Common Physical Care Problems of the Elderly
Upon completing this chapter, you should be able to:
1 Discuss five age-related common physical care problems of the elderly.
2 Identify three ways to promote mobility in the elderly.
3 List four ways for the elder to prevent falls in the home.
4 Review the physical and psychological consequences of chronic incontinence.
5 Discuss how multiple factors affecting the elderly may lead to an alteration in nutrition.
6 Explain techniques to facilitate communication and safety for the patient with a sensory deficit.
7 Recognize sexual concerns among the elderly population.
8 Identify five reasons why the elder is prone to the problem of polypharmacy.
9 Explain the effect of physical changes on the elderly person’s lifestyle.
1 Instruct a patient in how to prevent falls.
2 Formulate a plan to assist an elderly patient to decrease or prevent incontinence.
3 Teach an elderly patient specific ways to enhance nutritional status.
4 Assist a patient to develop a self-medication reminder system.
GETTING OLDER
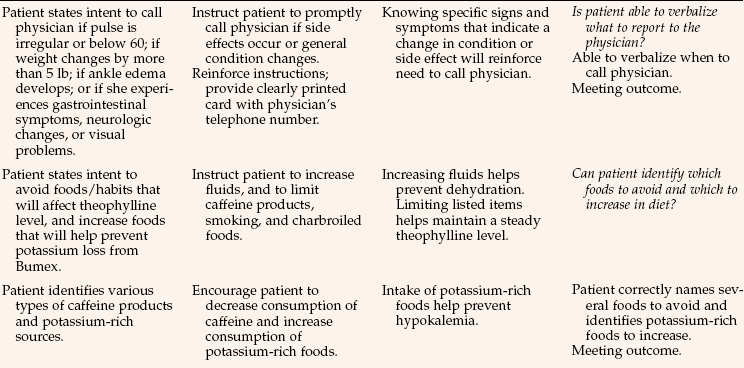
With aging, every body system undergoes some change that may not necessarily result in disease or illness, but will cause health problems to be more frequent (Table 40-1). Many of the physical problems, and nursing interventions to help them, are covered in the preceding chapters. This chapter reviews physical problems that are most common to the elderly and nursing interventions to assist the elder to attain an optimal level of function.
Table 40-1
Summary of Common Physiologic Changes with Aging
Modified from Kenney, P.A. (1982). Physiology of Aging: A Synopsis. Chicago: Year Book Medical Publishers; Shock, N.W., et al. (1984). Normal Human Aging: The Baltimore Study of Aging. NIH pub. no. 84-2450. Washington, DC: U.S. Government Printing Office; Timiras, P. (2002). Physiological basis of Aging and Geriatrics, New York: CBC Press; Beers, M.H., & Berkow, R. (Eds.), (2000). The Merck Manual of Geriatrics (3rd ed.). Whitehouse Station, NJ: Merck Research Laboratories.
Five of the most common physical care problems that plague the elderly population are (1) impaired mobility; (2) alteration in elimination (urinary incontinence, constipation, and fecal impaction); (3) alteration in nutrition; (4) sensory (vision and hearing) deficits; and (5) polypharmacy. Sexuality concerns are also addressed. Table 40-2 presents the causes of and contributing factors that add to these problems. Additional chronic illnesses such as Parkinson’s disease, arthritis, emphysema, or cardiac disease may compound these problems. Information on these chronic illnesses may be found in a medical-surgical nursing textbook.
Table 40-2
Common Physical Care Problems of the Elderly
| PHYSICAL CARE PROBLEM | EFFECT OF AGING ON SYSTEM | OTHER CONTRIBUTING FACTORS/DISEASES |
| Impaired mobility | Major loss of calcium, decreased bone density, decreased muscle mass, loss of joint flexibility | Osteoporosis, falls, gout, foot problems, obesity, arthritis, cardiac/respiratory disease, depression, neurologic disorders (e.g., multiple sclerosis) |
| Urinary incontinence | Altered sphincter control, loss of bladder muscle tone, enlarged prostate, cystocele, rectocele, uterine prolapse, diminished kidney function | Immobility, neurologic disorder (e.g., stroke), urinary tract infection, urinary retention |
| Constipation | Decreased bowel motility | Immobility, decreased abdominal musculature, insufficient fluid/fiber in diet, hemorrhoids, diverticulosis, depression, nervous system disorders, cognitive impairment, poor dentition, pain medications (e.g., codeine), other medications (e.g., antidepressants and anticholinergics) |
| Alteration in nutrition | Diseased teeth, poorly fitting dentures, decline in taste buds, decline in sense of smell, dysphagia | Neurologic deficit (e.g., stroke), impaired vision, impaired mobility, anorexia, lack of income/transportation/facilities, dementia, alcohol abuse, depression, taste alterations (e.g., cancer therapy), multiple medications |
| Vision deficit | Presbyopia, age-related macular degeneration, glaucoma, cataracts | Inadequate income for eye care, diabetes, arteriosclerosis, long-term steroid use |
| Hearing deficit | Presbycusis, tinnitus, otosclerosis | Long-term exposure to loud noise, heredity, Meniere’s disease, labyrinthitis |
| Polypharmacy | Affects multiple systems | Impaired senses, multiple chronic disorders, impaired cognitive functioning, forgetfulness, multiple physicians prescribing, borrowing drugs from others, use of multiple pharmacies, miscommunication/lack of education, use of over-the-counter medications |
IMMOBILITY
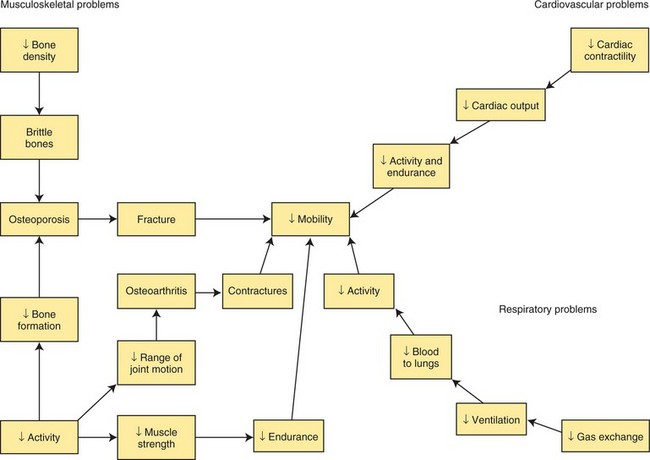
Decreased mobility often leads to numerous complications for the elderly. An acute health condition requiring bed rest may cause further immobility and, consequently, various other problems associated with immobility (see Chapter 39). Diseases that interfere with adequate circulation and oxygenation contribute to activity intolerance and immobility (Concept Map 40-1). For the person with such a problem, personal hygiene, eating, and socializing become too difficult because of exhaustion. Poor nutrition may result from immobility or the lack of energy to obtain or prepare food.
NURSING INTERVENTIONS TO PROMOTE MOBILITY
By immediately addressing mobility needs, you can often quickly get the patient back to her former level of activity, and avoid potential complications. The elderly need to be educated about engaging in activity throughout life that will help maintain optimal mobility (Health Promotion Points 40-1). It has been proven that walking 30 minutes a day is very beneficial, but doing this even three times a week is better than not walking at all. Strength training with resistance devices, using free weights or weight machines such as Nautilus, can help prevent muscle wasting, maintain bone density, and improve balance and walking endurance for elders even in their 90s. Dancing, gardening, home maintenance, and swimming can also promote mobility.
Participating in craft activities and arthritis programs can assist with preservation of fine motor movement. Proper treatment for arthritis and osteoporosis will help prevent immobility problems. Estrogen replacement therapy (ERT) and adequate dietary or supplemental calcium and vitamin D in combination with weight-bearing exercise are protective against osteoporosis in women. However, ERT’s potential side effects make its use controversial. Drugs such as alendronate sodium (Fosamax), risedronate sodium (Actonel), ibandronate sodium (Boniva), calcitonin-salmon (Miacalcin), and raloxifene hydrochloride (Evista) can help rebuild bone or stop its loss. Anti-inflammatory drugs such as nabumetone (Relafen) or diclofenac sodium (Voltaren) can also help maintain mobility. Etanercept (Enbrel), an immunomodulator, may be used for those patients with rheumatoid arthritis if they have poor response to other treatment.
The period of confined bed rest during illness needs to be as limited as possible. Merely transferring a patient from the bed to a chair has beneficial effects. Teach the bed rest patient active range-of-motion (ROM) activities and isometric exercises (applying pressure against resistance). An example of isometric exercise is instructing the patient to push into the bed with her hands and attempt to lift her hips, while sitting up in bed. If the patient is incapable of performing these exercises, assist with passive ROM exercises to maintain joint flexibility and help prevent muscle wasting. If the elderly patient is noncommunicative, assess for pain using the guidelines in Chapter 31 prior to attempting a ROM program.
With hospital stays so short, every effort to restore the patient to her maximum mobility potential should begin as soon as possible. When it is medically indicated, ambulate the patient with assistance. Make sure that appropriate assistance devices such as sturdy footwear, eyeglasses, walkers, and canes are brought from home. If the individual is too weak, seek a physical therapy (PT) referral. Such rehabilitative services are essential to promote quality of life for the elderly.
The nursing home setting allows the nurse to monitor and promote mobility over an extended period of time. All patients should be considered for assisted ambulation unless an underlying condition/illness (paralysis, severe cardiac disease) prevents it. The elder who is not ambulated will deteriorate and eventually be unable to walk. Although staff may be reluctant to encourage ambulation of a resident with an unsteady gait, many patients would rather risk a fall than be placed in a wheelchair. You may have to weigh the risk of the elder falling versus the negative effects of prolonged immobility.
PREVENTING FALLS
Falls are one of the most common safety problems for the elderly. Approximately one third of those over 65 years old and one half of those over 80 fall each year. Falls may not always result in serious injury; however, hip fractures are a leading cause of hospitalization and placement in long-term care facilities, with approximately 309,500 hip fractures reported annually (Centers for Disease Control and Prevention, 2006). Falls are the most common cause of traumatic brain injuries and accounted for 46% of falls that are fatal among older adults (Centers for Disease Control and Prevention, 2007).
Once an older person has fallen, there is the fear of falling again. This may cause limitation of activities and increased risk for the harmful effects of immobility. Caregivers and family members may also place restrictions on mobility and limit activities to prevent another fall.
Changes in the elder’s posture, balance, gait, and vision contribute to the risk of a fall (Health Promotion Points 40-2). Environmental factors such as clutter in walking areas, inadequate lighting or glare, improper footwear, and unsafe furnishings such as scatter rugs predispose to falls.
Medications frequently contribute to falls. With each additional medication consumed, the risk of falls is increased. Sedatives, hypnotics, and tranquilizers can decrease alertness and reaction time. Diuretics, antihypertensives, and antihistamines increase the risk of postural (or orthostatic) hypotension (unusually low blood pressure upon standing), which may cause the patient to become light-headed and fall (Safety Alert 40-1).
Most falls occur in the bedroom or bathroom. The home environment should be assessed to see how the patient navigates in these areas during activities of daily living. The patient and family should be educated about risk factors and made aware of measures to avoid falls. If the patient is cognitively impaired, a toileting schedule may be used to discourage self-toileting and a potential fall. Patients who unsafely attempt these actions should not be left unobserved for extended periods of time. The use of a mobility alarm can alert the staff that the patient has attempted to move unassisted.
Elderly patients need to be moved slowly out of bed to prevent possible orthostatic hypotension. Elastic support stockings may help prevent or lessen such hypotension. They should use appropriate footwear. A gait belt should be used until independent ambulation is established. Assistance devices, such as a cane or walker that can provide a wider base of support and increase stability, may be needed.
The call bell should be readily available to the patient who is in bed, in a chair, or in the bathroom. Beds should be in the low position with brakes engaged, unless a caregiver is at the bedside. Bells should be answered promptly to avoid unsafe attempts to stand or walk. Health care team members need to remember to keep walking paths clear, adjust lighting, and wipe up spills from the floor as soon as they are noticed.
Protective devices should be used only when there is a documented reason and only after the patient or her guardian has given permission, and they are ordered by the physician. This includes vest or waist devices, safety belts, and geri-chairs. Federal Omnibus Budget Reconciliation Act (OBRA) regulations are very specific about when and what types of devices are permissible. Check the guidelines at your place of employment and follow policy.
Both the patient and significant others need to be taught about hazards in the home and how to prevent falls in the home. If the individual is being discharged from the hospital and lives alone, a referral may be made for a member of the health care team to assess the home for potential safety hazards. Family members and significant others need to be encouraged to make regular visits to the elder’s home to check for unsafe conditions (Health Promotion Points 40-3).
Discourage the elderly from climbing a ladder or standing on a chair to reach high places. If a person needs to reach a high area, a stepstool with a broad base of support should be used. If balance is unsteady, the individual should be instructed not to reach for objects above head level. Devices to assist with reaching can be purchased to avoid the temptation to reach overhead.
ALTERATION IN ELIMINATION
Incontinence is one of the most common reasons that elder adults are institutionalized. Families who cope with other health problems are often unable to deal with incontinence. Embarrassment, social withdrawal, depression, and low self-esteem are common for the elderly patient who is incontinent.
Urinary incontinence is not a normal consequence of aging. Incontinence can be the result of an acute condition or a chronic problem. Approximately 30% of community-dwelling elders and more than 50% of nursing home residents are incontinent of urine (Palmer & Newman, 2004). Causes and treatment of incontinence are presented in Chapter 29. Temporary incontinence may develop as a result of an acute illness. If the patient is assisted to regain continence as soon as the acute episode is over, permanent incontinence can often be avoided. An underlying cause should always be sought when incontinence occurs. Bowel incontinence is not as common a problem and is covered in Chapter 30.
Nursing Interventions for Urinary Incontinence
Management of incontinence can be a frustrating problem for both patient and nurse. Incontinence is also costly; annual costs are estimated at $8.6 billion for care within the community and $3.8 billion for nursing home residents (Wilson et al., 2001). Treatment is based on the underlying cause and may include medication, such as oxybutynin chloride (Ditropan) or doxazosin mesylate (Cardura), to relax the smooth muscle of the bladder/prostate. Herbal approaches include the use of saw palmetto and pumpkin seeds, which can reduce prostate swelling (Banschbach, 2002). Treatment may also include surgery or behavioral interventions. Box 40-1 shows behavioral techniques commonly used with elders who experience urinary incontinence. Chapter 29 further describes training procedures, Kegel exercises, and nursing measures to reduce episodes of incontinence.
You can help prevent skin breakdown by keeping the patient who is incontinent clean and dry and by using a product such as Geri-Lav Free as a skin protector. The use of easy-release clothing, protective pads such as the DriStar system for women, and condom catheters such as the Pop-On for men can help hinder skin breakdown, avoid the soiling of bed and clothing, and prevent embarrassment for the patient. Encouraging fluids can decrease the urine concentration so it is less irritating, less predisposing to urinary tract infections, and less odoriferous.
Managing urinary incontinence depends not only on effective interventions, but also on a belief by the health care team that improvement is possible. A continence coordinator can be a valuable resource person in providing information and encouraging staff efforts in achieving patient goals.
CONSTIPATION AND FECAL IMPACTION
Constipation is a common problem among the elderly. Many older people believe anything other than a daily bowel movement is abnormal. Before deciding whether constipation is a problem, assess the frequency, amount, and consistency of stools as well as the possible contributing factors addressed in Chapter 30.
Fecal impaction can rapidly develop in the ill elder who, while on bed rest, is receiving pain medication and not eating a normal diet. Signs and symptoms may include abdominal cramping or rectal pain, abdominal distention, the passing of small amounts of liquid stool, and loss of appetite. Digital examination of the rectum often reveals a mass (Safety Alert 40-2). You need to check whether a physician’s order is required at your employing institution before performing this procedure.
Nursing Interventions for Constipation and Fecal Impaction
Along with the interventions covered in Chapter 30 for constipation, patient teaching should include specific diet remedies such as hot water and lemon juice first thing on arising, prunes, prune juice with carbonated drink, bran cereal or whole-grain breads, and roughage such as raw fruits and vegetables, as well as encouraging fluid intake of at least 2500 mL/day. Encourage an acceptable exercise program and advise the individual to heed the urge to defecate quickly to avoid a potential problem. Impacted stool may require manual removal. An oil-retention enema is ordered to soften stool before impaction removal.
ALTERATION IN NUTRITION
Nutritional needs of the elderly are discussed in Chapter 26. Although there is a decline in energy requirements as a person ages, there are no established recommendations for optimal nutrient intake for the elderly. The present Recommended Dietary Allowances (RDAs) reflect guidelines only for individuals to age 50 and do not consider requirements for additional nutrients as a result of decreased absorption, infection, or chronic illness.
It is recommended that the elderly reduce their sugar and fat intake and increase the roughage in their diet (Health Promotion Points 40-4). Controversy remains as to whether increased nutrients are needed. Some researchers suggest that an increase in whole-grain foods, fruits, and vegetables, as well as additional sources of protein, may help the elderly maintain proper nutrition. Table 40-3 displays dietary recommendations and rationales for the elderly individual. (Refer to MyPyramid for Older Adults in the Supplemental Image Collection on Evolve site http://elsevier.com/deWit/fundamental/.
Table 40-3
General Guidelines for Nutrient Needs of the Older Adult
| NUTRIENT | GENERAL GUIDELINE | RATIONALE/EXPLANATION |
| Calories | Average intake for men = 2000 kcal/day; average intake for women = 1600 kcal/day | Energy requirements tend to decrease with age. Health problems arise when intake totals <1500 kcal/day. |
| Protein | 1-1.25 g/kg, or 63 g/day for average-weight male and 50 g/day for average-weight female | 1 g/kg is needed to maintain a positive nitrogen balance. |
| Carbohydrate | 45%-65% of total daily calories from mostly complex carbohydrates | Impaired glucose tolerance may occur in the elderly if too many carbohydrates, especially simple ones such as sugars, are consumed. |
| Fat | At least 25%-35% of kcal/day | Mostly monounsaturated or polyunsaturated fats should be used. Animal fat intake should be very limited, as should intake of trans-fatty acids, because these tend to contribute to cardiovascular disease. |
| Calcium | 1500 mg/day for women and 1200 mg/day for men | Bone demineralization and osteoporosis are common among the elderly. |
| Vitamin D | 10-15 mcg/day (400-600 International Units/day) | Insufficient vitamin D results in bone demineralization. Sunlight provides vitamin D, but not when sunscreen is used. |
| Other vitamins and minerals | Nutrients should come from foods (i.e., 5-9 servings of fruits and vegetables per day). A multivitaminmineral tablet per day is recommended. | Vitamins and minerals are needed to maintain optimal nutritional status and health. Most elderly do not consume sufficient fruits and vegetables per day; therefore, a multivitamin-mineral tablet is recommended. |
| Water | 30-35 mL/kg per day; 1500 mL/day minimum intake | Elderly are very susceptible to dehydration. When fluid loss is excessive, water and electrolytes must be replaced. |
Adapted from Mahan, L.K., & Escott-Stump, S. (2008). Krause’s Food, Nutrition, and Diet Therapy (12th ed.). Philadelphia: Elsevier Saunders.
Obesity contributes to joint problems as well as being a risk factor for hypertension, heart disease, and stroke. Elders should adjust their caloric intake to coincide with their activity to maintain a weight that is within normal limits for their height and body build.
NURSING INTERVENTIONS FOR NUTRITIONAL SUPPORT
Meals can be made more enjoyable for the patient in a long-term care setting by serving the food in an attractive manner and by making the environment as pleasant as possible. Assess for social problems such as annoying table company, and then appropriately address the issue. A nutritionist can assist in determining the nutritional needs of the institutionalized patient. A liquid dietary supplement may be necessary to help the elderly patient meet dietary needs. Tube feedings and parenteral feedings may have to be used if attempts at oral feedings fail. Patients with dysphagia (difficulty swallowing) are at high risk for developing a nutritional deficit. These patients need to sit upright or in a high Fowler’s position and be fed very small amounts to avoid aspiration. Liquids may need to be thickened. The chin should be tucked when swallowing. The patient should remain in an upright position for 45 to 60 minutes after eating. Providing a stress-free environment is essential because stress can make dysphagia more pronounced.
SENSORY DEFICITS
Age-related eye changes can be debilitating if they are not recognized and corrected, and may result in a severe limitation of the patient’s overall independence. Visual accommodation (the ability to focus on near and far objects) decreases with age as a result of weakening of the muscles that control the lens. Beginning in their 40s, most people need bifocals or reading glasses to correct presbyopia (age-related decreased ability to focus on near objects) and to compensate for loss in accommodation.
The lens of the eye may yellow with age, causing a decline in color perception in the elderly. Because the iris has decreased ability to respond to light changes, the elder may experience difficulty adjusting from light to dark.
As the blood supply to the retina decreases, depth perception, peripheral vision, and night vision decrease. Any loss of peripheral vision should be further evaluated to rule out glaucoma. Glaucoma, a common disorder of the aging eye, is the accumulation of fluids inside the eye that exert pressure on the optic nerve, eventually causing blindness. It is often asymptomatic and a frequent cause of preventable blindness.
Frequently the elderly develop cataracts, a clouding of the lens. Cataracts occur to some extent in almost all elders, especially those with diabetes. Perhaps the most debilitating eye disorder is age-related macular degeneration, in which the elderly person gradually loses acute, central, and color vision. Unfortunately, there is no proven effective way to halt this disorder (Complementary & Alternative Therapies 40-1). Many medications, especially maintenance drugs such as oral hypoglycemics and thyroid replacement hormones, can affect vision. Thus a careful assessment of the patient’s medications, as discussed later in this chapter, is imperative.
Nursing Interventions for the Visually Impaired
Measures to enhance vision include the use of medications, surgery, and prosthetic devices. There are many degrees of vision loss, and interventions are geared to promote the individual’s maximum independence.
You must orient the patient to any new environment to avoid potential confusion and anxiety, as well as reduce the risk of accidents. The use of bright lights and bed rails and the removal of hazards in the room are imperative. All members of the health care team should be informed that the patient has a vision deficit. All persons should identify themselves on entering the patient’s room, and state when they are leaving to make sure the patient knows of their departure.
Do not rearrange the room or the patient’s personal belongings without permission or explanation. Speak before handing an object to her. To promote independence in eating, describe the positions of food on the plate in relation to clock position (e.g., 3 o’clock, 6 o’clock).
When walking with the patient with a visual impairment, offer your arm for guidance. It will be necessary to pause and explain any change in the environment, such as steps, to decrease fear of new surroundings.
For the patient with low vision, devices such as a closed-circuit TV system and the low-vision enhancement system (LVES) are available to magnify and light reading material. Telescopic lenses, TV screen magnifiers, large-print books, talking books, and large-number watches, clocks, and telephones all are examples of aids that can be beneficial. Bright, glare-free light may be necessary for the elderly person to move about safely. Night-lights may also be helpful. During the day, natural light may be preferable.
All interventions to assist with independence need to be explained to family members who may live with the elder at home. Additional teaching or referrals may be necessary for the person who is completely blind. A common concern is the visually impaired elder who continues to drive. This creates a psychosocial issue that involves not only the elder and family, but society as well. In coping with this concern, many states and provinces now require special testing before reissuing licenses to those over a certain age (ranging from 70 to 80 years of age). Individuals may be given limited licenses that restrict driving to specific distances and areas. Older persons who continue to drive must be encouraged to avoid night driving and to wear prescribed hearing aids or glasses to help enhance sensory awareness. The elder should also be advised not to drive under the influence of alcohol or drugs and to avoid driving in inclement weather to avoid a potential accident.
The use of sunglasses when outside and supplementation with vitamin and mineral antioxidants may help protect against macular degeneration. A diet rich in antioxidant foods such as beta-carotene (found in dark green leafy vegetables and deep orange vegetables and fruits), vitamin E (found in seeds, nuts, and wheat germ), and vitamin C (found in citrus fruits and dark green leafy vegetables) should be encouraged as a beneficial food choice.
HEARING DEFICIT
The inability to hear high-frequency sounds usually begins to become noticeable by late middle age. Presbycusis is the inability to hear high-pitched sounds and the inability to hear spoken words. This problem is often intensified with the presence of background noise. Tinnitus, or ringing in the ears, may also cause a further loss of hearing.
Presbycusis is commonly exacerbated by cerumen (earwax) accumulation. Removal of a wax impaction can make a significant difference in the elder’s hearing ability. It is of utmost importance to assess frequently if cerumen is contributing to the hearing loss. Products such as Debrox (carbamide peroxide) are effective in wax removal and can be periodically continued at home.
Hearing loss can lead to ongoing frustration and embarrassment for the individual. The person with a hearing deficit may complain of others mumbling, as well as have a reduced tolerance for loud noises. She may pretend to hear, when she really does not understand what has been communicated. This becomes an important concern when attempting to communicate about health-related issues. Hearing should be checked periodically.
Nursing Interventions for the Hearing Impaired
If the patient has a hearing aid, the nurse should know how to operate it. The hearing aid should be free from earwax and fit properly in the ear canal to function correctly. Chapter 19 describes how to care for the hearing aid. Periodic irrigation of the auditory canal to remove impacted cerumen is a high priority.
Communication with a person with a hearing loss can be difficult for both patient and nurse. Face the patient so she knows you are present, and speak clearly and distinctly in low tones, rephrasing sentences as needed (Figure 40-1). Facial expressions and gestures can be helpful in communicating messages. Conversations should take place in a well-lit area with minimal outside distractions. Speak toward the patient’s “good ear” if possible. If the patient wears glasses, they should be worn to aid in seeing facial expressions and to read lips. Environmental noise should be kept to a minimum to avoid confusion and improve the clarity of conversation. A pad and pencil can be used if messages are still unclear.

FIGURE 40-1 Communication with the elder with a vision or hearing deficit. Sit in front of the patient where your lips can be seen to communicate. Standing behind the patient causes miscommunication.
Family members may become frustrated with an elder who will not get a hearing aid, or who will not wear the hearing aid to communicate. As a result, the individual may gradually stop participating in conversation and become isolated. Work with patients and families to enhance communication techniques. Some patients may benefit from a cochlear implant.
SEXUALITY
In spite of the general view of the younger generation, the need for sexual expression does not disappear with age. People continue sexual activity into old age. Changing health status, age-related physical changes, and loss of a sex partner do have an effect on the sexual practices of the elderly. Sexual response time slows with age, but the ability to achieve orgasm continues. Sexuality may be difficult for you to discuss with an elderly patient, but it is an area that should be assessed. Try asking questions such as “Are you sexually active?” or “Are you happy with your sex life?” to begin an assessment.
The decreased levels of hormones may result in discomfort or pain (dyspareunia) during intercourse for the female. Thinning and dryness of the vaginal walls predispose to vaginitis. There may be an alteration in the numbers of normal microorganisms in the vagina that leads to a predisposition to vaginal yeast infection. Hormone replacement therapy (HRT) can help alleviate these issues, but because of the potential side effects of those medications, HRT must be closely monitored. Topical vaginal moisteners can be very helpful.
The elderly male may experience a slower sexual arousal. Erection is often less firm than when younger. It takes longer for the elderly male to reach an orgasm and there is less seminal fluid released. Diabetes may contribute to impotence. There are many resources available to help the male achieve erection. Sildenafil citrate (Viagra), vardenafil (Levitra), and tadalafil (Cialis) have been very successful in promoting a satisfying sex life for older men. Vacuum pumps, penile implants, and penile injections are other aids to achieve an erection. An elastic ring can help a man maintain an erection once it is achieved.
Chronic illness or disability may affect one partner or the other’s ability to participate in sexual activity. The nurse should explore other ways to help the couple express their sexuality and achieve sexual satisfaction.
A concern is the rise of human immunodeficiency virus (HIV) infection in the older heterosexual population. Elders don’t seem to think they need to practice safe sex since pregnancy is no longer an issue. It is imperative to teach about the dangers of unprotected sex and the possibility of the transmission of HIV and other sexually transmitted diseases. It is not uncommon for some elders to strike up a romance within an assisted living facility or a long-term care facility. The incidence of new cases of HIV among heterosexuals in the United States is greatest among the older population.
POLYPHARMACY
The greater the number of medications consumed by an individual, the greater the risk of undesirable reactions, drug interactions, and toxicity. Polypharmacy is the use of multiple medications, often inappropriately and excessively, at the same time. This often occurs when the patient sees multiple physicians and each is unaware of what the other is prescribing. Patients may use a local pharmacy and a mail-order pharmacy as well, so the pharmacist is unaware of all the drugs the patient is consuming. Individuals over 65 are the largest users of prescription and over-the-counter (OTC) drugs, and therefore are more likely to experience a polypharmacy situation (Figure 40-2).
In the older person, drug interactions and toxicity can result in behavioral or cognitive changes that may be mistaken for dementia. Unfortunately, when older persons experience adverse drug effects, these problems are often overlooked, inappropriately blamed on the aging process, or treated with yet another medication.
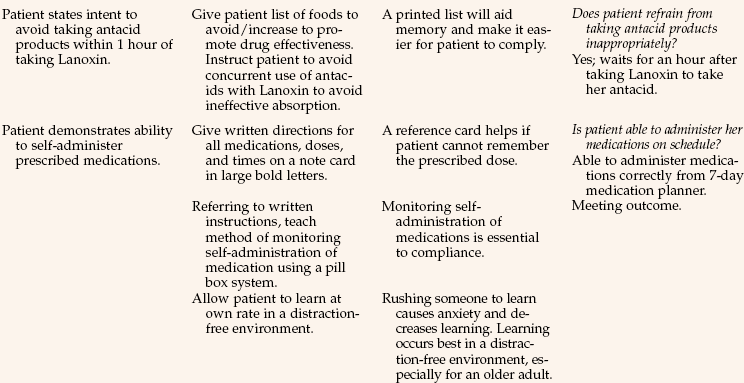
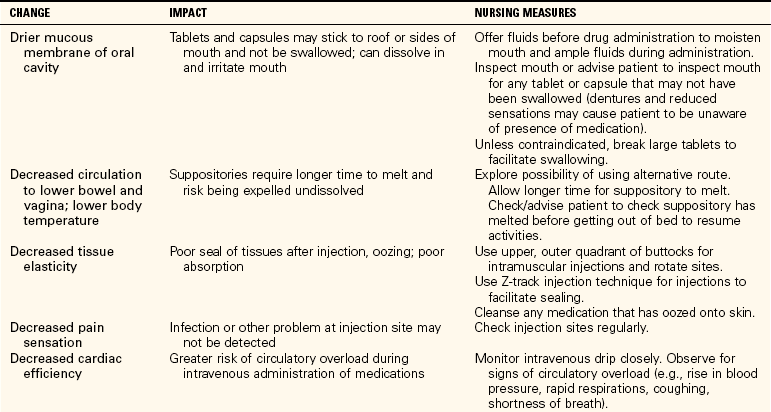
Many factors related to aging alter the rate at which drugs are metabolized and excreted in the elderly person. Absorption, storage, and serum binding factors all affect the way a drug is used within the body. Decreased body water, increased ratio of fat to muscle, and a low serum albumin all predispose the patient to drug toxicity and extended duration of action of drugs (Table 40-4). Alterations in enzyme function, cardiac output, and circulatory function can reduce blood flow to the liver. These changes decrease the liver’s effectiveness and speed in metabolizing drugs. As most drugs are metabolized in the liver, the risk of toxicity increases. The risk for toxicity can significantly increase if the elder is malnourished because medications metabolize more slowly when the diet is inadequate.
Table 40-4
Age-Related Changes Affecting Drug Therapy in Older Adults
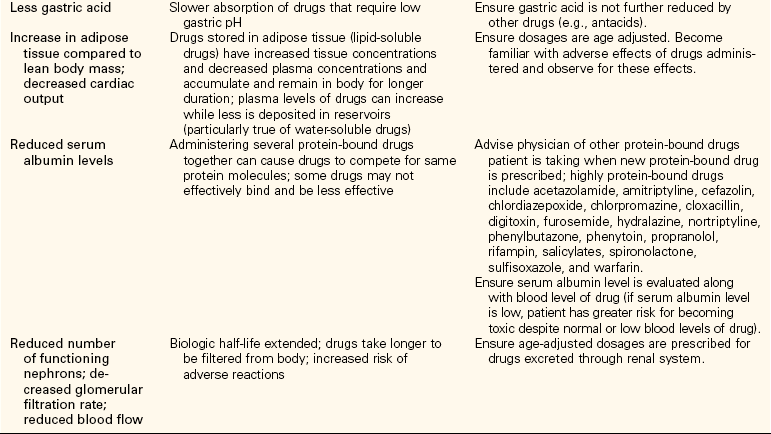
From Eliopoulos, C. Manual of Gerontologic Nursing (2nd ed.). St. Louis, 1999, Mosby.
Aging kidneys are significantly less effective in excreting drugs, resulting in elevated drug levels and symptoms of toxicity. Some medications, such as digoxin (Lanoxin), cause retention of other drugs in the presence of diminished renal function. The use of substances such as alcohol and nicotine can also cause changes in drug elimination in the elderly.
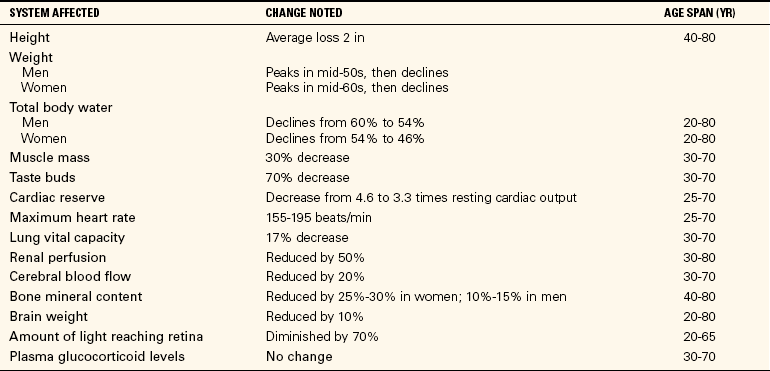
NURSING INTERVENTIONS FOR POLYPHARMACY
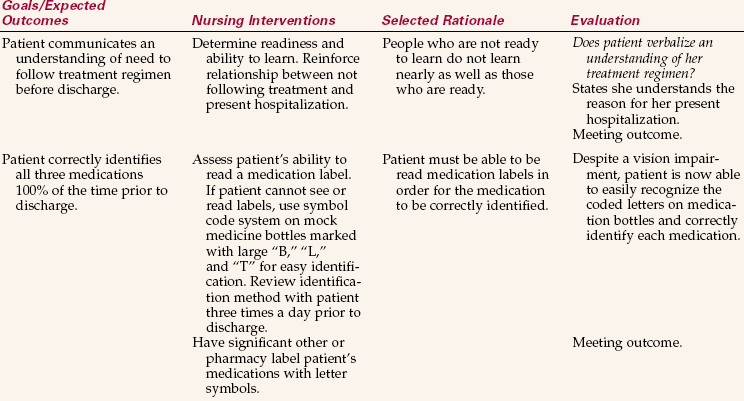
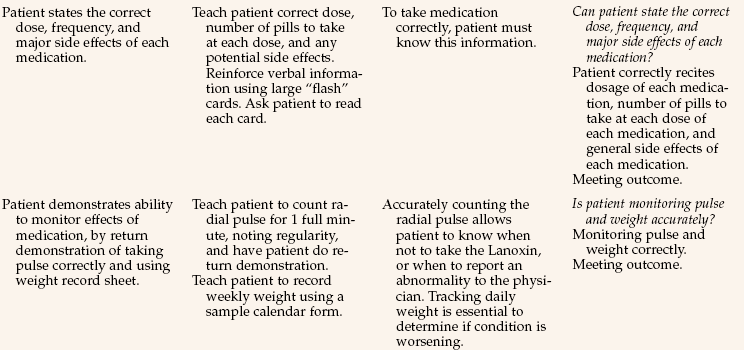
A thorough medication history is the initial step in preventing polypharmacy. A comprehensive assessment can help maintain a therapeutic medication regimen, identify educational needs, eliminate unnecessary medications, and reduce the risk of adverse drug reactions (Nursing Care Plan 40-1). Specifically, questions should be asked that provide information about the patient’s current prescriptions, OTC drugs, and any vitamins and herbal preparations being taken. Ask the patient to bring a bag with all the drugs she takes at home. Assessment data should also include the patient’s current administration schedule, knowledge about her medications, medication-related problems, noncompliance problems, frequency of physician visits, sensory deficits, mental and physical disabilities, ability to purchase and obtain medication, and the use of alcohol and caffeine. Ideally, a pharmacist or physician should address these questions. However, the nurse should be prepared to assess the patient’s drug history initially as well as continue to gather information so that a therapeutic medication regimen may be maintained.
In a long-term care facility, it is imperative to assess continually the number of medications, side effects, and the necessity for each being administered to avoid a potentially dangerous situation (Assignment Considerations 40-1).
You should attempt to reduce the complexity of the medication regimen by improving self-medication practices. Developing a drug reminder system and a schedule that is appropriate or compatible with the individual’s lifestyle can help decrease confusion and increase compliance. A referral to a home health nurse can provide for monitoring of compliance at home. A frequently used medication reminder system is the daily/weekly pill container that is available at pharmacies. A homemade egg carton container may be substituted for the elder affected with arthritic hands. Other reminder tactics can include the use of check-off systems, calendars, color- or symbol-coded medication bottles, an alarm clock, or a voice-mail system. The use of cueing with daily events such as brushing teeth can also be helpful to promote compliance.
NCLEX-PN® EXAMINATION–STYLE REVIEW QUESTIONS
Choose the best answer(s) for each question.
1. Prevention of mobility problems in the elderly can be addressed by encouraging: (Select all that apply.)
1. maintaining a normal weight.
2. treating arthritis pain adequately.
2. Factors that may contribute to falls in the elderly are: (Select all that apply.)
3. One of the most common reasons that elder adults are placed in long-term care facilities is:
4. Dietary substances that help prevent constipation include: (Select all that apply.)
5. Dietary recommendations for the elderly include:
1. between 50 and 63 g/day of protein.
2. 2000 to 2600 calories per day.
6. The elder with a sensory impairment as a result of the aging process may:
1. experience an abrupt awareness of the sensory loss.
2. be subject to safety problems.
7. Measures to try to prevent the development of macular degeneration include:
1. wearing sunglasses and a diet of antioxidant foods.
2. wearing sunglasses and a diet low in calcium oxidate.
8. Drug toxicity occurs more easily in the elderly due to: (Select all that apply.)
9. Drug use assessment to identify concerns related to polypharmacy should include:
10. The condition most likely to cause a vision loss in the elderly is ________________________________. (Fill in the blank.)
 ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,  ,
,