Chapter 16 Antianxiety, sedative and hypnotic drugs
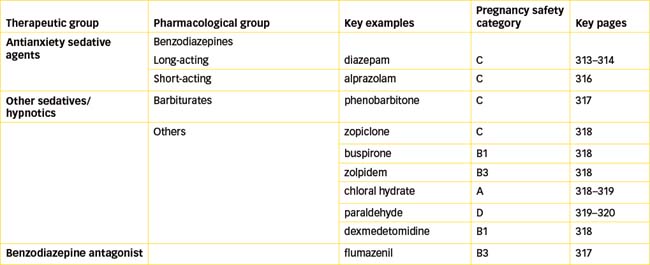
Anxiety, worry and insomnia are health problems that occur commonly across the lifespan. When anxiety or fear is in response to a threat or danger, this is a normal physiological response to a threatening situation. However, excessive anxiety or panic that interferes with daily functioning and sleep is counterproductive and usually requires medical intervention and treatment. Insomnia is a common sleep disorder and is often a concern in the elderly. This chapter reviews the antianxiety, sedative and hypnotic drugs available to treat these disorders. Barbiturates were previously used extensively as sedative–hypnotic agents, but because of their low selectivity and safety they have largely been replaced by the safer benzodiazepines, which have a specific anxiolytic (antianxiety) action, and newer related agents.
Key abbreviations
Key background: sleep and anxiety
Physiology of sleep
SLEEP is a recurrent, natural, reversible condition of inertia, reduced consciousness and reduced metabolism, during which a person is no longer in sensory contact with the immediate environment, and stimuli no longer attract attention or exert a controlling influence over voluntary and involuntary movements or functions. The purpose of sleep is unknown; however, prolonged sleep deprivation is harmful, causing depression, mental disturbances and hallucinations.
Stages of sleep
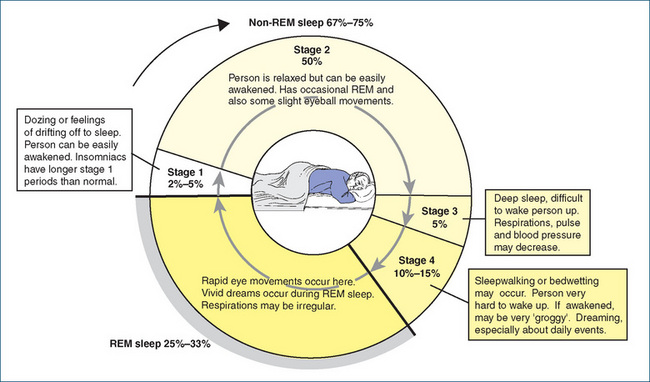
Sleep is not just one level of unconsciousness. It consists of two basic stages that occur cyclically: non-rapid eye movement (non-REM) sleep and rapid eye movement (REM) sleep (when eye movements show under the closed lids). The stages of sleep are based on electrical activity that can be observed in the brain by means of an electroencephalograph (EEG). The EEG provides graphic illustrations of brain waves, which are an indication of the electrical activity occurring in the brain, and is useful in the study of seizures and antiepileptic drugs (see Figure 17-1).
During sleep, the individual moves first through the four stages of non-REM sleep (Figure 16-1). These are characterised on an EEG by alpha waves, which are slow and of low amplitude. The sleeper then passes into REM sleep, the fifth stage of sleep, characterised by rapid eye movements, dreaming and fast, low-amplitude waves on an EEG. Periods of REM and non-REM sleep alternate throughout the night. Infants spend a greater proportion of sleep time in REM sleep than do adults (Figure 16-2). REM sleep is not synonymous with light sleep. It takes a more powerful stimulus to arouse a person from REM sleep than from synchronous slow-wave sleep.
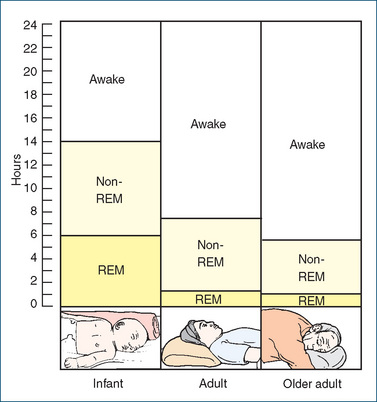
Figure 16-2 Sleep–wake cycles across the lifespan. Infants: approximately 40% of total sleep time is REM. Adults: 20% of total sleep time is REM. Older adults: total sleep time is slightly reduced; REM remains 20% of total. Source: Beare & Myers 1998.
Sleep research indicates that there are psychological and physiological reasons for the body to maintain equilibrium between the various stages of sleep. Physiological functions of the body tend to be depressed during non-dreaming and deep sleep: blood pressure (falls by 10–30 mmHg), pulse rate, metabolic rate, gastrointestinal tract activity, urine formation, oxygen consumption and carbon dioxide production, body temperature, respirations and body movement all decline. In contrast, during REM dreaming sleep, body and eye movements are more noticeable (moving of the arms and legs, talking, crying or laughing). When individuals are deprived of deep sleep, they become physically uncomfortable and depressive, tend to withdraw from friends and society and are less aggressive and outgoing.
Dreaming sleep is also important, as individuals deprived of dreaming sleep experience a range of undesirable effects: confusion, suspicion, withdrawal, anxiety, difficulty concentrating and increase in appetite with a definite weight gain.
Sleep disorders
Each individual establishes his/her own normal sleep pattern. This can vary from night to night and is influenced by the individual’s emotional and physical state. The sleep pattern is controlled from the ascending reticular activating system in the brainstem (see Figure 14-2, and section in Chapter 14 on CNS functional systems).
Insomnia
Insomnia is the inability to obtain adequate sleep, whether from difficulty in falling asleep, frequent nocturnal waking or early awakening. Excessive intake of CNS stimulants such as caffeine-containing drinks can cause insomnia, as can anxiety disorders, depression, alcohol abuse, environmental factors (heat, cold, noise), pain, cardiac or respiratory disorders and jet lag. Disorders of excessive daytime sleepiness may be due to inadequate sleep at night, excessive use of CNS depressants (including antidepressants, antihistamines and alcohol), narcolepsy (sudden sleep attacks) or sleep apnoea causing disturbed sleep at night. Clinical Interest Box 16-1 lists some drugs that can cause insomnia or sedation.
Anxiety
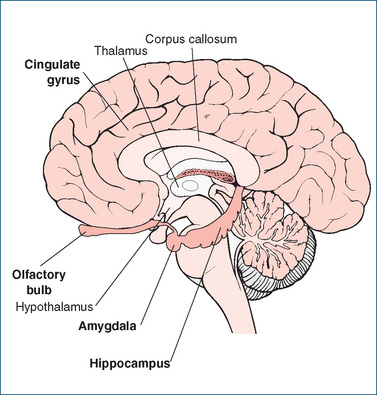
Anxiety is a state or feeling of apprehension, agitation, uncertainty and fear resulting from the experience or anticipation of some stress, threat or danger. It is usually a natural psychological and physiological response to a personally threatening situation, such as a threat to one’s health, body, loved ones, job or lifestyle. Generally, this anxiety effectively stimulates the person to take constructive actions to counteract the perceived threats. In its extreme form, anxiety can be characterised by autonomic nervous system responses including rapid heart rate, dry mouth, sweaty palms, insomnia, loss of appetite, muscle tremor, diarrhoea and dyspnoea. Anxiety is thought to be mediated in the limbic system of the cerebrum (Figure 16-3); neurotransmitters especially involved are 5-HT and GABA (see Chapter 14 and Table 14-1).
When excessive anxiety interferes with daily function ing, help may be necessary. Many non-pharmacological treat ments such as counselling and behaviour modification therapies are available, and anxiolytic drugs (antianxiety agents) are commonly prescribed for the short-term treatment of anxiety. These drugs reduce feelings of excessive anxiety, such as apprehension, fear and panic, and reduce the physiological responses, such as breathlessness and insomnia, thus improving sleep patterns. Hence anxiolytic drugs both directly and indirectly are also sedatives/hypnotics.
Related disorders
Generalised anxiety disorder is considered to exist when a patient has symptoms of excessive anxiety, worry, irritability, muscle tension and sleep disturbances about various events for a period of six months or longer. Other associated disorders include adjustment disorder with anxious mood, panic attacks, panic disorder, obsessive– compulsive disorder, phobic disorders and post-traumatic stress disorder. For most of these conditions drug therapy is not the preferred option. Recommended primary therapies include counselling, relaxation techniques, stress management and cognitive behaviour therapy. Short-term use of anxiolytic or antidepressant drugs is sometimes required.
Treatment of sleep disorders
Sleep hygiene
Management of sleep disorders requires careful attention to specific sleep history and patterns, drug history including use of ‘social’ drugs such as caffeine and alcohol and discussion of lifestyle and psychological factors that might impair good sleep cycles. Any physical or depressive disorders that might disturb sleep need treating. Nonpharmacological treatments include attention to ‘sleep hygiene’ (promotion of good sleep patterns; see Clinical Interest Box 16-2) before hypnotic drugs are tried. Owing to the risk of dependence, hypnotic drugs should be used only for limited periods, e.g. 2–4 weeks to assist with anxiety, impaired sleep cycles following jet lag or shift-work changes; or one-off doses as preoperative medication. Sedative drugs are not recommended for patients over 60 years, those who need to drive or make important decisions the next day or those who live alone.
Clinical interest Box 16-2 Sleep hygiene
Sleep hygiene includes various useful non-pharmacological strategies for sleep promotion.
Minimise stimuli that promote wakefulness, such as:
Sleep-enhancing influences include:
Adapted from: Therapeutic Guidelines: Psychotropics 2008.
Sedatives and hypnotics
Drugs used to promote sleep include the sedatives and hypnotics; all are central nervous system (CNS) depressants. Sedatives reduce alertness, consciousness, nervousness or excitability by producing a calming or soothing effect. Hypnotics induce sleep. The major difference between a sedative and a hypnotic is the degree of CNS depression induced: the same drug might be used in small doses for a sedative effect and in larger doses for hypnotic effects. These drugs were previously called the minor tranquillisers to distinguish them from the antipsychotic drugs (major tranquillisers) used in treating schizophrenia. Antipsychotics and tricyclic antidepressants are not recommended for treatment of insomnia; however, the selective serotonin reuptake inhibitors (SSRIs) are indicated for treatment of the more severe anxiety disorders including panic disorder and obsessive–compulsive dis order (see Chapter 18).
Paediatric drug use
Because young children are more sensitive than adults to the CNS-depressant effects of antianxiety, sedative or hypnotic drugs, use of these agents is not recommended and counselling and psychotherapy are usually tried first (see Clinical Interest Box 16-3). Paradoxical reactions (reactions contrary to the expected reaction) have been reported with the use of antihistamine and barbiturate sedatives in children. Such reactions include increased excitability, hostility, confusion, hallucinations and acute elevation of body temperature. However, sedation may be indicated for particular situations if the drug and dosage are carefully selected for the individual child. Antihistamines and chloral hydrate are generally safe for mild sedation.
Clinical interest Box 16-3 Paediatric implications
Antianxiety agents and sedatives
Indications for their use include treatment of convulsive disorders (see Chapter 17), as an adjunct pre-anaesthetic agent or for sedation of a child in intensive care to minimise the risk of removal of catheters. Benzodiazepines should be avoided except for short-term use in specific conditions, such as night terrors or sleepwalking; close monitoring and assessment by the health-care provider are required. Etomidate, an IV induction anaesthetic agent, is a useful drug for sedation of children before medical or surgical procedures
Geriatric drug use
Elderly people have more fragmented sleeping patterns than do younger adults; they may take multiple daytime naps, tend to go to bed earlier, may have difficulty in falling asleep and wake up earlier. Primary sleep disorders, including sleep apnoea and restless legs syndrome, and other factors such as retirement, death of a close friend or spouse, social isolation and increased use of medications also contribute to disturbed sleep (see Clinical Interest Box 16-4).
Clinical interest Box 16-4 Falls and fractures in the elderly
Sleep disturbance is one of the most frequent concerns of elderly people; anxiety may interrupt sleep, and reduced activity and increased ‘cat-naps’ during the day may reduce the need for long sleep at night. Elderly people should be evaluated for pre-existing health conditions that can alter sleep patterns, such as arthritic pain, hyperthyroidism, cardiac dysrhythmia, respiratory difficulties, paroxysmal nocturnal dyspnoea and the need to urinate.
Studies have shown that each year about 30% of people aged over 65 have a major fall, with the rate even higher in nursing homes (Cumming 1998); many falls lead to fractures, particularly hip fractures with severe associated morbidity and mortality. Tracing links between medications and falls reveals:
A recent study on the effects of CNS medications in older adults living in communities showed that the greater the use of CNS depressants such as benzodiazepines, antidepressants, antipsychotics and opioids, the worse was the decline in cognitive function over five years (Wright et al 2009). Higher doses and increased number of CNS medications increased the risk of falls, with an extra 2 falls per year likely (Hanlon et al 2009).
Given the high concentration of elderly patients with dementia in nursing homes and the lack of specific drugs effective in behavioural disturbance and dementias, it is not surprising that psychotropic agents are frequently prescribed. However, it is recommended that: hypnotics should be reserved to treat acute insomnia and, when prescribed, limited to short-term or intermittent use to avoid the development of tolerance and dependence; and that psychotropic drug use in the elderly should be minimised, especially in nursing home residents.
Hypnotic drugs are used about three times more pro rata by elderly persons than by younger adults. Drug interactions among multiple medications, altered pharmacokinetics (delayed elimination and hence increased accumulation) and increased sensitivity to CNS effects all compound to cause frequent problems. Paradoxical reactions (i.e. increased excitability, rage, hostility, confusion and hallucinations) have been reported in elderly patients taking barbiturates and, in rare instances, the benzo diazepines; these agents should be monitored.
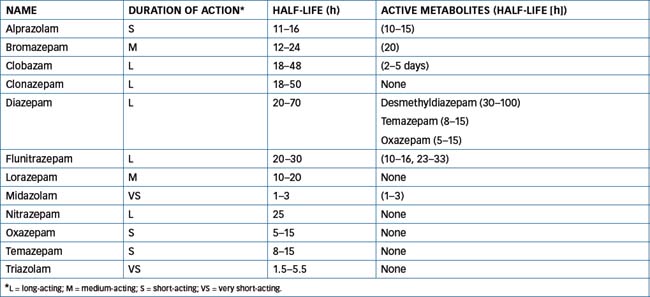
Careful drug selection and dosage are necessary to avoid producing excessive CNS depression in the elderly. Because elimination half-lives may be extended, drugs with shorter half-lives and no active metabolites are safer for geriatric patients. The short-acting benzodiazepines are much safer than the barbiturates, which are less effective anxiolytic and hypnotic agents and commonly cause confusion and ataxia. Oxazepam, lorazepam, temazepam, alprazolam and triazolam have short to intermediate half-lives (Table 16-1) and are usually recommended for elderly patients who require a benzodiazepine. Intake of hypnotic drugs should be limited to three or four times a week, allowing patients to select the nights on which they most need to take their medication. This schedule usually results in enhanced effectiveness, less daytime drowsiness or sedation and a decreased potential for inducing tolerance to the medication. Regular and careful monitoring and re-evaluation of the need for hypnotics are recommended.
Generalised anxiety in elderly people is often associ ated with depression. In this situation, antidepressant medication is more effective and safer than use of benzodiazepines, which carry an increased risk of oversedation, confusion, falls, respiratory depression and short-term memory impairment.
Benzodiazepines
The benzodiazepines are among the most widely prescribed drugs in clinical medicine, primarily because of their advantages over older hypnotic agents such as barbiturates, chloral hydrate and alcohol. These advantages include:
Diazepam (well known as Valium, see Drug Monograph 16-1) is the prototype benzodiazepine. It was the most commonly prescribed benzodiazepine for many years, until newer and safer (shorter-acting) benzodiazepines such as lorazepam and alprazolam were released. As the various benzodiazepines have similar pharmacodynamic effects, they will be discussed as a group; pharmacokinetic differences are summarised in Table 16-1.
Diazepam is the prototype benzodiazepine and as such has anxiolytic, sedative–hypnotic, muscle relaxant and antiepileptic actions by facilitating GABA-mediated CNS inhibitory pathways. However, owing to its metabolism to active derivatives and hence very long duration of action, other benzodiazepines may be indicated when short-acting sedatives are required, or for the elderly.
Indications
Diazepam is indicated for short-term (a few days) management of anxiety, acute withdrawal from alcohol, muscle spasm and spasticity, premedication and conscious sedation, and febrile seizures and epilepsy (as adjunctive treatment or for acute treatment of seizures).
Pharmacokinetics
Diazepam is one of the longest-acting benzodiazepines as it is very lipid-soluble and has active metabolites, some of which themselves are administered as benzodiazepines (see Table 16-1).
Adverse reactions
All benzodiazepines can cause excessive CNS depression, dependence and neurological dysfunction. Diazepam is likely to cause fatigue, drowsiness and muscle weakness. Less common adverse effects include disturbances of memory, GI tract function, genitourinary functions and vision and skin reactions. Paradoxical CNS stimulation can occur. Tolerance and dependence develop readily.
Drug interactions
Diazepam has additive CNS-depressant effects with all other CNS depressants including alcohol, other sedative–hypnotics, antihistamines, anaesthetics, antidepressants and antiepileptic agents. Anticholinergic effects of other drugs may be potentiated. Many drugs can inhibit the metabolism of diazepam and hence prolong its effects; examples are cimetidine and omeprazole (see also Drug Interactions 16-1).
Warnings and contraindications
Diazepam is contraindicated in people with chronic obstructive airways disease, severe respiratory or liver disease, sleep apnoea, myasthenia gravis, dependence on other substances or hypersensitivity to benzodiazepines. It should be prescribed only for short periods. Depend ence develops readily and a long withdrawal period may be necessary to avoid withdrawal seizures. Diazepam should be used only with caution in people with glaucoma, impaired kidney or liver function, depression or other psychosis, elderly or very young persons, or during pregnancy or lactation.
Dosage and administration
Dosage should be individualised depending on the person’s liver and kidney functions, age and the indication for which the drug is prescribed. Diazepam is normally given orally, the dose being 1–10 mg up to 3 times daily. It can also be administered IV or IM or by suppository.
Pharmacological effects
Benzodiazepines are not general CNS-depressants: specific actions include antianxiety, muscle-relaxant, antiepileptic, hypnotic and memory-impairing effects (see Clinical Interest Box 1-1, comparing lorazepam and ethanol as CNS depressants).
Mechanism of action
Benzodiazepines act via effects on receptors for the inhibitory CNS neurotransmitter γ-aminobutyric acid (GABA). This is the main inhibitory transmitter in the brain, at about 30% of all CNS synapses, in many pathways and brain areas (see Table14-1). There are at least 19 different subtypes of GABAA receptors; all are ligand-gated chloride channels in the membranes of postsynaptic cells and they mediate fast inhibition: when activated by GABA, there is an increase in chloride permeability and influx of chloride into the cell causing hyperpolarisation and decreased excitability of the neuron.
GABAA receptors have several sites at which drugs can act; particular sites have been identified as involved with different actions, e.g. sedative, anxiolytic, muscle relaxant or affecting cognition. The natural endogenous ligand is (obviously) GABA but other endogenous ligands have been identified, including some neuropeptides and steroid metabolites. These could be considered the body’s ‘natural diazepam’, by analogy with endorphins being named as the body’s endogenous morphine.
Benzodiazepines do not act as agonists by occupying the entire GABAA receptor, but act at a modulatory site (sometimes confusingly referred to as the benzodiazepine receptor) to facilitate GABA binding to the GABAA receptors and thus enhance chloride channel opening, leading to more neuronal inhibition. The limbic system (Figure 16-3), associated with the regulation of emotional behaviour, contains a highly dense area of benzodiazepine binding sites in the amygdala, suggesting that the antianxiety effects occur there. Patients with pathological anxiety have reduced numbers of GABA–benzodiazepine receptor complexes.
Other drugs also can bind to GABAA receptors, including the barbiturates, which have hypnotic/antiepileptic actions by acting as channel modulators at a different site on the GABAA receptors, not at the benzodiazepine binding site. Flumazenil (see later discussion) is an antagonist at the benzodiazepine binding site on the GABAA receptor, where it decreases the binding of GABA so the chloride channels remain closed. Flumazenil is anxiogenic and is used to treat benzodiazepine overdoses.
Indications for clinical use
The most common indications for benzodiazepines include anxiety disorders, preoperative medication, insomnia and sleep disturbances, seizure disorders, alcohol withdrawal, muscle spasm and panic disorder. They are also used to induce amnesia during cardioversion and endoscopic procedures. The choice of benzodiazepine depends on pharmacokinetic characteristics (Table 16-1), with longeracting (long half-life) agents such as diazepam preferred for treating anxiety and epilepsy and short-acting agents such as temazepam and midazolam preferred for induction of anaesthesia and sleep and treating insomnia. Medium-acting sedative drugs are useful for early-morning wakefulness.
Anxiety disorders
Diazepam or other long-acting benzodiazepines (clonazepam, lorazepam and flunitrazepam) are commonly used as antianxiety agents. There is overuse and abuse of these drugs (as ‘mother’s little helpers’) when the causes of anxiety should preferably be addressed. Long-term coping methods are generally better developed with behavioural therapies than with drugs. Antidepressants are also effective in generalised anxiety disorders, but have significant unwanted adverse effects.
Panic disorders
Panic is an acute condition characterised by intense fears, with palpitations, sweating, chest pain, sensations of choking or smothering and feelings of unreality or dizziness. It is often associated with anxiety about being in particular situations (alone, or in an enclosed space, in a crowd, on a bridge, in a vehicle).
Panic disorder involves recurrent and unexpected disabling panic attacks not associated with a situational trigger, with persistent concerns and behaviour changes.
First-line treatment is non-pharmacological: many patients respond to cognitive behavioural therapy and lifestyle changes, particularly control of caffeine and alcohol use.
Benzodiazepines (clonazepam or alprazolam) are effective, but the requirement for chronic administration (6–12 months) and the likelihood of dependence and sedation limit their usefulness. Various types of antidepressant drugs are also effective.
Sleep disorders
Education about sleep patterns and attention to sleep hygiene is first-line therapy for sleep disorders. Generally, sedative drugs are indicated only for short-term treatment of insomnia (2–4 weeks), owing to the risk of dependence developing and broken sleep after withdrawal. Temazepam is the preferred hypnotic for sleep disorders such as insomnia, or other short-acting agents (alprazolam, oxazepam or zolpidem or zopiclone).
Seizure disorders
Clonazepam, midazolam and clobazam are used as anticonvulsants (see Chapter 17). Parenteral diazepam is indicated for intractable, repetitive seizures, such as in status epilepticus, when its rapid onset of action is useful. Oral diazepam may be used for short-term adjunctive therapy (1–2 weeks) with other antiepileptics for the treatment of convulsions.
Preoperative medication
Diazepam, lorazepam and parenteral midazolam are used preoperatively, particularly in day-surgery and endoscopic procedures, to reduce anxiety and help induce general anaesthesia and to reduce the dose of anaesthetic needed (see Chapter 14). They can also produce a useful anterograde amnesic effect, i.e. decrease the patient’s memory of the procedure.
Pharmacokinetics
The pharmacokinetic properties of the benzodiazepines vary widely and determine the choice between the drugs in this group. For example, half-lives range from about 2 to 60 hours, and there are many metabolic interconversions to active metabolites with long half-lives (see Table 16-1).
Most benzodiazepines are lipid-soluble and readily absorbed from the gastrointestinal (GI) tract; diazepam and flunitrazepam are the most rapidly absorbed and produce a prompt and intense onset of action. The benzodiazepines become widely distributed in the body and brain. Redistribution from CNS to peripheral tissues can reduce the duration of action; for example, although diazepam has a long half-life, it has only a short duration of antiepileptic action after IV administration. Midazolam is water-soluble, so is readily formulated for injection. It has a short action as its (active) metabolite has a shorter half-life than the parent drug.
After multiple doses, they accumulate in the body’s fluids and tissues, which act as storage depots and account for the prolonged sedative actions even after the drugs have been discontinued. These drugs are mostly highly protein-bound (>85%); protein binding is reduced in newborns, in alcoholic patients and in patients with cirrhosis or impaired liver function.
The GI tract and the liver are the sites of metabolism. Benzodiazepines are often hydroxylated or demethylated to active derivatives, including desmethyldiazepam, a long-acting metabolite (30–100 hours). The long-acting benzodiazepines with active metabolites are more apt to accumulate, especially in the elderly, resulting in higher risk of falls and hip fractures. Oxazepam and lorazepam are metabolised to inactive metabolites and are preferred agents in elderly patients and people with liver disease. Metabolites are generally excreted by the kidney.
The injectable benzodiazepines include diazepam and midazolam. The onset of sedative, anticonvulsant, antianxiety and muscle-relaxant effects of these agents after intravenous administration occurs at about 1–5 minutes.
Drug interactions
Significant drug interactions can occur when benzodiazepines are used in combination with other CNS depressants or with drugs that affect their metabolism (see Drug Interactions 16-1). Effects are often unpredictable, so patients should be monitored closely. Drug metabolism interactions occur particularly with alprazolam, diazepam, midazolam and triazolam; there are relatively fewer metabolic interactions with lorazepam, oxazepam and temazepam.
Drug interactions 16-1 Benzodiazepines
| Drug or drug group | Likely effects and management |
| CNS depressants such as alcohol, antihistamines, antianxiety agents, opioids, other sedatives/hypnotics, psychotropic agents (especially clozapine) and antidepressants | Enhanced CNS-depressant effects, sedation and respiratory depression; monitoring is necessary because the dosage of one or both drugs may need adjustment |
| Many drugs can inhibit the metabolism of benzodiazepines (especially drugs that inhibit CYP3A4); examples are azole antifungals (ketoconazole and itraconazole), cimetidine, verapamil, omeprazole, macrolide antibiotics (erythromycin, clarithromycin), fluoxetine and some antivirals used against HIV infection | CNS depression and respiratory depression effects of benzodiazepines are prolonged; reduce dose or substitute a non-interacting drug |
| Drugs can increase benzodiazepine metabolism (carbamazepine, phenytoin, rifampicin, St John’s wort) | Higher dose of benzodiazepine may be required |
| Stimulant drugs such as theophylline may reduce the sedative effects of benzodiazepines | Increase benzodiazepine dose if necessary |
Adverse drug reactions
Excessive CNS depression
As a group, the benzodiazepines commonly cause excess CNS depression: drowsiness, ataxia, diplopia, vertigo, lassitude, memory loss, slurred speech and loss of dexterity. Less frequently, headaches, decreased libido, anterograde amnesia, muscle weakness and hypotension can occur, as well as increased behavioural problems (anger and impaired ability to concentrate), seen mostly with children. Neurological reactions include paradoxical insomnia, increased excitability, hallucinations and apprehension. There is a greater risk of falls and motor vehicle accidents, particularly in the elderly. Rarely, the patient can experience blood disorders, impaired liver functions and allergic reactions. See Clinical Interest Box 16-5 for the treatment of overdose.
Clinical interest Box 16-5 Management of benzodiazepine overdose
Benzodiazepine overdose is manifest as CNS depression, rang ing from confusion and drowsiness through to coma, hypotonia, hypotension and respiratory depression. Overdose is not usually life-threatening, unless multiple other drugs have been taken. Supportive treatment is necessary.
Ensure maintenance of an adequate airway, closely monitor vital signs, administer oxygen for depressed respiration and promote diuresis by administering IV fluids. Hypotension must be monitored and might require vasopressors such as noradrenaline or dopamine.
Intravenous administration of flumazenil as a specific benzodiazepine antagonist is sometimes required to avoid intubation and intensive care admission; however, it may precipitate withdrawal symptoms and seizures. Dialysis is of limited value in treating a benzodiazepine overdose.
Tolerance and dependence
With chronic administration, tolerance develops to the sedative effects, but less often to the anxiolytic effects. Dependence is common and leads to the overuse and abuse of these drugs. Dependence can develop after only a few days’ use of benzodiazepines, and withdrawal from chronic use of the drugs can be difficult. Withdrawal is characterised by CNS stimulation: anxiety, sleep disorders, aching limbs, palpitations and nervousness; seizures can occur in people who previously were taking high doses.
Withdrawal from hypnotic drugs is recommended, especially for older people who are at greater risk of harm. Withdrawal should be gradual, e.g. dose reduced by 10%–20% per week, with a few days to stabilise at each dose level. Rebound insomnia is likely, but usually lasts only 2–3 days (see NPS News 67, 2010).
Warnings and contraindications
Benzodiazepines are contraindicated in people with respiratory depression or sleep apnoea, severe hepatic impairment or myasthenia gravis. They should be used with caution in children and in the elderly, in women during pregnancy or lactation, in debilitated patients and in patients with hepatic and renal impairment.
A benzodiazepine antidote
Flumazenil, a specific benzodiazepine-receptor anta gonist, is indicated for the treatment of a benzodiazepine overdose or to reverse the sedative effects of benzodiazepines after surgical or diagnostic procedures. This drug will not reverse the effects of opioids or other non-benzodiazepine CNS-depressant drugs. Although it can reverse the sedative effects of benzodiazepines, reversal of the benzodiazepineinduced respiratory depression has not been demonstrated, so respiratory and cardiovascular support may be required.
It is administered intravenously, with antagonistic effects (reversal of sedation) occurring within 1–2 minutes and duration of action of about 1–3 hours. Because most benzodiazepines have a half-life longer than 1 hour, repeated injections of flumazenil are necessary. Flumazenil is metabolised in the liver and excreted by the kidneys.
Adverse reactions reported with this drug include headache, visual disturbance, increased anxiety, nausea and lightheadedness. Because it antagonises receptors at which the endogenous inhibitory neurotransmitter GABA acts, flumazenil can cause dangerous convulsions in patients taking benzodiazepines to control epilepsy, or in mixed overdoses with benzodiazepines and proconvulsant drugs such as antidepressants or CNS stimulants. Caution is advised when giving flumazenil to patients who are known to use benzodiazepines chronically because moderate to severe withdrawal symptoms and seizures may be precipitated.
In practice, because benzodiazepines are considerably safer than earlier sedative–hypnotics, overdose is rarely a clinical emergency and flumazenil is indicated only to avoid intubation or intensive care admission.
 Other anxiolytic and sedative/hypnotic agents
Other anxiolytic and sedative/hypnotic agents
Drugs related to benzodiazepines
Barbiturates
The barbiturates were once the most commonly prescribed class of medications for hypnotic and sedative effects; they are derivatives of barbituric acid, so named because it was discovered in 1863 on St Barbara’s Day. The first active drug in this group, barbitone, was used medically in 1903 and thousands of ‘me-too’ barbiturates soon followed. With few exceptions, barbiturates have been replaced by the safer benzodiazepines and more specific antiepileptic agents. Phenobarbitone, the prototype drug for this classification, is now used mainly as an antiepileptic (see Chapter 17), and thiopentone to induce general anaesthesia (Chapter 14).
These agents have virtually dropped out of use as sedatives. They are occasionally provided for elderly patients who remain dependent on them following chronic use.
The Z-drugs
Zopiclone
Zopiclone is a relatively new drug1 that is chemically unlike the benzodiazepines but has very similar pharmacological properties. It is a hypnotic indicated for short-term treatment of insomnia. It is rapidly absorbed, distributed and metabolised, with only one metabolite having weak CNS-depressant activity. The half-life is short (5–7 hours) but may be extended in the elderly and in people with impaired liver function.
The adverse reactions profile is similar to that of the benzodiazepines: CNS depression, possibility of dependence and withdrawal reactions. In addition, zopiclone can interfere with thyroid hormone balance. It alters taste sensation, causing bitter taste. Use during pregnancy or lactation and in children is not recommended.
Zolpidem
Zolpidem tartrate is another non-benzodiazepine that is more selective in its binding to a subunit of the GABAA receptor than the benzodiazepines; thus it has some sedative properties similar to those of benzodiazepines but lacks the anticonvulsant, muscle-relaxant and antianxiety properties associated with the benzodiazepines. It is approved for short-term treatment of insomnia, and is available as tablets. It has a rapid onset of action, short half-life and no active metabolites so should be taken immediately before retiring. Adverse effects, drug interactions and precautions are similar to those of the benzodiazepines. In addition, zolpidem is likely to cause diarrhoea and myalgia, and has been reported to cause bizarre CNS effects such as hallucinations, amnesia, sleepwalking and inappropriate behaviours, particularly when taken with other psychoactive drugs including alcohol.
Miscellaneous sedatives and hypnotics
Buspirone
Buspirone is not closely related pharmacologically to the other drugs discussed in this chapter. It is an anxiolytic with less sedative effect than the benzodiazepines and little anticonvulsant or muscle-relaxant activity. The exact mechanism of action is unknown, but the drug has a high affinity for and partial agonist activity at 5-hydro xytryptamine1A (5-HT1A, serotonin) receptors and a moderate affinity for brain dopamine D2 receptors in the CNS. It does not affect GABA, nor does it have any significant affinity for the benzodiazepine site on GABA receptors.
Buspirone is indicated for the treatment of anxiety disorders and is considered equivalent in efficacy to the benzodiazepines but usually with less sedation. It appears to have little risk of causing dependence and withdrawal reactions. Common adverse effects are CNS and GI tract disturbances. Due to its affinity for brain dopamine receptors it can cause dopamine-mediated dysfunction, including parkinsonian symptoms and endocrine disturbances; serotonin toxicity can be increased with other serotonergic agents and with grapefruit juice.
Antihistamines
The antihistamines (histamine H1-antagonists) have significant sedative effects as well as being useful in suppressing allergic reactions (see Chapter 47) and as antiemetics. Examples of antihistamines effective as sedatives are doxylamine, promethazine and diphenhydramine. They are readily available over the counter, and antihistamine mixtures are sometimes used as mild sedatives for children. When used as antiemetics to protect children against travel sickness, their sedative effects can be useful (for parents). There are significant hangover effects after antihistamine-induced sedation.
Dexmedetomidine
Dexmedetomidine is a new sedative and analgesic drug, related to the imidazole α2-adrenoceptor agonists such as clonidine and with similar pharmacological properties. It is used specifically by IV infusion for post-surgical and intensive care sedation of intubated patients; continuous infusion duration should not exceed 24 hours. It has cardiovascular and CNS adverse effects, but has little respiratory depressant effect.
Older drugs
Bromides
Bromide salts such as potassium bromide were used in medicine as antiepileptic agents and as sedative–hypnotics from the mid-1850s (see Clinical Interest Box 16-6); the term ‘bromide’ came to have a more general meaning: a conventional idea or trite remark—presumably by extension referring to an idea or remark so boring as to put someone to sleep. Bromide ion is absorbed in the body and replaces chloride (biologically the more common halide ion) in extracellular fluids. Bromide acts in the CNS as a depressant and sedative, and in (not much) larger doses it depresses motor activity and reflexes. At toxic levels it causes ataxia, delirium, coma and death and is particularly toxic as a cumulative poison so it has been replaced by safer drugs.
Clinical interest Box 16-6 Death by bromide and strychnine
Agatha Christie, the well-known English writer of detective fiction, was very knowledgeable about poisons and worked in a Red Cross hospital dispensary during both World War I and World War II. The plot of her first detective novel, The Mysterious Affair at Styles (1920), depends on some interesting toxicological and pharmaceutical information. (People wishing to read the story without knowing the ending are advised to stop here.)
An elderly wealthy woman, suffering insomnia, was prescribed bromide powders to help her sleep.
She also took a daily dose of a ‘tonic’ containing strychnine—low doses of strychnine used to be included in tonics partly because it is a CNS stimulant and because it tastes so bad that it should obviously do the patient some good.
The conspirators dropped a few bromide powders into the large, full bottle of tonic mixture. Because strychnine hydrochloride is incompatible with bromides, the strychnine precipitated as an insoluble bromide and settled to the bottom of the bottle.
The plotters then neglected to shake the bottle when they gave the old woman her dose of tonic, until the last dose contained virtually all the strychnine from the bottle.
This last dose was poured into the woman’s evening cup of coffee, which was sufficiently bitter to mask the taste of the strychnine, so she drank a lethal dose of strychnine (and probably of bromide too) and died from CNS stimulation, convulsions and paralysis of the respiratory muscles causing respiratory arrest.
Of course, to confuse the reader, there were several possible suspects, all of whom had enough medi cal/pharmaceutical knowledge to realise that ‘addition of a bromide to a mixture containing strychnine would cause the precipitation of the latter’, as pointed out by the detective Hercule Poirot in the denouement of the story.
The plot is certainly feasible from a pharmacological viewpoint: Strychnine Mixture (present in the British National Formulary as late as 1963) contained about 6.24 mg strychnine hydrochloride per 30 mL dose. A large bottle (say 500 mL) would contain more than 100 mg strychnine, a fatal dose.
Chloral hydrate
Chloral hydrate is a simple chemical substance (trichloroethanediol) related structurally to both chloroform and ethanol (see Figure 16-4). It is essentially a ‘prodrug’ that is converted in the body to active trichloroethanol, which has a rapid, powerful hypnotic action. Its exact mechanism of action is unknown. It has a general CNS depressant effect similar to that of alcohol.
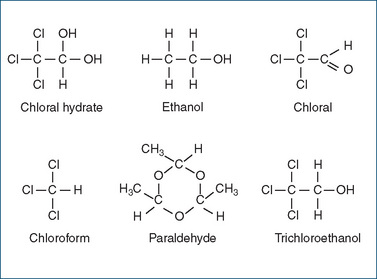
Figure 16-4 Chemical structures of some simple sedative drugs, showing close structural relationships between the sedative chloral hydrate, anaesthetic chloroform, depressant ethanol (alcohol) and sedative paraldehyde, which can be visualised as three molecules of ethanol joined in a cyclical ether formation. Most of these drugs are rarely used medically nowadays.
Chloral hydrate was formerly frequently used as a sedative and hypnotic and as premedication, particularly in children and the elderly, as both oral and rectal forms are rapidly absorbed. It was considered relatively safe but can be toxic in overdose, especially in combination with alcohol (see Clinical Interest Box 16-7), causing cardiac and respiratory failure; deaths have occurred with the use of this drug. It is still sometimes used as a mild hypnotic or preoperative sedative, particularly in children’s hospitals to sedate children for diagnostic procedures and in intensive care units so that catheters are not pulled out; continuous monitoring is required. A mixture form is available, containing 100 mg/mL sweetened with sucrose and saccharin.
Clinical interest Box 16-7 The ‘mickey finn’
The combination of chloral or chloral hydrate with alcohol is very potent and potentially toxic. This mixture, used with criminal intent and known as a Mickey Finn, or knock-out drops, is particularly dangerous because, not only are the CNS-depressant effects additive, but trichloroethanol also inhibits the metabolism of alcohol and prolongs its actions.
The drink is thought to have been named after Michael ‘Mickey’ Finn, who managed the Lone Star Saloon in Chicago from 1896 to 1903 and was accused of using knockout drops to incapacitate and rob some of his customers.
Paraldehyde
Paraldehyde is a polymer of acetaldehyde (see Figure 16-4); it is a colourless liquid with a strong odour and taste. The CNS-depressant effects of paraldehyde are similar to those of alcohol, barbiturates and chloral hydrate; it depresses various levels of the CNS including the ascending reticular
activating system. Paraldehyde is indicated for intramuscular administration as an anticonvulsant in status epilepticus and convulsive episodes arising from tetanus and from poisoning with convulsant drugs. Like alcohol, it is metabolised in the liver to acetaldehyde. Paraldehyde was used in the past as a sedative–hypnotic agent but has been superseded by safer and more effective drugs.
Complementary and alternative sedatives
Many natural products and techniques from complementary and alternative medicine (CAM) have been used to attain sleep or relieve stress and anxiety (see Clinical Interest Box 16-8).
Clinical interest Box 16-8 Complementary and alternative sedatives
For treating insomnia, the natural products valerian, kava kava, lavender, lemon balm, passionflower and L-tryptophan have been shown to be clinically effective. Melatonin, the natural hormone from the pineal gland, appears to reset the body’s circadian rhythm clocks and is used by many people to help overcome jet lag or adapt to altered shift-work hours (Clinical Interest Box 3-3). However, clinical evidence for effectiveness and mechanism is sparse. Other techniques that still require evidence of effectiveness include acu puncture and cranial electrostimulation.
CAM techniques used to alleviate stress include relaxation techniques (yoga, Qi Gong, exercise and meditation), lowenergy electromagnetic fields applied to the oral mucosa and dance classes; evidence of clinical effectiveness is hard to validate because of the difficulties of conducting double-blind controlled studies.
In the treatment of anxiety, music therapy, massage, acupuncture and the Chinese herb suanzaorentang have been shown to be effective. Yoga, meditation, homeopathic remedies and ‘electrosleep’ have shown little efficacy.


 Key points
Key points
 Sleep disturbances and insomnia cause many physiological dysfunctions. They are common, particularly in elderly persons.
Sleep disturbances and insomnia cause many physiological dysfunctions. They are common, particularly in elderly persons. Benzodiazepines such as diazepam are the most common drugs used to treat anxiety and insomnia; they act by facilitation of GABA-mediated CNS inhibitory pathways to cause sedation and muscle relaxation, and relieve anxiety and convulsions.
Benzodiazepines such as diazepam are the most common drugs used to treat anxiety and insomnia; they act by facilitation of GABA-mediated CNS inhibitory pathways to cause sedation and muscle relaxation, and relieve anxiety and convulsions. Because of their safety and effectiveness and the variety of conditions in which benzodiazepines are effective, they have largely replaced the barbiturates, chloral hydrate and other earlier sedatives.
Because of their safety and effectiveness and the variety of conditions in which benzodiazepines are effective, they have largely replaced the barbiturates, chloral hydrate and other earlier sedatives. Pharmacokinetic properties of benzodiazepines vary widely: half-lives range from 2 to 60 hours and many benzodiazepines are converted to pharmacologically active metabolites that prolong the sedative effects. Short-acting agents are used to induce anaesthesia or sleep and longeracting agents to treat anxiety or epilepsy.
Pharmacokinetic properties of benzodiazepines vary widely: half-lives range from 2 to 60 hours and many benzodiazepines are converted to pharmacologically active metabolites that prolong the sedative effects. Short-acting agents are used to induce anaesthesia or sleep and longeracting agents to treat anxiety or epilepsy. Common adverse reactions include excessive CNS depression, tolerance and dependence. Drug interactions frequently occur with other CNS depressants and with drugs that affect the metabolism of benzodiazepines.
Common adverse reactions include excessive CNS depression, tolerance and dependence. Drug interactions frequently occur with other CNS depressants and with drugs that affect the metabolism of benzodiazepines. Newer related agents are zolpidem and zopiclone; buspirone acts by different mechanisms and is less sedating.
Newer related agents are zolpidem and zopiclone; buspirone acts by different mechanisms and is less sedating. As geriatric patients are more s ensitive to these agents than the younger adult and are at risk of accumulation of active drug and of falls, non-pharmacological approaches are recommended to treat their sleep disturbances.
As geriatric patients are more s ensitive to these agents than the younger adult and are at risk of accumulation of active drug and of falls, non-pharmacological approaches are recommended to treat their sleep disturbances. Both paediatric and geriatric persons are at risk of paradoxical-type reactions (CNS stimulation rather than depression) from sedative drugs. It is recommended that prescriptions for these agents be limited in these groups, with close patient monitoring.
Both paediatric and geriatric persons are at risk of paradoxical-type reactions (CNS stimulation rather than depression) from sedative drugs. It is recommended that prescriptions for these agents be limited in these groups, with close patient monitoring.Review exercises
References and further reading
Anonymous. New drugs: melatonin. Australian Prescriber. 2010;33(2):54.
Austin D., Blashki G., Barton D., Klein B. Managing panic disorder in general practice. Australian Family Physician. 2005;34(7):563-571.
Australian Medicines Handbook 2010. Adelaide: AMH, 2010.
Beare P.B., Myers J.L. Adult Health Nursing, 3rd edn. St Louis: Mosby; 1998.
Braun L., Cohen M. Herbs and Natural Supplements: An Evidence-Based Guide, 2nd edn. Sydney: Elsevier Mosby; 2007.
Cumming R.G. Epidemiology of medication-related falls and fractures in the elderly. Drugs and Aging. 1998;12:43-53.
Da Settimo F., Taliani S., Trincavelli M.L., Montali M., Martini C. GABA A/Bz receptor subtypes as targets for selective drugs. Current Medicinal Chemistry. 2007;14(25):2680-2701.
Hanlon J.T., Boudreau R.M., Roumani Y.F., et al. Number and dosage of central nervous system medications on recurrent falls in community elders: the health, aging and body composition study. Journals of Gerontology A, Medical Sciences. 2009;64A(4):492-498.
Harrison N.L. Mechanisms of sleep induction by GABA(A) receptor agonists. Journal of Clinical Psychiatry. 2006;68(Suppl 5):6-12.
Kaplan E.M., DuPont R.L. Benzodiazepines and anxiety disorders: a review for the practicing physician. Current Medical Research and Opinion. 2005;21(6):941-950.
National Prescribing Service. Addressing hypnotic medicines use in primary care. NPS News 67, 2010.
Olson L.G. Hypnotic hazards: adverse effects of zolpidem and other z-drugs. Australian Prescriber. 2008;31(6):146-149.
Psychotropic Expert Group. Therapeutic Guidelines: Psychotropics, version 6. Melbourne: Therapeutic Guidelines Limited; 2008.
Roy-Byrne P.P. The GABA–benzodiazepine receptor complex: structure, function and role in anxiety. Journal of Clinical Psychiatry. 2005;66(Suppl 2):14-20.
Spencer J.W., Jacobs J.J. Complementary/Alternative Medicine: An Evidence-Based Approach. St Louis: Mosby; 1999.
Stahl S.M. Essential Psychopharmacology: Neuroscientific Basis and Practical Applications, 2nd edn. Cambridge: Cambridge University Press; 2000. [ch 8]
Tiller J.W.G. The management of insomnia: an update. Australian Prescriber. 2003;26(4):78-81.
Wright R.M., Roumani Y.F., Boudreau R., et al. Effect of central nervous system medication use on decline in cognition in community-dwelling older adults: findings from the health, aging and body composition study. Journal American Geriatric Society. 2009;57(2):243-250.
New Zealand Medicines and Medical Devices Safety Authority: www.medsafe.govt.nz
More weblinks at: http://evolve.elsevier.com/AU/Bryant/pharmacology/