Chapter 44The Tarsus
Anatomical Considerations
The tarsus consists of the tarsocrural, talocalcaneal, talocalcaneal-centroquartal (proximal intertarsal), centrodistal (distal intertarsal), and tarsometatarsal joints. The bones include the talus and calcaneus and the central, first and second fused, third, and fourth tarsal bones.1 The tarsocrural joint is a ginglymus joint based on the shape of deep grooves on the cochlear articular surface of the distal end of the tibia with the extensive surface of the trochlea of the talus. The articulation of these joints is at an angle of 12 to 15 degrees dorsolateral to the sagittal plane of the limb. The talocalcaneal-centroquartal (proximal intertarsal), centrodistal, and tarsometatarsal joints are plane joints and are capable of only small amounts of gliding (shear) movement.
The tibia follows an almost circular path along the talar ridges, and most movement occurs in the tarsocrural joint; however, there are translations and rotations at other sites.2 Hock flexion is associated with abduction of the distal part of the limb caused by an oblique axis of motion.3 There is outward rotation of the third metatarsal bone (MtIII) during the swing phase, followed by a small inward rotation during stance, when the hock is compressed. Thus at the gallop the hindlimbs swing outside the forelimbs as the tarsus flexes and then move back toward the midline as the tarsus extends before landing. Excessive rotation leads to visible wobbling of the tarsus. There is a locking mechanism among the talus, the central and third tarsal bones, and the MtIII.4 A process on the distal plantar aspect of the talus fits into an indentation on the proximal aspect of the central tarsal bone; a ridge on the distal aspect of the central tarsal bone engages with a fossa on the proximal aspect of the third tarsal bone. A triangular plantar process of the third tarsal bone prevents the third tarsal bone from sliding across the proximal aspect of the MtIII. The oblique dorsal ligament extends distally from a small origin on the talus, spreading across the central and third tarsal bones, limiting motion.
Biomechanical studies have shown greatest compression on the distal medial aspect of the tibia and the proximal lateral aspect of the MtIII, suggesting that compressive load is transferred from medial to lateral through the tarsus. Radiopharmaceutical uptake (RU) in normal horses is greatest dorsally and laterally in the distal aspect of the tarsus, suggesting increased adaptive bone modeling in response to high load.5 There are differences in subchondral bone and cartilage thickness in the central and third tarsal bones from medially to laterally, varying dependent on intensity and type of exercise history, reflecting loading.6,7 The distal tarsal joints function to absorb energy in the early stance phase and contribute to propulsion in the late stance phase. Conformation influences tarsal function.8 Horses with large tarsal angles (>165.5 degrees) have been shown to have less flexion and less energy absorption in the impact phase at the trot compared with horses with intermediate (155.5 to 165.5 degrees) or small (<155.5 degrees) angles.8 Horses with large hock angles generated less vertical impulse than horses with small angles, and net extensor force was lower.8 Thus large tarsal angles may result in less propulsion and less absorption of concussion, which may influence both performance and soundness. However, horses with small hock angles had greater flexion during the stance phase, which may compress the dorsal aspects of the bones. Abnormal tarsal conformation can lead to lameness. Anecdotally, horses with small hock angles (sickle hocks) often develop osteoarthritis (OA) of the distal hock joints, curb, and soft tissue injury in the distal, plantar aspect of the hock and may be prone to the development of fracture of the central and third tarsal bones. Horses with large hock angles (straight-hock conformation), surprisingly, may be less prone to the development of tarsal pain, but they appear predisposed to the development of suspensory desmitis and stifle region pain.
Flexion of the stifle and hock is synchronous because of the reciprocal apparatus; there is rapid flexion of the tarsus at the beginning of the stance phase of the stride and maximal extension at the end of the stance phase. There is a peak of flexion in the middle of the swing phase. There is also coupling of movement of the tarsus and fetlock in flexion and extension because of passive action of the superficial digital flexor tendon and the long digital extensor tendon, respectively.
The fibrous part of the combined tarsal joint capsule surrounds all synovial compartments and attaches proximally to the tibia and distally to the distal tarsal bones, blending with the collateral ligaments (CLs), and to the metatarsal bones.2 The dorsomedial aspect of the joint capsule is thin and uncovered by any tendons or ligaments and forms a fluctuant swelling over the medial trochlea of the talus. The proximal aspect of the plantar fibrous joint capsule is also thin and extends proximally about 5 cm caudal to the distal aspect of the tibia.2 The plantar distal aspect of the joint capsule consists of the plantar and tarsometatarsal ligaments, which are thick and tightly adherent to the distal tarsal bones. The tarsus is composed of four synovial compartments. The tarsocrural compartment lubricates the tarsocrural joint and the dorsal aspect of the proximal intertarsal joint. The tarsocrural compartment is the largest compartment and is composed of four pouches: the dorsomedial, dorsolateral, plantaromedial, and plantarolateral. This provides several sites at which arthrocentesis can be performed. The proximal intertarsal synovial sac lines the talus and calcaneus proximally and the plantar aspect of the central and third tarsal bones distally and communicates dorsally with the tarsocrural joint. The large fenestration between the tarsocrural and the proximal intertarsal joints allows loose osteochondral fragments to move freely between the conjoined joints. Disease of one joint obligatorily involves both compartments, because they function as one. In horses <1 year of age this opening appears small or slitlike or is not readily apparent when evaluated arthroscopically. The centrodistal joint lubricates the articulation between the central and third tarsal bones and the bones on each side, and the tarsometatarsal joint lubricates the third and fourth tarsal bones with the second metatarsal bone (MtII), the MtIII, and the fourth metatarsal bone (MtIV). The superficial location of the joint capsules makes them susceptible to penetration and the introduction of infection in association with trauma to the tarsus.
There is communication in 8% to 39% of the centrodistal and tarsometatarsal joints, but not necessarily in both hocks of the same horse,9-11 although substances may spread between them by diffusion even in the absence of frank communication. 12,13 Communication between the distal tarsal joints and the tarsocrural joint was demonstrated in 3% of horses after injection of radiodense contrast medium into the tarsometatarsal joints in live horses10; however, in a cadaver study mepivacaine injected into the centrodistal or tarsometatarsal joints spread to the tarsocrural joint within 15 minutes of injection in 88% and 92% of limbs, respectively.12
Anatomical aspects of the gastrocnemius and calcaneal bursae and the tarsal sheath are discussed elsewhere (Chapters 76, 79, and 80). The distal tendon of the long digital extensor muscle is enclosed within a synovial sheath as it passes over the dorsolateral aspect of the tarsus. This sheath is compressed by transverse retinacular bands, resulting in a loculated appearance if the sheath is distended. Such longitudinal swelling is a quite common incidental finding in both sound and lame horses either unilaterally or bilaterally and is only rarely associated with pain and lameness. Focal lesions of the long digital extensor tendon have been identified ultrasonographically, but usually unassociated with lameness.
Numerous ligaments surround the hock. Both the lateral and medial CLs have one long and three short components.14 The long lateral CL is superficial; originates at the caudal aspect of the lateral malleolus of the distal tibia; inserts on the distal lateral aspect of the calcaneus with additional fibers to the fourth tarsal bone, the MtIII, and the MtIV; and forms a canal for the tendon of the lateral digital extensor muscle. The short lateral CLs lie deep to the long lateral CL and originate from the cranial aspect of the lateral malleolus, pass plantad, and attach to the lateral surface of the calcaneus and the proximolateral plantar aspect of the talus. The long medial CL originates from the caudal aspect of the medial malleolus, attaches distally to the MtII and the MtIII, and also attaches to the medial aspect of the distal tarsal bones. The short medial CLs lie deep to the long medial CL and extend from the medial malleolus to the medial aspect of the calcaneus and sustentaculum tali. The long plantar ligament is a strong, flat band that originates at the proximal plantar surface of the calcaneus, extends distally, and attaches to the fourth tarsal bone and the MtIV. The dorsal tarsal ligament spreads out distally from the distal tuberosity of the talus and attaches to the central and third tarsal bones and proximal aspect of the MtIII and the MtIV. Numerous short intertarsal ligaments connect adjacent bones of the tarsus and have connections between tarsal and metatarsal bones.
The suspensory ligament (SL) also has an accessory ligament that extends proximally to originate from the plantar aspect of the fourth tarsal bone and the calcaneus.15 This anatomical relationship between the SL and the tarsus may explain why distal hock joint pain and suspensory injury may coexist, why some horses with primary SL pain show a positive response to tarsal flexion, and why there may be confusion with diagnostic analgesic techniques used to differentiate distal hock joint pain from proximal suspensory desmitis.
Diagnosis
Clinical Signs
Swelling is a variable feature of hock-related lameness. There are numerous common swellings of the tarsus. but the presence of swelling is not pathognomonic for tarsal region pain (see Chapter 6, page 58, and Figure 6-28Figure 6-29Figure 6-30Figure 6-31Figure 6-32). Swellings include capped hock, which must be differentiated from lateral dislocation or luxation of the superficial digital flexor tendon and swelling of the calcaneal bursae; tarsal sheath–associated or, less commonly, non–sheath associated thoroughpin; bog spavin (effusion of the tarsocrural joint); bone spavin (bony prominence of the dorsal and medial aspects of the distal tarsal region); curb (see Figure 78-1), a collection of soft tissue injuries involving the distal plantar aspect of the hock; and diffuse soft tissue swelling in the distal aspect of the crus and dorsal aspect of the tarsus associated with injury of the fibularis (peroneus) tertius. Rapid development of diffuse periarticular swelling may follow trauma of the tarsus or may herald periarticular cellulitis. Distention of the tarsocrural joint can be an incidental finding but may reflect primary joint pathology. Distention of the distal hock joint capsules is rarely detectable clinically, but if it occurs in association with OA, there may be firm enlargement on the medial aspect of the limb reflecting periarticular new bone and overlying fibrous tissue. The presence of this swelling, bone spavin, is neither required for horses to be lame as a result of distal hock joint pain nor pathognomonic for distal hock joint pain in horses in which it is found. Swelling restricted to the medial or lateral aspect of the tarsus may reflect CL injury and malleolar fractures of the distal aspect of the tibia.
Some horses with tarsal region pain resent passive flexion, but exaggerated lifting of the limb to avoid maximal flexion is more likely to reflect stifle pain. Although there are many advocates of the Churchill test for the detection of distal hock joint pain (see Chapter 6), we do not find this test particularly useful because there are many false-positive and some false-negative responses. This may reflect the degree of pressure applied, because one author (SJD) is rarely able to induce pain, whereas the other (MWR) frequently does elicit a pain response. Some horses with distal hock joint pain do manifest a positive reaction to palpation of the medial soft tissue structures and the proximal medial metatarsal region, likely reflecting the presence of periarticular soft tissue pain associated with OA. Horses often manifest a positive response to compression of the distal medial aspect of the tarsus and proximal medial aspect of the metatarsal region statically, and lameness can often be exacerbated with compression of this region followed by trotting, a dynamic test; yet pain in these horses is localized with diagnostic analgesia to the distal portion of the hindlimb. Proximal suspensory desmitis and lameness associated with the metatarsophalangeal joint are common diagnoses in these horses. It is possible that horses with distal hindlimb pain move abnormally and have coexistent pain in the region compressed using the Churchill test (see Figure 6-33Figure 6-34Figure 6-35). The absence of a positive Churchill test result should not lead the examiner to conclude the horse does not have tarsal region pain, a false-negative response. Unless clinical signs are diagnostic or a horse is suspected to have a fracture, diagnostic analgesia should always be used to confirm the presence of tarsal region pain.
Shoe wear can be excessive in horses with chronic tarsal region pain. Shoes are often worn on the toe or, most commonly, on the dorsal and lateral aspects (see Figure 6-38). Often, the fullering and toe grab, if present, are worn completely through, a finding that is most prominent in horses shod in aluminum shoes. Horses with pain causing lameness from other sources in the distal aspect of the hindlimb can manifest similar shoe wear, so this finding is not pathognomonic of distal hock joint pain. Horses with chronic tarsal region pain often have coexistent signs of pain on palpation of the gluteal and thoracolumbar area. Concurrent back and gluteal pain is likely secondary to chronic abnormal limb carriage causing muscle pain.
Lameness can range from mild to severe. Horses often warm out of lameness and are often able to perform with low-level distal hock joint pain. In racehorses, particular the Standardbred (STB), trainers often comment that the “horse throws away the lameness at speed.” There are no pathognomonic clinical signs or gait deficits associated with tarsal region pain. Gait abnormalities associated with hock-related lameness are very variable both in degree and in character, depending on the underlying cause of lameness. A reduction in the cranial phase of the stride at the trot is a consistent finding but is a common finding in horses with any source of pain causing hindlimb lameness. When observed from behind, a trotting horse with tarsal region pain during protraction swings the affected hindlimb medially toward the midline and then stabs laterally while landing, often called a “stabby” hindlimb gait. This is particularly noticeable when horses have bilateral hindlimb lameness. Based on the clinical observation of a stabby hindlimb gait and positive response to upper limb flexion (see later) a diagnosis of distal hock joint pain is made, particularly in Western performance horses or gaited breeds, and empirical treatment is undertaken and is successful. However, this stabby hindlimb gait is not pathognomonic for tarsal region pain, and horses with lameness as a result of pain originating anywhere in the distal aspect of the hindlimbs can manifest this type of gait abnormality. Diagnostic analgesia should be used if horses do not respond to initial treatment. Some horses with severe tarsal region pain and swelling carry the limb wide, avoid flexion, and swing the limb laterally during protraction. These horses are often reluctant to flex the hock while standing during the palpation and manipulation portions of a lameness examination.
Kinematic gait measurements were recorded after endotoxin-induced lameness of the distal tarsal joints.16 Both fetlock and tarsal joint extension during stance phase decreased, fetlock joint flexion and hoof height during swing phase increased, limb protraction decreased, and vertical excursion of the tuber coxae became more asymmetrical. These observations are not entirely consistent with the observations made in natural disease.
More recently, three-dimensional kinematic gait analysis was performed before and after experimental induction of synovitis of the centrodistal and tarsometatarsal joints resulting in mild lameness.17 There were significant decreases in tarsal joint flexion and in dorsal translation (sliding) of the metatarsal region relative to the tibia during the stance phase.17 Measurement of ground reaction forces with subtle lameness indicated reduced weight bearing on both the lame hindlimb and the contralateral forelimb but no change in the opposite hindlimb. Thus the gait may appear to have less bounce, rather than overt lameness being detectable. With mild increase in lameness there was reduced tarsal flexion in the stance phase and decreased forward sliding of the distal joints. This results in reduced propulsion, influencing quality of the gait, and less absorption of concussion. Movements that require maximum tarsal flexion are likely to be most painful, and resistance to perform such movements may be apparent before lameness is observed.
Horses with tarsal region pain often respond positively to an upper limb flexion test (see Chapter 8, page 84 and Figure 8-8). This test has erroneously been called the spavin test and a positive response should not be interpreted as pathognomonic for tarsal region pain. When it is suspected that a horse has tarsal region pain, this test often gives false-positive results. The most marked response to an upper limb flexion test may indeed be observed in horses with tarsal region pain, but a positive response can be seen with pain originating from the stifle, the hip region, and even the distal aspects of the limb. The upper limb flexion test is not specific, nor is the “hock extension test” (see Figure 8-10), a test used to exacerbate lameness in horses with tarsal region pain. There is no substitute for accurate diagnostic analgesia.
Diagnostic Analgesia
Analgesia of the hock region can be accomplished by perineural analgesia of the fibular (peroneal) and tibial nerves or by intraarticular analgesia. Although the latter is theoretically more specific, there are a number of important limitations. False negative results can occur in the presence of subchondral bone pain and/or extensive cartilage pathology. Horses with incomplete fractures of the talus or central tarsal bone often show little response to intraarticular diagnostic analgesia but do show a marked improvement after perineural analgesia of the fibular and tibial nerves. Lameness may be improved rather than abolished, and although this may be easy to appreciate in a moderately lame horse, it is less easy in a horse with a subtle lameness. Intraarticular analgesia has limited ability to influence periarticular soft tissue structures that may be contributing to pain causing lameness. The capacity of the centrodistal and tarsometatarsal joints is relatively small, and injection of too large a volume of local anesthetic solution results in leakage; the close proximity of the plantar outpouchings of the tarsometatarsal joint to the SL means that intraarticular analgesia of the tarsometatarsal joint may remove pain from the SL. With advanced joint space loss or periarticular new bone formation, intraarticular analgesia may not be physically possible.
Perineural analgesia of the fibular and tibial nerves is well tolerated by most horses (see Chapter 10). One of us (SJD) deposits a subcutaneous bleb of local anesthetic solution at both injection sites using a 25-G needle before performing the blocks. Although a 3.7-cm needle is adequate for most horses, to reach the deep branch of the fibular nerve requires a 5-cm needle in large (700 kg) horses. These nerves are large, and it takes longer for analgesia to develop than with more distal limb blocks. Do not be in a hurry to move proximally in the limb and perform intraarticular analgesia of the stifle or hip joints, because these blocks may take a full hour to work. We usually first evaluate the horse 20 minutes after injection and for up to an hour. It is important to recognize that successful blocks may increase or create a toe drag; improved stride length, rhythm, and symmetry of the hindquarters must therefore be used to evaluate improvement in lameness. Occasionally a horse will stumble slightly after fibular and tibial nerve blocks, but we commonly see horses ridden before and after and do not believe there are undue risks.
When performing intraarticular analgesia of the distal tarsal joints, we routinely block the tarsometatarsal joint first, because this is relatively easy and safe to perform, and commonly find that horses with centrodistal joint pathology are improved. If there is partial or no response, then the centrodistal joint is blocked. In a study using 66 cadaver limbs, mepivacaine (5 mL) was injected into either the tarsometatarsal or centrodistal joints; synovial fluid samples were collected from the tarsocrural, centrodistal, and tarsometatarsal joints 15 minutes later.12 Concentrations of mepivacaine that were potentially analgesic were found in the centrodistal and tarsocrural joints after injection of the tarsometatarsal joint in 64% and 4% of limbs, respectively After injection of the centrodistal joint, analgesic concentrations of mepivacaine were found in the tarsometatarsal and tarsocrural joints in 60% and 24% of limbs, respectively. Despite these results we have never clinically recognized improvement in tarsocrural joint pain after intraarticular analgesia of the centrodistal and/or tarsometatarsal joints. We use a maximum volume of 3 to 4 mL of mepivacaine and evaluate the response 5 to 10 minutes after injection. Larger volumes will leak out of the injection site, increasing the likelihood of inadvertent analgesia of the proximal SL and other metatarsal structures. False-negative results may occur even in the absence of detectable radiological abnormalities, and the response to intraarticular medication may be substantially better. However for the much larger tarsocrural joint we use at least 20 mL of mepivacaine and will wait up to 30 minutes before declaring that the response is negative. One of us (MWR) has found that volumes of local anesthetic solution of up to 40 to 50 mL may be required to abolish pain associated with severe OA of the tarsocrural joint, and often the examiner needs to wait 45 to 60 minutes for the full effect of the intraarticular block to work.
Diagnostic Imaging
Four radiographic images of the tarsus are required: lateromedial, dorsolateral-plantaromedial oblique, dorsomedial-plantarolateral oblique (DM-PILO), and dorsoplantar.18 Lesions may be detectable only in a single view; thus in our opinion all four views should be obtained routinely. To cut through the centrodistal and tarsometatarsal joint spaces, it is important that the horse be standing with the metatarsal region vertical and bearing weight evenly on each hindlimb. Because the centrodistal and tarsometatarsal joints slope distally from laterally to medially, to reliably cut through the joint spaces in a lateromedial image, the x-ray beam should be angled 10 degrees distally. If a horizontal x-ray beam is used, it can be difficult to cut through the entire centrodistal joint space in a dorsoplantar projection, and it may appear that one side of the joint is narrowed. An additional dorsal 5° proximal-plantarodistal oblique image helps to determine whether there is genuine joint space narrowing.
Some lesions may be missed in dorsoplantar images, such as an axial osteochondrosis lesion of the medial malleolus of the tibia or a parasagittal fracture of the talus. Additional views obtained by angling the x-ray beam slightly obliquely (dorsal 10- to 20° lateral-plantaromedial oblique image) may be required in selected horses. A flexed lateromedial image and a flexed skyline image can give important additional information in some horses, particularly those with lesions involving the proximal and plantar aspects of the talus, those with osteochondral fragments involving the plantar pouch of the tarsocrural joint, and those with radiolucent defects on the calcaneus. A flexed dorsoplantar image can be useful to evaluate the proximal aspect of the talus in horses with incomplete fractures of this bone but is difficult to obtain.
Nuclear scintigraphy is most useful when pain causing lameness has been localized to the tarsus but no radiological or ultrasonographic abnormalities are detected to explain the lameness.19 The identification of increased radiopharmaceutical uptake (IRU) may prompt acquisition of additional radiographic images that yield a diagnosis. Scintigraphy may also be useful in horses that are difficult to nerve block or those that are examined for poor performance rather than overt lameness. It is important to recognize that RU in the distal tarsal bones can be influenced by the type of work history. For example, there is greater RU in the dorsal aspect of the central and third tarsal bones in elite show jumpers compared with horses from other disciplines.5 In a plantar scintigraphic image of the tarsus it is common and considered normal to have greater RU in the subchondral bone of the lateral aspect of the tarsometatarsal joint and the proximal aspect of the MtIV compared with medially.20 This finding should not be interpreted as supportive of a diagnosis of distal hock joint pain. In young racehorses with early OA of the centrodistal and tarsometatarsal joints, focal moderate-to-intense IRU is found most often in the dorsal and lateral aspects of these joints, corresponding to radiological abnormalities detectable on the dorsomedial-plantarolateral radiographic image.21 The most common location for fractures of the central and third tarsal bones is on the dorsolateral aspect, and fractures can most reliably be seen in the dorsomedial-plantarolateral oblique radiographic image (Figure 44-1). These findings differ somewhat from most anecdotal reports, suggesting that it is the medial aspect of these joints that show early radiological changes and may be a reflection of a difference between racehorses and sports horses. In older racehorses with advanced OA and sports horses, scintigraphic and radiological evidence of OA is commonly found on both the medial and lateral aspects of the distal hock joints.

Fig. 44-1 A, Lateral (left two images) and plantar scintigraphic images of a 2-year-old Standardbred pacing filly with right hindlimb lameness as a result of a central tarsal bone fracture. Focal, moderate increased radiopharmaceutical uptake can be seen involving the dorsolateral aspect of this bone (arrows), a common location to find fractures or early osteoarthritis in racehorses. B, Dorsomedial-plantarolateral (DM-PlLO) digital radiographic image showing an incomplete fracture of the central tarsal bone (arrows). Fractures of the central and third tarsal bones and early signs of osteoarthritis can be seen most commonly in a DM-PlLO radiographic view, indicating disease in young racehorses is found in predominantly the dorsal and lateral aspects of the distal hock joints.
Ultrasonography is invaluable for the assessment of both periarticular soft tissues and the tarsocrural joint. An excellent review of normal anatomy and examples of abnormality are published elsewhere.22 Magnetic resonance imaging (MRI) and computed tomography (CT) have the potential to yield valuable additional information when a diagnosis cannot be reached by other means. Normal MRI and CT anatomy references are available.23-25
Articular Diseases of the Tarsus
Osteoarthritis of the Distal Hock Joints and Distal Hock Joint Pain
Distal hock joint pain is common in horses from all disciplines and is often associated with OA. Distal hock joint pain is known colloquially as bone or jack spavin or occult or blind spavin in the absence of radiological abnormalities. The term juvenile spavin has been used to describe early OA that had a prevalence of 20% in a group of horses younger than 2 years of age.26 Although it is usually seen in mature horses used for sport or pleasure, distal hock joint pain can occur in young Thoroughbred (TB) and STB racehorses and Western performance horses (see Chapter 120). Distal hock joint pain may be a sequela to incomplete ossification of the central and third tarsal bones (see page 517). Certain conformational abnormalities (such as sickle-hock, in-at-the-hock, or cow-hock conformation) or excessive straightness of the hindlimbs may predispose to distal hock joint pain, although this condition frequently occurs in normally conformed horses. Traditionally it has been proposed that OA of the distal hock joints is caused by excessive compression and rotation of the distal tarsal joints as the horse jumps or stops, which results in abnormal tension on the intertarsal ligaments. However, this theory is not consistent with the common recognition of distal hock joint pain in pleasure horses or its high incidence in Icelandic horses, a breed in which OA is thought to be a heritable condition.27 Distal hock joint pain is classically thought to begin on the dorsomedial aspect of the joints and to progress dorsally. However, it is our experience that in OA, scintigraphic or radiological abnormalities are frequently first identified only on the dorsolateral aspect of the joints, a region of high compressive strain. Previous exercise history and thus loading of the joints may be influential.28 Nuclear scintigraphic studies of clinically normal mature horses in active work has shown mild greater uptake of radiopharmaceutical on the lateral aspect, which is consistent with increased modeling, presumably the result of a relative increased loading laterally compared with medially.7
The centrodistal and tarsometatarsal joints are most commonly affected, either individually or together, but OA of the proximal intertarsal joint does occur, usually in association with OA of the more distal joints. The condition may be unilateral but is often bilateral. Occasionally OA of the talocalcaneal joint occurs either in isolation29,30 or together with OA of the centrodistal and tarsometatarsal joints31 (see page 516).
History
Clinical signs of distal hock joint pain vary considerably among horses, ranging from a moderate-to-severe unilateral lameness to subtle changes in performance without overt lameness (see Chapter 97Chapter 106Chapter 107Chapter 108Chapter 109Chapter 110Chapter 111Chapter 112Chapter 113Chapter 114Chapter 115Chapter 116Chapter 117Chapter 118Chapter 119Chapter 120Chapter 121Chapter 122Chapter 123Chapter 124Chapter 125Chapter 126Chapter 127Chapter 128Chapter 129). These signs include the horse becoming disunited in canter, being unwilling to canter with a particular lead, and being reluctant to turn or decelerate with proper engagement of the hindlimbs. The owner may comment that the farrier has experienced difficulties when shoeing the horse. Frequently a horse with bilateral distal hock joint pain has low-grade stiffness that wears off (warms out of pain) with work. Lameness frequently improves or resolves with rest but recurs when work is resumed. Treatment with nonsteroidal antiinflammatory drugs (NSAIDs) usually results in an improvement in lameness unless it is severe.
Clinical Signs
In many horses no abnormalities are detectable by visual inspection or palpation of the hock region. In horses with more chronic distal hock joint pain there may be enlargement over the medial or dorsomedial aspects of the distal hock joints, which is the result of periarticular soft tissue thickening. Distention of the tarsocrural joint capsule may occur either coincidentally or reflect involvement of the proximal intertarsal joint. Frequently there is secondary soreness of the epaxial muscles in the lumbar region and sometimes caudal gluteal muscle soreness. The toe and branches of the shoe of the lame limb, or both limbs, may wear abnormally. In our experience, shoe wear in this location, however, is not pathognomonic of distal hock joint pain. Some horses, if not properly trimmed, develop lateral flare of the hoof and mediolateral foot imbalance, with the foot higher medially. Lameness may worsen when shoe additives such as toe grabs and heel calks are applied, an observation that can be useful in therapeutically shoeing a horse with distal hock joint pain (see later). Flexion of the limb may be resisted slightly, but marked lifting of the limb during flexion is more likely to reflect stifle pain. The Churchill test (see Chapter 6) is helpful in identifying distal hock joint pain in some, but by no means all, horses. Soreness associated with specific acupuncture points (see Chapter 92) can also be suggestive of distal hock joint pain.
Lameness varies greatly in degree and is not necessarily correlated with the degree or type of osteoarthritic change detected radiologically. The horse should be assessed moving from the side, from behind, and from in front to appreciate all gait abnormalities. These abnormalities may include asymmetrical movement of the tubera coxae and tubera sacrale; reduced arc height of foot flight, with or without toe drag; shortening of the cranial phase of the stride; reduced extension of the fetlock; and a tendency for the limb to swing medially during protraction and slide laterally at ground contact. Lameness may be accentuated on a circle, in some horses with the lame or lamer limb on the outside, and in others with it on the inside. Gait abnormalities may be accentuated if the horse is ridden. However, none of these characteristics is pathognomonic for distal hock joint pain.
Proximal (upper) limb flexion tests (i.e., the so-called spavin test) are useful in accentuating lameness in some, but not all, horses with distal hock joint pain. The hindlimb should be held with the metatarsal region parallel to the ground for 60 to 90 seconds before the horse is trotted away. The limb may be held either by the toe of the foot or by cupping the hands behind the fetlock. Applying pressure to the digital flexor tendons should be avoided. The response to flexion should be interpreted in light of the discipline of the horse, current work history, the degree of accentuation of lameness, and its duration. Flexion of the nonlame or least lame limb should be performed first and the response compared with the contralateral limb. In some horses there is a paradoxical increase in lameness in the weight-bearing limb, presumably because of joint compression or increased subchondral bone pressure. Because of the reciprocal apparatus of the hindlimb, a positive response to proximal limb flexion is not specific for distal hock joint pain. The response to flexion may be recorded as none (0), mild (+1), moderate (+2), or severe (+3). A severe response is unusual in horses with distal hock joint pain.
Diagnostic Analgesia
Diagnostic analgesia is important to confirm the source(s) of pain. Although intraarticular analgesia is potentially more specific than perineural analgesia, the results can be misleading. A negative response to intraarticular analgesia does not preclude distal hock joint pain. Narrowing of the centrodistal joint space or periarticular new bone can prohibit intraarticular injection. In the presence of extensive subchondral bone damage the response to intraarticular analgesia is very poor. Even in the absence of radiological change the response to intraarticular medication is sometimes substantially better than that to intraarticular analgesia, but the converse is also true in some horses.
However, intraarticular analgesia is very useful in many horses. The degree of communication between the centrodistal and tarsometatarsal joints is variable.9,10 The techniques for intraarticular analgesia are described in Chapter 10. Improvement in lameness by 50% or more is considered a positive response. In our experience, lameness is often substantially improved within 10 minutes, although some practitioners reassess lameness after 30 minutes.32 We find reassessment of the response to flexion potentially misleading, although some practitioners routinely repeat flexion tests.32 Perineural analgesia of the superficial and deep fibular (peroneal) and tibial nerves (see Chapter 10), although not specific for distal hock joint pain, can be very helpful in confirming hock pain, assuming that pain arising from the more distal aspects of the limb has already been excluded. With practice these blocks are reliable and safe and often result in a much greater degree of improvement in lameness than intraarticular analgesia. Improvement is generally seen within 20 minutes, but occasionally the response is delayed, and it is preferable not to proceed with further blocks until at least 1 hour has elapsed. Horses with specific performance problems associated with distal hock joint pain, rather than overt lameness, may respond better to intraarticular medication than either intraarticular or perineural analgesia.
Radiography and Radiology
Both hocks should be examined radiographically because the condition is often bilateral, although at the time of examination lameness may be unilateral. Radiological abnormalities consistent with osteoarthritis include periarticular osteophyte formation (Figure 44-2), subchondral lucent areas (Figure 44-3), increased opacity of subchondral and trabecular bone, periosteal new bone, and narrowing of joint spaces. The correlation between the degree of lameness and the extent of radiological abnormalities is poor.33,34 Some horses show profound lameness initially, with no detectable radiological abnormality but with rapidly progressive lesions. Other horses respond to intraarticular analgesia but never develop radiological abnormalities. However, extensive changes may be present when lameness is first recognized. Some horses predominantly develop periarticular changes, whereas others have abnormalities confined to the central and third tarsal bones and the proximal aspect of the MtIII. The reason for these differences is currently unclear. Small osteophytes or enthesophytes on the dorsoproximal aspect of the MtIII can be incidental radiological abnormalities; they were found to occur in 25% of 455 horses, in 13% of which they were bilateral.35 Osteophytes and enthesophytes could not be reliably distinguished. There was no significant difference in frequency of occurrence in lame and nonlame horses; nor was there any significant difference in frequency of occurrence among horses with distal hock joint pain, proximal suspensory desmitis, or other causes of lameness unassociated with the hock.35 However, there was an association between the presence of a spur and the radiological grade of OA in the centrodistal and tarsometatarsal joints. Horses with severe subchondral radiolucency tend to be lamer and respond poorly to intraarticular analgesia and intraarticular medication. Involvement of the talocalcaneal-centroquartal (proximal intertarsal) joint merits a more guarded prognosis.

Fig. 44-2 A, Dorsolateral-plantaromedial oblique radiographic image of the tarsus of a horse with mild periarticular osteophyte formation (arrow) on the distal dorsomedial aspect of the central tarsal bone and increased radiopacity of the adjacent trabecular bone. B, Lateromedial radiographic image of the distal tarsal joints. There is a large periarticular osteophyte on the dorsoproximal aspect of the third metatarsal bone (arrow), traversing the tarsometatarsal joint.

Fig. 44-3 Dorsolateral-plantaromedial oblique radiographic image of the tarsus of a horse with osteoarthritis of the centrodistal joint. There is subchondral radiolucency involving the subchondral bone of the medial aspect of the centrodistal joint (arrow). There is also increased opacity in the region of the interosseous ligament between the central and third tarsal bones.
Nuclear Scintigraphy
In many horses nuclear scintigraphy is unnecessary, but it can be very helpful in difficult horses and those with performance problems rather than overt lameness.19,36 A region of IRU may be focal or more diffuse. Very focal IRU may reflect intertarsal ligament enthesopathy rather than OA.37 Intense IRU may be present in the absence of radiological abnormality, and these horses tend to respond poorly to intraarticular medication, despite a positive response to intraarticular analgesia. In young racehorses and in some sports horses, focal IRU can indicate the presence of a fracture of the central or third tarsal bone (see Figure 44-1), explaining the lack of response to intraarticular medication. Because IRU may occur in association with primary lameness originating from pain elsewhere in the limb, results should be interpreted cautiously, unless supported by radiological abnormalities.
Treatment
The aim of treatment is to provide pain relief so that the horse can remain in work. Traditionally it has been suggested that if the horse is maintained in work, the affected joints will fuse. However, progressive radiological ankylosis is rarely observed, although radiological examination tends to underestimate the degree of joint fusion. Horses with involvement of the talocalcaneal-centroquartal joint and extensive radiolucent defects of subchondral bone have a more guarded prognosis.
Treatment options include a combination of palliative therapy with NSAIDs; intraarticular medication with corticosteroids, hyaluronan, or polysulfated glycosaminoglycans (PSGAGs); with or without systemic treatment with PSGAGs, oral nutraceuticals, or both, combined with corrective trimming and shoeing38; and adaptation of the work program. Extracorporeal shock wave treatment has recently been described, but long-term results are lacking.39 Intravenous infusion of a bisphosphonate, tiludronate, may reduce the severity of lameness in some horses but rarely results in resolution of lameness.40 If medical therapy fails, surgical treatment, including cunean tenectomy, subchondral forage to reduce intraosseous pressure,41 drilling of the affected joints to promote arthrodesis,42 chemical induction of ankylosis using sodium monoiodoacetate43-51 or ethyl alcohol,46 and neurectomy47 are options.
Selection of treatment depends on the degree of lameness, extent of radiological abnormalities, use of the horse, regulations for competition, response to previous treatment, time available, and financial constraints. Resting the horse usually is not beneficial. Palliative treatment with NSAIDs such as phenylbutazone is useful in pleasure horses; the lowest dose that alleviates lameness should be used. Long-term use of phenylbutazone, 1 g twice daily for a 500-kg horse, is generally well tolerated. Any treatment should be combined with corrective trimming and shoeing to ensure correct mediolateral balance and to facilitate breakover by shortening the toe, squaring and rolling the toe of the shoe, or setting the shoe back from the toe. A lateral trailer14 or a lateral extension of the shoe provides symptomatic relief in some horses and tends to stop excessive twisting of the limb. However, these devices may be contraindicated in horses that have to stop and turn quickly, because the extension may dig into the footing and stop the distal limb abruptly, causing abnormal torque on the distal limb joints. Removing toe grabs and heel calks and using a flat shoe may reduce shear stress on the distal hock joints.
Intraarticular medication with corticosteroids, such as methylprednisolone acetate or triamcinolone acetonide, with or without hyaluronan, is extremely useful for management of horses with distal hock joint pain. However, horses with extensive radiological abnormalities, especially diffuse radiolucent regions in the subchondral bone, often have a limited response. Horses with scintigraphic abnormalities in the absence of radiological change also respond poorly. Some veterinarians routinely treat both the centrodistal and tarsometatarsal joints of both hocks by using 60 to 80 mg of methylprednisolone acetate in each joint.29 If the competition schedule allows, the horse is turned out for 3 to 4 days, followed by 3 to 4 days of light riding before resumption of normal activity. Phenylbutazone (2.2 mg/kg sid) is also recommended for 7 days to decrease the possibility of postinjection joint flare. Most horses are sound enough to resume work within 7 to 10 days and stay serviceably sound for 3 to 6 months, depending on severity of disease and level of horse use.
Similar results have been achieved using triamcinolone acetonide, 6 mg per joint (SJD). One of us (SJD) does not routinely combine intraarticular therapy with NSAIDs and usually treats only the tarsometatarsal joint. A study by Serena and colleagues demonstrated that therapeutic concentrations of methylprednisolone acetate were achieved in the centrodistal joint within 6 hours of injection of 80 mg into the tarsometatarsal joint in eight of nine horses (in the ninth horse concentrations were similar in both joints, indicating direct communication between the two joints).13 However, higher concentrations can be obtained by direct injection. There are no controlled clinical trials assessing the relative efficacy of different corticosteroids or the use of a combination of corticosteroids and hyaluronan, although some clinicians believe that combination therapy lasts longer. Hyaluronan alone is of dubious value. There are also no large-scale, long-term follow-up studies. However, in a retrospective study of 42 horses that were examined at a referral hospital and used predominantly for general purposes or amateur-level competitions and that showed a positive response (>50% improvement in lameness) to intraarticular analgesia of the tarsometatarsal or centrodistal joints, 38% became sound enough to resume full work after intraarticular medication with either triamcinolone acetonide or methylprednisolone acetate.48 In a different study with similar inclusion criteria, 52% of 46 horses were able to return to their former athletic function.49 The choice of drug did not influence outcome in either study. Both studies showed no relationship between the severity of radiological abnormality and outcome. However, we believe that this reflects one of the inclusion criteria that horses had to respond to intraarticular analgesia. In our experience horses with extensive subchondral radiolucent areas respond poorly to both intraarticular analgesia and medical treatment.
Corticosteroid injections can be repeated two or three times per year without promoting progressive radiological change. In some horses it is possible to predict when lameness will recur, and repeated treatment before this recurrence can maintain soundness. Although cunean bursitis is rarely recognized as a primary cause of lameness, some horses respond better if intraarticular treatment is combined with treatment of the bursa. In young racehorses with distal hock joint pain, one of us (MWR) uses a combination of intraarticular injection (tarsometatarsal and centrodistal joints) of a combination of corticosteroids (methylprednisolone acetate [40 to 80 mg/joint] and isoflupredone acetate [2 mg/joint]) and infiltration of this combination of corticosteroids and Sarapin into the cunean bursa and subcutaneously over the proximal aspect of the MtII. It is in this area on the medial aspect of the tarsus and proximal aspect of the metatarsal region that these horses show a positive response to deep palpation (see earlier). A series of intraarticular injections of PSGAG (three injections given every 2 weeks) can be useful in competition horses and racehorses with distal hock joint pain.
Systemic medication with PSGAG (500 mg intramuscularly [IM] once weekly for 6 weeks), hyaluronan (4 mg intravenously [IV] monthly), or oral nutraceuticals may be beneficial as adjunctive therapy. A small-scale study showed reduced frequency of intraarticular medication after the introduction of oral nutraceuticals.50 Anecdotally, treatment with PSGAG 3 to 4 days before an event may be useful. In some horses, increasing the dose of PSGAG to 1 g weekly gives better results. Clinical trials with intravenous administration of tiludronate have shown mixed results; overall there was a positive effect on the degree of lameness, but lameness did not resolve in the majority.40
In a small-scale study shock wave treatment that was performed with horses under general anesthesia, followed by 5 weeks of rest, resulted in an 80% improvement in lameness in horses 90 days later,39 but long-term results are not available.
A variety of techniques for surgical arthrodesis of the distal hock joints* and subchondral forage41 exists. Subchondral forage, which aims to reduce intraosseous pressure and therefore pain, can provide rapid pain relief in some horses, enabling return to work. However, this technique has not found widespread favor. Techniques aimed at achieving arthrodesis are more popular, but effective arthrodesis and resolution of lameness often takes up to 12 months using either drill or laser techniques. Careful surgical technique is essential to avoid the development of extensive periarticular new bone, which can itself cause pain. With use of the three-drill tract procedure,42,51 a 66% success rate has been reported.51 However, the results in upper-level competition horses have been less favorable.32 In Western performance horses a success rate of approximately 70% has been achieved.56 Generally both the centrodistal and tarsometatarsal joints are treated. Cunean tenectomy alone may result in temporary improvement in clinical signs but is unlikely to restore soundness.57 Chemical fusion with sodium monoiodoacetate has had excellent results in some horses,43,45 with reported success rates of 27 of 29 horses (93%) and 41 of 50 (82%) horses 12 months after treatment. However, even if positive radiographic contrast studies do not show physical communication between the centrodistal and talocalcaneal-centroquartal joint, it is likely that in some horses sodium monoiodoacetate can spread to these joints and result in progressive OA. Ethyl alcohol can also be used to achieve arthrodesis,46 but there are currently no long-term follow-up results, although anecdotally the results are favorable. Arthrodesis of the centrodistal and tarsometatarsal joints can be followed by either fracture of the central or third tarsal bone or the development of OA in the talocalcaneal-centroquartal joint. Once OA of this joint has developed, there is obligatory involvement of the tarsocrural joint, and chronic, severe lameness ensues. Neurectomy of the deep fibular nerve and a partial neurectomy of the tibial nerves relieves the pain associated with OA of the distal hock joints,47 and approximately 60% of treated horses return to full athletic function.
Osteoarthritis of the Talocalcaneal Joint
OA of the talocalcaneal joint is unusual and may occur in isolation29,30 or together with OA of the centrodistal and/or tarsometatarsal joints.31 There are frequently no localizing signs, although in a retrospective study there was distention of the tarsocrural joint in six of 18 horses.31 Lameness is resolved by perineural analgesia of the fibular and tibial nerves and may be improved by intraarticular analgesia of the tarsocrural joint. Radiological abnormalities are best identified in lateromedial or dorsomedial-plantarolateral oblique images, or in some horses a flexed proximoplantar-distal plantar image, and include subchondral lucency or increased radiopacity and narrowing of the joint space (Figure 44-4). Scintigraphy reveals focal, moderate-to-intense IRU in the subchondral bone of the talocalcaneal joint and can be differentiated from enthesopathy of the attachment of the lateral CL and lesions involving the sustentaculum tali (see later) by acquiring lateral, plantar, and, if necessary, medial and flexed lateral scintigraphic images. Occasionally lesions that are not evident radiologically can be identified using MRI or CT. The prognosis with conservative management is guarded to poor. Surgical arthrodesis has resulted in improvement in, but not resolution of, lameness.31
Osteoarthritis of the Tarsocrural Joint
OA of the tarsocrural joint may occur as a primary disease, may develop secondarily to osteochondrosis (see Chapter 56) or OA of the distal hock joints (see page 512), or may be a sequela to trauma. There may be distention of the tarsocrural joint capsule, but this is a variable feature. The joint capsule may feel thickened, more so than observed in horses with idiopathic effusion or a bog spavin as the result of osteochondritis dissecans (OCD). Initially horses respond favorably to intraarticular injections into the tarsocrural joint. There is controversy regarding the association of corticosteroid injections and the subsequent development of OA of this joint. Although in most horses with end-stage OA there is a history of numerous injections including corticosteroids into the tarsocrural joint, this is not always the case. We both believe that there is an association between the presence of OCD and the subsequent development of severe OA in older horses (6- to 8-year-old racehorses and sports horses), whether or not the affected horse had arthroscopic surgery to remove the fragments at a young age.
Lameness varies from mild to severe. Horses with longitudinal wear lines on the trochleas of the talus secondary to OCD of the cranial intermediate ridge of the distal aspect of the tibia often have only mild lameness. However, horses with focal partial- or full-thickness cartilage erosions on weight-bearing parts of the trochleas of the talus may have severe lameness (see Figure 56-11). The response to proximal limb flexion is variable. Lameness usually is partially improved by intraarticular analgesia, but occasionally there are false-negative results. A large volume (up to 50 mL) of local anesthetic solution may be necessary, and often it takes 45 to 60 minutes for lameness to improve in horses with severe OA of the tarsocrural joint. Perineural analgesia of the fibular and tibial nerves results in substantial improvement in lameness. In horses with primary OA of the tarsocrural joint, usually there are no detectable radiological abnormalities, or only subtle evidence of subchondral sclerosis and narrowing of the tarsocrural joint space, and scintigraphic examination is often inconclusive. Diffuse mild IRU may be all that is seen, sometimes localized to the cranial and caudal distal aspect of the tibia. In racehorses, scintigraphic examination often reveals IRU involving the distal aspect of the tibia and proximal aspect of the talus and must be differentiated from subchondral trauma or fracture of the distal tibia and talus.58 A flexed lateral scintigraphic image reveals that IRU involves both sides of the tarsocrural joint, unlike focal uptake, which remains associated with either the talus or the distal tibia. Ultrasonographic examination may reveal synovial proliferation even in the absence of detectable joint effusion. Definitive diagnosis is dependent on arthroscopic examination of the joint. The prognosis for resolution of lameness and return to full athletic function is generally poor to grave. Response to intraarticular medication is often disappointing.
Incomplete Ossification of the Central and Third Tarsal Bones
Incomplete ossification of the central and third tarsal bones is most common in premature or twin foals, but it can occur in full-term singles and is characterized by a sickle-hocked appearance. It may occur unilaterally or bilaterally. Radiologically the bones are smaller and more rounded than usual. Early recognition and treatment are essential to avoid crushing of these bones with resultant progressive OA. Foals with this condition must be rested in a stall or turned out in a small paddock with only their mare. However, many owners or farm managers are loath to give foals rest, and the condition becomes progressive, often leading to collapse and OA and fracture. Cylinder tube casts can be used effectively with good results. In some horses the condition goes unrecognized until a young horse increases work intensity, although the horse may have a preexisting curblike appearance of the hock. Lameness may be sudden in onset despite the existence of advanced radiological changes. Radiological examination reveals a wedge shape of the central and third tarsal bones, which are narrower dorsally (see Figure 128-4). One or more bones may be fractured. There is often advanced OA. Although affected horses may be used for pleasure riding, the prognosis for competition use is guarded.
Distention of the Tarsocrural Joint Capsule
There are many causes of acute or chronic synovitis of the tarsocrural joint (also known as bog spavin) including osteochondrosis, OA, trauma, poor conformation, hemarthrosis, infection, and idiopathic causes. There are case reports of eosinophilic synovitis59 and ectopic cartilage of unknown origin.60 Signalment varies and depends on origin. Clinical signs are excessive tarsocrural joint fluid, which is most easily recognized on the dorsomedial and plantarolateral aspects of the joint. Lameness may or may not be present and is dependent on the cause. Excessive distention of the joint capsule may result in mechanical lameness. Diagnosis is made on the basis of clinical appearance and the response to intraarticular analgesia if the horse is lame. Arthrocentesis may reveal hemorrhage. Oddly, the tarsocrural and antebrachiocarpal joints are the most common joints in which we have diagnosed intermittent severe lameness as a result of hemarthrosis.21 Large vessels that traverse the dorsal aspects of the joint capsules in both joints may be at risk for injury and cause subsequent bleeding into the joint. Radiographic examination should include four standard images, but if no radiological abnormality is detected, flexed lateromedial and flexed dorsoplantar (skyline) images may be helpful. Slightly oblique dorsoplantar images may be necessary to identify OCD of the medial malleolus of the tibia (see Chapter 56). The radiographs should be inspected carefully for evidence of previous surgery for removal of an osteochondral fragment from the cranial intermediate ridge of the distal aspect of the tibia or other common locations associated with OCD. Occasionally, small fragments remain at previous sites from which OCD lesions were removed, and it is possible that these small fragments or repair tissue at the site may be loose, causing persistent effusion. Lameness in these horses is usually minimal, and the decision to reoperate should be made on a case-by-case basis and reserved for those horses with pain that can be abolished with diagnostic analgesia. Effusion often persists even after removal of OCD fragments from the tarsocrural joint, and persistent effusion is usually not a cause of lameness but may be of concern cosmetically.
Ultrasonography is useful for characterizing the appearance of the fluid within the joint; synovial fluid is anechogenic, whereas blood is echogenic. Ultrasonography is also useful for assessment of the thickness of the joint capsule, the presence of synovial hyperplasia, and the thickness of the articular cartilage and may be more accurate than radiography for identification of osteochondral fragments.61 In the absence of radiological or ultrasonographic abnormalities, a diagnosis of idiopathic synovitis is made.
Treatment of horses with idiopathic synovitis involves fluid drainage and intraarticular injection of either 80 mg of methylprednisolone acetate or 12 mg of triamcinolone acetonide. Combining hyaluronan with the corticosteroids may provide joint protection, but the strong antiinflammatory effect of the corticosteroids seems most beneficial. Pressure bandages should be applied to help maintain joint decompression. Phenylbutazone (2.2 mg/kg) once daily for 7 days and confinement to a small area for 2 weeks is recommended. Approximately 50% of horses have resolution or decrease in effusion, although some horses may require retreatment. Intraarticular injection of atropine (8 mg) is sometimes successful. If joint effusion returns and the horse is not lame, the owner is advised that the horse has a cosmetic blemish that will probably not resolve completely. Horses that are lame and block to the tarsocrural joint but have no radiological lesions are candidates for scintigraphic examination and diagnostic arthroscopy (see discussion of OA of the tarsocrural joint, page 516). Hemarthrosis is discussed in Chapter 66.
Osteochondrosis of the Tarsocrural Joint
See Chapter 56 for a discussion of osteochondrosis of the tarsocrural joint (page 635).
Subchondral Bone Trauma
With the advent of MRI and CT there is increasing recognition of the role of subchondral bone trauma and pain in causing lameness.62 There are anecdotal reports of lesions involving the talus, calcaneus, and central and third tarsal bones, but as yet these lesions have been rather poorly defined, and risk factors and response to treatment have not been documented.
Osseous Cystlike Lesions
Occult osseous cystlike lesions, detected using CT but usually not by radiography, have been recorded in the medial malleolus of the tibia (five horses), intertrochlear groove of the talus (four horses), lateral malleolus (two horses), and cranial intermediate ridge of the distal aspect of the tibia (one horse).63 We have also seen single or multiple lesions in the distal subchondral bone plate of the tibia and the trochleas of the talus that were detectable scintigraphically and radiologically.64 There are usually no localizing clinical signs. Lameness is moderate to severe. In some but not all horses lameness is substantially improved by intraarticular analgesia of the tarsocrural joint. These lesions are associated with focal intense IRU. These lesions are believed to be of infectious or traumatic origin. Conservative management has resulted in persistent lameness in most but not all horses. Surgical curettage may offer a more favorable prognosis, but lesions involving the subchondral bone of the distal aspect of the tibia in the trochlear grooves are not accessible to arthroscopic evaluation and curettage. To access these lesions an extraarticular approach may be necessary. Four of six horses (67%) managed surgically returned to athletic function.63
Fragments in the Talocalcaneal-Centroquartal (Proximal Intertarsal) Joint
The tarsocrural joint communicates directly with the proximal intertarsal joint in immature horses through a slitlike opening and in adult horses through a broad opening in the dorsal reflection of the synovium that is located at the distal dorsal aspect of the talus (see Chapter 56). The proximal intertarsal joint is approached through this synovial fenestration during arthroscopic exploration of the tarsocrural joint. A report describes 17 horses with either a free-floating fragment, which was suspected to have originated and been dislodged from an associated OCD lesion in the tarsocrural joint, or a fragment located at the distal end of the medial trochlear ridge with attachment to the synovial reflection that separates the tarsocrural and proximal intertarsal joints.65 However, such fragments can be seen as incidental abnormalities and unassociated with lameness.18 Fragments associated with the distal aspect of the medial trochlear ridge of the talus can be seen in only a lateromedial radiographic image, whereas loose fragments within the proximal intertarsal joint most often can be seen on numerous radiographic images. Careful examination of the cranial intermediate ridge of the distal aspect of the tibia is necessary, because loose fragments within the proximal intertarsal joint most often dislodge from this location, and a depression will often be seen from which original fragment originated. Fragments associated with the distal aspect of the medial trochlear ridge are often enveloped in the joint capsule separating the tarsocrural and proximal intertarsal joints, medial to the fenestration between the joints. Sharp dissection is necessary to incise capsular attachments, and care must be taken to avoid damage to the articular surface of the central tarsal bone. Fourteen of 17 horses returned to racing or intended performance activity after arthroscopic removal of the fragment.65
Tarsal Bone Fractures and Luxations
Fractures of the Distal Tarsal Bones
Fractures of the central and third tarsal bones occur most frequently in STBs, cutting horses, or TB racehorses,66-70 but they occasionally occur in other horses, sometimes secondary to previous fusion of the centrodistal and tarsometatarsal joints. These fractures cause an acute onset of a moderate-to-severe hindlimb lameness that is usually most noticeable when the affected limb is on the inside of a circle.32 Despite acute onset of lameness, these fractures in young racing TBs may be the result of stress-related bone injury.69 The lameness is exacerbated by upper limb flexion. The degree of lameness diminishes after 1 to 2 weeks of rest, but lameness returns if the horse returns to work. Some horses with incomplete fractures of the central tarsal and third tarsal bones can race a number of times before lameness becomes pronounced. On initial diagnosis, some fractures appear chronic in both the TB and STB racehorse. Horses with bilateral third tarsal bone fractures may be examined for poor performance rather than overt unilateral hindlimb lameness. Within STB racehorses in North America, central and third tarsal bone fractures are more common than expected in pacers compared with trotters, even if the normal 3 : 1 pacer/trotter ratio is considered. Heat, soft tissue swelling, and pain on digital palpation of the distal tarsal bones usually accompany the fracture. Synovial effusion of the tarsocrural joint may occur in horses with central tarsal bone fractures but is not usually seen in horses with third tarsal bone fractures. Intraarticular analgesia is used to diagnose central and third tarsal bone slab fractures, but in some horses, particularly those with incomplete or complete, nondisplaced fractures, fibular (peroneal) and tibial nerve blocks are needed to abolish pain.
Diagnosis is made by radiography or scintigraphy, but a fracture may not be radiologically apparent until up to 10 days after injury, when demineralization of the fracture line occurs. Scintigraphy is useful in horses with mild or bilateral hindlimb lameness. Incomplete or bilateral fractures may be seen. Many fractures can often be identified on a lateromedial radiographic image but most consistently can be seen on a DM-PlLO image. If no radiological abnormality is detectable in standard images, additional oblique images, including a plantar 25° lateral-dorsomedial oblique image, should be obtained (or D65° M-PlLO image) (Figure 44-5). However, the precise location and orientation of fractures seem to vary between disciplines and between the central and third tarsal bones. Thus if a fracture is suspected, additional oblique images may be required. CT can be useful to determine the exact location and configuration of a fracture and to pinpoint screw location if surgical repair is elected. In STBs, two types of central tarsal bone fractures are seen. Authentic frontal (dorsal) plane slab fractures extending from the proximal-to-distal articular surfaces of the central tarsal bone are most common and are best seen in either a DM-PlLO or lateromedial image (see Figure 44-1). Another type of central tarsal bone fracture courses distodorsally from the proximal aspect of the central tarsal bone in the dorsal plane and breaks out of the dorsal cortex of the bone just proximal to the distal articular surface of the central tarsal bone (Figure 44-6). This second type of fracture can best be seen in a lateromedial radiographic image, and because the fracture line does not appear to extend to the distal articular surface, this fracture may not be an authentic slab fracture. Lameness is pronounced, and horses exhibit identical clinical signs to those with larger fragments. In Western performance horses the fracture line is generally located in a more plantar region of the third and central tarsal bones than is seen in racehorses. Third tarsal bone fractures are most commonly dorsal or dorsolateral. In TB racehorses a wedge-shaped conformation of the dorsolateral aspect of the third tarsal bone may be a risk factor for fracture.71 Comminuted fractures are more common in the central tarsal bone and may be difficult to identify radiologically.67 If comminution occurs, it is usually at the proximal aspect of the fracture, and fragments can be seen and removed using arthroscopic surgical techniques through the tarsocrural joint. Nuclear scintigraphy is invaluable for identifying the likely presence of a fracture if it cannot be determined radiologically.

Fig. 44-5 Plantar 25° lateral-dorsomedial oblique radiographic image of a tarsus. There is a complete slab fracture of the third tarsal bone. This radiographic image is the same projection as a dorsomedial-plantarolateral oblique image showing that the fracture is located on the dorsolateral aspect of the third tarsal bone.

Fig. 44-6 Lateromedial digital radiographic image of the right tarsus of a 3-year-old Standardbred filly with pronounced lameness abolished by perineural analgesia of the fibular (peroneal) and tibial nerves. Lameness did not change after intraarticular analgesia of the tarsocrural joint. There is an oblique dorsal plane fracture of the central tarsal bone (arrows) that courses distodorsally from the proximal articular surface of the central tarsal bone and to the dorsal cortex, just proximal to the centrodistal joint. Mild proliferative changes can be seen, indicating that at the time of diagnosis the fracture was chronic.
Horses may be treated conservatively69,70,72,73 or surgically.67,68,70,71 Seven horses with fractures of the third tarsal bone that were treated conservatively remained lame for 12 months after injury,67,68 whereas three horses treated by lag-screw compression returned to racing within 6 months.67 Six racehorses with central tarsal bone fractures remained lame, whereas six Quarter Horses treated surgically made a complete recovery.68 However, conservative management resulted in return to training within 8 months for 73% of 45 TB racehorses with fractures of the central or third tarsal bone,69 and this corresponds with our experience. In a retrospective study 20 of 24 horses with slab fractures of the central tarsal bone were STBs, and of these 82% raced after injury with conservative management.70 Of 28 horses with third tarsal bone slab fractures managed conservatively, 25 had unilateral and three had bilateral fractures, and there were 12 TBs, 15 STBs and one Quarter Horse.70 After conservative management, 87% of the STBs and 71% of the TBs raced after injury.70 During the study period five STBs with slab fractures of the central (one horse) and third (four horses) tarsal bones underwent surgical management with interfragmentary compression, and three raced after surgry.70 Ten of 14 STBs (71%) and two of six TBs (33%) returned to racing and started at least five races after injury, and four of five Quarter Horses (80%) returned to previous athletic function with conservative management.72 The prognosis in STBs appears satisfactory when conservative management is used, but there appears to be room for improvement in the TB racehorse. We do not know the long-term prognosis of a large group of TB racehorses managed surgically, however. If surgical treatment is performed, case selection is important, because many horses with central tarsal bone fractures have hidden fracture lines that could be inadvertently displaced during screw placement. The large head of a 4.5-mm cortex bone screw may cause soft tissue inflammation and a periosteal reaction. For third and central tarsal bone fractures, 3.5-mm cortex bone screws are preferred. One or two screws should be placed through stab incisions by using radiographic or fluoroscopic guidance, or by using CT. The use of a Herbert cannulated compression screw has been reported.68 Horses with fragments that are too small to allow lag-screw fixation, or those with chronic fractures of the third tarsal bone causing OA of the centrodistal or tarsometatarsal joints, can be managed by surgical drilling to facilitate arthrodesis of the joints.
Sagittal Fracture of the Talus
Sagittal fractures of the talus are rare, usually nondisplaced, can be difficult to diagnose, and have been recorded most frequently in STB and TB racehorses,74,75 but they can occur in any type of horse. Twelve racehorses had a history of chronic, mild hindlimb lameness that became acutely severe during a race.74,75 One of us (SJD) has also seen two endurance horses with acute-onset severe lameness after an endurance race.64 Lameness in other types of horses may be associated with trauma. Lameness is moderate to severe and is sometimes associated with distention of the tarsocrural joint capsule. The horse may stand with the limb somewhat protracted and show accentuation of lameness when turning. Intraarticular analgesia may improve lameness but rarely removes it completely, and negative results may also occur. Horses show marked improvement after fibular (peroneal) and tibial perineural analgesia. Fractures in racehorses usually originate at the proximal aspect of the sagittal groove of the talus and are often incomplete. Nondisplaced fractures can be difficult to identify radiologically; extra images, including a dorsal 10- to 20° lateral-plantaromedial oblique and a flexed dorsoplantar (skyline) image, can be helpful. Fractures caused by trauma are frequently comminuted, and the degree of damage may not be apparent radiologically. Nuclear scintigraphy can be helpful in confirming the presence of a fracture; there is usually intense focal IRU in the proximal aspect of the talus.74
Eleven racehorses with incomplete sagittal fractures of the talus were managed conservatively with a minimum of 1 month of stall rest followed by small paddock turnout. Seven returned to racing performance within 7 to 8 months after injury; approximately 50% had the same or improved performance.74 Both endurance horses were managed conservatively and returned to full athletic function.59 Horses with complete sagittal fractures have been managed by lag-screw compression using two 4.5-mm cortex bone screws.70 Prognosis may be favorable in horses with simple acute fractures, but the prognosis for horses with comminuted fractures is poor.
One of us (MWR) has seen two foals that had complete, nondisplaced slab fractures of the talus that healed well with conservative management.64 Acute lameness and moderate tarsocrural effusion were found in both foals; the fracture line could best be seen coursing from the proximal-to-distal articular surface of the talus in a dorsal 15° lateral-plantaromedial oblique radiographic image (Figure 44-7).

Fig. 44-7 Initial (A) and 6-week follow-up (B) digital dorsal 15° lateral-plantaromedial oblique radiographic images of a suckling Standardbred foal with acute hindlimb lameness and moderate tarsocrural joint effusion. A, A nondisplaced sagittal fracture of the talus can be seen (arrows) coursing from the proximal-to-distal articular surfaces. B, Six weeks later the fracture line appears blurred and cannot be seen at the proximal aspect of the talus but can still be seen at the distal aspect (arrows). This foal made a complete recovery using conservative management consisting of 10 weeks of box stall rest.
(Courtesy Dr. Jan Henriksen, Walnridge Equine Clinic, Creamridge, New Jersey, United States.)
Fractures of the Fibular Tarsal Bone
Fractures of the fibular tarsal bone (or calcaneus) are uncommon and usually the result of trauma. Physeal fractures in foals and fractures through the body of the bone are easily diagnosed because of the obvious loss of gastrocnemius muscle function, which results in a dropped-hock appearance. Chip fractures involving the plantar aspect of the calcaneus can be difficult to diagnose unless soft tissue swelling is present or a draining tract secondary to sequestra formation exists. Surgical removal of small fragments may be necessary, depending on size and location of the fragment (intraarticular or extraarticular). Diagnosis is confirmed radiologically. Flexed lateromedial and skyline images of the calcaneus are recommended in addition to standard views (Figure 44-8). Complete body and physeal fractures can be difficult to reduce and stabilize, but horses can be managed successfully with bone plates, screws, and wires by using the tension-band principle. It is not possible to place a bone plate directly plantad because of the presence of the superficial digital flexor tendon, but the plantarolateral or lateral surface of the calcaneus has been used successfully. One of us (MWR) has used a combination of interfragmentary compression and figure-eight tension band wiring to successfully repair fractures of the calcaneus in two miniature horses.64 Conservative therapy using casting methods alone has been unrewarding and is not recommended. Horses with open, comminuted fractures have a grave prognosis, and humane destruction should be advised. Prognosis for future performance activity in horses with physeal or full-body fractures is considered poor.
Fracture of the Lateral Malleolus of the Tibia
The lateral malleolus is considered to be the distal end of the fibula and develops as a separate center of ossification that fuses to the distal tibial epiphysis by 1 year of age. The long lateral and deeper short CLs originate on the lateral malleolus of the tibia, just plantar to the groove for the tendon of the lateral digital extensor muscle. Only a small portion of the lateral malleolus is intraarticular; therefore most fracture fragments are located within the joint capsule and CLs. The lateral malleolus is mostly covered by soft tissue attachments; therefore careful dissection and the use of a motorized synovial resector are necessary for successful removal of fracture fragments using arthroscopic techniques.
Lateral malleolar fractures are usually traumatic in origin. Small, well-rounded fragments, probably a manifestation of osteochondrosis, occur occasionally and should be differentiated because horses are often asymptomatic. Clinical and radiological signs and results of surgical removal of the fragments have been reported in 16 horses.76 All were TBs with injuries incurred either during a fall in a race over fences or from being kicked. All horses had a moderate degree of lameness and tarsocrural effusion. Approximately 50% of the horses had periarticular swelling, thickening of the CL, and pain on digital palpation of the lateral malleolus. All fractures were visible on a dorsoplantar radiographic image (Figure 44-9). Fourteen fractures were unilateral and two bilateral, with nine simple and nine comminuted. Thirteen of 16 fragments were displaced distally and rotated 90 degrees.

Fig. 44-9 Dorsoplantar radiographic image of a tarsus. There is a fracture of the lateral malleolus (arrow).
Ultrasonographic evaluation is useful to determine the location of the fracture in a dorsoplantar plane and to identify a concurrent collateral desmitis.22 Horses with small or minimally displaced fractures have been successfully managed conservatively. Surgical removal may result in a quicker recovery. The tarsocrural joint should be inspected arthroscopically to remove any debris, and surgical removal of most fragments is possible; use of a motorized synovial resector facilitates debridement of the joint capsule and CL attachments to the fracture fragment. In some horses the fragment can be easily removed via an incision through the lateral CL of the tarsocrural joint, depending on fragment orientation. Thirteen of 16 horses treated by fragment removal returned to full athletic function.76 If the fracture fragment is of adequate size or if there is instability of the tarsocrural joint, lag-screw fixation and tension band wiring should be considered. One of us (MWR) examined a horse with lateral and medial malleolar fractures; repaired the larger, comminuted, displaced lateral malleolar fracture using a single 4.5-mm cortex bone screw placed in lag fashion augmented by a figure-eight tension band wire; and repaired the nondisplaced medial fracture using interfragmentary compression.64 The repair was performed using conventional surgical techniques, and small fragments originating from the lateral malleolus were removed. With conservative or surgical management the prognosis is good.
Fractures of the Medial Malleolus of the Tibia
Fractures of the medial malleolus of the distal tibia are rare. Similar to fractures of the lateral malleolus (see earlier), occasionally, small rounded fragments are displaced distal to the medial malleolus, intercalated in the medial CL. These fragments may be a manifestation of osteochondrosis and are distinct from the more common OCD fragments originating from the cranial, articular component of the medial malleolus (usually axially), in the tarsocrural joint. Alternatively, these rounded fragments may be the result of an old fracture. Authentic fracture of the medial malleolus occurs rarely alone, or in combination with lateral malleolar fractures (see earlier).64,77,78
Tarsal Joint Luxation
Complete luxation or subluxation of the tarsocrural, talocalcaneal-centroquartal (proximal intertarsal), and tarsometatarsal joints may occur, with or without concurrent tarsal bone fractures.79,80 Tarsal luxations are the result of severe trauma from kicks from other horses or limb entrapment in fixed objects, such as a fence or cattle guards. Proximal intertarsal and tarsometatarsal luxations are most common. Luxation causes severe, non–weight-bearing lameness, and there may be abnormal deviation of the limb at the tarsus. Crepitus may be present with a fracture, and palpation reveals tarsal joint instability. Diagnosis is confirmed by radiological examination. Dorsoplantar radiographic images obtained with medial or lateral limb traction are recommended to determine the extent of CL damage (Figures 44-10, 44-11, and 44-12). Treatment consists of reduction of the luxation with the horse under general anesthesia and stabilization with the application of a full hindlimb cast extending from the foot to a point level with the tibial tuberosity. Alternatively, external coaptation consisting of a Robert Jones bandage with splints (custom-made) or external cast material (cast, bandage) can be applied to a standing, sedated horse. Although reduction will be less than ideal and invariably an angular deformity will persist, a successful outcome can be achieved.64 Internal fixation is rarely indicated but may be necessary with concurrent tarsal bone fracture. Double plating techniques using conventional or locking compression plates applied proximal to the fracture or luxation using the plantarolateral aspect of the calcaneus and the medial aspect of the hock and ending distally in the metatarsal bones, in combination with external coaptation, could be used. Tarsocrural or tarsal luxation with functionally intact CLs can be difficult to reduce, but manipulation of the tarsus with the limb in a flexed position may facilitate reduction. The limb should be maintained in a cast or other external coaptation constructed to be as rigid as possible for 4 to 6 weeks if the CLs are intact and 6 to 8 weeks if the CLs are ruptured.79,80 After the cast has been removed, the hindlimb is placed in a heavy cotton bandage with rigid splints for an additional 4 to 6 weeks before turnout in a small area is allowed. Of the seven reported horses with tarsal joint luxation (three proximal intertarsal, three tarsometatarsal, and one tarsocrural), all were treated with closed reduction and external coaptation, and all returned to either light riding, pasture soundness, or breeding activity. The presence of tarsal bone fractures did not affect outcome. All horses had a reduction in range of motion of the tarsus and OA that prevented the return to athletic soundness. Prognosis for horses with proximal intertarsal and tarsometatarsal joint luxations is reasonably good for pasture soundness.79 A guarded prognosis is warranted for horses with tarsocrural joint luxation because of the difficulty in reducing the luxation.

Fig. 44-10 Flexed lateromedial image of a hock. There is widening of the plantar aspect of the talocalcaneal-centroquartal joint (arrows), which is indicative of luxation.
Soft Tissue Injury of the Tarsus
Various soft tissue injuries of the tarsus are discussed elsewhere: calcanean bursitis (see Chapter 79), cunean tendon bursitis-tarsitis (see Chapter 108), curb (see Chapter 78), subcutaneous calcaneal bursitis (capped hock; see Chapter 79), distention of the tarsal sheath (thoroughpin; see Chapter 76), and dislocation/luxation of the superficial flexor tendon from the tuber calcanei (see Chapter 80). Distention of the long digital extensor tendon sheath is discussed previously (see page 509).
Collateral Ligament Damage
Complete extension of the tarsocrural joint is prevented by tension in the CLs. CL injury is usually the result of trauma or a fall; however, it is not a common injury. CL injury was identified in only 23% of 133 horses that underwent ultrasonographic evaluation of the tarsus because of suspected soft tissue injury.22 Lameness varies from mild to severe, depending on the degree of damage. There is often distention of the tarsocrural joint capsule and periarticular soft tissue swelling. Flexion is usually resented. Analgesic techniques are usually not required, but lameness may be improved in some horses by intraarticular analgesia of the tarsocrural joint. In an acute injury there often are no radiological abnormalities unless there is an avulsion fracture81; however, 4 to 6 weeks after injury, enthesophytes develop at the origin or insertions of the injured CLs. Nuclear scintigraphy is helpful in horses with mild injuries because it demonstrates intense, focal IRU at the ligament attachment sites.82 Ultrasonographic evaluation is used to identify the injured structure(s) and assess the severity of the injury (see Chapter 17).22 In a series of 23 horses, 18 sustained medial CL injury, including three with both medial and lateral CL injury, and five horses had lateral CL injury alone, with injury to the superficial components being most common either alone or together with injury to the deep component. Initial treatment involves stall rest, cold water therapy, topical dimethyl sulfoxide with or without corticosteroids, and NSAIDs. Long periods of rest (e.g., 6 months) followed by a controlled exercise program have been recommended.81 Prognosis depends on the severity of injury, but horses with very extensive periosteal new bone have been able to return to full athletic function, although some residual enlargement of the hock has persisted.21,64
Old avulsion fractures at the insertion of the lateral and less commonly the medial short CL are sometimes detected in horses with pain causing lameness localized to the hock with no other explanation for the cause of lameness. There is no associated IRU, and the clinical significance of such fractures is difficult to determine accurately. It is conceivable that low grade motion may cause pain.
Enthesopathy of the Lateral Collateral Ligaments of the Tarsocrural Joint
Enthesopathy of the long, and less commonly, the short lateral CLs is a rare condition that is recognized most often in STB racehorses, especially pacers, but does rarely occur in TBs. It results in lameness that is improved by analgesia of the tarsocrural joint. There may be distention of the tarsocrural joint capsule, and subtle, localized soft tissue swelling may be present. Diagnosis usually depends on scintigraphic findings83 with focal, intense IRU on the lateral aspect of the calcaneus. Entheseous new bone is usually detectable radiologically. Local injections with methylprednisolone acetate and Sarapin, an extract of the pitcher plant, may result in improvement, but rest is the treatment of choice.
Rupture of the Fibularis Tertius
See Chapter 80 for a discussion of rupture of the fibularis (peroneus) tertius.
Miscellaneous Tarsal Injuries
Osseous Cystlike Lesions in the Tuber Calcanei
Osseous cystlike lesions in the tuber calcanei have been identified as a cause of moderate to severe lameness either with no localizing clinical signs (Figure 44-13)64 or in association with distention of the calcaneal bursa.83 It has been suggested that such lesions may be a reaction at the enthesis of the gastrocnemius tendon, but no associated lesions of the gastrocnemius tendon have been seen.84 In two horses lameness developed after known trauma (a kick and a fall),84 but in other horses there was no known potential cause. In the latter horses lameness was abolished by fibular and tibial nerve blocks. Lateromedial, dorsolateral-plantaromedial oblique and skyline images of the calcaneus are required for accurate localization of the lesion. Treatment of two horses with associated distention of the calcaneal bursa by either conservative management or surgical debridement resulted in persistent lameness.84 The horses with no associated soft tissue swelling did not respond to rest, but intralesional injection of corticosteroids has resulted in resolution of lameness in two horses.64 Calcaneal bursitis is rarely caused by primary injury of the gastrocnemius tendon at the attachment to the calcaneus or a combined injury of the gastrocnemius and superficial digital flexor tendons (see Chapters 79 and 80).

Fig. 44-13 Flexed plantaroproximal-plantarodistal radiographic view of the calcaneus. There is a well-defined focal osteolytic lesion in the plantarolateral aspect of the tuber calcanei (arrow). Compare with Figure 44-14. There were no localizing clinical signs.
Infectious (Septic) Osteitis of the Calcaneus
Osteitis of the tarsal bones is uncommon. However, the enlarged end of the tuber calcanei has minimal soft tissue protection and is at risk for traumatic injury and subsequent infection. Management of these injuries can be complicated if the tarsocrural joint, calcaneal bursa, or tarsal sheath is involved. Most horses sustain a traumatic injury from kicking a fixed object or being kicked by another horse.85,86 Osteitis usually causes moderate-to-severe lameness, cellulitis, and tarsal tenosynovitis. The severity of lameness often decreases once drainage has been established. Twenty-two of 28 horses had a wound or draining tract over the plantar aspect of the calcaneus.85 Lateromedial, flexed lateromedial, and plantaroproximal-plantarodistal (skyline) radiographic images are the most helpful (Figure 44-14). Radiological signs of calcaneal osteitis or sequestra formation may take several days or weeks to appear, and thus sequential radiological evaluation is recommended. Rarely is the medullary cavity of the calcaneus involved; hence the term osteitis rather than osteomyelitis is preferred. Ultrasonography is useful to assess calcanean bursa or tarsal sheath involvement. If tarsal sheath involvement is suspected, cytological evaluation of the tendon sheath fluid with aerobic and anaerobic microbial culture and susceptibility testing is recommended (see Chapter 76). Treatment is based on resolving the infection and debriding any bony lesions. Debridement can often be done using bursoscopic techniques, but if wound revision is needed a conventional surgical approach to the infected bone can be used. One of us (MWR) has had success in managing horses with infectious calcaneal bursitis and calcaneal osteitis, using liberal debridement and primary wound revision and closure, closed suction drainage, and external coaptation using a full-limb or sleeve cast or bandage to immobilize the tarsus after surgery. External coaptation appears important in overall management because limiting motion improves the horse’s comfort and allows early healing of revised wounds in this region. Although debridement of all infected bone and soft tissue is an important principle in management of horses with infectious osteitis of the calcaneus, aggressive debridement of the calcaneus to remove large amounts of bone should be avoided. Broad-spectrum antimicrobial drugs such as penicillin (22,000 IU/kg q12h IM) and gentamicin sulfate (6.6 mg/kg q24h IV) are recommended until culture results are known. Pure bacterial cultures were isolated in 14 of 28 horses in one report,85 but mixed bacterial isolates do occur. The most common pure bacteria colonies isolated were Escherichia coli, Streptococcus zooepidemicus, Staphylococcus aureus, and Enterobacter cloacae. All isolates were susceptible to penicillin, gentamicin, or trimethoprim sulfamethoxazole. With acute infection, antimicrobial medication alone may be satisfactory, but surgical intervention to remove infected soft tissue and damaged bone or sequestra is usually required. Resection of the infected soft tissues and curettage of the bony lesion can resolve calcaneal lesions that do not involve the tarsal sheath. Infections involving the tarsal sheath require flushing the sheath and establishing drainage (see Chapters 24 and 76). Duration of antimicrobial therapy depends on clinical response, but therapy should continue for at least 7 days after resolution of the lameness and wound drainage. Phenylbutazone (2.2 mg/kg orally [PO]) should be used as needed for pain relief.
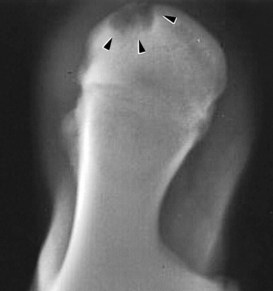
Fig. 44-14 Flexed plantaroproximal-plantarodistal radiographic view of the calcaneus. There is an osteolytic lesion in the tuber calcanei (arrows), the result of infection. There is also new bone on the lateral aspect (to the left) of the calcaneus.
The prognosis for horses with calcaneal osteitis depends on the structures involved, duration of infection before treatment, type and susceptibility of isolated bacteria, and the ability to get the original wound to heal. Long-term management (several weeks to months) is often needed, and an important but often limiting factor is the owner’s financial commitment. Chronic persistent drainage, persistent severe lameness, or contralateral laminitis can negatively influence prognosis, and aggressive, expensive therapy is often needed. Quick and aggressive medical and surgical treatment improves the chances of horses returning to athletic function. In one study, nine of 18 horses were used as broodmares and nine returned to athletic function.85,86
Osteitis of the Sustentaculum Tali
The sustentaculum tali is on the plantaromedial aspect of the calcaneus. Injuries involving the medial aspect of the hock often involve the sustentaculum tali and adjacent tarsal sheath. Injury usually occurs from direct trauma, most commonly from a kick wound. Lameness is often severe. Diagnosis can be difficult because of the severe soft tissue swelling that accompanies this injury, especially when acute. Although unusual, there can be communication of the site of infection or fragmentation of the sustentaculum tali with the tarsocrural joint. Radiographic examination should include dorsomedial-plantarolateral oblique, dorsoplantar, and plantaroproximal-plantarodistal images. Ultrasonography is useful to assess the deep digital flexor tendon (DDFT) and tarsal sheath. Infection of the tarsal sheath as a result of sustentaculum tali fragmentation (see Figure 76-3) or lysis requires surgical curettage of the sustentaculum tali and lavage and flushing of the tarsal sheath. Horses with bony irregularities in the tarsal groove of the sustentaculum tali can be severely lame, even without infection, because of motion of the DDFT against the roughened bone, which results in severe tendonitis. The tarsal retinaculum can become constrictive if the tendon is inflamed and swollen, which causes further tendon damage and pain. Surgery with the horse under general anesthesia is recommended to transect the tarsal retinaculum, explore and curette necrotic bone involving the sustentaculum tali, and drain and flush the tarsal sheath.87 The tarsal groove should be smoothed with a curette to avoid abrasion to the DDFT after surgery. Endoscopic examination of the tarsal sheath may be difficult in horses with severe swelling from concomitant infection. In horses with mild swelling, with drainage localized to the region of the sustentaculum tali, and without substantial tarsal tenosynovitis, a small incision should be made directly over the fragments. The fragments should be removed and the site curetted; the incision is closed primarily. In these horses, prognosis for future soundness is favorable. Horses should be treated with systemic antibiotics based on culture and susceptibility results. Antimicrobial therapy is continued for at least 7 days after resolution of clinical signs and may require 4 to 6 weeks of treatment. After surgery, horses should be confined to a stall or small run for 8 weeks with daily handwalking, followed by 6 more weeks of pasture turnout before returning to normal activity. Prognosis is good for returning to athletic activity. Seven of nine horses returned to previous use (three barrel racing, one cutting, and three pleasure riding) after surgery.87
Lesions of the Sustentaculum Tali
Lesions of the sustentaculum tali of the fibular tarsal bone may occur as a result of known direct trauma, such as a kick injury to the medial aspect of the hock,88 or in association with chronic injuries of the DDFT. Eight of eight horses with proliferative new bone on the plantar and/or medial aspect of the sustentaculum tali had marked distention of the tarsal sheath and lameness. Four had a history of a kick injury. Conservative or surgical management resulted in persistent lameness. Postmortem examination revealed marked fibrillation of the DDFT and adhesions to the tarsal sheath and/or the sustentaculum tali.
Chronic lesions of the DDFT may be associated with the development of dystrophic mineralization within the tarsal sheath and osseous irregularity of the sustentaculum tali. Distention of the tarsal sheath and lameness are present. The prognosis is poor.
Congenital Deformations of the Tarsus
Congenital dysplasia of the sustentaculum tali is rare and has been documented in TBs89 and Saddlebreds characterized clinically by a tarsal valgus conformation and a broader plantar profile than usual. The DDFT is positioned more dorsally and medially than usual because of flattening of the proximal aspect of the sustentaculum tali.
A complete fibula may be present in Shetland ponies.90,91 This results in an abnormal swelling on the distal lateral aspect of the tibia and outward splaying of the limbs distal to the hocks.
Periarticular Cellulitis (see also Chapter 107)
Peritarsal infection results in acute-onset, very severe non–weight-bearing lameness associated with localized swelling that is usually but not invariably on the dorsal aspects of the hock. The swelling is hot and exquisitely painful to palpation. These signs are associated with an elevated rectal temperature, neutrophilia, and hyperfibrinogenemia. In some horses, skin abrasions can be identified somewhere in the more distal part of the limb.
Prompt, aggressive treatment with oxytetracycline (5 mg/kg IV sid) or other antimicrobial agents and phenylbutazone (4.4 mg/kg) for at least 5 days, combined with forced walking exercise for as much as possible daily, usually results in rapid resolution of lameness. Horses can often start trotting within 3 days of the onset of clinical signs and should be trotted for 10- to 15-minute periods repeatedly through the day. The prognosis is usually favorable; 1 of 10 horses developed osteomyelitis of the third tarsal and fourth tarsal bones, although this horse ultimately made a complete recovery.92



