Chapter 33 Promoting mobility
Mastery of content will enable you to:
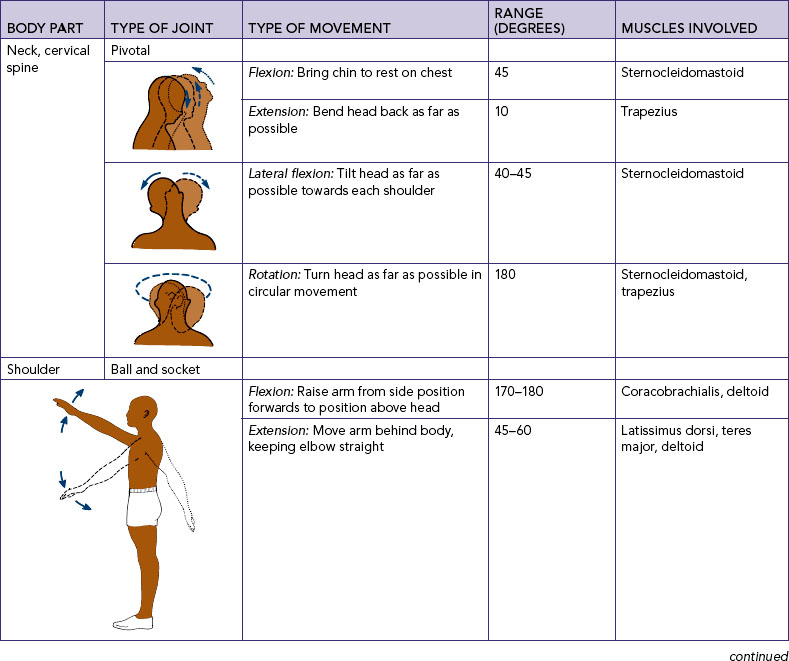
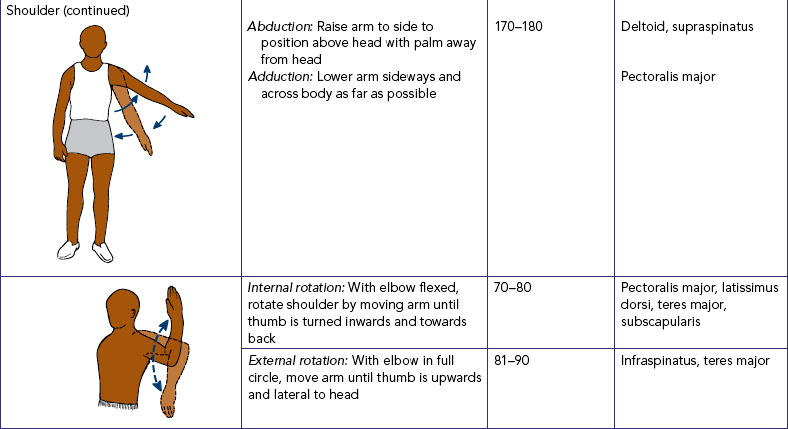
• Describe the role of musculoskeletal and nervous systems in the regulation of movement.
• Describe physiological and pathological influences on body alignment and joint mobility.
• Identify key changes in physiological and psychosocial function associated with immobility.
• Perform a focused nursing assessment of mobility and activity tolerance.
• Perform a body systems assessment for the complications of immobility.
• Describe and plan interventions for maintaining mobility and activity tolerance during the acute, restorative and continuing care of clients.
• Perform safe positioning and transfer techniques when helping a client to move up in bed, repositioning a client, helping a client into a sitting position and transferring a client from a bed to a chair or from a bed to a stretcher.
• Perform active and passive range-of-motion exercises.
• Describe essential techniques when helping a client to safely mobilise and use aids for walking.
• Describe important considerations when planning an exercise program for clients across the life span and for those with specific chronic diseases.
• Evaluate the nursing care plan for maintaining mobility and activity tolerance.
Promoting mobility and preventing immobility
Movement is often taken for granted until it is lost. Individuals experiencing health breakdown often develop problems with mobility and movement which make it difficult to get into and out of beds and chairs, stand up, sit down and walk. Losing the ability to move purposefully and easily impinges on the individual’s ability to remain physically independent in daily activities and invariably reduces quality of life.
Nurses use a range of interventions aimed at promoting mobility and movement. These typically include methods of helping patients walk, positioning of limbs, physical exercises, supportive equipment and techniques to help patients transfer from one place to another (Kneafsey, 2007). When working in acute care settings, encouraging patients to mobilise may be a low priority compared with meeting patients’ other needs. Yet, for the patient with impaired physical mobility, the resultant inactivity may lead to life-threatening complications such as a pressure injury, deep-vein thrombosis or pulmonary infection, as well as longer-term decreased functional ability.
This chapter will briefly review anatomy and physiology relating to the client’s activity–exercise pattern, outline the nursing assessment of mobility and discuss some key nursing interventions to promote mobility and movement and prevent the complications of immobility.
Scientific knowledge base
Overview of body mechanics, exercise and activity
The coordinated efforts of the musculoskeletal and nervous systems to maintain balance, posture and body alignment provide the foundation for safe and effective movement of the body during normal physical activity. Use of proper body mechanics is important for the safety and wellbeing of nurses and clients (see Table 33-1).
TABLE 33-1 BODY MECHANICS FOR HEALTHCARE WORKERS
| ACTION | RATIONALE |
|---|---|
| When planning to move a client, arrange for adequate help. Use mechanical aids | Two workers lifting together divide the workload by 50%. Mechanical aids reduce worker and client injury |
| Encourage client to help as much as possible | Promotes client’s independence and strength while minimising workload |
| Keep back, neck, pelvis and feet aligned. Avoid twisting | Reduces risk of injury to lumbar vertebrae and muscle groups. Twisting increases risk of injury |
| Flex knees; keep feet wide apart | A broad base of support increases stability |
| Position self close to client (or object being lifted) | The force is minimised. 5 kg at waist height close to body is equal to 50 kg at arms’ length |
| Use arms and legs (not back) | The leg muscles are stronger, larger muscles capable of greater work without injury |
| Slide client towards yourself using a slide sheet | Sliding requires less effort than lifting. Slide sheet minimises shearing forces, which can damage client’s skin |
| Set (tighten) abdominal and gluteal muscles in preparation for move | Preparing muscles for the load minimises strain and stabilises the trunk |
Body alignment
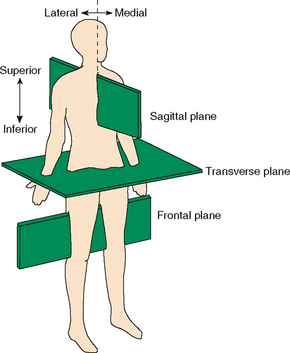
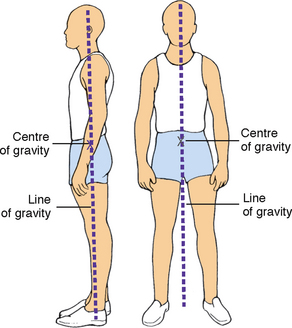
Body alignment refers to the relationship of one body part to another along a horizontal or vertical line. Correct alignment reduces strain on musculoskeletal structures, maintains adequate muscle tone and contributes to balance.
Body balance
This is achieved when a relatively low centre of gravity is balanced over a wide, stable base of support and a vertical line falls from the centre of gravity through the base of support. The base of support is the foundation. When the vertical line from the centre of gravity does not fall through the base of support, the body loses balance. Body balance is also enhanced by proper posture—the body position that most favours function, requires the least muscular work to maintain and places the least strain on muscles, ligaments and bones.
The maintenance of proper body alignment and posture is achieved by using two simple techniques. First, the base of support can easily be widened by separating the feet to a comfortable distance. Second, balance is increased by bringing the centre of gravity closer to the base of support. This is achieved by bending the knees and flexing the hips until the person is squatting and still maintaining proper back alignment by keeping the trunk erect.
The nervous system is responsible for muscle tone and regulates and coordinates the amount of pull exerted by the individual muscles.
Coordinated body movement
Coordinated body movement is a result of weight, centre of gravity and balance. Weight is the force exerted on the body mass by gravity. When an object is lifted, the lifter must overcome the object’s weight and be aware of its centre of gravity; in symmetrical objects, the centre of gravity is located at the exact centre of the object. The force of weight is always directed downwards. An object that is unbalanced has its centre of gravity away from the midline and falls without support. Because people are not geometrically perfect, their centres of gravity are usually at 55–57% of standing height and located in the midline. Like unbalanced objects, clients who fail to maintain a balance with their centre of gravity are unsteady, which places them at risk of falling.
Friction
Friction is a force that occurs in a direction opposing that of movement. As the nurse turns, transfers or moves a client up in bed, friction must be overcome. The greater the surface area of the object to be moved, the greater the friction. Friction can be reduced by following some basic principles, including using client-movement devices such as a slide sheet.
A passive or immobilised client has the potential to produce greater friction to movement. Thus, when possible, the nurse should use the client’s strength and mobility in association with the appropriate lifting aid when transferring or moving the client up in bed. This can be done by explaining the procedure and telling clients when to move. The use of a slide sheet reduces friction because the client is more easily moved along the bed’s surface.
Exercise and activity
Exercise is physical activity for the purpose of conditioning the body, improving health and maintaining fitness. It may also be used as a therapeutic measure. The exercise program chosen and developed for a client depends heavily on the individual’s activity tolerance, the kind and amount of exercise or activity that the person is able to perform. Physiological, emotional and developmental factors influence the client’s activity tolerance.
A program of regular physical activity and exercise promotes physical and psychological health (Department of Health and Ageing, 2010). An active lifestyle is important for maintaining and promoting health; it is also an essential treatment modality for many chronic diseases. A program of regular physical activity and exercise enhances functioning of all body systems, including cardiopulmonary functioning (endurance), musculoskeletal fitness (flexibility and bone integrity), weight control and maintenance (body image) and psychological wellbeing. For example, Dinas and colleagues’ (2011) review of the evidence suggests that exercise and physical activity have beneficial effects on depression symptoms that are comparable to those of antidepressant treatments.
The best program of physical activity includes a combination of exercises that produce different physiological and psychological benefits. Isotonic, isometric and resistive isometric are three categories of exercise classified according to the type of muscle contraction involved. Isotonic exercises cause muscle contraction and change in muscle length (isotonic contraction)—examples are walking, swimming, dance aerobics, jogging, bicycling, and moving arms and legs with light resistance. The benefits of isotonic exercises are increased circulation and respiratory functioning; increased osteoblastic activity (activity by bone-forming cells), thus combating osteoporosis; and increased muscle tone, mass and strength (Patton and Thibodeau, 2010).
Isometric exercises involve tightening or tensing of muscles without moving body parts (isometric contraction)—examples are quadriceps set exercises and contraction of the gluteal muscles. This form of exercise is ideal for clients who are unable to tolerate the increase in activity that is expected during isotonic exercises. Isometric exercises are easily accomplished by an immobilised client in bed. The benefits are increased muscle mass, tone and strength (thus decreasing the potential for muscle wasting); increased circulation to the involved body part; and increased osteoblastic activity (Patton and Thibodeau, 2010).
Isometric exercises may also be resistive. Resistive isometric exercises are those in which the person contracts the muscle while pushing against a stationary object or resisting the movement of an object. A gradual increase in the amount of resistance and length of time that the muscle contraction is held will increase muscle strength and endurance. Examples of resistive isometric exercises are push-ups, pushing against a footboard to move up in bed, and hip lifting. In hip lifting, the client, who is in a sitting position, pushes with the hands against a surface such as the seat of a chair and raises the hips. Resistive isometric exercises help to promote muscle strength and provide sufficient stress against bone to promote osteoblastic activity.
Regulation of movement
Coordinated body movement involves integrated functioning of the skeletal, muscular and nervous body systems. Because of the integrative nature of these three systems in mechanical support of the body, they are often considered as a single functional unit.
Musculoskeletal system
Bones perform five major functions in the body: support, protection, movement, mineral and fat storage and haematopoiesis (blood-cell formation) (Marieb and Hoehn, 2010). In the discussion of body mechanics, two of these functions—support and movement—are most important. In support, bones serve as the framework and contribute to the shape, alignment and positioning of the body parts. In movement, bones together with their joints constitute levers for muscle attachment. As muscles contract and shorten, they pull on bones, producing joint movement.
JOINTS
An articulation, or joint, is the connection between bones. Each joint is classified according to its structure and degree of mobility. On the basis of connective structures, joints are classified as fibrous, cartilaginous or synovial. Fibrous joints fit closely together and are fixed, permitting little, if any, movement. Cartilaginous joints have little movement but are elastic and use cartilage to unite separate body surfaces. Synovial joints, or true joints, are freely movable and are the most mobile, numerous and anatomically complex of the body’s joints.
LIGAMENTS, TENDONS AND CARTILAGE
These are structures that support the skeletal system. Ligaments are white, shiny, flexible bands of fibrous tissue that bind joints and connect bones and cartilage. Ligaments are elastic and aid joint flexibility and support. In some areas of the body, ligaments also have a protective function. Tendons are white, glistening, fibrous bands of tissue that connect muscle to bone. Cartilage is avascular, supporting connective tissue with the flexibility of a firm, plastic material. The characteristics of cartilage permit it to sustain weight and serve as a shock-absorber between articulating bones.
SKELETAL MUSCLE
When we walk, talk, run, breathe or participate in physical activity, we do so by the contraction of skeletal muscles. There are over 600 skeletal muscles in the body. In addition to facilitating movement, these muscles determine the form and contour of our bodies. Most of our muscles span at least one joint and attach to both articulating bones. When contraction occurs, one bone is fixed while the other moves. The origin is the point of attachment that remains still; the insertion is the point that moves when the muscle contracts (Marieb and Hoehn, 2010).
The muscles of movement are located near the skeletal region, where movement is caused by a lever system. The lever system makes the work of moving a weight or load easier. It occurs when specific bones, such as the humerus, ulna and radius, and the associated joints, such as the elbow, act as a lever. Thus, the force applied to one end of the bone to lift a weight at another point tends to rotate the bone in the direction opposite to that of the applied force. Muscles that attach to bones of leverage provide the necessary strength to move the object.
Gravity pulls on parts of the body all the time. The only way the body can be held in position is for muscles to exert a force on bones in the opposite direction. Muscles accomplish this counterforce by maintaining a low level of sustained contraction. Poor posture places more work on muscles to counteract the force of gravity. This leads to fatigue and can eventually interfere with bodily functions and cause deformities.
The antagonistic, synergistic and antigravity muscle groups are coordinated by the nervous system and maintain posture and initiate movement.
• Antagonistic muscles bring about movement at the joint. During movement, the active mover muscle contracts while its antagonist relaxes. For example, during flexion of the arm the active mover, the biceps brachii, contracts and its antagonist, the triceps brachii, relaxes. During extension of the arm the active mover, now the triceps brachii, contracts and the new antagonist, the biceps brachii, relaxes.
• Synergistic muscles contract to accomplish the same movement. When the arm is flexed, the strength of the contraction of the biceps brachii is increased by contraction of the synergistic muscle, the brachialis. Thus with synergistic muscle activity there are now two active movers—the biceps brachii and the brachialis—which contract while the antagonistic muscle, the triceps brachii, relaxes.
• Antigravity muscles are involved with joint stabilisation. These muscles continuously oppose the effect of gravity on the body and permit a person to maintain an upright or sitting posture. In an adult, the antigravity muscles are the extensors of the leg, the gluteus maximus, the quadriceps femoris, the soleus muscles and the muscles of the back.
Skeletal muscles support posture and carry out voluntary movement. The muscles are attached to the skeleton by tendons, which provide strength and permit motion. The movement of the extremities is voluntary and requires coordination from the nervous system.
Nervous system
Movement and posture are regulated by the nervous system. The major voluntary motor area, located in the cerebral cortex, is the precentral gyrus. A majority of motor fibres descend (via pyramidal pathways) from the motor cortex and cross at the level of the medulla. Thus the motor fibres from the right motor cortex initiate voluntary movement for the left side of the body, and vice versa. The cerebellum and basal ganglia integrate information from the motor cortex as well as sensory input to plan and coordinate complex motor activities (Marieb and Hoehn, 2010).
Transmission of impulses from the nervous system to the musculoskeletal system is an electrochemical event. The neurotransmitter acetylcholine transfers the electric impulse from the nerve across the neuromuscular junction to stimulate the muscle, causing contraction.
PROPRIOCEPTION
Proprioception is the awareness of the position of the body and its parts. Proprioceptors are specialised receptors located in skeletal muscles, tendons, joints, ligaments and connective-tissue coverings of bones and muscles (Marieb and Hoehn, 2010). During daily activities, proprioceptors constantly advise the brain of our body movements and position by monitoring how much the tissues containing the receptors are stretched.
BALANCE
Balance centres in the central nervous system (i.e. vestibular nuclei in the brain stem and cerebellum) respond to information from three main sources about the body’s position in space. The vestibular apparatus in the inner ear (receptors in the semicircular canals and vestibule) respond to changes in body position and send signals to the brain. Balance centres also receive input through vision as well as somatic receptors, such as proprioceptors (Marieb and Hoehn, 2010). These centres initiate reflexes that fix the eyes on objects and activate muscles to maintain balance.
Pathological influences on mobility
Many pathological conditions affect mobility. Although a complete description of each is beyond the scope of this chapter, an overview of four pathological influences is presented here: postural abnormalities, impaired muscle development, damage to the central nervous system and direct trauma to the musculoskeletal system. Common abnormal assessment findings of the musculoskeletal system are presented in Table 33-2.
TABLE 33-2 COMMON ASSESSMENT ABNORMALITIES OF THE MUSCULOSKELETAL SYSTEM
| FINDING | DESCRIPTION | POSSIBLE AETIOLOGY AND SIGNIFICANCE |
|---|---|---|
| Ankylosis | Scarring within a joint leading to stiffness or fixation | Chronic joint inflammation |
| Atrophy | Wasting of muscle, characterised by decreased circumference and flabby appearance leading to decreased function and tone | Muscle denervation, contracture, prolonged disuse as a result of immobilisation |
| Contracture | Resistance of movement of muscle or joint as a result of fibrosis of supporting soft tissues | Shortening of muscle or ligaments, tightness of soft tissue, incorrect positioning of immobilised extremity |
| Crepitation (crepitus) | Crackling sound or grating sensation as a result of friction or broken bone or cartilage bits in joint | Fracture, dislocation, chronic inflammation, osteoarthritis |
| Effusion | Fluid in joint possibly with swelling and pain | Trauma, especially to knees; inflammation |
| Ganglion | Small fluid-filled synovial cyst usually on dorsal surface of wrist or foot | Degeneration of connective tissue close to tendons and joints leading to formation of small cysts |
| Hypertrophy | Increase in size of muscle as a result of enlargement of existing cells | Exercise or other increased stimulation, increased androgens |
| Kyphosis (dowager’s hump) | Anteroposterior or forward bending of thoracic spine with convexity of curve in posterior direction | Poor posture, tuberculosis, arthritis, osteoporosis, growth disturbance of vertebral epiphyses |
| Lordosis | Lumbar spinal deformity resulting in anteroposterior curvature with concavity in posterior direction | Secondary to other spinal deformities, muscular dystrophy, obesity, flexion contracture of hip, congenital dislocation of hip |
| Pes planus | Flatfoot | Congenital condition, muscle paralysis, mild cerebral palsy, early muscular dystrophy |
| Scoliosis | Deformity resulting in lateral curvature of thoracic spine | Idiopathic or congenital condition, fracture or dislocation, osteomalacia |
| Subluxation | Partial dislocation of joint | Instability of joint capsule and supporting ligaments (e.g. from trauma, arthritis) |
| Valgus (bow legs) | Angulation of bone away from midline | Alteration in gait, pain, arthritis |
| Varus (knock-knees) | Angulation of bone towards midline | Alteration in gait, pain, arthritis |
From Brown D, Edwards H, editors, Lewis’s Medical–surgical nursing: assessment and management of clinical problems. ed 3. Sydney, Mosby.
Postural abnormalities
Congenital or acquired postural abnormalities affect the efficiency of the musculoskeletal system, as well as body alignment, balance and appearance. During assessment, the nurse observes body alignment and range of motion (ROM). Postural abnormalities can cause pain and impair alignment and mobility. Some postural abnormalities may limit ROM. Nurses intervene to maintain maximum ROM in unaffected joints and then may design interventions to strengthen affected muscles and joints, improve the patient’s posture and adequately use affected and unaffected muscle groups. Referral to and/or collaboration with a physiotherapist may enhance the nurse’s interventions for a patient with a postural abnormality.
Impaired muscle development
Injury and disease can lead to numerous alterations in musculoskeletal function. The muscular dystrophies are a group of familial disorders that cause degeneration of skeletal muscle fibres. The most prevalent of the muscle diseases in childhood, the muscular dystrophies are characterised by progressive, symmetrical weakness and wasting of skeletal muscle groups, with increasing disability and deformity (Nash, 2011).
Damage to the central nervous system
Damage to any component of the central nervous system that regulates voluntary movement results in impaired body alignment and mobility. Neurological diseases such as multiple sclerosis and Parkinson’s disease can cause progressive mobility problems. The motor cortex can be damaged by trauma such as a head injury, stroke or meningitis. Motor impairment is directly related to the location and amount of destruction of the motor cortex. For example, a person with a right-sided cerebral haemorrhage with complete necrosis is likely to have destruction of the right motor cortex and left-sided hemiplegia.
Trauma to the descending pathways in the spinal cord involved in motor control, such as the pyramidal (corticospinal) tracts, also impairs mobility. The most common trauma is transection of the spinal cord in which motor fibres are damaged. If the injury is complete, it is likely to cause a complete bilateral loss of voluntary motor control below the level of the trauma. Spinal cord trauma frequently results from motor vehicle accidents, gunshot or knife wounds to the neck and back.
Direct trauma to the musculoskeletal system
Direct trauma to the musculoskeletal system can result in contusions, sprains and fractures. A fracture is a disruption of bone tissue continuity. Fractures most commonly result from direct external trauma, but they can also occur as a consequence of some deformity of the bone (e.g. pathological fractures of osteoporosis, Paget’s disease or osteogenesis imperfecta). As the fracture heals, bone begins to repair. The fractured bone initiates a cellular process that results in bone formation. Young children are able to form new bone more easily than adults and, as a result, have few complications after a bone fracture. Treatment includes positioning the fractured bone in proper alignment and immobilising it to promote healing and to restore function. Immobilisation results in some muscle atrophy, loss of tone and joint stiffness.
Acquired or congenital conditions that affect the structure of the musculoskeletal or nervous system impair body alignment or joint mobility. Impairment can be temporary or permanent. Regardless of the duration of the impairment, the nursing care plan includes interventions that maintain the present level of alignment and joint mobility and/or increase the patient’s level of motor function.
Nursing knowledge base
Complications of immobility
Fully understanding mobility requires more than an overview of normal body mechanics and the regulation of movement by the musculoskeletal and nervous systems. Having knowledge of how immobility affects physical and psychosocial functioning can help you prevent, assess for and manage complications caused by impaired mobility. Putting this nursing knowledge and skill into practice can mean the difference between patient recovery and independence, and costly and life-threatening complications, functional decline and disability.
Nurses have always been concerned with the clinical problems caused by immobility and have developed a body of knowledge over time. It is instructive to read a collection of classic articles published almost half a century ago in the American Journal of Nursing, entitled ‘The hazards of immobility’, which summarised the physiological changes that occur in healthy, ill and injured people who undergo bed rest (Olson, 1967). The articles described the detrimental effects of immobility on cardiovascular, respiratory, gastrointestinal, musculoskeletal, urinary, metabolic and psychosocial health, with implications for nursing practice. Today there is a large and growing body of nursing research examining the effectiveness of interventions to prevent and manage the complications of immobility.
Mobility refers to a person’s ability to move about freely, whereas immobility refers to the inability to move about freely. Mobility and immobility are best understood as the end points on a continuum. Some patients move back and forth on this continuum, but for other patients immobility is absolute and continues indefinitely. The terms ‘bed rest’ and ‘impaired physical mobility’ are frequently used when discussing patients on the mobility–immobility continuum.
Bed rest is an intervention that restricts patients to bed for therapeutic reasons. For example, patients with acute myocardial infarction are initially encouraged to remain on bed rest to reduce oxygen demand and cardiac workload. Bed rest is most often prescribed by nursing and medical staff and may have different interpretations among healthcare professionals. For example, in some settings bed rest may mean strict confinement to the bed or ‘complete bed rest’, while in others patients on bed rest may be assisted to use a bedside commode or to the bathroom. Patients with a wide variety of conditions are placed on bed rest, and the duration of bed rest depends on the illness or injury and the patient’s prior state of health.
Impaired physical mobility is defined as a ‘state in which the individual experiences or is at risk of experiencing limitation of physical movement but is not immobile’ (Carpenito-Moyet, 2010:279). Alterations in the level of physical mobility can result from prescribed restriction of movement in the form of bed rest, physical restriction of movement because of external devices (e.g. a cast or skeletal traction), voluntary restriction of movement or impairment of motor or skeletal function.
The deleterious effects of muscular deconditioning associated with lack of physical activity may be apparent within days. The normal individual on complete bed rest loses muscle strength from baseline levels at a rate of 3% a day (Nash, 2011). Bed rest is also associated with other systemic complications. The term ‘disuse atrophy’ has been used to describe the pathological reduction in the normal size of muscle fibres after prolonged inactivity from bed rest, trauma, casting, or local nerve damage (Nash, 2011).
In a classic study, Deitrick and others (1948) found that even young healthy men put on bed rest had physiological problems. Periods of immobility or prolonged bed rest can cause major physiological and psychological effects. These effects can be gradual or immediate, and vary from patient to patient. The greater the extent and the longer the duration of immobility, the more pronounced the consequences. The patient with complete mobility restrictions is continually at risk of complications.
Systemic effects of immobility
All body systems work more efficiently with some form of movement. Exercise has been shown to have positive outcomes for all major systems of the body. Therefore, when there is an alteration in mobility, each body system is at risk of impairment. The severity of the impairment depends on the patient’s overall health, degree and length of immobility, and age. For example, older adults with chronic illnesses develop pronounced effects of immobility more quickly than do younger patients with the same degree of immobility.
Metabolic changes
Immobility disrupts normal metabolic functioning, including decreasing the metabolic rate; altering the metabolism of carbohydrates, fats and proteins; causing fluid, electrolyte and calcium imbalances; and causing gastrointestinal disturbances such as decreased appetite and slowing of peristalsis. However, in the presence of an infectious process, immobilised patients may have an increased basal metabolic rate as a result of fever or wound healing because these increase cellular oxygen requirements.
A deficiency in kilojoules and protein is characteristic of patients with a decreased appetite secondary to immobility. Proteins are constantly being synthesised and broken down into amino acids in the body to be reformed into other proteins. Amino acids that are not used are excreted. The body can synthesise certain non-essential amino acids, but depends on ingested proteins to supply the eight essential amino acids. When more nitrogen (the end-product of amino-acid breakdown) is excreted than is ingested in proteins, the body is said to have a negative nitrogen balance, and weight loss, decreased muscle mass and weakness result from tissue catabolism (tissue breakdown). Protein loss leads to muscle loss.
Another metabolic change is increased calcium loss from bones, resulting in hypercalcaemia. As a result, urinary excretion of calcium increases because immobility causes the release of calcium into the circulation.
Decreased gastrointestinal motility that develops from immobility can lead to various impairments of gastrointestinal functioning. Constipation is a common problem, although diarrhoea may result from a faecal impaction (accumulation of hardened faeces). This finding is not normal diarrhoea but rather liquid stool passing around the area of impaction (see Chapter 37). Left untreated, faecal impaction can result in a mechanical bowel obstruction that may partially or completely occlude the intestinal lumen, blocking normal propulsion of liquid and gas. The resulting fluid in the intestine produces distension and increases intraluminal pressure. Over time, intestinal function becomes depressed, dehydration occurs, absorption ceases and fluid and electrolyte disturbances worsen.
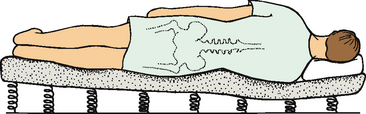
Respiratory changes
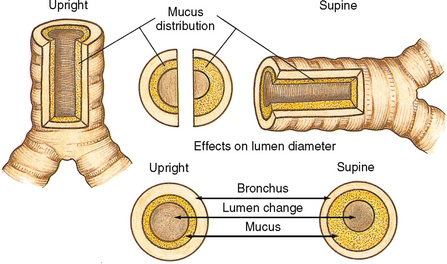
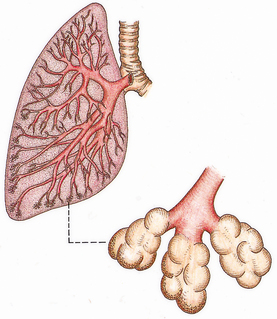
Regular aerobic exercise is known to enhance respiratory functioning. Lack of movement and exercise places patients at higher risk of respiratory complications. Postoperative and immobile patients are at high risk of developing pulmonary complications. The most common respiratory complications are atelectasis (collapse of alveoli) and hypostatic pneumonia (inflammation of the lung from stasis or pooling of secretions). In atelectasis a bronchiole or a bronchus becomes blocked by secretions and the distal lung tissue (alveoli) collapses as the existing gas is absorbed, producing hypoventilation. The extent of atelectasis is determined by the site of the blockage. A lung lobe or even a whole lung may be collapsed. Pooling secretions and decreased ability to cough productively increase the collection of mucus in the bronchi, particularly when the patient is in the supine, prone or lateral position (Figure 33-1). Secretions accumulate in the dependent regions of the airways (Figure 33-2). Because mucus is an excellent medium for bacterial growth, hypostatic pneumonia may result.
Cardiovascular changes
Orthostatic (or postural) hypotension is defined as a reduction in systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg within 3 minutes of standing from a lying position (Consensus Committee of the American Autonomic Society and the American Academy of Neurology, 1996). Patients with orthostatic hypotension may present with lightheadedness, blurred vision, dizziness, weakness and fatigue, or with syncope. In the immobilised patient, decreased circulating fluid volume, pooling of blood in the lower extremities and decreased autonomic response occur. These factors result in decreased venous return, followed by a decrease in cardiac output, which is reflected by a decline in blood pressure.
As the workload of the heart increases, so does oxygen consumption. The heart therefore works harder and less efficiently during periods of prolonged rest. As immobilisation increases, cardiac output falls, further decreasing cardiac efficiency and increasing workload.
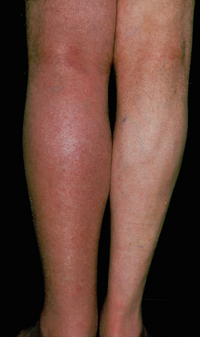
Patients are also at risk of thrombus formation, such as a deep-vein thrombosis (DVT) (Figure 33-3). A thrombus is an accumulation of platelets, fibrin, clotting factors and the cellular elements of the blood attached to the interior wall of a vein or artery, sometimes occluding the lumen of the vessel. There are three factors that contribute to venous thrombus formation (known as Virchow’s triad):
1. venous stasis (e.g. poor venous return associated with bed rest and immobility)
2. damage to the endothelium (inner lining of the vein), and
3. hypercoagulability of the blood (Soars, 2012).
A dislodged thrombus, called an embolus, may travel through the circulatory system to the lungs (called a pulmonary embolism or PE) or brain, where they are life-threatening.
Musculoskeletal changes
The effects of immobility on the musculoskeletal system can include permanent impairment of mobility. Restricted mobility may result in loss of endurance, strength and muscle mass. Other effects of restricted mobility affecting the skeletal system are impaired calcium metabolism and impaired joint mobility.
Decreased mobility and muscle atrophy—loss of muscle tissue—may occur with immobility. Atrophy is a phenomenon widely observed in response to illness, decreased activities of daily living (ADLs), and immobilisation (Boonyarom and Inui, 2006). Because of protein breakdown, the patient loses lean body mass, which is composed partially of muscle. Therefore, the reduced muscle mass is unable to sustain activity without increased fatigue. The muscle mass is decreased from metabolic causes and disuse. As immobility continues and the muscles are not exercised, there is continued decrease in mass. Loss of endurance, decreased muscle mass and strength, and joint instability subsequent to immobility put patients at risk of falls (see Chapter 15).
Immobilisation causes two skeletal changes: impaired calcium metabolism and joint abnormalities. Because immobilisation results in bone resorption, the bone tissue is less dense, or is atrophied and disuse osteoporosis results. When osteoporosis occurs, the patient is at risk of pathological fractures. Immobilisation and non-weightbearing activities increase the rate of bone resorption. Bone resorption also causes calcium to be released in the blood, and hypercalcaemia results.
One in two females and one in three males over the age of 60 years are likely to sustain a fracture due to osteoporosis (Department of Medicine, University of Melbourne, 2007). More women are affected because of the postmenopausal rapid decline of oestrogen, a hormone that plays a central role in the maintenance of bone mass balance. About 25% of Australians over 50 years of age with hip fractures die within the first 12 months, and 50% require long-term nursing care (Department of Medicine, University of Melbourne, 2007). Although primary osteoporosis is different in origin from the osteoporosis that results from immobility, it is imperative for nurses to recognise that immobilised patients may be at high risk of accelerated bone loss if they have primary osteoporosis. Early patient evaluation and consultation and referral to nutritionists and physiotherapists are important interventions for preventing disability in patients with primary osteoporosis who become immobilised.
Immobility can lead to joint contractures. A joint contracture is an abnormal and possibly permanent condition characterised by fixation of the joint (Figure 33-4). It is caused by disuse, atrophy and shortening of the muscle fibres. When a contracture occurs, the joint cannot obtain full range of motion. Contractures may leave a joint in a non-functional position, as seen in some patients who are permanently curled into a fetal position (Fergusson and others, 2007).
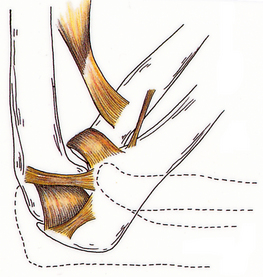
FIGURE 33-4 Contracture of the elbow: inability to extend to a 90-degree angle (dotted line) and to a 180-degree angle (not illustrated).
One common and debilitating contracture is footdrop (Figure 33-5). When footdrop occurs, the foot is permanently fixed in plantar flexion. Walking is difficult with the foot in this position, since the person cannot dorsiflex the foot. The patient with footdrop is therefore unable to lift the toes off the ground. Patients who have suffered strokes with resulting left- or right-sided paralysis (hemiplegia) are susceptible to footdrop.
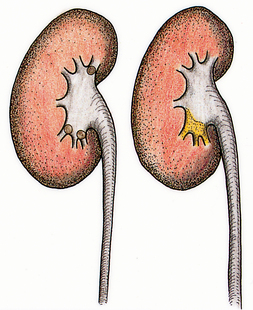
Urinary elimination changes
The patient’s urinary elimination is altered by immobility. In the upright position, urine flows out of the renal pelvis and into the ureters and bladder because of gravitational forces. When the patient is recumbent or flat, the kidneys and the ureters move towards a more level plane. Urine formed by the kidney must enter the bladder unaided by gravity. Because the peristaltic contractions of the ureters are insufficient to overcome gravity, the renal pelvis may fill before urine enters the ureters (Figure 33-6). This condition is called urinary stasis and increases the risk of urinary tract infection (UTI) and renal calculi (see Chapter 38).
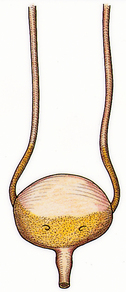
FIGURE 33-6 Stasis of urine with reflux to ureters.
From Potter PA, Perry AG 2013 Fundamentals of nursing, ed 8. St Louis, Mosby.
Renal calculi are calcium stones that lodge in the renal pelvis and pass through the ureters (Figure 33-7). Immobilised patients are at risk of calculi because of altered calcium metabolism and the resulting hypercalcaemia.
As the period of immobility continues, fluid intake can diminish; other causes, such as fever, increase the risk of dehydration. As a result, urinary output declines and urine is usually highly concentrated. This concentrated urine increases the risk of calculi formation and infection. Poor perineal care after bowel movements, particularly in women, increases the risk of urinary tract contamination by Escherichia coli bacteria. Another cause of UTIs in immobilised patients is the use of an indwelling urinary catheter.
Integumentary changes
The direct effect of pressure on the skin is compounded by the changes in metabolism that accompany immobility. Older adults and patients with paralysis also have a greater risk of developing pressure ulcers. Any break in the skin’s integrity is difficult to heal in the immobilised patient.
A pressure ulcer is an impairment of the skin as a result of prolonged ischaemia to tissues (see Chapter 30). The ulcer is characterised initially by inflammation and usually forms over a bony prominence. Ischaemia develops when the pressure on the skin is greater than the pressure inside the small peripheral blood vessels supplying blood to the skin.
Tissue metabolism depends on the body’s receipt of oxygen and nutrients from the blood supply and the elimination of metabolic wastes. Any factor that interferes with perfusion affects cellular metabolism and, as a result, the function of the cell. Pressure affects cellular metabolism by decreasing or obliterating tissue circulation. When a patient lies in bed or sits in a chair, the weight of the body is on bony prominences. The longer the pressure is applied, the longer the period of ischaemia and therefore the greater the risk of skin breakdown.
Psychosocial effects
Immobilisation may lead to emotional and behavioural responses, sensory alterations and changes in coping. These changes are individualised to each patient. In addition, immobilised patients may also have social and family difficulties.
The most common emotional changes are depression, behavioural changes, sleep–wake disturbances and impaired coping. The immobilised patient can become depressed because of changes in role, self-concept and other factors. Depression is an affective disorder characterised by extreme feelings of sadness, melancholy, dejection, worthlessness, emptiness and hopelessness out of proportion to reality. Depression can result from worrying about present and future levels of health, finances and family needs. Because immobilisation removes patients from their daily routine, they have more time to worry about disability. Worrying can quickly increase depression, causing withdrawal. Assessing behavioural changes throughout restricted mobility helps the nurse to identify changes in self-concept, recognise early signs of depression and develop nursing interventions (see Chapter 23).
Behavioural changes resulting from immobilisation vary widely, depending on the patient. Common behavioural changes include hostility, fear and anxiety. Early in the nursing process the nurse should interview the patient and the patient’s family and friends about normal behavioural patterns to gain baseline data. If unexpected behaviours are observed later, the nurse can intervene to reduce the effects of immobilisation on the patient’s behavioural patterns.
The immobilised patient requires frequent and regular nursing care. Because of physiological hazards, the patient cannot be allowed to sleep for 8 hours without a change of position or other nursing care. Disruption of normal sleeping patterns can further cause behavioural changes. Nursing interventions should be used to ensure that the patient receives sufficient sleep (see Chapter 35). The patient who is on bed rest and able to change position during sleep does not require continuous physical nursing care directed at reducing the hazards of immobility. Unless other treatment activities are required during the night, the care plan for the physiologically stable patient on bed rest should provide for uninterrupted sleep.
Long-term immobility or bed rest can affect usual coping patterns. Such a patient may withdraw and become passive. The passive patient allows nurses to provide care but is not interested in increasing independence or being involved in care. Early in the care of an immobilised patient, the nurse should assess the patient’s normal coping mechanisms. The nurse then designs a nursing care plan that will enable the patient to continue to use these coping abilities or help the patient develop new ones.
Developmental changes
Developmental changes tend to be associated more with immobility in the very young and in older adults. The immobilised young or middle-aged adult who has been healthy may experience few, if any, developmental changes. However, there are exceptions and patients must be fully assessed for developmental implications. One exception might be a mother who has complications at childbirth and as a result cannot interact with the newborn as expected.
INFANTS, TODDLERS AND PRESCHOOLERS
The newborn infant’s spine is flexed and lacks the anteroposterior curves of the adult (see Chapter 20). As the baby grows, musculoskeletal development permits support of weight for standing and walking. Posture is awkward because the head and upper trunk are carried forward. Because bodyweight is not evenly distributed along a line of gravity, posture is off-balance, and falls occur often. When the infant, toddler or preschooler is immobilised, it is usually because of trauma or the need to correct a congenital skeletal abnormality. Prolonged immobilisation can delay the child’s gross motor skills and intellectual development. Nurses caring for immobilised children should plan activities that provide physical and psychosocial stimulation.
ADOLESCENTS
The adolescence stage is usually initiated by a tremendous growth spurt (see Chapter 20) where growth is frequently uneven. Prolonged immobilisation may alter adolescent growth patterns, causing the adolescent to lag behind peers in gaining independence. When immobilisation occurs, social isolation is often a major concern for this age group.
ADULTS
An adult who has correct posture and body alignment feels good and generally appears self-confident. The healthy adult also has the necessary musculoskeletal development and coordination to carry out ADLs (see Chapter 21). When periods of prolonged immobility occur, all physiological systems are at risk. In addition, the role of the adult may change with regard to the family or social structure, such as loss of identity associated with a job.
OLDER ADULTS
A progressive loss of total bone mass occurs with the older adult. Some of the possible causes of this loss include decreased physical activity, hormonal changes and actual bone resorption. The effect of bone loss is weaker bones and, as a result, older adults may walk more slowly, walk bent over, take smaller steps and appear less coordinated. When balance is impaired, they are at greater risk of falls and injuries (see Chapter 22). Falls in older adults are associated with immediate serious consequences such as fractures and head injuries, as well as longer-term problems such as disability, fear of falling, and loss of independence (Rawsky, 1998).
Older adults are also at risk of decreased functional status and impaired mobility secondary to hospitalisation (see Box 33-1). Immobilisation of older adults may increase their physical dependence on others, which accelerates functional losses. Immobilisation of some older adults can result from degenerative diseases, trauma or chronic illness. For some older adults, immobilisation occurs gradually and progressively; whereas for others, especially those who have had a stroke, immobilisation is sudden. When providing nursing care for an older adult, the nurse should develop a care plan that encourages the patient to perform as many self-care activities as possible, thereby maintaining the highest level of mobility (see Research highlight). Murphy and Reid (2003) suggest that nurses may inadvertently contribute to a patient’s immobility by providing unnecessary help with activities such as bathing and transferring.
BOX 33-1 HAZARDS OF HOSPITALISATION OF THE OLDER ADULT
• For many older people, hospitalisation results in functional decline despite cure or repair of the condition for which they were admitted. Hospitalisation can result in complications unrelated to the problem that caused admission or to its specific treatment, and for reasons that are explainable and avoidable.
• Usual ageing is often associated with functional change, such as a decline in muscle strength and aerobic capacity; vasomotor instability; reduced bone density; diminished pulmonary ventilation; altered sensory continence, appetite and thirst; and a tendency towards urinary incontinence. Hospitalisation and bed rest superimpose factors such as enforced immobilisation, reduction of plasma volume, accelerated bone loss, increased closing volume and sensory deprivation. Any of these factors may thrust vulnerable older people into a state of irreversible functional decline.
• The factors that contribute to a cascade to dependency are identifiable and can be avoided by modification of the usual acute hospital environment by de-emphasising bed rest, removing the hazard of the high hospital bed with rails and actively facilitating ambulation and socialisation.
From Creditor MC 1993 Hazards of hospitalization of the elderly. Ann Intern Med 118(3):219.
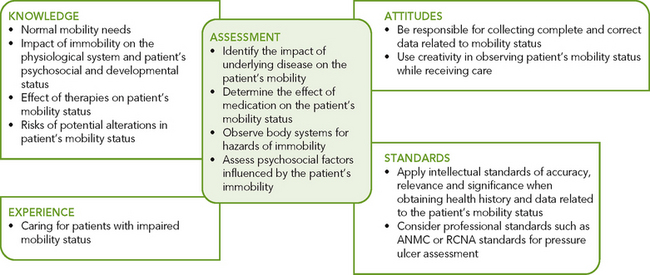
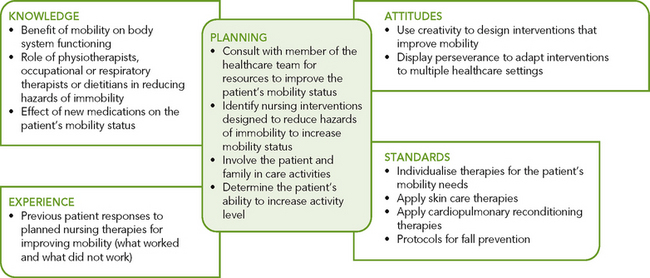
Critical thinking synthesis
Critical thinking and sound clinical judgment when caring for patients with impaired mobility requires nurses to draw on their knowledge of mobility and immobility and on previous experience, and apply critical-thinking attitudes and professional standards (Figure 33-8). Patients with impaired mobility often have multiple needs which must be prioritised. To understand the impact of immobility on the patient and family, the nurse integrates knowledge from nursing and other disciplines, previous experiences and information gathered from patients.
Research focus
In older patients, acute medical illness that requires hospitalisation is a sentinel event that often precipitates disability. This results in the subsequent inability to live independently and complete basic activities of daily living (ADLs). This nursing research examined the association between mobility levels of older adults during hospitalisation and functional outcomes at discharge and 1-month follow-up.
Research abstract
Design: Prospective cohort study.
Setting: A 900-bed teaching hospital in Israel.
Participants: 525 older (≥ 70 years) acute medical patients hospitalised for a non-disabling condition.
Measurements: In-hospital mobility was assessed using a previously validated scale. The main outcomes were decline from premorbid baseline functional status at discharge (ADLs) and at 1-month follow-up (ADLs and instrumental ADLs). Hospital mobility levels and functional outcomes were assessed according to prehospitalisation functional trajectories. Logistic regressions were modelled for each outcome, controlling for functional status, morbidity and demographic characteristics.
Results: 46% of participants had declined in ADLs at discharge and 49% at follow-up; 57% had declined in IADLs at follow-up. Mobility during hospitalisation was twice as high in participants with no pre-admission functional decline.
Low versus high in-hospital mobility was associated with worse basic functional status at discharge (adjusted odds ratio (AOR) = 18.03; 95% confidence interval (CI) = 7.68–42.28) and at follow-up (AOR = 4.72; 95% CI = 1.98–11.28) and worse IADLs at follow-up (AOR = 2.00; 95% CI = 1.05–3.78). The association with poorer discharge functional outcomes was present in participants with pre-admission functional decline (AOR for low vs high mobility = 15.26; 95% CI = 4.80–48.42) and in those who were functionally stable (AOR for low vs high mobility = 10.12; 95% CI = 2.28–44.92).
Evidence-based practice
• The results of this study show that low levels of in-hospital mobility were associated with functional decline of older adults at discharge and, even more so, at follow-up.
• In-hospital mobility, unlike personal and disease-related risk factors, is a potentially modifiable care aspect that has important implications for in-hospital care regimens.
• Level of mobility was significantly related to functional outcomes of patients whether or not they had functional decline before their hospitalisation, indicating the value of developing and evaluating a policy for the early and effective mobilisation of all older hospitalised patients in general medical units.
You are a student nurse caring for Albert Devereaux, an alert and oriented 81-year-old man, admitted to hospital after a fall with complaints of dizziness and syncope. His blood pressure (BP) on admission was 80/40 mmHg. At the aged-care nursing facility where he lives, he ambulated with a walker independently but, since a recent episode of syncope, he has complained of weakness and needs another person to assist him while walking as a fall precaution.
Nursing staff found Mr Devereaux lying on the floor on his right hip, and he explained ‘I had to go to the bathroom. I know I should have called for help, but the nurses are so busy. I figured I could go myself. Only two more steps and I could have reached my walker. I just slipped, is all.’ He reports pain in his right hip that is a 5 on a 0–10 numerical pain rating scale, which he describes as a ‘ache’ that is worse with movement of his right leg.
An X-ray of his right hip is taken, which is negative for a fracture. You take a set of orthostatic vital signs: lying BP = 110/80 mmHg, heart rate = 73 beats per minute; standing BP = 90/50 mmHg, heart rate = 92 beats per minute. His other vital signs are temperature 36.8°C, respiratory rate 16 breaths per minute, oxygen saturation (SpO2) 99% on room air. No injuries are noted on inspection and palpation of his head and neck. Pupils are equal and react briskly to light. His chest is clear to auscultation, heart sounds are irregular. There is full range of motion in the upper extremities and handgrip strength is bilaterally equal. His abdomen is soft and non-tender. There is no physical deformity of the right hip or other injuries apparent, but a moderate amount of ecchymosis is visible over his right hip that extends around to his lower back and right upper buttock. He demonstrates normal movement and sensation in both feet. He has requested the urinal once for 200 mL of clear yellow urine. An electrocardiogram confirms his known history of atrial fibrillation.
Mr Devereaux is admitted, and his plan of care includes assessment of orthostatic vital signs every shift and fall precautions. You explain to him how to use the call light and he remains on bed rest with side rails up. Later in the shift Mr Devereaux tells you he is worried about the consequences of this fall for his mobility and independence.
Adapted from Douglas C 2001 Pulling it all together. In Lewis P, Foley D, editors, Weber & Kelley’s Health assessment in nursing. Philadelphia, Lippincott Williams & Wilkins.