Chapter 42The Metatarsophalangeal Joint
Lameness of the metatarsophalangeal (MTP) joint is similar to that of the metacarpophalangeal joint, but historically it has largely been ignored and was mentioned only twice in a leading lameness textbook.1 With fastidious use of both intraarticular and perineural analgesia, the MTP joint is now known to contribute substantially to hindlimb lameness.2
Anatomy
The MTP joint is nearly identical to the metacarpophalangeal joint and is composed of the distal articular surface of the third metatarsal bone (MtIII), its sagittal ridge, and the medial and lateral condyles; the medial and lateral proximal sesamoid bones (PSBs); and the proximal articular surface of the proximal phalanx, which has a prominent axially located sagittal groove (see Chapter 36). Minor differences exist in the shape and length of the proximal phalanx between the forelimbs and hindlimbs but are not clinically relevant. The MTP joint normally is more upright than the metacarpophalangeal joint and can achieve a greater degree of flexion. The lateral-to-medial width of the lateral condyle of the MtIII is less than that of the medial condyle. In racehorses, based on the results of scintigraphic examination, stress-related bone injury occurs predominantly in the lateral aspect of the hindlimb, which may be related to the smaller surface area of the lateral condyle. The joint capsule, intersesamoidean and collateral sesamoidean ligaments, suspensory ligament (SL) attachments, and digital flexor tendons all function to move and support the MTP joint. The dense collateral ligaments have short deep, and long superficial components. In the hindlimb the lateral digital extensor tendon joins with the long digital extensor tendon in the proximal dorsal metatarsal region. Therefore only the long digital extensor tendon is encountered during arthrocentesis or surgical procedures performed in the dorsal aspect of the MTP joint.
Conformation
Fetlock valgus and varus deformities affect the MTP joint in foals, but fetlock varus deformity is of most concern and needs to be corrected early (see Chapter 58). Most normal horses are slightly toed out in the hindlimbs, but in some horses toed-out conformation may play a role in uneven load distribution and affect hindlimb gait. Horses with toed-out conformation tend to travel close behind and stab laterally during limb advancement, a gait that may cause excessive lateral shoe wear and hoof imbalance. Such gait and hoof imbalance may predispose the lateral aspect of the MTP joint to stress-related bone injury. Horses that are excessively straight behind have an abnormal degree of extension (or dorsiflexion) of the MTP joint. This conformation is undesirable because it places abnormal load on the SL and predisposes to suspensory desmitis, stifle joint lameness, and secondary osteoarthritis (OA) of the MTP joint. Horses with bull-nose foot conformation and long, weak hind pasterns may be predisposed to injury (see Chapter 4, Figure 4-34). When viewed from behind when walking and trotting, some horses—especially those with a base-narrow conformation—appear to collapse laterally over each hind fetlock.
Clinical Characteristics and Diagnosis of Metatarsophalangeal Joint Lameness
Lameness of the MTP joint occurs in most sports horses and is common in the racehorse. Both Standardbred (STB) and Thoroughbred (TB) racehorses are prone to injury of this joint, but MTP joint lameness is more common in the STB, because gait and load distribution predispose to hindlimb lameness in this breed (see Chapter 2). Lameness of the MTP joint should never be discounted in the TB racehorse, and in both the STB and TB racehorse in my referral practice, conditions of this joint are the most common cause of undiagnosed hindlimb lameness. Curiously, MTP joint lameness is apparently uncommon in Western performance horses despite the predominant use of the hindlimbs for many maneuvers and thus tremendous forces applied to the MTP joint (see Chapter 120). With Western performance horses, sporting activity may play a role because in barrel horses and team roping heading horses, lameness of the distal aspect of the hindlimb including the MTP joint was uncommon, but in team roping heeling horses, the MTP joint contributed substantially to lameness and poor performance.3,4 There is no pathognomonic historical information that incriminates the MTP joint more than other sources of hindlimb lameness, but racehorses are usually worse in turns. Absence of palpable abnormalities and clinical signs incriminating other areas of pain in the hindlimb, particularly in a racehorse, would make me consider the MTP joint region, because it is the most commonly overlooked area in my practice. In horses with bilateral MTP joint lameness, poor performance may be the only historical finding and overt signs of lameness may not be present, but a short, choppy gait or intermittent, shifting hindlimb lameness is seen. A gait typical of bilateral stress-related bone injury of the distal aspect of the MtIII in TB racehorses being trotted in hand is described as an “exaggerated pelvic excursion” in a dorsoventral direction (see Chapter 107).
Clinical signs of MTP joint lameness vary from subtle to overt and depend on the nature and severity of injury. Signs of inflammation may be absent in horses with stress-related bone injury but severe in horses with displaced or comminuted fractures. At the trot limb flight is similar to lameness originating from the metatarsal region and hock. As the limb moves forward, it deviates medially and is then stabbed laterally at the end of the cranial phase of the stride. The cranial phase is shortened commensurately with the degree of pain. Lameness is more pronounced with the affected limb on the inside of a circle. I find it useful to characterize clinical signs into three categories: severe, unrelenting lameness; intermittent, severe lameness; and chronic, low-grade lameness. TB racehorses often have bilateral MTP joint pain and show poor hindlimb action and a tendency to bunny-hop behind in canter.
Severe, Unrelenting Lameness
The severe, unrelenting form of MTP joint lameness is associated with intraarticular fractures or severe, end-stage OA. Horses are obviously lame at the walk, cannot be trotted, and may be non–weight bearing. Deformity of the MTP joint may be obvious, as in horses with comminuted fractures of the proximal phalanx. Effusion is obvious and diffuse; periarticular soft tissue swelling may be present. Horses with acute, displaced condylar fractures of the MtIII may have acute, progressive edema of the diaphyseal region, and those with comminuted fractures of the proximal phalanx often have severe soft tissue swelling. Palpation and flexion elicit severe pain and, in horses with comminuted or displaced fractures, crepitus. Radiographs are usually diagnostic. This category includes severe, complete, or comminuted fractures (e.g., spiral fractures of the MtIII); comminuted or complete fractures of the proximal phalanx; midbody fractures of the PSBs; complex fractures involving the MtIII, the proximal phalanx, and the PSBs; luxation or subluxation; and end-stage OA. Horses with acute tendonitis of the deep digital flexor tendon (DDFT) with tenosynovitis can be severely lame, and intrathecal analgesia of the digital flexor tendon sheath (DFTS) may only partially remove pain. Ultrasonographic examination is required. However, some sports horses with DDFT lesions show lameness that is challenging to diagnose because of its sporadic nature.
Intermittent, Severe Lameness
Horses with intermittent, severe lameness of the MTP joint may be able to train and perform at some level but develop severe lameness afterward. When exhibiting clinical signs, horses are lame at the walk, even toe-touching lame, and are obviously lame at the trot (grade 3 or 4 of 5), but after resting and receiving nonsteroidal antiinflammatory drugs (NSAIDs), horses are often able to gallop, jog, or train within 1 to 5 days. In some instances horses may be able to race, only to become lame once again. When walking in hand, horses often show marked lameness while turning, even if they are sound while walking in a straight line. Obvious signs of inflammation usually are not present, but horses generally respond positively to the lower limb flexion test and may show a painful response to deep palpation. Horses with incomplete midsagittal or dorsal (frontal) fractures of the proximal phalanx often manifest a painful response when firm digital pressure is placed on the proximal, dorsal aspect (see Figure 6-37). Effusion may be present, but it is often absent or minimal even in horses with incomplete fractures. Because clinical signs may be difficult to detect, diagnostic analgesia is often necessary. Radiographs are usually diagnostic, but if findings are equivocal or the radiographs are obtained before radiological changes develop, scintigraphic examination or follow-up radiographic examination in 10 to 14 days is required. Digital and computed radiography can be helpful. Conditions such as incomplete fractures of the MtIII, the proximal phalanx, and the PSBs and moderate OA are in this category.
Chronic, Low-Grade Lameness
Diagnosis of chronic, low-grade MTP joint lameness is difficult. Specific signs that localize lameness to the MTP joint are lacking, and lameness may be only subtle to mild (grade 1 of 5) at the trot in hand. Horses examined at the track and carrying a rider may show only mild lameness. In racehorses, effusion and the response to lower limb flexion varies, but it can be negative. There is often mild increase in temperature, a subtle but useful sign of subchondral bone injury. In nonracehorses there may be effusion of the MTP joint and often the DFTS, but effusion is often long-standing and may be easily overlooked if reported by the handler as preexistent. Palpation may reveal mildly suspicious areas (e.g., pain over the abaxial aspect of the PSBs) in horses with sesamoiditis, but in most horses no abnormalities are noted. Concomitant lameness of the MTP joint and stifle region, called intralimb compensatory lameness, occurs most often in racehorses but is recognized in nonracehorses, and clinical signs may not abate until both sites are blocked or treated. The association between the stifle and MTP joint is difficult to explain. In young horses with “loose stifles,” knuckling of the MTP joint occurs when horses, particularly STBs, are jogged or worked slowly. Perhaps stretching of MTP joint capsule attachments or early subchondral bone trauma occurs during knuckling. Horses with “loose stifles” are thought to have patellar ligament and muscular instability and laxity and may benefit from counterirritant injection and simultaneous management of the MTP joint problem.
Diagnostic analgesia is required to localize pain causing lameness to the MTP joint, but in many horses lameness is difficult to accurately assess with the horse at a trot in hand. It is extremely important to recognize the need to employ perineural diagnostic analgesic techniques in addition to or in lieu of intraarticular analgesia in order to abolish all pain associated with the MTP joint. Radiological findings may be normal and horses are referred for scintigraphic examination, which often reveals stress-related bone injury. Special radiographic images may be needed to evaluate the distal aspect of the MtIII or for accurate identification of osteochondral fragments located in the dorsal and plantar aspects of the joint. In this category are conditions such as stress-related bone injury of the MtIII, early OA, osteochondral fragments that occur traumatically or as the result of osteochondrosis, and sesamoiditis.
Diagnostic Analgesia
Articular pain originating from the MTP joint can usually be abolished or at least partially alleviated by intraarticular analgesia. Because only one injection is required, intraarticular analgesia is easier and safer to perform than perineural techniques, but pain originating from subchondral bone may not abate or may be only partially alleviated by intraarticular analgesia. Therefore, it is extremely important to recognize that the low plantar perineural technique or a variation must be used, because it is more effective in alleviating pain from all sources (see Chapter 10).
A variation of the low plantar block, the lateral plantar metatarsal block, can be performed in horses with stress-related bone injury of the distal plantarolateral aspect of the MtIII (see Chapter 107).5 This block is particularly valuable in horses with bilateral lameness, because after one limb is blocked, the horse becomes obviously lame in the other. Other sources of pain located laterally in the MTP joint, such as sesamoiditis, small fractures of the PSBs, can be blocked by this technique, but the most common reason horses improve after lateral plantar metatarsal analgesia is alleviation of subchondral bone pain of the distal aspect of the MtIII.
In horses with chronic, low-grade lameness it may be necessary to perform analgesia and watch the horse train. Resolution of subtle signs, such as bearing in or out, not feeling right behind, performing dressage maneuvers, or, in STB racehorses, being on a shaft or a line, may be the only sign of a positive response to diagnostic analgesia. Although perineural analgesia may result in slight loss of proprioception, it is generally preferable, because intraarticular analgesia may result in a false-negative response. If pain is elicited by firm palpation of the dorsoproximal aspect of the proximal phalanx, suspect a midsagittal fracture. Nerve blocks are contraindicated because of the risk of creating a complete or comminuted fracture.
The clinician should be aware that it is possible to inadvertently block pain associated with subchondral bone of the MTP joint when performing plantar digital or plantar perineural analgesia. This occurs most frequently in racehorses with midsagittal fracture of the proximal phalanx but can occur in horses with OA or other conditions (see Chapters 10 and 41).
Imaging Considerations
Radiography and Radiology
Examination should include dorsoplantar (DPl), lateromedial (LM), dorsolateral-plantaromedial oblique (DL-PlMO), and dorsomedial-plantarolateral oblique (DM-PlLO) images. A flexed LM image is useful to evaluate the sagittal ridge for the presence of osteochondrosis lesions and to see dorsal frontal fractures of the proximal phalanx. Vacuum phenomenon can occur because the MTP joint can be placed in extreme flexion. Sudden decompression of the joint during stress flexion is believed to cause what appears to be an air artifact in the distal plantar aspect of the MtIII.6
Horizontal oblique images are useful to evaluate the proximal-dorsal aspect of the proximal phalanx for the presence of osteochondral fragments, but overlap between the base of the PSBs and the proximal aspect of the proximal phalanx can hide lesions associated with the distal-plantar aspect of the joint. Overlap in the plantar aspect of this joint is more common than in the metacarpophalangeal joint and occurs when the distal hindlimb is not vertically positioned. The x-ray beam should be angled down 15 to 20 degrees to separate the PSBs and proximal phalanx (Figure 42-1).
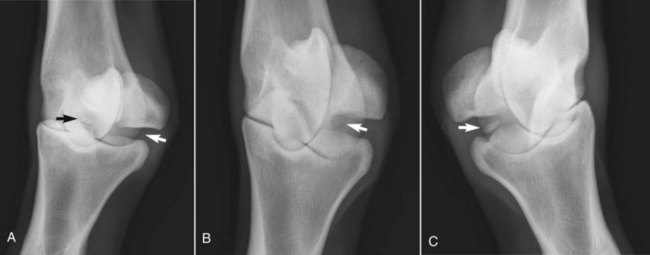
Fig. 42-1 A, Dorsal 45° lateral-plantaromedial oblique digital radiographic image of a 3-year-old Standardbred filly with maladaptive subchondral bone remodeling obtained using a horizontal x-ray beam. Often, there is overlap between the base of the proximal sesamoid bones (PSBs) and proximal aspect of the proximal phalanx (white arrow), but in this well-positioned view no overlap exists. A medial, plantar osteochondral fragment can be seen (black arrow). B, Dorsal 20° proximal, 45° lateral-plantarodistal medial oblique digital radiographic image of the same filly showing a large radiolucent lesion in the distal aspect of the lateral condyle of the third metatarsal bone (MtIII) that was not seen in a conventional oblique image (A). A proximodistal (down-angled) radiographic image opens up the space between the PSBs and the proximal phalanx. C, A similar down-angled oblique image of the plantaromedial aspect of the joint allows complete visibility of the plantar osteochondral fragment (arrow).
Using a horizontal x-ray beam in a DPl image, the PSBs are superimposed over the distal aspect of the MtIII and the MTP joint. To better evaluate these areas, dorsal 15° proximal-plantarodistal oblique (D15° Pr-PlDiO), flexed DPl, and standing 125-degree DPl images should be used. Proximolateral (medial)-distolateral (medial) and proximoplantar-distoplantar tangential images of the PSBs are occasionally used to evaluate the abaxial and plantar surfaces of the PSBs, respectively.
Approximately 5% to 10% of normal horses have a small unilateral or bilateral radiolucent notch (<1 mm in length) in the sagittal grove of the proximal phalanx that is seen in a DPl image and should not be confused with a midsagittal fracture. I have seen this “notch” most commonly in the DPl image of the STB racehorse. If clinical signs are consistent with midsagittal fracture, scintigraphic examination is recommended. Flattening of the plantar distal aspect of the MtIII condyles is not as common as in the metacarpophalangeal joint, but increased radiopacity of the plantar aspect of the MtIII can be seen in horses with stress-related bone injury and early OA if well-exposed LM and flexed LM images are obtained. I question the clinical significance of flattening of the condyles of the MtIII in most horses. Digital and computed radiographs are useful in the evaluation of horses with stress-related bone injury and incomplete fractures. Computed tomography (CT) and magnetic resonance imaging (MRI; see later) are also useful, but availability is limited.
Scintigraphic Examination
Scintigraphic examination is the best way to establish a diagnosis in many horses with intermittent, severe, or chronic low-grade lameness of the MTP joint. The most common scintigraphic findings in the MTP joint of STB and TB racehorses are focal areas of increased radiopharmaceutical uptake (IRU) that involve the distal plantarolateral aspect of the MtIII (see Figure 19-20, A; Figures 42-2 and 42-3).7 This IRU is a form of stress-related bone injury and early OA that is found in many racehorses with chronic, low-grade lameness, bilateral hindlimb lameness, and poor performance. Special radiographic images may then reveal increased radiopacity or radiolucent defects (see Figures 42-1 and 42-3). Similar scintigraphic findings are seen in horses with lateral condylar fractures of the MtIII. Focal areas of IRU are seen in horses with midsagittal or dorsal frontal fractures of the proximal phalanx (see Figure 19-20, C), sesamoiditis (Figure 42-4), and osteochondrosis of the plantar process of the proximal phalanx (see Figure 23-1; Figure 42-5). Often areas of IRU are found in unusual sites, such as those associated with the medial PSB (osteochondral fragments of the abaxial border and sesamoiditis), intersesamoidean ligament injury with radiolucent defects in one or both PSBs, incomplete fractures of the PSBs, and medial condylar fractures of the MtIII. Any focal area of IRU located medially in the MTP joint should be investigated, because incidental findings are unusual in this location.
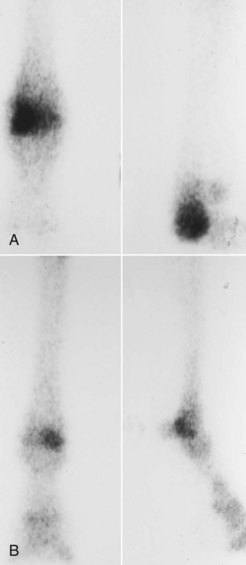
Fig. 42-2 A, Plantar (lateral to the left) and flexed lateral (on the right) left hindlimb and B, plantar (lateral to the right) and lateral (on the right) right hindlimb delayed (bone) phase scintigraphic images of the metatarsophalangeal (MTP) joint in two Standardbred racehorses. All images show focal increased radiopharmaceutical uptake of the distal, plantarolateral aspect of the third metatarsal bone, which is the most common scintigraphic finding in the MTP joint of racehorses.
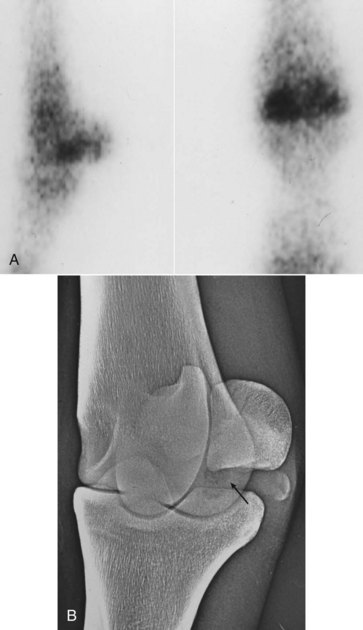
Fig. 42-3 A, Lateral (on the left) and plantar (lateral is to the left) bone phase scintigraphic images of a metatarsophalangeal joint. There is increased radiopharmaceutical uptake in the plantar aspect of the lateral condyle of the third metatarsal bone. B, Dorsolateral proximal-plantaromedial distal oblique xeroradiographic image showing a radiolucent defect (arrow) of the same area. This defect can easily be missed on routinely positioned images, but the increased radiopharmaceutical uptake seen in this area scintigraphically (A) prompted further investigation.
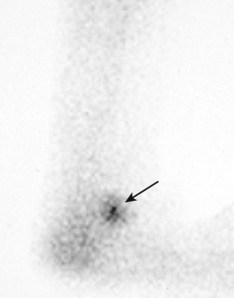
Fig. 42-4 Flexed lateral delayed (bone) phase scintigraphic image of a 2-year-old Standardbred racehorse with lateral sesamoiditis. There is focal moderate increased radiopharmaceutical uptake in the proximal sesamoid bones (arrow). When these findings were combined with those of the plantar image, the increased radiopharmaceutical uptake was localized to the lateral proximal sesamoid bone.

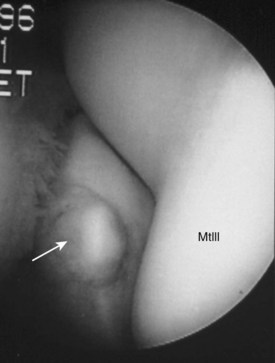
Fig. 42-5 A, Plantar (left, lateral is to the right) and flexed lateral delayed (bone) phase scintigraphic images of a 3-year-old Standardbred trotter. There is focal mild increased radiopharmaceutical uptake (IRU) involving the proximal aspect of the proximal phalanx (arrows), evidence of mild bone modeling associated with lateral and medial axial articular osteochondral fragments of the plantar process of the proximal phalanx. IRU of the lateral aspect of the distal phalanx in the hindlimb is a common incidental scintigraphic finding. B, Dorsal 20° proximal lateral-plantarodistal medial oblique digital radiographic image of the same horse showing the presence of lateral (white arrow) and medial (black arrow) articular osteochondral fragments. Osteochondrosis lesions occur in this region more commonly on the medial aspect of the proximal phalanx but can be biaxial. C, Intraoperative arthroscopic photograph (plantar is to the left and proximal is uppermost) showing the medial fragment interposed between the base of the medial proximal sesamoid bone (PSB) and the proximal phalanx. The medial condyle of the third metatarsal bone (MtIII) is immediately dorsal to the fragment. The arthroscope was positioned in the lateral plantar pouch, and separate instrument incisions were used to remove both the medial (shown) and lateral fragments.
Scintigraphic changes are usually less pronounced in nonracehorses, and negative or equivocal results often occur. The most common scintigraphic findings in jumpers and dressage horses with MTP joint lameness are diffuse mild areas of IRU in all bones or focal mild or moderate IRU in the dorsal or central aspects of the joint that involve the distal aspect of the MtIII and proximal aspect of the proximal phalanx and are associated with radiological evidence of marginal osteophytes and enthesophytes. There is a distinct difference in the scintigraphic and radiological appearance of the MTP joint of nonracehorses and racehorses, because in racehorses IRU is generally focal in nature and IRU and radiological changes involve the plantar aspect of the joint. In a 2004 study of clinically sound horses, generalized, even radiopharmaceutical uptake across the distal aspect of the MtIII and the proximal aspect of the proximal phalanx was found.8 Radiopharmaceutical uptake was significantly higher in the condyles of the MtIII of hindlimbs than in forelimbs, there was no effect of age, and there was a trend for region of interest ratios to be higher in the right hind MTP joint when compared with the left.8 In some nonracehorses arthroscopic examination has revealed full-thickness cartilage damage that primarily involves the distal dorsomedial aspect of the MtIII (medial condyle) and is consistent with OA. Focal IRU in the proximal aspect of the plantar pouch is seen in horses with severe OA (an ominous finding) (see Figure 19-20, B). I believe this finding is caused by accumulation of subchondral bone fragments in this location or modeling of the distal plantar aspect of the MtIII.
Magnetic Resonance Imaging
MRI is useful to evaluate bone and soft tissue abnormalities in the MTP joint and nearby structures (see Chapters 21, 107, and 108). In fact, in some horse-dense locations such as Newmarket, England, examination of the metacarpophalangeal and MTP joints using standing low-field MRI has become as commonplace as scintigraphic examination and is often preferentially requested by TB trainers.9 In TB and STB racehorses with maladaptive or nonadaptive bone remodeling of the distal aspect of the MtIII, MRI examination reveals extensive subchondral bone damage characterized predominately by low signal intensity of the plantar aspect of the lateral condyle of MtIII on T1- and T2-weighted images, a finding supporting the existence of chronic, sclerotic subchondral bone (Figure 42-6, A and B). Within the areas of low signal intensity is often a small area of high signal intensity near the articular cartilage (see Figure 42-6, A and B). In fat-suppressed short tau inversion recovery (STIR) image sequences, small, focal areas of high signal intensity within sclerotic bone are often found, indicating the presence of necrotic, and perhaps ischemic, bone, but widespread areas of high signal intensity consistent with bone edema from acute trauma are not often seen (Figure 42-6, C). Although numerous authors or speakers have characterized these lesions as bone bruises, bone edema (fluid accumulation) characteristic of bone bruises found in subchondral bone in people is not a hallmark of this common lesion in horses. Large areas of increased signal intensity likely indicated the presence of a fracture of the MtIII. Areas of increased signal intensity within sclerotic subchondral bone in horses with repetitive stress injuries could represent proteinaceous fluid, but likely represent regions of necrotic bone or granulation tissue.9 Areas of necrotic bone seen on magnetic resonance (MR) images correspond to radiolucent defects. Areas of bone loss, necrotic subchondral bone, or areas of intense resorption within sclerotic bone may warrant consideration when trying to manage horses with this lesion (see later). In horses with acute-onset clinical signs consistent with acute subchondral bone injury or fracture, bone edema can be more prominent. In 13 horses, most of which were nonracehorses, with lameness of metacarpophalangeal or MTP joints and without radiological abnormalities, the most common finding was decreased signal intensity in T1-weighted images, indicating the presence of sclerotic subchondral bone.10 In nine horses, decreased signal intensity in T-2*-weighted images was consistent with sclerosis, but five had increased signal intensity in fat-suppressed STIR images consistent with what was described as fluid accumulation within the sclerotic regions.10 Importantly, MRI abnormalities and subchondral bone lesions were found not only in racehorses but in horses used for show jumping and general purpose riding.10 Lesions similar to those described for racehorses were seen in the MTP joint of sports horses.11 Focal areas of IRU seen scintigraphically appeared in MR images as areas of low signal intensity on T1- and T2-weighted images with or without small areas of increased signal intensity in STIR images, indicating the presence of chronic, repetitive stress injuries of the distal aspect of the MtIII in sports horses in addition to acute, traumatic injuries.11 In an earlier study of 11 horses (eight racehorses), subchondral bone damage was identified using MRI, although there were no or equivocal radiological abnormalities.12 Four horses had lesions in the metacarpophalangeal or MTP joints. Horses with acute-onset lameness had subchondral bone injury characterized by increased signal intensity in STIR and T2-weighted images.12 In two horses, decreased signal intensity in proton density images (similar to T1-weighted images) indicated the presence of sclerotic subchondral bone of the distal aspect of the MtIII, but dense bone was surrounded by areas of increased signal intensity in STIR sequences.12 Only two horses had bone scintigraphy performed, and areas of IRU in the damaged subchondral bone were seen.12 Horses with acute subchondral bone injury should improve with rest, whereas those with chronic, sclerotic, and osteoarthritic subchondral bone may improve temporarily with rest but long-term prognosis is guarded. MRI was useful in the evaluation of horses with oblique and straight distal sesamoidean desmitis in 27 horses with lameness localized to the metacarpophalangeal or MTP joint region, of which 17 had lameness and injury in the hindlimb.13 Careful examination of soft tissue structures associated with the MTP joint, including use of diagnostic ultrasonographic examination, is necessary, because in some horses the results of diagnostic analgesia will be ineffective at differentiating authentic sources of pain in the region.
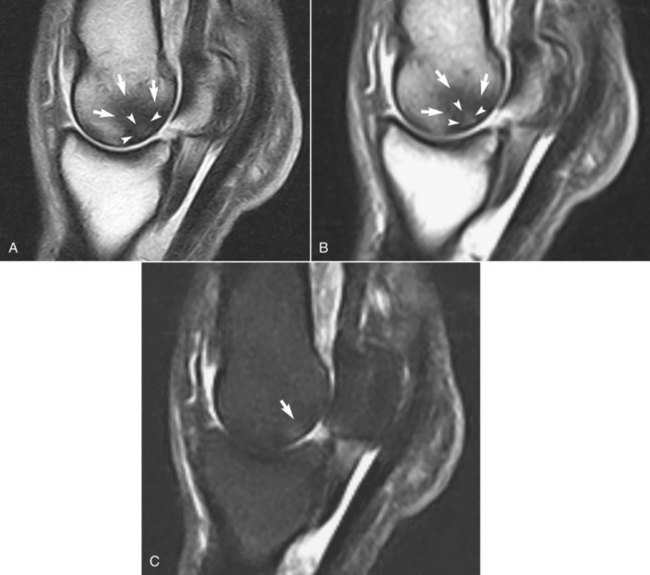
Fig. 42-6 Sagittal, low-field (0.25T) magnetic resonance images, obtained with the horse under general anesthesia, of a 4-year-old Thoroughbred racehorse with lameness localized to the lateral aspect of the right metatarsophalangeal joint by using lateral plantar metatarsal analgesia. A, T1-weighted image showing decreased signal intensity (arrows) surrounding an area of increased signal intensity (arrowheads). B, T2-weighted image showing the same signal distribution, indicating there is dense, sclerotic subchondral bone surrounding an area of necrotic, ischemic subchondral bone or fluid accumulation. C, Short tau inversion recovery (STIR) image showing increased signal intensity (arrow), confirming the presence of an area of necrotic subchondral bone within dense, sclerotic bone typical of a horse with stress-related subchondral bone damage.
Ultrasonographic Examination
Ultrasonographic examination of the MTP joint region is indicated for suspensory branch desmitis (see Chapter 72). The abaxial aspect of the PSBs should be examined carefully to identify tearing and small avulsion fractures. Proliferative synovitis (villonodular synovitis) is unusual in the MTP joint. The DDFT should be evaluated carefully if tenosynovitis of the DFTS is present14 (see Chapter 74). Ultrasonographic examination is useful in horses with intersesamoidean and collateral ligament injuries or those with wounds and draining tracts to look for foreign material or communication with the articular surface. The distal sesamoidean ligaments should also be examined carefully, because intraarticular analgesia of the MTP joint has the potential to resolve lameness associated with injury to these ligaments, which can be present with no localizing clinical signs.
Computed Tomography
CT (see Chapter 20) is useful to characterize complex fractures of the MTP joint, to aid in preoperative planning for surgical repair, and to study other defects of articular surfaces. CT has been found to be superior to radiology in detecting articular comminution, small cracks and lucencies in the MtIII condyles, and fractures of the PSBs.15 However, orthogonal radiography has been found to be superior to CT in detecting fractures of the dorsal aspect of the proximal phalanx, and both imaging modalities were poor at detecting plantar fractures of the proximal phalanx and coalescing cracks in the subchondral bone of the MtIII.15
CT is not as useful as scintigraphy and MRI in the evaluation of subchondral bone injury.
Arthroscopic Examination
Arthroscopic surgery is used frequently for removal of osteochondral fragments and fractures of the PSBs, assistance in fracture reduction and screw placement in horses with condylar fractures of the distal aspect of the MtIII and fractures of the proximal phalanx, and lavage and debridement in horses with infectious arthritis. Diagnostic arthroscopic examination is indicated if lameness is localized to the MTP joint but radiological findings are negative or suggestive of occult osteochondral fragments, but such examination should be undertaken after evaluating the results of advanced imaging such as scintigraphic imaging and MRI. Before I was able to routinely use scintigraphy I often elected to evaluate the articular surface of the MTP joint arthroscopically, only to be disappointed in my inability to substantiate obvious abnormalities. Using scintigraphy and more recently MRI, I can often characterize injury of the joint without the need for diagnostic arthroscopy. The most common diagnosis is subchondral bone injury without obvious overlying cartilage damage, findings that obviate the need to examine the joint arthroscopically. Diagnostic arthroscopy is indicated if cartilage damage or osteochondral fragments are suspected, and to confirm the extent of cartilage damage in horses with OA. Occult fragments involving the proximodorsal aspect of the proximal phalanx are occasionally found. Cartilage damage, sometimes full thickness, is found on the distal-dorsal aspect of the MtIII and the proximal aspect of the proximal phalanx in nonracehorses. In racehorses with OA, cartilage lesions are usually most pronounced in the plantar pouch, with extensive scoring or large areas of full-thickness damage and exposed subchondral bone on the PSBs. Although stress-related bone injury and later overlying cartilage damage is seen on the distal plantarolateral aspect of the MtIII, this area is difficult to evaluate during arthroscopic examination (Figure 42-7).
Specific Conditions of the Metatarsophalangeal joint
Stress-Related Subchondral Bone Injury and Osteoarthritis
The term OA implies disease of both the supporting bone and the articular surface of the MTP joint. The concept that the earliest lesion in OA of the MTP joint in racehorses begins in subchondral bone is essential to understanding clinical signs, successful use of diagnostic analgesia, progression of bone and cartilage loss, and the horse’s response (or lack thereof) to therapy. There are two syndromes of MTP joint OA; one is seen in racehorses and the other in nonracehorse sports horses.
In racehorses, OA begins as a maladaptive or nonadaptive stress-related bone injury in subchondral bone. Subchondral maladaptive or nonadaptive bone injury is the most common reason I examine TB and STB racehorses with hindlimb lameness or poor performance. Although the overlying cartilage may be biomechanically and biochemically inferior, obvious clinical signs such as synovitis and a positive response to lower limb flexion are not seen until later. Low-grade unilateral or bilateral lameness is present, which is localized best by low plantar or lateral plantar metatarsal analgesia. Often, horses have a short, choppy gait, mimicking what would be expected if horses had bilateral or, in some, quadrilateral foot pain. Most often, blocking one hindlimb produces obvious contralateral hindlimb lameness in horses with bilateral subchondral bone injury. Horses are often thought to have something “up high” and usually have been unsuccessfully treated for other suspected sources of hindlimb pain. Early stress-related bone injury is best substantiated using scintigraphic examination. Focal areas of IRU are present in the MtIII; the PSBs and the proximal aspect of the proximal phalanx also can be affected (see Figures 19-20, 42-2, and 42-3). Initial radiological findings either are negative or reveal subtle increased radiopacity, but later radiolucent defects develop in subchondral bone, which are best revealed in a DPrL-PlDiMO image (see Figure 42-3). Increased radiopacity is most obvious in the LM, flexed LM, and DPrL-PlDiMO images.
Later, overlying full-thickness cartilage damage develops (see Figures 19-20, B, 23-8, and 42-7; Figure 42-8). Stress-related bone injury can continue to the point where severe OA or fracture of the MtIII develops; this type of severe injury is most common in racehorses 4 to 6 years old (see Figures 19-20 and 23-8). However, in some STBs the process causes lameness when horses are 2- or early 3-year-olds and then subsides or stabilizes. The condition is rarely seen in STBs until training speeds faster than 2 minutes, 20 seconds for a mile are achieved. In TB racehorses, this remodeling process is common in later 2- and 3-year-olds but can also be seen in older horses. Older horses given time off because of undiagnosed lameness or other conditions are at risk to develop stress-related bone injury in the MTP joint 6 to 8 weeks after returning to training, when signs of poor gait or lameness develop and a focal area of IRU can be identified. In my experience, subchondral lucency occurs later in the TB than in the STB and is uncommon. Differences between the racing breeds related to gait, speed, and load distribution may account for this difference in progression of OA. End-stage OA develops in STB racehorses that have continued racing for many years and can be progressive in broodmares and breeding stallions.
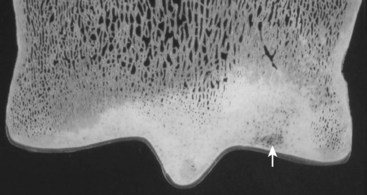
Fig. 42-8 Dorsal plane microradiograph (100 µm) of the distal aspect of the third metatarsal bone (lateral is to the right) showing dense subchondral sclerosis and an area of intense resorption or necrosis of bone (arrow). Cartilage overlying this area is intact. Severe subchondral modeling and remodeling and later osteoarthritis develop in the metatarsophalangeal joints of racehorses.
In nonracehorse sports horses OA is an insidious process usually without marked subchondral bone involvement. Bone and cartilage gradually deteriorate. Some horses affected may be ex-racehorses, but most are not. I have observed OA of the MTP joint mostly in upper-level jumpers and dressage horses. In these horses lameness is often chronic and low grade (grade 1 or 2 of 5), but it can progress to severe or intermittently severe. Effusion and a positive response to lower limb flexion are common findings. Concomitant tenosynovitis of the DFTS and previous lameness caused by suspensory desmitis and distal hock joint pain are common. Lameness is more consistently abolished using intraarticular analgesia in jumpers and dressage horses than in racehorses, but in some horses low plantar analgesia is required. Marginal osteophytes and enthesophytes are often detectable radiologically. Scintigraphy may reveal focal IRU in the central or dorsal aspect of the joint, diffuse IRU, or equivocal findings, and scintigraphic abnormalities are usually much less obvious than those found in racehorses. Occasionally, acute-onset lameness associated with focal IRU of the distal aspect of the MtIII occurs that is similar to that found in racehorses. This lameness may indicate acute subchondral overload trauma from landing wrong after jumping a fence, stepping on uneven ground, or sustaining a fall or other accident in a paddock. In nonracehorse sports horses, arthroscopic examination often reveals cartilage damage most extensive in the dorsal aspect of the joint, marginal osteophytes on the apices of the PSBs, and occasionally osteochondral fragments of the proximal dorsal aspect of the proximal phalanx.
Shoeing and hoof balance may play a role in development or expression of clinical signs of OA in all horses but may be more important in racehorses. In the STB racehorse clinical signs often develop within 2 to 3 weeks of a shoeing change, usually with the application of aluminum shoes with a low toe grab. Aluminum shoes are light and generally applied to pacers that are close to qualifying speed, but they are often used in trotters as well. Shear stress associated with these shoes may exacerbate existing disease or cause further trauma to subchondral bone. Aluminum shoeing is common in TB racehorses in North America, where these shoes are associated with other fetlock joint lameness and catastrophic breakdown. An aluminum shoe with a toe grab and with turned-down heels has been commonly used in recent years, and I have observed this shoe in many TBs with subchondral bone injury of the distal aspect of the MtIII, severe suspensory branch desmitis, and other catastrophic injuries of the MTP joint. Abnormal hoof wear caused by gait, the presence of concomitant distal hock joint or metatarsal region pain, or hoof imbalance may cause asymmetrical loading of the MTP joint and add to subchondral bone trauma.
Management of Stress-Related Bone Injury and Osteoarthritis
Reducing bone stress is key to initial management in racehorses with early OA characterized primarily by stress-related bone injury, because high-impact loading or high-strain cyclic fatigue of subchondral bone is the primary lesion. In STBs I previously recommended 4 to 6 weeks of light jogging (<2 miles per day), but results were poor even if recommendations were followed. I reassessed several horses after 6 weeks of light jogging, and although scintigraphic changes subsided, the horses were still as lame or slightly worse. I now recommend 3 weeks of walking and light jogging followed by reevaluation. Although 3 weeks’ reduction in training may allow early healing or remodeling of damaged subchondral bone and microfractures, bone and muscle undergo detraining and horses need several (i.e., 3 to 6) weeks of slow return to normal exercise intensity. If lameness resolves, horses are returned to training, but if lameness persists I recommend 3 to 4 months of rest. In TBs, recurrence is quite high if horses are given only 6 to 8 weeks of rest. I recommend either 3 to 4 months of turnout or a program of 3 weeks of handwalking, followed by 3 weeks of walking with a rider up, followed by 3 weeks of trotting either with a rider up or using an exercise pony. Longer periods of rest would likely be beneficial to allow complete healing of subchondral bone, but most often owners and trainers are reluctant to agree. A gradual return to normal exercise intensity is then recommended if horses are sound and moving well.
Hoof balance and shoeing characteristics should be evaluated and in most instances changed. A simple change in shoeing to an easier shoe, such as a flat steel or aluminum shoe, may reduce shear and torsion of the MTP joint. Toe grabs and any other shoe additives must be removed. Perhaps the best change, if possible, is to leave the horse barefoot for several weeks. If medial-to-lateral hoof imbalance is poor, it should be corrected. The relationship of track and training surface to the development of subchondral bone injury is currently unknown, but this type of injury is quite common in TB racehorses training and racing in Europe and other countries, in which grass and all-weather (synthetic) surfaces are used (see Chapter 107). Although incidence of race-day injuries may change from a change in track surface, it is the track surface on which the horse trains, and thus the surface that cancellous and cortical bone “sees” day to day, that likely influences bone modeling and remodeling. In an unpublished preliminary study, we found that areas of IRU of the distal aspect of the MtIII or the third metacarpal bone (McIII) were the most common scintigraphic abnormality in horses training on grass and a synthetic surface, and although MTP or metacarpophalangeal lameness was common, the prevalence of stress fractures of long bones was markedly reduced compared with a cohort of TB racehorses training on dirt.16 These results differ from anecdotal reports of injuries being discovered in TB racehorses being trained and raced on synthetic surfaces. Sporadic or clustering of injuries appears common, ranging from numerous horses developing unusual muscle injuries in the upper hindlimbs to an overabundance of stress fractures. Stress-related subchondral bone injury has been a predominant finding by some practitioners evaluating horses training on synthetic surfaces but not by all. In some racing jurisdictions, high toe grabs and turned-down shoes cannot be worn by horses racing on synthetic surfaces, a fact that may complicate epidemiological studies of injuries because this type of shoeing has been linked to substantial and sometimes fatal injuries of the metacarpophalangeal or MTP joints. In my opinion a change of shoeing philosophy to flat racing plates and, from the therapeutic standpoint, training horses without hind shoes may reduce negative forces acting on the MTP joint.
Because the initial lesion is in subchondral bone, intraarticular injections appear to have limited therapeutic benefit but may make theoretical sense. Active treatment may help in persuading trainers to follow the recommended work program. A series of three intraarticular injections of polysulfated glycosaminoglycans (PSGAGs) are given every other week. Alternatively, if horses are currently racing but have mild unilateral or bilateral lameness or scintigraphic evidence of stress-related bone injury and poor performance, I recommend intraarticular injection with hyaluronan and methylprednisolone acetate (80 mg). Intramuscular administration of PSGAGs (once weekly for 8 weeks) is recommended, but therapeutic benefit is difficult to assess. NSAIDs such as phenylbutazone (2.2 to 4.4 mg/kg bid) are recommended. NSAIDs may help horses in modified exercise programs “get over the hump” when lameness persists after scintigraphic evidence of stress-related bone injury subsides. Because pathogenesis involves sclerotic subchondral bone, the roles of ischemia and increased intraosseous pressure in causing bone pain or necrosis and subsequent collapse of weakened areas of subchondral bone have been questioned. I used to recommend the administration of isoxsuprine (400 mg bid orally) in an attempt to improve peripheral blood flow. However, research evidence supports neither the achievement of adequate blood levels nor increased blood flow by use of the drug, and I do not currently recommend its use. Other drugs, such as aspirin (17 mg/kg bid orally), may be useful in improving blood flow, but half-life is short and therapeutic benefit has yet to be established. If increased intraosseous pressure and early ischemia lead to pain and subchondral bone damage, a procedure such as subchondral bone drilling, which is used to manage stress-related bone injury in cortical bone of the McIII, may be beneficial, but it is currently only experimental. Topical counterirritation has historically been used and makes theoretical sense in horses with stress-related bone injury if increased blood flow occurs. The time-honored treatment of blistering and turning out may be the best method of management. I have used focused shock-wave therapy in some STB and TB racehorses with stress-related bone injury by aiming the shock waves at the plantarolateral aspect of the MtIII. Early results appear promising, but horses are given concurrent modified exercise programs and other therapy.
Bisphosphonate Therapy for Management of Subchondral Bone Pain
The bisphosphonate drug tiludronate has received considerable attention in recent years for management of numerous lameness problems, but although there are many anecdotal reports there is scant scientific evidence to support its use in the horse. Bisphosphonate drugs are largely antiresorptive and work by reducing osteoclastic activity. In maladaptive or nonadaptive bone remodeling and in horses with more advanced OA the predominant process is one of bone accumulation; dense sclerotic bone develops in the subchondral plate and adjacent cancellous bone, so in theory a drug to reduce osteoclastic resorption might have a net effect of increasing bone formation. How and why would antiresorptive drugs work in predominantly sclerotic subchondral bone? Bisphosphonate compounds may help to normalize metabolism in bone injuries characterized by abnormal resorption and formation, such as what is seen with navicular disease, a disease with similarities to maladaptive or nonadaptive remodeling of the MtIII and other bones. Based on this theory, in a double-blind, placebo-controlled study, there was improvement in lameness scores of horses with navicular disease given tiludronate at 1 mg/kg intravenously (IV) once daily for 10 days and horses returned to a normal level of activity 2 to 6 months after administration.17 Furthermore, horses with OA of the thoracolumbar vertebral column given the same dose of tiludronate showed significant improvement in dorsal flexibility compared with untreated controls.18 In horses, adaptive response to high-strain cyclic fatigue in the subchondral plate and adjacent subchondral bone occurs in response to race training. In a histological study of TB distal MtIII and McIII condyles, site-specific increases in microcrack density in calcified cartilage and resorption spaces in the adjacent subchondral plate were interpreted as evidence of mechanical failure of the joint surface from progressive endochondral ossification and modeling or remodeling of subchondral bone.19 Propagation of microcracks into subchondral bone may be critical to the subsequent development of condylar fractures or OA.19 In sclerotic subchondral bone, osteocyte morphology was abnormal and numbers were reduced, but site-specific microdamage, targeted remodeling of adjacent subchondral bone, and multiple pathways of mechanotransduction of the McIII were thought to be important in adaptation to exercise.20 In a study of 25 distal McIII condyles of TB racehorses, extensive microcrack formation leading to microfracture was found in sclerotic subchondral bone close to the calcified cartilage layer, and the presence of osteoclastic resorption along microfracture lines was proposed to have caused previous weakening.21 In these studies the presence of resorption and bone weakening in calcified cartilage and adjacent subchondral bone may lend evidence to justify the use of bisphosphonate compounds, primarily for reduction in resorption and potentiation of healing of microdamage. In people with OA of the knee, joint space narrowing and sclerosis of the nearby subchondral plate occurs, and sclerotic bone may act to stress-protect adjacent cancellous bone, called subarticular bone, because vertical and horizontal trabeculae number were reduced, resulting in bone loss.22 Through use of fractal signature analysis to measure differences of cancellous bone density in osteoarthritic medial knee compartments in people, increased trabecular number associated with thinning and fenestration of trabeculae in subarticular regions confirmed that overall, cancellous bone was osteoporotic.23 Osteoporosis, although not known to be found in horses with OA, could potentially be managed using bisphosphonate therapy. Bisphosphonate therapy alone24 and in combination with estrogen therapy25 slowed early changes in subchondral bone architecture and reduced the prevalence of osteoarthrosis-related subchondral bone lesions. Given the presence of intense resorption at various sites and the presence of osteoporotic subchondral bone, a case could be made for the administration of bisphosphonate drugs. Long-term studies and more double-blind, placebo-controlled studies17 need to be done.
Anecdotally, there may be benefit from use of tiludronate in horses with OA and subchondral bone injury, but it makes most sense to combine the drug with rest or a modification in exercise to allow healing of microdamage. Although lameness scores improved in horses with navicular disease,17 my limited experience in horses with subchondral bone pain of the distal aspect of the MtIII suggests that amelioration of lameness is subtle and that long-term evidence of benefit cannot be established. The drug can be used IV, at a dose of 1 mg/kg in a single infusion or divided over 10 days for a total dose of 1 mg/kg, because both dosage regimens resulted in similar plasma exposure and pharmacologic effects.26 There has been a trend to administer the drug to horses with single distal limb lesions using intravenous regional limb perfusion techniques, but this technique would be impractical in horses with numerous abnormalities involving more than a single limb and has not been studied. Use of the drug and continued training and racing may potentially lead to condylar fracture or other further injury, particularly in TB racehorses, a sequela that should be strongly considered. Anecdotal reports suggest that there may be immediate improvement in lameness scores after bisphosphonate administration, indicating that an analgesic effect may occur that could potentially lead to further training and racing. Currently I believe that targeting areas of bone resorption or necrosis and relative osteoporosis and attempting to normalize subchondral bone formation and healing using bisphosphonate therapy in combination with a reduction in exercise intensity comprise a reasonable approach, particularly in horses with bilateral hindlimb subchondral bone pain (or more numerous abnormalities). I prefer a single slow, IV infusion (1 mg/kg) while warning owners and trainers about the limited collective knowledge of complications in the horse, such as signs of colic during or immediately after drug administration, and of the known complication of osteonecrosis of the jaw associated with bisphosphonate use in people.27
Surgical Management of Subchondral Bone Injury
I have used the surgical technique of subchondral perforation (forage) in three horses—two TB and one STB racehorses—with unilateral hindlimb lameness in which lateral plantar metatarsal analgesia abolished lameness (horses did not show lameness in the contralateral hindlimb after blocking of the principal limb), and bone scintigraphy identified focal IRU of the distal, plantarolateral aspect of the MtIII. In one horse (Figure 42-9) MRI showed typical subchondral bone injury of the lateral MtIII condyle (see Figure 42-6). Arthroscopic examination of the plantar aspect of the MTP joint in all horses revealed normal-appearing articular cartilage, and by means of a combination of needles preplaced along the plantar aspect of the MtIII under arthroscopic guidance and intraoperative fluoroscopy, three 3.5-mm holes were drilled in a lateral-to-medial direction through the plantar aspect of the lateral MtIII condyle. Drill holes extended past the axis of the MtIII into but not through the medial condyle. Horses were given 4 months of rest before returning to training. The rationale for this approach is similar to what is done in horses with dorsal cortical fractures of the McIII, in which osteostixis is performed. Subchondral forage may allow marrow components from the medial condyle and adjacent lateral condyle to repopulate and heal damaged subchondral bone, and there may be immediate decompression of painful, sclerotic subchondral bone. All three horses raced after surgery, but in one TB lameness recurred after two race starts. An alternative surgical approach of inserting a positional or set cortex bone screw may make theoretical sense.
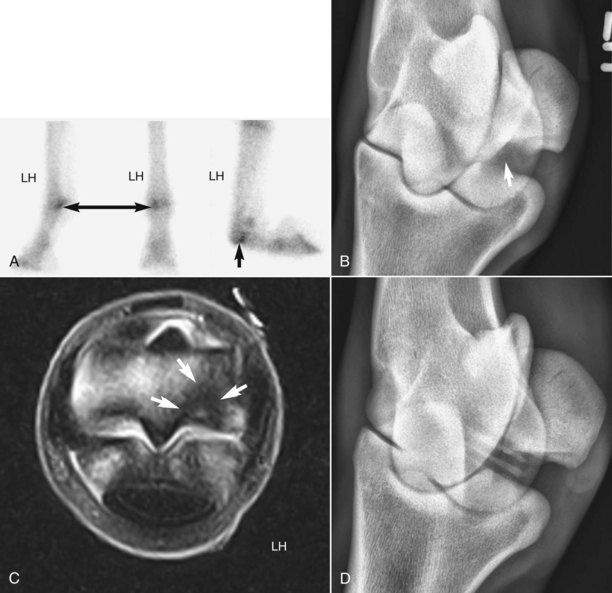
Fig. 42-9 A, Lateral (dorsal is to the left), plantar (lateral is to the left), and flexed lateral delayed-phase scintigraphic images of an unraced, 2-year-old pacing colt with left hindlimb lameness abolished with lateral plantar analgesia. Focal, moderate increased radiopharmaceutical uptake (IRU; arrows) of the distal, plantarolateral aspect of the third metatarsal bone (MtIII) is diagnostic for maladaptive or nonadaptive subchondral bone injury. B, Dorsal 20° proximal, 45° lateral-plantarodistal medial digital radiographic image showing a small radiolucent defect in the plantar aspect of the lateral condyle of the MtIII (arrow). C, T2-weighted magnetic resonance image of the left metatarsophalangeal joint (lateral is to the right; dorsal is uppermost) showing dense, sclerotic subchondral bone (arrows) surrounding an area of increased signal intensity in the region in which the radiolucent defect can be seen. An area of necrotic subchondral bone is present. D, Dorsal 20° proximal, 45° lateral-plantarodistal medial digital radiographic image obtained after three 3.5-mm holes were drilled from the lateral aspect of the lateral condyle through the damaged subchondral bone. This horse raced successfully as a 3-year-old.
In racehorses with more advanced OA the therapeutic value of intraarticular injections becomes greater, because overlying cartilage damage and synovitis become prominent. However, horses generally drop substantially in race class and eventually are retired. In TB racehorses, intraarticular injections have little benefit in horses in training but may have limited value in horses actively racing. The disease process appears to be self-limiting in TBs, because horses with continued chronic, low-grade lameness are often retired before the disease process advances, or horses develop compensatory lameness in the forelimbs. Although a putative relationship exits between horses with maladaptive or nonadaptive remodeling and the subsequent development of condylar fractures, this is difficult to substantiate. In three TB racehorses that subsequently developed condylar fractures, a previous bone scan showed IRU of the distal aspect of the McIII but radiographs were negative, lending some clinical evidence of a cause-and-effect relationship. I have seen numerous racehorses, most of which were STBs, that developed extensive OA of the MTP joint after earlier diagnosis with maladaptive or nonadaptive bone remodeling. It is possible that lameness from subchondral bone pain in numerous limbs may limit exertion, power, or race speed and cause poor performance, but not fracture. In essence, horses may not race fast enough to develop fractures. STB racehorses often go off stride or develop compensatory lameness problems, in the same limb or other limbs, that may lead to poor performance rather than fracture. In the TB racehorse subchondral radiolucency is unusual in my experience, but others have recognized progression of OA and the development of changes similar to those seen in STBs (see Chapter 108). Why some horses are able to race with persistence of IRU, radiolucency, and sclerosis whereas others cannot is not easy to answer. Prognosis for both racing breeds appears to be guarded to fair at best. Of 19 STBs with lameness and IRU of the plantarolateral aspect of the MtIII, 18 raced, but only 13 remained at the same racing class or improved.7 When radiolucent areas become prominent, arthroscopic examination and debridement may be an option, but it is difficult to manipulate instruments in the distal plantar pouch because manipulation must be done with the joint in flexion (see Figure 42-8). It is impossible to reach these lesions using a dorsal approach, because they are located approximately 8 mm plantar to the middle of the condyle. In horses with end-stage OA (i.e., loss of joint space, tilting of the sagittal ridge and groove, and severe proliferative and radiolucent changes), arthrodesis must be considered in broodmare or stallion prospects (see Figure 23-8). Humane destruction may be necessary.
Nonracehorses often respond favorably to intraarticular injections of PSGAGs, hyaluronan, and short-acting corticosteroids (e.g., triamcinolone acetonide, isoflupredone acetate) or long-acting corticosteroids (e.g., methylprednisolone acetate). Exercise level is reduced for a period of 2 to 3 weeks, and horses are given NSAIDs. Topical therapy using cold water hosing, poulticing, and bandaging is recommended. When lameness persists and scintigraphic examination reveals focal IRU in the dorsal aspect of the joint, or in horses with chronic lameness, long-term rest is necessary. Arthroscopic examination in these horses reveals areas of partial- or full-thickness cartilage damage that can be managed by debridement and microfracture into subchondral bone. However, the therapeutic value of arthroscopy is limited. If osteophytes are removed, they generally reform. If surgery is combined with rest, horses usually become sound, but lameness often returns when competition resumes. Prognosis for horses performing at the previous level of competition is guarded to poor. Rehabilitation of upper-level performance horses is quite difficult, because most have at least one compensatory lameness problem in addition to primary OA of the MTP joint. Horses may be able to perform at a lower level of competition.
Plantar Process Osteochondral Fragments
Fragmentation of the proximal plantar processes of the proximal phalanx is a common finding in young STBs and Warmbloods but is also seen in TBs, Arabians, and Western performance horses. This condition has become more frequently recognized since presale and postsale radiography has become common.
There are four distinct manifestations of decreasing frequency: axial articular fragments; abaxial, nonarticular fragments; nonarticular fragments originating from the base of the PSBs; and true acute fractures. (I prefer an anatomical description rather than reference to different types.28) The condition is much more common in the hindlimbs, except for nonarticular fragments from the base of the PSBs, which occur almost exclusively in forelimbs (see Chapter 36). Combinations of axial and abaxial fragments often occur. The condition can be unilateral or bilateral and can be biaxial (involving both sides of the same joint).
Axial Articular Fragments
Axial articular fragments are most important and are most often medial, but can be lateral, biaxial, and bilateral. Of 119 horses with axial articular fragments, 92% were STBs; 95% of fragments were in the hindlimbs, most commonly the medial aspect of the left hindlimb (44%).29 The incidence of axial articular fragments in 1- and 2-year-old STBs ranges from 5.6% to 28.8% but in TBs has been estimated at 2%.30 The etiology remains controversial, but because STBs and the hindlimbs are clearly predisposed and fragments are recognized at an early age, osteochondrosis is the most likely explanation. Heritability estimates of axial articular fragments in STBs using a nonlinear model were 0.21, and fragments were seen in 11.8% of foals.31 I feel it is implausible that a large number of STB foals develop traumatic fractures at this site, whereas other breeds do not. I believe hereditary factors are most important. A traumatic cause has been suggested in some studies, because portions of the fragments were irregular, were entrapped by mature fibrous tissue, and contained spicules of bone not covered by fibrocartilage, which gave the histological appearance of a fracture healed by fibrous union.30,32,33 Evidence of short distal sesamoidean ligament insertions was not found and fragments were old.30 Unfortunately, axial articular fragments examined were taken from horses with a mean age of 3.4 years and after horses had trained and raced, rather than from weanlings and yearlings, so degeneration and remodeling of fragments could have occurred. With only capsular attachments, how do alleged avulsion fractures occur? Etiology is most important when dispute or arbitration ensues after horses have been sold at public auction (see Chapter 99).
Chronic low-grade, high-speed MTP joint lameness can occur. Horses often have a previous history of other ipsilateral hindlimb lameness, such as distal hock joint pain. Effusion and a positive response to lower limb flexion are lacking or inconsistent. Lameness is alleviated most consistently with low plantar analgesia, but differentiation from early stress-related bone injury and OA can be difficult without scintigraphic examination. Stress-related bone injury or other bony abnormalities, such as midsagittal fracture of the proximal phalanx and occasionally condylar fractures of the MtIII, are commonly found simultaneously with axial articular fragments. Many horses with axial articular fragments never develop lameness, and fragments are detected only on survey radiographs. If and how axial articular fragments cause lameness is not well understood. Axial articular fragments may vibrate at speed or become interposed in the joint surface during flexion, but synovitis does not play a role. These fragments may affect mechanics of the ipsilateral PSB or impinge on distal sesamoidean ligaments.28 Nociceptive fibers have been found in soft tissue attachments, and stretching during full extension may cause pain.30 In older horses, evidence of full-thickness cartilage damage on the MtIII and the PSBs suggests that axial articular fragments may contribute to the development of OA.
Radiological examination reveals one or more fragments seen best in down-angled oblique views (see Figure 23-1, 42-1, and 42-5). If surgery is considered, both limbs should be examined radiographically. Scintigraphic examination may reveal mild abnormal bone modeling, but IRU is more commonly seen in horses with abaxial, nonarticular fragments (see Figure 42-5).
Axial articular fragments should be removed using arthroscopic surgery. In recent years I have advised removal of fragments before horses begin training, because “down time” associated with arthroscopic surgery is less than if surgery is performed in the middle of a racing year. Subjectively it appears that horses that undergo surgery earlier have fewer problems with stress-related bone injury and OA. In breeds such as the TB and Warmblood, axial articular fragments may complicate sales and can be removed prophylactically. During arthroscopic surgery fragments are carefully trimmed free of capsular attachments with a specially designed intraarticular blade and are removed.34 If arthroscopic surgery is performed before training begins, horses are given 7 days of stall rest, followed by 7 days of stall rest with handwalking, then 7 to 14 days of walking in the jog cart (STBs) or walking and light trotting with an exercise pony (TB). If lameness develops when horses are in advanced stages of training or are racing, I recommend at least 2 to 3 months of rest before training resumes. The prognosis is good for future soundness if the fragment(s) caused the lameness. In one study 63% of racehorses and 100% of nonracehorses had performance similar to preinjury levels after surgery, but the presence of cartilage damage or synovial proliferation was significantly associated with an adverse outcome.28
Abaxial, Nonarticular Fragments
Abaxial, nonarticular fragments can be single or multiple and may occur in combination with axial articular fragments, either on the same side or the opposite side of the joint. Abaxial, nonarticular fragments usually are lateral and can be bilateral. Abaxial, nonarticular fragments can be large and involve the entire lateral, plantar process (see Figure 23-1), including a small articular portion, but most are nonarticular. These fragments resemble old fractures radiologically, but I believe they are manifestations of osteochondrosis.31,33 Fragments are often seen in weanlings or yearlings without clinical signs of lameness, and when seen in older horses, lameness is rarely acute. Abaxial, nonarticular fragments have been described as ununited proximoplantar tuberosities, and in some horses fragments identified at a young age subsequently reunited with the parent bone.35 In my experience, union of abaxial, nonarticular fragments in older horses is rare but does occur.
Lameness is mild (grade 1 of 5 with the horse in hand), usually present at high speed, and worse around turns. Pain is abolished by low plantar analgesia. Palpation may reveal mild bony enlargement, but this enlargement is easily missed. Once horses are clipped, bony swelling is obvious. Response to lower limb flexion is inconsistent. Occasionally a weanling or yearling develops acute lameness with obvious soft tissue swelling that involves the fetlock joint. Radiographs reveal an old abaxial, nonarticular fragment, but generally lameness resolves quickly and is not related to the fragment.
Radiographs reveal one or more abaxial, nonarticular fragments, which are occasionally accompanied by axial articular fragments (see Figure 23-1). Fragments are old and rounded, and radiolucent changes of the parent plantar process of the proximal phalanx are common. A clear separation exists between the fragment and proximal phalanx that is filled by dense, fibrous tissue. Scintigraphic examination may reveal mild IRU.
Abaxial, nonarticular fragments may or may not cause lameness, and clear differentiation between sources of pain can be difficult. The decision of whether to perform surgery is often difficult, because often conventional surgery is required to remove these nonarticular pieces.34 Although the procedure is tedious and best done by using a motorized synovial resector, large abaxial fragments can be removed arthroscopically (see Chapter 23 and Figure 23-1). After surgery horses are given 4 weeks of stall rest, followed by 4 weeks of stall rest with handwalking, then 4 to 8 weeks of turnout in a small paddock or light jogging or galloping. Prognosis is excellent for future soundness, but among STB racehorses, pacers have a better prognosis than trotters. In yearlings with a combination of axial articular fragments and abaxial, nonarticular fragments, I usually recommend arthroscopic surgery to remove axial articular fragments and leave abaxial, nonarticular fragments in place unless clinical signs develop at a later date.
Although I strongly believe that axial articular fragments and abaxial, nonarticular fragments cause lameness and I recommend surgery both therapeutically and prophylactically, others question the clinical significance of these fragments. In a study evaluating radiological findings in STBs before beginning training and subsequent race performance, there was no significant association between the presence of axial articular fragments, abaxial, nonarticular fragments, and other forms of osteochondrosis and either race performance or racing longevity.36
Nonarticular Fragments Originating from the Proximal Sesamoid Bones
Nonarticular fragments originating from the PSBs, the most unusual form of fragmentation, are discussed in conjunction with plantar process fragmentation of the proximal phalanx since radiological findings can be similar to those associated with articular or nonarticular plantar process fragments. Nonarticular fragments originating from the PSBs occur almost exclusively in the forelimb and are rare in the hindlimb. Horses with this form of fragmentation have high-speed lameness and clinical signs are similar to those seen with the other, more common forms of plantar/palmar fragmentation. Radiologically, nonarticular fragments originating from the PSBs are best seen in LM radiographic images, are intercalated in the distal sesamoidean ligaments, can be singular or numerous, and are located plantar/palmar to the articular surface of the PSBs, usually midway between the PSBs and the proximal aspect of the proximal phalanx. These fragments may result from osteochondrosis or from avulsion injury that occurred when horses were sucklings. Nonarticular fragments originating from the PSBs can be removed by using a ligament-separating approach with conventional surgical techniques or by using arthroscopic techniques; a motorized synovial resector is required to debride capsular and distal sesamoidean ligament attachments. Damage to the distal sesamoidean ligaments is unavoidable and I question the value of surgical removal of these fragments. Horses generally return to racing or training at a level similar to that achieved before surgery and high-speed lameness often recurs.
Acute Fractures of the Proximal Plantar Process
True fractures of the proximal plantar process of the proximal phalanx occur, usually are recognized after known or suspected trauma, but are rare. Acute lameness and soft tissue swelling are present. Radiology reveals an acute fracture with a narrow, well-defined fracture line. The margins of the fracture are not rounded, nor are there radiolucent changes in the proximal phalanx. Internal fixation and fiberglass cast application are recommended. Prognosis depends on duration of the fracture before repair and fracture size. OA is a potential complication.
Osteochondrosis of the Sagittal Ridge of the Third Metatarsal Bone
A discussion of osteochondrosis of the sagittal ridge of the MtIII is presented in Chapters 36 and 56.
Osteochondral Fragments of the Dorsoproximal Aspect of the Proximal Phalanx
Osteochondral fragments of the dorsoproximal aspect of the proximal phalanx are common and occur in two forms. Well-rounded osteochondral fragments often occur in young horses, may be a manifestation of osteochondrosis, and are asymptomatic (Figure 42-10). In a recent study of 117 Warmblood horses with fragments in this location, histopathological examination of fragments removed arthroscopically revealed smooth hyaline cartilage surrounding a bony center, and fragments were thought to be a component of developmental orthopedic disease.37 Acute osteochondral fragments result in mild lameness or change in performance and are associated with an effusion and a positive response to lower limb flexion (see Figure 23-6). Arthroscopic surgery and removal of these osteochondral fragments is recommended. In older STB and TB racehorses, osteochondral fragments can be large and numerous, and after surgery a minimum of 8 weeks’ rest is given. Cartilage damage on the opposing surface of the MtIII is common, and the amount is commensurate with size and duration of osteochondral fragments.
Other Osteochondral Fragments
Osteochondral fragments may be identified dorsal or plantar to the collateral ligaments, usually laterally. These osteochondral fragments are usually traumatically induced and may originate from the distal dorsal aspect of the MtIII, but they are not avulsion fractures. Proliferative changes often develop. Treatment is by surgical removal, but prognosis is guarded in racehorses.
A rare finding in the MTP joint is a loose fragment located in the distal aspect of the plantar pouch. In some horses, small defects in the dorsal aspect of the sagittal ridge of the MtIII can be seen radiologically. A small fragment may have detached and migrated to the plantar pouch. Large, loose fragments may exist for some time in the plantar pouch without causing lameness.
Fractures of the Proximal Phalanx
One of the most common major fractures in the MTP joint is midsagittal fracture of the proximal phalanx or other fractures with a midsagittal component. These fractures occur most often in racehorses but also occur in other sports horses. In racehorses, midsagittal fractures of the proximal phalanx occur in STBs equally in hindlimbs and forelimbs, but in TBs, forelimb fractures are most common. These fractures are discussed in Chapters 35 and 36. Horses with moderately comminuted fractures of the proximal phalanx, in which an intact fragment of bone (strut) spans the distance between the proximal and distal articular surfaces of the proximal phalanx, can be managed successfully and salvaged for breeding purposes using open reduction and internal fixation. Those with massive comminution without an intact strut can be salvaged, but use of transfixation pin casting or external skeletal fixation to maintain axial alignment is necessary. In a study of 64 horses with comminuted fractures of the proximal phalanx, 26 fractures involved the hindlimbs, and overall, 33 of 36 (92%) horses with moderately comminuted fractures managed by open reduction and internal fixation were considered to have successful outcomes (salvaged for breeding, pasture soundness, or light riding).38 Twelve of 26 horses (46%) with severely comminuted fractures managed with external skeletal fixation or transfixation pin casting survived, but management was complicated and hospitalization was prolonged.38
Dorsal Frontal Fractures of the Proximal Phalanx
Dorsal frontal fractures of the proximal phalanx occur much more commonly in the hindlimbs than in the forelimbs, and large osteochondral fragments in the forelimb may cause similar clinical signs. Size and depth of fracture appear different between forelimbs and hindlimbs; in the forelimbs, when dorsal frontal fracture occurs it is usually a long fracture beginning deep within the articular surface and extending distally, well into the diaphysis of the proximal phalanx, as compared with the typical fracture in the hindlimbs, which is 7 to 10 mm deep (from dorsal to plantar) and approximately 20 mm in length. They occur in both TB and STB racehorses. Dorsal frontal fractures may be more common in the right hindlimb. Although these fractures are reported to be more common in TBs,39 in my experience the fracture is near equally as common in STBs and can be unilateral or bilateral. If a dorsal frontal fracture of the proximal phalanx is diagnosed scintigraphically, contralateral IRU of the dorsal proximal aspect of the proximal phalanx is commonly seen (Figure 42-11). IRU associated with a dorsal frontal fracture of the proximal phalanx must be differentiated from a midsagittal fracture. Midsagittal fractures are single-event injuries, but a dorsal frontal fracture of the proximal phalanx may be caused by stress-related bone injury, because gradations of IRU are seen in the proximal phalanx and concomitant contralateral IRU occurs. Although bilateral fracture or evidence of stress-related bone injury can be seen bilaterally simultaneously, horses may develop contralateral fracture the next year. TB racehorses appear to be able to tolerate pain associated with dorsal frontal fractures better than STB racehorses; I have seen many that have raced with this fracture. There may be chronic proliferative changes and a displaced fracture in a TB horse that raced within the prior 10 days. Displaced fractures do not occur in STBs, and lameness may be noticed earlier than in the TB racehorse. Pacers are most likely to have an obvious fracture, whereas fractures in trotters may be scintigraphically active with only subtle radiological changes.

Fig. 42-11 A, Delayed (bone) phase lateral and plantar scintigraphic images of a metatarsophalangeal (MTP) joint of a 3-year-old Thoroughbred filly showing focal, intense increased radiopharmaceutical uptake (IRU) associated with the proximal dorsal aspect of the proximal phalanx (arrow) in the left hindlimb (LH) Mild-moderate IRU is seen in the right hindlimb, associated with early maladaptive or nonadaptive bone remodeling of the distal plantarolateral aspect of the third metatarsal bone. B, Flexed lateromedial digital radiographic image of the LH MTP joint showing the typical configuration of a nondisplaced dorsal frontal fracture of the proximal phalanx (arrows). Because the fracture is nondisplaced and there are no interposed fragments in the fracture line, this horse can be managed conservatively with an excellent prognosis.
A dorsal frontal fracture of the proximal phalanx usually results in intermittent, severe lameness, but bilateral fractures may cause poor performance without causing obvious signs of lameness. Effusion is present but may be only mild unless fractures are displaced. The response to lower limb flexion is positive. Intraarticular or low plantar analgesia abolishes lameness in horses with complete or displaced fractures, but the low plantar technique should be used in those with stress-related bone injury or incomplete fractures. Radiographs reveal a single fracture line that is best recognized in LM or flexed LM images. Fractures are usually on the dorsolateral aspect of the proximal phalanx, and if seen in oblique radiographic images, are best seen in the DM-PlLO image, a position to keep in mind if surgical repair is contemplated. Fractures begin at the articular surface and course in a dorsodistal direction (see Figure 42-11). In TBs with displaced fractures an osteochondral fragment often is interposed between the main fracture fragment and the parent bone.
If fractures are nondisplaced, conservative management provides a good-to-excellent prognosis in both TBs and STBs. Horses are given 4 weeks of stall rest, followed by 4 weeks of stall rest with handwalking, then 4 to 8 weeks of turnout in a small paddock. Two treatment options are available for horses with displaced fractures. In those with large fragments and interposed osteochondral fragments, arthroscopic surgery is recommended to remove small osteochondral fragments and to repair the dorsal frontal fracture using one or two 3.5-mm screws. If the fracture cannot be reduced or is broken or small, the fragment should be removed. Prognosis is good to excellent for future racing, but horses may drop in class, particularly those with compensatory or numerous lameness problems. Long dorsal frontal fractures, such as those that occur in the forelimbs, cause acute, severe lameness and should be repaired (see Chapter 36).
Fractures of the Proximal Sesamoid Bones
Overall, fractures of the PSBs appear to be near equally distributed between the metacarpophalangeal and MTP joints, but distribution depends on fracture configuration. In STB racehorses, distribution of all PSB fractures likely favors the hindlimbs. In a study of TB racehorses less than 2 years old, 92% of apical fractures of the PSBs occurred in the hindlimbs, and overall 84% of horses raced after arthroscopic surgical removal of the fracture fragments, a prognosis similar to racing performance of maternal siblings.40 In another study, in TB racehorses that were 2-year-olds or older, 64% of apical fractures of the PSBs occurred in the hindlimbs, and prognosis for racing after arthroscopic removal of hindlimb fractures was 83%.41 In both studies, prognosis for racing was better when fractures occurred in a hindlimb than in a forelimb.40,41 Apical fractures of the PSBs are more common in the hindlimb of STBs and most often involve the lateral PSB. Fractures of the abaxial aspect of the PSBs, sometimes including an apical component, occur most commonly in the medial PSB in the forelimb. Midbody and basilar fractures of the PSBs appear to be more common in the forelimbs. Fractures of the PSBs can be traumatic or pathological. Young racehorses develop acute lameness and fracture without preexisting disease of the PSB or SL. However, the PSB undergoes extensive remodeling similar to the MtIII, and it is possible, perhaps even likely, that these fractures represent a form of stress-related bone injury. In older racehorses and in some nonracehorse sports horses, preexisting radiolucent and proliferative sesamoiditis and suspensory branch desmitis are present, and fractures of the PSB appear to develop as a pathological, secondary, end-stage injury. In some nonracehorse sports horses, fracture occurs as a single event without preexisting injury. Prognosis depends on the size of the fracture fragment and the degree of suspensory desmitis. In STB racehorses, prognosis is better in pacers than in trotters, and prognosis is poor in horses developing fractures early in training before racing begins (see Chapter 36). The prognosis is good in nonracehorse sports horses without preexisting injury. Arthroscopic surgical removal of apical, abaxial, and small basilar fracture fragments and repair of large basilar and midbody fractures are recommended (see Chapter 36).
Fractures of the Distal Aspect of the Third Metatarsal Bone
Condylar fractures of the distal aspect of the MtIII occur less frequently than those of the McIII (see Chapter 36). In a study of 135 horses with condylar fractures, 81% and 85% involved the forelimbs and lateral condyles, respectively.42 Lateral and medial condylar fractures of the MtIII occur, but lateral fractures are most common. Lateral condylar fractures can be short and incomplete, long and incomplete, or long and complete. Bilateral fractures occasionally occur simultaneously. Condylar fractures are primarily racing injuries. In a study of TB, STB, and Arabian racehorses, TBs were overrepresented and STBs underrepresented; TBs had significantly more lateral and forelimb fractures than STBs.43 Clinical signs are commensurate with the length and degree of displacement. Medial condylar fractures can be short, incomplete, and difficult to diagnose. However, most commonly lameness is severe and radiographs reveal that the fracture is long and incomplete but goes straight proximally to end abruptly in the diaphysis, forms a Y-shaped pattern (Figure 42-12), or spirals proximally to end near or at the tarsometatarsal joint (Figure 42-13). Occult fissure lines and spiraling should always be suspected, and it is critical to know the location of the fracture before horses are transported and prognosis is discussed. Horses with medial condylar fractures are at extreme risk for fracture propagation or comminution. Even after surgical repair, horses are at risk during recovery from general anesthesia and early in the postoperative period. In 15 horses with medial condylar fractures of the MtIII, the fractures of 12 horses were repaired, two horses suffered catastrophic fracture during recovery from general anesthesia, and three horses developed complete fracture within 4 days after surgery.44 Recovery from general anesthesia should be assisted and may best be performed using a pool recovery system, if available.

Fig. 42-12 Digital radiographic images before and after surgery of a 2-year-old Thoroughbred filly with a nondisplaced, spiral fracture of the third metatarsal bone (MtIII) beginning at the medial condyle. A, Dorsoplantar radiographic image (lateral is to the right) showing the fracture line (arrow) beginning from the medial condyle and propagating proximally in a slight spiral fashion. Both dorsal and plantar cortical lines can be seen. B, Dorsal 45° medial-plantarolateral radiographic image showing that the fracture line abruptly becomes oblique (arrows) and stops in the middiaphyseal region. This horse would be at risk for catastrophic injury without repair, and during or immediately after surgery if repair were performed with bone screws alone. C, Postoperative dorsoplantar radiographic image showing repair of the fracture using screws placed in lag fashion and a 12-hole limited-contact dynamic compression plate applied to the lateral aspect of the MtIII, using a dorsal, transtendonous approach. The distal two screws and the first four distal screws in the plate have been placed in lag fashion. The plate was later removed at 3 months after surgery, and the filly raced successfully as a 3-year-old.

Fig. 42-13 Dorsoplantar radiographic images of the metatarsophalangeal (MTP) joint and the entire metatarsal region. There is a spiral fracture of the third metatarsal bone (arrows) beginning at the medial condyle of the third metatarsal bone (medial is the left) in the MTP joint and extending to near the tarsometatarsal joint (confirmed at surgery after subperiosteal dissection) before (A) and after (B) surgery.
Horses with short, incomplete lateral and medial condylar fractures can be managed conservatively or can undergo surgical repair. Those with longer spiral or medial condylar fractures with a Y shape should undergo surgical repair. This repair can be accomplished by use of a combination of open observation of the fracture line and either screw fixation (see Figure 42-13) or a combination of screws and a dynamic compression plate or locking compression plate (see Figure 42-12). Prognosis depends on whether fractures are medial or lateral, whether they are displaced or nondisplaced, and whether a plate or numerous screws are used for repair. If fractures heal and plates (if used) are removed, prognosis for racing is favorable, but horses will often drop in race class or fail to reach full potential.
Sesamoiditis
In the STB, hindlimb sesamoiditis is most common in the lateral PSB but can occur medially and be a source of occult MTP joint lameness. In TBs sesamoiditis is most commonly observed in the forelimb. TBs can have obvious radiolucent lines in the PSBs in hindlimbs that are often asymptomatic. Disparity between limbs, rather than size or number of radiolucent lines, was found in a study to be most important in determining clinical significance in TBs; horses with three or more channels were less likely to race as 2-year-olds and had decreased earnings per start.45 In another study, in the STB racehorse the presence of one to three or more radiolucent defects less than or equal to 1 mm in width was not associated with lameness referable to the PSBs, but horses with wide, abnormally shaped defects developed lameness from sesamoiditis.46 Conversely, Grøndahl and colleagues reported that of 753 young STBs that underwent radiographic examination before training, 21 horses had severe sesamoiditis, fractures, or enlarged PSBs, but a correlation between sesamoid pathology and lameness or decreased racing performance and earnings could not be made. In that study hindlimb PSBs were affected in only six horses, and lameness developed in 14 horses.47 Although lameness could not be directly attributed to changes in the PSBs, in some horses MTP joint lameness was diagnosed, and perhaps compensatory lameness developed as a result of chronic, low-grade or high-speed lameness in these trotters. Seven of 21 horses had concomitant osteochondral fragments of the plantar/palmar process of the proximal phalanx, although a clear relationship could not be established.47
Radiolucent Defects of the Axial Border of the Proximal Sesamoid Bones
See Chapters 72 and 74 for a discussion of radiolucent defects of the axial border of the PSBs.
Flexural Deformity of the Metatarsophalangeal Joint
Dorsal subluxation of the MTP joint (buckle or knuckle forward) occurs in horses with flexural deformity. Intermittent subluxation occurs in those with mild deformity, but some horses with more severe deformity maintain the MTP joint in partial flexion. Horses with chronic, severe tenosynovitis of the DFTS with extensive adhesions may develop progressive, severe flexural deformity. Desmopathies of the accessory ligament of the DDFT may cause flexural deformity (see Chapter 71). In some horses, application of an extremely elevated heel shoe (e.g., 5 to 8 cm) may help alleviate pain (see Chapter 59).
Dropped fetlock or plantar subluxation (hyperextension) occurs in horses with severe chronic suspensory desmitis or those with severe, acute tearing of the superficial digital flexor tendon (SDFT), the DDFT, or both the SDFT and DDFT.
Soft Tissue Injuries of the Metatarsophalangeal Joint and Fetlock Region
Proliferative Synovitis
Proliferative synovitis (i.e., enlarged synovial pad or villonodular synovitis) occurs in the dorsal aspect of the MTP joint in horses with chronic OA. However, it is much less common than in the metacarpophalangeal joint and is a rare primary cause of pain (see Chapter 36).
Luxation and Subluxation: Tearing of a Collateral Ligament
Complete disruption of a collateral ligament causes luxation and results in severe, non–weight-bearing lameness and usually obvious valgus or varus deformity. This injury is more common in adult horses, because physeal fractures of the distal aspect of the MtIII and proximal phalanx are more likely in foals. Initially little swelling occurs, but within a few hours soft tissue swelling can be prominent and manipulation of the joint reveals instability. Diagnosis is confirmed radiologically using DPl and stressed DPl images. Radiographs should be examined carefully for the presence of concurrent fractures on the contralateral or plantar aspects of the joint. Ultrasonography is used to identify the injured portion of the collateral ligament and extent of injury. After manual reduction with the horse under general anesthesia, a fiberglass cast should be applied. The cast should be changed within 7 to 10 days, because swelling resolves and the cast loosens. Cast coaptation should be maintained for 8 to 10 weeks, and then a heavy bandage should be applied. If crushing of the opposite side or plantar aspect of the joint did not occur, prognosis for soundness is guarded to fair. OA and chronic desmitis of the collateral ligament are possible. In a study, eight of 17 horses with rupture of the collateral ligaments of the metacarpophalangeal or MTP joints had hindlimb injury, and the lateral collateral ligament was more commonly affected. The presence of avulsion fracture fragments did not negatively affect prognosis. Ultrasonographic examination was useful in characterizing injury. Eight of 16 horses managed with external coaptation returned to some form of rider exercise.48
Collateral Desmitis
Primary injury of the collateral ligament without luxation is rare in my experience. Clinical signs include firm soft tissue swelling and ultrasonographic evidence of desmitis in horses with lameness that is abolished by low plantar analgesia. Avulsion fractures may occur as a result of trauma.
Distal Sesamoidean Ligament Injury
See Chapter 72 for a discussion of injury of the distal sesamoidean ligaments.
Tenosynovitis of the Digital Flexor Tendon Sheath
See Chapter 74 for a discussion of tenosynovitis of the DFTS.
Deep Digital Flexor Tendonitis
See Chapters 70 and 74 for a discussion of deep digital flexor tendonitis.