34 STRESS
INTRODUCTION
The term stress is used frequently and often refers to a person’s ability to cope with potential or actual challenges. It is not uncommon for people to state that a person is ‘under stress’, referring to the individual’s capacity to complete certain tasks, such as a heavy workload, and it is this stress that may impact on the person’s health. Often there are no overt physical manifestations, yet the person is still stressed.
The concept that stress can influence immunity and resistance to disease has been investigated since the 1950s. In the 1970s, studies found that life changes or emotions, occurring over a prolonged period of time, were associated with decreased immune function. In more recent times, studies have investigated the interactions among social, psychological and biological factors and their role in causing and prolonging the course of disease. What is emerging from wide areas of research is that stress is a complex response that involves relationships among the central nervous system, autonomic nervous system, endocrine system and immune system. One specific example of stress, particularly in those working shift work, is the relationship between inconsistent sleep patterns and disturbances in physiological processes. In this sense, the altered sleep patterns form a type of stress. Sleep is a normal cyclic process that restores the body’s energy and maintains normal functioning; it is so essential to both physiological and psychological function that sleep deprivation causes a wide range of clinical manifestations.
Stress may cause or exacerbate several diseases, including those that are leading causes of death in Australia and New Zealand: cardiovascular disease, cancer and diabetes mellitus. Stress is also directly related to symptoms and outcomes in a number of diseases and conditions, including irritable bowel syndrome, gastric ulcers, asthma, autoimmune disorders, delayed wound healing, reproductive dysfunction, depression and some cancers (see Table 34-1). It has been suggested that chronic inflammation, which can be stimulated by stress, is important in the functional decline that leads to disability and untimely death.1 The mental interpretation of stress is also linked to physiological processes in the body. This chapter describes definitions of stress, the general stress response and its benefits and adverse consequences.
THE GENERAL ADAPTATION SYNDROME
Early research on stress by Selye in 1946 revealed that the body’s physiological responses to stress were the same, regardless of the type of original stress, such as cold, surgical injury or noxious stimulus (toxic chemicals).2 He called these stimuli stressors. Because many diverse agents caused the same responses, Selye named this the general adaptation syndrome — a generalised set of physiological processes that occur regardless of the initial cause of the stress. The stress response can be considered a response to a disturbance of homeostasis brought about by the stress. As well as the generalised stress response, some additional responses specific to the stress may also occur. For example, exposure to cold causes the general adaptation syndrome as well as shivering in an effort to maintain core temperature.
Three successive stages of the general adaptation response are:
These stages are discussed in more detail later in the chapter in the section ‘The detection of stress’.
THE STRESS STIMULUS
Physical stress
The most obvious example of stress is that of a physical nature. The physical stress may be an injury or a trauma, a disease, a physical threat or even heavy exercise. Of particular relevance in the healthcare setting is the physical stress of surgical procedures, which will activate the general adaptation syndrome. Other examples of physical stress are a dog growling and lunging towards you, having to run towards the closing doors on a train or attempting to shift heavy furniture that you can barely move. Intense levels of exercise can also initiate the stress response, such as exercising to exhaustion or exercising in a particularly difficult environment like cold water. The physical stress activates the hypothalamus directly, which then mediates the general adaptation syndrome.
Psychological stress
The other main type of stress is psychological stress, which encompasses those types of triggers that are not a physical threat to the body. These psychological stressors can be considered mental stressors (such as a work deadline or an examination) or emotional stressors (such as personal relationships). For these types of stressors, the perception of the threat is individualised. For example, having to speak in public may be a stress for many people, but of little concern to others. Another example is if someone has abused a particular person: the appearance of the abuser will cause a stress response in the victim, but not in someone else. In this way, the cerebral cortex and other regions of the brain involved in interpretation of the sensory stimulus and memory information (such as the memory of being abused) can actually process the stimulus, thereby determining whether the situation is a stress, and signal to the hypothalamus accordingly.
Interestingly, the stress response is associated not only with negative triggers, but also positive situations. For example, a surfer who walks onto the beach and sees a big swell would be extremely pleased and experience excitement and anticipation, which lead to the stress response. The sight of the swell might cause fear in a non-surfer — but surprisingly, the same set of general physiological processes would occur in both the excited and the fearful person. Similarly, a family reunion may bring excitement to some and dread to others, but either way the same stress response occurs — although someone with no strong feelings about the reunion would not have a stress response.
The interpretation of the situation in the brain is important in deciding whether to signal to the hypothalamus that a stress is occurring. People are not disturbed by the actual situation itself, but by the ways that they appraise and react to the situation. In general, a person experiences stress when the demand exceeds their coping abilities — their ability to control the situation is an important factor in how it is interpreted by the brain.
Contemporary stressors
Most of the common stressors in modern-day Australia and New Zealand are psychological stressors, derived from mental stress — for example, time stress is particularly common, as is handling deadlines at work, and even recreational activities such as playing computer games can cause adrenaline release due to their intensity. Other stressors have increased in the light of the global financial crisis of 2008–2009, as issues of housing affordability and finding and maintaining employment have become more widespread. Emotional stresses are also common as we become more time-poor and are faced with guilt and disappointment at ‘not having enough time’ to fit in everything, such as spending enough time with family and friends. These stressors are so commonplace that phrases such as ‘I don’t have enough time to …’ or ‘I’m so stressed …’ are now a normal part of conversation.
The types of responses that are usually required for mental and emotional stresses are not of a physical nature. The way we respond to our mental and emotional stressors can be termed ‘feed and faze out’3 — that is, we are most likely to react to the stress by eating or sitting down. The term emotional eating is used to describe a common response to stress: eating. Interestingly, eating further enhances elevated blood glucose and lipid levels, leading to an exacerbation of the physiological response — which is exaggerated even further if the food chosen is high in glucose and lipids.
THE DETECTION OF STRESS
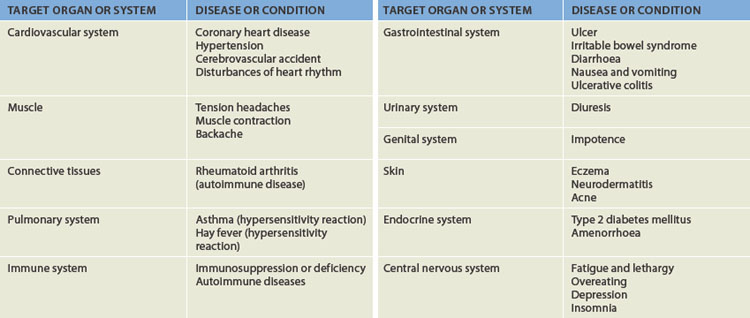
A psychological stress is first perceived or detected as sensory information by the cerebral cortex. After the signals are processed and interpreted as a stress by particular regions of the brain, the hypothalamus is quickly alerted (see Figure 34-1). The hypothalamus is then responsible for coordinating the stress response, resulting in the nonspecific physiological responses of the general adaptation syndrome. Importantly, a physical injury or a physiological disease will directly activate the stress response at the hypothalamus without any interpretation of the stimulus being required. For example, chronic inflammation in tissues activates the stress response, as does a surgical wound to internal organs.
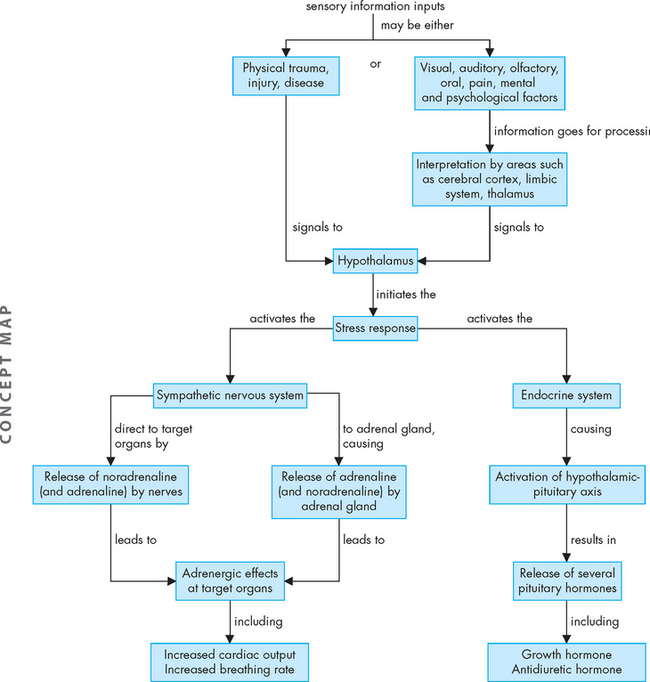
FIGURE 34-1 Sensory information, including that coming from the special senses, is interpreted before reaching the hypothalamus.
Although a large amount of sensory information is interpreted by the individual based on personality, life experiences, memory, emotion and other factors before being considered as a stress, a physical injury directly activates the hypothalamic stress response.
The alarm stage
The alarm stage begins when a stressor activates the hypothalamus and sympathetic nervous system. The entire sympathetic nervous system becomes activated simultaneously, a concept known as ‘mass discharge’, whereby the neurons throughout this system all send signals to their target organs throughout the body at the same time (see Figure 34-1). In addition, the sympathetic nervous system stimulates the adrenal gland to release hormones (adrenaline and noradrenaline) that enhance and extend the effects of the sympathetic nervous system. At the same time, the hypothalamus stimulates the release of pituitary gland hormones (known as the hypothalamic-pituitary-adrenal axis — review using Chapter 10), resulting in elevated levels of a range of hormones: cortisol, aldosterone, thyroid hormone, growth hormone and antidiuretic hormone. These hormonal changes allow the body to respond appropriately to the stress.
The resistance stage
If the stress continues for a longer period of time, the body progresses into the resistance or adaptation phase. Towards the end of the resistance stage, the sympathetic nervous system and levels of circulating hormones return to normal, as the body has adapted and so returns to a state of homeostasis.
If the stress persists, adaptation may actually occur during this phase, so that there is a perception change in the individual — that is, the individual no longer sees the original stress as being so negative. For example, when someone first moves into a home beside a train line, they may notice the train noise, but over time they will no longer notice the noise because they have adapted to the stress of the noisy living conditions.
The exhaustion stage
If the stress continues after the resistance reaction, the body moves into a state of exhaustion, which is strongly linked with the development of chronic disease. Exhaustion occurs if stress continues and adaptation is not successful, ultimately causing impairment of the immune response, heart failure and kidney failure leading to death.
PHYSIOLOGICAL PROCESSES OF THE STRESS RESPONSE
The two general branches of the stress response are coordinated by the systems responsible for the regulation of all body processes: the nervous system and the endocrine system. The hypothalamus initiates a number of steps that bring about a range of body responses, thereby ensuring that the body is physically and mentally prepared to respond to the stress. This includes: (1) activating the sympathetic nervous system; and (2) activating the hypothalamic-pituitary-adrenal axis.
The sympathetic nervous system
The sympathetic nervous system mediates many of the characteristic responses to stress, hence the descriptive term ‘fight or flight’, in which the body prepares for defence or to depart from a threat (see Chapter 6 to review the sympathetic nervous system — see also Table 34-2). Most of the direct effects from the sympathetic nervous system are controlled by noradrenaline (with adrenaline). Important effects of sympathetic activation include an increased heart rate, increased blood pressure and increased cardiac output. This is matched with bronchodilation and an increased breathing rate. Extensive vasoconstriction limits blood flow to areas such as the skin and abdominal organs, thereby increasing venous return to further enhance cardiac output. Vasodilation occurs at the working skeletal muscles. This is important because the person will need to utilise their muscles in ‘fight or flight’ and therefore an increase in muscle blood flow is required. Blood coagulation is enhanced (which is needed for the stress of haemorrhage). There is an overall decrease in digestive function, including decreased motility, constriction of the sphincters and decreased secretions. Blood glucose levels are increased by stimulating the secretion of glucagon and inhibiting the release of insulin. Pupillary dilation allows more light into the eyes and increases visual acuity. Reproductive and growth functions are inhibited during stress.
Table 34-2 PHYSIOLOGICAL EFFECTS OF THE CATECHOLAMINES
| ORGAN/CELL | EFFECTS |
|---|---|
| Brain | |
| Cardiovascular system | |
| Pulmonary system | |
| Muscle | |
| Liver | |
| Adipose tissue | |
| Skin | |
| Eye | Pupil dilation |
| Gastrointestinal and genitourinary tracts | |
| Lymphoid tissue | Acute and chronic stress inhibits several components of cellular immunity, particularly decreasing natural killer cells* |
| Macrophages | Inhibit and stimulate macrophage activity; depends on availability of type 1/proinflammatory cytokines, the presence or absence of antigenic stressors and peripheral corticotropin-releasing hormone (CRH) |
| * Natural killer cells appear to be the most ‘sensitive’ cells to the suppressive effect of stress and thus have become an important index of stress-induced suppression of cellular immunity. | |
Source: Adapted from Granner DK. Hormones of the adrenal medulla. In Murray RK et al. (eds). Harper’s biochemistry. 23rd edn. New York: McGraw-Hill; 1999; Elenkov IJ, Chrousos GP. Stress hormones, proinflammatory and antiinflammatory cytokines, and autoimmunity. Ann N Y Acad Sci 2002; 966:290–303.
The sympathetic nervous system also activates the adrenal medulla to secrete adrenaline and noradrenaline. There is a slight delay in the levels of these catecholamines increasing in the blood when secreted by the adrenal gland as hormones, compared with the immediate response at the target cell by direct sympathetic innervation. The release of these hormones from the adrenal medulla enhances and elongates the immediate neural responses; either way, the catecholamines have the same effect whether from the neural or the endocrine system. (In this chapter, when referring to the sympathetic nervous system response, both the direct neural effects and the extended hormonal effects are considered together.)
The hypothalamic-pituitary- adrenal axis
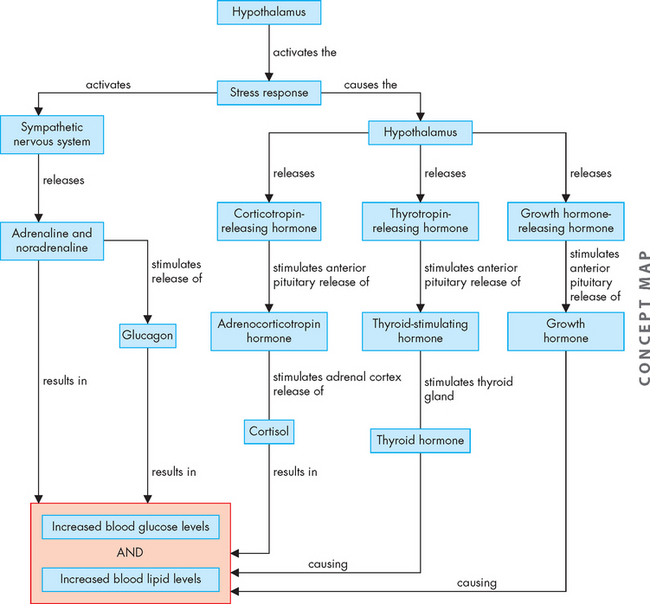
In response to stress, the hypothalamus stimulates particular regions of the pituitary gland, which leads to an increase in circulating levels of cortisol, aldosterone, thyroid hormone, antidiuretic hormone and growth hormone (see Chapter 10 to revise the hormones of the endocrine system). Each of these contributes to the overall stress response. In general terms, cortisol is considered one of the most important molecules of the stress response, and it increases blood glucose and blood lipid levels (see Table 34-3). Cortisol also interacts with the immune system (see ‘Effects of cortisol on immune function’ below). Aldosterone causes increased reabsorption (and retention) of sodium and water, while antidiuretic hormone also causes water retention. Thyroid hormone increases the heart rate and breathing rate and increases levels of glucose and lipids in the blood. Growth hormone increases blood glucose levels. All of these physiological events benefit the body in the short term in reacting to the stressful stimuli; however, if they continue to be released, their effects can considerably alter homeostasis and the body will become prone to the harmful effects of stress.
Table 34-3 PHYSIOLOGICAL EFFECTS OF CORTISOL
| FUNCTIONS AFFECTED | PHYSIOLOGICAL EFFECTS |
|---|---|
| Carbohydrate and lipid metabolism | Diminishes peripheral uptake and utilisation of glucose; promotes glucose production in liver to increase blood glucose levels; promotes breakdown of lipids in adipose tissue to increase blood lipid levels |
| Protein metabolism | Decreases protein synthesis (including immunoglobulin synthesis) in muscle, lymphoid tissue, adipose tissue, skin and bone; increases plasma level of amino acids |
| Anti-inflammatory effects (systemic effects) | High levels of cortisol used in drug therapy suppress the inflammatory response and inhibit pro-inflammatory activity of many growth factors and cytokines; however, over time some patients may develop tolerance to glucocorticoids causing an increased susceptibility to both inflammatory and autoimmune disease |
| Pro-inflammatory effects (possible local effects) | Cortisol levels released during the stress response may increase pro-inflammatory effects |
| Lipid metabolism | Lipolysis in the extremities and lipogenesis in the face and trunk |
| Immune effects | Treatment levels of glucocorticoids are immunosuppressive, thus they are valuable agents used in numerous diseases; cellular immunity is particularly affected by these larger doses of glucocorticoids with suppression of TH1 function or cellular immunity; stress can cause a different pattern of immune response; these non-therapeutic levels can suppress cellular (TH1) and increase humoral (TH2) immunity; several factors influence this complex physiology and include long-term adaptations, reproductive hormones (i.e. overall, androgens suppress and oestrogens stimulate the immune responses), defects of the hypothalamic-pituitary-adrenal axis, histamine-generated responses and acute versus chronic stress; thus stress seems to cause an increase in TH2 cells systemically whereas locally, under certain conditions, it can induce pro-inflammatory activities and by these mechanisms may influence the onset or course of infections, autoimmune/inflammatory diseases, allergies and cancers |
| Digestive function | Promotes gastric secretion |
| Urinary function | Enhances excretion of calcium |
| Muscle function | Maintains normal contractility and maximal work output for skeletal and cardiac muscle |
| Bone function | Decreases bone formation |
| Cardiovascular system | Maintains normal blood pressure; permits increased responsiveness of arterioles to the constrictive action of adrenergic stimulation; optimises myocardial performance |
| Central nervous system function | Modulates perceptual and emotional functioning, essential for normal arousal and initiation of daytime activity |
PHYSIOLOGICAL EFFECTS OF THE STRESS RESPONSE
The generalised response to stress by the sympathetic nervous system and the hormones stimulated by the hypothalamic-pituitary-adrenal axis lead to a number of physiological processes, including an increased heart rate and cardiac output, increased breathing rate, elevated blood pressure, elevated blood levels of glucose and lipids, altered immunity and suppression of pain.
Increased cardiac output and breathing rate
The sympathetic nervous system increases the heart rate and causes widespread vasoconstriction, which in turn increases venous return, thereby increasing cardiac output. Thyroid hormone also contributes to increased heart rate and enhances the effects of adrenaline and noradrenaline on the heart. Overall, therefore, cardiac function is increased. This occurs in conjunction with an increased breathing rate, mediated by the sympathetic nervous system, which causes bronchodilation to maximise airway diameter during stress. This enables the individual to increase the amount of air available for gas exchange in the lungs, and thereby contributes to increases in oxygenation.
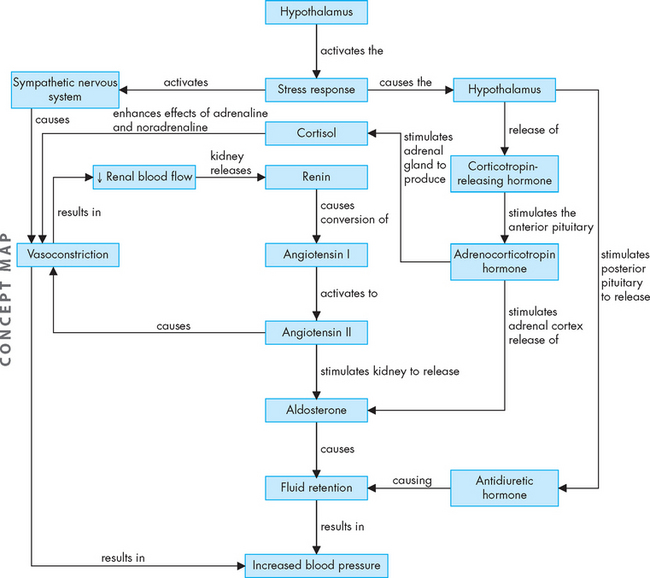
Elevated blood pressure
Sympathetic nervous system activity causes vasoconstriction of many blood vessels, which contributes to elevated blood pressure. Vasoconstriction at the kidneys is an important means of redirecting blood flow to other organs; however, in response, the kidneys secrete renin to activate the renin-angiotensin-aldosterone system (see Figure 34-2). The effects of aldosterone include the reabsorption of sodium and water, which increases blood volume. Similarly, antidiuretic hormone causes reabsorption of water, which further increases blood volume. This increase in blood volume also leads to elevated blood pressure.
Increased blood glucose and lipid levels
Adrenaline, noradrenaline, glucagon, cortisol, thyroid hormone and growth hormone all contribute to a rise in blood glucose and blood lipid levels (see Figure 34-3). Body stores of glucose, lipids and proteins are broken down and released into the blood. Consequently, stress may cause a substantial rise in blood glucose and blood lipid levels.
Altered immune response
Effects of cortisol on immune function
Cortisol secreted from the adrenal gland alters the immune system during stress. Cortisol secretion increases the innate immune response, which leads to increased inflammation, as well as an exaggerated allergic response (see Figure 34-4A).
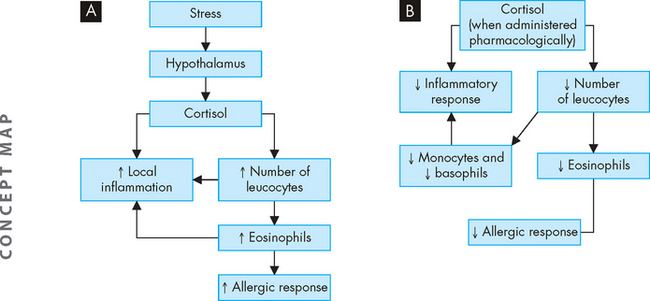
FIGURE 34-4 The effects of cortisol on innate immunity.
Note that the physiological effects are different from the effects seen with higher levels of cortisol from medication use. A Physiological levels of cortisol, as secreted during the stress response, enhance innate immunity. B Therapeutic levels of cortisol, due to pharmacological treatment, inhibit the innate responses, thereby suppressing the inflammatory response and allergic reaction.
The effects of stress on the other branch of the immune system, adaptive immunity, are more complex. At levels reached during stress cortisol and the catecholamines may paradoxically decrease cellular immunity by inhibiting TH1 cells and increase autoimmune (humoral) responses by enhancing TH2 cells (see Figure 34-5). Consequently, stress results in immunosuppression and an increased risk of infection (due to decreased cellular immunity) at the same time as there is a heightened antibody response and autoimmune disease (due to increased humoral immunity). This decrease in TH1 activity and increase in TH2 activity is called the TH2 shift.
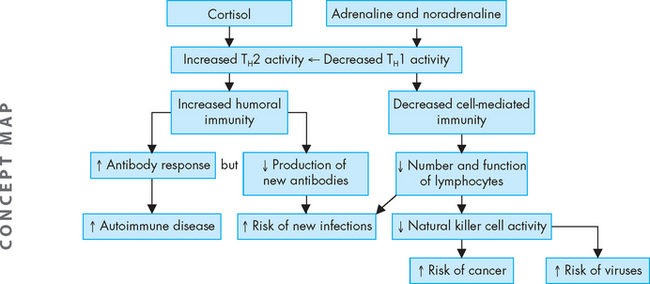
FIGURE 34-5 The effects of stress hormones on the adaptive immune system.
There is a decrease in cell-mediated immunity (T lymphocytes and natural killer cells) and an increase in humoral immunity (beta lymphocytes and antibodies). Similar general effects on adaptive immunity are seen with physiological levels of cortisol secreted during stress, as well as with therapeutic levels of cortisol administered as treatments.
The relationships among cortisol, the immune system and the cytokines (signalling molecules) produced by immune cells are complex, and the detailed mechanisms of the interactions are currently being researched;4 hence we consider only some general features here. The overall effects of stress are profound, with prolonged severe stress,5 including enlargement of the adrenal gland (due to increased activity to produce the cortisol), with simultaneous shrinkage of the thymus and lymph nodes, which may reflect the suppression of immune function.
Effects of cortisol used as a therapeutic agent
Cortisol and similar substances are used therapeutically in clinical practice as powerful anti-inflammatory and immunosuppressive agents. When administered to patients, the amount of cortisol used is much higher than the physiological amount secreted by the body during stress. It appears that this higher level has the opposite effect on innate immunity, such that the inflammatory response and the allergic response are lessened (see Figure 34-4B). The effects of therapeutic doses of cortisol on the adaptive immune response, in general terms, appear similar to that seen with physiological levels. However, some of the detailed processes may actually differ and are complex. Overall, treatment levels of cortisol are immunosuppressive across most of the immune system functions.
Effects of other components of the stress response on immune function
The stress response directly influences the immune system by mechanisms additional to cortisol. Immune cells have surface receptors for corticotropin-releasing hormone, adrenocorticotropic hormone, endorphins, noradrenaline, growth hormone and steroids.6 Lymphatic tissues and organs including the thymus, spleen, lymph nodes and bone marrow are innervated by the sympathetic nervous system. Endogenous opiates are released during stress and have both enhancing and suppressive effects on various immune cells.7–11 8 9 10 11
Growth hormone from the pituitary gland increases in the blood with stressful stimuli such as cardiac catheterisation, gastroscopy, surgery, fever and physical exercise. Immune cells are affected directly by growth hormone, as growth hormone receptors are present on lymphocytes. Interestingly, prolonged activation of the stress response (chronic stress) actually suppresses growth hormone, which may direct body resources towards the stress rather than the maintenance function of growth.
Prolactin (from the pituitary gland) levels in the plasma increase as a result of more intense stressors including surgery, motion sickness and after examinations.12,13 Immune cells are affected by prolactin, as lymphocytes have prolactin receptors, although the exact mechanisms of how prolactin interacts with immunity during stress is still being determined.
Immune system signalling to the hypothalamus
Cytokines released by immune cells have significant influence on neuroendocrine function and thus the immune system alerts other systems of threatening stimuli, such as infection, tissue damage and tumour cells, which may disrupt homeostasis. The immune system components release inflammatory mediators (such as interleukin-6, tumour necrosis factor-beta [TNF-β], interferon) due to bacterial or viral infections, cancer and tissue injury. This is an example of a stressor causing direct activation of the hypothalamus.
Suppression of pain
Beta (β)-endorphins (endogenous opiates) are released into the blood as part of the response to stressful stimuli, including traumatic injury and an acute intense stress situation such as severe physical injury. In inflamed tissue, immune cell–derived endorphins activate endorphin receptors on peripheral sensory nerves leading to pain relief or analgesia. This may contribute to some people not experiencing the intense pain that would be anticipated in some circumstances of physical injury (via the stress response).
BENEFITS OF THE STRESS RESPONSE
The stress response is necessary in mobilising body stores, such as glucose and ATP, and shunting blood to the working skeletal muscles, heart, lungs and brain, giving them access to oxygen and the nutrients necessary to protect and keep the body safe. These physiological changes equip the body to respond to a physical challenge or threat by either fight (defending itself) or flight (escaping). The key features of the stress response are sufficient blood pressure and blood flow and adequate levels of glucose and lipids in the blood as fuels delivered to the organs. The stress response enables these physiological processes to be maximised, thus preparing the body for a physical response. This is particularly beneficial in the short term. The term eustress describes a stress that causes this response when it is of benefit to the body, such as during exercise or a task that provides a challenge to the individual. For example, during exercise the stress response is vital to allow adequate glucose, lipids, oxygen, blood flow, cardiac output and respiratory rate to support the exercise activity.
HEALTH ALTERATIONS WITH LONG-TERM STRESS
The exhaustion stage of the general adaptation syndrome occurs when the stress persists for an extended period of time and is not resolved during the adaptation stage. In progressing to exhaustion, the stress is defined as distress, meaning the long-term effects of the stress are having a negative impact on the health of the individual, leading to pathophysiological processes. While all aspects of the physiological stress response may contribute to the pathophysiology, it is cortisol that is associated with most of these undesirable effects.
For example, extended periods of high levels of cortisol cause increased gastric secretions, which contribute to the risk of developing gastric ulcers. Although Helicobacter pylori is well-known as a main cause of gastric ulcer formation, it appears that there is still a role for stress in the development of this condition. Stress can increase acid secretion and impair mucosal defences, facilitating the colonisation of the stomach by Helicobacter pylori and hence the development of ulcers.14 In addition, the effects of the sympathetic nervous system causing vasoconstriction to the digestive tract result in a decrease in blood flow and a decrease in the secretion of protective mucus, which also contributes to gastric ulcers (see Figure 34-6).
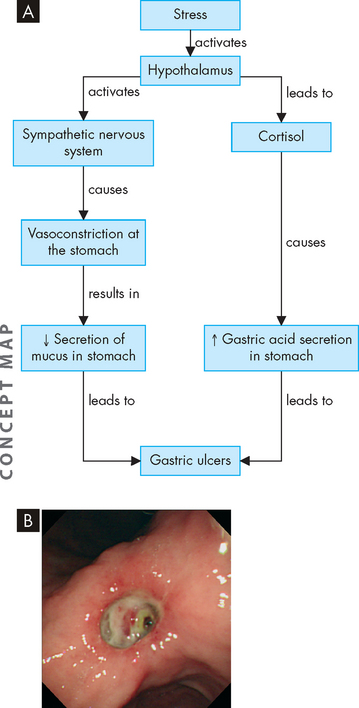
FIGURE 34-6 A The effects of stress on the development of gastric ulcers. B Gastric ulcer.
Source: Feldman M. Sleisenger & Fordtran’s gastrointestinal and liver disease. 8th edn. Philadelphia: Saunders; 2006.
Cortisol causes the breakdown of lipids and proteins to increase blood glucose levels; however, the decreased amount of protein production in the tissues can lead to complications including delayed wound healing (see Figure 34-7). The interaction of the glucocorticoids with the cytokines released from increased inflammation may contribute to the impaired wound healing.15 In fact, psychological stress in the time after surgery can lessen the repair of a surgical wound, which highlights the importance of reducing stress in patients in order to promote their recovery.16
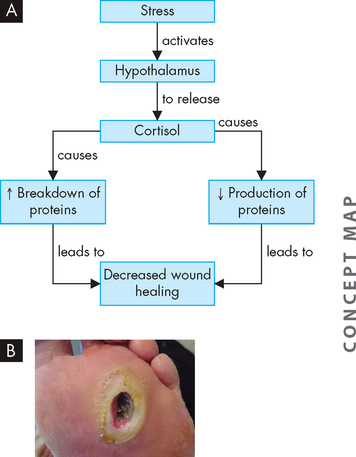
FIGURE 34-7 A The effects of stress on wound healing. B Wound healing of a vascular ulcer.
Source: Brown D, Edwards H. Lewis’s medical–surgical nursing. 2nd edn. Sydney: Mosby; 2007.
The breakdown of protein from bone, decreased calcium absorption from food and increased renal excretion of calcium, all of which occur with stress, lead to bone weakness and osteoporosis (see Figure 34-8). The muscle weakness due to the breakdown of muscle protein can make individuals prone to falls and, combined with weak bones, this increases the likelihood of bone fracture.
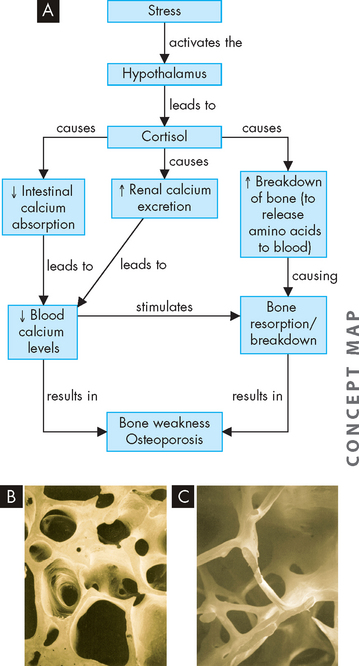
FIGURE 34-8 A Elevated levels of cortisol and the development of osteoporosis. Compare normal bone, B, with bone from osteoporosis, C. Images are scanning electron micrographs.
Source: Patton KT, Thibodeau GA. Anatomy & physiology. 7th edn. St Louis: Mosby; 2010.
In addition, stress interferes with a wide variety of neurological functions. The stress response is linked with a disruption to the blood–brain barrier, so that additional substances from the blood may be allowed to cross into the brain and contribute to alterations in brain activities.17 Cortisol affects mood and behaviour18 and stress is associated with changes in cognition, appetite, sleep and sensory perception.19 There is also evidence that stress impairs memory processes associated with the hippocampus, an important region of the brain involved in memory — as well, there is evidence of the hippocampus undergoing atrophy (shrinkage) with chronic stress.20,21 The functioning of both the hippocampus and the hypothalamus is altered with chronic stress.22,23
Stress, inflammation and chronic disease
Several conditions with various pathophysiological characteristics appear to have a common origin relating to chronic inflammation.24,25 These conditions include cardiovascular disease, type 2 diabetes mellitus, other diseases associated with ageing and some cancers. All are characterised by a prolonged presence of pro-inflammatory cytokines (which promote the inflammatory response by activating inflammatory mediators).24,25 Stress and negative emotions are associated directly with the production of increased levels of pro-inflammatory cytokines, providing a possible link between stress, immune function and disease.26–28 4 6 In fact, the individualised nature of the stress response is such that anticipatory stress and worry can elongate and enhance the adverse effects of stress on the cardiovascular, immune and other systems.29
The link between chronic disease, stress and inflammation is particularly relevant to Australian and New Zealand healthcare settings, as chronic diseases are particularly prevalent in our societies. The leading causes of death in Australia include heart disease (such as coronary heart disease, hypertension and heart failure), cerebrovascular accidents, diabetes mellitus and cancers (respiratory, colorectal, haematological, prostate, breast, pancreatic and skin).30 The list is similar in New Zealand, with coronary heart disease, cerebrovascular accidents and cancers (respiratory, colorectal, breast, prostate, stomach and cervical) all featuring as main causes of death.31
The stress response causes increased blood lipid levels, and hyperlipidaemia is strongly associated with the development of atherosclerotic processes in the heart leading to ischaemic heart disease, as well as in the brain leading to stroke. In addition, the increased blood volume leads to hypertension, a main contributor to cardiovascular disease (see Figure 34-9). For further details on cardiovascular disease, refer to Chapter 23.
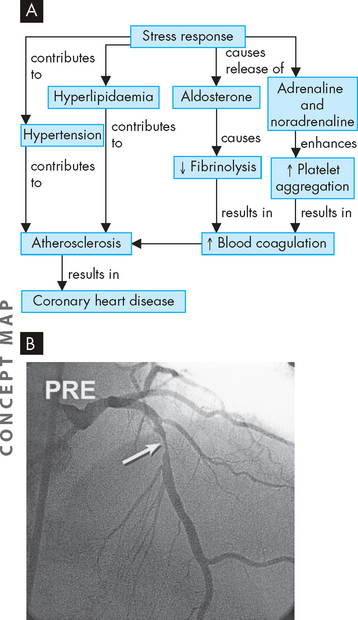
FIGURE 34-9 A The relationship between stress and coronary heart disease. B Angiographic image before placement of a sirolimus-eluting stent. The left anterior descending artery contains a tight stenosis (arrow).
Source: Goldman L. Cecil medicine. 23rd edn. Philadelphia: Saunders; 2007.
The elevated blood glucose levels that occur for extended periods during chronic stress can contribute to diabetes mellitus (see Figure 34-10), as well as pre-diabetic conditions and metabolic syndrome. In addition, there is a connection between stress and the development of abdominal or visceral obesity (as lipids are broken down from the body periphery and deposited around the abdomen).3 This chronic condition is associated with lower quality of life and has a strong relationship with the development and worsening of both diabetes mellitus and cardiovascular disease. (Obesity and diabetes mellitus are discussed in Chapter 35.)
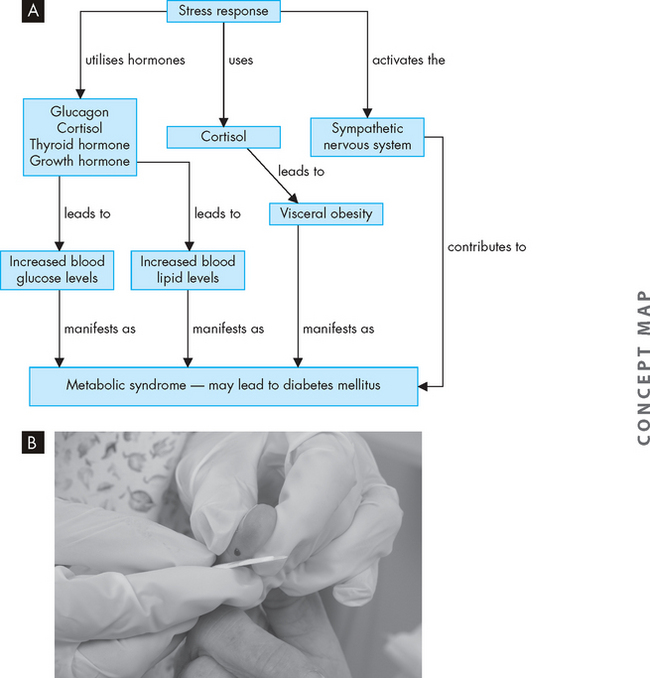
FIGURE 34-10 A The relationship between stress and diabetes mellitus. B Blood glucose monitoring for a patient with diabetes mellitus.
Source: Funnell R. Tabbner’s nursing care. 5th edn. Sydney: Churchill Livingstone; 2008.
There are strong relationships among stress, the immune system and cancer. Stress-induced immune changes affect many immune cell functions, including decreasing natural killer cell and T cell cytotoxicity. In addition, there is a relationship between infection and the development of cancer: approximately 15–20% of cancers are attributed to infection.32 For example, hepatitis C is strongly linked with liver cancer, human papillomavirus is related to cervical cancer and Helicobacter pylori is related to stomach cancer. Because the infection activates inflammation, cancer is actually described as an inflammatory disease in these cases.33–35 4 6 In addition, the inflammatory bowel disease ulcerative collitis is a risk factor for the development of colorectal cancer. Although the relationships among infection, inflammation and cancer may appear simple, in fact the detailed mechanisms by which these processes occur are quite complex and are still being researched33 (see Chapter 36 for detailed discussion on cancer). What is clear is that stress can adversely influence many disease processes, particularly those with an inflammatory process. Impairments of immune function may have dire health consequences for stressed individuals, including increased risk of infection and cancer.
MODULATION OF THE STRESS RESPONSE
Psychological influences on stress
Many stressors do not necessarily cause a physiological stress response if psychological factors are minimised. Stress itself is not an independent entity, but rather a system of interdependent processes moderated by the nature, intensity and duration of the stressor and the perception, appraisal and coping abilities and resources of the affected individual, all of which in turn mediate the psychological and physiological responses to stress.
In psychological distress, the individual feels a general state of unpleasantness after life events that manifests as physiological, emotional, cognitive and behavioural changes. Periods of depression and emotional upheaval are often associated with adverse life events and place the affected individual at risk for immunological deficits, increasing the risk of ill-health.5 Examples of triggering circumstances include bereavement (see the box ‘Health alert: partner’s survival and spouse’s hospitalisations or death’), academic pressures and marital conflict.
Stressful life events and mood have been reported as important factors preceding the onset or exacerbation of symptoms in acquired immune deficiency syndrome (AIDS) infection, diabetes mellitus and multiple sclerosis.36–38 4 6 In addition, interaction with healthcare providers in a clinical setting, the diagnosis of a major illness and various clinical procedures (e.g. blood sampling, injections, examinations, surgical procedures) may represent significant negative life events for many individuals (see Figure 34-11). These additional stressors may interfere with the efficacy of the medical intervention. Identifying and reducing stress in the clinical setting have particular applicability for both preventing disease and managing illness.
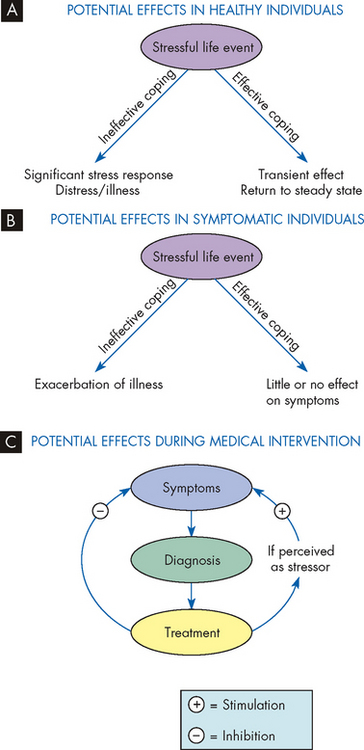
FIGURE 34-11 Health outcome determination in stressful life situations is moderated by numerous factors.
Whether a life-challenged individual experiences distress or illness depends on the subject’s appraisal of the event and the coping strategies used during the stressful period. Models A and B reflect possible outcomes in stressed healthy and symptomatic individuals. Model C illustrates the dynamic clinical setting in which the diagnosis of a serious illness and subsequent medical interventions may be perceived as stressful challenges and have potentially detrimental influences on physical outcome.
Personality types
Personality characteristics are associated with individual differences in the interpretation of stressors. A beneficial influence during stress has been shown with effective or adaptive coping strategies, especially if they are problem-focused and involve social support.39 Coping is the process of managing stressful challenges that tax the individual’s resources.39 Adverse consequences of stress may be minimised by coping styles, as the stress signal reaching the hypothalamus will be less intense. Coping styles associated with altered immunity include repression (unconscious forgetting of periods of intense stress), denial, escape-avoidance and concealment.6 Repression has been associated with lower monocyte counts, higher eosinophil counts, higher serum glucose and more self-reported medication reactions in medical outpatients.40 In addition, higher Epstein-Barr virus antibody titres have been observed in students who exhibit repression.41 Another study found increased markers of accelerated human immunodeficiency virus (HIV) infection in men who concealed their homosexual identity42 and therefore were living with the stress of keeping an important secret.
Partner’s survival and spouse’s hospitalisations or death
A spouse’s chances of dying increase not only when the partner dies but when that partner becomes seriously ill. In a 9-year follow-up study consisting of 518,240 elderly couples, mortality after the partner’s hospitalisation varied according to the spouse’s diagnosis. A wife’s hospitalisation increased her husband’s chances of dying within 1 month by 35%; a husband’s hospitalisation increased his wife’s chances of dying by 44%. Likewise, a wife’s death increased her partner’s 1-month mortality risk by 53% and a husband’s death raised his partner’s risk by 61%. The researchers commented that a spouse’s illness or death can increase a partner’s mortality by the bereavement causing severe stress, as well as removing a primary source of emotional, psychological, practical and financial support. In another study, those who were bereaved had higher levels of depression, anxiety and anger compared with those who had not recently lost their partner. In addition, those who were unprepared for the death, were of younger age and had decreased levels of sleep had more depressive symptoms.
Source: Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med 2006; 354(7):719–730; Buckley T et al. Prospective study of early bereavement on psychological and behavioural cardiac risk factors. Int Med J 2009; 39:370–378.
Mediating factors that may influence stress susceptibility or resilience include age, socioeconomic status, gender, social support, religious or spiritual factors, personality, self-esteem, genetics, past experiences and current health status. Evidence suggests that effective intervention may result in greater stress resilience and improved psychological and physiological outcomes.43 For example, women with recurrent metastatic breast cancer who were provided weekly group counselling in addition to routine medical treatment lived an average of 19 months longer than control subjects.44 On the other hand, those who had major stressors in their lives had increased incidence (or relapse) of their breast cancer.45 These important findings highlight the serious and adverse effects of stress on health.
The importance of social support for seriously ill individuals has focused attention on the health of caregivers. Significant stress manifested as depression, anxiety and fatigue has been noted in family caregivers of those with cancer, Alzheimer’s disease and burn trauma. Patients and caregivers exhibited suppression of various measures of immune function, with improved function associated with better perceived social support. Therefore, the improved ability to cope with the stress has had a positive outcome on the stressed individual.
Sex hormone influences on stress
Gender-based coping differences may be attributed, in part, to the sex hormones, with females more likely to offer social support, a behaviour with an oxytocin/oestrogen association.46 Oxytocin is a pituitary hormone with stress-decreasing properties: this has been shown in animal experiments, where elevations in oxytocin were associated with reduced hypothalamic-pituitary-adrenal axis activation and reduced anxiety.47 Oxytocin in some tissues works in concert with oestrogen; these two hormones have a calming effect during stressful situations.48 The oxytocin-mediated calming of the stress response may promote the ‘tend and befriend’ response, more commonly experienced by women because oestrogen is a co-mediator.46 Also, oestrogen is thought to mediate the more robust immunological profiles of females,49 resulting in enhanced resistance to infection but risk for autoimmune diseases.
Testosterone, secreted by the testes, actually decreases after stressful stimuli such as anaesthesia and surgery.50 In addition, psychological stimuli decrease testosterone levels, and individuals with respiratory failure, burns and congestive heart failure show a marked reduction in plasma testosterone.51 Decreased levels of testosterone occur during ageing and are associated with a lower cortisol responsiveness to stress-induced inflammation, suggesting a decreased physiological response to chronic stress in older men.24 Because testosterone decreases in response to such varied physical stresses, it has been suggested that testosterone may impair the ability to respond to stress. In acute, severe physical stress situations, males may be at a disadvantage because the presence of testosterone has not declined quickly enough. Males have a higher risk for morbidity after injury and testosterone exhibits immunosuppressive activity.51 Thus, different effects of stress on males and females may be partly explained by gender-related hormonal profiles that influence the characteristics, quality and outcomes of the stress response.
Strategies for coping with stress
Interventions to prevent or manage stress-related psychological or physical problems include both short- and long-term coping strategies. Educational components are specific to the individual’s problems. Exercise is one of the useful tools for minimising the adverse effects of stress, as discussed above. Relaxation techniques can lower the physiological stress response (see Figure 34-12) and may include meditation, imagery, massage, yoga, breathing exercises and biofeedback. These approaches may be used on an individual or support-group basis. In fact, breathing exercises are a suggested approach in the management of paroxysmal (short, frequent) hypertension.52 Incorporating these approaches into clinical training facilitates their use in the clinical arena. Future research should focus on the efficacy of such approaches with various populations.
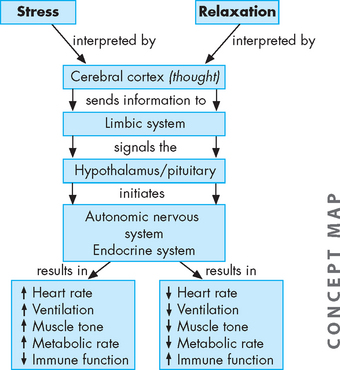
FIGURE 34-12 A simplified chart showing the cyclic mind–body and body–mind influences of stress and relaxation, and on health. As our body experiences the physical responses to stress and relaxation, our central nervous system remembers them, causing a continuation of the cycle and resulting in long-term positive or negative physical consequences.
Source: Based on Rakel D. Integrative medicine. 2nd edn. Philadelphia: Saunders; 2007.
Physical activity
The potential benefits of exercise on minimising the impact of stress are extensive.53 For example, with exercise there is a substantial improvement in glucose tolerance, which improves diabetes mellitus and related conditions.54 Hyperlipidaemia improves and abdominal fat decreases with exercise.55,56 The effects of chronic stress within the brain are effectively counteracted by moderate exercise.57 In fact, those who are more physically fit actually have a less heightened stress response,58,59 which shows the benefits for the body in minimising the undesirable effects of chronic stress.
However, the overall amount of physical activity that we undertake is quite low. In Australia, 35% of people lead sedentary lives and a further 37% undertake only low levels of exercise, meaning that 72% of people over the age of 15 do not undertake the recommended moderate exercise levels.60 The data are more positive in New Zealand, with only 49.5% of the population not undertaking regular physical activity61 — but this figure is still high.
CIRCADIAN RHYTHMS AND SLEEP
Many factors undergo regular daily patterns, such as body temperature and the secretion patterns of some hormones. In this section we explore how some hormones involved in the stress response are secreted in patterns associated with the circadian rhythm. We also consider how the stress of shift work and altered sleep patterns may influence disease.
Hormonal fluctuations with the circadian rhythm
Two key hormonal systems associated with circadian fluctuations are cortisol and growth hormone. The secretion of cortisol rises towards the end of the night, around the normal time of waking up. It is likely that the surge of cortisol at this time assists in elevating blood glucose levels, due to the lengthy time since eating prior to sleep. The effects of cortisol cause a morning breakdown of proteins to increase blood glucose. One of the benefits of eating breakfast is that it can help to counteract the effects of cortisol on protein breakdown, as glucose becomes available from the food. The secretion of growth hormone surges during the middle of the night. The increase of this hormone during the first few hours of sleep may be to enable the maintenance of growth and restorative processes, at a time when the body’s overall demands for oxygen and nutrients are low.
Although circadian rhythms set up the regular, cyclical patterns of hormonal secretion in the healthy individual who has regular sleep patterns, these rhythms are overcome by the stress response.62 This means that periods of stress cause surges in the hormones at times of the day that do not necessarily match the regular circadian patterns. The interactions between the circadian rhythm, stress and the hypothalamic response to stress can alter cortisol secretion and the immune system function (see Figure 34-13).
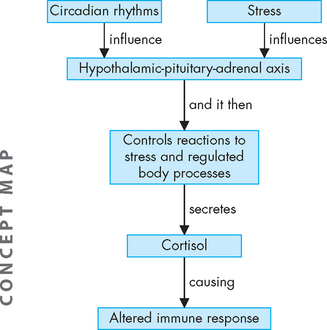
FIGURE 34-13 Alterations in the circadian rhythms and the effects of stress influence the hypothalamic-pituitary-adrenal axis, which in turn modifies secretion of cortisol to alter the immune system responses.
Source: Based on Johnson SL. Therapist’s guide to posttraumatic stress disorder intervention. London: Academic Press/Elsevier; 2009.
Disturbances to regular sleep patterns and alterations in hormonal secretion
The relationships between regular sleep patterns and the immune system are complex. The pineal gland regulates the immune response and mediates the apparent effects of circadian rhythm on immunity (the role of the pineal gland in sleep is discussed in Chapter 6). When melatonin production in the pineal gland is blocked (by continuous light or by pharmacological means), the immune response is suppressed; whereas administration of melatonin reverses these effects.63 This may affect immune changes found with sleep disturbances and altered circadian rhythms,64 which are common among acutely ill and stressed patients.
Irregular or inadequate levels of sleep can interrupt the body’s normal circadian rhythms. Insufficient sleep may link to weight gain (see Figure 34-14), which is a substantial issue in our society. Glucose tolerance and balance in the morning appear to be related to growth hormone secretion through the night and to the overall levels and fluctuations of blood glucose and insulin levels that occur during sleep.65,66 This suggests that insufficient sleep may lead to impaired tolerance to glucose — which is a contributing factor to diabetes mellitus. Alterations in sleep patterns are associated with additional surges in growth hormone secretion, even prior to the commencement of sleep. On the other hand, the secretion pattern of cortisol varies less with altered sleep than is seen with growth hormone. This suggests that cortisol levels are strongly tied with the cycle of day and night.67
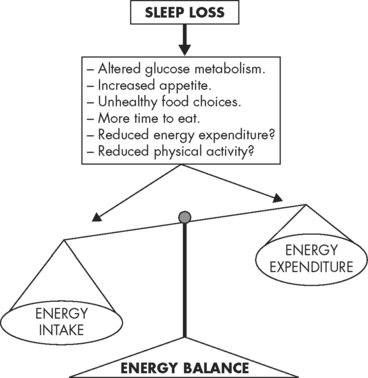
FIGURE 34-14 A schematic representation of potential pathways through which sleep loss may lead to a positive energy balance in which energy intake is greater than energy expenditure.
Source: Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin 2007; 2:187–197.
Shift work and disease
Above we have considered some of the benefits of maintaining adequate patterns of sleep, but many people do not maintain regular sleep patterns and in this section we explore some of the issues that may arise from irregular sleep. Of particular concern to healthcare workers is the impact of shift work on circadian rhythms and stress. In the healthcare industry (and other industries) where staff are required to work irregular shifts throughout the day and night, resistance to illness and disease may be altered.
Secretion of the hormones melatonin and cortisol remain similar to their regular pattern during the first few days of shift work, but the pattern of growth hormone secretion appears to be affected more quickly.68 In those whose employment is based on shift-work, there are decreased secretions of cortisol, with increased growth hormone.68 It can take two weeks of adaptation before the new circadian rhythm is reset62 — at this point, the shift worker may have been rotated to a different shift roster and so the process of adjusting needs to start all over again.
Shift work is associated with a decreased ability to perform tasks as well as gastrointestinal disturbance,69 insomnia and sleepiness at undesirable times70 — this is known as shift-work sleep disorder. There is some evidence of an increased risk of cancer (breast, colon and prostate)71,72 in those who work night shifts. In addition, melatonin secretion is decreased in those who work night shifts, which may be related to an increased risk of endometrial cancer71 — however, this risk has been shown to occur in obese people and not those of normal weight, which indicates the complex nature of this system.
There is also evidence to indicate that shift work may be associated with chronic disease such as coronary heart disease, metabolic syndrome and infection, but it is unclear why this is so and whether it is a result of the shift work itself or other lifestyle factors.73 Complicating the issue further is evidence that factors such as gender, age and weight are more significant than the influence of shift work on health complaints,74 as well as the finding that breast cancer risk is not linked to shift work.75 One theory that has been proposed over the last few decades is that the use of lighting at night may be a factor in some undesirable health effects, perhaps by causing a reduction in the amount of melatonin produced.72,75–77 4 6 The actual relationship between the altered hormonal and circadian patterns that occur with insufficient sleep and the medical alterations of shift workers is quite complex and is still being determined.68
AGEING AND STRESS
With ageing, a set of neurohormonal and immune alterations, as well as tissue and cellular changes, may develop. These changes include a rise in the blood concentration of adrenaline and noradrenaline (catecholamines), antidiuretic hormone and cortisol. There is also a pattern of chronic inflammation and increased blood coagulation. These stress-related alterations of ageing can influence the course of developing stress reactions and lower adaptive reserve and coping. In addition, the process of ageing itself can trigger a psychological stress for some people.78
The general adaptation syndrome
 Stress is defined as the state of affairs arising when a person relates to (i.e. interacts or transacts with) situations in a certain way. How the individual appraises and reacts to situations is important.
Stress is defined as the state of affairs arising when a person relates to (i.e. interacts or transacts with) situations in a certain way. How the individual appraises and reacts to situations is important.The stress stimulus
 Physical stressors directly activate the hypothalamus, while other stressors require integration of sensory information to determine whether the situation is a stress; if so, then the hypothalamus will become activated. The stress response is initiated when a stressor is present in the body or perceived by the mind.
Physical stressors directly activate the hypothalamus, while other stressors require integration of sensory information to determine whether the situation is a stress; if so, then the hypothalamus will become activated. The stress response is initiated when a stressor is present in the body or perceived by the mind.The detection of stress
 Stress is detected by the hypothalamus. While physical trauma activates the hypothalamus, other sensory information is interpreted by the hypothalamus, to determine whether it is a stress.
Stress is detected by the hypothalamus. While physical trauma activates the hypothalamus, other sensory information is interpreted by the hypothalamus, to determine whether it is a stress. In the alarm stage, the sympathetic nervous system becomes activated to undergo a mass discharge of activity. Hormones are released via the hypothalamic-pituitary axis.
In the alarm stage, the sympathetic nervous system becomes activated to undergo a mass discharge of activity. Hormones are released via the hypothalamic-pituitary axis.Physiological effects of the stress response
 In general, the sympathetic nervous system releases adrenaline and noradrenaline (catecholamines), which prepare the body to act by: increasing cardiac output and increasing blood flow to the heart, brain and skeletal muscles by dilating vessels that supply these organs; bronchodilation, which increases delivery of oxygen to the bloodstream; and increasing mental alertness.
In general, the sympathetic nervous system releases adrenaline and noradrenaline (catecholamines), which prepare the body to act by: increasing cardiac output and increasing blood flow to the heart, brain and skeletal muscles by dilating vessels that supply these organs; bronchodilation, which increases delivery of oxygen to the bloodstream; and increasing mental alertness. The hypothalamus stimulates the pituitary gland to secrete adrenocorticotropic hormone, which in turn stimulates the adrenal cortex to secrete cortisol: cortisol mobilises glucose, lipids and amino acids. Cortisol at low levels consistent with stress can increase humoral immunity, activate pro-inflammatory mediators and decrease cellular immunity. Cortisol at high levels (e.g. therapeutic levels) decreases both humoral and cellular immunity and is anti-inflammatory.
The hypothalamus stimulates the pituitary gland to secrete adrenocorticotropic hormone, which in turn stimulates the adrenal cortex to secrete cortisol: cortisol mobilises glucose, lipids and amino acids. Cortisol at low levels consistent with stress can increase humoral immunity, activate pro-inflammatory mediators and decrease cellular immunity. Cortisol at high levels (e.g. therapeutic levels) decreases both humoral and cellular immunity and is anti-inflammatory.Modulation of the stress response
 Personality characteristics are associated with individual differences in appraisal and response to stressors. Coping styles associated with altered immunity include repression, denial, escape-avoidance and concealment.
Personality characteristics are associated with individual differences in appraisal and response to stressors. Coping styles associated with altered immunity include repression, denial, escape-avoidance and concealment.Circadian rhythms and sleep
 Fluctuations in growth hormone and cortisol occur normally over a 24-hour cycle. Disturbances in sleep patterns can alter the cycle of hormone secretion, which is related to development of disease. Shift work may be associated with some adverse health effects, including decreases in concentration and the development of some cancers, although research into this is continuing.
Fluctuations in growth hormone and cortisol occur normally over a 24-hour cycle. Disturbances in sleep patterns can alter the cycle of hormone secretion, which is related to development of disease. Shift work may be associated with some adverse health effects, including decreases in concentration and the development of some cancers, although research into this is continuing.Stephen owns a small business in the swimming pool industry and had to take some time away from work recently to undergo knee surgery. Although Stephen was concerned about having to be away from his business at a time when the weather was warm and work was busy, his surgery was necessary so he booked into hospital. After the surgery, Stephen stayed in hospital overnight but found it very difficult to sleep due to the noise of the staff and other patients. On returning home, pain and discom fort from his knee kept waking him up through the night. In the days after surgery, Stephen undertook short periods of work, managing the accounts and taking orders, and was regularly on the phone to his staff. The knee surgery was a success, but after 2 weeks Stephen noticed that his wound had developed an infection, so he saw his doctor immediately. The infection was obviously clearing after a few days of antibiotic therapy.