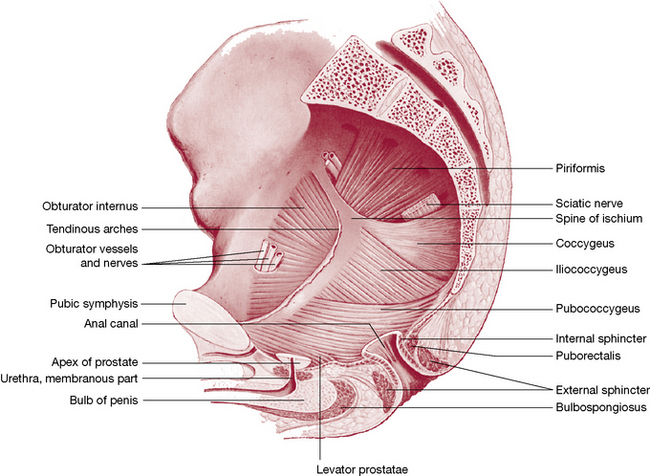
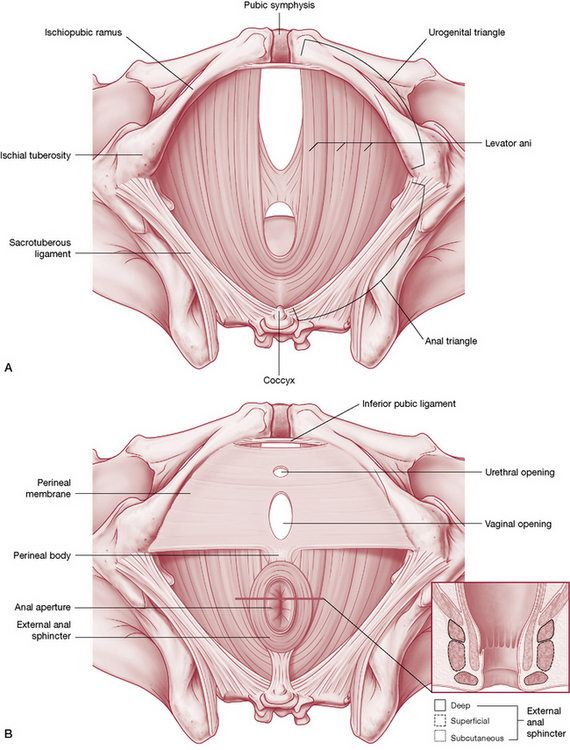
Prone pelvic assessment and si treatment protocols
Pelvic landmark observation and palpation
Observation and palpation are made of the relative positions and symmetry of landmarks such as the PSISs (for symmetry and orientation including ventral/dorsal, cranial/caudal), sacral sulci (for depth) and inferior lateral angles (for orientations including anterior/posterior, cranial/caudal).
Mobility of the sacrum assessment in prone
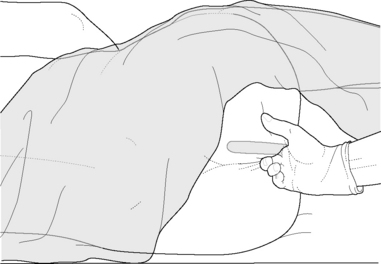
Inferior lateral angles (ILAs) spring test
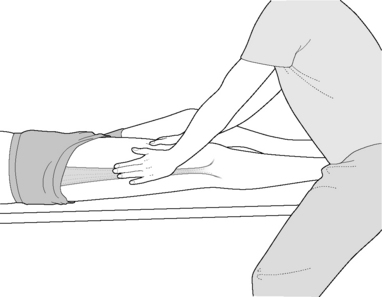
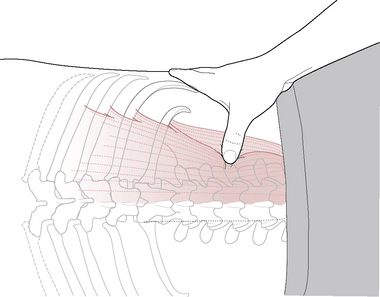
• The practitioner places the hands oriented cephalad so that the palm of each hand rests on an ILA and the tips of the fingers are on the sacral sulci (Fig. 11.20).
• With one hand at a time, pressure is applied directly cephalad (not obliquely) from one ILA toward the ipsilateral SI joint. This should produce a palpable cephalad movement of the sacrum.
• SI dysfunction is indicated if the degree of joint play on that side is distinctly less than the other. If both sides fail to register a degree of ‘give’, bilateral SI joint dysfunction may be present.
• The results of this test should correlate with the seated flexion test described earlier and the prone active straight leg raise test described below.
Lumbosacral spring test
CAUTION: This test should not be applied if a spondylolisthesis (forward slippage of the vertebra) is suspected or has been diagnosed.
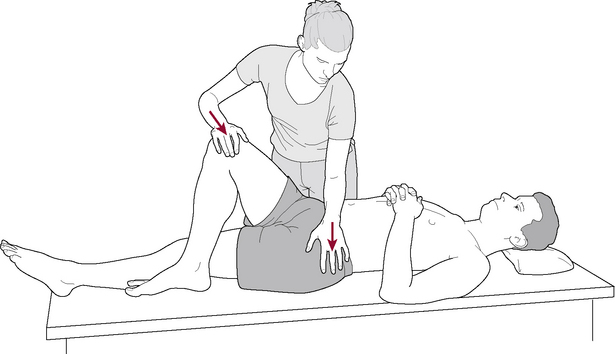
• The practitioner is at waist level facing the prone patient and places her hands transversely, one on the other, across the lumbar spine, at L5 level.
• A light degree of pressure is applied perpendicular to and through the spine (toward the floor) to evaluate the degree of resilience.
• If a hard, non-yielding resistance is noted the test is positive and a lumbosacral restriction exists.
Prone active straight leg raising test
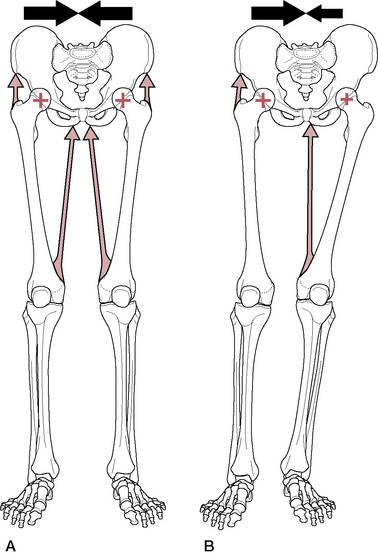
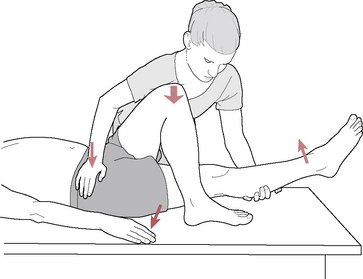
• The prone patient is asked to extend the leg at the hip by approximately 10°. Hinging should occur at the hip joint and the pelvis should remain in contact with the table throughout.
• Excessive degrees of pelvic rotation in the transverse plane (anterior pelvic rotation), and/or pain or difficulty in raising the leg is reported during the test, this suggests possible SI joint dysfunction as explained below.
• If form features (structural) of the SI joint are at fault, the prone straight leg raise will be more normal when the practitioner, with hands on the innominates, bilaterally applies firm medial pressure toward the SI joints during the procedure (Fig. 11.35C).
• Force closure may be enhanced during the exercise if latissimus dorsi can be recruited to increase tension on the thoracolumbar fascia. Lee (1999) states: ‘This is done by [the practitioner] resisting extension of the medially rotated [contralateral] arm prior to lifting the leg’ (Fig. 11.35D).
• As in the supine straight leg raising test (described earlier in this chapter), if force closure enhances more normal SI joint function, the prognosis for improvement is good, to be achieved by means of exercise and reformed use patterns.
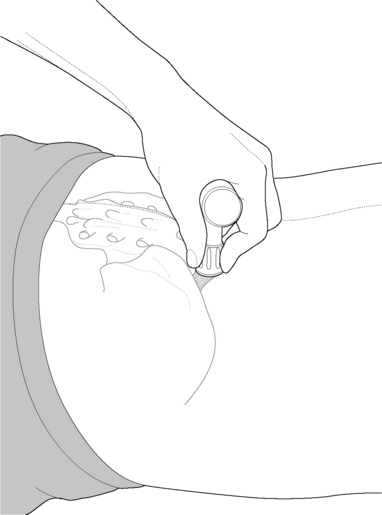
Prone SI joint gapping test (and MET treatment)
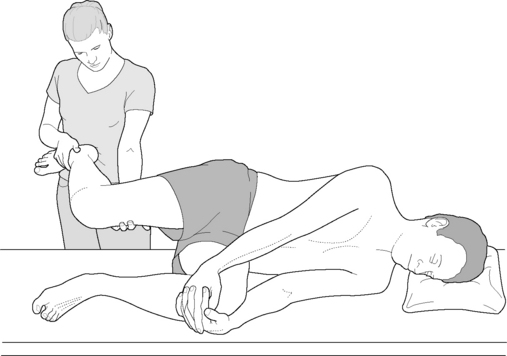
• The patient is prone and the practitioner stands on the side to be tested, while facing the table and holding the leg proximal to the ankle joint with her caudad hand.
• The patient’s knee is flexed with the thigh resting on the table so that the angle between the leg and the table is a little less than 90°.
• The practitioner’s cephalad hand palpates the SI joint as the leg is taken into internal rotation at the hip by pulling the leg laterally, a process that should produce a palpable gapping at the SI joint.
• The same assessment is carried out with the knee flexed to a greater degree, so that the angle between table and leg is greater than 90°. Gapping is again palpated for as internal rotation at the hip is produced by the practitioner via the long lever of the lower extremity.
• Failure of gapping may be treated by having the patient attempt to return the leg to its neutral position (i.e. by introducing external rotation of the hip and extension of the knee) against practitioner resistance. Force should be minimal (‘20% of available strength or less’) and maintained for 7–10 seconds. After this, the test should be repeated to evaluate any improvement. If joint play is not restored on retesting, other SI joint approaches should be used.
The seated flexion test, the ILA spring test and the various elements of the supine (see earlier this chapter) and prone active straight leg raising tests offer evidence of sacroiliac dysfunction.
MET for SI joint dysfunction
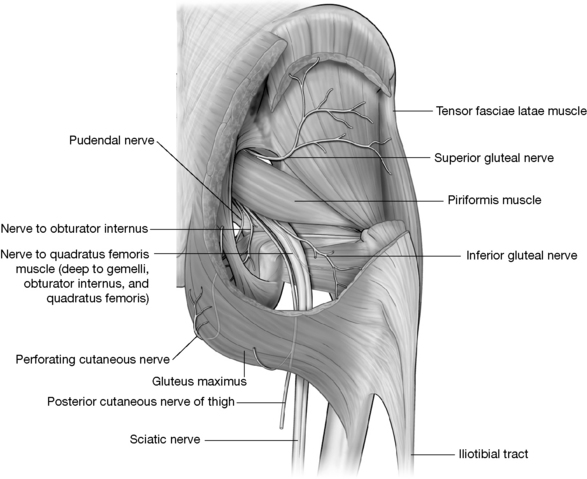
It is essential to normalize muscles attaching to the pelvis before considering ‘direct action’ to reduce hypomobility of the SI joint. While there are no muscles that actively move the SI joint, there are a great many that directly or indirectly influence its function, either through the transverse slings that engage the force closure mechanisms during the gait cycle (see Chapter 3) or by means of less obvious influences on pelvic mobility.
Lee (1999) says, for example:
When the regional muscles become tight (e.g. hamstrings, piriformis), the mobility of the pelvic girdle (innominate or sacrum) can be affected, however the SI joint remains mobile. This is why it is imperative to evaluate the mobility of the joint with tests [see ‘spring tests’ above] which do not involve active contraction or passive lengthening of the muscles. When the myofascial system is the primary source of dysfunction, specific muscle-lengthening techniques can be effective in restoring the osteokinematics of the pelvic girdle. These techniques are often referred to as ‘muscle energy’ techniques or active mobilization techniques. They facilitate the restoration of motion at the SI joint and can be used in conjunction with passive mobilization techniques.
SI joint dysfunction normalization might therefore include:
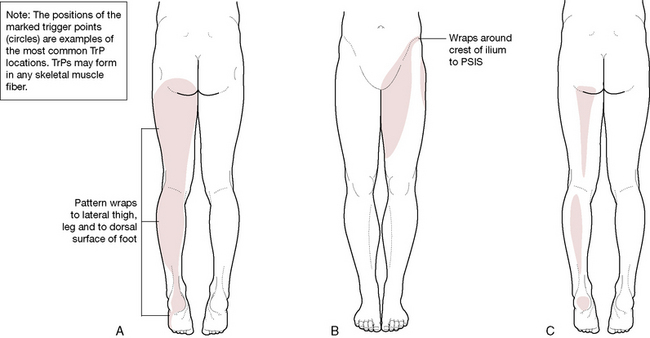
• specific focus on identification and normalization of shortened postural muscles attaching to, or closely associated with, the pelvis, including hamstrings, adductors, quadriceps (especially rectus femoris), tensor fasciae latae, piriformis, iliopsoas, quadratus lumborum, latissimus dorsi, multifidus and erector spinae. MET treatment of these will be found in the appropriate chapters of this book, including this one
• application of ‘shotgun’ technique as described earlier in this chapter to enhance normal ligamentous balance
• specific MET procedures directed at particular biomechanical dysfunction patterns relative to a hypomobile SI joint
• postural and proprioceptive reeducation (see Chapter 7 for rehabilitation and self-help measures)
Sacroiliac mobilization using MET
• If the seated flexion test (described earlier in this chapter) is positive, the side on which the thumb is seen to move cephalad during flexion is the dysfunctional side.
• The patient is supine and the practitioner stands contralaterally.
• The patient’s affected hip is flexed, with thigh vertical and slightly adducted.
• The practitioner places her caudad hand flat under the sacrum so that the index finger can palpate the contralateral SI joint area (Fig. 11.36A and B).
• The practitioner’s cephalad hand rests on the flexed knee, resisting the patient’s application of force from the knee into that hand (i.e. force is applied via the long axis of the femur toward the ceiling).
• The palpating hand should note a contraction in the tissues surrounding the SI joint during the 7–10 seconds contraction.
• After relaxation of the isometric effort the practitioner applies pressure from the knee, through the femur, toward the SI joint to evaluate any increase in its ability to display ‘spring’ (there should be a sense of localized joint play at the SI joint, on compression, rather than a solid movement of the entire pelvis).
• After one or two repetitions of this procedure the seated flexion test should be performed to evaluate relative improvement in the SI joint’s function.
Prone sacral PRT for pelvic (including SI joint) dysfunction
Two sets of sacral tender points used in PRT of SI and sacral dysfunction are described below.
In 1989, a series of sacral tender points were identified as being related to low back and pelvic dysfunction. These points were found to be amenable to very simple SCS methods of release (Ramirez et al 1989). Subsequently, additional sacral foramen tender points that are believed to relate to sacral torsion dysfunctions were identified (Cislo et al 1991).
One set lies on the mid-line of the sacrum or close to it, the so-called ‘medial tender points’. These lie in soft tissues over the bony dorsum of the sacrum; when digital palpating pressure is applied to them there is a sense of ‘hardness’ below the point. The characteristic dysfunctions linked to these points are described below, as are appropriate treatment approaches. The medial points, as a rule, require a vertical pressure toward the floor, applied in a way that ‘tilts’ the sacrum sufficiently to relieve the palpated tenderness. Because these points lie on a ‘hard’ surface and the tilting objective is the preferred treatment approach, a shorthand memory jogger (‘hard rock’) helps to differentiate the treatment method from that applied to other sacral points.
The other set of sacral points lies over the sacral foramina and so when pressure is applied to these, there is a sense of ‘softness’ in the underlying tissues. The treatment protocol for this is described below. Once this has been read it will become clear why the shorthand reminder for these points is ‘soft squash’.
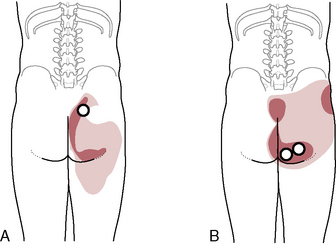
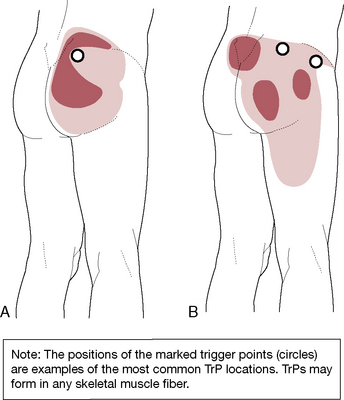
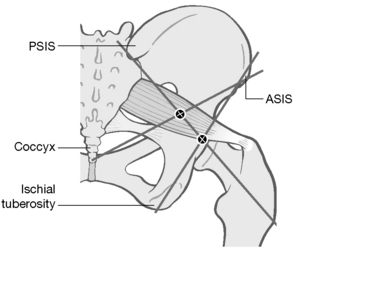
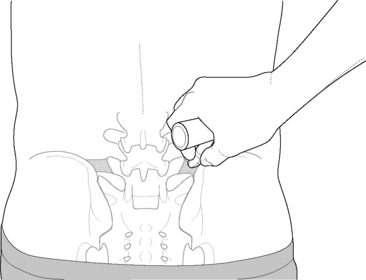
Location of sacral medial points (Fig. 11.37)
• The cephalad two points lie just lateral to the mid-line, approximately 1.5 cm (3/4 inch) medial to the inferior aspect of the PSIS bilaterally, and they are known as PS1 (PS = posterior sacrum).
• The two bilateral caudad points (PS5) are located approximately 1 cm (just under 1.2 inch) medial and 1 cm superior to the inferior lateral angles of the sacrum.
• The remaining three points are on the mid-line: PS2 lies between the 1st and 2nd spinous tubercles of the sacrum, PS3 lies between the 2nd and 3rd sacral tubercles, both of which are identified as being involved in sacral extension dysfunctions, and the last point (PS4) lies on the cephalad border of the sacral hiatus and relates to sacral flexion dysfunctions.
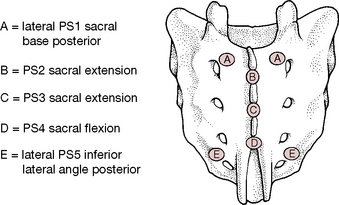
Figure 11.37 Positions of tender points relating to sacral dysfunction
(reproduced with permission from Chaitow 2007).
The original researchers (Ramirez et al 1989) report: ‘We have found that when these tender points occur in groups the associated sudomotor change is frequently confluent over the mid-sacrum. For this reason, we have begun to check all points on all patients with low back pain, even in the absence of sudomotor changes.’ (See notes on skin evaluation using skin drag method in Volume 1, Chapter 6). They report that this process of localization can be rapid if the bony landmarks are used during normal structural examination.
Treatment of medial sacral tender points
• With the patient prone, pressure on the sacrum is applied according to the tender point being treated. The pressure is always straight downward toward the floor, in order to induce rotation around either the transverse or oblique axis of the sacrum.
• The PS1 points require pressure at the ‘corner’ of the sacrum opposite the quadrant in which the tender point lies (e.g. left PS1 requires pressure at the right inferior lateral angle).
• The PS5 points require pressure near the sacral base on the contralateral side (e.g. a right PS5 point requires pressure on the left sacral base just medial to the SI joint).
• The release of PS2 (sacral extension) tender point requires downward pressure (to the floor) to the apex of the sacrum in the mid-line.
• The lower PS4 (sacral flexion) tender point requires pressure to the center of the sacral base.
• PS3 (sacral extension) requires the same treatment as for PS2 described above.
In all of these examples it is easy to see that the pressure is attempting to exaggerate the existing presumed distortion pattern relating to the point, which is in line with the concepts of SCS and positional release as explained earlier in Volume 1, Chapter 10.
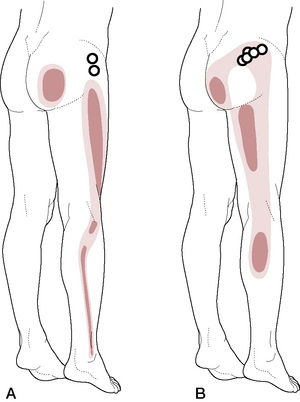
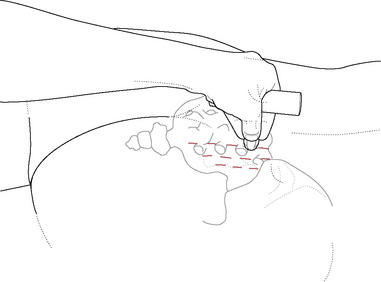
Sacral foramen tender points (Fig. 11.38)
The clinicians who first noted these points reported that a patient with low back pain, with a recurrent sacral torsion, was being treated using SCS methods with poor results. When muscle energy procedures proved inadequate, a detailed survey was made of the region and an area of sensitivity that had previously been ignored was identified in one of the sacral foramina.
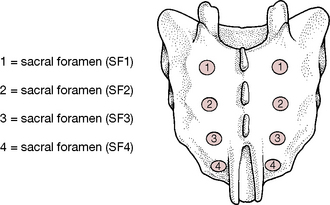
Figure 11.38 Sacral foramen tender points as described in the text
(reproduced with permission from Chaitow 2007).
Experimentation with various release positions for this tender point resulted in benefits and also the examination of this region in other patients with low back pain and evidence of sacral torsion. ‘All the patients [who were examined] demonstrated tenderness at one of the sacral foramina, ipsilateral to the engaged oblique axis [of the sacrum].’
The identifiers of the sacral foramina tender points (Cislo et al 1991) have named each pair of points according to their anatomic position.
Clinically, these tender points are located by their positions relative to the posterior superior iliac spines. The most cephalad of the points [SF1 – sacral foramen tender point 1] is 1.5 cm (just over half an inch) directly medial to the apex of the PSIS. Each successively numbered sacral foramen tender point [SF2, SF3, SF4] lies approximately 1 cm (two-fifths of an inch) below the preceding tender point location.
SCS for sacral foramen tender points
Evaluation of the sacral foramina should be a fairly rapid process. Once a sacral torsion has been identified, the foramina on the ipsilateral side are examined by palpation and the most sensitive of these is treated. A left torsion (forward or backward) would therefore involve the foramen on the left side being assessed.
Alternatively, palpation of the foramina, using the skin drag method for rapid evaluation (see Chapter 9), would reveal dysfunction, even if the precise nature of that dysfunction remains unclear. If there was obvious skin drag over a foramen and if digital compression of that foramen was painful, some degree of sacral torsion would be suggested on the same side as the tender foramen.
In this example, a left sacral torsion is assumed (anterior or posterior), with tenderness in the tissues overlying one of the left side sacral foramina.
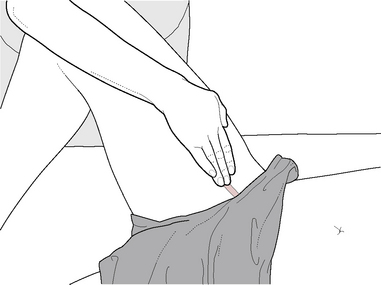
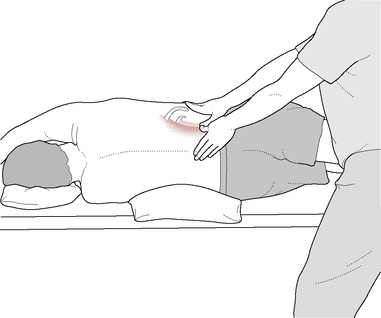
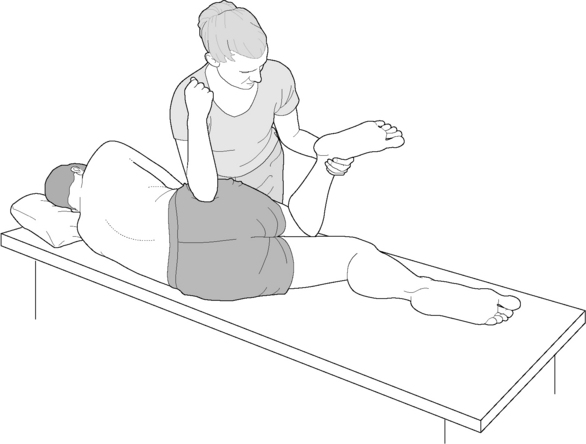
• The patient lies prone with the practitioner standing on the side contralateral to the foramen tender point to be treated, facing cephalad, i.e. right side in this example when a left torsion (foramen tender point) is being treated.
• The practitioner applies pressure to the sensitive foramen with her tableside (left) hand sufficient to create discomfort, which the patient registers as a score of ‘10’.
• The patient’s right leg (contralateral to the tender point side) is abducted to about 30°, with slight flexion at the hip and knee and external rotation at the hip, which allows the leg to be supported by the edge of the table. This should result in a report of some reduction in the pain score.
• The practitioner, while continuing to apply pressure to the sensitive foramen with her tableside hand, introduces compression to the gluteal musculature below the crest of the ilium on the right, directed anterosuperomedially, using her cephalad forearm or hand (right in this example) (i.e. she effectively ‘squashes’ the tissues).
• The arm or hand contact should be approximately 1 inch lateral to the patient’s right PSIS.
• The degree of relief of sensitivity initiated in the palpated sacral foramen tender point by the leg abduction, hip flexion and the crowding of the ilium anterosuperomedially should be approximately 70% and is frequently 100%.
• The practitioner maintains digital contact with the foramen point while the position of ease is held for 90 seconds, before a slow return to neutral is passively brought about (leg back to the table, contact released).
• Whether the sacral torsion is on a forward or backward axis it should respond to the same treatment protocol as described.
Note: Despite the extreme gentleness of all positional release methods (in general) and strain-counterstrain (in particular), in about a third of patients there will be a reaction in which soreness, fatigue, etc. may be noted, just as in more strenuous therapeutic measures. This reaction is considered to be the result of the homeostatic adaptation process of the organism in response to the treatment, which is a feature of many apparently very light forms of treatment. Since the philosophical basis for much bodywork involves the concept of the treatment acting as a catalyst, with the normalization or healing process being the prerogative of the body itself, the reaction described above is an anticipated part of the process and should be recognized as an indication of desirable change and not necessarily ‘bad’. The patient should therefore be forewarned to anticipate such symptoms for a day or two following any appropriate soft tissue manipulation. Suggestions can be given for relief (ice, heat, rest, movement, etc., as appropriate) should this occur.
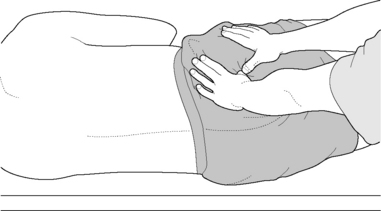
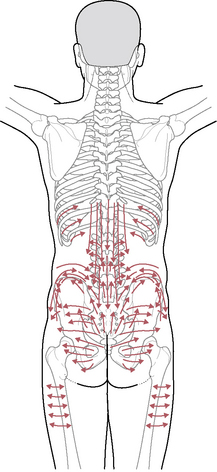
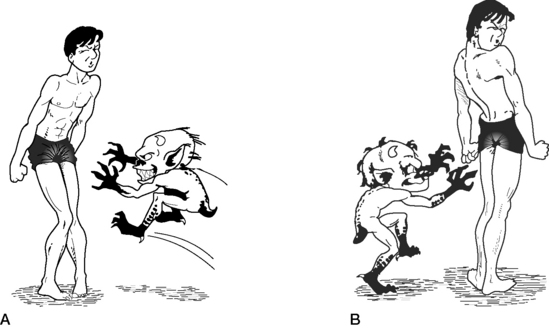
Mobilization with movement (MWM) treatment of SI joint dysfunction (Fig. 11.39)
See Chapter 9 for discussion of MWM methodology.
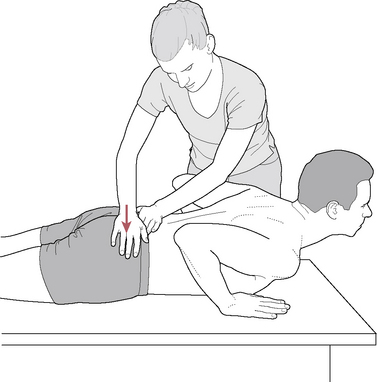
Figure 11.39 MWM for right SI joint with posterior innominate
(adapted with permission from Mulligan B 1999 Manual therapy. Plane View Services Ltd).
A positive seated flexion test identifies the dysfunctional sacroiliac side. The ilium on that side is evaluated as to whether it appears to be more anteriorly or posteriorly oriented (rotated) – see Figure 11.23 earlier in this chapter.
SI restriction with posterior innominate
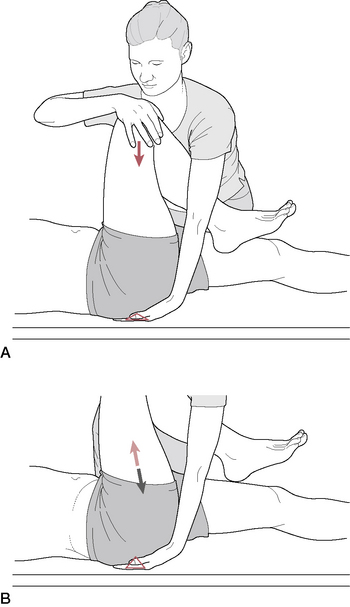
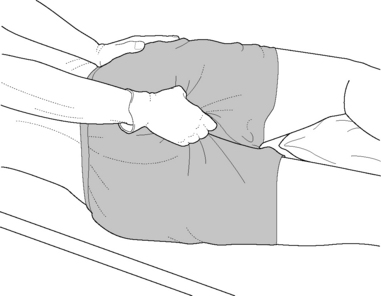
• If treating a restricted SI joint with a posterior innominate on that side, the patient is prone, with hands in position as though to do a press-up.
• The practitioner stands contralaterally and places her caudad hand (heel of hand, thenar eminence) close to the PSIS and applies lateral pressure to the posterior border of the ilium. There should be no pain.
• The patient is asked to rhythmically, using arm and back strength, perform a series of ‘half’ press-ups, 10 times (assuming no pain is noted; if pain is reported, the direction of thenar eminence pressure on the ilium is altered).
• The same sequence can be performed several times more (10 press-ups each time), following which reassessment of symptoms and seated flexion test should be undertaken.
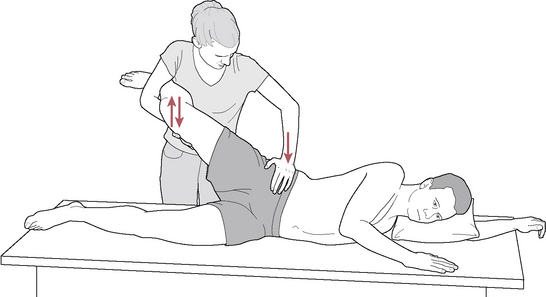
SI restriction with anterior innominate (Fig. 11.40)
• The patient is prone and the practitioner stands contralaterally, so that her caudad hand holds the ASIS, while her cephalad hand’s thenar or hypothenar eminence applies anteriorly directed (toward the floor) stabilizing pressure to the sacrum.
• The caudad hand eases the ilium toward the sacrum, painlessly, and the patient performs a series of 10 ‘half’ press-ups.
• This is repeated once or twice more, following which reassessment of symptoms and seated flexion test should be undertaken.