Radiation Protection
After completion of this chapter, the student will be able to do the following:
• Define the key words associated with radiation protection
• Describe in detail the basics of patient protection before x-ray exposure
• Discuss the different types of filtration, and state the recommended total filtration for dental x-ray machines operating above and below 70 kVp
• Describe the collimator used in dental x-ray machines, and state the recommended diameter of the useful beam at the patient’s skin
• List six ways to protect the patient from excessive radiation during x-ray exposure
• Describe the importance of receptor handling and processing after patient exposure to x-radiation
• Discuss operator protection in terms of adequate distance, shielding, and avoidance of the useful beam
• Describe personnel and equipment monitoring devices used to detect radiation
• Discuss radiation exposure guidelines, including radiation safety legislation, maximum permissible dose (MPD), maximum accumulated dose (MAD), and the ALARA concept
• Discuss with the dental patient what radiation protection steps will be used before, during, and after exposure to x-radiation
Many of the early pioneers in dental radiography suffered from the adverse effects of radiation. As discussed in Chapter 1, some of these pioneers lost their fingers, limbs, and, ultimately, lives to excessive doses of radiation. The hazards of radiation are now well documented, and radiation protection measures can be used to minimize radiation exposure to both the dental patient and the dental radiographer. The purpose of this chapter is to discuss patient protection before, during, and after exposure to x-rays; to detail operator protection methods; and to present radiation exposure and safety guidelines. In addition, this chapter includes a discussion of patient education about radiation protection.
Patient Protection
X-radiation causes biologic changes in living cells and adversely affects all living tissues. With the use of proper patient protection techniques, the amount of x-radiation received by a dental patient can be minimized. Patient protection techniques can be used before, during, and after exposure to x-radiation.
Before Exposure
Patient protection measures can be used before any x-radiation exposure. Proper prescribing of dental radiographs and the use of equipment that complies with state and federal radiation guidelines can minimize the amount of x-radiation that a dental patient receives.
Prescribing Dental Radiographs
The first important step in limiting the amount of x-radiation received by a dental patient is the proper prescribing, or ordering, of dental radiographs. The person responsible for prescribing dental radiographs is the dentist. The dentist uses professional judgment to make decisions about the number, type, and frequency of dental radiographs.
Every patient’s dental condition is different, and consequently, every patient should be evaluated for dental radiographs on an individual basis. A radiographic examination should never include a predetermined number of radiographs, nor should radiographs be taken at predetermined time intervals. For example, the dentist who prescribes a set number of radiographs (e.g., four bite-wings) at a set interval (e.g., every 6 months) for every patient is not taking the individual needs of the patient into consideration.
The American Dental Association (ADA), in conjunction with the U.S. Food and Drug Administration (FDA), has adopted guidelines for prescribing the number, type, and frequency of dental radiographic procedures. These guidelines summarize the recommendations that promote patient protection in diagnostic radiography (Table 5-1). For the latest information and changes on prescribing dental radiographs, visit www.ADA.org and www.FDA.gov.
TABLE 5-1
Guidelines for Prescribing Dental Radiographs*
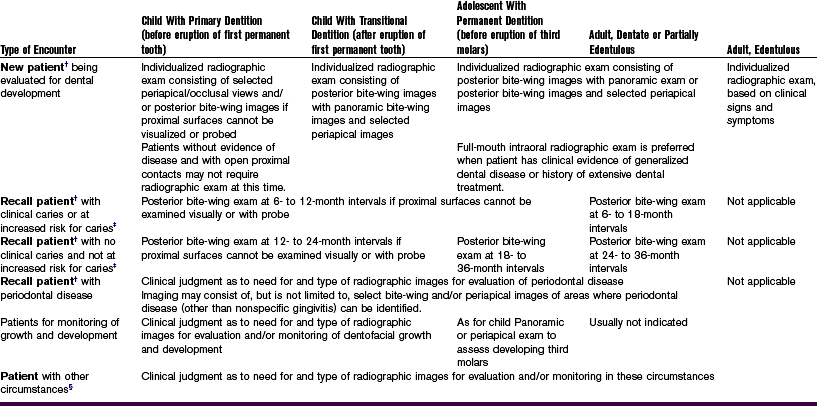
*The recommendations in this chart are subject to clinical judgment and may not apply to every patient. They are to be used by dentists only after reviewing the patient’s health history and completing a clinical examination. Because every precaution should be taken to minimize radiation exposure, protective thyroid collars and aprons should be used whenever possible. This practice is strongly recommended for children, women of childbearing age, and pregnant women.
†Clinical situations for which radiography may be indicated include, but are not limited to, the following:
A Positive historical findings: (1) previous periodontal or endodontic treatment, (2) history of pain or trauma, (3) familial history of dental anomalies, (4) postoperative evaluation of healing, (5) remineralization monitoring, or (6) presence of implants or evaluation for implant placement
B Positive clinical signs/symptoms: (1) clinical evidence of periodontal disease, (2) large or deep restorations, (3) deep carious lesions, (4) malposed or clinically impacted teeth, (5) swelling, (6) evidence of dental/facial trauma, (7) mobility of teeth, (8) sinus tract (“fistula”), (9) clinically suspected sinus pathology, (10) growth abnormalities, (11) oral involvement in known or suspected systemic disease, (12) positive neurologic findings in head and neck, (13) evidence of foreign objects, (14) pain and/or dysfunction of temporomandibular joint, (15) facial asymmetry, (16) abutment teeth for fixed or removable partial prosthesis, (17) unexplained bleeding, (18) unexplained sensitivity of teeth, (20) unusual tooth morphology, calcification, or color, (21) unexplained absence of teeth, or (22) clinical erosion.
‡Factors increasing risk for caries may include, but are not limited to, the following: (1) high level of caries experience or demineralization, (2) history of recurrent caries, (3) high titers of carcinogenic bacteria, (4) existing restoration(s) of poor quality, (5) poor oral hygiene, (6) inadequate fluoride exposure, (7) prolonged nursing (bottle or breast), (8) frequent high-sucrose content in diet, (9) poor dental health in family, (10) developmental or acquired enamel defects, (11) development of acquired disability, (12) xerostomia, (13) genetic abnormality of teeth, (14) many multisurface restorations, (15) chemotherapy and/or radiation therapy, (16) eating disorders, (17) drug/alcohol abuse, or (18) irregular dental care.
§Including, but not limited to, the following: (1) proposed or existing implants, (2) pathology, (3) restorative/endodontic needs, (4) treated periodontal disease, or (5) caries remineralization.
Modified from American Dental Association, US Food and Drug Administration: The selection of patients for dental radiographic examinations: www.ada.org: Accessed May 26, 2005.
Proper Equipment
Another important step in limiting the amount of x-radiation a dental patient receives is the use of proper equipment. The dental x-ray tubehead must be equipped with appropriate aluminum filters, lead collimator, and position-indicating device.
Filtration: Two types of filtration are used in the dental x-ray tubehead: inherent filtration and added filtration.
Inherent Filtration: Inherent filtration takes place when the primary beam passes through the glass window of the x-ray tube, the insulating oil, and the tubehead seal. The inherent filtration of the dental x-ray machine is approximately 0.5 to 1.0 millimeter (mm) of aluminum. Inherent filtration alone does not meet the standards regulated by state and federal laws. Therefore, added filtration is required.
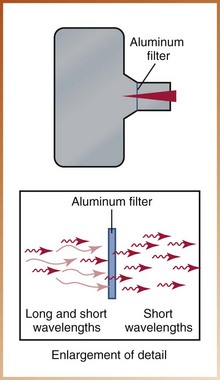
Added Filtration: Added filtration refers to the placement of aluminum discs in the path of the x-ray beam between the collimator and the tubehead seal in the dental x-ray machine (Figure 5-1). Aluminum discs can be added to the tubehead in 0.5-mm increments. The purpose of the aluminum discs is to filter out the longer-wavelength, low-energy x-rays from the x-ray beam (Figure 5-2). The low-energy, longer wavelength x-rays are harmful to the patient and are not useful in diagnostic radiography. Filtration of the x-ray beam results in a higher energy and more penetrating useful beam.
Total Filtration: State and federal laws regulate the required thickness of total filtration (inherent plus added filtration). Dental x-ray machines operating at or below 70 kilovoltage peak (kVp) require a minimum total of 1.5 mm aluminum filtration, and machines operating above 70 kVp require a minimum total of 2.5 mm aluminum filtration.
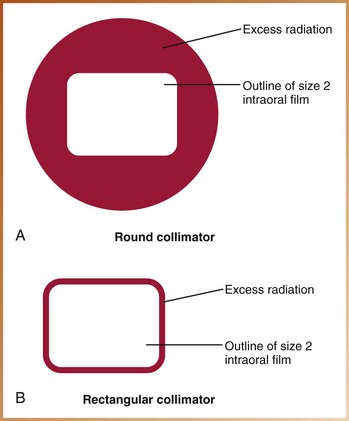
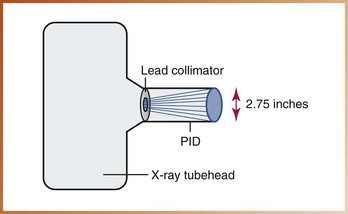
Collimation: Collimation is used to restrict the size and shape of the x-ray beam and to reduce patient exposure. A collimator, or lead plate with a hole in the middle, is fitted directly over the opening of the machine housing where the x-ray beam exits the tubehead (Figure 5-3).
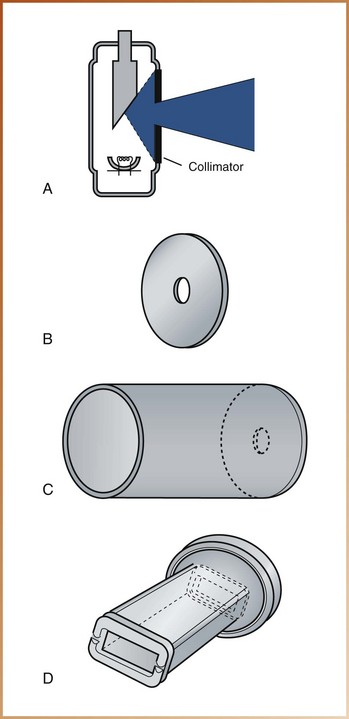
FIGURE 5-3 A, Collimation of an x-ray beam (shown in color) is achieved by restricting its useful size. B, Diaphragm collimator. C, Tubular collimator. D, Rectangular collimator. (From White SC, Pharoah MJ: Oral radiology: principles and interpretation, ed 5, St Louis, 2009, Mosby.)
A collimator may have either a round or rectangular opening (Figure 5-4). A rectangular collimator restricts the size of the x-ray beam to an area slightly larger than a size 2 intraoral film and significantly reduces patient exposure. A circular collimator produces a cone-shaped beam that is 2.75 inches in diameter, considerably larger than a size 2 intraoral film (Figure 5-5A). Rectangular collimators may also be added to the open end of a circular position-indicating device (PID) to reduce the amount of tissue being radiated (Figure 5-5B). When using a circular collimator, federal regulations require that the x-ray beam be collimated to a diameter of no more than 2.75 inches as it exits from the position-indicating device and reaches the skin of the patient (Figure 5-6).
Position-Indicating Device: The position-indicating device (PID), or cone, appears as an extension of the x-ray tubehead and is used to direct the x-ray beam. Three basic types of PIDs are currently used: (1) conical, (2) rectangular, and (3) round.
The conical PID appears as a closed, pointed plastic cone. When x-rays exit from the pointed cone, they penetrate the plastic and produce scatter radiation (Figure 5-7). To eliminate cone-produced scatter radiation, the conical PID is no longer used in dentistry. Open-ended, lead-lined rectangular or round PIDs limit the occurrence of scatter radiation (Figure 5-8).
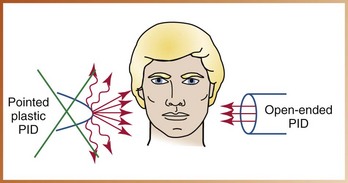
FIGURE 5-7 A plastic, pointed position-indicating device (PID) produces scatter radiation and is no longer used in dentistry.
Both rectangular and round PIDs are typically available in two lengths: short (8-inch) long (16-inch). The long PID is preferred because less divergence of the x-ray beam occurs (Figure 5-9).
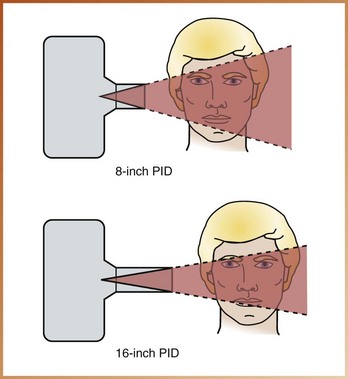
FIGURE 5-9 Compared with a short (8-inch) position-indicating device (PID), the longer (16-inch) PID is preferred because it produces less divergence of the x-ray beam.
Of the three types of PID, the rectangular type is most effective in reducing patient exposure.
During Exposure
Patient protection measures are used during x-ray exposure as well as before exposure. A thyroid collar, lead apron, fast film or digital imaging, and beam alignment devices are all used during x-ray exposure to limit the amount of radiation received by the patient. Proper selection of exposure factors and good technique further protect the patient from excessive exposure to x-radiation.
Thyroid Collar
The thyroid collar is a flexible lead shield that is placed securely around the patient’s neck to protect the thyroid gland from scatter radiation (Figure 5-10). The lead prevents radiation from reaching the gland and protects the highly radiosensitive tissues of the thyroid. The thyroid collar may exist as a separate shield or as part of the lead apron.

FIGURE 5-10 Thyroid collar. (From Bird DL, Robinson DS: Modern dental assisting, ed 10, St Louis, 2012, Saunders.)
The thyroid gland is exposed to x-radiation during oral radiographic procedures because of its location. The use of the thyroid collar is recommended for all intraoral exposures. However, use of the thyroid collar is not recommended with extraoral exposures because it obscures information and results in a nondiagnostic image.
Lead Apron
The lead apron is a flexible shield placed over the patient’s chest and lap to protect the reproductive and blood-forming tissues from scatter radiation; the lead prevents the radiation from reaching these radiosensitive organs (Figure 5-11). Use of a lead apron is recommended for both intraoral and extraoral exposures. Many state laws mandate the use of a lead apron on all patients. Recently, lead-free aprons made of alloy sheeting have become available for use during intraoral or panoramic radiography. Without the weight of lead, these aprons weigh 30% less and are comfortable and easy to handle while providing the same protection as does the traditional lead apron.
Fast Film
Fast film is the most effective method of reducing a patient’s exposure to x-radiation. Fast film is available for both intraoral and extraoral radiography. Currently, F-speed film, or InSight, is the fastest intraoral film available. Before the introduction of F-speed film, E-speed film, or Ektaspeed, was the fastest film available. F-speed film provides an additional 20% reduction in exposure over E-speed films (and 60% reduction in exposure from earlier D-speed film, or Ultra-Speed).
When compared with traditional film radiography, digital imaging requires less radiation exposure of the patient. The lowered absorbed dose is significant with regard to patient protection from excessive radiation. Digital imaging is discussed in detail in Chapter 25.
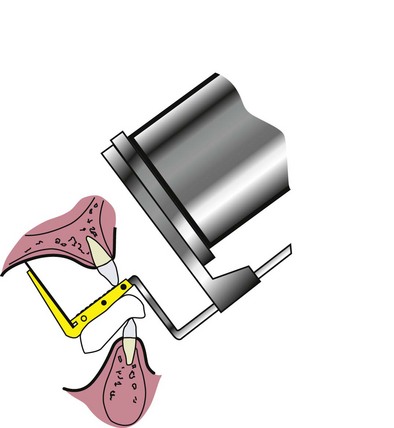
Beam Alignment Devices
Beam alignment devices are also effective in reducing a patient’s exposure to x-radiation. A beam alignment device helps stabilize the receptor in the mouth and reduces the chances of movement (Figure 5-12).
Exposure Factor Selection
Exposure factor selection also limits the amount of x-radiation exposure a patient receives. The dental radiographer can control the exposure factors by adjusting the kilovoltage peak, milliamperage, and time settings on the control panel of the dental x-ray machine. A setting of 70 to 90 kVp keeps patient exposure to a minimum. On some dental x-ray units, the kilovoltage peak and milliamperage settings are preset by the manufacturer and cannot be adjusted. (Chapter 3 discusses exposure factors and their effect on radiographs.)
Proper Technique
Proper technique helps ensure the diagnostic quality of images and reduce the amount of exposure a patient receives. Images that are nondiagnostic must be retaken; this results in additional exposure of the patient to radiation. Retakes must be avoided at all times.
To produce diagnostic images, the radiographer must have a thorough knowledge of the techniques most often used in dental radiography. Common approaches are the paralleling technique, bisecting technique, and bite-wing technique (see Chapters 17, 18 and 19, respectively). In addition to knowing how each receptor is exposed, an organized routine is important for the effective application of a technique.
After Exposure
The radiographer’s role in limiting the amount of x-radiation received by a patient does not end during exposure. After the receptors have been exposed, they must be handled and processed. Meticulous handling and proper processing techniques are critical for the production of high-quality diagnostic images.
Proper Film/Sensor Handling
Proper film and/or sensor handling is necessary to produce diagnostic images and to limit patient exposure to x-radiation. From the time the receptors are exposed until they are processed or retrieved, careful handling is crucial. Artifacts caused by improper handling result in nondiagnostic images (see Chapter 9). A nondiagnostic image must be retaken, which exposes the patient to excessive radiation.
Proper Film Processing/Image Retrieval
Proper film processing (developing) and proper retrieval of digital images are also necessary to produce diagnostic images and to limit patient exposure to x-radiation. Improper film processing or image retrieval can render images nondiagnostic, thereby requiring retakes and needlessly exposing the patient to excessive x-radiation.
Operator Protection
The dental radiographer must use proper protection measures to avoid occupational exposure to x-radiation (e.g., primary radiation, leakage radiation, scatter radiation). The use of proper operator protection techniques can minimize the amount of radiation that a dental radiographer receives. Operator protection measures include following protection guidelines and using radiation-monitoring devices.
Protection Guidelines
The purpose of operator protection guidelines is to provide the dental radiographer with the basic safety information needed when working with x-radiation. Such guidelines are based on the following rule: The dental radiographer must avoid the primary beam. Operator protection guidelines include recommendations on distance, position, and shielding.
Distance Recommendations
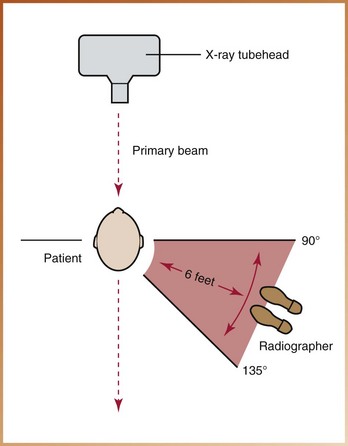
One of the most effective ways for the operator to avoid the primary beam and limit x-radiation exposure is to maintain an adequate distance during exposure. The dental radiographer must stand at least 6 feet away from the x-ray tubehead during x-ray exposure. When maintaining this distance is not possible, a protective barrier must be used.
Position Recommendations
Another important way for the operator to avoid the primary beam is to maintain proper positioning during x-ray exposure. To avoid the primary beam, which travels in a straight line, the dental radiographer must position himself or herself perpendicular to the primary beam, or at a 90-degree to 135-degree angle to the beam (Figure 5-13).
Shielding Recommendations
Adequate shielding can greatly reduce the occupational exposure of the dental radiographer. Protective barriers that absorb the primary beam can be incorporated into the office design, thus protecting the operator from primary and scatter radiation. Whenever possible, the dental radiographer should stand behind a protective barrier, such as a wall, during x-ray exposure. Most dental offices incorporate adequate shielding in walls through the use of several thicknesses of common construction materials such as drywall.
Radiation Monitoring
Radiation monitoring can also be used to protect the dental radiographer and includes the monitoring of both equipment and personnel. The use of radiation monitoring can identify excessive occupational exposure.
Equipment Monitoring
Dental x-ray machines must be monitored for leakage radiation. Leakage radiation is any radiation, with the exception of the primary beam, that is emitted from the dental tubehead. For example, if a dental x-ray tubehead has a faulty tubehead seal, leakage radiation results. Dental x-ray equipment can be monitored for leakage radiation through the use of a film device that can be obtained through the state health department or from the manufacturers of dental x-ray equipment.
Personnel Monitoring
The amount of x-radiation that reaches the body of the dental radiographer can be measured through the use of a personnel-monitoring device known as a radiation monitoring badge. A radiation monitoring badge can be obtained from a badge service company.
The radiation monitoring badge consists of a piece of radiographic film in a plastic holder (Figure 5-14). Each radiographer should have his or her own badge; the badge should be worn at waist level whenever the dental radiographer is exposing x-ray films or digital sensors. When badges are not worn, they should be stored in a radiation-safe area. A radiation monitoring badge should never be worn when the radiographer is undergoing x-ray exposure.

FIGURE 5-14 A radiation monitoring badge is used to measure the radiation exposure received by the dental radiographer. (From Bird DL, Robinson DS: Modern dental assisting, ed 10, St Louis, 2012, Saunders.)
After the dental radiographer has worn the badge for a specified interval (e.g., 1 week, 1 month), the badge is returned to the service company. The company processes and evaluates the badge for exposure and then provides the dental office with an exposure report for each radiographer.
Radiation Exposure Guidelines
All x-radiation is harmful. Radiation exposure guidelines have therefore been established to protect the patient and operator from excessive exposure. These guidelines include radiation safety legislation and exposure limits for the general public and for persons who are occupationally exposed to radiation. Strict adherence to radiation exposure guidelines is mandatory for all dental radiographers.
Radiation Safety Legislation
Radiation safety legislation has been established at both state and federal levels to protect the patient, the operator, and the general public from radiation hazards. At the federal level, the Radiation Control for Health and Safety Act was enacted in 1968 to standardize the operation of x-ray equipment. Also, the federal Consumer-Patient Radiation Health and Safety Act was enacted in 1981 to address the issues of the education and certification of persons operating radiographic equipment.
Radiation legislation in the United States varies greatly from state to state; the dental radiographer must be familiar with the laws that apply to his or her workplace. For example, in some states, before a dental radiographer can expose patients to radiation, he or she must successfully complete a radiation safety examination.
Maximum Permissible Dose
Radiation protection standards dictate the maximum dose of radiation that an individual can receive. The maximum permissible dose (MPD) is defined by the National Council on Radiation Protection and Measurements (NCRP) as the maximum dose equivalent that a body is permitted to receive within a specific period. The MPD is the dose of radiation that the body can endure with little or no injury.
The NCRP published the complete set of basic recommendations specifying dose limits for exposure to ionizing radiation. This most recent report in 2003 states that the current MPD for occupationally exposed persons, or those who work with radiation (e.g., dental radiographers), is 5.0 rems/year (0.05 Sv/year). For nonoccupationally exposed persons, the current MPD is 0.1 rem/year (0.001 Sv/year). The MPD for an occupationally exposed pregnant woman is the same as that for a nonoccupationally exposed person, or 0.1 rem/year (0.001 Sv/year).
Maximum Accumulated Dose
Occupationally exposed workers must not exceed an accumulated lifetime radiation dose. This is referred to as the maximum accumulated dose (MAD). MAD is determined by a formula based on the worker’s age. To determine the MAD for an occupationally exposed person, the following formula is used:
where N refers to the person’s age in years. (Note that the number 18 refers to the minimum required age of a person who works with radiation.)
ALARA Concept
The ALARA (As Low As Reasonably Achievable) concept states that all exposure to radiation must be kept to a minimum. To provide protection to both patients and operators, every possible method of reducing exposure to radiation should be employed to minimize risk. The radiation protection measures detailed in this chapter can be used to minimize patient and operator exposure, thus keeping radiation exposure “as low as reasonably achievable.”
Radiation Protection and Patient Education
Patients often have questions about radiation exposure. The dental radiographer must be prepared to answer such questions and to educate the dental patient about radiation protection topics. Patient education about radiation protection may take the form of an informal conversation or printed literature.
The dental radiographer must be prepared to explain exactly how patients are protected before, during, and after x-ray exposure. An informal discussion can take place as the dental radiographer prepares the patient for x-ray exposure. For example, while placing the lead apron and thyroid collar on the patient, the dental radiographer can make the following comments:
• “Before we get started, let me tell you just how our office does all that is possible to protect you from unnecessary radiation.”
• “Before we expose you to any x-rays, the dentist custom-orders your x-rays based on your individual needs. The x-ray equipment we use is frequently tested to ensure that state and federal radiation safety guidelines are met.”
• “During x-ray exposure, we use a thyroid collar and a lead apron to protect your body from excessive radiation. We use the fastest film available and a device to hold the film so that your fingers are not exposed to radiation. We also use an effective technique so that we can avoid making mistakes that require further exposure.”
• If using digital radiography: “Our office utilizes digital imaging procedures which reduce your exposure to radiation significantly when compared with traditional, film-based radiography.”
• “Even after your dental x-ray films have been taken, we take steps to process the films carefully so that we don’t have to take them again.”
• “Hopefully, this quick review of radiation protection techniques has answered some of the questions you may have about dental x-rays. Do you have any other questions before we begin?”
In addition to such an informal discussion, printed handouts or pamphlets outlining the steps used to protect patients from excessive radiation can be provided to the patient. Pamphlets on radiation protection can be placed in the reception area or in the room where dental radiographs are taken.
Summary
• Before x-ray exposure, proper prescribing of dental radiographs and proper use of radiographic equipment can minimize the amount of radiation that a patient receives.
• The dentist must prescribe radiographs on the basis of the individual needs of patients.
• In the x-ray tubehead, aluminum discs are used to filter out the longer-wavelength, low-energy x-rays from the x-ray beam.
• In the x-ray tubehead, a collimator (lead plate with a hole in the middle) is used to restrict the size and shape of the x-ray beam.
• A position-indicating device (PID) is used to direct the x-ray beam; the rectangular PID is most effective in reducing patient exposure to x-rays.
• A thyroid collar, a lead apron, fast film, digital imaging, and film-holding devices can be used during x-ray exposure to protect the patient from excessive exposure to radiation. Proper selection of exposure factors and good technique can also be used to protect the patient.
• After x-ray exposure, careful film/sensor handling, film-processing techniques, and image retrieval are critical for the production of diagnostic images.
• During x-ray exposure, the dental radiographer must always follow operator protection guidelines; he or she must avoid the primary beam (by maintaining an adequate distance) and use proper positioning and shielding.
• The dental radiographer must never hold a receptor or the tubehead in place for a patient during x-ray exposure.
• Radiation monitoring must include the monitoring of both equipment and personnel.
• Federal and state laws protect the patient, the operator, and the general public from radiation hazards.
• Exposure limits have been established for the general public and persons who work with radiation. The maximum permissible dose (MPD) for persons who work with radiation (e.g., dental radiographers) is 5.0 rems/year (0.05 Sv/year), and the MPD for persons who do not work with radiation is 0.1 rem/year (0.001 Sv/year).
• The ALARA (as low as reasonably achievable) concept states that all exposure to radiation must be kept to a minimum.
• The dental radiographer must be prepared to explain to patients how they are protected before, during, and after x-ray exposure.
Bernstein, DI, et al. Perceived quality of radiographic images after rapid processing of D- and F-speed direct-exposure intraoral x-ray films. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(4):486–491.
Frommer, HH, Savage-Stabulas, JJ, Operator protection. Radiology for the dental professional, ed 9, St Louis, Mosby, 2011.
Frommer, HH, Savage-Stabulas, JJ, Patient protection. Radiology for the dental professional, ed 9, St Louis, Mosby, 2011.
Haring, JI, Lind, LJ. The importance of dental radiographs and interpretation. In: Radiographic interpretation for the dental hygienist. Philadelphia: Saunders; 1993.
Johnson, ON, Thomson, EM, Patient relations and education. Essentials of dental radiography for dental assistants and hygienists, ed 8, Pearson, Upper Saddle River, NJ, 2007.
Johnson, ON, Thomson, EM, Radiation protection. Essentials of dental radiography for dental assistants and hygienists, ed 8, Pearson, Upper Saddle River, NJ, 2007.
Langland, OE, Langlais, RP, Preece, JW, Radiologic health and protection. Principles of dental imaging, ed 2, Baltimore, Lippincott Williams and Wilkins, 2002.
Miles, DA, Van Dis, ML, Jensen, CW, Ferretti, A, Intraoral radiographic technique. Radiographic imaging for the dental team, ed 4, St Louis, Saunders, 2009.
Miles, DA, Van Dis, ML, Jensen, CW, Ferretti, A, Radiation biology and protection. Radiographic imaging for the dental team, ed 4, St Louis, Saunders, 2009.
National Council on Radiation Protection and Measurements (NCRP): Limitation of exposure to ionizing radiation, NCRP Report No 116, 1993, NCRP.
White, SC, Pharoah, MJ, Health physics. Oral radiology: principles of interpretation, ed 6, St Louis, Mosby, 2009.
American Dental Association (ADA), www.ada.org/prof/resources/topics/radiography.asp.
U.S. Food and Drug Administration (FDA), www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures.
True or False
____1. Every patient should be evaluated individually for dental radiographs.
____2. The 8-inch PID is more effective than the 16-inch PID in reducing radiation exposure of the patient.
____3. Pointed cones should not be used because of increased scatter radiation.
____4. The thyroid collar must be worn for both intraoral and extraoral exposures.
____5. If necessary, the dental radiographer may hold a receptor in the patient’s mouth to ensure a diagnostic image.
Multiple Choice
____6. Which of the following describes the use of a filter in a dental x-ray tubehead?
a. A filter reduces the size and shape of the beam.
b. A filter removes low-energy x-rays.
c. A filter removes the dose of radiation to the thyroid gland.
____7. Which of the following is not a component of inherent filtration?
____8. Which of the following is the most effective method of reducing patient exposure to radiation?
____9. Which of the following position-indicating devices is most effective in reducing patient exposure?
____10. Which of the following devices restricts the size and shape of the x-ray beam?
____11. Which of the following is used as a collimator?
____12. Which of the following describes the function of filtration?
____13. Which of the following is the recommended size of the beam at the patient’s face?
____14. Which of the following terms describes the dose of radiation that the body can endure with little or no chance of injury?
____15. Which of the following is true of radiation monitoring badges?
Fill in the Blank
16. Provide the requirements for proper filtration:
a. Machines operating at 70 kVp or lower require __________ mm aluminum.
b. Machines operating above 70 kVp require __________ mm aluminum.
17. State the angle that the dental radiographer should stand to the primary beam:__________ degrees.
18. State the formula for maximum accumulated dose:
19. State the maximum permissible dose for occupationally exposed persons: __________ rems/year (__________ Sv/year).
20. State the maximum permissible dose for nonoccupationally exposed persons: __________ rem/year (__________ Sv/year).