Lymphatic System
1 Define and pronounce the key terms and anatomic terms in this chapter.
2 List and discuss the lymphatic system and its components.
3 Locate and identify the lymph nodes of the head and neck on a diagram and patient.
4 Locate and identify the tonsils of the head and neck on a diagram and patient.
5 Identify the lymphatic drainage patterns for the head and neck.
6 Describe and discuss pathology of lymphoid tissue associated with the head and neck.
7 Correctly complete the review questions and activities for this chapter.
8 Integrate an understanding of the head and neck lymphatic system into clinical dental practice.
(ef-er-ent) Type of lymphatic vessel in which lymph flows out of the lymph node in the area of the node’s hilus.
(hi-lus) Depression on one side of a lymph node where lymph flows out by way of an efferent lymphatic vessel.
(lim-fad-in-op-ah-thee) Process in which there is an increase in the size and a change in the consistency of lymphoid tissue.
(lim-fat-ik) Larger lymphatic vessels that drain smaller vessels and then empty into the venous system.
Organized, bean-shaped lymphoid tissue that filters the lymph by way of lymphocytes and is grouped into clusters along the connecting lymphatic vessels.
Lymphatic System Overview
The lymphatic system is part of the immune system that consists of vessels, nodes, ducts, and tonsils. It helps fight disease processes and serves other functions in the body. Although not part of the lymphatic system, the thymus gland also works as a part of the immune system and is discussed in Chapter 7.
Lymphatic Vessels
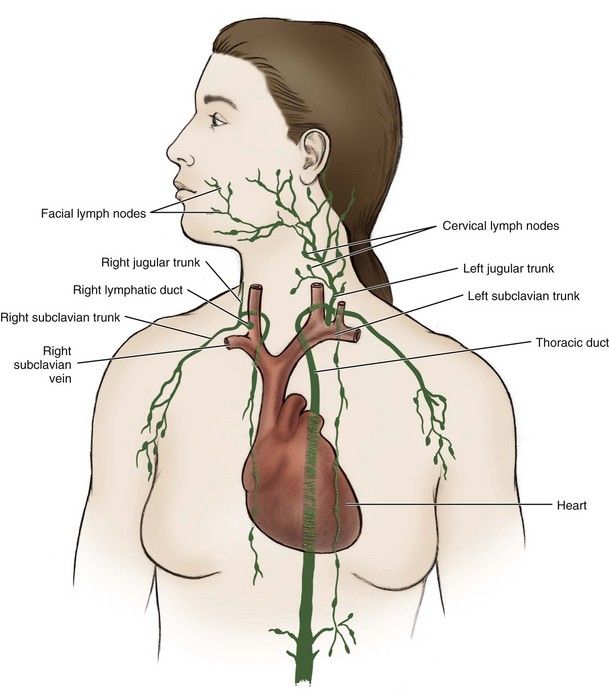
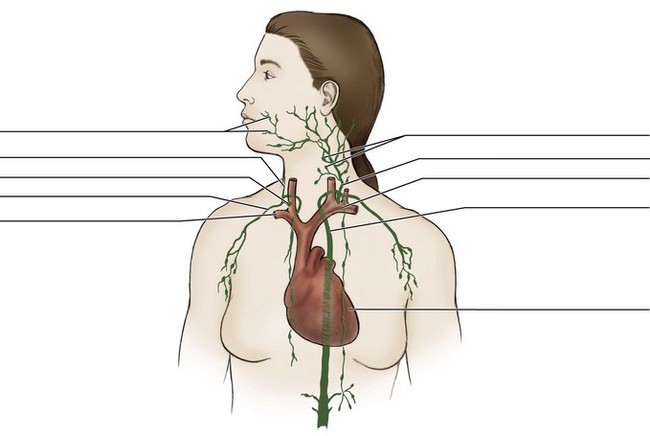
The lymphatic vessels are a system of channels that parallel the venous blood vessels yet are more numerous (Figure 10-1). Tissue fluid drains from the surrounding region into the lymphatic vessels as lymph. Not only do the lymphatic vessels drain their region, but they also communicate with each other. Lymphatic vessels are larger and thicker than the vascular system’s capillaries. Unlike capillaries, lymphatic vessels have valves similar to many veins. These valves ensure a one-way flow of lymph through the lymphatic vessel. Lymphatic vessels are even found within tooth pulp.
Lymph Nodes
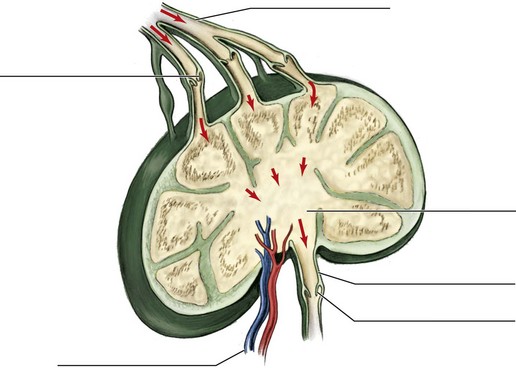
The lymph nodes are bean-shaped bodies grouped in clusters along the connecting lymphatic vessels (Figure 10-2). Along the lymphatic vessels, the lymph nodes are positioned to filter toxic products from the lymph to prevent their entry into the vascular system. The lymph nodes are composed of organized lymphoid tissue and contain lymphocytes, white blood cells of the immune system that actively remove toxins. The removal of the toxins helps fight disease processes in the body.
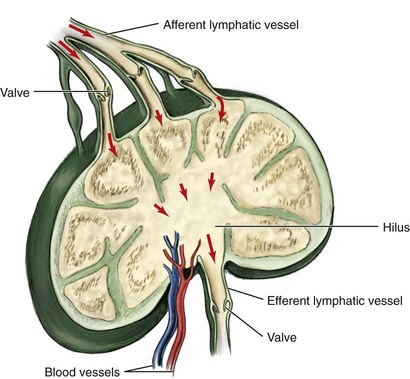
FIGURE 10-2 Lymph node and components showing flow of lymph into and out the node, with adjacent blood vessels noted (red, artery; blue, vein).
Lymph nodes can be superficially located with superficial veins or located deep in the tissue with deep blood vessels. Lymph nodes are named for adjacent anatomic structures. In healthy patients, lymph nodes are usually small, soft, and free or mobile in the surrounding tissue. Therefore lymph nodes normally cannot be visualized or palpated during an extraoral examination of a healthy patient.
Drainage Patterns of Lymph Nodes
The lymph flows into the lymph node by way of many afferent vessels (see Figure 10-2). On one side of the node is a depression or hilus, where the lymph flows out of the node by way of a single efferent vessel.
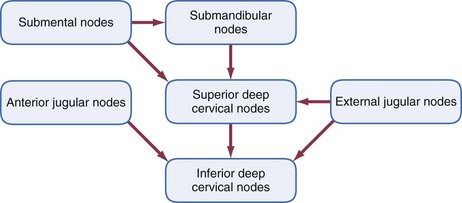
Lymph nodes can be classified as either primary or secondary. Lymph from a particular tissue region drains into a primary node, regional node, or master node. Primary nodes, in turn, drain into a secondary node or central node. The drainage pattern can be outlined in the tissue of the oral cavity (Table 10-1), face and scalp (Table 10-2), and neck (Table 10-3) as well as looking at the flow of lymph through the nodes (see Figures 10-8, 10-11, and 10-16).
TABLE 10-1
Oral Cavity Lymph Node Drainage
| STRUCTURES | PRIMARY NODES | SECONDARY NODES |
| Buccal mucosal tissue | Buccal and mandibular | Submandibular |
| Anterior hard palate | Submandibular and retropharyngeal | Superior deep cervical |
| Posterior hard palate | Superior deep cervical and retropharyngeal | Inferior deep cervical |
| Soft palate | Superior deep cervical and retropharyngeal | Inferior deep cervical |
| Maxillary anterior teeth and associated tissue | Submandibular | Superior deep cervical |
| Maxillary first and second molars and premolars and associated tissue | Submandibular | Superior deep cervical |
| Maxillary third molars and associated tissue | Superior deep cervical | Inferior deep cervical |
| Mandibular incisors and associated tissue | Submental | Submandibular and deep cervical |
| Mandibular canines, premolars, and molars and associated tissue | Submandibular | Superior deep cervical |
| Floor of mouth | Submental | Submandibular and deep cervical |
| Tongue apex | Submental | Submandibular and deep cervical |
| Tongue body | Submandibular | Superior deep cervical |
| Tongue base | Superior deep cervical | Inferior deep cervical |
| Palatine tonsils and lingual tonsil | Superior deep cervical | Inferior deep cervical |
TABLE 10-2
Head and Face Lymph Node Drainage
| STRUCTURES | PRIMARY NODES | SECONDARY NODES |
| Scalp | Retroauricular, anterior auricular, superficial parotid, occipital, and accessory | Deep cervical and supraclavicular |
| Lacrimal gland | Superficial parotid | Superior deep cervical |
| External ear | Retroauricular, anterior auricular, and superficial parotid | Superior deep cervical |
| Middle ear | Deep parotid | Superior deep cervical |
| Pharyngeal tonsil and tubal tonsil | Superior deep cervical | Inferior deep cervical |
| Paranasal sinuses | Retropharyngeal | Superior deep cervical |
| Infraorbital region and nasal cavity | Malar, nasolabial, retropharyngeal, and superior deep cervical | Submandibular and deep cervical |
| Cheek | Buccal, malar, mandibular, and submandibular | Superior deep cervical |
| Parotid salivary gland | Deep parotid | Superior deep cervical |
| Upper lip | Submandibular | Superior deep cervical |
| Lower lip | Submental | Submandibular and deep cervical |
| Chin | Submental | Submandibular and deep cervical |
| Sublingual salivary gland | Submandibular | Superior deep cervical |
| Submandibular salivary gland | Submandibular | Superior deep cervical |
TABLE 10-3
| STRUCTURES | PRIMARY NODES | SECONDARY NODES |
| Superficial anterior cervical triangle | Anterior jugular | Inferior deep cervical |
| Superficial lateral and posterior cervical triangles | External jugular and accessory | Deep cervical and supraclavicular |
| Deep posterior cervical triangle | Inferior deep cervical | Pass directly into the jugular trunk on the right side or thoracic duct on the left |
| Pharynx | Retropharyngeal | Superior deep cervical |
| Thyroid gland | Superior deep cervical | Inferior deep cervical |
| Larynx | Laryngeal | Inferior deep cervical |
| Esophagus | Superior deep cervical | Inferior deep cervical |
| Trachea | Superior deep cervical | Inferior deep cervical |
Tonsils
Tonsils consist of masses of lymphoid tissue located in the oral cavity and pharynx. Tonsils, like lymph nodes, contain lymphocytes that remove toxins. Tonsils are located near airway and food passages to protect the body against disease processes from toxins.
Lymphatic Ducts
In the outer tissue of the body, smaller lymphatic vessels containing lymph converge into larger lymphatic ducts (see Figure 10-1), which empty into the venous system of the blood in the chest area. The final drainage endpoint of the lymphatic vessels into the lymphatic ducts depends on which side of the body is involved.
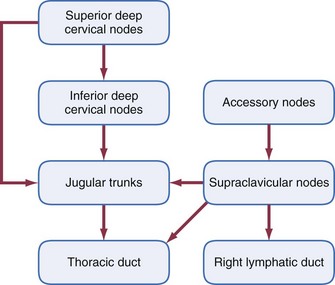
The lymphatic system of the right side of the head and neck converge by way of the right jugular trunk (jug-you-lar), joining the lymphatic system from the right arm and thorax to form the right lymphatic duct, which drains into the venous system at the junction of the right subclavian and right internal jugular veins.
The lymphatic vessels of the left side of the head and neck converge into the left jugular trunk, actually a short vessel, and then into the thoracic duct (tho-ras-ik), which joins the venous system at the junction of the left subclavian and left internal jugular veins. The lymphatic system from the left arm and thorax also joins the thoracic duct. The thoracic duct is much larger than the right lymphatic duct because it drains the lymph from the entire lower half of the body (both the right and left sides).
Lymph Nodes of Head
The lymph nodes of the head are located in either a superficial or deep position relative to the surrounding tissue. All nodes of the head can drain either the right or left tissue, structures, or organs in each region, depending on their location; older terms are included for completeness.
Superficial Lymph Nodes of the Head
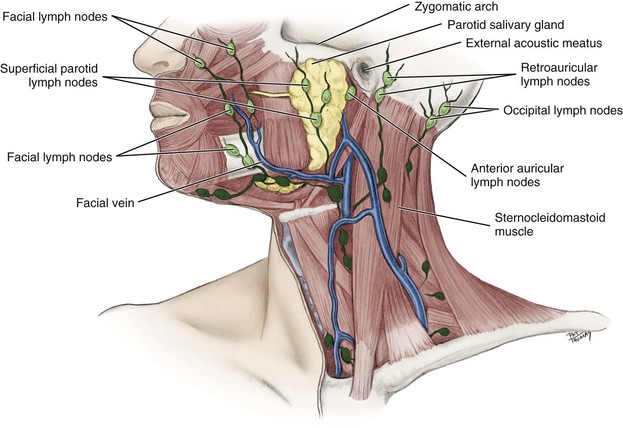
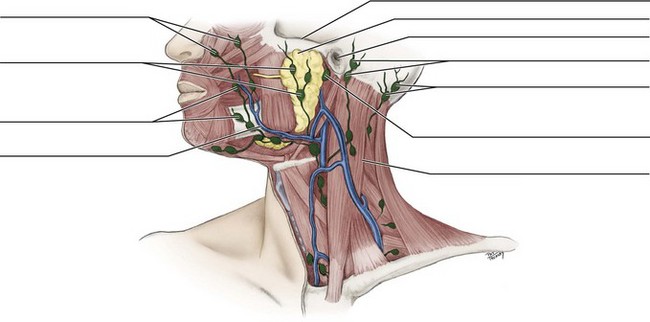
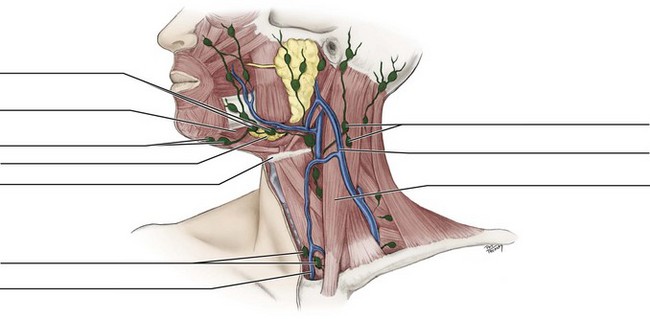
Five groups of paired superficial lymph nodes are located in the head: the occipital, retroauricular, anterior auricular, superficial parotid, and facial (Figure 10-3; see Figure 10-8).
Occipital Lymph Nodes.: The occipital lymph nodes (ok-sip-it-al) (1 to 3 in number) are located on the posterior base of the head in the occipital region and drain this part of the scalp (see Figure 3-21). Have the patient lean the head forward, allowing for effective bilateral palpation during an extraoral examination at the base of each side head for these nodes (Figure 10-4). The occipital nodes empty into the deep cervical nodes.
Retroauricular, Anterior Auricular, and Superficial Parotid Lymph Nodes.: The retroauricular lymph nodes (ret-ro-aw-rik-you-lar) or mastoid glands or posterior auricular nodes (1 to 3 in number) are located posterior to each auricle (and external acoustic meatus), where the SCM inserts on the mastoid process (see Figures 2-4 and 4-1 ). The anterior auricular lymph nodes (aw-rik-you-lar) (1 to 3 in number) are located anterior to each auricle.
The superficial parotid lymph nodes (pah-rot-id) or paraparotid nodes (up to 10 in number along with the deep parotid group) are located just superficial to each parotid salivary gland (see Figure 7-2). Anatomists may group the anterior auricular and superficial parotid nodes together.
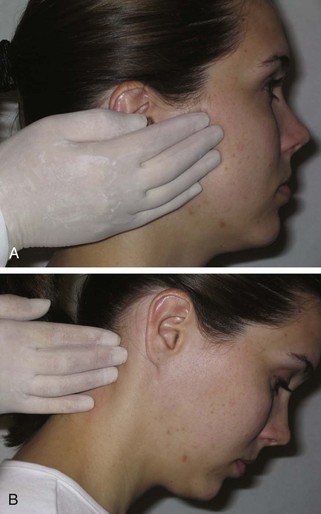
The retroauricular, anterior auricular, and superficial parotid nodes drain the external ear, lacrimal gland, and adjacent regions of the scalp and face. All of these nodes empty into the deep cervical nodes. During an extraoral examination, stand near the patient and bilaterally palpate these nodes, as well as the face and scalp anterior to and around each auricle (Figure 10-5).
Facial Lymph Nodes.: The facial lymph nodes (up to 12 in number) are superficial nodes located along the length of the facial vein. These nodes are usually small and variable in number. The facial nodes are further categorized into four subgroups: malar, nasolabial, buccal, and mandibular.
Nodes in the infraorbital region are the malar lymph nodes (may-lar) or infraorbital nodes. Nodes located along the nasolabial sulcus are the nasolabial lymph nodes (nay-zo-lay-be-al) (see Figure 2-7). Nodes around the labial commissure and just superficial to the buccinator muscle are the buccal lymph nodes (see Figure 4-11). Nodes in the tissue superior to the surface of the mandible, anterior to the masseter muscle, are the mandibular lymph nodes (man-dib-you-lar) (see Figure 4-19).
Each facial node subgroup drains the skin and mucous membranes where the nodes are located. The facial nodes also drain from one to the other, superior to inferior, and then finally drain together into the deep cervical nodes by way of submandibular nodes. During an extraoral examination, bilaterally palpate these nodes on each side of the face, moving from the infraorbital region to the labial commissure, and then to the surface of the mandible (Figure 10-6). Infections from the teeth may spread to one of these nodes, which when undergoing lymphadenopathy, can be described as being firm like a pea.
Deep Lymph Nodes of Head
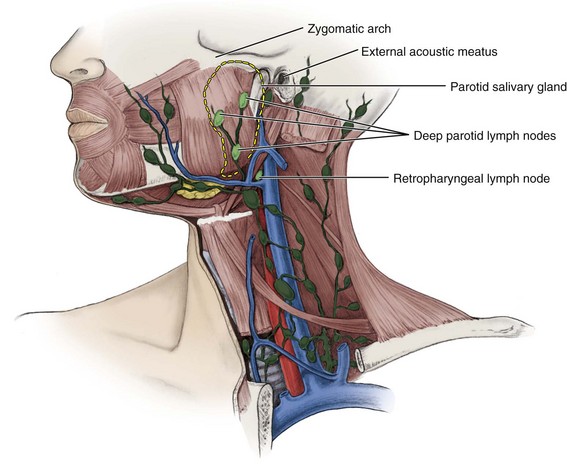
Deep lymph nodes in the head region can never be palpated during an extraoral examination due to their increased depth in the tissue. The deep nodes of the head include the deep parotid and retropharyngeal nodes (Figures 10-7 and 10-8). All of these deep nodes of the head drain into the deep cervical nodes.
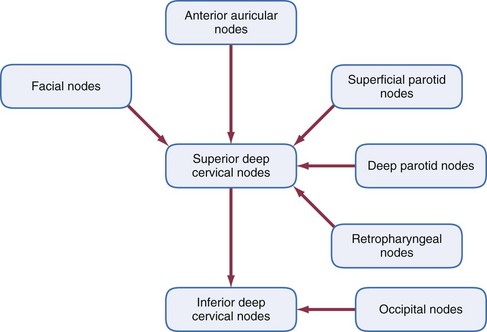
FIGURE 10-8 Lymphatic drainage of the head into the neck (note that external jugular nodes may be secondary nodes for the occipital, retroauricular, anterior auricular, and superficial parotid nodes).
Deep Parotid Lymph Nodes.: The deep parotid lymph nodes (up to 10 in number along with the superficial parotid nodes) are located deep within the parotid salivary gland and drain the middle ear, auditory tube, and parotid salivary gland.
Retropharyngeal Lymph Nodes.: Also located near the deep parotid nodes and at the level of the atlas, the first cervical vertebra, are the retropharyngeal lymph nodes (ret-ro-far-rin-je-al) (up to 3 in number), which drain and are posterior to the pharynx, palate, paranasal sinuses, and nasal cavity.
Cervical Lymph Nodes
Nodes of the neck or cervical lymph nodes can be in either a superficial or deep location in the tissue. All the cervical nodes drain either the right or left parts of the tissue, structures, and organs in which they are located, except the midline submental nodes, which drain the tissue in the region bilaterally.
Many clinicians record all the cervical nodes (except those directly inferior to the chin) in relationship to the large SCM, which defines the triangular regions of the neck (see Figure 2-23). Thus the cervical nodes can be discussed as if they were in three overlapping categories: upper/middle/lower, anterior or lateral/posterior, and superficial/deep. This chapter is more specific in its discussion but recognizes this other method as workable for clinicians in a dental setting; older terms are included for completeness.
In addition, there is an imaging-based classification used by the medical community dividing certain cervical lymph nodes into six areas or levels (Figure 10-9). Levels (as well as related sublevels) use Roman numerals for each area, increasing in value towards the chest. Other nodes not within this classification can continue to be known by their anatomic name such as the external and anterior jugular nodes and as the supraclavicular nodes. This text will include both the anatomical and level designations to reduce confusion for clinicians. However, note that clinical terminology continues to evolve. A recent study advocates a 3-by-3 grid system of 11 designations for more specific coverage of the neck using an overlay of both superficial and deep dissection.
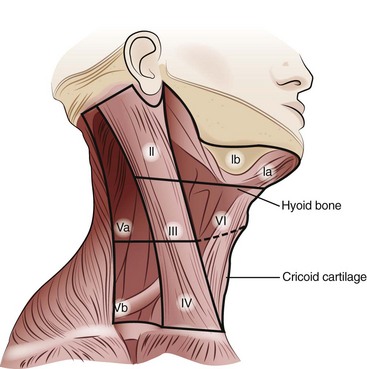
FIGURE 10-9 Levels (as well as related sublevels) noted for cervical lymph nodes by region using Roman numerals, which increases towards the chest.
Superficial Cervical Lymph Nodes
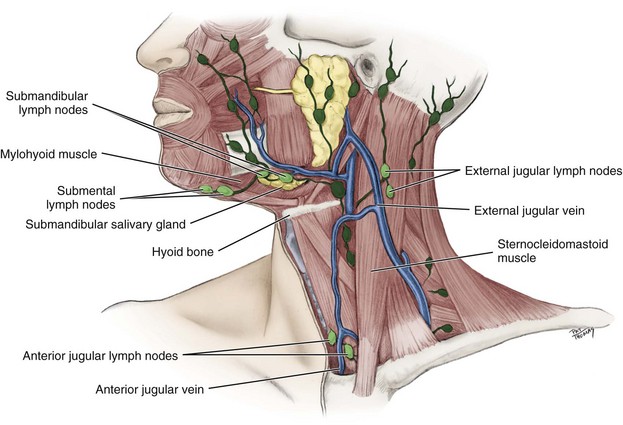
The four groups of superficial cervical lymph nodes include: the submental, submandibular, external jugular, and anterior jugular (Figures 10-10 and 10-11).
Submental Lymph Nodes.: The submental lymph nodes (sub-men-tal) (2 to 3 in number) or suprahyoid nodes are located inferior to the chin in the submental fascial space (see Figure 11-11). The submental nodes are near the midline inferior to the mandibular symphysis in the suprahyoid region, and also just superficial to the mylohyoid muscle (see Figure 4-25). These nodes are considered to be within Level I, sublevel A (see Figure 10-9). These nodes drain the lower lip, both sides of the chin, the floor of the mouth, the apex of the tongue, and the mandibular incisors and associated tissue. The submental nodes then empty into the submandibular nodes or directly into the deep cervical nodes.
Submandibular Lymph Nodes.: The submandibular lymph nodes (sub-man-dib-you-lar) (3 to 6 in number) are located at the inferior border of the ramus of the mandible, just superficial to the submandibular salivary gland, and within the submandibular fascial space (see Figure 11-12). They are considered to be within Level I, sublevel B (see Figure 10-9). These nodes drain the cheeks, upper lip, body of the tongue, anterior hard palate, and all teeth, except the mandibular incisors and maxillary third molars.
The submandibular nodes may be secondary nodes for the submental nodes and facial regions. The lymphatic system from both the sublingual and submandibular salivary glands also drains into these nodes. The submandibular nodes then empty into the deep cervical nodes.
During an extraoral examination, manually palpate the submental and submandibular nodes directly inferior to the chin after having the patient lower the chin (Figures 10-12 and 10-13). Then for the more laterally placed submandibular nodes, push the tissue in the area over the bony inferior border of mandible on each side, where it is grasped and rolled. Dental professionals also recommend that the patient’s chin be up, the mouth slightly open, and the apex of the tongue on the hard palate to allow palpation of the nodes directly inferior to the chin against the mylohyoid muscle.
External Jugular Lymph Nodes.: The external jugular lymph nodes (jug-you-lar) or superficial cervical nodes are located on each side of the neck along the external jugular vein, superficial to the SCM. The external jugular nodes may be secondary nodes for the occipital, retroauricular, anterior auricular, and superficial parotid nodes. These nodes then empty into the deep cervical nodes.
Anterior Jugular Lymph Nodes.: The anterior jugular lymph nodes or anterior cervical nodes are located on each side of the neck along the length of the anterior jugular vein, anterior to the larynx, trachea, and SCM, and drain the infrahyoid region of the neck (Figure 4-27). The anterior jugular nodes then empty into the deep cervical nodes.
During an extraoral examination of the external and anterior jugular nodes in the midpart of the neck, have the patient turn the head to the opposite side, which makes the important landmark of the SCM more prominent (Figure 10-14). Palpate these nodes on each side by starting at the angle of the mandible and continue the whole length of the surface of the SCM to the clavicle.
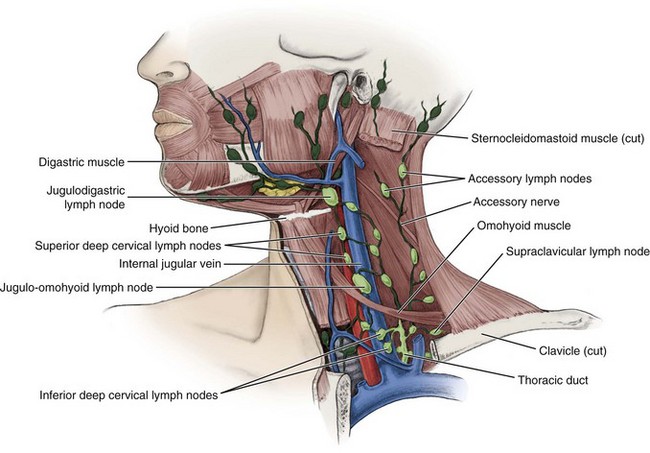
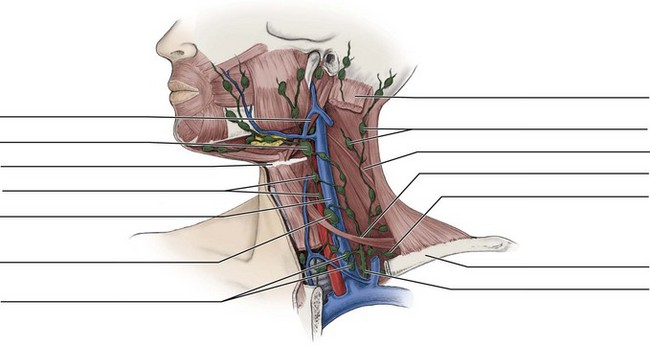
Deep Cervical Lymph Nodes
The deep cervical lymph nodes (15 to 30 in number) are located along the length of the internal jugular vein on each side of the neck, deep to the SCM (Figures 10-15 and 10-16). They extend from the base of the skull to the root of the neck, adjacent to the pharynx, esophagus, and trachea.
The deep cervical nodes can be divided into two groups based on the vertical anatomic position of the nodes to the point where the omohyoid muscle crosses the internal jugular vein: superior and inferior (see Figure 10-15). However, the specificity of this division is not as important in the overall drainage of the head and neck to dental professionals as it is to medical professionals.
These deep cervical nodes are also considered to be within Levels II, III, IV, and V (see further discussion below and see Figure 10-9). Level II nodes include the upper third of the deep cervical nodes, including the jugulodigastric node. This region is bound by the digastric muscle superiorly and the hyoid bone (clinical landmark), or the carotid bifurcation (surgical landmark) inferiorly. More specifically, Level II, Sublevel A contains nodes in the region anterior to the (spinal) accessory nerve and Sublevel B is posterior to the nerve.
Level III includes the middle third of the deep cervical nodes, extending from the carotid bifurcation superiorly to the cricothyroid notch (clinical landmark), or inferior edge of cricoid cartilage (radiological landmark), or omohyoid muscle (surgical landmark). Level IV includes the lower one third of the deep cervical nodes, extending from the omohyoid muscle superiorly to the clavicle inferiorly.
Level V nodes extend from the skull base, at the posterior border of the attachment of the sternocleidomastoid muscle, to the level of the clavicle as seen on each axial scan. More specifically, Level V has Sublevel A superior to the inferior border of the cricoid cartilage and Sublevel B between inferior border of the cricoid cartilage and the superior border of the clavicle. Level VI nodes lie inferior to the lower body of the hyoid bone, and between the medial margins of the left and right common carotid arteries or the internal carotid arteries.
Unlike the deep nodes of the head that cannot be palpated, the deep cervical nodes can be palpated on each side of the neck. Again, during an extraoral examination, have the patient turn the head to the opposite side, which makes the important landmark of the SCM more prominent and increases accessibility for effective palpation of these nodes (Figure 10-17). Palpation of the deep cervical nodes is performed on the underside of both the anterior and posterior aspects of the SCM in contrast to the superficial cervical nodes that are on the muscle’s surface. Using bidigital palpation start at the angle of the mandible and continue down the length of the SCM to the clavicle.

FIGURE 10-17 Palpating the deep cervical lymph nodes during an extraoral examination by having the patient’s head turned using the landmark of the sternocleidomastoid muscle, and using bidigital palpation on the underside of the muscle from the angle of the mandible to the clavicle.
Superior Deep Cervical Lymph Nodes.: The superior deep cervical lymph nodes are located deep beneath the SCM, superior to where the omohyoid muscle crosses the internal jugular vein. The superior deep cervical nodes are primary nodes for and drain the posterior nasal cavity, posterior hard palate, soft palate, base of the tongue, maxillary third molars and associated tissue, esophagus, trachea, and thyroid gland. However, remembering that the lymphatic drainage of the base of the tongue is bilateral in the posterior region, the contralateral node may be affected if there is pathology.
The superior deep cervical nodes may be secondary nodes for all other nodes of the head and neck, except inferior deep cervical nodes. The superior deep cervical nodes empty into the inferior deep cervical nodes or directly into the jugular trunk.
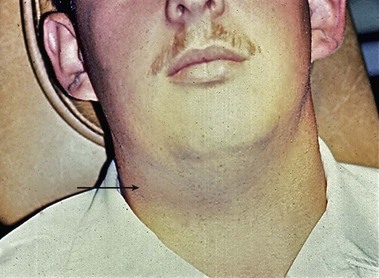
One node of the superior deep cervical nodes, the jugulodigastric lymph node (jug-you-lo-di-gas-tric) or tonsillar node, easily becomes palpable when the palatine tonsils undergo lymphadenopathy. The jugulodigastric node is located inferior to the posterior belly of the digastric muscle.
Inferior Deep Cervical Lymph Nodes.: The inferior deep cervical lymph nodes are a continuation of the superior deep cervical group. The inferior deep cervical nodes are also located deep to the SCM, but inferior to where the omohyoid muscle crosses the internal jugular vein, extending into the supraclavicular fossa, superior to each clavicle. The inferior deep cervical nodes are primary nodes for and drain the posterior part of the scalp and neck, the superficial pectoral region, and a part of the arm.
A possibly prominent node of the inferior deep cervical nodes, the jugulo-omohyoid lymph node (jug-you-lo-o-mo-hi-oid), is located at the actual crossing of the omohyoid muscle and internal jugular vein. The jugulo-omohyoid node drains the tongue and submental region as well as associated structures and regions.
The inferior deep cervical nodes may be secondary nodes for the superficial nodes of the head and superior deep cervical nodes. Their efferent vessels form the jugular trunk, which is one of the tributaries of the right lymphatic duct (on the right side) and the thoracic duct (on the left). The inferior deep cervical nodes also communicate with the axillary lymph nodes that drain the breast region. These nodes in the area of the armpit may be involved when the patient has breast cancer (adenocarcinoma), which is discussed later.
Accessory and Supraclavicular Lymph Nodes
In addition to the deep cervical lymph nodes are the accessory and supraclavicular node groups in the most inferior part of the neck (see Figure 10-15). The (spinal) accessory lymph nodes or posterior lateral superficial cervical nodes (2 to 6 in number) are located along the eleventh cranial or accessory nerve. They drain the scalp and neck regions and then drain into the supraclavicular nodes.
The supraclavicular lymph nodes (soo-prah-klah-vik-you-ler) or transverse cervical chain of nodes (1 to 10 in number) are located along the clavicle and drain the lateral cervical triangles. The supraclavicular nodes may empty into one of the jugular trunks or directly into the right lymphatic duct or thoracic duct. These nodes are located in the final endpoint of lymphatic drainage from the entire body. For instance, cancer arising from the lungs, esophagus, and stomach may present in these nodes (see later discussion). Therefore inspection of these nodes is important in any comprehensive patient assessment.
For those nodes near the clavicle such as the inferior deep cervical and supraclavicular nodes, have the patient raise the shoulders up and forward, allowing for effective palpation during an extraoral examination (Figure 10-18).
Tonsils
Unlike lymph nodes, tonsils are not located along lymphatic vessels. Instead, all the tonsils drain into the superior deep cervical lymph nodes, particularly affecting the jugulodigastric lymph node if there is an infection in the region (considered the tonsillar node) (see Tables 10-1 and 10-2 and Figure 10-15). Changes can also occur in the tonsils similar to lymph nodes (see later discussion).
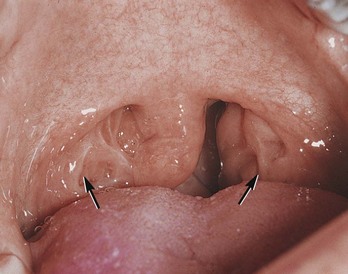
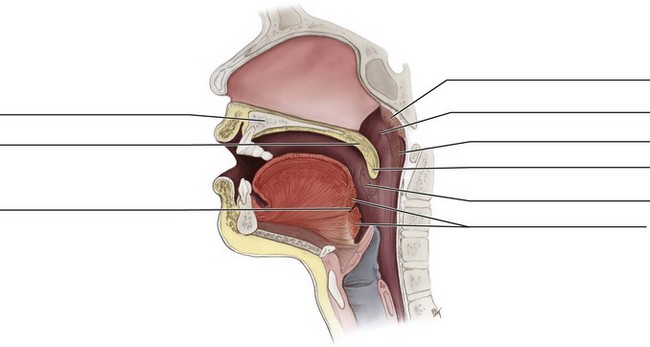
Palatine and Lingual Tonsils
The palatine tonsils, what patients call their “tonsils”, are two rounded masses of variable size located in the oral cavity between the anterior and posterior faucial pillars on each side of the fauces (Figure 10-19; see Figures 2-21, 4-28, and 4-31).
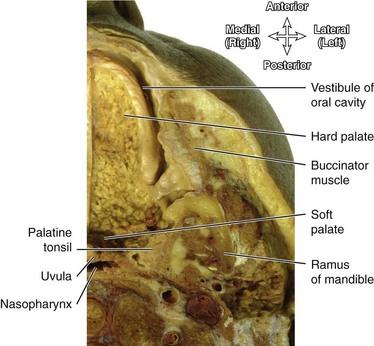
FIGURE 10-19 Dissection showing a transverse section of the right palatine tonsil, palate, and oral cavity. (From Logan BM, Reynold PA, Hutching RT: McMinn’s color atlas of head and neck anatomy, ed 4, London, 2010, Mosby Ltd.)
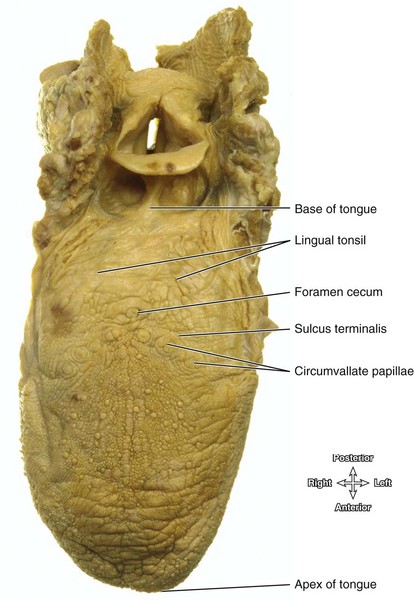
The lingual tonsil is an indistinct layer of lymphoid nodules located intraorally on the dorsal surface of the base of the tongue (Figure 10-20 and see Figure 2-17).
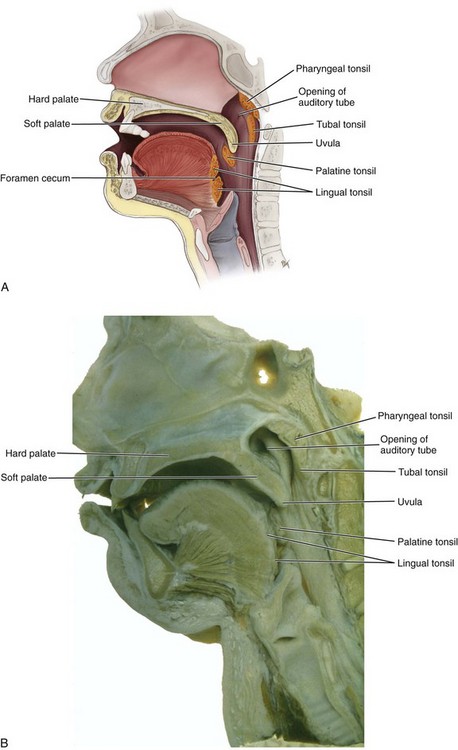
Pharyngeal and Tubal Tonsils
The pharyngeal tonsil (fah-rin-je-il) is located on the midline of the posterior wall or roof of the nasopharynx (Figure 10-21). This tonsil is also called the adenoids (ad-in-oidz) and is normally enlarged in children but can undergo even further enlargement. The tubal tonsil is also located in the nasopharynx, posterior to the openings of the eustachian or auditory tube (see Figure 10-21).
Identification Exercises
Identify the structures on the following diagrams by filling in each blank with the correct anatomic term. You can check your answers by looking back at the figure indicated in parentheses for each identification diagram.
1. (Figure 10-1)
2. (Figure 10-2)
3. (Figure 10-3)
4. (Figure 10-7)
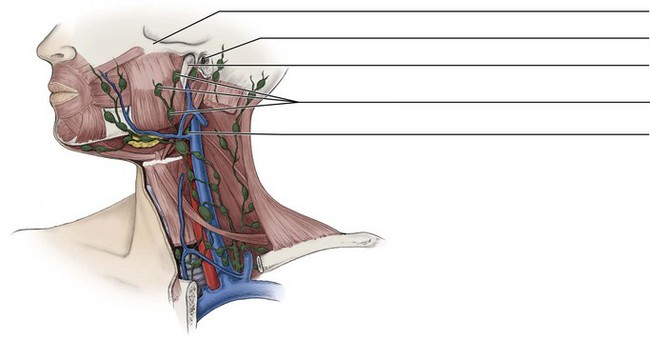
5. (Figure 10-10)
6. (Figure 10-15)
7. (Figure 10-21, A)
1. Which of the following lymph nodes have BOTH superficial and deep nodes?
2. Which of the following structures leave each individual lymph node at the hilus?
3. Which of the following lymph nodes are considered subdivisions of the facial lymph nodes?
A Sublingual, submandibular, zygomatic, and buccal nodes
B Infraorbital, nasal, buccal, and submental nodes
C Mandibular, lingual, malar, and zygomatic nodes
4. Which of the following components of the lymphatic system have one-way valves?
5. Which type of nodes drain lymph from a local region before the lymph flows to a more distant region?
6. The buccal lymph nodes are located superficial to which of the following structures?
7. Which of the following lymph nodes extends from the base of the skull to the root of the neck?
8. Where are the external jugular lymph nodes located?
9. Into which area does the thoracic duct empty?
B Superior vena cava of the body
C Junction of the right and left brachiocephalic veins
D Junction of the left internal jugular and subclavian veins
10. Which of the following are the primary lymph nodes draining the skin and mucous membranes of the lower face?
11. Which of the following are secondary lymph nodes for the occipital nodes?
12. Which of the following pairs of lymph nodes are both considered parts of the superficial cervical lymph nodes?
A External and anterior jugular nodes
B Superficial and deep jugular nodes
13. Which of the following statements concerning the submental lymph nodes is CORRECT?
A They are located deep to the mylohyoid muscle.
B They are located between the mandible’s symphysis and hyoid bone.
14. Which muscle needs to be made more prominent on a patient to achieve effective palpation of the region where the superior deep cervical lymph nodes are located?
15. Where is the lingual tonsil located in the head and neck?
16. Which of the following nodes often becomes easily palpable when the palatine tonsils are inflamed?
17. Which of the following are primary nodes for the maxillary third molar if it becomes infected with caries or periodontal disease?
18. If a patient with breast cancer has involvement with the axillary nodes, which lymph nodes in the neck area primarily communicate with these nodes?
19. At which site in the oral cavity are the palatine tonsils located?
20. What characterizes lymph nodes when involved in metastasis?
21. What is the last location noted for the lymph before reentering systemic circulation?
22. Enlargement of the lymph nodes occurs because of which of the following situations?
A Amount of intergland lymph is large.
B Accumulation of bacteria and viruses causes the node to expand.
C More protein is lost from the circulatory system and winds up in the nodes.
D White blood cells in the node multiply to fight an infection.
23. Which of the following are prominent nodes that drain BOTH the tongue and submental region?
24. Which tonsil is also called the adenoids and can be normally enlarged in children?
25. Which of the following nodes drain the infrahyoid region of the neck?