Chapter 40The Elbow, Brachium, and Shoulder
Anatomical Considerations
The elbow joint consists of the humerus, radius, and ulna. The distal aspect of the humerus develops from three ossification centers: the diaphysis, the distal epiphysis, and the epiphysis of the medial condyle. These close radiologically at 11 to 24 months of age. The radius and ulna have a single proximal epiphysis. The radial physis closes radiologically at 11 to 24 months of age, but the ulnar physis does not close until 24 to 36 months of age. Physeal closure occurs later in non-Thoroughbred (TB) breeds.
The cranial aspect of the olecranon of the ulna has articular and nonarticular components. The anconeal process and trochlear notch articulate with the humerus. At the distal part of the trochlear notch is a distinct ridge. Distal to this is a large, non–weight-bearing synovial fossa.
The elbow is a ginglymus joint, supported medially and laterally by collateral ligaments. The medial collateral ligament consists of a long superficial part and a deeper short part. The medial collateral ligament arises from an eminence on the medial epicondyle of the humerus. The deep part inserts on the radial tuberosity; the superficial part inserts on a more distal prominence, just distal to the interosseous space between the radius and ulna. The lateral collateral ligament arises from a depression in the lateral epicondyle of the humerus and inserts on the lateral tuberosity of the radius, just distal to the joint margin. The joint capsule is extremely thin caudally, where it forms a pouch in the olecranon fossa. Cranially the joint capsule is strengthened by oblique fibers and blends with the collateral ligaments medially and laterally.
The most readily palpable landmarks are the olecranon of the ulna and the lateral collateral ligament of the humeroradial joint. Minimal soft tissue covers the lateral aspect of the elbow, making it vulnerable to the effects of direct trauma and penetrating wounds.
The humerus is surrounded by muscles, which largely protect it from the effects of direct trauma. The deltoid tuberosity on the craniolateral aspect is usually readily palpable and is potentially vulnerable to the effects of direct trauma. The deltoid tuberosity is the most useful landmark for identifying the point for needle insertion for synoviocentesis of the intertubercular (bicipital) bursa. The proximal aspect of the humerus has several centers of ossification for the humeral head and the greater and lesser tubercles, which gradually fuse at 3 to 5 months of age. Radiological closure of the proximal humeral physis occurs at 24 to 36 months of age.
The scapula has four centers of ossification: the scapular cartilage, body of the scapula, cranial part of the glenoid cavity of the scapula, and supraglenoid tubercle and coracoid process. The ossification center for the cranial part of the glenoid cavity fuses directly with the body of the scapula, and this is complete radiologically by 5 months of age. The physis between the supraglenoid tubercle and coracoid process and the body of the scapula closes radiologically at 12 to 24 months of age—earlier in TB and TB crossbreeds than in ponies. These physeal lines remain weak links, and it is through these that fractures of the supraglenoid tubercle and cranial part of the glenoid cavity of the scapula tend to occur.
The scapula is attached by the serratus ventralis muscles to the axial skeleton. Other muscles involved in attachment of the thoracic limb to the trunk and neck are the four pectoral muscles, the brachiocephalicus, and omotransversarius.
The brachial plexus lies on the axial aspect of the scapula and is derived from the sixth, seventh, and eighth cervical nerve roots and the first thoracic nerve. These nerve roots are potentially vulnerable to trauma where they exit the cervical and cranial thoracic vertebrae, and these are relatively common sites for neuroma formation after trauma. The nerves of the brachial plexus are responsible for innervation of many of the principal muscles of the shoulder region.
The scapulohumeral or shoulder joint is unusual because of the absence of collateral ligaments. Stability therefore depends on muscular support on the medial and lateral aspects by the subscapularis, teres minor, infraspinatus, and supraspinatus. Cranial support is provided by the biceps brachii and supraspinatus, and caudal support is rendered by the long head of the triceps brachii. Overlying muscles make it impossible in mature horses to appreciate distention of the joint capsule by palpation. The joint capsule attaches closely to the margins of the scapulohumeral joint, and this, together with the surrounding muscles, restricts arthroscopic evaluation within the joint. The suprascapular nerve wraps around the cranial margin of the scapula proximal to the supraglenoid tubercle and provides innervation to the infraspinatus and supraspinatus muscles.
Considering its embryological development and function, the so-called intertubercular (bicipital) bursa would be more appropriately called a tendon sheath.1 The bursa surrounds the tendon of biceps brachii, which originates from the supraglenoid tubercle of the scapula. The craniodistal pull of the biceps brachii results in cranial and distal displacement of fractures of the supraglenoid tubercle. Communication was identified between the scapulohumeral joint capsule and the intertubercular bursa using contrast arthrography in 3 of 18 limbs (17%)2; thus in some horses intraarticular analgesia of the scapulohumeral joint has the potential to cause improvement in lameness caused by pain arising from the intertubercular bursa. The tendon of biceps brachii is partially cartilaginous proximally and passes over the smooth intertuberal groove of the humerus and then becomes predominantly muscular with a tendonous core.
The most important palpable landmarks in the shoulder region are the cranial and caudal eminences of the greater tubercle of the humerus. The notch between these eminences provides the portal for arthrocentesis of the scapulohumeral joint. The scapular spine is usually readily palpable except in exceptionally fat horses or heavily muscled individuals and becomes more prominent if the supraspinatus or infraspinatus muscles atrophy.
Diagnosis
Clinical Signs
In the adult horse lameness associated with the elbow or shoulder region is comparatively rare, except after direct trauma caused by a fall, collision with a solid object such as a gatepost, or collision with another horse. In immature athletic horses, stress fractures of the scapula, humerus, and radius; osseous cystlike lesions; and osteochondrosis are quite common.
Lameness associated with the shoulder or elbow region is usually sudden in onset and generally moderate to severe. After trauma to the shoulder or elbow, or in association with severe lameness, the horse tends to stand with its weight inclined toward the contralateral limb, not fully load bearing on the lame limb. The horse may resent turning on the limb. Muscle atrophy in the shoulder region is not specific for lameness associated with the proximal aspect of the limb but is often more severe than if the pain arises farther distally. Rapid loss of the bulk of supraspinatus and infraspinatus muscles alone is likely to reflect damage to the suprascapular nerve, whereas involvement of additional muscles is more likely to reflect a brachial plexus injury. Swelling in the elbow or shoulder region usually reflects direct trauma but may be seen with subluxation or luxation of the shoulder or elbow joint. Patchy sweating is sometimes seen with a lesion of the brachial plexus. Pain elicited by deep palpation is relatively unusual and is generally associated with direct trauma. Care should always be taken to compare the reaction with that to palpation of the contralateral limb. The reaction to manipulation of the proximal limb joints should also be interpreted with care because many normal horses resent extreme flexion, extension, or abduction.
Many normal horses show some resentment of firm palpation of the brachiocephalicus muscles at the base of the neck. These muscles often become sore with a more distal source of pain causing lameness. Primary muscle pain causing lameness does sometimes occur and is associated with a more marked pain reaction on palpation and muscle spasm. It may cause a lameness most evident when the horse is ridden at the walk, characterized by lifting of the head and neck as the ipsilateral limb is protracted. Lesions of the tendon of biceps brachii are also sometimes associated with lameness that is worse at walk than trot.
If lameness is mild, then the character of the lameness is nonspecific; but if lameness is moderate to severe, it is often characterized by a shortened cranial phase of the stride, a reduced height of the arc of foot flight, and a marked head lift and nod. ![]() These gait characteristics are evident at the walk and the trot. Observation of the moving horse from the front and the side is particularly useful. The horse may pivot on the lame limb when turning. The gait characteristics of shoulder slip (see page 473) are more easily identified by observing the horse walking toward you. Lameness is frequently accentuated with the lame limb on the outside of a circle. In horses with proximal limb lameness, especially associated with muscle fibrosis, lameness may be evident only when the horse is ridden, performing specific movements. Manipulative tests of the proximal limb joints are rather nonspecific and frequently unrewarding.
These gait characteristics are evident at the walk and the trot. Observation of the moving horse from the front and the side is particularly useful. The horse may pivot on the lame limb when turning. The gait characteristics of shoulder slip (see page 473) are more easily identified by observing the horse walking toward you. Lameness is frequently accentuated with the lame limb on the outside of a circle. In horses with proximal limb lameness, especially associated with muscle fibrosis, lameness may be evident only when the horse is ridden, performing specific movements. Manipulative tests of the proximal limb joints are rather nonspecific and frequently unrewarding.
Lameness may fluctuate in degree under different circumstances and within an examination period; therefore it is important to observe the horse for a sufficient length of time before proceeding with local analgesic techniques. If lameness is apparent only when the horse is ridden, the horse may be sensitive to the diagonal on which the rider sits.
Lameness caused by trauma resulting in only bruising usually improves rapidly, within a few days. Persistence of lameness merits further investigation.
Local Analgesia
It is important to recognize the potential effect of a median nerve block, performed in the proximal antebrachium, on elbow pain. Elbow lameness may be substantially improved, presumably because of local diffusion of the local anesthetic solution. Techniques for intraarticular analgesia of the elbow and shoulder and intrathecal analgesia of the intertubercular bursa are described in detail in Chapter 10. Intraarticular analgesia of the elbow and shoulder joints usually improves but rarely eliminates pain associated with either joint. The elbow and shoulder joints are relatively large; therefore use of at least 10 mL of local anesthetic solution (mepivacaine, 2%) is recommended for the elbow joint and 20 mL for the shoulder joint. Retrieving synovial fluid from each joint is usually possible. Absence of resistance to injection is not a guarantee that the needle is in an intraarticular location. Walking the horse after the block facilitates circulation of the local anesthetic solution throughout the joint. Although improvement in lameness may be seen rapidly, within 10 to 15 minutes after injection, at least 1 hour should elapse after the block before the result is considered negative. The block generally is effective for up to 2 hours. The block usually has no influence over pain associated with periarticular structures.
When performing intraarticular analgesia of the shoulder, it is important to recognize that there is communication with the intertubercular bursa in some horses. In some horses instability of shoulder, so-called shoulder slip, appears transiently (for up to 2 hours) after injection of local anesthetic solution. This prohibits interpretation of the nerve block. The cause is presumably diffusion of local anesthetic solution to nerves innervating the muscles responsible for maintaining stability of the shoulder. Positive-contrast arthrography has shown that injection of volumes greater than 20 mL pose a danger of pooling at the site of injection or leakage from the joint capsule.. An experimental study demonstrated that deposition of mepivacaine over the suprascapular nerve could result in transient shoulder slip, but this may be the result of diffusion to affect the brachial plexus (see page 473).3
Intrathecal analgesia of the intertubercular bursa may improve lameness associated with lesions of the tendon of biceps brachii, the bursa itself, or the humeral tubercles, but accurate intrathecal injection may not be reliable.4 The bursa is large, and use of 20 mL of local anesthetic solution is recommended.
False-negative results to both intraarticular analgesia of the shoulder and elbow joints and intrathecal analgesia of the intertubercular bursa may occur, and radiological, scintigraphic, and ultrasonographic evaluation of these areas is indicated if clinical signs are suggestive of shoulder or elbow region pain. Many other potential sources of pain in the proximal limb cannot be desensitized by local analgesic techniques. If the response to distal limb analgesia and the blocks described previously is negative, nuclear scintigraphic evaluation may be warranted.
Assessment of Muscles
Electrical stimulation of muscles may help to identify muscle-related pain (see page 824).
Imaging
Radiography and Radiology
Radiographic examination of the elbow requires a minimum of mediolateral and craniocaudal images.5 The limb should be pulled forward sufficiently to avoid the pectoral muscle mass to evaluate the distal aspect of the humerus properly. Additional oblique images may be of value in selected horses. Routine radiographic examination of the scapulohumeral joint should include mediolateral and craniomedial-caudolateral oblique images. In some horses cranioproximal-craniodistal oblique images of the humeral tubercles are useful. Examination of the entire length of the humerus can be difficult, because often when such examination is indicated, the horse has pain and is reluctant to allow the limb to be adequately protracted. Accurate evaluation of the entire scapula is also not easy because of superimposition over the thoracic vertebrae and the contralateral limb.
Fast-speed, rare earth screens and appropriate film are essential if using conventional radiography. Use of a grid will greatly enhance image quality, especially in the shoulder region. High exposure factors are required (e.g., 100 kV, 100 mAs, for a mediolateral image of the shoulder). Underexposure will result in lesions being missed.
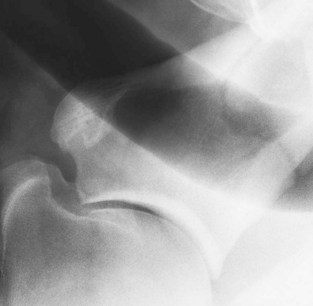
It is important to recognize that the cranial articular margin of the proximal radius has several lips that should not be confused with osteophytes (Figure 40-1). The cranial tuberosity of the proximal aspect of the radius may appear roughened in slightly oblique mediolateral views.

Fig. 40-1 Mediolateral radiographic image of the elbow joint of a normal adult horse. The lips on the cranioproximal aspect of the radius are a normal radiological feature.
In the scapulohumeral joint a small circular radiolucent region is sometimes seen in the subchondral bone in the middle of the glenoid cavity of the scapula (Figure 40-2). A radiolucent edge effect is often seen in the proximal humerus, the result of superimposition of the lateral rim of the glenoid cavity of the scapula.

Fig. 40-2 Mediolateral radiographic image of a scapulohumeral joint of a normal adult horse. There is a small lucent zone in the subchondral bone in the middle of the glenoid cavity of the scapula (arrow). Note also the radiolucent band crossing the humeral head and the edge effect caused by superimposition of the articular margins of the scapula.
Ultrasonography
Diagnostic ultrasonography is invaluable for assessing muscle structure in the shoulder region. Normal muscle has a homogeneous echogenicity. Identification of hyperechogenic regions indicative of muscle necrosis, fibrosis, or mineralization is usually associated with lameness.
Evaluation of the elbow joint itself is limited in the weight-bearing position because of the difficulty in getting access medially. Examination of the lateral collateral ligament of the humeroradial joint is straightforward. For evaluation of the medial aspect, the limb should be pulled forward, but unless the medial collateral ligament is under tension, its echogenicity may lack homogeneity.
In the shoulder region ultrasonography is important for assessing the intertubercular bursa, humeral tubercles, tendon of biceps brachii (Figure 40-3, A and B), tendons of insertion of the supraspinatus and infraspinatus muscles (Figure 40-3, C and D), and the infraspinatus bursa (Figure 40-3, B).6-10 Care should be taken to ensure that the horse is fully load bearing on the limb, because hypoechogenic artifacts can be created, especially in the tendon of biceps brachii, unless the musculature is under tension. The medial and lateral lobes of the tendon of biceps brachii and the isthmus between them should each be evaluated individually, because getting the entire structure into focus simultaneously is difficult.
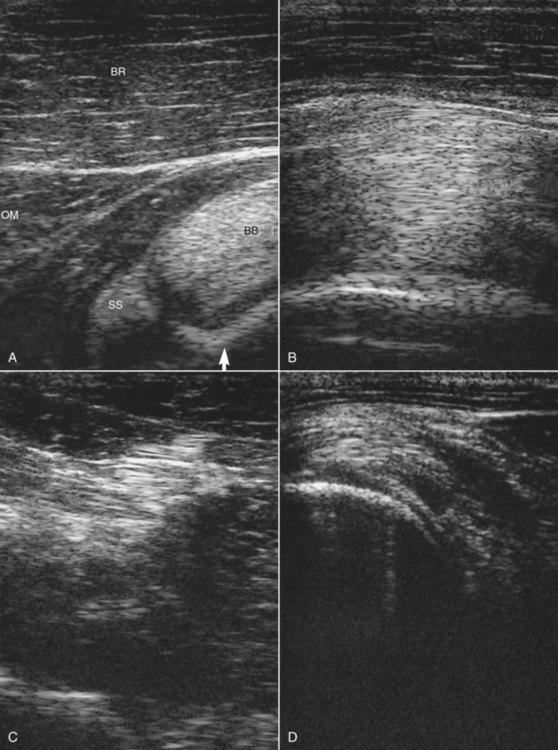
Fig. 40-3 A, Transverse ultrasonographic image of the cranial proximal aspect of the humerus of a normal horse. Medial is left. There is a small amount of anechogenic fluid within the intertubercular bursa, and the contour of the humeral tubercle is smooth (arrow). B, Longitudinal ultrasonographic image of the tendon of biceps brachii and the overlying brachiocephalicus muscle. Proximal is left. C, Transverse image of the tendon of infraspinatus within the infraspinatus muscle. D, Transverse ultrasonographic image of the insertion of the infraspinatus on the proximal aspect of the humerus. The anechogenic space, the infraspinatus bursa, appears between the tendon of insertion and the bone. BB, Medial lobe of the tendon of biceps brachii; BR, brachiocephalicus; OM, omotransversarius; SS, medial tendon of insertion of the supraspinatus.
Nuclear Scintigraphy
Nuclear scintigraphic evaluation of the proximal aspect of the forelimbs is indicated if the responses are negative to median and ulnar nerve blocks, intraarticular analgesia of the elbow and shoulder joints, and intrathecal analgesia of the intertubercular bursa. Scintigraphy is also indicated if history and clinical signs suggest a stress fracture. Scintigraphy has also been useful for identifying enostosis-like lesions (bone islands) in the humerus and fractures of the deltoid tuberosity of the humerus. Care should be taken to localize any region of increased radiopharmaceutical uptake (IRU) as precisely as possible to identify the likely underlying pathological condition. IRU in the first rib can easily be misinterpreted unless a cranial image is obtained to separate the scapula and humerus from the underlying rib. Examination of the scintigraphic images should include careful assessment of the soft tissues, because abnormal uptake of the radiopharmaceutical in muscle can sometimes be identified in bone phase images.
Differential Diagnosis
Elbow
Osteoarthritis
Osteoarthritis (OA) of the elbow is relatively unusual and tends to be seen in older athletic horses. Often the horse has a history of trauma. The horse may resent manipulation of the elbow, but appreciating joint effusion is usually not possible. Lameness often varies in degree, within and between examinations, and is usually worst on a hard surface, especially on a circle.
Intraarticular analgesia improves lameness. Periarticular osteophyte formation, alterations in subchondral bone opacity, and narrowing of joint space width may be seen radiologically (Figure 40-4). Care should be taken not to misinterpret as osteophytes normal bony lips on the dorsoproximal aspect of the radius in a mediolateral image.

Fig. 40-4 Mediolateral (A) and craniocaudal (B) (medial is to the left) radiographic images of the elbow joint of a 9-year-old event horse with left forelimb lameness alleviated by intraarticular analgesia of the elbow. The periarticular osteophytes (arrows) and subtle narrowing of the joint space medially indicate osteoarthritis. The horse failed to respond to intraarticular medication.
The repeated use of intraarticular polysulfated glycosaminoglycans has been most effective in resolving lameness, but the long-term prognosis for return to full athletic function is guarded.
Osseous Cystlike Lesions
Osseous cystlike lesions occur most commonly medially in the proximal radial epiphysis (Figure 40-5) and usually result in acute-onset, relatively severe lameness in immature athletic horses.

Fig. 40-5 Craniocaudal radiographic image of the proximal aspect of the radius of a 3-year-old Thoroughbred racehorse with left forelimb lameness, which substantially improved with intraarticular analgesia of the elbow. There is a well-defined osseous cystlike lesion in the proximomedial aspect of the radius. Note also the periosteal new bone on the proximomedial aspect of the radius. Intraarticular medication with hyaluronan resolved lameness, and the horse raced successfully.
Lameness may vary greatly in degree, within and between examinations, and is usually substantially improved by intraarticular analgesia. In addition to a well-defined osseous cystlike lesion, there is often periosteal new bone on the proximal medial metaphyseal region of the radius. Intraarticular medication with hyaluronan or corticosteroids (triamcinolone acetonide or methylprednisolone acetate) has resulted in successful resolution of lameness.1,11 In some horses the osseous cystlike lesions have resolved radiologically. Surgical treatment by curettage of the cyst using an extraarticular approach has been successful in some horses, but fracture through the cyst has been a recognized complication.12 Recurrent lameness after surgical treatment is also possible.13 An ill-defined osseous cystlike lesion is occasionally seen in older horses with OA of the elbow with no known previous history of lameness; it is likely that the cystlike lesion had been present asymptomatically before the development of pain associated with OA.
Less commonly, large, less well-defined osseous cystlike lesions have been identified in the distal aspect of the humerus in young Thoroughbreds being prepared for the yearling sales or just after entering training.1 Lameness is acute in onset, persists despite box rest, and is generally not influenced by intraarticular analgesia of the elbow. Nuclear scintigraphic examination reveals a region of IRU in the distal aspect of the humerus, more centrally located than that associated with a stress fracture (see page 463). Careful radiological examination reveals a less well-defined osseous cystlike lesion. Conservative management has resulted in persistent lameness, and the results of surgical treatment have been disappointing. Young horses with smaller osseous cystlike lesions in the distal medial humerus have been identified and have responded to conservative management.12
Osteochondrosis
The elbow is a relatively rare location for osteochondrosis, but occasionally lameness is identified in young TBs and STBs in training associated with osteochondrosis lesions of the distal aspect of the humerus or the proximal aspect of the radius. Lameness is improved by intraarticular analgesia. Various radiological changes have been identified. Results of medical and surgical management have been disappointing. Osteochondrosis lesions of the anconeal process of the ulna also occur rarely,14 but they should not be confused with a separate ossification center in young foals.15
Stress Reactions in Subchondral Bone
Intermittent lameness has been identified in a small number of event horses associated with an assumed stress reaction in the subchondral bone of the distal aspect of the humerus.1 Lameness is induced by jumping but tends to resolve if the horse is not jumped. Lameness may be improved by intraarticular analgesia of the elbow (curious). No bony abnormalities have been identified radiologically. Nuclear scintigraphic examination reveals a region of IRU in the subchondral bone of the distal aspect of the humerus. Treatment with box rest and controlled walking exercise for 3 months has resulted in resolution of lameness and a normal distribution of the radiopharmaceutical. Horses have been able to return to full athletic function without recurrent injury.
Collateral Ligament Injury
Injury to the collateral ligaments of the elbow is not common and usually results from a traumatic injury such as a fall. Damage to the lateral collateral ligament has been identified most frequently. Severe injuries may also be associated with injury to the joint capsule, and osteoarthritis may ensue. Lameness is acute in onset. Subtle soft tissue swelling may be appreciated in the elbow region, and manipulation of the elbow may induce pain. Lameness may be partially improved by intraarticular analgesia of the elbow. If damage is restricted to extraarticular structures, then the response may be negative. Nuclear scintigraphic examination may be helpful in these horses. IRU occurs at the sites of ligament attachment on the distal aspect of the humerus and proximal aspect of the radius.
Definitive diagnosis requires ultrasonographic examination and identification of disruption of the normally linear pattern of echoes within the ligament. Sometimes periosteal new bone or avulsion fractures can be identified at the region of ligamentous attachment.16 Radiographic examination should also be performed to identify any concurrent pathological condition of the bone, such as enthesophyte formation, an avulsion fracture, or secondary OA (Figure 40-6).
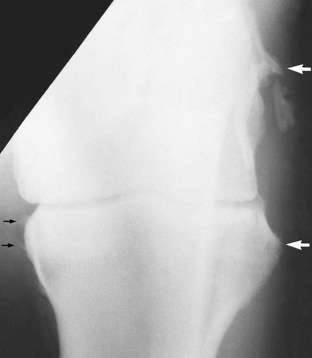
Fig. 40-6 Craniocaudal radiographic image of the elbow of 15-year-old pony that had chronic left forelimb lameness after a fall. There is entheseous new bone at the attachments of the lateral collateral ligament of the humeroradial joint (white arrows) with mineralization within the ligament. There is also new bone on the proximomedial aspect of the radius (black arrows). Periarticular osteophyte formation was also visible in a mediolateral image. Ultrasonographic examination revealed poor fiber pattern within the lateral collateral ligament. Postmortem examination confirmed desmitis of the lateral collateral ligament and osteoarthritis of the elbow joint.
Horses with minor lesions have responded well to a period of box rest and controlled walking exercise, but those with lesions that have been associated with entheseous new bone formation often have had persistent lameness and have developed OA.
Luxation
Luxation of the elbow joint is usually seen with a fracture of the olecranon or proximal aspect of the radius or separation of the radius and ulna, although luxation occasionally occurs alone. Lameness is acute in onset and severe and is associated with considerable swelling in the elbow region. Comprehensive radiographic examination is essential to determine if one or more concurrent fractures are present. Surgical repair can be considered, but the prognosis for athletic function is poor.
Enthesopathy of the Biceps Brachii
Tearing of the attachment of the biceps brachii from the cranioproximal aspect of the radius may be associated with a traumatic injury such as a fall, but frequently history does not suggest the cause. Lameness is sudden in onset and often not associated with any localizing signs, except pain on manipulation of the elbow in horses with acute lameness. The lameness has no particular characteristics. The response to local analgesic techniques is negative. Radiographic examination may reveal periosteal new bone on the cranioproximal aspect of the humerus in horses with chronic lameness17 (Figure 40-7). Sometimes an adjacent mineralized fragment is present, an avulsion fracture or dystrophic mineralization. Some new bone formation on the cranioproximal aspect of the radius can be seen in normal horses, reflecting previous injury; therefore care should be taken in interpreting its current clinical significance. Nuclear scintigraphic examination is helpful for acute lameness before periosteal new bone develops and in horses with chronic lameness. Ultrasonographic evaluation has not been helpful. Treatment is by rest. The prognosis is guarded to fair.
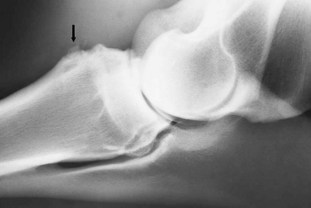
Fig. 40-7 Mediolateral radiographic image of the right elbow of 9-year-old show jumper with chronic right forelimb lameness that no local analgesic technique influenced. There is new bone on the cranial tuberosity of the radius at the site of insertion of the biceps brachii (arrow). Nuclear scintigraphy gave evidence of increased bone modeling at this site. The horse had persistent lameness despite prolonged rest.
Avulsion of the Origin of the Ulnaris Lateralis
The ulnaris lateralis functions to flex the carpus and extend the elbow. An avulsion fracture at the origin of the ulnaris lateralis, from a site caudal and distal to the origin of the lateral collateral ligament of the humeroradial joint, is a rare cause of lameness. Lameness is acute in onset and moderate to severe, following a fall, resulting in diffuse soft tissue swelling on the lateral aspect of the elbow. Diagnosis is based on radiography and ultrasonography. A nonarticular avulsion fragment and enlargement and marked disruption of the tendon of origin of the ulnaris lateralis are present.18
Fracture of the Olecranon
Fracture of the olecranon of the ulna usually results from a kick or fall, resulting in acute-onset, severe lameness. The horse may stand with the elbow dropped because of lack of an effective attachment of the triceps, the principal extensor of the elbow. Soft tissue swelling may or may not be palpable. Traction on the summit of the olecranon elicits pain. Although many fractures are comminuted, detecting crepitus is unusual. Radiographic examination should include mediolateral and craniocaudal images to assess the configuration of the fracture and to identify any other bony lesions (see Figure 13-3). Fractures have been classified into five types19:
A fracture that enters the trochlear notch should be examined carefully to determine whether it involves the articular or nonarticular portion. Treatment by internal fixation usually warrants a fair-to-good prognosis,20-23 provided that the fracture is identified early and unless comminution is excessive. Conservative management has also been successful if the fracture is not displaced; the best results are achieved with type 5 fractures.24 If the horse is treated conservatively, healing should be monitored radiologically to ensure that no displacement has occurred. Potential complications of conservative management include nonunion, OA, development of a flexural deformity or contralateral laminitis, or development of an angular limb deformity in the contralateral limb.
Humerus
Fractures of the Deltoid Tuberosity
Fracture of the deltoid tuberosity of the humerus occurs occasionally.5,25 Often no cause is identifiable, although in some horses trauma has been recognized. Lameness is acute in onset and moderate to severe, depending on the configuration of the fracture. Generally no soft tissue swelling is detectable, although deep palpation in the region may cause pain in acute, but not chronic, injuries. Turning on the limb induces pain. In the absence of localizing signs, nuclear scintigraphic examination may be the best indicator of the injury (Figure 40-8, A).
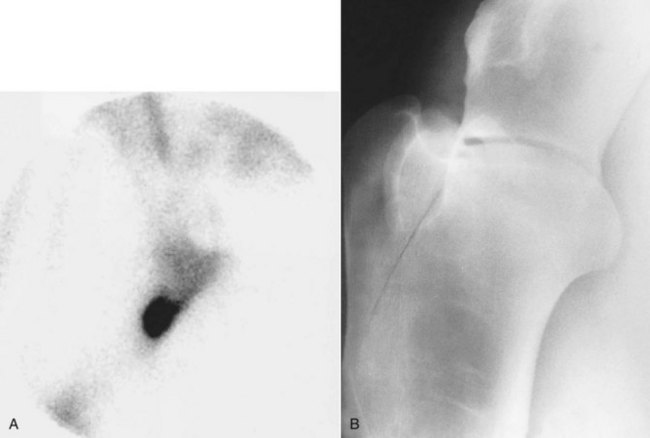
Fig. 40-8 A, Lateral scintigraphic image of the right shoulder of 7-year-old dressage horse with acute-onset, moderately severe lameness of 2 weeks’ duration with no associated localizing clinical signs. There is marked focal increased radiopharmaceutical uptake in the region of the deltoid tuberosity of the humerus. Radiographic examination revealed an incomplete fracture line through the base of the tuberosity and slight periosteal callus. B, Craniomedial-caudolateral oblique radiographic image of the proximal aspect of the humerus of a 3-year-old Thoroughbred broodmare with acute-onset, severe right forelimb lameness. There is an incomplete fracture of the deltoid tuberosity of the humerus. The mare made a complete functional recovery, but a radiologically visible osseous cystlike lesion developed distal to the greater tubercle of the humerus.
Diagnosis is by radiographic examination. A craniomedial-caudolateral oblique image is essential (Figure 40-8, B), because abnormalities may not be detectable in mediolateral images. Several configurations of fracture have been identified: small chip fractures, single or comminuted, a longitudinal fracture through the tuberosity itself, and an incomplete oblique fracture extending proximocaudally through the humeral diaphysis and metaphysis. Conservative management results in a favorable outcome, unless an oblique fracture is displaced, for which internal fixation is recommended. The prognosis is good.
Stress Fractures
Stress fractures of the humerus are relatively common in young Thoroughbreds in training. Humeral stress fractures occur frequently in 3-year-old and older racehorses within 4 to 8 weeks of retraining, and in North America they are often seen from February to April. The most common locations are the proximocaudal aspect of the humerus and the distal cranial and caudal aspects.26-28 Unilateral lameness is usually acute in onset and relatively severe. This lameness often improves relatively rapidly with box rest. Despite preexisting callus formation indicative of previous ongoing bony reaction, previous lameness has often not been recognized. Usually no localizing signs are apparent, and the response to distal limb nerve blocks is negative. Nuclear scintigraphic examination is the most sensitive means of detecting a fracture and should be performed if a stress fracture is suspected on clinical grounds, because premature return to work may potentially result in a more catastrophic fracture. A focal region of IRU is identified in the proximocaudal aspect of the humerus or the distal cranial or caudal aspects (Figure 40-9). Fractures are usually medial. Rarely there is a pattern of IRU consistent with an incomplete spiral fracture of the humeral diaphysis. Radiological examination is less sensitive, although in some horses new bone formation can be identified on the caudal aspect of the proximal epiphysis, sometimes with increased radiopacity of the subchondral bone or new bone on the cranial aspect of the distal metaphysis and physis. Identification of new bone associated with a distal caudal fracture is rare.28 With treatment of box rest and controlled walking exercise for a minimum of 3 months, followed by a graduated return to work, the prognosis is good.
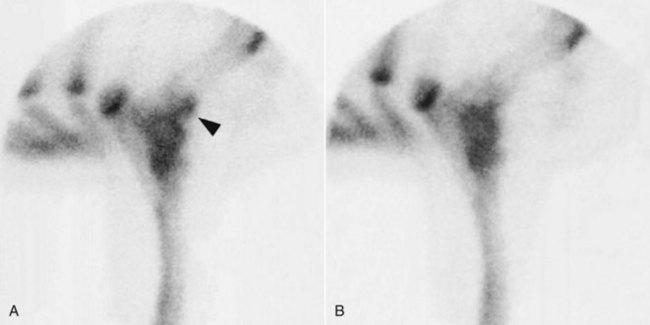
Fig. 40-9 Lateral scintigraphic images of the left (A) and right (B) elbows of 2-year-old Thoroughbred racehorse with acute-onset, severe left forelimb lameness that improved rapidly with rest. The image of the left elbow is reversed to facilitate comparison with the right. There is moderate, focal increased radiopharmaceutical uptake in the craniodistal aspect of the right humerus (arrow), compatible with a stress fracture. Radiographic examination revealed slight periosteal and endosteal callus on the craniodistal aspect of the humerus.
Fractures of the Greater or Lesser Tubercles
A fracture of the greater or lesser tubercle of the humerus is an occasional cause of unilateral forelimb lameness.6,29-33 The history is often unknown, and usually no localizing clinical signs are apparent. Lameness varies in degree. Intrathecal analgesia of the intertubercular bursa may improve the lameness. Although some fractures may be suspected on a mediolateral radiographic image, craniomedial-caudolateral oblique and cranioproximal-craniodistal (skyline) oblique radiographic images are often necessary. A caudolateral-craniomedial oblique image may be useful to highlight a fracture of the cranial aspect of the greater tubercle.5,30 Fracture fragments may also be accurately localized using diagnostic ultrasonography29 and in some horses are detectable only ultrasonographically (Figure 40-10). The overlying intertubercular bursa and tendon of biceps brachii should be inspected carefully. Small fractures may be removed surgically. Endoscopy of the intertubercular bursa permits reasonable access to the greater tubercle but not the lesser tubercle.29 Outcome is usually favorable.
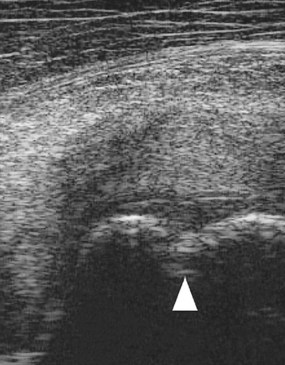
Fig. 40-10 Transverse ultrasonographic image of the humeral tubercles and tendon of biceps brachii of a 2-year-old Thoroughbred filly with severe lameness at the walk. Lateral is to the right. There was slight soft tissue swelling in the shoulder region, but no focus of pain could be identified. Nuclear scintigraphic examination revealed marked focal increased radiopharmaceutical uptake in the humeral tubercles. There were no radiological abnormalities. Cortical disruption (arrow) is apparent.
Diaphyseal Fractures
Diaphyseal fractures of the humerus usually result from a fall or other traumatic incident and may be oblique, spiral, or severely comminuted. Lameness is acute in onset and severe, associated with considerable swelling, pain, and crepitus. The horse may stand with the elbow dropped, slight carpal flexion, and the weight only on the toe. Radial nerve paralysis may occur concurrently (see pages 144 and 474). The diagnosis is usually obvious, and the prognosis is poor, so humane destruction is justified.34 Successful repair may be achieved in selected horses younger than 3 years of age.35 Conservative management in foals with diaphyseal fractures is a reasonable choice, but breakdown of soft tissues and angular limb deformities of the contralateral limb are potential complications.
Proximal Physeal Injuries
Injuries of the proximal humeral physis are rare, but Salter-Harris type I and II fractures have been seen in horses younger than 2 years of age.36 The prognosis with conservative management is poor.
Enostosis-like Lesions (Bone Islands)
Enostosis-like lesions, or solitary bone islands, have been recognized only since the advent of nuclear scintigraphy (see Chapters 19 and 39). An enostosis is defined as bone developing within the medullary cavity or on the endosteum, resulting in an area of increased radiopacity. In the horse, enostosis-like lesions have been described as focal or multifocal intramedullary sclerosis in the diaphyseal region of long bones, near the nutrient foramen, often developing on the endosteal surface of the bone. The cause of these lesions is unknown. Such endosteal reactions must be differentiated from endosteal callus secondary to a stress fracture. The presence of such radiopaque lesions is not always associated with lameness.
In the humerus, enostosis-like lesions occasionally cause acute-onset, moderate-to-severe lameness in young Thoroughbreds and older athletes, but they may be present asymptomatically. Usually no localizing clinical features are present. Lameness resolves relatively rapidly with rest, thus mimicking the behavior of horses with a stress fracture and therefore warranting nuclear scintigraphic examination. A region of intense IRU occurs in the distal caudal aspect of the humerus, distinguishable from a stress fracture because of its slightly more proximal and medullary location (Figure 40-11, A). Radiological examination usually reveals a relatively large, oval-shaped opacity within the medulla, adjacent to the nutrient foramen (Figure 40-11, B). However, initial radiological evaluation may be negative. Because lesions may be present asymptomatically, it is important to rule out other potential causes of lameness.
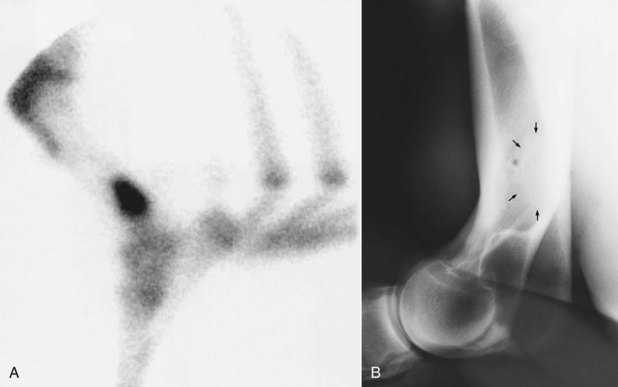
Fig. 40-11 Lateral scintigraphic (A) and mediolateral radiographic images (B) of the left humerus of 3-year-old Thoroughbred filly in race training with left forelimb lameness of 3 weeks’ duration. The lameness was not altered by local analgesic techniques. A, The nuclear scintigraphic image shows a region of intense focal increased radiopharmaceutical uptake in the distal diaphyseal region of the humerus, proximal to the usual site of stress fractures. B, There is a well-circumscribed area of increased radiopacity (arrows) adjacent to the principal nutrient foramen. This is an enostosis-like lesion. Lameness resolved after 2 months of box rest, and the lesion was scintigraphically silent, although there was no change in radiological appearance. The horse remained sound when returned to training.
Treatment is similar to that for a horse with a stress fracture: box rest and controlled walking exercise for approximately 3 months. An area of increased radiopacity may persist radiologically. Follow-up scintigraphic evaluation sometimes reveals normal radiopharmaceutical uptake, although in some horses there is persistent IRU despite resolution of lameness. The prognosis is usually good, although occasionally horses have lesions in several limbs and lameness may shift from limb to limb.
Scapulohumeral Joint
Osteochondrosis
Osteochondrosis of the scapulohumeral joint is often clinically evident in the first year of life, but in some horses it is not manifested until the horse is 2 to 5 years of age, although periods of unexplained lameness may occur. Delayed-onset lameness is often associated with relatively subtle radiological changes, which are more localized compared with those in horses that have lameness evident earlier. Lameness is often acute in onset and moderate to severe and is generally characteristic of proximal limb lameness. Often the foot of the most severely affected limb rapidly becomes more upright and boxy. In young, immature athletic horses radiological changes are often present bilaterally, although clinical signs may be evident only unilaterally. Intraarticular analgesia usually results in improvement in lameness rather than complete alleviation; therefore the clinical significance of lesions in the contralateral limb can be difficult to interpret.
Radiological abnormalities involve the glenoid cavity of the scapula, the humeral head, or both and include flattening of the articular surfaces, resulting in loss of congruity of the articular surfaces, irregular lucent zones in the subchondral bone, modeling of the ventral angle of the scapula, and blurring of the normally sharp outline of the glenoid cavity, because of modeling of the articular margins (Figures 40-12 and 40-13). Generally a good correlation exists between the degree of lameness and the severity of radiological abnormalities. However, radiology may underestimate the degree of lesion severity.36
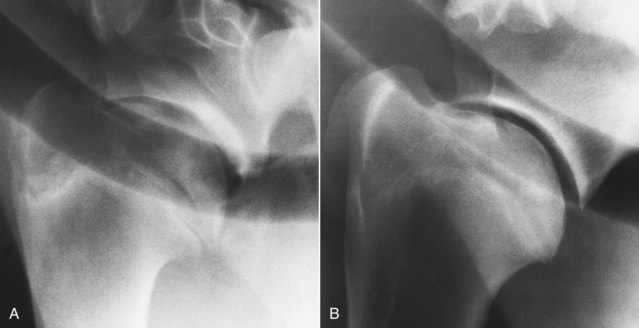
Fig. 40-12 A, Mediolateral radiographic image of the scapulohumeral joint of an 8-month-old Thoroughbred colt with severe left forelimb lameness. Radiolucent areas in the subchondral bone of the distal scapula and increased radiopacity and modeling of the glenoid cavity and ventral angle of the scapula are compatible with osteochondrosis. The humeral head also has variable radiopacity. B, The same horse 15 months after surgical debridement. The horse was sound. Substantial modeling of the glenoid cavity of the scapula has occurred. The horse trained and raced.

Fig. 40-13 Craniomedial-caudolateral oblique image of the scapulohumeral joint of a 3-year-old Thoroughbred with lameness alleviated by intraarticular analgesia of the scapulohumeral joint. A well-defined depression in the proximal articular surface of the humerus is compatible with mild osteochondrosis (arrow). This was the only detectable radiological abnormality. With repeated intraarticular medication the mare raced successfully, winning several more Group 1 races.
If lameness is recognized in a horse younger than 18 months of age, conservative management usually results in persistent lameness. Surgical treatment by radical arthroscopic debridement has resulted in some young horses being able to withstand race training, although their longer-term future has been poorly documented. In one study 45% of treated horses were able to return to athletic activity.37 However, in another study only 15.4% of 26 potential racehorses started a race.38 In some horses treated early, the bone shows a remarkable capacity to remodel (see Figure 40-12), whereas in others there is no change. Most horses show clinically significant improvement, even if lameness persists. However, surgical treatment in older horses is much less rewarding. In horses with minor radiological abnormalities, identified when in race training, periodic intraarticular medication with sodium hyaluronan and triamcinolone acetonide has permitted the horses to remain in training and race, although lameness has tended to recur. In weanlings and yearlings with moderate-to-severe lesions, conservative management, including stall rest, intraarticular injections of hyaluronan, and periodic radiological assessment of healing, has been successful.1
Subchondral Bone Cysts and Other Osseous Cystlike Lesions
True subchondral bone cysts occur in the middle of the glenoid cavity of the scapula (Figure 40-14). Other osseous cystlike lesions have been identified less frequently in the humeral head. Subchondral bone cysts in the distal aspect of the scapula and other osseous cystlike lesions most commonly cause lameness in immature athletic horses, 1 to 3 years of age, but subchondral bone cysts in the distal aspect of the scapula have also been identified in much older horses with no prior history of lameness. Trauma may be an inciting cause. Lameness is usually acute in onset and moderate to severe. In some horses the lameness varies extremely, within and between examination periods, from barely detectable at any gait to obvious at the walk. Lameness is usually substantially improved by intraarticular analgesia of the scapulohumeral joint. However, interpretation can be extremely difficult in those horses that show marked spontaneous variations in lameness.

Fig. 40-14 Mediolateral radiographic image of the scapulohumeral joint of 9-year-old hunter with episodic severe right forelimb lameness. There is a large, well-defined subchondral bone cyst in the middle of the distal scapula. The lameness responded to intraarticular medication with corticosteroids (triamcinolone).
Small radiolucent zones are occasionally seen in the middle of the opaque band of subchondral bone of the glenoid cavity of the scapula in clinically normal horses and in the contralateral limb of horses with lameness associated with a large subchondral bone cyst in the distal aspect of the scapula. Lameness that is improved by intraarticular analgesia associated with such lesions but no other radiological change is seen infrequently.1,2,39 This has been correlated with defects in the articular cartilage extending into the subchondral bone.39 More commonly a large circular or dome-shaped radiolucent area is seen, surrounded by a narrow rim of increased radiopacity. In some older horses in which such subchondral bone cysts have been identified, the cysts have been less well defined because they are less radiolucent. In skeletally mature horses similar lesions have occasionally been identified bilaterally associated with apparently unilateral lameness.
In skeletally immature horses subchondral bone cysts have been seen to enlarge progressively, and some appear to move proximally in the bone. Those identified in skeletally mature horses seem to persist unchanged. Osseous cystlike lesions in the proximal aspect of the humerus occur as circular radiolucent regions in the middle-to-caudal aspect. Some of these have been seen to fill in radiologically with time. Solitary subchondral bone cysts in the distal aspect of the scapula are generally not associated with any other detectable radiological change, whereas other osseous cystlike lesions are sometimes seen together with remodeling of the ventral angle of the scapula.
Nuclear scintigraphic examination may be helpful in horses in which lameness varies extremely in degree within an examination period. Subchondral bone cysts are associated with active bone modeling; therefore there is intense focal IRU.
Intraarticular medication of the scapulohumeral joint using hyaluronan and methylprednisolone acetate has been successful in resolving lameness in immature athletic horses, but results have been poorer in older horses.
Surgical treatment of subtle, small lucent zones has been successful,39 but effective debridement of large lesions is impractical.
Osseous Cystlike Lesions in the Humeral Tubercles
Osseous cystlike lesions in the humeral tubercles are discussed on page 471.
Osteoarthritis in Miniature Breeds
Sudden-onset, severe lameness is sometimes seen in Shetland and Falabella ponies and Miniature horses.40 Dysplasia of the joint predisposing to instability may be a predisposing factor for OA in some.40,41 Usually no known history of previous lameness or trauma exists. Lameness is typical of proximal limb pain. Manipulation of the shoulder may cause pain. Lameness is improved but rarely alleviated by intraarticular analgesia. Radiological examination sometimes reveals evidence of advanced OA, including periarticular osteophyte formation, and modeling of the ventral angle of the scapula (Figure 40-15). Occasionally, fragmentation of the ventral angle of the scapula occurs. Often new bone forms on the distal caudal border of the scapula and the proximal caudal aspect of the humerus in the regions of attachment of the joint capsule. In some ponies the contour of the glenoid cavity of the scapula appears flattened (see discussion of dysplasia on page 468), resulting in loss of congruity between the distal aspect of the scapula and the humeral head. In ponies with less severe abnormalities, radiological abnormalities may be detectable only in a craniomedial-caudolateral oblique image. In those ponies with minor radiological change at the time of onset of clinical signs, changes tend to have been rapidly progressive.
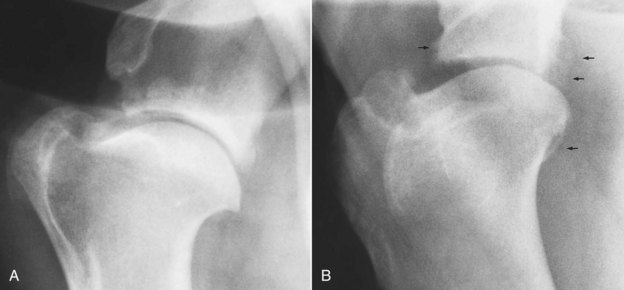
Fig. 40-15 A, Mediolateral radiographic image of the scapulohumeral joint of a 4-year-old Shetland pony with acute-onset, severe lameness that improved with intraarticular analgesia. There is marked modeling of the ventral angle of the scapula, periosteal new bone formation, and generalized increased radiopacity of the distal aspect of the scapula caused by extensive new bone. B, Craniomedial-caudolateral oblique radiographic image of a scapulohumeral joint of 5-year-old Miniature horse. There is poor congruity between the glenoid cavity of the scapula and the humeral head. Note also the periarticular periosteal new bone (arrows).
Arthroscopic evaluation of the joint reveals extensive softening of the articular cartilage, and surgical debridement has resulted in some clinical improvement, although lameness has persisted. The prognosis for athletic function is guarded. Surgical arthrodesis has been described.42
Osteoarthritis in Nonminiature Breeds
OA in the scapulohumeral joint is relatively uncommon,36 except as a sequela to osteochondrosis, an intraarticular fracture, or a tear of the scapulohumeral joint capsule. Lameness is mild to moderate and is usually improved by intraarticular analgesia, but false-negative responses do occur. Radiological abnormalities include loss of congruity between the glenoid cavity of the scapula and the humeral head, because of flattening of the humeral head or modeling of the ventral angle of the scapula; periarticular osteophyte formation, most easily seen on the cranial articular margins of the scapula; and radiolucent areas in the subchondral bone. The response to intraarticular medication is usually poor, and the prognosis for athletic function is guarded.
Care should be taken when evaluating the scapulohumeral joint arthroscopically, because widespread aging changes occur in the articular cartilage, especially of the distal aspect of the scapula.2 These include softening of the articular cartilage and extensive fissure formation (Figure 40-16). Modeling changes of the articular margins of the glenoid cavity of the scapula may also occur.
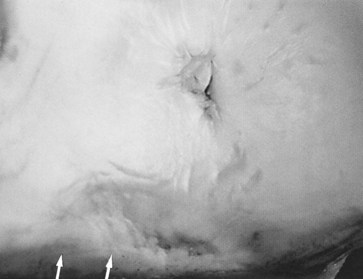
Fig. 40-16 Postmortem appearance of the glenoid cavity of the scapula of an 8-year-old Thoroughbred with no history of lameness. There is modeling of the articular margin (arrows), and the articular cartilage appears irregular. This was bilaterally symmetrical and is a typical normal finding in mature horses.
Tearing of the Scapulohumeral Joint Capsule
Localized tearing of the scapulohumeral joint capsule is an unusual cause of lameness that is improved by intraarticular analgesia. In the acute stage no detectable radiological abnormalities may be apparent, but with more chronic lameness entheseous new bone may be seen in the region of damage. Nuclear scintigraphic examination may reveal focal or more generalized IRU in the region of the scapulohumeral joint. Although ultrasonographic examination may be helpful if the lesion is lateral, medial lesions cannot be seen. Definitive diagnosis is based on diagnostic arthroscopy of the scapulohumeral joint. The prognosis for recovery for athletic function is guarded.
Dysplasia
Dysplasia of the scapulohumeral joint has been identified in Shetland ponies41 and Miniature horses,1 sometimes together with subluxation of the joint or with OA (see the earlier discussion of OA in miniature breeds, page 467). Flattening of the radius of curvature of the glenoid cavity of the scapula occurs.
Luxation
Luxation of the scapulohumeral joint has been seen in ponies2 more frequently than in horses and results in acute-onset, severe lameness associated with extensive swelling in the shoulder region (Figure 40-17, A). If the humerus has luxated laterally, the scapular spine is less easy to palpate than usual. The horse is reluctant to bear full weight on the limb at rest and is usually non–weight bearing at the walk. Diagnosis is confirmed by radiographic examination (Figure 40-17, B). Mediolateral and craniomedial-caudolateral oblique images should be obtained to determine whether a concurrent fracture is present and whether the luxation is medial or lateral. The humerus can luxate cranioproximally or caudoproximally.

Fig. 40-17 A, An 8-year-old pony gelding with acute-onset, severe right forelimb lameness associated with swelling in the shoulder region. B, Mediolateral radiographic view of the scapulohumeral joint showing cranioproximal luxation of the humerus. The luxation was successfully reduced with the pony under general anesthesia, and the pony made a complete functional recovery.
A horse with simple acute luxation, without any concurrent fracture, can be treated by manual reduction of the luxation with the horse under general anesthesia in dorsal recumbency. A hobble is placed around the distal aspect of the affected limb, and the limb is maximally extended vertically. Pressure is applied to the shoulder region to reduce the luxation. An assisted recovery from general anesthesia is recommended, followed by cross-tying to prevent the horse from lying down, minimize the risks of reinjury, and allow the traumatized joint capsule to heal. Periarticular fibrosis inevitably develops, and treating the horse with nonsteroidal antiinflammatory drugs and a controlled exercise program to restore normal joint mobility may be necessary. A complete functional recovery has been achieved in a small number of ponies. The presence of any concurrent fracture predisposes to recurrent luxation and warrants an extremely guarded prognosis. Persistent luxation results in the rapid development of a deep groove in the humeral head, extending from cranially to caudally; thus the prognosis is poor.2
Fracture of the Articular Surface of the Scapula or the Proximal Aspect of the Humerus
Fracture of the articular surface of the scapula may result from a fall when the horse is jumping, resulting in acute-onset, severe lameness.43 Manipulation of the joint may produce pain, and sometimes crepitus can be elicited. Periarticular soft tissue swelling occurs in the acute stage, but this resolves relatively rapidly. Diagnosis requires high-quality radiographs, because the only detectable radiological abnormality may be loss of clarity of the articular margins of the distal aspect of the scapula. Mediolateral and craniomedial-caudolateral oblique images should be obtained. Follow-up radiographs may show modeling of the ventral angle of the scapula. The prognosis for athletic function is hopeless.
Crushing of the caudal aspect of the humeral head has been seen as a result of a fall, resulting in acute-onset severe lameness. There may be no detectable radiological abnormality, but there is intense IRU in the humeral head. Severe lameness persists, yet follow-up radiographs may reveal only modeling of the ventral angle of the scapula. Postmortem examination has confirmed the diagnosis.44
Periarticular Trauma
Periarticular trauma—the result of a fall, collision between two horses, or collision between a horse and a solid object—may result in sudden-onset, severe, unilateral forelimb lameness because of severe bruising. Extensive periarticular soft tissue swelling may develop rapidly, with pain on deep palpation. In the acute stage determining whether a concurrent fracture is present may be difficult, especially fracture of the supraglenoid tubercle of the scapula or the first rib, because history and clinical signs are so similar.
If damage is restricted to bruising, lameness generally rapidly improves over the following 7 days. However, if concurrent trauma to the suprascapular nerve or its branch to the infraspinatus muscle occurred, clinically significant neurogenic atrophy of the supraspinatus or infraspinatus muscles may occur within 7 days (see page 473). If moderate-to-severe lameness persists, then radiographic examination is indicated. If damage is restricted to soft tissue structures, then treatment with nonsteroidal antiinflammatory drugs combined with restriction to box rest and controlled exercise usually results in a rapid and complete recovery.
Intertubercular Bursa
Congenital abnormalities of the bicipital apparatus are a rare cause of lameness, sometimes not recognized until maturity.45 Lameness is characterized by a shortened cranial phase of the stride at both the walk and the trot. Affected horses have generalized atrophy of the shoulder musculature or specifically of the biceps brachii, and abnormal prominence of the point of the shoulder. Contraction of the ipsilateral foot is probably a reflection of a chronic problem, despite reported acute onset of lameness. It may occur unilaterally or bilaterally. Mediolateral and cranioproximal-craniodistal oblique radiographic images should be obtained. Abnormalities include absence of a lesser tubercle of the humerus, narrowing of the groove between the greater and intermediate tubercles, and evidence of OA of the scapulohumeral joint, probably the result of instability. Ultrasonography reveals either complete medial displacement of the tendon of biceps brachii or an abnormal shape and position of the tendon.
Rupture of the Tendon of Biceps Brachii
Rupture of the tendon of biceps brachii is a rare injury sustained as the result of a fall while jumping at speed.46 It results in severe lameness at the walk, associated with diffuse soft tissue swelling around the shoulder. Diagnosis is based on radiographic and ultrasonographic examinations. The tendon may rupture through the isthmus between the medial and lateral lobes. The prognosis is hopeless.
Tendonitis of Biceps Brachii
Injury of the tendon of biceps brachii is a relatively uncommon cause of forelimb lameness, with no typical history. Frequently no localizing signs suggest the source of pain. In some horses forced retraction of the limb induces discomfort, but this is an unreliable finding. Lameness varies from mild to severe, and only if lameness is severe are the gait characteristics typical of proximal limb lameness. In some horses lameness is more obvious in the walk than at any other pace. Lameness is usually improved by intrathecal analgesia of the intertubercular bursa, although it may take up to half an hour. Some false-negative results occur in association with severe lesions.44
Diagnosis is based on ultrasonographic examination. The entire length of the tendon of biceps brachii should be examined carefully from its origin on the supraglenoid tubercle of the scapula to the musculotendonous junction. The horse should be standing fully load bearing on the limb to avoid hypoechoic artifacts within the tendon. It is important to be aware of the anatomy of the tendon, which changes in shape from proximally to distally.8,10 Examining the medial and lateral lobes independently is often necessary, because maintaining both lobes in focus simultaneously is difficult. The tendon should be examined in transverse and longitudinal planes and careful comparison made with the contralateral limb. Ultrasonographic abnormalities include enlargement of the tendon, loss of definition of one of its margins, hypoechoic defects within the tendon, and loss of fiber pattern in longitudinal images. The humeral tubercles should be inspected carefully for evidence of any concurrent damage. Concurrent evidence of bursitis characterized by an abnormal amount of fluid within the sheath (bursa) may also be present and results in an increased anechogenic space between the tendon and the humerus. Horses with chronic lameness may show evidence of hyperechogenic foci within the tendon, representing fibrosis, mineralization, or ossification. Adhesions may develop between the tendon and the wall of the bursa. Occasionally, echogenic bodies are seen free within the bursa.
Treatment of horses with tendonitis of biceps brachii consists of box rest and controlled walking exercise.47 Injection of hyaluronan may be beneficial. The tendon should be monitored by ultrasonography at up to 3-month intervals. At least 6 to 9 months of convalescent time are required for horses with acute lesions, which have a fair prognosis. The prognosis for horses with chronic injuries is poor. Permanent enlargement of the tendon within the confined space between the brachiocephalicus muscle and the humerus and loss of normal gliding function cause persistent pain. Tenectomy or tenotomy has been described.48
Osteitis of the Humeral Tubercles
Osteitis of the humeral tubercles is a rare cause of forelimb lameness.31 Horses show moderate-to-severe lameness and resent manipulation of the shoulder. Abnormalities of the humeral tubercles are seen radiologically as lucent areas or by ultrasonography as a roughened surface to the bone and overlying cartilage. The intertubercular bursa may contain an abnormal amount of fluid and the tendon of biceps brachii may be enlarged, with peritendonous reaction. Surgical exploration may reveal necrotic areas of bone that are readily debrided, resulting in improvement in lameness.
Fracture of the Humeral Tubercles
A discussion of fracture of the humeral tubercles appears on page 463 (see Figure 40-10). ![]()
Infection
Infection of the intertubercular bursa occasionally causes acute-onset, moderate-to-severe forelimb lameness.49-51 Infection may be a sequela to known trauma, a previous injection, and a penetrating wound, but it has been recognized with no history of trauma or evidence of a wound, presumably infection being hematogenous in origin. Infection occurs in immature athletic horses and older horses.
The horse may stand slightly favoring the lame limb. Deep palpation in the region of the bursa may elicit pain. Retraction of the limb is resented. Lameness is often evident at the walk. Synovial fluid withdrawn from the bursa is usually grossly brown discolored and turbid, and therefore intrathecal analgesia is usually unnecessary. Diagnostic ultrasonography reveals an abnormal amount of fluid within the bursa; sometimes echogenic material is seen within the fluid, and the surface of the tendon of biceps brachii may be less well defined than normal because of fibrin deposition. Diagnosis is confirmed by measuring differential white blood cell count and total protein concentration and by cytological examination of the synovial fluid, with polymorphonuclear leukocytes dominating.
Treatment is by radical surgical debridement and thorough lavage of the bursa by open surgery49 or endoscopy,50 combined with long-term, broad-spectrum antimicrobial therapy (e.g., crystalline penicillin and gentamicin) and the use of nonsteroidal antiinflammatory analgesic drugs. If a penetrating wound is identified, consideration should be given to using metronidazole. When the acute inflammatory response has subsided, controlled exercise is important to try to limit adhesion formation. If the condition is recognized and treated early and aggressively, a favorable outcome can be achieved, but prolonged therapy is often required.49
Noninfectious Bursitis
Noninfectious bursitis does occur occasionally alone, together with tendonitis of biceps brachii (see page 470), or with osteitis of the humeral tubercles.6,52 Lameness varies in degree and is usually substantially improved by intrathecal analgesia. Diagnosis is verified by ultrasonographic examination of the intertubercular bursa. The bursa has an abnormal amount of fluid but no abnormalities of the enclosed tendon or the humeral tubercles. Treatment by intrathecal administration of hyaluronan and triamcinolone acetonide, combined with controlled exercise, is usually successful.
Mineralization
Mineralization or ossification within the tendon of biceps brachii has been seen alone, or as a sequela to a previous fracture of the supraglenoid tubercle.1,53 Ectopic mineralization within the bursa has been associated with substantial proliferation of the synovial membrane of the intertubercular bursa.9 No typical history is known. Lameness varies in degree and only if moderate to severe is typical of a proximal limb lameness. Lameness may be improved by intrathecal analgesia of the intertubercular bursa. Mineralization may be identified radiologically, but it can be obscured by the humeral tubercles. Radiography is useful to identify any previous fracture. There may be associated IRU.53 Diagnostic ultrasonography provides more accurate information about the precise site and extent of mineralization and any concurrent pathological condition of the tendon. The prognosis for return to full athletic function is guarded.
Osseous Cystlike Lesions in the Humeral Tubercles
Osseous cystlike lesions in the humeral tubercles may develop secondary to trauma such as a fall or change in biomechanics resulting from other causes of lameness, or they may arise from an unknown cause.44,54-56 There is acute-onset moderate-to-severe lameness, usually with no localizing clinical signs. There is often no or limited response to either intraarticular analgesia of the scapulohumeral joint or intrathecal analgesia of the intertubercular bursa. Either lesions are identified using survey radiology or their presence is highlighted by scintigraphic evaluation demonstrating focal moderate-to-intense IRU. Lesions are sometimes not evident on mediolateral radiographs but may be seen in craniomedial-caudolateral oblique images. If a lesion involves the cortex of the tubercle, osseous and cartilage defects may be identified using ultrasonography. In some horses there are also lesions in the biceps brachii tendon. Lameness has generally resolved with rest, with or without medication of the intertubercular bursa, although a radiolucent lesion may persist. Successful surgical treatment has also been described.55
Scapula
Fracture of the Supraglenoid Tubercle
The scapula has four centers of ossification: the scapular cartilage, body of the scapula, cranial part of the glenoid cavity of the scapula, and supraglenoid tubercle. The cranial part of the glenoid cavity of the scapula fuses with the body by 5 months of age. The physis of the supraglenoid tubercle closes at 12 to 24 months of age. Fracture of the supraglenoid tubercle of the scapula is a relatively common injury, resulting from a collision with a solid object or fall. Fractures frequently occur through the original physes.43 The fracture may be simple or comminuted, involving only the supraglenoid tubercle, without an articular component. Alternatively, the fracture may pass through the glenoid notch of the scapula, which may result in one large fracture or separation of both original physes.
Lameness is sudden in onset and moderate to severe. Over the first week the horse may show progressive improvement, but lameness persists. Neurogenic atrophy of the supraspinatus and infraspinatus muscles may develop within 7 days if a concurrent injury of the suprascapular nerve occurred. Disuse atrophy develops more slowly.
A palpable thickening in the region of the supraglenoid tubercle exists, but crepitus is rarely appreciated.
Diagnosis is confirmed radiologically (see Figure 13-1). The fracture fragments are often displaced craniodistally, because of the pull of the biceps brachii, and if treated conservatively a nonunion develops. The radiographs should be inspected carefully to determine if the fracture has an articular component, which warrants a more guarded prognosis. Rarely, there will be concomitant luxation of the scapulohumeral joint.
The prognosis with conservative treatment is poor for return to athletic function. Surgical treatment by removal of the fracture fragment(s) has been successful in some horses, although the level of work to which horses have returned has not been well documented. Various methods of internal fixation have been attempted, but the large distracting forces of biceps brachii have to be overcome. A small number of horses younger than 2 years of age and less than 400 kg body weight have been successfully treated by complete tenotomy of the biceps brachii and internal fixation using three 5.5-mm cortical bone screws.57 Alternatively, in foals, yearlings, and small horses, the fracture can be repaired using a tension band technique with either a small plate or screws, preserving the biceps tendon.
Stress Fractures
Stress fractures of the body of the scapula are an occasional cause of acute-onset forelimb lameness in young Thoroughbreds in training.1,58,59 Usually no localizing clinical signs are present, although occasionally focal pain can be identified. Lameness often frequently improves spontaneously with rest. A premature return to training may result in a catastrophic fracture. Scintigraphic examination reveals IRU in the mid-to-distal aspect of the scapula. Occasionally a fracture can be confirmed using ultrasonography. Treatment requires 6 to 8 weeks of box rest and controlled walking exercise, followed by a graduated return to full work. In my experience the prognosis has been good, but in a report from North America two of seven horses (29%) that resumed training had recurrent injury.59
Fracture of the Body of the Scapula
Fractures of the body of the scapula usually result from the horse falling at a fence when jumping at speed. Complete fractures result in severe lameness and extensive soft tissue swelling and merit destruction on humane grounds. Diagnosis is usually obvious based on clinical signs, and radiographic examination is not necessary. Radiography or scintigraphic examination is required for the diagnosis of incomplete fractures (Figure 40-18). High-quality radiographs are required, and this may be difficult because the horse may resent protraction of the limb because of pain. Horses with fractures that enter the scapulohumeral joint have a poor prognosis. However, horses with extraarticular, incomplete fractures of the body of the scapula have a good prognosis for return to full athletic function with conservative management.
Fracture of the Scapular Spine
Fractures of the scapular spine result from a fall, collision with a solid object, or occasionally a kick. Acute-onset, moderate lameness occurs with associated localized soft tissue swelling and pain on palpation. Oblique radiographic skyline views of the scapular spine are necessary to identify a fracture. Diagnostic ultrasonography may be more helpful in identifying a fracture. Most horses with fractures heal adequately with conservative management. Occasionally a sequestrum develops, necessitating surgical debridement. The prognosis for return to full athletic function is good.
Infection of the Infraspinatus Bursa
Injury of the infraspinatus bursa and tendon seldom occur except as a result of a penetrating injury in the shoulder region, resulting in infectious bursitis.60 Signs include generalized swelling in the shoulder region, pain on manipulation of the shoulder, and lameness characterized by a shortened cranial phase of the stride. Ultrasonography reveals distention of the infraspinatus bursa with echogenic fluid, with thickening of the synovium if chronic. Evaluation of the greater tubercle of the humerus may reveal roughening or a fracture. Treatment includes lavage of the bursa, surgical debridement if indicated, and broad spectrum antimicrobial therapy. The prognosis is good.
Muscle
Muscle Lesions: Brachiocephalicus, Biceps Brachii, and Pectorals
Lesions of muscles in the shoulder region have not been well documented and probably occur more commonly than recognized. However, clinical signs are rather nonspecific, and diagnosis is difficult. A number of dressage horses have been identified that have shown forelimb lameness only while performing lateral work. Palpation has revealed no detectable abnormality. Local analgesic techniques have not altered the lameness. Ultrasonographic examination has revealed hyperechogenic areas of fibrosis or mineralization within the brachiocephalicus in the lame limb only.
A dressage horse showed lameness only at the walk. Local analgesic techniques were ineffective. Nuclear scintigraphic evaluation revealed focal moderate IRU in the musculature cranioproximal to the elbow. This correlated with a hyperechogenic region within the biceps brachii.
Some horses have forelimb lameness associated with palpable soreness of the pectoral muscles, which responds well to physiotherapy. Soreness of the brachiocephalicus muscles is often seen with lameness caused by distal limb pain. Lameness is sometimes seen associated with primary brachiocephalicus muscle damage in dressage horses, show jumpers, event horses, and horses that race over fences. In most horses with acute lameness, palpation reveals muscle soreness and induces muscle spasm. However, in horses with chronic muscle injury pain can be more difficult to identify. In some horses lameness was evident only in walk and was characterized by lifting of the head and neck as the ipsilateral limb was protracted.
Rupture of Serratus Ventralis
The serratus ventralis muscles arise from the third to seventh cervical vertebrae and the first eight to nine ribs and insert on the medial proximal aspect of each scapula. They sling the thorax between the forelimbs. Rupture of one or both of these muscles is a rare injury, caused by trauma. The proximal border of the scapula moves proximally. If rupture is bilateral, the scapulae become higher than the summits of the dorsal spinous processes in the withers region. Rupture of the serratus ventralis should be differentiated from neurological disease causing loss of function of the muscle.1
The horse tends to stand with the forelimbs close together. Palpation of the withers region or manipulation of the forelimbs causes pain. The horse is reluctant to move, takes small steps, and nods the neck stiffly.
Radiographic examination should be performed to rule out a fracture of the scapula or the dorsal spinous processes of the cranial thoracic vertebrae. The prognosis for athletic function is poor.
Nerve
Atrophy of Supraspinatus and Infraspinatus Muscles: Damage to the Suprascapular Nerve
The suprascapular nerve wraps around the cranial aspect of the neck of the scapula and in this position is vulnerable to trauma resulting in perineural edema, stretching, and neuroma formation. Neuroma formation usually results in permanent loss of function and subsequent neurogenic atrophy of supraspinatus and infraspinatus muscles. This can occur within 7 days of injury. Atrophy results in abnormal prominence of the scapular spine, but damage to the suprascapular nerve alone does not result in any loss of stability of the scapulohumeral joint. Lameness may be the result of trauma at the time of the injury but generally resolves rapidly, unless a concurrent fracture is present.
This condition has been called Sweeny, but this can be confusing because this term has also been used to describe instability of the shoulder or shoulder slip resulting from loss of collateral support of the shoulder musculature. This latter condition is separate and should not be confused (see the following discussion). Experimental transection of the suprascapular nerve in two ponies and one adult horse resulted in rapid atrophy of the supraspinatus and infraspinatus muscles, which persisted over the long term but produced no gait abnormality.2
The injury usually results from a fall or collision with another horse or solid object. Permanent muscle atrophy may ensue, but this results only in a cosmetic defect, not a functional deficit. Electromyography can be used to determine whether any other muscles are affected, which would suggest an injury to the brachial plexus or to other nerves in addition to the suprascapular nerve. Patchy sweating indicates a lesion elsewhere.
Surgical treatment has been performed to decompress the suprascapular nerve by cutting out a notch on the craniodistal aspect of the scapula and removing fibrotic material from around the nerve.44 Surgical treatment has resulted in restoration of more normal muscle mass.61 Care must be taken not to traumatize the scapula unduly, because this may predispose to fracture.
Instability of Shoulder: Damage to the Brachial Plexus
Lack of collateral support to the scapulohumeral joint by loss of function of the muscles on the medial (subscapularis) and lateral aspects of the joint results in so-called shoulder slip. As the horse starts to bear weight on the limb, the shoulder joint bulges abaxially (Figure 40-19; see Figure 6-19).![]() Concurrently the heel of the foot tends to rotate outward. This gait abnormality is evaluated most easily viewing the horse walking toward the observer. The gait abnormality may be slight or severe.
Concurrently the heel of the foot tends to rotate outward. This gait abnormality is evaluated most easily viewing the horse walking toward the observer. The gait abnormality may be slight or severe.
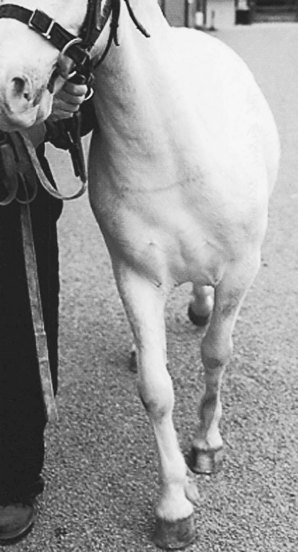
Fig. 40-19 A 7-year-old driving pony with acute-onset instability of the left shoulder joint probably caused by a brachial plexus injury. The injury was of 12 days’ duration. Note the medial placement of the left front foot. The heel rotated laterally as the foot broke over. There was moderate atrophy of the left infraspinatus, supraspinatus, and triceps muscles. The pony was treated conservatively, progressively improved, and made a complete functional recovery.
Instability of the shoulder was formerly ascribed to atrophy of the supraspinatus and infraspinatus nerves secondary to suprascapular nerve damage, but profound atrophy of these muscles can be present with no detectable gait abnormality.2,11 Experimental transection of the suprascapular nerve has resulted in profound atrophy of supraspinatus and infraspinatus muscles but no detectable gait abnormality.2 Seven horses with persistent instability of the shoulder that were humanely destroyed and examined post mortem had atrophy of at least the supraspinatus, infraspinatus, and subscapularis muscles. All horses had neuroma formation involving nerves of the brachial plexus or the ventral nerve roots of the contributing nerves. The suprascapular nerve appeared normal as it passed over the cranial aspect of the scapula.
Instability of the shoulder invariably results from trauma, usually the horse colliding with a solid object. Pain-related lameness may also be present initially, but this generally resolves within 1 to 2 weeks, provided that a concurrent fracture does not exist. Similar clinical signs occasionally occur transiently (for 1 to 3 hours) after intraarticular analgesia of the scapulohumeral joint, presumably because of extraarticular leakage of local anesthetic solution. Instability of the shoulder has also been seen in a Miniature horse with dysplasia of the scapulohumeral joint and advanced OA.
After trauma, initially no muscle atrophy is detectable, but atrophy of several muscles is usually detectable within 7 to 10 days. Patchy sweating may develop in the caudal neck region or over the scapula, depending on which nerves have been damaged. Electromyography can be used to determine accurately which muscles are affected.
Prognosis depends on the nature of the nerve damage and the ability to achieve reinnervation of the affected muscles. Nerve regeneration occurs at approximately 1 mm per day. Progressive improvement in gait is a good prognostic sign. A normal gait may be restored despite persistence of atrophy of the supraspinatus and infraspinatus muscles.2,62 However, a persistent gait abnormality 6 months after injury warrants a guarded prognosis. Surgical treatment is impractical because of the inaccessibility of the brachial plexus or the ventral nerve roots. Scapular notch resection is not indicated, because nerves in addition to or other than the suprascapular nerve are involved. This procedure also risks secondary fracture of the scapula.
Radial Nerve Paralysis
Radial nerve paralysis is an occasional cause of lameness.63,64 The clinical signs depend on the site or sites of damage. Complete radial nerve paralysis is most common, with loss of function of the extensor muscles of the elbow, carpus, and digit, and results in inability to stand on the limb. The elbow is dropped, and the horse tends to stand with the affected limb forward, with the antebrachium at an angle of approximately 45 degrees to the ground, with the carpus and fetlock semiflexed (see Figure 5-14). Less commonly only the extensor muscles of the elbow are affected, so although the limb may be advanced forward, the elbow will drop during weight bearing. Occasionally only the extensor muscles of the carpus and digit are affected, so that the limb is advanced and placed normally, but then the carpus or fetlock may slightly knuckle forward. The horse has a tendency to stumble.
Lameness is usually sudden in onset. The horse may have a history of trauma. Paralysis occurs most commonly in young horses turned out together. Although damage to the radial nerve itself may be the cause of lameness,63,64 many injuries are probably caused by compression of the brachial plexus between the scapula and the ribs or can be associated with a fracture of the dorsal aspect of a rib involving the eighth cervical nerve. An electromyogram may demonstrate involvement of more than the radial nerve. Equine protozoal myelitis should be considered in older horses, especially if evidence of other lower motor neuron pathological conditions exists (see page 140).
Many horses make a slow progressive recovery. Electrical stimulation of the affected muscles may help to maintain muscle mass. Problems may arise in young horses with overload of the contralateral limb, unless symptoms resolve quickly. An improvement within 2 to 4 weeks warrants an optimistic prognosis. Persistence of clinical signs for more than 6 months warrants a guarded prognosis.
Fracture of the First Rib
Occasionally, acute-onset, severe lameness follows trauma from a fall or collision with a solid object associated with a fracture of the first rib. The lameness is typical of a proximal limb injury, but no other localizing signs are present. Atrophy of the infraspinatus alone has also been recognized in some horses. Diagnosis is by radiographic examination. Nuclear scintigraphic examination may facilitate diagnosis. The prognosis is good after rest.