Chapter 9 The Concept of Lower and Upper Motor Neurons and Their Malfunction
1. The lower motor neuron is classically defined as the alpha (α) motor neuron.
2. Disease of lower motor neurons causes stereotypical clinical signs.
3. Upper motor neurons lie completely in the central nervous system and control lower motor neurons.
4. Signs of upper motor neuron disease differ from signs of lower motor neuron disease.
The majority of veterinary patients with neurological disease display some abnormality of posture and locomotion. The abnormalities range from weakness or paralysis to spasticity, rigidity, and convulsions. The goal of the diagnostic process for such patients is to determine the location, the extent, and the cause of the lesion. Central to diagnostic logic in neurology is deciding whether the patient’s lesion is located in the lower motor neurons or the upper motor neurons. (The two other possible locations of lesions causing movement disorders are the neuromuscular junction and skeletal muscle.)
This chapter defines lower and upper motor neurons because these concepts are useful in understanding the physiology of posture and locomotion and are essential in locating pathological processes in the nervous system. Malfunctions of these two neuron populations are also described briefly.
The Lower Motor Neuron Is Classically Defined as the Alpha (α) Motor Neuron
The concept of a lower motor neuron is decades old in neurology. The alpha (α) motor neuron is classically defined as a neuron whose cell body and dendrites are located in the central nervous system (CNS) and whose axon extends out through the peripheral nerves to synapse with the extrafusal skeletal muscle fibers (Figure 9-1). The cell bodies of these neurons are located either in the ventral horn of spinal cord gray matter or in cranial nerve nuclei of the brainstem. This is the “final common pathway” through which the CNS channels commands to respective skeletal muscles, or combinations of those muscles, to produce movement. This definition predates the discovery of gamma (γ) motor neurons, which innervate muscle spindles, and some authors would include γ motor neurons in the definition of lower motor neurons. Some also consider postganglionic autonomic neurons to be lower motor neurons (see Chapter 13). Virtually all the clinical signs caused by lower motor neuron disease, however, can currently be explained by the loss or malfunction of the α motor neuron.
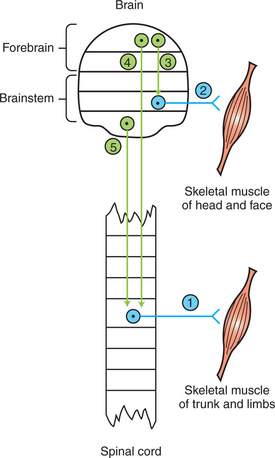
FIGURE 9-1 General organization of lower and upper motor neurons. Blue, Lower motor neurons typically originate in the ventral horn of the spinal cord (neuron 1) or in cranial nerve nuclei (neuron 2) and synapse within skeletal muscle. Green, Upper motor neurons typically originate in the brain and project to and control lower motor neurons. Upper motor neurons usually belong to the corticobulbar (neuron 3), corticospinal (neuron 4), or bulbospinal, also called brainstem motor (neuron 5), pathways. Arrowheads indicate that local synapses may be interposed between the upper and lower motor neurons. Horizontal lines delimit either spinal cord segments (e.g., L1, L2) or major brain divisions (e.g., medulla, pons).
Disease of Lower Motor Neurons Causes Stereotypical Clinical Signs
Regardless of the pathological basis for disease of lower motor neurons, a stereotypical set of clinical signs results in the skeletal muscles they innervate.
1. Paralysis or paresis. Disease of the α motor neurons usually prevents the neurons’ action potentials from reaching the neuromuscular junction. Therefore, despite the brain’s command to the muscle to contract, the message cannot reach the muscle, and paralysis is the result. In fact, such paralysis can be so complete that the adjective flaccid is used to describe the paralysis in which no muscle contraction occurs. Because not all the α motor neuron axons of a peripheral nerve may be affected by an insult, and because muscles can be supplied by axons of more than one spinal nerve, paralysis may be incomplete. This symptom is referred to as paresis.
2. Atrophy. Atrophy is the shrinking or wasting of skeletal muscle mass distal to the lower motor neuron lesion. This occurs within days of the injury to a nerve. The exact origins of this atrophy are controversial. However, evidence indicates that the reduced frequency of muscle stimulation caused by α motor neuron insult and the resulting reduced use of the muscle trigger reductions in muscle protein synthesis and increases in muscle proteolysis. The magnitude of this denervation atrophy can be reduced by direct electrical stimulation of the muscle itself.
3. Loss of segmental and intersegmental reflexes. Segmental and intersegmental reflexes require a viable α motor neuron in the reflex arc for the reflex response to occur (see Chapter 7). Therefore, such reflexes as the muscle stretch (knee jerk) reflex and the toe-pinch withdrawal (nociceptive) reflex, as well as the proprioceptive positioning reaction, fail to occur because the motor neuron portion of the arc, which activates the skeletal muscle, is gone.
4. Electromyographic changes. Within a few days of damage to α motor neurons, abnormal electrical activity of the muscle can be observed on an electromyogram (see Chapter 6).
Damage of α motor neurons occurs often on insult to a peripheral nerve that also contains axons of sensory neurons. Therefore, there may be an accompanying loss of sensory modalities, although this is not a cardinal sign of lower motor neuron damage.
Upper Motor Neurons Lie Completely in the Central Nervous System and Control Lower Motor Neurons
Upper motor neurons are the neurons of the CNS that influence the lower motor neurons. They are typically considered the neurons of origin of the corticospinal (cerebral cortex to spinal cord), corticobulbar (cerebral cortex to brainstem), and brainstem motor (brainstem to spinal cord; also called bulbospinal) pathways (see Chapter 10). Upper motor neurons send axons down to the spinal cord or into the brainstem to control the lower motor neurons (see Figure 9-1).
Signs of Upper Motor Neuron Disease Differ from Signs of Lower Motor Neuron Disease
Lesions of upper motor neurons cause clinical signs that are significantly different from those produced by lower motor neuron disease, although paralysis/paresis may be seen in both scenarios.
1. Inappropriate movement. Lesions of upper motor neurons can cause a variety of movement disorders, depending on the location of the lesion. Spinal cord disease, affecting portions of upper motor neurons projecting to the cord, often causes various degrees of weakness below the lesion. Disease of the brain that affects upper motor neurons may cause seizures, rigidity, circling gaits, and other inappropriate movements. More specific examples of this general category are presented in Chapters 10, 11, and 12 on the central control of movement, the vestibular system, and the cerebellum, respectively.
2. No atrophy. Because the lower motor neuron is intact, the muscle does not atrophy. (Modest disuse atrophy may develop much later.)
3. Retained but exaggerated segmental reflexes. Because the neuronal circuitry of the segmental reflex arc (see Chapter 7) is not interrupted in upper motor neuron disease, reflexes such as the muscle stretch and toe-pinch withdrawal are retained, whereas in lower motor neuron disease reflexes are depressed or lost. Because upper motor neurons are normally capable of exerting significant inhibitory control over spinal reflexes, however, damage to these neurons can decrease this inhibition, resulting in exaggeration of the reflex response (hyperreflexia).
4. Normal electromyogram. Because the muscle is not atrophied and the lower motor neurons are intact, the electrical activity of the muscle appears normal.
The following clinical correlations illustrate common examples of lower and upper motor neuron disease. Before going to Chapter 10, the reader should understand these concepts and why these dogs have the clinical signs mentioned.
CLINICAL CORRELATIONS
Lower Motor Neuron Disease
History.
A 2-year-old male German short-haired pointer was admitted to the local veterinary clinic. His vaccinations were current, and the dog had no history of contributing prior illness.
A few days before admission, the dog had a fight with a skunk. For 48 hours before admission, an ascending paralysis developed, characterized initially by weakness and then by the lack of voluntary movement, of first the back legs and then the front legs. No barking was noticed during the illness. The dog was able to control his bladder and bowel and to move his head.
Clinical Examination.
On admission, the dog was unable to bear weight on any of his four legs. Other than an elevated respiratory rate, physical examination deficits were limited to the nervous system. The dog was able to eat, drink, and move his head. A severe paralysis was noted in all legs, and no motor response to a toe pinch or tapping of the quadriceps tendon could be elicited. There was widespread atrophy of the muscles of all four legs, as well as those of the thorax and abdomen. The dog did seem to be aware of painful stimuli (deep pain response). There were no cranial nerve deficits. Results of routine blood cell counts and serum chemistry results were within normal limits.
Comment.
Generalized atrophy, paralysis, and loss of segmental reflexes indicate widespread, bilateral loss of lower motor neuron function. Fortunately, the disease has spared the muscles of the head and the diaphragm, although the dog’s elevated respiratory rate indicates an attempt to compensate for paralysis of some of the respiratory muscles. A clinical diagnosis of polyradiculoneuritis (“coonhound paralysis”) was made. This disease is often preceded by the bite of another animal. Pathological changes are found predominantly in the ventral roots of the spinal cord, where the axons of the lower motor neurons leave the spinal cord. The dorsal roots are usually spared, which explains this dog’s apparent ability to feel pain. The clinical signs are those of widespread lower motor neuron disease. The syndrome resembles Guillain-Barré syndrome in humans, and both syndromes have been suggested to be autoimmune in origin.
Upper Motor Neuron Disease
History.
A 5-year-old male dachshund is brought to a local veterinary clinic. His vaccination history is current, and the dog has had no contributing past medical or surgical illnesses. Two days before admission, he seemed to be in pain. Throughout the next day the dog became progressively weak in the hind legs.
Clinical Examination.
Physical examination abnormalities were limited to the nervous system. The dog was bright, alert, responsive, and able to bear weight normally on the front legs. However, he was weak and unsteady on the hind legs. No atrophy was apparent. All cranial nerve reflexes were normal, as were the spinal segmental reflexes of both front and hind legs. Intersegmental responses, including the proprioceptive positioning reaction, were normal in the front legs but absent in the hind legs (see Chapter 7). (Failure to exhibit the normal proprioceptive placing reaction indicates a lesion somewhere along the sensory or motor routing for this response. This routing includes the peripheral nerves for that limb, the spinal cord rostral to that limb on the same side, and the contralateral side of the brain.) Results of a complete blood cell count and serum chemistry analysis were within normal limits.
Comment.
The absence of atrophy and the retention of segmental reflexes in the affected limbs indicate that the lower motor neurons, neuromuscular junction, and skeletal muscle are normal and that this is an upper motor neuron disease. Because only the hind limbs are affected by weakness and exhibit a deficit in proprioceptive placing, the cervical spinal cord and brain must be normal since motor commands to the front legs are transmitted reliably. Therefore the lesion must be between the front and hind limbs. This is a typical history and a typical clinical presentation for a dog with a herniated intervertebral disk.
Treatment.
Treatment and prognosis depend on the severity of the spinal cord trauma. Medical management is aimed at reducing edema, vasospasm, inflammation, and other metabolic consequences of the disease that worsen the damage to the spinal cord. When surgery is indicated by the severity of the trauma, the goal is to relieve spinal cord compression. With appropriate medical and surgical management, many dogs recover useful spinal function.
Brodal P. The central nervous system: structure and function, ed 3. New York: Oxford University Press, 2004.
Dow DE, Dennis RG, Faulkner JA. Electrical stimulation attenuates denervation and age-related atrophy in extensor digitorum longus muscles of old rats. J Gerontol A Biol Sci Med Sci. 2005;60(4):416.
Jackman RW, Kandarian SC. The molecular basis of skeletal muscle atrophy. Am J Physiol Cell Physiol. 2004;287:C834.
Kandel ER, Schwartz JH, Jessell TM. Principles of neural science, ed 4, New York: McGraw-Hill, 2000.
Lorenz MD, Kornegay J. Oliver and Lorenz’s handbook of veterinary neurology, ed 4. Philadelphia: Saunders, 2004.
Purves D, Augustine G, Fitzpatrick D, et al. Neuroscience, ed 3. Sunderland, Mass: Sinauer Associates, 2004.
PRACTICE QUESTIONS
1. Which of the following would not be considered an upper motor neuron?
2. You examine a dog that is unable to stand and bear weight on the right rear leg. The right rear leg is much smaller in diameter than the left rear leg. Pinching the toe on the left rear leg results in withdrawal of the left rear leg, but pinching the toe on the right rear leg results in no movement of the right rear leg. The proprioceptive placing response to the left rear leg is normal, but to the right rear leg it is absent. Where is this dog’s pathological lesion?
3. You examine a dog that is bright, alert, and responsive. She can stand and bear weight on both front legs, but she cannot stand or bear any weight on the back legs. Her knee jerk and toe-pinch withdrawal reflexes are normal in all four legs. There is no atrophy. The proprioceptive positioning response is normal in the front legs but absent in both rear legs. Injecting acetylcholinesterase-inhibiting drugs causes no change in the clinical signs. Where is this dog’s pathological lesion most likely located?
4. You examine a dog that is bright, alert, and responsive but unable to stand on any of the four legs. Toe-pinch and knee jerk local (segmental) reflexes are normal in all four legs. There is no atrophy. The proprioceptive positioning response is absent in all four legs. Injecting an acetylcholinesterase-inhibiting drug does not change the clinical signs. Where is this dog’s pathological lesion most likely located?
5. You are presented with a horse that is unable to stand or support any weight on the hind legs. You electrically stimulate both the sciatic and the femoral nerve with a sufficient stimulus, but neither stimulation results in muscular contraction. However, direct stimulation of both the gastrocnemius and the quadriceps femoris muscle of the rear leg results in muscular contraction. From these observations, what do you logically conclude to be the location of this horse’s pathological lesion?
6. You examine a cat that cannot bear weight on the hind legs. The cat is bright, alert, and responsive. Atrophy is present in the back legs. Cranial nerve reflexes are within normal limits, as are segmental reflexes and the proprioceptive positioning responses of the front legs. Knee jerk and toe-pinch withdrawal reflexes are absent in the hind legs. What is the most likely location for this cat’s pathological lesion?