Naevi
A naevus is a benign proliferation of one or more of the normal constituent cells of the skin. Naevi may be present at birth or may develop later. The commonest naevi are those containing benign collections of melanocytic naevus cells, but other types of naevus are found (Table 1). Vascular naevi are dealt with on page 117.
Table 1 A classification of naevi
| Group | Example |
|---|---|
| Melanocytic | |
| Vascular | |
| Epidermal | |
| Connective tissue |
Tuberous sclerosis (p. 92) |
Melanocytic naevi
Melanocytic naevi (‘moles’) are common. They are present in most caucasoids but are less prevalent in mongoloids and black Africans.
Aetiopathogenesis and pathology
The naevus cells in melanocytic naevi are thought to be derived from melanocytes that migrate to the epidermis from the neural crest during embryonic development (p. 3). The reason for the development of naevi is unknown, but they seem to be an inherited trait in many families.
The position of the naevus cells within the dermis determines the type of naevus (Fig. 1). The junctional type has clusters of naevus cells at the dermoepidermal junction, the intradermal type has nests of naevus cells in the dermis and the compound naevus shows both components.
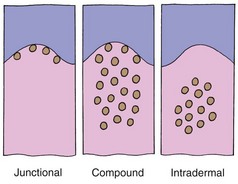
Fig. 1 Types of melanocytic naevus.
The site of the naevus cells, either at the dermoepidermal junction or in the dermis, or at both places, determines the type of melanocytic naevus.
Naevus cells produce melanin and, if the pigment is deep in the dermis, an optical effect can give the lesion a blue colour, as in a blue naevus.
Clinical presentation
A congenital naevus, that is one present at or soon after birth, is seen in about 1–3% of infants, but most naevi develop during childhood or adolescence. Their number reaches a peak in the third decade, and they tend to become less numerous thereafter. However, it is not unusual to see a few new naevi appear after the third decade, especially if provoked by excessive sun exposure or pregnancy. The average young white adult has between 20 and 50 melanocytic naevi. Dermoscopy is helpful in assessment (p. 20). The clinical features of different types of naevus are as follows:
 Congenital naevi. Present at or shortly after birth, they are usually more than 1 cm in size, vary in colour from light brown to black and often become protuberant and hairy. They can be disfiguring, as in the rare bathing trunk naevus, and carry a lifetime risk of up to 5% for the development of malignant melanoma (p. 102).
Congenital naevi. Present at or shortly after birth, they are usually more than 1 cm in size, vary in colour from light brown to black and often become protuberant and hairy. They can be disfiguring, as in the rare bathing trunk naevus, and carry a lifetime risk of up to 5% for the development of malignant melanoma (p. 102).
 Junctional naevi. These are flat macules, varying in size from 2 to 10 mm and in colour from light to dark brown (Fig. 2). They are usually round or oval in shape and have a predilection for the palms, soles and genitalia.
Junctional naevi. These are flat macules, varying in size from 2 to 10 mm and in colour from light to dark brown (Fig. 2). They are usually round or oval in shape and have a predilection for the palms, soles and genitalia.
 Intradermal naevi. The intradermal naevus is a dome-shaped papule or nodule that may be skin coloured or pigmented, and is most often seen on the face or neck.
Intradermal naevi. The intradermal naevus is a dome-shaped papule or nodule that may be skin coloured or pigmented, and is most often seen on the face or neck.
 Compound naevi. Compound naevi are usually less than 10 mm in diameter, have a smooth surface and vary in their degree of pigmentation (Fig. 3). Larger lesions may develop a warty or cerebriform appearance. They may occur anywhere on the skin surface.
Compound naevi. Compound naevi are usually less than 10 mm in diameter, have a smooth surface and vary in their degree of pigmentation (Fig. 3). Larger lesions may develop a warty or cerebriform appearance. They may occur anywhere on the skin surface.
 Spitz naevi. A Spitz naevus is a firm, reddish–brown, rounded nodule seen typically on the face or leg of a child. The initial growth may be rapid. Histologically, the naevus cells are proliferative, and the dermal blood vessels are dilated. Differentiation from malignant melanoma is important.
Spitz naevi. A Spitz naevus is a firm, reddish–brown, rounded nodule seen typically on the face or leg of a child. The initial growth may be rapid. Histologically, the naevus cells are proliferative, and the dermal blood vessels are dilated. Differentiation from malignant melanoma is important.
 Blue naevi. This variant, so-called because of its steely-blue colour, is usually solitary and is most common on the extremities, particularly the hands and feet.
Blue naevi. This variant, so-called because of its steely-blue colour, is usually solitary and is most common on the extremities, particularly the hands and feet.
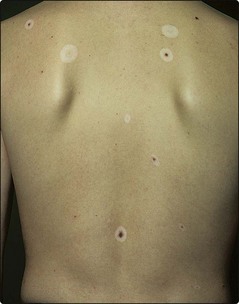
 Halo naevi. Halo (or Sutton’s) naevi are mainly seen on the trunk in children or adolescents and represent the destruction, by the body’s immune system, of naevus cells in a naevus. A white halo of depigmentation surrounds the pre-existing naevus that subsequently involutes (Fig. 4). This may be due to antimelanocyte autoimmune attack. There is an association with vitiligo. Multiple halo naevi often appear simultaneously.
Halo naevi. Halo (or Sutton’s) naevi are mainly seen on the trunk in children or adolescents and represent the destruction, by the body’s immune system, of naevus cells in a naevus. A white halo of depigmentation surrounds the pre-existing naevus that subsequently involutes (Fig. 4). This may be due to antimelanocyte autoimmune attack. There is an association with vitiligo. Multiple halo naevi often appear simultaneously.
 Becker’s naevi. This rare variant usually develops in adolescent males as a unilateral lesion on the upper back or chest (Fig. 5). Hyperpigmented at first, it later becomes hairy and is prone to acne. It may represent mosaicism.
Becker’s naevi. This rare variant usually develops in adolescent males as a unilateral lesion on the upper back or chest (Fig. 5). Hyperpigmented at first, it later becomes hairy and is prone to acne. It may represent mosaicism.
 Dysplastic naevi. Dysplastic (atypical) naevi show some irregularity in outline and in pigmentation (p. 103).
Dysplastic naevi. Dysplastic (atypical) naevi show some irregularity in outline and in pigmentation (p. 103).
Management
Over recent years, publicity in the media and in public health campaigns has promoted the early diagnosis of malignant melanoma. This has led to a greater public awareness about the significance of change in pigmented lesions, and many patients are now referred because of concern about their ‘moles’. Any change merits serious attention (p. 102). The differential diagnosis of melanocytic naevi is shown in Table 2. Naevi are excised because of:
 concern about malignancy, e.g. recent increase in size or itching
concern about malignancy, e.g. recent increase in size or itching
 an increased risk of malignant change, e.g. in a large congenital naevus
an increased risk of malignant change, e.g. in a large congenital naevus
 cosmetic reasons, e.g. ugly naevi, usually on the face or neck
cosmetic reasons, e.g. ugly naevi, usually on the face or neck
 repeated inflammation, e.g. bacterial folliculitis, often in hairy facial naevi
repeated inflammation, e.g. bacterial folliculitis, often in hairy facial naevi
 recurrent trauma, e.g. naevi on the back that catch on bra straps.
recurrent trauma, e.g. naevi on the back that catch on bra straps.
Table 2 Differential diagnosis of melanocytic naevi
| Lesion | Distinguishing features |
|---|---|
| Freckle | Tan-coloured macules on sun-exposed sites (p. 75) |
| Lentigine | Usually multiple, onset in later life (p. 75) |
| Seborrhoeic wart | Stuck-on appearance, warty lesions, may show keratin plugs, but easily confused (p. 94) |
| Haemangioma | Vascular but may show pigmentation |
| Dermatofibroma | On legs, elevated nodule, firm and pigmented (p. 94) |
| Pigmented basal cell carcinoma | Often on face, pearly edge, increase in size, can ulcerate, other photodamage may coexist |
| Malignant melanoma | Variable colour and outline, may have increased in size, be inflamed, bleed or be itchy (p. 102) |
All excised naevi should be sent for histology. Some clearly benign protuberant naevi that require removal for cosmetic reasons can be dealt with by shave biopsy (p. 110).
Epidermal naevi
Epidermal naevi are usually present at birth or develop in early childhood. They are warty, often pigmented and frequently linear (Fig. 6). Most are a few centimetres long, but they can be much larger and involve the length of a limb or the side of the trunk. They can be excised, but recurrence is common. A variant on the scalp, naevus sebaceus, carries a risk of malignant transformation and should be excised.
Connective tissue naevi
Connective tissue naevi are rare. They appear as smooth, skin-coloured papules or plaques and may be multiple. Coarse collagen bundles are seen in the dermis on histology. An example is the collagen-containing cobblestone naevus (shagreen patch) seen in tuberous sclerosis (p. 92).
Naevi
 Melanocytic naevi are very common, usually multiple, pigmented and benign. They appear during childhood or adolescence. Young white adults have 20–50. Variants include:
Melanocytic naevi are very common, usually multiple, pigmented and benign. They appear during childhood or adolescence. Young white adults have 20–50. Variants include:
 Epidermal naevi are warty, pigmented and often linear. Usually small, they are sometimes extensive. A scalp variant, naevus sebaceus, should be excised as it has malignant potential.
Epidermal naevi are warty, pigmented and often linear. Usually small, they are sometimes extensive. A scalp variant, naevus sebaceus, should be excised as it has malignant potential.
 Connective tissue naevi are skin-coloured papules composed of coarse collagen in the dermis. They can occur as cobblestone naevi (shagreen patches) in tuberous sclerosis.
Connective tissue naevi are skin-coloured papules composed of coarse collagen in the dermis. They can occur as cobblestone naevi (shagreen patches) in tuberous sclerosis.