planning for diabetics is based on the food exchange list system of the American Diabetes Association.
Insulin Therapy
Persons with type 1 diabetes have essentially no pancreatic insulin, are unresponsive to oral sulfonylurea hypoglycemic agents, and are ketosis-prone; they are therefore dependent on lifelong administration of exogenous insulin. Approximately 40% of people with type 2 diabetes use insulin to control hyperglycemia, 49% use oral medications, and 10% use a combination of insulin and oral medications.
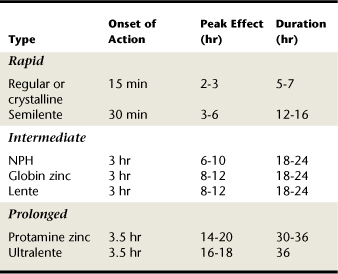
Human insulin and insulin analogues are categorized by speed of onset, peak effect, and time of action as follows:
Insulin may be injected subcutaneously with an insulin syringe or a penlike device. Insulin pumps are widely used to deliver a programmed, steady drip of insulin (basal rate) under the skin 24 hours a day. A push of a button on the pump delivers a bolus dose to respond to the number of carbohydrate grams consumed at a meal. Alternative routes of insulin delivery include inhaled insulin (Exubera) and implantable insulin pumps, used in Europe. Exubera is a powdered form of insulin inhaled into the lungs through the patient's mouth using a specially designed inhaler. Table 43-7 illustrates insulin types that may be used alone or in combination. Dosages, frequency, and times of administration are highly individualized.
Oral Drug Therapy
When type 2 control of hyperglycemia is not achieved with diet and exercise, oral drug therapy is prescribed by the physician (endocrinologist). Generally, oral drug therapy stimulates the pancreas to secrete more insulin, increases the body's response to insulin, slows digestion, or decreases glucose production, as follows:
 Sulfonylureas (glyburide [Glynase Pres Tab, Micronasc], glipizide [Glucotrol]) stimulate the pancreas to increase insulin production and with the extended-release formulas have low risk of weight gain and hypoglycemia.
Sulfonylureas (glyburide [Glynase Pres Tab, Micronasc], glipizide [Glucotrol]) stimulate the pancreas to increase insulin production and with the extended-release formulas have low risk of weight gain and hypoglycemia. Metformin (Glucophage) decreases the amount of glucose secreted by the liver. Hypoglycemia is not a side effect, but this medication usually decreases appetite. Metformin is contraindicated with several other medications commonly prescribed for diabetic conditions.
Metformin (Glucophage) decreases the amount of glucose secreted by the liver. Hypoglycemia is not a side effect, but this medication usually decreases appetite. Metformin is contraindicated with several other medications commonly prescribed for diabetic conditions. Alpha-glucosidase inhibitors (AGIs) (acarbose [Precose], miglitol [Glyset]) inhibit enzymes in the small intestines, which are responsible for the digestion of starchy food, thus delaying carbohydrate metabolism.
Alpha-glucosidase inhibitors (AGIs) (acarbose [Precose], miglitol [Glyset]) inhibit enzymes in the small intestines, which are responsible for the digestion of starchy food, thus delaying carbohydrate metabolism. Thiazolidinedione (Actos, Avandia) make the body more sensitive to insulin. Target cell response to insulin is improved, thus reducing insulin doses. Used for individuals with type 2 diabetes treated with insulin whose hyperglycemia is not adequately controlled. Sometimes referred to as “insulin reducers.”
Thiazolidinedione (Actos, Avandia) make the body more sensitive to insulin. Target cell response to insulin is improved, thus reducing insulin doses. Used for individuals with type 2 diabetes treated with insulin whose hyperglycemia is not adequately controlled. Sometimes referred to as “insulin reducers.”DENTAL HYGIENE PROCESS OF CARE
Well-controlled diabetes occurs when the client's blood glucose is within the normal range as a result of a careful balance of medication, diet, and exercise. (Blood glucose concentration of 80 to 120 mg/dL is normal). Clients with well-controlled diabetes can be treated safely, provided that their daily routine is not affected. Diabetics with well-controlled disease have a reduced incidence of dental caries.
Infections of any type can cause a profound disturbance of glycemic control, potentially leading to ketoacidosis and diabetic coma. When infection is present, counterregulatory hormone secretion increases (specifically cortisol and glucagon), leading to hyperglycemia and increased ketogenesis. Infection is the most common precipitating factor for severe ketoacidosis. In the client with poorly controlled diabetes, phagocytic function is impaired and resistance to infection decreased. Prevention of oral diseases and infections is critical to the diabetic control of the client, and poor diabetic control may aggravate the oral disease status.
Several unmet human needs relate to dental hygiene care for individuals with diabetes. For example, emotional stress induced by a dental appointment causes the release of epinephrine, which mobilizes glucose from glycogen stored in the liver. Stress, therefore, can contribute to a hyperglycemic condition becoming ketoacidotic. Periods of waiting and treatment time should be minimized to meet the client's need for freedom from stress.
Diabetes in people on intensive regimens of multiple insulin injections and daily self-monitoring of blood glucose may abruptly become uncontrolled as a result of an active periodontal infection. When unrecognized, the periodontal infection may cause the human needs for skin and mucous membrane integrity and protection from health risks to become compromised. Table 43-3 reflects some unmet human needs and their effect on outcomes of self-monitoring of blood glucose. Figures 43-2 and 43-3 show clinical examples of periodontal disease in diabetics.
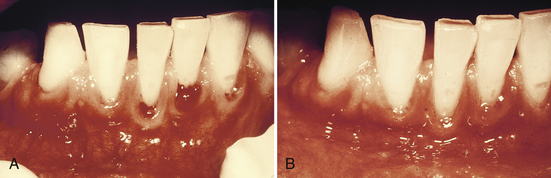
Figure 43-2 Diabetes and periodontal disease. A, An adult with diabetes (blood glucose level of 400 mg/100 mL). Note gingival inflammation, spontaneous bleeding, and edema. B, Same person after 4 days of insulin therapy (glucose level less than 100 mg/100 mL). Gingivae have improved in the absence of professional mechanical therapy.
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds: Carranza's clinical periodontology, ed 10, St Louis, 2006, Saunders.)

Figure 43-3 Uncontrolled diabetes and periodontal therapy. A, An adult with uncontrolled diabetes. Note enlarged, smooth red gingiva with initial enlargement in the anterior area. B, Same person. Note the inflamed, enlarged area around teeth 27 to 30. C, Suppurating abscess, facial or maxillary cleft area in a person with uncontrolled diabetes.
(From Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds: Carranza's clinical periodontology, ed 10, St Louis, 2006, Saunders.)
Assessment
Health History
In taking the health history the dental hygienist questions the client regarding the signs and symptoms of ketoacidosis (see Box 43-3) to determine whether an undiagnosed diabetic condition is present.7 High-risk factors for developing diabetes include the following:
Among the aging, classic symptoms do not usually manifest. Rather, clinical findings are related to chronic complications of the disease, such as vascular disorders or neuropathic syndromes.
If the person is a known diabetic, the client and health history interview should address the following:
The decision to continue the assessment, consult with a physician, or defer treatment and refer to the physician should be made based on client response to questions during health history and pharmacologic assessment (Boxes 43-11, 43-12, and 43-13).
BOX 43-11 Levels of Blood Glucose for Care Planning
With permission from Fehrenbach MJ: Dental care for the diabetic patient, Prev Angle Newsl 4:1, 2005.
∗ Indicates dental hygiene care should not be provided at this blood glucose level.
BOX 43-12 When to Refer to a Physician
Adapted from Little JW, Falace DA: Dental management of the medically compromised patient, ed 7, St Louis, 2007, Mosby.
Refer client to physician for diagnosis and/or treatment when client has the following:
Oral Assessment
Intraoral findings may reveal the following conditions common in poorly controlled diabetes (Table 43-8):
TABLE 43-8 Oral Complications of Diabetes Mellitus
| Clinical Signs and Symptoms | Pathophysiology |
|---|---|
| Salivary and Oral Changes | |
| Xerostomia | Increased fluid loss |
| Bilateral, asymptomatic parotid gland swelling with increased salivary viscosity | |
| Increased dental caries, especially in cervical region | Secondary to xerostomia and salivary glucose levels |
| Unexplained odontalgia and percussion sensitivity (acute pulpitis) | Pulpal arteritis from microangiopathies |
| Lingual erosion of anterior teeth∗ | Complications of anorexia nervosa and bulimia |
| Periodontal Changes | |
| Infection and Wound Healing | |
| Tongue Changes | |
| Other Changes | |
AGE, Advanced glycation end product.
∗ Although not a complication of diabetes per se, this pattern is seen when the person wants to maintain the weight-loss aspect of diabetes while ignoring or tolerating the hyperglycemic side effects. Client may not be taking proper insulin doses and may not be truthful when asked about this.
† Periodontal disease is seen in up to 40% of diabetic patients. Adequate periodontal therapy may result in decreased insulin requirements.
Adapted from Lalla RV, D'Ambrosio JA: Dental management considerations for the patient with diabetes mellitus, J Am Dent Assoc 132:1425, 2001.
Diabetes is an important risk factor for periodontal disease. The American Academy of Periodontology published a comprehensive review on diabetes mellitus and periodontal disease.5 Prevalence and severity of periodontal disease increase in individuals with both type 1 (insulin deficient) and type 2 (insulin resistant) forms of diabetes, as compared with nondiabetics. Diabetics with blood glycated hemoglobin A1c levels >8% have a greater increase in periodontal inflammation, attachment loss, and bone loss than diabetics with A1c levels <8%.8 Presence of hyperglycemia contributes to enhanced periodontal inflammation and alveolar bone loss in diabetes. Hyperglycemia progressively leads to an increase of proinflammatory cytokines such as TNF-α, interleukin 6 (IL-6), and others that destroy the connective tissue and bone. The chronic increased cytokine levels augment inflammatory tissue destruction. Control of hyperglycemia reduces the level of proinflammatory cytokines. Glycemic control is an integral part of the control of periodontal disease in individuals with diabetes (see Figure 43-2).5
Uncontrolled diabetes increases dental caries risk as a result of reduced saliva secretion and increased glucose in saliva. Other oral complications associated with diabetes may affect nutrition by causing the person to select foods that are easy to chew but nutritionally inadequate.
Diagnosis and Planning
A dental hygiene care plan focuses on the client's unmet human needs and allows the clinician to manage risks of potential diabetic emergencies, thereby protecting the client from health risks. Persons with diabetes may not be under good glycemic control. In a study of 97 patients who entered a dental clinic, 28 patients were found to be hyperglycemic (>130 mg/100 mL) and 2 were noted to be hypoglycemic (<70 mg/100 mL)9 (see Box 43-11). Appointments should be brief to minimize anxiety and stress and avoid interference with medication and eating schedule. Morning appointments are ideal because most people with diabetes are best controlled at this time. An hour to an hour and a half after breakfast is best for appointments to avoid the peak action time of medication. Regular (fast-acting) insulin, often taken in the morning or at each meal, peaks within 2 to 3 hours after the injection. Oral hypoglycemic agents do not cause peaks.
Therapeutic scaling and periodontal debridement are contraindicated for people in the uncontrolled diabetic condition (blood glucose levels <70 mg/dL and >240 mg/dL) (see Box 43-11and Figure 43-3). Clients should be treated in consultation and referred to the physician of record for systemic evaluation. Dental hygiene care should not begin until the diabetic condition is controlled. The short-term risk for infections in persons with diabetes has been shown to increase with average blood glucose levels of 200 to 230 mg/100 mL.3 When care is planned, interventions are likely to include the following:
 Fluoride and chlorhexidine therapies and use of xylitol-containing and amorphous calcium phosphate – containing products (see Chapter 31)
Fluoride and chlorhexidine therapies and use of xylitol-containing and amorphous calcium phosphate – containing products (see Chapter 31)A sample dental hygiene care plan is shown in the Critical Thinking Exercises section. Other management concerns are shown in Box 43-14.
BOX 43-14 Alterations in Dental Hygiene Care of Older Adults with Diabetes
Data from Little JW, Falace DA: Dental management of the medically compromised patient, ed 7, St Louis, 2007, Mosby; prepared by Pamela P. Brangan.
Potential Risk Relating to Dental Hygiene Care
In controlled diabetic older adult:
Prevention of Medical Complications
Older adult receiving insulin:
Advise older adults to inform you of any symptoms of insulin reaction when they first occur
Implementation
Therapeutic Scaling and Periodontal Debridement
Gingival and periodontal diseases associated with systemic factors, as found in persons with diabetes, may not respond well to subgingival scaling, periodontal debridement, and oral biofilm control. However, removal of hard and soft deposits and bacterial toxins from crown and root surfaces of teeth is critical in the prevention of periodontal infection in people with diabetes. Unnecessary tissue manipulation and trauma are avoided to minimize risk of postoperative infection and poor healing.
Severe periodontitis is associated with increased risk of poor glycemic control; therefore, severe periodontitis may be a risk factor in the progression of diabetes. Also, evidence suggests that antimicrobial treatment, specifically systemic doxycycline (100 mg for 2 weeks—therapeutic antimicrobial dose), has the potential to improve glycemic control following scaling and root debridement in diabetic clients.5
Increased glucose in gingival crevicular fluid may result in proliferation of oral microflora, increasing risk of periodontal disease and dental caries. The short-term (3 to 4 months) response in clinical parameters (i.e., probing depths, bleeding on probing, attachment levels, subgingival microbiota) of diabetics to nonsurgical periodontal therapy (NSPT) appears to be equivalent to the response in nondiabetic clients; however, poorly controlled diabetic clients have more rapid clinical attachment loss and a compromised long-term response. At 5 years after NSPT and surgical periodontal treatment in combination with regular periodontal maintenance therapy, diabetic clients who were well controlled had clinical attachment levels similar to those of nondiabetic clients.5
A well-controlled diabetic with no evidence of infection does not require prophylactic antibiotic premedication.3,11 In fact, antibiotic use in diabetic persons may lead to oral or systemic fungal infections. If an infection is present, preoperatively or postoperatively, antibiotic therapy is mandatory. Prophylactic antibiotic premedication before periodontal instrumentation should be considered for the uncontrolled diabetic after consultation with the client's physician.
Diabetic microangiopathy causes blindness and kidney disease. Therefore a client exhibiting eye disorders also may suffer from kidney disease. Medications that are excreted renally may be retained in the body of the diabetic client with kidney disease, causing toxic effects. When local anesthetic agents are administered, minimal use of vasoconstrictors is required because epinephrine is capable of raising blood glucose.
Evaluation
The periodontal tissues of the client with well-controlled diabetes respond positively to nonsurgical periodontal therapy. Delayed healing, however, may indicate hyperglycemia, which decreases the normal healing actions of leukocyte phagocytosis, chemotaxis, and adherence properties. Frequent oral assessments, periodontal maintenance, and monitoring of diabetic control with current hemoglobin A1c test results are recommended.
CLIENT EDUCATION TIPS
 Relate diabetic client's greater risk of infection and increased healing times to need for oral biofilm control.
Relate diabetic client's greater risk of infection and increased healing times to need for oral biofilm control. Teach use of daily subgingival irrigation for target delivery of antimicrobial agent or twice daily use of an American Dental Association–accepted antimicrobial mouth rinse; use of an antiplaque, antigingivitis dentifrice; use of caries control products (fluoride mouth rinse, xylitol mints and chewing gum, products containing amorphous calcium phosphate [ACP]); and use of saliva replacement therapy (artificial saliva, sucking on ice chips, xylitol gum and mints).
Teach use of daily subgingival irrigation for target delivery of antimicrobial agent or twice daily use of an American Dental Association–accepted antimicrobial mouth rinse; use of an antiplaque, antigingivitis dentifrice; use of caries control products (fluoride mouth rinse, xylitol mints and chewing gum, products containing amorphous calcium phosphate [ACP]); and use of saliva replacement therapy (artificial saliva, sucking on ice chips, xylitol gum and mints).LEGAL, ETHICAL, AND SAFETY ISSUES
KEY CONCEPTS
 Type 1 diabetes involves about 5% to 10% of the diabetic population. These individuals need to take insulin injections.
Type 1 diabetes involves about 5% to 10% of the diabetic population. These individuals need to take insulin injections. Presence of certain human leukocyte antigens creates a genetic predisposition for the autoimmune cause of type 1 diabetes mellitus.
Presence of certain human leukocyte antigens creates a genetic predisposition for the autoimmune cause of type 1 diabetes mellitus. Type 2 diabetes involves about 90% to 95% of the diabetic population. These individuals usually respond well to weight reduction, dietary management, exercise, or oral medications.
Type 2 diabetes involves about 90% to 95% of the diabetic population. These individuals usually respond well to weight reduction, dietary management, exercise, or oral medications. Insulin resistance or a defect in insulin secretion is the cause of type 2 diabetes. Risk of developing type 2 diabetes increases with obesity, age, inactivity, history of gestational diabetes mellitus (GDM), hypertension, and dyslipidemia.
Insulin resistance or a defect in insulin secretion is the cause of type 2 diabetes. Risk of developing type 2 diabetes increases with obesity, age, inactivity, history of gestational diabetes mellitus (GDM), hypertension, and dyslipidemia. GDM occurs in 4% of pregnancies. Those at high risk include women with obesity, family history of diabetes, and previous GDM.
GDM occurs in 4% of pregnancies. Those at high risk include women with obesity, family history of diabetes, and previous GDM. GDM usually disappears after birth because the condition is a consequence of the normal anti-insulin effects of pregnancy hormones and the diversion of natural glucose to the fetus.
GDM usually disappears after birth because the condition is a consequence of the normal anti-insulin effects of pregnancy hormones and the diversion of natural glucose to the fetus. Without insulin, glucose remains in the blood (hyperglycemia) rather than being stored or used by the cells to produce energy. Suspicion of diabetes is gleaned from a history of symptoms: glucosuria, polyuria, polydipsia, weight loss, polyphagia, and blurred vision.
Without insulin, glucose remains in the blood (hyperglycemia) rather than being stored or used by the cells to produce energy. Suspicion of diabetes is gleaned from a history of symptoms: glucosuria, polyuria, polydipsia, weight loss, polyphagia, and blurred vision. Diabetes mellitus causes severe multisystem, long-term complications. Kidney and eye diseases predominate in type 1 diabetes mellitus; atherosclerosis predominates in type 2; peripheral nerve disease occurs in both.
Diabetes mellitus causes severe multisystem, long-term complications. Kidney and eye diseases predominate in type 1 diabetes mellitus; atherosclerosis predominates in type 2; peripheral nerve disease occurs in both. Hypoglycemia, the most common emergency in persons with type 1 diabetes mellitus, results from an excess of insulin and a deficiency of glucose.
Hypoglycemia, the most common emergency in persons with type 1 diabetes mellitus, results from an excess of insulin and a deficiency of glucose. Well-controlled diabetes occurs when the individual's blood glucose level is within the normal range as a result of a careful balance of medication, diet, and exercise.
Well-controlled diabetes occurs when the individual's blood glucose level is within the normal range as a result of a careful balance of medication, diet, and exercise. Emotional stress (induced in the oral healthcare setting) causes a release of epinephrine, which mobilizes glucose in the body, contributing to a hyperglycemic condition becoming ketoacidotic.
Emotional stress (induced in the oral healthcare setting) causes a release of epinephrine, which mobilizes glucose in the body, contributing to a hyperglycemic condition becoming ketoacidotic. Strict application of oral care protocols increases the chances of achieving good clinical outcomes for individual with diabetes.
Strict application of oral care protocols increases the chances of achieving good clinical outcomes for individual with diabetes.CRITICAL THINKING EXERCISES
Bettie Douman is a 40-year-old professional secretary employed full-time at a large university. She has had type 1 diabetes mellitus for 20 years. Bettie has been using the insulin pump for 2 years, which has greatly lowered her blood glucose levels. Her 24-hour blood sugar test results average 180 mL/dL, and 3-month HgA1c was 8%. Bettie walks the family dog at a fast pace every evening for 30 minutes. She is embarrassed that she has not been careful about eating a nutritionally balanced diet in the last year and a half. On examination the dental hygienist notes low risk for dental caries, generalized moderate gingival bleeding on probing, with localized 4- and 5-mm pocket depths in the molar areas.
 What emergency would you prepare for when treating this client? What steps would you take to prevent this emergency?
What emergency would you prepare for when treating this client? What steps would you take to prevent this emergency?| Dental Hygiene Diagnosis | Goal or Expected Behavior |
|---|---|
| Unmet need for conceptualization and problem solving | By 12/1, client explains the role of oral biofilm in causing periodontal disease. |
| Unmet need for responsibility for oral health | By 12/1, client verbalizes the role of oral infection in glycemic control. |
| Client reports improvement in hyperglycemia through the control of periodontal disease | By 1/1, client decreases bleeding points by 75%. |
| Dental Hygiene Diagnosis | Goal or Expected Behavior |
|---|---|
| Unmet need for skin and mucous membrane integrity of the head and neck (undernutrition and increased frequency of carbohydrate consumption) |
1. Warayan K.M., Boyle J.P., Thomson T.J., et al. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884.
2. American Diabetes Association. Standards of medical care in diabetes. Position statement. Diabetes Care. 2007;30(Suppl):4.
3. Little J.W., Falace D.A. Dental management of the medically compromised patient, ed 7. St Louis: Mosby; 2007.
4. Centers for Disease Control and Prevention: National diabetes fact sheet. Available at: www.cdc.gov/diabetes/pubs/extimates.htm. Accessed December 23, 2007.
5. Mealey B.L., Oates T.W. AAP-commissioned review. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77:1289.
6. American Diabetes Association: Complications of diabetes in the United States. Available at: www.diabetes.org/utils. Accessed December 24, 2007.
7. Campbell P.R., Shuman D., Bauman D.B. ADHA graduate student/faculty research project: health history. J Dent Hyg. 1993;67:378.
8. Engebretson S.P., Hey-Hadavi J., Ehrhardt F.J., et al. Gingival crevicular fluid levels of interleukin-1β and glycemic control in patients with chronic periodontitis and type 2 diabetes. J Periodontol. 2004;75:1203.
9. Rhodus NL, Vibeto B., Hamamoto D.T. Glycemic control in patients with diabetes mellitus upon admission to a dental clinic: considerations for dental management. Quintessence Int. 2005;36:474.
10. Gulch J.I. Commentary on “The effect of periodontal therapy on TNF-α, IL-6 and metabolic control in type 2 diabetics,”. Access. 21:(26), 2007.
11. Lalla R.V., D'Ambrosio J.A. Dental management considerations for the patient with diabetes mellitus. J Am Dent Assoc. 2001;132:1425.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..