CHAPTER 18 Impact of Periodontal Infections on Systemic Health
 Explain why the presence of bleeding on periodontal probing means that the “door is open” for a wide range of adverse effects on the overall health of the individual.
Explain why the presence of bleeding on periodontal probing means that the “door is open” for a wide range of adverse effects on the overall health of the individual. Explain the potential connection between periodontal diseases and coronary heart disease (atherosclerosis, myocardial infarction), cerebrovascular disease (stroke), pregnancy complications and adverse outcomes, diabetes mellitus, pulmonary diseases, neurologic diseases, gastrointestinal diseases, and cancer of the stomach and pancreas.
Explain the potential connection between periodontal diseases and coronary heart disease (atherosclerosis, myocardial infarction), cerebrovascular disease (stroke), pregnancy complications and adverse outcomes, diabetes mellitus, pulmonary diseases, neurologic diseases, gastrointestinal diseases, and cancer of the stomach and pancreas.Emerging evidence implicates periodontal infections as one of several important factors that exert negative effects on systemic health. The potential impact of oral infections on systemic health has had extensive coverage in the lay press. Accordingly, dental hygienists and other oral healthcare professionals are often asked to explain the potential connection between gum disease and serious medical problems such as atherosclerosis (hardening of the arteries), myocardial infarction (heart attack), cerebrovascular disease (stroke), diabetes mellitus (DM), and adverse pregnancy outcomes. This chapter reviews how periodontal infections might affect systemic health and provides information needed to answer questions about this important topic.
Box 18-1 lists those associations between periodontal infections and adverse systemic outcomes for which there is scientific evidence supporting the connections. For most of these associated conditions, the connection begins with the entry of bacteria into the bloodstream from infected periodontal tissues. The presence of bacteria in the bloodstream (bacteremia) is a common occurrence in patients with periodontitis because the epithelial lining of the soft-tissue wall of the pocket is ulcerated (i.e., the pocket wall is disrupted and has holes in it) (Figure 18-1). Bacteria infecting periodontal pockets easily enter the bloodstream at these ulcerated sites. “Bleeding gums,” a commonly reported symptom of gum disease, is often noticed by the individual after routine daily activities such as eating or toothbrushing. In contrast, healthy gum tissues do not bleed under these normal mechanical stimuli. The presence of bleeding gums strongly suggests sufficient gingival inflammation to cause pocket-wall ulcerations that lead to repeated episodes of bacteremia throughout the day. In addition, an important clinical sign of inflammation is the presence of bleeding when the site is gently examined with a periodontal probe (Figure 18-2). Such sites bleed when probed because the epithelial lining of the pocket wall is thin and ulcerated. Therefore the presence of bleeding means that the “door is open” and bacteria from periodontal pockets can readily enter the bloodstream. If bacteremias occur on a chronic basis, the blood-borne bacteria can contribute to a wide range of adverse effects on the overall health of the individual.
BOX 18-1 Potential Associations between Periodontal Infections and Adverse Systemic Outcomes
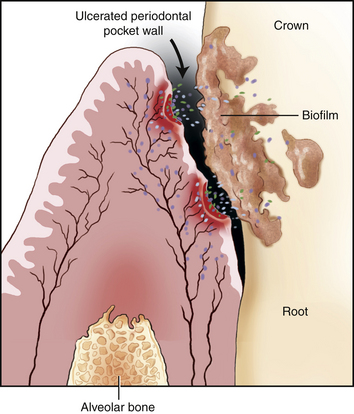
Figure 18-1 Drawing of the interface between the gingiva and tooth in a case of periodontal disease. The epithelium of the pocket wall is ulcerated. These ulcerations allow subgingival bacteria in the adjacent periodontal pocket access to the systemic circulation.
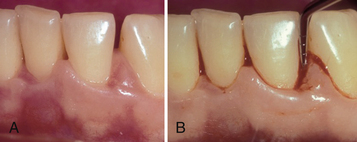
Figure 18-2 A, Clinical appearance of the mouth of a 55-year-old woman with chronic periodontitis. Clinical signs of inflammation include redness and swelling (edema) of the gingival papillae. B, Bleeding on probing in the same patient shown in A.
CORONARY HEART DISEASE (ATHEROSCLEROSIS) (SEE CHAPTER 42)
In coronary heart disease the walls of key arteries to the heart (coronary arteries) thicken. Thickening of the arterial walls is not the simple accumulation of fats and lipids. Research clearly indicates that coronary heart disease is an inflammatory disease in which the blood vessel walls thicken in response to chronic injury.1,2 This thickening may become so extensive that the artery becomes completely occluded, thereby blocking the flow of blood to a portion of the heart. When this happens a myocardial infarction (heart attack) occurs and may lead to death or disability.
The potential connection of periodontal disease to this process starts with chronic bacteremias. Some blood-borne bacteria attach to, invade, and injure the single layer of endothelial cells that line the circulatory system. Injured endothelial cells trigger inflammation of the blood vessel wall that subsequently leads to the development of an atheroma or intimal thickening of the vessel wall. Well-developed atheromas contain lipids such as cholesterol covered with a fibrous cap surrounding a necrotic core laden with scavenging macrophages. Periodontal bacteria are not the only source of chronic injury to endothelial cells. Other factors can injure endothelial cells and contribute to atheroma formation; these include certain viruses, environmental toxins, components of cigarette smoke, hypertension, and diets leading to hyperlipidemia. Therefore it is important to realize that coronary heart disease is a multifactorial disease in which many risk factors play a role. A common event leading to a heart attack is the disruption of a well-developed atheroma by vascular inflammation induced by one or more of these risk factors. Disruption of the atheroma can lead to the formation of a blood clot that occludes or blocks the vessel (Figure 18-3).
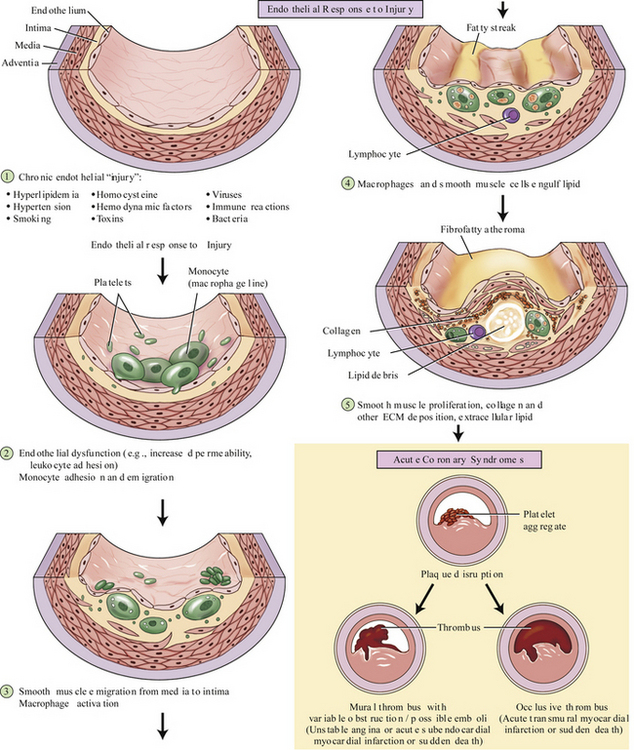
Figure 18-3 Development and eventual disruption of an atherosclerotic plaque (atheroma) that can lead to heart attacks and nonhemorrhagic strokes. ECM, Extracellular matrix.
Evidence suggesting that periodontal infections contribute to coronary heart disease includes the following:
 Periodontal pathogens, such as Porphyromonas gingivalis, are capable of adhering to, invading, and replicating within endothelial cells2
Periodontal pathogens, such as Porphyromonas gingivalis, are capable of adhering to, invading, and replicating within endothelial cells2 Plausible mechanisms by which periodontal pathogens trigger inflammatory reactions that promote the formation and disruption of atheromas1
Plausible mechanisms by which periodontal pathogens trigger inflammatory reactions that promote the formation and disruption of atheromas1Although there are no conclusive data to show an unequivocal cause-and-effect relationship between periodontal infections and cardiovascular disease, the association is strong enough that prudent clinicians should include “improvement in overall systemic health” as one of the probable benefits of treating periodontal disease.
NONHEMORRHAGIC (ISCHEMIC) STROKE (SEE CHAPTER 42)
A stroke is the sudden interruption of the blood supply to part of the brain. There are two general types of strokes: hemorrhagic and nonhemorrhagic. The hemorrhagic type accounts for about 20% of all strokes and occurs when there is bleeding within or around the brain, usually because of the spontaneous rupture of an artery. The nonhemorrhagic or ischemic type accounts for approximately 80% of all strokes and is caused by a clot or other blockage of one or more of the arteries supplying blood to the brain (e.g., the internal carotid arteries). The process of blocking the artery usually involves the same atherosclerotic changes in blood vessels that lead to coronary heart disease. Indeed, the risk factors for nonhemorrhagic (ischemic) stroke are identical to those for coronary heart disease. Atherosclerotic changes in the carotid arteries are strongly associated with the amount of periodontal bone loss.4 At the present time, however, no intervention data show that treatment of periodontal infections lowers the risk of developing an ischemic stroke. However, a strong circumstantial argument can be made that periodontal therapy might decrease the development of atherosclerotic changes in blood vessels and thereby decrease the risk of having a stroke.
PREGNANCY COMPLICATIONS AND OUTCOMES (SEE CHAPTER 53)
The presence of infection, particularly in the cervical area of the uterus, increases the risk of delivering a preterm low-birthweight baby (PTLBW). (Preterm birth is defined as a pregnancy of less than 37 weeks, and low birthweight is less than 5.5 pounds or 2400 grams.) One suggested explanation is that endotoxin from gram-negative bacteria enters the circulation at high enough levels to stimulate production of inflammatory mediators, such as prostaglandin E2 (PGE2), by the amnion. PGE2 and other inflammatory mediators are potent inducers of labor.5 The connection between periodontal infections and adverse pregnancy outcomes is supported by epidemiologic studies.5,6 The association is even stronger in women whose periodontal disease is progressing or getting worse.6
For blood-borne periodontal bacteria to trigger preterm birth, they must first reach the amnion and the fetus by crossing the placental barrier. There is clear evidence that this does happen, because umbilical cord blood from some preterm infants contains antibodies (immunoglobulin M [IgM]) of fetal origin directed against periodontal pathogens such as Campylobacter rectus and Prevotella intermedia.7 Intrauterine access of bacteria to the developing baby also appears to retard fetal growth, because mothers with moderate to severe periodontitis tend to deliver babies that are small for their gestational age.8
A serious complication of pregnancy linked to periodontal infections is preeclampsia.9 This complication is characterized by hypertension, edema or swelling of the ankles, and proteinuria (protein in the urine). Failure to control these physiologic abnormalities can lead to eclampsia, in which convulsions, coma, and death of the mother may occur.
Although there is a strong relationship between periodontal infections and several adverse pregnancy outcomes, it has not been determined if periodontal therapy decreases the incidence of these outcomes. A preliminary study in Chile found that nonsurgical periodontal therapy reduced the number of preterm low-birthweight babies compared with controls.10 However, in a larger randomized controlled clinical trial, the Obstetric and Periodontal Therapy (OPT) Study, on a U.S. population, it was found that periodontal treatment did not significantly alter the rates of preterm birth, low birthweight, or fetal development.11 Therapy in the OPT study consisted of conventional or standard-of-care treatment that included oral hygiene instructions, full-mouth scaling and root planing, monthly evaluation, and additional scaling “as needed.” Data revealed that the treated population of 413 women exhibited a significant decrease in bleeding on probing (BOP) compared with baseline values (baseline sites with BOP = 69.6% versus posttreatment sites with BOP = 45.9%, P < .001). The untreated control group of 410 women did not exhibit any significant change in baseline %BOP versus postdelivery %BOP (69% versus 66.9%) (Figure 18-4). Although in the treated group there was a statistically significant reduction in the percentage of sites with BOP, the extent of the reduction was less than expected after nonsurgical treatment. For example, in a typical nonpregnant population the expected posttreatment percentage of sites with residual BOP should be approximately 10% (Figure 18-5).2 In the OPT study the posttreatment percentage of sites with BOP was 45.9% (see Figure 18-4), strongly suggesting that the standard-of-care treatment in the OPT study was insufficient to control the periodontal disease in the study population. Indeed, the high percentage of sites with BOP after treatment means that the patients were still infected at the end of the study. This finding might mean that pregnant women need more intensive periodontal maintenance care than nonpregnant women.
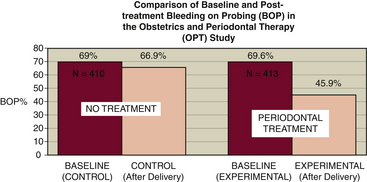
Figure 18-4 Comparison of baseline and posttreatment bleeding on probing (BOP) in the Obstetrics and Periodontal Therapy (OPT) Study.11 Compared with controls, there is a statistically significant reduction (P < .001) in the percentage of sites with BOP in the women who received nonsurgical therapy during pregnancy.
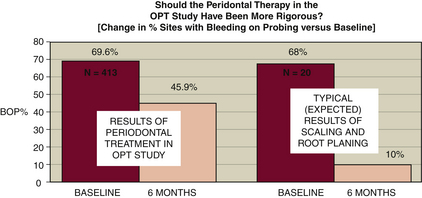
Figure 18-5 Comparison of the percentage reduction in bleeding on probing (BOP) in the treated population in the Obstetrics and Periodontal Therapy (OPT) Study11 versus what would typically be expected after nonsurgical treatment in a nonpregnant population.12 The high percentage of sites with residual BOP in the OPT Study (45.9%) versus that expected (10%) in a typical population suggests that pregnant individuals may require more frequent periodontal care than nonpregnant patients.
DIABETES MELLITUS (SEE CHAPTER 43)
Diabetes mellitus is a group of diseases that results in high levels of glucose in the blood because of either an insufficient supply of insulin or the impaired availability of this pancreatic hormone, which regulates carbohydrate metabolism. In type 1 DM a severe deficiency of insulin exists, usually resulting from the destruction of the insulin-producing pancreatic beta cells. The disease represents only about 10% to 20% of all cases of DM and occurs with the highest frequency in people of Northern European descent (e.g., those from Sweden and Finland). In type 2 DM, which accounts for 80% to 90% of all cases, there is a chronic hyperglycemia (elevated blood sugar) that causes the exhaustion of pancreatic beta cells. In early stages of the disease there is enough insulin, but it is not able to regulate glucose levels in the peripheral tissues. This condition is known as insulin resistance. Obesity is an extremely important environmental risk factor that is linked to the onset of type 2 DM. In many people with long-standing type 2 DM, supplemental insulin injections are needed because the exhausted pancreatic beta cells eventually die.
People with uncontrolled or poorly controlled DM are more susceptible to infections, including periodontal diseases. This susceptibility to infections is partly due to impaired antibacterial functions of neutrophils and wound-healing problems associated with vascular and connective tissue abnormalities. People with diabetes whose disease is under poor metabolic control have more severe periodontitis than those whose disease is medically well controlled.13 Depending on the severity of the DM, the metabolic control of the disease can sometimes be achieved by a carefully planned dietary program. In other people, ingestion of hypoglycemia agents (e.g., tolbutamide [Orinase]) or daily insulin injections are necessary to achieve metabolic control of the disease. Medical regulation of blood sugar levels is hampered by the presence of infections such as untreated periodontitis. Through a number of mechanisms, infections can increase insulin resistance in peripheral tissues and make diabetic control difficult. In some but not all patients, nonsurgical treatment of periodontitis makes the metabolic control of DM easier.14 Indeed, physicians sometimes request that oral healthcare professionals treat periodontitis in their DM patients to facilitate metabolic control of the disease.
PULMONARY DISEASES (SEE CHAPTER 49)
Periodontal infections have been implicated as important in the development of a number of pulmonary diseases including: aspiration pneumonias, ventilator-associated pneumonias (VAPs), and chronic obstructive pulmonary disease. In all of these conditions, members of the oral microbiota gain access to and infect tissues of the pulmonary tree.
Aspiration pneumonias occur most often in patients who have impaired gag and swallowing reflexes. It is a common occurrence in nursing home residents and is sometimes called nursing home–associated pneumonia.15 People at the highest risk are those who have dysphagia (difficulty in swallowing) from a stroke, Parkinson's disease, or other neurologic problems (see Chapter 46). The disease develops when oral fluids containing large numbers of microorganisms are aspirated into the bronchial tree and lungs. Some data suggest that periodontal infections alter the local intraoral environment in such a way that the mouth becomes colonized with elevated numbers of respiratory pathogens.15
Ventilator-associated pneumonias (VAPs) occur most often in patients who need prolonged hospital care in an intensive care unit (ICU). The risk of acquiring VAP dramatically increases in patients who are intubated for longer than 4 to 5 days. In such cases the breathing tube passes through the mouth and oropharynx and becomes colonized by the microbiota from these sites. There is strong evidence from randomized controlled clinical trials that oral hygiene procedures performed on ICU patients by hospital personnel reduce the risk of development of VAP.15-17
Chronic obstructive pulmonary disease (COPD), a common respiratory illness characterized by chronic bronchitis and emphysema, is especially prevalent in cigarette smokers. A statistically significant association between COPD and periodontal infections has been demonstrated in a number of epidemiologic studies in which loss of teeth, deep probing depths, and clinical attachment loss were used as surrogate markers for the presence of periodontal disease.16 No studies show that the presence of periodontal infections influences the pathophysiology of COPD. However, it is possible that periodontal disease promotes the colonization of the mouth by respiratory pathogens that subsequently leads to chronic bronchitis. It is also possible that there is no causal link between periodontal infections and COPD, because smoking is a risk factor shared by the two conditions and the association might be coincidental.
Lung cancer also is linked to periodontal infections. A statistically significant association was demonstrated in a retrospective large national epidemiologic study, even when the data were adjusted for history of smoking. However, problems in accurately measuring smoking history may explain the apparent connection. Perhaps the two conditions have no causal relationship and the association is spurious.18
NEUROLOGIC DISEASES (SEE CHAPTER 46)
Hematogenous spread of oral infections to the central nervous system (CNS) is a rare occurrence. CNS infections of oral origin include unusual brain abscesses and extremely rare cases of meningitis. The rarity of these conditions is probably related to the presence of the blood-brain barrier, which consists of continuous tight junctions between epithelial cells of the choroid plexus and capillary endothelial cells in the brain. Spread of oral infections to the CNS also can occur locally by a variety of anatomic routes such as the infratemporal fossa through the greater wing of the sphenoid bone near the foramen ovale. Spread of infection by either route is rare, and the literature addressing these conditions usually consists of case reports.19
In Alzheimer's disease (AD) there is a progressive atrophy of the cerebral cortex with a gradual loss of short-term and long-term memory. Characteristic brain lesions contain abnormal proteins that take the form of senile plaques with an amyloid core surrounded by dystrophic neurites and neurofibrillary “tangles” composed of cytoskeletal intermediate filaments. Components of some microorganisms such as Chlamydia pneumoniae and spirochetes (the genus Treponema) have been found in brain tissues of persons with AD. In addition, antigens from oral spirochetes have been detected in brain tissues at a higher rate in AD patients (87.5%) compared with non-AD controls (22.2%).20 However, a cause-and-effect relationship has not been shown, because the microbial material may have been secondarily deposited in previously damaged tissue. Nevertheless, one should not rule out a role for oral infections in AD, because a recent long-term epidemiologic study suggests that the development of dementia is significantly associated with tooth loss21 (see Chapter 46).
GASTROINTESTINAL DISEASES AND CANCER (SEE CHAPTER 44)
It is well established that certain gastrointestinal diseases such as chronic gastritis and peptic ulcers can be caused by Helicobacter pylori, a gram-negative microaerophilic motile bacterium that colonizes the stomach. The main suggested connection between these gastrointestinal diseases and oral infections is that the oral cavity can be a reservoir for this pathogenic microorganism.21-22 In addition, a strong association exists between chronic infection of gastric tissues with H. pylori and the development of stomach cancer.23-24 Data from some epidemiologic studies also suggest an association among periodontal infections, tooth loss, and the development of pancreatic cancer18,24-27 and even lung cancer.18 Although a cause-and-effect relationship between periodontal infections and these conditions has not been shown, the epidemiologic associations are a good justification for more research in this area.
LEGAL, ETHICAL, AND SAFETY ISSUES
KEY CONCEPTS
 Strong evidence supports that periodontal disease is one of several important risk factors for the development of coronary heart disease (atherosclerosis) and nonhemorrhagic (ischemic) stroke. Because these diseases are multifactorial, it is unlikely that periodontal therapy alone will prevent heart attacks and strokes. However, periodontal therapy should be part of a multidisciplinary program of risk reduction that might include smoking cessation, dietary counseling, weight reduction, and treatment of other chronic infections (e.g., chronic bronchitis caused by Chlamydia pneumoniae and peptic ulcers caused by Helicobacter pylori) (see Chapters 33 and 34).
Strong evidence supports that periodontal disease is one of several important risk factors for the development of coronary heart disease (atherosclerosis) and nonhemorrhagic (ischemic) stroke. Because these diseases are multifactorial, it is unlikely that periodontal therapy alone will prevent heart attacks and strokes. However, periodontal therapy should be part of a multidisciplinary program of risk reduction that might include smoking cessation, dietary counseling, weight reduction, and treatment of other chronic infections (e.g., chronic bronchitis caused by Chlamydia pneumoniae and peptic ulcers caused by Helicobacter pylori) (see Chapters 33 and 34). Convincing data suggest that the presence of moderate to severe periodontitis during pregnancy adversely affects birth outcomes, increases the risk of preeclampsia, and has negative effects on fetal development. Because nonsurgical periodontal therapy during pregnancy has been shown to be safe, it is highly recommended that treatment of periodontal infections should be part of prenatal care programs.
Convincing data suggest that the presence of moderate to severe periodontitis during pregnancy adversely affects birth outcomes, increases the risk of preeclampsia, and has negative effects on fetal development. Because nonsurgical periodontal therapy during pregnancy has been shown to be safe, it is highly recommended that treatment of periodontal infections should be part of prenatal care programs. A two-way relationship exists between periodontitis and diabetes mellitus (DM). Persons with poorly controlled DM are at an elevated risk for developing periodontitis because of a number of DM-associated factors that increase susceptibility to infections. The presence of untreated infections, including periodontitis, makes the metabolic control of DM more difficult. Treatment of periodontitis in persons with DM positively affects both oral and systemic health.
A two-way relationship exists between periodontitis and diabetes mellitus (DM). Persons with poorly controlled DM are at an elevated risk for developing periodontitis because of a number of DM-associated factors that increase susceptibility to infections. The presence of untreated infections, including periodontitis, makes the metabolic control of DM more difficult. Treatment of periodontitis in persons with DM positively affects both oral and systemic health.1. Armitage G.C. Periodontal infections and cardiovascular disease—how strong is the association? Oral Dis. 2000;6:335.
2. Paquette D.W., Brodala N., Nichols T.C. Cardiovascular disease, inflammation, and periodontal infection. Periodontology 2000. 2007;44:113.
3. Tonetti M.S., D'Aiuto F., Nibali L., et al. Treatment of periodontitis and endothelial function. N Engl J Med. 2007;356:911.
4. Engebretson S.P., Lamster I.B., Elkind M.S.V., et al. Radiographic measures of chronic periodontitis and carotid artery plaque. Stroke. 2005;36:561.
5. Michalowicz B.S., Durand R. Maternal periodontal disease and spontaneous preterm birth. Periodontology. 2007;2000(44):103.
6. Offenbacher S., Boggess K.A., Murtha A.P., et al. Progressive periodontal disease and risk of very preterm delivery. Obstet Gynecol. 2006;107:29.
7. Boggess K.A., Moss K., Madianos P., et al. Fetal immune response to oral pathogens and risk of preterm birth. Am J Obstet Gynecol. 2005;193:1121.
8. Boggess K.A., Beck J.D., Murtha A.P., et al. Maternal periodontal disease in early pregnancy and risk for a small-for-gestational-age infant. Am J Obstet Gynecol. 2006;194:1316.
9. Boggess K.A., Lieff S., Murtha A.P., et al. Maternal periodontal disease is associated with an increased risk of preeclampsia. Obstet Gynecol. 2003;101:227.
10. López N.J., Smith P.C., Gutierrez J. Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: a randomized controlled trial. J Periodontol. 2002;73:911.
11. Michalowicz B.S., Hodges J.S., DiAngelis A.J., et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355:1885.
12. Apatzidou D.A., Kinane D.F. Quadrant root planing versus same-day full-mouth root planing. I. Clinical findings. J Clin Periodontol. 2004;31:132.
13. Mealey B.L., Ocampo G.L. Diabetes mellitus and periodontal disease. Periodontology 2000. 2007;44:127.
14. Faria-Almeida R., Navarro A., Bascones A. Clinical and metabolic changes after conventional treatment of type 2 diabetic patients with chronic periodontitis. J Periodontol. 2006;77:591.
15. Raghavendran K., Mylotte J.M., Scannapieco F.A. Nursing home–associated pneumonia, hospital-acquired pneumonia and ventilator-associated pneumonia: the contribution of dental biofilms and periodontal inflammation. Periodontology. 2007;2000(44):164.
16. Scannapieco F.A., Bush R.B., Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann Periodontol. 2003;8:54.
17. Mori H., Hirasawa H., Oda S., et al. Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med. 2006;32:230.
18. Hujoel P.P., Drangsholt M., Spiekerman C., Weiss N.S. An exploration of the periodontitis-cancer association. Ann Epidemiol. 2003;13:312.
19. Corson M.A., Postlethwaite K.P., Seymour R.A. Are dental infections a cause of brain abscess? Case report and review of the literature. Oral Dis. 2001;7:61.
20. Riviere G.R., Riviere K.H., Smith K.S. Molecular and immunological evidence of oral Treponema in the human brain and their association with Alzheimer's disease. Oral Microbiol Immunol. 2002;17:113.
21. Stein P.S., Desrosiers M., Donegan S.J., et al. Tooth loss, dementia and neuropathology in the Nun Study. J Am Dent Assoc. 2007;139:1314.
22. Dye B., Kruszon-Moran D., McQuillan G. The relationship between periodontal disease attributes and Helicobacter pylori infection among adults in the United States. Am J Public Health. 2002;92:1809.
23. Umeda M., Kobayashi H., Takeuchi Y., et al. High prevalence of Helicobacter pylori detected by PCR in the oral cavities of periodontitis patients. J Periodontol. 2003;74:129.
24. Stolzenberg-Solomon R.Z., Blaser M.J., Limburg P.J., et al. Helicobacter pylori seropositivity as a risk factor for pancreatic cancer. J Natl Cancer Inst. 2001;93:937.
25. Stolzenberg-Solomon R.Z., Dodd K.W., Blaser M.J., et al. Tooth loss, pancreatic cancer. Helicobacter pylori, Am J Clin Nutr. 2003;78:176.
26. Abnet C.C., Kamangar F., Dawsey S.M., et al. Tooth loss is associated with increased risk of gastric non-cardia adenocarcinoma in a cohort of Finnish smokers. Scand J Gastroenterol. 2005;40:681.
27. Michaud D.S., Joshipura K., Giovannucci E., Fuchs C.S. A prospective study of periodontal disease and pancreatic cancer in U.S. male health professionals. J Natl Cancer Inst. 2007;99:171.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..