Management of lumbar spine disorders
Introduction
Low back pain is characterized by pain and discomfort localized below the costal margin and above the inferior gluteal fold, with or without leg pain (Burton et al. 2009). Low back pain is a part of everyday life in Western industrialized countries and will affect 80% of all adults in their lifetime (Nachemson & Jonsonn 2000). Acute low back pain normally settles within 4–6 weeks, but the majority of people often will experience recurrence at some time or other (Burton et al. 2009). In a small percentage of cases pain becomes persistent and impacts significantly on healthy living and health care costs (Burton et al. 2009).
Although the latter may seem a relatively small percentage, the prevalence of chronic disability due to (non-specific) low back pain (NSLBP) increased significantly in Western industrialized countries in the last two decades of the 20th century. This has led to a discussion on the basic assumptions and paradigms regarding causes of the pain and disability, treatment and research involved (Borkan et al.1998, Waddell 2004) and to the development of programmes to the secondary prevention of chronic disability due to low back pain.
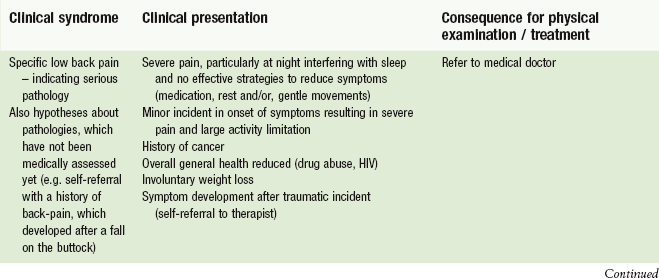
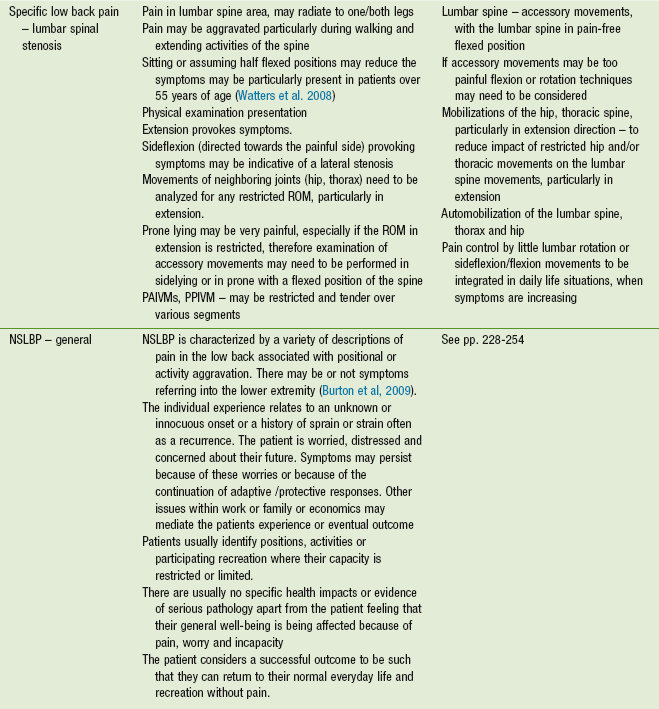
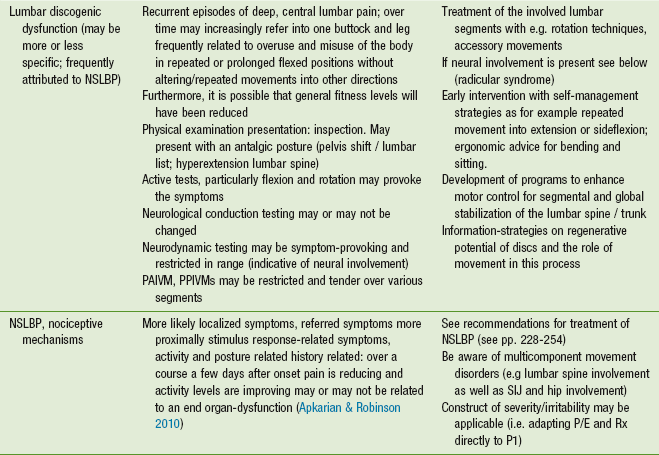
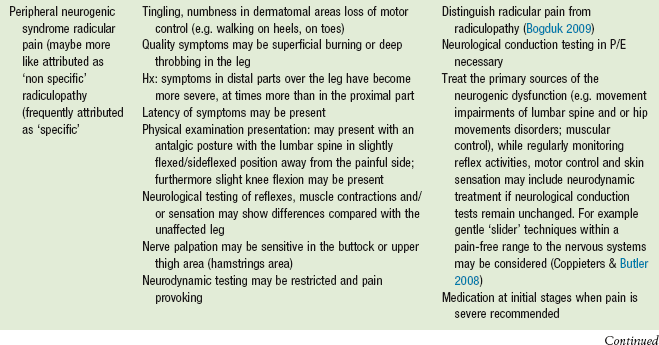
If serious pathologies, such as cancer, fractures, visceral pathologies, systemic inflammation, infection or severe neurological deficits can be ruled out as a source of the pain, it has been suggested NSLBP should be de-medicalized and patients' complaints should be grouped according to symptoms into four categories (see Table 6.1; International Paris Task Force on Back Pain: Abenhaim et al. 2000).
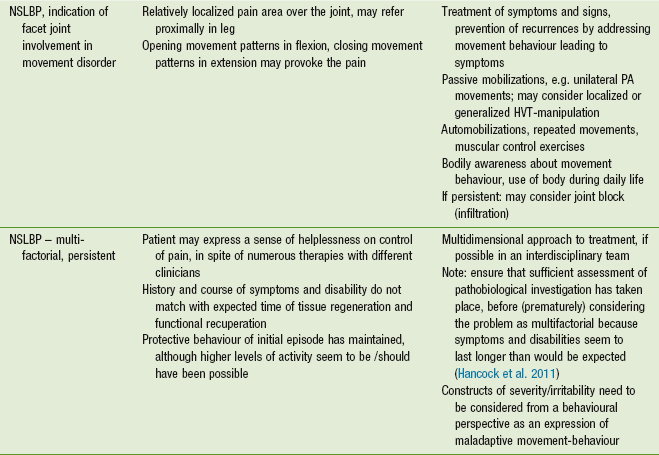
Table 6.1
Abenhaim et al. (2000) defined four categories of non-specific low back pain based on patients' complaints. Recommendations have been given for the treatment of the different categories
Several guidelines have been developed over the years (Airaksinen et al. 2004, Van Tulder et al. 2006, Vleeming et al. 2008), in which it has been recommended to stay as active as possible and to reduce rest or bed rest to a minimum (Abenhaim et al. 2000). The role of physiotherapeutic care has been discussed in relatively broad terms, but without detailed description and recommendation of the kind of passive movements and exercises in acute, subacute and chronic phases of NLSBP. Nevertheless, the Paris Task Force on Low Back Pain suggests in subacute intermittent and recurrent low back pain to encourage patients to follow an active exercise programme, as well as in chronic low back pain to perform physical, therapeutic or recreational exercises (Abenhaim et al. 2000). Furthermore, the Paris Task Force concludes that scientific evidence exists in favour of strength training, stretching and fitness, which must be based on a medical assessment by a competent professional and on the patient's compliance to the prescribed course of action (Abenhaim et al. 2000, p.3S).
Demedicalization and conceptualization of NSLBP
Sheehan (2010), among others, recognized the need to de-medicalize low back pain and emphasized the need for such a condition to be managed in the community rather than hospitals. Waddell (2004) recognized the inadequacies of a back pain revolution driven by the biomedical model of diagnosis and treatment. Waddell also made the medical communities aware of the consequences of medicalization of low back pain and its psycho-socioeconomic impact on Western industrialized populations. He suggested following a bio-psychosocial paradigm in the management of low back pain disorders (Waddell 1987). Chronic NSLBP is associated with a combination of physical, cognitive, social, behavioural, life style and neurophysiological factors. The latter with changes in processes of the peripheral and central nervous system. Taken these factors together, they have the potential to maladaptive cognitive behaviours (as fear avoidance, catastrophizing, unfavourable beliefs), pain behaviours (as communication and avoidance), and movement behaviours, leading to a vicious circle of ongoing pain sensitization and disability (O'Sullivan 2011).
Burton et al. (2009) recommended that the focus of prevention and management of NSLBP is directed towards physical activity and education. National strategies on prevention and management of low back pain have also placed conservative measures at the forefront of policy (Briggs & Buchbinder 2009, NICE 2009). Briggs & Buchbinder (2009) also recognized that the most important aspect of low back pain lays in its consequences rather than in the mere the fact that it exists. NICE (2009) highlights the need for individualized, patient-centred, needs-based management of NSLBP.
Policy makers therefore need to re-think what de-medicalization means to health care professions, to individual people, to populations, particularly in Western industrialized countries and to societies as a whole. Furthermore, it seems necessary to analyze those factors contributing to NSLBP and disability and conceptualize them in subgroups for treatment and better-aimed research efforts (Kent et al. 2009a).
One may learn from history how to approach such a dilemma in relation to health care, healthy living, promotion of healthy life expectancy as well as the financial and governmental consequences of low back pain in society. Low back pain was formally known as ‘lumbago’ or ‘muscular rheumatism’ (Gowers 1904). In the modern era lumbago is being used as a partner term for low back pain on many health care web pages. The term lumbago is a term which may suit de-medicalization well. It is non-threatening and places the condition in its true context of non-specificity. Compare this with terms like ‘slipped disc’, ‘degenerating vertebrae’, ‘trapped nerve’ etc., which are all terms used specifically for a non-specific condition. The consequences of the term lumbago are also less impacting on the individual. Moseley (2004) demonstrates a strong association between a sense of threat (e.g. knowledge that you have been told you have a crumbling disc) and pain perceptions. The road to de-medicalization is, therefore, in the terminology used. Lumbago seems to be fashionable again as a means of explaining pain experienced between the costal margins and the inferior gluteal folds.
The best way to treat low back pain, as reported by the HEN (Health Evidence Network) associated with WHO/Europe (2000), is:
… by staying active, returning to work, and exercising at an appropriate and increasing intensity. Anti-inflammatory and muscle relaxant drugs offer effective pain relief.
(WHO/Europe 2000, p. 1)
Back pain and its consequences are not isolated physical problems, but are associated with social, psychological, and workplace-related factors such as stress, worry, and anxiety; effective prevention and treatment must take these into account. Dealing with this situation can play a decisive role in preventing the development of chronic back pain.
(WHO/Europe 2000, p. 1)
A shift in culture about low back pain therefore needs to continue to evolve. This shift should move away from a reductionist, biomedical model, in which numerous interventionist pathways as medications, radiological examinations, injections and surgical interventions, may heighten patients' expectations and demands, ultimately leading to a dependency upon all different interventions. The alternative model should be based upon the viewpoint that low back pain is a problem of painful movements and movement-sensitivity, even though structural changes and some pathology may be present. In this model it is essential to consider the following aspects:
• Support recovery from injury or strain
• Gradually expose or reintroduce the structures and the patient to loading
• Condition the lumbar spine and associated structures
• Gradually condition to recover capacity and performance
• Use movement as a painkiller-evidence
• Use passive movement to support tissue and cellular function, as well as to introduce sensomotor learning processes towards active movement
• Creating independency and self-advocacy rather that creating dependency.
Policy makers also need to recognize which health care professions are best placed to lead on design of individual exercises and activity programmes and the delivery of non-threatening, de-medicalized information about lumbago and its potential consequences. As stated in an Australia based study, it seems that professions linked to manual therapy more likely connect subgroups of NSLBP to different treatment needs than primary care medical practitioners (Kent et al. 2009b). Health care professions such as physiotherapy are now mature enough to lead on policy supported by medical needs such as prescription medication and diagnostic imaging (rather than the other way round). Physiotherapists are best placed to ensure that individuals who experience lumbago move quickly from health care support back into healthy living. In effect, lumbago has become a public health issue rather than a medical issue.
The route to de-medicalization of NSLBP, therefore, is:
• Health care led supported by medical practitioners, who are skilled in guiding patients towards an active life style
• Early transition from health care needs to healthy living
• An emphasis on management to restore physical capacity and performance with less emphasis on biomedical diagnosis, medication and diagnostic imaging
• Embed the management of low back pain within the public health domain rather than the domain of health services
• Non-specific classification as, for example, using the term lumbago as well as the development of research classifications related to movement capacity and performance to guide research endeavours.
Conceptualization
As discussed in the previous paragraph, it seems necessary to define de-medicalization of NSLBP in greater depth. As a consequence, the conceptualization of the factors contributing to the development and maintenance of NSLBP, including its clinical assessment and treatment, should be investigated. This should be discussed in systematic studies and clinical practice. Also it appears that decisions on a political level are necessary whereby health care professions should play a pivotal role in the prevention and treatment of NSLBP and associated disability.
Some studies have been designed around the question of how clinicians perceive the nature of NSLBP.
Kent et al. (2009a) concluded, based on questionnaire information from 544 attendees at major conferences on low back pain in Europe and Australia, that consensus between different groups of clinicians existed on the following points:
• NSLBP is more likely to be an expression of numerous conditions rather than one single condition. This has implications for systematic studies. Currently many studies include heterogeneous cohorts of persons with NSLBP. Therefore, external validity of the studies suffer and will lead to only limited generalizability to clinical practice.
• Most respondents preferred to sub group NSLBP on the basis of a cluster of symptoms and signs rather than based on patho-anatomic changes.
• Pain, physical impairment (range of movement [ROM], muscle strength), activity (ability to perform activities of daily living e.g. sitting, walking standing, lifting), participation (abilities to perform social roles such as in work, family, hobbies, social contacts) and psychosocial function (e.g. depression, anxiety, coping, fear avoidance beliefs) were considered essential aspects of clinical assessment of the patients concerned and needing different, individualized approaches to treatment.
Furthermore in another Australia based study, it appears that primary clinicians such as manual therapists, chiropractors and osteopaths often link the subgroups to different treatment needs more than to medical practitioners (Kent et al. 2004).
Clinical assessment
The clinical assessment of persons with low back and/or leg pain should encompass various aspects of clinical analysis regarding pathobiological processes, movement analysis and contributing psychosocial factors. Furthermore, the clinician needs to incorporate different paradigms or perspectives in their clinical reasoning processes in order to be able to develop a comprehensive, meaningful, individualized treatment programme for the patient.
If a person presents with low back and/or leg pain, the clinician should consider all of the following points:
• The presenting dysfunction, referring to nociceptive pain mechanisms, which are in direct relationship to patho-anatomical and pathophysiological dysfunctions in bodily tissues (‘endorgan-dysfunction’, Apkarian & Robinson 2010).
• Within this perspective, the clinician is evaluating whether serious pathologies such as cancer, fractures, visceral pathologies, systemic inflammation, infection or severe neurological deficits may be present, which require specialized medical care. If serious pathologies can be ruled out, possible tissue processes may need to be considered as a precaution to (physiotherapeutic) treatment. Additionally, in the absence of contra-indications and precautions to physiotherapeutic treatment, the physiotherapist may have certain structures in mind, which may be contributing to the clinical pattern of the movement disorder of the patient, while considering treatment options (e.g. it may be possible in the treatment of a movement disorder of a person, that physiotherapists select, next to other techniques, rotation of the lumbar spine as a first treatment technique, because of the recognition of a movement disorder based on a discogenic dysfunction).
• If serious pathologies can be ruled out, the central core of clinical assessment should be the analysis of the movement disorder, the movement capacity and the movement potential of the patient (Cott et al. 1995; see also Chapters 1 and 2 of volume 2).
• The movement diagnosis may be expressed in the terms of levels of functioning as described in the International Classification of Functioning, Disabilities and Health (ICF; WHO 2001). Information on the movement capacity and restrictions may be found mainly during the subjective examination and observation of these, while the more specific physical examination procedures will inform the NMS-physiotherapist about the level of local movement (dys)functions (impairments).
• Information regarding movement capacities on the levels of function, activity and participation serves as a basis for the collaborative definition of treatment goals with the patient. Pathobiological processes may define precautions to the therapeutic objectives, while psychosocial aspects of the individual illness experience may be decisive in the treatment priorities and the integration of other therapeutic measures as for example patient education and the development of coping strategies as a means of patient-empowerment (Fig. 6.1).
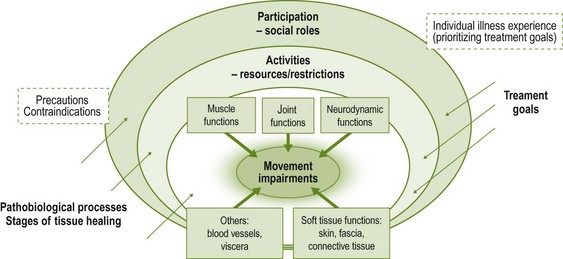
Figure 6.1 The analysis of movement dysfunctions should incorporate the current movement capacities of a person on function, activity and participation levels as described in the International Classification of Functioning, Disabilities and Health (ICF, WHO 2001). Adapted from Hengeveld (1999) with permission.
• Although numerous practice guidelines recommend the assessment of functional activity levels and psychosocial contributing factors, it appears that between various primary care professions considerable difference is present in the utilization of assessment tools and in the focus on activity levels. In a study between physiotherapists, manipulative physiotherapists, osteopaths, chiropractors, general medicine and musculoskeletal medicine it was shown that the assessment of pain and physical impairment, as for example ROM, was a more common denominator between professional disciplines, while activity limitations and psychosocial function were less commonly assessed, with marked differences between groups. It has been recommended to standardize procedures, including the assessment of activity levels and psychosocial factors, as this information may be prognostically important and useful for outcome assessment. Furthermore the information from activity levels and psychosocial factors should aid in the identification of subgroups, requiring different treatment (Kent et al. 2009b)
• In order to enhance standardization in assessment, the International Paris Task Force on Back Pain summarized criteria to assess and decide upon meaningful therapeutic goals regarding optimal mobility and optimal performance of activities of daily living. They are based on selected functional and quality of life indexes, such as The Nottingham Health profile, Health Assessment Questionnaire, Sickness Impact Profile, SF-36, Roland Morris Questionnaire, Oswestry, Quebec Back Pain Disability scale (Quebec Task Force on Spinal Disorders, 1987), Dallas Pain Questionnaire (Abenhaim et al. 2000).
• Criteria for optimal mobility:
 able to walk for several hours or several kilometres
able to walk for several hours or several kilometres
 capable of remaining seated for several hours; however, within a lifestyle where sitting is interrupted regularly and preferably where sitting does not occur for the majority of the day
capable of remaining seated for several hours; however, within a lifestyle where sitting is interrupted regularly and preferably where sitting does not occur for the majority of the day
 able to remain standing for more than 1 hour
able to remain standing for more than 1 hour
 not having to go to bed or lie down to rest; not having to get out of, or turn over in, bed because of pain
not having to go to bed or lie down to rest; not having to get out of, or turn over in, bed because of pain
 capable of climbing several flights of stairs
capable of climbing several flights of stairs
 able to go down stairs frequently
able to go down stairs frequently
 able to travel for over 2 hours; able to open a car door; get in and out of cars.
able to travel for over 2 hours; able to open a car door; get in and out of cars.
• The criteria of optimal performance of activities of daily living are listed as follows (Abenhaim et al. 2000):
 lean forward without difficulty; lean over a sink for 10 minutes
lean forward without difficulty; lean over a sink for 10 minutes
 bend over, kneel and crouch without difficulty; pick up objects from the ground without support
bend over, kneel and crouch without difficulty; pick up objects from the ground without support
 get dressed and undressed, putting on socks/stockings and shoes without difficulty
get dressed and undressed, putting on socks/stockings and shoes without difficulty
 wash oneself completely without difficulty, wash one's hair, brush one's teeth, get in and out of the bath tub
wash oneself completely without difficulty, wash one's hair, brush one's teeth, get in and out of the bath tub
 run errands without difficulty; pick up bags weighing at least 2 kg without difficulty
run errands without difficulty; pick up bags weighing at least 2 kg without difficulty
 do housework without difficulty or resting, do the laundry, vacuum, move tables, make the bed, bend over to clean the bathtub, not avoiding heavy housework
do housework without difficulty or resting, do the laundry, vacuum, move tables, make the bed, bend over to clean the bathtub, not avoiding heavy housework
 stretch out one's arm to lift heavy or light objects located on the ground or above one's head; reaching a high shelf; carrying a large valise.
stretch out one's arm to lift heavy or light objects located on the ground or above one's head; reaching a high shelf; carrying a large valise.
Individualized assessment of persons with low back pain may encompass more activities than the ones listed above; however, it seems appropriate to include questions and observations about these activities in clinical examination procedures.
• Contributing psychosocial factors. Numerous psychosocial factors (‘yellow flags’) that hinder or enhance complete recovery to full function have been described over the past few decades (Kendall et al. 1997, Watson & Kendall 2000, Waddell 2004). Those hindering recovery have been described in an acronym ‘ABCDEFW’, which does not indicate a ranking in relative importance (Kendall et al. 1997). This list of yellow flags is quite extensive, but in relation to the physiotherapeutic treatment of movement disorders and pain the following psychosocial factors may be conclusive:
 ‘beliefs and expectations’ with regard to the causes of the problem, as well as the possible treatment options
‘beliefs and expectations’ with regard to the causes of the problem, as well as the possible treatment options
 confidence in own capabilities to control pain and/or well-being
confidence in own capabilities to control pain and/or well-being
 sense-of-control over own well-being
sense-of-control over own well-being
 movement behaviour during daily life activities, when the pain occurs
movement behaviour during daily life activities, when the pain occurs
 level of activities and participation
level of activities and participation
 reactions of social environment (boss, spouse, colleagues, friends).
reactions of social environment (boss, spouse, colleagues, friends).
A detailed description of these contributing psychosocial factors can be found in Chapter 8.
The assessment of psychosocial risk factors and resources should be an integral part of the assessment of persons with low back pain as they are mostly expressions of normal human illness experiences and may have a considerable effect on short-term and long-term treatment outcomes. Contrary to some guidelines, they should be taken into consideration within the first encounter with the patient. Particularly a sense of helplessness needs to be addressed early in treatment. An individualized programme of self-management strategies, in which the patient experiences a sense of control over the pain and/or well-being, needs to be incorporated in the initial therapeutic sessions.
Treatment/advice to the patient
The Paris Task Force on Low Back Pain suggested that patients' complaints of NSLBP are categorized into four groups (Table 6.1) and should be differentiated into acute, sub-acute or chronic pain (Abenhaim et al. 2000). They recommend the following approach with regards to bed rest, activity and exercises:
• Acute phase of pain (lasting less than 7 days). Bed rest is contraindicated for the groups 1–3. For group 4, bed rest should only be authorized if the pain indicates it. If bed rest is authorized, it should be intermittent rather than continuous. After 3 days of bed rest the patient should be strongly encouraged to resume their activities.
• In sub-acute phases (lasting between 4 and 12 weeks) and in chronic phases, bed rest is not only contraindicated, but should be stopped in patients still resting in bed at this stage.
The task force did not recommend any exercises or functional restoration for the acute phases of NSLBP in the first 7 days, but for sub-acute and chronic phases they found sufficient scientific evidence to recommend patients to follow an active exercise programme.
However, the recommendations to the kind of exercises and movement approaches have been kept in general terms, such as strength training, stretching and fitness, in which no movement concept was found to be more superior to another.
Furthermore no distinction seems to be made if the acute pain is of a recurrent nature or occurring for the first time. Recurrences of acute NSLBP and disability need to be prevented (Burton et al. 2009) and the clinician should evaluate in which circumstances recurrences develop, in order to be able to define an adequate individualized (behavioural-) movement therapy programme aimed at the prevention of such episodes.
It is suggested that low back pain should be treated in the primary care setting, with a focus on a concept of reduced activity, rather than resting, recommending patients to stay as active as possible and to take NSAIDs if necessary for a period of 7–10 days, provided that no special ‘red flags’ indicative of more serious pathology are present (CSAG 1994). In addition, Waddell (2004) suggested examining a patient within 48 hours, treating patients with medication or manipulative therapy and, further, to follow the guidelines of the Clinical Standards Advisory Group (CSAG 1994). However, in a study with audiotaped interviews and questionnaires with 1-month follow-up, Turner et al. (1998) conclude that providers typically addressed medical issues, but did not (or only inconsistently) assess functional limitations related to pain and did not discuss how to resume normal activities, although this was a highly rated goal for most patients. Physicians often did not adequately reassure patients that serious conditions were ruled out, nor did they consistently address worries by the patient. In fact, at times patients felt more insecure about the (self-)management of their problem than before the consultation.
It appears that deliberate measures should be taken by the primary care clinician to provide the patient with a sense of control over the pain. This probably is best obtained within a single session with a specialist of movement rehabilitation and pain management, as for example a physiotherapist specialized in musculoskeletal (MSK) rehabilitation (manipulative physiotherapist).
Referral of patients with acute low back pain
If the pain and disability do not settle as quickly as desired, a second opinion in the primary care setting should be considered. This opinion could be provided by a family doctor with special interest and expertise in back pain or by a physiotherapist, chiropractor or osteopath (Waddell 2004).
If patients, in whom specific pathologies have been ruled out, do not improve and remain off work after 3–6 weeks, they should be referred to rehabilitation services, in which physiotherapy has a key role to play. However, rehabilitation is often only considered after medical treatment is complete or has failed (Waddell 2004). The restoration of movement functions appears to be considered an automatic process, in which patients are expected to resume their normal level of activities and assume their participatory roles in society on their own. Although quite a number of persons with back pain may do so, it is essential to recognize those individuals, who do not resume their normal levels of activity within the expected time of recuperation and to refer them to a physiotherapist.
Only if patients should be investigated and treated for specific pathology should they be referred to specialist services (CSAG 1994). However, Waddell (2004) argues that they should be referred with a clear and explicit goal in mind, being the exclusion of more serious problems, pain control or rehabilitation. The choice of specialist, the facilities they provide and the outcome measures should reflect these goals. As Waddell states: ‘there is no point referring a patient to a surgeon and judging success in surgical terms if what the patient really needs is rehabilitation’ (p. 444).
The Clinical Guidelines for the Management of Acute Low Back Pain (RCGP 1999) summarize the process of diagnostic triage and referral recommendations, as described in Box 6.1.
Scope of practice of physiotherapists regarding NSLBP
With the conceptualization of NSLBP, physiotherapists may need to (re-)consider their scope of practice, both in the emphasis of clinical work and in the development of subgroups of patient classifications needing different approaches of movement therapy.
Pillars of physiotherapy practice
It is essential that physiotherapists remain aware of the overall scope of their profession and the possibilities it offers in treating patients suffering from pain, and to not reduce their work to active exercises aimed at muscle strengthening, stretching or general fitness, just because many reviews have qualified studies of these aspects of human movement therapies as acceptable evidence.
In the UK the scope of practice of physiotherapists is defined by four pillars of practice and the fostering and development of such being massage, exercise and movement, electrotherapy and kindred methods of treatment (Chartered Society of Physiotherapy 2008). As stated in numerous places in this book, there is ample evidence for passive movement, therapeutic touch and physical applications being equivalent to active therapies, and in certain cases it even may be better to start with these treatment forms before embarking on an active movement programme. In relation to low back pain, evidence suggests that the following should be included in the current best practice for the management of NSLBP:
• Staying active and work productive
• Engaging in physical activity and exercise
• Being informed and educated about low back pain in a non-threatening way
• Simple analgesic and NSAID support
• Timely manipulation and acupuncture (NICE 2009).
All these recommendations (apart from prescribing, which is an extended scope practice) fall within the four pillars of practice.
Paradigms
Furthermore, it is important to note that every intervention aimed at anatomical structures or to enhance movement will also influence emotional or other aspects of a person.
In a discussion on paradigms, Coaz (1993) argues that physiotherapists may implicitly be working within a bio-psychosocial paradigm, although their explicit viewpoint may be a biomedical one. He states that the perspective of the average physiotherapist and especially of manual therapists is focused on bones, muscles, connective tissue and sometimes on circulatory problems in which emotional dimensions hardly reach the awareness of the physiotherapist. However, Coaz (1993) argues that physiotherapists:
… have an access to and influence emotional aspects, even when this does not reach the consciousness of the physiotherapist – and neither the consciousness of the patient. (p. 4)
It seems that since this statement numerous studies have dealt with the bio-psychosocial viewpoints on the physiotherapeutic work. However, it is possible, in spite of the increasing number of studies, that physiotherapists still work more implicitly than explicitly within a bio-psychosocial paradigm (Hengeveld 2001). When the bio-psychosocial effects are being reflected and conceptualized, they can be deliberately integrated in treatment rather than being an implicit, intuitive aspect. In fact, it is recommended that physiotherapists develop a phenomenological viewpoint to their work, in which they guide patients from individual illness experience and illness-behaviour towards an individual sense-of-health and health promoting behaviours with regards to movement functions and general well-being (Hengeveld 2001).
International Federation of Orthopaedic Manipulative Physiotherapists' competencies and scope of practice
Physiotherapists also need to be clear therefore about where their role in the management of low back pain begins and ends. Best practice management of low back pain demands that physiotherapists acquire, foster and develop a broad and deep knowledge and skills clinical framework supported by professional, analytical and reflective attributes (IFOMPT 2008).
The physiotherapists' scope of practice for low back pain should encompass the dimensions and competencies detailed by the International Federation of Orthopaedic Physical Therapists (IFOMPT 2008; see Box 6.2). This should be viewed within the specific context of manipulative and movement therapies related to neuromusculoskeletal low back pain.
Treatment objectives
In the development of treatment, the physiotherapist, in collaboration with the patient, should define short-term and long-term treatment goals, which ideally should lead to optimum movement functions, overall well-being and purposeful actions in daily life, in order to allow the patient to participate in their chosen activities of life (in their roles as spouse, family member, friend; in sports, leisure activities and work).
Sense of control: A core objective of treatment should be at all times to support patients to develop a sense of control over their pain, or, if this seemingly cannot be achieved easily, as in chronic pain, a sense-of well-being in spite of the pain. The process of developing a sense-of control, and with this working on the self-efficacy and internalizing of locus of control with regards to pain, may be well expressed in the following quote:
One of the main goals of the infant is to try to gain some control over his or her environment. The attempt to reduce uncertainty and establish control seems to be one of the most fundamental human drives. One of the key aspects of personality is the strength of this drive and the balance between our personal needs for control and the needs of others. These beliefs are probably not innate, but more likely a product of learning and social conditioning …] In rearing children every parent has to find the right balance between affection and nurturing on the one hand, and the imposition of control on the other.[…] Our self-confidence is related in part to the extent to which we have established sufficient control over our environments to meet our needs[…] As a result of this life experience, we all form beliefs about the extent to which we are able to get control of our lives […].
[…] Gaining control over back pain means actually mastering the pain and associated disability. The ability to do this is largely dependent upon the individual's own judgement of their capabilities.
Waddell 1998, p. 196
If patients learn self-management strategies, which they can apply easily in daily life, at initial stages of treatment, the confidence to take on activities that they might have believed to be harmful may be enhanced. Therefore self-management strategies play a central role in the secondary prevention of chronic disability due to low back pain. As this relates to changing movement behaviour, altering movement patterns and thought patterns regarding movement and pain, a cognitive behavioural approach to treatment is essential, in which every action such as communication, education, information and touch are applied in a reflected manner. In this context, Fordyce (1982, 1995) suggests focusing on the question why people develop certain kinds of behaviour, rather than primarily asking which nociceptive processes cause the behaviour. A cognitive behavioural attitude, in which it is acknowledged that behaviour does not change overnight, is important in this process. In the development of these self-management strategies, patients may go through different phases of change (Prochaska & DiClemente 1994) before a desired behaviour may be fully integrated in habitual daily life activities.
It is essential that the strategies are simple enough, that they can be applied or adapted directly to daily life situations and that the patient is guided towards a sense of success
Furthermore, to enhance compliance and a sense of success, it is often useful, to provide patients with the possibilities of (telephone) contact, if any queries or insecurities about the self-management strategies would come up, particularly in those cases of an acute phase of (nociceptive) NSLBP, in which a patient is only seen a single time (see also Chapter 8).
Physiotherapists with their specific professional expertise have numerous possibilities to guide patients towards a sense-of-control over their pain or well-being, as for example:
• Repeated movements, often in contrasting direction to the habitual movement patterns (McKenzie 1981)
• Automobilizations, stretching exercises
• Muscle recruitment exercises
• Pacing strategies in which active and relaxing cycles in daily life follow each other
• Body awareness, including the awareness of thoughts, emotions and behaviours on bodily reactions and pain
Optimizing movement capacity: Another important goal of treatment is the optimization of the movement capacity of a person. In order to motivate patients towards the normalization and optimization of movement functions and activity, a process of collaborative goal-setting is essential (see Chapter 3). Within this process it is important to recognize the possible barriers to the restoration of full function and to address them in treatment by implementing self-management strategies, educational interventions about neurophysiological pain mechanisms, the role of movement in pain or stress-physiology in an early phase of treatment. Furthermore, also in this phase of treatment, a cognitive-behavioural approach to physiotherapeutic treatment is essential to enhance continuous and profound changes with the patients concerned.
In order to provide a meaningful rehabilitation towards full activity, the subjective and examination procedures should be directed towards questions about restrictions and possibilities of activities and to the establishment of the conditions required to achieve optimum activity levels. The core sets of ICF (Box 6.3; WHO 2001) may be more comprehensive than the activities as outlined by the Paris Task Force on Low Back Pain (Abenhaim et al. 2000). They may aid in the definition of collaborative outcomes and the fostering and development of a public health framework within the physiotherapist's scope of practice.
Psychosocial aspects in treatment: As stated before, treatment will always have psychosocial effects, in one form or another. They may be a part of the implicit, intuitive process; however, there are clinical situations in which a deliberate multidimensional approach to treatment should be taken. In this approach, goals on cognitive, affective and behavioural levels should be defined explicitly next to objectives on the enhancement of movement behaviour and movement capacity. It seems that these factors are first considered when a pain problem has become chronic. However, it may be of use to consider these factors immediately in a first consultation of acute NSLBP, or when a patient is seen for a second session after approximately 7–10 days.
Vlaeyen & Crombez (1999) postulated that a pain experience may change over time. Within 2–4 weeks after an acute nociceptive situation cognitive and affective factors, for example anxiety, helplessness, different cognitions about causes of the problem, and treatment options for the pain, may become important contributing factors in the maintenance of pain, disability and distress. Therefore any concerns a person has because of the pain need to be addressed in the first consultation and creating a climate in which the patient feels they can ask questions or seek advice, even between treatment sessions, may become central in the process of secondary prevention of chronic pain.
It has been recognized that physiotherapists are aware of the need for a more multidimensional approach to treatment – at the latest in the fourth treatment session, once they notice that the patient's reduction of pain and improvement of activity levels have not improved as expected in the prognosis at the first consultation. In fact, discrepancies between pain, disability and the expected time of functional restoration with regard to physiological tissue regeneration appear to be core factors in the determination of a need for a more multidimensional approach to treatment (Hengeveld 2001).
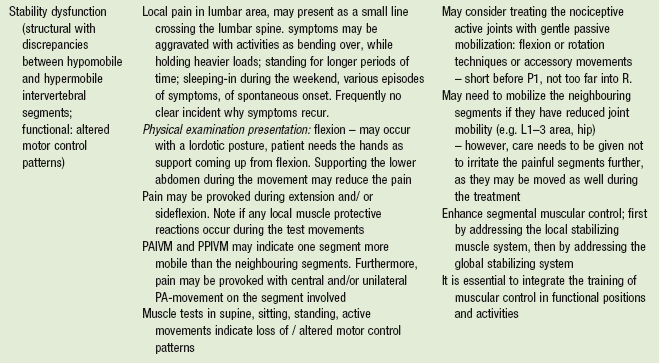
Phases of NSLBP and physiotherapeutic treatment: Maher et al. (1999) suggested physiotherapeutic treatment objectives, which are described in Table 6.2. However, it needs to be noted that defining sub-acute and chronic phases only based on the course of time may be problematic. It is important to know which kind of treatment the patient has received so far. Pain may be persisting because of interventions, which have not been thoroughly reassessed, hence they have not been perceived by the patient as being effective. Some patients may not have had any treatment at all for their problem. Also, generalized exercises, without specific self-management strategies to control pain, may be not effective enough. Furthermore, in some neurogenic pain states, severe pain may last much longer than a more simple nociceptive process. History taking, including exact information on the treatment so far, their immediate effects and a detailed analysis of the self-management strategies (which ones? when are they performed? can they be integrated in daily life? and what are the immediate effects on the pain/well-being?) should be the basis of every physiotherapeutic treatment programme, regardless of the phase in time of the symptoms and signs.
Table 6.2
Physiotherapeutic activities recommended for the different phases of NSLBP based on an extensive literature review (Maher et al.1999)
*Additional note from the authors of this chapter.
Classifications, subgroups and models: Current best evidence confirms the beneficial effects of movement in the treatment of NSLBP; however, several studies show that no active therapy seems more superior than another. It would be oversimplified to conclude that ‘it would not matter what is done’; it appears more likely that different treatment approaches, as for example motor control exercises and graded activity, have similar effects (Macedo et al. 2012). It seems that the quality of, and the therapeutic climate in which, the exercises are implemented is important and that better results are being observed in individualized, supervised exercise programmes (Hayden et al. 2005, O'Sullivan 2011).
In spite of results in favour of individualized, supervised exercises in which therapists may follow their personal preferences, numerous questions should be answered in studies in which a better subgrouping of patients out of the heterogeneous group of NSLBP is undertaken.
Questions that may need to be pursued deeper in systematic study with well-defined subgrouping of the included subjects are:
• Which kind of patients react better to individualized, supervised treatment in contrast to group treatment?
• Is it possible that patients with a clear motor deficit respond better to motor control programmes, while persons with higher fear avoidance behaviour and lower fitness levels may react better to a graded activity approach? (Macedo et al. 2012)
• Which group of patients reacts better to spinal manipulative therapy in combination with a certain kind of exercises, or which groups need an approach with repeated movement and which groups would respond more to general bodily awareness and relaxation?
• Which groups of patients may need to be considered more from a perspective of changes in the brain, based on cortical reorganization and degeneration rather than singled out in subgroups of bio-psychosocial diagnosis and treatment (Wand & O'Connell 2008). Additionally, with a more complex question into clinicians' attitudes and models: which groups would respond best to an approach in which clinicians apply treatments as usual, but from the perspective of supraspinal (re)learning and reorganization?
Primary research and evaluation of best practice informs physiotherapists about the meaningfulness of their manual examination and intervention methods for low back pain (O'Sullivan 2005, Kamper et al. 2010, Flynn et al. 2002, Smart et al. 2012, Schafer et al. 2011, Slater et al. 2012).Therefore, if treatment based sub-groups could be reliably identified, it would represent an important advance in low back pain treatment and the pursuit of this goal has been identified as a priority for low back pain researchers (Kamper et al. 2010).
The necessity to define subgroups for scientific inquiry and decision-making regarding treatment of low back pain has been increasingly acknowledged in the past two decades. However, Billis et al. (2007) described in a cross-country review in nine countries, that most studies were classified according to patho-anatomic and/or clinical features. Only a few studies utilized a psychosocial and bio-psychosocial approach. They concluded that no internationally established, effective, reliable and valid classification system is available, which incorporates the different subgroups for the definition of valid inclusion-criteria and statistical analysis. McCarthy et al. (2004), based on a literature review with 32 studies, suggest developing an integrated system, which allows for the assessment of NSLBP from biomedical, psychological and social constructs. This viewpoint is shared by Ford and Hahne (2012), who argue that researchers in low back pain need to incorporate both pathobiological and psychosocial perspectives, without emphasizing one model and neglecting the other. Furthermore, they recommend researchers to follow the clinical reasoning of clinician physiotherapists and to develop subgroups, which reflect daily clinical decision-making processes.
Also, various physiotherapists have suggested the development of subgroups based on movement-preferences of patients, with consequences for the selection of active movement therapies based on repeated movements (McKenzie 1981) and motor control exercises (Maluf et al. 2000).
In spite of missing international uniformity, numerous studies have been performed in which different subgroups have been established and which demonstrate the effectiveness of different physiotherapeutic approaches:
In particular, research has investigated sub-groups of patients who are more likely to respond to manual therapy or neural mobilization. The role of motor control strategies based on well developed knowledge have also been shown to influence back pain in many groups of patients (Hodges 2011, Dankaerts & O'Sullivan 2011, Hides et al. 2010, Macedo et al. 2009).
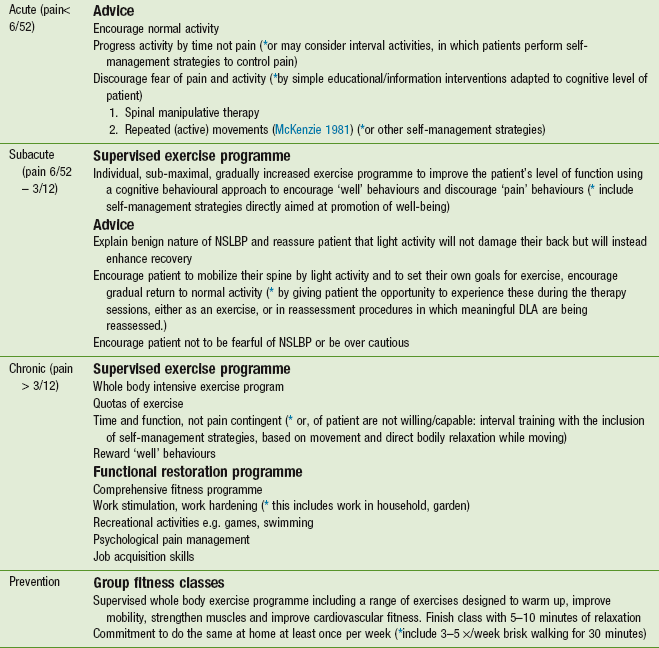
O'Sullivan (2005) has proposed a sub-classification of chronic NSLBP which identifies dysfunction at an impairment level. O'Sullivan is of the opinion that a range of models (Table 6.3), which identify the reasons for chronic low back pain, are needed within a bio-psychosocial framework; however, physiotherapists need to be aware of classifications which link directly to their domain of practice, that is, movement therapies.
Table 6.3
Models of low back pain classification
| Classification model | Clinical application |
| Patho-anatomical model | Conditions such as protruded intervertebral (IV) disc, spondlolysthesis, stenosis |
| Neurophysiological model | Cortical disorganization and the pain experience |
| (Bio)-psychosocial model | The impact of back pain on the individual and in society |
| Signs and symptoms model | Pain provoked by movement and motion testing |
| Mechanical loading model | Occupational/postural stresses and ergonomics |
| Motor control model | Failure in segmental and global motor control |
| Peripheral pain generator model | Pain generated by the IV disc, facet, sacroiliac joint |
| Disability model | Movement disorders: impairment, activity andparticipation levels |
Classifying chronic low back pain at an impairment level, O'Sullivan (2005) proposes that particular direction specific provocative spinal postures and movement patterns indicate the presence of either movement (restriction) or control impairments. The former being characteristic of restricted movement associated with fear avoidance, anxiety and both peripheral and central neurophysiological sensitization and responding well to manual techniques and active strategies which restore ideal movement and enhance movement conditioning. The latter being characterized by impairment of the motor system such that tissue strain in specific movement directions is not restricted but poorly controlled and responds well to motor control and muscle balance strategies to enhance pain relief and improved function.
In follow-up to these proposals, Dankaerts & O'Sullivan (2011) reviewed randomized control trials evaluating the validity of the motor control impairment sub-classification and note that it is good practice to utilize not only functional activation of the motor system but also cognitive-behaviour strategies to enhance motor control and reduce maladaptive movement.
Slater et al. (2012) carried out a systematic review to investigate the effectiveness of sub-group specific manual therapy for low back pain. Seven studies were identified for their methodological standard, although graded low in quality. The review suggested that there were significant treatment effects when heterogenous sub-groups were identified for intervention using manual therapy compared with pain treatments and activity.
Flynn (2002) provided the clinical prediction rule (CPR; Box 6.4) in the better quality studies (PEDro www.pedro.org.au/) and therefore the basis of the subgroup of patients with low back pain for which manual therapy provides a significant treatment effect.
Schafer et al. (2011) carried out an experimental design cohort study on sub-groups of patients with low back pain and leg pain to find out whether pain and disability outcomes differed between these sub-groups following neural mobilization techniques.
Seventy-seven recruited patients were sub-classified following interview and examination by experienced manual therapists. Patients' sub-groups were those classified as:
• Neuropathic sensitization (predominance of parasthesia and dysaesthesia with pin-prick hypo/hyperalgesia)
• Denervation (nerve conduction loss/ neurological deficit)
• Peripheral nerve sensitivity (nerve trunk mechanosensitivity with positive straight leg raise (SLR), PKB and positive nerve palpation)
All recruits received seven neural mobilization interventions twice per week that incorporated two passive mobilization techniques. The techniques were a foraminal opening technique (lateral flexion in sidelying), and a neural sliding technique (hip and knee flexion and extension in sidelying).
Outcome measures consisted of a numerical pain rating scale, the Roland Morris disability questionnaire and a global perceived changes scale from 1– ‘completely recovered’ to 7– ‘worse than ever’. Results indicate that patients classified as peripheral nerve sensitivity showed the best outcome scores and a more favourable prognosis.
This study suggests that it is important for physiotherapists to consider the type of presenting neural symptoms in order to apply specific neural mobilization techniques to the most appropriate subgroup of patient for best effect.
Smart et al. (2012), in a cross-sectional trial between subjects, investigated the discriminant validity of a mechanisms-based classification of patients with low back pain (with or without leg pain) by analyzing data on the self-reporting of pain, quality of life, disability and anxiety/depression.
One aim of the study was to improve clinical outcomes by using mechanism-based classifications to help physiotherapists apply appropriate clinical practice approaches. Using interview and examination, patients in the study (N=464) were classified into mechanism-based subgroups:
• Nociceptive pain (peripheral receptor terminal activity-tissue based)
• Peripheral neurogenic pain (lesions or dysfunction in peripheral nerves)
• Central sensitization pain (abberent processing and sensitivity within the central nervous system pain neuromatrix).
On analysis of the self-reporting in each subgroup it became clear that patients with nociceptive pain report less severe pain, have fewer quality of life and disability issues and suffer less anxiety and depression. In contrast, patient in the subclass central sensitization pain reported higher scores in each of the areas. Peripheral neurogenic pain classified patients reporting was in between the other two.
The suggestion here is that if physiotherapists can recognize patients in each of these mechanism subgroups they can be confident that, in general, patients with nociceptive pain will respond to tissue based interventions (manual therapy, active strategies) without cognitive behaviour barriers. Patients with peripheral neurogenic pain will respond to neural mobilization with some need to address cognitive behavioural issues. Whereas patient with central sensitization pain will need more interventions directed towards the maladaptive central nervous system processing (i.e. cognitive behavioural strategies) in conjunction with the application of tissue based approaches.
May & Aina (2012) investigated the centralization of symptoms and preference in movement directions in a literature review. It was found that the centralization phenomenon is more prevalent in acute than in sub-acute or chronic symptoms. They found 21 of 23 studies supporting the prognostic validity of centralization, including three high-quality studies. They conclude that findings of centralization or directional preference may be useful indicators of management strategies and prognosis in acute low back pain.
Kent & Kjaer (2012) investigated in a literature review if subgroups of people with particular psychosocial characteristics, such as fear avoidance, anxiety, catastrophizing, could be targeted with different treatment approaches. It appeared that graded activity plus treatment based classification aimed at people with high fear of movement was more effective in reducing this fear than treatment-based classification alone. Also, they describe that active rehabilitation with physical exercise classes based on cognitive behavioural principles was more effective than GP care at reducing activity limitations. However, they conclude that only few studies have investigated targeted psychosocial interventions. Overall they suggest more properly designed and adequately powered trials to find further responses to these queries.
It may be concluded that researchers in low back pain have recognized the necessity of subgroups in classifications for scientific studies. Many of these studies seem to reflect the clinical reasoning processes of physiotherapists, however currently it may be challenging to develop trials, which mirror the complexity of the clinical decision-making processes fully.
Clinical reasoning
The scope of the Maitland Concept, underpinned by open-minded clinical reasoning and patient-centred practice, is within the domain of rehabilitation. A classic example of this scope is evident from the following experience of one of the authors.
Whilst leading a course week on The Maitland Concept in a major European city with 20 students, a patient demonstration was arranged.
The patient, a 17-year-old male handball player, presented with low back pain and left-sided sciatica. He had hurt his back when he threw a ball in mid-air and landed awkwardly, twisting his back. He had had these symptoms for several months without resolution and he was only able to train for handball for half an hour before his symptoms became severe enough for him to have to stop.
He informed the group that he had a spondylolisthesis. His X-ray, in fact, showed a pars defect of congenital origin at L4. The group as a whole then began to think exclusively about the spondylolisthesis as the major factor in his problem and the focus of management.
Clinical examination, however, revealed a restriction in lumbar flexion, which became more so with cervical flexion as an addition but easier when deep abdominal muscles were activated. Lumbar extension was very restricted and reproduced his buttock and calf pain. When he jumped, as in handball, on initiation of the jump he lost control of his trunk lateral flexion. His SLR was restricted on the left and his L5 segment was stiff. He felt most comfortable lying on his right side.
Based on these findings and evidence he began to be able to control his symptoms and increase his exercise tolerance (1 hour training) over 4 days of functional interventions including:
• Restoration of pain-free SLR by the use of neural gliding techniques in right side lying with lumbar rotation and activation of deep abdominal muscles
• Mobilization of L5 whilst activating deep abdominal muscles
• Tonic control of the trunk in gradually loaded positions up to jumping and throwing.
The message here is that independent of pathological defects within the spine, which do not fully explain the onset and nature of the patient's symptoms, functional restoration and conditioning can and does have an effect on movement related symptoms, activity limitations and participation restrictions.
This example demonstrates the complexity of the clinical reasoning processes of physiotherapists, with the different paradigms and theoretical models, which they employ during assessment and treatment. With the ‘brick wall model’ of clinical reasoning, as developed by Maitland (1986), it is suggested that physiotherapists follow a different decision-making process from that of other professionals (e.g. medical practitioners), as the core of a physiotherapists' work lies in the analysis and treatment of movement functions. With the brick wall model Maitland moved away from the biomedical diagnosis as primary basis for decisions regarding the selection and application of physiotherapy treatments. Furthermore, he accentuated the necessity of independent decision-making processes in order to provide the best MSK-physiotherapy care (manipulative physiotherapy) possible. However, Maitland (1995) emphasized that manipulative physiotherapy should always occur under the umbrella of recognized health-care practice.
Physiotherapists often employ various forms of clinical reasoning, dependent on the particular needs of a situation. Most known is procedural clinical reasoning, with assessment and treatment procedures based on hypotheses generation and testing as well as on clinical pattern recognition (Jones 1995; for example, a physiotherapist examining a patient with sciatica and numbness in the big toe would include neurological examination and SLR as part of the assessment procedure). It has been recognized that therapists employ other forms of clinical reasoning as for example interactive, narrative, conditional or educational reasoning in addition to procedural reasoning strategies (Edwards 2000, Hengeveld 1998). As the subjective examination follows mostly a semi-structured interview, there is ample opportunity to integrate both procedural and interactive and narrative clinical reasoning, in which patients are enabled to give an account of their experience in sufficient depth.
Sound clinical reasoning is based on a profound and wide clinical knowledge base and cognitive and metacognitive abilities (Jones 1995). Also, theoretical knowledge from varied basic sciences is being applied to clinical situations: for example, the physiotherapist might think that a patient has nociceptive facet joint pain if the patient complains of deep unilateral aching stiffness in the lumbar spine when moving. This analysis is born out of knowledge of structure, mechanics and specific innervations of structures. Therefore, physiotherapists need a reflective and analytical approach to most, if not all, decisions they make in clinical practice and to develop an attitude of lifelong learning, in which they recognize their current specific learning needs.
Hypotheses generation and testing
At the moment a patient registers for treatment with a physiotherapist, the process of hypotheses generation will start, on the one hand by the physiotherapist, on the other hand by patients themselves.
Categorization of hypotheses support clinicians to distinguish relevant information from irrelevant information, to become aware of subtle expressions of the patient indicative of the individual illness experience with the illness-behaviour and to become more comprehensive when summarizing information from assessment procedures (Thomas-Edding 1987, Jensen et al. 1999). These hypotheses categories are described in Chapters 2 and 7.
Patients may focus on questions such as ‘what do I have’, ‘what can be done for it’, ‘how long will it take’. Their attitude towards treatment will be affected by their thoughts, emotions, belief-system, influences from their social environment and earlier experiences with therapy. For example, a patient may reveal that they are frightened of bending since they hurt their back because they don't want the same experience of pain again. They say ‘I do not want you to hurt me’. The analysis here is that the therapist must try to employ mobilization techniques in a way that also helps the patient to regain confidence in movement again. Explanation and inclusion in treatment decisions therefore become crucial. As these factors may be crucial in final treatment outcomes, they need to be considered by the therapist as contributing factors to the (movement) disorder or even determining factors in the individual illness experience of their clients. Therefore, physiotherapists should include hypotheses categories such as ‘contributing factors’ and ‘individual illness-experience’ in the reflection and planning of assessment, treatment and the therapeutic relationship.
Overall, the hypotheses and clinical decisions of physiotherapists may pivot around three main issues (Mattingly 1991):
1. What are possible causes and contributing factors to the patient's disorder? This relates to questions and tests regarding:
a. Possible pathobiological processes, including red flags
b. Analysis of causes of movement dysfunctions (movement behaviour)
c. Analysis of (movement-)impairments, activities, participation, contributing factors
d. Contribution of the individual illness-experience and behaviour, including yellow flags. E. e. Neurophysiological pain mechanisms
f. Physiological tissue-processes, as for example stages of tissue-healing.
2. Which treatment approaches may be most effective? This is associated with decisions on the current best evidence of therapies, but also with the question whether the current best evidence seems suitable to the patient as an individual. Therapists need to understand the role of passive and active movement, as well as other physical applications in treatment.
Possible habitually selected treatments based on the notion ‘I've always done it this way and it worked' need to be reflected upon; however, it is equally important to remain attentive of following injudiciously the favourite current treatment forms of a clinical and scientific cultural society. For any treatment chosen, clinical proof of its effects need to be given by consequent, comprehensive and well-reflected reassessment procedures (see Box 6.5).
3. How can patients be actively engaged in the therapeutic process?
There is increasing scientific support for the role of the therapeutic relationship in treatment outcomes and person-centred, multidimensional approaches with a cognitive behavioural perspective (Asenlöf et al. 2005, 2009). Also active engagement of a patient into treatment should support the process of patient-empowerment, as advocated by the World Health Organization (WHO 2008). Hall et al. (2010), in a review on the influence of the therapeutic relationship on treatment outcome, concluded that particularly beneficial effects could be found in treatment compliance, depressive symptoms, treatment satisfaction and physical function.
The question of active engaging patients in the therapeutic process is related to consideration of:
a. The roles of both therapist and patient in treatment (e.g. coach, educator, curative role, preventive role) (e.g. is the patient expecting something to be done to them or are they expecting the therapist to inform them on what they can do for themselves)
b. Expectations of the patients towards therapy (do they expect to be given manipulation or exercises for their back pain; also, do they have positive expectations towards the treatment)
c. Cognitive factors as belief systems about the causes and treatment options. Also the paradigms and perspectives patients have on their problem. If this differs from that of the physiotherapist, educational strategies at an early stage are necessary (e.g. the patient might think that moving and exercising will cause damage to their back whilst the therapist thinks that movement is necessary for recovery and reducing pain)
d. Affective factors, as for example gentle guidance towards more confidence in trusting to move (both in reassessment procedures as in explicit movement/exercise experiences)
e. Influence on, and by, the social environment. In this relationship at times the concept of secondary gain has been brought forward. Secondary gain is described as a social advantage attained by a person as a consequence of an illness; however, tertiary gains may also exist, in which others in the direct environment benefit from the illness of the person. It is warned not to focus solely on secondary gain of a person with pain without asking what may be the secondary losses to the person (Fishbain 1994). (Here the patient and therapist must have the same goals e.g. to return a patient with back pain to a working and productive life or, as in the case of chronic disability, to provide the patient the strategies to master their situation themselves.)
f. Behavioural factors, as for example movement behaviour, expression, guarding, confronting.
It is recommended that within a therapeutic relationship patients need to be treated as equals and experts in their own right, and that their reports on pain need to be believed and acted upon. Opportunities need to be provided to communicate, to talk with and listen to the patients about their problems, needs and experiences. In addition, independence in choosing personal treatment goals and interventions within a process of setting goals with, rather than for, a patient needs to be encouraged (Mead 2000). See also Chapter 3.
Experiential knowledge, clinical patterns
While reassessment-procedures primarily aim at monitoring clinical evidence of treatment-outcomes, they also fulfill an important role in the development of the experiential knowledge base of clinicians, as described by Schön (1983). It appears that experts may have more patterns in memory and may be capable of overseeing a situation quickly and are capable to find more comprehensive and effective solutions, faster than novices in a field (De Groot 1946). This is often an intuitive, implicit process. The concept of clinical patterns as a part of the experiential knowledge base has found acceptance in physiotherapy education and practice (Jones 1995). Studies between experts and novices demonstrated differences in ‘if … then …’ rules as a form of forward reasoning, being more present with experts. These rules may be considered as an expression of clinical pattern recognition and students need to be encouraged to express their ‘if … then … rules’ explicitly and to engage in consequent, written planning of assessment-procedures and treatment sessions (for example, an expert physiotherapist will have the experiential knowledge and professional knowledge to know quickly whether a patient with back pain will respond to manual therapy or will need cognitive approaches. In this way expert physiotherapists will reach a successful outcome quicker than the novice or move the patient on to self-management more quickly).
The development of clinical patterns cannot occur only by theoretical learning. Direct clinical experiences are necessary, in which clinical presentations and individual stories of patients are being encapsulated in clinical memory (Schmidt & Boshuyzen 1993). The application of theoretical knowledge, direct patient-contact, disciplined processes of hypotheses-generation and testing with consequent reassessment procedures and structured reflexion are prerequisites to the development of clinical patterns and expertise.
The following groups of clinical patterns may be distinguished:
• Movement disorders in conjunction with pathobiological processes. This is related to the question if, in the background of the movement disorder, pathobiological processes are present. Associated issues are:
How do they influence the short term and long term prognosis of the movement disorder?
In cases of NSLBP: are any movement patterns attributable to nociceptive processes in lumbar spine structures (e.g. disc, facet joint) or clinical syndromes (e.g. lumbar stenosis, neurogenic pain, lumbar structural/functional stability dysfunction), which need a specific approach to treatment?
• One-component versus multicomponent movement disorder. Movement disorders where it is more likely that one movement component is involved versus multiple movement components. One-component movement disorders may occur more frequently in younger people, with a single trauma in history (e.g. knee-distortion) with pain-reduction and improvement of activity levels occurring to the expected time of tissue-healing. Multicomponent movement disorders are more likely to occur where there is a degenerative, osteoarthritic background. In the latter case, screening of possible contributing areas to the nociception is important in the first three treatment sessions (e.g. pain in the buttock area often requires assessment of the lumbar spine, sacroiliac joint, hip, neurodynamic functions, possibly thoracic spine, and muscular functions).
• Approach to treatment: one-dimensional versus multidimensional approach. A movement disorder, which requires an explicit multidimensional approach to treatment. This means that contributing factors such as cognitive, affective, sociocultural and behavioural factors need to be explicitly defined in treatment-planning and in reassessment-procedures. In this case the quality of the therapeutic relationship, communication (interactive clinical reasoning), education and information may play a crucial role. This multidimensional approach is more likely to be required in chronic pain states or where recuperation of normal function and pain-reduction take much longer than normally expected. This is particularly necessary in those cases, where patients express a sense of helplessness, hopelessness or strong frustration with the provided health-care, with conflicting information; differ in beliefs / paradigms regarding causes and treatment; present avoidance-behaviour which has become maladaptive; perceive their state as highly disabling; demonstrate hypervigilant movement behaviour.
Prognosis and clinical prediction rules
Making a prognosis is an important skill in physiotherapy practice. However, often it is a daunting task (Maitland et al. 2005) as clinicians are more likely to be dealing with probabilities more than with certainties. Making a prognosis is a skill, in which clinicians match the clinical presentation of a patient's problem with theoretical knowledge (e.g. tissue healing) and clinical experiences made with patients who present with similar dysfunctions and resources. Hence, it contains elements of clinical pattern recognition. The years of experience which a clinician has spent with the assessment and treatment of particular disorders of persons will certainly aid in making a more accurate prognosis; however, experienced clinicians probably express themselves carefully while making a prognosis, as more stories may be encapsulated in their clinical memory in which patients' processes of recuperation differed from the initial prognosis made by the therapist.
Nevertheless, a clinician frequently needs to estimate in which way results may be achieved, how long treatment may take and which concrete results may be achieved. Patients often want to know, what is wrong with them, what can be done about it and how long it is going to take? Also, from the viewpoint of insurance companies and referring doctors, a physiotherapeutic prognosis may be essential.
Prognosis takes place in various phases:
1. At the beginning of a treatment series:
a. What can be achieved on a short-term basis: which results can be expected within the first three or four sessions (for example, the therapist might think, if the patient with acute low back pain improves by 80% within the first 3–4 sessions then there is a high probability that they will return to their normal duties)?
b. What can be achieved on a long-term basis during the overall process of physiotherapy?
2. During the treatment series, especially during retrospective assessment in every third or fourth session. It is essential to reflect on all the hypotheses formed and rejected thus far in the therapeutic process; especially the reflection on the prognosis may aid the clinician to learn profoundly from each encounter with a patient, and to develop and deepen clinical patterns in memory (for example, the therapist may find that the patients back pain is settling within 2–3 sessions of mobilization but their leg pain is not changing. The therapist may then think that the problem may take longer to sort out and other, additional treatment approaches may need to be considered).
3. At the end, during final analytical assessment – making a prognosis for the time after the therapy has been be completed:
a. The likely restraints on lifestyle.
b. The likelihood of recurrences of episodes of the disorder, and the possible early warning signs that the patient must heed in order to minimize the severity of the recurrence, and the steps the patient then needs to take.
c. The need for specific ongoing exercises, intermittent maintenance treatment, or follow-up assessment (for example, one patient with back pain may feel that they do not need any further advice where as another may be pain free and yet still fear that they will hurt their back again if they go back to work. In the second case it is important for therapy to include graded work hardening to ensure sustainable recovery and a favourable prognosis).
Specific hypothesis categories should also be considered to make a comprehensive prognosis:
1. Disorders that are easy or difficult to help (e.g. complex regional pain syndromes).
2. Nature of the person, including attitudes, beliefs, feelings, values, expectations, (movement) behaviour, and so on.
3. Nature of the disorder (intraarticular and periarticular disorders; mechanical osteoarthritis/inflammatory osteoarthritis; acute injury/chronic degenerative injury, nociception alone/nociception with peripheral neurogenic or central sensitization).
4. The body's capacity to inform and adapt. (The way the patient ‘feels’ about the disorder often correlates well with other aspects of prognosis. For example: ‘I've had back pain for 20 years so I know I'll never totally get rid of it, but I've been able to cope with it so far'.)
5. Contributing factors and other barriers to recovery (structural anomalies, systemic disease, general health problems such as diabetes, ergonomic/socioeconomic environments such as: keyboarding, heavy manual work; repetitive, monotonous activities; little control over work circumstances).
6. Expertise of the physiotherapist, especially in the field of communication and handling.
The bio-psychosocial model of the ICF (WHO 2001) may serve as an aid in considering aspects of a prognosis. If only function impairments are present – as, for example, slight restricted mobility of the hip and muscle imbalance in an otherwise healthy patient who is without great activity limitations, participation restriction and no relevant context factors – the prognosis will be, of course, much more favourable than if disturbances of all elements are present. The physiotherapist has to evaluate whether discrepancies among the elements of the model are present.
In prognosis-making, numerous factors need to be taken into consideration in either short-term or long-term prognosis:
• Stage of tissue healing and damage
• Mechanical versus inflammatory presentation of the disorder
• Irritability of the disorder
• Relationship between impairments, activity limitations and participation restrictions
• Onset of the disorder, duration of the history, stability of the disorder and progression/course of the disorder (are attacks more frequent or disabling?)
• Pre-existing disorders and dysfunctions (e.g. the patient has fallen on the shoulder; however, they may have had degenerative changes in the neck with some pain for some years)
• One- or multicomponent movement disorder (e.g. only local movement dysfunction in elbow, or the disorder has more components contributing to it: shoulder, cervical and thoracic spine, neurodynamic dysfunction)
• Contributing factors – ‘cause of the source’ (e.g. posture, muscle weakness or tightness, discrepancies in mobility of joint complexes, such as spine or wrist)
• Cognitive, affective, sociocultural aspects, learning processes: patient's beliefs, earlier experiences, expectation, personality, life style, learning behaviour, movement behaviour
• Multidimensional approach to treatment: consideration if the cognitive, affective and behavioural dimensions need to be addressed in treatment.
After some years of clinical experience, physiotherapists learn to recognize which kinds of clinical presentation react more or less favourably to treatment (Table 6.4).
Table 6.4
| Disorders easy to help | Disorders which may be more difficult to help |
| Strong relationship of patient's symptoms and movement | Weak relationship between the symptoms and movements in the patient's mind |
| Recognizable/typical syndrome or pathology | Atypical, unclear patterns, syndromes or pathology |
| Predominantly primary hyperalgesia and tissue-based pain mechanisms (nociception; peripheral neurogenic) | Predominantly secondary hyperalgesia from central nervous system sensitization rather than stimulus-response related tissue responses |
| Model of patient: helpful thoughts and behaviours (‘I can still do some things’; ‘I have found ways to get relief’) | Maladaptive thoughts and behaviour: (‘I don’t think I ever get better’; ‘I dare not move because always hurts me’) and other yellow flags |
| Familiar symptoms which the patient recognizes as tissue based (‘it feels like a bruise’) | Unfamiliar symptoms which the patient has difficulty describing in sensory terms |
| No or minimal barriers to recovery of predictors of chronicity (‘yellow flags’) | Multifactorial/multicomponent /complex regional pain syndromes |
| Severity, irritability and nature of the patient's symptoms correspond to the history of the disorder/to injury or strain to the structures of the movement system | Severity, irritability and nature do not fit with the history or stage in the natural history of the disorder |
| The patient has had a previously favourable sampling experience with manipulative physiotherapy | Previous unfavourable sampling experiences or knowledge of manipulative therapy (‘my mate had manipulation of his shoulder and he said it |
| There are easily identifiable signs of impairment and activity limitations which have a strong relationship with movement | was much worse afterwards')Evidence of movement impairments but with little correspondence to the degree of activity limitation |
| Patients are touch tolerant (gain relief by touch, rubbing or massage) | Patients are touch intolerant (‘I don’t like anyone touching my knee’) |
| An internal locus of control (‘I just need to know how I can help myself’); locus of control with regard to health and well-being is consistent | An externalized locus of control (‘you are the physiotherapist, you sort me out’) or inconsistency in locus of control with regards to health and well-being |
| The patient has realistic expectations for recovery which correspond with the natural history of the disorder | Unrealistic expectations for recovery (‘I wish I would wake up and all the pain would be gone’) |
| Patients will resume appropriate activity and exercise at relevant stages of recovery | Ongoing pain states with little changes in symptoms over a long period of time |
At the third or fourth treatment session, and the final analytical assessment, the manipulative physiotherapist should be able to answer the following questions about a patient's disorder in the quest for a prognosis:
• What is the biomedical diagnosis and which pathobiological mechanisms (tissue mechanisms – pathology, healing processes; neurophysiological pain mechanisms)?
• What is the source(s) of the patient's symptoms?
• What are the contributing factors to the source of the symptoms (‘cause of the source’)
• To what extent is movement impaired and activities/participation restricted by the symptoms?
• To what extent is severity or irritability limiting movement and activity?
• Which predictions can be made about the natural history of the disorder based on its onset, stage of pathological development, and pathological stability/lability (e.g. healing phases of a lumbar disc)?
• Which predisposing factors are influencing the course of the disorder (pre-existing pathology, comorbidity, weak link, the nature and extent of injury, age-related processes, general health state, physique, occupation, hobbies, life style, genetic predisposition, etc.)?
• Which factors are contributing to a favourable or unfavourable prognosis?
• Is the disorder one that will be easy or difficult to help based on examination and response to treatment)?
• What do we understand about the patient's nature and response to injury and illness (adaptive/maladaptive behaviour; beliefs, thoughts, feelings, attitude, former experiences, values, etc.)?
In summary, prognosis is a forecast of the future history of a patient's disorder based on the probability of physical, psychological and functional recovery of the patient and the disorder. Therefore, consideration should be given to:
1. The natural history of a particular disorder. (Careful: some studies claim that some disorders, e.g. tennis elbow or frozen shoulder, recuperate over 2 years; however, what is the amount of remaining functional impairment?)
2. The response to MSK/manipulative physiotherapy – has the progress been acceptable?
3. What is acceptable to the patient – has the main problem been solved?
4. Possible need for prophylaxis – is a self-management programme needed to complement or maintain recovery? Is the patient capable of implementing elements of this programme at adequate moments? Is ‘top up’ treatment required periodically?
It is essential to maintain at all times a self-critical attitude towards prognosis and regularly pose the same questions as in retrospective assessment, if therapy seems to be stagnating:
• Have I compared the subjective and physical parameters (‘asterisks’) regularly enough and in sufficient detail?
• Did I ensure that the patient would become aware of positive changes in these parameters as well?
• Did I follow up the correct physical asterisks, which reflect the patient's main problem and the goal of the therapeutic intervention?
• Have I performed a review of the therapeutic process with retrospective assessment procedures, collaboratively with the patient?
• Has the right source of the symptoms been treated?
• Have the self-management procedures been pursued profoundly enough? Did these procedures provide the patient with sufficient control over the pain and well-being on all daily life situations? Did I teach them well enough?
Even if physiotherapists embark on a therapeutic process with a less favourable prognosis, they should bear in mind that a prognosis deals with probabilities and hypotheses, hence still maintain a positive attitude towards treatment. The following quote relating to neurological rehabilitation may serve as a demonstration of this principle:
A positive approach right from the start can contribute greatly to the success of treatment. I find it helpful when I first start treating a patient to picture him walking out of the hospital unaided one day, well-dressed and waving goodbye with a smile, even if things look bleak during the early days following his admission. Should a patient not survive the initial trauma or sadly never regain consciousness, nothing will have been lost by the active intervention, but so much gained. All too often I am told that things went so wrong because everyone thought that the patient would not survive for long. Statistical studies concerning prognosis can also lead to negative attitudes, but statistics are not about individuals, and there have been many surprising exceptions. It has been wisely pointed out that the clinician's attitude may influence the recovery to the extent that cessation of recovery after 6 months, a widely held belief, may possibly in fact be the result of a self-fulfilling prophecy.
Davies 1994 (p. XI)
Clinical prediction rules
Clinical prediction rules have found increasing attention in the field of clinical physiotherapeutic research. These rules are clinical decision making tools designed to aid clinicians in determining a diagnosis, prognosis, or likely response to an intervention. They contain predictor variables obtained from patients' history, examination and diagnostic tests, which have been statistically analyzed and found to be meaningful predictors of a condition or outcome (Glynn & Weisbach 2011). They are not meant to replace individual decision-making processes, but should be considered within the philosophy of evidence-based practice, in which clinicians are encouraged to incorporate the best available evidence in their examination and treatment procedures. Hence they are meant to support the clinical decision making processes (Cleland 2011). Clinical prediction rules should not be blindly incorporated in clinical reasoning processes, as they can only be applied to similar patient populations which are similar to the population in which they have been researched (Huijbregts 2011).
Some clinical prediction rules with regards the lumbar spine and low back pain are listed in Table 6.5 (for further reference: Glynn & Weisbach, 2011).
Reflective practice
Clinical reasoning and assessment procedures are twin elements of this concept in NMS-physiotherapy. In order to enhance reflective practice and to develop expertise, it is essential that therapists make their hypotheses and decisions explicit during critical phases of the assessment and therapeutic process, reflect upon them and to plan the following steps of action in therapy.
The structuring of thought processes is best made explicit in the following critical phases of the therapeutic process:
• During the initial contact (‘welcoming phase’)
• First session: during the subjective examination
• First session: planning the physical examination and the first treatment
• Planning of the second (and third) session
• Planning of overall treatment (latest at the end of the third session)
• Planning retrospective assessments (in about every fourth or fifth session)
Simple comprehensive recording is highly relevant in, which should give a quick overview of the most essential details. The recordings should include:
• All relevant information from subjective, physical examination and treatment
• All relevant reflections, hypotheses and planning steps made by the physiotherapist.
Planning steps may be expressed in a flowchart, particularly if several decision options are simultaneously present. An example of written planning to enhance pattern development and reflective practice is included in Figure 6.2.
Examination of the lumbar spine: subjective examination
In the process of examining low back and/or leg pain it is the specific task of the MSK-physiotherapist to systematically investigate whether movement disorders are present. There may be relevant movement-impairments in the lumbar spine, sacroiliac joints, and/or hip. In some cases the other pelvic connections need to be examined as well. Furthermore, neurodynamic dysfunctions may contribute to pain and disability. Also it needs to be investigated whether changes in muscular control are contributing to the movement disorder. Analysis of movement habits in daily life (e.g. sitting habits), the general level of fitness, the impact of the problem on the life of the patient and information about the belief system about causes and treatment-options may also be part of the assessment procedures of the therapist.
Using semi-structured interviews, facilitating collaborative responses, listening for key words or phrases and following up with questions that qualify misunderstandings and ambiguities supports an attention to detail in the collecting of subjective data as a measure of the patients experience of their low back pain
The clinical reasoning model of the ‘symbolic permeable brick wall’ helps the clinician to categorize information into clinical evidence and theoretical knowledge.
Hypotheses categories can then be established, which help to shape and design physical examination and intervention based on the patient's individual needs.
When a person presents with low back and/or leg pain, during the subjective examination, the therapist may decide to pursue the procedures of the interview along a more strict protocol; to use paralleling techniques, in which the line of thought of the patient is guiding the interview; or to engage in narrative clinical reasoning, with active listening, in which patients can give a full account of the history of the problem and treatment. In any form of interviewing, it is essential that the therapist is aware of the hypotheses generated and modulated during the information-process and asks clarifying questions if necessary. Novices in the field, practising the art and skill of interviewing, may prefer to use a more strict protocol; however, also in this case it is essential to pursue clarifying and deepening questions, in order to confirm, modify or reject hypotheses generated during the discussion with the patient. A well-balanced approach between procedural and interactive reasoning will always be necessary (see also Chapter 2).
The subjective examination is an essential part of the overall assessment. Due to time restrictions, therapists may decide to shorten the interview or to start to control the interview with strict sets of (closed) procedural questions. However, important information may be missed, resulting in superficial clinical decisions. It is recommended that physiotherapists engage in other forms of clinical reasoning, as for example narrative or interactive reasoning next to procedural reasoning. This allows the therapist:
… to get an account of the patient's individual story rather than controlling the patient with strict assessment criteria in which the patient may only be allowed to talk about those aspects which are relevant to physiotherapeutic diagnosis and treatment-planning from the perspective of the physiotherapist.
(Thomson, 1998, p. 90)
By shortening the necessary time interviewing, conclusions about causes and treatment may be based on first sight information, which should have been refined during the subjective examination. Frequently this leads to disappointing results, as parameters to compare treatment outcomes are not detailed enough to allow for thorough comparison of changes in later sessions.
Subjective examination may be considered as a first phase of a learning process, in which not only the therapist learns about patients' problems and the impact on their life, but also patients may learn to see relationships between their pain, disability, activities and life-style. Furthermore it may set the tone for a person-centred agenda of treatment (Greenhalgh & Hurwitz, 1998). Hence the subjective examination is intrinsically therapeutic and should be allocated sufficient time in the encounters with a patient.
The procedures of the subjective examination may be grouped into five main categories:
1. Establishing the main problem from the perspective of the patient
3. Behaviour of symptoms in relation to activities
4. History (current, previous)
5. Medical and health screening questions (‘special questions’).
Particularly for novices in the field it is useful to follow these groups in sequence, but especially in cases of a recent, traumatic incident leading to the patient's symptoms, therapists may decide to follow up the history of the problem immediately after the establishment of the main problem. If a long lasting or recurrent history is present, at times it is better to wait with collection of the information regarding history, but to get a clear picture what is bothering the patient in the ‘here and now’. On the other hand, if patients with persistent symptoms and disability appear to be frustrated with the provided health care, telling their full story from their perspective may be intrinsically therapeutic, as they learn to make more sense of their experience and learn to cope better with a situation (Kleinmann 1988, Heath 1998, Main & Spanswick 2000). However, within this process of engaging in narrative reasoning the therapist should attempt to keep an overview of the basic procedures and of the planning of next steps of assessment and treatment. Otherwise it may be better to follow more procedural steps of interviewing and to seek support from a more experienced peer.
Introduction to the assessment process
It may be difficult for a patient to understand that each member in a multidisciplinary team follows a unique frame of reference, which in a sense is exclusive to their profession (Kleinmann 1988). Therefore, it is essential to inform the patient about the specific role of the physiotherapist in the diagnosis and treatment of movement dysfunctions, being complementary to medical diagnosis. This information needs to be given at an early phase of the encounter, before embarking on the examination and treatment process.
Furthermore, explanations need to be given about the setting and the steps that will be followed in the first session (interview, physical examination/movement testing, first probationary treatment, reassessment). It may be necessary to explain that this examination is highly important to individualize the treatment to the specific problem and needs of the patient.
Additionally, it is necessary to find out whether or not the patients/clients have been expecting physiotherapy as a treatment option for their problems (particularly in those cases where a patient has been referred by another medical practitioner). Also, it is useful to grasp if the patient understands that physiotherapy encompasses many various methods of movement therapy (hence, not only gymnastics), touching (e.g. passive mobilizations, manipulations, soft-tissue techniques) and other modalities.
In this introductory phase, by means of careful listening and observing, the therapist may become aware of some sensitivities of the patient with regard to therapy, setting and therapist, which can also be addressed (Main & Spanswick 2000).
Main problem
It is essential to establish the current main problem from the patient's perspective. Allowing the patient to express in their own terms what is bothering them provides the therapist with several hypotheses, as for example:
• Does patient's problem seem to be a movement disorder, or does it give an impression of another, pathobiological problem, which may need the attention of another primary clinician?
• Does it seem that the movement disorder can be treated from a one-dimensional approach, or does it need a multidimensional approach, in which extra care is given to the communication with the style of questioning and information processes during the overall examination and treatment? Also more time often needs to be allocated for the interview and the therapist should remain aware not only to ask questions about pain, but also about the current movement capacity and activity limitations. Central questions, at a later stage in the interview, will relate to how the patient is able to cope with the problem in daily life.
• Does it appear to be a movement disorder with severe or irritable symptoms, which needs extra caution during initial examination and treatment procedures?
People with lumbar movement disorders frequently present with low back, buttock and/or leg pain. Other symptoms may be, for example, stiffness or a sense of tiredness in the back and/or legs, numbness or paraesthesia in defined areas of the leg.
This may be expressed in different terms, which at times provide a therapist with first hypotheses about possible structures, clinical syndromes or movement components involved. For example:
• A sense of tiredness in the back, particularly if it spreads in a small line across the spine may be indicative of a stability disorder with discrepancies between more mobile and stiff intervertebral segments in the lumbar spine
• A band-like sensation of stiffness across the area of lower back may hint towards a movement disorder with discogenic features, particularly if these symptoms occur when rising from bed in the morning or rising from a chair after a prolonged period of sitting
• Sensation of muscle tiredness, cramp-like sensations may support hypotheses on neurogenic pain mechanisms and neurodynamic dysfunction.
Perceived disability
Next to the establishment of the main problem from the perspective of the patient, at this stage it is important to seek information in general terms about how patients perceive their disability and current movement capacities with their symptoms. First hypotheses will be developed about the question if the level of disability appears to be adaptive to the current process of nociception, or does it seem that the patient has developed maladaptive avoidance behaviour? For example: a man presents with a localized area of pain on the right unilateral side of L4–5, and reports that this pain has severely limited him in several daily life functions for the past few days only. The patient has learned to avoid the activities concerned, but has remained as active as the pain allows. Furthermore, the patient says that it seems that the pain has reduced somewhat already and he feels slightly more capable of using his body. This problem may be classified as severe (nociceptive) pain, with adaptive movement behaviour. On the other hand, if, for example, 4 months later the same patient reports that he still cannot carry out many daily life activities, it is possible that the protective behaviour has become maladaptive and may be labelled as ‘fear avoidance behaviour’ (provided that no other pathobiological processes can explain the pain and disability).
Also based on this information, the therapist can decide if a multidimensional approach to the examination and treatment needs to be adopted.
Localization and quality of symptoms
Precise description of the perceived symptoms on a body chart is essential in assessment. It will serve the therapist and patient in reassessment procedures in consecutive treatment-sessions and in the development of clinical patterns in the physiotherapist's memory. By comparing body charts with the symptom areas, therapists will develop hypotheses if typical, recognizable pain-patterns are present (i.e. end organ-dysfunction related to a recognizable incident in recent history or nociceptive or peripheral neurogenic patterns or at times, autonomic nervous system patterns). If the symptom distribution is atypical, caution should be given if a pathology is present, which needs further investigation (e.g. multiple sclerosis), or if a generalized tenderness has developed based on central nervous system sensitization processes. In this case the question should be followed up why central nervous system modulation seems to have taken place: are any pathophysiological processes present, which may be contributing cognitive, affective and /or behavioural factors?
With sufficient attention to detail clinicians may start to subgroup clinical patterns in their memory, which may serve in the research of the development of scientific subgroups and clinical prediction rules. The following text from Maitland (1986, p 259–260) demonstrates this principle:
Yet with all the programmes that have been published (and there are many), none of the authors seem to realize that a patient who feels pain as a very localized spot between the spinous processes of L4 and L5 (say), does not have the same problem as the patient who has pain spreading in a line across his back at the L4/5 interspinous space. Nor do they seem to realize that a patient who has a band of pain across his back, which may extend superiorly to L3 or L4 and inferiorly to S1, is different again, as is the patient who has a band of pain spreading across his back at the middle or lower sacral level is yet another different group. These areas of pain that have been mentioned do not take into account the differences that exist if the patient has pain that spreads across his back but is greater on one side than on the other, or if his pain is only felt on one side of his back. Similarly, these are all different from the patient who feels his pain in the area of the sacroiliac joint or in his gluteal area, yet these are still frequently classed in the (non-specific) back pain grouping for survey purposes. It is my belief that for any project to determine usefully the effect of manipulative treatment, the groupings of patients must be made much more specific. And this is relating the problems to ‘site-of-pain’ only. The behaviour of the pains then needs to be classified into separate groups.
As neurophysiological pain mechanisms seem to play a growing role in clinical decision-making processes and appear to become increasingly relevant inclusion criteria to research projects, Bogduk (2009) discusses the necessity to make a clear distinction between nociceptive back pain, somatic referred pain, radicular pain and radiculopathy. If radicular pain is not distinguished from somatic referred pain, diagnostic errors may occur and patients may be allocated to faulty (sub-) groups in scientific research leading to erroneous results (Table 6.6). Bogduk postulates that nociceptive back pain and somatic referred pain occur more frequently than radicular pain and radicular pain may be investigated with MRI or X-ray procedures, while somatic referred pain often gives inconclusive MRI and X-ray results.
Behaviour of symptoms
Information of the behaviour of symptoms during the day, week or even a month, provides information regarding:
• Parameters for reassessment procedures in consecutive sessions
• Precautions: information about the intensity of the perceived pain and concomitant level of activity will often be a decisive factor in the determination of the dosage of examination and treatment techniques
• Functional capabilities (capacity, performance, mediators) as well as confidence to move
• Coping strategies: deliberate (physiotherapeutic /movement, relaxation, heat/cold applications; medical advice, advice from complementary medicine, e.g acupuncture), intuitive (guarding postures, rubbing, movements)
• Neurophysiological symptom-mechanisms, sources of dysfunction
• Defining treatment objectives: rehabilitation of activity limitations and participation restriction, coping strategies to control pain and well-being, contributing factors as for example information from lifestyle as for example, average activity levels during a week, stress.
Next to the behaviour of symptoms, information about the general activity levels and preferences need to be sought, in order to develop hypotheses about the current movement capacity and resources of a patient.
Particular activities and postures in which lumbar spine movement dysfunctions may be (co-)involved are, for example:
• Sitting, rising up from sitting – note differences if sitting in a high chair, low chair, with legs crossed influences the symptoms
• Bending over as, for example, lifting something from the floor, putting on socks in standing, cleaning a kitchen cupboard
• Walking vigorously or slowly
• Activities in half-flexion as for example washing hair over a bathtub, shaving in standing over a faucet, cleaning /polishing surfaces.
Other activities related to lumbar spine disorders haven been described in the ICF-domains (see p. 232).
It is important not only to find aggravating factors but also easing factors, for example when a patient having lower back pain in sitting, shifts his weight to the other buttock and the pain reduces, it is possible that the lumbar spine is involved with a lateral flexion disorder or preference, respectively. Also, this may be indicative of a sacroiliac involvement. If the patient additionally stretches the leg forward and pushes himself slightly up on the arm rests of the chair to ease the pain, an associated hip disorder next to a lumbar spine dysfunction may be suspected.
In pursuing information regarding coping strategies it is important to seek detailed information about the deliberate or intuitive strategies a person has developed.
Deliberate, explicit strategies may encompass:
• Suggestions from a physiotherapist (which ones, and to which effect)
Other strategies, as for example prescription-free medication.
With intuitive strategies, patients may describe that they feel helpless when the pain increases. However, most patients will somehow intuitively grasp or move the area, without being conscious of this. Often exactly these strategies may be suitable to employ in treatment and as self-management strategies. It needs detailed observation of the patient's movement behaviour and careful communication in guiding the patient towards an increased bodily-awareness, with meaningful self-management strategies. This process may start at times already during the subjective examination (see Box 6.6).
‘Making features fit’
‘Making features fit’ as a principle has been described by Maitland (1986), meaning that at all times during the subjective examination, physical examination as well as during treatment and reassessment, all information needs to be reflected upon, to judge if the information would fit in with a certain clinical pattern. For example, from the body-chart a therapist may develop different hypotheses about different sources of the nociceptive process (e.g. lumbar spine, hip, sacroiliac joint); during the phase of ‘24h behaviour of symptoms’ it appears that some activities in which the pain occurs may be linked to movements of the hip and others may be related to movements of the lumbar spine.
If the physiotherapist is confronted with a situation in which features do not fit, meaning that no known clinical pattern can be recognized, further questioning is essential. In some cases, when the symptoms and signs, and at times the treatment-reactions, do not develop into a picture where the features would fit, the patient may need to be referred to a medical practitioner or a second opinion with another physiotherapist may need to be sought.
Features of some typical activities and postures related to the lumbar spine fitting to hypotheses structural involvement of discs, facets joints, neurodynamic functions (possibly minor end-organ dysfunction leading to nociceptive and/or peripheral neurogenic processes):
• Pain or a sense of stiffness when getting up from sitting, as well as activities in semi-flexed positions such as shaving or washing hair, may be indicative of a discogenic disorder being part of the movement dysfunction
• Facet joints frequently, but not exclusively, may provoke more localized, unilateral/bilateral symptoms while stretching the joint structures towards flexion and contralateral sideflexion and/or compressing the structures towards extension and ipsilateral sideflexion
• Pain provoking activities, as for example using the gas pedal while driving a car, may give a hint towards a neurodynamic dysfunction.
History of symptoms
The history of the symptoms and disability is an important phase of the subjective examination. Particularly details about the onset of the problem may give worthwhile information about risk factors, movement behaviours as well as mediators of pain and, particularly in cases of recent traumatic onset of pain and disability, possible structures involved.
Recent history
This relates to questions such as:
• When did the symptoms occur for the first time (when did ongoing symptoms increase)?
• Which circumstances have led to the onset/increase of the symptoms (traumatic, spontaneous onset)?
• Course of symptoms and activity levels since onset/increase?
• Current symptoms and disability compared with the period on onset/increase (e.g. ‘how is it now compared with 2 weeks ago, when it got worse’)?
In cases of spontaneous onset, questions about the use of the body, the capability of the structures to bear stress and the general stress levels/stress capacity of a person will be very informative for the selection of therapies regarding self-management strategies and prevention (e.g. long unilateral movements in awkward positions without interruption may need regular interruption with repeated movements in contralateral directions or light bracing with motor control actions). Particularly challenging for patient and therapist are work situation in which a high concentration is asked of the person, as particularly in these circumstances it may be challenging to change habitual patterns of movement behaviour and general tension. For example: a puppeteer in a theatre is standing for a long time with puppets held high above her head with the lumbar spine in extension, right rotation and left sideflexion. She is advised to change the position of the puppets used in the show from her left side to the right side on the floor, in order to achieve flexion and sideflexion during the show; during breaks as a first thing to do, she is encouraged to perform repeated movements in flexion, rotation left and/or sideflexion right and to relax physically and mentally with breathing exercises, combined with a visualization technique).
Especially in cases of recurrent symptoms of acute low back pain the history of the problem, the kind of treatment received and its immediate and long-term effects may provide highly relevant information about the first actions in therapy to take. It is essential to be thorough with follow-up questions. Patients may state that physiotherapy or medication have not helped ‘at all’; however, with some clarifying questions, the patient may say that the interventions have helped for a certain period of time, but that the symptoms returned. A central question will be why this may have occurred:
• Certain techniques may have been helpful, but effects did not remain. This, for example, may be because progression of treatment techniques should have been followed up (e.g. treatment of accessory movements of the spine in an end-of-range position).
• Quality of the self-management strategies. It is possible that the patient has not developed an awareness of the specific objectives of the exercises/interventions concerned, as for example knowing which strategies to select when increase of pain occurs and which exercises are meant to optimize motor control or general fitness. Often patients are provided with a list of exercises, with a consequence that they perceive that the list has to be worked off (mechanically) at a regular basis. Also, they may not have gained a sense of success regarding self-management to control pain, as the exercise may have been taught once and not been reassessed on its effectiveness in consecutive session or during final analytical assessment procedures (see Chapter 1).
• Stage and stability of the disorder. In some cases, as for example neurogenic pain mechanisms with radicular symptoms, recurrence may occur because the disorder was not stable enough. Patients may have resumed higher levels of activities, including work, but the pain was still quite severe. Particularly radicular symptoms in contrast to simple nociceptive processes, frequently need more time to resume (Bogduk 2009) and therefore a more cautious progression towards higher levels of activity.
Previous history
In long lasting or recurrent episodes, information on the historical context of a problem establishes mediators and risk factors, which may needs to be followed up in treatment planning. Question about the previous history should encompass questions as:
• Episodes of symptoms and activity limitations: which episodes and when did they occur?
• How did the episodes usually start (habitual time patterns and patterns of movement behaviour, e.g. lumbar symptoms in periods of high stress and concentration in the office; yearly recurring activities as for example potato harvest on the farm)?
• How were the symptoms and activity levels between episodes (some patients, especially after a large trauma, with subclinical or clinical nerve trauma, may state that the pain recurs at times, but that the overall activity levels have improved over the course of years)?
• How did the symptoms and particularly activity levels change over the course of time?
• How is the current episode in comparison with former episode? (It is possible that a more ‘discy’, degenerative movement-disorder changes towards a presentation of lumbar stenosis; other may state that the current episode of low back pain is better than before, as they walk more regularly since they have retired from sedentary work.)
Medical and health screening questions
Several questions must be asked so that the physiotherapist is aware of any inherent dangers from treatment or should limit treatment in general. In certain circumstances, as for example osteoporosis, dizziness based on possible vertebrobasilar insufficiency (VBI), treatments such as manipulations with high velocity thrust will not be indicated, but gentle passive movement may be the treatment of choice as long as possible side-effects are monitored.
Special or screening questions encompass the following:
• General health, medication (which, to which effect), involuntary weight loss, medical imaging (incl. results)
• ‘Red flags’ (see p. 235)
• Information regarding osteoporosis, long-term steroid and anti-coagulant use, diabetes, neurogenic disorders (polyneuropathy)
• Questions regarding bodily systems as cardiac, pulmonary, gastrointestinal, genito-urinary, vascular and musculoskeletal functions, which are part of the screening process of possible biomedical disease. These questions are particularly important in cases of direct contact/self- referral of the patient; however, also, the questions may also be relevant in cases of medical referral as the clinical presentation may have changed since contact with the medical doctor (see pp. 28 and 53 in Chapter 2).
• Additional questions concerning yellow flags, provided the information has not been gained yet during previous questions of the subjective examination (see p. 233 of this chapter).
Typical patterns of clinical presentation
Table 6.7 provides information about some typical clinical presentations in which the lumbar spine may be involved. Clinical patterns may contain clinical prediction rules, but, as they are normally a result from a theoretical and individual experiential knowledge base, they may differ in details from person to person.