Chapter One Methods and health research
Introduction
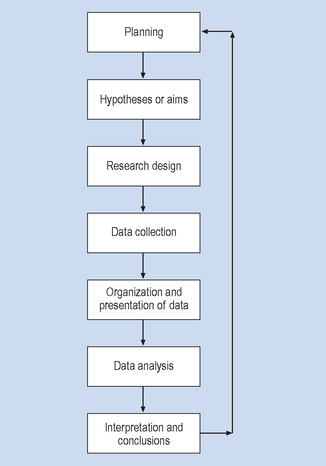
Health research is a systematic and principled way of obtaining evidence (data, information) for solving health care problems and investigating health issues. Research is systematic in that researchers tend to follow a sequential process (Fig. 1.1) and principled in that research is generally carried out according to explicit rules. These rules or principles constitute the method.
The primary aim of this chapter is to outline the key characteristics of methods for conducting enquiry. Special emphasis is placed on method as a means for conducting applied research and producing the best possible evidence for solving health problems.
Methods and knowledge
Patient care involves the acquisition of a set of specific skills, the practice of which is justified in terms of a body of professional knowledge. This body of knowledge is based on the use of appropriate methods. In general the term ‘method’ refers to a systematic procedure for carrying out an activity and in the present context implies a set of rules which specify:
Before we begin a discussion of the scientific method it is useful, as a means of contrast, to look at some of the other methodological approaches.
Authority
According to this method, knowledge is considered true because of tradition, or because an experienced and distinguished clinician says that it is true. As a student, you are often asked to accept statements as true because your teachers and clinical supervisors say they are true. To maintain their authority, the ‘sources’ of knowledge acquire and cultivate various signs of expertise, such as the appellation of ‘Professor’, or encourage the performance of status rituals. For example, consider the ‘Consultant’ who sweeps into a hospital ward followed by a retinue of students, registrars and nurses. Who would dare to question the truth of any of the consultant’s sacred utterances? However, there are problems with the method of authority: what happens when the statements arising from one authority are contradicted by those made by an equally prestigious authority? For example, say Authority X claims that in their experience psychoanalysis is effective, while Authority Y states that the technique is useless. How can we resolve such conflicting claims? In practice, unless objective and acceptable criteria for resolution can be found, we will have unending arguments, ad hominem (personal) attacks, or in instances of some religious or political disagreements, violence. That is, the controversy is resolved by denigrating or silencing the dissenting authority. In contrast, the scientific method emphasizes the evaluation of the evidence for establishing the truth of conflicting statements.
Reasoning
Reasoning is commonly used to arrive at true knowledge. It is assumed that if the rules of logic are applied correctly, then the conclusions are guaranteed to be valid. As an example, let us look at the following syllogism:
Logic guarantees that the conclusion (3) is true, provided that the syllogism is in a valid form and the premises (1) and (2) are true. Clearly, the limitation of formal (that is, ‘content-independent’) reasoning is that it works in practice only if we have means for establishing the factual truth of the premises. In the above example, conclusion (3) might be empirically false, given that the premise (1) is factually false.
Logic and mathematics are very much a part of science but we require strong evidence to support the effective logic and mathematical operations.
Intuition
Knowledge is sometimes acquired by sudden insights which arise without conscious reasoning. Truth is judged by the clarity of the experience and its emotional content (the ‘Eureka!’ experience). For example, after working with a patient without success, you might have a sudden insight about how to change your treatment programme. Sometimes these insights lead to new theories and treatments. Unfortunately, even the strongest intuitions are sometimes proven false by cold, boring facts. Newton has referred to the disappointment that occurs when a beautiful hypothesis is destroyed by an ugly fact.
Discoveries are sometimes resisted because they seem counterintuitive. Ignaz Semmelweis, a perceptive and humane 19th-century physician, noticed appalling levels of puerperal (child birth-related) fever and maternal death at his hospital. He argued that the infection was spread by med-ical students and staff who went to delivery rooms from the morgue without adequately washing their hands. In 1848, Semmelweis introduced antiseptic procedures in his wards and demonstrated a substantial reduction in mortality from puerperal fever. However, his colleagues were offended by the notion that physicians were carriers of disease. Semmelweis was dismissed from his post, ostracized by the medical establishment and died in pitiful circumstances. Clearly, in the light of contemporary knowledge we can say that Semmelweis’ insights were correct, while his colleagues’ intuitions were mistaken. Authority, logic and intuition all have their places in health care and research. In a general way the scientific method can be contrasted with other methods in that it emphasizes the need for evidence. What constitutes scientific evidence and what the evidence indicates are complex matters that are being addressed in this book.
The scientific method and positivism
The scientific method has crystallized over a period of several centuries, concomitantly with the growth of scientific research. The beginnings of modern Western science are generally traced to the 16th century, a time in which Europe experienced profound social changes and a resurgence of great artists, thinkers and philosophers. Gradually, scholars’ interests shifted from theology and armchair speculation to systematically describing, explaining and attempting to control natural phenomena. These changed circumstances allowed philosophers such as Descartes and Francis Bacon to challenge tenets of medieval thinking, and scientists such as Galileo, Newton and Harvey to propose new models of natural phenomena.
The approaches of such great thinkers had three basic elements, which are the basis of scientific method:
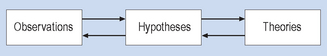
The scientific method is represented in a simple form in Figure 1.2. This representation is consistent with a view of natural science methodology called ‘positivism’ by the 19th-century philosopher Comte, as well as ‘reductionism’. Both these terms have acquired multiple meanings in the area of philosophy of science. Our interpretation of Figure 1.2 is explained below.
Observations, description and measurement
Considering Figure 1.2, let us start with obser-vations. The description of phenomena involving the precise, unbiased recording of observations of aspects of persons, objects and events forms the empirical basis of all branches of science. Observations can be expressed as either verbal descriptions or sets of measurements (see Section 4). The perceptions of the investigator must be transformed into descriptive statements and measurements that can be understood and replicated by other investigators. Some research is based on observation made with instruments (such as recording electrodes, microscopes and standardized clinical tests), while other research calls for observation unaided by instruments. Although advances in instrumentation have contributed enormously to scientific knowledge, the use of complex instrumentation is not a necessary feature of scientific observation. Rather, the key attributes of scientific observation are accuracy and replicability by other scientists. When observations are appropriately summarized and are confirmed by others, they form the factual bases of scientific knowledge.
Generalization and induction
Statements representing observations or measurements are integrated into explanatory systems called hypotheses and theories. The logic underlying scientific generalizations is called induction. Induction involves asserting general propositions (hypotheses, theories) about a class of phenomena on the basis of a limited number of observations of select elements. For example, having observed that penicillin is useful for curing pneumonia in a limited set of patients, we make the generalization ‘The administration of penicillin cures pneumonia (in all patients)’.
Hypotheses
The statement ‘The administration of penicillin cures pneumonia’ is an example of a hypothesis. Scientific hypotheses are statements that specify the expected nature of the relationship between two or more sets of variables. In this instance, the first variable relates to the administration of penicillin and the second variable is related to changes in clinical observations or measurements concerning pneumonia. As we shall see in subsequent sections, an important feature of scientific hypotheses is that the terms used must have clear-cut, observable referents. When these hypotheses acquire strong empirical support, they may be called laws.
Theories
Scientific theories are essentially conjectures representing our current state of knowledge about the world. Hypotheses are integrated into more general explanatory systems called theories. A theory will clarify the relationships between diverse classes of observations and hypotheses. For example, a theory to explain why drugs called antibiotics are effective in curing some infectious diseases integrates evidence from diverse sources such as microbiology, pharmacology, cell physiology and clinical medicine. Other examples of theories are the heliocentric theory of the solar system, the DNA theory of genetic inheritance, and the neur-onal theory of central nervous system functioning. It is an essential feature of scientific theories that they are statements based on the correct use of language and logic. Some theories entail a model (see Fig. D1.1, p. 16), which is a mathematical or physical representation of how the theory works. In this way, theories specify the causes of events and provide conceptual means for predicting and influencing these events. In health care, theories are important for explaining the causes of health and illness and predicting the probable effectiveness of treatment outcomes.
Deduction
A scientific theory should lead to a set of empiric-ally verifiable statements or hypotheses. In add-ition to being generalizations based on evidence, hypotheses are also deduced logically from the statements and/or mathematical models which specify the causal relationships postulated by the theories. For example, if we hold the theory that the patterns of activity of a set of neurones in the occipital lobe mediate visual sensation in humans, then the hypothesis follows that the activation of these neurones (say, by electrical stimulation) will lead to the report of visual sensations. Such hypotheses have been the bases for subsequent spectacular clinical advances such as artificial vision through cortically implanted electrodes.
Controlled observation
It is desirable that hypotheses are tested under controlled conditions. The aim of control is to discount other competing hypotheses for explaining the predicted phenomenon. For example, if we intend to show that occipital lobe stimulation causes the visual sensations, we must show that we are controlling for any type of brain stimulation causing such changes. Conversely, we would need to show that occipital lobe stimulation does not lead to a host of other types of sensations. Only by discounting alternative explanations through control can we have confidence in the relevance of our observations for our research hypothesis. Of course control must be ethical, as we shall see in later chapters.
Verification and falsification
An essential characteristic of a scientific propos-ition is that it should be ‘falsifiable’. That is, there should be a clear empirical outcome that could, if found, show that the proposition was false. For example, consider Einstein’s hypothesis that E = mc2. If laboratory researchers found that the energy locked up in matter corresponded to, say, E = mc3, then Einstein’s hypothesis would be shown to be false. This seems not to have happened yet, so that E = mc2 is falsifiable but not false. After the evidence has been collected, the investigator decides whether or not the findings are consistent with the predictions of the hypothesis. If the hypothesis is supported by the evidence, then the theory from which the hypothesis was deduced is strengthened or verified. However, when the data do not support the hypothesis, the related theory is falsified. If a theory can no longer predict or explain evidence in its empirical domain, it becomes less useful and is usually later discarded in favour of new, more powerful theories. Therefore, scientific theories are not held to be absolute truths, but rather as provisional explanations of available evidence.
The application of the above process has contributed to the spectacular growth of scientific knowledge. Observation and measurement, facilitated by new instrumentation, resulted in the discovery of an enormous number of accurate and reproducible facts about health and illness. New facts both challenge existing theories and call for the creation of novel, more powerful theories. The new theories serve as impetus for more research, resulting in new instrumentation and observations. Advances in scientific knowledge have been applied to creating new technologies, which in turn contribute to new discoveries and advances in scientific knowledge. For example, the invention of computers was possible because of advances in electronics, chemistry and mathematics. In turn, the use of computers is now contributing to making and summarizing scientific observations or formulating explanatory models. In addition, the use of computers as information-processing systems has generated useful metaphors for theoretical advances, such as explaining the human brain and mental functioning. In this way, the scientific method contributes to advancing theory and practice, helping us to describe, explain, predict and sometimes control the world in which we live.
Controversies concerning the nature of method: post-positivism
The above description is not the only interpretation of scientific method. Rather, there are good reasons why the positivist view of the scientific method was challenged in the second half of the 20th century.
First, the scientific method is a set of rules devised and applied by philosophers and scientists. They are not eternal truths, but conventions believed to be useful for conducting scientific enquiry. In this way, not only the content but also the methodology of science is open to criticism, debate and change.
Second, the interpretation of what constitutes the scientific method is an activity pursued by philosophers of science and epistemologists. In exploring different conceptual frameworks (realism, instrumentalism, anarchism, idealism, etc.) concerning the nature of reality and knowledge, philosophers generate unending controversies over the nature of the scientific method.
Third, advances in science contributed to changes to our methods and the ways in which we explain the world. For example ‘quantum theory’ and the ‘theory of relativity’ challenged the mechanistic, clockwork-like view of reality. Modern theories of physical reality are fuzzier and more probabilistic and the observers are not seen as being outside the phenomena they are studying.
The following ideas represent key aspects of the post-positivist view of scientific methodology.
The theory-dependence of observation
Critics such as Chalmers (1976) argued that it is simplistic to believe that observations are made independently of theoretical notions held by the observer. The observer is selective with regard to what is recorded as evidence. Our observations and facts are ‘theory-dosed’, that is, theories specify what observations are of importance and what aspects of these observations should be recorded or ignored. Schatzman & Strauss (1973) put this point elegantly when they stated that the researcher ‘harbours, wittingly or not, many expectations, conjectures and hypotheses which provide him with thought and directives on what to look for and what to ask about’. For instance, in observing the electroencephalogram (EEG) of an epileptic patient, our perception is guided by theories of the electrical activity of the brain and the nature of brain pathology. We will also hold ideas about how the EEG machine works (for example, electrode sensitivity, amplification, etc.) and identify artefacts in the evidence. What is observed as evidence of epilepsy by an expert could be perceived as meaningless squiggles by a naive observer. We shall take account of this point later in this book, when we discuss the reliability and validity of measurement.
The validity of induction
Philosophers of science have questioned the logical validity of making general claims on the basis of a limited set of observations. To quote Chalmers (1976): ‘any observational evidence will consist of a finite number of observation statements, whereas a universal statement makes claims about an infinite number of possible situations’.
For example, we might have observed that the administration of penicillin cured pneumonia in 100 000 patients. This does not necessarily guarantee the logical ‘truth’ of the universal statement ‘penicillin cures pneumonia’, or that patient number 100 001 will be cured. We will look at the theories-related issue of generalization from samples in this book. Scientific theories are seen as probabilistic, in the sense that new, inconsistent evidence might emerge in the future, challenging the generality of the theory. Also, it has been argued by some philosophers of science that hypotheses need not be based on induction, but may arise from any source, provided that they have falsifiable empirical consequences.
What constitutes falsification?
It was stated earlier that when novel empirical evidence is inconsistent with the predictions of a theory, the theory is ‘falsified’ and is eventually modified or discarded. Commentators such as Lakatos (1970) argued that theories are not, in practice, so readily modified or discarded by scientists. Rather, they are structures which have an inner hard core of propositions protected by an outer belt of auxiliary, modifiable hypotheses. Evidence inconsistent with predictions based on the theory results in the modification of auxiliary hypotheses, rather than discarding the ‘core’. Consider, for example, the ‘germ’ theory of infectious disease, on the basis of which one would predict that penicillin (which kills germs) will cure bacterial infections. Suppose that we administer penicillin to a number of patients with an infectious disease and find, contrary to what was predicted, no clinically useful changes. On the basis of this falsification, will we discard the germ theory of disease? No. Rather, we will utilize an auxiliary hypothesis to explain our findings, such as ‘the development of penicillin-resistant bacteria’. The methodological issue which remains controversial is the logical basis for discarding one theory and accepting its rival (see Feyerabend 1975). As we shall see, we judge the outcome of a research programme in the context of an overall pattern of related findings and theories.
Science and the cultural context
Science as a human activity
An important aspect of post-positivism has been the recognition that human values are an integral part of scientific inquiry. Scientific enquiry is conducted in particular social settings, by individuals with personal aims and values. Some more recent formulations of methodology take into account the social and interpersonal conditions which influence scientists’ professional activities (Feyerabend 1975, Kuhn 1970). In this text, we will pay attention to social values, in the context of ethical considerations for designing and conducting research (Ch. 2). Also, we recognize that the formulation of hypotheses and theories are creative acts, rather than the outcomes of the automatic application of induction. In this way, the questions asked by health researchers and the ways in which they explain their findings are influenced in subtle ways by the cultures in which they live and work.
To understand the nature of scientific research in general, and health research in particular, it is useful to examine how they fit into an overall social context. That is, the way in which persons living in a society view health and illness and the ways in which health workers carry out their professional roles influence the range and scope of health care research (e.g. Taylor 1979). Until recently, the ‘medical model’ was by far the most dominant approach to understanding illness in Western society. Briefly, in terms of the medical model, illness is represented by a particular lesion or dysfunction within the human body. The role of the health professional is to identify the location and nature of the lesion or the clinical imbalance and to implement appropriate measures to correct the problem. The patient is assigned a rather passive role in this process, being the ‘locus’ of the lesion or imbalance and a person complying with the health professionals’ recommendations. In the context of the medical model, the most appropriate research is seen as that which improves the technical effectiveness and, therefore, the social power of the health professional.
In Western society the medical model has been, and will continue to be, an influential model for guiding clinical practice and health research. Nevertheless, there have been gradual changes in health care that require the questioning of the generality of the medical model for the following reasons:
The more holistic approach, which also informs health care research, is called the psychosocial or biopsychosocial model (Engel 1977), and currently has had considerable influence in how we conceptualize health care and how we plan and carry out research. At the same time, the medical model strongly based on positivist thinking remains influential in research aimed at understanding the workings of the human body and improving the technical aspects of health care.
Pragmatism: the combined use of quantitative and qualitative methods
Not all scholars agreed with the notion that qualitative and quantitative methods could be logically combined. The controversy was resolved on pragmatic grounds; both methods are needed to solve applied problems in areas such as health care (McGartland & Polgar 1994).
Pragmatism is a system of philosophy that avoids speculation about nebulous abstractions such as ‘The Truth’; rather it defines truth as what works (Tashakkori & Teddlie 1998). A pragmatic, problemsolving approach is followed in the present book, emphasizing the need for both qualitative and quantitative methods for effectively solving health problems.
The introduction of a biopsychosocial approach has raised questions about the combination of methodologies relevant to health sciences research. We perceive patients or clients in two different but interrelated frameworks: first, as broken down or malfunctioning biological systems; and second, as persons, like ourselves, living in a society and who are attempting to make sense of and cope with their particular health care problems.
As argued earlier, the first view informs a reductionist or quantitative approach to research and knowledge. That is, we view our patients object-ively, as natural objects, and attempt to identify and measure important variables which represent the causes and expressions of a clinical condition. We develop models and theoretical frameworks which systematically explain how these variables are interrelated and undertake therapeutic actions which serve to diminish the variables representing illness or disability. Our therapeutic actions are the technical applications for our scientific theories; their outcomes and effectiveness should be tested under controlled conditions.
The second view informs a qualitative or interpretive approach to research and knowledge. We view our patients as persons and attempt to gain insights into their subjective experiences and the reasons for their actions in particular situations. We develop theories for interpreting the nature and development of their personal points of view, and to inform our therapeutic actions so that they seem meaningful and appropriate to our patients.
Take, as an illustration of the above approaches, a patient with cancer. In a quantitative analysis we attempt to quantify the problem by using appropriate instrumentation which measures variables such as the size and location of the tumour and the extent of its spread within the organism. Consistent with current theories of the nature of cancer, various techniques such as surgery, radiology or chemotherapy might be brought into play, the effectiveness of which will be judged in terms of controlling specific variables associated with the condition, such as levels of pain, weight or time of survival of the patient.
With a qualitative perspective, we may address the meaning of the condition from the patient’s personal point of view, within the context of his or her family setting and social circumstances. That is, the patient’s value systems must be clarified and understood before actions such as assessments and therapeutic actions are undertaken. Enquiry might uncover conflicting values, for instance, concerning the implementation of a programme of chemotherapy. From the clinician’s point of view, a radical programme of chemotherapy might seem appropriate, as probably quantitatively extending the patient’s life by several years. However, from the patient’s point of view, the quality of life under chemotherapy might seem inadequate, and also they might not wish to be a burden on their families. Clearly, both in clinical practice and in related research, evidence from both quantitative and qualitative enquiries should be integrated to ensure effective health care.
Although there are differences in how health scientists approach problems, Figure 1.1 shows the sequence of procedures commonly involved in quantitative research. You will find that the organization of this book follows the sequential stages of the research process, as outlined below.
Research and clinical practice
Research methods cover a wide variety of skills and techniques aimed at the methodologically valid investigation of questions of interest to the researcher. These methods of enquiry are not restricted to research laboratories, nor need they involve expensive equipment or large research teams. Rather, these methods imply an approach to stating and answering questions in any setting.
Applied research in the health sciences focuses on issues such as the prevalence and causes of illness, the usefulness and accuracy of assessment techniques, or the effectiveness of treatments. Applied research which is published aims at producing findings that are of general interest to groups of professionals working in the health field.
Research methods interact with health practices in multiple and mutually productive ways. An important general aim of this textbook is to discuss the relationships between theories, practices and the ways in which research methods contribute to improvments in health care. The term ‘evidence-based medicine’ has been defined by Sackett et al (2000) as ‘… the integration of best research evidence with clinical expertise and patient values’. Evidence-based health care (EBHC) is a contemporary movement aimed at ensuring that health services are based on the best available scientific and clinical evidence. The fundamental question which is explored in this book is ‘what constitutes best research evidence?’ The evidence is, of course, produced by applied health research conducted in accordance with the principles of the scientific method. Clearly if you expect to participate in the programme of EBHC you will need to understand research methods sufficiently for making informed and critical judgments concerning the quality of the available evidence.
Finally, we need to keep in mind that the research is produced by the hard work of men and women who were undergraduate students, just like you. Ultimately it will be up to you (as nurses, podiatrists, physiotherapists, speech pathologists and occupational therapists) to carry out the research which underpins the effectiveness, advancement and prestige of your profession. If not you, then who?
Summary
There are several common methods used for acquiring, stating and establishing knowledge. The scientific method is one of these and it underpins the validity of diagnoses and clinical interventions in Western health care systems. The scientific method is concerned with applying a set of rules or conventions that will allow us to produce scientifically valid knowledge. These rules specify how observations should be made, and how theories and hypotheses should be stated and evaluated.
Theories and hypotheses obtained and verified through scientific enquiry are not held to be absolutely ‘true’. An inherent part of the scientific approach is scepticism regarding both the contents of knowledge and the underlying methodology. We have pointed out that there are controversies concerning what constitutes scientific methodology. It was argued that the scientific method is directly applicable to conducting research in the health sciences. In general, the stages for research include planning, stating aims or hypotheses, and formulating designs; collecting, summarizing and analysing the data; and drawing conclusions. This process can be applied to ensuring advances in health care and to problem solving in specific clinical settings. EBHC is a current approach to using best available research evidence for delivering health care. There is a close relationship between professional practices and health sciences research. The rest of the book is organized to follow the stages involved in performing and applying health research.
Self-assessment
Explain the meaning of the following terms: