Periodontal Diseases
Several distinct yet related disorders of the periodontium are collectively known as periodontal diseases. They are a set of conditions characterized by an inflammatory host response in the periodontal tissues that may lead to localized or generalized alterations in the soft tissues around the teeth, loss of supporting bone, and ultimately, loss of the teeth. Periodontal diseases are broadly classified as gingival diseases and periodontitis. Gingival diseases may be dental plaque-induced or non–plaque-induced. Bacterial plaque-associated gingivitis is much more common than non–plaque-induced inflammatory diseases affecting the gingiva such as viral or fungal infections, mucocutaneous and allergic conditions, and traumatic injuries. Gingivitis presents as inflammation of the soft tissue surrounding the teeth with gingival swelling, edema, and erythema.
Periodontitis is classified, primarily by the clinical presentation, as chronic, aggressive, and periodontitis as a manifestation of a systemic disease. Other subtypes of periodontal conditions include necrotizing periodontal diseases, periodontal abscesses, and periodontitis associated with endodontic lesions. Periodontitis is distinguished from gingivitis by the clinically detectable destruction of host tissues seen as the loss of soft tissue attachment and supporting bone of the involved teeth. Although periodontitis is always preceded by gingivitis, gingivitis does not always progress to periodontitis.
Dental plaque, which may vary greatly in its bacterial composition, plays a primary role in the initiation of periodontitis. Periodontitis-implicated plaque bacteria species, predominantly gram-negative rods and spirochetes, have the ability to colonize on the tooth and root surfaces, spread into the region between the root and the gingival margin, and in some cases invade the surrounding tissue. These bacteria are capable of causing damage to the host tissue either directly, through the release of toxins, or more significantly, indirectly, by stimulating a host inflammatory reaction. As part of the host response, the release of inflammatory mediators, especially from neutrophils, is responsible for much of the injury to the surrounding soft tissue and stimulation of osteoclastic bone resorption. The resulting inflammatory response causes loss of, and apical migration of, the epithelial attachment, resulting in pocket formation and thus further enhancing bacterial colonization.
The clinical manifestation of this interplay between bacterial plaque and the host tissues are clinical signs of inflammation. Gingivitis seen as gingival swelling, edema, and erythema is the most common first clinical sign. Progression to periodontitis is manifested with pocket formation, the universal presentation of this disease. Other clinical signs include bleeding, purulent exudate, edema, resorption of the alveolar crest, and tooth mobility. Rather than progressing smoothly from mild to moderate to severe, periodontitis often progresses in bursts. There are active periods of inflammation and tissue destruction followed by healing and quiescent periods (often years) of no appreciable change. The extent of disease activity is best measured by longitudinal probing of periodontal attachment level. This cycle of disease activity may repeat. The relative duration of the destructive and quiescent phases depends on the form of periodontitis, the nature of the bacterial pathogens, and the host response. Host factors such as systemic disease, age, genetic predisposition, immune system status, occlusal trauma, and stress influence the onset and progression of the disease. Spontaneous remission of the destructive process may even occur. The disease usually is painless, and most patients are unaware of its presence. Various forms of therapy are effective, including oral hygiene, scaling, and surgical treatment.
Those more prone to periodontal disease include smokers, older individuals, and people with poor education, neglected dental care, previous periodontal destruction, and systemic diseases such as diabetes or infection with human immunodeficiency virus.
The prevalence of periodontal disease in the American population depends on the method of assessment and the threshold used. If loss of attachment by the formation of pockets measuring greater than 4 mm is used, then the prevalence is about 23%. The incidence of adult periodontitis increases with age. The prevalence of aggressive periodontitis is less than 1%. It also appears that the prevalence of periodontal disease in the United States has declined in the last 30 years, but this may change with an increasing elderly population and an increase in retention of teeth.
Assessment of Periodontal Disease
Radiographs play an integral role in the assessment of periodontal disease. They provide unique information about the status of the periodontium and a permanent record of the condition of the bone throughout the course of the disease. Radiographs aid the clinician in identifying the extent of destruction of alveolar bone, local contributing factors, and features of the periodontium that influence the prognosis. Important features related to periodontal status that may be identified radiographically are listed in Box 18-1.
It is important to emphasize that the clinical and radiographic examinations are complementary. The clinical examination should include periodontal probing, a gingival index, mobility charting, and an evaluation of the amount of attached gingiva. Features that are not well delineated by the radiograph are most apparent clinically, and those that the radiograph best demonstrates are difficult to identify and evaluate clinically. Radiographs are an adjunct to the diagnostic process. Although a radiograph demonstrates advanced periodontal lesions well, other equally important changes in the periodontium may not be seen radiographically. Therefore a complete diagnosis of periodontal disease requires insight from a clinical examination of the patient combined with radiographic evidence.
LIMITATIONS OF RADIOGRAPHS
Radiographs may provide an incomplete presentation of the status of the periodontium. They have the following limitations:
1. Radiographs provide a two-dimensional view of a three-dimensional situation. Because the radiographic image fails to reveal the three-dimensional structure, bony defects overlapped by higher bony walls may be hidden. Also, because of overlapping tooth structure, only the interproximal bone is seen clearly. However, subtle changes in the density of the root structure (which is more radiolucent) may indicate bone loss on the buccal or lingual aspect of the tooth. Furthermore, use of multiple images made at different angulations, as in a full-mouth set, allows the viewer to use the buccal object rule to obtain three-dimensional information such as whether cortical plate loss has occurred on the buccal or lingual aspects.
2. Radiographs typically show less severe bone destruction than is actually present. The earliest (incipient) mild destructive lesions in bone do not cause a sufficient change in density to be detectable.
3. Radiographs do not demonstrate the soft-tissue-to-hard-tissue relationships and thus provide no information about the depth of soft tissue pockets.
4. Bone level is often measured from the cementoenamel junction; however, this reference point is not valid in situations where there is overeruption or where there is severe attrition with passive eruption.
For these reasons, although radiographs play an invaluable role in treatment planning, their use must be supplemented by careful clinical examination.
Technical Procedures
The usefulness of radiographs in the evaluation of periodontal disease can be improved by making radiographs with high technical quality. Interproximal (bitewing), in some cases vertical bitewings, and periapical radiographs are useful for evaluating the periodontium. This material is covered in greater detail in the chapters on projection geometry and intraoral radiographic technique (Chapters 4 and 9, respectively), but the features that are particularly important for imaging the alveolar bone are emphasized here.
FILM PLACEMENT AND BEAM ALIGNMENT
The film should be placed parallel with the long axis of the teeth or as near to this ideal position as the size and structure of the mouth permit. The x-ray beam is directed perpendicular to the long axis of the tooth and the plane of the film. These measures result in the best undistorted images of the teeth and periodontal tissues. Interproximal (bitewing) images more accurately record the distance between the cementoenamel junction (CEJ) and the crest of the interradicular alveolar bone because with interproximal views the beam is oriented at right angles to the long axis of the teeth, thus providing an accurate view of the relationship of the height of the alveolar bone to the roots. Periapical views, especially in the posterior maxilla, may present a distorted view of the relationship between the teeth and the height of the alveolar bone because the presence of the hard palate often requires the x-ray tube to be oriented slightly downward toward the posterior teeth to see the apices of these teeth. In this circumstance, the level of the buccal alveolar bone may be projected near or even above the level of the lingual CEJ, thus making the bone height appear greater than it actually is.
The teeth will be depicted in their correct positions relative to the alveolar process when there is (1) no overlapping of the proximal contacts between crowns, (2) no overlapping of roots of adjacent teeth, and (3) overlapping of the buccal and lingual cusps of molars.
In recent years some periodontists have recommended the use of vertical interproximal radiographs for patients with periodontal disease. This method uses seven No. 2 films as vertical interproximal radiographs to cover the molar, premolar, canine, and midline regions. These views have the advantageous orientation of the interproximal views yet show the alveolar bone level even when bone loss has been considerable. Panoramic radiographs are not recommended for evaluation of periodontal disease because the distortion and poor image detail of panoramic views tend to lead the clinician to underestimate minor marginal bone destruction and overestimate major destruction.
For radiography of the alveolar bone, a beam energy of 80 kVp should be used. Films that are slightly light are more useful for examining cortical margins of bone. A properly collimated beam reduces scattered radiation and improves image definition.
SPECIAL CONSIDERATIONS AND TECHNIQUES
The dentist must determine the optimal frequency of radiographic examination for patients with periodontal disease. Certainly, radiographs of all diseased areas must be available at the beginning of periodontal therapy to allow treatment planning and provide a baseline for later comparisons. The extent of continued disease activity, which can be determined clinically, should dictate the frequency of subsequent radiographic examinations.
Some clinicians have found it useful to superimpose fine wire grids when exposing radiographs to aid the measurement of relative bone height. Typically the grids form 1-mm squares (which show as fine, radiopaque lines on the resultant radiograph) that allow quantitative measurement of the position of the alveolar bone with respect to the dentition. This procedure can be useful in evaluating osseous changes over time but may be limited by difficulties in maintaining the same film position at subsequent examinations, resulting in variations in image geometry.
In recent years computers and image-processing techniques have been used to enhance radiographs to achieve improved detection of alveolar bone loss associated with periodontal disease. The most widely used of these techniques is subtraction radiography (see Chapters 7 and 14). The advantage of this method is that it allows better detection of small amounts of bone loss between radiographs made at different times than may be achieved by visual inspection. However, radiographic subtraction is difficult to use because the images must be made with the same orientation of the primary x-ray beam, bone, and film at each examination, which is impractical and difficult to accomplish in general practice. The more recent introduction of software programs that can correct for discrepancies in positioning and alignment in sequential digital images makes subtraction radiography more forgiving. Nonetheless, this diagnostic technique remains primarily a research tool.
Normal Anatomy
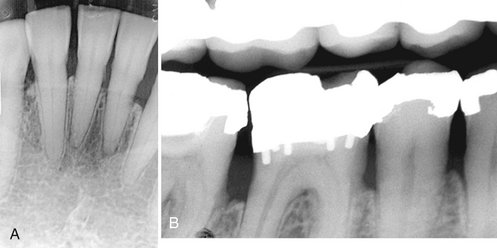
The normal alveolar bone that supports the dentition has a characteristic radiographic appearance. A thin layer of opaque cortical bone often covers the alveolar crest. The height of the crest lies at a level approximately 0.5 to 2.0 mm below the level of the CEJs of adjacent teeth. Between posterior teeth the alveolar crest also is parallel to a line connecting adjacent CEJs (Fig. 18-1). Between anterior teeth the alveolar crest usually is pointed and may have a well-defined cortex (Fig. 18-2). A well-mineralized cortical outline of the alveolar crest indicates the absence of periodontitis activity. However, lack of a well-mineralized alveolar crest may be found in patients with or without periodontitis.

FIG. 18-1 The normal alveolar crest lies 0.5 to 2.0 mm below the adjacent cementoenamel junctions and forms a sharp angle with the lamina dura of the adjacent tooth. Note that the crests may not always appear with a well-defined outer cortex.

FIG. 18-2 Between the anterior teeth, the normal alveolar crest is pointed and well corticated, coming to within 0.5 to 2.0 mm of the adjacent cementoenamel junctions.
The alveolar crest is continuous with the lamina dura of adjacent teeth. In the absence of disease, this bony junction between the alveolar crest and lamina dura of posterior teeth forms a sharp angle next to the tooth root. The periodontal ligament (PDL) space is often slightly wider around the cervical portion of the tooth root, especially in adolescents with erupting teeth. In this situation, if the lamina dura still forms a sharp, well-defined angle with the alveolar crest, the condition is a variant of normal and is not an indication of disease. The thickness of alveolar crests varies widely, and it may be very thin coronally. This may appear radiographically as an increase in radiolucency toward the crest. These sorts of variations in density alone are not an indication of disease and may be a variation of normal.
Because gingivitis is an inflammatory condition confined to the gingiva, there are no significant changes to the underlying bone and therefore the radiographic appearance of the bone is normal.
General Radiographic Features of Periodontal Disease
No matter the type of periodontal disease, the changes seen radiographically reflect changes seen with inflammatory lesions of bone. These changes can be divided into changes in the morphologyof the supporting alveolar bone and changes to the internal density and trabecular pattern. Changes in morphology become apparent as a result of loss of the interproximal crestal bone and bone overlapping the buccal or lingual aspects of the tooth roots. Changes to the internal aspect of the alveolar bone reflect either a reduction or an increase in bone structure or a mixture of both. A reduction is seen as an increase in radiolucency because of a decrease in number and density of existing trabeculae. An increase in bone is seen as an increase in radiopacity (sclerosis) as the result of an increase primarily in the thickness, density, and number of trabeculae. Similar to all inflammatory lesions of bone, periodontal disease usually has a combination of bone loss and bone formation or sclerosis. However, acute early lesions display predominantly bone loss, whereas chronic lesions have a greater component of bone sclerosis.
The following patterns of bone loss may be seen radiographically in the assessment of periodontitis.
CHANGES IN MORPHOLOGY OF THE ALVEOLAR BONE
The early lesions of chronic periodontitis appear as areas of localized erosion of the interproximal alveolar bone crest (Fig. 18-3). The anterior regions show blunting of the alveolar crests and slight loss of alveolar bone height. The posterior regions may also show a loss of the normally sharp angle between the lamina dura and alveolar crest. In early periodontal disease, this angle may lose its normal cortical surface (margin) and appear rounded off, having an irregular and diffuse border. Even if only slight radiographic changes are apparent, the disease process may not be of recent onset because significant loss of attachment must be present for 6 to 8 months before radiographic evidence of bone loss appears. Also, variations in angle of projection of the x-ray beam can cause a slight change in the apparent height of the alveolar bone. Small regions of bone loss on the buccal or lingual aspects of the teeth are much more difficult to detect.
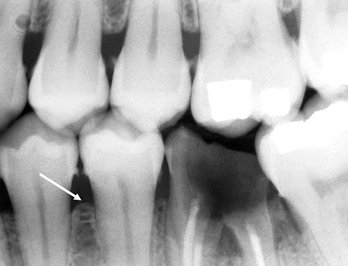
FIG. 18-3 Initial periodontal disease is seen as a loss of cortical density and a rounding of the junction between the alveolar crest and the lamina dura (arrow). Note also the more pronounced bone loss around the mandibular first molar and the generalized interproximal calculus.
A mild lesion does not necessarily develop into a more severe lesion later; however, if the periodontitis progresses, the destruction of alveolar bone extends beyond early changes in the alveolar crest and may induce a variety of defects in the morphology of the alveolar crest. These patterns of bone loss have been divided into horizontal bone loss, vertical (angular) defects, interdental craters, buccal or lingual cortical plate loss, and furcation involvement of multirooted teeth. The presence and severity of these bone defects may vary between patients and even within a patient. A radiograph is valuable in showing the extent and morphology of residual bone, but complete assessment of bone loss and the diagnosis and staging of periodontitis requires integration of the radiologic information with the results of a clinical examination.
Horizontal Bone Loss
Horizontal bone loss is a term used to describe the radiographic appearance of loss in height of the alveolar bone where the crest is still horizontal (i.e., parallel to an imagined line joining the CEJs of adjacent teeth) but is positioned apically more than a couple of millimeters from the CEJs. Horizontal bone loss may be mild, moderate, or severe, depending on its extent. Mild bone loss may be defined as approximately a 1- to 2-mm loss of the supporting bone, and moderate loss is anything greater than 2 mm up to loss of half the supporting bone height. Severe loss is anything beyond this point. Care must be taken in using the CEJ as a reference point in cases of overeruption and severe attrition (Fig. 18-4). With overeruption the alveolar bone will not necessarily remodel to keep a normal relationship to the CEJ and similarly in passive eruption, which may accompany severe attrition. Although in this case bone loss is not due to periodontitis, there may be still loss of attachment, which could be of clinical significance.
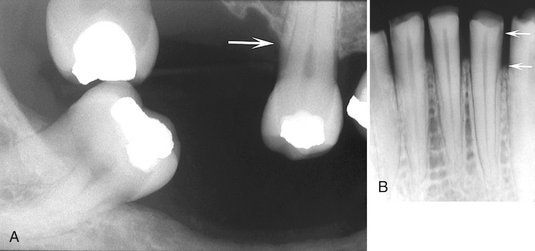
FIG. 18-4 A, This maxillary second bicuspid is overerupted; the etiology of the low bone level (arrow) relative to the cementoenamel junction (CEJ) is not necessarily the result of periodontal disease. Similarly, B is an example of passive eruption related to severe attrition, and the apparent increase in the distance from the CEJ to the bone height (arrows) cannot be attributed to periodontal disease. However, the resultant change in bone level relative to the CEJ may still be clinically significant.
In horizontal bone loss, the crest of the buccal and lingual cortical plates and the intervening interdental bone have been resorbed (Fig. 18-5). The extent of bone loss evident at a single examination does not indicate the current activity of the disease. For example, a patient who previously had generalized periodontal disease and subsequent successful therapy will likely always show bone loss, but the bone level may remain stable.
Vertical Bone Defects
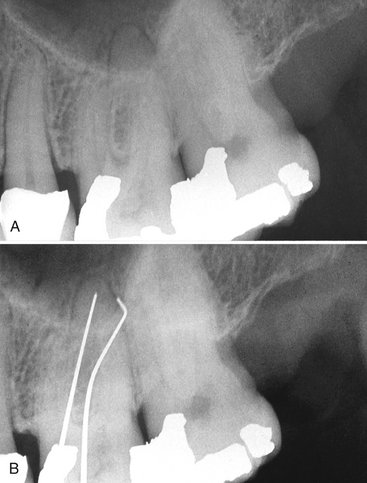
The term vertical (or angular) osseous defect describes a bony lesion that is localized to a single tooth, although an individual may have multiple vertical osseous defects. These defects develop when bone loss progresses down the root of the tooth, resulting in deepening of the clinical periodontal pocket. The radiographic presentation is a vertical deformity within the alveolus that extends apically along the root of the affected tooth from the alveolar crest. The outline of the remaining alveolar bone typically displays an oblique angulation to an imaginary line connecting the CEJ of the affected tooth to the neighboring tooth. In its early form, a vertical defect appears as abnormal widening of the PDL space at the alveolar crest (Fig. 18-6, A). The vertical defect is described as three walled (surrounded by three bony walls) when both buccal and lingual cortical plates remain; it is described as two walled when one of these plates has been resorbed and as one walled when both plates have been lost (Fig. 18-6, B). The distinctions among these groups are important in designing the treatment plan.
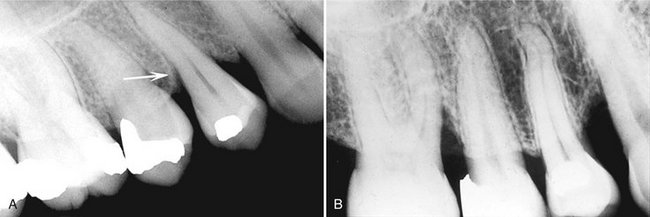
FIG. 18-6 A, Example of a developing vertical defect; note the abnormal widening of the periodontal ligament space (arrow). B, Maxillary periapical film reveals two examples of more severe vertical defects affecting the mesial surface of the first molar and the distal surface of the canine.
Often vertical defects are difficult or impossible to recognize on a radiograph because one or both of the cortical bony plates remain superimposed over the defect. Clinical and surgical inspections are the best means of determining the number of remaining bony walls. Visualization of the depth of pockets may be aided by inserting a gutta-percha point. The point follows the defect and appears on the radiograph because gutta-percha is relatively inflexible and radiopaque (Fig. 18-7).
Interdental Craters
The interproximal crater is a two-walled, troughlike depression that forms in the crest of the interdental bone between adjacent teeth. The buccal and lingual outer cortical walls of the interproximal bone extend further coronally than does the cancellous bone between them, which has been resorbed. Radiographically this presents as a bandlike or irregular region of bone with less density at the crest, immediately adjacent to the more dense normal bone apical to the base of the crater (Fig. 18-8). These defects are more common in the posterior segments, likely as a result of the broader buccal-lingual dimension of the alveolar crest in these regions.
Buccal or Lingual Cortical Plate Loss
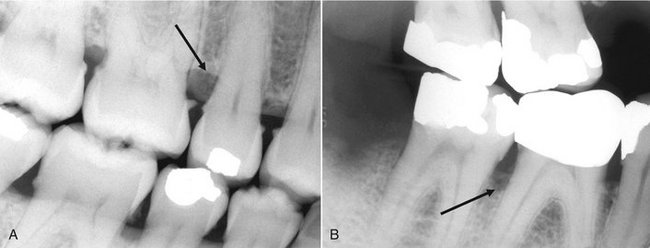
The buccal or lingual cortical plate adjacent to the teeth may resorb. Loss of a cortical plate may occur alone or with another type of bone loss such as horizontal bone loss. This type of loss is indicated by an increase in the radiolucency of the root of the tooth near the alveolar crest. The shape seen usually is a semicircular shadow with the apex of the radiolucency directed apically in relation to the tooth (Fig. 18-9). Lack of bone loss at the interproximal region of the tooth may make this kind of defect difficult to detect.

FIG. 18-9 A, Loss of the lingual alveolar crest adjacent to this mandibular first bicuspid without associated interproximal bone loss. B, Loss of the buccal cortical bone adjacent to the maxillary central and lateral incisors. The black arrow indicates the level of the buccal alveolar crest, which demonstrates more profound loss relative to the lingual alveolar crest (white arrow).
Osseous Deformities in the Furcations of Multirooted Teeth
Progressive periodontal disease and its associated bone loss may extend into the furcations of multirooted teeth. As bone resorption extends down the side of a multirooted tooth, eliminating the bone covering the root, it can reach the level of the furcation and beyond. Widening of the PDL space at the apex of the interradicular bony crest of the furcation is strong evidence that the periodontal disease process involves the furcation (Fig. 18-10, A). If sufficient bone loss has occurred on the lingual and buccal aspects of a mandibular molar furcation, the radiolucent image of the lesion becomes prominent (Fig. 18-10, B). The bony defect may also involve only the buccal or lingual cortical plate and extend under the roof of the furcation. In such a case, if the defect does not extend through to the other cortical plate, it appears more irregular and radiolucent than does the adjacent normal bone. By use of the buccal object rule with films of different angulations, it may be possible to determine whether the buccal or the lingual cortical plate has been resorbed.
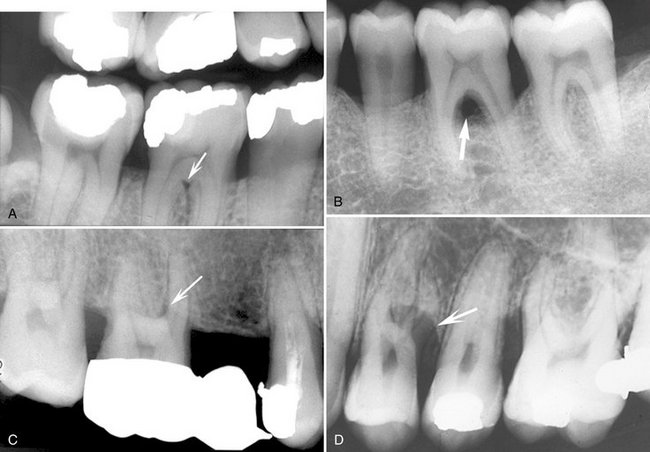
FIG. 18-10 A, A periapical film revealing very early furcation involvement of a mandibular molar characterized by slight widening of the periodontal ligament space in the furcation region (arrow). B, A periapical film revealing a profound radiolucent lesion within the furcation region (arrow) resulting from loss of bone in the furcation region and the buccal and lingual cortical plates. C, The angulation of this periapical view of a maxillary first molar projected the palatal root away from the trifurcation region revealing early widening of the furcation periodontal ligament space (arrow). D, Example of an inverted “J” shadow (arrow) resulting from bone destruction extending into the trifurcation region of a three-rooted maxillary first bicuspid.
If the crestal bone is below the furcation but the disease process has not extended into the interradicular bone, the width of the periodontal membrane space appears normal. Also, the septal bone may appear more radiolucent but otherwise be normal. In the mandible, the external oblique ridge may mask furcation involvement of the third molars. Convergent roots may also obscure furcation defects in maxillary and mandibular second and third molars.
The loss of interradicular bone in the furcation of a maxillary molar may originate from the buccal, mesial, or distal surface of the tooth. The most common route for furcation involvement of the maxillary permanent first molar is from the mesial side. The image of furcation involvement is not as sharply defined around maxillary molars as around mandibular molars because the palatal root is superimposed on the defect (see Fig. 18-10, C). However, occasionally this pattern of bone destruction is prominent and appears as an inverted “J” shadow with the hook of the J extending into the trifurcation (see Fig. 18-10, D) or as a radiolucent triangle superimposed over the roots of the involved tooth with its apex pointing toward the furcation.
Definitive diagnosis of complex furcation deformities requires careful clinical examination and sometimes surgical exploration. Radiographs, though, are an important tool in identifying potentially involved sites as well as providing important information about root morphology and length, which is of significance to treatment planning and prognosis.
CHANGES TO INTERNAL DENSITY AND TRABECULAR PATTERN OF BONE
As with all other inflammatory lesions, the periodontal lesion may stimulate a reaction in the surrounding bone. The peripheral bone may appear more radiolucent, or more sclerotic (radiopaque), or more commonly with a mixture of these patterns. Very rarely no apparent change will be seen in the surrounding bone. A radiolucent change reflects loss of density and number of trabeculae. The trabeculae appear very faint, which is more commonly seen in early or acute lesions (Fig. 18-11, A). If the trabeculae are sufficiently decalcified, they may not appear in the radiographic image although they are still present. This accounts for the apparent reformation of bone in some cases where the acute inflammation resolves with successful treatment and the trabeculae remineralize. The sclerotic bone reaction appears radiopaque because of deposition of bone on existing trabeculae at the expense of the marrow, resulting in thicker trabeculae that may eventually be so dense as to appear as an amorphous radiopaque mass (Fig. 18-11, B). This sclerotic reaction may extend some distance from the periodontal lesion, sometimes to the inferior aspect of the mandible. Usually the surrounding bone reaction is a mixture of both bone loss and sclerosis.
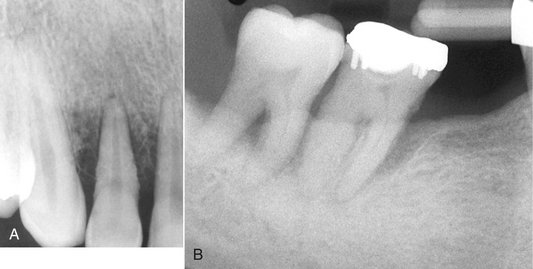
FIG. 18-11 A, Example of a primarily radiolucent reaction around this maxillary lateral incisor. Note that the trabeculae toward the alveolar crest on the mesial and distal aspect of the tooth are barely perceptible and the marrow spaces are enlarged. B, A periapical film revealing a predominantly sclerotic bone reaction resulting from the periodontal disease involving the mandibular molars. Note that the trabeculae are thickened and the marrow spaces are barely perceptible.
Inflammatory products from a periodontal lesion can even extend through the cortex of the floor of the maxillary sinus to cause a regional mucositis (Fig. 18-12). In rare cases a periosteal reaction might be seen on the buccal or lingual aspect of the alveolar process.
Other Patterns of Periodontal Bone Loss
A periodontal abscess is a rapidly progressing, destructive lesion that usually originates in a deep soft tissue pocket. It occurs when the coronal portion of the pocket becomes occluded or when foreign material becomes lodged between a tooth and the gingiva. Clinically, pain and swelling and sometimes a draining sinus are present in the region. If the lesion is acute, there may be no visible radiographic changes. If the lesion persists, a radiolucent region appears, often superimposed over the root of a tooth. The radiolucency may be a rounded area of rarefaction and a bridge of bone may be present over the coronal aspect of the lesion, separating it from the crest of the alveolar ridge (Fig. 18-13). After treatment, some of the lost bone may regenerate.

FIG. 18-13 Example of a periodontal abscess related to the maxillary canine; note the well-defined area of bone loss over the midroot region of the tooth and extending in a mesial direction toward the lateral incisor. There appears to be a layer of bone (arrow) separating the area of bone destruction from the crest of the alveolar process.
AGGRESSIVE PERIODONTITIS
Aggressive periodontitis refers to periodontal disease of an aggressive and rapid nature that usually occurs in patients younger than 30 years. The severity of the disease appears to be an exuberant reaction to a minimum amount of plaque accumulation and may result in early tooth loss. The term aggressive periodontitis has replaced the term early-onset periodontitis, which included three former classifications: localized juvenile periodontitis, generalized juvenile periodontitis, and rapidly progressing periodontitis. Aggressive periodontitis is now subclassified into localized aggressive periodontitis and generalized aggressive periodontitis. The cause of aggressive periodontitis is not known; however, specific bacterial pathogens, especially Actinobacillus actinomycetemcomitans, functional defects of polymorphonuclear leukocytes, exuberant immune responses, and inheritable genetic factors have been implicated.
Clinical Presentation
Localized aggressive periodontitis is associated with attachment loss involving the incisors and first molars. In this form, the amount of bone loss correlates with the time of tooth eruption, in that the teeth that erupt first (incisors and first molars) have the most bone loss. This disease usually commences around puberty and the bone loss is rapid; up to three to four times the rate seen in chronic periodontitis. Of interest is the fact that there are usually very few signs of soft tissue inflammation or plaque accumulation despite the presence of deep bony pockets. Often the patient will present with drifting and mobile incisors and early loss of first molars.
Generalized aggressive periodontitis can involve a variable number of teeth, from at least three to all of the dentition, and by definition is not confined to the first molars and incisors. This rapidly progressing disease usually affects individuals younger than 30 years. The gingiva may appear normal as in the localized form or may have an exuberant inflammatory response. If there is a history of premature loss of deciduous teeth and the permanent teeth are rapidly lost soon after erupting, a possible diagnosis of Papillon-Lefèvre syndrome might be considered. This syndrome is usually seen with an associated hyperkeratosis of palmar and plantar surfaces.
Estimates of prevalence of aggressive periodontitis are 0.53% and 0.13% for the localized and generalized forms, respectively, in the United States. Black individuals are affected more commonly than whites are with both the localized and generalized forms. Black male patients are more commonly affected with localized disease than are black female patients, whereas white female patients are more likely than white men to have localized disease.
Radiographic Appearance
The radiographic appearance of the bone loss in localized aggressive periodontitis typically consists of deep vertical defects (Fig. 18-14). Maxillary teeth are involved slightly more often than mandibular teeth, and strong left-right symmetry is common. The generalized form of aggressive periodontitis can involve several teeth or all the dentition and the rapid bone loss may be of the vertical or horizontal pattern.
Treatment
Early identification and treatment of aggressive periodontitis is important because of the rapid progression of this condition and the associated tooth loss. Response to conventional periodontal therapy is not predictable but is more likely to be successful when initiated earlier. Treatment often consists of scaling, curettage, and administration of antibiotics and may also include surgical and regenerative therapies.
Dental Conditions Associated with Periodontal Diseases
Various changes in the dentition and its supporting structures that have been associated with and potentially can exacerbate periodontal disease may be evident in the radiographic examination. These conditions, including occlusal trauma and tooth mobility, open contacts, and local irritating factors such as overhanging and faulty restorations and calculus, should be identified as part of a complete clinical and radiologic assessment.
OCCLUSAL TRAUMA
Traumatic occlusion causes degenerative changes in response to occlusal pressures that are greater than the physiologic tolerances of the tooth’s supporting tissues. These changes occur either as a result of maladaptation in response to excessive occlusal force on teeth or by normal occlusal forces on a periodontium already compromised by bone loss. In addition to clinical signs and symptoms such as increased mobility, wear facets, unusual response to percussion, and a history of contributing habits, there are associated radiographic findings that include widening of the PDL space, thickening of the lamina dura, bone loss, and an increase in the number and size of trabeculae. Other sequelae of traumatic occlusion include hypercementosis and root fractures. Traumatic occlusion alone does not cause gingivitis or periodontitis, affect the epithelial attachment, nor lead to pocket formation, but in the presence of preexisting periodontitis bone loss may be accelerated. Traumatic occlusion can be definitively diagnosed only by clinical evaluation and not by the radiographic findings alone.
TOOTH MOBILITY
Widening of the PDL space suggests tooth mobility, which may result from occlusal trauma or a lack of bone support arising from advanced bone loss. If the affected tooth has a single root, the socket may develop an hourglass shape. If the tooth is multirooted, it may show widening of the PDL space at the apices and in the region of the furcation. These changes result when the tooth moves about an axis of rotation at some midpoint on the roots. In addition, the radiographic image of the lamina dura may appear broad and hazy and show increased density.
OPEN CONTACTS
When the mesial and distal surfaces of adjacent teeth do not touch, the patient has an open contact. This condition may be dangerous to the periodontium because of the potential for food debris to become trapped in the region. Trapped food particles may damage the soft tissue and induce an inflammatory response and contribute to the development of localized periodontal disease. Open contacts are associated with periodontal disease more than closed contacts are. Similar potential situations where periodontal disease may develop are discrepancies in the height of two adjacent marginal ridges or tipped teeth (Fig. 18-15). Abnormal tooth alignment does not cause periodontal disease but provides an environment where the disease may develop as a result of difficulty in maintaining adequate oral hygiene.

FIG. 18-15 The second molar has tipped mesially after loss of the first molar, creating an abnormal tooth alignment that was difficult for the patient to maintain and leading to localized periodontal disease. Note the calculus on the mesial surface of the second molar. The crown on the second premolar was constructed with an enlarged distal contour to stop further tipping of the molar.
LOCAL IRRITATING FACTORS
Other local factors that are radiographically apparent may provide an environment where periodontal disease may develop or may aggravate existing periodontal disease. For instance, calculus deposits (Fig. 18-16) can prevent effective cleansing of a sulcus and lead to enhanced plaque formation and the progression of periodontal disease. Calculus is most commonly seen on the mandibular incisors but may be localized to any surface or generalized throughout the dentition. Defective restorations with overhanging or poorly contoured margins can also lead to the accumulation of plaque, thus providing an environment where periodontal disease may develop (Fig. 18-17). Radiographs often reveal these conditions.
Evaluation of Periodontal Therapy
Radiographs may show signs of successful treatment of periodontal disease. In some cases there may be reformation of the interproximal cortex (Fig. 18-18) and the sharp line angle between the cortex and lamina dura. The relatively radiolucent margins of bone that were undergoing active resorption before treatment may become more sclerotic (radiopaque) after successful therapy. In some cases there may have been considerable mineral loss of the cancellous bone (appearing radiolucent) so that the bone is not radiographically apparent. Successful treatment may then result in remineralization, causing the bone to become visible in the radiographic image, giving the false impression that bone has actually grown into periodontal defects. In many cases there will be no apparent radiographic changes after successful treatment. Also, radiographs do not disclose the therapeutic elimination of (radiolucent) soft tissue periodontal pockets; healing therefore is best assessed by clinical evaluation.
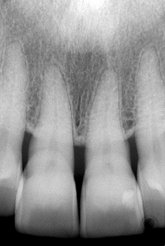
FIG. 18-18 An example of a case where the interproximal cortex of the alveolar crest has reformed after successful periodontal therapy.
Sequential radiographs made with different beam angulations may give the false impression that bone has grown into the periodontal defects. Therefore in a longitudinal study effort should be given to duplicate the image geometry as well as using ideal exposure and processing variables. For instance, too high an x-ray exposure or too long a developing time increases the density of the image (more radiolucent) and thin bone such as the alveolar crest may not be apparent, giving the false impression that the bone has been resorbed. Alternatively, underexposed or underdeveloped films may give the false impression of bone growth.
The clinical crown-to-tooth ratio is a useful criterion not only for determining the nature of the restorative treatment to be performed on a tooth but also for deciding on the prognosis of an individual tooth. It is a measure of the tooth’s bony support, relating the proportion of tooth length that is beyond the level of bone (clinical crown) to that supported by the lowest level of bone (bony investment). Teeth have an unfavorable crown-to-root ratio when the length of the tooth out of bone exceeds the length of root supported by bone.
DIFFERENTIAL DIAGNOSIS
The majority of cases of bone loss around teeth are caused by periodontal diseases. This fact can make the clinician less sensitive to other diseases with similar manifestations that should always be considered in the differential diagnosis. Occasionally, more serious diseases are missed or recognized late. The most likely clinical sign of disease other than periodontal disease is the presence of one or a few adjacent loose teeth when the rest of the mouth shows no signs of periodontal disease. Radiographically, suspicion should be heightened if the bone destruction does not have the pattern or morphology normally associated with periodontal disease. Squamous cell carcinoma of the alveolar process occasionally is treated as periodontal disease, resulting in an unfortunate delay in diagnosis and treatment (Fig. 18-19, A). This malignancy may display characteristics that suggest its true nature, such as extensive bone destruction of a localized region or invasive characteristics (see Chapter 23), or it may mimic periodontal disease. In some cases only the clinical characteristics of the lesion and the failure to respond to treatment indicate the presence of malignancy.
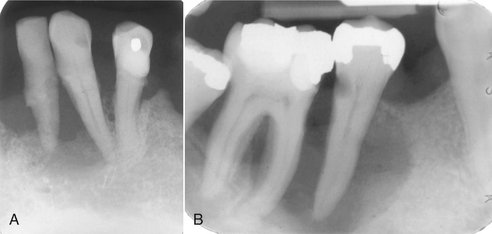
FIG. 18-19 A, A periapical film of a case of squamous cell carcinoma of the alveolar process of the mandible; note the irregular bone destruction. B, A periapical film of Langerhans’ cell histiocytosis demonstrating an alveolar lesion with bone destruction; note that the epicenter would be at the midroot region instead of the alveolar crest, as seen in periodontal disease.
Any lesion of bone destruction that has ill-defined borders and a lack of peripheral bone response (sclerosis) should be viewed with suspicion. Another disease to be considered is Langerhans’ cell histiocytosis (Fig. 18-19, B). Often this disease may manifest as single or multiple regions of bone destruction around the roots of teeth, similar to periodontal disease. The condition may appear similar to localized aggressive periodontitis except that the bone destruction does not correlate with the time of tooth eruption, as is seen in periodontitis. Also, in histiocytosis the midroot region is the epicenter of bone destruction, which gives early lesions an “ice cream scoop” appearance (see Chapter 24). The alveolar crest may remain intact.
Effect of Systemic Diseases on Periodontal Disease
Although systemic diseases do not cause periodontal disease, they do influence its course by interfering with the body’s natural defenses against irritants or limiting its capacity to repair. Although any systemic disease may have some influence on other body systems, only a few appear to influence the periodontium and periodontal treatment. These include diabetes mellitus, hematologic disorders (e.g., monocytic conditions and, less often, myelogenous leukemia, neutropenia, hemophilia and nonhemophilic polycythemia vera), genetic and hereditary disturbances (e.g., Papillon-Lefèvre syndrome, Down syndrome, hypophosphatemia, Chédiak-Higashi syndrome), hormonal changes (e.g., puberty, pregnancy, menopause), and stress.
ACQUIRED IMMUNODEFICIENCY SYNDROME
The incidence and severity of periodontal disease is high in patients with acquired immunodeficiency syndrome. In these individuals the disease process is characterized by a rapid progression that leads to bone sequestration and loss of several teeth. These patients may not respond to standard periodontal therapy.
DIABETES MELLITUS
Diabetes mellitus is the most common and important systemic disease to influence the onset and course of periodontal disease. Uncontrolled, it may result in protein breakdown, degenerative vascular changes, lowered resistance to infection, and increased severity of infections. Consequently, patients with uncontrolled diabetes are more disposed to the development of periodontal disease than are those with normal glucose metabolism. Patients with uncontrolled diabetes and periodontal disease also show more severe and rapid alveolar bone resorption and are more prone to the development of periodontal abscesses. In patients whose diabetes is under control, periodontal disease responds normally to traditional treatment.
RADIATION THERAPY
Although not a systemic disease, high-dose irradiation to the oral tissues as a treatment for malignant conditions may have a detrimental effect on the periodontium. Radiation therapy to the jaws results in bone that is hypovascular, hypocellular, and hypoxic. This bone may be less able to remodel and be more susceptible to infections, resulting in rapid bone loss that is indistinguishable from the radiographic characteristics of periodontal disease. Teeth that have been exposed to high-dose radiation fields have been shown to demonstrate greater recession, attachment loss, and mobility than do teeth in the same mouth that were not within the field.
CLINICAL CHARACTERISTICS OF PERIODONTAL DISEASES
Armitage, GC. Periodontal diseases: diagnosis. Ann Periodontol. 1996;1:37–215.
Herrera, C, González, I, Sanz, M. The periodontal abscess (I): clinical and microbiological findings. J Clin Periodontol. 2000;27:387–394.
Newman, MG, Takei, HH, Klokkevold, PR, et al. Carranza’s clinical periodontology. Philadelphia: WB Saunders.; 2006.
Walsh, TF, al-Kohail, OS, Fosam, EB. The relationship of bone loss observed on panoramic radiographs with clinical periodontal screening. J Clin Periodontol. 1997;24:153–157.
Melvin, WL, Sandifer, JB, Gray, JL. The prevalence and sex ratio of juvenile periodontitis in a young racially mixed population. J Periodontol. 1991;62:330–334.
Papapanou, PN. Periodontal diseases: epidemiology. Ann Periodontol. 1996;1:1–36.
Position paper: epidemiology of periodontal diseases. American Academy of Periodontology. J Periodontol. 1996;67:935–945.
Bimstein, E, Garcia-Godoy, F. The significance of age, proximal caries, gingival inflammation, probing depths, and the loss of lamina dura in the diagnosis of alveolar bone loss in the primary molars. ASDC J Dent Child. 1994;61:125–128.
Page, RC, Offenbacher, S, Schroeder, HE, et al. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Periodontol 2000. 1997;14:216–248.
Salvi, GE, Lawrence, HP, Offenbacher, S, et al. Influence of risk factors on the pathogenesis of periodontitis. Periodontol 2000. 1997;14:173.
Schwartz, Z, Goultschin, J, Dean, DD, et al. Mechanisms of alveolar bone destruction in periodontitis. Periodontol 2000. 1997;14:158.
Van Dyke, TE, Serhan, CN. Resolution of inflammation: a new paradigm for the pathogenesis of periodontal diseases. J Dent Res. 2003;82:82–90.
Gutteridge, DL. The use of radiographic techniques in the diagnosis and management of periodontal diseases. Dentomaxillofac Radiol. 1995;24:107–113.
Jeffcoat, MK, Wang, IC, Reddy, MS. Radiographic diagnosis in periodontics. Periodontol 2000. 1995;7:54–68.
Khocht, A, Zohn, H, Deasy, M, et al. Screening for periodontal disease: radiographs vs PSR. J Am Dent Assoc. 1996;127:749–756.
Koral, SM, Howell, TH, Jeffcoat, MK. Alveolar bone loss due to open interproximal contacts in periodontal disease. J Periodontol. 1981;52:447–450.
Mann, J, Pettigrew, J, Beideman, R, et al. Investigation of the relationship between clinically detected loss of attachment and radiographic changes in early periodontal disease. J Clin Periodontol. 1985;12:247–253.
Nielsen, IM, Glavind, L, Karring, T. Interproximal periodontal intrabony defects: prevalence, localization, and etiological factors. J Clin Periodontol. 1980;7:187–198.
Rams, TE, Listgarten, MA, Slots, J. Utility of radiographic crestal lamina dura for predicting periodontitis disease activity. J Clin Periodontol. 1994;21:571–576.
Waite, IM, Furniss, JS, Wong, WM. Relationship between clinical periodontal condition and the radiological appearance at first molar sites in adolescents: a 3-year study. J Clin Periodontol. 1994;21:155–160.
Albandar, JM, Brown, LJ, Löe, H. Dental caries and tooth loss in adolescents with early onset periodontitis. J Periodontol. 1996;67:960–967.
Albandar, JM, Brown, LJ, Löe, H. Clinical features of early onset periodontitis. J Am Dent Assoc. 1997;128:1393–1399.
Brown, LJ, Albandar, JM, Brunelle, JA, et al. Early onset periodontitis: progression of attachment loss during 6 years. J Periodontol. 1996;67:968–975.
Loe, H, Brown, LJ. Early onset periodontitis in the United States of America. J Periodontol. 1991;62:608–616.
Page, RC, Altman, LC, Ebersole, JL, et al. Rapidly progressive periodontitis: a distinct clinical condition. J Periodontol. 1983;54:197–209.
Bragger, I. Radiographic diagnosis of periodontal disease progression. Curr Opin Periodontol. 1996;3:59–67.
Gröndahl, K, Gröndahl, HG, Webber, RL, et al. Influence of variations in projection geometry on the detectability of periodontal bone lesions: a comparison between subtraction radiography and conventional radiographic technique. J Clin Periodontol. 1984;11:411–420.
Pepelassi, EA, Diamanti-Kipioti, A. Selection of the most accurate method of conventional radiography for the assessment of periodontal osseous destruction. J Clin Periodontol. 1997;24:557–567.
Reed, B, Polson, A. Relationships between bitewing and periapical radiographs in assessing crestal alveolar bone levels. J Periodontol. 1984;55:22–27.
Eickholz, P, Hausmann, E. Evidence for healing of periodontal defects 5 years after conventional and regenerative therapy: digital subtraction and bone level measurements. J Clin Periodontol. 2002;29:922–928.
Burgett, FG. Trauma from occlusion: periodontal concerns. Dent Clin North Am. 1995;39:301–311.
Wank, GS, Kroll, YJ. Occlusal trauma: an evaluation of its relationship to periodontal prostheses. Dent Clin North Am. 1981;25:511–532.
Emrich, LJ, Shlossman, M, Genco, RJ. Periodontal disease in non-insulin-dependent diabetes mellitus. J Periodontol. 1991;62:123–131.
Epstein, JB, Lunn, R, Le, N, et al. Periodontal attachment loss in patients after head and neck radiation therapy. Oral Surg Oral Med Oral Path Oral Radiol Endod. 1998;86:673–677.
Farzim, I, Edalat, M. Periodontosis with hyperkeratosis palmaris and plantaris (the Papillon-Lefèvre syndrome): a case report. J Periodontol. 1974;45:316–318.
Nelson, RG, Schlossman, M, Budding, LM, et al. Periodontal diseases and NIDDM in Pima Indians. Diabetes Care. 1990;13:836–840.
Rateitschak-Plüss, EM, Schroeder, HE. History of periodontitis in a child with Papillon-Lèfèvre syndrome. A case report. J Periodontol. 1984;55:35–46.
Winkler, JR, Grassi, M, Murray, PA. Clinical description and etiology of HIV-associated periodontal disease. In: Robinson PB, Greenspan JS, eds. Prospectus on oral manifestations of AIDS. Littleton, MA: PSG Publishing, 1988.