Chapter 36 Nutrition
Alternative or complementary therapies
Basal metabolic rate (BMR), p. 1065
Bioelectrical impedance analysis (BIA)
Conditionally essential amino acids
Estimated average requirement (EAR)
Medical nutrition therapy (MNT)
Non-essential amino acids, p. 1066
Recommended dietary allowance (RDA)
Recommended dietary intake (RDI)
Resting energy expenditure (REE)
Mastery of content will enable you to:
• Define the key terms listed.
• Explain why each major nutrient is necessary for nutrition.
• Explain the importance of a balance between energy intake and energy requirements.
• List the end products of carbohydrate, protein and fat metabolism.
• Explain the significance of saturated, unsaturated and polyunsaturated fats.
• Describe the food guide pyramid and the healthy eating index and discuss their value in planning meals for good nutrition.
• Explain dietary reference intakes.
• List seven dietary guidelines for health promotion.
• Explain the variance in nutritional requirements throughout growth and development.
• Discuss the major methods of nutritional assessment.
• Identify three major nutritional problems and describe patients at risk.
• State the goals of enteral and parenteral nutrition.
• Describe the procedure for initiating and maintaining tube feedings.
• Describe ways to avoid complications of tube feedings.
• Describe ways to avoid complications of parenteral nutrition.
• Discuss medical nutrition therapy in relation to three medical conditions.
• Discuss diet counselling and client teaching in relation to patient expectations.
Food provides sustenance, but also holds symbolic meaning. The giving or taking of food is part of ceremonies, social gatherings, holiday traditions, religious events, the celebration of birth and the mourning of death. The difficulty of the decision to withdraw food in a terminal illness, even in the form of intravenous (IV) nutrients, is testimony to the symbolic power of food and feeding.
Florence Nightingale understood the importance of nutrition, stressing the nurse’s role in the science and art of feeding during the mid-1800s (McDonald, 2010). Since then, the nurse’s role in nutrition and diet therapy has changed. In the early 19th century, the description of a calorie as a unit of energy obtained from food moved nutrition into the realm of science (Lutz and Przytulski, 2011). Malnutrition is now recognised as a disease that needs specific treatment (Bocock and others, 2008). In some illnesses, such as type 2 diabetes mellitus or mild hypertension, diet therapy may be the major treatment for disease control. Other conditions, such as inflammatory bowel disease, may require specialised nutrition support such as enteral or parenteral nutrition. Standards now exist that clearly designate the standard of care for promotion of optimal nutrition in all healthcare patients.
Scientific knowledge base
Nutrients: the biochemical units of nutrition
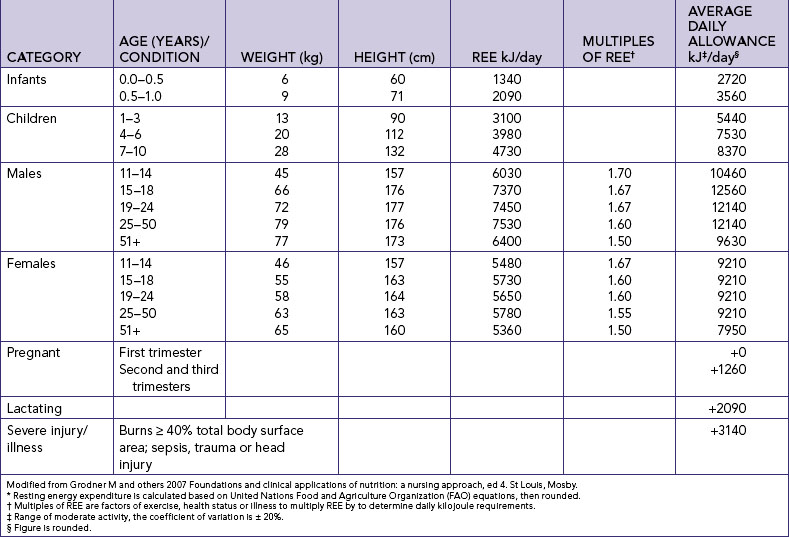
The body requires fuel to provide energy for cellular metabolism and repair, organ function, growth and body movement. An individual’s energy requirements are influenced by several factors. The energy requirement of a person at rest is called the basal metabolic rate (BMR). This is the energy needed to maintain life-sustaining activities (breathing, circulation, heart rate and temperature) for a specific period of time. Factors such as age, body mass, gender, fever, starvation, menstruation, illness, injury, infection, activity level or thyroid function affect energy requirements. The resting energy expenditure (REE) is a measurement that accounts for BMR plus energy to digest meals and perform mild activity. REE (Table 36-1) is a baseline of energy requirement that accounts for approximately 60–75% of our daily needs. Factors that affect metabolism include illness, pregnancy, lactation and activity level. In hospitals, energy requirements may be estimated by measuring oxygen consumption, carbon dioxide production and nitrogen excretion by means of a metabolic chart. These are specialised measurements, and are used mainly for seriously to critically ill patients.
In general, when energy requirements are completely met by kilojoule (kJ) intake in food, weight does not change. When the kilojoules ingested exceed energy demands, a person gains weight. If the kilojoules ingested fail to meet energy requirements, a person loses weight.
Nutrients are the elements necessary for body processes and function. Energy needs are met from six categories of nutrients: carbohydrates, proteins, fats, water, vitamins and minerals. Water is a vital body component that acts as a solvent for metabolic processes. Vitamins and minerals do not provide energy but are essential to metabolic processes, including acid–base balance.
Foods are sometimes described according to their nutrient density, the proportion of essential nutrients to the number of kilojoules. High-nutrient-density foods, such as fruits and vegetables, provide a large number of nutrients in relationship to kilojoules. Low-nutrient-density foods, such as alcohol or sugar, are high in kilojoules but are nutrient-poor.
Carbohydrates
Carbohydrates are the main source of energy in the diet. Carbohydrates yield 16.7 kJ per gram and serve as the main source of fuel (glucose) for the brain, skeletal muscles during exercise, erythrocyte and leucocyte production, and cell function of the renal medulla. Carbohydrates are obtained mainly from plant foods, and lactose (milk sugar).
Carbohydrates are classified according to their carbohydrate units, or saccharides. Monosaccharides such as glucose (dextrose) or fructose cannot be broken down into a more basic carbohydrate unit. Disaccharides such as sucrose, lactose and maltose are composed of two monosaccharides and water. Both monosaccharides and disaccharides are classified as simple carbohydrates, and are found mainly in fruits, vegetables and manufactured foods. Polysaccharides such as glycogen are composed of many carbohydrate units and are classified as complex carbohydrates. They are insoluble in water and are digested to varying degrees. Starches are polysaccharides. Starch digestion and absorption consists of several steps (Table 36-2).
TABLE 36-2 SUMMARY OF CARBOHYDRATE DIGESTION AND ABSORPTION
| FOODSTUFF | ENZYMES/ACTION |
|---|---|
| Mouth | |
| Starch | Salivary amylase |
| Stomach | |
| None | Starch hydrolysis continues briefly |
| Small intestine | |
| Lactose | Lactase → glucose* + galactose* |
| Maltose | Maltase → glucose* + glucose* |
| Sucrose | Sucrase |
→ produces.
*absorbed by capillaries in the villi and transported around the body.
Adapted from McCance K, Huether S 2010 Pathophysiology: the biologic basis for disease in adults and children, ed 6. St Louis, Mosby.
Some polysaccharides cannot be digested because humans do not have enzymes capable of breaking them down. Fibre has received attention as a dietary factor in disease prevention and in treatment and prevention of diarrhoea in tube-fed patients. Insoluble fibres are not digestible and include cellulose, hemicellulose and lignin. These aid in adding bulk to chyme and aiding digestion. Soluble fibres include pectin, guar gum and mucilage. Soluble fibre is beneficial because it reduces cholesterol by binding to it and carrying it out of the body.
Proteins
Proteins can be metabolised to release energy, yielding 16.7 kJ per gram for synthesis (building) of body tissue in growth, maintenance and repair. Collagen, hormones, enzymes, immune cells, DNA and RNA are all composed of protein. In addition, blood clotting, fluid regulation and acid–base balance require proteins. Nutrients and many pharmacological substances are transported in the blood by proteins.
The simplest form of protein is the amino acid. Essential amino acids are a group of nine amino acids that the body cannot synthesise; they must be provided from the diet (Box 36-1). A second type of amino acids are non-essential amino acids that the body can synthesise from other substrates already in the body, and a third type of amino acids are conditionally essential amino acids that are needed by the body in special situations when the body has undergone stress, trauma or illness. Amino acids can be linked together to form dipeptides, tripeptides and oligopeptides. Albumin and insulin are simple proteins because they contain only amino acids or their derivatives. The combination of a simple protein with a non-protein substance produces a complex protein, such as lipoprotein, formed by a combination of a lipid and a simple protein.
BOX 36-1 AMINO ACIDS REQUIRED IN NUTRITION
Adapted from Lutz C, Przytulski K 2011 Nutrition and diet therapy: evidence-based applications, ed 5. Philadelphia, FA Davis.
A complete protein contains all essential amino acids in sufficient quantity to support growth and maintain nitrogen balance. Ingestion of proteins is not primary for meeting energy needs, but is most important for ensuring a positive nitrogen balance. Complete proteins are also referred to as high-quality proteins. Incomplete proteins lack one or more of the nine essential amino acids and include those found in cereals, legumes (beans, peas) and vegetables. Complementary proteins are pairs of incomplete proteins that, when combined, supply the total amount of protein provided by complete protein sources.
Protein is 16% nitrogen and serves as the only source of nitrogen for the body. Nitrogen balance is achieved when the intake and output of nitrogen are equal. When the intake of nitrogen exceeds the output the body is in positive nitrogen balance, which is required for growth, normal pregnancy, maintenance of lean muscle mass and vital organs, and wound healing. The nitrogen retained by the body is used for building, repair and replacement of body tissues. Negative nitrogen balance occurs when the body loses more nitrogen than it gains, for example with infection, sepsis, burns, fever, malnutrition, starvation, head injury and trauma. The increased nitrogen loss is the result of body-tissue destruction or loss of nitrogen-containing body fluids. Nutrition during this period must provide protein to put patients into positive balance for healing.
Protein can be used to provide energy, but because of protein’s essential role in growth, maintenance and repair, adequate kilojoules should be provided in the diet from non-protein sources. Protein is spared as an energy source when there is sufficient carbohydrate in the diet to meet the energy needs of the body. The required dietary intake of protein for adults is shown in Table 36-3. Additional protein is required during pregnancy and lactation (Schenkler and Roth, 2011).
Fats
Fats (lipids) are the most concentrated source of energy, yielding 38 kJ per gram. Fats are composed of triglycerides and fatty acids. Triglycerides circulate in the blood and are made up of three fatty acids attached to a glycerol. Fatty acids are composed of chains of carbon and hydrogen atoms with an acid group on one end of the chain and a methyl group at the other. Synthesis of fatty acids is called lipogenesis. Fatty acids can be saturated, where each carbon in the chain has two attached hydrogen atoms; or unsaturated, where an unequal number of hydrogen atoms are attached and the carbon atoms attach to each other with a double bond. Monounsaturated fatty acids have one double bond, whereas polyunsaturated fatty acids have two or more double carbon bonds. The various types of fatty acids have significance for health and the incidence of disease, and are referred to in dietary guidelines.
Fatty acids are also classified as essential or non-essential. Linoleic acid, an unsaturated fatty acid, is the only essential fatty acid manufactured in humans. Linolenic acid and arachidonic acid (also unsaturated fatty acids) are important for metabolic processes but can be manufactured by the body only when linoleic acid is available. Deficiency occurs when fat intake falls below 10% of daily nutrition. Most animal fats have high proportions of saturated fatty acids, whereas vegetable fats have higher amounts of unsaturated and polyunsaturated fatty acids. See Figure 36-1 for a summary.
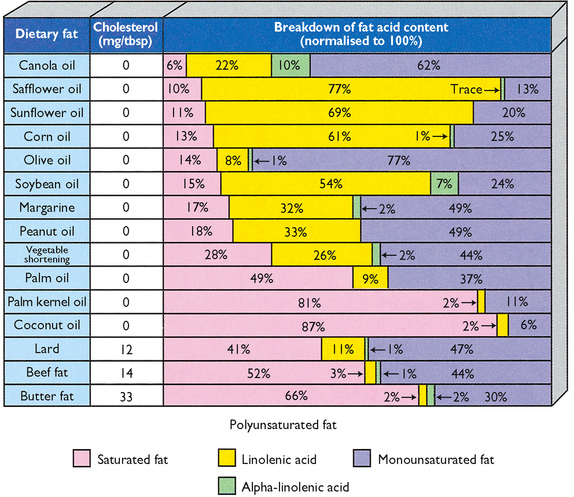
FIGURE 36-1 Comparison of fats in terms of cholesterol, saturated and unsaturated dietary intake.
From Byrd-Bredbenner C and others 2008 Wardlaw’s Perspectives in nutrition, ed 8. New York, McGraw-Hill.
Newer margarines contain plant sterols to reduce elevated low-density lipoprotein levels to lower serum cholesterol (Lutz and Przytulski, 2011). These spreads can be a useful part of a healthy diet, but all fats contain kilojoules. They should not be simply added to the diet, but used to replace conventional spreads or oils.
Water
Water is a critical component of the body because cell function depends on a fluid environment. Water constitutes 60–70% of total bodyweight. The percentage of total body water is greater for lean people than for obese people because muscle contains more water than any other tissue except blood. Infants have the greatest percentage of total body water, and older people have the least. When deprived of water, a person cannot survive for more than a few days.
Fluid needs are met by ingesting liquids and solid foods high in water content, such as fresh fruits and vegetables. Water is also produced during digestion when food is oxidised. In a healthy individual, fluid intake from all sources equals fluid output through elimination, respiration and sweating (see Chapters 37 and 38. An ill person can have an increased need for fluid (e.g. with fever or gastrointestinal losses). However, an ill person can also have a decreased ability to excrete fluid (e.g. with cardiopulmonary or renal disease), which may lead to the need to restrict fluid intake.
Vitamins
Vitamins are organic substances present in small amounts in foods that are essential for normal metabolism. The body is unable to synthesise vitamins in the required amounts, and depends on dietary intake. Vitamins are affected by processing, storage and preparation. Vitamin content is usually highest in fresh foods that are used quickly after minimal exposure to heat, air or water. Vitamins are classified as fat-soluble and water-soluble.
FAT-SOLUBLE VITAMINS
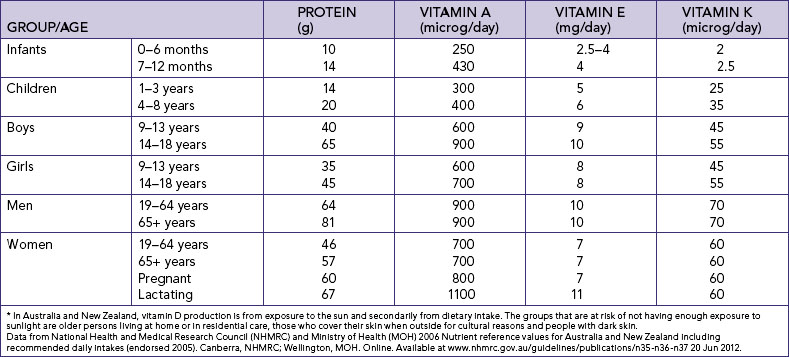
The fat-soluble vitamins (A, D, E and K) can be stored in the body. With the exception of vitamin D, these vitamins are provided through dietary intake. Hypervitaminosis of fat-soluble vitamins can result from megadoses (intentional or unintentional) of supplemental vitamins, excessive amounts in fortified food and large intake of fish oils. Table 36-3 summarises the recommended intake of fat-soluble vitamins.
Certain vitamins are currently of considerable interest in their role as antioxidants that neutralise substances called free-radicals, which are thought to produce oxidative damage to body cells and tissues. These vitamins include beta-carotene and vitamins A, C and E, and their antioxidant effect was found to be present when the intake was from food sources rather than supplements.
WATER-SOLUBLE VITAMINS
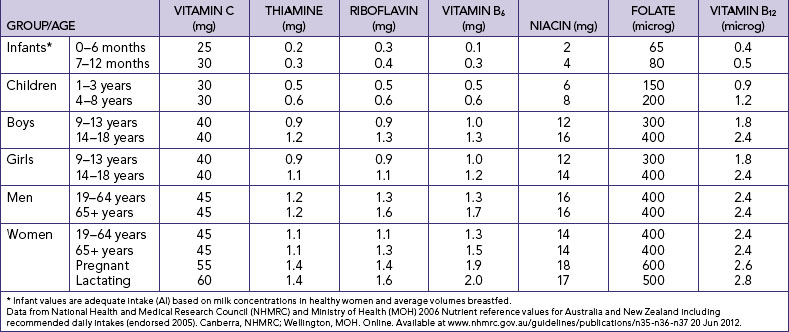
The water-soluble vitamins are vitamin C and B-complex (which consists of eight vitamins). Water-soluble vitamins cannot be stored in the body and must be provided in the daily food intake. Although water-soluble vitamins are not stored, toxicity may still occur. Vitamins are chemicals used as catalysts in biochemical reactions. When there is enough of any specific vitamin to meet the catalytic demands, the rest of the vitamin supply acts as a free chemical and may be toxic to the body. Table 36-4 summarises the recommended dietary allowances and adequate intakes of water-soluble vitamins.
Minerals
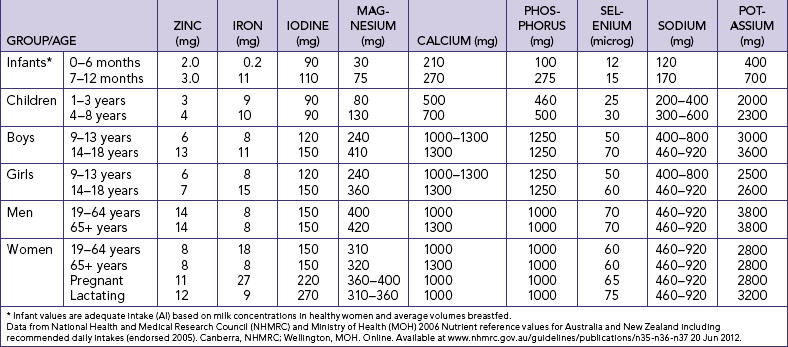
Minerals are inorganic elements essential to the body as catalysts in biochemical reactions. Minerals are classified as macrominerals when the daily requirement is 100 mg or more, and as microminerals or trace elements when less than 100 mg is needed daily. Both macrominerals and trace element requirements are summarised in Table 36-5. Selenium is a trace mineral that also has antioxidant properties. Silicon, vanadium, nickel, tin, cadmium, arsenic, aluminium and boron may play an as-yet unidentified role in nutrition. Toxic effects of arsenic, aluminium and cadmium are documented.
Anatomy and physiology of the digestive system
Digestion
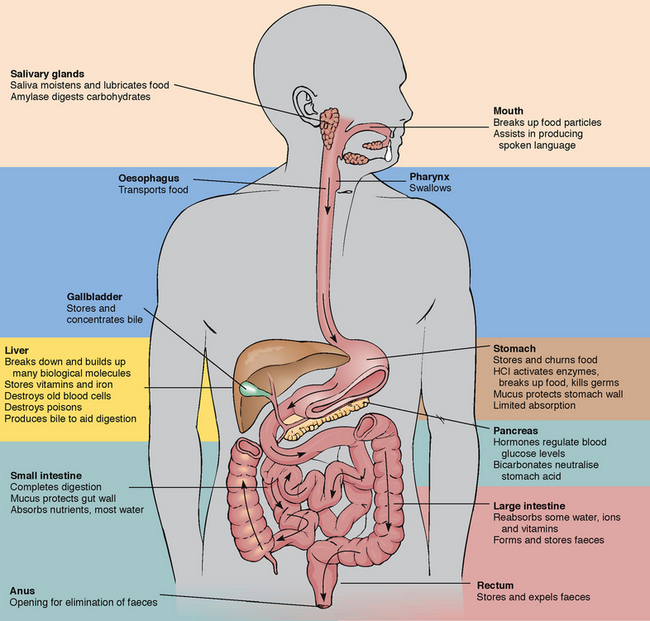
Digestion of food consists of mechanical breakdown that results from chewing, churning and mixing with fluid, as well as chemical reactions by which food is reduced to its simplest form. Each part of the gastrointestinal (GI) system has an important digestive or absorptive function. Enzymes are an essential component of the chemistry of digestion. Enzymes are the protein-like substances that act as catalysts to speed up chemical reactions.
Most enzymes have one specific function. Each enzyme functions best at a specific pH. The secretions of the GI tract have vastly different pH levels. For example, saliva is relatively neutral, gastric juice is highly acidic and the secretions of the small intestine are alkaline. For anatomical reference of the digestive system, see Figure 36-2.
The mechanical, chemical and hormonal activities of digestion are interdependent. Enzyme activity depends on the mechanical breakdown of food to increase its surface area for chemical action. Hormones regulate the flow of digestive secretions needed for enzyme supply, and digestion may also be decreased or increased by strong emotional states. The secretion of digestive juices and the motility of the GI tract are also regulated by physical, chemical and hormonal factors, as they are bound to psychological, emotional and nervous system alterations. Gastrointestinal tract action is increased by nerve stimulation from the parasympathetic nervous system (e.g. the vagus nerve).
Digestion begins in the mouth, where food is mechanically broken down by chewing. The food is mixed with saliva, which contains ptyalin (salivary amylase), an enzyme that acts on cooked starch to begin its conversion to maltose. The longer food is chewed, the more starch digestion occurs in the mouth. Proteins and fats are broken down physically, but remain unchanged chemically because enzymes in the mouth do not react with these nutrients. Chewing reduces food particles to a size suitable for swallowing, and saliva provides lubrication to further ease swallowing of the food. The epiglottis is a flap of skin that closes over the trachea to prevent aspiration as swallowing occurs. Swallowed food enters the oesophagus and is moved along by wavelike muscular contractions (peristalsis) to the base of the oesophagus, above the cardiac sphincter. Pressure from a bolus of food at the cardiac sphincter causes it to relax, allowing the food to enter the fundus, or uppermost portion, of the stomach. Difficulty with swallowing is referred to as dysphagia.
In the stomach, pepsinogen is secreted by chief cells and then activated by hydrochloric acid (HCl) to pepsin, a protein-splitting enzyme. Parietal cells secrete HCl as well as intrinsic factor (IF), which is necessary for absorption of vitamin B12 in the ileum. Gastric lipase and amylase are produced to begin fat and starch digestion, respectively. The stomach’s pyloric glands secrete gastrin, a hormone that triggers parietal cells to secrete HCl. The lining of the stomach is protected from autodigestion by a thick layer of mucus. Alcohol and aspirin are two substances directly absorbed through the lining of the stomach. The stomach acts as a reservoir where food remains for approximately 3 hours, with a range of 1–7 hours.
Food leaves the antrum, or distal stomach, via the pyloric sphincter and enters the duodenum. Food has now become an acidic, liquefied mass called chyme. Chyme flows into the duodenum and is quickly mixed with bile, intestinal juices and pancreatic secretions. Secretin and cholecystokinin (CCK) are hormones secreted by the mucosa of the small intestine. Secretin activates the release of bicarbonate from the pancreas, raising the pH of chyme. Cholecystokinin inhibits further gastrin secretion and initiates release of additional digestive enzymes from the pancreas and gallbladder.
Bile is manufactured in the liver and stored in the gallbladder. Bile acts as a detergent, as it emulsifies fat to permit enzyme action while suspending fatty acids in solution. Pancreatic secretions contain six enzymes: amylase to digest starch; lipase to break down emulsified fats; and trypsin, elastase, chymotrypsin and carboxypeptidase to break down proteins.
Peristalsis continues in the small intestine, mixing the secretions with the chyme. The mixture becomes increasingly alkaline, inhibiting the action of the gastric enzymes and promoting the action of the duodenal secretions. The epithelial cells of the small intestinal brush-border microvilli secrete enzymes to facilitate digestion. These include sucrase, lactase, maltase, lipase and peptidase. The major portion of digestion occurs in the small intestine, producing glucose, fructose and galactose from carbohydrates (see Table 36-2); amino acids and dipeptides from proteins; and fatty acids, glycerides and glycerol from lipids. Approximately 5 hours are required to pass food through the small intestine via peristalsis.
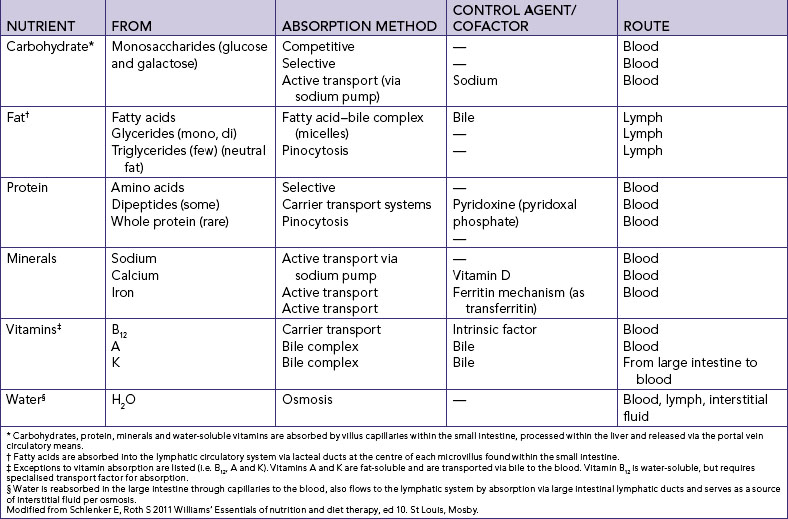
Absorption
The small intestine is the primary absorption site for nutrients. It is lined with finger-like projections called villi, which increase the surface area available for absorption. Nutrients are absorbed by means of passive diffusion, osmosis, active transport and pinocytosis. Table 36-6 describes the means and route of absorption of major food groups.
The main source of water absorption is via the intestine. Approximately 8.5 L of GI secretions and 1.5 L of oral intake, totalling 10 L of fluid, must be managed daily within the GI tract. The small intestine reabsorbs 9.5 L, and approximately 0.4 L is reabsorbed in the colon. The remaining 0.1 L is eliminated in faeces. In addition to water, electrolytes and minerals are absorbed, and bacteria in the colon synthesise vitamin K and some B-complex vitamins. Finally, faeces are formed in the colon for elimination.
Metabolism and storage of nutrients
Metabolism refers to all the biochemical reactions within the cells of the body. Metabolic processes can be anabolic (building) or catabolic (breaking down). Anabolism is the building of more-complex biochemical substances by synthesis of nutrients, and occurs when lean muscle is added through diet and exercise. Amino acids are anabolised into tissues, hormones and enzymes. Catabolism is the breakdown of biochemical substances into simpler substances. Starvation is an example of catabolism, when wasting of body tissues occurs. Normal metabolism and anabolism are physiologically possible when the body is in positive nitrogen balance, whereas catabolism occurs during physiological states of negative nitrogen balance.
Nutrients absorbed in the intestines, including water, are transported through the circulatory system to body tissues. Through the chemical changes of metabolism, nutrients are converted into a number of substances required by the body. Carbohydrates, protein and fat undergo metabolism to produce chemical energy and to maintain a balance between anabolism and catabolism. To carry out the body’s work, the chemical energy produced by metabolism is converted to other types of energy by different tissues. Muscle contraction involves mechanical energy, nervous system function involves electrical energy and the mechanisms of heat production involve thermal energy. All these forms of energy originate in metabolism. The interrelationships of protein, carbohydrate and fat metabolism are depicted in Figure 36-3.
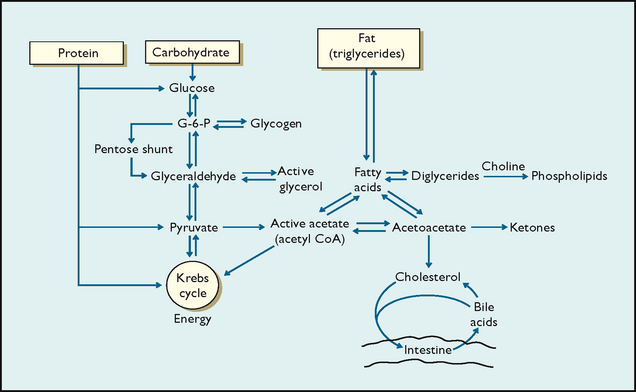
FIGURE 36-3 Interrelationship of macronutrient metabolism.
From Schlenker E, Roth S 2011 Williams’ Essentials of nutrition and diet therapy, ed 10. St Louis, Mosby.
Some of the nutrients required by the body are stored in tissues. The body’s major form of reserve energy is fat, stored as adipose tissue. Protein is stored in muscle mass. When the body’s energy requirements exceed the energy supplied by ingested nutrients, stored energy is used. Monoglycerides from the digested portion of fats can be converted to glucose by gluconeogenesis. Amino acids can also be converted to fat and stored or catabolised into energy via gluconeogenesis. All body cells except red blood cells and neurons can oxidise fatty acids into ketones for energy in the absence of dietary carbohydrates (glucose). Glycogen, synthesised from glucose, provides energy during brief periods of fasting. Glycogen is stored in small reserves in liver and muscle tissue. For example, blood glucose levels are maintained by this mechanism during sleep. Nutrient metabolism consists of three main processes:
Elimination
Chyme is moved by peristaltic action through the ileocaecal valve into the large intestine, where it becomes faeces. As faeces move towards the rectum, water is absorbed in the mucosa. The longer the material stays in the large intestine, the more water is absorbed, causing the faeces to become firmer. Exercise and fibre stimulate peristalsis, and water maintains consistency. Faeces contain cellulose and similar indigestible substances, sloughed epithelial cells from the GI tract, digestive secretions, water and microbes.
Dietary guidelines
Recommended dietary intake
Recommended dietary intake (RDI) guidelines have been developed for Australia and New Zealand (National Health and Medical Research Council, 2006). This format presents a range of acceptable intakes in place of absolute values. ‘Recommended dietary intake’ serves as a generic term, referring to four different values that include the estimated average requirement, recommended dietary allowance, adequate intake and tolerable upper intake level. The estimated average requirement (EAR) serves as a minimum indicator, meeting the nutrient needs of only 50% of any gender- or age-specific group. The recommended dietary allowance (RDA) continues to be a sufficient average indicator, necessary for all healthy people. When the RDA is not known, adequate intake (AI) is presented. Average intake values are derived from expert judgment; although less evidence-based, they are deemed to meet nutrient needs of all individuals in a group. Finally, the tolerable upper intake level (UL) is the maximum level of daily nutrient intake that is evidenced to be unlikely to induce toxicity (Schenkler and Roth, 2011). Figure 36-4 depicts the meaning of these four different reference values.
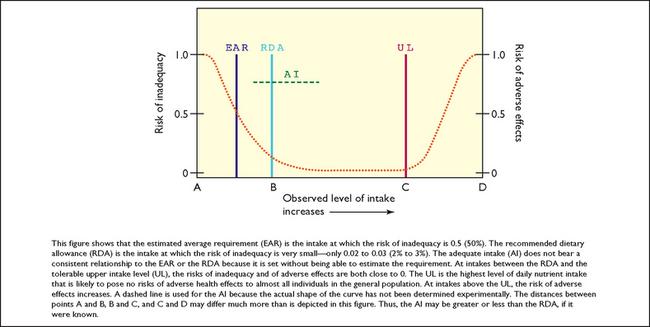
FIGURE 36-4 Summary of recommended dietary reference intakes.
From Food and Nutrition Board 1998 Dietary reference intakes: thiamine, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington DC, National Academy Press.
As research has expanded the scientific body of nutrition knowledge, absolute values are no longer sufficient. Studies investigating the reduction of risk of chronic diseases such as cardiovascular disease, cancer and osteoporosis have launched a need for expanded nutrient information. Specifically, seven nutrient groups are being re-evaluated: calcium, vitamin D, phosphorus, magnesium and fluoride; folate and other B-complex vitamins; antioxidants (vitamins C and E, selenium); macronutrients (protein, fat, carbohydrates); trace elements (iron, zinc); electrolytes and water; and other food components (fibre, phyto-oestrogens). Updated recommendations are currently available for thiamine, riboflavin, niacin, folate, vitamin B6, vitamin B12, pantothenic acid, choline, biotin, calcium, phosphorus, vitamin D, magnesium and fluoride, as shown in Tables 36-3, 36-4 and 36-5.
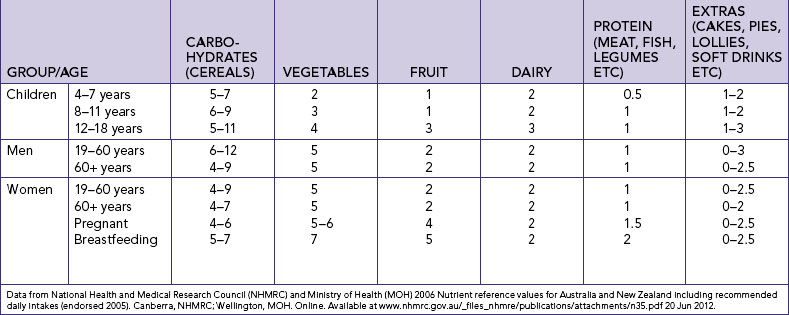
Food guidelines
The Australian Department of Health and Ageing takes a leading role in maintaining and improving the nutritional status of Australians through the development of a National Public Health Nutrition Strategy, including an action plan for Aboriginal and Torres Strait Islander people. Among the wide variety of materials available from government sources are useful guides such as the Australian Guide to Healthy Eating (Figure 36-5) and a guide for Aboriginal and Torres Strait Islander people called Sharing Good Tucker Stories produced by the Department of Family and Community. Box 36-2 gives some general dietary guidelines, and Table 36-7 indicates the average number of daily servings required to achieve a healthy diet.
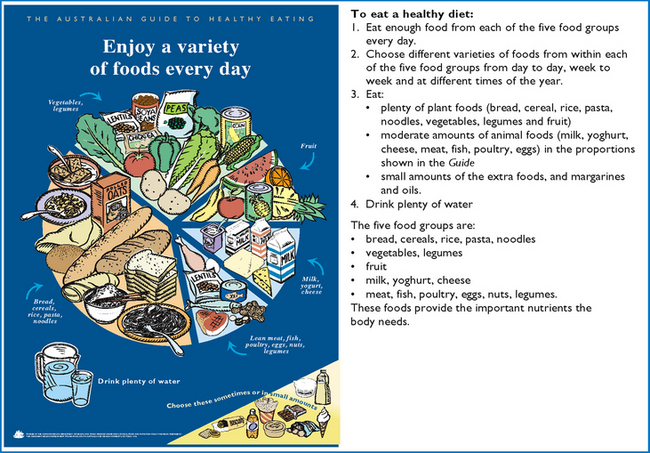
FIGURE 36-5 Guide to healthy eating.
Adapted from Department of Health and Ageing (DoHA) 2001 Australian Guide to Healthy Eating. Canberra, DoHA. Online. Available at www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-food-guide-index.htm 24 Aug 2012. Used with permission of the Australian Government.
BOX 36-2 GENERAL DIETARY GUIDELINES
• Maintain a healthy weight; balance your food with physical activity.
• Choose a diet low in fat, saturated fat and cholesterol.
• Choose a diet with plenty of vegetables, fruits and grain products.
See Australian Guide to Healthy Eating, ww.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-food-guide-index.htm
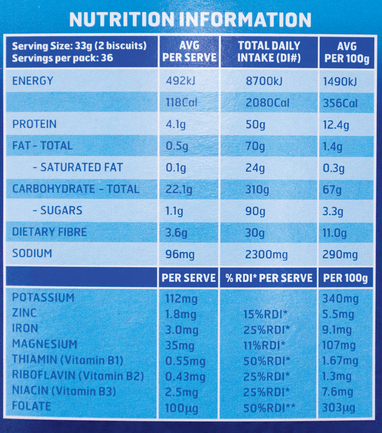
Food labels
In Australia and New Zealand, food labelling is controlled by Food Standards Australia New Zealand (FSANZ). The nutritional information must be accurate and in a standard format. The label must state the normal serving size and also express the nutritional information per 100 g of the food. Specific nutrients such as vitamins are also expressed as a percentage of the RDI. The ingredients list must show all the ingredients contained in the food, arranged in the order of decreasing content. Food colours and preservatives must be identified by reference to the International Numbering System for food additives (FSANZ, 2003) (see Figure 36-6).
Australian national nutritional health policies
Nutrition is an important factor in the health of all Australians, but also contributes to the marked differences in health status of Australia’s different ethnic groups. Many immigrants have better health on arrival in Australia but lose this advantage as a result of limited job opportunities and by adopting this country’s health habits. Nutrition also plays a role in the serious health inequality experienced by Australia’s Aboriginal and Torres Strait Islander peoples (Talbot and Verrinder, 2010).
The Department of Health and Ageing has a number of initiatives to reduce the inequality gap and has been providing nutritional advice to Australians for over 75 years. This has included advice on RDIs and dietary guidelines, as well as culturally relevant food and dietary patterns that not only achieve sustenance but also help to reduce the risk of chronic disease. The last 20 years have seen the development of numerous national government policies and programs designed to reorient healthcare systems towards promoting health. Many of these policies have tackled nutrition and diet, including the role they play in the pathogenesis of many major causes of illness and death. Since 2000, there have been a number of priority areas set by the Australian federal government, including asthma, arthritis and musculoskeletal disorders. The inclusion of these priority areas has meant that the nutritional and dietary focus identified in the report Goals and targets for Australia’s health in the year 2000 and beyond (Nutbeam and others, 1993) has been reduced in priority even though it could be strongly argued that sound nutrition has a key role in the prevention of many of the identified priority conditions.
The 2007/08 National Health Survey in Australia identified that the 65- to 74-year-old age group has the highest rates of ‘overweight’ or ‘obese’, at 75%; the situation is similar in New Zealand. There is an increasing awareness within the Australian and New Zealand communities about its ‘obesity epidemic’ and the need for programs that raise awareness for healthy eating and exercise at a national level.
Nursing knowledge base
Nutrition during human growth and development
Infants
Infancy is marked by rapid growth and high protein, vitamin, mineral and energy requirements. The average birthweight of an Australian baby is 3360 g. The infant usually doubles birthweight by 4–5 months and triples it by 1 year. An energy intake of about 450 kJ/kg of bodyweight is needed in the first half of infancy, and 340 kJ/kg in the second half (NHMRC, 2005).
Commercial formulas and human breast milk both provide approximately 2800 kJ/L. A full-term newborn is able to digest and absorb simple carbohydrates, proteins and a moderate amount of emulsified fat. Amylase, the starch-splitting enzyme, is not present until approximately 2½ to 3½ months. Infants need about 100–150 mL/kg/day of fluid because a large portion of total bodyweight is water.
BREASTFEEDING
Relatively simple cost-effective measures such as breastfeeding can have a significant impact on the health of women and children (Box 36-3). The Australian National Better Health Targets for the year 2000 were that 80% of infants would be exclusively breastfed at 3 months of age and 60% exclusively breastfed at 6 months. There were a number of initiatives to help meet these targets, but there is still some way to go. In 2008, nearly 90% of babies were breastfed at birth, but this fell to about 54% by 3 months of age (Australian Breastfeeding Association, 2009). The Public Health Association of Australia (2007) suggests that the breastfeeding rate would be enhanced by: (1) all maternity hospitals becoming baby-friendly hospitals; (2) workplace provisions supporting breastfeeding times and locations; (3) enhanced education for healthcare providers; (4) greater community awareness of the benefits of breastfeeding; (5) public acceptance of breastfeeding anywhere; and (6) the establishment of breast-milk banks for the use of babies whose mothers are unable to breastfeed. A number of organisations in both countries provide help with and information about breastfeeding (see Online resources).
• Protects your baby from illness and infection
• Provides the correct food for your growing baby
• Helps develop your baby’s eyesight, speech and intelligence
• Lowers the risk of cot death
• Reduces the likelihood of allergy
• Saves money—no need to buy expensive formulas and feeding equipment
• Breastfed babies are healthier so you’ll save on medical bills
• Environmentally friendly—saves fuel, energy and resources
Adapted from Australian Breastfeeding Association (ABA) n.d. Why breastfeeding is important. Melbourne, ABA. Online. Available at www.breastfeeding.asn.au 30 Jun 2012.
Multidisciplinary promotion of breastfeeding in several countries has resulted in 50–60% of mothers electing to breastfeed. Many hospitals now have nurse lactation consultants who work individually with mothers for successful breastfeeding, including making home visits. The advent of portable electric breast pumps has made breastfeeding feasible for working mothers. Some employment policies allow 1 hour per 8-hour shift for ‘lactation time’.
Infection with hepatitis C, HIV or cytomegalovirus (CMV) are contraindications to breastfeeding, since these viruses have been isolated in breast milk, increasing the chance of infectious transmission to the infant.
FORMULA
Infant formulas are designed to contain the approximate nutrient composition of human milk. Protein in the formula is typically supplied as whey, soy, cow’s milk base, casein hydrolysate or elemental amino acids. The addition of nucleotides to infant formula was intended to more closely parallel human milk and boost immune function. It has been found that preterm infants fed nutrient-enriched formulas (including nucleotides) after hospital discharge have higher rates of catch-up growth than do infants fed standard formulas for full-term infants (NHMRC, 2003). However, there are no definitive findings in regard to immune development. No comparison was done with breast milk.
Regular cow’s milk should not be used for infant formula during the first year of life; it may cause GI bleeding and is too concentrated for the infant’s kidneys to manage. The NHMRC has released a reference document entitled Infant feeding guidelines for health workers. This document alerts health workers to the link between cow’s milk given in the first 6 months of life and the later development of type 1 diabetes mellitus. The document also emphasises that no supplementary feeding is necessary for a breastfed baby until it is 6 months old (NHMRC, 2003).
INTRODUCTION TO SOLID FOOD
The NHMRC’s Dietary guidelines for children and adolescents in Australia (2003) suggest the following:
• Until the infant is 6 months old, breast milk is the only nutritional requirement.
• From 6 months, solid foods are introduced slowly. Start with cereals (iron-fortified), then add vegetables, fruits and finally meats.
• Add only one food at a time. Wait 5–10 days before introducing anything new.
• If there is a history of allergies in the family, do not introduce allergenic foods until the child is considerably older—up to 3 years. Foods to delay introducing include cow’s milk and dairy products, soy milk, nuts, egg white, fish and shellfish (see Working with diversity).
• Foods not suitable for infants and small children include honey, tea, fruit juices (whole fruit is preferable), cow’s milk and reduced fat milks.
When introducing solid foods, the digestibility and safety of the food must be considered. Raw fruits (apples, pears), fruit with seeds (kiwifruit, passionfruit), vegetables and nuts can be aspirated. Foods should be cooked and well mashed during early feeding attempts.
WORKING WITH DIVERSITY FOCUS ON INFANTS AND CHILDREN
Food sensitivity is seen in young children as new foods are introduced into their diet. Foods can cause an allergy or an intolerance. Common foods to which children may be sensitive include:
Care should be taken when introducing any new food, but sensitisation can occur at any time, so a food sensitivity might not be apparent until the child has had the food a few times.
Data from Hockenberry M, Wilson D 2007 Wong’s Nursing care of infants and children, ed 8. St Louis, Mosby.
Toddlers and preschoolers
The growth rate slows during the toddler years (1–3). The toddler needs fewer kilojoules but an increased amount of protein in relation to bodyweight; consequently, appetite may decrease at 18 months of age. Growth does not occur evenly in children but rather in spurts, which means that protein intakes should be sufficient to meet the high demand periods when weight gain is maximal. Toddlers exhibit strong taste preferences and become picky eaters with food fads. Small, frequent meals—breakfast, lunch and dinner with three interspersed high-nutrient-density snacks—may improve nutritional intake. The amount of food consumed by young children can vary greatly from day to day. The quality of the food consumed is more important than the quantity (Hockenberry and Wilson, 2007). Calcium and phosphorus are important for healthy bone growth. See Table 36-5 for a summary of recommended dietary intake.
Toddlers who consume more than 720 mL of milk daily in lieu of other foods may develop milk anaemia, since milk is a poor source of iron. Whole milk should be used until the toddler reaches 2 years of age, to help ensure adequate intake of fatty acids necessary for brain and neurological development. Certain foods such as nuts, boiled lollies, grapes and raw vegetables have been known to cause choking deaths, and should be avoided.
• CRITICAL THINKING
During a well-child checkup, Mrs Quan asks if she should be concerned about John, her 20-month-old son. She reports that his appetite was good until a few months ago, when he became a picky eater. She worries that he is not getting adequate nutrition. What is your response?
The dietary requirements of preschoolers (3–5 years of age) are similar to those of toddlers. They consume slightly more than toddlers, and nutrient density is more important than quantity.
School-age children
School-age children, 6–12 years old, grow at a slower and steadier rate, with a gradual decline in energy requirements per unit of bodyweight. The school-age child gains 3–5 kg in weight and 6 cm in height per year until puberty.
Despite better appetites and more varied food intake, school-age children’s diets should be carefully assessed for adequate protein and vitamins A and C (see Tables 36-3 and 36-4). School-age children often do not eat a proper breakfast and have unsupervised intake at school. A high fat, sugar and salt intake can result from too many snack foods. Neumark-Sztainer and others (2003) found that the frequency of family meals was positively associated with the intake of nutrient-rich foods and negatively associated with the consumption of soft drink.
Adolescents
During adolescence, physiological age is a better guide to nutritional needs than chronological age. Energy needs increase to meet the greater metabolic demands of growth. The daily requirement of protein also increases. Calcium is essential for the rapid bone growth of adolescence, and girls need a continuous source of iron to replace menstrual losses. Boys also need adequate iron for muscle development. Iodine supports increased thyroid activity, and use of iodised table salt assures availability. B-complex vitamins are needed to support heightened metabolic activity (see Tables 36-3 and 36-4).
The adolescent’s diet is influenced by many factors other than nutritional needs, including concern about body image and appearance, desire for independence, and fad diets. Nutritional deficiencies may occur in adolescent girls as a result of dieting and use of oral contraceptives (Table 36-8). The adolescent boy’s diet may be inadequate in total kilojoules, protein, iron, folic acid, B vitamins and iodine. Snacks provide approximately 25% of the teenager’s total dietary intake. Fast food is common and adds extra salt, fat and kilojoules. Skipping meals or eating meals with wrong choices of snacks contributes to nutrient deficiency and obesity (Hockenberry and Wilson, 2009).
TABLE 36-8 SAMPLE OF DRUG–NUTRIENT INTERACTIONS*
| DRUG CLASS | DRUG | EFFECT |
|---|---|---|
| Analgesic/narcotic | Aspirin | Absorbed directly through stomach; decreased drug absorption with food; decreased folic acid, vitamins C and K and iron absorption |
| Opiates | Decreased peristalsis; constipation | |
| Paracetamol | Decreased drug absorption with food; overdose associated with liver failure | |
| Antacid | Aluminium hydroxide | Decreased phosphate absorption |
| Sodium bicarbonate | Decreased folic acid absorption | |
| Antiarrhythmic | Amiodarone | Taste alteration |
| Digoxin | Anorexia, decreased renal clearance in older persons | |
| Propranolol | Increased drug absorption with food | |
| Antiarthritic | Methotrexate | Decreased drug absorption with food, decreased folic acid |
| Penicillamine | Taste alteration | |
| Antibiotic | Amoxicillin | Decreased drug absorption with food |
| Ampicillin | Taste alteration, decreased drug absorption with food | |
| Cephalosporin | Decreased vitamin K | |
| Clarithromycin | Taste alteration | |
| Doxycycline | Decreased drug absorption with food | |
| Gentamicin | Anorexia, decreased renal excretion in older persons | |
| Metronidazole | Anorexia | |
| Neomycin | Decreased fat, nitrogen, vitamin B12, lactose, sucrose, sodium, potassium, iron, calcium | |
| Nitrofurantoin | Increased drug absorption with food | |
| Penicillin | Decreased drug absorption with food | |
| Rifampicin | Decreased vitamin B6, niacin, vitamin D | |
| Tetracycline | Decreased drug absorption with milk and antacids, decreased nutrient absorption of calcium, riboflavin, vitamin C due to binding | |
| Trimethoprim/sulfamethoxazole | Decreased folic acid | |
| Anticoagulant | Warfarin | Acts as antagonist to vitamin K |
| Anticonvulsant | Carbamazepine | Increased drug absorption with food |
| Phenobarbitone | Decreased drug absorption with food, decreased vitamin D | |
| Phenytoin | Decreased calcium absorption; decreased vitamins D and K and folic acid; taste alteration; decreased drug absorption with food | |
| Primidone | Decreased calcium absorption, increased metabolism of vitamins D and K | |
| Antidepressant | Amitriptyline | Appetite stimulant |
| Clomipramine | Taste alteration, appetite stimulant | |
| Fluoxetine (selective serotonin re-uptake inhibitors [SSRIs]) | Taste alteration, anorexia | |
| Antifungal | Amphotericin B | Anorexia |
| Griseofulvin | Taste alteration, enhanced absorption with food | |
| Antigout | Allopurinol | Taste alteration |
| Colchicine | Decreased vitamin B12, vitamin A (carotene), lactose, sodium, potassium | |
| Antihistamine | Astemizole | Increased appetite, decreased drug absorption with food |
| Cyproheptadine | Increased appetite | |
| Antihypertensive | Atenolol | Taste alteration (weight gain for all beta-blockers) |
| Captopril | Taste alteration, anorexia | |
| Hydralazine | Enhanced drug absorption with food, decreased vitamin B6 | |
| Methyldopa | Decreased vitamin B12, folic acid, iron | |
| Anti-inflammatory | All steroids | Increased appetite and weight, increased folic acid, decreased calcium (osteoporosis with long-term use), promotes gluconeogenesis of protein |
| Indomethacin | Decreased iron absorption | |
| Sulphasalazine | Decreased folic acid | |
| Antimanic | Lithium carbonate | Anorexia, nausea, vomiting, diarrhoea, mucositis, decreased folic acid |
| Antiparkinson | Levodopa | Taste alteration, decreased vitamin B6 and drug absorption with food |
| Antipsychotic | Chlorpromazine | Increased appetite |
| Thiothixene | Decreased riboflavin, increased need | |
| Antituberculosis | Isoniazid | Decreased calcium, niacin, vitamins B6 and D |
| Bronchodilator | Albuterol sulfate | Appetite stimulant |
| Theophylline | Anorexia | |
| Cholesterol-lowering | Cholestyramine | Decreased fat-soluble vitamins (A, D, E, K); vitamin B12; iron |
| Diuretic | Furosemide | Decreased drug absorption with food |
| Spironolactone | Increased drug absorption with food | |
| Thiazides | Decreased magnesium, zinc and potassium | |
| Triamterene | Decreased folic acid | |
| Oestrogen/progestin | Oral contraceptive | Decreased vitamin B6, B12, folic acid, zinc; increased transferrin |
| Hormone replacement therapy (HRT) | ||
| Laxative | Mineral oil | Decreased absorption of fat-soluble vitamins (A, D, E, K), carotene |
| Phenolphthalein | Decreased calcium, potassium, vitamin D | |
| Muscle relaxant | Baclofen | Taste alteration |
| Dantrolene | Taste alteration, anorexia | |
| Platelet aggregate inhibitor | Dipyridamole | Decreased drug absorption with food |
| Potassium replacement | Potassium chloride | Decreased vitamin B12 |
| Stimulant | Dexamphetamine | Taste alteration, anorexia |
| Methylphenidate | Anorexia, decreased weight, decreased growth | |
| Tranquilliser | Benzodiazepines | Increased appetite |
*Not intended to be an exhaustive or all-inclusive list. Always check pharmacology references before administering medications.
Fortified foods (nutrients added) are important sources of vitamins and minerals. Snack food from the dairy and fruit/vegetable groups are good choices. To counter obesity, increasing physical activity is often more important than curbing intake. The onset of eating disorders such as anorexia nervosa or bulimia nervosa often occurs during adolescence. Recognition of eating disorders (Box 36-4) is essential for early intervention.
BOX 36-4 DIAGNOSTIC CRITERIA FOR EATING DISORDERS
ANOREXIA NERVOSA
A. Refusal to maintain bodyweight over a minimal normal weight for age and height, e.g. weight loss leading to maintenance of bodyweight less than 85% of ideal bodyweight; or failure to make expected weight gain during period of growth, leading to bodyweight less than 85% of that expected.
B. Intense fear of gaining weight or becoming fat, although underweight.
C. Disturbance in the way in which one’s bodyweight, size or shape is experienced, e.g. the person claims to ‘feel fat’ even when emaciated, believes that one area of the body is ‘too fat’ even when obviously underweight.
D. In females, absence of at least 3 consecutive menstrual cycles when otherwise expected to occur (primary or secondary amenorrhoea). (A woman is considered to have amenorrhoea if her periods occur only following hormone, e.g. oestrogen, administration.)
BULIMIA NERVOSA
A. Recurrent episodes of binge-eating (rapid consumption of a large amount of food in a discrete period of time).
B. A feeling of lack of control over eating behaviour during the eating binges.
C. The person regularly engages in self-induced vomiting, use of laxatives or diuretics, strict dieting or fasting or vigorous exercise in order to prevent weight gain.
D. A minimum average of 2 binge-eating episodes a week for at least 3 months.
From American Psychiatric Association (APA) 1994 Diagnostic and statistical manual of mental disorders, ed 4 revised. Washinton DC, APA.
Sports and regular moderate-to-intense exercise necessitate dietary modification to meet increased energy needs for adolescents. Carbohydrates, both simple and complex, should be the main source of energy, providing 55–60% of total daily kilojoules. Protein needs are increased to 1.0–1.5 g/kg/day. Fat needs are not increased. Adequate hydration is very important for all athletes. Water should be ingested before and after exercise to prevent dehydration, especially in hot, humid environments. Vitamin and mineral supplements are not required, but intake of iron-rich foods is needed to prevent anaemia.
Parents often have more influence on the adolescent diet than they believe. Effective strategies include limiting the amount of unhealthy food choices kept at home and enhancing the appearance and taste of healthy foods. Making healthy food choices more convenient and available and working to change social norms of what foods are ‘cool’ are also ways to promote optimal nutritional health in adolescents (Hockenberry and Wilson, 2007).
Pregnancy occurring within 4 years of menarche may place mother and fetus at risk because of anatomical and physiological immaturity. Malnutrition at the time of conception increases risk to the adolescent and her fetus. Most teenage girls do not want to gain weight. Counselling related to nutritional needs of pregnancy may be difficult, and suggestions are better tolerated than rigid directions. The diet of pregnant adolescents is often deficient in calcium, iron and vitamins A and C. Prenatal vitamin and mineral supplements are recommended.
Young and middle-aged adults
The demands for most nutrients are reduced as the growth period ends. Mature adults need nutrients for energy, maintenance and repair. Energy needs usually decline over the years. Obesity may become a problem due to decreased physical exercise, dining out more often and increased ability to afford more luxury foods. Adult women who use oral contraceptives may need extra vitamins. Iron and calcium intake continues to be important. Table 36-7 shows the required servings of each food group per day.
PREGNANCY
Poor nutrition during pregnancy can cause low birthweight in infants and decreased chances of survival. Generally, the fetus’s needs are met at the expense of the mother. However, if nutrient sources are not available, both suffer. The nutritional status of the mother at the time of conception is important. Significant aspects of fetal growth and development often occur before pregnancy is even suspected.
The energy requirements of pregnancy are related to the mother’s bodyweight and activity. An average weight gain of 11–14 kg occurs during pregnancy. Rigid recommendations about weight gain should be avoided. Pregnant women should be cautioned against fasting as a method of weight control, because fasting may lead to ketoacidosis (metabolic acidosis caused by excess build-up of ketone bodies) which can be dangerous to the fetus as well as the mother. The quality of nutrition during pregnancy is more important than weight gain per se or kilojoules consumed per day. Food intake in the first trimester should include balanced portions of essential nutrients with emphasis on quality. Protein intake throughout pregnancy is increased to 60 g.
Calcium intake is especially critical in the third trimester, when fetal bones are mineralised. Iron may be supplemented to provide for increased maternal blood volume, for fetal blood storage and for blood loss during delivery. Iodine needs increase 15–17% because of increased activity of the thyroid gland. Folic acid intake is particularly important for DNA synthesis and the growth of red blood cells. Folate is particularly important in the very early stages of pregnancy as the neural tube of the fetus is formed. This often occurs before women know they are pregnant and, therefore, folic acid supplements are recommended in the month preceding conception as well as in the first trimester. Inadequate intake may lead to fetal neural tube defects, as well as anencephaly or maternal megaloblastic anaemia (NHMRC, 2005). Prenatal care usually includes vitamin and mineral supplementation to ensure daily intakes; however, pregnant women should not take supplements beyond prescribed amounts. For example, vitamin A is essential to maternal and fetal health but is teratogenic (leading to the increased risk of birth defects) when consumed to excess (Langstroth and others, 2011).
Pregnant women should drink at least eight glasses of water daily. They should avoid artificial sweeteners, alcohol, excessive caffeine and all drugs not specifically ordered. Adequate fluid and fibre intake, in addition to moderate exercise, helps prevent the constipation commonly associated with pregnancy.
LACTATION
The lactating woman needs 2090 kJ/day above the usual allowance. The production of milk increases energy requirements. Protein requirements increase to 65 g/day. The need for calcium remains the same as during pregnancy. There is an increased need for vitamins A and C. Daily intake of water-soluble vitamins (B and C) is needed to ensure adequate levels in breast milk. Fluid intake should be adequate but need not be excessive. Caffeine, alcohol, nicotine by-products and drugs are excreted in breast milk and should be avoided. Tobacco use can decrease milk production (Hockenberry and Wilson, 2007).
Older adults
Adults 65 years and older have a decreased need for energy, as metabolic rate slows with age. However, vitamin and mineral requirements remain unchanged from middle adulthood. Numerous factors influence the nutritional status of the older adult. Income is significant, because living on a fixed income may reduce the amount of money available to buy food. Health is another important influence. The older adult may be on a therapeutic diet or have difficulty eating because of physical symptoms, dentures or lack of teeth or be at risk of drug–nutrient interactions. More teeth per patient are lost to periodontal disease than any other reason. The key periodontal disease risk indicators are age, male gender, smoking, lack of professional maintenance, inadequate oral hygiene, diabetes mellitus, hypertension, rheumatoid arthritis and anterior tooth type (Al-Shammari and others, 2005). See Working with diversity for a review of factors affecting nutritional status. Thirst sensation may diminish, leading to inadequate fluid intake or dehydration (see Chapter 38). Meats may be avoided because of cost or because they are difficult to chew.
WORKING WITH DIVERSITY FOCUS ON OLDER ADULTS
Modified from Linton A, Lach H 2007 Gerontological nursing: concepts and practice, ed 3. St Louis, Saunders.
Cream soups and meat-based vegetable soups are nutrient-dense sources of protein. Cheese, eggs and peanut butter are also useful high-protein alternatives. Milk continues to be an important food for older people, who need adequate calcium to protect against osteoporosis (a decrease of bone mass density). Statistics identify that 6% of older women and 3% of older men in the community are underweight (Holmes, 2006). The diet of older adults should contain choices from all food groups and may require a vitamin and mineral supplement.
Good nutrition for older adults is important in minimising morbidity and premature death and in maintaining an independent lifestyle for as long as possible. Healthcare costs increase sharply with age and many of these costs are incurred in treating diet-related problems. Appropriate nutrition has the potential to reduce the number of hospital admissions, to shorten the length of hospital stays and to improve outcomes from community-managed care. This will become even more important in the future because the proportion of Australians aged over 65 years is increasing more rapidly than any other age group.
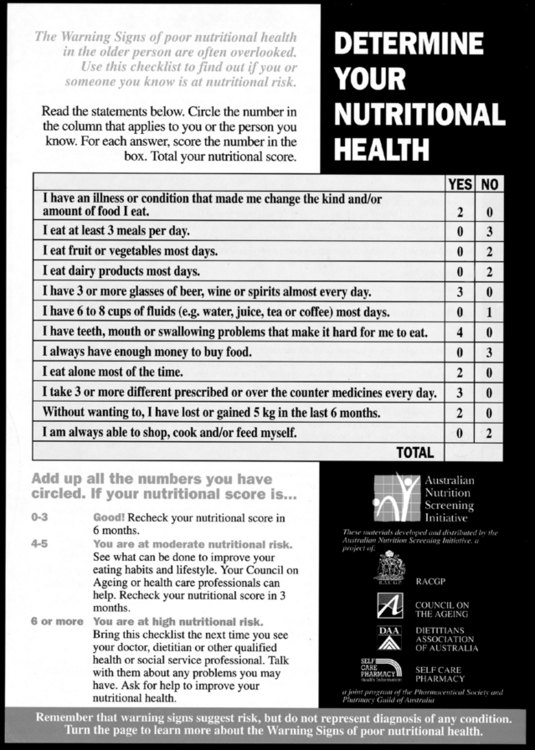
Around 7% of older Australians live in residential care (Australian Institute of Health and Welfare, 2010), and even more receive assistance with meal preparation; the Australian guidelines include additional information for meal-assisted older people and residents of aged-care accommodation. The principles that underlie the guidelines are also generally applicable to Indigenous Australians aged over 65 years. The guidelines contain nutritional screening tools, including the Australian Nutrition Screening Initiative, which identify warning signs of malnutrition in older adults. Twelve key risk factors for determining nutritional health appear in the checklist (Figure 36-7).
Alternative food patterns
Long before recommended allowances and guidelines were issued, many people followed special patterns of food intake based on religion and cultural background (see Working with diversity boxes), ethics, health beliefs, personal preference or concern for the efficient use of land to produce food. Such special diets are not necessarily more or less nutritious than diets based on the food pyramid or other nutritional guidelines, because good nutrition depends on a balanced intake of all required nutrients. A common alternative dietary pattern is the vegetarian diet.
Vegetarianism is the consumption of a diet consisting predominantly of plant foods. Vegetarians may be ovolacto-vegetarian (avoid meat, fish and poultry but eat eggs and milk), lactovegetarians (drink milk but avoid eggs) or vegans (consume only plant foods). Vegan, zen macrobiotic (consume mainly brown rice, other grains and herb teas) and fruitarian (eat only fruit, nuts, honey and olive oil) diets are nutrient-poor and can result in malnutrition. Knowledge related to complementary use of complete and incomplete proteins is necessary (Box 36-5). Children who follow a vegetarian diet are especially at risk of protein and vitamin deficiencies, such as vitamin B12.
BOX 36-5 COMPLETE VERSUS INCOMPLETE PROTEIN SOURCES
FOODS CONTAINING COMPLETE PROTEINS
Fish, shellfish, chicken, turkey, duck, beef, lamb, pork
Hard cheeses: Muenster, Swiss cheese
FOODS CONTAINING INCOMPLETE PROTEINS
Wheat, rice, corn, oats/oatmeal, barley, pasta, bagels, bread
Lentils, beans, peanuts/peanut butter, chickpeas, split peas
FOOD COMBINATIONS THAT PROVIDE COMPLETE PROTEIN
Adapted from Grodner M and others 2007 Foundations and clinical applications of nutrition: a nursing approach, ed 4. St Louis, Mosby.
Alternative or complementary therapies are now becoming more accepted (see Chapter 32). Many involve nutrition. Alternative therapists have their own professional organisations, such as the Australian Traditional Medicine Society (ATMS) which represents about 65% of the total complementary medicine profession (ATMS, 2011).
WORKING WITH DIVERSITY FOCUS ON CULTURAL CARE
RELIGIOUS DIETARY REQUIREMENTS
WORKING WITH DIVERSITY Focus on cultural care
LACTOSE INTOLERANCE
The incidence of lactose intolerance around the world occurs from high to low in the following ethnic or racial groups: Asian-Pacific, African, Mexican, Middle Eastern, followed by white Caucasian. This condition affects nutrient absorption, and calcium deficiency results. Calcium is necessary for maintaining bone mass density. Alternative sources of calcium with low lactose are aged cheddar or Swiss cheese, green leafy vegetables, legumes, tofu, sardines, nuts and low-lactose milk products.
‘HOT’ AND ‘COLD’ FOODS
The theory of hot and cold foods predominates in many cultures. The origin appears to be from Hippocratic beliefs concerning health and the four humours. Arabs were keepers of this knowledge during the Dark Ages and later influenced the Spanish to adopt this belief system in the later Middle Ages. The foundation is keeping harmony with nature by balancing ‘cold’, ‘hot’, ‘wet’ and ‘dry’. Some cultures may plan their meals based on these beliefs. Food classification as hot or cold varies slightly from one culture to another.
Classification has nothing to do with spiciness but is a symbolic representation of temperature. Hot foods include rice, grain cereals, alcohol, beef, lamb, chillies, chocolate, cheese, temperate-zone fruits, eggs, peas, goat’s milk, oils, onions, pork and radishes. In contrast, cold foods encompass beans, citrus fruits, tropical fruits, dairy products, most vegetables, honey, raisins, chicken, fish and goat. Foods can be made hot or cold through methods of preparation. A blending of hot and cold balances food. Menstruation, cancer, pneumonia, earache, colds, paralysis, headache and rheumatism are cold illnesses requiring hot foods. Pregnancy, fever, infections, diarrhoea, rashes, ulcers, liver problems, constipation, kidney problems and sore throats are believed to be hot conditions; thus cold foods may be eaten during these times.
Modified from Giger J, Davidhizar R 2008 Transcultural nursing: assessment and intervention, ed 5. St Louis, Mosby.
Alcohol
Alcoholic beverages are consumed on a regular basis by 42% of adult men and 24% of adult women in Australia. Alcohol contributes approximately 5% of the energy intake of adult Australians. The consumption of alcohol declines with age, as does the safe limit of consumption. Ethyl alcohol is a nutrient but is also a drug affecting the brain, and if consumed in amounts above the socially beneficial dose, becomes a toxin to many organs in the body. As well, alcohol can be morbidly or even mortally incompatible with many medications and over-the-counter drugs. The effects of alcohol on the brain combined with the toxic effects make it responsible for 1 death in every 34 in Australia (Lobo and others, 2010). Alcohol does have health benefits if consumed in small regular amounts (1–2 standard drinks/day on most days). Older people, especially, benefit from the protective effect that small amounts of daily alcohol have against coronary artery disease and impaired cognitive function. One study shows that the risk of cognitive impairment was reduced by 20% for those that drank moderately (Lobo and others, 2010).
Critical thinking synthesis
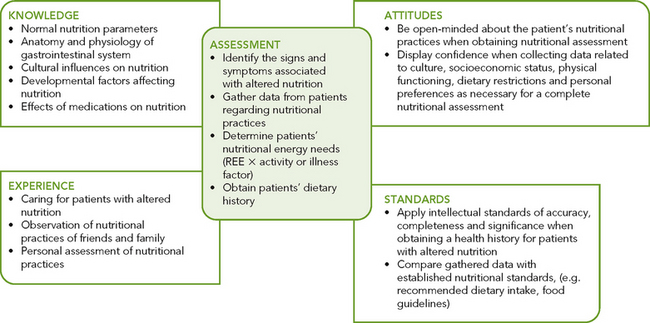
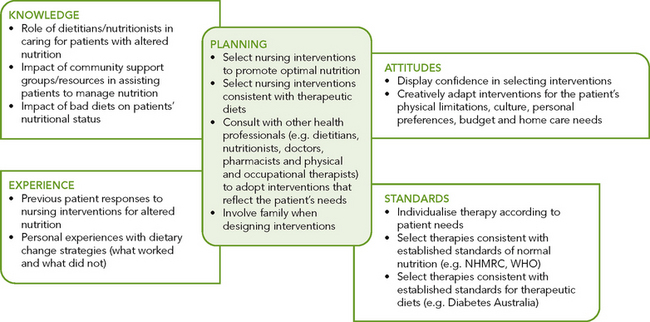
Successful critical thinking requires a synthesis of knowledge, experience, information collected from patients, critical-thinking attitudes, and intellectual and professional standards. Clinical judgments require the nurse to anticipate the required information, analyse the data and make decisions regarding patient care. Critical thinking is a dynamic process. During assessment (Figure 36-8), the nurse must consider all elements that build towards making appropriate nursing diagnoses.
In the case of nutrition, the nurse must integrate knowledge from nursing and other disciplines, previous experiences, and information gathered from patients and families regarding customary food preferences, as well as recent dietary history. The use of professional standards, such as RDIs (Tables 36-3, 36-4 and 36-5), the Australian guide to healthy eating, dietary guidelines such as those in Box 36-2 and the number of daily servings (Table 36-7) provide help in maintaining good health. Other professional organisations such as the Heart Foundation and Diabetes Australia or Diabetes New Zealand provide valuable information on nutrition. This information is research-based and continually updated for optimal patient care.
As part of being an advocate for good nutrition, the nurse should be also consuming a healthy diet. When nurses are in a state of good health, it enables them to effectively care for their patients.
NURSING PROCESS AND NUTRITION
Nurses are in an excellent position to recognise signs of poor nutrition and to take steps to initiate change. Close contact with patients and their families enables nurses to make observations about physical status, food intake, weight changes and response to therapy.
ASSESSMENT
Early recognition of malnourished or at-risk patients has a strong positive influence on both short- and long-term health outcomes (Bocock and others, 2008). Assessment of nutritional status is essential due to the common need of all human beings for nutrients, energy and fluids. Nutrition assessment centres on five major areas: anthropometry, laboratory tests, dietary and health history, clinical observation and patient expectations.
Anthropometry
Anthropometry is a measurement system of the size and makeup of the body. Anthropometric measurements that aid in identifying nutritional problems include the ratio of height to wrist circumference, mid-upper-arm circumference (MAC), triceps skinfold (TSF) and mid-upper-arm muscle circumference (MAMC). Significant variation may result unless the examiner is skilled and has proper equipment. Values for MAC, TSF and MAMC are compared with standards and calculated as a percentage of the standard. Changes in values for an individual over time are of greater significance than isolated measurements.
Height and weight should be obtained for each patient on hospital admission or entry to any healthcare setting. If height cannot be measured with the patient standing, position the patient lying flat in bed as straight as possible, arms folded across the chest, and measure the patient lengthwise. If possible, the patient should be weighed at the same time each day, on the same scale and with the same clothing or linen. Rapid weight gain usually reflects fluid shifts. One litre of fluid approximately equals one kilogram. Height and weight can be compared with standards for height–weight relationships. Recent weight changes should be documented.
BODY MASS INDEX
Body mass index (BMI) measures weight corrected for height, and serves as an alternative to traditional height–weight relationships. Calculation of BMI is achieved by dividing the patient’s weight in kilograms by their height in metres squared. A BMI of less than 20 places a patient at higher medical risk of morbidity and prolonged hospitalisation; a BMI of greater than 30 places a patient at higher medical risk of coronary heart disease, some cancers, diabetes mellitus and hypertension, and increased morbidity with major operations (Lutz and Przytulski, 2011). Both high and low BMIs are associated with low functional and health status, especially among adults of 65 years and older or hospitalised adults (Schenkler and Roth, 2011).
• CRITICAL THINKING
Jean, aged 35, has just had surgery for a bowel obstruction. Her medical history includes Crohn’s disease. Before this exacerbation, 3 months ago, Jean’s weight was 55.8 kg. Admission weight was 52.2 kg; 3 days after surgery she now weighs 49.0 kg. Her height is 165 cm. Reported laboratory values are white blood cell count 8.5 × 109/L, lymphocytes 1.1 × 109/L and albumin 23 g/L.
BIOELECTRICAL IMPEDANCE ANALYSIS (BIA)
This technique is non-invasive and is increasingly replacing traditional anthropometric methods, but it is not available in all healthcare settings. Assessment is derived from measurement of an innocuous electrical current that travels from one (of four) externally attached pole to another (placed distally on each arm and leg). The speed of current is different for lean versus fat tissue. BIA is considered to be a more direct and immediate measure of lean body mass (Lutz and Przytulski, 2011).
Laboratory and biochemical tests
No single laboratory or biochemical test is diagnostic for malnutrition. Factors that may alter test results include fluid balance, liver function, kidney function and the presence of disease. Common laboratory tests used to study nutritional status include measures of plasma proteins such as albumin, transferrin, prealbumin, retinol-binding protein, total iron-binding capacity and haemoglobin. After feeding, the response time for changes in these proteins ranges from hours to weeks. The metabolic half-life of albumin is 21 days, of transferrin 8 days, of prealbumin 2 days and of retinol-binding protein 12 hours. This range demonstrates why albumin level, for example, is not an accurate short-term indicator of serum protein status (Pagana and Pagana, 2007). Furthermore, serum albumin levels are affected by the following factors: hydration; haemorrhage; renal or hepatic disease; high-output drainage of wounds, drains, burns or the gut; steroid administration; exogenous albumin infusions; age; and trauma, stress or surgery. In summary, albumin level is a better indicator for chronic illnesses while pre-albumin level is preferred for acute conditions.
Nitrogen balance is important for establishing serum protein status (see the discussion of protein in this chapter). Nitrogen intake is calculated by dividing the total grams of protein ingested in a day (24 hours) by 6.25. The output of nitrogen is established through laboratory analysis of a 24-hour urinary urea nitrogen (UUN). For patients with diarrhoea or fistula drainage, a further addition of 2–4 g of nitrogen output is estimated. Nitrogen balance is found by subtracting the nitrogen output from the nitrogen intake. A positive (more nitrogen is taken in than is put out) 2–3 g nitrogen balance is ideal for anabolism. By contrast, negative (more nitrogen is put out than is taken in) nitrogen balance is present when catabolic states exist, seen in either starvation or physiological stress.
Dietary history and health history
In addition to the general nursing history, the nurse obtains a more specific diet history to assess the patient’s actual or potential needs. The diet history focuses on the patient’s habitual intake of foods and liquids, as well as information about preferences, allergies and other relevant areas, such as the patient’s ability to obtain food. The nurse gathers information about the patient’s illness/activity level to determine energy needs (see Table 36-1) and compares food intake. Nursing assessment of nutrition includes health status; age; cultural background and religion (see Working with diversity boxes, above); socioeconomic status; personal preference; psychological factors; use of alcohol or illegal drugs; vitamin, mineral or herbal supplements; prescription or over-the-counter drugs (see Table 36-8); and nutrition knowledge (Grodner and others, 2007).
In outpatient settings, a food diary kept over 3–7 days may be kept by the patient. This allows the nurse to calculate nutritional intake and to compare it with RDIs to see if dietary habits are adequate. Food-frequency questionnaires may be used to establish patterns over time.
Clinical observation
Clinical observations can be among the most important aspects of a nutritional assessment. As in other kinds of nursing assessment, the nurse observes the patient for signs of nutritional alterations. Because improper nutrition affects all body systems, clues to malnutrition may be observed during physical assessment (see Chapter 27). When the general physical assessment of body systems is complete, the nurse can recheck pertinent areas to evaluate the patient’s nutritional status. The clinical signs of nutritional status (Table 36-9) provide guidelines for observation during physical assessment.
TABLE 36-9 CLINICAL SIGNS OF NUTRITIONAL STATUS
| BODY AREA | SIGNS OF GOOD NUTRITION | SIGNS OF POOR NUTRITION |
|---|---|---|
| General appearance | Alert: responsive | Listless, apathetic, cachexia, cachectic appearance |
| Weight | Weight normal for height, age, body build | Obesity or underweight appearance (special concern for underweight) |
| Posture | Erect posture; straight arms and leg | Sagging shoulders; sunken chest; humped back |
| Muscles | Well-developed, firm muscles; good tone; some fat under skin | Flaccid appearance, poor tone, underdeveloped tone; tenderness; oedema; wasted appearance; inability to walk properly |
| Nervous system control | Good attention span; lack of irritability or restlessness; normal reflexes; psychological stability | Inattention; irritability; confusion; burning and tingling of hands and feet (paraesthesia); loss of position and vibratory sense; weakness and tenderness of muscles (may result in inability to walk); decrease or loss of ankle and knee reflexes; absent vibratory sense |
| Gastrointestinal function | Good appetite and digestion; normal regular elimination; no palpable organs or masses | Anorexia; indigestion; constipation or diarrhoea; liver or spleen enlargement |
| Cardiovascular function | Normal heart rate and rhythm; lack of murmurs; normal blood pressure for age | Rapid heart rate (above 100 beats/minute), enlarged heart; abnormal rhythm; elevated blood pressure |
| General vitality | Endurance; energy, good sleep habits; vigorous appearance | Easily fatigued; lack of energy; falling asleep easily, tired and apathetic appearance |
| Hair | Shiny, lustrous appearance; firmness; strands not easily plucked, healthy scalp | Stringy, dull, brittle, dry, thin and sparse, depigmented appearance; strands that can be easily plucked |
| Skin (general) | Smooth and slightly moist skin with good colour | Rough, dry, scaly, pale, pigmented, irritated appearance; bruises; petechiae; subcutaneous fat loss |
| Face and neck | Uniform colour; smooth, pink, healthy appearance; lack of swelling | Greasy, discoloured, scaly, swollen appearance; dark skin over cheeks and under eyes; lumpiness or flakiness of skin around nose and mouth |
| Lips | Smoothness; good colour; moist (not chapped or swollen) appearance | Dry, scaly, swollen appearance; redness and swelling (cheilosis); angular lesions at corners of mouth; fissures or scars (stomatitis) |
| Mouth, oral membranes | Reddish-pink mucous membranes in oral cavity | Swollen, boggy oral mucous membranes |
| Gums | Good pink colour; healthy and red appearance; lack of swelling or bleeding | Spongy gums that bleed easily; marginal redness, inflammation; receding gums |
| Tongue | Good pink or deep reddish colour; lack of swelling; smoothness, presence of surface papillae; lack of lesions | Swelling, scarlet and raw appearance; magenta colour, beefiness (glossitis); hyperaemic and hypertrophic papillae; atrophic papillae |
| Teeth | Lack of cavities and pain; bright, straight appearance; lack of crowding; well-shaped jaw; clean appearance with no discolouration | Unfilled caries; absent teeth; worn surfaces; mottled (fluorosis), malpositioned appearance |
| Eyes | Bright, clear, shiny appearance; lack of sores at corner of membranes; eyelids moist and healthy pink colour; prominent blood vessels or lack of mound of tissue or sclera; lack of fatigue circles beneath eyes | Pale eye membranes (pale conjunctivae); redness of membrane (conjunctival infection); dryness; signs of infection; Bitot’s spots, redness and fissuring of eyelid corners (angular palpebritis); dryness of eye membrane (conjunctival xerosis); dull appearance of cornea (corneal xerosis); soft cornea (keratomalacia) |
| Neck (glands) | Lack of enlargement | Thyroid enlargement |
| Nails | Firm, pink appearance | Spoon shape (koilonychia); brittleness; ridges |
| Legs, feet | Lack of tenderness, weakness or swelling; good colour | Oedema; tender calf; tingling; weakness |
| Skeleton | Lack of malformations | Bowlegs; knock-knees; chest deformity at diaphragm; prominent scapulae and ribs |
From Schlenker E, Roth S 2011 Williams’ Essentials of nutrition and diet therapy, ed 10. St Louis, Mosby.
Patient expectations
Patients rely on healthcare professionals to identify problems of which they may not be aware. Most nutritional problems tend to develop insidiously over weeks and months, not overnight. Schaller and James (2005) studied Australian nurses’ nutritional knowledge in regional Victoria; the older nurses with more years of clinical experience scored higher average scores. The nurses’ score in this study was ‘low to moderate’ by definition based on previous studies that used the same nutrition knowledge questionnaire. The nurses indicated that they sourced nutrition information from dietitians, nurses and the Heart Foundation. A firm knowledge base is important to meet patient expectations (Grodner and others, 2007).
NURSING DIAGNOSIS
Assessment enables the nurse to determine the existence of actual or potential nutrition problems (Box 36-6). Knowledge of normal nutrition parameters, anatomy and physiology of the GI system, and cultural, developmental, pharmacological and dietary guidelines is necessary for complete assessment. A problem may occur when overall intake is significantly decreased or increased, or when one or more nutrients are not ingested, completely digested or completely absorbed. Specific diagnoses are related to the actual nutrition problem (e.g. inadequate intake), but may also involve problems that place the patient at risk of nutritional deficiencies, such as oral trauma, severe burns or infections.
NUTRITION-RELATED
Aspiration, risk of, in enteral nutrition (EN) therapy
Health-seeking behaviours (nutrition)
Infant feeding pattern, ineffective
Management of therapeutic regimen, individuals: ineffective
Nutrition, altered: less than body requirements
Nutrition, altered: more than body requirements
The nursing diagnostic statement is based on defining characteristics present in the assessment database (Box 36-7). In addition, the suspected health problem related to the nursing diagnosis is stated.
BOX 36-7 SAMPLE NURSING DIAGNOSTIC PROCESS
| NUTRITION | ||
|---|---|---|
| ASSESSMENT ACTIVITIES | DEFINING CHARACTERISTICS | NURSING DIAGNOSIS |
| Body mass index (BMI) | BMI = 17 | Altered nutrition: less than body requirements |
| Bodyweight within gender/age/height range | ||
| 24-hour food history | ||
| Fluid intake | ||
| Physical assessment | ||
| Laboratory values | Serum albumin 26 g/L; lymphocyte count 2 × 109/L | |
| Knowledge of nutrition | Unfamiliar with food pyramid or dietary guidelines | |
| Review medical history | ||
| Medication | Sertraline, captopril | |
| Diagnoses | Depression | |
| Review social history | Death of spouse 6 months ago | |
PLANNING
Planning to maintain optimal nutritional status requires a higher level of care than simply correction of problems. Synthesis of patient information from multiple sources is necessary (Figure 36-9). Critical thinking is the best way to ensure that all data sources are considered in developing a plan of care. Referring to professional standards for nutrition is especially important during this step, since published standards are based on scientific findings. The identification of patients at risk of nutritional problems should result in a care plan that will prevent or minimise nutritional problems (see Sample nursing care plan). No complications will result from nutritional therapies.
The intake of food is often altered in the perioperative period. Preoperative nutrition support should be administered to patients with malnutrition. The resumption of food intake postoperatively depends on the return of bowel function, the extent of the surgical procedure and the presence of any complications (see Chapter 43).
Patients who have had oral and throat surgery must chew and swallow food in the presence of excision sites, sutures or otherwise manipulated tissue. The ingestion of food causes discomfort, so patients are usually reluctant to eat or drink. Fluids are usually offered first. The use of a straw may help in some cases, but it is specifically contraindicated in others such as dental extractions, dental surgeries and cleft palate repairs. Soft foods are sometimes easier to swallow than liquids. Hot fluids, tart juices, spicy food and coarse food that is difficult to chew should be avoided after throat or mouth surgery. Parenteral or enteral nutrition may be required.
Nasogastric suction is often used following GI surgery to prevent distension and pressure on resected areas (see Chapter 37). When oral intake is restricted, fluids are usually given intravenously, but these fluids are characteristically nutrient-poor. Standard 5% glucose solution contains only 710 kJ/L. Gastric resections may limit the amount of food that can be ingested per meal if the remaining gastric pouch is small. Frequent small meals may be advised. Other surgeries on the stomach and intestines may require an alternative method of feeding. Intestinal surgery may interfere with absorption of nutrients (malabsorption) or the amount of stool losses if large portions of the intestine are resected or bypassed or if an ileostomy or mucous fistula is created (see Chapter 37). Patients with ileostomies may lose the ability to absorb vitamin B12 since the ileum is the site of absorption for this vitamin.
Extended immobilisation can result in deossification and osteoporosis of bones. Without weight-bearing activity, calcium leaves the bones. This further results in hypercalcaemia (see Chapter 33). Hypercalcaemia predisposes patients to kidney and bladder stones. Extended immobilisation becomes a particular problem for children and adolescents because of their rapid bone growth. Walking is the best way to prevent demineralisation of bone from immobility. When walking is not possible, adequate quantities of high-biological-value proteins help prevent skin breakdown and infections, and high phosphorus intake in the early weeks of immobilisation reduces serum calcium levels. Generous fluid intake safeguards against kidney stones. Range-of-motion exercises for uninvolved joints provide some protection.
Nutritional education and counselling are important for patients on regular diets to prevent disease and promote health.
Goals and outcomes
Patients on therapeutic diets who understand the rationale for the diet are more likely to be compliant. For this group of patients, the care plan is based on one or more of the following goals:
• Patient will return to appropriate BMI height–weight range or within 10% of ideal bodyweight.
• Patient will maintain fluid and electrolyte balance within normal limits.
• Patient will ingest or have administered a nutrition that, at a minimum, meets the RDIs.
Meeting nutritional goals requires multidisciplinary input. Knowledge of each discipline’s role in provision of nutrition support is necessary to maximise nutritional outcomes. As with any healthcare team, the doctor directs the overall plan of care: ordering diets and laboratory tests, diagnosing, monitoring and prescribing. A good plan of care requires exchange of accurate information between disciplines.
Setting priorities is difficult in the area of nutrition. Although adequate nutrition is essential for life, for wound healing and for quality of life, it is often not rated as a high priority if the person is well nourished when admitted to acute care and the patient’s body can maintain itself while more-urgent problems are overcome. Thus the priority of nutritional problems depends a great deal on the assessment of the person and the contribution that poor nutrition is making to their illness or condition.
Individualised patient planning cannot be over-emphasised. Mutually planned goals negotiated between the patient, dietitian, doctor and nurse will go a long way towards success. Obese patients tend to respond better to regular reviews and assessment of their ongoing weight management, rather than a long-term, infrequent-review approach (Tan and others, 2006).
ALTERED NUTRITION: LESS THAN BODY REQUIREMENTS
ASSESSMENT*
Mrs Cooper’s vital signs were all within normal limits. Three months had passed since Mrs Cooper had been started on sertraline for depression related to the loss of her husband 6 months ago. This was an initial episode of depression. Mrs Cooper had also been referred for counselling 3 months ago for help with grief and depression through a local senior service agency. After checking Mrs Cooper’s weight and reviewing her chart, Marie realised her client was 20% below her IBW (ideal bodyweight) and had a low BMI of 17. This weight loss had occurred in 6 months, down 11 kg. Mrs Cooper said, ‘I’m just not interested in food. It has no taste.’ Mrs Cooper also said she gets full quickly. Marie observed dull, thinning hair, dry scaling skin, pale conjunctivae and mucous membranes in addition to 12 pitting oedema bilaterally in the ankles. Mrs Cooper complained of chronic constipation and said she tires easily. Marie noted generalised poor muscle tone and a stooped posture. Laboratory data revealed a serum albumin 26 g/L; total lymphocyte count (TLC) 2 × 109/L. Laboratory values also suggested dehydration. Mrs Cooper said she drinks some juice in the morning and 2 or 3 cups of coffee. Mrs Cooper complained of loneliness, and said she does not get out much, although her psychologist recommended more socialising. She said she likes her counsellor and that she feels better but has not returned to her old self. Her friends at church call her to come back to meetings, but she is just not ready. When Marie inquired as to her financial situation, Mrs Cooper responded that it was tight living on the pension, but she was able to manage. She thanked Marie for finding a psychologist that she could afford.
NURSING DIAGNOSIS: Altered nutrition: less than body requirements related to an inability to ingest food as a result of psychological depression.
PLANNING
| GOALS | EXPECTED OUTCOMES |
|---|---|
| Patient will progressively gain weight. | Patient will gain 500 g to 1 kg a month until a goal of 60 kg is reached. |
| Patient will learn key nutritional concepts. | Patient will demonstrate an understanding of dietary guidelines. |
| Patient will consume adequate nourishment each day. | Patient will ingest 8000 kJ/day including 50 g of protein per day. |
| Patient will exhibit no signs of malnutrition. | Physical assessment and laboratory values will be within normal limits. |
| INTERVENTIONS† | RATIONALE |
|---|---|
| Nutritional counselling | |
| Successful nutrition care planning is a multidisciplinary approach throughout the continuum of care. | |
| Individualised meal planning is more useful to the patient. | |
| Frequent small meals offset early satiety. | |
| NHMRC recommendations for optimal nutrition. | |
| Nutritional monitoring | |
| Weight gain should be slow and progressive. Serum albumin > 35 g/L and TLC > 4 × 109/L (Grodner and others, 2007). | |
| Nutritional management | |
| Consistent oral hygiene promotes taste sensation. | |
| This allows for necessary energy for eating and digestion (Schlenker and Roth, 2011). | |
| SSRIs diminish taste and appetite. | |
| Older adults need eight 250-mL servings per day of fluid. Concentrating intake in morning and early afternoon is acceptable to prevent nocturia. | |
| Adequate fluid, fibre and exercise deter constipation. | |
| Meal participation would encourage good nutrition and promote socialisation with peers. |
†Intervention classification labels from Bulechek G M and others 2008 Nursing interventions classification (NIC), ed 5. St Louis, Mosby.
EVALUATION
Ask patient to identify groups depicted in the food pyramid and representative food choices.
Ask patient to re-state number of servings from each group necessary for her optimal nutrition.
Ask patient to state amount of kilojoules and protein she needs each day.
Observe and monitor physical nutrition status (weight, biochemical indicators).
*Defining characteristics are shown in bold type.
Healthcare personnel supervised by the nurse are of invaluable assistance in planning and delivering nutritional care. Meals should be delivered at a palatable temperature. The food consistency should be appropriate for the patient. For instance, patients who are very short of breath require soft-textured and easily chewed food to reduce energy expenditure. Ill patients may need assistance with tray set-up or feeding. Patients who have difficulty manipulating equipment and material will need assistance. Adapted implements are available for those who cannot use normal equipment. Nurses are responsible for seeing that patients have the equipment needed to feed themselves—wrapping material and containers may need to be removed as well. Oral care before meals and after enhances appetite. Patients may need help getting into a chair, where they may feel more like eating.
Collaboration with a registered dietitian ensures appropriate nutrition treatment plans. When energy intake needs to be assessed, assistance is necessary in obtaining accurate data. Laboratory tests may require all urine to be saved over a 24-hour period. Weights and heights should consistently be on each chart. Nurse assistants are also important sources of information regarding observation and assessment of the patient. Two-way communication is essential between the registered nurse and assistants, in addition to communication with personnel in other disciplines.
The nurse is responsible for coordinating and administering the plan of care. The nurse’s role in physical assessment of nutritional status is vital. The nurse also monitors dietary intake to ensure that the patient receives a nutritionally balanced diet. Documentation of patient response to therapy is also essential.
• CRITICAL THINKING
Mrs Caine is 85 years old. She has been hospitalised for a fractured left hip and is now ready for discharge. She has always been active, and she lives alone. She has no family nearby, but a few close friends. What arrangements would you make to continue her nutritional intake at home while she recovers?
The dietitian monitors the patient’s nutritional status and intake and makes recommendations for changes, based mainly on data documented in the patient’s chart. Dietitians are expert in the choice of enteral formulas and dietary modifications required for specific disease states.
The pharmacist is expert in drug–nutrient interactions and mixture of total parenteral nutrition. In addition, occupational therapists work with patients and families to identify devices that help patients eat, or to rearrange food preparation areas in an effort to maximise the patient’s functional capacity.
Continuity of care
Because changes in nutritional status usually require an extended period of time, care of the patient requiring nutritional care is long-term as well as multidisciplinary. The patient’s family will also need to be involved, because often the patient is not the person responsible for purchasing food or preparing it. Family education is crucial to the success of implementing nutritional changes. In both the Aboriginal Australian and the New Zealand Māori populations, poor nutrition is recognised as a causal agent for both communicable and non-communicable diseases. Social and poor economic circumstances for obtaining and cooking food are significant barriers to good nutrition. The one common crucial factor influencing good nutrition was the family (Abbott and others, 2010; Grant and others, 2010).
IMPLEMENTATION
Ill or debilitated patients often have poor appetites (anorexia). The ketosis that accompanies starvation is an appetite suppressant, and surgical procedures and trauma cause pain. Deficiencies in certain vitamins and minerals can cause anorexia. Nurses can help patients to understand the factors that cause anorexia and use creative approaches to stimulate appetite. During hospitalisation, diagnostic testing disrupts many mealtimes or requires nil by mouth (NBM) status before tests. Patients worried about families, finances, employment or illnesses are often not able to eat an adequate diet. Both physiological stress due to illness and emotional stress influence dietary need and intake (Box 36-8). Medications may interfere with taste, cause nausea, interfere with absorption or affect metabolism (see Table 36-8).
BOX 36-8 METABOLIC RESPONSES TO SEVERE STRESS
From Grodner M and others 2007 Foundations and clinical applications of nutrition: a nursing approach, ed 4. St Louis, Mosby.
A nurse can help stimulate the patient’s appetite. The environment may be adapted by minimising odours, attending to oral hygiene, removing reminders of treatment and positioning the patient before meals. Consultation with a dietitian is necessary. Interviewing the patient for a dietary history helps in provision of special diets with food preferences the patient is more likely to eat. Assessing patients for the need for pharmacological agents to stimulate appetite, such as cyproheptadine, or to manage symptoms that interfere with nutrition may require doctor consultation. Socialisation has a major impact on nutritional intake. Fostering a pleasant social atmosphere with family, friends or other patients helps the patient to maximise intake.
Health promotion
Nurses are in a key position to educate patients about good nutritional habits. Incorporating knowledge of nutrition into lifestyle serves as prevention against the development of many diseases. Outpatient and community-based settings may be the best locations for nursing assessment of nutritional practices and status. Early identification of potential or actual problems is the best way to avoid more-serious problems. Similarly, in other healthcare settings, patients with nutritional problems such as obesity may require help with menu planning and compliance strategies. The nurse’s role as educator often includes educating families and providing information about community resources. Providing a way of contacting a dietitian or nurse, such as telephone numbers, for follow-up questions should always be part of counselling.
Meal planning must take into account the family’s budget and different preferences of family members. Specific foods are chosen on the basis of the dietary prescription and food groups. For families on limited budgets, substitutes can be used. For example, bean or cheese dishes can often replace meat in a meal, and evaporated milk or dry skim milk can be used for cooking. The method of preparation may also be modified when it is necessary to minimise certain substances. Baking rather than frying reduces fat intake, and lemon juice or spices can be used to add flavour to low-sodium diets.
Planning menus a week in advance has several benefits. It helps ensure good nutrition or compliance with a specific diet, and helps the family stay within the allotted budget. Menus may in turn be checked by a nurse or dietitian for content. Often a simple tip can be of value in meal planning, such as advice to avoid grocery shopping when hungry, which can lead to spontaneous purchases of more-expensive or less-nutritional foods that are not included in meal plans. Food safety is also an important public health issue. Nurses should be aware of the factors related to food safety (Table 36-10 and Box 36-9).