Chapter 53The Cervical Spine and Soft Tissues of the Neck
This chapter discusses disorders of the neck that may give rise to lameness or poor performance or result in an abnormal neck shape, abnormal neck posture at rest or while moving, or neck stiffness. Transient neurological conditions, conditions caused by trauma resulting in other injuries, and gait abnormalities that may be confused with lameness are considered, but those associated with compression of the cervical spinal cord are discussed in Chapter 60.
Anatomy
The neck consists of seven cervical vertebrae, which articulate both by intercentral articulations and by synovial articulations, which have large joint capsules to accommodate the degree of movement between adjacent vertebrae. Interposed between the vertebral bodies are intervertebral fibrocartilages to which is attached the dorsal longitudinal ligament, which lies on the floor of the vertebral canal. The ligamentum flavum connects the arches of adjacent vertebrae. The atlas (the first cervical vertebra) and the axis (the second cervical vertebra) have a unique shape and specialized joints. The atlanto-occipital joint is a ginglymus joint, which permits flexion and extension and also a small amount of lateral oblique movement. The atlantoaxial joint is a trochoid or pivot joint; the atlas and head rotate on the axis. The ligament of the dens is strong and fan shaped and extends from the dorsal surface of the odontoid peg (dens) to the ventral arch of the axis. The ligamentum nuchae extends from the occiput to the withers and consists of funicular and lamellar parts. The lamellar part separates the two lateral muscle groups. The atlantal bursa is interposed between the funicular part of the ligamentum nuchae and the dorsal arch of the atlas; a second bursa may exist between the ligament and the spine of the axis. The muscles of the neck can be divided into lateral and ventral groups. The neck has eight cervical nerves, the first of which emerges through the intervertebral foramen of the atlas, the second through that of the axis, and the eighth between the seventh cervical vertebra and the first thoracic vertebra. The sixth to eighth cervical nerves contribute to the brachial plexus.
Reasons for Clinical Presentation
A horse may be presented for evaluation of the neck for a variety of reasons. The horse may have a history of a fall on the neck while jumping, having reared up and fallen over backward, or having collided with another horse or solid object, thus sustaining neck trauma. The horse may have neck pain from having pulled backward while being tied up. The horse may have no history of trauma but have abnormal neck posture, swelling, a stiff neck, neck pain, or difficulties in lowering and raising the head. The horse may have a performance-related problem such as unwillingness to work on the bit, an unsteady head carriage, or abnormal head posture. A neck lesion should also be considered in a horse with forelimb lameness when pain cannot be localized to the limb. Subtle hindlimb gait abnormalities, such as a tendency to stumble, may be caused by a neurological deficit without overt ataxia, reflecting a compressive lesion of the cervical spinal cord.
Clinical Examination
It is important to recognize that head and neck carriage depends in part on conformation: the way in which the neck comes out of the shoulder and the shape of the neck. The shape of the neck is also influenced by the way in which the horse works. If a horse carries the head and neck high, with the head somewhat extended, the ventral strap muscles tend to be abnormally well developed, resulting in a ewe-neck conformation. Many horses naturally bend more easily to the right than to the left or vice versa, and the muscles on the side of the neck, especially dorsocranially, are developed asymmetrically. Such asymmetry is particularly obvious if the neck is viewed from above by the rider. If a horse is excessively thin, then the cervical vertebrae become prominent and the caudodorsal neck region becomes dorsally concave, whereas in a fit, well-muscled horse that works regularly on the bit, this region is dorsally convex. Most stallions and many native pony breeds have a prominent dorsal convexity to the neck region, resulting in a cresty appearance. A horse that is excessively fat tends to lay down plaques of fat throughout the body, including the neck region, and this can be misinterpreted as abnormal neck swelling.
If a horse is particularly thick through the jaw, that is, has a large mandible, it is physically difficult to work on the bit (i.e., flexing at the poll so that the front of the head is in approximately the vertical position). Although neck pain can cause a reluctance to work on the bit, more common causes include rider-associated or training problems, mouth pain, forelimb or hindlimb lameness, and back pain. Some horses strongly resist the rider’s aids to work on the bit, despite the absence of pain. The use of artificial aids such as draw or running reins, which give the rider a mechanical advantage, may help to break a vicious cycle and encourage the horse to become more submissive and compliant. Similarly, work on the lunge line using a chambon (a device that runs from the girth via a headpiece to the bit rings) can encourage the horse to work in a correct outline and develop fitness and strength of the appropriate musculature. Working the horse in trot over appropriately spaced trotting poles can also help to encourage a horse to work in a correct outline, with a round and supple back.
A rider may complain of neck stiffness or difficulties in getting a horse to bend correctly in a circle. Although this may be caused by neck pain, neck stiffness may be a protective mechanism by the horse to avoid pain associated with lameness, especially forelimb lameness. A horse with left forelimb lameness, for example, may be reluctant to bend properly to the left, and when unrestrained by a rider on the lunge, on the left rein may hold the neck and head slightly to the right, giving the appearance of looking out of the circle. Thus load distribution is altered and lameness minimized. Such lameness actually may not be evident during riding, although this may be the only circumstance under which the rider recognizes the problem. The lameness may be more obvious on the lunge or even in hand in straight lines. When a horse has an abnormal neck and/or head posture, a comprehensive clinical evaluation of the entire horse should be performed. Neck pain or abnormal posture may reflect a primary lesion elsewhere (e.g., central or peripheral vestibular disease, fracture of the spinous processes of the cranial thoracic vertebrae, a mediastinal or thoracic abscess, or a systemic disease such as tetanus).
Detailed examination of the neck should include assessment of the neck conformation, the shape and posture at rest, and the position of the head relative to the neck and trunk. The veterinarian should note any patchy sweating or change in hair color reflecting intermittent sweating that may suggest local nerve damage. Look carefully at the musculature to identify any localized atrophy. Palpate the right and left sides of the neck to assess symmetry and the presence of abnormal swellings or depressions and to identify any neck muscle pain, tension, or fasciculation. Deep palpation should be performed on the left and right sides of the neck to identify pain.
A series of nine equidistant acupoints (acupuncture points) exist along an arc on the crest of the neck.1 The most cranial is in the depression just cranial to the wing of the atlas and just caudal to the ear. The most caudal point is a few centimeters dorsocranial to the dorsocranial aspect of the scapula. Six intervertebral acupoints also exist between the vertebrae. An abnormal response to firm palpation of these points may reflect neck pain.
Neck flexibility should be assessed from side to side and up and down. This can be done by manually manipulating the neck, but many normal horses resist this. Holding a bowl of food by the horse’s shoulder to assess lateral flexibility is helpful. Ideally the horse should be positioned against a wall, so that the horse cannot swing its hindquarters away from the examiner during this assessment. The clinician should try to differentiate between the horse properly flexing the neck and twisting the head on the neck. Compare flexibility to the left and to the right. To assess extension of the neck, the veterinarian should evaluate the ease with which the horse can stretch to eat from above head height. Observing the horse grazing is helpful to assess ventral mobility of the neck. Especially with lesions in the caudal neck region a horse may have to straddle the forelimbs excessively to lower the head to the ground to graze (Figure 53-1, A). The horse should also be observed moving in small circles to the left and the right, and loose on the lunge.
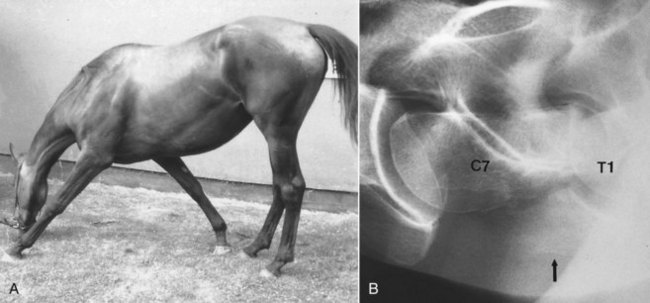
Fig. 53-1 A, A 3-year-old Thoroughbred filly with severe neck pain and restricted forelimb gait associated with a displaced articular fracture of the ventral processes of the seventh cervical vertebra. The horse must adopt the straddled forelimb stance to lower the head to graze. B, Lateral radiographic image of the caudal cervical vertebrae (sixth cervical to first thoracic vertebrae) of the same horse. Cranial is to the left. The ventral processes of the seventh cervical vertebra are displaced (arrow). The intercentral joint space between the seventh cervical (C7) and first thoracic (T1) vertebrae is narrowed greatly, with abnormal orientation of the vertebral bodies.
Assessing skin sensation and local reflexes, such as the cervicofacial and the thoracolaryngeal reflexes, and comparing carefully the right and left sides may be useful. The consistency and patency of the jugular veins should be evaluated.
The horse should be observed moving in hand and on the lunge, and if necessary should be ridden, to assess neck posture and the presence of neurological gait abnormalities, restriction in forelimb gait, or lameness. The clinician should note how any gait abnormality is influenced by the positions of the head and neck. Forelimb lameness occasionally is associated with a primary cervical lesion, usually, but not invariably, together with other clinical signs referable to the neck.2
Imaging Considerations
Radiography and Radiology
Comprehensive radiographic examination of the neck requires at least five exposures, assuming that large cassettes or imaging plates are used, including the poll, cranial, midneck and caudal neck regions and the base of the neck to evaluate the first and second thoracic vertebrae.3 Lateral-lateral images are obtained easily in the standing position, but ventrodorsal images are best obtained with the horse in dorsal recumbency under general anesthesia, except in small ponies and foals. Positioning of the neck is important, because any rotation of the head and neck makes evaluation difficult, in particular the synovial articulations. Relatively large exposures are required for the more caudal neck regions, so radiation safety is important, and the cassette should be supported in a holder, not held by hand. A grid is useful, especially in the caudal neck region, to reduce scattered radiation. Obtaining exposures from left to right and right to left may be useful. Lateral oblique images of the cervical vertebrae may give additional information.
A number of variations of the normal radiological appearance of the cervical vertebrae should not be mistaken for lesions. A spur on the dorsocaudal aspect of the second cervical vertebra may project into the vertebral canal. The ventral processes of the sixth cervical vertebra and occasionally other vertebrae have small separate centers of ossification. The ventral lamina on the sixth cervical vertebra may be transposed onto the ventral aspect of the seventh cervical vertebra, unilaterally or bilaterally. The seventh cervical vertebra has a small spinous process, which may be superimposed over the synovial articulation between the sixth and seventh cervical vertebrae and should not be confused with periarticular new bone. In older horses small spondylitic spurs may be seen on the ventral aspect of the vertebral bodies. Modeling of the dorsal synovial articulations between the fifth and sixth and between the sixth and seventh cervical vertebrae is common in middle-aged and older horses3-5 (Figure 53-2).
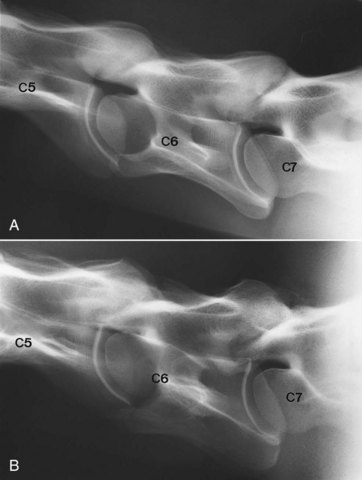
Fig. 53-2 A, Lateral radiographic image of the caudal cervical vertebrae of normal 4-year-old Thoroughbred. The synovial articulations between the fifth (C5) and sixth (C6) cervical and sixth and seventh (C7) cervical vertebrae are outlined smoothly. The intervertebral foramina are distinct. Compare with part B and Figure 53-8. B, Lateral radiographic image of the caudal cervical vertebrae of 9-year-old clinically normal horse. The synovial articulations are enlarged between the fifth (C5) and sixth (C6) cervical vertebrae and particularly between the sixth and seventh (C7) cervical vertebrae.
Major radiological abnormalities such as fusion of two adjacent vertebrae can be present subclinically, in part because of the great mobility between adjacent vertebrae (Figure 53-3, A). The clinical significance of such lesions may also be determined by the athletic demands placed on the horse.
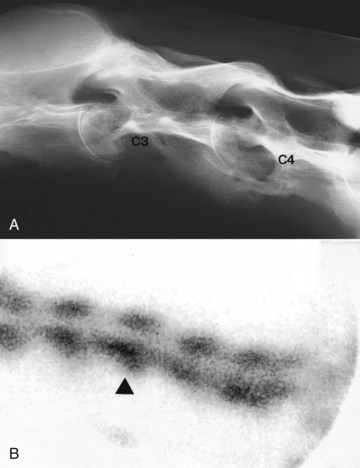
Fig. 53-3 A, Lateral radiographic image of a 15-year-old Arabian international-level endurance horse that had been competing successfully with no clinical signs referable to the neck. There is abnormal angulation between the third (C3) and fourth (C4) cervical vertebrae. The vertebral bodies of the third and fourth cervical vertebrae are osteoporotic. Extensive new bone has formed over the ventral aspect of the intercentral articulation between the third and fourth cervical vertebrae, with narrowing of the intercentral joint space and thinning of the caudal end plate of the third cervical vertebra. The ventral profile of the more cranial aspect of the third cervical vertebra is abnormal. B, Lateral scintigraphic image of the midneck region of the same horse. Note the increased radiopharmaceutical uptake in the vertebral body of the fourth cervical vertebra (arrowhead).
Nuclear Scintigraphy
Lateral and ventral scintigraphic images of the neck can be obtained. Ideally, images should be obtained from the left and right sides. In normal horses there is usually greater radiopharmaceutical uptake in the synovial articulations between the fifth and sixth and sixth and seventh cervical vertebrae, compared with the more cranial articulations reflecting the mobility of these joints and the biomechanical forces imposed on these articulations. There is often greater radiopharmaceutical uptake in the odontoid peg (dens) of the axis, compared with the surrounding vertebrae.
Increased radiopharmaceutical uptake (IRU) is not necessarily synonymous with a lesion that is clinically significant; therefore images must be interpreted with care (see Figure 53-3, B). The clinician should compare images obtained from the left and right sides carefully, because disparity in radiopharmaceutical uptake may be clinically significant. The veterinarian should evaluate the actual conformation of the synovial articulations, because a change in shape even without IRU may be important. Fractures are not always associated with prominent IRU, and lesions may be missed in the caudal neck region because of the overlying muscle mass and the scapulae.
Ultrasonography
The indications for ultrasonographic examination include evaluating swellings, assessing painful muscles and lesions of the ligamentum nuchae, assessment of the intercentral and synovial vertebral articulations (facet joints), documenting jugular vein thrombophlebitis, and administering ultrasound-guided injections.6-8
Computed Tomography
Computed tomography (CT) has the potential to give three-dimensional information about the cervical vertebrae and with contrast-enhanced studies can give information about spinal cord and nerve compression. However, general anesthesia is required, and it is practical to image only the cranial cervical vertebrae.9-11
Thermography
Thermographic examination of the neck is discussed in detail elsewhere (see Chapters 25 and 95). However, I have found thermography of limited usefulness, except for identifying acute superficial muscle injuries.
Electromyography
Electromyography (EMG) can be used to quantify the motor unit action potential and to identify insertional activity and pathological spontaneous electrical activity in muscle that can help to differentiate between myopathy and neuropathy and to localize the source of a lesion. It has been suggested that EMG can be used to help to determine the clinical significance of radiological abnormalities of the cervical vertebrae by detection of evidence of neuropathy.12
Other Diagnostic Tests
In selected horses with neck pain, valuable information may be obtained from hematological and serum biochemical tests. Measuring Brucella titers and tuberculosis testing are occasionally useful. Bone biopsy may be valuable for determining the cause of some bony lesions.
Clinical Conditions
Occipito-Atlantoaxial Malformation
Occipito-atlantoaxial malformation (OAAM) is a congenital abnormality,13 and although it can occur in any breed,14 OAAM appears to be a heritable condition in Arabian horses15 (see Chapter 123). Clinical signs are usually recognizable within the first few weeks of life and include an abnormal neck shape in the poll region, with prominence on the left or right sides or both, and/or scoliosis (Figure 53-4, A). These signs are best appreciated when viewed from above. Usually no associated soft tissue swelling or pain exists, although an abnormal clicking sound may be audible because of subluxation of the atlantoaxial joint. The horse may have an abnormal limitation of movement in the poll region. The gait should be assessed carefully for neurological abnormalities; however, in many horses no neurological gait deficits are apparent.

Fig. 53-4 A, Dorsal view of the poll region of a 6-month-old Thoroughbred filly with an abnormal asymmetrical shape and scoliosis of the cranial neck region and neck stiffness associated with occipito-atlantoaxial malformation. B, Ventrodorsal radiographic image of the same horse. Note the distorted shape of the atlas, its fusion with the occiput, and the abnormal orientation of the intercentral articulation between the first (C1) and second (C2) cervical vertebrae.
Diagnosis is confirmed radiologically using lateral and ventrodorsal views. Bony abnormalities include fusion of the atlas to the occiput, atlantoaxial luxation, and abnormal shapes of the atlas and axis, often asymmetrical (see Figure 53-4, B).
No treatment is available for horses with OAAM. Prognosis for athletic function is determined by the degree of neck stiffness. Because of the heritable nature of this condition in Arabian horses, breeding of affected horses or the sire or the dam is inadvisable.
Other Congenital Abnormalities
OAAM is the most common congenital abnormality of the cervical vertebrae, but congenital torticollis is seen occasionally, caused by malformation of more caudal cervical vertebrae. Vertebral body fusion usually is seen with a meningomyelocele, resulting in neurological abnormalities, and therefore is not considered further.
Subluxation of the First and Second Cervical Vertebrae
Subluxation of the first and second cervical vertebrae is an unusual condition, probably related to trauma such as a fall, although the horse may have no recent history of such.16-22 The condition is associated with damage of the ligament of the dens or the ventral longitudinal ligament between the first and second cervical vertebrae or occurs secondary to a fracture of the dens.17,18 An affected horse usually has a stiff neck and a tendency for the head and neck to be somewhat extended (Figure 53-5, A). Differentiating between neck pain and stiffness may be difficult. An audible clicking noise may emanate from the region, and occasionally abnormal movement between the vertebrae can be appreciated. Because of the relatively wide sagittal diameter of the vertebral canal at this site, generally no associated compression of the cervical spinal cord occurs. Occasionally, neurological abnormalities are seen in horses with a displaced fracture of the dens.22
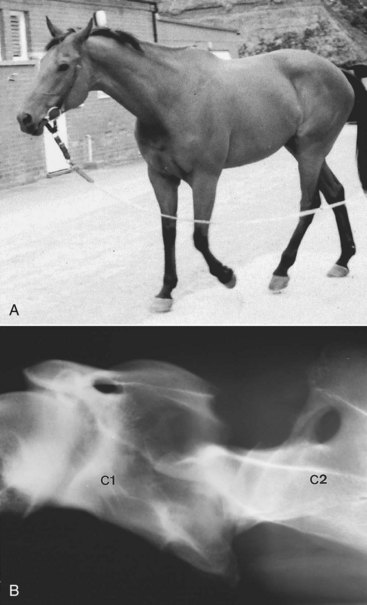
Fig. 53-5 A, A 9-year-old advanced event horse that had shown neck stiffness since traveling from the United States to Great Britain. The head is extended somewhat, and there was significant neck stiffness or guarding. A clicking sound emanated from the cranial neck region. B, Lateral-lateral radiographic image of the cranial neck region of the same horse. There is an abnormal orientation between the first (C1) and second (C2) cervical vertebrae. Space between the dorsal aspect of the dens and the ventral aspect of the dorsal lamina of the vertebral arch of the first cervical vertebra is reduced. The dorsal aspect of the dens is irregular because of new bone formation. Postmortem examination confirmed partial disruption of the ligament of the dens.
Diagnosis is based on radiographic examination, using lateral-lateral images with the neck in natural (neutral) and extended positions. Radiological abnormalities may include abnormal orientation between the first and second cervical vertebrae (see Figure 53-5, B). The position of the dens may be abnormal, resulting in narrowing of the space between it and the dorsal lamina of the vertebral arch of the first cervical vertebra. In a study of yearling Thoroughbreds the mean minimum sagittal diameter was 34 mm and the minimum was 26 mm.20 Narrowing of the distance between the vertebral arch of the first and second cervical vertebrae may occur in the extended versus neutral position of the neck. The shape of the dens may be altered because of secondary new bone formation. Occasionally the dens is fractured, usually at the junction between the odontoid process and the body of the vertebra.22 The synovial facet joints between the first and second cervical vertebrae may be altered in shape.
Foals with fractures of the odontoid peg have been successfully treated by surgical stabilization, but limited information exists about long-term prognosis.18,19,21 Foals with subluxation without neurological abnormalities have a good prognosis for life; prognosis for athletic function is fair, depending on the intended level of competition. No reports of successful management of subluxation in adult horses exist, and the prognosis for return to athletic function with conservative management is poor. However, it was reported that four of five horses with an acute fracture of the dens returned to athletic function, despite neurological gait abnormalities at the time of acute injury, although one had a tendency to trip.22
Subluxation of the Sixth and Seventh Cervical Vertebrae
Subluxation of the sixth and seventh cervical vertebrae is usually recognized in adult horses with a complaint of lack of hindlimb power or with difficulties in performing movements requiring collection or, if a breeding stallion, difficulties in mounting either mares or a dummy. Careful clinical examination usually reveals mild-to-moderate hindlimb ataxia. Radiographic examination reveals dorsal displacement of the head of the seventh cervical vertebra. Subluxation of the sixth and seventh cervical vertebrae has less commonly been identified as a cause of bilateral forelimb lameness.23
Insertional Desmopathy of the Nuchal Ligament and Injury to Semispinalis
The nuchal ligament is a bilobed structure, fans at its insertion on the occiput, and is surrounded by muscle, the semispinalis to the left and right and the rectus capitis ventrally. New bone formation at the insertion on the occiput may be an incidental finding. Examination of 302 Warmbloods from 1 to 22 years of age revealed new bone in 85%. A postmortem study of Warmbloods revealed a similar high proportion of horses with chondroid metaplasia at the insertion of the ligament and dystrophic mineralization.24 A smaller radiological study of Thoroughbreds revealed new bone on the caudal aspect of the occiput in only 5%.24
Horses with insertional desmopathy of the nuchal ligament or injury to the tendon of insertion of semispinalis often have a history of trauma to the region (e.g., pulling back when tied up) or an excessive amount of lunging exercise while restricted with side or draw reins.24-26 Horses should be examined while being lunged, with and without side reins, and ridden. Clinical signs include permanent resistance against the reins, with difficulty or unwillingness to lower and flex the head and neck when ridden and poor flexion at the poll. In contrast to horses with back pain, hindlimb impulsion is usually good. The horse may have a tendency to rear or shake its head.
Pain cannot usually be elicited by palpation. Radiological examination may reveal new bone on the caudal aspect of the occiput that may extend farther ventrally and dorsally than the actual insertion of the ligamentum nuchae (Figure 53-6). Mineralization sometimes is seen dorsal to the first cervical vertebra as an incidental radiological finding, unassociated with clinical signs. Scintigraphic examination findings may be negative. Ultrasonographic examination is not easy, and interpretation is difficult. Mineralization within the ligament may cause shadowing artifacts. CT offers the most sensitive means of detecting lesions in either the nuchal ligaments or the border of insertion of semispinalis.24 Diagnosis depends on a positive response to infiltration of local anesthetic solution. Fifteen milliliters of mepivacaine are infiltrated on the left and right sides, and the response is assessed after 15 to 30 minutes. Care must be taken not to inject into the epidural space, which will result in ataxia.

Fig. 53-6 Lateral-lateral radiographic image of the head of an 8-year-old Warmblood show jumper with a history of reluctance to accept and go forward to the bit and stiffness. There is enthesophyte formation on the caudal aspect of the occiput at the insertion of the nuchal ligament (arrows). The horse responded well to local infiltration with corticosteroids and local anesthetic solution and modification of the training program.
Treatment consists of repeated infiltration of corticosteroids, Traumeel (a homeopathic remedy), and local anesthetic solution and modification of the training program, with no work on the bit for 8 weeks.26 The horse should be worked principally in straight lines. In the stable the horse should be encouraged to flex the poll region gently from side to side and up and down. The use of acupuncture or magnetic field therapy, laser therapy, ultrasound, or shock wave therapy may help some horses. The results vary. Seventy percent of 26 horses return to full work, although not all are completely normal. Extracorporeal shock wave therapy, two or three applications at 14-day intervals, in addition to 4 weeks of work without requiring flexion of the poll has been reported to be successful in resolving clinical signs in 12 of 22 horses and in improving signs in six other horses.27 Surgical treatment by transection of the nuchal ligament and the fascia of semispinalis has resulted in improvement in a small number of horses refractory to conservative management.24
Disorders of the Neck Musculature
The clinical significance of localized muscle soreness and/or tenseness is poorly understood and documented. I have had experience with a number of horses with subtle performance problems, including slight neck stiffness, reluctance to work properly on the bit and to accept an even contact, and intermittent, slight gait irregularities associated with soreness around and in front of the wings of the axis. Clinical improvement has been seen after relief of this pain by rapid and sudden rotation of the head about the axis.24
Many horses resent firm palpation of the brachiocephalicus muscles at the base of the neck. This may be more obvious in horses with forelimb lameness, especially those with pain in the distal part of the limb. This muscle soreness is generally a secondary rather than a primary cause of lameness. Transient improvement in gait may be seen after local therapy using laser therapy, H-wave therapy, ultrasound, and/or massage.
Primary brachiocephalicus pain at the base of the neck has been seen in performance horses, causing subtle gait abnormalities at the walk when ridden, characterized by abnormal lifting of the neck as the limb was advanced and a shortened cranial phase of the stride ipsilateral to the sore muscle. Bilateral brachiocephalicus muscle pain has also been seen in association with throwing up of the head when in the air over a fence and on landing. Treatment of the sore muscles abolished this behavior.
Local muscle soreness also may be seen with a poorly fitting saddle or girth or with a rider who is unable to ride truly in balance with the horse. The primary problem must be addressed if treatment is to be successful. Some driving horses develop forelimb lameness that is seen only when the horse is pulling and may be associated with pressure from the harness. Adaptation of the harness may relieve the problem.
Some horses seem to need to learn how to use the neck and forelimb musculature to maximum advantage and have a restricted forelimb gait without appearing overtly lame. The gait is not altered by distal limb nerve blocks. Some improvement may be achieved by daily massage of the muscles at the base of the neck and manual full protraction of the forelimbs. This is combined with exercise to encourage the horse to lengthen the forelimb stride and to round the back. Lunging in a chambon, trotting over appropriately placed trot poles, and repeatedly lengthening and shortening the stride all may be beneficial. Trotting down the tramlines in a field of corn or rapeseed can also be of enormous help.
Occasionally as the result of a fall or pulling back when tied, acute severe neck muscle soreness develops. The horse is best treated initially with nonsteroidal antiinflammatory drugs (NSAIDs), rest, and local physiotherapy, followed by progressive remobilization when the acute muscle soreness has subsided. The prognosis is good.
I have examined several horses that have had episodic transient attacks of profound neck pain and stiffness, holding the neck relatively low. In some horses a severe unilateral forelimb lameness occurs, often resulting in the limb being held in a semiflexed position at rest. These attacks vary in duration (hours to days), and generally horses have been completely normal between episodes. To date, neither a definitive cause nor an effective treatment has been identified for this syndrome. However, there is usually a very marked enlargement of the caudal cervical facet joints, with narrowing of the intervertebral foramen, and it is suspected that nerve root impingement may cause episodic pain. Careful manipulation of the caudal neck region may result in instantaneous relief of clinical signs.
Dystrophic mineralization is seen sometimes as an incidental radiological finding in the neck musculature, secondary to previous intramuscular injections.
Muscle Abscess
Horses sometimes develop localized muscle soreness and swelling at the site of intramuscular injection, especially equine influenza injections, which can result in neck stiffness and a restricted forelimb gait. Signs usually resolve within 24 to 48 hours. Treatment is generally unnecessary, although hot packing and analgesia may be beneficial. More irritant drugs, such as iron injections, may result in the development of a sterile abscess.
The development of a single or multiloculated abscess cavity filled with malodorous material is usually a sequela to an intramuscular injection of a variety of drugs administered within the previous few weeks. Clinical signs include neck pain and stiffness, localized neck swelling with or without focal patchy sweating, and sometimes pyrexia. Diagnosis is based on the history and clinical signs and can be confirmed by ultrasonography. The abscess cavity is usually filled with anechogenic material surrounded by a hyperechogenic abscess wall.
Treatment is by surgical drainage, which is easily performed in the standing horse. The abscess cavity should be thoroughly lavaged. Systemic antimicrobial drugs usually are not required, unless clostridial myositis is suspected based on the fulminant nature of the condition (see Chapter 83). The prognosis for most horses with muscle abscesses is good, provided that adequate drainage is established. However, surgical removal of the entire abscess occasionally is required.
Osteoarthritis
Anatomical studies have shown that approximately 50% of normal mature horses have some unilateral or bilateral modeling of the synovial facet joints between the sixth and seventh cervical vertebrae. The modeling often is accompanied by extension of fibrocartilage across the cranial border of the dorsal arch of the seventh cervical vertebra and irregular enlargement of the articular processes.4,5 The spinous process of the seventh cervical vertebra may become flattened or fragmented by contact with the sixth cervical vertebra when the neck is extended. Radiologically these changes result in irregularity of the normally smooth outline of the synovial articulations. Similar modeling changes also occur in the synovial articulation between the sixth and seventh cervical vertebrae.24 A bony knob may develop on the ventral aspect of one or both cranial articular processes at the articulations between the fifth and sixth cervical vertebrae and between the sixth and seventh cervical vertebrae. When well developed, this knob forms a buttress that impinges onto the body or the arch of the more cranial vertebra and forms a false joint. The buttress partially obliterates the intervertebral foramen, but it is often of no clinical significance.3-5 Buttresses occur at the articulation between the sixth and seventh cervical vertebrae in 18% of normal horses.4
The potential exists for large amounts of new bone associated with osteoarthritis of the cervical synovial articulations to encroach axially into the vertebral canal, resulting in compression of the spinal cord and hindlimb weakness and ataxia, or into the intervertebral foramen, resulting in nerve root compression with local or referred pain and possibly lameness and patchy sweating. Severe osteoarthritic change may progress to partial or complete fusion and thus neck stiffness. With enlargement of a synovial articulation also generally comes enlargement of the joint capsule, and synovial outpouchings or cysts may develop that may impinge on the spinal cord.
Radiological abnormalities associated with osteoarthritis include enlargement of one or more of the articular facets and alteration in joint space width (Figure 53-7). Widening of the joint space is usually associated with asymmetrical facet enlargement; narrowing is caused by articular cartilage degeneration. Pitted lucent zones may develop in the articular facets, with extension of the dorsal laminae between adjacent vertebrae and partial or complete obliteration of the adjacent intervertebral foramina. Sometimes fractures are seen dorsal to a joint. Abnormalities often develop on the left and right sides but are frequently asymmetrical. With substantial asymmetry of the synovial articulations the affected and immediately more cranial vertebrae may appear rotated on a lateral radiographic image, although the horse had appeared to be standing with its head and neck straight in the sagittal plane. Radiographic examination from left to right and from right to left and oblique radiographic images can help to determine on which side a unilateral lesion is present. A lesion that is close to the cassette is clearer and magnification is less than if the lesion is on the opposite side of the neck. Ultrasonography can also be used to demonstrate periarticular modeling and increased synovial fluid within a joint.

Fig. 53-7 Slightly oblique lateral-lateral radiographic image of the caudal cervical region of a 7-year-old riding horse with mild right forelimb lameness and an abnormally low head and neck carriage. Lameness was unaltered by comprehensive diagnostic analgesia of the right forelimb. There is extensive modeling of the articular facet joints between the sixth (C6) and seventh (C7) cervical vertebrae, with a large radiodense mass with heterogeneous opacity extending dorsally. Obtaining a true lateral-lateral image was not possible. The obliquity of the radiograph makes it difficult to assess the intervertebral foramen. Postmortem examination revealed compression of the seventh cervical spinal nerve at the level of the foramen.
The clinical importance of osteoarthritis of one or more synovial articulations can be difficult to determine by clinical and radiographic examinations alone, except by exclusion. The greater the degree of abnormality and the larger the number of articulations involved, the more likely the condition is clinically significant. In normal horses, finding osteoarthritic change cranial to the articulation between the fifth and sixth cervical vertebrae is rare. Unilateral forelimb lameness has been seen with lesions between the fourth cervical and first thoracic vertebrae.2 Nuclear scintigraphic examination may give further information in horses with neck stiffness or forelimb lameness apparently not referable to the limb itself. Ultrasound-guided intraarticular analgesia may help to determine the clinical significance of radiological abnormalities (Figure 60-5).
In one report, seven of eight horses with forelimb lameness associated with radiological abnormalities of the cervical vertebrae also had subtle to obvious signs of neck pain.2 Patterns of muscle atrophy in the neck and shoulder regions varied. The character of lameness varied. Radiological abnormalities included substantial modeling of the synovial articulations in the caudal neck region in three horses; a fourth had modeling and a fracture involving the synovial articulation between the fourth and fifth cervical vertebrae. One horse had abnormalities of the intercentral articulation between the seventh cervical and first thoracic vertebrae and a discrete mineralized fragment dorsal to it. Large lucent zones were identified in a vertebral body (the fourth and sixth cervical vertebrae) in two horses. A fracture of the vertebral body of the seventh cervical vertebra was seen in one horse.
Nerve root impingement in the caudal neck region may cause radicular or referred pain and account for forelimb lameness. Neck pain itself can also cause forelimb lameness. Compression of the seventh cervical nerve was confirmed post mortem in a horse with osteoarthritis of the articulations between the sixth and seventh cervical vertebrae and between the seventh cervical and first thoracic vertebrae.2 Nerve root compression with severe osteoarthritis has also been demonstrated using contrast-enhanced CT.9
In horses with mild ataxia, neck stiffness or forelimb lameness associated with osteoarthritis of cervical synovial articulations, the response to rest and treatment with NSAIDs has been limited. Local periarticular or intraarticular infiltration of corticosteroids, performed using ultrasonographic guidance, may bring temporary relief. There is limited documented evidence for the efficacy and duration of effect of medication of the synovial articulations of the caudal cervical vertebrae. In a recent study of 59 sports or pleasure horses with ataxia, neck stiffness or pain, or obscure forelimb lameness, 19 horses (32%) returned to full function and 18 horses (31%) improved more than 50%.28 However, the effect was generally short lived, with 55% showing improvement for a duration of less than 1 month to up to 6 months. The inclusion criteria for the study were poorly defined and follow-up results were based on the owners’ subjective opinions. Epidural injection of corticosteroids performed with the horse under general anesthesia has been shown to result in relief of neck stiffness in a horse with osteoarthritis of the synovial articulation between the fourth and fifth cervical vertebrae and clinical evidence of nerve root compression.29
Osteoarthritis, especially in the caudal neck region, may result in associated enlargement of the joint capsule(s) and subsequent pressure on the spinal cord. In horses with mild osteoarthritis obvious ataxia may not be seen, but the history may include the tendency to stumble or to knuckle behind, or lack of hindlimb impulsion. Such signs often have been attributed to lameness but are invariably unaltered by diagnostic treatment with NSAIDs. Clinical signs may be subtle and intermittent. Such horses usually show abnormal weakness if pulled to one side by traction on the tail while the horse is walking—the sway test. A normal horse easily may be pulled off line once, but then strongly resists. A weak horse can be pulled off line repeatedly. Weakness may also be apparent as the horse decelerates from trot to walk, with exaggerated up-and-down movement of the hindquarters and asymmetric hindlimb placement. This may result in irregular movement of each patella and may be confused with mild intermittent upward fixation or delayed release of the patella (see Chapters 46 and 48). At faster speeds the horse may look completely normal, although some affected horses demonstrate a remarkably croup-high canter when on the lunge. In a young horse, advanced osteoarthritis of one or more caudal cervical synovial articulations is strong circumstantial evidence of cause and effect (Figure 53-8). Definitive diagnosis in an older horse is much more difficult, because radiological evidence of osteoarthritis may be present without associated clinical signs. Myelography may help.30 The prognosis is poor, and the horse may be potentially unsafe to ride. Surgical treatment can be considered and generally results in clinical improvement, but few sports horses become upper level athletes, and some develop recurrent ataxia several years later.

Fig. 53-8 Lateral radiographic image of the caudal cervical vertebrae of 4-year-old dressage horse with mild hindlimb weakness and a tendency to stumble behind, especially in downward transitions from trot to walk. The synovial articulations between the fifth (C5) and sixth (C6) cervical and sixth and seventh (C7) cervical vertebrae are enlarged greatly (compare with Figure 53-2, A). The joint spaces are widened, reflecting asymmetrical modeling of the articular processes. There is a ventral buttress at the articulation of the sixth and seventh cervical vertebrae, with reduction in size of the intervertebral foramen.
Diskospondylitis
A survey of the cervical intervertebral disks of 103 horses from birth to 23 years of age confirmed that they consisted solely of fibrocartilage, with no nucleus pulposus.31 Age-related degenerative changes were identified, but even with severe disintegration of the disks, no referable clinical signs had been apparent.
Diskospondylitis is a rare cause of neck pain, forelimb lameness, or ataxia.30,31 Although diskospondylitis is usually an infectious condition in dogs, no proven relationship occurs in the horse, and trauma may be an inciting cause. Lesions in the horse have been identified in the caudal neck region (the articulations between the sixth and seventh cervical vertebrae and the seventh cervical and first thoracic vertebrae) and between the third and fourth cervical vertebrae in association with severe neck pain and a bilaterally short, stiff forelimb lameness or episodic, unilateral forelimb lameness. Occasionally a horse may be reluctant to work “on the bit.” High-quality radiographs are required for accurate diagnosis. Lesions are characterized by loss of the normal opacity of the cranial and caudal endplates of the affected vertebrae, with or without alteration in the intercentral joint space. Scintigraphic examination may help to localize the affected joint(s). Ultrasonography may be more sensitive in the identification of early bone lesions and abscess formation. The prognosis is guarded, although in one report a broodmare that was admitted with profound neck pain and periodic severe left forelimb lameness, associated with roughening of the endplates at the intercentral articulation between the sixth and seventh cervical vertebrae and narrowing of the intercentral space, after a collision with a fence, made a spontaneous recovery.32 A second horse was treated by surgical debridement of the disc space and implantation of a cancellous bone graft, with resolution of clinical signs.33
Fracture
Fractures of the cervical vertebrae usually result from trauma: the horse rearing up and falling over backward or sideways; pulling back when tied up; or falling while jumping, usually at speed. Clinical signs are sudden in onset and include holding the neck in an abnormally low position, stiffness, a focal or more diffuse area of pain, with or without localized or more diffuse soft tissue swelling, and muscle guarding. Audible or palpable crepitus is sometimes detected. The horse may be unable to lower its head to the ground or may be able to do so only by straddling of the forelimbs (see Figure 53-1, A). Associated hindlimb and forelimb ataxia may be apparent, which can be transient and self-resolving, or persistent. Patchy sweating and localized muscle atrophy may develop. Occasionally an associated unilateral or bilateral forelimb lameness occurs.
Diagnosis is confirmed radiologically (see Figure 53-1, A) (Figure 53-9). Most fractures are detectable on lateral-lateral images, although ventrodorsal images give additional information about the extent of the fractures, especially those involving the atlas or axis. Lateral oblique images can also be helpful in selected horses. Care should be taken not to confuse physes and separate centers of ossification with fractures.
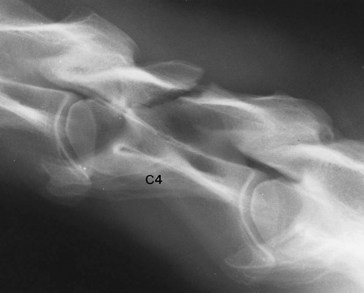
Fig. 53-9 Lateral radiographic image of the third to fifth cervical vertebrae of a 9-year-old Dutch Warmblood dressage horse with severe neck pain, stiffness, and incoordination after a fall 12 days previously. The fourth cervical vertebra (C4) has a comminuted, slightly displaced fracture of the dorsal arch. Ataxia resolved within another 14 days, and the horse made a complete functional recovery.
The prognosis depends on the site and configuration of the fracture(s), the degree of displacement, and hence the likelihood of permanent compression of the spinal cord, either by a displaced fracture or by subsequent callus formation.
Fractures of the atlas and axis, especially through the physis of the separate center of ossification of the dens, are particularly common in foals. The prognosis for complete recovery is fair with conservative management, provided that no evidence of ataxia exists. Usually no treatment is required other than confinement to a box or small pen.
Fractures of the cervical vertebrae in adults more commonly involve the vertebral body or arch in the midneck region (the third to sixth cervical vertebrae) or the synovial articular facets of the more caudal vertebrae (the fifth to seventh cervical vertebrae). Local hemorrhage and edema may result in ataxia, which usually resolves within a few days. Persistence of ataxia warrants a guarded prognosis. Most fractures heal by callus formation, and this may subsequently impinge on the spinal cord, causing later ataxia. A fracture of a vertebral body also may result in damage to the adjacent intervertebral disk and associated ligaments, which subsequently may protrude into the vertebral canal and cause ataxia. Thus in the acute stage giving an accurate prognosis may be difficult. However, many fractures of the vertebral bodies and synovial articulations do heal, and horses may be able to return to athletic function, although residual neck stiffness may be present.
In the acute stage the horse should be confined to box rest. Analgesics may be necessary to control severe pain, but they should be used judiciously to avoid encouraging excessive movement of the neck. The position of the water bucket and manger should be adjusted so that the horse can drink and eat from normal head height. The hay should be fed at a height level with the head, preferably loose, or if in a hay net, a net with large holes, with the hay well shaken first. The horse should not be tied up during the convalescent period in case it pulls back. Reappraising the horse clinically and radiologically every 6 to 8 weeks is helpful. Maximum clinical improvement may not be seen until 6 to 9 months after injury. Selected fractures may require surgical stabilization.8
Myeloma
Myeloma is a myeloproliferative disorder that can cause radiolucent lesions in any bone, including the cervical vertebrae, with associated bone pain.24,34 Cervical vertebral myeloma was diagnosed in several horses of a wide range of breeds and ages.34 Clinical signs included intermittent pyrexia, severe neck pain and stiffness, episodic forelimb lameness, weight loss, and a variety of other abnormalities. Diagnosis is based on hematological, radiographic, and bone biopsy examinations. Hematological abnormalities include anemia, leukocytosis, neutrophilia, and lymphocytosis. Total protein concentration is elevated greatly. Protein electrophoresis shows a clinically significant monoclonal peak in the gamma region. Radiological examination of affected bones reveals clearly demarcated lucent zones, usually without a sclerotic rim. Bone biopsy is useful to confirm the diagnosis, but currently no treatment is available and the prognosis is hopeless.
Other Cystlike Lesions in Cervical Vertebrae
Occasionally, single or several well-demarcated radiolucent zones are identified in one or more adjacent vertebrae, associated with profound neck pain, with or without forelimb lameness.35 These lesions have not been proved to be caused by osteomyelitis or myeloma, although a definitive diagnosis has not always been possible by bone biopsy or postmortem examination. One horse with extremely severe neck pain and forelimb lameness had radiolucent zones in the fifth and sixth cervical vertebrae, and bone biopsy revealed accumulation of abnormal plasma cells, but the horse made a most spectacular and complete recovery after exploratory surgery and returned to international show jumping. A show pony had a large cystlike lesion in the fourth cervical vertebra with profound neck pain and left forelimb lameness (Figure 53-10). Postmortem examination revealed a cavity filled with granulation tissue, surrounded by a large area of bone necrosis, but no suggestion of the underlying cause.
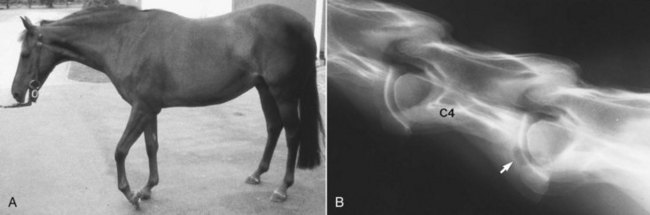
Fig. 53-10 A, A 13-year-old show pony with exquisite neck pain, worse on the left side, and episodic severe left forelimb lameness. The pony showed a shortened cranial phase of the stride at the walk, and periodically the pony stopped, holding the limb in a semiflexed position, and was reluctant to move forward. There was hyperesthesia of the caudal half of the left side of the neck. B, Lateral-lateral radiographic image of the midneck region of the same pony. A large radiolucent zone (arrow) is visible in the caudal aspect of the vertebral body of the fourth cervical vertebra (C4). There is a loss of continuity of the caudal cortex.
Vertebral Osteomyelitis
Cervical vertebral osteomyelitis usually occurs secondary to a systemic disease such as Rhodococcus equi infection in foals, Streptococcus equi infection (strangles), tuberculosis, or brucellosis; or as an extension of soft tissue infection4; or through hematogenous spread. Clinical signs may include pyrexia, neck stiffness or pain, and an abnormal neck posture, poor appetite, and weight loss. Usually leukocytosis, neutrophilia, and hyperfibrinogenemia are also present. Radiological examination of the cervical vertebrae may reveal focal radiolucent zones, with or without surrounding increased radiopacity, in one or more vertebrae.4 Useful diagnostic tests include bone biopsy, tuberculosis skin testing, and measurement of Brucella titers. Aggressive antimicrobial treatment may result in amelioration of clinical signs, but the prognosis is guarded.
Jugular Vein Thrombophlebitis
Thrombophlebitis of the jugular vein is a common condition associated with intravenous injection and chemical irritation, mechanical trauma to the vessel wall through catheterization, or a coagulation disorder. The vein feels abnormally hard, but unless the left and right sides are affected, the thrombus is infected, or thromboemboli settle elsewhere, usually no other clinical signs are apparent.
Occasionally a long length of the jugular vein is occluded by a thrombus in which bacteria are seeded, resulting in infectious thrombophlebitis. Clinical signs include neck stiffness and pain, localized heat and swelling, and pyrexia. If a long length of the vessel is involved, ipsilateral swelling of the head may occur. Diagnosis is based on clinical signs and ultrasonography.6 A heterogeneous, cavitating echogenic thrombus can be seen in the jugular vein. Usually leukocytosis, neutrophilia, and hyperfibrinogenemia are present. A horse with a localized, small infected thrombus usually responds well to prolonged systemic antimicrobial therapy. Injection of antimicrobial drugs into the thrombus may be indicated if there is inadequate response to systemic therapy. The lesion should be monitored clinically and ultrasonographically. With more extensive lesions or associated toxemia or bacteremia, surgical ligation and removal of the vein may be required, combined with systemic antimicrobial treatment.
Inadvertent perivascular injection of an irritant drug, such as phenylbutazone, may result in the rapid development of localized pain and swelling caused by chemical irritation. This may be followed by an aggressive inflammatory response, leading to sloughing of the skin. If perivascular injection is suspected, then the area should be treated by local infiltration with a balanced electrolyte solution (1 L) to dilute the drug, combined with local anesthetic solution (10 to 20 mL mepivacaine) to reduce pain. Periodic hot packing seems to ameliorate clinical signs. If the condition is initially untreated and local tissue necrosis supervenes, a skin slough is almost inevitable, and prophylactic antimicrobial therapy may be indicated.
Neck Stiffness and Cervical Vertebral Mobilization under General Anesthesia
Assessment of neck flexibility has been described (see page 607). Restricted neck mobility associated with other clinical signs suggestive of neck pain, for example, reluctance to accept the bit, may be an indication for cervical vertebral mobilization under general anesthesia (see Chapter 95). The aim is to assist in restoring normal function to soft tissue components of joints. However, horses with preexisting osteoarthritic changes are unlikely to respond. Repeated or maintained end-of-range passive joint movements may lower intraarticular pressure, inhibit reflex muscle contraction around a joint, and reduce muscle tension on the periarticular soft tissues and thus relieve pain. The manipulations are performed with the horse in left and right lateral recumbency under general anesthesia. Nine manipulations are performed in sequence to include extension of the head and neck, extension with rotation to the left and then to the right, rotation of the head to the left and to the right, flexion of the neck to the left and to the right, and flexion and rotation in each direction. For each maneuver the head and neck are moved to a position at the end of the resistance-free range. Constant pressure then is applied so that movement through the stiff and reduced range can be initiated. The pressure then is maintained until the joints and associated soft tissues move through the range of resistance. When movement ceases, a new end range is established and pressure is released. The maneuver may then be repeated. After treatment, horses are rested for 5 days and then start light work. Clinical improvement usually is appreciable within 2 weeks.36 Repeated treatment may be necessary in selected horses. Occasionally, clinical signs deteriorate after treatment.