Chapter 56Diagnosis and Management of Osteochondrosis and Osseous Cystlike Lesions
The pathogenesis of osteochondrosis (OC), palmar or plantar osteochondral fragments of the proximal phalanx, ununited palmar or plantar eminences of the proximal phalanx, subchondral bone cysts, and other osseous cystlike lesions is discussed in Chapters 36, 42, and 54. In this book the term subchondral bone cyst is used for large radiolucent areas in the subchondral bone of the medial femoral condyle; these cysts have a consistent pathological structure with a true cellular cyst lining. Osseous cystlike lesions in other locations vary more in structure. This chapter discusses the diagnosis and management of these lesions and other osseous fragments believed to be at least predominantly developmental in origin. The joints most commonly affected include the hock, stifle, fetlock, and shoulder. It is common for matching joints to have lesions but much less common to find OC lesions in different joints. This is consistent with the concept of such lesions occurring during some finite window of vulnerability during development that is specific for a given anatomical location.
Clinical signs of OC range from none to severe lameness. Moderate-to-severe joint effusion often occurs with minimal or no lameness. The clinical signs are not necessarily coincident with the development of the lesion. Most OC lesions are probably formed before 6 months of age, yet most are diagnosed at a later age. Some lesions seen radiologically heal, or they at least become stable enough never to cause a clinically apparent lameness. Lesions in racing Thoroughbreds (TBs) and Standardbreds (STBs) are usually recognized by 2 years of age, but in Warmbloods (WBLs) that are older when they begin training, clinical signs may not be seen until the horse is 5 to 6 years of age or even older. Acute, more severe lameness in older horses occurs occasionally when osteochondritis dissecans (OCD) fragments become loose.
Diagnosis is based on typical clinical signs and radiology. Most OCD flaps in horses have an osseous component and so can be identified using plain radiography. Defects in subchondral bone contours are also easily identified. Radiologically apparent defects in subchondral bone must be interpreted with caution in foals, especially in areas where endochondral ossification occurs later, such as the femoral or talar trochlear ridges and the third metacarpal or metatarsal sagittal ridge. An irregularity in the contour of subchondral bone does not mean that an articular defect is necessarily present; the lesion still possibly may heal. Therefore surgical intervention should be delayed until it is clear that either a loose fragment is present or the healing is progressing inadequately. Radiologically apparent lesions must always be interpreted with the clinical signs, because some do not cause clinical signs. If a lesion is identified, the contralateral joint should always be examined radiologically, because bilateral involvement (quadrilateral in the fetlock) is common. The presence of bilateral radiologically apparent lesions in a horse that is unilaterally lame is not unusual and further emphasizes the need to clinically evaluate the individual horse fully.
Decisions concerning treatment should take into consideration the age of the horse, its intended use, the severity of the lesions and anatomical location, whether the horse is intended for sale through public auction, and, if so, the timing of the sale and the conditions of sale. Prophylactic removal of OCD lesions for economic reasons may be justified in all horses intended for future sale. Most buyers are more willing to purchase horses after an OCD lesion has been removed and the horse has returned to work.
Lesions in the Metacarpophalangeal and Metatarsophalangeal Joints
Osteochondritis Dissecans of the Sagittal Ridge of the Third Metacarpal and Metatarsal Bones
Most foals and yearlings with OCD lesions of the sagittal ridge of the third metacarpal bone (McIII) or third metatarsal bone (MtIII) are not recognized as lame. A variable degree of joint effusion occurs, and the lesions are usually first identified on presale radiographs. Unstable lesions cause lameness and persistent effusion when a horse starts work. Lameness is eliminated by intraarticular or perineural analgesia.
Lesions are more common in the MtIII than in the McIII, but all fetlocks should be examined radiologically if a lesion is recognized in one, using perfectly exposed (or slightly underexposed) flexed lateromedial images (Figure 56-1). Lesions on the dorsoproximal aspect of the sagittal ridge are easiest to recognize, but lesions may occur farther distally or, less commonly, on the palmar or plantar aspect of the sagittal ridge. The latter can also be seen radiologically on the dorsopalmar (plantar) image. The larger fragments extend abaxially along the proximal margin of the articular cartilage under the dorsal synovial fold.

Fig. 56-1 A typical distal sagittal ridge osteochondritis dissecans lesion (arrows) of the third metacarpal bone is seen best on a slightly underexposed flexed lateromedial radiographic image (A) and a well-exposed dorsopalmar image (B).
Conservative management should always be considered in horses younger than 18 months old, because lesions can show improvement radiologically and presumably heal. Surgery is indicated in young horses with fetlock effusion and lameness. Young horses treated surgically often do well clinically, but the long-term radiological appearance is inferior to that seen in horses in which the lesions heal spontaneously. Older horses of training age with unstable fragments are treated by arthroscopic debridement. Proximal lesions are technically easy to approach and debride, but lesions that are more distal can be exposed only by slight or moderate flexion of the joint. The arthroscope portal therefore should be made more distal than usual, and a needle should be used to identify a suitable instrument portal. Debriding a sagittal ridge lesion with a portal placed through the extensor tendon directly over the lesion is easiest. Long reaches across a flexed joint may result in undesirable iatrogenic trauma.
The prognosis depends on the size and location of the flap. Probably 90% of horses with typical lesions of the more proximal portion of the sagittal ridge go on to athletic function. Horses with distal lesions in a more weight-bearing location do not do as well as those with flaps at the proximal articular margin, and the radiological appearance does not improve spontaneously as often.
Osseous Cystlike Lesions
Osseous cystlike lesions occur on the weight-bearing surface of the condyles of the McIII and the MtIII. Most occur in the medial condyle and are diagnosed in horses 1 to 2 years of age. The lesions are easy to recognize radiologically (Figure 56-2) and result in obvious lameness, exacerbated by distal limb flexion. Lameness is improved by perineural or intraarticular analgesia. Lameness associated with an osseous cystlike lesion sometimes occurs in foals. At the time of onset of lameness no lesion may be identifiable radiologically, or only a subtle defect in the outline of the subchondral bone may be apparent. However, sequential radiographs obtained over the following 6 to 8 weeks may reveal development of an osseous cystlike lesion. Surgical debridement may be successful,1 but corticosteroids administered intraarticularly or intralesionally also may result in clinically significant improvement in young horses. Although simple debridement of the McIII and the MtIII osseous cystlike lesions has been reasonably successful, the intensity of loading on the distal aspect of the McIII and the MtIII in athletic horses makes horses with these lesions good candidates for advanced joint resurfacing techniques.
Palmar or Plantar Osteochondral Fragments of the Proximal Phalanx
Osteochondral fragments arising from the proximal palmar or plantar aspect of the proximal phalanx are common radiological findings in WBLs, STBs, and TBs, especially in the hindlimbs. Palmar or plantar osteochondral fragments and ununited palmar or plantar eminences may not cause clinical signs or merely cause mild discomfort at high levels of performance. Assessment of clinical importance and management are discussed in detail in Chapters 36 and 42.
Osteochondral Fragments on the Dorsoproximal Aspect of the Proximal Phalanx
Small, well-rounded osseous opacities on the dorsoproximal aspect of the proximal phalanx are common radiological findings. Most probably occur as small chip fractures of the developing dorsal rim of the proximal phalanx in foals that subsequently ossify. Whether a true underlying developmental defect (OCD) in this location exists is unclear. Although fragments in this location do not always cause overt lameness, they often are removed in valuable prospective athletic horses and sales horses. Many of these fragments are loosely tethered along the dorsal rim of the proximal phalanx and can cause damage to the distal aspect of the McIII or the MtIII in an intensively exercised horse. Arthroscopic removal is quick and easy, and the prognosis is close to 100% for full function. Horses can be returned to full work within 4 to 6 weeks after removal of these fragments. Often fragments in this location are removed before horses enter training or before a public auction.
Lesions of the Proximal Interphalangeal Joint
Lesions in the proximal interphalangeal joint usually cause lameness at a young age, often when the horse is a weanling. Single, discrete, well-defined osseous cystlike lesions or multiple poorly defined radiolucent lesions may be identified, occurring most commonly in the distal condyles of the proximal phalanx (Figure 56-3). Surgical access to most pastern osseous cystlike lesions is difficult, and simple debridement is not usually feasible. Lesions may be advanced when lameness is first recognized, and although occasionally horses spontaneously improve without treatment, horses that are obviously lame usually develop osteoarthritis (OA). Therefore horses that do not respond adequately to corticosteroids administered intraarticularly probably should have an early arthrodesis, especially if a hindlimb is affected. Arthrodesis in young or small horses has been accomplished with one of the well-described techniques using two or three transarticular 5.5-mm screws placed in lag fashion2-5 or a three-hole narrow plate and two transarticular screws.6 In larger horses I currently use two to four transarticular 5.5-mm screws and a central dorsal three-hole locking pastern arthrodesis plate.7 The prognosis for athletic function after pastern arthrodesis appears to depend highly on the desired level of activity. Little doubt exists, however, that the prognosis is far superior in a hindlimb than in a forelimb. Most retrospective studies have reported greater than 80% return to athletic function after a hindlimb pastern arthrodesis, but prognosis after a forelimb arthrodesis is likely only around 50%. The intensity of the exercise is probably critical. Few successful elite-level athletic horses (racehorses, upper-level dressage horses, jumping horses) have fused front pastern joints.

Fig. 56-3 Lateromedial (left) and dorsopalmar (right) radiographic images of a proximal interphalangeal joint. The most common manifestation of osteochondrosis in the pastern is an osseous cystlike lesion (arrows) in the distal aspect of the condyle of the proximal phalanx.
Small osteochondral fragments of the proximal interphalangeal joint occur both dorsally and palmarly or plantarly.8-10 Like the fragments in the fetlock, many of these appear to be juvenile traumatic injuries that are diagnosed later in life, but a developmental cause cannot be excluded. These fragments do not always cause lameness, so perineural or intraarticular analgesia should be used to confirm the clinical significance of the fragments. The dorsal fragments are relatively straightforward to remove arthroscopically. The palmar fragments require a more technically demanding surgery.8
Lesions of the Distal Interphalangeal Joint
Well-rounded osteochondral fragments on the dorsoproximal aspect of the extensor process of the distal phalanx are also believed to be developmental in origin. Small fragments are frequently incidental radiological findings, and treatment is not necessary unless associated lameness exists. Lameness should be improved substantially by intraarticular analgesia. Nuclear scintigraphy may help definitive diagnosis. Treatment of horses with lesions associated with lameness is arthroscopic removal of the fragment. The prognosis is excellent (>90%) if the fragment is removed before OA of the distal interphalangeal joint has developed. These fragments are often well embedded in the extensor tendon insertion, so not all fragments adversely affect joint function. As with many other small osteochondral fragments, removal is sometimes done prophylactically.
Osseous cystlike lesions of the distal phalanx can be large and associated with dramatic lameness (Figures 56-4 and 56-5). The pathogenesis may be similar to that of subchondral bone cysts of the distal aspect of the femur. An attempt usually is made to manage such lesions with medications administered intraarticularly. If that is unsuccessful, intralesional corticosteroid injection under fluoroscopic or computed tomographic guidance through the hoof wall is an option. Arthroscopic debridement in young horses with accessible lesions has resulted in good success.11 Extremely large (deep) cysts can be debrided by removing the extensor process in order to provide access.
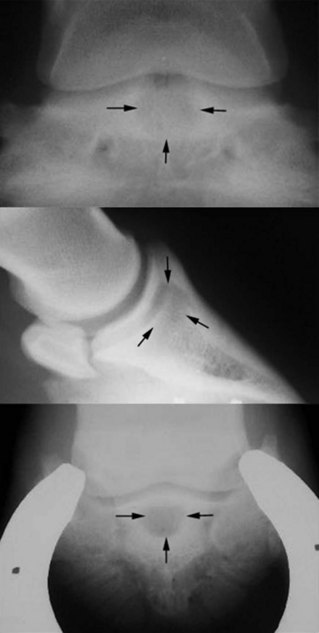
Fig. 56-4 Dorsopalmar (top), lateromedial (middle), and dorsoproximal-palmarodistal oblique (bottom) radiographic images of a foal. There is a large osseous cystlike lesion in the distal phalanx (arrows). Large osseous cystlike lesions of the distal phalanx are difficult management problems because they are relatively inaccessible to surgical debridement.
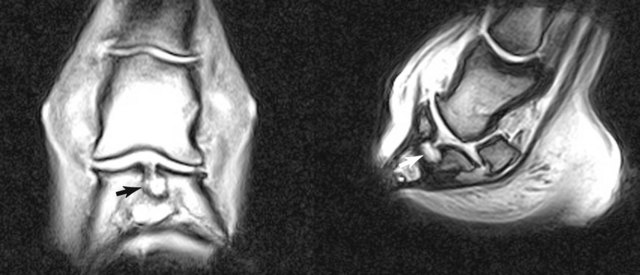
Fig. 56-5 Dorsal (left) and sagittal plane magnetic resonance images of a large osseous cystlike lesion of the distal phalanx. There is a large round area of increased signal intensity (arrows) in the subchondral bone of the distal phalanx that appears to communicate with the articular surface of the distal interphalangeal joint. Intralesional or intraarticular corticosteroids are often used to treat horses with such lesions, but debridement is feasible using an arthroscopic technique.
Lesions of the Scapulohumeral Joint
OC of the scapulohumeral joint may involve the glenoid of the scapula or the humeral head. Humeral head lesions can be solitary, but scapular lesions usually appear with substantial pathological abnormalities of the humeral head in young horses (<2 years old). Lameness can develop insidiously or acutely, presumably after an acute disruption of an unstable osteochondral flap. Recognizing a developing flexural deformity or clubfoot may confuse diagnosis of shoulder lameness in a chronically lame young horse. Occasionally, mild lesions are not recognized until a horse starts training. Lameness is improved by intraarticular analgesia but often is not eliminated. Radiological abnormalities may include poorly defined subchondral radiolucent areas, with or without sclerosis, flattening of the articular surfaces, and modeling of the articular margins, especially the ventral angle of the scapula (see Chapter 40).
Lameness in some young horses improves with rest, and early surgery should not be encouraged in foals younger than 8 to 10 months old unless they are intractably lame. Affected foals should be confined to a stall or small paddock and reexamined clinically and radiologically at 60-day intervals. Intraarticular medication has not been consistently helpful in weanlings and yearlings. The outcome after arthroscopic treatment of OC of the scapulohumeral joint is unpredictable, and lameness can dramatically worsen after surgery. Of 26 potential racehorses, only four (15.4%) started a race, whereas four of six nonracehorses were sound in a recent study of 32 horses that underwent management for osteochondrosis of the scapulohumeral joint.12 There were no differences between horses managed surgically and those managed conservatively.12 Radiography may underestimate the severity of lesions, especially those involving the humeral head. It is important to emphasize to an owner before surgery that considerable uncertainty exists about the clinical outcome in any given horse with OC in the shoulder. Solitary osseous cystlike lesions also occur, most commonly in the middle of the distal aspect of the scapula but sometimes in the humeral head (see Chapter 40, Figure 40-14).
Osteochondrosis of the Tarsocrural Joint
OC of the tarsocrural joint is common in many breeds. Obvious joint capsule distention (bog spavin) may precede recognition of any gait abnormality. Effusion may not be recognized in racehorses examined for poor performance associated with OC, but in show horses with lameness, effusion almost invariably occurs. Horses with radiologically identified lesions are not always lame; therefore diagnosis should be confirmed by intraarticular analgesia or by response to intraarticular medication with corticosteroids. At least four radiographic images should be obtained, because numerous lesions may be present. If OC is suspected clinically but no lesion is identified radiologically, repeating the dorsoplantar image with slightly different angles of projection is worthwhile, because medial malleolar lesions can be difficult to see (Figure 56-6). Flexed lateromedial images may be necessary to identify lesions involving the plantar aspect of the tarsocrural joint.
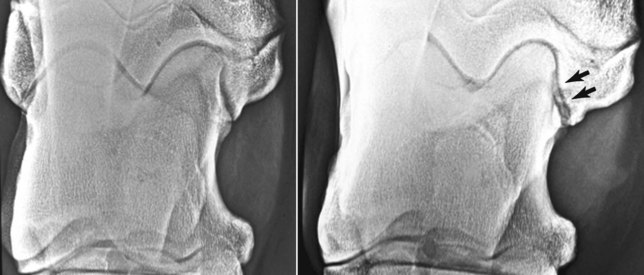
Fig. 56-6 Dorsoplantar (left image) and dorsal 10° lateral-plantaromedial oblique xeroradiographic images of a hock. Identification of osteochondritis dissecans lesions of the medial malleolus requires well-positioned radiographic images. Identifying the lesion on the dorsoplantar image is difficult, but a slight alteration in the obliquity (right image) reveals a large defect (arrows).
OC of the tarsocrural joint is recognized as a common radiological finding in STBs, TBs, and WBLs, but it is not always associated with lameness. Few of the common OC lesions in the hock heal spontaneously after 5 months of age, so surgical removal in young horses, especially sales yearlings, has become commonplace. These lesions are almost always in peripheral, less than completely weight-bearing locations, and removal does not seriously compromise joint function. Prognosis is excellent. However, fragments that cause lameness at a later age are a greater problem because the loose fragments and debris often cause extensive cartilage damage. Older show jumpers in particular may dislodge distal tibial OCD lesions and develop acute clinical signs of effusion and lameness (Figure 56-7).

Fig. 56-7 Dorsomedial-plantarolateral oblique radiographic image of the hock of an adult jumper. A defect (arrowheads) is evident in the cranial aspect of the intermediate ridge of the tibia. The osteochondritis dissecans fragment displaced from that location was crushed into numerous pieces distributed throughout the tarsocrural joint (arrows).
The cranial aspect of the intermediate ridge of the tibia is the most common site of lesions (Figure 56-8). These lesions rarely cause overt lameness unless major effusion occurs. Arthroscopic removal of the fragment is straightforward and nearly always results in reduction of the lameness and effusion. Lesions may be identified radiologically bilaterally, although only one limb is chronically affected. Loose fragments may become detached in the tarsocrural joint and can become lodged in the communicating proximal intertarsal joint (see Figure 56-8). The opening from the tarsocrural joint into the proximal intertarsal joint at the distal margin of the talar trochlear groove is small or not patent or is small in young foals or weanlings, but as the opening enlarges in older horses, large fragments can move into the proximal intertarsal joint pouches.13 If a fragment of bone is found dorsal to (or even on the distal edge of) the central tarsal bone, the fragment is probably one loose in the proximal intertarsal joint that gravitated into that pouch. Fragments associated with lameness should be removed, but it is certainly possible for fragments to localize in this joint and remain stable, causing no clinical signs. It is important to recognize that the fragments in the proximal intertarsal joint usually are not easily seen with an arthroscope and often have to be removed blindly with a rongeurs guided arthroscopically into the joint pouch.

Fig. 56-8 Dorsomedial-plantarolateral oblique radiographic image of a hock with a loose osteochondritis dissecans fragment in the proximal intertarsal joint (open arrow). This fragment (open arrow) “dropped” from the cranial aspect of the intermediate ridge of the tibia, where a larger fragment still resides (arrows).
Lesions of the distal aspect of the lateral trochlear ridge of the talus can be enormous and if loose may cause acute severe lameness and substantial effusion (Figure 56-9). This lesion seems to be more common in heavy breeds and STBs. Horses with small, well-attached lesions can be managed conservatively, but any displaced fragment should be removed. The prognosis generally depends on how proximally and axially the lesion extends, but even large lesions can be removed with a good prognosis.

Fig. 56-9 Dorsomedial-plantarolateral oblique xeroradiographic image of a hock. Osteochondritis dissecans fragments (arrow) arising from the distal aspect of the lateral trochlear ridge of the talus are often large, but after surgical removal horses have a good prognosis regardless of size of the lesion.
OCD lesions of the medial malleolus of the tibia are easily missed because they are always on the axial rather than the distal (more visible) part of the malleolus (see Figure 56-6). Medial malleolar OCD lesions usually cause more lameness and more effusion than the more common lesions of the cranial aspect of the intermediate ridge of the tibia. Unless the lesion is unusually large, the prognosis after arthroscopic removal is excellent. Early removal is recommended, because erosive lesions on the medial trochlea of the talus can become severe over time.
Medial trochlear ridge lesions should be interpreted with caution; most distal medial trochlear ridge lesions are incidental radiological findings, and affected horses do not require treatment. Some fragments ostensibly are unstable or somehow irritating because they will be associated with clinical signs (Figure 56-10). Distal medial trochlear ridge lesions may be on the proximal or distal side of the capsular attachment separating the tarsocrural and proximal intertarsal joints. These fragments can reliably be seen only in a lateromedial radiographic image, a radiological finding that is useful to differentiate horses with distal medial trochlear ridge fragments and those with loose fragments within the proximal intertarsal joint. The fragments wholly within the tarsocrural joint appear to be less stable and more likely to cause lameness. In all horses the decision for surgical removal should be based on a definitive response to intraarticular analgesia. The arthroscopic removal of the tarsocrural lesions is easy and can be done with minimal dissection. Lesions under the capsular attachment often require sharp dissection of the attachment to expose the fragment. Care should always be taken to dissect the minimal amount of soft tissue, especially because the attachments course abaxially.

Fig. 56-10 Lateromedial radiographic image of a hock. Small fragments (arrows) along the distal dorsal aspect of the medial trochlear ridge of the talus commonly do not cause lameness, but some are unstable and induce effusion and lameness, particularly fragments on the proximal side of the proximal intertarsal joint capsule.
More centrally positioned, smoothly outlined depressions in the surface of the medial trochlear ridge of the talus are common in large WBLs, draft horses, and draft-cross horses. The subchondral bone architecture is usually normal, and no associated clinical signs are apparent. These lesions rarely have an unstable chondral or osteochondral flap that can be removed.
Lateral malleolar fragments are usually traumatic (see Chapter 44) and are only rarely (about 1%) OC lesions. Unlike the traumatic fractures, lateral malleolar OCD lesions have irregular diffuse radiolucency within the malleolus instead of a distinctly separated fragment. Arthroscopic debridement of lateral malleolar OCD lesions is difficult because of the extensive collateral ligament attachments that obscure the structure.
Arthroscopic removal of OCD lesions from the hock usually can be followed by a short convalescence and rapid return to work or pasture exercise. Typically a horse is walked in hand for 4 to 6 weeks and then reevaluated. If the effusion has resolved and the horse is jogging soundly, the level of exercise can be increased steadily. Sodium hyaluronan is administered intraarticularly at about the time of suture removal.
Most horses with OCD of the hock have an excellent prognosis, especially if lesions are removed early, before substantial damage to the joint occurs. The specific location of the OCD lesion probably makes less difference than the size, because most hock OCD lesions occur on the peripheral, less than fully weight-bearing surfaces of the bones. Controversy remains about the need to remove all hock OCD lesions, but clearly horses have an excellent (>80%) chance of performing at the expected level after arthroscopic removal of typical lesions.14-16
The tarsocrural joint appears to be particularly vulnerable to a form of erosive OA that can result in extensive, full-thickness loss of articular cartilage (Figure 56-11). This occurs in the absence of known trauma or radiologically evident lesions, but most horses with the lesion have a history of intraarticularly administered corticosteroids used to manage an effusion. The exact mechanism of this process in the tarsocrural joint is not known, but corticosteroids should be used cautiously to manage effusions of this joint.
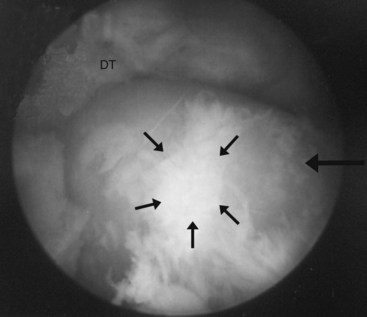
Fig. 56-11 Unlike in most other joints in the horse, full-thickness cartilage erosion of the talus (medial trochlear ridge) (large arrow) and distal aspect of the tibia (DT) occurs with surprisingly few bony changes such as subchondral lysis or marginal osteophytes. Arthroscopy affords the best means of making the diagnosis. The medial trochlear ridge is nearly devoid of cartilage except for loose and fibrillated cartilage on its summit (small arrows).
Lesions of the Stifle
Diagnosis and management of OC of the femoropatellar joint, subchondral bone cysts in the medial femoral condyle, and other osseous cystlike lesions in the stifle are discussed in detail in Chapter 46.
