Assessment and Intervention for Perceptual Dysfunction
After reviewing this chapter, the student or practitioner will be able to do the following:
1 Describe how perceptual dysfunction affects participation in occupational performance.
2 Identify standardized and functional assessments for visual perception, visual-spatial perception, tactile perception, body schema perception, and perceptual motor skills.
3 Differentiate between remedial and adaptive approaches to intervention for perceptual dysfunction and how they facilitate engagement in occupation.
4 Describe specific occupational therapy interventions for targeted perceptual motor deficits that facilitate improved performance skills, client factors, and participation in occupation.
“Perception is the gateway to cognition.”15
Perception is the mechanism by which the brain interprets sensory information received from the environment. This perceived information is then processed by the various cognitive centers in the brain (described in Chapter 26). The individual may then choose to respond with a motor act or a verbal expression. For example, when waiting in a checkout line in a grocery store, a person may observe the array of brightly wrapped candy lining the aisle, may remember the sweet taste of the chocolate, may remember a recent resolution to lose weight, and may choose to resist adding any candy bars to the grocery cart. The person may look over to the next aisle, recognize a neighbor, and begin a conversation. In a few minutes, the person may notice that another register has a shorter line and may choose to move over to that line to be able to complete grocery shopping in a shorter amount of time. Perception of the environment provides the information to enable these response options.
In early development, tactile, proprioceptive, vestibular, and visual perception provide an internalized sense of body scheme, which is basic to all motor function.7,69,109 Highly developed spatial skills are critical to the successful occupational performance of an architect, plumber, designer, or artist.40 The process of interpreting visual stimuli is a learned skill, as evidenced by blind individuals who, when sight is restored later in life, have difficulty interpreting what they see.90
Acquired perceptual deficits are noted in persons with cerebrovascular accident (CVA), traumatic brain injury (TBI), and other neurologic disorders, such as multiple sclerosis and Parkinson’s disease.65,82 Spatial disorders and apraxia of a progressive nature are also seen in Alzheimer’s disease.6,14
Severe perceptual deficits, frequently combined with cognitive impairments, can affect every area of occupation (e.g., activities of daily living [ADLs], instrumental activities of daily living [IADLs], education, work, play, leisure, and social participation) and can present with grave safety concerns.56 For example, an individual who is not able to judge distance and the spatial relationship of his foot to the top step of a stairwell may be in danger of a serious fall. Another person who cannot judge the position of the dial on the stove when preparing a meal may cause a fire. It is often the occupational therapy practitioner’s role to evaluate safe and independent functioning in valued occupations and to assess visual and perceptual skills using both standardized instruments along with observations of occupational performance in context.
This chapter describes the client factors of visual per-ception, visual spatial perception, tactile perception, body schema perception, motor perception, and the potential deficits in occupational performance that result from impairment to these client factors. Suggestions for standardized and functional testing are provided. General occupational therapy (OT) approaches to intervention are reviewed, and suggestions for treatment are presented.
General Principles of the Occupational Therapy Assessment
When assessing perceptual skills, several assessment tools may be required. The optimal battery of standardized assessments includes tools that require a verbal response (e.g., naming a picture) or a motor response (e.g., drawing or constructing) or have flexible response requirements of either mode (multiple choice indicated by verbalizing the number or letter or by pointing to the chosen item). This enables the OT practitioner to assess visual perceptual dysfunction in a client with severe limitations in cognitive or communication ability. With a variety of such assessments, the OT practitioner is able to gather information to discriminate between an impairment in the reception of information and an impairment in the motor or verbal output.25 This, in turn, influences the occupational therapy intervention approach. Observation of occupational performance in context and the analysis of the perceptual-motor demands of functional activities further complement the analysis of perceptual dysfunction via standardized assessment tools and enable the determination of underlying causes of deficits in occupational performance. Assessment methods should be conducted in the specific context of the occupation being performed.
Warren emphasized the importance of using a bottom-up approach to evaluate impairments in visual foundation skills,99,100 such as visual acuity, oculomotor function, visual field function, visual attention, and visual scanning prior to evaluating the higher-level perceptual skills covered in this chapter. For example, a deficit in visual acuity could be the underlying cause of poor performance on a test of perceptual processing. The normal aging process also results in impairments related to visual foundation areas, and a variety of age-related eye diseases such as macular degeneration, glaucoma, diabetic retinopathy, and cataracts can affect visual acuity or visual field function.62 It is also possible that performance on global perceptual tests may be affected by deficits in cognitive areas such as attention, memory, or executive function (see Chapter 26). For example, an individual with severely limited attention is unlikely to perform well on many standardized assessments, regardless of the modality or nature of the task. Tsurumi and Todd also analyzed the cognitive skills involved in the commonly used assessments of visual perceptual functions and warn that an individual’s performance using two-dimensional representations of visual stimuli may not predict the person’s performance in a dynamic three-dimensional world.98
Arnadottir recommended the use of ADLs to assess neurobehavioral dysfunction, including perceptual dysfunction and its effect on the performance of tasks essential to functional independence.5 She maintained that it is preferable for occupational therapists to assess neurobehavioral deficits directly from the ADL evaluation. She developed the Arnadottir OT-ADL Neurobehavioral Evaluation (A-ONE), which evaluates perceptual and perceptual-motor dysfunction in the context of ADL and functional mobility tasks, including ideational apraxia, ideomotor apraxia, unilateral neglect, body scheme disorders, organization/sequencing dysfunction, agnosias, and spatial dysfunction.3–5
Toglia’s Multicontext Treatment Approach focuses on remediating and compensating for perceptual and cognitive impairments by promoting generalization of functional skills across multiple contexts.96 Visual processing strategies, task analysis, incorporation of the specific learning needs of the client, establishment of criteria for the transfer of learning, metacognitive training, and practice in multiple environments are key components of Toglia’s approach. This approach also assists the client with TBI to gain self-awareness of perceptual and cognitive strengths and weaknesses to promote the use of strategies for remediation or compensation of skills across multiple contexts.97 Toglia’s Dynamic Object Search Test is one assessment that can be utilized to assess visual processing, visual scanning, and visual attention.96
Another occupation-based assessment tool that can be used to assess the impact of deficient performance skills on functional tasks is the Assessment of Motor and Process Skills (AMPS).38 This standardized assessment evaluates the performance skills necessary for engagement in areas of occupation by assessing 16 motor skills and 20 process skills (e.g., temporal organization, organizing space and objects). Each performance skill is evaluated in the context of client-identified and culturally relevant IADLs from a list of standardized activities at various levels of difficulty. The AMPS has a high rate of reliability and validity, and the evaluator must be an occupational therapist who has received advanced training and certification to administer this assessment.
The Loewenstein Occupational Therapy Cognitive Assessment (LOTCA)57 and Rivermead Perceptual Assessment Battery32,103 provide a comprehensive profile of visual perceptual and motor skills and involve both motor-free and constructional functions. Various other assessment tools require either a verbal or a simple pointing response. The Motor-Free Visual Perceptual Test-Revised (MVPT-R)24,70 assesses basic visual perceptual abilities. An alternative version of the test presents the multiple choices in a vertical format (MVPT-V) to reduce the interference of hemianopsia or visual inattention.73 The MVPT-V has been shown to be predictive of on-the-road driving performance and can be used as a screening tool to identify persons who would not be safe drivers.71 The Test of Visual Perceptual Skills-Upper Level (TVPS-UL)42 also provides a multiple-choice format and has been normed for adults. Test items require a higher level of visual analysis compared with the MVPT, and the test is untimed.16–18 The Hooper Visual Organization Test53 requires that the individual mentally assemble fragmented drawings of common objects. The Minnesota Paper Form Board Test66 is a high-level assessment of visual organization, requiring mental rotation of fragmented geometric shapes.
General Approaches to Occupational Therapy Intervention
An underlying assumption about perceptual-motor function is that perceptual deficits will adversely affect occupational performance. Further, it is assumed that remediation of or compensation for perceptual deficits will improve occupational performance.74 In her critical analysis of approaches to treatment for perceptual deficits, Neistadt described two general classifications of approaches: the adaptive and the remedial.74 Adaptive approaches provide training in occupational performance to facilitate the client’s adaptation to unique contextual environments.2 In contrast, the remedial approaches seek to produce some change in central nervous system (CNS) functions.74 The effectiveness of the various approaches to the remediation of perceptual deficits has not been well documented and requires further scientific investigation.33,74,89
The OT practitioner may use one approach or a com-bination of approaches when designing an intervention plan to address the effects of perceptual dysfunction. The remedial and adaptive approaches can be used along a continuum, beginning with remediating basic visual perceptual skills and gradually incorporating compensatory techniques as the deficits persist.58 The occupational therapy literature suggests specific activities for the intervention of perceptual deficits, but protocols for the use of such activities require further research.109 For measuring the effectiveness of occupational therapy intervention, criteria are needed for successful performance, task grading, objective methods of evaluating performance, and guidelines for task modification.75 In the absence of such objective criteria, the occupational therapist relies on empirical methods to measure and document functional improvement. Several studies have demonstrated the relationship between perceptual deficits and functional performance.8,32,88,89
Remedial Approaches
Remedial, or transfer of learning, approaches assume that multiple practice opportunities with a particular perceptual skill produce carryover of performance to similar activities or tasks requiring comparable perceptual skills.74 For example, practice in reproducing pegboard designs for spatial relations training could carry over to dressing skills that require spatial judgment (such as orienting a blouse sleeve to an arm and discriminating between right and left shoes). The capacity for persons to improve their performance on perceptual tests following perceptual training has been documented.47 However, additional research has also shown that remediative strategies for optimizing perceptual skills may not be as effective as using occupation-based interventions in context to promote changes in perceptual awareness and abilities.33,68,76,77,109
Adaptive Approaches for Perceptual Dysfunction
Adaptive approaches are characterized by the repetitive practice of targeted occupational performance tasks that help the person with neurologic dysfunction gain independence by utilizing alternate strategies to compensate for perceptual impairments.74 The therapist does not retrain specific perceptual skills when utilizing an adaptive approach. Rather, the person is made aware of the problem and is instructed on adaptive strategies for the perceptual deficit during occupational performance. For example, if the client has difficulty with dressing because of a body schema perceptual impairment, the therapist may set up a regular dressing routine and provide cues with repetitive practice on how to compensate for the perceptual challenges in context. With these adaptations, the client may learn to dress independently. Adaptation of the physical environment or the specific activity demands (e.g., objects used in the environment and their properties) is another way to compensate for a perceptual deficit. For example, if an individual has difficulty discriminating a white shirt against the white sheets of the bed, the therapist may encourage the person to select a patterned shirt or may lay the white shirt on a colored towel or bedspread to provide a contrasting background.
Assessment and Intervention of Specific Perceptual Impairments
Walt has difficulty recognizing the faces of his two children and identifying the difference between the brushes he uses for painting. He requires verbal cues to identify the unique features that distinguish the faces of his two children and to identify the appropriate painting utensil to use during an art project. He also has difficulty identifying and recognizing the significance of various traffic signs, which would prevent him from driving safely.
Walt presents with a visual perception disorder, which impairs the person’s ability to recognize and identify familiar objects and people.108 Although these individuals may have intact visual anatomic structures, objects and people may appear distorted, or larger or smaller than they actually are. These individuals also have difficulty interpreting the meaning of objects in their environment, such as signs and maps. In addition, they can have difficulty recognizing, identifying, or remembering the names of colors in their environment. These visual perception disorders can lead to safety problems in dynamic environments and may affect social skills, as the person has difficulty recognizing family members, friends, and coworkers.
Agnosia
Visual object recognition refers to the ability to verbally identify objects via visual input. An impairment in this area is called agnosia, and it is caused by lesions in the right occipital lobe or posterior multimodal association area.54,65 The individual with agnosia can demonstrate normal visual foundation skills. The inability to name objects is not caused by a language deficit in naming the object, as noted in aphasic disorders. Rather, the person is unable to recognize and identify an item using only visual means. If the person holds the object, he or she can identify that object via tactile input, or by olfactory means if the object has a distinguishable odor, such as a flower or an onion.91
Assessment of agnosia is performed by asking the individual to identify five common objects by sight, such as a pencil, comb, keys, a watch, and eyeglasses. If the client demonstrates word-finding difficulties, offer the client a choice of three answers. Ask the client to indicate the correct choice through a head nod (yes or no). If the client is unable to name four out of the five objects, visual agnosia may be indicated.
OT intervention for visual agnosia will focus on adaptive or compensatory methods of keeping frequently used objects, such as a hairbrush, in consistent locations, and teaching the client to rely more heavily on intact sensory modalities, such as stereognosis and tactile discriminatory touch, to seek and find desired items for functional use.54 Remediative approaches can include having the client practice identifying objects that are needed for occupational performance, such as a paintbrush for Walt, or using nonverbal, tactile-kinesthetic guiding during occupations.108 Following the activity, have the client practice naming the items that were used. Current research has found that efforts to remediate object recognition have met with limited success.55
Color Agnosia and Color Anomia
Color agnosia refers to the client’s inability to remember and recognize the specific colors for common objects in the environment.50 For example, Walt was unable to recognize the color of the paints he was using during his landscape painting. He confused the green paint he was using to paint the grass with the blue paint he intended to use for the sky. Alternatively, color anomia refers to the client’s inability to name the color of the objects. Although these clients understand the differences between the different colors of objects, they are unable to name the object accurately. For example, Walt was able to recognize the color red but was not able to name it as such.
To assess color agnosia, present the client with two common objects that are accurately colored and two objects that are not accurately colored. Ask the client to pick out those common objects that are not accurately colored. If the client is unable to choose the objects that are inaccurately colored, color agnosia may be clinically present.
To assess color anomia, ask the client to name the color of various objects in his or her environment. If the patient has aphasia, ask him or her to nod yes or no after offering the patient choices of colors. If the client is unable to correctly name the colors of various objects, color anomia may be present.
OT intervention for color agnosia and color anomia will focus on providing the client with opportunities to recognize, identify, and name various colors of objects in his or her environment. Intervention is best provided in a familiar context and can be incorporated functionally during occupational performance. For example, while Walt is painting a landscape, the therapist would provide verbal cues that assist him in recognizing, identifying, and naming the various colors of paint he is using.
Metamorphopsia
Metamorphopsia refers to the visual distortion of objects, such as the physical properties of size and weight.108 For example, when Walt was playing sports with his two children, he could not distinguish between the basketball, the football, the baseball, or the volleyball. Each of the balls appeared heavier, lighter, larger, or smaller than they actually were, making it difficult to distinguish the differences between them through observation alone.
Assessment for metamorphopsia includes presenting the client with various objects of different weights and sizes (e.g. balls, drinking glasses filled with water, puzzle pieces). Ask the client to place each object in order according to size or weight through observation alone. Metamorphopsia may be indicated if the client is unable to determine the weight and size of the various objects.
OT intervention for metamorphopsia includes providing the client with opportunities to practice distinguishing objects in the natural environment through intact sensory modalities (e.g., tactile-kinesthetic-proprioception). The functional use of objects during occupational performance will provide the client with feedback about the sizes and shapes of different objects. The therapist should also provide specific verbal descriptors of the object when using this approach. Other treatment modalities include puzzles, board games, and computer games that help the client to gain experience distinguishing the sizes and shapes of different objects.
Prosopagnosia
Prosopagnosia refers to an inability to recognize and identify familiar faces caused by lesions of the right posterior hemisphere.19,54,91 The individual with prosopagnosia may have difficulty recognizing his or her own face, faces of family members and friends, or of recognizable public figures because the person cannot recognize the unique facial expressions that make each face different. When attempting to identify family members and acquaintances, the person will tend to compensate by relying on auditory cues such as the sound of the family member’s voice or a distinctive feature such as long, wavy hair.
Brain lesions can also impair the ability to interpret facial expressions, which can have significant social con-sequences.21,106 For example, one client tended to be very suspicious of others. He was observed to have difficulty describing the expressions of various persons depicted in photographs. Because he had immigrated to the United States from another country, his difficulty was originally thought to be a result of cultural differences. He was asked to bring in a newspaper that he regularly received from his native country. The captions of the photographs were occluded, and he was asked to describe the emotional expressions of the persons shown. He was then asked to translate the photo captions and became aware that he was unable to discriminate the emotions apparent on the faces.
A standardized Test of Facial Recognition12 is available, which presents a multiple-choice matching of faces presented in front view and side view and under various lighting conditions. Informal functional assessments could include having the client identify the names of the people in photographs, with family members at a dinner table (e.g., Walt’s two children side by side), or by having the client identify his or her own face in a mirror. Photographs of famous public figures could also be used during assessment. If aphasia is present, have the client communicate through gestures, such as head nodding (e.g., yes or no) in response to multiple choices. If the client is unable to identify him or herself or family members, prosopagnosia may be present. A formal test of facial expression discrimination is not available in the literature,65 but an informal assessment is possible using pictures and photographs of familiar people.
OT interventions for prosopagnosia include remedial approaches such as providing face-matching exercises.108 Adaptive approaches include providing pictures of family members and famous people with names and assisting the client to associate the family member’s face with other unique characteristics and features, such as weight, height, mannerisms, accents, and hairstyle.
Simultanognosia
Simultanognosia refers to the inability to recognize and interpret a visual array as a whole, and it is caused by lesions to the right hemisphere of the brain.35 Clients with simultanognosia are able to identify the individual components of a visual scene, but are unable to recognize and interpret the gestalt of the scene. For example, Walt is able to identify the flowers and the trees in one of his paintings, but he is not able to recognize and interpret this painting as the landscape surrounding the family home where he grew up.
Assessment includes presenting the client with a photograph with a detailed visual array (e.g., Walt’s family photo-graph at the beach), asking the client to describe the scene in detail, and assessing whether or not the client can describe the scene as a whole. Many clients will be able to identify specific features of the visual array (e.g., the sand castle) but cannot describe the context or meaning of the whole scene (e.g., a family trip to the beach). Simultanognosia is clinically significant when the client cannot recognize and interpret a visual array as a whole.
OT intervention will focus on helping the client to construct meaning of a visual array through verbal cues and therapeutic questions to facilitate abstract reasoning. Intervention is best provided in familiar contexts, such as a client’s home, work setting, or during a community outing to the shopping mall.
Visual-Spatial Perception Disorders
Walt presents with difficulty distinguishing the right and left side of his body and often confuses right and left when given directions. He often gets lost and requires a family member to be with him at all times when he is in unfamiliar community environments. When painting, Walt has also been observed to have difficulty with distinguishing the foreground and the background in his paintings and is unable to determine the differences between the amounts of paint in each of the cups next to him. In addition, he is often observed missing the canvas in front of him when attempting to apply the paint.
Walt presents with visual-spatial perception dysfunction. Visual-spatial perception refers to the capacity to appreciate the spatial arrangement of one’s body, objects in relationship to oneself, and relationships between objects in space. Various efforts have been made to subdivide spatial skills into components, but recent authors acknowledge that spatial skills cannot be isolated easily from one another.22 It is generally acknowledged that the right hemisphere, which controls spatial abilities, tends to function in the gestalt (whole), whereas the left hemisphere, tends to focus on discrete details.65
Visual-spatial perception occurs instantaneously. Because of this rapid processing of spatial information it is possible to react quickly to another driver’s actions to avoid a collision when operating a motor vehicle. An individual with a mild visual-spatial perception impair-ment may need additional time to perform a task but processes the information correctly, possibly by compensating with verbal analysis of the perceptual components. Severe impairment may result in the incorrect response despite additional time used in attempting to solve the problem.
Visual-spatial skills are not limited to the visual domain.63 Sounds can be localized in space, and the mobility and daily occupations of blind individuals are heavily dependent on the tactile appreciation of the spatial arrangements of objects.83 For example, a blind person’s ability to navigate through a familiar room requires awareness of the layout of each piece of furniture in the physical environment and continual shifting of the individual’s “cognitive map” while changing positions in the room.
As a pencil rolls across a desktop, it is the skill of visual-spatial perception that enables a person to appreciate the relative orientation of the pencil to the table surface as the pencil nears the edge and is about to fall to the floor. Figure 25-1 illustrates the complexity of visual-spatial perceptual function.
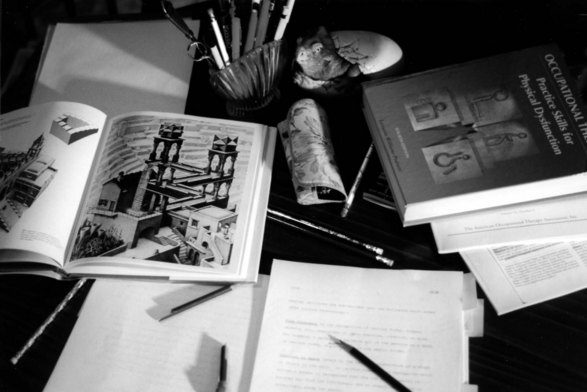
FIGURE 25-1 Visual-spatial functions in real life. Note that all components of spatial functions can be found in this scene.
Figure-Ground Discrimination Dysfunction
Figure-ground discrimination allows a person to perceive the foreground from the background in a visual array.108 For example, Walt is unable to locate a particular painting utensil from the other writing utensils in the pencil holder, thereby demonstrating difficulty with distinguishing the targeted object from the background.
Figure-ground discrimination can be assessed functionally in a variety of contexts. During a dressing activity, you may ask the client to identify the white undershirt that is located on top of his or her white sheets. In the kitchen, you can ask the client to pick out all of the spoons from a disorganized utensil drawer. Figure-ground discrimination dysfunction may be indicated if the client is unable to discriminate the foreground from the background in a complex visual array.
Using a remedial approach, intervention for figure-ground discrimination dysfunction should focus on challenging the client to localize objects of similar color in a disorganized visual array.108 The task could be incorporated contextually into meaningful occupation. For example, the therapist working with Walt may have him localize the exact pencil he would like to use for his sketch drawings. The task can be downgraded by making the visual array less complex and upgraded by making the visual array more complex.
An adaptive approach to intervention would focus on modifying the environment to increase the organization of common functional objects (e.g., placing only the most necessary objects needed for self-care), decreasing the complexity of the visual array that the client has to discriminate (e.g., have only one paintbrush in front of Walt at a given time), or marking common objects with colored tape so that objects are easily distinguished from one another, particularly when the objects are of a similar color.107
Toglia’s multicontextual approach may be used to help the client gain self-awareness of his or her figure-ground discrimination dysfunction and develop effective organizational and visual scanning strategies for discriminating the foreground and background in the environment.96 This intervention approach also focuses on the generalization of skill to multiple functional contexts by using strategies that the client has identified as effective in locating objects in the environment.
Form-Constancy Dysfunction
Form constancy is the recognition of various forms, shapes, and objects, regardless of their position, location, or size.108 For example, a person can perceive all of the pencils on a desk, in various sizes or in various positions in the pencil holder.
To assess form constancy, ask the client to identify familiar objects in his or her environment through observation alone when those objects are placed upside down or on their side. For example, in the kitchen, you may ask Walt to identify a cup that is turned upside down or a toaster oven that is placed on its side. Form-constancy dysfunction may be indicated if the client is unable to identify objects in a position that varies from the norm.
Intervention for form-constancy dysfunction would include using tactile cues to feel objects in various positions so that the client learns their constancy despite their position, size, or location. Activities can be graded from positioning all objects in an upright position to placing objects in odd positions. Intervention is best provided with common objects that the client utilizes in everyday occupational performance.
Position in Space
Position in space, or spatial relations, refers to the relative orientation of a shape or object to the self. It is this component of perception that allows a person to recognize that the tip of the pencil is pointed away from him, and so directs the hand to effectively grasp the pencil.
To assess position in space, have the client place common objects in relation to the self or other objects using the following directional terms: top/bottom, up/down, in/out, behind/in front of, and before/after. For example, ask Walt to place his paintbrush on top of his computer or his basketball behind his back. Position in space dysfunction may be indicated if the client is unable to discern the relationships of objects to the self or other objects through directional terms.
Intervention for position in space includes providing the client with opportunities to experience the organization of objects in the environment to the self. For example, Walt could practice placing various objects in relation to one another in a graphic design program on the computer so that directional concepts of up/down, in/out, behind/in front of, and before/after can be reinforced.
Right-Left Discrimination Dysfunction
Right-left discrimination is the ability to accurately use the concepts of right and left.108 An individual with right-left discrimination dysfunction may confuse the right and left side of his or her body or confuse right and left in directional terms when navigating through the environment.
To assess right-left discrimination, ask the client to point to various body parts (e.g., left ear) or assess the client’s ability to accurately navigate the environment through verbal commands using right and left (e.g., turn right at the end of the hallway). Right-left discrimination dysfunction may be indicated if the client is unable to differentiate between right and left in relation to his or her body and the environment.
Intervention for right-left discrimination will focus on assisting the client to practice reciting right and left while interacting with his or her own body (e.g., “I am now placing my right arm into the shirt sleeve”) or the environment (e.g., “I am now turning left at the stop sign”). Remediation of right-left discrimination can significantly improve topographic orientation as the client learns to navigate in a more dynamic home and community environment.
Stereopsis
Stereopsis is the inability to perceive depth in relation to the self or in relation to various objects in the environment.108 Depth perception is critical to function in a three-dimensional world and to safety in driving and community mobility. Clients with visual dysfunction in one eye or who wear an eye patch to compensate for double vision may demonstrate stereopsis because binocular visual input from both eyes is required to perceive depth.
To assess depth perception, place a variety of common objects on a table surface and ask the client to identify which object is closer and which object is farther away. In a community context, the client may also be assessed functionally by asking him or her to identify buildings or landmarks that are closer or farther away. Stereopsis may be indicated if the client is unable to judge the distance between objects in the environment.
Computer-assisted software has been developed that can help the client with developing depth perception by judging the relative distance of objects in relation to one another on a computer screen.108 Tactile-kinesthetic approaches also help the client judge distances through the use of tactile input.1
Tactile Perception Disorders
Walt is unable to identify the objects he uses for painting by touch alone. He is unable to discriminate between different types of materials or different forms and shapes by tactile means and must compensate visually to determine the objects he is using during occupational performance.
Walt presents with an impairment in tactile perception, which involves tactile discriminative skills of the second somatosensory area of the parietal lobes.72 These skills require a higher level of synthesis than the basic tactile sensory functions of light touch and pressure described in Chapter 23.
Astereognosis
Stereognosis, also known as tactile gnosis,27 is the perceptual skill that enables an individual to identify common objects and geometric shapes through tactile perception without the aid of vision. It results from the integration of the senses of touch, pressure, position, motion, texture, weight, and temperature and is dependent on intact parietal cortical function.44 Stereognosis is essential to occupational performance because the ability to “see with the hands” is critical to many daily activities. It is the skill that makes it possible to reach into a handbag and find a pen and to find the light switch in a dark room. Along with proprioception, stereognosis enables the use of all fine-motor activities without the need to concentrate visually on the objects being manipulated. Examples of stereognosis are knitting while watching television, reaching into a pocket for house keys, and using a fork to eat while engaged in conversation.
A deficit in stereognosis is called astereognosis. Persons who have astereognosis must visually monitor the use of their hands’ during activities. Thus, they must be very slow and purposeful in their movements and tend to be generally less active.
The purpose of a stereognosis test is to assess a client’s ability to identify common objects and perceive their tactile properties.10,26,49,60 A means to occlude the person’s vision is needed, such as a curtain, patch, or folder as described in Chapter 23. Typical objects that could be used for identification include a pencil, pen, a pair of sunglasses, a key, nail, safety pin, paper clip, metal teaspoon, quarter, nickel, and a button. Any common objects may be used, but it is important to consider the client’s social and ethnic background to ensure that he or she has had previous experience with the objects. Three-dimensional geometric shapes (e.g., a cube, sphere, or pyramid) can also be used to test shape and form perception.
The test should be conducted in an environment that has minimal distractions. The therapist should sit across from the client being tested. The client’s vision is occluded, with the dorsal surface of the hand resting on the table. Objects are presented in random order. Manipulation of objects is allowed and encouraged. The therapist assists with the manipulation of items in the client’s hand if the person’s hand function is impaired. The client should be asked to name the object, or, if he or she is unable to name the object, to describe its properties. Clients with aphasia may view a duplicate set of test objects after each trial and point to a visual choice. The person’s response to each of the items presented is scored. The therapist notes if the object is identified quickly and correctly, if there is a long delay before the identification of the object, or if the individual can describe only properties (e.g., size, texture, material, and shape) of the object. The therapist also notes if the person cannot identify the object or describe its properties.
A graded intervention program for astereognosis has been described by Eggers.34 Initially, the client manipulates the object while looking at it and making noise with the object such as tapping it on the tabletop. This approach allows the client to see and hear an object while feeling it for the benefit of intersensory facilitation; then vision is occluded during the tactile exploration. Finally, a pad is placed on the tabletop so that both auditory and visual clues are eliminated and the person relies on tactile-kinesthetic input alone. The program for tactile-kinesthetic reeducation begins with gross discrimination of objects that are very dissimilar—for example, smooth and rough textures or round and square shapes. Next, the client is asked to estimate quantities (such as the number of marbles in a box) through touch. Then the client must discriminate between large and small objects hidden in sand and progress to discriminating between two- and three-dimensional objects. Finally, the client is required to pick a specific small object from among several objects.
Farber also described a treatment approach to retrain stereognosis for adults and children with central nervous system dysfunction.37 First, the client is allowed to examine the training object visually as it is rotated by the therapist. The client is then allowed to handle the object in the less affected hand while observing the hand. In the next step, the client is allowed to manipulate the object with both hands while looking. Then the object is placed in the affected hand and the client manipulates the object while looking at it. The individual may place the hand in a mirror-lined, three-sided box to increase visual input during these manipulations. This sequence is then repeated with the client’s vision occluded. Once several objects can be identified consistently, two of the objects may be hidden in a tub of sand or rice. The client is then asked to reach into the tub and retrieve a specific object. If the sensation of the sand or rice is overstimulating or disturbing, the objects can be placed in a bag.37
Agraphesthesia
An additional test of tactile perception that measures parietal lobe function is the test for graphesthesia, or the ability to recognize numbers, letters, or forms written on the skin.23,44,80 The loss of this ability is called agraphesthesia. To test graphesthesia, the examiner occludes the client’s vision and traces letters, numbers, or geometric forms on the fingertips or palm with a dull-pointed pencil or similar instrument. The client tells the therapist which symbol was written.80 If the client has aphasia, pictures of the symbols may be provided for the individual to indicate a response after each test stimulus. Agraphesthesia is clinically indicated if the client is unable to state or identify the symbol written on the palm of the hand.
OT intervention for agraphesthesia will focus on providing the client with opportunities for tactile discrimination through the use of his or her hands. The therapist can grade the intervention from tracing letters and numbers to words and geometric forms on the palm of the hand. With vision occluded, client can also practice writing his or her name in the opposite palm.
Body Schema Perception Disorders
Walt demonstrates unilateral inattention to the left side of his body and his environment. He demonstrates asymme-trical visual scanning to the left side of his environment, misses details in his drawings on the left, and routinely neglects the functional use of his left upper extremity during functional tasks. He often states that his left arm is owned by someone else and has difficulty holding a painting utensil because of impairments with spatial relationships between his fingers.
Following a CVA or TBI, a person’s sense of his or her body’s shape, position, and capacity frequently is distorted. This is known as a disorder of body schema, or autotopagnosia.11 This can be noted in attempts to draw a human figure (Figure 25-2) or in a person’s unrealistic expectations of performance abilities.65 For example, an individual with left hemiplegia after a TBI expressed his intention to return to his previous manual labor job of installing garage doors. The disorder can affect egocentric perception of one’s own body or allocentric orientation of another person’s body.79,82 A person may neglect one side of the body or demonstrate generally distorted impressions of the body’s configuration. The person may confuse his or her body with that of another, such as the person who thought that her wedding ring had been stolen by the therapist, not realizing that the hand she was viewing was her own. Finger agnosia, or the inability to discriminate the fingers of the hand, can also be part of the disorder.11 An impaired body scheme will also affect participation in occupation and performance skills.89

FIGURE 25-2 Example of a body schema perception disorder. Drawing on the left is the person’s first attempt to draw a face. The occupational therapist asked the person to try again. The second effort is the drawing on right.
Body schema perception disorders can be assessed by asking the individual to draw a human figure (Figure 25-2) or point to body parts on command (e.g., “Touch your left hand” and “Touch your right knee”). Finger agnosia is evaluated by occluding the person’s vision and asking him or her to name each finger as the therapist touches it. Unilateral body neglect can be observed functionally during occupational performance as the client ignores the affected limb or states that a body part is not his or her own. A body schema perception disorder may be clinically indicated if the client is unable to correctly identify parts of his or her body.
A remedial approach to intervention for body schema perception disorders should focus on providing the client with opportunities to reinforce body knowledge through tactile and proprioceptive stimulation.108 For example, while Walt is dressing or painting, have him incorporate his affected left upper extremity into the activity and verbally acknowledge that this is in fact his left arm and hand being used. Tactile-kinesthetic guiding or constraint-induced movement therapy strategies can also be used if the client has difficulty initiating the use of the affected limb. As the client incorporates the use of the affected limb into occupational performance, the client will begin to gain perceptual awareness of his or her body and the relationship between various body parts.
Motor Perception Disorders
When given a shirt to don, Walt attempts to put his legs through the sleeves of the shirt. During drawing and painting activities, he seems to hesitate and is unable to initiate a motor plan without physical cues. He knows that he is painting and knows what he would like to paint, but is unable to translate this idea into a motor action. Walt is also unable to operate the mouse on the computer for a graphic design activity because of his difficulty with motor planning. In addition, when given a three-dimensional craft project, he is unable to use effective problem-solving strategies during the construction of the design.
Praxis is the ability to plan and perform purposeful movement. Walt presents with a motor perception disorder that affects his motor planning. Apraxia has been classically defined as a deficit in “the execution of learned movement which cannot be accounted for by either weakness, incoordination, or sensory loss, or by incomprehension of or inattention to commands.”43 The disorder can result from damage to either side of the brain or to the corpus callosum,51,105 but it is more frequently noted with left hemisphere damage.52 Apraxia is often seen in persons with aphasia; however, not all aphasic persons are apraxic, nor are all apraxic persons aphasic.48,51 This type of dysfunction may occur after CVA or TBI. Progressive apraxia is also noted with degenerative disorders such as Alzheimer’s disease.45,51,81 (See also Chapters 33, 34, and 35.)
Apraxia has been strongly correlated with dependence in areas of occupation.93,101 For example, in a severe case of apraxia, an individual referred to as Ms. S initially required total assistance with basic activities of daily living (BADLs). Ms. S was fully cognizant of ongoing events but could not direct her arm and leg movements in a way that would assist the nursing staff during dressing. When asked to pick up a pencil, Ms. S walked around all four sides of the table in an attempt to position her hand correctly to grasp the object. She could describe the desired action in words (“I want to pick up the pencil between my thumb and index finger, with the lead point of the pencil close to the tips of my fingers”) but reported after returning to her seat that her hand never “looked like it was in the right position” to take hold of the pencil.
The categories of apraxia are difficult to differentiate, and authors differ in their use of terms.94 The principal types recognized in the literature are ideational apraxia, ideomotor apraxia, dressing apraxia, and constructional disorder. Because the distinction between ideational and ideomotor apraxia is often perplexing, some authors recommend simply using the term apraxia.61,65
Ideational Apraxia
Ideational apraxia is a conceptual deficit, seen as an inability to use real objects appropriately.28,31,48 More recent authors suggest the use of the term conceptual apraxia.52,81 The individual also may have difficulty sequencing acts in the proper order,51 such as with folding a sheet of paper and inserting it into an envelope. The individual may use the wrong tool for the task or may associate the wrong tool with the object to be acted on, such as by attempting to write with a spoon.51 This deficit has significant functional implications in a variety of areas of occupation.
Ideomotor Apraxia
Ideomotor apraxia is an inability to carry out a motor act on verbal command or imitation. However, the person with ideomotor apraxia is able to perform the act correctly when asked to use the actual object.30,51,84 For example, a person is unable to mime the action of brushing his teeth on request but is observed using a toothbrush correctly when he is performing grooming activities in context. Observation of the person in areas of occupation is critical to the identification of ideomotor apraxia. Impairments are demonstrated only in the testing environment and appear to have little functional impact, as compared with ideational apraxia.94
Dressing Apraxia
Another category of motor perception disorders recognized in the literature is dressing apraxia. Dressing apraxia contributes to the inability to plan effective motor actions required during the complex perceptual task of dressing one’s upper and lower body. The classification of dressing impairment as a form of apraxia has been questioned in recent years because the difficulties in ADLs are considered to be caused by perceptual or cognitive dysfunction20,101,109 (if apraxia is not noted in other activities) or are seen as an extension of an ideational or ideomotor apraxic disorder.
General Principles in the Assessment and Treatment of Apraxia
It is important that assessments of sensory function, muscle strength, and dexterity are completed before the test of praxis because deficits in these areas would complicate any assessment of apraxia. If a person has a hemiplegia, the unaffected hand is used for testing. Input from the speech-language pathologist is important for establishing an individual’s capacity for basic comprehension via words or gestures. Because of the frequent association of apraxia with aphasia and left hemisphere brain damage, an apraxia screening is included as a part of many aphasia batteries94 used by speech-language pathologists.
The literature20 offers several apraxia assessments used in research, such as the Florida Apraxia Screening Test (FAST),87,88 the Movement Imitation Test,29,30 and the Use of Objects Test.29 The Loewenstein Occupational Therapy Cognitive Assessment (LOTCA)57 includes a praxis subsection, as does the Rivermead Perceptual Assessment Battery,103 both of which serve as screening tools for the disorder. The Santa Clara Valley Medical Center Praxis Test and the Solet Test for Apraxia are two additional evaluation tools developed by occupational therapists.108
A thorough assessment includes functional items presented, such as those shown in Table 25-1,51 and involves both transitive movements (action involving both tool and use, such as writing with an imaginary pen) and intransitive movements (movements for communication, such as waving farewell). Lists of gestures used in assessment are noted in several studies.20,51,85,87,104
TABLE 25-1
Elements of a Comprehensive Apraxia Assessment
| Test Condition | Example |
| Gesture to command | “Show me how you would take off your hat.” (transitive) |
| “Show me how you would throw a kiss.” (intransitive) | |
| Gesture to imitation | “Copy what I do.” Therapist shrugs shoulders. (intransitive) Therapist flips an imaginary coin. (transitive) |
| Gesture in response to seeing the tool | “Show me how you would, seeing the tool, use this object.” Therapist provides screwdriver for display. |
| Gesture in response to seeing the object upon which the tool works | “Show me how you would use this object.” Therapist provides screwdriver and block of wood with screw partially inserted. |
| Actual tool use | “Show me how you would use this object.” Therapist provides screwdriver for use. |
| Imitation of the examiner using the tool | “Copy what I do.” Therapist makes stirring motion, using a spoon. |
| Discrimination between correct and incorrect pantomimed movements | “Is this the correct way to blow out a match?” Therapist pantomimes holding a match in an unsafe manner (e.g., match held upside down, with the head of the match near the palm of hand). |
| Gesture comprehension | “What object am I using?” Therapist pantomimes by shaving face with a razor. |
| Serial acts | “Show me how you would open an imaginary can of soda, pour it into a glass, and take a drink.” |
From Heilman KM, Rothi LJG: Apraxia. In Heilman KM, Valenstein E, editors: Clinical neuropsychology, New York, 1993, Oxford University Press.
Returning to the case of Ms. S, who has severe apraxia, she was first treated by practicing basic motor movements, then she followed a developmental sequence to more advanced functional motor activities. For example, following repetition of basic movement patterns, the client with apraxia progressed to coloring geometric shapes on note cards (felt-tip markers were initially placed in a vertical stand for easy grasp) and gradually to writing exercises. Independent telephone use was important to Ms. S, so a large calculator was used for keystroke practice. She gradually progressed to a disconnected telephone and then to a functional telephone. By the termination of the intervention program, Ms. S was independent in most areas of occupation, although additional time was needed for each activity.
For another client with apraxia, the clinical reasoning process was used in planning the treatment, beginning with spoken instruction for each sequence in the task, written or pictorial instructions, and visual monitoring of her limbs throughout each aspect of the task.20 Another case study of apraxia treatment involved conductive education—that is, breaking the task into smaller units and verbally guiding the sequence.76 The individual improved on targeted tasks, but minimal generalization was noted in everyday occupations across various contexts.
OT interventions for dressing apraxia involves problem solving with the client on effective dressing strategies, such as distinguishing from right and left or from front to back on specific clothing items. An effective strategy is to have the client position the garment the same way each time (e.g., positioning a shirt with the buttons face-up and pants with the zipper face-up). Labels, small buttons, or ribbons can be used as cues to differentiate the front from the back of the garment.108,109
Constructional Disorder
The term constructional disorder is now favored over the previously used term of two- and three-dimensional constructional apraxia since the deficit does not clearly fall within the definition of apraxia.13,20,65 Many occupations depend on visuoconstructional skills, or the ability to organize visual information into meaningful spatial representations. Constructional deficits refer to the inability to organize or assemble parts into a whole, as in putting together block designs (three-dimensional) or drawings (two-dimensional). Constructional deficits can result in significant dysfunction in occupations that require constructional ability, such as dressing, organizing food in a refrigerator, following instructions for assembling a toy, and loading a dishwasher.78,95 Figure 25-3, which shows evidence of left inattention, also demonstrates constructional deficits. An individual acts on his or her contextual environment based on the information he or she perceives. Therefore, deficits in perception become more apparent when a person interacts with the environment in maladaptive ways.

FIGURE 25-3 Example of a two-dimensional constructional disorder and left-sided inattention in a drawing of a house by a retired architect who suffered a right CVA.
Traditional tests of constructional abilities in a two-dimensional mode are the Test of Visual-Motor Skills for Adults,41 the copy administration of the Benton Visual Retention Test,92 and the Rey Complex Figure assessment.65 The latter two tests also are used to evaluate visual memory skills. Use of the Rey Complex Figure has been suggested for a quick screening of visual perceptual function.67 The Three-Dimensional Block Construction8 involves the use of various blocks to copy a design from a three-dimensional model. Nonstandardized tests that may be used are drawing, constructing matchstick designs, assembling block designs, or building a structure to match a model.108 In daily living, occupations such as dressing or setting the table require constructional skills. To perform such tasks successfully, an individual must have integrated visual perception, motor planning, and motor execution.9,46,75,102,109
Several studies have gathered data on the constructional skills of unimpaired subjects for use as a normative reference for persons with CVA and TBI.36,75 In a study of constructional abilities in the well elderly, Fall demonstrated that results are influenced by the type of test administration.36 Subjects tended to score higher on tests that used three-dimensional models as guides for construction than on those that used photographs or drawings. The implications of this finding for occupational therapists are that (1) the type of test administration affects scores, and (2) in teaching persons with constructional disorders, models or demonstrations of desired performance are likely to produce better results than would photographs or drawings.36
The remedial approach to intervention involves the use of perceptual tasks such as paper and pencil activities, puzzles, and three-dimensional craft projects to improve constructional skills. The adaptive approach would include participation in occupational performance and developing compensatory approaches to the functional performance skill impairments. Many areas of occupation are suitable for treatment of constructional deficits, such as folding towels, setting the dinner table, and weeding the garden.
Behavioral Aspects of Perceptual Dysfunction
Some degree of accurate self-awareness and recognition of the effect of the disability on one’s functioning is needed if the person is to invest energy in the therapy process.39 An individual who is unaware of perceptual deficits may be a serious safety risk and may attempt occupations that are well beyond present physical abilities. Denial is often noted in early stages of recovery from CVA or TBI and may serve as a protective coping mechanism that allows the individual to gradually absorb the effect of the injury on his or her functioning. A person’s innate trust of the accuracy of perceptions often is a basis for unrealistic self-confidence; demonstrating to the individual that his or her perceptions are now distorted and no longer trustworthy can profoundly affect the person’s sense of self. A therapist needs to respect and be sensitive to the individual’s sense of self and be prepared to aid the client in understanding the changes in perceptual capacity and in reestablishing an accurate sense of self. Several questionnaires are available to assess an individual’s self-awareness.59 The questionnaires typically are issued to the person with deficits as well as to a family member or close acquaintance. The discrepancies in the two questionnaires are used as a measure of the accuracy of the individual’s insight and serve as the basis for intervention. The individual’s behavior may also be the result of a disorder in executive function.59 See Chapter 26 for additional discussion of this possibility.
An individual who has some degree of awareness of the disability often is depressed, which seems an appropriate response given the effect of perceptual impairments on participation in occupational role performance. The therapist needs to recognize and appreciate this emotional response and assist the individual in achieving an emotional balance to reestablish quality of life through celebrating progress in therapy while acknowledging the impact of the perceptual impairments on participation in occupation.39,86 (See also Chapter 6 on social and psychological aspects.)
1. Describe the effects of visual perception, visual-spatial perception, tactile perception, body schema perception, and motor perception on occupational performance.
2. Compare the advantages and disadvantages of formal perceptual testing and functional assessment in the context of occupational performance.
3. Describe one assessment used to test perceptual impairments in the following areas: visual perception, visual-spatial perception, tactile perception, body schema perception, and motor perception.
4. Describe the two approaches to treatment of perceptual deficits, and give one example of an occupational therapy intervention for each.
5. Describe an intervention for each of the following types of perceptual dysfunction: visual perception, visual-spatial perception, tactile perception, body schema perception, and motor perception.
References
1. Affolter, FD. Perception, interaction, and language: interaction of daily living: the root of development. Berlin: Springer-Verlag; 1987.
2. American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process, second edition. Am J Occup Ther. 2008;62:625–683.
3. Arnadottir, G. Evaluation and intervention with complex perceptual impairment. In: Unsworth C, ed. Cognitive and perceptual dysfunction: a clinical reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
4. Arnadottir, G. Impact of neurobehavioral deficits on activities of daily living. In Gillen G, Burkhardt A, eds.: Stroke rehabilitation: a function-based approach, ed 2, St. Louis: Mosby, 2004.
5. Arnadottir, G. The brain and behavior: assessing cortical dysfunction through activities of daily living. St. Louis: Mosby; 1990.
6. Ashford, JW, et al. Diagnosis of Alzheimer’s disease. In: Kumar V, Eisdorfer C, eds. Advances in the diagnosis and treatment of Alzheimer’s disease. New York: Springer-Verlag, 1998.
7. Ayres, AJ. Sensory integration and learning disorders. Los Angeles: Western Psychological Services; 1972.
8. Baum, B, Hall, K. Relationship between constructional praxis and dressing in the head injured adult. Am J Occup Ther. 1981;35:438.
9. Benton, AL, Fogel, ML. Three-dimensional constructional praxis: a clinical test. Arch Neurol. 1962;7:347.
10. Benton, AL, Schultz, LM. Observations of tactile form perception (stereognosis) in pre-school children. J Clin Psychol. 1949;5:359.
11. Benton, AL, Sivan, AB. Disturbances of the body schema. In: Heilman KM, Valenstein E, eds. Clinical neuropsychology. New York: Oxford University Press, 1993.
12. Benton, AL, et al. Contributions to neuropsychological assessment: a clinical manual. Oxford: Oxford University Press; 1983.
13. Benton, AL, Tranel, D. Visuoperceptual, visuospatial, and visuoconstructive disorders. In: Heilman KM, Valenstein E, eds. Clinical neuropsychology. New York: Oxford University Press, 1993.
14. Binetti, G, et al. Visual and spatial perceptions in the early phase of Alzheimer’s disease. Neuropsychology. 1998;12(1):29–33.
15. Blakemore, C, Movshon, JA. Sensory system: introduction. In: Gazzaniga MS, ed. The cognitive neurosciences. London: MIT Press, 1996.
16. Brown, T, Mullins, E, Stagnitti, K. The reliability of performance of healthy adults on three visual perceptual tests. Br J Occup Ther. 2008;71(10):438–447. [16].
17. Brown, GT, Rodger, S, Davis, A. Motor-Free Visual Perception Test-Revised: A review and critique. Br J Occup Ther. 2003;66:159–167.
18. Brown, GT, Rodger, S, Davis, A. Test of Visual Perceptual Skills-Revised: A review and critique. Scand J Occup Ther. 2003;10:3–19.
19. Bruce, V, Young, A. In the eye of the beholder: the science of face perception. Oxford: Oxford University Press; 1998.
20. Butler, JA. Evaluation and intervention with apraxia. In: Unsworth C, ed. Cognitive and perceptual dysfunction: a clinical reasoning approach to evaluation and intervention. Philadelphia: FA Davis, 1999.
21. Calder, AJ, et al. Facial emotion recognition after bilateral amygdala damage: differentially severe impairment of fear. Cogn Neuropsychol. 1996;13:699.
22. Caplan, BM, Romans, S. Assessment of spatial abilities. In: Goldstein G, Nussbaum PD, Beers SR, eds. Neuropsychology. New York: Plenum Press, 1998.
23. Chusid, JG. Correlative neuroanatomy and functional neurology, ed 19. Los Altos, CA: Lange Medical Publications; 1985.
24. Colarusso, RP, Hammill, DD. Motor-Free Visual Perception Test, ed 3. Novato, CA: Academic Therapy Publications; 2003.
25. Cooke, DM, McKenna, K, Fleming, J, Darnell, R. Criterion validity of the occupational therapy adult perceptual screening test. Scand J Occup Ther. 2006;13:38–44.
26. DeJong, R. The neurologic examination. New York: Paul B. Hoeber; 1958.
27. Dellon, AL. Evaluation of sensibility and re-education of sensation in the hand. Baltimore, MD: Williams & Wilkins; 1981.
28. De Renzi, E. Methods of limb apraxia examination and their bearing on the interpretation of the disorder. In: Roy EA, ed. Neuropsychological studies of apraxia and related disorders. Amsterdam: North-Holland, 1985.
29. De Renzi, E, et al. Modality-specific and supramodal mechanisms of apraxia. Brain. 1982;105:301.
30. De Renzi, E, et al. Imitating gestures: a quantitative approach to ideomotor apraxia. Arch Neurol. 1980;37:6.
31. De Renzi, E, et al. Ideational apraxia: a quantitative study. Neuropsychologia. 1968;6:41.
32. Donnelly, SM, et al. The Rivermead Perceptual Assessment Battery: its relationship to selected functional activities. Br J Occup Ther. 1998;61:27.
33. Edmans, JA, Lincoln, NB. Treatment of visual perceptual deficits after stroke: single case studies on four patients with right hemiplegia. Br J Occup Ther. 1991;54:139.
34. Eggers, O. Occupational therapy in the treatment of adult hemiplegia. Rockville, MD: Aspen Systems; 1984.
35. Ellis, AW, Young, AW. Human cognitive neuropsychology. Hillsdale, NJ: Lawrence Erlbaum; 1988.
36. Fall, CC. Comparing ways of measuring constructional praxis in the well elderly. Am J Occup Ther. 1987;41:500.
37. Farber, SD. Neurorehabiliation, a multisensory approach. Philadelphia: WB Saunders; 1982.
38. Fisher, AG. Assessment of motor and process skills. Fort Collins, CO: Three Star Press; 1995.
39. Fleming, J, Strong, J. Self-awareness of deficits following acquired brain injury: considerations for rehabilitation. Br J Occup Ther. 1995;58:55.
40. Gardner, H. Frames of mind: the theory of multiple intelligences. New York: Basic Books; 1983.
41. Gardner, MF. The Test of Visual-Motor Skills (TVMS). Burlingame, CA: Psychological and Educational Publications; 1992.
42. Gardner, MF. The Test of Visual Perceptual Skills—Revised (TVPS-R). Hydesville, CA: Psychological and Educational Publications; 1997.
43. Geschwind, N. The apraxias: neural mechanisms of disorders of learned movement. Am Sci. 1975;63:188.
44. Gilroy, J, Meyer, JS. Medical neurology. London: Macmillan; 1969.
45. Glosser, G, Gallo, J, Duda, N, et al. Visual perceptual functions predict instrumental activities of daily living in patients with dementia. Neuropsychiatric, Neuropsychology, & Behavioral Neurology. 2002;15(3):198–202.
46. Goodglass, H, Kaplan, E. Assessment of aphasia and related disorders, ed 2. Philadelphia: Thomas; 1972.
47. Gordon, WA, et al. Perceptual remediation in patients with right brain damage: a comprehensive program. Arch Phys Med Rehabil. 1985;66:353.
48. Haaland, KY, Harrington, DL. Neuropsychological assessment of motor skills. In: Goldstein G, Nussbaum PD, Beers SR, eds. Neuropsychology. New York: Plenum Press, 1998.
49. Head, H, et al. Studies in neurology. London: Oxford University Press; 1920.
50. Hecaen, H, et al. The syndrome of apractognosis due to lesions of the minor cerebral hemisphere. Arch Neurol Psychiat. 1956;75:400.
51. Heilman, KM, Rothi, LJG. Apraxia. In: Heilman KM, Valenstein E, eds. Clinical neuropsychology. New York: Oxford University Press, 1993.
52. Heilman, KM, et al. Conceptual apraxia from lateralized lesions. Neurology. 1997;49:457.
53. Hooper, HE. Hooper Visual Organization Test. Los Angeles: Western Psychological Association; 1983.
54. Humphreys, GW, Riddoch, MJ. To see but not to see: a case study of visual agnosia. Hove, UK: Lawrence Erlbaum; 1987.
55. Humphreys, GW, Riddoch, MJ. Visual object processing in normality and pathology: implications for rehabilitation. In: Riddoch MJ, Humphreys GW, eds. Cognitive neuropsychology and cognitive rehabilitation. Hove, UK: Lawrence Erlbaum, 1994.
56. Ishihara, K, Ishihara, S, Nagamachi, M, et al. Independence of older adults in performing instrumental activities of daily living (IADLs) and the relation of this performance to visual abilities. Theoretical Issues in Ergonomics 34 Science. 2004;5(3):198–213.
57. Itzkovich, M, et al. The Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) manual. Pequannock, NJ: Maddock; 1990.
58. Katz N, ed. Cognition and occupation in rehabilitation, ed 2, Bethesda, MD: AOTA Press, 2005.
59. Katz, N, Hartman-Maeir, A. Metacognition: the relationships of awareness and executive functions to occupational performance. In: Katz N, ed. Cognition and occupation in rehabilitation: cognitive models for intervention in occupational therapy. Bethesda, MD: American Occupational Therapy Association, 1998.
60. Kent, BE. Sensory-motor testing: the upper limb of adult patients with hemiplegia. Phys Ther. 1965;45:550.
61. Kimura, D, Archibald, Y. Motor functions of the left hemisphere. Brain. 1974;97:337.
62. Kline, DW, Scialfa, CT. Visual and auditory aging. In Birren JE, Schaie KW, eds.: Handbook of the psychology of aging, ed 4, San Diego, CA: Academic Press, 1996.
63. Kritchevsky, M. The elementary spatial functions of the brain. In: Stiles-Davis J, Kritchevsky M, Bellugi U, eds. Spatial cognition: brain bases and development. Hillsdale, NJ: Lawrence Erlbaum, 1988.
64. Law, M, et al. The Canadian Occupational Performance Measure, ed 3. Ottawa, ONT: CAOT; 1998.
65. Lezak, MD. Neuropsychological assessment. New York: Oxford University Press; 1995.
66. Likert, R, Quasha, WH. The revised Minnesota Paper Form Board Test. New York: Psychological Corporation; 1970.
67. Lincoln, NB, et al. The Rey figure copy as a screening instrument for perceptual deficits after stroke. Br J Occup Ther. 1998;61:33.
68. Lincoln, NB, et al. An evaluation of perceptual retraining. Internat Rehabil Med. 1985;7:99.
69. MacDonald, J. An investigation of body scheme in adults with cerebral vascular accident. Am J Occup Ther. 1960;14:72.
70. Martin, NA. Test of Visual Perceptual Skills, ed 3. Novato, CA: Academic Therapy; 2006.
71. Mazer, BL, et al. Predicting ability to drive after stroke. Arch Phys Med Rehabil. 1998;79:743.
72. Mercier, LAT, Audet, T, Hebert, R. Impact on motor, cognitive, and perceptual disorders on abilities to performance activities daily after stroke. Stroke. 2001;32(11):2602–2608.
73. Mercier, L, et al. Motor-free visual perception test—vertical (MVPT-V). Novato, CA: Academic Therapy Publications; 1997.
74. Neistadt, ME. A critical analysis of occupational therapy approaches for perceptual deficits in adults with brain injury. Am J Occup Ther. 1990;44:299.
75. Neistadt, ME. Normal adult performance on constructional praxis training tasks. Am J Occup Ther. 1989;43:448.
76. Neistadt, ME. Occupational therapy treatments for constructional deficits. Am J Occup Ther. 1992;46:141.
77. Neistadt, ME. Perceptual retraining for adults with diffuse brain injury. Am J Occup Ther. 1994;48:225.
78. Neistadt, ME. The relationship between constructional and meal preparation skills. Arch Phys Med Rehabil. 1993;74:144.
79. Newcombe, F, Ratcliff, G. Disorders of visuospatial analysis. In: Boller, F, Grafman, J, eds. Handbook of neuropsychology, vol 2. Amsterdam: Elsevier Science; 1989.
80. Occupational Therapy Department, Rancho Los Amigos Hospital. Upper extremity sensory evaluation: a manual for occupational therapists. Downey, CA: Rancho Los Amigos Hospital; 1985.
81. Ochipa, C, et al. Conceptual apraxia in Alzheimer’s disease. Brain. 1992;115:1061.
82. Ogden, JA. Spatial abilities and deficits in aging and age-related disorders. In: Boller, F, Grafman, J, eds. Handbook of neuropsychology, vol 4. Amsterdam: Elsevier Science; 1990.
83. Pick, HL. Perception, locomotion, and orientation. In: Welsh RL, Blasch BB, eds. Foundations of orientation and mobility. New York: American Foundation for the Blind, 1980.
84. Pilgrim, E, Humphreys, GW. Rehabilitation of a case of ideomotor apraxia. In: Riddoch MJ, Humphreys GW, eds. Cognitive neuropsychology and cognitive rehabilitation. Hove, UK: Lawrence Erlbaum, 1994.
85. Poole, JL, et al. The mechanisms for adult-onset apraxia and developmental dyspraxia: an examination and comparison of error patterns. Am J Occup Ther. 1997;51:339.
86. Radomski, MV. There is more to life than putting on your pants. Am J Occup Ther. 1995;49:487.
87. Rothi, LJG, Heilman, KM. Acquisition and retention of gestures by apraxic patients. Brain Cogn. 1984;3:426.
88. Rothi, LJG, Heilman, KM. Ideomotor apraxia: gestural discrimination, comprehension, and memory. In: Roy EA, ed. Neuropsychological studies of apraxia and related disorders. Amsterdam: North-Holland, 1985.
89. Rubio, KB, Van Deusen, J. Relation of perceptual and body image dysfunction to activities of daily living after stroke. Am J Occup Ther. 1995;49:551.
90. Sacks, O. An anthropologist on Mars. New York: Knopf; 1995.
91. Sacks, O. The man who mistook his wife for a hat and other clinical tales. New York: Summit Books; 1985.
92. Sivan, AB. The Benton Visual Retention Test. San Antonio, TX: Psychological Corporation; 1992.
93. Sundet, K, et al. Neuropsychological predictors in stroke rehabilitation. J Clin Exp Neuropsychol. 1988;10:363.
94. Tate, RL, McDonald, S. What is apraxia? The clinician’s dilemma. Neuropsychol Rehabil. 1995;5:273.
95. Titus, MN, et al. Correlation of perceptual performance and activities of daily living in stroke patients. Am J Occup Ther. 1991;45:410.
96. Toglia, J. A dynamic interactional approach to cognitive rehabilitation. In Katz N, ed.: Cognition and occupation across the lifespan: models for intervention in occupational therapy, ed 2, Bethesda, MD: AOTA Press, 2005.
97. Toglia, J. Generalization of treatment: a multi-contextual approach to cognitive-perceptual impairment in the brain-injured adult. Am J Occup Ther. 1991;45:505.
98. Tsurumi, K, Todd, V. Theory and guidelines for visual task analysis and synthesis. In: Scheiman M, ed. Understanding and managing vision deficits: a guide for occupational therapists. Thorofare, NJ: Slack, 1997.
99. Warren, M. A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury: Part I. Am J Occup Ther. 1993;47:42.
100. Warren, M. A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury: Part II. Am J Occup Ther. 1993;47:55.
101. Warren, M. Relationship of constructional apraxia and body scheme disorders to dressing performance in adult CVA. Am J Occup Ther. 1981;35:431.
102. Warrington, E, et al. Drawing ability in relation to laterality of lesion. Brain. 1966;89:53.
103. Whiting, S, et al. RPAB—Rivermead Perceptual Assessment Battery. Windsor, UK: NFER-Nelson; 1985.
104. Willis, L, et al. Ideomotor apraxia in early Alzheimer’s disease: time and accuracy measures. Brain Cogn. 1998;38:220.
105. York, CD, Cermack, SA. Visual perception and praxis in adults after stroke. Am J Occup Ther. 1995;49:543.
106. Young, AW, et al. Face perception after brain injury: selective impairments affecting identity and expression. Brain. 1993;116(Pt 4):941.
107. Zoltan, B. Remediation of visual-perceptual and perceptual-motor deficits. In: Rosenthal M, Griffith ER, Bond MR, et al, eds. Rehabilitation of the adult and child with traumatic brain injury. Philadelphia: FA Davis, 1990.
108. Zoltan, B, Vision, perception, and cognition. (rev). ed 3, Thorofare, NJ, Slack, 1996.
109. Zoltan, B, et al. Perceptual and cognitive dysfunction in the adult stroke patient,, ed 2. Thorofare, NJ: Slack; 1986.
Gentile, M. Functional visual behavior in adults: An occupational therapy guide to evaluation and treatment options, ed 2. Bethesda, MD: AOTA Press; 2005.
Scheiman, M. Understanding and managing vision deficits: a guide for occupational therapists. Thorofare, NJ: Slack; 1977.
Zoltan, B. Vision, perception, and cognition: a manual for the evaluation and treatment of the neurologically impaired adult. Thorofare, NJ: Slack; 2005.