Chapter 107The European Thoroughbred
History of Horse Racing in the United Kingdom
As long as people have ridden horses, matches of speed have been held informally between proud owner-riders. Racing horses under saddle was certainly established in England by the time of the Roman occupation. Chester boasts the longest running unbroken series of race meetings in the United Kingdom on the original site, the strangely named Roodeye. This area of land (translated, island of the cross) has been used for horse racing continuously since 1539. Interestingly, racing was introduced to replace football (soccer), which had been banned a few years earlier because of the number of severe injuries and fatalities it produced. The original prize money was substantial for the time, being “in the XXXI yere (31st year) of King Henry Theght (VIII), a bell of sylver, to the value of three shillings and three pence, is ordayned to be the reward of that horse which shall runne before all others.”
Since the time of James I (1603 to 1625), a link has existed between royalty and the town of Newmarket in Suffolk, leading to its reputation as the headquarters of racing in the United Kingdom. Charles I, the successor of James I, established regular spring and autumn race meetings in Newmarket and built a palace and stables, some of which have survived. Racing at that time consisted of matches between pairs of horses, over long distances by modern standards, usually accompanied by hefty personal wagers between their aristocratic owners. Distances as long as 4 to 6 miles were not unusual. During the succeeding two centuries the race distances declined, as did the age at which horses were allowed to race. Initially horses had to be older than 5 years of age, but this was reduced gradually until in 1859 even yearlings were allowed to race. This practice soon ceased, but 2-year-old racing had become established and became, unfortunately in the opinions of many, part of the Thoroughbred (TB) spectrum. During this time the breed itself changed considerably.
Arab horses had been imported sporadically to Britain from the time of the Crusades (twelfth century AD). Usually seized in battle, these Arab horses would have been relatively slow and sturdy horses, used for carrying warriors into battle. In the seventeenth century, a marriage alliance between Charles I and the Portuguese Royal Household allowed Charles access to the Arab horses of the Barbary Coast, and several stallions made the long journey, mainly over land, back to the United Kingdom. Three horses alone—the Byerley Turk, the Darley Arabian, and the Godolphin Barb—founded the entire breed of the TB we know today, producing profound changes in size and conformation from the native English stock. Eighty percent of the TB racehorses alive today are descended from just one of these stallions, the Darley Arabian, through his great-great-grandson Eclipse.
As the distance of races decreased, speed became an increasing factor, and the fields of competitors increased in size. Eventually the handicap system was introduced in an attempt to avoid the dominance of the sport by a few exceptionally gifted individual horses. All this led to an increase in interest in racing as a spectator sport and a vehicle for gambling. From the nineteenth century onward, racing was more or less recognizable as the sport we enjoy today.
Pattern of Racing
The most prestigious races in Europe belong to a worldwide system of accreditation, which groups together races of similar standing. The best horses competing at top level meet each other in a group of internationally acknowledged races known as Group 1. This group includes all the classics in the United Kingdom and the most prestigious races throughout Europe and North America. Beneath Group 1 are two other groupings (Group 2 and Group 3) for horses that have excellent ability but are not up to the extreme rigors of Group 1 racing. Competitors in these races face a weight for performance penalty system. For example, a Group 1 winner running in a Group 2 race carries a weight penalty in an attempt to equalize the competition.
The next tier down from Group races includes the Listed races. Again, the International Pattern Committee decides which races are of sufficient stature to belong to this list. Usually horses enter a Listed race when they have already won a maiden and possibly another race with specific conditions. Such horses have few other realistic options because after two wins a horse carries a lot of weight in an open handicap. Often success in a Listed race increases potential breeding value far more than winning such a handicap. These limited opportunities are often the reason why horses that are good, but not good enough to be top class, are sold out of Europe to continue racing in North America, where races are more suitable. Horses racing in North America are also often able to recoup in prize money the owner’s investment, a situation that is often impossible racing in Europe, with its relatively lower prize money.
Beneath the upper echelon of horses racing in Listed and Group company is an open handicap system in which horses are allocated weight according to speed rating. These speed ratings are assessed by professional handicappers, who monitor the performance of the horses when they run in the first three maiden races or less if they win. The horse’s rating rises and falls during its racing career, depending on its most recent form. Although this system is obviously open to abuse by trainers running horses at inappropriate distances or on unsuitable ground to lower their racing weight, the system does allow horses of moderate or differing ability to compete against one another on near equal footing and produce an exciting finish. The handicappers’ dream is of all horses finishing within a length or so of each other.
Until recently all flat racing in the United Kingdom took place on turf. This led to a certain divergence in bloodlines and ability patterns of racehorses in North America and Europe. About 20 years ago, all-weather racing on a synthetic surface was developed at two tracks, Lingfield and Southwell. Although initially introduced for hurdle racing as a way of keeping the betting public satisfied when the National Hunt cards had to be abandoned through bad weather, both tracks rapidly discontinued hurdle racing on all-weather surfaces because of the high injury rate. This left the way open for flat racing on the all-weather tracks to become established. Since that time, new synthetic tracks have also opened at Wolverhampton, Kempton, and Great Leighs.
The synthetic all-weather track surface is not the same as the dirt commonly used in North America. The depth of the cushion is greater, and the material is a composite of oil, plastics, fibers, and sand. Few races with large prize money are run on the synthetic surfaces, and the racing has tended to be of a more humble grade, but that is slowly beginning to change. These tracks give horses of limited ability somewhere to race and also allow trainers with small stables to compete with each other in the absence of both top-level horses and the larger yards, although this too is beginning to change. Several successful all-weather horses have made a transition to racing in North America to end up running in Group (graded stakes) races on dirt, and the all-weather surface can act to some extent as a screening academy to pick out horses that seem particularly adept at performing on these artificial surfaces, although not all horses make a successful transition from synthetic surfaces to dirt racing.
Flat racing is popular in the United Kingdom, Ireland, and France but less so in the rest of Europe. Although training centers exist in Germany along with a substantial number of high-grade races, flat racing has not really caught the imagination of the public in the same way as in Britain and Ireland and receives little media attention. Ireland always has had a strong tradition of horsemanship, and racing, centered around the Curragh, is buoyant and popular. Standardbred racing is equally popular in France, Germany, and Scandinavia, where flat racing opportunities are limited. Many European countries enjoy racing in the absence of a substantial breeding industry, and this creates a market for the surplus racehorses produced and raced in the United Kingdom, Ireland, and France. Horses in these countries are raced at 2 years of age and, ability permitting, 3 years of age, and at the end of the 3-year-old career many are submitted for sale if they have not shown sufficient ability to be retained for racing as older horses. This makes room in the yards for the incoming yearlings. These large dispersal sales at the end of the 3-year-old career supply the horses for National Hunt racing in the United Kingdom and for flat racing areas of the world lacking breeding programs. The need for yards to clear out the less gifted 3-year-olds to make room for the influx of yearlings also produces enormous pressure on trainers and consequently their veterinary surgeons to have a racehorse fit and able to race at 2 and 3 years of age, often without consideration for the long-term consequences of any treatments.
The small window of opportunity available to these horses impinges directly on many of the surgical and medical management decisions that need to be made when problems arise. The economics and practicality of any advice given have to be considered from the owner’s viewpoint and the welfare of the horse.
Comparisons with Racing in North America
One of the major differences between training and racing in North America and Europe is in the geographical location and logistics of stabling and training of the horses. In the United States, almost all horses train at the racetrack and are stabled there continuously. In Europe, the horses live and train in yards often well away from the racetrack. These yards tend to be clustered around a training area, with gallops and conditioning canters available for use by local trainers. The horses travel daily to race at racecourses that may be up to 200 miles away.
In the United States, the horses, trainers, jockeys, and veterinary surgeons tend to move from one racecourse to another, but they stay at each track for long periods. Racing at each location takes place for many days or even weeks before horses and trainers move on to another track. Although some horses stay behind at one track, racing does not occur at that track when the primary focus is elsewhere.
In Europe, racing seldom occurs at any one racecourse for more than 3 consecutive days. Horses are trained in traditional stables, some of which date back many centuries. Horses travel to racecourses the day before racing, if the journey is particularly long, or even on the day of the race. Some horses make extremely long round trips. For example, it is not unusual for a trainer in Arundel on the south coast to send horses as far north as Ayr in Scotland, a round trip of 936 miles. Obviously the cost of transport has to be weighed against the potential gains, but the traditional system of training and traveling to the races in the United Kingdom seems to be holding up for now.
In 2000, two of the all-weather racetracks opened training barns adjacent to the track with a view to introducing American-style training, track side. How popular and successful this system is going to be and whether it will spread to other racecourses remain to be seen.
In North America, almost all training and racing takes place on a left circle (counterclockwise), and this might be expected to have influences on the incidence rates of injury to the left and right limbs for many lesions, such as proximal sesamoid bone (PSB) fractures, third metacarpal (McIII)/metatarsal (MtIII) bone condylar fractures, and tendonitis (see Chapter 106). In the United Kingdom, much conditioning work and even race speed training take place in straight lines (Figure 107-1). Racing itself can be on straight tracks (e.g., 1000 and 2000 Guineas at Newmarket), predominantly to the left (Epsom Derby), or to the right (Doncaster St. Ledger). The tracks themselves divide into about one third right-handed and two thirds left-handed throughout the country. This has an important impact on the lack of specific incidence of injury to the left or right limbs. One large fracture survey in Newmarket showed few instances of left or right dominance for any injury.1
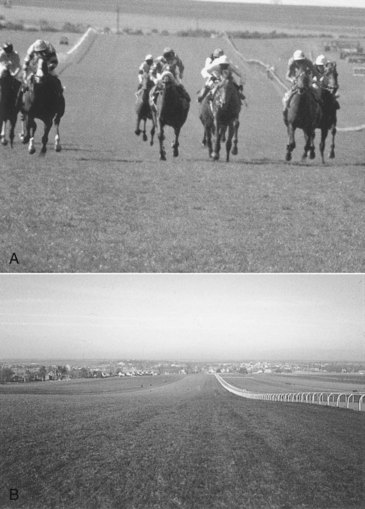
Fig. 107-1 A, Horses approach the finish of the long and lonely Rowley mile racetrack at Newmarket. This photograph illustrates the undulating nature of the straight 1-mile track over which both 3-year-old Group 1 classics are run. B, The long straight of the training track gallops up Warren Hill just outside Newmarket. Two different all-weather synthetic surfaces are also available (between the white railings). The rest of the heath is used in strips, which are changed daily using movable markers. Each strip of grass is used only once every 3 years.
Making categorical comments about the impact the new synthetic tracks have made on specific lameness and injury in the United Kingdom is difficult for several reasons:
Training Regimens in Europe
Yearlings arrive in the yards for breaking from the sales in September and October and, unlike the situation in North America, often go straight to the trainer for breaking rather than to a specialist pretraining center.
After breaking, the yearlings usually start steady cantering exercise until Christmas. As the racing season approaches, horses showing precocity and ability to withstand faster exercise step up in pace throughout February and March. The first 2-year-old races occur in April, encouraging hard training of skeletally immature horses. However, until the racing calendar changes and while these races are open and available, trainers will train horses for them.
All-weather racing has altered the seasonal impact of flat racing in the United Kingdom forever, and some flat race horses now train throughout the year. However, most of the high-quality flat race horses do not compete on the all-weather circuit and are put into a slow-speed maintenance program from November until January, involving light cantering and trotting. Fillies may be turned out for a period.
All this is substantially different from the position in North America, where the horses often do not arrive at the racetrack until they are fully broken, in cantering exercise, and ready to do fast work. The breaking and pretraining often takes place in specialized pretraining centers, away from the city center tracks. This has important effects on the perception of racetrack veterinarians in North America concerning the incidence of developmental orthopedic disease linked to lameness. In North America, developmental orthopedic disease often causes lameness leading to diagnosis and removal from training before a horse reaches the racetrack; therefore horses with developmental orthopedic disease are not commonly seen by track veterinarians. An example is a subchondral bone cyst in the medial femoral condyle. Subchondral bone cysts are a regular occurrence in the annual intake of yearlings in the United Kingdom, diagnosed by the trainers’ veterinarians. Discussion with colleagues working at California racetracks reveals that they rarely see horses with subchondral bone cysts, presumably because of the effect of the earlier screening at the pretraining centers.
Once on the track in North America the racing is often less seasonal and less age specific, removing a lot of the pressure for success at 2 or 3 years of age within a short season. Whether a horse races on turf or dirt does not matter: historically, all training took place on dirt, and this should be borne in mind by veterinarians assessing horses for potential purchase to move from Europe to America. Asking potential purchasers whether the horse is intended for turf or dirt racing is largely irrelevant because the daily training almost certainly will be on dirt. The dirt surface is more testing in many ways than anything these horses have seen before, and horses able to train and perform well on grass sometimes fail to make the transition to dirt. In the past couple years, a few training tracks and racetracks in North America have moved to synthetic surfaces. It will be interesting to see whether this makes for an easier transition for horses moving from Europe to race in North America, and what impact it has on the types and frequency of training and racing injuries.
Clinical History
Taking a detailed history is a prerequisite for a medical examination in any species. In racehorse practice one often sees a succession of lame horses during any morning in several different yards, and the detailed information may be limited. The trainer may not be present to supply it. However, one should always try to ascertain the following information before examining a TB racehorse for lameness:
Stress-induced bone injuries are more likely to become apparent as work intensity increases. Stress-induced bone injuries include all of the long bone stress fractures of the humerus, tibia, the McIII, and the MtIII, and the ilial wing and shaft of the pelvis. Similarly, in a 2-year-old that has reached advanced training speed, the carpus and metacarpophalangeal joint are common sources of forelimb lameness, and lateral condylar stress injuries of the MtIII are common causes of hindlimb lameness. A 2-year-old in advanced training is less likely to have lameness associated with a subchondral bone cyst, osseous cystlike lesion, or OCD because these lesions usually cause lameness when the horse is younger and beginning its conditioning exercise. However, occasionally subchondral bone cysts and osseous cystlike lesions may arise or result in clinical signs for the first time at 3 years of age or even older.
If a horse did not race at 2 years of age, then all the differential diagnostic criteria used in the recently broken 2-year-old should be applied to the 3-year-old.
In horses with acute-onset, severe lameness, questions of clinical history become less important because the horse is often not bearing weight, and a suspicion of skeletal failure is raised. Knowing whether this horse has been a good mover before onset of severe lameness is often helpful because some injuries (McIII/MtIII bone condylar fractures, PSB fractures) often are associated with poor gait before the actual fracture takes place. The same is true of horses with slab fractures of the third carpal bone, which often are preceded by a long period of subchondral bone sclerosis associated with bilateral third carpal bone pain (Figure 107-2). One of the most useful questions to ask about a horse with severe lameness is what stage of training the horse has reached because only advanced training to fast canter or gallop speeds usually results in bone failure. However, bacterial infection subcutaneously or within the hoof also can produce severe lameness.
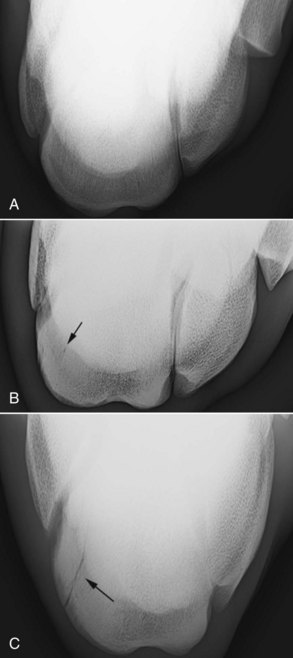
Fig. 107-2 Flexed dorsal 60° proximal-dorsodistal oblique radiographic images of the left third carpal bone (C3) of three Thoroughbreds (TBs). Lateral is to the right. A, Normal. However, this complete lack of increased radiopacity is rare in a TB in advanced training, most of which show some degree of radiopacity of the radial fossa of C3. B, Dense increased radiopacity of the radial fossa of C3. Normal trabecular pattern is lost, and the bone has a “ground glass” appearance. There is increased osteolysis at the site of a normal nutrient foramen (arrow in the center of increased radiopacity). This stiffening of the bone predisposes it to injury or fracture. C, A nondisplaced sagittal fracture of C3 that propagates through the center of an area of severe increased radiopacity representing mineralization of bone (arrows).
Clinical Examination
The veterinarian always should get the horse out and see it walk and trot to determine which limb is lame. Riders are notoriously unreliable at detecting the correct lame limb. The veterinarian should determine whether the lameness is unilateral or bilateral by the way the horse moves. Many racehorses are slightly lame in all limbs and have a typical crouching, shuffling trot or may try repeatedly to break into a canter because trotting is so uncomfortable. New lameness may be superimposed on a chronic level of unsoundness.
Increasing experience usually leads one away from the belief that any one injury is linked to a particular gait. Lameness typical of a shoulder or a stifle tends to become a more remote belief because so-called typical lamenesses so often are linked eventually to the most unexpected site. However, a few types of lameness do remain that seem to be linked to one particular pathological syndrome. Young TBs often show bilateral forelimb lameness related to carpal pain. These horses often trot with the limbs abducted from the midline and not fully flexed during forward motion. This gives a rolling, stiff-legged forelimb gait. The horse’s attempt to get the contralateral limb down quickly to get off the sore limb as soon as possible shortens the forward phase of the stride, leading to a choppy, stilted action. However, horses affected with bilateral front fetlock pain or PSD trot in a very similar way if the pain level is the same in both limbs, and it may simply be that because carpal lameness is a common manifestation of this gait, we have come to link the two more firmly than we should.
Pain associated with the metatarsophalangeal joint is often bilateral and leads to a fairly characteristic gait typified by low limb flight, often with dragging of the toe during protraction, and an exaggerated rocking pelvic excursion dorsoventrally on both sides (sometimes termed the Marilyn Monroe trot) because the horse dips off each painful limb. Horses with a humeral stress fracture often abduct the limb, with shortened cranial protraction at the walk. One Newmarket trainer described this gait recently as “trotting like a pig in a tight skirt,” which, although not a likely scenario, is in fact just how they look..
Having ascertained which limb is the lamest, the limb should be examined in detail using basic examination protocols (see Chapters 4 through 8 and 10). The following specific points apply to the TB racehorse.
Running a finger distally on the shin with a horse bearing weight often causes a horse to buckle the limb even if it has been months or even years after shin soreness has subsided and is not a reliable diagnostic test.

Fig. 107-3 Application of torsion to the tibia. The metatarsophalangeal joint is rotated medially, the os calcis laterally, and firm shoulder pressure maintained with the stifle. Horses with a stress fracture of the tibia often show a sharp pain response to this test and will often be unwilling to bear weight on the limb for some seconds subsequently.
Imaging Considerations
Radiography and Radiology
Many lesions in the TB racehorse are associated with subtle changes in bone density and structure rather than overt fragmentation of bone. These variations result in subtle changes in radiopacity (increased radiolucency or radiopacity), which often are seen best on high-quality radiographs using single-screen film and excellent radiographic technique or more recently by using digital radiography. However, we should be aware when using digital radiography that the “standard” appearance of bone is lost. By altering the algorithms and scaling, we can alter contrast and obliterate the signs of increased radiopacity of bone at will. This is particularly true in appraisal of the “skyline” projection of the third carpal bone, where assessment of increased radiopacity is critical in advising on future workload of young horses and can be made MORE difficult by the ease of image manipulation now available to us digitally.
Radiography is notoriously unreliable in detecting early fracture lines and subchondral bone collapse. For this reason, if lameness is linked to a particular site by diagnostic analgesia and nothing is visible radiologically, repeating the radiography 2 weeks later is often advisable. Any horse with subtle changes in bone density can be rested long enough where additional damage can be seen. During investigation of individual joints, special projections are often most useful (Figure 107-4). Radiographic examination of the metacarpophalangeal and metatarsophalangeal joints always should include the flexed dorsopalmar image, which is extremely useful for evaluating the palmar and plantar aspect of the condyles (see Figures 107-4 and 107-5).3,4 In a hindlimb this view often is achieved best as a plantarodorsal image. The limb is cupped loosely by a hand underneath the tarsus and allowed to hang in a semiflexed position. The cassette is placed in a cassette holder and positioned on the dorsal aspect of the metatarsophalangeal joint, and the x-ray machine is positioned above and behind to achieve the orthodox 125-degrees image.
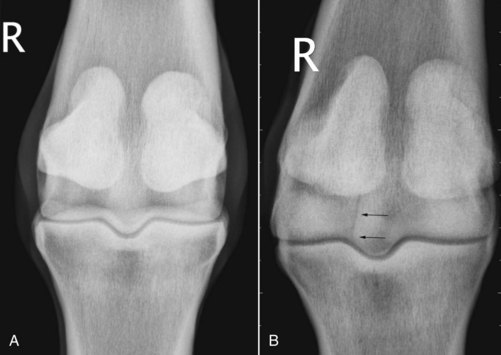
Fig. 107-4 A, Weight-bearing dorsal 20° proximal-palmarodistal oblique radiographic image of a right metacarpophalangeal (MCP) joint. Lateral is to the left. No gross abnormality is seen. B, Flexed dorsal 125° distal-palmaroproximal oblique radiographic image of the same MCP joint. There is an incomplete linear fracture (arrow) in the lateral condyle that was not visible on any other image.

Fig. 107-5 A, Dorsal 60° proximal-palmarodistal oblique image of the left metacarpophalangeal (MCP) joint; lateral is to the right. This steeply angled dorsopalmar image was developed in an attempt to see subchondral bone change diagnosed by magnetic resonance imaging examination, but not seen on conventional radiographs. There is a zone of severe bone mineralization (increased radiopacity, arrows) associated with an advanced subchondral bone injury in the medial condyle. Normal trabecular pattern of the condyle is lost (cf., lateral condyle). B, Dorsal 60° proximal-palmarodistal oblique image of a right fore MCP joint; lateral is to the left. There is less marked mineralization of the medial condyle (white arrows) than in A, but there is radiolucency/fissuring in the most palmar portion of the parasagittal aspect of the medial condyle (black arrows). This horse was lame at the walk, and pain was localized to the MCP joint by local analgesia. This fissuring was not visible on orthodox radiographic images. C, Dorsal 30° proximal 45° lateral-plantarodistal medial oblique image. This image highlights the region of the lateral condyle in contact with the lateral proximal sesamoid bone when the joint is at full weight bearing, a common site of focal stress injury. Focal bone mineralization (increased radiopacity) is evident (white arrows) with a central area of radiolucency (black arrow), which probably represents bone necrosis and resorption. This degree of change is usually irreversible and associated with chronic lameness. These changes cannot be seen on any other radiographic image.
The lateral condyle of the MtIII bone is a predilection site for subchondral bone injury, represented by sclerosis in the early stages and subchondral bone loss and radiolucency as the condition advances. This can be highlighted by a dorsal 30° proximal 45° lateral–plantarodistal medial oblique image (down angled oblique) developed by Ross5 (see Figure 107-5, C).
Another unorthodox image that can be helpful in trying to evaluate subchondral bone radiopacity and fissuring in the distal palmar/plantar aspect of the McIII/MtIII is a steeply angled (60°) dorsopalmar/plantar image (i.e., dorsal 60° proximal-palmarodistal oblique view), centered on the palmar/plantar aspect of the condyles, projecting the PSBs proximally. Areas of fissuring and radiolucency adjacent to the sagittal ridge of the McIII/MtIII or prominent increased radiopacity of the subchondral bone can sometimes only be seen on this image (see Figure 107-5, A). This image was developed in response to frustration in being unable to see marked changes in this site seen on magnetic resonance imaging (MRI) examination using conventional radiographic images (Figure 107-6).

Fig. 107-6 Dorsal 15° proximal-palmarodistal oblique (A) and lateromedial (B) images of the left fore fetlock of a 2-year-old TB, with lameness localized to the metacarpophalangeal (MCP) joint by regional and intraarticular analgesia. There is mild increased radiopacity of the palmar aspect of the medial condyle (arrows), but within the range one might encounter in sound horses. T1-weighted gradient echo motion-corrected low-field magnetic resonance images, dorsal (C) and parasagittal (D) plane, of the same MCP joint. There is diffuse marked decreased signal intensity within the palmar aspect of the medial condyle (arrows) and to a lesser extent in the lateral condyle. This is consistent with mineralization (bone sclerosis) underestimated in the radiograph.
(Courtesy Sarah Powell, Rossdale and Partners, Newmarket, England.)
Radiographic examination of the carpus always should include a flexed dorsal 55° proximal-dorsodistal oblique (skyline) image of the third carpal bone, which is sometimes the only image in which lesions in this bone can be seen clearly. The image is easy to do well but is still often done poorly. Small changes in the angle of projection make a substantial difference to the amount of the third carpal bone visible in the resultant image.6 One should not be satisfied unless the entire radial fossa is seen clearly (see Figure 107-2).
The relevance of changes in bone density should not be underestimated. Many stress fractures of the long bones are seen only by the occurrence of endosteal or periosteal callus. Periosteal callus may only be visible with the aid of a bright light or more extreme digitally produced “windowing.” Fracture lines are relatively rare. Despite the difficulty in imaging incomplete fracture lines sometimes, some horses may go on to develop complete, displaced fractures during periods of box rest, reminding us that the evidence must have been there if only we could have seen it.
Scintigraphy
Scintigraphy has allowed enormous advances to be made in the detection and understanding of stress fractures in the racehorse.7-9 Scintigraphy should not be used as a first line of investigation in horses with obvious single-limb lameness, unless a strong clinical suspicion exists that the humerus, pelvis, or tibia is involved and radiography has been unrewarding. Examination of an entire TB racehorse that cannot trot and has multilimb lameness is often useful. These horses are difficult to assess using diagnostic analgesia because one is often racing against time, moving from one limb to another with the predominant lameness constantly changing. Scintigraphy in these horses often results in a list of lesions that can be investigated radiologically and by judicious use of diagnostic analgesia. The other roles of scintigraphy include examining a site identified by diagnostic analgesia but in which no abnormality can be found radiologically and safety screening of an initially severely lame horse that has become sound before a diagnosis has been reached. Thus making a diagnosis in these horses at post mortem is avoided. Clients should be educated to not request the scintigraphic “fishing trip” as a first line of enquiry.
Ultrasonography
Ultrasonography is the imaging modality of choice for investigating soft tissue injuries in the metacarpal and metatarsal regions (see Chapter 16). In the young TB affected with PSD, lesions are often subtle, with enlargement and bulging of the palmar border with consequent loss of the neat rectangular shape of the normal SL as the only finding.l Large anechogenic defects and obvious fiber tearing are not common.
The clinical relevance of bilateral enlargement of the superficial digital flexor tendons along with intratendonous edema in a 2-year-old may be difficult to interpret because normal tendons increase in size in response to training10 (see Figure 99-2). If obvious distortion of the contour of the tendons exists, I advise that the horse not gallop or race at 2 years of age. The horse is maintained in alternate-day trotting and cantering for 3 months. This treatment has not led to true tendonitis at 3 years of age in any horse. I refer to these horses as having juvenile tendonitis but have never been comfortable that this degree of caution is mandatory. Perhaps these horses could do more work without further injury.
Ultrasonography is also useful for detecting and monitoring some fractures of the ilial wing and shaft and ischium of the pelvis (see Chapter 49).
Diagnostic Analgesia
Having carried out the clinical examination described, one structure causing lameness may be obvious. For example, the horse may show a sharp pain response on palpation of the SL or distention of the middle carpal joint capsules with pain on flexion. Diagnostic analgesia may not be necessary in these horses, and diagnostic imaging of the site may be the next step. Many horses have a list of diagnostic possibilities: the horse may have shown a pain response to hoof testers and some tenderness to palpation of the SL and have some distention of the middle carpal joint capsule. To tease apart these findings, diagnostic analgesia is mandatory. Diagnostic analgesia is done most efficiently at a clinic rather than a training yard because the procedure is time consuming. If a horse is fresh when admitted for diagnostic analgesia, the increase in muscle tone and general excitement can obscure a mild lameness, and acetylpromazine (2 to 5 mg/horse intravenously) can help settle the horse without affecting its ability to trot.
If the horse is admitted to a clinic for a day, a positive block can be allowed to wear off, so that more localized blocks can be carried out. For this reason, my own first block in a forelimb is usually biaxial palmar digital nerve blocks so that the foot can be eliminated or investigated in greater detail later. Many horses with mild lameness exhibit a detectable worsening of the degree of lameness if the foot is desensitized and is not the source of pain, which can be useful when investigating intermittent or low-grade lameness. I used to first perform palmar (abaxial sesamoid) blocks, but I increasingly found that this often abolished pain from the fetlock or the distal metacarpal or metatarsal regions and thus was not reliable as an indicator of primary foot pain.
If lameness is abolished using palmar digital analgesia, a more detailed investigation of the foot and distal extremity is carried out, perhaps with the shoe removed. If effusion of the distal interphalangeal joint is present, an intraarticular block is performed. In rare instances, palmar digital nerve blocks will abolish pain later proven to originate from the distal condyle of the McIII or the MtIII; therefore this should also be checked by intraarticular analgesia of the fetlock joint if the subsequent block results do not make logical sense.
If the horse is unchanged after palmar digital analgesia, a low palmar and palmar metacarpal (four-point) block is used. This may alleviate lameness; not improve lameness, indicating the problem is much higher; or give a 30% to 50% improvement in lameness, which is observed commonly in horses with PSD. However, recently I have become aware that horses with severe, advanced subchondral bone sclerosis and injury of the distal aspect of the McIII/MtIII seen on MRI may not be rendered completely sound by either a low four-point block or intraarticular analgesia of the fetlock joint, although the lameness may be substantially improved by both. There is a danger if one assumes that a 50% improvement in lameness following a low four-point block, followed by total soundness after a subcarpal block indicates that the origin of pain is in the proximal aspect of the SL or the McIII. This block response may divert attention away from the actual site of pathology in the fetlock.
The next logical step is the subcarpal block, which I perform using 1.6-cm needles and 2.5 mL of mepivacaine in the recess immediately palmar to the top of the second and fourth metacarpal bones. Short needles and small volumes of local anesthetic solution are used in an attempt to reduce the frequency of false-positive analgesia of the middle carpal joint. False-positive responses can occur by inadvertent direct penetration of the distopalmar outpouchings of the carpometacarpal joint11,12 or by diffusion of local anesthetic solution up the fascial planes to a site proximal to the middle carpal joint.
A positive subcarpal block is always allowed to wear off, and the middle carpal joint is blocked subsequently to ascertain which site is responsible for the pain causing lameness. Unfortunately, in some horses complete soundness follows both the middle carpal joint and subcarpal blocks. When this occurs, ultrasonographic examination of the proximal aspect of the SL and a radiographic examination of the carpus are performed before an informed guess is made about the most likely source of lameness. If no lesions are found after imaging both sites, defining the source of pain categorically may not be possible, and the horse is a candidate for nuclear scintigraphy. MRI is also proving extremely useful in unpicking the complexity of lameness in this site.13 I avoid using the lateral palmar nerve block because in my hands it is too nonspecific and has abolished lameness that originates from the SL, proximal aspect of the McIII, and both joints of the carpus on occasions. In an experimental study, no penetration of the antebrachiocarpal and middle carpal joints occurred as a result of lateral palmar analgesia, although commonly the carpal synovial sheath was penetrated (Editors).12
Negative subcarpal and middle carpal analgesia are followed by median and ulnar nerve blocks. Although these blocks leap-frog the antebrachiocarpal joint, median and ulnar nerve blocks usually abolish lameness associated with lesions of this joint. Intraarticular analgesia of the antebrachiocarpal joint may fail to abolish pain associated with chip fractures of the distal aspect of the radius in some horses.14 The jump directly to median and ulnar blocks avoids the possibility of false-negative responses misleading the lameness diagnosis.
Negative median and ulnar blocks usually are followed by advice to carry out scintigraphy because scapulohumeral joint lameness is relatively rare and intraarticular analgesia does not alleviate lameness associated with humeral stress fractures, which are common. Although OCD and osseous cystlike lesions of the scapulohumeral joint are found in late yearlings and early 2-year-olds, these often show scintigraphically and can be confirmed later by radiological examination and diagnostic analgesia if necessary. Intraarticular analgesia of the elbow and scapulohumeral joints is performed if the median and ulnar blocks and scintigraphy fail to establish the seat of pain causing lameness. However, it has been my experience that intraarticular analgesia of the elbow joint can on occasion abolish lameness later proven to have originated from a site more distal in the limb, presumably by diffusion of local anesthetic solution from the joint in proximity to the median nerve; therefore a positive elbow block may need to be interpreted with caution.
Hindlimb investigation follows a slightly less rigorous approach for three reasons:
Shoeing Considerations
TB racehorses have notoriously bad horn quality and hoof conformation. They appear to have uniformly thin soles and a tendency to develop long toes and low heels. Medial to lateral hoof balance is vital to the TB racehorse remaining sound, but it is sometimes not pursued adequately. All horses should be shod wide at the heel to allow full weight bearing by the horn structures. However, in racehorses this tends to produce an abundance of pulled shoes by the trapping of the metal of one shoe underneath the other foot in the stable, particularly on rubber floors, which do not allow the trapped shoe to slip out. This encourages farriers to tuck the shoes out of reach under the foot, which leads to progressive collapse of the heel and long-toe, low-heel conformation. Farriers have to be reassured that they will not be held responsible for pulled shoes within the stable and that the health of the horse’s foot is more important than the management problems sometimes associated with correct shoeing.
Interference injuries are not as common in the TB as in Standardbreds and are more common when horses are on a reduced exercise plane or in 2-year-olds in early training. Interference injuries seem to become less common as the horse strengthens and becomes more fit. In every horse such injuries should be approached as a joint exercise, with the full involvement of the farrier. Interference injuries, such as scalping, that suddenly begin to occur regularly in a horse previously unaffected can be an early sign of gait alteration reflecting pain, and the horse’s action at the walk and trot should be carefully evaluated.
The following approaches may be helpful.
Brushing Injuries of the Hindlimbs
Hindlimb brushing injuries are caused by the contralateral foot in flight and produce cuts on the medial aspect of the fetlock or the proximal aspect of the pastern. Most of these horses toe out and are base narrow, and some swing the foot inward during protraction at walk and trot. Traditionally three-quarter round shoes have been used, with the medial branch missing. Over time, however, this shoeing results in progressive collapse of the medial hoof wall, pushing the limb even further out of line, and brushing may actually increase. An alternative is to use light steel or alloy plates behind. This lowers the weight of the foot and often stops the problem. If this fails, we use a 2-cm lateral trailer on the shoe. Half-round shoes are always a help because they remove the cutting edge if interference does take place.
Brushing Interference in the Forelimbs
Brushing in forelimbs is difficult to treat. Affected horses usually toe out considerably from distal to the metacarpophalangeal joint and are base narrow. Horses often first show interference when galloping at speed, and injury causes substantial hemorrhage and swelling over the medial PSB. This swelling then makes future interference even more likely, and a downward spiral begins. The steps I usually take involve careful correction of medial to lateral hoof imbalance by the farrier, rest and antiinflammatory treatment to reduce swelling, and application of closely fitted half-round section shoes. Topical application of dimethyl sulfoxide containing flumethasone is indicated unless there is an open wound. If a full-thickness skin wound is present, topical antisepsis and systemic antibiotic treatment may be indicated to prevent undue swelling at the site. Ultrasonographic examination sometimes reveals a subcutaneous seroma, which responds well to needle drainage and injection of a small amount of corticosteroids (dexamethasone, 2 to 4 mg).
Protection of the site of injury on return to training with a thin layer of cohesive exercise bandage can help, but great care should be taken in applying this type of bandage because the lack of padding can all too easily produce a bandage bow (bind). Even with all these measures, it is not uncommon for affected horses to suffer repeated intermittent problems throughout their careers.
Scalping, Forging, and Overreaching
Scalping, forging, and overreaching are produced by the hind foot arriving in the site occupied by the front foot too soon in the gait cycle.
Scalping produces cuts on the dorsal aspect of a hindlimb pastern, too dorsal to have been caused by the contralateral limb. Scalping is caused by the tip of the front shoe striking the front of the advancing hind pastern, as the horse just misses forging. Such injuries often are avoided by a four-point trim or shortening the toe and using a rolled-toe shoe in front to speed breakover fractionally, thus getting the front foot out of the way by the time the hind foot arrives. If this alone fails, then using a light steel or alloy plate with a square toe in front and heavy steel shoes behind often eliminates the problem. The same measures are used to reduce true forging, when the hind shoe strikes the tip of the front shoe, producing the characteristic steel-on-steel noise from which the name is derived. Forging can be more common when horses jog on a soft synthetic or sand surface, which “holds” the front foot and prevents its early clearance, and rolling and damping these track surfaces before use can help. Overreaching, when the hind toe strikes the bulb of the front heel, can be approached in the same way. Overreach boots can help but can only be used in slow work. Overreaching is most common when the horse is fresh and being restrained hard in its exercise or is being exercised in deep sand, preventing easy limb clearance. For this reason these horses can be helped by judicious use of mild sedation before exercise (10 to 25 mg of acetylpromazine orally, 30 minutes before exercise) and by exercising on a nonimpeding surface. In many horses all these measures can cease as the horses become fully fit.
Ten Most Common Lameness Conditions
The following are the 10 most common lameness conditions; these are discussed in detail in this section.
Foot-Related Lameness
TB feet are usually thin soled, and most racing TBs have a pain response to hoof testers, even in the absence of genuine lameness. To minimize laminar bruising, good shoeing technique is essential, and horses should not be exercised on a surface that is too firm. Medial-to-lateral foot balance is also vital but often neglected. Farriers often are expected to shoe in the dark of the early morning, with the horse loose in the stable on deep bedding. This often leads to poor visual assessment of foot–pastern axis and balance. Clinicians should help farriers to change this attitude in favor of a system that allows these skilled professionals to achieve their potential. Such a change involves providing staff members to lead out and hold the horses for the farrier to inspect.
Bruising usually is diagnosed when the horse shows an exquisite pain response to hoof testers in a fairly localized area, but no obvious tract leading to the deeper structures. Careful paring with a hoof knife often reveals pink discoloration in the horn layers immediately above the area of the bruise. Removing the shoe and applying a poultice to the foot for a day is usually successful in managing this condition. If the horse is close to a race and time is of the essence, the foot is iced morning and night in an attempt to decrease the pain associated with the bruise. Once the pain is clearly found to be only from the bruising and no pus pocket has formed under the sole, poulticing is stopped to dry up the sole again before shoeing. If foot lameness is associated with infection, then draining the subsolar abscess is mandatory. Although traditional textbooks talk about radical curettage and establishing sufficient drainage, in the racing TB removal of too much horn is associated with an extended period of lameness because of laminar damage and pain from exposed soft horn. Initially the hole to the pus pocket should be as small as possible. Once drainage has been established, hoof testers can be used to expel pus and to pull in soaking agents or hydrogen peroxide. The hole often can be enlarged using a bent 16-gauge needle. The foot usually is soaked then in warm salt water for 10 minutes morning and night and in between is wrapped in saline-soaked cotton wool dressing contained within polyethylene. Walking these horses twice a day if the degree of lameness permits is a good idea to encourage extrusion of the pus, which leads to quicker return to full work and decreases the risk of rhabdomyolysis on return to training. Some infections within the foot are infuriating because although an exquisite pain response occurs and a clear penetration tract leads into the foot, blood in the sensitive laminae is reached before the infected focus is found. The horse then usually resents further digging in the sensitive laminae. Radiological examination is justified in these horses to rule out infectious osteitis of the distal phalanx, usually evident as a radiolucent area. This condition, if confirmed, is treated by radical curettage after sedation, local nerve blocks, and application of a tourniquet. A treatment (hospital) plate is then applied.
Traumatic corns can be one of the most frustrating conditions with which to deal. Affected horses usually have a long-toe, low-heel conformation and inwardly collapsing heel bulbs. Intense pain occurs when hoof testers are applied across the seat of the corn, and yet exploration simply reveals subsolar blood pockets or bleeding tissue. When these are exposed, localized prolapse of the sole may occur at the seat of the corn. These horses take a long time to regain soundness and normally are shod with a bar shoe to bridge the weight bearing from the nonaffected heel to the wall of the other quarter. The horse should be kept in walking exercise only for at least 2 weeks to allow some horn growth before an attempt at retraining. Training and racing on hard surfaces is contraindicated, which can be realistic advice in the United Kingdom. These horses may be more difficult to manage if sold to train on the tracks in North America. The farrier should be involved in attempting to bring up the heel angle in these flat-footed horses, and the four-point trim is often helpful in achieving this quickly. Medial-to-lateral balance should be checked because traumatic corns often occur on the lower aspect of a heel of a horse that has been allowed to become unbalanced. This seems to occur because of second contact concussion as the foot strikes the ground in a biphasic manner, which is corrected by lowering the longer side of the heel to make sure that the foot strikes the ground evenly.
Sometimes a breach in the horn at the seat of the corn allows infection to enter, producing an infected corn. The condition often is linked to swelling and pain or even discharge of pus at the bulb of the heel above the corn. Drainage, poulticing, and remedial shoeing are the standard treatments.
For lameness associated with the horse being pricked by the farrier, with or without development of infection, use of a glue-on shoe when the horse is reshod after the problem has been resolved is sometimes a good idea. Most farriers shoeing racehorses are extremely skilled, and if they have managed to puncture the sensitive laminae during a routine shoeing, the cause is usually because the horse has extremely little wall outside the white line. The direct glue-on technique, using a normal alloy racing plate stuck directly to the sole without nails, allows the horse 3 to 4 weeks of extra horn growth before further nailing is done. The more traditional tab-glue shoes are less satisfactory because the shoes tend to become loose and the horse’s foot shape may change. This is not the case with direct glue-on shoes. Horses that repeatedly lose shoes and have increasing wall avulsion and damage are treated best using direct glue-on shoes to allow time for wall recovery. More recently another type of glue-on shoe has been developed by farrier Rob Sigafoos (the Sigafoos shoe). This is constructed incorporating a collar of strong synthetic fabric into the structure of the shoe, which is glued directly to the dorsal wall of the hoof. The advantages with this shoe are that the heel bulbs are not bound in and can expand over the shoe, and that the shoe can be set properly under the foot in a normal position. Horses have trained and raced with success in these shoes.
Suspensory Desmitis
The forelimb SL can be injured at any location, but PSD is most common in a young racehorse. PSD is often bilateral, although the lameness observed is almost always unilateral. PSD is characterized by weight-bearing lameness of grade of 1 to 3 of 5, which seems to disappear rapidly after periods of rest. Even 24 hours of box rest often renders these horses sound. However, within an exercise period, the lameness is typified by becoming worse the more the horse does (warms into the lameness). Horses with PSD often show pain when the SL is squeezed between the thumb and the back of the McIII with the limb flexed. The veterinarian should start at the apex of the PSB and work along the SL, squeezing it against the bony structures of the limb. The response should be compared with the contralateral limb. Most normal young TBs show some degree of tenderness to palpation of the SL, although unbroken and untrained horses of the same age usually do not. This may indicate that many racehorses suffer a degree of PSD during early training in the absence of observable clinical signs. Lesions of the origin of the SL can be present without pain on palpation because it is difficult to apply accurate digital pressure in the proximal metacarpal region.
Local analgesia is discussed on page 1001. When performing subcarpal analgesia, the needles should be applied to the syringe before injection to prevent the introduction of air into the fascial planes, which can preclude later ultrasonographic examination. This air appears as a hyperechogenic band between the SL and the accessory ligament of the deep digital flexor tendon, obscuring evaluation of the SL.
The other common predilection site for injury of the SL is the interface of the distal aspect of a branch and the ipsilateral PSB. These lesions usually occur when the horse starts fast exercise. In horses with conformational defects, the same site can be affected in both forelimbs. For example, in a horse with offset carpi and toed-in conformation, the lateral branch of the SL and the lateral PSB are affected. Typical radiological changes of sesamoiditis are seen with clear disruption of the SL/PSB interface. Central hypoechoic lesions are identified by use of ultrasonography, along with irregularity of the PSB surface and even fragment avulsion. The SL branches often are enlarged palpably, but ultrasonographic imaging often reveals this to be a zone of periligamentous fibrosis, rather than true swelling of the branch itself.
Horses with PSD are confined to box rest for 2 to 4 weeks until clinically sound and then walk on a horse walker for 4 to 6 weeks, followed by 1 month of walking and trotting exercise. Ultrasonographic reassessment is recommended to determine whether the horse should start alternate-day cantering exercise or continue trotting for another month. Horses with distal branch lesions may have a guarded prognosis if substantial sesamoiditis exists. Most of these horses are taken out of training altogether as 2-year-olds and given the same rest program as horses with PSD. At the end of the period of controlled exercise, the horse usually is turned out and brought back in at the end of the year for further education, before resuming training as a 3-year-old. This distal branch/proximal sesamoid bone surface interface lesion is one of the few clinical situations in which I have been convinced that extracorporeal shock wave therapy (ESWT) has improved prognosis and reduced reinjury rate. I use weekly treatments of 3000 to 4000 shocks using a dual lithotripsy machine in ballistic mode at 4 Bar for 6 weeks in conjunction with controlled exercise.
Most young racehorses with PSD have an increase in the dorsopalmar thickness of the proximal aspect of the SL to greater than 1 cm, and irregularity of contour, with bulging of the normally flat palmar border (palmar bowing), detectable by ultrasonography. The fiber pattern may be heterogeneous. Ultrasonographic monitoring of these lesions may reveal a decrease in size of the SL, with more linear borders as healing progresses. However, in many horses, the SL never returns to normal. Exercise level is increased when the ligament shows good echogenicity, although it still may be enlarged. Some horses seem to have long-term hypoechoic lesions within the SL that do not change with further rest.
Less commonly, a unilateral, acute, focal core lesion occurs in the SL after a race or gallop associated with lameness, swelling in the subcarpal region, and an exquisite pain response to palpation. Occasionally the SL seems to split, with the most dorsal surface being linearly avulsed, presumably by fluid or hemorrhage. This results in considerable thickening and striation of the SL.
The prognosis for mild to moderate PSD in 2-year-old TBs is good, but the prognosis is more guarded in horses with acute core injuries. Some of these horses take 4 to 5 months before they are able to withstand training and have a risk of reinjury. The prognosis in older horses is also guarded to poor.
In a 3-year-old horse that had PSD at 2 years of age, mild lameness may recur as training speed increases, in the absence of any real changes that can be identified using ultrasonography, radiography, or scintigraphy. This lameness always can be abolished by subcarpal analgesia. These horses with subcarpal “ache” often can be managed by administration of 5 to 10 mg of triamcinolone acetonide in 3 mL of local anesthetic solution, injected in the same site as a subcarpal block. Lameness often is abolished for long periods after this treatment, without apparent degeneration of the SL, even with continued training. It is vital to complete a full diagnostic evaluation before treatment in these horses to eliminate the possibility of training horses tolerating incipient catastrophic lesions under the influence of corticosteroids. For those working under jurisdictions that do not allow the presence of drugs at race time, such as in the United Kingdom, clinicians should be aware that the detection period for triamcinolone acetonide at this site can approach 30 days, and shorter-acting agents such as dexamethasone may be preferred.
Fetlock Lameness and Subchondral Bone Injuries to the Distal Aspect of the Third Metacarpal/Metatarsal Bone
All racehorses begin training when they are skeletally immature and relatively weak, and this leads to frequent damage to the pressure points on either side of high motion joints. Lameness can result from impingement lesions at the site of contact between the distal extremity of the McIII and the proximal eminence of the proximal phalanx as the fetlock sinks in hyperextension. Lesions include damage to the cartilage, synovitis, osteochondral fragmentation, or very often a combination of all three. The typical early sign is of a distended fetlock with pain on flexion and a mild degree of lameness. Radiological examination often reveals new bone at the proximal extremity of the sagittal ridge of the McIII and remodeling or minor fragmentation of the proximal eminence of the proximal phalanx. We should resist the temptation to “fix” these joints in a 2-year-old by intraarticular medication because heat and inflammation tell us that the joint is having problems. These horses need some time. External application of ice, in conjunction with reduction of exercise to jogging for a couple of weeks, with or without the use of oral NSAIDs, gives these horses some chance to recover. The treatment may need to be repeated two or three times before the horse can train without trouble. There is often substantial pressure to keep such horses in training, with a request for intraarticular corticosteroid treatment. We all succumb to this pressure on occasion, but we should always point out to the trainer and owner that after corticosteroid administration, any healing processes will cease for a considerable time. The pain response, which is protecting the joint from overuse, will also be abolished or diminished, allowing more damage to occur. There will be a price to be paid later in the horse’s career. In an older horse, ongoing OA can often be traced back to an early interventional therapy, followed by a cycle of continued intraarticular treatment. There is often an ever-diminishing response to treatment until there is an end-stage joint with cartilage wear, fibrillation, or collapse, along with severe pathological change in the subchondral bone.
Subchondral bone injury is an extremely common cause of lameness in young TBs and is vastly underacknowledged. Subchondral bone pain seems to be increasingly implicated in much joint-related lameness in other classes of horses (e.g., navicular syndrome, tarsal pain, and third carpal bone pain). In the young TB, subchondral bone injuries in the distal aspect of the MtIII and the McIII often are linked to bilateral or quadrilateral lameness, which limits performance. Horses with bilateral subchondral bone injuries of the distal aspect of the MtIII fail to push from behind at exercise. Often these horses appear to bunny hop for the first section of canter. The rider reports that the horse feels wrong behind and does not perform as well as it previously did. The clinical history (see page 997) and response to diagnostic analgesia (see page 1001) have been described. With American-bred horses, equine protozoal myelitis (EPM) is an important differential diagnosis because the clinical appearance can be similar. Onset of clinical signs can be delayed, so that a yearling bred in America and sold in Europe could have EPM.
Subchondral bone injuries are extremely difficult or impossible to identify radiologically. If lesions are visible radiologically, these are usually end stage, and horses warrant a guarded prognosis (see Figure 107-5). These lesions usually represent necrosis and collapse of subchondral bone and are visible as a crescent-shaped radiolucency in the middle of the lateral condyle of the MtIII, seen on flexed plantarodorsal or flexed dorsoplantar images (see Figure 107-4, B). Increased radiopacity of the lateral condyle also occurs and is most visible on a lateromedial image. Deliberate overexposure may be necessary to demonstrate a triangular region of increased radiopacity just palmar/plantar to the midpoint of the articular surface (Figure 107-7). All racing TBs seem to develop some degree of sclerosis in this site as a normal physiological response to loading from the PSB as the limb assumes full extension. MRI examination reveals changes associated with dense mineralized subchondral bone and sometimes focal areas of increased signal intensity in fat-suppressed images, which may reflect microfracture, fibrosis, or bone necrosis (see Figure 107-6).

Fig. 107-7 Post mortem specimen of the distal aspect of a third metatarsal bone from a horse with plantarolateral focal increased radiopharmaceutical uptake seen on a bone scan. Lateral is to the left. The specimen was collected when the horse was euthanized for unrelated reasons. The area in the center of the plantarolateral aspect of the condyle is dark, and the cartilage surface is irregular (arrows). Histopathological sections cut through the site revealed abnormal irregular and necrotic subchondral bone. Compare with the lesion in Figure 107-5, C.
On scintigraphic examination, these stress injuries are remarkable because increased radiopharmaceutical uptake (IRU) is focal in nature and markedly increased. On a plantar image, IRU in the MtIII is mistaken easily for IRU in a PSB because the shape of the lesion is similar to that bone. However, on a lateral image, the PSBs can be seen clearly plantar to the region of the IRU, localized within the condyle itself (Figure 107-8). In the forelimb, subchondral bone injuries in the metacarpophalangeal joint seem to occur most commonly in the medial condyle, but can also be present in the lateral condyle or both. Horses usually have bilateral lameness and trot with the head held low with a short, stumbling gait as they try to get off each weight-bearing limb as fast as possible. If all fetlock joints are injured, a horse may refuse to trot and attempt to break into a slow, rolling canter as speed increases. Lameness often becomes apparent in the contralateral limb after local analgesia of one metacarpophalangeal/metatarsophalangeal joint. Radiological examination is often unremarkable, but scintigraphy confirms focal IRU in an active early lesion. Use of flexed dorsal and flexed lateral scintigraphic images is helpful in pinpointing the exact location of the lesion, particularly in the front limb (see Figure 107-8). In the more chronic stage, there may be only mild IRU, yet the pain and lameness can be more intense. We should not forget that the mere presence of mild IRU does not necessarily mean painful and vice versa.
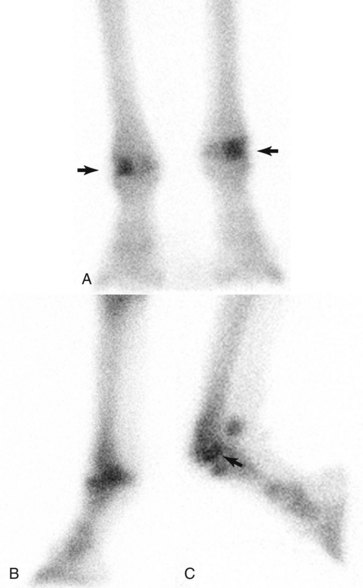
Fig. 107-8 A, Plantar delayed (bone) phase scintigraphic image of horse with bilateral stress injuries to the lateral condyle of the third metatarsal bone. The shape and distribution of the increased radiopharmaceutical uptake (IRU; arrows) easily can be mistaken for that associated with the lateral proximal sesamoid bone (PSB). B, Lateral delayed (bone) phase scintigraphic image of the same horse. If there is doubt as to the exact location of the IRU, a flexed lateral image (C) is useful in moving apart the PSB and the plantar aspect of the lateral condyle. This clearly shows the IRU to be situated in the plantar aspect of the condyle (arrow) rather than the PSBs, which are moved away from the joint in this image.
(Courtesy Sue Dyson, Animal Health Trust, Newmarket, England.)
Treatment is difficult, and we have no protocol that results in uniform resolution of lameness. Many different treatment regimens have been used, including intraarticular injection with hyaluronan or corticosteroids; systemic medication with isoxsuprine, aspirin, polysulfated glycosaminoglycans, or tiludronate; and rest alone.16 Often the lameness disappears rapidly after the instigation of rest but returns when the horse resumes fast galloping speed. Although some horses have been able to perform without further problems, predicting which horses may respond favorably is not possible. However, those with subchondral lucency and sclerosis rarely remain sound. This does not mean that these horses cannot perform, and many racehorses seem to withstand training despite lameness. However, this may be a performance-limiting problem that directly interferes with racing ability and determines the level at which the horse can compete.
Because horses with advanced lesions rarely return to sustained soundness, it is advisable to stop hard training as soon as the condition is noted in a 2-year-old and allow 3 months of rest. This is not a guarantee that the problem will not recur at 3 years of age, but going on with training these young horses in the face of this lameness seems illogical. Many horses can be trained at 3 years of age without problems. When the clinical syndrome appears in a horse aged 3 or more for the first time, the prognosis is much worse than when subchondral bone lesions occur in a 2-year-old and the horse is allowed to rest. In an older horse, end-stage pathological damage in the affected condyle is more common. These horses may well have been trained through the problem at 2 years of age, with a low-grade bilateral lameness that was not recognized.
Some horses first show hindlimb lameness associated with the lesions in the lateral condyles of the MtIII after a race on unsuitably firm ground. They are described as “jarred up.” Although the clinical appearance of a jarred-up horse has long been recognized, no precise definition of the syndrome has ever been made. The syndrome may well represent multifocal subchondral bone pain. Affected horses may never regain normal action. The reasons why some horses become progressively lamer whereas others can race with success and maintain a steady-state lameness are not understood.
A few horses with subchondral bone injury have been examined at post mortem (see Figure 107-7). The degree of damage to the subchondral bone at the injury site easily explains why some horses are untrainable. We need to understand why some horses develop these lesions whereas others do not, whether the type of training surface may be a predisposing factor, what pathological mechanisms are involved, and why these lesions produce pain. Ideally, we also need to track some young TB horses using repeat MRI scans from the time they are broken right through training to see when these lesions develop and what impact they have on gait and race performance.
Lameness Associated with the Middle Carpal Joint
Several distinct syndromes are associated with the middle carpal joint. One of the most common syndromes is exemplified by a 2-year-old in early training that develops an increasingly short, choppy gait at the trot. The limbs are held abducted during the protraction phase, and the carpi are barely flexed. This gives a stiff, rolling action. Often the horse has bilateral middle carpal joint effusion and pain on carpal flexion. Injection of local anesthetic solution into one middle carpal joint produces lameness (grade 1 to 2 of 5) in the contralateral limb. The gait changes so that the desensitized limb is often brought back toward the midline. Some of these horses have mild increased radiopacity of the third carpal bone, seen on a skyline image, but others have no detectable radiological abnormality. These horses probably are suffering from pain produced by concussion of immature cartilage and excessive torsion on untrained ligaments within the carpus, and should be given rest. If excessive effusion occurs, the joint may be drained and medicated with triamcinolone acetonide (5 mg) and hyaluronan, but only if rest is to follow. Nonsteroidal antiinflammatory drugs (NSAIDs) may be administered for the first 4 or 5 days of rest. Most horses are restricted to box rest for 1 month, followed by walking exercise for 2 weeks, followed by 1 month of trotting before resuming full training. Many horses never show lameness again during the second introduction to exercise loading.
The second syndrome, which may include some horses in the first category if training has continued, involves development of more severe sclerosis in the third carpal bone and remodeling of the distal aspect of the radial carpal bone. Focal overloading of the third carpal bone results from a conformational defect (offset carpi with toe in is the worst) or from a mismatch between loading of the limb and time allowed for adaptation. These horses are usually bilaterally lame; often one lame limb dominates, and contralateral limb lameness is only recognized when the lamest limb is blocked. Radiological signs include increased radiopacity in the radial fossa of the third carpal bone seen on the skyline image, associated with local areas of rarefaction around the nutrient foramina or with small comma-shaped fissure fractures extending from the dorsal aspect of the third carpal bone. Further training of these horses risks development of a full sagittal fracture (see Figure 107-2).
Despite statements to the contrary in the literature, I believe that the early sclerotic changes in the third carpal bone are reversible after a period of box rest. However, there seems to be a certain degree of pathological damage from which there is no return. Once the radial fossa becomes completely devoid of trabecular detail and has a “ground glass” appearance radiologically, the changes are often permanent. These lesions often are associated with recurrent lameness each time the horse reaches racing speed. Therefore identifying increased radiopacity of the third carpal bone at an early stage is vital. Screening radiographic examinations of the third carpal bone in a 2-year-old may be useful before starting full race-speed galloping. Without radiological information, lameness may be the first indicator of sclerosis, which may already be advanced.
Lame horses with third carpal bone sclerosis are confined to box rest for 2 months, followed by 1 month of walking exercise. Radiographic examination is then repeated. I advise that these horses are not trained with a view to racing at 2 years of age, although they may reenter the training environment so that they acclimatize to respiratory disease and other management problems that might influence the 3-year-old career.
Problems related to the distal aspect of the radial carpal bone are also common, associated with lameness and distention of the middle carpal joint capsule. Radiological abnormalities include spur formation on the distal aspect of the radial carpal bone and radiolucent changes in the same site leading to modeling of the dorsal margin. This usually leads to or is associated with coexistent secondary sclerosis of the opposing third carpal bone because the load becomes borne by the medullary bone, instead of the weight-bearing pillar of the dorsal cortex. These radiological abnormalities result from overloading the carpus, leading to bone stiffening, cartilage damage, and secondary OA. Debate exists over whether spurs should be removed surgically. OA of the middle carpal joint is already established. Although removing the spur is logical, it is not curative, and the horse will still require treatment the following season. With cheap horses and in yards where money is tight, many horses with mild carpal OA can be treated once by intraarticular medication with hyaluronan and triamcinolone acetonide, followed by 4 to 6 weeks of rest and a graded return to exercise.
If a chip fracture occurs, then removal of the fragments is probably still mandatory. One should explain to the owner and trainer, however, that the horse has preexisting OA that will persist after surgery and that further problems should be anticipated the following season.
The antebrachiocarpal joint is more forgiving than the middle carpal joint in the amount of pathological change that can be seen radiologically in the absence of clinical signs. Large fragments can be removed surgically with a favorable prognosis for horses the following season. Some horses can continue to train and race without obvious impairment even with chip fractures left in situ in this joint.
A small group of horses with middle carpal joint pain remains in which lameness recurs after periods of rest, despite absence of radiological changes. These horses often have unilateral lameness associated with middle carpal joint effusion. Some of these horses have tears of the palmar intercarpal ligaments. Response to conservative treatment often is disappointing, and even after prolonged periods of rest, lameness recurs as soon as work intensity increases. I normally medicate these horses with hyaluronan and corticosteroids, but in the absence of a firm diagnosis, this empirical treatment is illogical and usually unrewarding. Diagnostic arthroscopy probably is always indicated in these horses but is also often unhelpful in producing a permanent cure. We should also always be aware that local anesthetic solution in the middle carpal joint can abolish pain arising from the SL, carpal ligaments, and many other structures, and it may be very simplistic to assume a positive middle carpal joint block means we have problems only in the middle carpal joint. MRI examinations of some of these horses have been carried out recently and reveal a catalog of abnormalities in structures all around the site of the block.13
Lameness Subsequent to Bacterial Infection
Bacterial infection in a limb of a horse can cause a degree of pain greater than almost any other injury, including a displaced fracture. Although wounds in any part of a limb can become infected, leading to an obvious swelling and lymphangitis, some discrete syndromes in the racehorse deserve mention.
Staphylococcal Abscesses on the Palmar Aspect of the Metacarpophalangeal Joint
Horses exercising on sand, synthetic, or wood chip surfaces seem to be prone to bacterial infections around the ergot that produce small, focal abscesses, which can be difficult to find if the horse has a winter coat. The horse often initially points the limb, is severely lame (grade 4 of 5), with swelling on the palmar aspect of the metacarpophalangeal joint. Manipulation of the joint is resented. The abscess can mimic the appearance of an infected joint and must be differentiated because synoviocentesis inadvertently may introduce infection into the joint. Careful evaluation shows that the metacarpophalangeal joint capsule is not distended. By working through the hair coat with the fingernails, localizing the point of a small abscess is often possible. The horse shows a severe pain response, and a pink porelike hole may be observed discharging serosanguineous pus. Bacteriological culture almost invariably results in the growth of a hemolytic Staphylococcus aureus.
Treatment is by external application of kaolin paste or a similar open poultice, combined with systemic antibiotic therapy along with NSAIDs and forced walking exercise. Horses are normally sound after 12 to 24 hours, and if this is not the case, then the diagnosis should be reestablished. Bandaging should be avoided because the limb often continues to swell and the bandage may become constricting, which can lead to ischemic necrosis and sloughing of the skin.
Focal Peritarsal Cellulitis
Focal peritarsal cellulitis is a syndrome that appears to be related to the architecture of lymphatic drainage and is characterized by acute-onset severe lameness (grade 4 or 5 of 5), often with a shocklike state, hyperventilation, and sweating.16 Rectal temperature is elevated (39 to 40° C). Clinical examination of the limb reveals an exquisitely painful area on the dorsomedial aspect of the hock with focal swelling (Figure 107-9). Brushing this area lightly with the fingertips usually causes the horse to stagger sideways and abduct the limb sharply to get away from the pain. Almost always a small skin lesion of some sort is evident in the distal part of the limb, through which the initial infection may have entered.

Fig. 107-9 A horse with focal peritarsal cellulitis. There is tight focal distention caused by swelling associated with infection in the deep fascia beneath the skin, retained at either extremity of the tarsus by the retinacular ligaments. This produces a profound degree of pain for the horse.
Although the horse is severely lame in the stable, if forced to walk, the lameness usually improves after a few steps, and the horse bears weight reasonably well. The focal swelling on the medial aspect of the tarsus appears to be linked to a nidus of lymphatic drainage because the swelling is so consistently positioned. The pain is so great because of involvement of the retinaculum and fascia immediately above and beneath the site, causing a compartment-like syndrome. Some North American clinicians describe emergency surgical drainage of these abscesses, with or without fasciotomy. However, conservative treatment using antibiotics (oxytetracyclines or ceftiofur), along with NSAIDs administered morning and night, and forced exercise several times daily is usually adequate.
Often within 24 hours the swelling changes from a small egg-sized swelling on the medial aspect of the hock to involve the entire distal part of the limb. Swelling gradually resolves with exercise over the next month.
A great risk of laminitis in the contralateral limb exists in the early stages because of the combination of severe lameness in the affected limb and toxin production from the abscess. Therefore it is vital that the horse is stabled on deep bedding during its initial treatment and that regular exercise is encouraged despite obvious lameness in the affected limb.
Axillary and Scrotal Intertrigo Infections
Horses are affected by skinfold infections, particularly in the axilla and groin. The infection begins in the fold of skin and causes an exudative, purulent dermatitis. The swelling of the affected region results in more occlusion and development of anaerobic infections deep in the skin folds. Affected horses often stand with the limb abducted and appear as if they have a proximal long bone fracture. Because the swollen skin folds close themselves off, these lesions can be missed unless the limb is pulled away from the body to expose the raw pink exudative dermatitis. Treatment is by systemic administration of antibiotics and analgesics and topical cleansing of the affected area with a debriding agent, followed by application of an antibiotic ointment. Fusidic acid creams are often effective because most of these infections involve staphylococci. Topical treatment often requires profound sedation of the horse so as to be carried out safely because of the pain involved. Exercise should be limited to a short period of handwalking, until the edema of the skin folds of the axilla subsides, because walking produces friction that makes the condition worse. Less commonly the area between the scrotum and the medial aspect of the thigh can be involved, especially in horses exercising on dirt or sand. Affected horses walk in a crouching gait, with abduction of each hindlimb during protraction. Once the acute infection has resolved, daily use of a talcum powder designed for use in babies is helpful in avoiding recurrent chaffing of the edematous skin during exercise for the first couple of weeks.
Stress Fractures of the Long Bones and Pelvis
Post mortem studies carried out on racehorse fatalities in California have revealed that many horses have evidence of previously undetected stress fractures of the long bones. We have been aware clinically of these fractures for some time, particularly when they became complete and displaced in horses in training. With the advent of scintigraphy, the early diagnosis of these stress fractures increased.
Certain rules apply to all stress fractures in the TB. Fractures usually occur after repeated cyclical loading of bone over time rather than as an acute incident. Lameness itself may be acute in onset, as the bone reaches the stage where it can no longer bear weight and the cortex begins to collapse. However, because the lesions are chronic in nature, radiological signs that we tend to link to bone healing and remodeling, such as periosteal new bone formation, irregular ill-defined lucencies in the cortex, and occasionally cortical displacement, may be detectable at the onset of lameness. Because stress fractures result from repeated focal overloading, they tend to occur in predilection sites in the bone, reflecting the architecture of that bone and the manner in which weight is borne during locomotion. The repeatability of these sites makes looking for these injuries on radiographs more straightforward.
Skeletal bone seems to detrain almost as effectively as it can be trained. For this reason, any horse that has been removed from training for longer than 3 weeks should be given sufficient time to allow reconditioning of the skeleton on return to training. Stress fractures may occur in horses of any age if they have been removed from training for a period of more than 1 month and have been returned to cantering exercise too rapidly.
Periostitis of the Dorsal Cortex of the Third Metacarpal Bone (Sore or Bucked Shins)
Sore shins are a common problem in 2-year-old racehorses or in older horses that have not reached race speed previously or have had a long layoff. Most of these horses are not shown to a veterinary surgeon. The stable staff and trainers know how to recognize sore shins and treat them in a variety of traditional methods. It is advisable to restrict the horse to trotting until the area is no longer painful to light fingertip pressure with the limb flexed. The horse is then reintroduced to the exercise level one step beneath the level that produced the soreness. This speed is maintained for 1 month before increasing. If the shin soreness returns as speed increases, the cycle is repeated.
Rarely, more invasive therapy is required for horses that have three serial episodes and for which normal management strategies have failed. The shin is pin fired under local analgesia, and the horse is walked for 2 weeks and then trotted for 2 weeks before gradually increasing speed work. Freeze-firing is a local temporary neurectomy only and confers no long-term benefit. The shin is a barometer of what is going on in the rest of the skeleton, and when sore the shin indicates that the skeleton needs more time to adapt. Freeze-firing simply lets us ignore this and allows the horse to develop real damage elsewhere. This subject is controversial, and the views expressed here are not shared by all veterinarians.
Fracture of the Dorsal Aspect of the Third Metacarpal Bone
Fracture of the dorsal aspect of the McIII presents as an extension of the sore shin complex. When a true stress fracture (dorsal cortical fracture) is present, the pain to palpation usually is localized to one area rather than being distributed across the entire surface of the shin. Normally a periosteal callus is present at the site of the fracture, causing a bump on the surface of the McIII. Radiographic examination should include unorthodox lesion-oriented oblique images because the fracture lines are often extremely difficult to see, particularly in the acute phase of the injury. Horses are usually slightly lame, but continued training results in an increase in lameness after each exercise period, which reduces rapidly. A lame horse with focal periostitis that is painful to palpation should be considered to have a stress fracture at that site, even if the fracture is not visible radiologically. Treatment is by rest, which can include walking exercise. These injuries normally take about 1 month to heal, after which light training may begin, but 3 months should elapse before full training speeds are achieved. If the injury has progressed to a clear tangential fracture line in the cortex, some veterinarians recommend surgical drilling (osteostixis), or even screw insertion across the fracture line, to encourage healing. This has never been necessary in my experience. ESWT is also used to treat horses with this type of fracture, but its clinical efficacy remains to be proved. Normally early diagnosis allows full healing with conservative treatment alone.
Tibia
Stress fractures of the tibia are one of the most common causes of hindlimb lameness in 2-year-old racehorses in race training. In the seasonal racing calendar, when yearlings enter training in October or November, peak incidence of tibial stress fractures is in April or May as speed work increases. The tibia has three main predilection sites. The most common in naive horses entering training for the first time is the proximolateral cortex, 7 to 8 cm distal to the proximal articular surface of the tibia. Stress fractures in this site are visible radiologically as poorly defined callus, often associated with an oblique fracture line in the cortex itself. The second common predilection site, often seen in a 3-year-old or in a 2-year-old in more advanced training, is in the caudal distal cortex, 10 cm proximal to the tarsocrural joint. On radiological examination endosteal callus can be seen as a subtle sunburst of increased radiopacity extending forward from the caudal cortex on a lateromedial image. On a caudocranial image, a lucent line is usually visible, surrounded by an area of increased radiopacity in the middle of the distal aspect of the tibia. The third common site is the middle of the medial cortex. In this site, the injuries usually are seen as periosteal and endosteal new bone formation only, and fracture lines are visible only rarely.
Occasionally a complete, comminuted displaced fracture of the tibia can occur during racing or training. The prognosis in these horses usually is hopeless. In Newmarket complete tibial fractures occurring at exercise have almost disappeared following the advent of scintigraphy, suggesting that in the past some complete fractures were the end stage of chronic stress fractures, which are now detected early.
Diagnosis of tibial stress fracture is difficult because these injuries may not be affected by diagnostic analgesia. The typical history is of a 2-year-old being brought into faster speed exercise or of a 3-year-old that did not race at 2 years of age being prepared in the same way. The lameness is usually acute in onset and can be severe (grade 3 or 4 of 5) but usually diminishes rapidly with rest. Forced flexion of the hock and torsion of the tibia produce pain in horses with severe lameness (see Figure 107-3). Scintigraphy is ideal to confirm these lesions, but the degree of IRU seen in the middiaphyseal and distal metaphyseal sites is often mild, particularly if the horse is imaged early.
Treatment is by rest and a gradual return to training. The horse is restricted to box rest initially for 2 to 6 weeks depending on the severity of the radiological signs. Occasionally stress fractures of the tibia become complete and displaced during periods of convalescence after normal recumbency. The horse should be tied up by the head for the first 3 to 4 weeks if the weight-bearing ability of the tibia is severely compromised (for precautions, see Chapter 49). Less severely affected horses are exercised as soon as it is practical. If a treadmill or horse walker is available, horses can be walked as soon as clinically sound, allowing a total healing period of between 2 and 3 months. Trotting exercise can be included in the second and third months.
Humerus
A horse with a humeral stress fracture has acute-onset forelimb lameness with features of proximal forelimb pain. The horse walks with a short cranial phase to the stride and circumducts the limb in protraction. Substantial weight-bearing lameness is evident at the trot. Horses often drag the toe of the affected limb in the bedding during protraction in the stable. The lameness rapidly diminishes, and in 2 days horses may be sound, only to go severely lame again after return to exercise.
Two main predilection sites exist for humeral stress fractures. Scintigraphic examination is ideal for diagnosis. One site is on the caudal cortex just distal to the humeral head, about 5 cm distal to the weight-bearing surface. Loose periosteal callus usually is visible, with increased radiopacity of adjacent bone and occasionally incomplete tangential fracture lines. The other site is the cranial or, less frequently, caudal cortex of the distal aspect of the humerus about 5 cm proximal to the elbow joint surface. A focal sunburst of callus usually is visible on a mediolateral radiographic image, and a linear fracture line is sometimes seen. Treatment is as described for tibial stress fractures. Complete, displaced humeral fractures can occur in exercise, and horses have a hopeless prognosis.
Pelvis and Axial Skeleton
Fractures of the sacral wing of the ilium are often stress fractures and are described in detail elsewhere (see Chapter 49). Laminar stress fractures of the vertebrae immediately adjacent to the pelvis have been described.17 A full review of the scintigraphic appearance of stress fractures in the TB has been published.9 There is usually a unilateral lameness for which no other reason can be ascribed after routine diagnostic analgesia and survey radiography. Scintigraphic examination of these horses reveals focal IRU associated with the lumbar vertebrae on the same side as the lameness. Some horses simply show bilateral poor hindlimb propulsion, short stepping at the walk, and a hunched-up lumbar spine, coupled with poor performance without obvious lameness. Being certain that the laminar stress fracture is the cause of the reduced performance is difficult. However, if scintigraphy reveals an active bone injury in the spine, continuing full training cannot make sense, and these horses subsequently are allowed to rest. Although this lesion is described as widespread in the Californian pathological survey, the clinical presentation is uncommon. I have examined the lateral lumbar spine routinely in all bone scan images over a 2-year period and have not encountered the lesion as a common incidental finding.
Exostosis of the Second and Fourth Metacarpal/Metatarsal Bones (Splints)
Splints are more of a nuisance in a racehorse than a major problem. They are clinically obvious, and a sharp pain response can be elicited by squeezing the area. Splints normally are associated with lameness in the initial stages, although this can subside rapidly. Splint lameness is one of the few conditions with which lameness is often more obvious with the affected limb on the outside of a circle. Splints are common in horses of 2 years of age but can occur in horses of any age, particularly if they experience a change in loading because of a different type of training surface or, paradoxically, a reduction in training workload, or a different angle of camber in the surface on which they are training. In many horses a fracture line is not detectable radiologically, but most horses with obvious exostosis formation associated with lameness probably do have fractures within the body of the bone, which often can be identified scintigraphically. Many of these “splints” will continue to show marked IRU for months or even years after clinical signs have settled. A period of stable rest with walking exercise is probably indicated until the horse is clinically sound. The horse then can recommence trotting for 2 to 4 weeks to allow the injury to heal fully. If pain on palpation and lameness immediately recur when the horse returns to exercise, then pin firing may be considered to encourage more aggressive callus formation. This is one of the few orthopedic indications in which firing achieves a good clinical result in most horses. Horses with displaced fractures of the distal aspect of the second and fourth metacarpal/metatarsal bones are treated by surgical removal of the distal portion of the bone.
Numerous comminuted fractures of the second and fourth metacarpal/metatarsal bones sometimes result from external trauma and heal surprisingly well. Many fragments may be identified by digital palpation with a gloved finger through an open wound and confirmed radiologically. Most horses with fractures heal satisfactorily with antibiotic treatment, bandaging of the wound, and stable rest. If infectious osteitis does occur with sequestrum formation and recurrent fistulation, then affected bone should be removed surgically. Open comminuted fractures of the fourth metatarsal bone can lead to infection ascending into the TMT joint and should be closely monitored.
Undiagnosed Hindlimb Lameness
Despite all our modern diagnostic aids, the cause of hindlimb lameness in a large number of horses remains elusive. Given the huge muscle mass involved in the hindquarters of the horse, some must have muscular origin and insertion pathological conditions, as well as pain from muscular overexertion. In human athletes, lameness is commonly linked to strains, tears, and cramps in the semimembranosus and semitendinosus muscle groups and in the adductor and gluteal muscles. Horses are presumably no different. As yet, no definitive test appears to be available to confirm genuine muscle injury. Thermography is helpful in some horses but is disappointing in others, and only reflects changes in skin temperature. Increases in CK and aspartate transaminase levels, although pathognomonic for exertional rhabdomyolysis, do not seem to occur following genuine tears of muscle tissue. Presumably these tears result in little cellular disruption, the damage being more in the fascial planes and connective tissue.
If a horse remains undiagnosed after all available diagnostic analgesia and imaging modalities have been used, then the horse is confined to box rest with walking exercise only for 1 month. Most horses become sound in this period. The horse then returns to walking and trotting exercise for 1 month before resuming a normal ascending exercise program. Although admitting defeat and being unable to give a definitive diagnosis is frustrating, one should try to avoid attributing a definite cause for the lameness if no evidence exists to support it. Trainers and clients should be educated to accept the fact that ascribing lameness to injury of a specific structure in every horse is not possible.
Fractures of the Proximal Phalanx and Distal Condyles of the Third Metacarpal/Metatarsal Bone
The most dramatic example of a proximal phalanx fracture is a split pastern that is a frequent injury, particularly in a 2-year-old racehorse as it enters fast work. The length and configuration of these fractures include complete sagittal fractures involving both articular surfaces, multiple comminuted displaced fractures, and incomplete fractures extending short distances from the proximal articular surface. Diagnosis is usually straightforward in horses with a complete fracture or an extensive incomplete fracture. With extreme injury, a horse pulls up severely lame during or at the end of exercise. With less severe injuries, horses may finish exercise apparently sound but become increasingly lame on return to the stable. The horse is usually not bearing weight by the time of examination. Pain always occurs on flexion of the metacarpophalangeal or metatarsophalangeal joint and on pressure applied with the fingertips to the proximal phalanx along its sagittal dorsal midline. Radiological examination is usually confirmatory.
Short incomplete sagittal fractures of the proximal phalanx can be notoriously difficult to see radiologically, when the fracture line only extends 1 or 2 cm into the bone. Clinical signs are of a severe lameness (grade 3 of 5) that rapidly improves so that the horse may be sound within 2 days. Flexion of the fetlock joint is usually not painful. Firm squeezing of the proximal dorsal surface of the proximal phalanx usually is resented, particularly approaching the proximal articular surface, and this is a reliable clinical sign. A horse with this type of fracture should be given box rest for at least 2 weeks before further radiography. Short, incomplete fractures easily become complete comminuted fractures if a horse is exercised after 2 weeks of rest because the fracture weakens by normal osteoclastic activity. Therefore although the horse may be sound, a premature return to work may result in a catastrophic fracture. See Chapter 35 for a discussion of management of horses with fractures of the proximal phalanx.
Fractures of the condyles of the McIII or the MtIII are a frequent injury, but they occur more often in 3- and 4-year-olds than in 2-year-olds. The lateral or medial condyle can be affected, and fractures of the medial condyle of the MtIII often spiral proximally. The whole fracture may not be seen on one radiographic image, and several oblique images should be obtained to determine the extent of the fracture before contemplating general anesthesia for surgical fixation. Spiral fractures present a risk during recovery from general anesthesia.
A complete, displaced condylar fracture presents little diagnostic challenge. The horse is extremely lame and resents palpation of the lateral or medial condyle. Flexion of the metacarpophalangeal/metatarsophalangeal joint invariably is associated with sharp pain, and joint capsule distention and effusion usually occur because of hemorrhage. Short, incomplete condylar fractures are more difficult to diagnose. Lameness is usually severe (grade 2 or 3 of 5) and diminishes rapidly with rest. Horses often become lame again as soon as they are returned to cantering exercise. Diagnostic analgesia localizes lameness to the metacarpophalangeal/metatarsophalangeal joint, but nothing may be seen radiologically. A flexed dorsopalmar image is vital if these lesions are to be seen adequately.3 If radiography is performed in the field, using portable equipment, then an upright flexed image that moves the PSBs proximally is useful to identify the fracture4 (see Figure 107-4).
If a condylar fissure is suspected, the horse should be restricted to walking and trotting exercise for 2 weeks before follow-up radiography is performed. Many horses that eventually develop full, displaced condylar fractures are described as having been bad movers before injury, and almost certainly prodromal pathological damage contributes to the cause of these fractures. See Chapter 36 for a discussion of management of horses with fractures of the McIII and the MtIII.
Pain Associated with the Tarsometatarsal Joint
Sore hocks are probably much more common in the United States than they are in the United Kingdom. TMT joint lameness can be bilateral or unilateral and often does not resolve with rest, and the response to intraarticular administration of corticosteroids varies extremely. I treat horses with triamcinolone acetonide (10 mg) at the time of intraarticular analgesia to avoid having to reenter the joint. After this therapy, many horses are sound, and lameness never returns. However, other horses require intermittent repeated medication, and others will not respond at all. The withdrawal period for racing free of medication is probably longer for triamcinolone acetonide than many other corticosteroids and can be in excess of 20 days after injections of the distal hock joints in the United Kingdom.
Horses with bilateral lameness are more difficult to diagnose. Bilateral plantar stress injuries in the distal aspect of the MtIII should be eliminated first by diagnostic analgesia because the gait of affected horses is similar. If diagnostic analgesia is negative, local analgesia of one TMT joint should be performed in the hope that an obvious lameness will become visible in the contralateral limb. Care should be taken if medicating both TMT joints to avoid a laminitis-inducing dose of corticosteroid (i.e., no more than 20 mg of triamcinolone acetonide per horse). The very prolonged detection period of depot preparations of drugs such as methylprednisolone acetate virtually rules out the use of this drug in horses racing under European medication rules.