Chapter 13 The Autonomic Nervous System and Adrenal Medulla
1. The autonomic nervous system differs from the somatic motor system in at least two important ways.
2. The autonomic nervous system has two major subdivisions.
3. The sympathetic nervous system arises from the thoracolumbar spinal cord.
4. The parasympathetic nervous system arises from the brainstem and spinal cord.
5. Most autonomic neurons secrete either acetylcholine or norepinephrine as a neurotransmitter.
6. Acetylcholine and norepinephrine have different postsynaptic receptors.
7. There are general differences in sympathetic and parasympathetic function.
8. The autonomic nervous system participates in many homeostatic reflexes.
9. Preganglionic neurons are influenced by many regions of the brain.
10. Loss of autonomic neurons results in the hypersensitivity of the target organ to transmitter.
The autonomic nervous system (ANS) is a part of the nervous system that is generally not under conscious control. For this reason, this segment of the nervous system is called autonomic, from two Greek words meaning “self-governing” or “independent.” The ANS is usually defined as a peripheral motor system innervating smooth muscle, cardiac muscle, and some glandular tissue, although it is subject to reflex and cerebral control. It regulates such subconscious body functions as blood pressure, heart rate, intestinal motility, and the diameter of the eye’s pupil. The ANS has unique anatomy, synaptic transmission, and effect on its various target organs. It is the site of action of a large number of drugs and is essential for homeostasis.
This chapter describes the general anatomy and function of the ANS. The specific effect of the ANS on particular target organs is described in the chapters for each of the body’s systems.
The Autonomic Nervous System Differs from the Somatic Motor System in at Least Two Important Ways
The ANS differs from the somatic motor system in its target organs and in the number of neurons in its peripheral circuit. The somatic motor system innervates skeletal muscle, which is the muscle responsible for all movements of the body, as described in Chapters 5 and 6. In contrast, the ANS innervates smooth muscle, cardiac muscle, and some glands (Box 13-1). Cardiac muscle is the muscle of the heart (see Chapter 19). Smooth muscle is the muscle in blood vessels, in most of the gastrointestinal tract, in the bladder, and in other hollow visceral structures.
The ANS also differs in the number of neurons it has in the peripheral nervous system (Figure 13-1). The somatic nervous system has one neuron whose cell body is located in the central nervous system (CNS) and whose axon extends, uninterrupted, to the skeletal muscle, where the peripheral chemical synapse occurs. In contrast, the ANS has two peripheral neurons. The first, called a preganglionic neuron, also has its cell body in the CNS, but its axon innervates a second neuron in the chain, called the postganglionic neuron. Its cell body is in a peripheral structure called a ganglion, a collection of nerve cell bodies outside the CNS (recall the example of the dorsal root ganglia of sensory nerves leading to the spinal cord). There are chemically mediated synapses both between the preganglionic and postganglionic neurons and between the postganglionic neuron and its target organ.
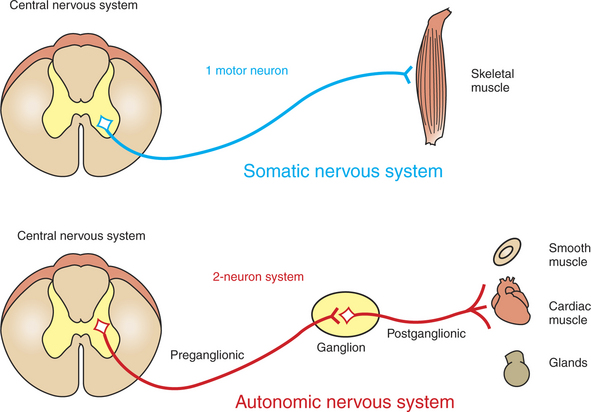
FIGURE 13-1 The autonomic nervous system (ANS) differs from the somatic motor system in the number of neurons that it has in the peripheral nervous system. The somatic motor system has one neuron, whose cell body is located in the central nervous system (CNS) and whose axon extends, uninterrupted, to the skeletal muscle, where the peripheral chemical synapse occurs. In contrast, the ANS has two neurons in the path from the CNS to the target. The first, called a preganglionic neuron, also has its cell body in the CNS, but its axon innervates a second neuron in the chain, called the postganglionic neuron. Its cell body is in a peripheral structure called a ganglion.
The ANS also differs from the somatic motor system in the amount of myelin along the peripheral axons; postganglionic neurons are usually unmyelinated. In addition, somatic motor neurons always excite their skeletal muscle targets, whereas the autonomic postganglionic neurons can either excite or inhibit their targets.
The Autonomic Nervous System Has Two Major Subdivisions
The ANS is divided into two major subdivisions based on the anatomical origin of their preganglionic neurons and on their synaptic transmitters at the target organ. These two subdivisions are the sympathetic nervous system and the parasympathetic nervous system.
The Sympathetic Nervous System Arises from the Thoracolumbar Spinal Cord
The sympathetic nervous system generally has short preganglionic and long postganglionic axons. Preganglionic axons of the sympathetic nervous system leave the spinal cord by way of the ventral roots of the first thoracic through the third or fourth lumbar spinal nerves (Figure 13-2). For this reason, the sympathetic nervous system is often called the thoracolumbar system. The preganglionic axons pass through the ventral root and then a communicating branch (ramus) to enter the paravertebral sympathetic ganglion chain (also called the “sympathetic trunk”), where most synapse with a postganglionic neuron (Figure 13-3). The ganglion chain actually extends from cervical to sacral regions. The postganglionic axons then extend to one of the hollow visceral organs or reenter the spinal nerves to extend to more distal structures such as blood vessels, sweat glands, and hair erector muscles of the body wall. A few preganglionic axons pass through the paravertebral ganglia, forming splanchnic nerves that synapse with postganglionic neurons in prevertebral ganglia, usually named for neighboring blood vessels. Postganglionic neurons of the prevertebral ganglia also innervate hollow visceral organs.
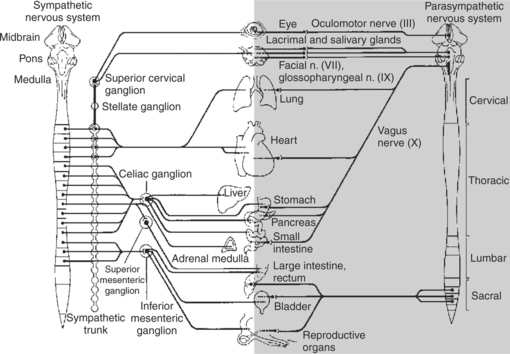
FIGURE 13-2 The site of origin of preganglionic neurons in the central nervous system for both the sympathetic nervous system (left) and the parasympathetic nervous system (right). Several sites of projection of postganglionic axons are also shown.
(From Kandel ER, Schwartz JH: Principles of neural science, ed 2, New York, 1985, Elsevier Science Publishing.)
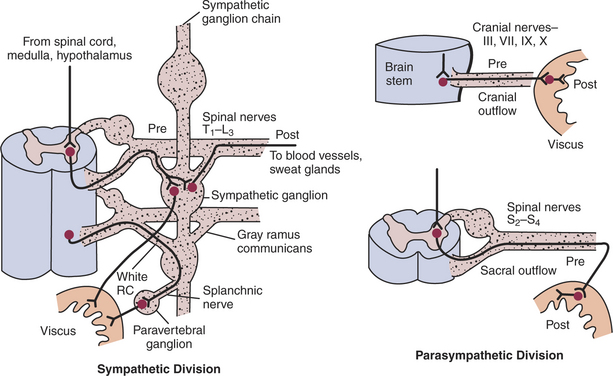
FIGURE 13-3 Synaptic organization of preganglionic (Pre) and postganglionic (Post) neurons of the sympathetic and parasympathetic divisions of the autonomic nervous system. RC, Ramus communicans (communicating branch).
(From Ganong WF: Review of medical physiology, ed 13, Norwalk, Conn, 1987, Appleton & Lange.)
The adrenal medulla is a special variation on this anatomical theme. A few sympathetic preganglionic axons extend all the way to the adrenal medulla, where they synapse with rudimentary postganglionic neurons that make up the adrenal medullary secretory cells. These vestigial postganglionic neurons secrete their transmitter substance directly into the circulating blood. The transmitter substance, acting as a true hormone, is carried by the blood to all tissues of the body.
The Parasympathetic Nervous System Arises from the Brainstem and Spinal Cord
The parasympathetic nervous system generally has long preganglionic and short postganglionic axons. Preganglionic axons of the parasympathetic system leave the CNS by way of cranial nerves III, VII, IX, and X and through several sacral spinal nerves. For this reason, it is called the craniosacral system (see Figure 13-2). The long preganglionic axons pass to parasympathetic ganglia in or near the target organ, where they synapse with short postganglionic neurons. (In the gastrointestinal system, postganglionic neurons participate in an extensive enteric neuron network called the intrinsic gastrointestinal nervous system, described in Chapter 27.)
Most viscera receive both sympathetic and parasympathetic innervation. Although the parasympathetic system originates in brainstem and sacral regions, it can provide parasympathetic innervation to organs in the thoracic and lumbar parts of the body by way of the vagus nerve (cranial nerve X), which wanders to regions of the body cavity. The sympathetic thoracolumbar system can influence organs in cranial and sacral regions by way of preganglionic sympathetic axons that travel to sympathetic postganglionic neurons in cervical and sacral regions of the sympathetic ganglion chain.
Most Autonomic Neurons Secrete Either Acetylcholine or Norepinephrine as a Neurotransmitter
As described in Chapter 5, acetylcholine is the neurotransmitter at the somatic neuromuscular synapse. Acetylcholine is also the neurotransmitter at all autonomic ganglia (Figure 13-4). The neurotransmitter secreted by parasympathetic postganglionic neurons is also acetylcholine. Acetylcholine-releasing synapses are often called cholinergic. Most anatomically sympathetic postganglionic neurons secrete norepinephrine. However, anatomically sympathetic postganglionic neurons traveling to blood vessels of skeletal muscle produce vasodilation and secrete acetylcholine, as do sympathetic, postganglionic neurons to sweat glands in some species. Norepinephrine-releasing synapses are often called adrenergic.
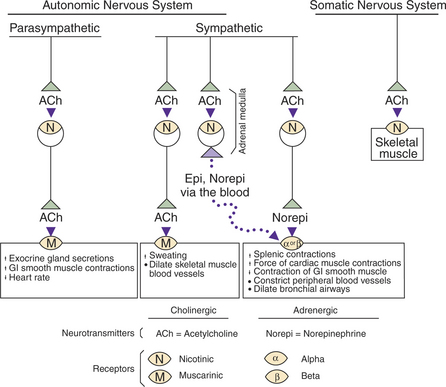
FIGURE 13-4 Classification of autonomic and somatic motor neurons with regard to their transmitter or mediator released, their postsynaptic receptors, and their general influence on the effector organ. Acetylcholine (ACh), released from the presynaptic membrane, can stimulate either a muscarinic (M) or a nicotinic (N) postsynaptic receptor, depending on the particular location of the synapse. Similarly, norepinephrine (Norepi) can stimulate either α or β receptors, again depending on the location of the synapse. Epi, epinephrine; GI, gastrointestinal.
In the case of the adrenal medulla, incoming preganglionic axons release acetylcholine, but the vestigial, postganglionic neurons of the adrenal medullary tissue release primarily epinephrine and some norepinephrine into the circulating blood.
It is important that, once released, the neurotransmitter not linger in the synaptic cleft. The neurotransmitter must be either destroyed in the cleft or dissipated so that the postsynaptic membrane can recover its resting potential and be ready for the next synaptic transmission. Because some synapses can transmit impulses up to several hundred times per second, neurotransmitter destruction must occur quickly. In the case of acetylcholine, acetylcholinesterase destroys the transmitter in the cleft. For norepinephrine, reuptake by the presynaptic neuron is the principal way in which its synaptic effect on the postsynaptic membrane is terminated. The hormonal actions of circulating epinephrine and norepinephrine released by the adrenal medulla, however, are primarily terminated by the enzyme catechol-O-methyltransferase (COMT), with a lesser contribution of the enzyme monoamine oxidase (MAO). These enzymes are widely distributed in the body, with highest concentrations in the liver and kidney.
Acetylcholine and Norepinephrine Have Different Postsynaptic Receptors
The neurotransmitters secreted by the ANS all stimulate their target organ by first binding with a postsynaptic receptor. These receptors are proteins in the cell membrane. When the transmitter binds with the postsynaptic receptor, the membrane’s permeability to selected ions is changed, and the postsynaptic membrane potential either increases or decreases, with a resulting change in the probability of action potentials in the postsynaptic cell.
Acetylcholine stimulates two different types of receptors (Figure 13-4). Muscarinic acetylcholine receptors are found on all the target cells stimulated by postganglionic parasympathetic neurons and cholinergic postganglionic neurons of the sympathetic nervous system. Nicotinic receptors are found at all synapses between autonomic preganglionic and postganglionic neurons and at the somatic neuromuscular junction.
Muscarinic receptors were named because they are stimulated by muscarine, a toadstool poison. Muscarine does not stimulate nicotinic receptors. Nicotine stimulates the nicotinic receptors but not muscarinic receptors. Acetylcholine stimulates both, and different drugs block each receptor. For example, atropine blocks muscarinic receptors, whereas curare blocks nicotinic receptors.
There are two major types of adrenergic receptors, called alpha (α) and beta (β) receptors. The β receptors have been further subdivided into β1 and β2 receptors, on the basis of the effect of adrenergic blocking and stimulating drugs. There is now evidence for a third class of β receptor (β3) and for two classes of α receptor (α1 and α2).
There Are General Differences in Sympathetic and Parasympathetic Function
Although the sympathetic and parasympathetic systems are both important for homeostasis—maintaining the constancy of the internal environment—there are some important general differences in their function.
In physical and some emotional stress, the sympathetic (adrenergic) system discharges as a unit, resulting in widespread stimulation of the body. This causes an increase in heart rate and blood pressure, dilation of the pupil of the eye, an elevation in levels of blood glucose and free fatty acids, and an increased state of arousal. All these widespread effects are useful in responding to an emergency. Therefore the sympathetic system is sometimes referred to as the “fight or flight” system. The effect of sympathetic discharge not only is widespread but lasts longer than parasympathetic (cholinergic) discharge because of the prolonged circulation of epinephrine and norepinephrine. Indeed, the adrenal medulla’s secretion of epinephrine and norepinephrine into the circulating blood provides prolonged adrenergic stimulation to the entire body, even to some tissues that do not have direct sympathetic postganglionic stimulation.
Although the adrenergic system usually has a widespread effect, it is also capable of discrete control of particular organs. For example, the dilator smooth muscle in the iris causes enlargement of the pupil in low ambient light without more widespread effects on the body.
In contrast, the parasympathetic (cholinergic) system has more discrete effects on particular organs and is more concerned with the restorative aspects of daily living. For example, cholinergic stimulation assists digestion and absorption of food by increasing gastric secretion, increasing intestinal motility, and relaxing the pyloric sphincter. For this reason, the parasympathetic nervous system is sometimes called the anabolic or restorative nervous system, as well as the “rest and digest” system.
Many organs of the body have both sympathetic (adrenergic) and parasympathetic (cholinergic) innervation, each with a reciprocal effect. For example, adrenergic stimulation increases heart rate, whereas cholinergic stimulation decreases heart rate. Adrenergic stimulation enlarges pupillary diameter, whereas cholinergic stimulation causes pupillary constriction.
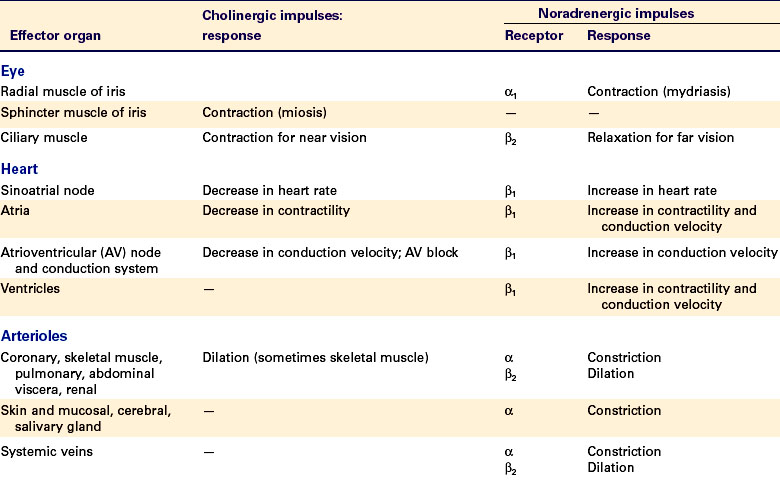
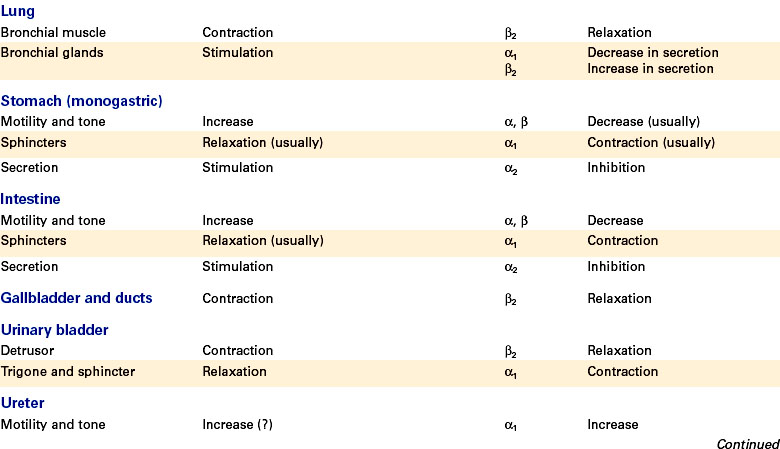
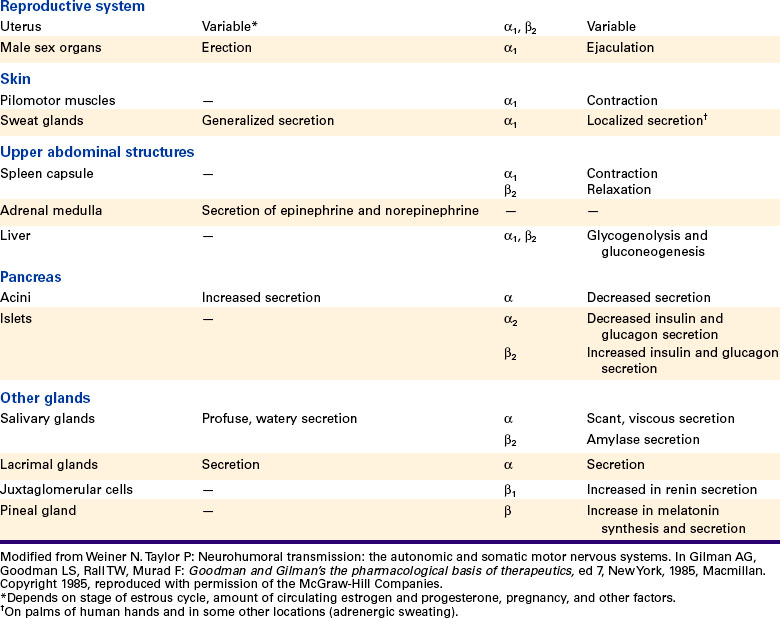
Table 13-1 gives a more complete listing of the response of various organs to adrenergic and cholinergic stimulation.
The Autonomic Nervous System Participates in Many Homeostatic Reflexes
Many of the body’s visceral functions are regulated by autonomic reflexes. As with reflex arcs in the somatic nervous system (see Chapter 7), autonomic reflex arcs also include a sensory side to the arc, including a visceral receptor; a sensory neuron, often called a visceral afferent neuron; and one or more synapses in the CNS. The ANS is usually defined as the peripheral motor preganglionic and postganglionic neurons. Visceral afferent neurons are often not included in this definition but generally are essential parts of the autonomic reflex arc.
Autonomic reflexes are extremely common and are described in detail for each body system in later chapters. A few are described briefly here as examples.
Control of Blood Pressure
Stretch receptors in the internal carotid artery and the aorta detect systemic blood pressure. As blood pressure rises above normal limits in animals, sympathetic adrenergic vaso-constrictor nerves are inhibited, and blood pressure falls back to within normal limits. (It is not clear why this does not happen in hypertensive humans.)
Pupillary Light Reflex
When a flashlight is shone into an animal’s eye, light stimulates photoreceptors in the retina (see Chapter 14). Sensory action potentials are then transmitted to the brainstem along the optic nerve, where, through several interneurons, parasympathetic cholinergic neurons stimulate the constrictor smooth muscle of the iris. This causes the pupillary diameter to become smaller.
Gastric secretion of digestive fluids in anticipation of food and emptying of the rectum and bladder in response to filling are but a few of the many other autonomic reflexes described in more detail throughout this book.
Preganglionic Neurons Are Influenced by Many Regions of the Brain
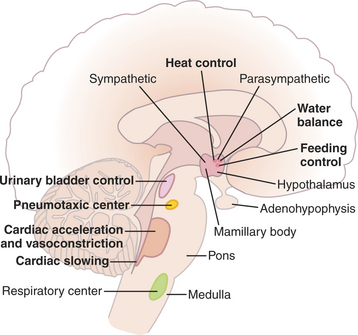
Much as the lower motor neuron of the somatic system is influenced by the upper motor neuron (see Chapter 9), the preganglionic autonomic neuron is also influenced by CNS axons descending from the brainstem, hypothalamus, and even the cerebral cortex. Many brainstem nuclei are known to influence preganglionic neurons in order to control particular visceral functions; Figure 13-5 illustrates several such regions. In turn, each of these brainstem regions can be influenced by the hypothalamus and cerebral cortex of the forebrain, creating a complex system of upper motor neurons within the CNS that helps coordinate autonomic reflexes and directly influences action potential frequency within preganglionic neurons. As more is learned about these central systems controlling the ANS, their role in such conditions as hypertension and various gastrointestinal diseases may become clearer.
Loss of Autonomic Neurons Results in the Hypersensitivity of the Target Organ to Transmitter
When the postganglionic neuron to a target organ is lost, the smooth muscle of that organ becomes hypersensitive to any transmitter circulating in the blood. For example, the arterioles of the skin are usually under some adrenergic stimulation, which results in some vasoconstriction. If the postganglionic adrenergic neuron to the skin is destroyed, vasodilation occurs. However, if norepinephrine is injected into the blood supply to this area of skin, a dramatic (hypersensitive) vasoconstriction occurs. This is thought to be caused, at least in part, by an increase in numbers of postsynaptic receptors at the denervated synapse.
CLINICAL CORRELATIONS
Horner’s Syndrome
History.
A 7-year-old male golden retriever is brought to your clinic for examination. The owner states that during the past 3 weeks, the dog has become progressively weaker in his left front leg and now cannot bear weight on that limb. The owner has also noticed that the dog’s left upper eyelid seems to be droopy.
Clinical Examination.
Physical examination abnormalities are limited to the nervous system. The dog is bright, alert, and responsive. Except for the left front leg, cranial nerve and spinal segmental reflexes and all intersegmental responses are within normal limits. The dog cannot bear weight on the left front leg, and the leg muscles are atrophied. No segmental reflexes (e.g., toe-pinch withdrawal) or intersegmental responses (e.g., proprioceptive placing) can be elicited in the left front leg. The left upper eyelid droops lower than the right upper lid, and the left pupil is smaller than the right pupil. The left nictitating membrane (third eyelid) is prolapsed over part of the cornea, and the left eye seems more sunken into the orbit than the right eye.
Comment.
This dog has a lesion of the left brachial plexus, probably a neoplasm. It has caused a lower motor neuron syndrome to the left front leg with atrophy, paralysis, and loss of reflexes. The tumor has damaged the preganglionic neurons of the left sympathetic nervous system as they leave the first two thoracic segments on their way toward the eye. Loss of the sympathetic innervation to the region of the eye causes smallness of the pupil (miosis), drooping of the upper eyelid (ptosis), a sunken appearance in the eye (enophthalmos), and prolapse of the nictitating membrane. This constellation of clinical signs is called Horner’s syndrome.
Sympathetic preganglionic neurons pass through the brachial plexus (where they were damaged in this dog) and ascend in the vagosympathetic trunk to synapse with the postganglionic neurons in the cranial cervical ganglia. The postganglionic cell axons then go to the region of the eye, where they innervate the dilator smooth muscle cells of the iris. When paralyzed, the constrictor fibers of the iris are unopposed, resulting in miosis. The sympathetic nervous system also innervates several smooth muscle fibers that lift the upper eyelid and help position the nictitating membrane and the eye within the socket. Because the preganglionic fibers are relatively exposed in the neck, they are usually damaged.
Horner’s syndrome can also result from damage to either the postganglionic neurons or the neurons that descend from the hypothalamus to the rostral thoracic cord to control the preganglionic neurons.
Boron WF, Boulpaep EL. Medical physiology: a cellular and molecular approach, updated edition. Philadelphia: Saunders, 2005.
Brodal P. The central nervous system: structure and function, ed 3. New York: Oxford University Press, 2004.
Guyton AC, Hall JE. Textbook of medical physiology, ed 11. Philadelphia: Saunders, 2006.
Haines DE. Fundamental neuroscience for basic and clinical applications. Philadelphia: Churchill Livingstone, 2006.
Strain GM. Autonomic nervous system. Reece WO, ed. Duke’s physiology of domestic animals, ed 12, Ithaca, NY: Comstock Cornell University Press, 2004.
Stromberg MW. The autonomic nervous system. Evans HE, ed. Miller’s anatomy of the dog, ed 3, Philadelphia: Saunders, 1993.
Westfall TC, Westfall DP. Neurotransmission: the autonomic and somatic motor nervous systems. Brunton LL, Lazo JS, Parker KL. Goodman and Gilman’s the pharmacological basis of therapeutics, ed 11, New York: McGraw-Hill, 2006.
PRACTICE QUESTIONS
1. Choose the incorrect statement below:
2. The chemical neurotransmitter between preganglionic and postganglionic neurons of the parasympathetic component of the autonomic nervous system is:
3. The neurotransmitter most often found at the synapse between sympathetic postganglionic neurons and their targets is:
4. Which of the following is true regarding sympathetic preganglionic neurons?