Adduction of the thigh
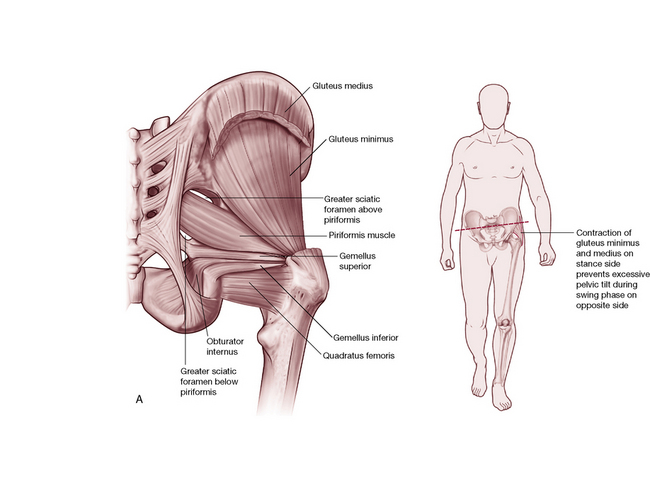
As mentioned with the pelvic discussion of these medial thigh muscles, adduction of the thigh includes moving the femur toward the mid-line from a neutral position or toward neutral from an abducted position. Adduction of the thigh is primarily achieved by the pectineus, adductors brevis, longus, magnus and minimus, gracilis, quadratus femoris (Platzer 2004), obturator externus (Kapandji 1987, Platzer 2004) and some fibers of gluteus maximus (Kapandji 1987, Platzer 2004). Kapandji (1987) also notes that the obturator internus and the hamstrings play a role in adduction (Platzer agrees with some hamstring action) while Travell & Simons (1992) note them to be antagonists to adduction. The adductor group can also play a role in lateral or medial rotation of the thigh (depending upon the starting position of the femur) while adductor magnus can contribute to extension of the thigh.
There exists considerable debate as to whether the adductors laterally or medially rotate the thigh. It is apparent that initial positioning of the thigh will most probably influence the role that the adductors play in rotation, as it does with many of the hip muscles. The movement these muscles produce will also be influenced by whether the femur is weight bearing or not, as well as whether the person is gait or stationary.
Gray’s anatomy (2005) notes:
Extensive or forcible adduction of the femur is not often required. Although the adductors can act in this way, they more commonly act as synergists in the complex pattern of gait activity, and to some degree controllers of posture … Magnus and longus are probably medial rotators of the thigh. The adductors are inactive during adduction of the abducted thigh in the erect posture (when gravity assists), but active in other postures, such as the supine position, or during adduction of the flexed thigh when standing.
Levangie & Norkin (2005) offer a supported theory that ‘the adductors function not as prime movers, but by reflex response to gait activities’. They also note:
Although the role of the adductor muscles may be less clear than that of other hip muscle groups, the relative importance of the adductors should not be underestimated. The adductors as a group contribute 22.5% of the total muscle mass of the lower extremity compared to only 18.4% for the flexors and 14.9% for the abductors.
The relationship of the muscles can be seen in cross-section (Fig. 12.20).
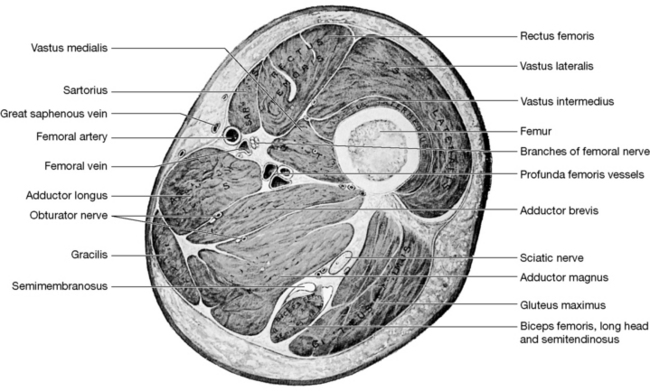
Figure 12.20 Transverse section through the right thigh at the level of the apex of the femoral triangle: proximal (superior) aspect
(reproduced with permission from Gray’s anatomy, 1995).
Gracilis (Fig. 12.21)
Attachments: From near the symphysis on the inferior ramus of the pubis to the medial proximal tibia (pes anserinus superficialis)
Innervation: Obturator nerve (L2–3)
Muscle type: Phasic (type 2), with tendency to weaken and lengthen if chronically stressed
Function: Adducts the thigh, flexes the knee when knee is straight, medially rotates the leg at the knee
Synergists: For thigh adduction: primarily adductor group and pectineus
Antagonists: To thigh adduction: the glutei and tensor fasciae latae
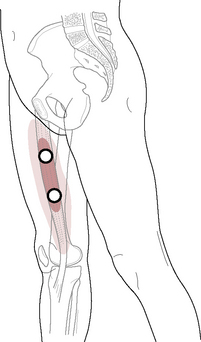
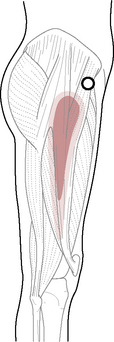
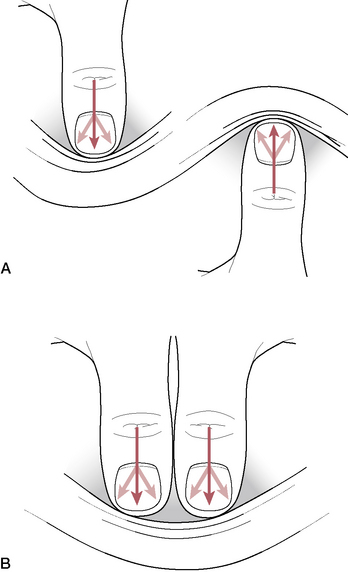
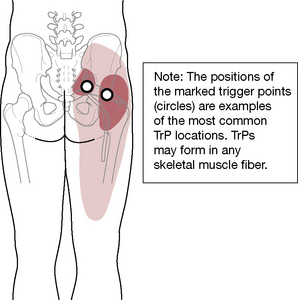
Figure 12.21 The trigger points of gracilis lie within its common target zone of referral
(adapted with permission from Travell & Simons 1992).
Pectineus (Fig. 12.22)
Attachments: From the pecten of the pubis to the femur (pectineal line) between the lesser trochanter and the linea aspera
Innervation: Femoral and obturator nerves (L2–4)
Muscle type: Phasic (type 2), with a tendency to weaken and lengthen if chronically stressed
Function: Flexes and adducts the thigh
Synergists: For thigh adduction-flexion action: iliopsoas, adductor group, rectus femoris, and gracilis
For thigh adduction: primarily adductor group and gracilis
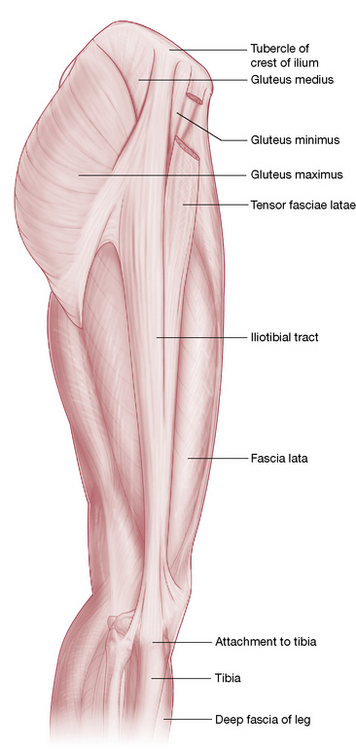
Antagonists: To flexion: gluteus maximus and hamstrings To adduction: gluteus medius and minimus, tensor fasciae latae and (sometimes) upper fibers of gluteus maximus
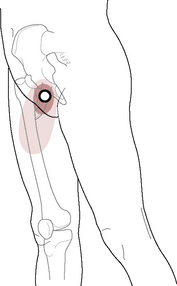
Figure 12.22 The trigger point referral pattern of pectineus
(adapted with permission from Travell & Simons 1992).
Adductor longus (Fig. 12.23)
Attachments: From the front of the pubis between the crest and symphysis to the middle third of the medial lip of linea aspera
Innervation: Obturator nerve (L2–4)
Muscle type: Postural (type 1), with tendency to shorten when chronically stressed
Function: Adducts and flexes thigh and has (controversial) axial rotation benefits, depending upon femur position (see below)
Synergists: For thigh adduction: remaining adductor group, gracilis and pectineus
Antagonists: To adduction: gluteus medius and minimus, tensor fasciae latae, upper fibers of gluteus maximus
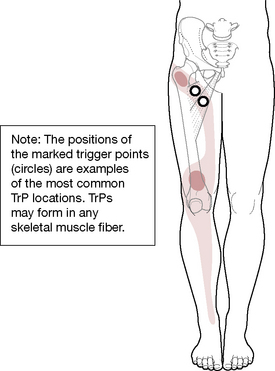
Figure 12.23 The trigger point referral pattern of adductor longus and brevis courses from the groin to just above the foot
(adapted with permission from Travell & Simons 1992).
Adductor brevis
Attachments: From the inferior ramus of the pubis to the upper third of the medial lip of the linea aspera
Innervation: Obturator nerve (L2–4)
Muscle type: Postural (type 1), with tendency to shorten when chronically stressed
Function: Adducts and flexes thigh and has (controversial) axial rotation benefits, depending upon femur position (see below)
Synergists: For thigh adduction: remaining adductor group, gracilis and pectineus
Antagonists: To flexion: gluteus maximus, hamstrings, portions of adductor magnus
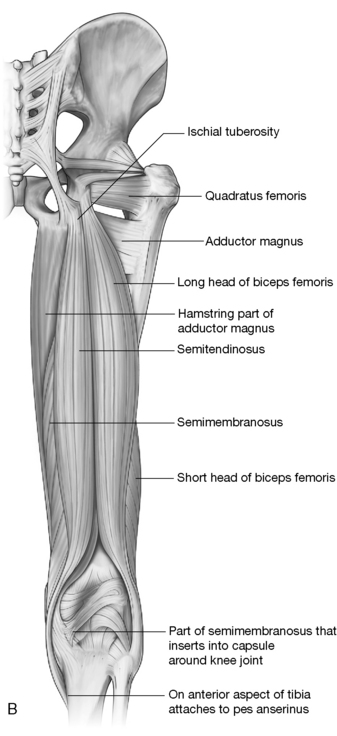
Adductor magnus (Figs 12.24, 12.25)
Attachments: From the inferior ramus of the ischium and pubis (anterior fibers) and the ischial tuberosity (posterior fibers) to the linea aspera (starting just below the lesser trochanter and continuing to the adductor hiatus) and to the adductor tubercle on the medial condyle of the femur
Innervation: Obturator nerve (L2–4), tibial portion of sciatic nerve (L4–S1)
Muscle type: Postural (type 1), with tendency to shorten when chronically stressed
Function: Adducts the thigh, flexes or extends the thigh depending upon which fibers contract, and medially rotates the femur; lateral axial rotation benefits may exist (Kapandji 1987, Platzer 2004, Rothstein et al 1991) – see below
Synergists: For thigh adduction: remaining adductor group, gracilis and pectineus
Antagonists: To adduction: gluteus medius and minimus, tensor fasciae latae, upper fibers of gluteus maximus
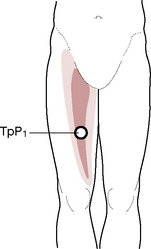
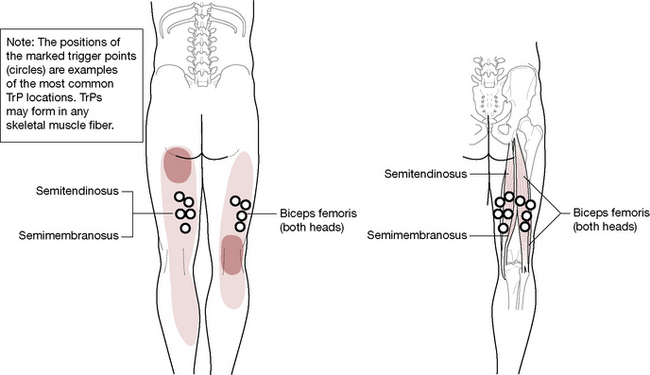
Figure 12.24 The trigger point referral pattern of adductor magnus covers the medial thigh and also (not illustrated) into the pelvis, including the pubic bone, vagina, rectum and bladder
(adapted with permission from Travell & Simons 1992).
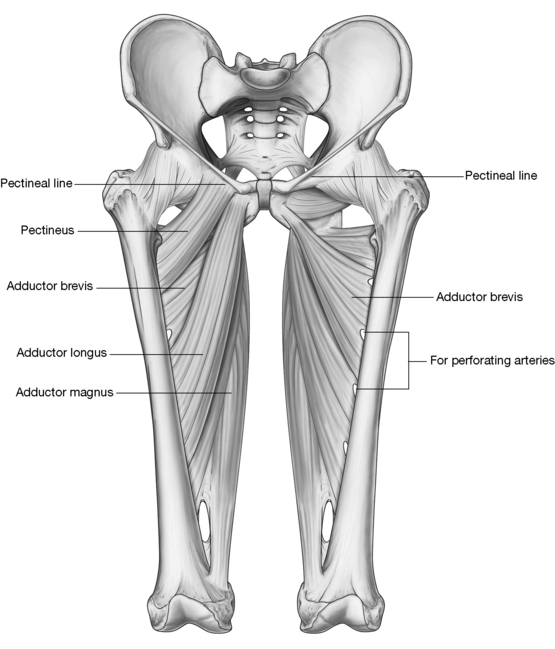
Figure 12.25 Thigh adductors are shown fully on the left side of this illustration. On the right side, the superficial layer is removed to reveal the underlying obturator externus, adductor brevis and the adductor magnus, which is the deepest and largest of the adductor group. Notice that the adductor magnus attaches distally to the adductor tubercle and forms the adductor hiatus, the opening through which passes the neurovascular components that serve most of the leg.
(Reproduced, with permission, from Gray’s anatomy for students, 2nd edn, 2010, Churchill Livingstone)
A thorough discussion of the adductors, including indications for assessment and treatment, is found in Chapter 11 on pp. 350–351 due to the extensive role they play in pelvic positioning. Adductor magnus is also treated with the hamstrings on pp. 441–442.
Travell & Simons (1992) note the following regarding the role of the adductors in walking.
• The adductor longus becomes active around the time of toe off, and the adductor magnus around the time of heelstrike during walking, jogging, running, and sprinting.
• The adductor magnus becomes active during ascent of stairs but is inactive during descent.
• It [adductor magnus] is also active when ‘stemming’ during skiing and while gripping the sides of the horse with the knees when riding. …
• During the early swing phase (pick up), the adductor magnus brings the limb toward the midline.
• During late swing phase, the adductors and gracilis help increase and maintain hip flexion for the forward reach of the limb.
• During the earliest part of the stance phase the gracilis may be functioning to assist the other pes anserinus muscles and the vastus medialis in controlling the valgus angulation of the knee as body weight is shifted onto that foot.
• During early stance, the ischiocondylar part of the adductor magnus is in a position to assist the hamstrings and gluteus maximus in restraining the tendency toward hip flexion that is produced by body weight.
• Later in stance, as weight is shifting toward and across the midline to the other foot, the adductor longus and adductor magnus restrain abduction, controlling the weight shift and adding stability.
Before beginning hands-on applications the following points should be considered. These are discussed more fully with the supine treatment of the adductors in Chapter 11, on pp. 353–354.
• The practitioner should discuss with the patient why this region needs to be treated.
• Only a mild pressure should be used until tissue tenderness has been assessed as these muscles are often exceptionally tender.
• If the adipose tissue ‘bunches up’ and prevents the smooth passage of the hands, short (2–3 inch) repetitious gliding strokes may be applied instead of long gliding strokes.
• The pubic attachments cannot be easily reached in the sidelying position, but are fully described in the supine version of this treatment in Chapter 11.
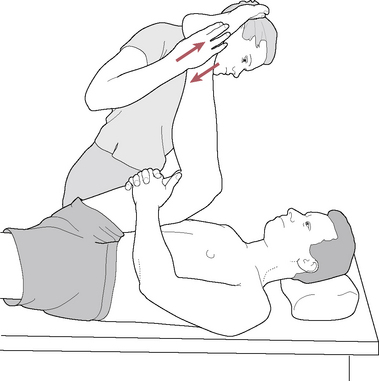
NMT for adductor muscle group: sidelying position
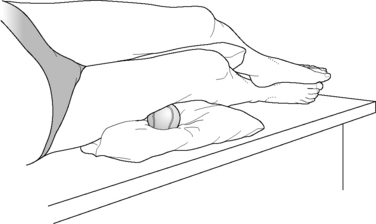
• The patient is in the sidelying position with the uppermost hip fully flexed and supported on a cushion or lying directly on the table if stretch of the piriformis and obturator internus is not uncomfortable. The lower leg is straight and the medial thigh of the lowermost leg is undraped to reveal the adductor muscles.
• The practitioner stands behind the patient at the level of the knee or sits on the table posterior to the lower leg if the table is sufficiently wide.
• The practitioner can visualize the outline of the sartorius, which forms the anterior boundary of the adductor muscle group. The hamstrings form the posterior boundary and the proximal attachments at the pubic region form the cephalad boundary, though the uppermost portion of the adductors is not readily accessible in this sidelying position. Caution should be exercised at the top of this region just distal to the inguinal ligament where the femoral artery, nerve and vein course into the thigh and where the femoral pulse can usually be palpated.
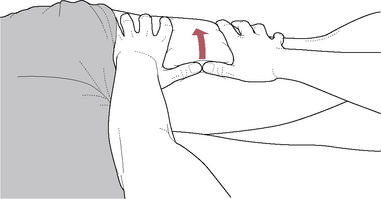
• Gliding strokes are applied to the medial thigh muscles from the region of the medial knee toward the pubic attachments, although the attachments will not be reached (Fig. 12.26).
• The strokes are repeated 4–5 times to the same tissue and then the thumbs are moved onto the next segment. The first gliding stroke will lie beside the sartorius, with the next line of the stroke lying beside the first and posterior to it. The gracilis muscle courses from the medial knee to the pubic bone and, when clothed, lies directly beneath the medial seam (inseam) of the pants. This muscle demarcates the boundary between the anterior and posterior thigh from a medial aspect. Since a large portion of adductor magnus lies posterior to the gracilis, the gliding strokes should be continued posteriorly until the hamstrings are encountered. Encroachment upon the hamstrings will indicate the point at which the adductor palpation ceases, although the gliding can be continued onto the hamstrings as well.
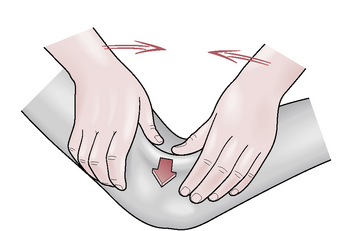
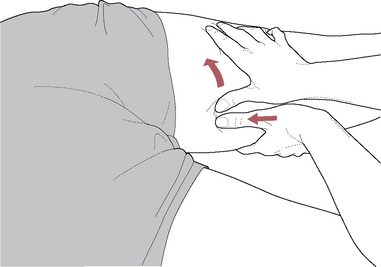
• Adductor magnus continues its course deep to the hamstrings. A double thumb stroke can be applied to separate the two muscle groups by applying one thumb onto the adductor magnus and the other thumb onto the hamstrings with a slight ‘separating’ pressure as the thumbs are slid along the length of the muscles (Fig. 12.26).
• The entire routine of application of gliding strokes may be performed 2–3 times to the adductor region in one session, if tolerable. The tenderness found in these muscles should decrease with each application. If, however, tenderness increases, lymphatic drainage techniques can be applied to the region and positional release techniques employed until local tissue health improves.
• The pubic attachments of the adductor muscles can best be treated with direct contact in a supine position, which is discussed in Chapter 11, pp. 353–354. as are MET and PRT treatment variations for these muscles. In a prone position, connective tissue between the medial hamstrings and adductor magnus can be encouraged to soften, as discussed later in this chapter on pp. 440–443.

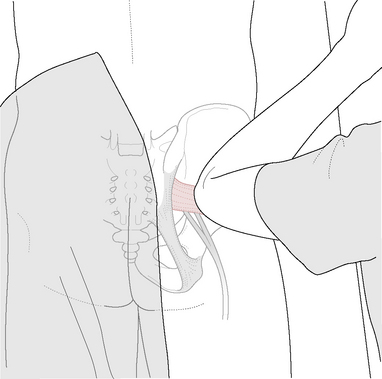
Figure 12.26 The adductor muscle bellies on the inner thigh of the lowermost leg are easily accessible in a sidelying position. After general gliding strokes are applied, specific work can be applied. Here, a double thumb stroke applies the pressure of one thumb onto the adductor magnus and the other thumb onto the hamstrings with a slight ‘separating’ pressure as the thumbs are slid along the length of the muscles. The groin attachments of the adductor muscles, however, are best treated in a supine position (see p. 354).