Chapter 13 Imaging of the Pelvis and Hip
Imaging of the pelvis can be required following minor or major trauma and for nontraumatic painful conditions. In this chapter, we review a systematic approach to interpretation of the standard pelvis x-ray, correlating abnormalities with computed tomography (CT) findings. We also discuss high-risk pelvic bony injuries associated with soft-tissue and vascular injuries—which are examined in detail in related chapters on genitourinary imaging (Chapter 12), abdominal trauma (Chapter 10), and interventional radiology (Chapter 16). Because fractures of the proximal femur are often clinically indistinguishable from fractures of the pelvis, we illustrate these injuries here, with more discussion in the chapters on extremity injuries (Chapter 14) and musculoskeletal magnetic resonance imaging (MRI, Chapter 15). Along the way, we consider a number of critical clinical questions:
How Common Are Pelvic Injuries? What Injuries Are Associated With Pelvic Trauma?
An 8-year retrospective review of the trauma registry at the Los Angeles County and University of Southern California trauma center found that 9.3% of 16,630 adult admissions sustained some type of pelvic fracture. In patients with pelvic fractures, 16.5% had associated abdominal injuries, including liver (6.1%), bladder and urethra (5.8%), spleen (5.2%), diaphragm (2.1%), and small bowel (2%). In severe pelvic fractures (defined by an Abbreviated Injury Scale score ≥4), intrabdominal injuries rose in frequency to 30.7% of patients, and the bladder and urethra were most commonly injured, in 14.6% of patients.1 Aortic rupture was seven times more common in patients with pelvic fracture than in those without, although still rare (1.4%, compared with 0.2%).
How Dangerous Are Pelvic Injuries?
Mortality in patients with pelvic fractures is high—13.5% in adults in one large study. However, only about 0.8% of deaths are directly attributed to pelvic injuries. These are high-energy injuries that frequently coexist with severe injuries to the head, chest, abdomen, spine, and extremities. When pelvic injuries are noted on imaging studies, careful attention should be given to determining the presence of other injuries.1 The low mortality directly attributed to pelvic injuries should not suggest that these injuries themselves are unimportant. This low mortality is achieved when patients are treated at major trauma centers and receive aggressive therapy for pelvic injuries, including blood transfusion, orthopedic fixation, and angiographic embolization of pelvic vascular injuries. In one study, 38.5% of pelvic fracture patients received blood transfusion, with a mean transfusion of nearly 1 L.1 In severe pelvic fracture patients, 60.6% received transfusion, with a mean of more than 3.5 L. When severe pelvic injury was the only significant injury, more than 50% received transfusion, with a mean of 2.7 L. Overall, 16.6% of pelvic fracture patients required more than 2 L of blood in transfusion. Angiography (discussed in detail in Chapter 16) was performed in 4.7% of patients with pelvic injuries, and therapeutic embolization was performed in 2.3%, or half of those undergoing angiography.
Pelvic X-ray and Computed Tomography Techniques
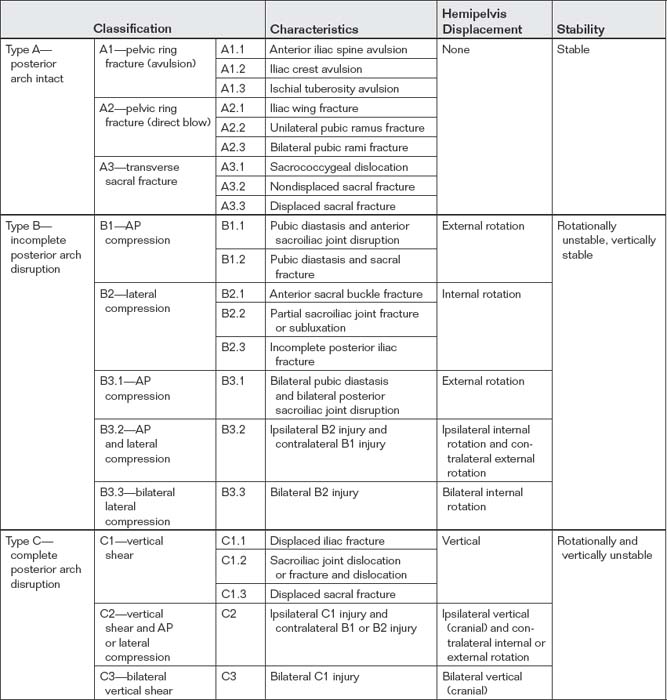
The routine initial view of the pelvis is the anterior–posterior (AP) x-ray (Figure 13-1). This image is obtained with the patient supine and the x-ray beam oriented 90 degrees to the patient’s long axis, passing through the patient from anterior to posterior. Additional plain films can be obtained when injuries are seen on the AP image or if occult injuries are suspected with a normal AP view. These include oblique (Judet) views for characterization of acetabular fractures (Figure 13-2), and inlet and outlet views for characterization of pelvic ring fractures (Figure 13-3). Inlet views are obtained with the patient supine and the x-ray tube positioned at the patient’s head, angled 45 degrees toward the patient’s feet. This allows assessment of pelvic brim integrity, AP displacement of the hemipelvis, internal or external rotation of the hemipelvis, and anterior displacement of the sacrum. Outlet views are also obtained with the patient supine, with the x-ray tube at the patient’s feet and angled 45 degrees toward the head. This provides an excellent view of the sacrum, which is perpendicular to the x-ray beam in this position. The sacral neural foramina are seen well in this view, and vertical displacement of the hemipelvis may be evident. These additional views may be unnecessary if CT of the pelvis is planned, particularly if multiplanar two-dimensional images or three-dimensional models can be constructed, which depends on local software. Most modern picture archiving and communication system (PACS) software allows multiplanar two-dimensional reconstructions from multidetector CT image data, and three-dimensional capability is becoming routine. Three-dimensional reconstruction (Figure 13-4) depends on high-quality original image data but is otherwise a postprocessing function and does not require a different CT protocol during the image acquisition phase.
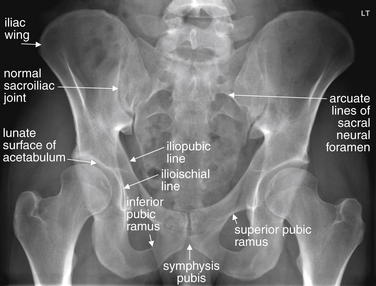
Figure 13-1 The normal anterior–posterior pelvis.
This normal pelvis x-ray is from a 24-year-old with no history of direct trauma. Normal findings are labeled. Patients commonly have subtle asymmetry from right to left. Overlying bowel gas frequently hides portions of the bony pelvis, and you will have to make careful judgments about abnormal lucency indicating fracture versus overlying gas.
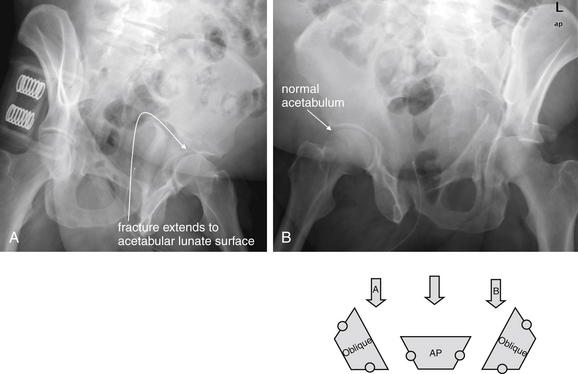
Figure 13-2 Oblique (Judet) views of the pelvis for evaluation of the acetabulum.
Oblique (Judet) views of the pelvis are useful for evaluation of the acetabula for fractures. The patient is rolled onto the left and right side at a 45-degree angle, which isolates the hemipelvis and acetabulum, removing posterior pelvic structures from the x-ray path. This provides an en-face view of the dependent iliac wing and places the acetabular lunate surface in relief, preventing overlap by other lines that may simulate or obscure fractures. In this patient, an obvious left acetabular fracture is present, but more subtle fractures may be revealed by this technique. A, An oblique view with left hip in dependent position (called LPO for left posterior oblique) allows evaluation of the left acetabulum. B, An oblique view with right hip in dependent position (called RPO for right posterior oblique) allows evaluation of the right acetabulum. The schematic shows the position of the pelvis relative to the x-ray tube (block arrow).
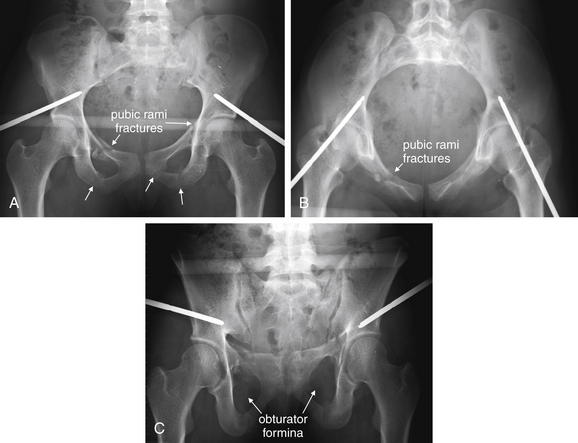
Figure 13-3 Inlet and outlet views of the pelvis for evaluation of pelvic ring fractures.
This patient has fractures of the bilateral superior and inferior rami and a vertical sacral fracture seen on computed tomography (arrows in panel A). An external fixator has been placed. A, Standard anterior–posterior (AP) view for comparison. B, The inlet view reveals the pelvic ring in detail, allowing assessment of pelvic brim integrity, AP displacement of the hemipelvis, internal or external rotation of the hemipelvis, AP displacement of the sacrum, and AP displacement of pubic rami fractures. C, The outlet view provides a good view of the sacrum, which is perpendicular to the x-ray beam in this position. The sacral neural foramina are seen well in this view, and vertical displacement of the hemipelvis may be evident when present. The obturator foramina are also seen well in this view.

Figure 13-4 Three-dimensional computed tomography (CT) reconstruction of the pelvis.
CT images can be reconstructed in three dimensions using postprocessing software. These CT images were created using axial images from a standard CT scan with intravenous contrast performed for the evaluation of trauma. The patient has a right posterior hip dislocation (A), more evident a posterior view of the pelvis (B), where the femoral head is exposed rather than hidden within the acetabulum. The acetabulum is also fractured posteriorly. While this model is of high quality, a stair-step pattern is visible in the pelvis because of the relatively thick two-dimensional slices used to reconstruct the three-dimensional model. Higher-quality models can be rendered when thinner slices are acquired during CT. Models can be rotated in three dimensions, and structures can be digitally removed. The aorta, inferior vena cava, and iliac arteries and veins have intentionally been left visible to emphasize the potential for vascular injuries when bony pelvic injuries occur.
Fracture detection with CT does not require the administration of IV or oral contrast. However, in most cases, IV contrast is given because the pelvic CT is obtained with the abdominal CT for detection of visceral injury. IV contrast allows recognition of active bleeding from pelvic vascular structures. Oral contrast is often not administered in the setting of trauma because it has little impact on diagnosis of bowel injuries (see the chapter on imaging of abdominal trauma, Chapter 10). A single CT scan of the pelvis can provide information about both soft-tissue and bony injuries. Urinary tract injuries require special CT techniques for diagnosis, as mentioned later and explored in more detail in the chapter on genitourinary imaging (Chapter 12). When more detail of fractures is needed, fine-cut, dedicated “bony pelvis” CT can be performed without contrast, although not all injuries mandate this. In the past, dedicated bony pelvis CT was often obtained to characterize pelvic fractures in greater detail when fractures were seen on body CT performed for evaluation of visceral injury. Today, thin-slice multidetector body CT images offer good resolution of fractures, and bony pelvis CT may not be routinely required. CT images can be reconstructed in three dimensions for further characterization of fractures and dislocations (see Figure 13-4).
Interpretation of the Pelvic X-ray
The bony pelvis is a ring structure in which isolated fractures are rare. When reviewing a pelvic x-ray, detection of a single break in the ring mandates search for a second injury. Certain injury patterns are common, and detection of one component of a pattern logically guides your evaluation for the remaining components of the injury. In the figures that follow, a number of frequently encountered fracture patterns are described and illustrated. Figure 13-1 shows a normal pelvis x-ray with labels. Figures 13-5 to 13-19 show common patterns of injury schematically, with displaced fragments highlighted in dark gray. These injuries are also shown in actual x-rays and CTs in the figures that follow. In many cases, multiple injury types are present, so review the schematics first to understand the simplified key features of isolated injuries. Table 13-1 lists the injury patterns and associated figures in this chapter.
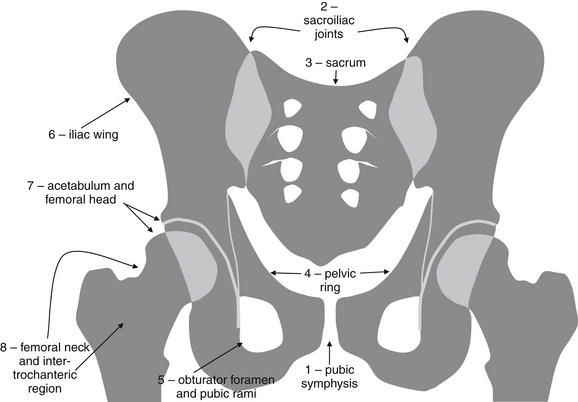
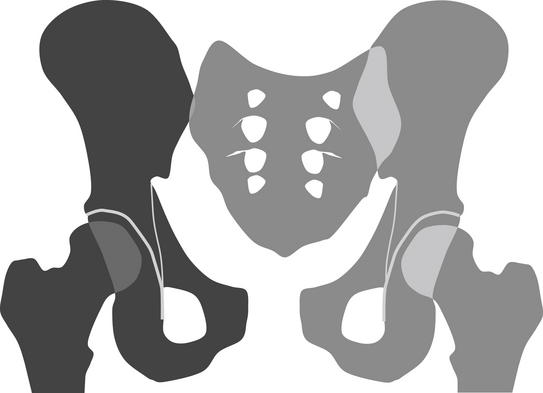
Figure 13-5 The normal pelvis.
This schematic shows a normal pelvis. When reviewing a pelvis x-ray, take the following steps.
This schematic of an open-book pelvis shows separation of the pubic symphysis and right sacroiliac joint. Diastasis of the pubic symphysis, combined with either diastasis of one or both sacroiliac joints or fractures of the pelvis ring, allows the pelvis to “open” anteriorly, with a hinge joint posteriorly. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
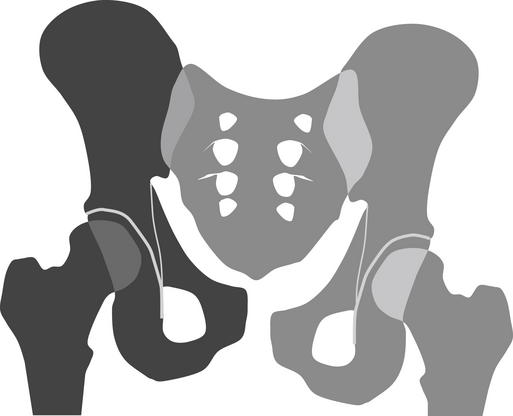
Figure 13-7 Vertical shear injury.
Vertical shear can separate the pubic symphysis and sacroiliac joints in a cephalad–caudad direction. Alternatively, fractures may occur vertically, allowing vertical offset of the pelvis. In this schematic, the right sacroiliac joint and pubic symphysis are diastatic. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
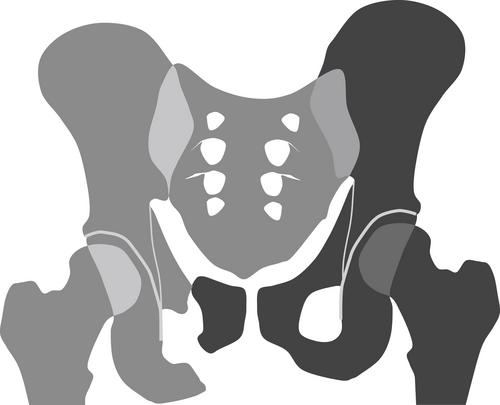
Figure 13-8 Pubic ramus fractures with vertical shear: Bucket-handle pattern.
When pubic rami fractures and sacroiliac joint diastasis are contralateral, a bucket-handle pattern is present. In this schematic, the right pubic rami are fractured, and the left sacroiliac joint is diastatic. Because the pubic symphysis is intact, the left pelvis carried the small right pubic fragment with it in its cephalad migration. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
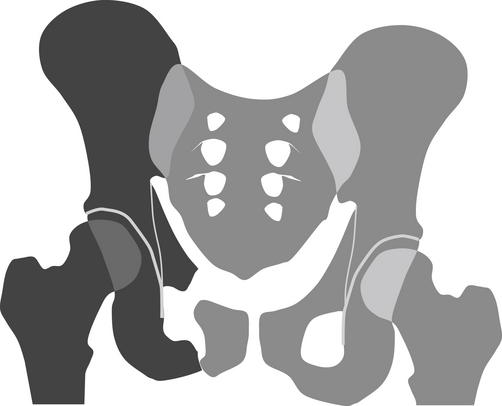
Figure 13-9 Pubic ramus fractures with vertical shear: Malgaigne pattern.
When pubic rami fractures and sacroiliac joint diastasis (or sacral fracture) are ipsilateral, a vertical shear injury called a Malgaigne fracture is present. A common mechanism is landing from height on an outstretched leg. In this schematic, the right sacroiliac joint is diastatic and the right pubic rami are fractured. Because the pubic symphysis is intact, the small right pubic bone fragment remains attached to the left pelvis, whereas the entire right pelvis moves cephalad. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
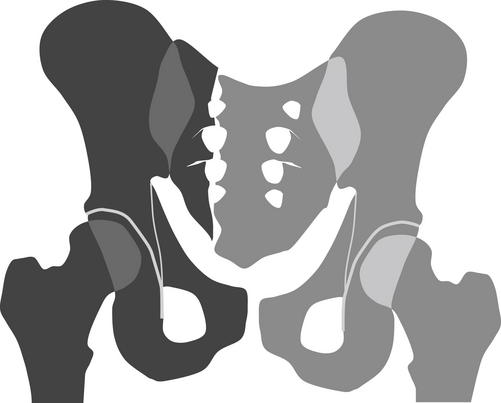
Figure 13-10 Sacral fractures.
Sacral fractures may occur in isolation or with other fractures. Vertical sacral fractures can occur with vertical pelvic shear, and commonly other fractures or diastasis of the pubic symphysis are seen. Transverse fracture of the sacrum may be seen in isolation and may not compromise the integrity of the pelvic ring. In this schematic, a vertical sacral fracture is depicted with vertical offset of the pubic symphysis. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
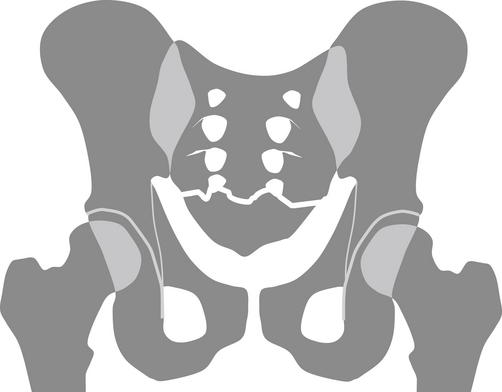
Figure 13-11 Transverse sacral fracture.
Transverse sacral and coccygeal fractures may occur with little clinical consequence because they do not affect the structural integrity of the pelvic ring. Transverse sacral fractures may intersect sacral nerve foramen, with potential for nerve injury. In this schematic, a transverse sacral fracture is depicted intersecting sacral foramen.
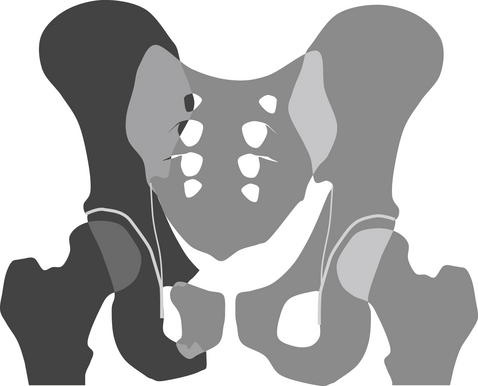
Figure 13-12 Lateral compression of the pelvis.
Lateral compression of the pelvis can disrupt the pelvic ring anteriorly and posteriorly. Commonly, one sacroiliac joint folds inward, although sacral or iliac wing fractures may occur. Anteriorly, pubic rami fractures are common, as well as disruptions of the sacroiliac joint. In this schematic, the right sacroiliac joint has folded inward and the right superior and inferior pubic rami have fractured. The darkened region indicates the portion of the pelvis that has become traumatically displaced.
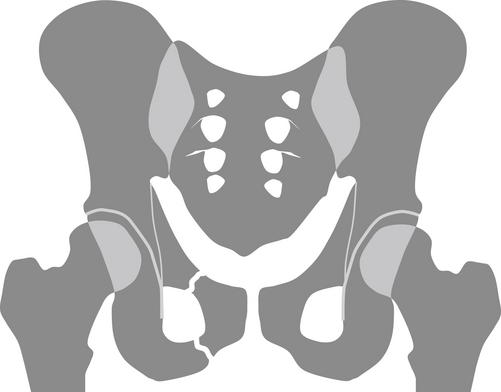
Figure 13-13 Pubic ramus fractures.
Pubic ramus fractures, as in this schematic, either occur singly or involve the superior and inferior pubic rami. Usually, a single fracture occurs only if minimally displaced. An offset of a single fracture usually creates tension in the pelvic ring that is relieved through a second fracture or diastasis of a joint.
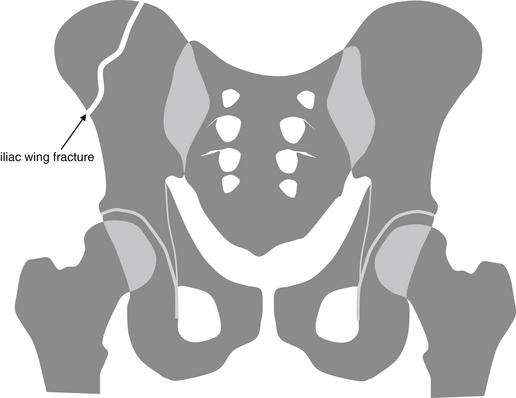
Figure 13-14 Iliac wing fracture.
Inspect the iliac wings for fractures. Overlying bowel gas may create rounded lucencies overlying the iliac bones, whereas linear lucencies are more suggestive of fracture. Follow lucencies to determine whether they intersect the outer border of the iliac bones, which should be smooth continuous curves without cortical step-offs.
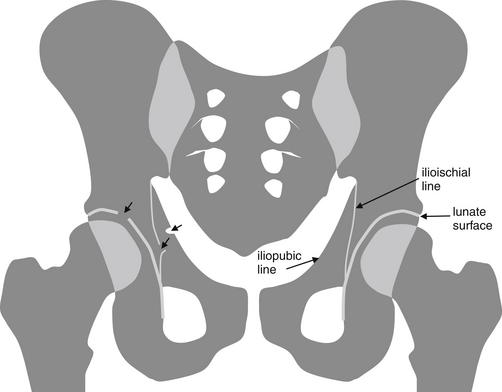
Figure 13-15 Acetabular fractures.
Acetabular fractures can be subtle on x-ray and are best diagnosed by computed tomography. Clues to the diagnosis are disruptions of the iliopubic line, which forms the medial border of the anterior column of the acetabulum; disruption of the ilioischial line, which forms the medial border of the posterior column of the acetabulum; and disruptions of the articular surface of the acetabulum, called the lunate surface. In this schematic, defects in each of these lines are shown by short arrows on the patient’s right, whereas the patient’s left side is normal. In an actual x-ray, fracture fragments may or may not be visible.
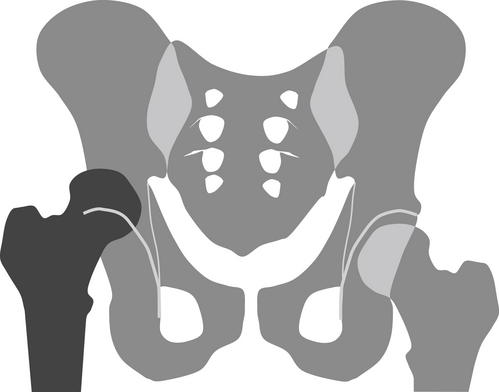
Figure 13-16 Posterior hip dislocation.
Hip dislocation most frequently occurs in a posterior direction, with a common scenario being anterior-posterior force directly against a flexed and adducted hip in a seated patient in a vehicle collision. If the hip is abducted at the moment of impact, anterior dislocation sometimes occurs. Once dislocated posteriorly, as in this schematic, the femur is usually pulled cephalad by hip flexors. The darkened region indicates the traumatically dislocated hip.
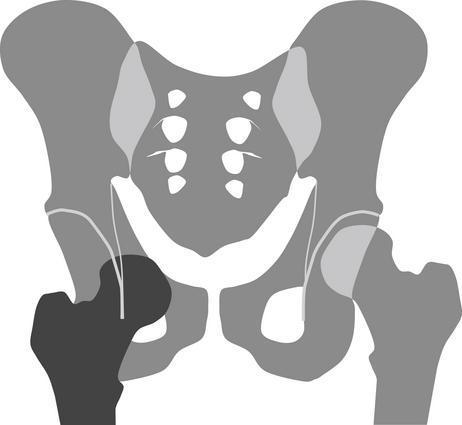
Figure 13-17 Anterior hip dislocation.
Anterior hip dislocation, shown in this schematic, is less common than posterior dislocation but may position the femoral head medially relative to the acetabulum. The darkened region indicates the traumatically dislocated hip.
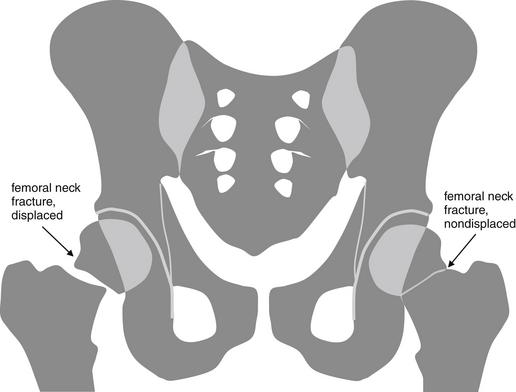
Figure 13-18 Femoral neck (hip) fracture.
Fractures of the femoral neck can be overt or subtle. Often, these occur in older patients with osteopenia, making cortical and trabecular abnormalities more difficult to see. In this schematic, an obvious fracture is diagrammed on the right, whereas a more subtle fracture is depicted on the left. Sometimes all that is seen is a faint band of increased density in nondisplaced fractures. Magnetic resonance imaging, computed tomography, or bone scan can clarify equivocal fractures.
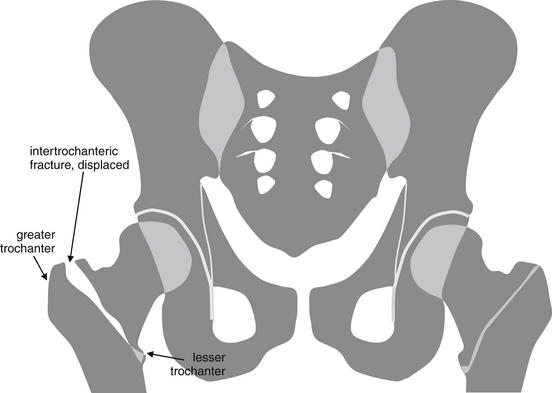
Figure 13-19 Intertrochanteric femoral (hip) fracture.
Intertrochanteric hip fractures are a common form of fracture in patients over the age of 65 years, with relatively minor mechanisms of injury, such as falls from standing, predominating. As the name suggests, they typically run between the greater and the lesser trochanters. They may be comminuted and displaced. Sometimes, these fractures are more subtle and require magnetic resonance imaging, computed tomography, or bone scan for confirmation. In this schematic, an overt intertrochanteric fracture is depicted on the patient’s right, with a more subtle abnormality on the left.
TABLE 13-1 Guide to Figures in This Chapter
| Content | Figure Number |
|---|---|
| Approach to pelvic image interpretation | |
| 13-1, 13-5 | |
| 13-2 | |
| 13-3 | |
| 13-4 | |
| 13-5 to 13-19 | |
| Pelvic ring pathology | |
| 13-6, 13-20 to 13-30 | |
| 13-7 to 13-10, 13-36 to 13-41 | |
| 13-12, 13-31 to 13-35 | |
| 13-38 | |
| 13-8, 13-9, 13-12, 13-13, 13-31, 13-33, 13-39, 13-40, 13-44, 13-51, 13-55 to 13-57 | |
| 13-10, 13-11, 13-40, 13-41, 13-52 to 13-54 | |
| 13-14, 13-28, 13-31, 13-32, 13-43 | |
| 13-42 | |
| 13-30 | |
| Injuries of the hip | |
| 13-15, 13-28, 13-29, 13-43 to 13-46, 13-48 to 13-50, 13-62, 13-64, 13-65 | |
| 13-4, 13-16, 13-62 to 13-65 | |
| 13-17, 13-34, 13-66, 13-67 | |
| 13-68 | |
| 13-18, 13-69, 13-70 | |
| 13-19, 13-71 | |
| 13-72, 13-73 | |
| 13-74 | |
| Low-mechanism pelvic injuries | |
| 13-58 | |
| 13-59 | |
| 13-60, 13-61 | |
| 13-75, 13-76 | |
| 13-77 to 13-79 |
We begin with the normal AP pelvis x-ray (labeled, see Figure 13-1). Each structure examined on x-ray should also be reviewed when interpreting CT scan. Stepwise inspection of the AP pelvic x-ray should include evaluation of the following (see Figure 13-5):
Patterns of Pelvic Injury
Fractures of the pelvis can range from innocuous, requiring no treatment, to immediately life threatening. Their appearance on x-ray can be subtle or overt, and the emergency physician must be able to recognize key injuries immediately to take appropriate stabilization measures, plan interventions such as angiographic embolization, consider additional imaging, and arrange safe disposition. We examine a number of common fracture patterns, recognizing that often a mixture of injury patterns may be present in the same patient.
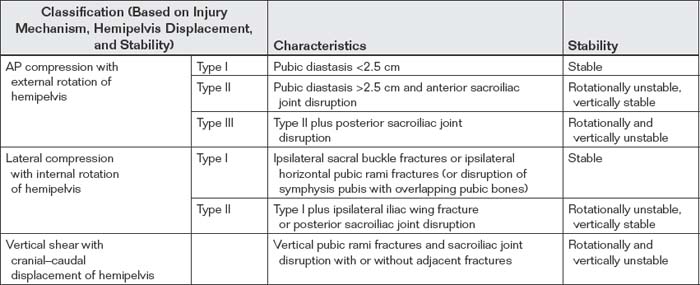
Two major systems of classification of pelvic fractures are the Young-Burgess classification and the Tile classification systems (Tables 13-2 and 13-3). The Young-Burgess classification2 describes injuries in terms of mechanism and type of injury, direction of hemipelvis displacement, and stability. The Tile classification3 divides fractures into three main categories, each with multiple subtypes, including stable fractures with an intact posterior arch (type A), unstable anterior and lateral compression fractures with incomplete disruption of the posterior arch (type B), and vertical shear injuries with complete disruption of the posterior arch (type C). While these are useful for orthopedists in surgical planning, emergency physicians can understand injuries and communicate them clearly to specialty colleagues with simple descriptions, based on recognition of several common injury patterns.
Two primary categories of injury should be considered from an emergency medicine perspective: fractures that disrupt the major pelvic ring and those that do not. Fractures that compress or open the pelvis ring can disrupt blood vessels passing through the pelvis. In addition, because they change the geometry of the pelvis from a stable cone with a fixed volume to an expandable structure with the ability to increase in size, substantial bleeding can occur in the pelvis from these fracture types. Identification of a fracture in this group should prompt pelvic stabilization, preparation for potentially massive transfusion, and consideration of angiographic embolization. Fractures that do not affect the pelvic ring in this way can be important for other reasons, but rarely are they as immediately life-threatening. For example, fractures near the pubic symphysis involving the inferior or superior pubic rami may be associated with bladder and urethral injuries, as well as vaginal lacerations in female patients. Acetabular fractures, while associated with disability from posttraumatic arthritis, do not pose an immediate life-threat to the patient.
Forces That Disrupt the Major Pelvic Ring
Fractures that affect the stability of the pelvic ring can be subcategorized in several additional ways—for example, by mechanism of injury. In theory, fractures that compress the pelvic ring laterally may be less likely to stretch and tear vascular structures, compared with structures that involve AP compression, opening the pelvis at the pubic symphysis and sacroiliac joints. Vertical shear injuries to the pelvis may disrupt vascular structures and result in damage to nerve roots at the level of the sacrum. Important pelvic ring disruptions involve fractures or diastasis of joints at two or more sites of the anterior and posterior pelvic arcs. Separation of the pubic symphysis and diastasis of the sacroiliac joints can cause pelvic ring disruption in the absence of a fracture. Two or more fractures can also result in pelvic ring disruption. A combination of one fracture and one diastatic joint may also occur. Because the bony pelvis is a ring, a single disruption usually does not occur; rather, a disruption in one location results in fracture or diastasis at a second point in the ring. When one disruption in the pelvis ring is seen, a second should be suspected and sought. Sometimes the second disruption is at the pubic symphysis or sacroiliac joint and may be unapparent on x-ray because these joints can open and close with repositioning of the patient once the joint has been destabilized.
Anterior-posterior compression injuries
AP compression of the pelvic ring typically separates the pubic symphysis anteriorly while opening the sacroiliac joint posteriorly (Figures 13-20 to 13-30; see also Figure 13-6). This fracture pattern is often called an open-book pelvic fracture and can be a life-threatening injury. It results from substantial force and can shear pelvic veins and arteries. Significant bleeding into the pelvis often occurs with this injury. Because this injury increases the volume of the potential space within the pelvis, tamponade of bleeding does not occur, and the patient’s entire blood volume can be accommodated within the pelvis. When this injury is recognized on x-ray or on CT scan, the pelvis should be closed using some type of external compression device. Urethral injuries are also associated with this type of pelvic injury. Evaluation of urethral injury is discussed in detail in the chapter on the genitourinary system (Chapter 12).
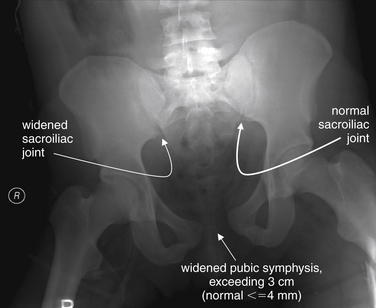
Figure 13-20 Open-book pelvis.
This patient has substantial widening of the pubic symphysis without an evident fracture. Given the usual stability of the pelvic ring, there must be at least one additional point of motion to allow the pelvic ring to open to this degree. The most likely locations in the absence of fracture are one or both sacroiliac joints. Look carefully at the right sacroiliac joint, which appears wide compared with the left. Compare with Figure 13-21, showing the patient’s pelvis minutes later—after application of an external binder—and with the computed tomography that follows in Figure 13-22. How much force is required to open the pelvis? This patient also suffered an aortic tear and diaphragm rupture. He was a Jehovah’s Witness, refused blood transfusion, and expired.
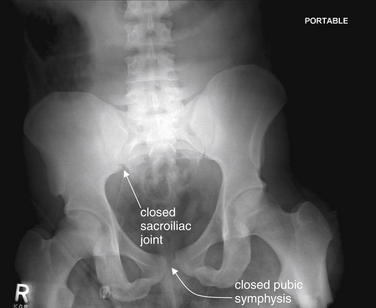
Figure 13-21 Open-book pelvis.
Same patient as in Figure 13-20 and 13-22. An external pelvic binder has been applied, and the right sacroiliac joint has flexed closed, in turn closing the pubic symphysis. Compare with Figure 13-20. This x-ray looks essentially normal—beware of unstable pelvis diastasis that can be missed on x-ray if external pelvic stabilization has been performed.
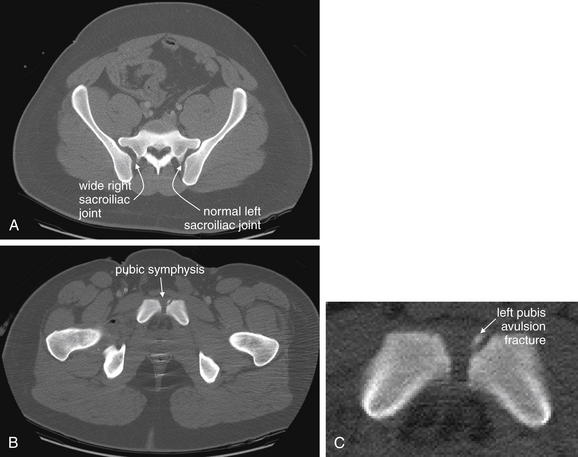
Figure 13-22 Open-book pelvis.
Same patient as in Figures 13-20 and 13-21. What are the CT findings of an open-book pelvis injury? Remarkably, in this patient with an apparent open-book pelvis on initial x-ray, the external binder has closed the pelvis almost completely. The patient’s pelvis injury is primary ligamentous, affecting the pubic symphysis and right sacroiliac joint, with no significant fractures. A, The right sacroiliac joint continues to look slightly widened. B, The pubic symphysis is normal in appearance, with the exception of a tiny avulsion fracture from the left pubis. C, Close-up from B.

Figure 13-23 Pelvic ring disruption.
This 20-year-old female was near term in her pregnancy when she was pinned in a motor vehicle collision. In the emergency department, her pelvis was found to be unstable and ultrasound showed fetal bradycardia. An emergency Cesarean section was performed in the trauma bay. Once the fetus was delivered, this x-ray was performed, showing a dramatically open pubic symphysis.
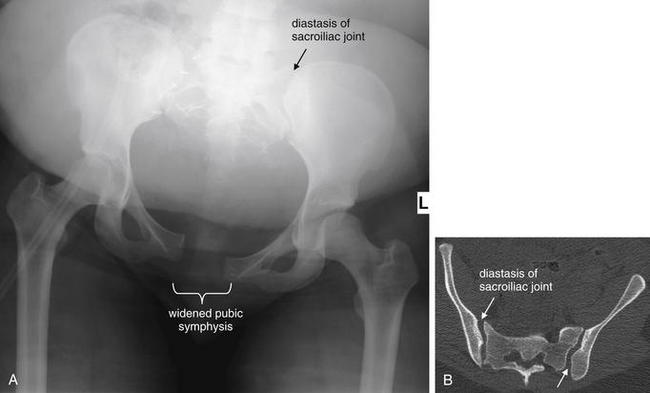
Figure 13-24 Open-book pelvis.
A, Another x-ray from the same patient as in Figure 13-23 shows persistent dramatic diastasis of the pubic symphysis despite an external stabilizer. The sacroiliac joints are diastatic (compare with CT in B). Remarkably, no other fractures were present. The patient had surgical fixation performed (Figure 13-25).
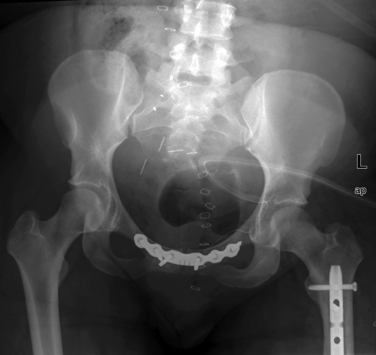
Figure 13-25 Open-book pelvis after fixation.
Same patient as in Figures 13-23 and 13-24 after stabilization of the pubic symphysis.
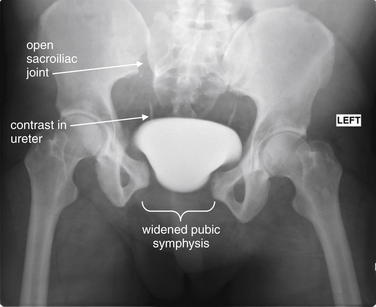
Figure 13-26 Pelvic ring disruption.
This patient has an open pubic symphysis and complete disruption of the right sacroiliac joint. The left sacroiliac joint also appears wide. Contrast material is seen in the bladder and both ureters from computed tomography performed at an outside hospital before transfer to the trauma center. Pelvic stabilization with an external binder could have been helpful in this patient to contain the pelvic volume and limit bleeding.
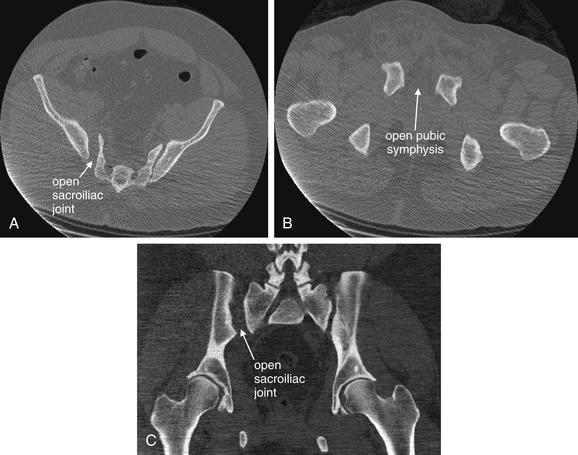
Figure 13-27 Open-book pelvis.
CT images, bone windows. This patient has complete separation of the right sacroiliac joint and marked diastasis of the pubic symphysis. Remarkably, no other pelvic fractures are present. A large hematoma is present anterior to the pubic symphysis. Was this pelvis stable on examination? Naturally, it should not have been, but 10 cm of soft tissue separates the skin surface from the iliac crest. The examination may have been difficult to interpret. A, B, Axial views. C, Coronal view.

Figure 13-28 Pelvic ring disruption with sacroiliac joint diastasis and iliac wing fracture.
Both sacroiliac joints are widened, the right more so than the left. The left iliac bone has fractured transversely with extension into the left acetabulum. This likely resulted from significant anterior–posterior compression of the pelvis. Compare with the CT in Figure 13-29.
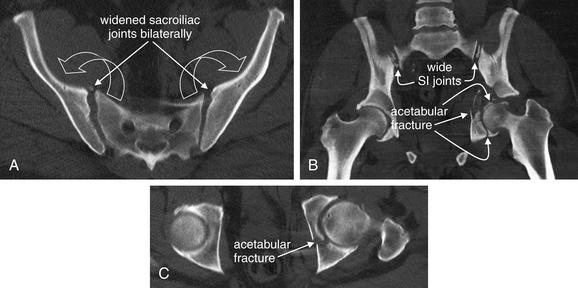
Figure 13-29 Widened sacroiliac joints and iliac wing fracture involving left acetabulum.
CT, bone windows. Again, take a moment to appreciate the sacroiliac joint widening on CT, and look again at the x-ray from the same patient in Figure 13-28. The iliac wing fracture is impressive, but sacroiliac joint diastasis is also a significant contributor to the instability of this pelvis, which has open-book characteristics, although the pubic symphysis appears narrow. A, Axial CT reconstruction showing bilateral sacroiliac joint diastasis. Imagine the two iliac wings as the covers of a book being opened. Anterior–posterior compression of the pelvis can have this effect. B, Coronal CT reconstruction. The wide sacroiliac joints are still visible. This image suggests a competing or additional mechanism of injury: lateral compression applied to the left pelvis. The femoral head has been driven like a hammer into the acetabulum, fracturing the medial wall and pushing it medially into the pelvis. C shows this in axial section.
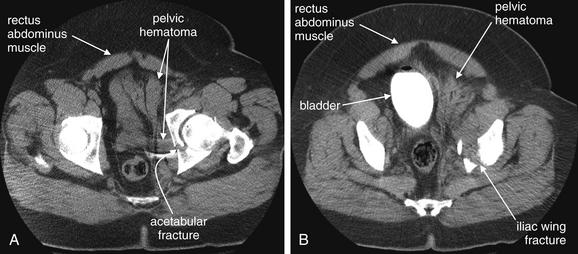
Figure 13-30 Soft-tissue injuries associated with pelvic fractures.
CT with IV contrast, soft-tissue windows. These images are in fact taken from the same scan as in Figure 13-29, but displayed using a different window setting. CT offers the ability to assess both bony and soft-tissue injuries. A, Soft-tissue injuries of the bladder and pelvic blood vessels are discussed in more detail in the genitourinary and abdominal trauma sections. However, recognize that it is the hemorrhage associated with major pelvic fractures that can make them an immediate life threat. The large pelvic sidewall hematoma is associated with the iliac fracture shown in Figure 13-29. On soft-tissue windows, this hematoma is the same intermediate gray as the rectus abdominus muscles. B, The hematoma displaces the bladder (filled with contrast).
Lateral compression injuries
Lateral compression of the pelvis may result in a posterior injury in which the sacroiliac joint on the affected side folds inward or the iliac wing or sacrum fractures (Figures 13-31 to 13-35; see also schematic Figure 13-12). Often, the posterior injury is matched anteriorly by fractures of the superior and inferior pubic rami or pubic symphysis (see Figures 13-31 and 13-33). Again, injury to the urethra may occur, and vaginal penetrating injuries may be sustained in female patients—consider these injuries when pubic rami fractures are present. A vaginal exam should be performed to evaluate for laceration. Bladder injuries are also possible with this fracture pattern. Serious pelvic bleeding is somewhat less common with this injury pattern because pelvic blood vessels are folded rather than stretched and sheared. The volume of the pelvis may be decreased, contributing to tamponade effect that may limit bleeding. Nonetheless, this is an extremely high-energy injury, frequently associated with other injuries to the head, chest, abdomen, spine, and extremities. Vascular injury should be considered as a possible complication.
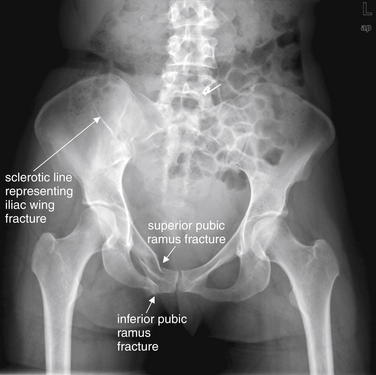
Figure 13-31 Iliac wing fracture with superior and inferior pubic rami fractures.
This young female was involved in a motor vehicle collision. As is frequently the case, an injury to one portion of the pelvis is accompanied by a second injury in this patient. Deformation in one part of the pelvic ring builds tension elsewhere, which is relieved by fracture or joint diastasis. Two separate types of injuries are visible here, one obvious and the second more subtle. First, the right superior and inferior pubic rami are fractured and deformed. Compare with the normal left side. Second, a fine sclerotic line crosses the right iliac wing—a fracture line. An isolated fracture of a single iliac wing is called a Duverney fracture. These fractures do not disrupt the pelvic ring, though hemorrhage may occur from injury to vessels hugging the iliac bone, particularly the internal iliac arteries. Compare with the CT in Figure 13-32.
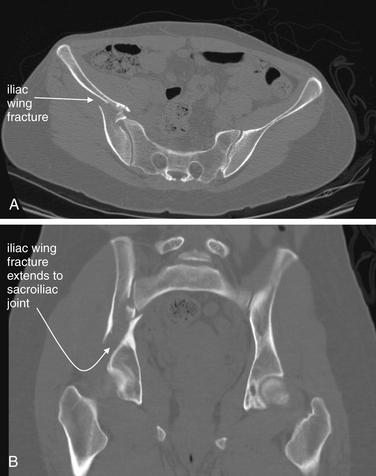
Figure 13-32 Iliac wing and pubic rami fractures.
Same patient as in Figure 13-31. This CT viewed with bone windows shows a fairly dramatic right iliac wing fracture. The sacroiliac joint itself appears intact on the axial view (A), but in the coronal reconstruction (B) the fracture appears to extend to the right sacroiliac joint. How could this be so plain on CT yet so subtle on x-ray? Although the fracture is complete, the fragments are not fully distracted from one another, and on a frontal projection they overlap and are nearly invisible. Additional x-ray views such as inlet and outlet views could throw these into relief, but in the trauma patient, CT is the preferred modality because it can simultaneously evaluate internal soft-tissue injuries.

Figure 13-33 Pubic ramus fractures.
Same patient as in Figure 13-31 and 13-32. These CT images show the pubic ramus fractures in more detail. A, Axial view. B, Coronal reconstruction. This injury alone would not significantly affect the stability of the pelvic ring.
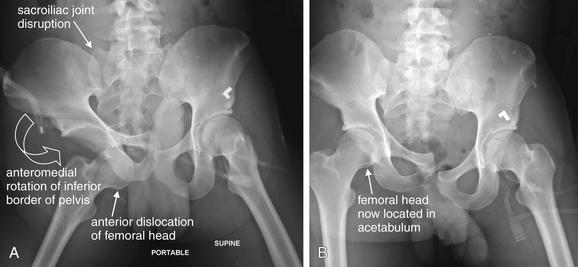
Figure 13-34 Pelvic ring disruption with sacroiliac and symphysis pubis disruption, as well as anterior hip dislocation.
This patient has complete separation of the right sacroiliac joint, as well as disruption of the symphysis pubis. A, The right hip is dislocated anteriorly. The right hemipelvis has rotated in an anterior, as well as a medial, direction. B, The right hip has been reduced, and the anterior rotation of the hemipelvis is somewhat reduced. Compare with the CT in Figure 13-35.
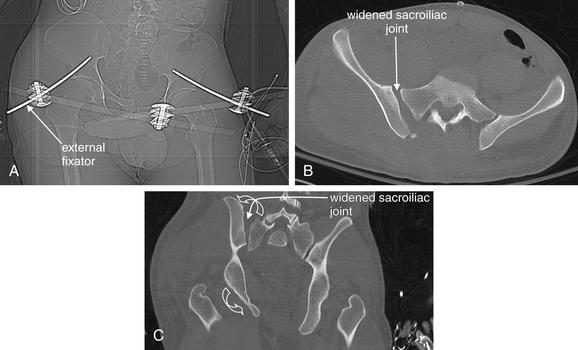
Figure 13-35 Unstable pelvis with complete diastasis of right sacroiliac and symphysis pubis joints.
A, The CT scout image shows an external fixator has been placed, with fixators placed into the ischium. B, An axial image shows widening of the right sacroiliac joint. C, A coronal image shows a wide right sacroiliac joint with medial angulation of the lower right hemipelvis. The right pelvis has rotated counterclockwise on the fulcrum of the lower right sacroiliac joint (open curved arrows). B and C, Bone windows.
Vertical shear injuries
Vertical shear injuries are also a common injury pattern (Figures 13-36 to 13-41; see also schematic Figures 13-7 to 13-10). These may occur with falls from great height or deceleration injuries with a single outstretched leg, which distributes force asymmetrically to the pelvis. The pelvic ring is disrupted at a posterior and an anterior location, commonly one sacroiliac joint posteriorly and the pubic symphysis anteriorly. Alternatively, the sacrum or the pubic rami may fracture vertically. Spinal and lower extremity injuries are common with pelvic vertical shear injuries.
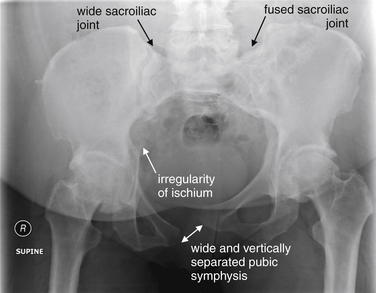
Figure 13-36 Vertical shear injury.
This patient presented with chronic pain after a pelvic fracture 20 years earlier. Her x-ray shows a markedly abnormal pelvis, with a horizontally widened and vertically distracted pubic symphysis. The left sacroiliac joint is obscured, and the left iliac wing appears to be riding somewhat high in relationship to the sacrum. Her original injury was probably a vertical shear injury along the left sacroiliac joint, which fused long ago in this abnormal position. The right sacroiliac joint appears widened. The right ischium and pubic bone are irregular along their medial border, likely indicating an old fracture. Compare with the CT in Figure 13-37.
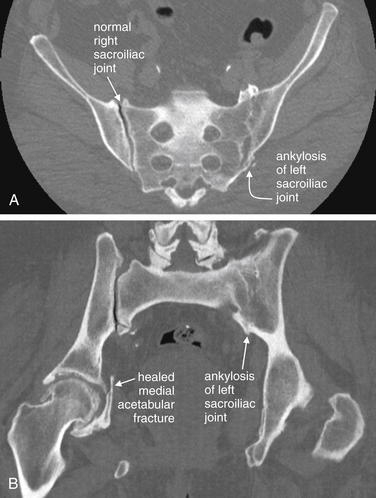
Figure 13-37 Old sacroiliac joint injury.
CT, bone windows. Same patient as in Figure 13-36. A, An axial image shows a normal right sacroiliac joint but an abnormal left sacroiliac joint with ankylosis. B, The coronal view also shows this sacroiliac joint abnormality. The right acetabulum does have an old healed fracture, as suggested on the x-ray in Figure 13-36.
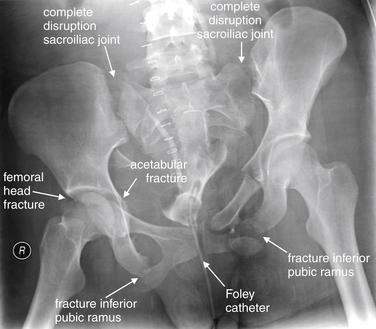
Figure 13-38 Pelvic ring disruption.
This patient has remarkable disarticulation of the pelvic ring—sometimes called a “sprung pelvis.” The bilateral sacroiliac joints have separated completely, leaving the sacrum and lumbar spine free of the iliac wings. The bilateral inferior pubic rami have displaced fractures. The right femoral head is fractured, associated with a fracture of the medial wall and anterior column of the right acetabulum. The left acetabulum also has a fracture through its anterior column at the junction with the superior pubic ramus. Is any portion of the pelvis intact? The pubic symphysis is not diastatic because tension in the pelvic ring was dissipated through other fractures and disruption of the sacroiliac joints. This x-ray was taken after other emergency interventions. The patient has a Foley catheter in place, and some contrast is seen in the bladder and right ureter. Skin staples are also visible. Packing material is visible overlying the lower pelvis.

Figure 13-39 Pubic symphysis fracture with pelvic ring disruption. This 30-year-old female experienced a vertical shear and lateral compression injury in a horse-riding accident. She has a comminuted fracture of the right medial pubic bone. Be wary of fractures in this region. This was an open fracture, with lacerations extending into the patient’s vagina. Fractures near the pubic symphysis should raise consideration of vaginal and urethral injuries. The orientation of the right pelvis does not match that of the left; the right pubic bone points obliquely down, compared with the nearly horizontal position of the left pubic bone. Another pelvic injury must exist that has not yet been identified. Is it diastasis of one or both sacroiliac joints? Bowel gas obscures these regions and the sacrum. Computed tomography (Figure 13-40) reveals the answer.
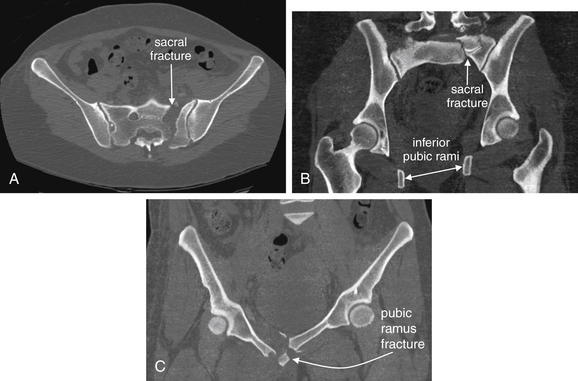
Figure 13-40 Sacral fracture with pubic rami fractures.
Same patient as in Figure 13-39. CT viewed on bone windows reveals the explanation for the odd orientation of the right pelvis relative to the left on the previous x-ray. A complete vertical fracture through the left sacrum is present. The sacroiliac joints are intact. A, Axial view. This fracture is seen running nearly in a perfect anterior–posterior direction, separating the left ilium and a piece of the sacrum from the bulk of the sacrum and right pelvis. B, Coronal reconstruction. The left pelvis and attached sacral fragment are seen to be displaced vertically compared with the right pelvis—accounting for the x-ray appearance. Note the relative positions of the right and left femoral heads and inferior pubic rami. The entire left pelvis and femur have moved cephalad relative to the right. The left femoral neck is not visible; this is not a fracture but simply the result of the plane of this slice not intersecting the femoral neck. C, Coronal view. The pubic rami fractures are again seen. This is a bucket-handle type injury pattern, with vertical shear through contralateral injury sites.

Figure 13-41 Pelvic ring disruption.
In this patient, the pubic symphysis is widened, and the left pubic symphysis is positioned cephalad relative to the right. No other fractures or disruptions are seen on this x-ray, although you will recognize by now that an isolated disruption of the pelvic ring is extremely unlikely. If no other fractures are present, a discontinuity through the sacroiliac joint is likely. Not surprisingly, CT showed a similar left sacral fracture to the one explored in Figure 13-40.
While blunt mechanisms are the most frequent cause of serious pelvic trauma, penetrating trauma can also result in severe pelvic injury; Figure 13-42 shows an open pediatric pelvic injury resulting from a riding lawn mower.
Fractures That Do Not Disrupt the Major Pelvic Ring
Fractures that may not affect the stability of the pelvic ring include sacral transverse fractures (Figures 13-52 to 13-54; see schematic Figure 13-11), some lateral iliac wing fractures (see schematic Figure 13-14), some acetabular fractures (see schematic Figure 13-15), isolated inferior and superior pubic ramus fractures (Figures 13-55 to 13-57; see also schematic Figure 13-13), and avulsion fractures.

Figure 13-52 Transverse sacral fracture.
Sacral fractures may or may not disrupt the pelvis ring. Vertically oriented fractures through the body of the sacrum can disrupt the ring, as can disruptions of the sacroiliac joints. This patient has an isolated transverse fracture of the sacrum, approximately at the level of the inferior margin of the left sacroiliac joint. This runs through the neural foramen of the sacrum so that the arcuate lines of the foramen do not form a complete circle. Because the fracture only separates the caudad portion of the sacrum from the cephalad portion, the sacrum continues to form a complete bridge between the iliac wings, and the pelvis remains stable. A close-up view is seen in Figure 13-53.

Figure 13-53 Transverse sacral fracture.
Close-up from the same patient as in Figure 13-52. This patient has an isolated transverse fracture of the sacrum, approximately at the level of the inferior margin of the left sacroiliac joint. This runs through the neural foramen of the sacrum, so that the arcuate lines of the foramen do not form a complete circle. Because the fracture only separates the caudad portion of the sacrum from the cephalad portion, the sacrum continues to form a complete bridge between the iliac wings, and the pelvis remains stable. Compare with the CT in Figure 13-54.
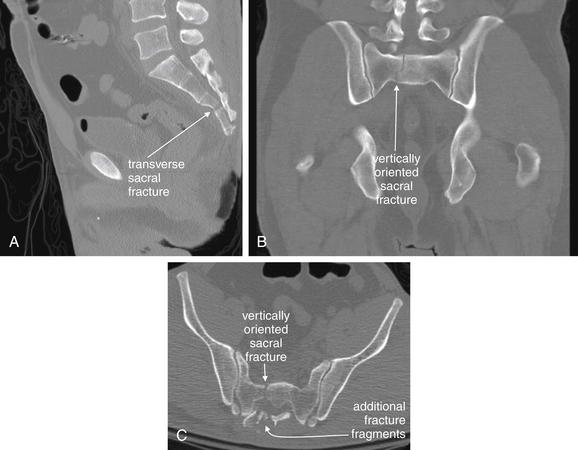
Figure 13-54 Comminuted sacral fracture.
Same patient as in Figures 13-52 and 13-53. CT, bone windows. Fracture patterns in real patients can be far more complex than textbook examples. This 40-year-old male fell 25 feet from a roof onto an air-conditioning unit, sustaining a comminuted sacral fracture. The x-ray in the earlier figures suggested an isolated transverse fracture, but CT shows otherwise. The fracture runs in multiple planes and cannot be fully appreciated on a single CT series. A, A midsagittal view suggests a transverse fracture through the distal sacrum. B, A coronal view shows a vertically oriented fracture line through the proximal sacrum. C, Axial view. A comminuted sacral fracture is visible.
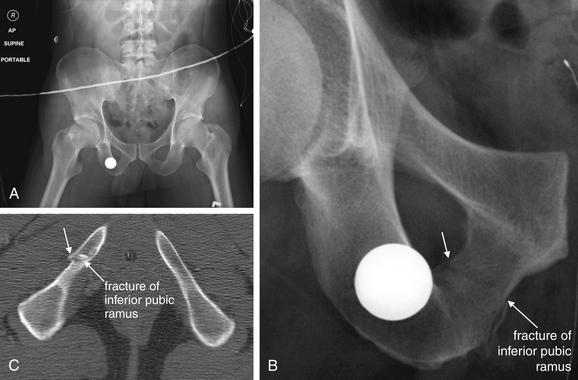
Figure 13-55 Isolated inferior pubic ramus fracture.
We have argued that an isolated fracture of the pelvic ring is rare. This patient has an apparently isolated fracture of the inferior right pubic ramus (AP x-ray A, and B). Is there a second occult injury? No, this fracture is so minimally displaced that it does not introduce tension elsewhere in the pelvic ring. Compare with the axial CT image in C. No other injuries were found on CT.
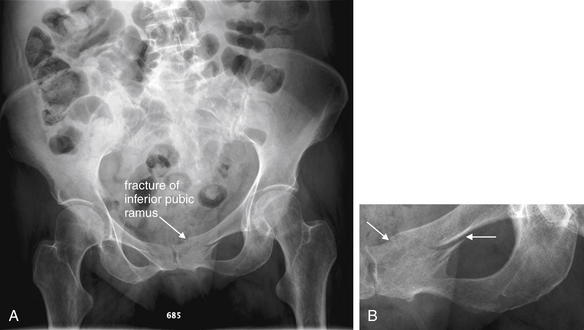
Figure 13-56 Isolated superior pubic ramus fracture.
This 64-year-old female fell from standing. An isolated fracture of the left superior pubic ramus is seen. Again, careful inspection for a second fracture should occur. Radiology recommended CT, but magnetic resonance imaging was performed—showing the same left pubic ramus fracture and a left sacral alar fracture. This pattern is commonly called a pelvic insufficiency fracture. It is attributed to weakened bone giving way under stress induced by a second injury. In this case, presumably the fall caused the sacral fracture, introducing stress into the pelvic ring that resulted in the anterior arch fracture. A, AP pelvis. B, Close-up from A.
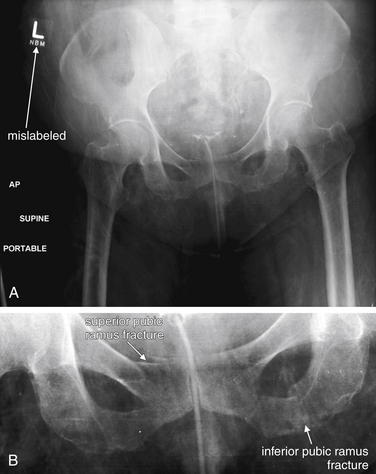
Figure 13-57 Pubic ramus fracture and labeling error.
A, AP pelvis x-ray. B, Close-up from A. This x-ray demonstrates several teaching points. First, the x-ray is mislabeled—an “L” is visible in the upper right corner. Technically, we cannot determine this from this x-ray, but this is a firm reminder to confirm your orientation before performing an invasive procedure. Second, this patient is quite osteopenic, making fractures more difficult to identify. Remember to look for two or more areas of discontinuity if one is found. Inspect the close-up, and you will see a fracture of the right superior pubic ramus, as well as one of the left inferior pubic ramus. Compare this with the CT in Figure 13-58, which confirms our suspicion about the labeling error.
Acetabular fractures
Acetabular fractures can occur in isolation or in combination with other pelvic fractures (Figures 13-43 to 13-51; see also schematic Figure 13-15). Fractures of the acetabulum can be difficult to recognize on plain x-ray but are readily evident with CT. Clues to the diagnosis are disruptions of the iliopubic line, which forms the medial border of the anterior column of the acetabulum; disruption of the ilioischial line, which forms the medial border of the posterior column of the acetabulum; and disruptions of the articular surface of the acetabulum, called the lunate surface.
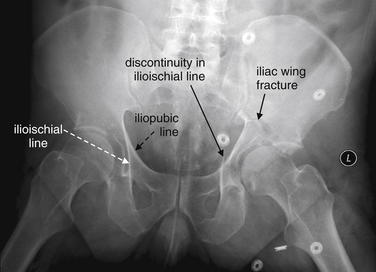
Figure 13-43 Acetabular fractures.
Two lines help to define the normal acetabulum. The anterior column of the acetabulum is defined by the iliopubic line, a curve from the medial ilium to the pubic symphysis. The posterior column of the acetabulum is bounded by the ilioischial line, a nearly vertical line from the medial ilium to the ischial tuberosity. These two lines are labeled on the patient’s right, where they are normal. On the patient’s left, the ilioischial line is disrupted, indicating a fracture of the posterior column of the acetabulum. In addition, a transverse fracture of the left ilium is visible and runs toward the left sacroiliac joint. The left superior and inferior pubic rami are fractured. Compare with the computed tomography images in Figures 13-44 and 13-45.
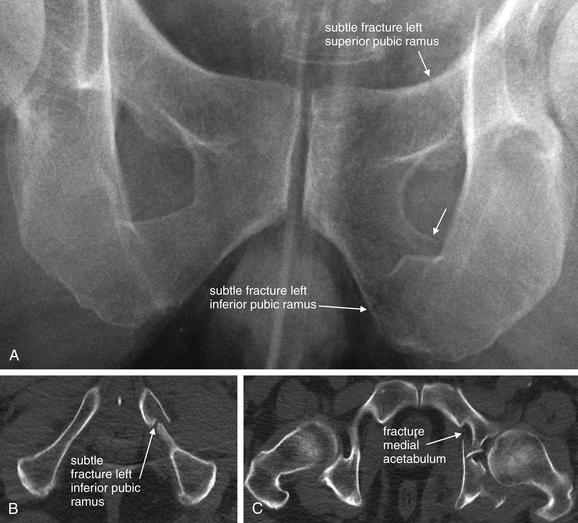
Figure 13-44 Acetabular fractures.
Same patient as in Figure 13-43. A, Subtle fractures of the superior and inferior pubic rami appear to be present on the original x-ray, magnified. Are these real? Look at the axial computed tomography slices, seen on bone windows (B, C).
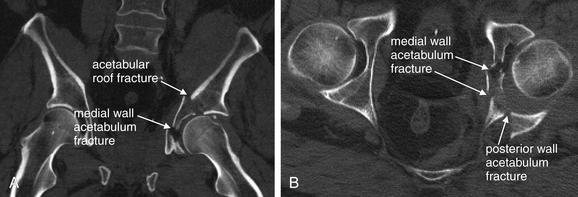
Figure 13-45 Acetabular fracture.
Same patient as in Figures 13-43 and 13-44. These CT images explore the left acetabular fracture in more detail. The fracture fragments have been pushed medially by the impact of the femoral head into the acetabular cup. A, Coronal view, bone windows. B, Axial view, bone windows. The lunate surface (the articular surface of the acetabulum) has been disrupted by the fractures. The acetabular cup has increased in size because of radial spread of fragments in B. Acetabular fractures are frequently associated with femoral head dislocations.
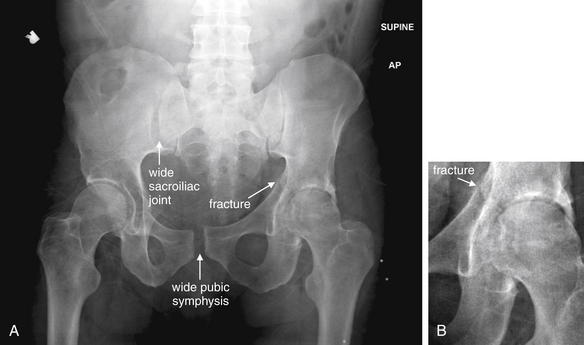
Figure 13-46 Pelvic ring disruption with acetabular fracture.
Multiple patterns of injury may combine in a given patient. A, This patient has both a widened pubic symphysis and a widened right sacroiliac joint. In addition, the right acetabulum is slightly irregular. A fracture also extends into the left acetabulum from the curve of the pelvis (B, Close-up). Compare with the CT in Figure 13-47.
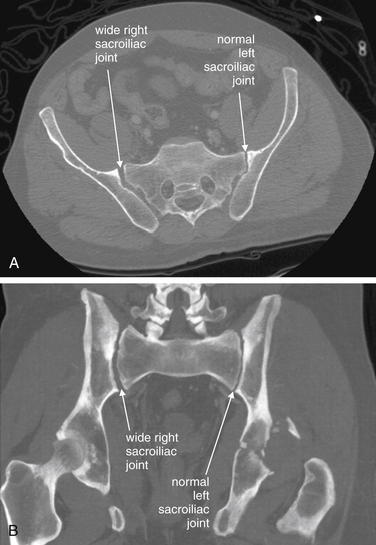
Figure 13-47 Widened sacroiliac joint.
CT, bone windows. Same patient as in Figure 13-46. Sacroiliac joint injuries are extremely important to recognize. They allow opening of the pelvic “book,” with the potential for serious hemorrhage as pelvic vessels are stretched. Look carefully at the CT images and refer back to the x-ray in Figure 13-46. A, Axial image showing a widened sacroiliac joint. B, Coronal reconstruction indicating the same finding.
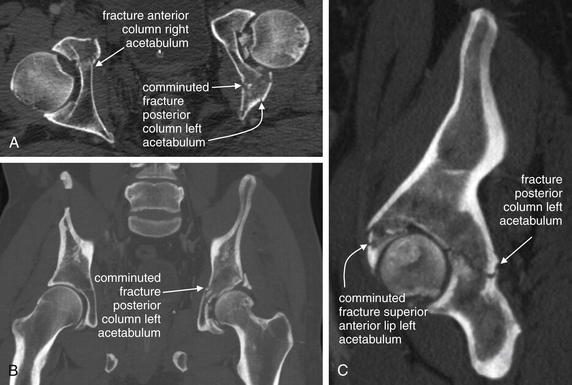
Figure 13-48 Acetabular fracture.
CT, bone windows. Same patient as Figures 13-46 and 13-47. Spend a moment gaining a better understanding of acetabular fractures on x-ray by studying the CT images. A, Axial image showing bilateral acetabular fractures. The left is more obvious than the right. B, Coronal reconstruction showing the same injury. You begin to sense the three-dimensional destruction of the left acetabular cup. C, Sagittal reconstruction illustrating the same abnormality.
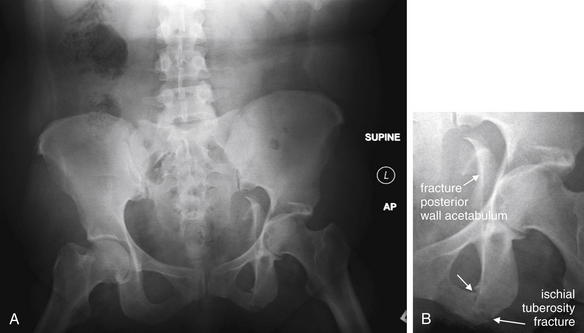
Figure 13-49 Pelvic ring disruption with acetabular fracture.
A fracture extends through the left ischial tuberosity. A fracture fragment from the posterior wall of the left acetabulum has been displaced medially into the pelvis. Compare with the CT in Figure 13-50. A, AP pelvis x-ray. B, Close-up from A.
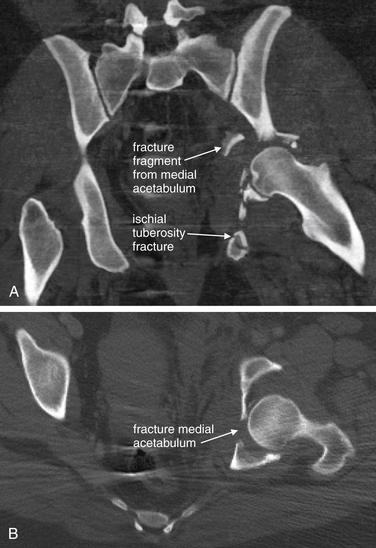
Figure 13-50 Acetabular and inferior pubic ramus fractures.
CT, bone windows. Same patient as Figure 13-49. A, A coronal reconstruction shows both the ischial tuberosity fracture and a comminuted fracture of the medial wall of the left acetabulum. B, An axial view shows the same acetabulum fracture.
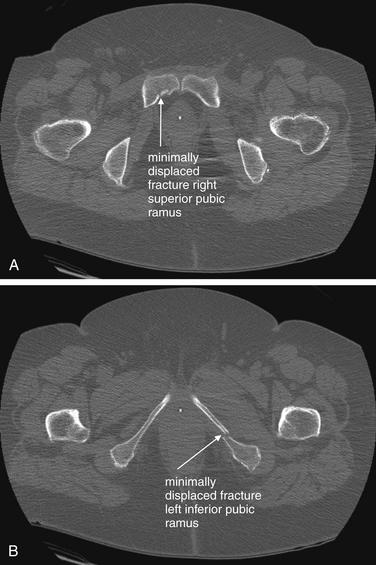
Figure 13-51 Right superior and left inferior pubic rami fractures.
Axial CT images, bone windows. A, B, CT shows a right superior pubic ramus fracture and a left inferior pubic ramus fracture. Remember to look for a second pelvic fracture when one is detected. However, in this case, either of these fractures might have occurred in isolation. When fractures are quite minimally displaced, they may not introduce enough tension into the pelvic ring to result in a second fracture. Certainly, the right superior ramus fracture is minimally displaced. Typically, fractures such as this are not associated with significant additional injuries.
Avulsion fractures
Avulsion fractures of the pelvis, common in pediatric and adolescent patients, occur at points of muscle attachment. Avulsion fractures can transpire with surprisingly modest mechanisms of injury, such as stretching, lifting, and sporting events with forceful contraction of a muscle without direct trauma. Consequently, they are not usually associated with other serious injuries but are important sources of continued pain and dysfunction if not recognized and treated. Examples include avulsion of the anterior superior iliac spine by contraction of the sartorius muscle (Figure 13-58), avulsion of the anterior inferior iliac spine by contraction of the rectus femoris (Figure 13-59), and avulsion of the ischial tuberosity by contraction of the hamstring muscles (Figures 13-60 and 13-61). Some pelvic injuries, such as fractures of the coccyx, require no imaging because their management is not influenced by radiographic findings.
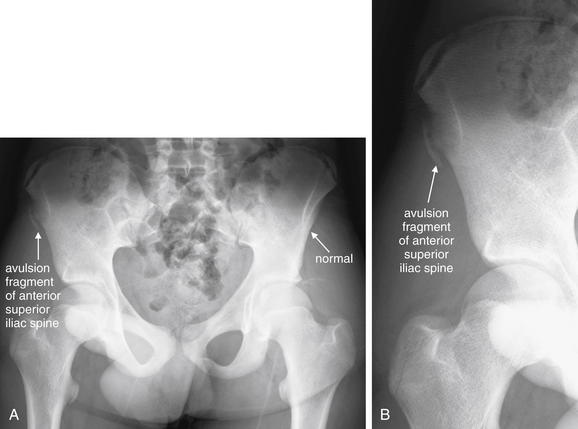
Figure 13-58 Avulsion fracture of anterior superior iliac spine by sartorius muscle.
This 15-year-old boy had acute right hip pain accompanied by a “popping” sound while running the first 100 m of a 400-m track race. He was unable to continue running and was brought to the emergency department for evaluation. A, The right anterior superior iliac spine is avulsed—compare with the normal left side. The fracture fragment appears as an ossified crescent. This is the insertion site of the origin of the sartorius muscle and may be avulsed by forceful contraction of the sartorius, which flexes the hip and knee. B, Close-up. Do not confuse this avulsion fracture with the lucent growth plates along the iliac crest, which are normal in this adolescent. Use symmetry to assist you here.

Figure 13-59 Avulsion of the anterior inferior iliac crest apophysis by the rectus femoris muscle.
This 16-year-old male presented with right hip pain after lifting a heavier person 2 days earlier. Since the incident, the patient has had trouble flexing his leg at the hip. He complains of pain in the right lateral and anterior hip. The x-ray shows an avulsion fracture fragment from the anterior inferior iliac spine. The donor site is clearly visible. This is the attachment point for the rectus femoris muscle. With forceful contraction of this muscle, the apophysis can be pulled off. Compare with the normal left. No clinical action was taken, though the patient’s cause of pain was now clear.

Figure 13-60 Avulsion of the ischial tuberosity by the hamstring muscles.
This 15-year-old male complained of pain in his right buttock and numbness in his right groin after doing an accidental “complete split.” He had slipped while walking at school, and his right hip flexed and left hip extended. During the split, he states that he heard something “pop.” His x-ray shows an avulsion fragment from the ischial tuberosity at the point of attachment of the hamstring muscles. Compare with the opposite normal side. The patient underwent operative repair of this injury to restore the function of the hamstring muscles (Figure 13-61).

Figure 13-61 Avulsion of the ischial tuberosity by the hamstring muscles.
Same patient as in Figure 13-60. His x-ray in the previous figure showed an avulsion fragment from the ischial tuberosity at the point of attachment of the hamstring muscles (semitendinosus, semimembranosus, and biceps femoris). Because this muscle group is functionally important for hip flexion and knee extension, the bony fragment was repositioned and fixed in place with the muscle origins still intact.
Hip Dislocations
Hip dislocations of native (nonprosthetic) hips usually occur only following extremely high-energy mechanisms of injury because this weight-bearing joint is one of the most stable mobile joints in the body. Acetabular fractures are common with hip dislocation. Commonly, the hip dislocates posteriorly when a seated motor vehicle passenger sustains AP force to the flexed and adducted hip (Figures 13-62 to 13-65; see also Figures 13-4 and 13-16). This injury is associated with posterior acetabular fractures. The femoral head usually appears cephalad to the acetabulum and may be laterally displaced. Anterior hip dislocations are less common but can occur if the hip is flexed and abducted at the time of an AP force (Figures 13-66 and 13-67; see Figure 13-17). The femoral head appears medially and is often inferiorly displaced relative to the acetabulum. Dislocations of prosthetic hips can occur with trivial force, such as flexion of the hip beyond 90 degrees. The acetabular component of the prosthetic hip usually remains in appropriate position while the femoral component dislocates. Posterior dislocation is most common, and the prosthetic femoral head appears cephalad and medial to the acetabulum (Figure 13-68).
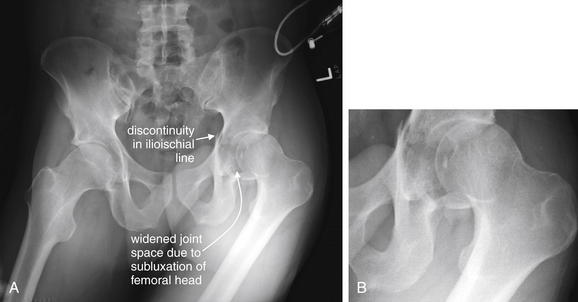
Figure 13-62 Posterior hip dislocation with acetabular fracture.
A, This patient has a comminuted left-sided acetabular fracture with discontinuity of the ilioischial line and a lucency extending into the acetabulum. The ilioischial line marks the posterior column of the acetabulum, so we should predict a posterior column fracture on CT. There is apparent subluxation or dislocation of the left femoral head—likely a posterior dislocation, explaining the posterior acetabular fracture. Disbelieve this finding? Note the unusual position of the femur. Compare with the CT in Figure 13-63. B, Close-up.
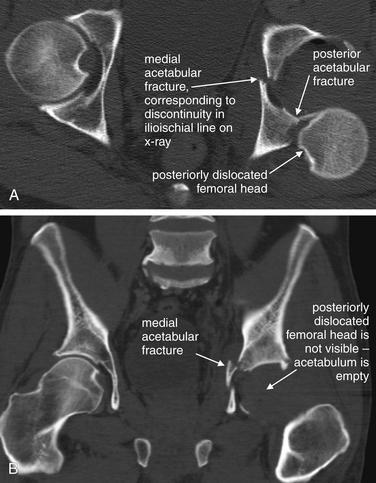
Figure 13-63 Posterior hip dislocation with acetabular fracture, CT bone windows. Same patient as in Figure 13-62. A, Axial view. The left femoral head is positioned completely posterior to the cup of the acetabulum, which is fractured medially and posteriorly. Because the femoral head was displaced in a posterior direction but remains aligned in a cephalad–caudad direction, the x-ray in Figure 13-62 is deceptive. Remember that two orthogonal views are needed to rule out dislocation on x-ray. B, Coronal view. The left femoral head is not visible because it lies behind the coronal plane of this image.
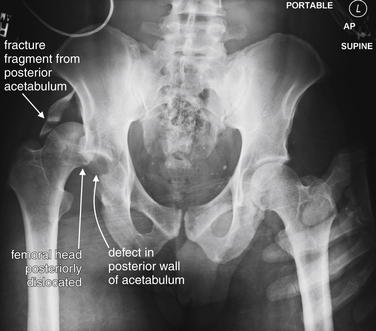
Figure 13-64 Hip dislocation with posterior acetabular fracture.
Dislocations of the hip are often accompanied by fracture of the acetabulum. In this case, the femoral head has dislocated posteriorly, fracturing the posterior wall of the acetabulum. The fracture fragment is visible cephalad to the femoral head Compare with the CT in Figure 13-65.
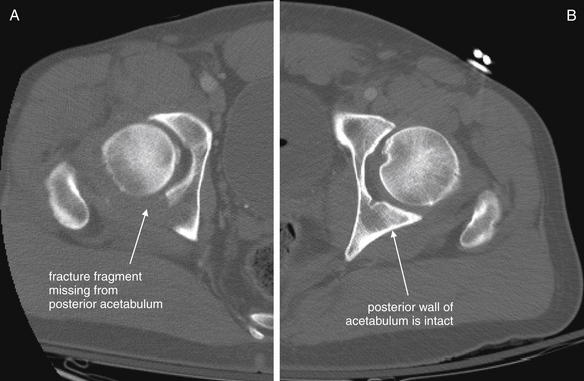
Figure 13-65 Posterior acetabular fracture.
Same patient as in Figure 13-64. The hip dislocation has been reduced before CT scan. A, A large fracture fragment is missing from the posterior wall of the right acetabulum. Because the patient was not aligned well in the CT scanner, the two acetabula did not appear in the same CT slice, but the same level through the left acetabulum has been selected and displayed for this illustration B.

Figure 13-66 Anterior hip dislocation.
This 18-year-old male was involved in a motor vehicle collision. The femoral head is dislocated medially and inferiorly—typical of anterior dislocation. This pattern is less common than posterior dislocation, which may happen when a patient seated in a vehicle with the hip flexed and adducted impacts the knee on a dashboard, forcing the femur posteriorly. The mechanism of anterior dislocation is believed to be force along an abducted and flexed hip. Remarkably, this patient had no pelvic fractures on CT (Figure 13-67).
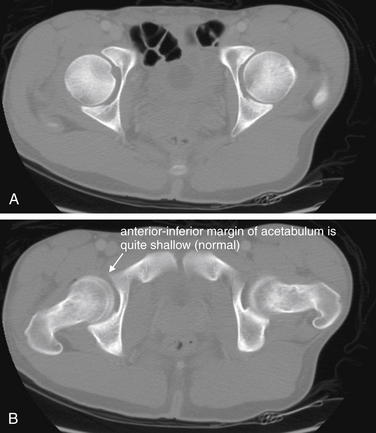
Figure 13-67 Anterior hip dislocation: Postreduction CT, bone windows.
Same patient as in Figure 13-66. These images, acquired following reduction, show no fractures of the acetabulum. A, Axial slice at the cephalad–caudad midpoint of the acetabulum. B, Slice at the level of the pubic symphysis, corresponding to the inferior margin of the acetabulum. Notice how shallow the anterior inferior rim of the acetabulum is, allowing dislocation without fracture if forces are applied in the correct vector.

Figure 13-68 Hip dislocation: Prosthetic.
Dislocation of a prosthetic hip may occur with relatively little force. Simple hyperflexion of the hip is often sufficient. The femoral head is then drawn cephalad and posterior by contraction of the hip muscles. A, The femoral component of the prosthesis is dislocated, while the acetabular cup remains in normal position. B, the femoral component has been reduced.
Hip Fractures
Fractures of the proximal femur, often called hip fractures, commonly occur with low-energy mechanisms such as falls from a standing position in osteoporotic patients age 65 years and older. Consequently, they are not highly associated with other serious pelvic soft-tissue injuries, such as vascular injuries, although dangerous injuries including cervical spine fractures and traumatic intracranial injury can occur. Common sites of fracture are the femoral neck and intertrochanteric region (Figures 13-69 to 13-71; see also Figures 13-18 and 13-19). Fractures through the femoral head (Figures 13-72 and 13-73) and at the juncture between the femoral head and the femoral neck (subcapital fractures, as in Figure 13-74) may also occur. All of these injuries can be subtle on x-ray when nondisplaced because osteoporotic bone makes recognition of the cortical and trabecular defects more difficult. A detailed discussion of the evidence for MRI and CT in the evaluation of these injuries is included in the chapter on musculoskeletal MRI (Chapter 15).
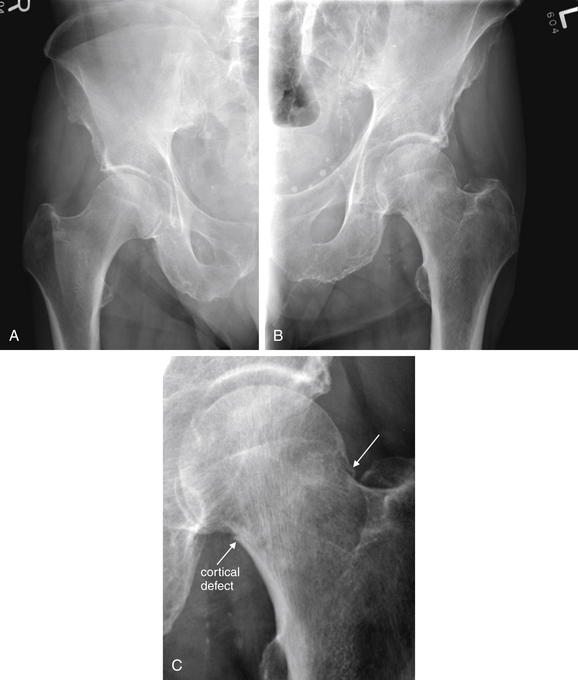
Figure 13-69 Fractures of the proximal femur: Neck, transcervical.
Compare the normal right side (A) to the subtle fracture of the left femoral neck, which is complete but nondisplaced (B). Bearing weight on this injury would likely lead to a displaced fracture. Minute cortical defects are visible, and the zone of fracture appears slightly denser because of impaction (C, close-up from B).

Figure 13-70 Femoral neck fracture.
This 84-year-old female had an unwitnessed fall. A, Normal right hip, osteoporotic. B, Left hip, another relatively subtle femoral neck fracture. Note the smudging of the trabeculae of the femoral neck. In addition, the distal fragment has shifted medially, creating an overhanging ledge of the femoral head not seen on the opposite normal side. Some femoral neck fractures are more obvious.

Figure 13-71 Intertrochanteric femur fracture: Three parts (proximal, distal, and one trochanter).
Intertrochanteric femur fractures are common, with the mechanism often being a fall from standing in an elderly patient. The major fracture line usually runs obliquely between the greater and the lesser trochanters. These fractures may have two, three, or four parts classically, although badly comminuted combinations are also possible. Two-part fractures consist of the proximal and distal fragments. Three-part fractures also include a fragment of one trochanter. Four-part fractures include fragments of both trochanters. This 86-year-old female had an unwitnessed fall. She has a typical three-part fracture, with a fragment of the lesser trochanter visible. Note her generalized severe osteopenia.

Figure 13-72 Fractures of the proximal femur: Femoral head fracture.
A, AP pelvis x-ray. B, Close-up from A. Fractures of the femoral head are usually associated with hip dislocation or acetabular fracture. We have already seen this radically comminuted pelvis, a reminder of the forces that often are associated with these injuries. Note the discontinuity of the iliopubic line on the right, indicating fracture of the anterior column of the acetabulum. Compare with the CT in Figure 13-73.
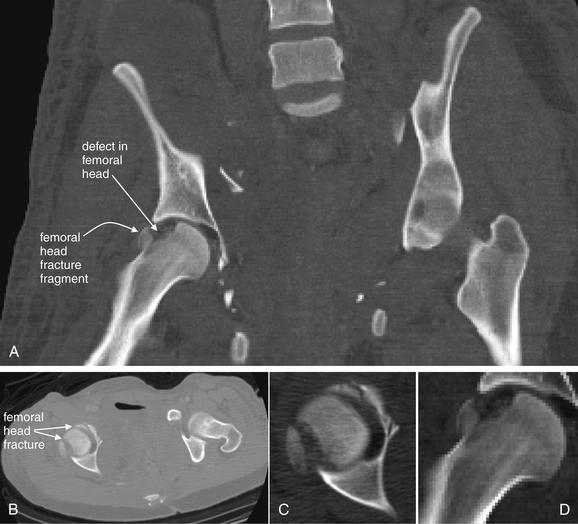
Figure 13-73 Femoral head fracture.
CT, bone windows. Same patient as in Figure 13-72. A, Coronal reconstruction showing fracture of femoral head. Note the scalloped defect in the femoral head. B, Axial view showing fractures. Two fractures are visible. C, Close-up from BD, Close-up from A.
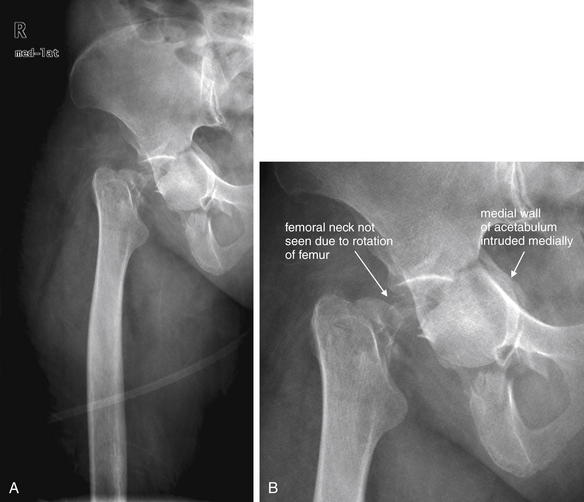
Figure 13-74 Subcapital femoral fracture.
A subcapital femoral fracture separates the femoral head from the femoral neck. This patient had an unwitnessed fall and sustained an impacted fracture of the right acetabulum. The femoral head remains in the acetabulum, the medial wall of which appears intruded into the pelvis. The femoral neck is not clearly seen because the femur has rotated, placing the femoral neck perpendicular to the plane of the x-ray. A, AP x-ray. B, Close-up from A.
Nontraumatic hip abnormalities
Nontraumatic abnormalities of the hip are an important cause of hip pain or limping in pediatric patients. Avascular necrosis (AVN) of the femoral head (Figures 13-75 and 13-76) may present with hip pain or limp. AVN may occur from previous trauma with disruption of the blood supply to the hip, from chronic steroid use, from sickle cell anemia with microvascular infarction, or as an idiopathic form, Legg-Calvé-Perthes disease. The latter occurs at a rate of 1 in 1200 children under the age of 15 years in the United States, most commonly in patients ages 3 to 12 years. It is a cause of limp in toddlers, and a frequent pitfall is x-ray of the distal leg without consideration of the hip. X-ray findings of AVN of any cause include a moth-eaten, irregular, and flattened femoral head and narrowed joint space. Another cause of AVN is slipped capital femoral epiphysis (SCFE) (Figures 13-77 to 13-79), a rare condition seen in around 1 in 10,000 U.S. children. Obesity and male gender are risk factors, with males developing the condition at 2.4 times the female rate. The common age range at diagnosis is 10 to 16 years. Bilateral involvement is common, occurring in up to 20% initially and 40% with passage of time, so both hips should be imaged when the diagnosis is suspected. SCFE may present with hip pain or with referred pain to the knee. Frog-legged x-ray views can assist in detection. Internal fixation is usually performed in an attempt to prevent further displacement and AVN. The x-ray findings of SCFE include a widened physis (growth plate) and a femoral epiphysis medially displaced relative to the femoral neck. A line drawn along the lateral aspect of the femoral neck should intersect the normal femoral capital epiphysis but will not intersect a SCFE, because the epiphysis is displaced medially. This appearance is sometimes described as resembling an ice cream cone with the scoop of ice cream (femoral epiphysis) slipping off of the cone (femoral neck). This injury is a Salter-Harris I fracture. The Salter-Harris classification system is described in detail in the chapter on the extremities (Chapter 14).
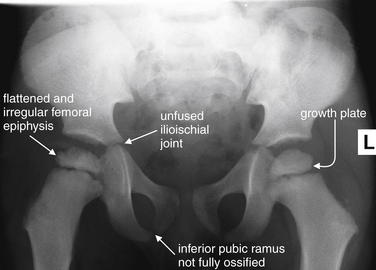
Figure 13-75 Avascular necrosis (AVN), Legg-Calvé-Perthes disease: Pediatric.
This 4-year-old male had persistent limping on his left lower extremity for 2 months. The patient had been seen by his primary care physician and an urgent care for the same problem. The father suggested the child might have fallen from a bicycle. This x-ray shows the classic signs of AVN of the bilateral proximal femoral epiphyses, or Legg-Calvé-Perthes disease. The epiphyses appear irregular and flattened with some sclerosis. The history is typical as well, with diagnostic delay. Notice that the findings are bilateral, slightly worse on the right than left, though clinically the patient was thought to be favoring the left leg. Incidentally, the patient has normal skeletal immaturity. The ilium and ischium have not fully fused, the femoral growth plates remain open, and the inferior pubic rami have not fully ossified. These should not be mistaken for fractures.

Figure 13-76 Avascular necrosis (Legg-Calvé-Perthes): Pediatric, advanced.
A, B, This 17-year-old male shows advanced findings of Legg-Calvé-Perthes disease. The femoral head is collapsed and flattened with subchondral lucencies. Notice how the acetabulum has also remodeled.
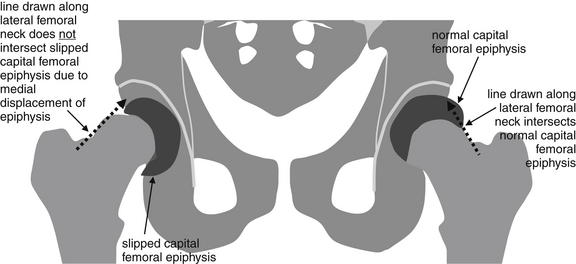
Figure 13-77 Slipped capital femoral epiphysis (SCFE).
SCFE is a rare condition of adolescents and preteens. Obesity and male sex are risk factors. The x-ray findings include a widened physis (growth plate) and a femoral epiphysis medially displaced relative to the femoral neck. A line drawn along the lateral aspect of the femoral neck, as in this schematic, should intersect the normal femoral capital epiphysis but will not intersect a SCFE because the epiphysis is displaced medially. This appearance is sometimes described as resembling an ice cream cone with the scoop of ice cream (femoral epiphysis) slipping off of the cone (femoral neck). Frog-legged x-ray views can assist in detection. Because bilateral involvement occurs in 20% at initial presentation, both hips should be x-rayed. Internal fixation is usually performed in an attempt to prevent further displacement and avascular necrosis. This is a Salter-Harris I injury. The Salter-Harris classification is described in detail in Chapter 14.
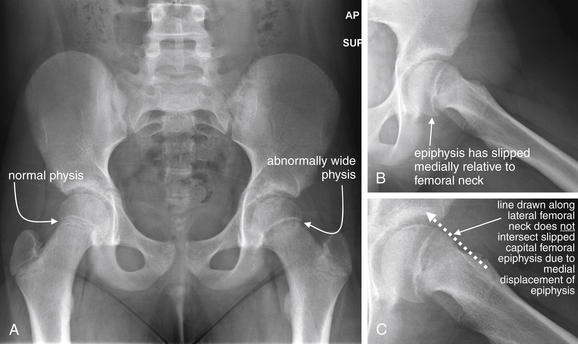
Figure 13-78 Slipped capital femoral epiphysis (SCFE).
This 10-year-old female presented with 6 weeks of nontraumatic left hip pain, starting insidiously around the thigh. She limps occasionally and is unable to participate in sports. A, The anterior–posterior pelvis shows widening of the physis, concerning for SCFE (a Salter-Harris I fracture). B, A frog-leg view reveals subtle posteromedial displacement of the epiphysis, consistent with SCFE. C, A close-up frog-leg view shows that a line drawn along the lateral aspect of the femoral neck does not intersect the physis as it normally would.
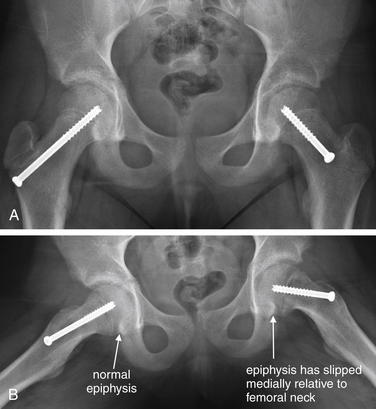
Figure 13-79 Slipped capital femoral epiphysis.
Same patient as in Figure 13-78, 1 month later, after internal fixation of both capital femoral epiphyses. A, Anterior–posterior view. B, Frog-legged view. Note the subtle medial displacement of the left femoral capital epiphysis, compared with the normal right, which was pinned prophylactically.
Other nontraumatic hip abnormalities include osteoarthritis, rheumatoid arthritis, and septic arthritis; gout; and toxic synovitis. Ultrasound is the preferred diagnostic imaging modality when joint infection is suspected because it can confirm joint effusion and guide joint aspiration, which is diagnostic. Less common imaging studies of the hip include nuclear medicine studies and MRI. These are discussed in more detail in the chapter on musculoskeletal MRI (Chapter 15).
Interpretation of Pelvic Computed Tomography
Pelvic CT for evaluation of bony injuries should be evaluated using a bone window setting. The evaluation of soft-tissue injuries to pelvic organs requires the use of soft-tissue windows and is discussed in more detail in the chapters on genitourinary imaging (Chapter 12) and abdominal trauma (Chapter 10). Axial images are routinely available and should be evaluated first. The pelvis has a complex structure, and the rings seen on plain x-ray are not fully oriented in the axial plane. It may take some time for you to feel comfortable recognizing injuries by tracking an obliquely oriented portion of the pelvic ring through several adjacent CT slices. Nonetheless, axial images are excellent for detecting the range of pelvic injuries described earlier on x-ray. Review of sagittal and coronal planar images can clarify some injury patterns. The key to diagnosis of fractures on CT is identification of a cortical discontinuity, which may be the only evidence of a nondisplaced fracture. Displaced fractures are readily apparent on CT. The pubic symphysis and sacroiliac joints can be measured using digital PACS tools. In the figures throughout this chapter, plain x-ray and multiplanar CT images depicting the same pelvic injuries are shown, allowing you to develop your skills in recognition of important fractures and dislocations. CT images should be reviewed for the same abnormalities as described earlier for x-ray. The figures in this chapter contain detailed guidance on CT interpretation, not repeated here. Pelvic fractures are often associated with important vascular injuries, seen best on soft-tissue windows. These are described in detail in the chapter on interventional radiologic procedures in emergency medicine (Chapter 16). Bladder and urethral injuries may accompany pelvic fractures. These are seen best on soft-tissue CT windows and are described in more detail in the chapter on genitourinary imaging (Chapter 12).
How Reliable Is a Physical Examination for Detecting Pelvic Injury?
When does a blunt trauma patient require imaging of the pelvis? Can some patients avoid pelvic imaging altogether? Advanced Trauma Life Support guidelines have historically called for pelvis x-ray in all blunt trauma patients,4 but selective imaging based on patient history and examination could improve the yield, saving time and money and reducing radiation exposure. Clinical predictors of pelvic injury would be particularly helpful in pregnant women, in whom pelvic irradiation is especially undesirable. Numerous studies suggest that in awake, alert patients, a normal examination of the pelvis combined with a normal neurologic examination eliminates the need for pelvic x-ray. We review several of these studies here.
In 2004, Sauerland et al.5 conducted a meta-analysis of the reliability of the clinical examination in detection of pelvic fractures in blunt trauma patients. The authors identified 12 studies with 5454 patients and found a pooled sensitivity of 90%, with a 95% confidence interval (CI) of 85% to 93%, and a specificity of 90% (95% CI = 84%-94%). They found that clinically relevant injuries were extremely rare in patients with a normal Glasgow Coma Score (GCS) and a normal examination of the pelvis and concluded that in stable and alert trauma patients, pelvic x-ray is unnecessary when examination is normal. Many individual studies included in this meta-analysis are examined later because the details of their methods are important to us in deciding their applicability to our patients.
In 2008, Duane et al.6 prospectively compared clinical examination and x-ray against a gold standard of CT scan for the diagnosis of pelvic fracture. They evaluated 1388 patients undergoing pelvic x-ray and CT scan for hip pain, internal rotation of the leg, or tenderness over the sacrum, hip, or diffuse pelvis. The authors reported the sensitivity of x-ray as 79% (133 of 168 fractures). All injuries detected by x-ray were also detected by physical examination, and examination was 96.4% sensitive compared with CT (detecting 162 of 168 patients with fractures). The authors recommended that x-ray be eliminated as a routine screening tool in patients with GCS greater than 13. This study follows an earlier publication by the same group in 2002,6a which prospectively evaluated 520 patients for whom a detailed physical examination questionnaire had been completed. In that study, 45 patients were found to have fractures by x-ray, and the gold standard in patients not undergoing x-ray was absence of clinical symptoms until hospital discharge. The investigators considered the presence of any of the questionnaire history or examination findings a “positive” history and physical. The sensitivity of a positive history and physical was 100%, and the specificity was 37.2%. The absence of any pelvic complaints or examination findings had a negative predictive value of 100% for pelvic fracture, and would have safely eliminated the need for pelvis x-ray in two-thirds of patients.
Gross and Niedens7 prospectively validated a clinical decision rule for imaging the pelvis following blunt trauma. Fractures were classified as significant or insignificant, following the previously published Tile classification,3 which focuses on pelvic stability. All blunt trauma patients undergoing pelvic x-ray were enrolled and rated upon five criteria, similar to those of the National Emergency X-radiography Utilization Study (NEXUS) cervical spine criteria (discussed in Chapter 3): altered level of consciousness, complaint of pelvic pain, pelvic tenderness on examination, distracting injury, or clinical intoxication. The Gross and Niedens study enrolled 973 patients, of whom 62 (6.4%) had pelvic fractures. The sensitivity of the five criteria was 96.8% for any pelvic fracture (95% CI = 92.4%-100%). If only clinically significant fractures were included, the sensitivity was 100% (95% CI = 95.2%-100%). Application of the five criteria would have eliminated 44% of x-rays. A larger prospective sample is required for external validation and to narrow confidence intervals.7
An earlier study by Gonzalez et al.8 reached similar conclusions. In this prospective study including 2176 patients (14 years or older) with a GCS of 14 or 15, patients were evaluated for pelvic pain, neurologic complaints or deficits, and pelvic examination abnormalities, including abrasions or contusions over bony prominences; ecchymosis about the pubis, perineum, or scrotum; or blood at the urethral meatus. In addition, pelvic examination included medial and posterior compression of the iliac wings, compression of the pubic symphysis, inspection for limb length discrepancies, hip flexion, internal and external hip rotation, and rectal examination for gross blood. The gold standard for diagnosis was pelvic fracture based on final readings of all radiologic studies by board-certified attending radiologists. Physical examination detected 90 of 97 pelvic fractures (sensitivity = 93%, 95% CI = 85%-97%). X-ray detected 84 of 97 pelvic fractures (sensitivity = 87%, 95% CI = 78%-92%). Application of the clinical criteria would have reduced x-ray utilization by 88%. In the subgroup of 185 patients with a GCS of 14, clinical examination missed two of nine pelvic fractures (22%). Among the 1991 patients with a GCS of 15, only 5 of 88 patients with fracture were missed by examination (sensitivity 94%). The authors noted that none of the 7 injuries missed by physical examination required surgical intervention, and only 2 were treated with non-weight-bearing status. This study also included 463 patients with ethanol levels greater than 100 mg/dL. Clinical examination identified 19 of 20 patients with pelvic fractures (95% sensitivity). The undiagnosed injury was an acetabular fracture. The authors concluded that routine pelvic x-ray in awake and alert blunt trauma patients is unnecessary and not cost-effective, and that ethanol intoxication does not substantially alter the sensitivity of examination.
These results are concordant with numerous earlier studies. Yugueros et al.9 published a retrospective study of 608 Colombian blunt trauma patients. They asserted that physical examination detected 57 of 59 patients (96.6%) with pelvic fractures and that the 2 patients with missed injuries were stable and required no treatment. They advocated that x-ray is not required in hemodynamically stable adult patients with normal pelvis examination, no spinal injury, and a GCS greater than 10.
Koury et al.10 reported a prospective study of 125 alert and oriented blunt trauma patients and concluded that a normal physical examination of the pelvis eliminated the need for x-ray, with no injuries detected on x-ray in this group.
Salvino et al.11 reported on 810 prospectively evaluated blunt trauma patients with a GCS of 13 or greater. They found that only 3 of 743 patients (0.4%) with neither pain nor abnormal pelvis physical examination findings had fractures. Among 39 patients with fractures, pelvis pain by history or abnormal pelvis examination findings were 92% sensitive for fracture.
Civil et al.12 prospectively evaluated 265 blunt trauma patients for pelvic fracture. Patients were classified as unconscious; impaired; awake, alert and symptomatic; or awake, alert, oriented, and asymptomatic for pelvic fracture. No fractures were identified in 110 patients in the category of awake, alert, oriented, and asymptomatic.
Gillott et al.13 argued for routine pelvic x-ray during the early resuscitation of blunt trauma patients, noting a 16.7% incidence of pelvic injury among 669 patients and a higher requirement for blood transfusion, higher injury severity scores, and a higher incidence of chest and abdominal injuries in patients with pelvic injury on x-ray. However, the authors did not investigate the predictive value of history and physical examination.
In summary, medical literature supports the use of clinical assessment to determine the need for pelvic x-ray in adult blunt trauma patients. X-ray appears unnecessary in patients with normal mental status and normal pelvis physical examination findings.
How Common Are Pelvis Injuries in Children? How Serious Are These Injuries in Pediatric Patients? Could a Clinical Decision Rule Reduce Unnecessary Imaging in This Group?
Pelvis fractures are rarer in children than in adults, occurring in only 2.4% to 7.5% of serious trauma,14-15 with lower associated mortality in children.14 Naturally, when an injury or disease process is rare, many normal x-rays would need to be obtained to identify a single injury. As a consequence, the published negative predictive value of the pediatric physical examination is reported to be high, but the more important clinical question is the sensitivity of the examination. Numerous studies have assessed the value of clinical indications for pelvic x-ray in pediatric patients, although the strength of evidence is poorer than in adults because of the small numbers of patients enrolled, the wide age range of patients, and frequently retrospective methods.
Ramirez et al.16 published a retrospective chart review using case-control design of 33 pediatric patients with pelvic fractures and 63 patients without fracture, all with GCS of 14 or 15. Blunt trauma patients 14 years and younger were included. The authors found that pelvic contusion or abrasion, hip or pelvic pain, abdominal pain and distention, back pain, hip held in rotation, and femur deformity or pain independently predicted pelvic fracture. They noted that the absence of all these findings has a negative predictive value of 87% and concluded that clinical findings could be useful in assessing the need for pelvic x-ray in awake and alert pediatric blunt trauma patients. The sensitivity of a simple four-part rule incorporating the absence of hip or pelvic pain, pelvic abrasions or contusions, abdominal pain or distension, and thigh pain or deformity was 73%, with a specificity of 92%. They estimated a reduction in x-ray use by 73% using this rule. Their study is quite limited by its retrospective methods because it is uncertain whether the absence of documentation of these physical examination findings truly represents their absence in a given patient.
Junkins et al.17 reported a prospective study of 140 pediatric blunt trauma patients. An abnormal pelvic examination identified 11 of 16 patients with pelvic fractures (69% sensitivity). The specificity and negative predictive value were 95% and 91%, respectively. However, a lack of standardization of the pelvic examination and broad age ranges make this study difficult to apply clinically. Moreover, the reported sensitivity is inadequate to exclude fracture; the reported negative predictive value is more a reflection of the rarity of pelvic fractures in the group (11%) than of the strength of the diagnostic test.
In a separate retrospective study of 174 patients between the ages of 3 months and 18 years (median age = 8 years), Junkins et al.18 classified the pelvic examination as normal or abnormal. Using this binary classification, the sensitivity of examination was 92% (95% CI = 89%-95%), with a specificity of 79% (95% CI = 74%-84%). The positive predictive value was 84%, with a negative predictive value of 89%. The authors noted that examination appeared unreliable in patients with a GCS of less than 15 and those with distracting injury. However, retrospective methods such as those in the study may be unreliable. For example, it is possible that physical examination abnormalities were not written in the chart, although they may have been noted at the time of examination. In addition, it is unclear whether the reviewers abstracting the charts were blinded to the study question, an important practice to reduce bias in this type of study.19
Rees et al.20 performed a retrospective chart review of 444 pediatric blunt trauma patients in Auckland, New Zealand. The 347 performed x-rays identified only one pelvic fracture, which appeared clinically obvious from documentation in the medical record. The authors suggest that screening pelvic x-rays are unnecessary in patients without findings of injury. Pelvic fractures were extremely rare in this group, concordant with other studies of pediatric blunt trauma. However, this study does not provide rigorous proof that physical examination is sensitive for detection of pelvic injury. A larger number of injured patients are required for this purpose. Two research methods could enrich the number of injured patients. First, a case-control study could be conducted, ensuring that a target number of injured patients is included. However, this would require retrospective methodology, which would fall prey to the same limits of chart review mentioned earlier, including uncertainty about the meaning of undocumented physical examination findings. Second, a large prospective multicenter trial could be conducted to assess physical examination sensitivity. This is unlikely to occur given the cost of such a study.
Soundappan et al.21 retrospectively reviewed charts of 274 blunt trauma patients under the age of 16 years and argued for selective rather than routine use of pelvic x-ray. However, the limitations of the retrospective methods and the small number of patients with pelvic injuries reduce the validity of this study in assessing physical examination.
Quick and Eastwood22 reviewed the pediatric pelvic trauma literature and recommended against pelvic screening x-ray in hemodynamically stable pediatric patients with GCS greater than 10, no spinal cord injury, a normal pelvic examination, and no hematuria. Overall, it appears likely that clinical exam can reliably exclude pelvic fractures in older adolescents using criteria similar to those demonstrated for adults. However, younger children are less well-studied and routine pelvis x-ray may be warranted at this time.
Have Airbags and Seatbelts Changed the Rate of Pelvic Fracture? Is a Patient Less Likely to Have a Pelvic Injury If Airbags and Seatbelts Are in Use?
Data from 1988 to 2003 suggest that airbags and seatbelts in use at that time were not protective against pelvic fractures. However, newer side-impact airbags were not evaluated in these studies.23-25
When Pelvic X-ray Is Normal, Who Needs CT? In Other Words, How Sensitive Is X-ray for Fracture?
As described earlier, x-ray is likely not indicated in alert and awake patients with no pelvic pain and no abnormal physical examination findings. If x-rays are obtained in this group and are normal, no further imaging is generally required for evaluation of the bony pelvis. Other clinical concerns for abdominal injuries may warrant abdominal and pelvic CT; these are reviewed in detail in the chapter on imaging of abdominal trauma (Chapter 10).
In the Patient With Pelvic Pain or Abnormal Pelvis Physical Examination Findings after Blunt Trauma, Does a Negative X-ray Rule Out Fracture?
Numerous studies have shown x-ray to be relatively insensitive for pelvis fractures, compared with a gold standard of CT scan. Gonzalez et al.8 found x-ray to be only 87% sensitive for fracture, including both positive and “equivocal” x-rays. When only x-rays prospectively read as positive for fracture are considered “true positives,” the sensitivity was only 79%. As described earlier, Duane et al.6 also reported the sensitivity of x-ray to be only 79%, compared with CT.
Vo et al.27 found that x-ray detected only 81% of fractures detected by CT scan and 87% of patients with injuries detected by CT. This retrospective study, like many studies of diagnostic imaging, had no independent gold standard. CT was assumed to be correct when injuries are detected. Moreover, it is not certain that all pelvic injuries missed on x-ray but detected on CT scan had any clinical significance. Nonetheless, it does suggest that x-ray misses a substantial number of bony pelvic injuries.
These studies suggest that when a specific concern for pelvic fracture exists, based on patient complaints or physical examination findings, x-ray is insufficient to rule out fracture. Additional pelvic imaging should be performed. In the major trauma patient, CT is the routine test of choice because of its ability to detect other abdominal and pelvic soft-tissue and vascular injuries. The proper follow-up test for suspected pelvis or hip fracture following lower-energy injuries, such as falls from standing, is in debate. We consider some evidence for MRI in comparison to CT and nuclear medicine studies in the chapter on musculoskeletal MRI (Chapter 15).
If CT Scan Is Planned for Evaluation of Other Abdominal and Pelvic Soft-Tissue Injuries, Is Pelvis X-ray Needed? If so, in Which Patients?
CT of the abdomen and pelvis provides detailed information about the bony pelvis. It would appear redundant to obtain pelvic x-ray in a stable patient if CT of the abdomen and pelvis is planned for evaluation of other injuries. Multiple studies have investigated the utility of pelvic x-ray in this scenario and conclude that it is unnecessary.
Kessel et al.26 performed a retrospective trauma registry review of all stable blunt trauma patients at two trauma centers from 2001 through 2004. Compared with a gold standard of CT, x-ray was only 64.4% sensitive and 90% specific. The authors suggested eliminating routine pelvic x-ray when CT is planned in a stable patient.
Vo et al.27 conducted a retrospective study of 509 patients undergoing both CT scan and x-ray. CT identified 163 pelvic injuries in 60 patients, whereas x-ray identified only 132 injuries in 52 patients. No patient with a negative CT scan had an injury detected on x-ray. In contrast, 8 patients with negative x-rays had injuries detected on CT scan. Compared with CT scan, the sensitivity of x-ray was only 81% on a per-fracture basis and 87% on a per-patient basis. The authors concluded that x-ray should be eliminated in stable blunt trauma patients who will undergo CT.
Stewart et al.28 retrospectively reviewed 397 patients undergoing both pelvic x-ray and abdominopelvic CT. Compared with a gold standard of CT, the portable pelvic x-ray detected only 58 of 109 fractures (sensitivity = 53%) and did not identify 9 of 43 injured patients (sensitivity = 79%). X-ray was particularly insensitive for detection of sacroiliac fractures. Investigators reported four “false positive” x-rays, blaming reporting errors and film artifact for these. As with other studies we have discussed, the lack of an independent diagnostic standard limits the study results; however, from a practical standpoint, CT is the current clinical gold standard in major trauma patients. It appears unlikely that pelvis x-ray provides clinically useful information in stable trauma patients undergoing abdomen and pelvis CT.
Guillamondegui et al.29 performed a retrospective review of all blunt trauma patients undergoing immediate abdominal and pelvic CT scan. The sensitivity and specificity of portable pelvis x-ray were 68% and 98%, respectively, compared with the gold standard of CT scan. The authors concluded that portable pelvis x-ray should not be performed in hemodynamically stable patients who will undergo immediate CT scan of the abdomen and pelvis. They recommended x-ray in unstable patients and those who cannot or will not undergo CT scan because of other clinical interventions.
Using a pediatric trauma registry, Guillamondegui et al.15 performed a retrospective review of 130 pediatric patients younger than 18 years with pelvic fractures over an 8-year period. In this series, x-ray detected only 81 of 151 fractures noted on CT (54% sensitivity). The authors recommended against pelvic x-ray in pediatric patients for whom CT scan is planned. They continued to advocate for x-ray in unstable patients or those in whom CT will not be performed.
Overall, in the hemodynamically stable blunt trauma patient, it is probably reasonable to forgo pelvic x-ray when pelvic CT is planned, saving both time and money.
Are Clinical Factors Useful in Identifying a Subset of Patients With Unstable Fractures? Should These Patients Undergo X-ray for Early Diagnosis, Even If Computed Tomography Will Be Performed?
Even if CT of the abdomen and pelvis will be performed, it is possible that x-ray in the trauma bay could provide immediate information with clinical utility. A prospective study of 979 emergency department trauma patients examined a binary rating of the pelvic examination as stable or unstable. Unstable pelvis on physical examination was 99% specific for fracture, indicating that when a physician finds the pelvis to be unstable on examination, a pelvic injury is almost certain to be present. However, the sensitivity of pelvic instability for fracture was only 44%.30 The authors concluded that pelvic radiography should be routine, a practice not supported by other trauma literature (as reviewed earlier). The authors did not evaluate the sensitivity of a more detailed history and examination, including factors such as pelvic tenderness, pelvic pain, or examination findings such as ecchymosis or abrasion. Some patients in this study were clinically difficult to assess because of severe injuries and endotracheal intubation. The authors did note a higher rate of blood transfusion requirements in patients with pelvic instability on examination, suggesting that when this finding is present, an early aggressive plan for blood products and potential pelvic embolization should be considered.
A second retrospective study of 1502 consecutive patients found that unstable pelvic ring on physical examination was poorly sensitive (26%, 95% CI = 15%-43%) but highly specific (99.9%, 95% CI = 99%-100%) for mechanically unstable pelvic fractures. Pelvic deformity was 55% sensitive (95% CI = 38%-70%) and 97% specific (95% CI = 96%-98%) for mechanically unstable pelvic fractures. Although the authors focused on the poor sensitivity of physical examination, the high specificity implies that when these examination abnormalities are present, an unstable fracture is virtually certain. In awake and alert trauma patients with a GCS of more than 13, pelvic pain or tenderness was highly sensitive (100%, 95% CI = 85%-100%) for unstable pelvic fracture.31
Overall, evidence supports the presence of an unstable or deformed pelvis on examination as a specific though insensitive sign of an unstable pelvic fracture. It may be reasonable to perform portable pelvic x-ray in the trauma room of patients with pelvic instability on examination to identify gross fractures and allow earlier pelvic stabilization. The insensitivity of the physical examination for mechanically unstable pelvic fracture may make bedside portable pelvic x-ray a good choice in patients with unstable vital signs. Alternatively, if CT scan can be rapidly performed, patients with an unstable pelvis on examination or unstable vital signs could be treated empirically with external pelvic binding and fluid resuscitation. If CT will not be performed because of hemodynamic instability, pelvic x-ray should be performed.
How Much Does Pelvic X-ray Cost? How Long Does a Pelvic X-ray Take To Obtain?
In 2008, an AP pelvis x-ray cost $245, with an additional $22 fee for radiologist interpretation.6 Duane et al.6 calculated substantial savings by elimination of routine pelvic x-ray. X-ray of the pelvis is rapid to obtain because only a single view is performed. However, given the number of tasks that must be accomplished in the trauma patient, every effort should be made to eliminate unnecessary steps with little clinical benefit. When CT is planned as part of the evaluation, x-ray appears of little value in stable patients, and even the minimal time required for pelvic x-ray may be wasteful. In less stable patients, pelvic x-ray can provide rapid and valuable information by identifying or excluding the pelvis as a probable source of hemorrhagic shock as described in more detail in Chapter 10.
When Pelvic Fractures Are Detected, Should Bladder and Urethral Injuries Be Evaluated?
Pelvic fractures are associated with bladder and urethral injuries, which occur in about 6% of all pelvic fractures and almost 15% of severe pelvic fractures in adults.1 Do all pelvic fractures mandate additional radiographic evaluation for these injuries, or are some fractures riskier than others with regard to genitourinary injuries? The indications for imaging and the specific features of the diagnostic tests used for evaluation of these injuries are reviewed in detail in the chapter on genitourinary imaging (Chapter 12). However, because pelvic fractures are one potential predictor of bladder and urethral injury, we discuss the implications of pelvic fractures and the appropriate genitourinary imaging tests here. Briefly, retrograde urethrogram is used to assess for urethral injury, whereas conventional or CT cystogram assesses for bladder rupture. Some authors believe that anterior pelvic injuries including pubic rami fractures and pubic symphysis diastasis mandate imaging of the urethra and bladder.
Basta et al.32 evaluated the subtypes of pelvic fracture most associated with genitourinary injury. Using a retrospective nested case-control method, the investigators reviewed x-rays and CT scans and recorded location, displacement, and estimated direction of force in 119 male patients with pelvic fractures. They detected 25 patients with urethral injuries, all with anterior pelvic fractures or diastasis of the symphysis pubis. No urethral injuries were found in isolated acetabular fractures. The authors performed logistic regression and found an increased risk for urethral injury in patients with displaced fractures of the inferomedial pubic bone (odds ratio = 6.4, 95% CI = 1.6-24.9) and symphysis pubis diastasis (odds ratio = 11.8, 95% CI = 4.0-34.5). The authors noted a 10% increase in risk for urethral injury with each millimeter of diastasis or displacement in these two pelvic injury patterns.32 Limits of this study include the small sample of injured patients (because of the overall rarity of this injury) and exclusion of female patients. The urethra is shorter in females and less prone to injury, and it is uncertain whether the risk for urethral injury would follow the same trends in female patients. Urethral injuries occur in as many as 25% of males with pelvic injury but only 4.6% of female patients with pelvic injury. This study is concordant with previous studies suggesting that urethral injuries are restricted to patients with fractures of the anterior pelvic arch. However, the study is too small to establish with certainty whether some anterior pelvic injuries do not require follow-up evaluation for urethral injury. Other studies are reviewed in Chapter 12.
In the Presence of Pelvic Fractures, When Should Additional Imaging Be Performed To Detect Pelvic Vascular Injury? What Is the Role of Angiographic Embolization?
In cases of stable pelvic fractures from low energy mechanisms, such as as pubic rami fractures following a fall from a standing position, no further imaging may be required. These injuries are almost never associated with pelvic vascular or abdominal injuries. In contrast, severe pelvic fractures from high energy blunt trauma often are complicated by vascular injuries and significant pelvic bleeding. Treatment is generally nonsurgical, using angiographic embolization to achieve hemostasis. CT with IV contrast should be performed, providing detailed information about both fractures and vascular injuries. In most cases, active extravasation of parenteral contrast on CT scan is considered an indication for embolization. See the chapter on interventional radiologic techniques in emergency medicine (Chapter 16) for a detailed discussion of angiographic treatment of pelvic vascular injuries.
Why Is Magnetic Resonance Imaging Recommended for Some Pelvic Injuries and CT for Others? Is This an Evidence-Based Practice?
As described earlier, x-ray is known to be relatively insensitive for the detection of pelvic fractures. Fractures of the hip (proximal femur) may also be missed with x-ray. CT is routinely used to exclude pelvic fractures in major trauma patients, without recourse to MRI. In contrast, MRI is often used rather than CT in the evaluation of osteoporotic patients with hip pain and negative x-rays after relatively minor trauma, such as falls from standing. The evidence basis for this practice is critically examined in the chapter on musculoskeletal MRI (Chapter 15).
Summary
Pelvic fractures are a common source of serious morbidity and less commonly mortality in trauma patients. X-ray provides an initial screening examination for the symptomatic patient, with CT providing a highly sensitive assessment of fractures and associated vascular injuries. A normal pelvis physical examination in a neurologically intact and asymptomatic trauma patient likely is sufficient to rule out pelvic fractures.
1. Demetriades D., Karaiskakis M., Toutouzas K., et al. Pelvic fractures: Epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195:1-10.
2. Young J.W., Burgess A.R., Brumback R.J., Poka A. Pelvic fractures: Value of plain radiography in early assessment and management. Radiology. 1986;160:445-451.
3. Tile M. Pelvic ring fractures: Should they be fixed? J Bone Joint Surg Br. 1988;70:1-12.
4. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support. Chicago: ATLS Instructor Manual; 1998. American College of Surgeons
5. Sauerland S., Bouillon B., Rixen D., et al. The reliability of clinical examination in detecting pelvic fractures in blunt trauma patients: A meta-analysis. Arch Orthop Trauma Surg. 2004;124:123-128.
6. Duane T.M., Dechert T., Wolfe L.G., et al. Clinical examination is superior to plain films to diagnose pelvic fractures compared to CT. Am Surg. 2008;74:476-479. discussion 479-80
6a. Duane T.M., Tan B.B., Golay D., et al. Blunt trauma and the role of routine pelvic radiographs: a prospective analysis. J Trauma. 2003;53(3):463-468.
7. Gross E.A., Niedens B.A. Validation of a decision instrument to limit pelvic radiography in blunt trauma. J Emerg Med. 2005;28:263-266.
8. Gonzalez R.P., Fried P.Q., Bukhalo M. The utility of clinical examination in screening for pelvic fractures in blunt trauma. J Am Coll Surg. 2002;194:121-125.
9. Yugueros P., Sarmiento J.M., Garcia A.F., Ferrada R. Unnecessary use of pelvic x-ray in blunt trauma. J Trauma. 1995;39:722-725.
10. Koury H.I., Peschiera J.L., Welling R.E. Selective use of pelvic roentgenograms in blunt trauma patients. J Trauma. 1993;34:236-237.
11. Salvino C.K., Esposito T.J., Smith D., et al. Routine pelvic x-ray studies in awake blunt trauma patients: A sensible policy? J Trauma. 1992;33:413-416.
12. Civil I.D., Ross S.E., Botehlo G., Schwab C.W. Routine pelvic radiography in severe blunt trauma: Is it necessary? Ann Emerg Med. 1988;17:488-490.
13. Gillott A., Rhodes M., Lucke J. Utility of routine pelvic X-ray during blunt trauma resuscitation. J Trauma. 1988;28:1570-1574.
14. Demetriades D., Karaiskakis M., Velmahos G.C., et al. Pelvic fractures in pediatric and adult trauma patients: Are they different injuries? J Trauma. 2003;54:1146-1151. discussion 1151
15. Guillamondegui O.D., Mahboubi S., Stafford P.W., Nance M.L. The utility of the pelvic radiograph in the assessment of pediatric pelvic fractures. J Trauma. 2003;55:236-239. discussion 239-40
16. Ramirez D.W., Schuette J.J., Knight V., et al. Necessity of routine pelvic radiograph in the pediatric blunt trauma patient. Clin Pediatr (Phila). 2008;47:935-940.
17. Junkins E.P.Jr., Nelson D.S., Carroll K.L., et al. A prospective evaluation of the clinical presentation of pediatric pelvic fractures. J Trauma. 2001;51:64-68.
18. Junkins E.P., Furnival R.A., Bolte R.G. The clinical presentation of pediatric pelvic fractures. Pediatr Emerg Care. 2001;17:15-18.
19. Gilbert E.H., Lowenstein S.R., Koziol-McLain J., et al. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996;27:305-308.
20. Rees M.J., Aickin R., Kolbe A., Teele R.L. The screening pelvic radiograph in pediatric trauma. Pediatr Radiol. 2001;31:497-500.
21. Soundappan S., Smith N.F., Lam L.T., et al. A trauma series in the injured child: Do we really need it? Pediatr Emerg Care. 2006;22:710-716.
22. Quick T.J., Eastwood D.M. Pediatric fractures and dislocations of the hip and pelvis. Clin Orthop Relat Res. 2005:87-96.
23. Rowe S.A., Sochor M.S., Staples K.S., et al. Pelvic ring fractures: Implications of vehicle design, crash type, and occupant characteristics. Surgery. 2004;136:842-847.
24. Loo G.T., Siegel J.H., Dischinger P.C., et al. Airbag protection versus compartment intrusion effect determines the pattern of injuries in multiple trauma motor vehicle crashes. J Trauma. 1996;41:935-951.
25. Inaba K., Sharkey P.W., Stephen D.J., et al. The increasing incidence of severe pelvic injury in motor vehicle collisions. Injury. 2004;35:759-765.
26. Kessel B., Sevi R., Jeroukhimov I., et al. Is routine portable pelvic X-ray in stable multiple trauma patients always justified in a high technology era? Injury. 2007;38:559-563.
27. Vo N.J., Gash J., Browning J., Hutson R.K. Pelvic imaging in the stable trauma patient: Is the AP pelvic radiograph necessary when abdominopelvic CT shows no acute injury? Emerg Radiol. 2004;10:246-249.
28. Stewart B.G., Rhea J.T., Sheridan R.L., Novelline R.A. Is the screening portable pelvis film clinically useful in multiple trauma patients who will be examined by abdominopelvic CT? Experience with 397 patients. Emerg Radiol. 2002;9:266-271.
29. Guillamondegui O.D., Pryor J.P., Gracias V.H., et al. Pelvic radiography in blunt trauma resuscitation: A diminishing role. J Trauma. 2002;53:1043-1047.
30. Pehle B., Nast-Kolb D., Oberbeck R., et al. [Significance of physical examination and radiography of the pelvis during treatment in the shock emergency room]. Unfallchirurg. 2003;106:642-648.
31. Shlamovitz G.Z., Mower W.R., Bergman J., et al. How (un)useful is the pelvic ring stability examination in diagnosing mechanically unstable pelvic fractures in blunt trauma patients? J Trauma. 2009;66:815-820.
32. Basta AM., Blackmore CC., Wessells H. Predicting urethral injury from pelvic fracture patterns in male patients with blunt trauma. J Urol. 2007;177(2):571-575.