Cerebrovascular Accident/Stroke
Evaluation and intervention procedures for clients who sustained a stroke
Top-down approach to assessment
Effects of neurologic deficits on performance in areas of occupation
Adopting a framework for intervention
Functional limitations commonly observed after stroke
Inability to perform chosen occupations while seated
Inability to engage in chosen occupations while standing
Inability to communicate secondary to language dysfunction
Inability to perform chosen occupations secondary to neurobehavioral/cognitive-perceptual impairments
Inability to perform chosen tasks secondary to upper extremity dysfunction
Inability to perform chosen tasks secondary to visual impairment
After studying this chapter, the student or practitioner will be able to do the following:
1 List and describe evaluation procedures for survivors of a stroke.
2 Discuss the neuropathology of a stroke.
3 Identify risk factors associated with a stroke.
4 Identify multiple factors (impaired client factors, performance skills, etc.) that impede performance in areas of occupation after a stroke.
5 Describe evaluation procedures for impaired body functions related to neurobehavioral deficits.
6 Identify balance strategies (a body function) that support performance of areas of occupation.
7 Describe the motor control dysfunction (impaired body function) associated with stroke.
8 Identify standardized stroke assessments for multiple areas of dysfunction.
9 Apply a client-centered approach to stroke rehabilitation.
10 Develop comprehensive occupation-based treatment plans to remediate or compensate for underlying deficits.
Introduction
This chapter focuses on occupational therapy (OT) assessment and intervention for individuals who have sustained a stroke. Specifically, it focuses on improving participation in chosen areas of occupation. After a person has a stroke, multiple client factors and performance skills are affected and potentially limit participation and engagement in occupation.5 These multiple problems are addressed throughout this chapter.
Cerebrovascular accidents (CVAs), or strokes, continue to be a national health problem despite recent advances in medical technology. The American Heart Association4 publishes stroke statistics that demonstrate the severity of this problem. Selected statistics include the following4:
• Stroke ranks as the third leading cause of death behind heart disease and cancer.
• On average, a U.S. citizen suffers a stroke every 40 seconds; every 4 minutes someone dies of a stroke.
• Each year, 795,000 people suffer a new or recurrent stroke. Approximately 610,000 strokes are first attacks and 185,000 are recurrent.
• The prevalence of stroke in 2006 was 6,400,000.
• Of people who suffer a stroke, 28% are younger than 65 years. For people older than 55, the incidence of stroke more than doubles with each successive decade.
• The incidence of stroke is about 1.25 times higher in men than in women.
• The aftermath of a stroke is a substantial public health and economic problem, with stroke being a leading cause of serious, long-term disability in the United States.
• Stroke accounts for more than half of all clients hospitalized for acute neurologic disease.
• Among long-term clients who sustained a stroke, 50% have hemiparesis, 30% cannot walk, 26% are found to be dependent in activity of daily living (ADL) scales, 19% are aphasic, 35% are clinically depressed, and 26% require home nursing care.
Obviously, stroke rehabilitation as a practice area for occupational therapists is a specialization that crosses multiple settings, from the intensive care unit to community-based programs.
Definition of Stroke
A CVA, or stroke, is a complex dysfunction caused by a lesion in the brain. The World Health Organization100 defines stroke as an “acute neurologic dysfunction of vascular origin with symptoms and signs corresponding to the involvement of focal areas of the brain.” Stroke results in upper motor neuron dysfunction that produces hemiplegia, or paralysis of one side of the body, including the limbs and trunk and sometimes the face and oral structures that are contralateral to the hemisphere of the brain with the lesion. Thus, a lesion in the left cerebral hemisphere (left CVA) produces right hemiplegia. Conversely, a lesion in the right cerebral hemisphere (right CVA) produces left hemiplegia. When reference is made to the client’s disability as right or left hemiplegia, the reference is to the paralyzed side of the body and not to the locus of the lesion.
Accompanying the motor paralysis may be a variety of dysfunctions other than the motor paralysis. Some of these dysfunctions include sensory disturbances, cognitive and perceptual dysfunction, visual disturbances, personality and intellectual changes, and a complex range of speech and associated language disorders. The neurologic deficits must persist longer than 24 hours to be labeled a CVA.
Causes of Stroke
Bartels describes a stroke as “essentially a disease of the cerebral vasculature in which failure to supply oxygen to the brain cells, which are the most susceptible to ischemic damage, leads to their death. The syndromes that lead to stroke comprise two broad categories: ischemic and hemorrhagic stroke.”10 Ischemic strokes account for the majority of strokes, whereas hemorrhagic strokes account for less.
Ischemia
Ischemia refers to insufficient blood flow to the brain to meet metabolic demand. Ischemic strokes may be the result of embolism to the brain from cardiac or arterial sources. Cardiac sources include atrial fibrillation (pooling of blood in the dysfunctional atrium leads to the production of emboli), sinoatrial disorders, acute myocardial infarction, endocarditis, cardiac tumors, and valvular (both native and artificial) disorders. Cerebral ischemia caused by perfusion failure occurs with severe stenosis of the carotid and basilar arteries, as well as with microstenosis of the small deep arteries.4,10
Age, gender, race, ethnicity, and heredity are considered nonmodifiable risk factors for ischemic strokes. In contrast, a major focus of stroke prevention and education programs is on the potentially modifiable risk factors discussed in the following list4,50:
1. Hypertension is considered the single most important modifiable risk factor for ischemic stroke. Those with blood pressure lower than 120/80 have about half the lifetime risk for stroke as those with high blood pressure.4
2. Management of cardiac diseases, particularly atrial fibrillation, mitral stenosis, and structural abnormalities (patent foramen ovale and atrial septal aneurysm), can reduce the risk for stroke.
3. Management of diabetes and glucose metabolism can also reduce the risk for stroke.
4. Cigarette smoking increases the relative risk for ischemic stroke nearly two times.
5. Although excessive use of alcohol is a risk factor for many other diseases, moderate consumption of alcohol may reduce the incidence of cardiovascular disease, including stroke.
6. Use of illegal drugs, particularly cocaine, is commonly associated with stroke. Other drugs linked to stroke include heroin, amphetamines, LSD, PCP, and marijuana.
7. Lifestyle factors such as obesity, physical inactivity, diet, and emotional stress are associated with risk for stroke.
“The realization that the probability of stroke is increased several fold by the presence of multiple risk factors may help the patient to fully appreciate the need for serious risk factor management.”4 The responsibility for stroke prevention education (including prevention of recurrence) falls on each member of the stroke rehabilitation team.
Hemorrhage
Hemorrhagic strokes include subarachnoid and intracerebral hemorrhages, which account for only 13% of the total number of strokes.4 This type of stroke has numerous causes. The four most common are deep hypertensive intracerebral hemorrhages, ruptured saccular aneurysms, bleeding from arteriovenous malformations, and spontaneous lobar hemorrhages.58
Related Syndromes
Cerebral anoxia and aneurysm can also result in hemiplegia. Some of the treatment approaches outlined in this chapter may be applicable to hemiplegia resulting from causes other than CVA or stroke, such as head injuries, neoplasms, and infectious diseases of the brain.
Transient Ischemic Attacks
Vascular disease of the brain can result in a completed stroke or transient ischemic attacks (TIAs). A TIA is characterized by mild, isolated, or repetitive neurologic symptoms that develop suddenly, last from a few minutes to several hours but not longer than 24 hours, and clear completely. A TIA is seen as a sign of an impending stroke.4 Most TIAs occur in people with atherosclerotic disease. Of those who experience TIAs and do not seek treatment, an estimated third will sustain a completed stroke, another third will continue to have additional TIAs without a stroke, and a third will experience no further attacks.78 If the TIA is caused by extracranial vascular disease, surgical intervention to restore vascular flow (carotid endarterectomy) may be effective in preventing the stroke and resultant disability.
Effects of Stroke
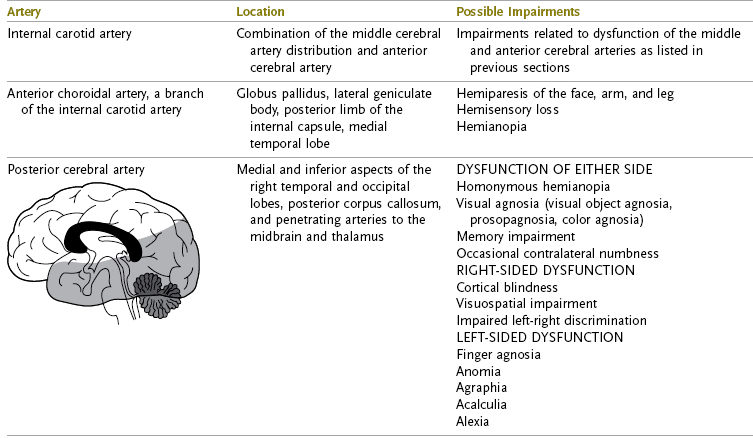
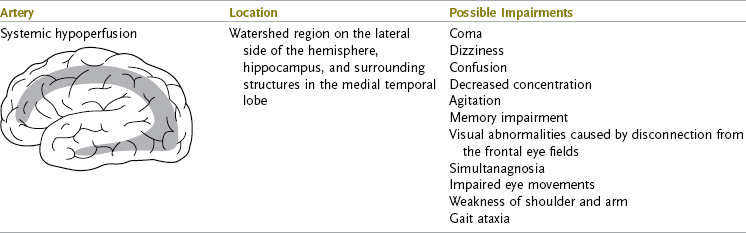
The outcome of a stroke depends on which artery supplying the brain was involved (Figure 33-1). Stroke diagnostic workups help localize the lesion and find a cause of the stroke. Techniques include cerebrovascular imaging such as computed tomography (CT), magnetic resonance imaging (MRI), and more recently, positron emission tomography (PET) and single-photon emission computed tomography (SPECT).10 The information collected with these techniques (e.g., the extent of damage and location of the lesion) may help the occupational therapist identify neurologic deficits that affect function. The information may also help the therapist develop hypotheses regarding recovery and plan appropriate treatment. Initial information may be collected during a medical record review that focuses on the chief complaint of the client on admission, previous medical and surgical history, results of diagnostic tests, and current pharmacologic management. The following section and Tables 33-1 and 33-2 explain patterns of impairment resulting from stroke in both the cortical and subcortical areas.
TABLE 33-1
Cerebral Artery Dysfunction: Cortical Involvement and Patterns of Impairment
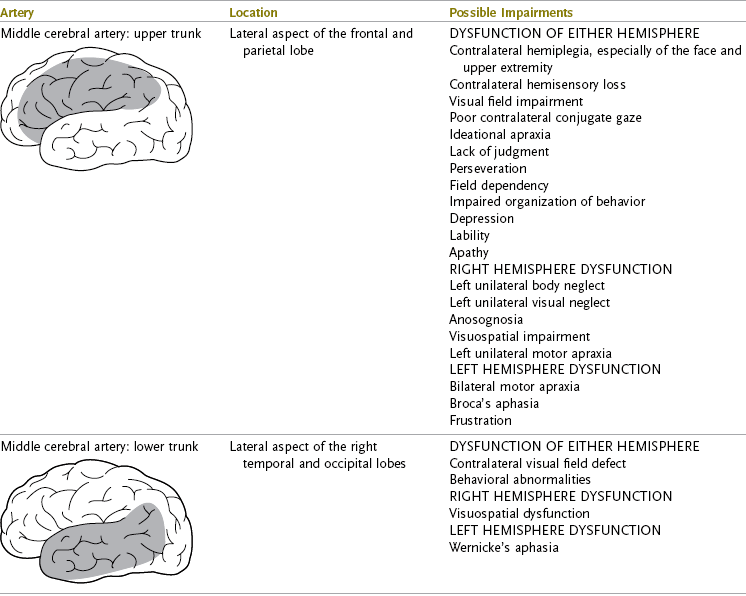


From Arnadottir G: Impact of neurobehavioral deficits of activities of daily living. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.
TABLE 33-2
Cerebrovascular Dysfunction in Noncortical Areas: Patterns of Impairment
From Arnadottir G: Impact of neurobehavioral deficits of activities of daily living. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.
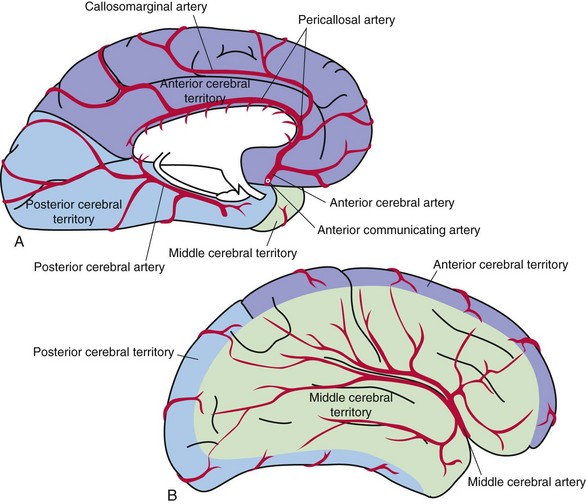
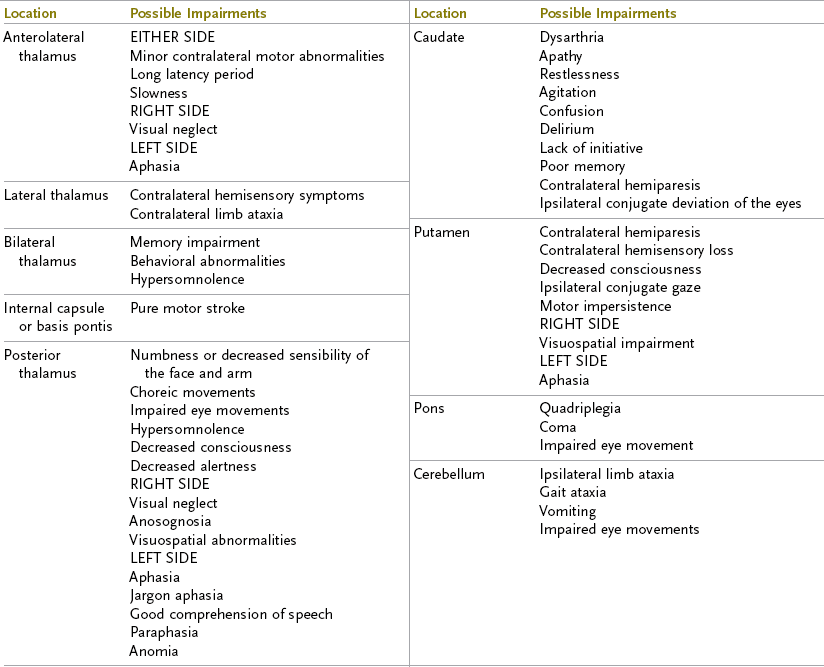
FIGURE 33-1 Blood supply to the brain. The middle cerebral, anterior cerebral, and posterior cerebral arteries supply blood to the cerebral hemispheres. A, Medial surface. B, Lateral surface. (Modified from Mettler FA: Neuroanatomy, ed 2, St. Louis, 1948, Mosby. In Nolte J: The human brain: an introduction to its functional anatomy, ed 6, Philadelphia, 2009, Elsevier.)
Internal Carotid Artery
In the absence of adequate collateral circulation, occlusion of the internal carotid artery results in contralateral hemiplegia, hemianesthesia, and homonymous hemianopia.6,10 Additionally, involvement of the dominant hemisphere (i.e., the cerebral hemisphere containing the representation of speech/language and controlling the arm and leg used preferentially in skilled movements, usually the left hemisphere) is associated with aphasia, agraphia or dysgraphia, acalculia or dyscalculia, right-left confusion, and finger agnosia. Involvement of the nondominant hemisphere is associated with visual perceptual dysfunction, unilateral neglect, anosognosia, constructional or dressing apraxia, attention deficits, and loss of topographic memory.
Middle Cerebral Artery
Involvement of the middle cerebral artery (MCA) is the most common cause of stroke.7,10,21 Ischemia in the area supplied by the MCA results in contralateral hemiplegia with greater involvement of the arm, face, and tongue; sensory deficits; contralateral homonymous hemianopia; and aphasia if the lesion is in the dominant hemisphere. There is pronounced deviation of the head and neck toward the side on which the lesion is located.22,31 Perceptual deficits such as anosognosia, unilateral neglect, impaired vertical perception, visual spatial deficits, and perseveration are seen if the lesion is in the nondominant hemisphere.6
Anterior Cerebral Artery
Occlusion of the anterior cerebral artery (ACA) produces contralateral lower extremity weakness that is more severe than that of the arm. Apraxia, mental changes, primitive reflexes, and bowel and bladder incontinence may be present. Total occlusion of the ACA results in contralateral hemiplegia with severe weakness of the face, tongue, and proximal arm muscles and marked spastic paralysis of the distal end of the lower extremity. Cortical sensory loss is present in the lower extremity. Intellectual changes such as confusion, disorientation, abulia, whispering, slowness, distractibility, limited verbal output, perseveration, and amnesia may be seen.6,10
Posterior Cerebral Artery
The scope of posterior cerebral artery (PCA) symptoms is potentially broad and varied because this artery supplies the upper brainstem region, as well as the temporal and occipital lobes. Possible results of PCA involvement depend on the arterial branches affected and the extent and area of cerebral compromise. Some possible outcomes are sensory and motor deficits, involuntary movement disorders (e.g., hemiballism, postural tremor, hemichorea, hemiataxia, intention tremor), memory loss, alexia, astereognosis, dysesthesia, akinesthesia, contralateral homonymous hemianopia or quadrantanopia, anomia, topographic disorientation, and visual agnosia.6,10,31
Cerebellar Artery System
Occlusion of the cerebellar artery results in ipsilateral ataxia, contralateral loss of pain and temperature sensitivity, ipsilateral facial analgesia, dysphagia and dysarthria caused by weakness of the ipsilateral muscles of the palate, nystagmus, and contralateral hemiparesis.6,10,22,31
Vertebrobasilar Artery System
A stroke in the vertebrobasilar artery system affects brainstem functions. The outcome of the stroke is some combination of bilateral or crossed sensory and motor abnormalities, such as cerebellar dysfunction, loss of proprioception, hemiplegia, quadriplegia, and sensory disturbances, along with unilateral or bilateral involvement of cranial nerves III to XII.
Medical Management
Specific treatment of stroke depends on the type and location of the vascular lesion, the severity of the clinical deficit, concomitant medical and neurologic problems, availability of technology and personnel to administer special types of treatment, and the cooperation and reliability of the client.
Early medical treatment involves maintenance of an open airway, hydration with intravenous fluids, and treatment of hypertension. Appropriate steps should be taken to evaluate and treat coexisting cardiac or other systemic diseases. Measures should be taken to prevent the development of deep venous thrombosis (DVT). DVT is the formation of a blood clot (thrombus) in a deep vein, usually in the lower extremity, a common risk in clients who have prolonged periods of bedrest and immobility. The incidence of DVT in individuals with stroke ranges from 22% to 73%. Emboli that are released from deep veins and subsequently lodge in the lungs are referred to as pulmonary emboli. Pulmonary embolism is the most common cause of death in the first 30 days after a stroke.10,20
The physician oversees routine surveillance for thrombosis, which includes daily evaluation of leg temperature, color, circumference, tenderness, and appearance. Preventive treatments of DVT may involve medication, the use of elastic stockings, the use of reciprocal compression devices, and early mobilization of the client.
Respiratory problems and pneumonia may complicate the early post-stroke course. The National Survey of Stroke reported that a third of clients who had sustained strokes also had respiratory infections.77
Symptoms are a low-grade fever and increased lethargy. Medical management involves the administration of fluids and antibiotics, aggressive pulmonary hygiene, and mobilization of the client. Ventilatory insufficiency is a major factor contributing to the high frequency of pneumonia. The hemiparesis associated with stroke involves the muscles of respiration. Exercise programs that involve strengthening and endurance training of both the inspiratory and expiratory muscles help improve breathing and cough effectiveness and reduce the frequency of pneumonia.20
Cardiac disease is another frequently occurring condition that complicates the post-stroke course. The stroke itself may cause the cardiac abnormality, or the client may have had a pre-existing cardiac condition. The former is treated in the same manner as any new cardiac diagnosis. A pre-existing cardiac condition is re-evaluated and the treatment regimen modified as appropriate. Monitoring of the heart rate, blood pressure, and electrocardiogram (ECG) during self-care evaluations is frequently indicated to determine the cardiac response to activity.
During the acute phase, bowel and bladder dysfunction is common. The physician is responsible for ordering a specific bowel program that includes a time schedule, adequate fluid intake, stool softeners, suppositories, oral laxatives, and medications or procedures to treat fecal impaction. A timed or scheduled toilet program is essential in treating urinary incontinence. Catheterization may be necessary during stroke rehabilitation.
Evaluation and Intervention Procedures for Clients Who Sustained a Stroke
Tables 33-1 and 33-2 provide information related to patterns of impairments that are typically observed and that vary depending on the area of the brain that has been damaged. The location of the stroke is determined by CT or MRI and is generally documented in the medical record. Understanding this information is the first step of the evaluation process; it should take place before meeting the client and helps the therapist focus his or her evaluation procedures and begin to understand which client factors are impaired and affecting performance in areas of occupation.
For example, Jasmine has documented damage in her right frontal and parietal lobes (most likely secondary to MCA occlusion). Patterns of impairment that are typically observed with this type of stroke include contralateral motor loss, contralateral sensory loss, difficulty interpreting spatial relationships (e.g., depth/distance, foreground from background), decreased attention or neglect of left-sided information (personal and extrapersonal), and left limb motor-planning deficits. These impairments may in turn affect Jasmine’s ability to engage in meaningful areas of occupation. Her sensory-motor loss may prevent her from fulfilling her role as a mother (e.g., assisting her child in the bath, lifting her son into the crib, preparing meals) and as a worker (e.g., typing, filing). Simultaneously, her attention deficits (left-sided neglect) will make driving unsafe, interfere with self-care and care of her child, affect her computer use (e.g., finding information on the left side of the screen), and impede her ability to manage her household (e.g., read and write bills and checks, prepare meals.)
Typically, a client’s clinical findings immediately after a stroke (the acute stage) represent the worst-case scenario. In other words, once the stroke is complete and the client who sustained the stroke is medically stabilized, the lesion is considered static or not progressive. At this point, a client who sustained a stroke may exhibit little to no contralateral motor function (hemiparesis or hemiplegia) because of severe weakness, no response to contralateral sensory stimuli, and a severe attention deficit; the client may also require assistance performing his or her job. Fortunately, barring another neurologic insult, the client is usually expected to improve from both a neurologic and functional perspective. Unfortunately, predicting the amount of improvement and the length of time necessary for improvement to take place is difficult. Clinicians generally agree that the first 3 to 6 months after a stroke is the most crucial time and that the greatest improvement takes place during this period. This time frame remains controversial and should be used only as a guideline. For example, more studies87 have documented improvements in upper extremity (UE) function in clients who sustained a stroke many years earlier. It is important to note that some clients may recover only slightly and slowly whereas others may recover fully.
Given this information, it is important to understand that neurologic recovery and functional recovery are different aspects to consider. A motor control (i.e., the process that must be performed to achieve movement) example will be used to illustrate this point. Clients A and B may share similar findings (no motor function on the left side of the body) immediately after experiencing a stroke. Client A may recover substantial motor function and resume engagement in previous occupations such as shopping and dressing with few residual impairments (perhaps a “limp” or mild clumsiness) resulting from the stroke. Client B may not benefit from the same level of neurologic motor recovery and yet still be able to resume engagement in previous occupations by using adaptive methods. Dressing may require learning new one-handed techniques, wearing clothing with a looser fit, and using equipment such as a reacher. Shopping may be accomplished with the use of powered mobility (e.g., scooter or wheelchair), an ankle-foot orthotic and a cane, or the Internet. Despite these differences, both client A and client B are able to participate in meaningful occupations.
Client-Centered Assessments
“Client-centered practice is an approach to providing occupational therapy which embraces a philosophy of respect for, and partnership with, people receiving services. Client-centered practice recognizes the autonomy of individuals, the need for client choice in making decisions about occupational needs, the strengths clients bring to a therapy encounter, the benefits of client-therapist partnership, and the need to ensure that services are accessible and fit the context in which a client lives.”63
Law and colleagues62 and Pollack73 suggest that therapists implementing this approach to evaluation include the following concepts:
1. Recognizing that recipients of OT are uniquely qualified to make decisions about their occupational functioning
2. Offering the client a more active role in defining goals and desired outcomes
3. Making the client-therapist relationship an interdependent one to enable the solution of performance dysfunction
4. Shifting to a model in which occupational therapists work with clients to enable them to meet their own goals
5. Evaluation (and intervention) focusing on the contexts in which clients live, their roles and interests, and their culture
6. Allowing the client to be the “problem definer” so that the client will in turn become the “problem solver”
7. Allowing the client to evaluate his or her own performance and set personal goals62,73
Through the use of these strategies, the evaluation process becomes more focused and defined, clients become immediately empowered, the goals of therapy are understood and agreed on, and a client-tailored treatment plan may be established. The Canadian Occupational Performance Measure63 (COPM) is a standardized tool that uses a client-centered approach to allow the recipient of treatment to identify areas of difficulty, rate the importance of each area, and rate his or her satisfaction with current performance. It is a particularly useful tool to use with clients who sustained a stroke because of the multiple and extensive problems that this population experiences in performance of areas of occupation.
The COPM would be a good assessment to use with Jasmine. It would give the occupational therapist insight into the occupations that should be prioritized, assist in goal writing, and facilitate treatment planning. In addition, use of the COPM would empower Jasmine as an active participant in the rehabilitation process. When Jasmine completed the COPM, the results identified toilet transfers, computer use, grooming, feeding, and child care as the occupations that she wanted to pursue first—in other words, these occupations would be the focus of her initial OT. Jasmine indicated that gaining mastery in the occupations would make her feel better about herself (“boost my self-esteem”) and give her hope that she could return to work (“and provide for my child”).
Top-Down Approach to Assessment
A top-down approach to the assessment process has been described in the literature92 and is applicable to the evaluation of clients who sustained a stroke. Principles of this approach include the following:
1. Inquiry into role competency and meaningfulness is the starting point for evaluation.
2. Inquiry is focused on the roles that are important to the client who sustained a stroke, particularly those in which the client was engaged before the stroke.
3. Any discrepancy of roles in the past, present, or future is identified to help determine a treatment plan.
4. The tasks that define a person are identified, as well as whether those tasks can be performed and the reasons that the tasks are problematic.
5. A connection is determined between the components of function and occupational performance.
A top-down approach to evaluation is in contrast to a bottom-up approach, which first focuses on dysfunction of client factors.92
Effects of Neurologic Deficits on Performance in Areas of Occupation
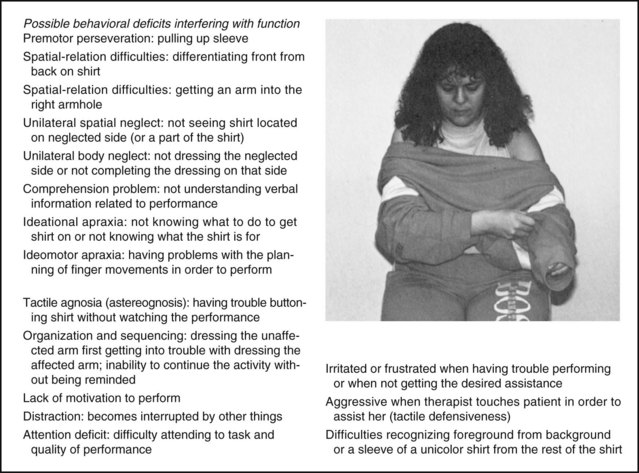
Using activity analysis and keen observation allows therapists to identify errors during task performance and to analyze the errors and determine the underlying deficits blocking independent functioning. Arnadottir states that “… therapists can benefit from detecting errors in occupational performance while observing ADL and thereby gain an understanding of the impairments affecting the patient’s activity limitation. Therapists can use the information based on observed task performance in a systematic way as a structure for clinical reasoning to help them assess functional independence related to the performance and to subsequently detect impaired neurological body functions. Such information can be important when intervention methods are aimed at addressing occupational errors”6 (Figure 33-2).

FIGURE 33-2 Dysfunction of multiple client factors such as ideational apraxia and spatial relationships can be revealed by activity and error analysis during functional tasks such as feeding. (Modified from Arnadottir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, Mo, 1990, Mosby.)
Because performance of a single functional task (e.g., donning a shirt) requires the use of multiple underlying client factors and performance skills that may have been affected by a stroke, multiple variables may be evaluated in the context of one client-chosen activity (Figure 33-3).6,7
Standardized Tools
Occupational therapists use assessment tools that are reliable, valid, and sensitive to change. In addition, assessment tools focused on task performance should be used. Tools that are focused on evaluation of client factors in isolation from performance in areas of occupation, that use novel nonfunctional tasks, and that do not consider the effect of environmental context should be interpreted with caution. Tools are available to the occupational therapist that directly relate performance dysfunction observed during ADLs to the effect of underlying skills necessary for independent performance of activities.
The Arnadottir Occupational Therapy Neurobehavioral Evaluation6,7 (A-ONE) objectively documents the way that dysfunction of client factors (e.g., left-sided neglect, apraxia, and spatial dysfunction) affects self-care and mobility tasks. The A-ONE has more recently been referred to as the ADL-focused Occupation-based Neurobehavioral Evaluation.8,9 The Assessment of Motor and Process Skills40 (AMPS) uses predominantly instrumental activities of daily living (IADLs) to evaluate underlying performance skills related to the completion of various IADLs (e.g., reaching, grasping, and posture) and process skill dysfunction (e.g., using items and searching and locating). Table 33-3 provides a summary of standardized assessments used with clients who have sustained a stroke. The A-ONE was used to objectively document the ways that Jasmine’s various impairments (e.g., neglect, spatial relationship dysfunction, loss of motor control, topographic disorientation) affected her ability to perform basic activities of daily living (BADLs) and mobility (e.g., bed mobility, transfers, wheelchair mobility, and walking when applicable). Errors observed and documented included not dressing the left side of her body, not able to locate grooming items on the left side of the sink, and difficulty dressing the lower part of her body and getting out of bed secondary to loss of motor control in her left limbs and trunk.
TABLE 33-3
Assessments Used with Clients Who Sustained a Stroke
| Instrument | Description and Usage |
| NIH Stroke Scale23 | Stroke deficit scale that scores 15 items (e.g., consciousness, vision, extraocular movement, facial control, limb strength, ataxia, sensation, speech and language) |
| Canadian Neurological Scale30 | Stroke deficit scale that scores 8 items (e.g., consciousness, orientation, speech, motor function, facial weakness) |
| Rankin Scale19 | Global disability scale with 6 grades indicating degrees of disability |
| Canadian Occupational Performance Measure (COPM)63 | Client-centered assessment tool based on clients’ identification of problems in performance in areas of occupation (clients rate the importance of self-care, productivity, and leisure skills, as well as their perception of performance and satisfaction with performance) Used as an outcome measure, as well as a client satisfaction survey |
| Barthel Index66 | Measure of disability in performing BADLs that ranges from 0 to 20 or 0 to 100 (by multiplying each item by 5); includes 10 items: bowels, bladder, feeding, grooming, dressing, transfer, toileting, mobility, stairs, and bathing |
| Kohlman Evaluation of Living Skills (KELS)89 | Living skills evaluation that includes ratings of 17 tasks (e.g., safety awareness, money management, phone book use, money and bill management) |
| Functional Independence Measure (FIM)55 | Measure of disability in performing BADLs that includes 18 items scored on a 7-point scale; includes subscores for motor and cognitive function; performance areas include self-care, sphincter control, mobility, locomotion, cognition, and socialization |
| Frenchay Activities Index*52 | 15-item IADL scale that evaluates domestic, leisure, work, and outdoor activities |
| PCG Instrumental Activities of Daily Living*64 | IADL evaluation of telephone use, walking, shopping, food preparation, housekeeping, laundry, public transportation, and medication management |
| Assessment of Motor and Process Skills40 | 16 motor skills (e.g., reach, manipulation, calibration, coordination, posture, mobility) and 20 process skills (e.g., attends, organizes, searches and locates, initiates, sequences) evaluated within the context of client-chosen IADL skills; clients choose familiar and culturally relevant tasks from a list of 50 standardized activities of various difficulties |
| Mini-Mental State Examination*41 | Mental status screening test for orientation to time and place, registration of words, attention, calculation, recall, language, and visual construction |
| Glasgow Coma Scale*88 | Level-of-consciousness scale that includes 3 sections scoring eye opening, motor, and verbal responses to voice commands or pain |
| Arnadottir Occupational Therapy Neurobehavioral Evaluation (A-ONE)7 | Evaluates apraxias, neglect syndromes, body scheme disorders, organization/sequencing dysfunction, agnosias, and spatial dysfunction via BADL and mobility tasks; directly correlates impairment and disability levels of dysfunction |
| Neurobehavioral Cognitive Status Examination*57 | Mental status screening test that includes the domains of orientation, attention, comprehension, naming, construction, memory, calculation, similarities, judgment, and repetition |
| Fugl-Meyer Test*43 | Motor function evaluation that uses a 3-point scale to score the domains of pain, range of motion, sensation, volitional movement, and balance |
| Functional Test for the Hemiparetic Upper Extremity99 | Arm and hand function is assessed via 17 hierarchic functional tasks based on Brunnstrom’s view of motor recovery; sample tasks are folding a sheet, screwing in a light bulb, stabilizing a jar, and zipping a zipper |
| Arm Motor Ability Test (AMAT)60 | Arm function evaluated by functional ability and quality of movement; test involves performance of 28 tasks (e.g., eating with a spoon, opening a jar, tying a shoelace, using the telephone) |
| TEMPA34,35 | Upper extremity performance test composed of 9 standardized tasks (bilateral and unilateral) measured by 3 criteria: length of execution, functional rating, and task analysis; sample tasks are handling coins, picking up a pitcher and pouring water, writing and stamping an envelope, and unlocking a lock |
| Jebsen Test of Hand Function54 | Hand function evaluation; includes 7 test activities: writing a short sentence, turning over index cards, simulated eating, picking up small objects, moving empty and weighted cans, and stacking checkers during timed trials |
| Motor Assessment Scale*25 | Motor function evaluation; includes disability and impairment measures, arm and hand movements, tone, and mobility (bed, upright, and ambulation) |
| Motricity Index*33 | Measures impairments in limb strength with a weighted ordinal scale |
| Trunk Control Test42 | Trunk control evaluated on a 0- to 100-point scale; tasks used: rolling, supine to sitting, and balanced sitting |
| Berg Balance Scale*14 | Balance assessment of 14 items scored on a 0- to 4-point ordinal scale |
| Tinetti Test90 | Evaluates balance and gait in the older adult population |
| Rivermead Mobility Index*29 | Measures bed mobility, sitting, standing, transfers, and walking on a pass or fail scale |
| Functional Reach Test37 | Balance evaluation; objectively measures length of forward reach in the standing posture |
| Boston Diagnostic Aphasia Examination*48 | Assesses sample speech and language behavior, including fluency, naming, word finding, repetition, serial speech, auditory comprehension, reading and writing |
| Western Aphasia Battery*56 | Includes an “Aphasia Quotient” and “Cortical Quotient” scored on a 100-point scale; assesses spontaneous speech, repetition, comprehension, naming, reading, and writing |
| Beck Depression Inventory*13 | 21-item, self-rating scale with attitudinal, somatic, and behavioral components |
| Geriatric Depression Scale*102 | Self-rated depression scale of 30 items with a yes or no format |
| Family Assessment Device*38 | Family assessment of problem solving, communication, roles, affective responsiveness, affective involvement, behavioral control, and general functioning |
| Medical Outcomes Study/Short-Form Health Survey (SF-36)*98 | Quality-of-life measure that includes the domains of physical functioning, physical and emotional problems, social function, pain, mental health, vitality, and health perception |
| Sickness Impact Profile*15 | Quality-of-life measure in the format of a 136-item scale with 12 subscales that measure ambulation, mobility, body care, emotion, communication, alertness, sleep, eating, home management, recreation, social interactions, and employment |
| Activity Card Sort (ACS)12 | Uses a Q-sort methodology to assess participation in 80 instrumental, social, and high– and low–physical demand leisure activities. Clients sort the cards into different piles to identify activities that were done before their stroke, activities they are doing less, and those they have given up since their stroke. The ACS uses cards with pictures of tasks that people do every day |
| Stroke Impact Scale61 | A stroke-specific measure that incorporates function and quality of life into one measure. It is a self-report measure with 59 items and 8 subgroups, including strength, hand function, BADLs and IADLs, mobility, communication, emotion, memory and thinking, and participation |
BADL, basic activities of daily living; IADL, instrumental activities of daily living.
*Recommended in the Agency for Health Care Policy and Research’s Clinical Practice Guidelines #16, Post-Stroke Rehabilitation, 1995.
Adopting a Framework for Intervention
Therapists should consider overarching themes when deciding which interventions to use to address a client’s inability to resume meaningful roles and successfully participate in chosen occupations. Embracing evidence-based practice should serve as the foundation for all OT interventions. To be successful in this endeavor, practitioners must remain abreast of new and emerging research in the OT literature, as well as related fields. Review papers65,83,95 and evidence-based libraries and search engines such as the Cochrane Library are sources of up-to-date information.
Over the past several years there has been a paradigm shift related to the intervention philosophies typically used with clients who sustained a stroke. In the past, sensorimotor approaches were used to treat individuals who sustained a stroke (see Chapter 31). These approaches were developed by Rood, Bobath, Knott, and Voss (proprioceptive neuromuscular facilitation) and by Brunnstrom and are based on an understanding of central nervous system (CNS) dysfunction at the time that these clinicians were doing their research (the mid-1900s). Although these interventions are commonly used, their effectiveness is being challenged as occupational therapists move toward models of evidence-based practice.75 At present, there is limited research to support these neurofacilitation approaches. Indeed, the Bobath approach, or neurodevelopmental treatment (NDT), though commonly used in the clinic, has not been shown to be superior to other treatment approaches and in fact is inferior to more current models of practice. For example, a large nonrandomized, parallel group study (N = 324) compared the NDT approach with conventional treatment. Subjects were monitored for 12 months. The authors concluded that “the NDT approach was not found effective in the care of stroke patients in the hospital setting. Health care professionals need to reconsider the use of this approach.”51 Similarly, a systematic review of 16 studies involving 813 patients with stroke concluded that “there was no evidence of superiority of Bobath on sensorimotor control of upper and lower limb, dexterity, mobility, activities of daily living, health-related quality of life, and cost-effectiveness. Only limited evidence was found for balance control in favor of Bobath.” “This systematic review confirms that overall the Bobath Concept is not superior to other approaches.”59
In contrast, approaches that focus on the use of functional activities as the therapeutic change agent (e.g., task-oriented approaches) show promise from both a research and a clinical perspective.67,68 A recent systematic review of task-oriented approaches concluded that “studies of task-related training showed benefits for functional outcome compared with traditional therapies. Active use of task-oriented training with stroke survivors will lead to improvements in functional outcomes and overall health-related quality of life.” The authors recommended “creating opportunities to practise meaningful functional tasks outside of regular therapy sessions.”76 One final note on the subject is that approaches focused on the use of functional tasks are more consistent with traditional and current principles of OT.
Mathiowetz67 has outlined a series of intervention principles based on use of the Occupational Therapy Task Oriented Approach.68 These principles include the following:
• Help clients adjust to role and task performance limitations by exploring new roles and tasks.
• Create an environment that includes the common challenges of everyday life.
• Practice functional tasks or close simulations that have been identified as important by participants to find effective and efficient strategies for performance.
• Provide opportunities for practice outside therapy time (e.g., homework assignments).
Functional Limitations Commonly Observed after Stroke
Multiple factors can impede effective and efficient performance of various tasks on which the client desires to focus during OT. The following section reviews problem areas that are typically observed during work with clients who have sustained a stroke.
Inability to Perform Chosen Occupations While Seated
A commonly observed deficit after stroke is loss of trunk and postural control. Impairment of trunk control may lead to the following problems45:
1. Dysfunction of limb control
3. Impaired ability to interact with the environment
4. Visual dysfunction secondary to resultant head and neck malalignment
Loss of trunk and postural control (i.e., “controlling the body’s position in space for the dual purposes of stability and orientation”79) after a stroke may be manifested as an inability to sit in proper alignment, loss of righting and equilibrium reactions, inability to reach beyond the arm span because of lack of postural adjustments, and falling during attempts to function.
Clients who sustained a stroke and lose trunk control need to use the more functional UE for postural support to remain upright and prevent falls. In these cases, the client effectively eliminates the ability to engage in ADLs and mobility tasks because lifting the more functional arm from the supporting surface can result in a fall. “Trunk control appears to be an obvious prerequisite for the control of more complex limb activities that in turn constitute a prerequisite to complex behavioral skills.”42 Studies have found trunk control to be a predictor of gait recovery, sitting balance,17 Functional Independence Measure (FIM) scores,42 and scores on the Barthel Index81 after a stroke.
Specific effects of a stroke on the trunk include the following:
1. Inability to perceive the midline as a result of spatial relationship dysfunction and leading to sitting postures that are misaligned from the vertical
2. Assumption of static postures that do not support engagement in functional activities (e.g., posterior pelvic tilt, kyphosis, lateral flexion)
3. Multidirectional trunk weakness18
4. Spinal contracture secondary to soft tissue shortening
5. Inability to move the trunk segmentally (i.e., the trunk moves as unit; examples of this phenomenon are clients using “logrolling” patterns during bed mobility and an inability to rotate the trunk while reaching for an item across the midline)
6. Inability to shift weight through the pelvis anteriorly, posteriorly, and laterally
Specific deficits in trunk control are evaluated during observation of task performance (Box 33-1). Observing tasks allows the therapist to evaluate trunk control in many directions (i.e., isometric, eccentric, and concentric control of the trunk muscle groups [extensors, abdominal muscles, and lateral flexors]) and the client’s limits of stability. The phrase limits of stability refers to “boundaries of an area of space in which the body can maintain its position without changing the base of support”84 or “an area about which the center of mass may be moved over any given base of support without disrupting equilibrium.”38 The therapist must differentiate between the client’s perceived limits of stability and the actual limits of stability. After a stroke, it is common to experience a disparity between the two because of body scheme disorder, fear of falling, or lack of insight into or awareness of disability. If the client’s perceived limits are greater than his or her actual limits, there is a risk for falls. In other cases, the client’s perceived limits are less than the actual limits. In such instances the client will not attempt more dynamic activities or will rely too greatly on adaptive equipment.
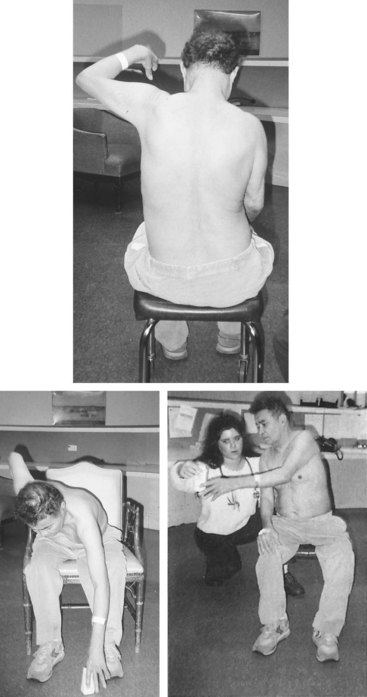
Treatment interventions aimed at increasing the client’s ability to perform chosen tasks in seated postures include the following45:
1. Establishing a neutral yet active starting alignment (i.e., a position of readiness to function). This starting alignment (similar to a typist’s posture) is a prerequisite to engaging the limbs in an activity. The desirable posture is as follows:
• Feet flat on the floor and bearing weight
• Equal weight bearing through both ischial tuberosities
2. The client should attempt reaching activities from the above posture (Figure 33-4).
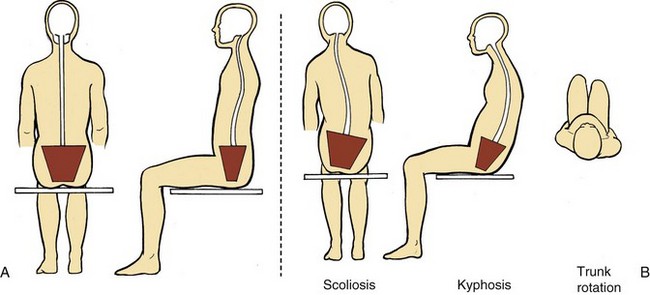
FIGURE 33-4 Normal and post-stroke sitting alignment. (From Donato SM, Pulaski KH: Overview of balance impairments: functional implications. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.)
3. Establishing the ability to maintain the trunk in the midline by using external cues. Many clients have difficulty assuming and maintaining the correct posture. The therapist can provide verbal feedback (e.g., “sit up nice and tall”). Visual feedback (e.g., using a mirror or the therapist assuming the same postural misalignment as the client) may be helpful. Environmental cues may be used to correct the posture. For example, the client may be instructed to maintain contact between the shoulder and an external target such as a bolster or wall, positioned so that the trunk is in the correct posture.
4. Maintaining trunk range of motion (ROM) by wheelchair and armchair positioning that maintains the trunk in proper alignment. The therapist can provide an exercise program focused on trunk ROM and flexibility. Activities that elicit the desired movement patterns can be chosen, and hands-on mobilization of the trunk can be used if needed. Trunk ROM that should be addressed include flexion, extension, lateral flexion, and rotation.
5. Prescribing dynamic weight-shifting activities to allow practice of weight shifts through the pelvis. The most effective way to train the client in weight shifts is to coordinate the trunk and limbs. Randomized controlled trials have confirmed that sitting training protocols that involve practice reaching tasks beyond arm’s length significantly improve function.32 Successfully engaging in meaningful occupations that require reach beyond the span of either arm requires clients to adjust their posture. The client is encouraged to reach beyond arm span in all directions while seated (preferably while reaching for an object) and to analyze the corresponding postural adjustment of the pelvis and trunk. The position and goal of the task will dictate the required weight shift (Table 33-4).
TABLE 33-4
Effects of Object Positioning on Trunk Movements and Weight Shifts during Reaching Activities*
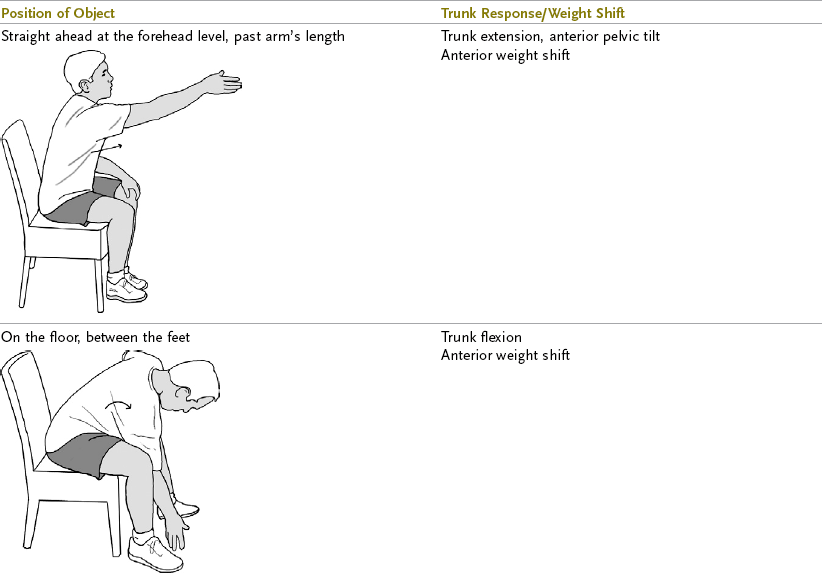
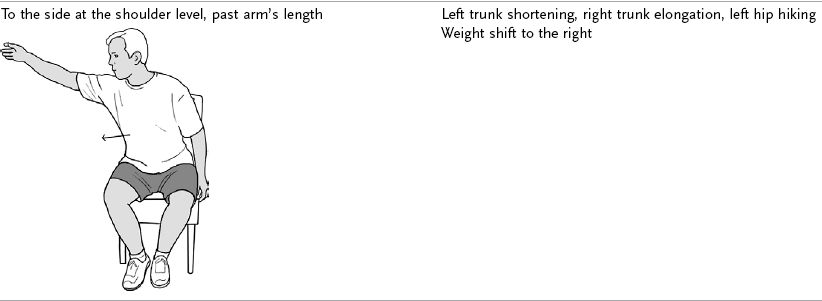
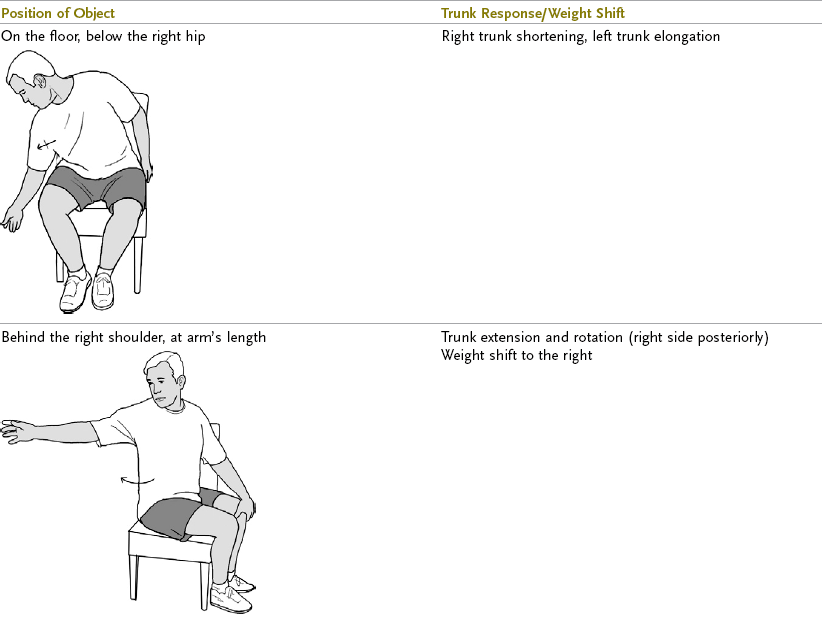
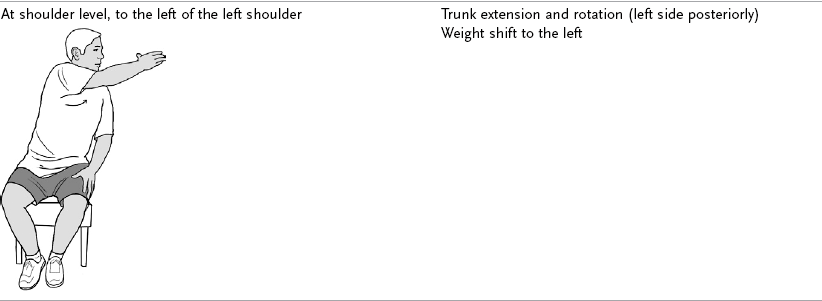

*These examples are for a patient with left hemiplegia. The left-hand column indicates where to position objects during a reaching task (with the right upper extremity). The right-hand column indicates the resultant trunk position and weight shift.
From Gillen G: Trunk control: supporting functional independence. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.
6. Strengthening the trunk, best achieved by tasks that require the client to control the trunk against gravity. Some examples are bridging the hips in the supine position to strengthen the back extensors and initiating a roll with the arm and upper part of the trunk to strengthen the abdominal muscles. Strengthening occurs within the context of an activity.
7. Using compensatory strategies and environmental adaptations when trunk control does not improve to a sufficient level and the client is at risk for injury. Examples of interventions include wheelchair seating systems (e.g., lateral supports, lumbar rolls, chest straps, tilt-in-space frames with head supports) and adaptive ADL equipment (e.g., reachers, long-handled equipment) to decrease the amount of required trunk displacement (see Chapter 10).
For Jasmine, therapy first focused on her ability to keep her trunk stable (i.e., not moving) while using her limbs to engage in occupations. Occupations that do not require substantial weight shifting while sitting (e.g., hair care, upper body washing, feeding, card playing) were chosen first, followed by those that required progressively more weight shifting in all directions (e.g., wiping after use of the toilet, lower body dressing, scooting, reaching to the floor to pick up shoes, washing her feet). As needed, the therapist provided external support at Jasmine’s shoulders during these activities to increase her confidence, prevent falls, and provide necessary support to compensate for Jasmine’s weakness. As Jasmine improved, more challenging seated activities were chosen and external support was diminished.
Inability to Engage in Chosen Occupations While Standing
An inability to assume and maintain a standing posture has a significant effect on the type of activities in which a person may engage; it may also play a significant role in the eventual discharge destination for a hospitalized client recovering from a stroke. Impaired upright control has been correlated with an increased risk for falls,101 as well as with less than optimal functional outcomes66 on the Barthel Index. Because many BADLs and IADLs, work, and leisure skills require control of standing postures, early training in upright control is a necessary component of stroke rehabilitation programs. Postural strategies (e.g., ankle, hip, and stepping strategies) are typically impaired after a stroke.
Similar to the deficits seen while sitting, upright standing postures are characterized by asymmetric weight distribution; unlike deficits occurring while sitting, the weight distribution while standing is seen through the lower extremities,101 in addition to the trunk. Clients who sustained a stroke often experience an inability to bear weight through the affected leg. Reasons for this disability include fear of falling or buckling of the knee, patterns of weakness that will not support the weight of the body, spasticity impeding proper alignment (i.e., plantar flexion spasticity that effectively blocks weight bearing through the sole of the foot),44 and perceptual dysfunction.
In addition to asymmetry and an inability to bear weight or shift weight through the affected leg, many clients who have sustained a stroke lose upright postural control and balance strategies. Effective upright control depends on the following automatic postural reactions36,84,85:
1. Ankle strategies are used to maintain the center of mass over the base of support when movement is centered on the ankles. These strategies control small, slow, swaying motions such as standing in a movie line, engaging in conversations while standing, and stirring a pot on a stovetop. They are most effective when the support surface (e.g., floor) is firm and longer than the foot. Ankle weakness, loss of ankle ROM, and proprioceptive deficits may all contribute to ineffective ankle strategies and balance.
2. Hip strategies are used to maintain or restore equilibrium. These strategies are used specifically in response to larger, faster perturbations, when the support surface is compliant, or when the surface is smaller than the feet (e.g., walking on a beam).53
3. A stepping strategy is used when ankle and hip strategies are ineffective or are perceived to be ineffective. This strategy results in movement of the base of support toward the center of mass movement. A step is taken to widen the base of support. Tripping over an uneven sidewalk or standing on a bus that unexpectedly stops elicits this strategy.
Both loss of postural reactions and an inability to bear and shift weight onto the affected leg will result in such functional limitations as gait deviations or dysfunction; an inability to climb stairs, transfer, and perform upright BADLs and IADLs; and an increased risk for falls. The assessment process provides the therapist with more specific information regarding the cause of the dysfunction. “Specifically, therapists should observe what happens when patients have to move their center of mass over their base of support, move their head, stand on uneven surfaces, function in lower lighting, move from one type of surface to another, or function on a narrower base of support. Therapists should also observe patients’ postural alignment, whether a bias in posture exists and in which direction that bias occurs, patients’ limits of stability, the width between their feet during functional tasks, and what patients do after losing their balance.”36
Treatment strategies aimed at improving the patient’s ability to perform chosen tasks in standing postures include the following36,84,101:
1. Establishing a symmetric base of support and proper alignment to prepare to engage in occupations. This starting alignment is assumed to provide ample proximal stability and to support engagement in functional tasks. The therapist may use hands-on support or visual or verbal feedback to establish proper alignment as follows:
2. Establishing the ability to bear and shift weight through the more affected lower extremity.36 The ability to bear weight may be graded at first. For example, if a client cannot assume a standing position because of postural insecurity or imbalance, sitting on a high surface (e.g., stool or raised therapy mat) allows the client to begin to bear weight but does not require bearing full body weight. As the client improves, full standing is encouraged, followed by graded weight shifts and progression to full weight bearing on the affected leg. For example, a modified soccer activity requires the client to fully shift weight to kick the ball. The environment (e.g., work surface height and placement of objects) is manipulated in conjunction with the client’s positioning to elicit the required weight shift.
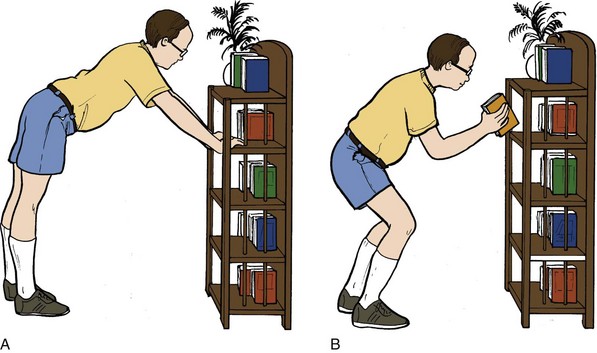
3. Encouraging dynamic reaching activities in multiple environments to develop task-specific weight-shifting abilities. For example, kitchen activities that necessitate retrieval of cleaning supplies under the sink, in a broom closet, and in overhead cabinets require mastery of multiple postural adjustments and balance strategies.
4. Using the environment to grade task difficulty and provide external support. Proper use of the environment can decrease the client’s fear of falling and simultaneously improve confidence and challenge underlying balance skills. Examples include working in front of a high countertop, using one hand for bearing weight as a postural support, and using a walker for support. The client must not rely too much on external supports because balance strategies may not be fully challenged to reach optimal recovery.
5. Training upright control within the context of the functional tasks that are graded. Tasks are graded in relation to the length of required reach, speed, and progressively more challenging bases of support. Examples include making a bed, changing a pet’s food bowl, setting a table, stepping up on a curb, cleaning a wall mirror, playing horseshoes or shuffleboard, and doffing slippers in a standing posture. All these activities require shifting of body weight, balance strategies, and the ability to bear weight through both lower extremities. The choice of activity is driven by the client’s desires, and the therapist designs positioning and set-up of the activity to elicit the desired postural strategies (Figure 33-5).
Jasmine was quickly engaged in activities that required standing despite persistent issues related to sitting balance. Standing was first attempted in front of stable work surfaces (e.g., kitchen counter, sink) to provide a balance point, increase Jasmine’s feeling of security and safety, and highlight the functional relevance of standing. As needed, the therapist stabilized the weak joints (e.g., hip and knee) with manual support, and Jasmine wore an ankle-foot orthotic to protect the integrity of her ankle. As Jasmine improved, she was asked to begin to use the upper part of her body for function while controlling her standing. Examples include wiping the counter, organizing a shelf, and grooming while standing. Progressively more demanding occupations from a standing balance perspective were chosen (e.g., modified games such as volleyball, vacuuming, emptying a dishwasher, stand-pivot transfers), and external manual and environmental support was decreased as Jasmine improved. All occupations were chosen to improve Jasmine’s ability to accept and shift weight through her left lower extremity.
Inability to Communicate Secondary to Language Dysfunction
Stroke may result in a wide variety of speech or language disorders ranging from mild to severe. These deficits occur most frequently with stroke resulting from damage to the left hemisphere of the brain. They can also occur less frequently after damage to the right hemisphere. All persons with stroke should be evaluated by a speech-language pathologist for the presence of speech and language disorders. The speech-language pathologist can provide valuable information to other members of the rehabilitation team and to the family regarding the best techniques for communicating with a particular client. The occupational therapist should continue the work of the speech therapist in the treatment sessions, as appropriate. Carryover may occur in reinforcing communication techniques that the client is learning and in presenting instruction in ways that the client is able to understand and integrate.86
The specific speech and language dysfunctions described in the following sections can exist in mild to severe forms and in combination with one another.
Aphasia
Aphasia is an acquired communication disorder caused by brain damage that is characterized by impairment of language modalities: speaking, listening, reading, and writing; it is not the result of a sensory or motor deficit, a general intellectual deficit, confusion, or a psychiatric disorder.49
Global Aphasia: Global aphasia is characterized by loss of all language skills. Oral expression is lost, except for some persistent or recurrent utterance. Global aphasia is usually the result of involvement of the MCA of the dominant cerebral hemisphere. A client with global aphasia may be sensitive to gestures, vocal inflections, and facial expression. Consequently, the client may appear to understand more than he or she actually does.
Broca’s Aphasia: Poor speech production and agrammatism characterize Broca’s aphasia. This aphasia is manifested as slow, labored speech with frequent misarticulations. Syntactic structure is simplified because of the agrammatism, sometimes referred to as telegraphic speech. A client with this form of aphasia demonstrates good auditory comprehension, except when speech is rapid, grammatically complex, or lengthy. Reading comprehension and writing may be severely affected, and a client with Broca’s aphasia usually has deficits in monetary concepts and the ability to perform calculations.86
Wernicke’s Aphasia: Wernicke’s aphasia is characterized by impaired auditory comprehension and feedback, along with fluent, well-articulated paraphasic speech. Paraphasic speech consists of word substitution errors. Speech may occur at an excessive rate and may be hyperfluent. The client uses few substantive words and many function words. The client produces running speech composed of English words in a meaningless sequence. English-speaking clients produce neologisms (non-English nonsense words) interspersed with real words. Reading and writing comprehension is often limited, and mathematic skills may be impaired.86
Anomic Aphasia: Persons with anomic aphasia have difficulty in word retrieval. Anomia, or word-finding difficulty, occurs in all types of aphasia. However, clients in whom word-finding difficulty is the primary or only symptom may be said to have anomic aphasia. The speech of these clients is fluent, grammatically correct, and well articulated but accompanied by significant difficulty in word finding. This problem can result in hesitant or slow speech and the substitution of descriptive phrases for the actual names of things. Mild to severe deficits in reading comprehension and written expression occur, and mild deficits in mathematic skills may be present.2,86
Dysarthria
Clients with dysarthria have an articulation disorder, in the absence of aphasia, because of dysfunction of the CNS mechanisms that control the speech musculature. This disorder results in paralysis and incoordination of the organs of speech, which causes the speech to sound thick, slurred, and sluggish.
Communication with Clients Who Have Aphasia
Although the speech-language pathologist is responsible for the treatment of speech and language disorders, the occupational therapist can facilitate communication and meaningful interaction with clients who have aphasia.
The use of gestures for communication should be encouraged. Having the client demonstrate through performance is the best way to ensure that the instructions are understood.
The occupational therapist can use routine ADLs as opportunities to encourage speech. The client should be reassured that the language disorder is part of the disability, not a manifestation of mental illness. Additional strategies for the occupational therapist to use with clients and their caregivers include the following:
• Understanding is facilitated when one person talks at a time. Extra noise creates confusion.
• Give the client time to respond.
• Carefully phrase questions to make it easier for the client to respond; for example, use “yes/no” and “either/or” questions.
• Use visual cues or gestures with speech to help the client understand.
• Do not rush communication because this may increase frustration and decrease the effectiveness of communication.86
Given that Jasmine sustained a right hemispheric stroke, aphasia would not typically be expected. Jasmine did exhibit severe sensory motor loss related to her left oral structures. She had moderate dysarthria, occasional drooling, and difficulty managing food in the left side of her mouth. Jasmine was encouraged to speak slowly and overenunciate. In addition, her occupational therapist taught her safe feeding strategies, including eating slowly, alternating solids and liquids, shifting food to the right side of her mouth, tilting her head to the right at a 45-degree angle, using her finger to sweep her mouth and clear out food pocketing on the left, and performing supervised oral care after each meal.
Inability to Perform Chosen Occupations Secondary to Neurobehavioral/Cognitive-Perceptual Impairments
A neurobehavioral deficit is defined as “a functional impairment of an individual manifested as defective skill performance resulting from a neurologic processing dysfunction that affects performance components such as affect, body scheme, cognition, emotion, gnosis, language, memory, motor movement, perception, personality, sensory awareness, spatial relations, and visuospatial skills.”6 A major responsibility of the occupational therapist treating a client who has sustained a stroke is evaluating which neurobehavioral deficits are blocking independent performance of chosen occupations.
Arnadottir6 proposed a relationship among the ability to perform daily activities, neurobehavioral impairments, and the CNS origin of the neurobehavioral dysfunction (a stroke, for the purposes of this chapter). She supports this theory with the following relational statements:
1. Behaviors required for task performance are related to neuronal processing at the CNS level. Therefore, a relationship also exists between the defective behavioral responses of an individual with CNS damage during performance of ADLs and the dysfunction of neuronal processing and performance components resulting from the CNS damage.
2. Performance of daily activities requires adequate function of specific parts of the nervous system. Consequently, CNS impairment may result in dysfunction of specific aspects of ADLs. For example, a stroke caused by a lesion of the posteroinferior parietal lobe of the left hemisphere commonly results in bilateral motor apraxia. “This neurobehavioral impairment may make manipulation of objects difficult during functional activities such as combing hair, brushing teeth, or holding a spoon while eating.”6
3. Neurologic impairment can be observed through the client’s engagement in daily activities. Thus, by analysis of ADLs, the integrity of the CNS can be evaluated (Box 33-2).
To properly evaluate the effect of neurobehavioral deficits on task performance, the therapist must develop activity analysis skills with the goal of analyzing which components of performance are necessary to achieve an outcome that is satisfactory to the client. Even the simplest of BADL tasks challenges multiple underlying skills (Boxes 33-3 and 33-4; also see Figure 33-3).6,79
Arnadottir6,7 proposed a system of observing clients engaged in functional activities in which errors are allowed to occur (as long as they are safe), the errors are analyzed, and finally, impairments that are interfering with performance of tasks are detected so that an appropriate treatment plan can be developed. She cautioned that when the therapist analyzes errors and observed behavior, knowledge of neurobehavior, cortical function, activity analysis, and clinical reasoning must be considered in the results of the evaluation (Table 33-5).
TABLE 33-5
Evaluating the Effect of Neurobehavioral Dysfunction on Task Performance
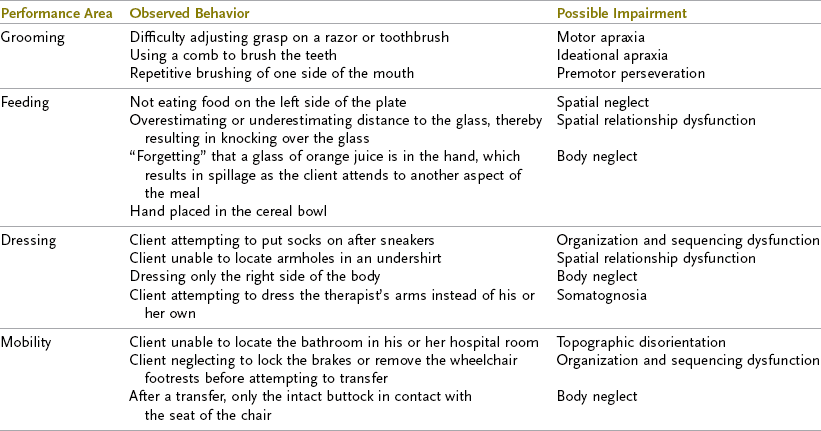
From Arnadottir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, Mo, 1990, Mosby; and Anadottir G: Impact of neurobehavioral deficits of activities of daily living. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.
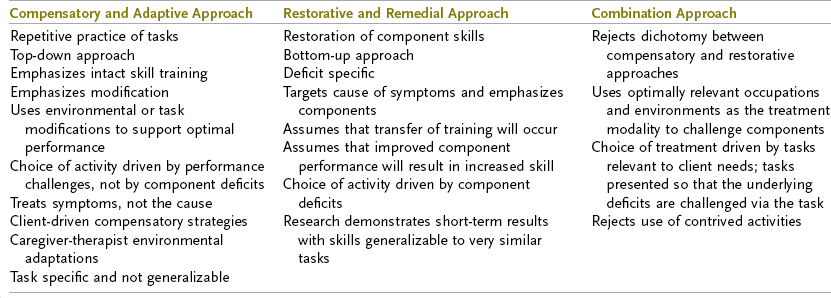
Treatment aimed at counteracting the effects of neurobehavioral dysfunction may be based on an adaptive and compensatory approach or on a restorative and remedial approach.47,70,72,79 A combination of approaches has also been suggested (Table 33-6).1
Decisions regarding the selection of a particular treatment approach may be difficult. Neistadt71,72 suggested evaluating a client’s learning potential in the context of ADL evaluation and training, with a focus on such issues as the number of repetitions needed to learn new approaches to tasks and the type of transfer of learning that is demonstrated.
Toglia91 has suggested that transfer of learning from one context to another (e.g., transferring skills learned from making a cup of tea in the OT clinic to meal preparation at home) may be facilitated by the therapist through the following methods:
1. Varying treatment environments
2. Varying the nature of the task
3. Helping clients become aware of how they process information
Toglia91 has identified degrees of transfer of learning. The degree of transfer is defined by the number of task characteristics that differ from those of the original task. Examples of these characteristics are spatial orientation, mode of presentation (e.g., auditory or visual), movement requirements, and environmental context.
A near transfer of learning involves transfer between two tasks that have one or two differing characteristics. Intermediate transfer involves transfer of learning to a task that varies by three to six characteristics. A far transfer involves a task that is conceptually similar but has one or no characteristics in common. Finally, a very far transfer involves the “spontaneous application of what has been learned in treatment to everyday living.”91
From her review of the literature, Neistadt70 reached the following conclusions:
1. Near transfer from remedial tasks to similar tasks is possible for all clients with brain injury.
2. Intermediate, far, and very far transfer from remedial to functional tasks will occur only in clients with localized brain lesions and good cognitive skills and after training with a variety of treatment tasks.
3. Far and very far transfer from remedial to functional tasks will not occur in clients with diffuse injury and severe cognitive deficits.
Using a functional and meaningful task as a treatment modality promotes the acquisition of a desired skill, and the therapist may use this task to challenge multiple underlying impairments.1,47,79 It is up to the therapist to present the task by manipulating the environment in a way that challenges the underlying skills (see Box 33-3). If a compensatory approach is chosen, adaptive techniques are used to counteract the effects of the underlying neurobehavioral deficits (see Box 33-4).
Jasmine’s left-sided neglect had a substantial impact on her ability to perform relevant occupations independently and safely. A variety of strategies were used to improve her ability to attend to the left side. Organized visual scanning was taught during daily activities such as feeding and grooming. Occupations were chosen that required scanning to both the left and the right to be successful (e.g., finding ingredients in the refrigerator, locating the toothbrush on the left side of the sink and toothpaste on the right, reading, describing a room). Vanishing physical and verbal cues were used as Jasmine progressed. Another strategy that was helpful for Jasmine was the use of a left-sided anchor. A red strip of tape was placed on the left side (e.g., the left side of the computer monitor, placemat, sink, book), and Jasmine focused on scanning to the anchor to ensure that she was attending to all of the information required to be successful at performing each occupation. Because Jasmine’s neglect persisted, driving was not an option. Other modes of transportation were considered, including supervised use of public transportation, assistance with transport by friends and neighbors, and local access-a-ride companies. See Chapters 11, 25, and 26.
Inability to Perform Chosen Tasks Secondary to Upper Extremity Dysfunction
Loss of UE control is common after a stroke, with 88% of clients who sustained a stroke having some level of UE dysfunction.74 The client’s ability to integrate the affected arm into chosen tasks may be limited by multiple factors, including the following46:
3. Loss of selective motor control
4. Weakness21
5. Superimposed orthopedic limitations
6. Loss of postural control to support UE control
7. Learned nonuse87
8. Loss of biomechanical alignment24
Integration into Function
UE evaluation procedures should focus primarily on assessing the client’s ability to integrate the UE into the performance of functional tasks—in other words, to use the affected UE to support performance in areas of occupation. Standardized evaluations such as the Test d’Evaluation des Membres Supérieurs de Personnes Agées (TEMPA),34,35 Arm Motor Ability Test (AMAT),60 Jebsen Test of Hand Function,54 and AMPS40 (see Table 33-3) are available to objectively measure the client’s ability to use the affected extremity during performance of tasks. In addition, self-reported measures of UE function are recommended. Examples include the following:
1. The Motor Activity Log is a self-reported questionnaire (reported by the patient or family) related to actual use of the involved UE outside structured therapy time. It uses a semistructured interview format. Quality of movement (“how well” scale) and the amount of use (“how much” scale) are graded on a six-point scale. At present, there are 30-, 28-, and 14-item versions of the tool. Sample items include holding a book, using a towel, picking up a glass, writing/typing, and steadying oneself.96,97
2. The 36-item Manual Ability Measure (MAM-36) is a new Rasch-developed, self-reported disability outcome measure. It contains 36 gender-neutral, commonly performed everyday hand tasks. The patient is asked to report the ease or difficulty of performing such tasks. It uses a four-point rating scale, with 1 indicating “unable” (I am unable to do the task all by myself), 2 indicating “very hard” (it is very hard for me to do the task and I usually ask others to do it for me unless no one is around), 3 indicating “a little hard” (I usually do the task myself, although it takes longer or more effort now than before), and 4 indicating “easy” (I can do the task without any problem). The MAM-36 can be accessed.28 A look-up table from raw scores to converted 0 to 100 Rasch measures is available.27
The UE may be used during functional performance in different ways (Table 33-7), including but not limited to the following42:
TABLE 33-7
Suggestions for Categorizing Upper Extremity Tasks
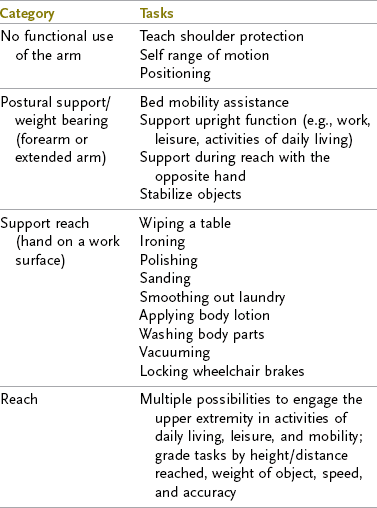
From Gillen G: Upper extremity function and management. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.
1. Weight bearing or accepting partial body weight through a limb. Weight bearing through the hand and forearm with an extended elbow is a pattern used during ADLs and mobility tasks. Establishment of weight bearing is a goal of UE rehabilitation.16 Effective control of weight bearing depends on the presence of sufficient trunk and scapula stability to accept partial body weight, control of active elbow extension, and ability of the hand to bear weight without losing the palmar arches. Once weight bearing is established, the client can effectively use the arm as a postural support (e.g., by supporting upper body weight with the affected arm while wiping crumbs from the table with the more functional arm), as an aid during transitional movements (e.g., while pushing up from lying on the side to sitting), and for preventing falls (increased postural support is provided).46
2. Moving objects across a work surface with a static grasp (supported reach). Activities such as ironing clothes, opening or closing a drawer, polishing furniture, and sliding a paper across the table are all examples of UE control of movement that does not occur with the arm in space. The hand is in contact with the objects involved in the task or is supported on the work surface; therefore, these types of tasks do not require the same control as and may require less effort than activities performed while the client is reaching in space, such as removing dishes from a cabinet or reaching for food in the refrigerator. This movement pattern can be used for multiple tasks and at the same time strengthens the various muscle groups used to eventually support reach in space.46
3. Reach and manipulation. Reviews of research on UE motor control2,46 have identified two components of function during reaching activities. The first is the transportation component, which is defined as the trajectory of the arm between the starting position and the object. The second is the manipulation component, which is the formation of grip by combined movements of the thumb and index finger during arm movement. Finger posturing anticipates the real grasp and occurs during transportation of the hand toward the object.2 Shaping of the hand is independent of the manipulation itself. Trombly’s reaching studies of clients with left hemiparesis documented that the ability to reach smoothly and with coordination was significantly less on the affected than on the unaffected side.94 The continuous movement strategy was lost, movement time was longer, peak velocity occurred earlier, and weakness indicators were present.
Trombly93 demonstrated that although muscular activity did not improve in the clients in her study, the discontinuity improved over time. She stated that the “level and pattern of muscle activity of these subjects depended on the biomechanical demands of the task rather than any stereotypical neurological linkages between the muscles.”
Clients are commonly observed demonstrating the use of stereotypic movement patterns of the UE. These patterns are characterized by scapula elevation and fixation, humeral abduction, elbow flexion, and wrist flexion. Mathiowetz and Bass Haugen68 suggested that the use of these movement patterns is evidence of attempts to use the remaining systems to complete tasks. They gave an example of a client with weak shoulder flexors trying to lift an arm. The client flexes the elbow when trying to raise the arm because this movement strategy shortens the lever arm and eases shoulder flexion.
The following are examples of using treatment activities to improve the client’s ability to integrate the UE into tasks2,24,44,46,80,85:
1. Using objects of different sizes and shapes to encourage control of the hand during reach and manipulation
2. Choosing activities that are appropriate to the client’s level of available motor control
3. Using constraint-induced movement techniques (Box 33-5): techniques in which the less affected UE is constrained (e.g., with a sling and splint or similar device) to compel use of the affected extremity, thereby providing massed practice of graded activities for the affected side to increase functional use83
4. Specifically training the arm to be used in weight bearing, reach, and manipulation situations within the context of ADLs and mobility
5. Presenting the client with graded tasks related to the number of degrees of freedom, the level of antigravity control required, and the resistance involved in the task (Figure 33-6).
Jasmine had very little motor activity throughout her left UE. Therapy focused on having Jasmine position her arm correctly (on the work surface and within her sight lines) during activities to prevent it from dangling all day, as well as use her arm as a stabilizer (e.g., using the weight of her arm to stabilize a paper while writing or holding a book open). As Jasmine improved, she was encouraged to use her arm in weight bearing as a postural support (e.g., pushing up when transitioning from the supine position to a seated position, pushing up to stand, reaching back to sit, and using the arm as support when standing at a sink or counter). Occupations were chosen that matched her available motor control and challenged her current level.
Upper Extremity Complications after Stroke
Subluxation: Subluxation, or malalignment caused by instability of the glenohumeral joint, is a common occurrence after stroke. The subluxation may be inferior (head of the humerus below the glenoid fossa), anterior (head of the humerus anterior to the fossa), or superior (head of the humerus lodged under the acromion-coracoid).80 Cailliet24 and Basmajian11 described the mechanism of inferior subluxation, in which the humeral head drifts inferior to the glenoid fossa. This common subluxation occurs as a result of malalignment of the scapula and the trunk. The normal position of the scapula is one of upward rotation, an orientation that cradles the head of the humerus and stabilizes it in alignment. The weight of the arm combined with instability and malalignment contributes to subluxation.
A common misunderstanding about subluxation is that it is associated with pain. The literature does not support this relationship.103 Because the shoulder is unstable after a stroke, care must be taken to support the flail shoulder in bed (e.g., using pillows to maintain alignment), in a wheelchair (e.g., with lap boards or pillows), and in the upright position (e.g., putting the hands in a pocket or taping the shoulder). Treatment to reduce subluxation should focus on achieving trunk alignment and scapula stability in a position of upward rotation.80
Abnormal Skeletal Muscle Activity: A change in the resting state of the limb and postural muscles is common after stroke.16 Immediately after a stroke, a change in available, or resting, skeletal muscle activity occurs. Most commonly, the acute state is characterized by low tone (“low-tone stage”). During this low-tone stage, the limbs and trunk become increasingly influenced by the pull of gravity. Little or no muscle activity is available at this stage, thereby resulting in deviations from the normal resting alignment of the musculoskeletal system.
An inability to recruit and maintain muscle activity is generally the greatest limiting factor at this stage. Because of the generalized lack of muscle activity and the dependent nature of the trunk and limbs, secondary problems can occur,44 including the following:
1. Edema affecting the dorsal surface of the hand and pooling under the extensor tendons, thereby effectively blocking active or passive digit flexion
2. Overstretching of the joint capsule of the glenohumeral joint
3. Eventual shortening of muscles that are passively positioned in an effort to support a weak limb (Commonly, flaccid UEs are positioned in the client’s lap, on a pillow, on a lap tray, or in a sling. Although they support the arm, these static positions result in prolonged positioning of certain muscle groups [internal rotators, elbow flexors, and wrist flexors] in a shortened position, which places them at risk for mechanical shortening. Interestingly, these are the muscle groups that tend to become spastic as time progresses.)
4. Overstretching of the antagonists to the previously mentioned muscles
5. Risk of joint and soft tissue injury during ADLs and mobility tasks (Because of the lack of control associated with a low-tone stage, the arm dangles and is not positioned appropriately during dynamic activities. Common examples include an arm being caught in the wheel during wheelchair mobility, pinning of the arm during bed mobility or rest, sitting on the arm after a transfer, or weight bearing through a flexed wrist during engagement in self-care activities.)
Progression to a state of increased or excessive skeletal muscle activity (increased tone), such as clonus, stereotypic posturing of the trunk and limbs, hyperactive stretch reflexes, and increased resistance to passive limb movements that are dependent on velocity, may occur within several days or months of the stroke.44
As spasticity increases, the risk for soft tissue shortening is heightened. This factor may lead to a vicious circle of spasticity to soft tissue shortening to over-recruitment of shortened muscles to increased stretch reflexes. Secondary problems that may occur if the spasticity is not managed in a therapy program include the following44:
1. Deformity of the limbs, specifically the distal end of the upper limb (elbow to digits)
3. Possible masking of underlying selective motor control
4. Pain syndromes resulting from loss of normal joint kinematics (These syndromes are usually related to soft tissue contracture that blocks full joint excursion. A typical example is loss of full passive external rotation of the glenohumeral joint. Attempts at forced abduction in these cases will result in a painful impingement syndrome of the tissues in the subacromial space.)
5. Impaired ability to manage BADL tasks, specifically UE dressing and bathing of the affected hand and axilla when flexor posturing is present
Prevention of Pain Syndromes and Contracture:
Protection of Unstable Joints: During the low-tone stage, joints tend to become malaligned secondary to loss of muscular stabilization. In these cases, clients are at risk for injury to unstable joints (e.g., traction injuries and joint trauma) because of the joint instability. The glenohumeral and wrist joints are particularly at risk. The glenohumeral joint (usually already inferiorly subluxated at this stage) is at risk for a superimposed orthopedic injury if another individual unknowingly pulls on the affected arm during self-care and mobility or during unskilled passive range of motion (PROM) of the joint. The unstable glenohumeral joint is in a malaligned state, which puts the client at risk for an impingement syndrome during PROM if normal joint mechanics is not addressed. Key joint motions of concern are upward rotation of the scapula and external (lateral) rotation of the shoulder. If these motions are not present and ROM is forced, the client is at risk for the development of an impingement and pain syndrome.44
Clients with low tone also have an unstable wrist. Care should be taken to protect the wrist if the clients are not controlling the joint during ADL and mobility tasks. Clients commonly practice a bed mobility or lower extremity dressing sequence and then complete the task while bearing weight through a malaligned flexed wrist. These clients are at risk for orthopedic injury (traumatic synovitis) and may be considered candidates for splinting to protect the wrist.46
Maintaining Soft Tissue Length: Clients who have both increased and decreased skeletal muscle activity are at risk for soft tissue contracture secondary to the immobilization that occurs during both low-tone and increased-tone stages. Maintenance of tissue length is a 24-hour regimen. It involves frequent variations in resting postures during waking hours, teaching the client and significant others appropriate ROM procedures, daytime and nighttime positioning programs, and staff and family education so that positioning and exercise programs may be carried out in the home environment.44
Prolonged static positioning (e.g., prolonged use of a sling) must be avoided. Rather, teaching clients to adjust their resting postures during the day will help prevent soft tissue tightness.
Positioning Programs: The same wheelchair- and bed-positioning programs should not be applied to every client. Instead, positioning should be individualized and focus on (1) promoting normal resting alignment of the trunk and limbs in an effort to maintain tissue length on both sides of the joints (2) providing stretch to muscle groups that have been identified as being prone to contracture or already shortened, and (3) placing particular focus on maintaining passive external rotation of the shoulder.3
Soft Tissue Elongation: If soft tissue shortening and length-associated changes have already developed, the treatment of choice is low-load prolonged stretch (LLPS). LLPS involves placing the soft tissues in question on submaximal stretch for prolonged periods. This technique is quite different from the common PROM with terminal stretch (high-load brief stretch) programs commonly used to treat this population.69
LLPS can be implemented in various ways, including splinting, casting, and positioning programs. For example, during a UE assessment a client is noted to have tightness in the internal rotators, overactive internal rotation during attempts to move, and weakened external rotators. An effective LLPS program would involve having the client rest in a supine position with the arm abducted to 45 degrees and in external rotation. This position has been shown to decrease the potential for contracture.3
LLPS can also be achieved through splinting programs. A common example is the use of a splint designed to elongate the long flexors of the hand during sleeping hours.
Splinting: Commonly a controversial subject in the management of stroke, splinting should be considered on a case-by-case basis and may be quite effective for many clients.69 The most common uses for splints during the low-tone stage are for maintaining joint alignment, protecting the tissues from shortening or overstretching, preventing injury to the extremity, and serving as an adjunctive treatment to control edema.69 Specifically, splinting support may be needed to provide palmar arch support and maintain neutral wrist deviation and a neutral position of the wrist between flexion and extension. In most cases the fingers do not require splinting in this stage of recovery.69
Splints may also be effective for clients in whom spasticity is developing. In these cases the splints may be used to maintain soft tissue length, provide LLPS, place muscles at their resting lengths on both sides of the joints, and attempt distal relaxation by promoting proximal alignment.69
Client Management: In addition to the interventions already described, it is helpful to train the client to manage his or her UE. For a client with low tone, the most important information to share with the client and significant others is the method for protecting the unstable joints and maintaining full ROM. In the spastic stage, the treatment of choice is to teach positioning that will provide prolonged elongation of the overactive muscles and prevent contracture. Examples of positions that may be prescribed during leisure or self-care activities include the following44:
1. Weight bearing on the extended arm (elongates the commonly shortened UE musculature)
2. In the supine position, hands behind the head while allowing the elbows to drop toward the bed (provides stretch of the internal rotators)
3. In the supine position, a pillow protracting the scapula and under the elbow to promote glenohumeral joint alignment
4. Lying on a protracted scapula to maintain stretch of the retractors and scapulothoracic mobility
5. Supporting the involved wrist with the more functional hand and reaching down toward the floor with both hands (This pattern will elongate muscles that tend to contract during difficult activities, which is particularly helpful after gait activities or difficult self-care activities.)
6. Cradling the affected arm with the stronger arm, lifting it to chest level, and gently raising and lowering (staying below 90 degrees) and gently abducting or adducting the arm (Figure 33-7). Cautionary note: Clasping the hands and lifting the affected arm overhead should be discouraged because of the risk for increasing pain, causing an impingement syndrome, and stressing the carpal ligaments (Figure 33-8). Similarly, overhead pulleys should be avoided.
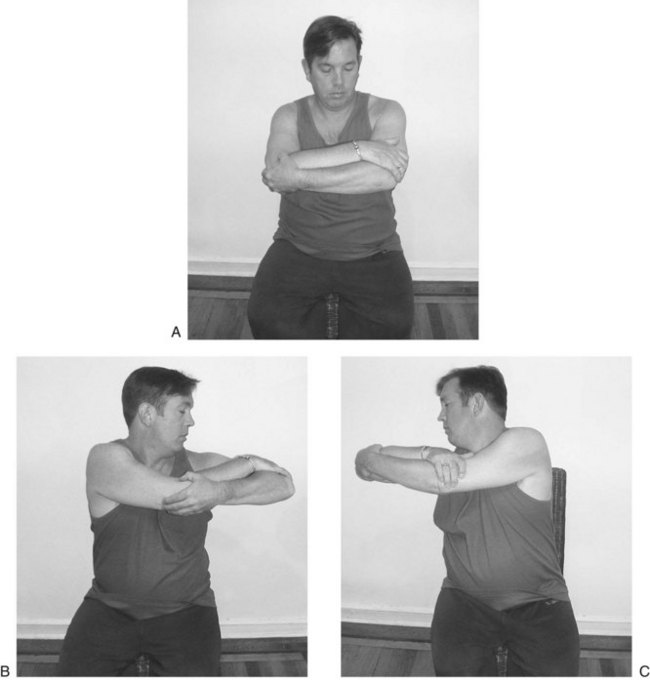
FIGURE 33-7 “Rock the baby.” The client lifts the right upper extremity to chest level (A), adducts (B), and abducts (C) horizontally to allow trunk rotation. (From Gillen G: Upper extremity function and management. In Gillen G, editor: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo, 2011, Mosby.)
The keys to prescribing a proper resting posture are to identify muscle groups in the trunk and upper limb that are shortening, overactive, or at risk for the development of shortening and to select a comfortable posture that elongates the muscle group for a prolonged period.
Jasmine and her family were taught appropriate positioning when in bed and on chairs and during upright activities. In addition, Jasmine learned how to safely perform self-ROM exercises and was provided with a resting hand splint at night.
The Nonfunctional Upper Extremity
Although restoration of UE control is a realistic goal for some clients, many clients will not regain enough control to integrate the affected UE into ADL and mobility tasks. Clients who will not regain sufficient control require extensive retraining in BADLs and IADLs74 (see Chapter 10) with one-handed techniques and prescription of appropriate assistive devices (Box 33-6). Persons in this population are also candidates for dominance retraining. Control of deformity to prevent body image issues is paramount for these clients.
Inability to Perform Chosen Tasks Secondary to Visual Impairment
Processing of visual information is a complex act that requires intact functioning of multiple peripheral nervous system and CNS structures to support functional independence. The site of the lesion determines the visual dysfunction and the effect on performance of tasks (Figure 33-9).7
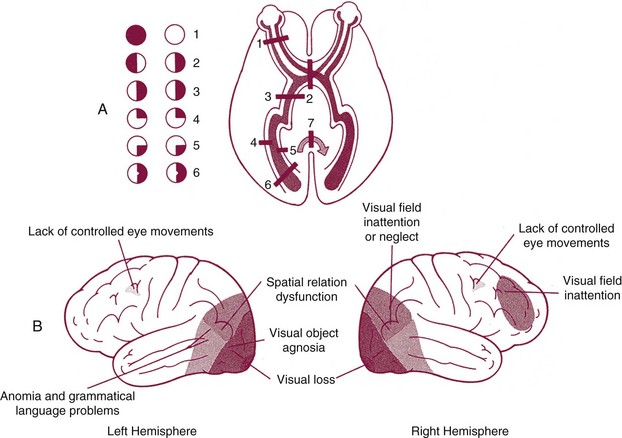
FIGURE 33-9 Visual-processing deficits. (From Arnadottir G: The brain and behavior: assessing cortical dysfunction through activities of daily living, St Louis, Mo, 1990, Mosby.)
Visual dysfunction and its treatment are detailed in Chapter 24. In general, treatment approaches may focus on remediation, such as eye calisthenics, fixations, scanning, visual motor techniques, and bilateral integration. Adaptive techniques are also used, including a change in working distance, the use of prisms, adaptations for driving and reading, changes in lighting, and enlarged print.82
Psychosocial Adjustment
The psychologic consequences of a stroke are substantial. The incidence of depression in this population is 35% according to statistics collected by the American Heart Association.4 The highest reported incidence is found in clients in acute and rehabilitation hospitals, and the lowest is in samples of those living in the community following stroke. Other psychologic manifestations that have been documented in survivors of stroke include anxiety, agoraphobia, substance abuse, sleep disorders, mania, aprosody (difficulty expressing or recognizing emotion), behavioral problems (e.g., sexual inappropriateness, verbal outbursts, aggressiveness), lability (alteration between pathologic laughing and crying), and personality changes (e.g., apathy, irritability, social withdrawal).39
A critical role of the occupational therapist is to help the client adjust to hospitalization and, more important, to disability. Much patience and a supportive approach by the therapist are essential. The therapist must be sensitive to the fact that the client has experienced a devastating and life-threatening illness that has caused sudden and dramatic changes in the client’s life roles and performance. The therapist must be cognizant of the normal adjustment process and must gear the approach and expectations of performance to the client’s level of adjustment. Frequently, the client is not ready to engage in rehabilitation measures with wholehearted effort until several months after onset of the disability.
Family education is extremely important throughout the treatment program. Family members are better equipped to assist their loved one in adjusting to disability when they are knowledgeable about the disability and its implications.
Many clients dwell on the possibility of full recovery of function; they should gradually be made aware that some residual dysfunction is likely. The therapist may approach this probability by discussing in objective terms what is known about the prognosis for functional recovery after stroke. It may be necessary to review this information many times before the client begins to apply it to his or her recovery. This education should be done in a way that is honest and yet does not destroy all hope.
Falk-Kessler39 has provided occupational therapists with guidelines related to interventions for the psychologic manifestations of stroke, including the following:
• Fostering an internal locus of control related to recovery
• Using therapeutic activities to improve self-efficacy or confidence in the performance of specific activities
• Promoting the use of adaptive coping strategies, such as seeking social support, information seeking, positive reframing, and acceptance
• Promoting success in chosen occupations to improve self-esteem
• Encouraging social support networks, such as families, friends, or support groups
In addition to the aforementioned interventions, it is important to remember that pharmacologic interventions have been shown to be effective in this population and should not be overlooked39 as part of a team approach. Such interventions include but are not limited to antidepressants for depression or for individuals with a pathologic affect, benzodiazepines for generalized anxiety disorder, and neuroleptic medications for those with post-stroke psychosis.26
The OT program should focus on the skills and abilities of the patient. The patient’s attention should be focused, through the performance of activity, on his or her remaining and newly learned skills. The OT program can also include therapeutic group activities for socialization and sharing of common problems and their solutions. The discovery that there are residual abilities and perhaps new abilities and success at performing many daily living skills and activities that were initially thought to be impossible can improve the patient’s mental health and outlook.
Summary
Stroke is a complex disability that challenges the skills of professional health care workers. Although the number and effectiveness of approaches for the remediation of affected motor, sensory, perceptual, cognitive, and performance dysfunctions have increased considerably, many limitations in treatment remain. The occupational therapist must bear in mind that the degree to which the patient achieves treatment goals depends on the CNS damage and recovery, psychoneurologic residuals, psychosocial adjustment, and the skilled application of appropriate treatment by all concerned health professionals.
Some patients remain severely disabled despite the noblest efforts of rehabilitation workers, whereas others recover quite spontaneously with minimal help in a short period. Most patients benefit from the professional skills of occupational therapists and other rehabilitation specialists and achieve improvement of performance skills and resumption of meaningful occupational roles.
Jasmine demonstrated a clear relationship between her impaired body functions (e.g., loss of motor control, sensory loss, visual dysfunction, and neglect) and her ability to return to her previous lifestyle and engage in chosen areas of occupation. Through standardized assessments and skilled observation made while Jasmine was performing her chosen occupations of feeding, grooming, toilet transfers, computer use, and child care it was determined that several impairments were affecting Jasmine’s ability to perform independently:
• Feeding: Jasmine was unable to cut or open containers secondary to unilateral UE weakness on the left, she had a tendency to eat only the food on the right side of her plate, and she was unable to locate utensils on the left side of the plate. In addition, food remained between her left gums and cheek (“pocketing”) after meals, thereby resulting in oral hygiene issues and putting Jasmine at risk for aspiration.
• Grooming: Jasmine had difficulty opening and applying toothpaste with one hand. She attended only to the right side of her body while grooming, with the left side of her mouth and hair not being cared for during oral and hair care.
• Toilet transfers: Jasmine required moderate physical assistance to transfer to the toilet secondary to an inability to bear weight on her left leg and an inability to control her trunk (she falls laterally when sitting on the toilet). The occupational therapist also noted that when Jasmine “completed” the transfer to the toilet, only the right side of her body was sitting on the toilet. She neglected to include the left side of her body in the transfer and left it in the wheelchair.
• Computer use: During attempts to use the computer, Jasmine became easily frustrated and made comments such as “I feel like a failure” and “I can’t even provide for my child anymore.” Jasmine agreed to attempt to write a letter to her friend on the computer. Multiple mistakes were noted because Jasmine seemed to “not see” the left-sided keys, could not control the shift keys, and generally appeared disorganized in her approach to the task.
• Simulated child care: A weighted doll was used to observe Jasmine’s ability to care for her child. It was quickly decided that this area of occupation would be deferred until Jasmine’s status improved. Jasmine and her occupational therapist made this decision collaboratively on the basis of safety concerns and Jasmine’s emotional status. Jasmine was gravely concerned about her ability to care for her child. The occupational therapist wanted to focus on occupations that Jasmine could master, build her confidence, and upgrade her occupations systematically according to Jasmine’s abilities.
The above findings were determined based on the initial assessment choices. The first assessment administered was the COPM.62,63 Because multiple areas of occupation are limited after a stroke, it is imperative to use a tool such as this to determine the client’s priorities for intervention. These priorities then in turn become the client’s initial goals. In addition, the FIM55 and the A-ONE6–9 were used to objectify limitations in daily function and to determine limiting factors. The FIM is typically used in inpatient rehabilitation settings and documents the level of caregiver burden related to BADLs and mobility. The A-ONE is complementary to the FIM and determines the reasons for lack of independence by evaluating client factors that result in errors in occupational performance by skilled observations of tasks performed in natural contexts.
Several interventions were considered to address Jasmine’s inability to participate in chosen occupations (toilet transfers, computer use, grooming, feeding, and child care). Task-specific training of grooming, feeding, and toileting served as the basis for her initial OT. A system of vanishing physical and verbal cues was used as Jasmine relearned the tasks at hand. Jasmine had substantial motor loss in her left limbs, thus making training with adaptive equipment imperative. Examples included a rocker knife and Dycem for feeding and a grab bar and raised toilet seat. To ensure continued integration of her affected upper limb, Jasmine was taught to use her left limb as a stabilizer during tasks. She was also taught to keep her arm positioned on a surface and in her line of sight. A strategy that was used to help Jasmine overcome her neglect was use of a perceptual anchor. In addition to her left arm being positioned on the left side of a surface, a strip of red tape was placed on the left edge of work surfaces (e.g., on the table to the left of her place setting and on the left side of the sink). As Jasmine gained mastery of these tasks, task-specific training of work tasks via similar strategies was introduced.
1. Define stroke and list two of its causes.
2. List the disturbances that can result from occlusion of the MCA, ACA, PCA, and cerebellar arteries.
3. Name three modifiable risk factors associated with stroke.
5. Name three functional deficits that occur as a result of loss of trunk control.
6. Besides paralysis of the limbs and trunk after stroke, what important motor disturbances can result?
7. Name two components of a “client-centered approach” to evaluation.
8. What are two frames of reference used to treat neurobehavioral impairments after stroke?
9. Name three postural reactions that support standing activities.
References
1. Abreu, B, et al. Occupational performance and the functional approach. In: Royeen C, ed. AOTA self-study: cognitive rehabilitation. Bethesda, Md: American Occupational Therapy Association, 1994.
2. Ada, L, et al. Task-specific training of reaching and manipulation. In: Bennett KMB, Castiello U, eds. Insights into the reach to grasp movements. New York, NY: Elsevier Science, 1994.
3. Ada, L, Goddard, E, McCully, J, et al. Thirty minutes of positioning reduces the development of shoulder external rotation contracture after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2005;86(2):230–234.
4. American Heart Association. Heart disease and stroke statistics 2010 update. Dallas, Tex: American Heart Association; 2010.
5. American Occupational Therapy Association. Occupational therapy practice framework: domain and process, edition 2. Am J Occup Ther. 2008;62(6):625–683.
6. Arnadottir, G. Impact of neurobehavioral deficits of activities of daily living. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
7. Arnadottir, G. The brain and behavior: assessing cortical dysfunction through activities of daily living. St Louis, Mo: Mosby; 1990.
8. Árnadóttir, G, Fisher, AG. Rasch analysis of the ADL scale of the A-ONE. Am J Occup Ther. 2008;62(1):51–60.
9. Árnadóttir, G, Fisher, AG, Löfgren, B. Dimensionality of nonmotor neurobehavioral impairments when observed in the natural contexts of ADL task performance. Neurorehabil Neural Repair. 2009;23(6):579–586.
10. Bartels, MN. Pathophysiology and medical management of stroke. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
11. Basmajian, JV. The surgical anatomy and function of the arm-trunk mechanism. Surg Clin North Am. 1963;43:1471.
12. Baum C, Edwards D: The Activity Card Sort: Form C, Unpublished Version, 2001.
13. Beck, AT, Steer, RA, Beck Depression Inventory Manual. rev ed, New York, NY, Psychological Corp, 1987.
14. Berg, K, Wood-Dauphinee, S, Williams, JI, Gayton, D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311.
15. Bergner, M, Bobbitt, RA, Carter, WB, Gilson, BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805.
16. Bobath, B. Adult hemiplegia: evaluation and treatment, ed 3. Oxford, England: Butterworth-Heinemann; 1990.
17. Bohannon, RW. Recovery and correlates of trunk muscle strength after stroke. Int J Rehabil Res. 1995;18(4):162.
18. Bohannon, RW, Cassidy, D, Walsh, S. Trunk muscle strength is impaired multidirectionally after stroke. Clin Rehabil. 1995;9(1):47.
19. Bonita, R, Beaglehole, R. Recovery of motor function after stroke. Stroke. 1988;19(12):1497.
20. Bounds, JV, Wiebers, DO, Whisnant, JP. Mechanisms and timing of deaths from cerebral infarction. Stroke. 1981;12(4):414.
21. Bourbonnais, D, Vanden Noven, S. Weakness in patients with hemiparesis. Am J Occup Ther. 1989;43(5):313.
22. Branch, EF. The neuropathology of stroke. In: Duncan PW, Badke MB, eds. Stroke rehabilitation: the recovery of motor control. Chicago, Ill: Year Book, 1987.
23. Brott, T, Adams, HP, Jr., Olinger, CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–870.
24. Cailliet, R. The shoulder in hemiplegia. Philadelphia, Pa: FA Davis; 1980.
25. Carr, JH, Shepherd, RB, Nordholm, L, Lynne, D. Investigation of a new motor assessment scale for stroke patients. Phys Ther. 1985;65(2):175–180.
26. Chemerinski, E, Robinson, RG. The neuropsychiatry of stroke. Psychosomatics. 2000;41(1):5.
27. Chen CC, Bode RK: MAM-36: psychometric properties and differential item functioning in neurologic and orthopedic patients. Paper presented at the 88th Annual Conference of the American Occupational Therapy Association, Long Beach, Calif, April 10, 2008.
28. Chen, CC, Kasven, N, Karpatkin, HI, Sylvester, A. Hand strength and perceived manual ability among patients with multiple sclerosis. Arch Phys Med Rehabil. 2007;88:794–797.
29. Collen, FM, Wade, DT, Robb, GF, Bradshaw, CM. The Rivermead mobility index: a further development of the Rivermead motor assessment. Int Disabil Stud. 1991;13(2):50–54.
30. Côté, R, Hachinski, VC, Shurvell, BL, et al. The Canadian Neurological Scale: a preliminary study in acute stroke. Stroke. 1986;17(4):731–737.
31. Chusid, J. Correlative neuroanatomy and functional neurology, ed 19. Los Altos, Calif: Lange; 1985.
32. Dean, CM, Channon, EF, Hall, JM. Sitting training early after stroke improves sitting ability and quality and carries over to standing up but not to walking: a randomised trial. Aust J Physiother. 2007;53(2):97–102.
33. Demeurisse, G, Demol, O, Robaye, E. Motor evaluation in vascular hemiplegia. Eur Neurol. 1980;19(6):382.
34. Desrosiers, J, Hébert, R, Bravo, G, Dutil, E. Upper extremity performance test for the elderly (TEMPA): normative data and correlates with sensorimotor parameters. Arch Phys Med Rehabil. 1995;76(12):1125–1129.
35. Desrosiers, J, Hebert, R, Dutil, E, Bravo, G. Development and reliability of an upper extremity function test for the elderly: the TEMPA. Can J Occup Ther. 1993;60(1):9–16.
36. Donato, SM, Pulaski, KH. Overview of balance impairments: functional implications. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
37. Duncan, PW, Weiner, DK, Chandler, J, Studenski, S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–M197.
38. Epstein, NB, Baldwin, LM, Bishop, DS. The McMaster family assessment device. J Marital Fam Ther. 1983;9(2):171–180.
39. Falk-Kessler, J. Psychological aspects of stroke. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
40. Fisher, AG. Assessment of motor and process skills: vol 1, Development, standardization, and administration, ed 6. Fort Collins, Colo: Three Star Press; 2006.
41. Folstein, MF, Folstein, SE, McHugh, PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198.
42. Franchignoni, FP, Tesio, L, Ricupero, C, Martino, MT. Trunk control test as an early predictor of stroke rehabilitation outcome. Stroke. 1997;28(7):1382–1385.
43. Fugl-Meyer, AR, Jääskö, L, Leyman, I, et al. The post-stroke hemiplegic patient: a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7:13–31.
44. Gillen, G. Managing abnormal tone after brain injury. OT Pract. 1998;3:8.
45. Gillen, G. Trunk control: supporting functional independence. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
46. Gillen, G. Upper extremity function and management. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
47. Gillen, G. Cognitive and perceptual rehabilitation: optimizing function. St. Louis, Mo: Mosby; 2009.
48. Goodglass, H, Kaplan, E. Boston diagnostic aphasia examination. Philadelphia, Pa: Lea & Febiger; 1983.
49. Hallowell, B, Chapey, R. Delivering language intervention services to adults with neurogenic communication disorders. In Chapey R, ed.: Language intervention strategies in aphasia and related neurogenic communication disorders, ed 5, Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins, 2008.
50. Helgason, CM, Wolf, PA. American Heart Association prevention conference IV: prevention and rehabilitation of stroke. Dallas, Tex: American Heart Association; 1997.
51. Hafsteinsdóttir, TB, Algra, A, Kappelle, LJ, Grypdonck, MHF. Neurodevelopmental treatment after stroke: a comparative study. J Neurol Neurosurg Psychiatry. 2005;76:788–792.
52. Holbrook, M, Skilbeck, CE. An activities index for use with stroke patients. Age Ageing. 1983;12(2):166.
53. Horak, FB, Nashner, L. Central programming of postural movements: adaptation to altered support surface configurations. J Neurophysiol. 1986;55(6):1369.
54. Jebsen, RH, Taylor, N, Trieschmann, RB, et al. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50(6):311–319.
55. Keith, RA, et al. The functional independence measure: a new tool for rehabilitation. In: Eisenberg, MG, Grzesiak, RC, eds. Advances in clinical rehabilitation, vol 1. New York, NY: Springer-Verlag; 1987.
56. Kertesz, A. Western Aphasia Battery. New York, NY: Grune & Stratton; 1982.
57. Kiernan, RJ. The Neurobehavioral Cognitive Status Examination. Northern California Neuro Group; 1987.
58. Kistler, JP, Ropper, AH, Martin, JB. Cerebrovascular disease. In: Isselbacher KJ, et al, eds. Harrison’s principles of internal medicine. New York, NY: McGraw-Hill, 1994.
59. Kollen, BJ, Lennon, S, Lyons, B, et al. The effectiveness of the Bobath concept in stroke rehabilitation: what is the evidence? Stroke. 2009;40:e89–e97.
60. Kopp, B, Kunkel, A, Flor, H, et al. The arm motor ability test: reliability, validity, and sensitivity to change of an instrument for assessing disabilities in activities of daily living. Arch Phys Med Rehabil. 1997;78(6):615–620.
61. Lai, SM, Studenski, S, Duncan, PW, Perera, S. Persisting consequences of stroke measured by the stroke impact scale. Stroke. 2002;33(7):1840–1844.
62. Law, M, Baptiste, S, Mills, J. Client-centered practice: what does it mean and does it make a difference? Can J Occup Ther. 1995;62(5):250.
63. Law, M, et al. The Canadian Occupational Performance Measure, ed 4. Ottawa, Canada: CAOT Publications ACE; 2005.
64. Lawton, MP. Instrumental activities of daily living scale: self-rated version. Psychopharmacol Bull. 1988;24(4):785.
65. Ma, HI, Trombly, CA. A synthesis of the effects of occupational therapy for persons with stroke. Part II: remediation of impairments. Am J Occup Ther. 2002;56(3):260.
66. Mahoney, FI, Barthel, DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61.
67. Mathiowetz, V. Task-oriented approach to stroke rehabilitation. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
68. Mathiowetz, V, Bass Haugen, J. Motor behavior research: implications for therapeutic approaches to central nervous system dysfunction. Am J Occup Ther. 1994;48(8):733.
69. Milazzo, S, Gillen, G. Splinting applications. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
70. Neistadt, ME. A critical analysis of occupational therapy approaches for perceptual deficits in adults with brain injury. Am J Occup Ther. 1990;44(4):299.
71. Neistadt, ME. Occupational therapy treatments for constructional deficits. Am J Occup Ther. 1992;46(2):141.
72. Neistadt, ME. Perceptual retraining for adults with diffuse brain injury. Am J Occup Ther. 1994;48(3):225.
73. Pollock, N. Client-centered assessment. Am J Occup Ther. 1993;47(4):298.
74. Post-Stroke Rehabilitation Guideline Panel. Post-stroke rehabilitation: clinical practice guidelines # 16. Rockville, Md: U.S. Department of Health and Human Services, Agency for Healthcare Policy and Research; 1995.
75. Rao, A. Approaches to motor control dysfunction: an evidence-based review. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
76. Rensink, M, Schuurmans, M, Lindeman, E, Hafsteinsdottir, T. Task-oriented training in rehabilitation after stroke: systematic review. J Adv Nurs. 2009;65(4):737–754.
77. Roth, EJ. Medical complications encountered in stroke rehabilitation. Phys Med Rehabil Clin North Am. 1991;2(3):563.
78. Rubenstein, E, Federman, D. editors: Neurocerebrovascular diseases. New York, NY: Scientific American; 1994.
79. Rubio, KB, Gillen, G. Treatment of cognitive-perceptual deficits: a function-based approach. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
80. Ryerson, S, Levit, K. The shoulder in hemiplegia. In Donatelli RA, ed.: Physical therapy of the shoulder, ed 2, Edinburgh, Scotland: Churchill Livingstone, 1991.
81. Sandin, KJ, Smith, BS. The measure of balance in sitting in stroke rehabilitation prognosis. Stroke. 1990;21(1):82.
82. Scheiman, M. Understanding and managing vision deficits: a guide for occupational therapists. Thorofare, NJ: Slack; 1997.
83. Steultjens, EM, Dekker, J, Bouter, LM, et al. Occupational therapy for stroke patients: a systematic review. Stroke. 2003;34(3):676.
84. Shumway-Cook, A, Horak, FB. Balance rehabilitation in the neurological patient. Course syllabus. Seattle, Wash: NERA; 1992.
85. Shumway-Cook, A, Woollacott, M. Motor control: theory and practical applications, ed 3. Baltimore, Md: Lippincott Williams & Wilkins; 2006.
86. Stewart, C, Riedel, K. Managing speech and language deficits after stroke. In Gillen G, ed.: Stroke rehabilitation: a function-based approach, ed 3, St Louis, Mo: Mosby, 2011.
87. Taub, E, Miller, NE, Novack, TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993;74(4):347–354.
88. Teasdale, G, Jennett, B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2(7872):81.
89. Thomson-Kohlman, L. The Kohlman evaluation of living skills,, ed 3. Bethesda, Md: American Occupational Therapy Association; 1992.
90. Tinetti, ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119.
91. Toglia, J. Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991;45(6):505.
92. Trombly, CA. Anticipating the future: assessment of occupational function. Am J Occup Ther. 1993;47(3):253.
93. Trombly, CA. Deficits in reaching in subjects with left hemiparesis: a pilot study. Am J Occup Ther. 1992;46(10):887.
94. Trombly, CA. Observations of improvements in five subjects with left hemiparesis. J Neurol Neurosurg Psychiatry. 1993;56(1):40.
95. Trombly, CA, Ma, HI. A synthesis of the effects of occupational therapy for persons with stroke, Part I: restoration of roles, tasks, and activities. Am J Occup Ther. 2002;56(3):250.
96. Uswatte, G, Taub, E, Morris, D, et al. The Motor Activity Log-28: assessing daily use of the hemiparetic arm after stroke. Neurology. 2006;67(7):1189–1194.
97. Uswatte, G, Taub, E, Morris, D, et al. Reliability and validity of the upper-extremity Motor Activity Log-14 for measuring real-world arm use. Stroke. 2005;36(11):2493–2496.
98. Ware, JE, Sherbourne, CD. The MOS 36-item short form health survey: conceptual framework and item selection. Med Care. 1992;30(6):473.
99. Wilson, DJ, Baker, LL, Craddock, JA. Functional test for the hemiparetic upper extremity. Am J Occup Ther. 1984;38:159.
100. World Health Organization. International classification of diseases—10. Geneva, Switzerland: WHO; 2007.
101. Wu, SH, Huang, HT, Lin, CF, Chen, MH. Effects of a program on symmetrical posture in patients with hemiplegia: a single-subject design. Am J Occup Ther. 1996;50(1):17–23.
102. Yesavage, JA, Brink, TL, Rose, TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37–49.
103. Zorowitz, RD, Hughes, MB, Idank, D, et al. Shoulder pain and subluxation after stroke: correlation or coincidence? Am J Occup Ther. 1996;50(3):194–201.