chapter 14 Functional mobility
After completing this chapter, the reader will be able to accomplish the following:
1. Recognize the impact of impairment on mobility tasks.
2. Analyze specific movement patterns observed during mobility tasks and common compensatory strategies.
3. Use a function-based approach to retraining mobility patterns.
4. Understand the impact of environmental changes on mobility tasks.
5. Understand how to structure the environment to promote learning of mobility tasks.
6. Understand how to use specific strategies to promote learning of mobility tasks.
Terminology
Many terms have been used in occupational therapy practice to describe an individual’s ability to change the position of the body in space and move within the environment. Mobility broadly refers to movements that result in a change of body position or location. The term bed mobility has been used interchangeably with gross mobility within the rehabilitation setting and traditionally has included tasks such as rolling to both sides, rolling to side lying, moving from a sitting to a supine position and vice versa, and moving from sitting to standing. Transfer refers to movement from one surface to another such as from a bed to a wheelchair, from a wheelchair to a toilet, or from a wheelchair to a car, and involves varied methods of achievement.
Overview of the literature
Within the literature, numerous studies have carefully examined mobility functions of the adult in relation to gait and locomotion. Unfortunately, few studies have examined functional mobility tasks. The analysis of the normal sit-to-stand sequence of movement has received attention and is reviewed later in this chapter.19,20,30,82,83 Rising from bed has been examined in relation to age differences and the most common movement strategies selected.36 This research demonstrates that age-related trends occur across the life span, but great variety remains evident in the selection of specific movement strategies. A limitation of this study is that the oldest age group examined was the 50- to 59-year-old group; thus, information concerning older adults most at risk for stroke was not included. A study of normal adult rolling patterns also has shown that adults exhibit great variability in the selection of movement patterns. In addition, the authors of this study have noted indications that a developmental sequence of movement patterns exists but is not inclusive of all individuals. Clearly many aspects of functional mobility still warrant further investigation.91
Functional mobility: relationship to activities and participation
Occupational therapists have always approached functional mobility from the perspective that individual elements involved in changing the position of the body were necessary to achieve competency in broad areas of occupation. Improvement in activities of daily living (ADL), instrumental activities of daily living (IADL), education, work, play, leisure, and social participation has always been the ultimate goal of occupational therapy. The American Occupational Therapy Association, in “Practice Framework: Domain and Process,” describes functional mobility as “moving from one position or place to another (during performance of everyday activities), such as in-bed mobility, wheelchair mobility, transfers (wheelchair, bed, car, tub, toilet, tub/shower, chair, floor). Performing functional ambulation and transporting objects.”4
Within the Practice Framework, functional mobility is presented as a separate activity category of basic ADL, in which mobility functions occur relative to taking care of one’s own body.
Alternatively, in the International Classification of Functioning, Disability and Health, the World Health Organization presents mobility as a separate domain under the broader category of Activities and Participation. Mobility “is about moving by changing body position or location or by transferring from one place to another, by occupying, moving or manipulating objects, by walking, running or climbing, and by using various forms of transportation.”97
In this more global perspective, mobility is presented as much more than a function of personal self-care. Mobility is viewed as essential to enabling an individual to engage in a full range of life areas and is central to enabling the individual to participate in life situations.
In planning comprehensive treatment programs, the occupational therapist should be mindful that functional mobility is not just relevant to performing self-care tasks but is necessary to permit engagement in education, work opportunities, community life, recreation, leisure, religious pursuits, and domestic life. In practice, the extent to which these areas are addressed may be limited by time constraints imposed by the venue of treatment. Clinicians working within an acute care setting often emphasize basic bed mobility tasks to prepare the patient for independence in grooming, bathing, and dressing activities (see Chapter 1). Within a rehabilitation setting, occupational therapists may have the opportunity to approach functional mobility more comprehensively in relation to more advanced tasks such as community mobility and tasks related to specific work and home-management requirements. The occupational therapist determines goals of treatment with the patient, contingent on imminent and future plans to resume responsibility for activities demanding advanced mobility.
The task-related approach of occupational therapy to intervention to improve functional mobility is consistent with present motor learning research emphasizing the important role environment plays in the organization of movement to solve motor problems (see Chapters 4 to 6).10,39
Impairments of body functions and structures and performance skills have been used to assess abilities in the patient with hemiplegia. Each patient has different strengths, abilities, and impairments that affect the performance of functional mobility. A patient may have strong neuromusculoskeletal and movement-related functions but demonstrate significant impairment in mental functions of sequencing complex movements (e.g., apraxia). Alternately, a patient may have several problems affecting the neuromusculoskeletal system, including decreased alignment and postural stability that interfere with the ability to roll efficiently toward the nonaffected side. Nevertheless, such a patient may demonstrate the ability to learn new strategies to sequence movement to accomplish the task.
Influence of contextual factors on functional mobility
Contextual factors represent a variety of interrelated conditions and situations that may influence an individual’s ability to become proficient in performing mobility tasks. Personal and environmental factors affect the patient with hemiplegia and may support or impede performance.
Personal factors are unique to the individual’s life and living situation and influence the selection of mobility interventions. The occupational therapist considers factors such as age, gender, race, and social background.
When considering the age of an individual who has sustained a stroke and assessing expectations of the potential for functional mobility, the therapist must use caution. Many factors besides age contribute to the differences in the abilities older adults exhibit in functional mobility. The reader is encouraged to explore the literature examining the effect of aging on postural control and life span mobility.
Certainly the patient’s stage in the life cycle more clearly guides assessment and interventions in the consideration of overall mobility needs. The young patient with hemiplegia who attends college has specific mobility needs. Sit-to-stand movements must be accomplished in changing environments and under varying conditions. For example, using public transportation, which may be moving or stationary; rising from a low seat at a football stadium; sitting down in a crowded and darkened movie theater; and getting into a truck present different challenges. These mobility tasks are not unique to young persons, however. The retired person who enjoys traveling frequently and visiting family members also has special mobility needs.
Social and cultural variations also have an effect on the success of functional mobility interventions. The therapist must consider culturally derived boundaries of interaction,57 because the therapist must frequently work within an intimate distance during mobility retraining.43 The physical environment in which interventions occur also affects the patient’s willingness to participate actively. Some patients prefer treatment to occur in the privacy of their hospital rooms, whereas others are more comfortable with these “close encounters” occurring in the open space of a therapeutic gymnasium. The patient, family, significant individuals, and therapist have perceptions and beliefs founded on their cultural conditionings. Similarities and differences of belief may occur in three areas influencing the success of functional mobility retraining: the perceived state of health and illness, the perceived relevance of therapeutic interventions, and the belief that functional mobility is relevant to resuming previous occupations.60
The therapist’s ability to listen to personal needs and appreciate individual values helps ensure success.60 The degree of independence a patient finds acceptable must be self-determined. The therapist must remember that cultural variations influence patient participation and successful outcomes of home programs.4,60,65
Environmental factors are external to the individual and are considered at two levels, individual and societal. Individual environmental factors include the immediate environment of the individual, which can be viewed as the hospital or clinical venue, and the natural environments. Environment determines a patient’s function. The patient with hemiplegia may be able to roll to either side and come to a seated position on a mat or plinth within the clinical setting and engage in donning and doffing of upper extremity clothing. However, in bed within a home setting, the patient may not be able to roll as efficiently or come to a seated position without some assistance. Grooming and dressing tasks may not be practical because of changes in the height and firmness of the supporting surface. These occurrences and the reasons underlying the performance deficits are well-represented in the current motor learning literature. The postural adjustments necessary to roll and come to a seated position to engage in self-care tasks can be learned only in the context of task performance1,21 and in the expected environment.39,40
The treatment of a patient with hemiplegia often occurs on a continuum from acute care through community reintegration. Many treatment environments impose constraints that limit the therapist’s interventions. For example, in intensive care unit settings, therapists must contend with multiple lines, monitors, and alarms (see Chapter 1). Ideally the relearning of motor skills and tasks should occur in the actual environment in which the task will be performed.22,69
Societal environmental factors directly influence the patient’s ability to resume participation in IADL and include systems within the community or society that can assist the individual to resume an active lifestyle outside of one’s immediate living situation.
Functional mobility: the outcome of multiple processes
Functional mobility requires the successful interaction of a number of systems. Carrying out skilled rolling, sitting, and standing does not depend solely on the integrity of the neuromusculoskeletal system. Occupational therapists must be mindful of the interdependence of various sensory, perceptual, and cognitive functions in the execution of these tasks and create evaluation tools that respect this relationship, such as the Árnadóttir Occupational Therapy Neurobehavioral Evaluation (see Chapter 18).This awareness ensures more comprehensive assessment than do evaluations that look at motor behaviors in isolation. Occupational therapists’ knowledge and expertise in task analysis render them uniquely qualified to evaluate and plan treatment to improve functional mobility skills while keeping all the patient’s needs in mind.
Individual differences and variations in movement strategies may be related to factors such as the patient’s build (short, tall, obese, thin) and performance patterns before the stroke (i.e., the patient was a trained athlete, dancer, physically inactive, occasional exerciser, or physical laborer). Additionally, each patient presents with individual habits, routines, and roles that influence movement.29 The psychological state may indeed be reflected in movement (e.g., inhibitions or lack thereof and reactive depression about the current situation). Pain from preexisting conditions or pain as secondary impairment to the stroke may affect movement patterns. These individual differences and their effects on functional mobility have been explored in the literature.91 The occupational therapist must be cognizant of these factors and others in assessment and treatment planning.
Impairment of body functions and structures and skills
Many sequelae associated with a stroke impede performance of functional mobility tasks. The occupational therapist uses basic knowledge of body functions and structures, performance skills, and impairments as a means to organize assessment of an individual’s capacity for functional mobility. The following table summarizes impairments resulting from stroke and their effects on performance of functional mobility skills (Table 14-1).
Table 14-1 Managing Impairments that Affect Functional Mobility
| IMPAIRMENTS OBSERVED DURING TREATMENT | SUGGESTED STRATEGIES/INSTRUCTIONS |
|---|---|
| Reduced visual field | Teach compensation by reinforcing head-turning during functional mobility tasks. See Chapter 16. |
| Reduced perceptual processing | Anticipate that patients may misperceive distance between themselves and supporting surfaces. Help the patient to reappraise distances prior to moving. See Chapter 16. |
| Reduced arousal | Arousal can vary over the course of the day. Monitor for optimal state of arousal to determine when treatment should be carried out. Observe for signs of diminishing arousal during therapy. See Chapter 19. |
| Reduced attention | Work in distraction-free environments. Use patient’s room prior to using the therapy rooms. Gradually introduce stimuli into treatment as the patient tolerates. See Chapter 19. |
| Reduced awareness of impairments | Heighten awareness of impairments. Engage patients before they attempt the activity as to how they feel they can execute the activity; posttask ask the patients for feedback on performance; consider use of videotaped feedback. See Chapter 19. |
| Unilateral inattention | Increase attention to the affected side and engage extremities wherever possible. See Chapter 19. |
| Reduced learning | Use “Show” versus “Tell” when teaching functional mobility tasks. |
| Reduced problem-solving | May manifest in novel situations; offer varying practice conditions (i.e., rolling on a mat or in a bed with sheets and a blanket) to provide opportunities to develop strategies for solving movement challenges. |
| Reduced language/communication | Avoid speaking in a loud voice. Give the patient ample time to respond. Observe the patient for signs of fatigue or anxiety. Encourage self-expression through gestures, if necessary. If the patient has comprehension problems, ask simple, short questions and augment verbal with pantomime and gestures. Use tactile cueing. See Chapter 20. |
| Reduced pragmatics | Minimize distractions. Use demonstration and do not rely on self-report. Provide feedback on statements irrelevant to the situation. |
| Reduced motor planning | Use tactile-kinesthetic cues. Keep environment and context appropriate to task. See Chapter 19. |
Functional mobility tasks
Functional mobility tasks occur throughout the daily routine under varying circumstances within changeable environments. Each task requires the individual to stabilize the body in space or exhibit dynamic postural control. Das and McCollum27 identified three major requirements for locomotion that can be applied to all functional mobility tasks:
1. Progression or movement in a desired direction
2. The ability to stabilize the body against the forces of gravity
3. The ability to make changes in movement in relation to specific tasks within different environments
This view of functional mobility is congruent to a systems approach for analyzing and explaining normal movement, which emphasizes the interaction of the individual, task, and environment.84
Activities in the supine position
The performance of supine activities is often associated with the acute stages of the rehabilitation process. Bridging, rolling, and movement from side lying-to-sit are basic functional mobility tasks that are necessary to the provision of nursing care and movement of the client from a bed to a wheelchair. However, these mobility sequences are also important in enabling the client to participate in a wide range of life areas. For example, consider the individual who chooses to lie on a beach to enjoy the sun and surf. The soft surface of the sand may require the individual to assume a bridge position to shift his or her position if rolling is inadequate. Supine activities require the individual to gain control of flexor and extensor patterns of the trunk, which can be viewed as a prerequisite for more advanced trunk positions.
Bridging
Analysis of movement.
In the functional mobility task of bridging, the back and hip extensors support the body against the forces of gravity. The arch formed when the upper back and feet are in contact with the supporting surface is maintained by the activation of muscles located on the underside of the arch. Use of the arms or legs increases the demands placed on the trunk musculature. When an arm or leg is raised (as in attempts to dress), the muscles located above the arch (the oblique abdominal muscles) must become active to support the limb.28
Selected problems.
The mobility task of bridging is a challenge for patients with hemiplegia because of loss of activity in the extensors and the abdominal muscles. This problem, when combined with early return of extensor activity, results in ineffective and inefficient movement patterns.
Observations in supine indicating decreased abdominal activity include the following:
 Outward flaring of the ribcage (that is, the affected side rides higher in the cavity because the abdominal muscles do not tether the ribcage downward)
Outward flaring of the ribcage (that is, the affected side rides higher in the cavity because the abdominal muscles do not tether the ribcage downward)
 Shortening of the neck resulting from unopposed elevation of the shoulder girdle
Shortening of the neck resulting from unopposed elevation of the shoulder girdle
 Hypotonic appearance of the abdomen
Hypotonic appearance of the abdomen
 Shift of the umbilicus to the nonaffected side
Shift of the umbilicus to the nonaffected side
 Reduced proximal stability effecting the lower extremities
Reduced proximal stability effecting the lower extremities
 Difficulty moving or maintaining the position of the lower extremity due to reduced proximal stability
Difficulty moving or maintaining the position of the lower extremity due to reduced proximal stability
Treatment strategies.
Bridging is an important position that the patient should be instructed to assume early in the intervention process. Bridging is a mobility function necessary for the use of a bedpan, reduction of pressure on the buttocks, and movement within the bed (bed scooting).53
The patient with hemiplegia may have trouble in assuming the crook-lying position and forming a bridge because of a variety of underlying causes. The lack of selective muscle activity on the affected side, caused by the use of mass patterns, prevents the patient from combining the necessary hip components of flexion and adduction.13 Patient attempts to place the affected leg usually result in a mass pattern of movement characterized by hip flexion and external rotation and supination of the foot. The patient’s inability to stabilize the pelvis while attempting this movement results in increased extension of the lumbar spine combined with forced extension of the nonaffected side into the supporting surface. Another possible reason for the increase in the extension of the lumbar spine is tightness of the hip flexors,86 although this is unlikely in the early stages after stroke unless the patient exhibited tightness before sustaining the stroke.
The therapist can assist the patient to assume the crook-lying position. The therapist encourages the patient to assist with active flexion of the unaffected leg and may be required to assist and hold the required crook-lying position. Active flexion on the affected leg helps position the pelvis forward and may promote active holding of the affected leg in a flexed position.53 The therapist may provide downward pressure on the flexed knee of the affected side to ensure appropriate foot placement.13
Active bridging can be used to improve selective extension of the hip and abdominal muscle activity. As the patient lifts the buttocks from the supporting surface, the therapist should make sure the patient does not use excessive extensor activity, which is characterized by extension of the hips, overarching of the back, and pushing of the head into the supporting surface. To improve selective movement, the therapist encourages the patient to initiate the movement by actively tilting the pelvis upward. The therapist may need to prepare the patient for this movement (Fig. 14-1). After tilting the pelvis forward, the patient lifts the buttocks off the surface while holding the pelvis level. The therapist may assist this movement by placing one hand under the hemiplegic hip and one hand on the abdominals. If the feet are positioned close to the body, the therapist also may guide the femoral condyles forward toward the feet while applying downward pressure (Fig. 14-2).

Figure 14-1 In bridging, one should avoid increased extensor activity that results in arching of the back. To assist with selective movement of the pelvis, the therapist cues the gluteal region and the lower abdominals. This sequence may be applied first to the unaffected side and then to the hemiplegic side.

Figure 14-2 A, As the patient gains selective control over the pelvis, the therapist can provide downward pressure through the knees and guide the femoral condyles forward toward the feet. B, The therapist asks the patient to lift the buttocks off the bed. Physical assistance can be diminished as the patient gains control.
After the patient can maintain this position, the next step is to lift the unaffected foot off the surface while maintaining the pelvis level. The therapist should observe any asymmetries or rotation of the pelvis. The therapist must not permit the patient to drop the unaffected side to gain more stability. This task is difficult for the patient with hemiplegia because it places demands on the oblique abdominal muscles22,29,86 and the other weakened core trunk muscles. Bridging can be graded according to the patient’s ability to control movements selectively. Placement of the feet further away from the buttocks requires a greater degree of selective activity to maintain knee flexion with hip extension.29 Alternate lifting of the feet off the supporting surface while maintaining the level of the pelvis requires increased muscular activity and greater coordination (Figs. 14-3 and 14-4).86

Figure 14-3 Lifting a leg off the supporting surface places increased demands on the abdominal muscles because the pelvis must be held up. The therapist asks the patient to lift the unaffected foot off the bed so that all the patient’s weight is placed on the affected side. The patient must maintain the pelvis in a level position. This patient is experiencing difficulty maintaining the optimal pelvic position (left hemiplegia).
Bridging can be used to move up in bed and don pants while in a supine position. Therapists should instruct caregivers in the appropriate techniques to ensure that these movements are transferred into the patient’s daily life routine. The occupational therapist can incorporate these movement strategies while training the patient in self-care activities.
Rolling
Analysis of movement.
Rolling is an important part of bed mobility and an essential part of many other tasks. Research has demonstrated that normal adults use a variety of movement strategies to roll from supine to prone.72
One of the most common movement strategies used by young adults in rolling from supine to prone includes a lift-and-reach arm pattern. Movement of the head and trunk is initiated by the shoulder girdle; a unilateral lift of the leg also occurs. Rotation of the spine, which results in dissociation of the shoulder and pelvic girdles, is not observed (Fig. 14-5).72 This rotation was once assumed a prerequisite to attaining the ability to roll in a normal pattern of movement.13

Figure 14-5 Research has determined that a common form of rolling observed in adults is initiated by a lift-and-reach above shoulder level; the shoulder girdle leads the movement, and a unilateral lift of the lower extremity follows. Many subjects also use a unilateral push of the lower extremity. A great variety of patterns is observed because of individual differences in build and strength and in the support surface.
The most important finding of this study72 is that normal adults have a repertoire of movements available to them, unlike patients after stroke, who are limited to stereotypical patterns of movement.26 The environmental conditions of this study were limited to rolling on an exercise mat, and the subjects were asked to roll “as fast as you can.” Thus, the variety of patterns observed may relate to the temporal demands and implied goal of the task. The strategies used to roll for speed may differ significantly from the strategies used to target a particular object in the environment. Therapists who work with patients with hemiplegia must consider the rolling surface (environment), the goal of changing the position of the body while supine, and future mobility goals such as attaining supine-to-sit. Thus, therapists must determine movement sequences most suitable for ensuring safety and achieving the goal of the movement. Rotation of the spine during rolling is just one strategy that may be useful in providing a greater variety of movement possibilities for the patient with hemiplegia.22,28,29
Rolling to the hemiplegic side: selected problems and treatment strategies.
The patient with hemiplegia frequently rolls over using an extensor pattern to initiate the movement sequence because of lack of flexor control of the trunk and the early return of extensor activity. The patient relies on the unaffected side to push against the supporting surface, resulting in an arching of the axial spine as the body is thrust forward in the direction of the roll.
Davies28 suggested that rolling activities can be used to promote active flexion of the trunk and achieve subsequent improvement in active control of the trunk musculature. The need exists balance the concentric and eccentric contractions of the trunk muscles in proportion to the change in force exerted by gravity as the patient changes position.
The hemiplegic arm requires protection before rolling to the affected side is practiced. The therapist can provide this protection by prepositioning the arm, assisting the patient in bringing the shoulder and arm forward, and giving physical support to the hemiplegic arm while standing on the affected side.
The patient is encouraged to lift the unaffected arm and leg up and forward across the body; this movement is consistent with the pattern identified by Richter, Van Sant, and Newton.72 This movement should occur without the patient pushing against the supporting surface with the unaffected foot (Fig. 14-6). The patient may repeat this movement by returning to the supine position. A part of or the whole leg should be held in abduction and slowly lowered to the surface as the patient returns to the supine position.

Figure 14-6 Rolling toward the hemiplegic side (left hemiplegia) is accomplished by lifting the unaffected leg over the hemiplegic side without pushing off the bed surface. The therapist assists with movement of the shoulder and pelvic girdles.
As the patient gains control of this movement sequence, the next step is to lift the head from the surface to assist with initiation of movement. As the patient turns, the head is rotated toward the direction of the movement. Throughout the sequence, physical assistance should decrease as changes in the patient’s ability to control movement occur.
Rolling to the unaffected side: selected problems and treatment strategies.
Rolling to the unaffected side may be more difficult for the patient with hemiplegia. The movement is frequently initiated by an extensor pattern that includes extension of the head, neck, and back. The patient relies on extension of the back to bring the hemiplegic leg over the trunk in a pattern of extension that may be viewed as an inefficient compensatory strategy. The affected arm may be left behind as the patient rolls (Fig. 14-7).29

Figure 14-7 Rolling toward the unaffected side. The patient should avoid using the back extensors to bring the lower extremity forward while neglecting the hemiplegic arm (left hemiplegia).
When teaching patients to roll to the unaffected side, the therapist’s goals are to decrease maladaptive compensatory strategies contributing to inefficient movement and to enhance more effective and efficient patterns of movement. The patient may be instructed to use the stronger arm (Fig. 14-8) to bring the hemiplegic arm up and forward while the therapist attempts verbally or physically to cue the movement of the pelvis and lower extremity. The therapist supports the affected leg while assisting with anterior movement of the pelvis (Fig. 14-9).

Figure 14-8 Early in the rehabilitation process, the therapists instructs the patient with left hemiplegia to use the stronger hand to assist in bringing the shoulder forward; the therapist positions the hemiplegic leg in hip and knee flexion to avoid an extensor pattern.
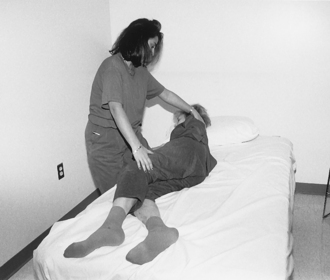
Figure 14-9 Assistance can be decreased as the patient gains control of the movement. The therapist assists with knee flexion and protraction of the shoulder (left hemiplegia).
Repetition of this sequence may assist with learning. The therapist encourages the patient to lift the affected leg off the supporting surface and lower it slowly after returning to the supine position. This strategy is used to assist the patient in maintaining a slight degree of hip and knee flexion, which decreases reliance on the extensor compensatory pattern. An alternative method is to flex both legs to roll.13,29
Supine-to-sit
Analysis of movement.
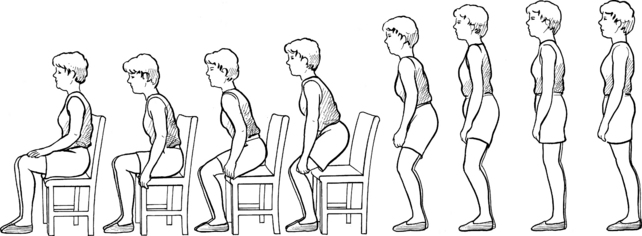
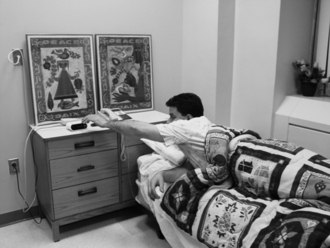
The transitional movement from supine-to-sit may be achieved through a variety of movement strategies. Adults have a tendency to use a momentum strategy to achieve the goal (Fig. 14-10). Their movements are smooth and efficient as they “bound” out of bed, off the couch, or out of a chair. A momentum strategy requires forces within the trunk to be generated and transferred to the lower extremities to initiate the rolling sequence. Trunk muscles must contract concentrically to initiate and propel the movement; eccentric muscle contractions provide control. The reciprocal shortening and lengthening of muscle contractions provide maintained stability.

Figure 14-10 The most common movement strategy used by adults to get out of bed relies on momentum. Strategies vary greatly.
Many older adults demonstrate a tendency to use a force control strategy (Fig. 14-11). The individual transfers forces from one body part to another as graduated changes in position occur. Rolling to side lying, then pushing up with the upper extremities, and swinging the lower extremities over the side of the bed is an example of this strategy. This method provides increased stability because concentric and eccentric forces are required in increments. Increased effort (force) must be used if momentum is lacking.20,22,29,72,81
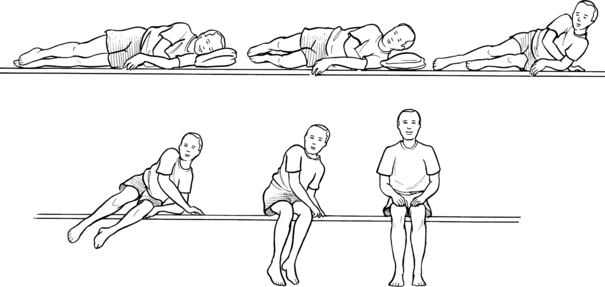
Figure 14-11 A force control strategy for getting out of bed has the individual performing the task in two parts: the patient moves from supine to side lying and then pushes to a seated position. This strategy is useful for patients who exhibit reduced stability functions.
Evidence exists to support that older adults use their upper limbs to assist the trunk musculature when moving from supine-to-sit.3 Thus, therapists need to consider the movement strategies and positioning of the arms when retraining the supine-to-sit sequence. A great variety of movement possibilities to achieve a supine-to-sit sequence remains. The described sequence often is used spontaneously by patients after stroke and by the therapists as a method of instruction.22 This sequence is referred to as side lying-to-sit for the remainder of this chapter.
Selected problems.
Movement from the side lying to seated position becomes a challenge for the patient after stroke because of the combined effects of limited muscular activity and maladaptive compensatory strategies. Patients lack appropriate postural alignment and stability.22,28 The lack of flexor control of the trunk and early return of extensor activity interfere with the patient’s ability to grade concentric and eccentric muscle activity effectively relative to the changing forces of gravity.28 If inadequate control of the trunk musculature is evident, the patient must rely on compensatory strategies that may include overuse of the unaffected arm or leg or exaggerated use of head movements. The patient applies these compensatory strategies instead of effective lateral movements of the neck and trunk. When side lying, the patient flexes the head forward instead of laterally and uses the unaffected arm to move the body away from the supporting surface. The forward movement of the head may be a compensatory strategy to shift the center of gravity forward. The patient may be unable to combine lateral flexion and extension of the trunk because of lack of selective muscle activity. Hooking of the unaffected leg under the affected leg to lift and lower the leg over the side of the bed is yet another compensatory strategy many patients are instructed to perform. This strategy prevents selective movement of the pelvis in an anterior and lateral direction.22,28 The patient with hemiplegia experiences difficulty whether rising from the hemiplegic or the unaffected side because of the problems presented.
Additionally, while changing positions, the patient may not exhibit appropriate head-righting responses; this deficit requires the patient to flex the neck laterally while controlling eccentric muscle activity on the opposite side. Furthermore, the patient also may be unable to move or place the affected limbs appropriately in preparation for transitional movement or may neglect the affected limbs entirely.
Treatment strategies.
Many methods are suggested to retrain the patient in the supine-to-sit movement sequence. One method suggests that patients with hemiplegia be taught initially to roll toward the affected side to decrease the amount of effort required and to reduce maladaptive strategies such as pulling and pushing to achieve the seated position.22 Others suggest that the patient with hemiplegia be instructed to rise from both sides early in treatment to prevent associated reactions.12,28,29 Another option is for the patient to start the movement sitting upright and learn to lie down first. This method may decrease the force gravity exerts on the trunk musculature as the patient first learns to control movement into gravity using eccentric muscle activity.28 The physical environment and the patient’s premorbid preferences for movement sequences also may influence the methods selected. Patients may benefit from learning more than one method to move more effectively in different environments.
Side lying-to-sit toward the affected side.
The therapist assists the patient in lifting the hemiplegic leg over the side of the bed; the head, neck, and upper thorax are brought forward, requiring the neck to flex laterally. Concurrently the nonaffected arm must be brought across the body and placed on the bed. The unaffected leg also must be lifted over the side of the bed as the patient pushes down with the hand. The movement of the unaffected leg as the patient simultaneously pushes with the hand adds a momentum strategy to this movement sequence; the weight of the leg assists the patient in attaining a seated posture. The therapist may need to assist with bringing the unaffected shoulder forward over the base of support of the body. The therapist may place hands on the shoulder and pelvic girdle to give support and to assist with movement of the unaffected leg (Fig. 14-12). As the patient gains some control over this movement, the therapist may provide support to just the unaffected shoulder and pelvis (Fig. 14-13). The therapist can use verbal cues or downward pressure on the shoulder physically to cue lateral flexion of the trunk and appropriate head righting. To reverse this sequence, the patient may require assistance with lifting the hemiplegic leg onto the bed. Care should be directed toward maintaining the hemiplegic shoulder in a forward position as the patient turns and lowers the body to the bed surface.28

Figure 14-12 The therapist uses one arm around the patient’s shoulders while the other hand provides downward pressure to the pelvis to assist with weight transfer in movement to a seated position (left hemiplegia).

Figure 14-13 When the patient is able to control the trunk muscles actively, the therapist can decrease assistance. The therapist may cue lateral flexion of the head and trunk by providing downward pressure to the shoulder and pelvic girdles of the unaffected side.
When assuming a sitting position from the affected side, the patient is active in the trunk, particularly while bearing weight on the affected upper extremity; therapists should be mindful of this. Furthermore, the therapist may have to cue movement of the trunk on both sides to promote the correct sequence of lateral flexion and extension responses (Fig. 14-14).
Side lying-to-sit toward the unaffected side.
The sequence of movement in side lying-to-sit toward the unaffected side remains the same as that in the previous example; however, the placement of the therapist’s hands to assist movement changes. The therapist should instruct the patient to lift the affected arm while lifting the unaffected leg over the side of the bed. The therapist assists with movement of the affected leg forward and over the edge of the bed as the patient lifts the head, neck, and upper thorax over the sound arm (Fig. 14-15). The therapist needs to ensure that the hemiplegic shoulder remains in a forward position as the patient begins to push down with the unaffected side. A movement sequence that begins as a force control strategy can with increased motor control of the head, neck, and trunk become a momentum strategy.

Figure 14-15 Rising from the unaffected side. For patients who require significant support, the therapist places one hand on the scapula while assisting with movement of the legs.
Patients demonstrating a lack of lateral flexion of the neck require preparatory interventions. The patient should be positioned side lying on the unaffected side with the head on the bed (Fig. 14-16, A). The patient lifts the head with the therapist’s assistance as needed (Fig. 14-16, B). The therapist then asks the patient to lower the head to the bed; this movement requires eccentric contraction of the lateral flexors. This maneuver is followed by active lifting of the head, which requires concentric muscle contractions. The therapist should not permit the patient to rotate or flex forward while performing this task. A visual target such as an alarm clock, television, or family picture may assist in establishing this task-related goal.22
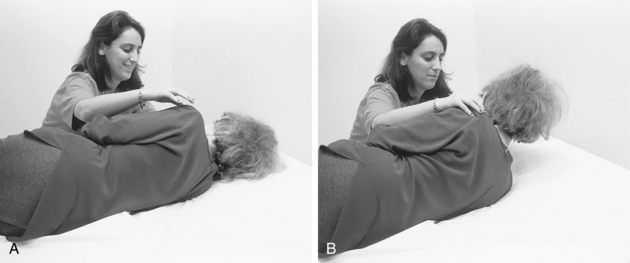
Figure 14-16 A, To encourage active control of the lateral neck muscles, the patient first learns to control eccentric contraction while lowering the head to the bed. B, This is followed by active lateral neck flexion while raising the head.
Additional interventions to promote lateral flexion and extension of the trunk, which are necessary to perform side lying-to-sit, are described in the section on sitting.
Activities in sitting
The ability to maintain a seated position and perform ADL safely and efficiently is a goal many occupational therapists seek with their patients (see Chapter 7). In the acute stages after stroke, the therapist should begin to work on control of sitting and standing with the patient as soon as possible to promote the ability to manage the upright position and increase overall visual input in functional positions.22
Analysis of movement
For controlled movement in sitting the ability to bear and shift weight anteriorly, posteriorly, laterally, and in a rotary pattern must be present. This suggests that the concentric and eccentric abilities of the trunk flexors and extensors and the ability to activate these muscle groups selectively relative to the task demand must be present. For example, for controlled anterior weight shift through the pelvis, the need for concentric contraction of the low back extensors and an associated eccentric contraction of the trunk flexors (abdominals) is evident. In a posterior weight shift through the pelvis, the need for concentric contraction of the trunk flexors and an associated eccentric contraction of the trunk extensors is evident. With lateral weight shift through the pelvis the trunk extensors and flexors work together concentrically (shortening) on the nonweight-bearing side and eccentrically (lengthening) on the weight-bearing side.13 During trunk rotation, the primary muscles involved are the oblique muscles.
Selected problems
The trunk is crucial in postural control. Many patients display difficulty with voluntary trunk control in sitting following the stroke. Messier and colleagues63 looked at trunk flexion in sitting poststroke and noted decreased displacement of the center of pressure and lower extremity weight-bearing through the feet. They felt that this was probably indicative of minimal anterior tilt of the pelvis, and most of the trunk motion initiating from the upper trunk.63
There is electromyography (EMG) evidence to support alterations in trunk muscle activity following stroke. Trunk velocity during flexion and extension is lower following stroke compared to normal subjects.33 With the addition of voluntary arm and leg movements, there is delayed onset of contraction and reduced activation of paretic trunk muscles.33 In contrast to Dickstein and associates’ findings, Winzeler-Mercay and Mudie96 found that muscle activity in the paretic rectus abdominis and erector spinae following stroke were the same as normal subjects during forward and backward voluntary sway and reaching, but for the task of donning the shoes, the rectus abdominus showed reduced activity. The erector spinae activation was much higher in the stroke group during all postural activities.96
The therapist must begin an assessment on functional capabilities in this area by close examination of the patient’s ability to control movements in sitting (see Chapter 7). A full appreciation of the normal ranges of motion (ROMs) within the spine is useful when comparing patients with hemiplegia and the patterns they use with the normal population. The therapist must be cognizant that these ranges decrease with age; ascertaining the baseline from which these patients were operating before the onset of hemiparesis is important. Mohr64 emphasized the importance of establishing a patient’s ROM in spinal extension and flexion, lateral flexion, and rotation before treatment is implemented. This provides the therapist with information needed to decide whether interventions should include increasing ranges in these areas with the goal of promoting activation by the patient in these patterns for function. Davies28 also recommended this approach. For example, passive mobilization of the lumbar spine for lateral flexion may be an important preparatory treatment to working on increased trunk control in activities requiring a lateral weight shift such as side lying-to-sit. The therapist, having encouraged increased mobility in this plane, can progress to facilitation of the appropriate muscle contractions needed to hold and move into this position by placing the hand in the patient’s axilla and assisting the side to lengthen while placing the other hand on the patient’s opposite trunk to guide shortening on that side. Conversely, many clinicians with a motor learning perspective suggest that the therapist set up the environment to create a natural situation that places increased demand on trunk muscles for function.
A deeper look at the location of movement and the way it is initiated is necessary before proceeding in evaluation. Mohr64 provided guidance by categorizing trunk movements in sitting by dividing them into movements initiated from the upper trunk versus the lower trunk. Mohr further analyzed anterior, lateral, and posterior weight shifts in each of these categories and then provided functional examples for each movement pattern.
Functional activities in sitting
Task-oriented functional practice must follow all “preparatory” trunk activity such as mobilization. Following hands-on treatment, one hopefully will see gains in passive mobility or the patient’s ability to “find” the muscle and activate it. However, the patients themselves must use these gains immediately particularly in the context of a functional activity; otherwise, carryover is doubtful (Figs. 14-17 and 14-18).
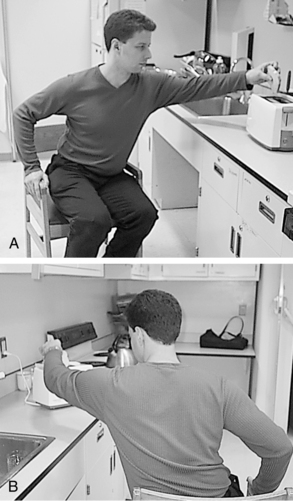
Figure 14-17 A, Reaching for toast combines patterns of trunk lateral flexion and extension. B, Using the right affected arm to bear weight on the armrest results in scapula depression, which contributes to the shortening of the trunk muscles on the right side.

Figure 14-18 A pet therapy dog is used to encourage trunk flexion and weight-bearing on the affected left arm and leg.
Gentile37 proposed two distinct processes that mediate skill learning: an explicit process and an implicit process. In the explicit process, patients consciously involve themselves with shaping the movements to achieve a specific goal. In the implicit process, the main concern is the dynamic of force generation, which is not under the conscious control of the patient. Implicit processes rely on the interplay of muscle contractions against the passive components affected by gravity and joint torques. Gentile suggested that for the explicit process to occur, therapists can use information consciously available to the patient and provide coaching such as around how a movement is organized and features in the environment. For implicit learning to occur, therapists must challenge themselves creatively to set up the environment to elicit a response from the patient that produces force generation as a byproduct of the functional activity in which they are engaged. Clearly, the therapist must set up opportunities for practice for the greatest benefit to occur to the learner.
Dean and Shepherd30 designed a study specifically to look at the efficacy of task-related training, which proves to be an excellent example of using explicit and implicit learning processes in treatment. Their intent was to increase the distance stroke patients could perform forward reach in sitting and to note the contribution of the affected lower limb to support and balance in this activity. Twenty subjects were used in this study, and they had to be a minimum of one year poststroke. They were randomized into two groups—an experimental group that received treatment involving reaching forward for natural objects beyond arm’s length (in a gradual progression) and a control group that received sham training with cognitive tasks within arm’s length. EMG, videotaping, and two force plates (to evaluate the amount of lower extremity force generated during the activity and sit-to-stand) were used before and after training to gain objective measures. After training, subjects were capable of reaching farther and faster, suggesting that the affected lower limb was assisting more in support. Furthermore, the researchers noted that subjects demonstrated improved force generation of the affected lower limb in sit-to-stand. The explicit learning process subjects were engaged in was demonstrated by the problem-solving and practicing of forward reaching farther and farther. The implicit learning process was activating the lower extremity in the process.30,37
Scooting
Analysis of movement.
Scooting, or “butt walking,” involves the transfer of weight over first one buttock and then the other, creating overall movement of the body anteriorly in a seated position.12 Appropriate elongation of the trunk on the weight-bearing side and shortening on the nonweight-bearing side is required. This movement pattern is useful for a number of functional activities such as donning and doffing pants in a seated position. From a mobility perspective, it allows the individual to approach the edge of a supporting surface to transfer.
Selected problems.
As indicated previously, problems with passive restriction in the trunk and the inability to activate trunk muscles selectively are of primary concern with this activity and may preclude the appropriate balance reactions needed for success and safety. The patient must have intact skin on the buttocks to practice scooting.
Treatment strategies.
Verbal or physical cueing to assist patients with scooting can be accomplished in a variety of ways, depending on the level of involvement of the individual. The therapist may elicit the desired movement pattern through a series of contacts in which the therapist first cues a lateral weight shift and then places the hand on the patient’s pelvis to cue forward advancing of the hip on the nonweight-bearing side.12 The therapist then changes hands to cue forward movement of the opposite buttock (Fig. 14-19). Patients with more profound physical involvement may require added assistance by the therapist, particularly in advancing the buttock (Fig. 14-20).

Figure 14-19 Scooting is an important skill for moving to the edge of a bed or seat and can be a useful movement pattern in activity of daily living tasks such as donning pants in a seated position. A, The patient begins in symmetrical sitting. B, The therapist can encourage scooting by first cueing a lateral weight shift and then advancing the nonweight-bearing buttock to move anteriorly (C).
Transfers
Analysis of movement.
The ability to move from a given surface to an adjacent surface safely and efficiently is a primary goal in treatment for many of the patients with whom occupational therapists work. This maneuver requires enough forward flexion of the trunk over the feet to allow the individual to pivot about the feet and sit on the nearby surface.
Selected problems.
Patients with neglect who attempt to transfer often succeed in transporting only half the body onto the supporting surface. Additionally, the left foot may be neglected, and the patient may be oblivious to proper left foot placement before transferring.
Many patients require considerable help to maintain a flat foot on the floor. This may be because of unilateral inattention, poor sensation on the affected side, shortened trunk muscles resulting in asymmetrical sitting, and shortening of the calf muscles on the affected side.
Treatment strategies.
Bobath12 and Davies29 described the anterior weight shift that can be facilitated through contact on the patient’s pelvis or scapulae. Carr and Shepherd22 recognized the same forward weight shift and encouraged patients to move the shoulders forward during active participation in transfers (Fig. 14-21). All four therapists described ways the therapist may use manual contact to the knee to draw the knee forward and encourage weight-bearing on the hemiplegic side.

Figure 14-21 To teach a patient to perform a squat-pivot transfer, the therapist should encourage the appropriate amount of anterior weight shift by instructing the patient to move the shoulders forward.
Patients have varying degrees of motor control for this activity. The therapist needs to create an environment in which the patient has enough guarding by the therapist to make training safe and enough “room” to try to make the transfer with as little assistance as possible. This is not always easy to do, and some patients inevitably require much assistance to transfer. However, the more the patient can be encouraged to do, the more the patient learns during the session. Consistent grading of the level of assistance a patient requires (i.e., minimal, moderate, or maximal) is important in measuring progress and communicating to other staff members the amount of help required by the patient to carry out the task.
In the initial stages of transfer training, a patient may require maximal assistance, and the therapist may need to clasp both hands around the pelvis to pivot the patient from one surface to another. As the patient gains greater strength and control over balance, the therapist may reduce this level of assistance to a lighter hold around the pelvis and then the scapula.
Patients tend to be taught stand-pivot or modified stand-pivot (sit-pivot) transfers. Many therapists train stand-pivot transfers for the presumed benefits they afford in getting the patient into an upright position and putting full weight on the involved lower extremity. However, these transfers do not resemble the maneuvers performed by normal subjects in moving from one surface to the other (i.e., coming to a full stand or turning and sitting down on an adjacent surface). As Shumway-Cook and Woollacott84 pointed out, stand-pivot transfers may be more difficult because they do not allow the patient to use a momentum strategy; the need to come to a stand instead of pivoting blocks the benefits the momentum strategy provides. When training pivot transfers, foot placement is important. One foot is slightly in front of the other at the outset and is adjacent to the surface to which the patient is moving (Fig. 14-22). With environmental constraints or more advanced patients, a stand-and-step transfer may be used.
Promoting weight shift onto the affected lower extremity is important during transfers and sit-to-stand activities. The therapist may position both knees around the patient’s affected knee physically to assist a forward weight shift onto the lower extremity and to guard against buckling at the patient’s knee. For patients requiring less cueing and guarding, the therapist may assist the knee by placing a hand on the patient’s distal femur and gently pulling anteriorly and then down toward the floor as the patient takes weight on the leg.
The role of the arms in this training process has become controversial. Bobath12 and Davies29 supported using clasped hands in front of the body to facilitate a forward weight shift, placing the arms on a stool, chair, or other supporting surface. However, a study by Carr and Gentile19 examined the role of the upper extremities in sit-to-stand and determined that “fixing” the arms (by holding a rod as subjects in the study did) had a tendency to cause an increase in what was described as extension force (the force needed by the lower extremities to extend the body into an upright position) and a decrease in momentum of the body during sit-to-stand; this determination may have implications for transfers. The authors advocated that patients work on increasing strength in the lower extremities (particularly in extension) to enhance functioning in sit-to-stand. They contended that although patients tend to use the hands to push down on the armrests of a chair to stand or alternatively swing the arms forward to assist horizontal and vertical propulsion of the body mass, these strategies cannot be used in varying environmental conditions19 (Figs. 14-23 to 14-27).

Figure 14-23 A, Use of a grab bar can encourage a forward weight shift in a transfer requiring greater physical assistance. B, Positioning and proper handling can be difficult with space constraints. This requires problem-solving for the therapist, patient, and caregiver. C, While this patient may require moderate physical assistance to perform the transfer, he is actively encouraged to use the movements he is capable of in the transfer, in this case, thoracic extension.

Figure 14-24 A typical short sliding board and a Beasy board. These devices can be used to assist patients who have greater physical needs.

Figure 14-25 A, Early practice with car transfers may take place using a simulated car in the clinic and where possible should progress to an actual vehicle. B, Controlled descent into gravity requires coactivation of the abdominal muscles (flexors) and back extensors to avoid injury in a constrained space. C, The patient is shown how to manage the affected leg during the transfer.
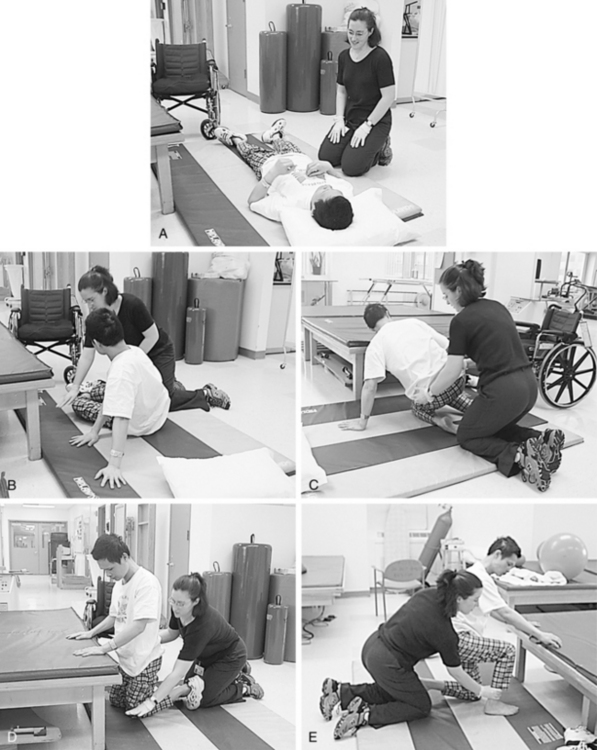
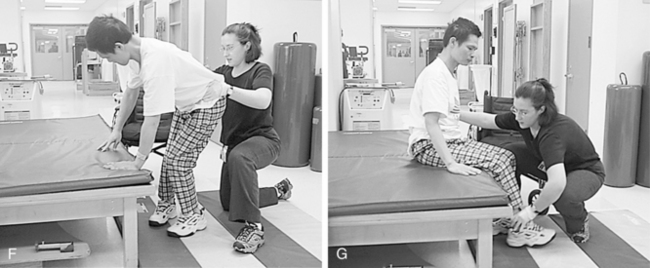
Figure 14-27 A, Teaching the patient and caregiver how to get up safely from the floor is important before discharge to the community. B, The therapist instructs this patient with right-sided weakness to assume a side-sitting position on the left arm and hip. C, The therapist or caregiver assists the patient at the pelvis to assume weight on his knees. She uses a surface immediately in front of the patient to allow for arm support. D, The patient now is supported fully on his hands and knees. She prepares him for the next stage by asking him to shift his weight to his left. E, When the patient shifts weight over to the left knee, he is able to move his weaker right leg into a half-kneeling position. F, From the half-kneeling position the patient assumes a standing position and begins to shift his weight to sit on the adjacent surface. G, The patient is seated safely.
A study by Gillen and Wasserman40 analyzed how altering the environmental context of a transfer activity affected mobility performance in patients receiving inpatient rehabilitation. They compared performance in transfers carried out in a traditional clinic setting and in a more naturalistic apartment-like setting. Twenty-five participants carried out four transfer tasks in each environment: two bedside commode transfers and two bed-to-chair transfers. The Functional Independence Measure (FIM) was used to provide the level of assistance required in transfers.
Their findings revealed that environment plays a role in mobility performance. Forty-four percent of the patients performed better in the traditional clinic setting. Twenty percent performed better in the simulated apartment. Sixty-four percent of patients were inconsistent with the same transfer task between the two environments, while 36% of the patients transferred consistently in the two environments, as per the FIM data. Therapists asked to provide FIM data early in the inpatient rehabilitation stay must never assume that performance in the clinic equals performance in other environments.
Sit-to-stand
Analysis of movement.
Sit-to-stand can be divided into different phases, depending on the description of the researcher (Fig. 14-28). Shepherd and Gentile82 described sit-to-stand using the terms preextension phase, a phase characterized by the beginning of the movement to the position in which the thighs are off the surface; and extension phase, the phase from the thighs-off position through the end of movement (full stand). Shenkman and colleagues81 described four phases in sit-to-stand (Fig. 14-29). Phase 1 (Fig. 14-30, A) is referred to as the flexion momentum phase and is used to generate the initial momentum for rising. During this phase, the center of mass is within the base of support, and eccentric contractions of the erector spinae are required to control forward motion of the trunk. Phase 2 (Fig. 14-30, B) begins as the individual leaves the chair seat and ends at maximal ankle dorsiflexion. Forward momentum of the upper body is transferred to forward and upward momentum of the total body. The center of mass now moves from within the base of support of the chair to the feet. By definition, the phase is unstable and requires coactivation of hip and knee extensors. Phase 3 (Fig. 14-30, C) is an extension phase during which the body rises to its full upright position by expansion of the hips and knees. The stability requirements are not as great as in phase 2 because the center of mass is well within the base of support of the feet. Phase 4 (Fig. 14-30, D) is a stabilization phase in which complete extension of the hips and knees occurs. Regardless of the way researchers divide the task, an appreciation of the biomechanics of this movement pattern is crucial in training and in understanding potential problems that occur in hemiplegia.
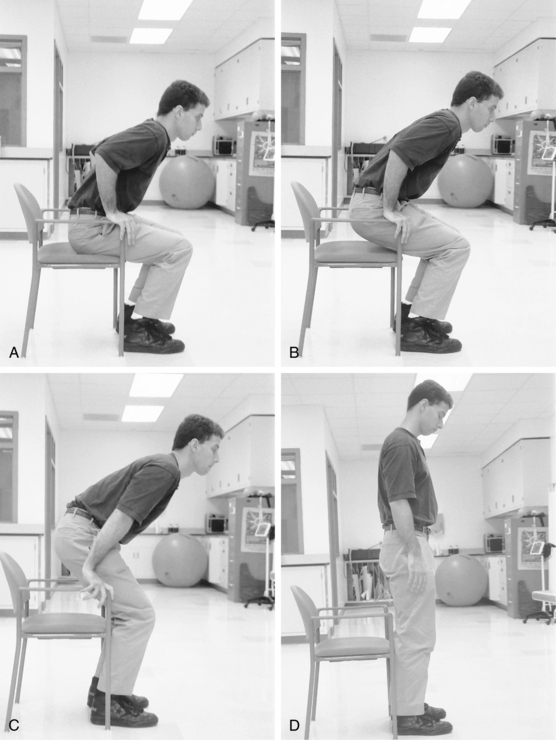
Figure 14-30 A, Phase 1 of sit-to-stand. B, Phase 2 of sit-to-stand. C, Phase 3 of sit-to-stand. D, Phase 4 of sit-to-stand.
Carr and Shepherd20 outlined key factors that influence the way sit-to-stand is executed in normal individuals. The therapist must consider the role of foot position, the starting position of the trunk, the speed of movement, and the role of the upper limbs in balance and propulsion. Carr and Shepherd stated that:
1. Sit-to-stand is accomplished most easily when the initial starting position of the foot is in a posterior position (with the ankle in approximately 75 degrees of dorsiflexion).
2. Initiating active trunk flexion from the erect position and encouraging the individual to swing the trunk forward at a reasonable speed allows for the greatest generation of extension force in the lower limbs to raise the body vertically.
3. Increased velocity of trunk flexion facilitates extensor force in the lower limbs.
4. Constraint of the arms (as in holding the hemiplegic arm forward while attempting sit-to-stand) results in increased time producing sufficient lower limb extensor forces to stand.
Janssen, Bussman, and Stam51 reviewed key factors affecting sit-to-stand by searching the literature for the most frequently mentioned determinants, and they found that chair height, use of armrests, and foot position significantly influence the ability to carry out sit-to-stand. Use of a higher chair resulted in decreased movements needed at the knee and hip, while using armrests reduced the movements needed at the hip. Repositioning the feet from anterior to posterior reduced the maximum mean extension movements at the hip.
Selected problems.
As mentioned in the previous section, patients may have difficulty maintaining their feet flat on the floor because of poor sensation, unilateral inattention, or shortening of the trunk and calf muscles.
Difficulties with spatial relations and praxis have been noted during transfer training, regardless of whether the therapist is training the patient for pivot transfers or sit-to-stand. Certain patients lean backward instead of forward while the therapist is attempting to transfer. These patients’ actions are unpredictable and often run counter to those expected after instruction from the therapist.
As Arnadottir6 noted, transfers also reveal problems with organizing and sequencing and conditions such as ideational apraxia. These problems may become evident when a patient attempting to rise from bed omits the appropriate steps of handling the bedclothes in preparation to transfer (see Chapter 18).
Motor impersistence, a term first introduced by Fisher35 to describe failure to persist at various tasks such as eye closure, breath holding, conjugate gaze, and tongue protrusion may explain some patients’ inabilities to persevere with certain tasks such as transfers, sit-to-stand, and ambulation. These patients tend to collapse midway through the task, sometimes without warning, and reduced muscle strength, per se, does not appear to be the cause. Impersistence, in most studies, has been found to correlate more with right-hemisphere lesions than with left-hemisphere lesions.35,54
The manner in which the sit-to-stand movement pattern is executed may reveal who is at risk for falls. Cheng and colleagues23 found that when comparing stroke survivors who had a history of falls against stroke survivors who had no history of falls, the differences were clear in measurable parameters such as body weight distribution. Stroke patients with a history of falls executed the task of sit-to-stand asymmetrically, taking much more weight on their sound side.23 This suggests that, certainly from the point of view of safety concerns, stroke survivors need as many opportunities as possible to develop better control of their affected lower limbs in sit-to-stand.
Treatment strategies.
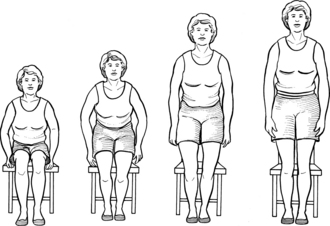
Bobath12 described the need to begin training patients in sit-to-stand from a high seat (Fig. 14-31, A), progressing gradually to lower seats or a plinth (Fig. 14-31, B). Similarly, the environment can be used to change the demands required to transition from sit to stand (Fig. 14-32). Other studies have substantiated her assertion, including the conclusion that high-surface chairs can decrease significantly the joint ROMs needed at the hip and knee and the strength requirements to lift the body.18,85
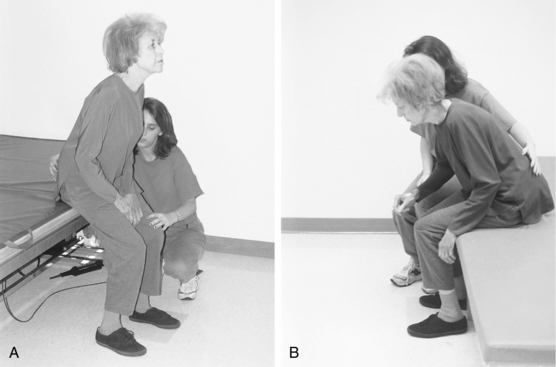
Figure 14-31 A, During the initial stages of learning, patients may find standing from a high surface easier. Among other things this provides the patient with a feeling of success. B, The patient can attempt lower surfaces after becoming more skillful. Varying the surfaces from which patients practice standing is important to promote learning and enables the patient to cope with varying situations that arise in the real world.

Figure 14-32 A-F, Training sit-to-stand and transfers using a variety of functional seating surfaces.
Verbal or physical cues may be required to promote appropriate weight-bearing on the affected lower extremity as recommended for transfer training. In Fig. 14-33, the therapist’s assistance provides much stability for the patient. In Fig. 14-34, the therapist needs only to cue the patient through the distal femur to get the desired response.
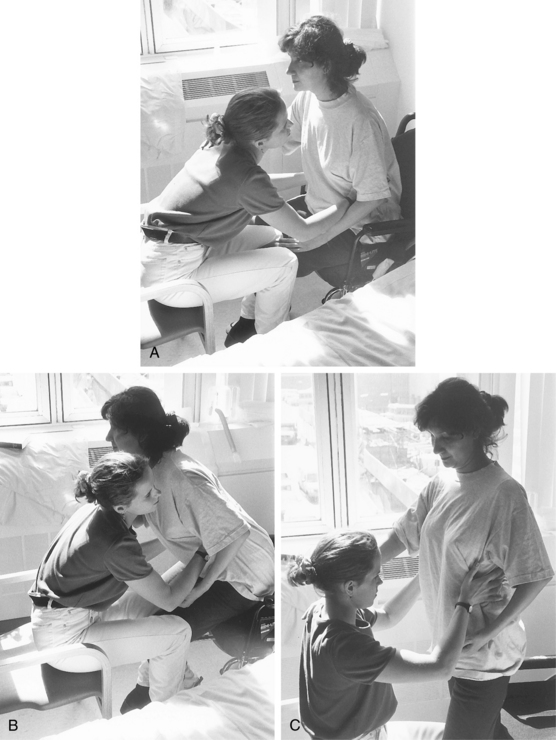
Figure 14-33 A, The therapist promotes weight bearing on the patient’s affected lower extremity in sit-to-stand by placing the knees around the patient’s affected knee, drawing the patient forward (B), and discouraging “buckling” when the patient achieves the standing position (C).
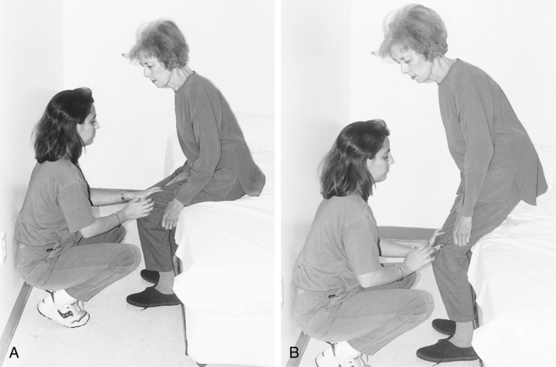
Figure 14-34 Patients with greater motor control still may require some cueing to equalize the weight-bearing between the lower extremities if they have a tendency to stand up using their unaffected side more than the other. A, The therapist places a hand on the distal femur of the affected lower extremity, draws the knee anteriorly, and then applies downward pressure as the patient comes to stand (B).
Because getting the feet back and under in sit-to-stand is so important, training patients to move to the edge of the supporting surface is necessary for optimal foot placement. This enables forward flexion of the trunk and movement of the center of mass over the base of support. A patient who attempts to stand without appropriate foot placement will encounter difficulty (Fig. 14-35).
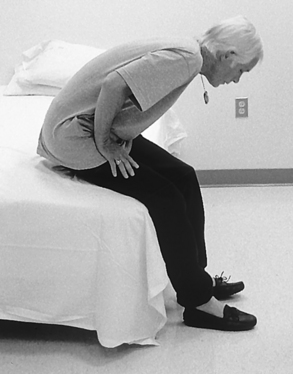
Figure 14-35 Foot placement is important in sit-to-stand. Note how far forward this individual’s feet are as he attempts to stand.
Normal subjects frequently use a momentum strategy in mobility skills as a way to move with less energy requirements and hence with greater efficiency. Momentum strategy is used frequently in rising from bed, and no cessation of movement occurs. The momentum strategy can be used in a modified way with appropriate patients who have sustained a stroke, because it allows them to use the force generated by forward flexion to take them into an upright position. They then need adequate stability when their thighs are off the supporting surface to prevent them from falling forward. Momentum provides the patient with a strategy to move but by definition requires increased control of stability functions. Patients with poor trunk control or significant cognitive impairments are not candidates for using such a strategy. When introducing the momentum strategy in therapy, the therapist must adequately guard the patient to prevent a possible fall.
Practicing forward reach while sitting appears to improve the ability of the affected foot to accept weight and improves weight-bearing in sit-to-stand activities.30 These were Dean and Shepherd’s30 conclusions from their study using individuals who were at least one year poststroke. Dean and colleagues31 have since looked at the effects of sitting training in the acute stages following a stroke. In this study, the researchers provided a two-week sitting training protocol that improved sitting ability as measured by distances reached and quality as measured by reaching performance. They also explored whether the two-week sitting training protocol benefited patients’ ability to stand up and walk, and they further examined if any gains were maintained six months following training. This study was set up as a randomized placebo-controlled clinical trial (CCT) involving six experimental and six control group subjects, all having sustained a stroke in under three months. Participants in the experimental group received the training protocol designed by Dean and Shepherd.30 Participants in the control group completed a sham sitting training protocol involving cognitive manipulative tasks.
Sitting ability, the main outcome measure, was significantly improved as measured by the average maximum reach distance during forward and across reaches, compared with the control group. In addition, the quality of reach improved in the experimental group, as evidenced by use of the standardized “reach to grasp and drink from a glass” task in forward and across directions. The carryover to standing up was evident, but not to walking, and there was some evidence of effectiveness of the interventions six months later.31
The operative word for improving sit-to-stand performance appears to be practice. A randomized controlled study by Britton and colleagues16 looked at the amount of practice that could be carried out by a physical therapy assistant in 30 minutes a day over a two-week period in a stroke rehabilitation unit and its potential effects on sit-to-stand. Eighteen patients all requiring supervision in sit-to-stand were divided evenly into experimental and control groups. The experimental group practiced sit-to-stand and leg strengthening exercises for 30 minutes on weekdays for two weeks (in addition to their rehabilitation program) while the members of the control group received upper extremity therapy.
Results showed that the provision of 30 minutes of practicing sit-to-stand resulted in a mean of 50 stands per day above what was practiced in the routine rehabilitation program. The researchers noted a significant mean difference of 10% body weight taken through the affected foot after one week of the program. In addition, the control group showed reduced weight through the affected leg while the experimental group showed increased weight on the affected leg.16 The findings of this study indicate that rehabilitation practitioners need to provide as many opportunities as possible for practicing newly acquired skills. This will require creative solutions and reassessment of current models of treatment delivery.
Activities in standing
Analysis of movement
The ability to stand is a goal many patients with hemiplegia want to achieve because the drive to be upright is strong. Patients should be provided the opportunity to practice standing and shifting their centers of gravity in all directions and reaching for functional objects in the environment. The trunk responses needed for controlled sitting (i.e., selective lengthening and shortening depending on the requirements of the task) also are needed for controlled standing; however, these trunk responses are carried out over a much narrower base of support.
Selected problems
Standing may prove challenging for patients with severe hemiplegia who have only one side of the body available to use for movement; moving with one half of the body is stressful work. The slow, laborious effort of standing and attempting to move in this position causes an increase in posturing and skeletal muscle activity. Movements often are lacking in spontaneity and must occur at a conscious level for the patient. Postural deviations noted in sitting in these patients become even more exaggerated in standing. For example, the patient who tends to “fix” the upper limb to stay upright while sitting will present with greater fixation of the upper limb when challenged in the standing position.
Studies have shown that the role of the paretic leg typically reflects its contribution in compensatory strategies, rather than in the restoration of support functions and equilibrium reactions.32,73 This speaks to the need to train weight-bearing over the affected leg in reaching and sit-to-stand activities as mentioned previously in this chapter.
Postural control performance in individuals with stroke is affected by attentional tasks.9,73 This implies a high degree of cognitive vigilance on the part of the patient to maintain balance, and whenever there is a demand on cognitive systems, there may be a risk for losing postural control.
Treatment strategies
As stated previously, standing as early as possible if medical clearance is permitted is ideal for patients. Standing helps increase the patient’s level of arousal and can be motivating. Bobath,12 Davies,29 and Carr and Shepherd22 emphasized the need to help the patient stand so that body segments are aligned properly and weight is accepted through the affected lower extremity. For some patients, accomplishing this requires all of their attention and energy. Therefore, the therapist should be mindful of the need (at least initially) to train the patient to stand and take weight on the affected lower extremity in a quiet, minimally distracting environment. This may be even more critical for patients with attention disorders manifesting as distractibility, impulsivity, and irritability with increased stimulation. As noted earlier, the therapist must consider the need to incorporate competing stimuli into therapy gradually; otherwise, the therapist cannot assert that functional balance has been achieved.
Achieving weight shift in standing requires a substantial amount of cueing by the therapist, because patients often are fearful of standing on the affected leg due to reduced muscle strength, postural control, and sensation. Visual disturbances also may make standing a frightening activity for the patient.
Early in treatment, the use of a wall (Fig. 14-36) may be desirable to offer the patient substantial support; however, this should not be used to train functional reach in standing, because postural muscle activity in the legs is reduced (with the help of the wall) when the patient makes an arm movement. A manually guided approach is useful to help the patient learn the desired end of the movement pattern. Contact by the therapist directly on the pelvis (with one hand on each side) offers optimal control to guide the weight shift, and the therapist gradually can taper the amount of guidance required as the patient begins to activate more.

Figure 14-36 A wall can be a helpful starting place in teaching a patient to maintain a standing position. The wall can assist the patient to achieve alignment of body parts in what can be a frightening position to assume. However, the wall does not substitute for the need to learn to stand and function in open space.
Free-standing balance should be attempted as soon as possible (see Chapter 8). Standing while simultaneously scanning the environment or having a conversation with the therapist is challenging and meaningful (Fig. 14-37).
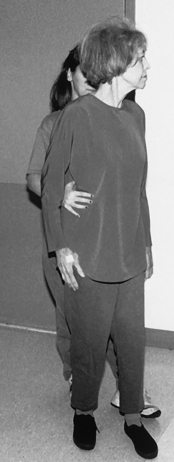
Figure 14-37 The therapist cues weight shifting in standing while encouraging the patient to scan the environment. Standing and looking around a room can prove challenging for patients in the initial stages of learning to stand.
A progression to standing and reaching prepares the patient to be able to perform personal self-care and IADL safely and efficiently in a standing position. The patient needs to practice reaching in all directions in functional environments (Fig. 14-38). As Carr and Shepherd22 outlined, this should include reaching overhead, to the side, backward, and down, progressing to unilateral and bilateral reaching to the floor. Task-specific training provides the patient with the opportunity to develop strategies to solve problems encountered in standing.
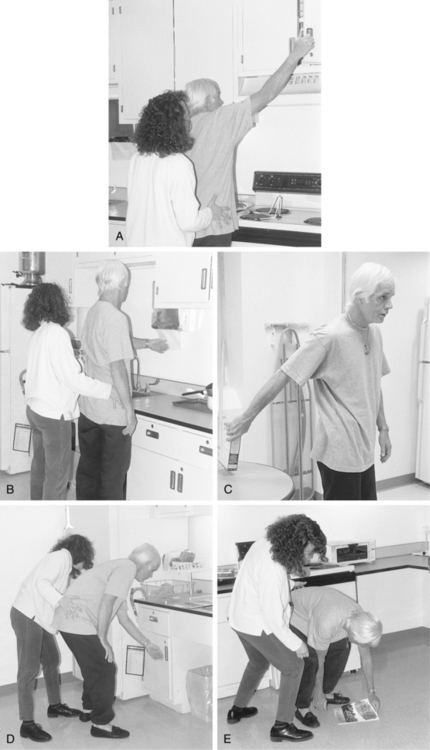
Figure 14-38 Training for weight shifting and reaching in standing should occur within a functional context because task-specific training is most beneficial to the learner. Reaching up (A), forward (B), backward (C), reaching down (D), and toward the floor (E). These patterns are among the many patterns of movement the patient should practice within functional activities. Occupational therapists are uniquely qualified with their expertise in task analysis to train patients to perform basic and instrumental activities of daily living.
A commonly held view about asymmetrical hemiparetic gait is that it may be subject to amelioration by balance training emphasizing weight-bearing on the paretic lower extremity. However, a study by Winstein and colleagues,93 in which hemiparetic subjects received specific balance training with a specially designed feedback device, revealed that balance in standing may be improved, but no carryover into a more symmetrical gait pattern occurs. This suggests that skill acquisition has a task-specific nature, and therapists cannot assume progress achieved in one skill area can be carried over or transferred to another. This finding calls into question many commonly held beliefs about the use of developmental progression to increase functional capabilities in upright positions.
Sit-to-stand and stand-to-sit may be the same in certain basic ways. However, the key differences have implications for treatment. First, movement duration has been found to be longer in stand-to-sit than in sit-to-stand.56,83 In stand-to-sit, lower limb extensors are working in a flexed position and execute the task by eccentric (lengthening) rather than concentric (shortening) the way they do in sit-to-stand. Controlling the descent is a difficult task for muscles with compromised strength, and certainly in the initial stages following stroke, many patients with hemiplegia sit by letting go and almost collapsing into a seated position, rather than executing a smooth, controlled descent into a seat. Practicing stand-to-sit with patients is important and should be practiced as often as sit-to-stand. Gaining control in sit-to-stand does not translate to stand-to-sit.
Falls prevention
It has been identified that falls in the elderly have been associated with underlying precipitants, such as intrinsic factors (related to physiological changes, pathological conditions, and adverse medication effects) and situational factors (length of stay in institutional settings, time of falling, and availability of caretakers).71 These factors apply similarly to the stroke population as well.
Falling can be a major complication during stroke rehabilitation. Nyberg and Gustafson67 studied the incidences, characteristics, and consequences of falls in an inpatient rehabilitation setting. They sampled 161 patients consecutively admitted for geriatric stroke rehabilitation. They found that 62 patients (39%) sustained a fall, and 39 patients (24%) suffered more than one fall. Most of these falls occurred during transfers or from sitting in a wheelchair or some other type of furniture.
Nyberg and Gustafson67 further noted that extrinsic factors (slips, trips, furniture moving, etc.) accounted for 17 falls (11%), while intrinsic factors were involved in 49 falls (32%). Intrinsic factors were specifically related to impaired balance, motor issues such as the legs giving way, and cognitive impairments such as perceptual issues and distraction or inattention. Six falls (4%) involved fractures or other serious injury. The authors concluded that falls constitute a significant problem in stroke rehabilitation, and fall prevention strategies must be developed and incorporated into rehabilitation programs.67
It appears that fear of falling in stroke patients has a relationship to a history of earlier falls and functional characteristics of these individuals, as noted by a study conducted by Andersson and colleagues.5 The study included 140 patients who had been treated in a stroke unit during a 12-month period. The Falls Efficacy Scale, Swedish version (FES-S) and tests of motor ability, functional mobility, and balance were used to evaluate factors contributing to fear of falling. In univariate analysis, there was a significant association between increased age, female sex, previous falls, visual and cognitive impairment, low mood, and impaired physical functioning with low fall-related self-efficacy. In multivariate analysis, only a history of previous falls and physical function remained significant. Fear of falling was associated significantly with poor physical function and previous falls. The findings in this study support the importance of offering fall prevention programs to stroke survivors, whether they have sustained a fall or not.5
This study raises the important topic of excess disability. Excess disability is defined as the restriction of ADL beyond that which the person is physically and cognitively capable of performing. This concept has been gaining increased attention in the public health literature over the past few decades.
Even among the general aging population, there is evidence of excess disability created by the fear of falling. Yardley and Smith98 explored feared consequences of falling with over 200 community-living people over the age of 75 years. Their findings showed many individuals had a loss of functional independence and damage to their identities from the fear of falling. Fears were correlated with avoidance of activity (after adjusting for age, sex, and recent falling history) and predicted further avoidance in activity months later.98
Lach58 reported that having two or more falls, feeling unsteady, and reporting fair or poor health status were independent risk factors for developing fear of falling. Bruce and colleagues17 saw that fear of falling is common in healthy, high-functioning older women and is independently associated with reduced levels of participation in recreational physical activity.
It is clear that a program of falls prevention for stroke survivors, starting in the inpatient rehabilitation setting, is important to help these individuals develop strategies for dealing with changes in physical and cognitive functioning. These programs also have the potential to help address fear of falling that may exist whether or not the patients have actually fallen.
To date, there are no publicized randomized controlled trials (RCTs) researching the effectiveness of falls prevention strategies in stroke survivors. The Falls Prevention After Stroke Survivors Return Home (FLASSH) study8 is an RCT seeking to evaluate stroke survivors now living at home, who have been discharged from inpatient rehabilitation. The patients present at a high risk for falling and will participate in a multifactorial prevention program. In the future, the results of this study will be important to contributing to the evidence-based practice in fall prevention programs.
As of the writing of this chapter, there are a number of web-based fall prevention resources available (Box 14-1).
Box 14-1 Fall Prevention Websites
National Center for Injury Prevention and Control, CDC: Preventing Falls: How to Develop Community-Based Fall Prevention Programs for Older Adults: www.cdc.gov/ncipc/preventingfalls/
National Council on Aging, Center for Healthy Aging: National Action Plan: www.healthyagingprograms.org/content/asp?sectionid=69
Creative Practices in Home Safety Assessment and Modification Study: www.healthyagingprograms.org/content.asp?sectionid=31&ElementID=568&FromSEarchResult= creative
Adjunct techniques to enhance skill acquisition
Feedback
Patients rely on feedback for performance of all mobility tasks. For example, before initiating a transfer, a patient uses visual information about the appropriate position of the limbs before movement begins. As the patient begins to rise from the seated position, the somatosensory system provides information about the forces exerted and the ongoing changes in limb position. On completion of this task, the results of the sequence provide additional feedback. The patient uses the feedback given to gain a sense of how it felt to rise to a standing position. Was it efficient? Was it difficult? This information gained during or after the mobility sequence is termed movement-produced feedback.78
As discussed in Chapter 5, feedback is divided into two broad categories: intrinsic and extrinsic (augmented). Intrinsic is information from the sensory systems while extrinsic (augmented) is information that supplements sensory information such as verbal directives provided by the therapist.78 For example, the therapist tells the patient to “straighten your hips and stand tall,” as the patient rises to stand at a sink for grooming.
Feedback is important to the rehabilitation process, and the therapist should carefully select the type of feedback provided, the amount, and the schedule. Feedback should be distinguished from encouragement, which facilitates continued participation of the patient in the mobility task. “Try more” or “Keep going!” are examples of encouragement that recognize the patient’s effort. Forms of feedback for coming to the stand position would include: “Good job. You were able to stand at the sink” (knowledge of results [KR]) or “Next time you need to lean forward more before rising”(knowledge of performance [KP]). Gentile38,39 described two kinds of augmented feedback that are illustrated in two examples:
1. Knowledge of results: defined as knowledge of information about the performer-environment interaction
2. Knowledge of performance: defined as knowledge of information about movement
Gentile suggested that the demands of the task best dictate the most effective form of feedback. Activities that can be characterized according to the taxonomy of tasks as closed and consistent motion tasks require information about the movement to be transmitted from the instructor to the learner. For example, when training a patient in rolling over in bed or achieving sit-to-stand from a wheelchair, the provision of feedback about placement of the extremities and maintenance of alignment is useful. Using Gentile’s taxonomy, tasks that can be categorized as open and variable motionless tasks are performed under changing environmental conditions. These tasks require that feedback to the learner should focus on directing attention to environmental factors that may influence selection of movement strategies and patterns. For example, standing up while on a bus requires anticipation of the motion of the bus, movement of persons in the immediate environment, and consideration of changing space constraints. See Chapter 5.
Almost all of the research investigating the efficacy of feedback has emphasized knowledge of results focusing on the relative frequency and timing of delivery. Winstein and Schmidt95 compared the performance of two groups and the frequency of feedback. In this study, one group received feedback on a fading schedule (50% of the trials) while the other group received feedback on 100% of the trials. The study found that during the acquisition phase, the group receiving 100% frequency had a slight advantage; however, it also found that the group receiving 50% frequency performed better on a delayed retention test. The investigators proposed that the decreased KR provided to the 50% group encouraged development of alternative strategies, while the group receiving 100% feedback may have come to rely too heavily on the KR.
In another study, Lavery and Suddon59 compared summary and immediate feedback and the effects on transfer of skills. The study explored the results of the schedule of feedback and performance of three groups of subjects. One group received immediate feedback on every trial, a second group received summary (at the end of a block of 20 trials), and a third group received both types of feedback. At the end of the acquisition trials, the groups receiving feedback after each trial (groups 1 and 3) performed better than group 2. When groups were compared on a subsequent transfer test where no feedback was provided, group 2’s (summary feedback) performance was significantly better than groups 1 or 3. At first glance, summary feedback appears more effective than immediate feedback. Schmidt and Lee78 suggested that the results indicate that immediate KR is detrimental to learning, based on the findings that group 3, which received both immediate and summary, did not perform as well as group 2. They hypothesized that too much information and overreliance on the immediate KR were disadvantageous to learning information. Alternatively, summary KR encourages the subject to develop strategies that are flexible and suitable to transfer. The findings of these two studies give cause for reflection on the degree, frequency, and timing on when the therapist should provide feedback during mobility training. Winstein92 posited that less information feedback creates an environment conducive to facilitating the learner to develop problem-solving strategies. Information about movement and performance of mobility tasks should be precise and should identify movements that are critical to efficiency and safety. At all times, a therapist should avoid “liberal” use of feedback and inaccurate or untruthful feedback. An example of this would include the therapist who spontaneously says “great job” when a patient performs a transfer just because he or she made it to the transfer surface, even though the feet were not positioned correctly or the hips were not adequately extended. This feedback may negatively affect performance and learning. Patients may discount their own abilities to assess performance and to identify errors because of the powerful influence a therapist’s feedback can have on shaping future efforts.
Many therapists videotape patients to provide information about performance and measure improvement in skill. This can prove useful, particularly with patients who may lack awareness about their performance (see Chapter 19). The use of videotape as a form of augmented feedback is not new to the rehabilitation process, but the increased ease in taping with a wide variety of commercially available products has increased the viability. A videotape captures the client’s movement, features in the environment that are stable and do not change, and the everyday spontaneous occurrences that require immediate adaptations. Videotaping may be instrumental to assisting clients in developing flexible movement strategies that can solve the movement dilemmas encountered during participation in routine tasks.
Research supports that just showing a video tape does not influence performance; it must be supplemented with structured feedback by the clinician. Videotape has been used to improve awareness of performance and to assist patients in identifying behaviors that impede performance in clients exhibiting unilateral neglect. The therapist identifies salient features, provides verbal feedback during review of the videotapes, and focuses the patient’s attention to details.87 Hodges, Chua, and Franks46 identified that videotape may be used to augment the learning of complex motor skills and may contribute to retention of these skills.
Mental practice
A substantial body of research suggests that mental practice can improve learning of new motor skills in healthy individuals and, as a result, has been getting increased attention in the rehabilitation literature.50 The past several years have seen an increase in research conducted on the efficacy of mental practice with a stroke population. Braun and colleagues14 conducted a systematic literature search of studies published through August 2005. These included four RCTs, one CCT, two patient series, and three case reports. The studies examined the use of four different mental practice strategies with most tasks involving mental rehearsal of arm movements. They noted that studies were limited in size and determined that no definite conclusions could be made except that further research is needed for a clear definition of the content of mental practice and standardized measurements of outcomes.14
Braun and colleagues15 set out to provide a framework for integrating mental practice into therapy by looking at the available evidence and theory. Drawing on sports literature and their own experiences, they described five steps to facilitate the patient’s imagery capabilities: (1) assessing mental capacity to learn imagery technique, (2) establishing the nature of mental practice, (3) teaching imagery technique, (4) embedding and monitoring imagery technique, and (5) developing self-generated treatments.15
Manual guidance
Manual guidance is a technique frequently used during the rehabilitation process, which is often described as assisting the patient to “feel” the appropriate movement pattern or to position the patient in a desired posture using physical handling techniques. The degree of manual guidance provided and when it is supplied remains a controversial subject. Two types of manual guidance have been identified in the literature: passive movement and spatiotemporal constraint (physical restriction); both forms are often incorporated during mobility training.48,49,62 For example, during the mobility task of rolling toward the affected hemiplegic side, the paretic arm is often passively moved and placed in a safe position in preparation for the patient to move his or her body over the prepositioned arm. Another application of this strategy occurs when a patient attempts to roll toward the nonaffected side. The therapist passively moves the paretic arm up and across the body before the patient attempts to move the trunk. The passive movement of the arm is thought to serve as a “guide” for the patient to gain an understanding of what actions are necessary to effectively roll (e.g., scapular protraction or flexion of the humerus). Likewise, spatial constraint is also used during retraining of many mobility tasks such as sit-to-stand or transfer training. A therapist may stabilize a part of a limb while the patient attempts to control only part of the limb (limit the degrees of freedom). An example of spatial-restraint during the sit-to-stand sequence is when the therapist applies an external force to stabilize the foot on the floor, thus enabling the patient to optimally use any muscular activity generated by the quadriceps combined with the extensor forces of the hip, knee, and ankle to rise vertically to the standing position.
The use of manual guidance during intervention needs to occur with careful consideration of the research findings that have identified significant concerns about the benefits or efficacy of the techniques.78,79 The literature supports that guidance may be most effective during the acquisition of motor skills, when the requirements and demands of the task are new to the learner. The literature also recommends that therapists attempt to integrate active practice trials with interspersed passive guidance.94
Evaluation tools
Many therapists perform a subjective assessment of functional mobility based on clinical observation. However, it is advantageous to use a recognized evaluation tool to support the need for services, to document progress, and to assess treatment efficacy. Table 14-2 includes a list of relevant tools for evaluating mobility functions. Currently the only standardized evaluation for mobility skills is Carr and Shepherd’s Motor Assessment Scale for Stroke Patients.20 This test assesses the following eight areas:
Table 14-2 Tools for Evaluating Mobility Functions
| ASSESSMENT/AUTHOR | POPULATION/PURPOSE | SOURCE/CONTACT |
|---|---|---|
| Activities-Specific Balance Confidence Scale (ABC)70 | Adults with balance deficits: evaluate balance confidence in daily activities. A 16-item scale in a questionnaire format | Contact: Anita Myers Department of Health Studies and Gerontology, University of Waterloo, Waterloo, ON N2L 3G1 |
| Falls Efficacy Scale (FES) (1990)89 | Elderly individuals in a community setting: survey related to perceived self-confidence connected to daily activities | |
| Frenchay Activities Index47 | Adults: to assess function in adults status poststroke: ADL and IADL | |
| Functional Independence Measure (FIM)41 | Adults with various impairments: measures functional status; reflects the impact of disability on the individual and on human and economical resources in the community. 18 activities, 13 with a motor emphasis related to self-care, 5 with a cognitive emphasis involving communication | Uniform Data System for Medical Rehabilitation. 270 Northpointe Parkway, Suite 300, Amherst, NY 14228 (716) 817-7800 |
| Home Falls and Accidents Screening Tool (HOME-FAST)61 Environment Checklist |
Adults at risk of falling: to identify environment and functional safety at home | |
| Melville-Nelson Self-Care Assessment (SCA)66 | Adults in subacute rehabilitation and nursing homes: to assess self-care skills including bed mobility, transfers, toileting, personal hygiene, and bathing | http://hsc.utoledo.edu/allh/ot/melville.html |
| Morse Fall Scale (MFS) | Adults with balance deficits: rapid and simple method of assessing a patient’s likelihood of falling. Acute care hospital and long-term inpatient settings | Contact: Janice M. Morse. Pennsylvania State University, School of Nursing, 201 Health and Human Development East, University Park, PA 16802-6508 |
| Stroke Impact Scale (SIS), (SIS-16)34 | Adults: measures stroke recovery in 8 domains: strength, hand function, mobility, ADL, emotion, memory, communication, and social participation | Langdon Center on Aging. University of Kansas Medical Center Mail Stop 1005, 3901 Rainbow Boulevard, Kansas City, KS 66160. (913) 588-1203 www2.kumc.edu/coa/SIS/Stroke-Impact-Scale.htm |
| Timed Get Up and Go (TGUG)68 | Adults with balance deficits | |
| Tinnetti Balance Test of the Performance-Oriented Assessment of Mobility Problems (Tinnetti)88 |
Adults with balance deficits | |
| Trunk Control Test25 | Adults with stroke: assess the motor impairment in a patient who has had a stroke. Rolling, balance in sitting, and sit up from lying down | |
| Westmead Home Safety Assessment24 | Older adults at risk of falling: to identify fall hazards in the home |
The advantages of the Motor Assessment Scale include the following:
1. It tests recovery specific for the patient recovering from stroke.
2. It takes less time to administer and infringes little on treatment time.
3. It is simple to administer and has objective and clear descriptions of criteria for rating patients.
4. It is sensitive to changes in patients’ motor recovery status and therefore is useful in describing patient progress over time.
The FIM was developed by the Uniform Data System at the State University of New York at Buffalo as a standardized way for professionals to evaluate patient progress regarding levels of assistance needed to perform personal self-care, functional mobility, communication, cognition, and social interaction. Each area is graded on a scale of 1 to 7, with a score of 1 indicating total dependence and 7 indicating complete independence. The areas of functional mobility covered in this test include transfers to bed, chair, toilet, tub, locomotion, and stairs. This test is used in rehabilitation centers across the United States and has been found to have good to excellent reliability.41,42
The Assessment of Motor and Process Skills is a standardized test created by occupational therapists that simultaneously evaluates motor and process skills to predict effect on the ability to perform IADL. Such an evaluation tool, if developed for functional mobility skills, would prove invaluable for occupational therapists (see Chapter 21).
Anticipating changing environments
The ultimate goal of functional mobility retraining is to have the patient resume the roles and activities associated with the lifestyle before the stroke. This goal presumes that patients need to transfer reacquired mobility skills to environments unique to the individual lifestyle and participation patterns. The treatment setting presents a predictable environment in which the physical aspects of therapeutic equipment and furnishings remain unchanged from one treatment session to another. The patient’s home environment also may be viewed as predictable because of the patient’s familiarity with the surroundings. The physical layout and home furnishings change little over time, even if home modifications are introduced. Nevertheless, therapists frequently observe problems as the patient attempts to make the transition from the treatment setting to the home environment. Unexpected problems occur within the closed home environment, and community-based activities challenge the individual’s ability to solve newly encountered problems. The occupational therapist is well-qualified to address these dilemmas through task analysis of occupations and careful consideration of the environmental contexts in which each task is performed.75 The patient recovering from stroke is required to generalize and adapt mobility skills learned in the clinic setting to meet the changing environmental demands encountered on discharge. This generalization and adaptation occurs through the interaction among multiple systems: perceptual, cognitive, sensory, and motor. This chapter previously presented specific strategies for ameliorating performance impairments influencing functional mobility. These strategies should be incorporated throughout the intervention process as a means to attain generalization and encourage participation in life situations or IADL on discharge.
Strategy development
The research examining normal movement sequences has found great variety in the movement patterns used to perform each mobility task. A single pattern may be identified as occurring more frequently during rolling, although many subjects use alternative patterns that are equally effective. Similarly, the methods described to retrain patients to roll over also vary. No single correct strategy is available to achieve this mobility task. Strategy development is more than learning to use a normal pattern of movement; it results from the patient’s exploration of movement possibilities in relation to tasks occurring in different environments.84 Thus, the occupational therapist may use several methods of instruction while assisting the patient in learning movement limitations and determining future mobility potentials.75,84 The two primary strategies for functional mobility include a force control strategy and a momentum strategy.26 Early in the intervention process, patients may benefit from instruction in a force control strategy to prevent secondary impairments of fixations and resultant development of inappropriate compensatory strategies.12,20,22,28,29 This method of instruction also is preferred for patients who do not have adequate stability of the trunk musculature because it may facilitate independent performance.22 A momentum strategy or a combination of momentum and force control may be introduced if stability of the trunk is evident. Momentum is more efficient, requires less muscular activity, and approximates more normal-looking movement.
Not all patients can achieve a momentum strategy, but many patients may attempt to do their own in the home environment, particularly if it was their preferred method of movement before the stroke. Therapists need to anticipate this possibility and explore momentum as an alternative before discharge. Transition from a force control to a momentum strategy requires simple, concise instruction to move quickly without stopping the movement. The therapist may use manual cues at the shoulder girdle to ensure safety, and demonstration by the therapist is also helpful. The practice of momentum strategies also may prepare the patient to control movement during stressful life situations that occur unexpectedly and require quick transitional movements.
Practice conditions
To prepare the patient to resume the previous lifestyle, the occupational therapist must consider carefully the conditions under which practice takes place. The goal of intervention is to maximize retention and transfer of acquired skills to everyday life situations the patient will encounter.44 The therapist must increase the demands of the learning context during practice to prepare the patient to respond to unpredictable events. Chapter 5 presented an overview of factors the therapist considers when structuring the practice conditions in stroke rehabilitation. The following are considerations specific to functional mobility retraining.
Blocked and random practice.
Blocked practice in functional mobility retraining is the rote practice of mobility functions in sequence. For example, the patient initially practices rolling to the unaffected side, then to the affected side, and then to the seated position. Repetition of experiences and a degree of mastery must occur at each level before the patient proceeds to the next level of skill. This method of structuring practice initially may assist the patient in gaining proficiency during the practice session but is not effective in preparing the patient to engage in self-care tasks in which changes in the position of the body occur randomly in response to task requirements. For example, the patient rolls to the left to reach for a brush on the table; it is just beyond reach. The patient rolls back to supine and assumes a bridge position, pushing upward in bed. The patient then rolls again and is able to grasp the brush. Random practice of mobility tasks improves learning, retention, and the ability to solve motor problems encountered in life situations.80 Schmidt76 recommended that randomized practice be incorporated throughout the intervention process. Mobility tasks should be interspersed with other tasks such as ADL training in which the patient must make transitional movements in a natural context. The trial-and-error exploration of functional mobility in this context initially may prove difficult for the patient. Progress may be slow, and the therapist may be tempted to instruct the patient in a single movement strategy to speed progress. Varying the practice conditions increases the contextual interference, facilitating generalization as the patient relies on multiple processes and promoting the development of versatile motor strategies.52,90
Schmidt noted one exception in which a part-to-whole method of practice may be beneficial. Early in the intervention process, when the patient is acquiring foundational skills, practicing of component movements may be necessary. For example, the patient initially may need to gain control of lateral flexion of neck and trunk muscles before these movements can be incorporated into the side lying-to-sit sequence. Schmidt suggested that as soon as patients are able to perform these component movements, they should be integrated immediately into programs emphasizing random practice.76 This method of practice can be used only with mobility functions that are readily divided into natural component parts.77,92
Varying the practice conditions for specific tasks.
Gentile’s taxonomy of motor tasks38,39 is useful for determining the most appropriate practice conditions for each mobility task. Objects, persons, and the spatial temporal characteristics of each task influence the motor strategies selected. Sabari75 suggested that the occupational therapy process inherently considers the importance of the regulatory conditions to task performance. Occupational therapists frequently adapt and regulate the environment to facilitate mobility functions, as in adjusting the height of a bed in preparation for a transfer (Figs. 14-39 and 14-40). Similarly, the amount of verbal cues and physical assistance is adjusted to foster independent performance and skill development. Sabari also directed attention to the crucial role occupational therapists assume as regulators throughout mobility retraining.
Closed tasks
Early in the treatment process, most functional mobility tasks may be considered closed, and the environmental features are regulated easily to improve performance. Rolling over and coming to a seated position in a hospital bed occurs on a stationary surface. The therapist can regulate the environment further by positioning pillows and bed linens appropriately, raising the bed guard rails, adjusting the height of the bed, limiting the number of persons moving around the patient’s bed, and positioning the body in a fairly static position to assist the patient if needed. Another important characteristic of a closed task is that movement is self-paced and no temporal constraints are placed.
The therapist’s role as a regulator can be equated with the degree of assistance or handling provided. The therapist initially may give significant physical assistance and use a variety of adjunct techniques to promote perceptual, cognitive, and sensory processing. As the patient regains control of movements in desired sequences, physical assistance and the amount of cueing is reduced gradually or eliminated.75
Variable motionless tasks
Bed mobility becomes a variable motionless task if the therapist is not present to regulate certain features of the environment. Patients preparing to get out of bed independently may find the pillows and bed linens in disarray, making movement difficult; the bed guard rails are lowered, the top of the bed remains slightly elevated, and the height of the bed may be too high. Simultaneously the patient may be receiving verbal encouragement to “hurry up.” Without the therapist present to structure the environment, the patient may experience difficulty and may use compensatory strategies incompatible with the restoration of performance component deficits. The patient may hook the unaffected leg under the affected leg and use the hands to pull up to a seated position.
This comparison illustrates the way overstructuring the environment does not prepare the patient recovering from stroke to develop flexible motor strategies. The patient needs to have opportunities to process information and acquire the ability to solve future problems.2,76 Abreu1 studied the effects of environmental regulation on postural control and found that unpredictable environments elicited improved control. These findings are contrary to beliefs occupational therapists have held concerning the grading of tasks from simple to complex and the structuring of environments from predictable to unpredictable. Abreu1 postulated that the results of this study indicate that both types of environments should be incorporated concurrently in the intervention process. The therapist may regulate the environment but not on all trials. Perhaps the height of the bed is adjusted and the guard rails are elevated on one trial, whereas the next session may require the patient to instruct the therapist verbally in the arrangement of the immediate surroundings in preparation for the mobility task.
Consistent motion tasks
During consistent motion tasks, the pace of the environment remains the same and the environment moves. These tasks are associated with mechanical devices such as conveyor belts. Most functional mobility tasks do not meet this criterion.
Open tasks
Many advanced mobility skills meet the criterion of an open task in which the spatial and temporal parameters of movement are determined by events occurring in the environment. Open tasks require more precise timing of movement, and the patient is challenged to anticipate and react to unexpected events. Sit-to-stand on a moving train, plane, or bus are examples of open tasks. Practice of these tasks should occur in the actual environment whenever possible.45,75 Patients who are physically capable of attempting these advanced skills should be engaged in them while in the rehabilitation setting whenever possible.
Patients who do not have adequate foundational skills while hospitalized can benefit from interventions to improve future potential for the acquisition of advanced mobility skills. Patients need to be introduced to unpredictable environments in which they have the opportunity to explore movement strategies and develop problem-solving abilities. Early in the intervention process, the therapist’s handling techniques to prepare and assist the patient can be modulated using different degrees of tactile, proprioceptive, and kinesthetic input as the patient engages in functional mobility tasks. For example, as the patient learns to transfer, the therapist can vary the sensory cues and amount of assistance.11 Responding to changes in sensory input may be helpful in the development of anticipatory postural adjustments.84
Summary
The performance of functional mobility tasks should not occur in isolation, as in a gross mobility mat program. Practice of mobility skills while the patient is engaged in life tasks presents opportunities to solve unexpected problems that arise as the patient manipulates different objects and encounters changing support surfaces and changing temporal demands. The following are some suggestions for altering the regulatory features in the clinical environment.
Rolling
 Practice rolling on a narrow surface such as a sofa.
Practice rolling on a narrow surface such as a sofa.
 Encourage abrupt change in direction, as in reversing the movement in midstream.
Encourage abrupt change in direction, as in reversing the movement in midstream.
 Practice rolling under a heavy quilt.
Practice rolling under a heavy quilt.
 Try rolling with an object such as a newspaper in the hand.
Try rolling with an object such as a newspaper in the hand.
 Attempt propping to side lying to adjust pillows.
Attempt propping to side lying to adjust pillows.
Sit-to-stand
Reclining chair with a significant seat depth
Chair with wheels such as a desk chair
Seat on public transportation (such as a bus or subway)
 Incorporate varying standing surfaces:
Incorporate varying standing surfaces:
 Include varying speed of movement.
Include varying speed of movement.
 Account for varying objects and pets in the environment.
Account for varying objects and pets in the environment.
 Incorporate changing lighting.
Incorporate changing lighting.
Review questions
1. What effect does the patient’s place in the life cycle have on planning relevant treatment in functional mobility retraining?
2. What are the impairments associated with stroke and how do they affect functional mobility tasks?
3. What is the force control strategy?
4. What are the three major task requirements for locomotion that can be applied to all functional mobility tasks?
5. What three possible interventions can be used to maximize a patient’s ability to achieve lateral trunk flexion?
6. What implications for treatment may be derived from the research done by Carr, Shepherd, and Gentile on sit-to-stand?
7. What does the research show regarding the use of practice in rehabilitation?
8. How can the therapist structure the practice of functional mobility tasks, considering the venue of care?
1. Abreu BC. The effect of environmental regulations on postural control after stroke. Am J Occup Ther. 1995;49(6):517-525.
2. Abreu BC, Toglia JP. Cognitive rehabilitation. a model for occupational therapy. Am J Occup Ther. 1987:45;7:439-448.
3. Alexander NB, Grunawalt JC, Carles S, et al. Bed mobility task performance in older adults. J Rehabil Res Dev. 2000;37(5):633-638.
4. American Occupational Therapy Association. Practice framework. domain and process, 2nd ed. Am J Occup Ther. 2008:62;6:625.
5. Andersson AG, Kamwendo K, Appelro P. Fear of falling in stroke patients. relationship with previous falls and functional characteristics. Int J Rehabil Res. 2008:31;3:261-264.
6. Árnadóttir G. The brain and behavior: assessing cortical dysfunction through activities of daily living. St Louis: Mosby; 1990.
8. Batchelor FA, Hill KD, Mackintosh SF, Said CM Whitehead CH. The FLASSH study. protocol for a randomized controlled trial evaluating falls prevention after stroke and two sub-studies. BMC Neurol. 2009;31:9-14.
8. Benoussan L, Viton JM, Schieppati M, et al. Changes in postural control in hemiplegic patients after stroke performing a dual task. Arch Phys Med Rehabil. 2007;88(8):1009-1015.
9. Bernstein N. The coordination and regulation of movement. Elmsford, NY: Pergamon; 1967.
10. Bly L. What is the role of sensation in motor learning? What is the role of feedback and feedforward. NDTA Network. 1996;5:5.
11. Bobath B. Adult hemiplegia. evaluation and treatment, ed 3. Oxford: Butterworth-Heinemann. 1990.
12. Bobath B. Adult hemiplegia. evaluation and treatment, ed 2. London: Heinemann. 1978.
13. Braun SM, Beurskens AJ, Borm PJ, et al. The effects of mental practice in stroke rehabilitation. a systematic review. Arch Phys Med Rehabil. 2006:87;6:842-852.
14. Braun S, Kleyman M, Schols J, et al. Using mental practice in stroke rehabilitation. a framework. Clin Rehabil. 2008:22;7:579-591.
15. Britton E, Harris N, Turton A. An exploratory randomized controlled trial of assisted practice for improving sit-to-stand in stroke patients in the hospital setting. Clin Rehabil. 2008;22(5):448-458.
16. Bruce DG, Devine A, Prince RL. Recreational activity levels in healthy older women. the importance of fear of falling. J Am Geriatr Soc. 2002:50;1:84-89.
17. Burdett RG, Habasevich R, Pisciotta J, et al. Biomechanical comparison of rising from two types of chairs. Phys Ther. 1985;65(8):1177-1183.
18. Carr JH, Gentile AM. The effect of arm movements on the biomechanics of standing up. Hum Mov Sci. 1994;13(2):175.
19. Carr JH, Shepherd RB. Neurologic rehabilitation. optimizing motor performance. Oxford: Butterworth-Heinemann. 1998.
20. Carr JH, Shepherd RB. A motor learning model for rehabilitation. In: Carr JH, Shepherd RB, editors. Movement science: foundations for physical therapy in rehabilitation. Rockville, MD: Aspen, 1987.
21. Carr JH, Shepherd RB. A motor relearning programme for stroke. Oxford: Butterworth-Heinemann; 1987.
22. Cheng PT, Wu SH, Liaw MY, et al. Symmetrical body weight distribution training in stroke patients and its effect on fall prevention. Arch Phys Med Rehabil. 2001;82(12):1650-1654.
23. Clemson L. Home fall hazards. a guide to identifying fall hazards in the homes of elderly people and an accompaniment to the assessment tool, the Westmead Home Safety Assessment (WeHSA). West Brunswick, Victoria: Coordinates Publications. 1997.
24. Collin C, Wade D. Assessing motor impairment after stroke. a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990:53;7:576-579.
25. Crutchfield CA, Barnes MR. Motor control and motor learning in rehabilitation. Atlanta: Stokesville; 1993.
26. Das P, McCollum G. Invariant structure in locomotion. Neuroscience. 1988;25(3):1023-1034.
27. Davies PM. Right in the middle. selective trunk activity in the treatment of adult hemiplegia. New York: Springer-Verlag. 1990.
28. Davies PM. Steps to follow. a guide to treatment of adult hemiplegia. New York: Springer-Verlag. 1985.
29. Dean CM, Shepherd RB. Task-related training improves performance of seated reaching tasks after stroke. a randomized controlled trial. Stroke. 1997:28;4:722-728.
30. Dean CM, Channon EF, Hall JM. Sitting training early after stroke improves sitting ability and quality and carries over to standing up but not to walking. a randomized controlled trial. Aust J Physiother. 2007:53;2:97-102.
31. De Haart M, Geurts AC, Huidekoper SC, et al. Recovery of standing balance in postacute stroke patients. a rehabilitation cohort study. Arch Phys Med Rehabil. 2004:85;6:886-895.
32. Dickstein R, Shefi S, Marcovitz E, Villa Y. Anticipatory postural adjustments in selected trunk muscles in post stroke hemiparetic patients. Arch Phys Med Rehabil. 2004;5(2):261-267.
33. Duncan PW, Wallace D, Lai SM, et al. The stroke impact scale version 2.0. evaluation of reliability, validity and sensitivity to change. Stroke. 1999:30;10:2131-2140.
34. Fisher CM. Left hemiplegia and motor impersistence. J Nerv Ment Dis. 1956;123(3):201.
35. Ford-Smith CD, Van Sant AF. Age differences in movement patterns used to rise from a bed in the third through fifth decades of age. Phys Ther. 1992;73(5):305.
36. Gentile AM. Implicit and explicit processes during acquisition of functional skills. Scand J Occup Ther. 1998;5(1):7-16.
37. Gentile AM. Skill acquisition. action, movement and neuromotor processes. Carr JH, Shepherd RB, editors. Movement science: foundations for physical therapy in rehabilitation. Rockville, MD: Aspen, 1987.
38. Gentile AM. A working model of skill acquisition with application to teaching. Quest. 1972;17:3-23.
39. Gillen G, Wasserman M. Mobility. examining the impact of the environment on transfer performance. Phys Occup Ther Geriatr. 2004:22;4:21-29.
40. Granger CV, Hamilton BB. The Uniform Data System for medical rehabilitation report of first admissions for 1990. Am J Med Rehabil. 1992;71(2):108-113.
41. Granger CV, Hamilton BB, Linacre JM, et al. Performance profiles of the Functional Independence Measure. Am J Phys Med Rehabil. 1993;72(2):84-89.
42. Hall ET. The hidden dimension. New York: Doubleday; 1966.
43. Hartman-Maeir A, Soroker N, Oman SD, et al. Awareness of disabilities in stroke rehabilitation: a clinical trial. Disabil Rehabil. 2003;25(1):35-44.
44. Higgins JR, Spaeth RK. Relationship between consistency of movement and environmental condition. Quest. 1972;17:61.
45. Hodges NJ, Chua R, Franks IM. The role of video in facilitating perception and action of a novel coordination movement. J Mot Behav. 2003;35(3):247-260.
46. Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing. 1983;12(2):166-170.
47. Holding DH. Learning without errors. In: Smith LE, editor. Psychology of motor learning. Chicago: Athletic Institute, 1970.
48. Holding DH, Macrae AW. Guidance restriction and knowledge of results. Ergonomics. 1964;7(3):289-295.
49. Jackson PL, Lafleur MF, Malouin F, et al. Potential role of mental practice using motor imagery in neurologic rehabilitation. Arch Phys Med Rehabil. 2001;82(8):1133-1141.
50. Janssen WG, Bussman HB, Stam HJ. Determinants of the sit-to-stand movement. a review. Phys Ther. 2002:82;9:866-879.
51. Jarus T. Motor learning and occupational therapy. the organization of practice. Am J Occup Ther. 1994:48;9:810-816.
52. Johnstone M. Restoration of motor function in the stroke patient, ed 2. New York: Churchill Livingstone; 1983.
53. Joynt RL, Benton AL, Fogel ML. Behavioral and pathological correlates of motor impersistence. Neurology. 1964;12:876.
54. Kernodle MW, Carlton LG. Information feedback and the learning of multiple-degree-of-freedom activities. J Mot Behav. 1992;24(2):187-196.
55. Kralj A, Jaeger RJ, Munih M. Analysis of standing up and sitting down in humans. definitions and normative data presentation. J Biomech. 1990:23;11:1123-1138.
56. Krefting LH, Krefting D. Cultural influences on performance. In: Christiansen C, Baum C, editors. Occupational therapy: overcoming human performance deficits. Thorofare, NJ: Slack, 1991.
57. Lach HW. Incidence and risk for developing fear of falling in older adults. Public Health Nursing. 2005;22(1):45-52.
58. Lavery JJ, Suddon FH. Retention of simple motor skills as a function of the number of trials by which KR is delayed. Percept Mot Skills. 1962;15:231-237.
59. Levine RE. Culture. a factor influencing the outcomes of occupational therapy. Occup Ther Health Care. 1987:4;1:3.
60. Mackenzie L, Byles J, Higginbotham N. Designing the home falls and accidents screening tool (home fast); selecting the items. Brit J Occup Ther. 2000;63(6):260-269.
61. Macrae AW, Holding DH. Method and task in motor guidance. 1965;8(3):315-320.
62. Messier S, Bourbonnais D, Desrosiers J, Roy Y. Dynamic analysis of trunk flexion after stroke. Arch Phys Med Rehabil. 2004;85(10):1619-1624.
63. Mohr JD. Management of the trunk in adult hemiplegia. the Bobath concept, topics in neurology. Alexandria, VA: American Physical Therapy Association. 1990.
64. Mosey AC. Psychosocial components of occupational therapy. New York: Raven; 1986.
65. Nelson DL, Melville LL, Wilkerson JD, et al. Interrater reliability, concurrent validity, responsiveness, and predictive validity of the Melville-Nelson Self-Care Assessment. Am J Occup Ther. 2002;56(1):51-59.
66. Nyberg L, Gustafson MD. Patient falls in stroke rehabilitation. a challenge to rehabilitation strategies. Stroke. 1995:26;5:838-842.
67. Podsiadlo D, Richardson S. The timed “Up & Go”. a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991:39;2:142-148.
68. Poole JI. Application of motor learning principles in occupational therapy. Am J Occup Ther. 1991;45(6):531-537.
69. Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. J Gerontol. 1995;50A(1):M28-M34.
70. Rein Tideiksaar. Falls in older persons. prevention and management, 2nd ed. Baltimore: Health Proffessions Press. 1998.
71. Richter RR, Van Sant AF, Newton RA. Description of adult rolling movements and hypothesis of developmental sequences. Phys Ther. 1989;69(1):63-71.
72. Roerdink M, Geurts AC, de Haart M, Beek PJ. On the relative contribution of the paretic leg to the control of posture after stroke. Neurorehabil Neural Repair. 2009;23(3):267-274.
73. Ryerson S, Levit K. Functional movements reeducation. New York: Churchill Livingstone; 1997.
74. Sabari JS. Motor learning concepts applied to activity-based interventions with adults with hemiplegia. Am J Occup Ther. 1991;45(6):523-530.
75. Schmidt RA. Motor learning principles for physical therapy. In: Lister MJ, editor. Contemporary management of motor control problems: proceedings of the Second STEP Conference. Alexandria, VA: Foundation for Physical Therapy, 1991.
76. Schmidt RA, Lee TD. Motor control and learning. a behavioral emphasis, ed 2. Champaign, IL: Human Kinetics. 1999.
77. Schmidt RA, Lee TD. Motor control and learning. a behavioral emphasis, ed. 4. Champaign, IL: Human Kinetics. 2005.
78. Schmidt RA, Wulf G. Continuous concurrent feedback degrades skill learning. implications for training and simulation. Hum Factors. 1997;39:509-525.
79. Shea JB, Morgan RL. Contextual interference effects on the acquisition, retention, and transfer of a motor skill. J Exp Psychol Learn Mem Cogn. 1979;5:179.
80. Shenkman M, Berger RA, Riley PO, et al. Whole-body movements during rising to standing from sitting. Phys Ther. 1990;70(10):638-648.
81. Shepherd RB, Gentile AM. Sit-to-stand. functional relationship between upper body and lower limb segments. Hum Move SCI. 1994:13;6:817.
82. Shepherd RB, Hirschorn AD. Standing up and sitting down at two different seat heights. Tokyo: Proceedings of the sixteenth International Society of Biomechanics Congress; 1997.
83. Shumway-Cook A, Woollacott MH. Motor control. theory and practical applications, ed 2. Baltimore: Lippincott Williams & Wilkins. 2001.
84. Shumway-Cook A, Woollacott MH. Motor control. translating research into clinical practice, ed 3. Baltimore: Lippincott Williams & Wilkins. 2007.
85. Sullivan PE, Markos PD, Minor MD. An integrated approach to therapeutic exercise. theory and clinical application. Reston, VA: Reston. 1982.
86. Tham K, Tegnér R. Video feedback in the rehabilitation of patients with unilateral neglect. Arch Phys Med Rehabil. 1997;78(4):410-413.
87. Tinnetti ME. Performance-oriented assessment of mobility in elderly patients. J Am Geriatr Soc. 1986;34(2):119-126.
88. Tinetti M, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):239.
89. Toglia J. Generalization of treatment. a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther. 1991:45;6:505-516.
90. VanSant A. Life-span development in functional tasks. Phys Ther. 1990;70(12):788-798.
91. Winstein CJ. Knowledge of results and motor learning-implications for physical therapy. Phys Ther. 1991;71(2):140-149.
92. Winstein CJ, Gardner ER, McNeal DR, et al. Standing balance training. effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil. 1989:70;10:755-762.
93. Winstein CJ, Pohl PS, Lewthwaite R. Effects of physical guidance and knowledge of results on motor learning. support for the guidance hypothesis. Res Q Exerc Sport. 1994:65;4:316-323.
94. Winstein CJ, Schmidt RA. Reduced frequency of knowledge of results enhances motor skill learning. J Exp Psychol Learn Mem Cogn. 1990;16(4):677-691.
95. Winzeler-Mercay J, Mudie H. The nature of the effects of stroke on trunk flexor and extensor muscles during work and rest. Disabil Rehabil. 2002;24(17):875-886.
96. World Health Organization. International classification of functioning, disability and health (short version). Geneva: The Organization; 2001.
97. Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older adults. Gerontologist. 2002;42(1):17-23.