CHAPTER 179 Neurology Assessment
CHAPTER 179 Neurology Assessment
The process and interpretation of the neurologic examination varies with age. The newborn examination is unique with many transient and primitive reflex patterns, whereas the examination of an adolescent is similar to that of an adult.
HISTORY
Gathering neurologic history follows the traditional medical model with two additions: the pace of the process and the localization of problem within the neuraxis. The pace or evolution of symptoms provides clues to the underlying nature of the disease process as symptoms may evolve in a progressive, static, or episodic fashion. Progressive symptoms may evolve suddenly or hyperacutely (seizures or stroke); acutely over minutes or hours (extradural hemorrhage); subacutely over days or weeks (brain tumor); or follow an indolent, slowly progressive course (hereditary neuropathies). Static neurologic abnormalities are observed in the first few months of life and do not change in character over time (cerebral palsy). They are often caused by congenital abnormalities of the brain or brain injury sustained during the prenatal or neonatal period. Intermittent attacks of recurrent, stereotyped episodes suggest epileptic or migraine syndromes. Episodic disorders are characterized by periods of symptoms, followed by partial recovery (demyelinating, autoimmune, and vascular diseases).
PHYSICAL EXAMINATION
Because the brain and skin have the same embryonic origin (ectoderm), abnormalities of hair, skin, teeth, and nails are associated with congenital brain disorders (neurocutaneous disorders) such as neurofibromatosis (NF type 1) in which café au lait macules (flat, light brown areas of skin) are characteristic. Adenoma sebaceum, fibrovascular lesions that look like acne on the nose and malar face regions, is commonly seen in older children and adults with tuberous sclerosis.
The head circumference is measured in its largest occipitofrontal circumference and plotted against appropriate standard growth curves (see Chapter 5). Microcephaly and macrocephaly represent an occipitofrontal circumference 2 standard deviations (SDs) below or above the mean, respectively. Measurements are plotted over time and may show an accelerating pattern (hydrocephalus) or a decelerating pattern, indicating brain injury or degenerative neurologic disorder. The anterior fontanelle is slightly depressed and pulsatile when a calm infant is placed in the sitting position. A tense or bulging fontanelle may indicate increased intracranial pressure (ICP) but may be seen in a crying or febrile infant. Premature closure of one or more of the sutures (craniosynostosis) results in an unusual shape of the head. Abnormal shape, location, and condition of the face, eyes, nares, or ears are found in many genetic syndromes.
A careful ocular examination is an essential component of a complete neurologic assessment and should include a search for epicanthal folds, coloboma, conjunctival telangiectasias, or cataracts. A direct ophthalmoscopic examination assesses the optic disks and macula. A complete examination of the retina requires dilating the pupil and using an indirect ophthalmoscope.
Examination of the hands and feet reveals the presence of abnormal creases, polydactyly, or syndactyly (see Chapters 50 and 201). The neck and spine should be examined for midline defects that may be obvious (spina bifida with myelomeningocele) or subtle (cutaneous dimples, sinus tracts, tufts of hair, or subcutaneous lipomas). Kyphosis and scoliosis may result from abnormalities of the central or peripheral nervous system (see Chapter 202).
NEUROLOGIC EXAMINATION OF A NEONATE
Because of the developmental immaturity of infants, the neurologic examination primarily assesses the function of the basal ganglia, brainstem, and more caudal structures and, because of the plasticity of the developing nervous system, the results of the examination should be used cautiously in predicting developmental outcome.
Reflexes
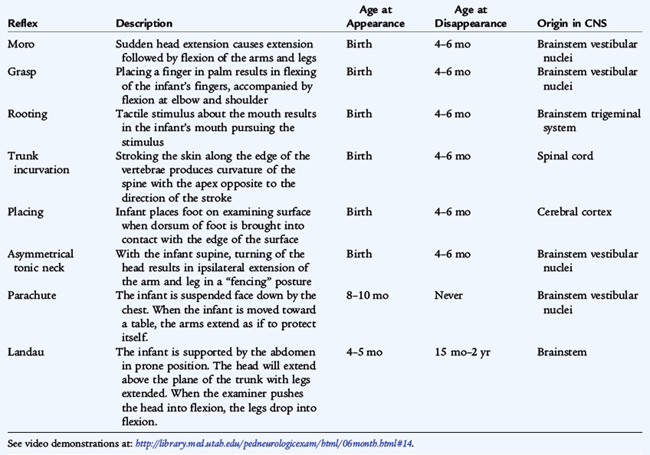
Numerous primitive reflexes, many present at birth, are stereotyped motor responses that assess the functional integrity of the brainstem and basal ganglia (Table 179-1). They are symmetrical and disappear at 4 to 6 months of age, indicating the normal maturation of descending inhibitory cerebral influences (Moro reflex). The grasp and rooting reflexes are inhibited by maturation of frontal lobe structures but may reappear later in life with frontal lobe lesions. Other primitive reflexes emerge after the newborn period and indicate proper maturation of appropriate brain structures (Landau, parachute reflexes). Asymmetry or persistence of the primitive reflexes may indicate focal brain or peripheral nerve lesions.
Posture
Posture is the position that a calm infant naturally assumes when placed supine. An infant at 28 weeks of gestation shows an extended posture. By 32 weeks, there is a slight trend toward increase in tone of the lower extremities and more lower extremity flexion. At 34 weeks, the lower extremities are flexed; the upper extremities are extended. The term infant flexes lower and upper extremities. Recoil, the liveliness with which an arm or leg springs back to its original position after passive stretching and release, is essentially absent in a small premature infant but is brisk at term.
Movement and Tone
Spontaneous movements of a small premature infant are slow and writhing; those of a term infant are more rapid. The popliteal angle, heel-to-ear maneuver, scarf maneuver, and head control are used in assessing muscle tone and estimating gestational age (see Chapter 58).
NEUROLOGIC EXAMINATION OF A CHILD
The purpose of the neurologic examination is to localize or identify the region within the neuraxis from which the symptoms arise. The mental status examination assesses the cerebral cortex. The cranial nerve examination evaluates the integrity of the brainstem. The motor examination evaluates upper and lower motor neuron function. The sensory examination assesses the peripheral sensory receptors and their central reflections. Deep tendon reflexes assess upper and lower motor connections. Gait assessment evaluates the motor system in a dynamic state for better functional assessment.
Mental Status Evaluation
Alertness is assessed in infants by observing spontaneous activities, feeding behavior, and visual ability to fix and follow the movement of objects. Response to tactile, visual, and auditory stimuli is noted. In circumstances of altered consciousness, the response to painful stimuli is noted. Observation of toddlers at play allows a nonthreatening assessment of developmentally appropriate skills. Older children can be tested for orientation to time, place, person, and purpose.
The best way to assess intellectual abilities is through language skills. Language function is receptive (understanding speech or gesture) and expressive (speech and use of gestures). Abnormalities of language resulting from disorders of the cerebral hemispheres are referred to as aphasias. Anterior, expressive, or Broca aphasia is characterized by sparse, nonfluent language. Posterior, receptive, or Wernicke aphasia is characterized by an inability to understand language. Speech is fluent but nonsensical. Global aphasia refers to impaired expressive and receptive language.
Many simple bedside measures exist to evaluate age-appropriate language and social skills (see Chapters 7 and 8). In addition to expressive and receptive language function, older children can be tested for reading, writing, numerical skills, fund of knowledge, abstract reasoning, judgment, humor, and memory.
CRANIAL NERVE EVALUATION
The evaluation of cranial nerve function assesses the integrity of the brainstem but depends on the stage of brain maturation and the ability to cooperate. A colorful toy may capture a young child’s attention and permit observation of cranial nerve function, coordination, and movements.
Cranial Nerve I
The sense of smell can be assessed in verbal, cooperative children older than 2 years of age. Aromatic substances, such as perfumes and vanilla, should be used, not volatile substances (ammonia), which irritate the nasal mucosa.
Cranial Nerve II
Full-term newborns in the quiet awake state follow a human face, a light in a dark room, or a large, opticokinetic strip. Visual acuity has been estimated to be 20/200 in newborns and 20/20 in infants 6 months old. Standard visual charts displaying pictures instead of letters assess visual acuity in toddlers. Peripheral vision is tested by surreptitiously bringing objects into the visual field from behind. A reduced pupillary reaction to light suggests lesions of the anterior visual pathways, including the retina, optic nerves, and chiasm. Unilateral optic nerve lesions are identified by the swinging flashlight test. Normally, both pupils constrict when a light shines in one eye. With an optic nerve problem, both pupils constrict when the light is directed into the normal eye. When the light is swung over to the abnormal eye, both pupils dilate inappropriately; this is called an afferent pupillary defect or Marcus Gunn pupil. Lesions of the posterior visual pathway, including the lateral geniculate, optic radiations, and occipital cortex, have normal pupillary light reactions, but are expressed by loss of visual fields.
Cranial Nerves III, IV, and VI
These three cranial nerves control the movement of the eyes and are most easily examined with the use of a colorful toy to capture the child’s attention. For infants too young to fix and follow, rotating the infant’s head assesses oculocephalic vestibular reflexes (doll’s head maneuver). The oculocephalic reflex is uninhibited when turning the head in one direction elicits an immediate movement of the eyes in the opposite direction. While normal in a newborn, in an older child, an uninhibited doll’s head response indicates that the cortex is not functioning properly to inhibit the brainstem. The oculocephalic response is incomplete when the eyes do not move fully and conjugately in response to head turning. An incomplete response indicates dysfunction of the brainstem.
Abnormalities of these cranial nerves may cause diplopia (double vision). Cranial nerve III (oculomotor nerve) innervates the pupil; levator palpebrae superioris; medial, superior, and inferior recti; and inferior oblique muscles. Cranial nerve IV (trochlear nerve) innervates the superior oblique muscle. Cranial nerve VI (abducens nerve) innervates the lateral rectus muscle. Because cranial nerve VI has a long intracranial route within the subarachnoid space, failure of abduction of one or both eyes is a frequent but nonspecific sign of increased intracranial pressure (ICP).
Cranial nerve III controls the pupillary light reaction, which is present after 30 weeks of gestation. Lesions of the third cranial nerve produce a dilated, mydriatic pupil. Anticholinergic and sympathomimetic drugs dilate the pupil, and cholinergic, narcotic, and sedative drugs constrict the pupil. Third nerve lesions may be associated with incomplete eye movements. Interruption of the sympathetic innervation of the pupil and lid may produce Horner syndrome with meiosis, ptosis, and unilateral facial anhidrosis.
Cranial Nerve V
The muscles of mastication can be observed as an infant sucks and swallows. The corneal reflex can be tested (cranial nerves V and VII) at any age. Facial sensation of light touch and pain can be determined with cotton gauze and pinprick. Facial sensation can be functionally assessed in an infant by gently brushing the cheek, which will produce the rooting reflex (the infant turns its head and neck with mouthing movement seeking to nurse).
Cranial Nerve VII
Facial muscles are assessed by observing the face at rest, with crying, and with blinking. At older, cooperative ages, children can be asked to smile, blow out their cheeks, blink forcibly, and furrow their foreheads. Weakness of all muscles of the face, including the forehead, eye, and mouth, indicates a lesion of the ipsilateral facial nerve (Bell’s palsy). If the weakness affects only the lower face and mouth, a contralateral lesion of upper motor neuron in the brain (tumor, stroke, abscess) must be considered because the upper third of the face receives bilateral cortical innervation.
Cranial Nerve VIII
Lesions of cranial nerve VIII cause deafness, tinnitus, and vertigo. Alert neonates blink in response to a bell. Four-month-old infants turn their head and eyes to localize a sound stimulus. Hearing can be tested in a verbal child by whispering a word in one ear while covering or masking the opposite ear. Lesions of the vestibular component of cranial nerve VIII produce symptoms of vertigo, nausea, vomiting, diaphoresis, and nystagmus. Nystagmus is an involuntary beating eye movement with a rapid phase in one direction and a slow phase in the opposite direction. By convention, the direction of the nystagmus is defined by the fast phase and may be horizontal, vertical, or rotatory.
Cranial Nerves IX and X
The gag reflex is brisk at all ages except the very immature neonate. An absent gag reflex suggests a lower motor neuron lesion of the brainstem, cranial nerves IX or X, neuromuscular junction, or pharyngeal muscles. Uvula deviation toward one side suggests palsy of cranial nerves IX or X on the opposite side. Weak, breathy, or nasal speech; weak sucking; drooling and inability to handle secretions; and gagging and nasal regurgitation of food are additional symptoms of cranial nerve X dysfunction.
Cranial Nerve XI
Observing the infant’s posture and spontaneous activity assesses the functions of the trapezius and sternocleidomastoid muscles. Head tilt and drooping of the shoulder suggest lesions involving cranial nerve XI. In later childhood, strength in these muscles can be tested directly and individually.
MOTOR EXAMINATION
Power
Power in infants is assessed by observation of spontaneous movements and movements against gravity. Arm and leg movements should be symmetrical, seen best when the infant is held supine with one hand supporting the buttocks and one supporting the shoulders. The limbs should be lifted easily off the bed. Power is graded on a scale of declining function, as follows:
Strength in toddlers is assessed by observing functional abilities. The child should be able to reach high above his or her head, wheelbarrow walk, run, hop, easily go up and down stairs, and arise from the ground. Subtle asymmetry can be detected when the child extends his or her arms out in front with the palms upward and eyes closed. The hand on the weaker side cups and begins to pronate slowly (pronator drift). Cooperative children can undergo individual muscle strength testing. Muscle fasciculations indicate denervation from disease of the anterior horn cell or peripheral nerve.
Tone
Tone represents the dynamic resistance of muscles to movement across a joint (stretch) or to gravity. Lower motor and cerebellar lesions produce decreased tone (hypotonia). Upper motor lesions produce increased tone (spasticity). In extrapyramidal disease, an increase in resistance is present throughout passive movement of a joint (rigidity).
Bulk
Muscle bulk represents the volume of muscle tissue. In many lower motor neuron conditions (neuropathies or SMA [spinal muscle atrophy]), muscle bulk is diminished or atrophic. Excessive muscle bulk is seen in myotonia congenita and Duchenne muscular dystrophy (pseudohypertrophy).
Coordination
Lack of coordination of movement is termed ataxia. The cerebellum and its associated pathways modulate volitional movement. If either the afferent (joint position senses) or efferent cerebellar connections (cerebellum through thalamus to cerebral cortex) are disturbed, the patient has ataxia. Truncal ataxia reflects disturbances of the midline cerebellar vermis (medulloblastoma, acute postinfectious cerebellar ataxia, or ethanol intoxication). Appendicular ataxia reflects disturbances of the ipsilateral cerebellar hemisphere (cystic cerebellar astrocytoma). Observation and functional analysis help assess coordination in infants and toddlers. Watching the child sit or walk assesses truncal stability. Exchanging toys or objects with the child permits assessment of intention tremor and dysmetria, signs of cerebellar dysfunction. Cooperative children can do repetitive finger or foot tapping to test rapid alternating movements. Cerebellar and corticospinal tract dysfunction produce slow, rapidly alternating movements.
Gait
Watching a child creep, crawl, cruise or walk is the best global assessment for the motor and coordination systems (see Chapter 197). Subtle deficits in power, tone, or balance or subtle asymmetries may be observed. The toddler gait is normally wide-based and unsteady. The base of the gait narrows with age. By 6 years, a child is able to walk high on toes and heels and tandem walk (heel to toe). Cerebellar dysfunction results in a broad-based, unsteady gait accompanied by difficulty in executing turns. Corticospinal tract dysfunction produces a stiff, scissoring gait and toe walking. Arm swing is decreased, and the arm is flexed across the body. Extrapyramidal dysfunction produces a slow, stiff, shuffling gait with dystonic postures. A waddling gait occurs with hip weakness due to lower motor neuron disorders. A steppage gait results from weakness of ankle dorsiflexors (common peroneal palsy).
Reflexes
Deep tendon reflexes can be elicited at any age. These reflexes are decreased in lower motor neuron diseases and increased in upper motor neuron disease. Clonus may be present in upper motor neuron disorders. Babinski response, or extensor plantar reflex, is an upward movement of the great toe and flaring of the toes on noxious stimulation of the side of the foot and is a sign of corticospinal tract dysfunction. This reflex is unreliable in neonates except when asymmetrical because the “normal” response at this age varies. The plantar response should consistently be flexor (toes down) after 18 months of age.
SENSORY EXAMINATION
The sensory examination of newborns and infants is limited to observing the behavioral response to light touch or gentle sterile pinprick. Stimulation of the limb should produce a facial grimace. A spinal reflex alone may produce withdrawal movement of the limb. In a cooperative child, the senses of pain, touch, temperature, vibration, and joint position can be tested individually. The cortical areas of sensation must be intact to identify by touch an object placed in the hand (stereognosis) or a number written in the hand (graphesthesia) or to distinguish between two sharp objects applied simultaneously and closely on the skin (two-point discrimination).
SPECIAL DIAGNOSTIC PROCEDURES
Cerebrospinal Fluid Analysis
Analysis of cerebrospinal fluid (CSF) is essential when central nervous system (CNS) infection is suspected and provides important clues to other diagnoses (Table 179-2). Differentiating a hemorrhagic CSF caused by a traumatic lumbar puncture (LP) from a true subarachnoid hemorrhage may be difficult. In most cases of traumatic LP, the fluid clears significantly as the sequence of tubes are collected. Caution must be exercised before performing an LP to limit risk of cerebral herniation if there is clinical evidence of increased ICP (papilledema, depression of consciousness, or focal neurologic deficits). A computed tomography (CT) scan should be performed before the LP if increased ICP is suspected. If increased ICP is present, it must be treated before an LP is performed.
TABLE 179-2 Analysis of Cerebrospinal Fluid (CSF)
| CSF Finding | Normal CSF Values | |
|---|---|---|
| Newborn | >1 Month Old | |
| Cell count* | 10–25/mm3 | 5/mm3 |
| Protein | 65–150 mg/dL | <40 mg/dL |
| Glucose | ||
| CSF Change | Significance |
|---|---|
| Increased polymorphonuclear and decreased CSF glucose | |
| Increased lymphocytes and decreased CSF glucose | |
| Increased lymphocytes and normal CSF glucose | |
| Increased CSF protein | |
| Mild CSF pleocytosis | |
| Bloody CSF |
ADEM, acute disseminated encephalomyelitis; HSV, herpes simplex virus.
Electroencephalography
The electroencephalogram (EEG) records electrical activity generated by the cerebral cortex. EEG rhythms mature throughout childhood. There are three key features present: background, symmetry, and presence or absence of epileptiform patterns. The background varies with age, but there should be general symmetry between the background of the two hemispheres without a localized area of higher amplitude or slower frequencies (focal slowing). Fixed slow wave foci (1 to 3 Hz) delta rhythms suggest an underlying structural abnormality (brain tumor, abscess, or stroke). Bilateral disturbances of brain activity (increased ICP or metabolic encephalopathy) must be suspected when there is diffuse slow wave activity (delta frequency). Spikes, polyspikes, and spike-and-wave abnormalities, either in a localized region (focal) or distributed bihemispherically (generalized), indicate an underlying seizure tendency.
Electromyography and Nerve Conduction Studies
Electromyography (EMG) and nerve conduction velocities (NCVs) assess abnormalities of the neuromuscular apparatus, including anterior horn cells, peripheral nerves, neuromuscular junctions, and muscles. Normal muscle is electrically silent at rest. Spontaneous discharge of motor fibers (fibrillations) or groups of muscle fibers (fasciculation) indicates denervation, revealing dysfunction of anterior horn cells or peripheral nerves. Abnormal muscle responses to repetitive nerve stimulation are seen with diseases of the neuromuscular junction, such as myasthenia gravis and botulism. The amplitude and duration of the muscle compound action potential are decreased in primary diseases of muscle. NCVs assess the transmission along peripheral nerves. NCVs are slowed in demyelinating neuropathies (Guillain-Barré syndrome). The amplitude of the signal is diminished in axonal neuropathies.
Neuroimaging
Imaging the brain and spinal cord is accomplished using CT or magnetic resonance imaging (MRI). CT is quick and accessible for emergency purposes. MRI provides fine detail and, with different sequences, permits detection of subtle cerebral abnormalities, vascular anomalies, low-grade tumors, and ischemic changes. For a child with a head injury or sudden headache, cranial CT is the study of choice. For a child with new onset complex partial seizures, MRI is the study of choice. MRI may also provide excellent views of the entire spinal cord. Cranial ultrasonography is a noninvasive bedside procedure that can visualize the brain and ventricles of infants and young children with open fontanelles.