Chapter 24 Anatomy of male and female reproduction
After reading this chapter, you will have:
Introduction
An understanding of the anatomy of human reproduction enables the translation of abstract concepts of anatomy to normal physiology, function and processes of conception, pregnancy, labour, birth, postpartum and related disorders. This chapter provides a reference point for application to midwifery practice, increasing understanding of the physiological aspects of the birthing process. This brings together theory and practice, enabling knowledge and understanding to be applied in the midwife’s practice and in health promotion. Greater understanding of the structure of the human body increases knowledge of how it functions and why it sometimes deviates from the norm.
The chapter, with its supportive literature, links with other chapters demonstrating how anatomy and physiology may be applied to midwifery practice.
The pelvis
The human pelvis supports the upper body and transmits its weight to the lower limbs, enabling movement in an upright posture. In the female, the pelvis serves as a protective bony ring encircling the reproductive organs, bladder and rectum. In pregnancy, physiological processes effect subtle changes in the composition, shape, plane of inclination and internal dimensions of the true pelvis. These changes enable the female skeleton to support the gravid uterus and are essential to the mechanisms involved in the process of childbirth.
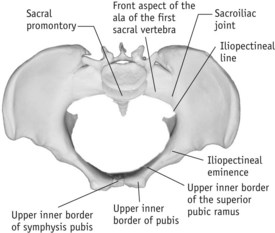
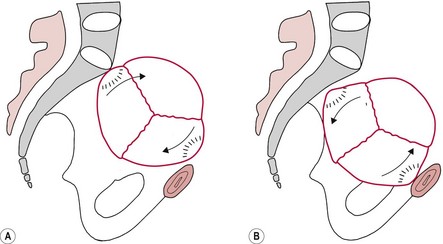
The pelvis consists of four pelvic bones (see Fig. 24.1):
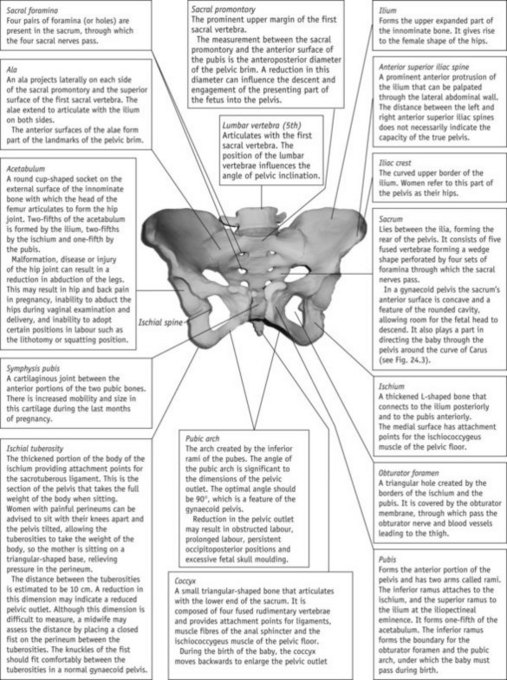
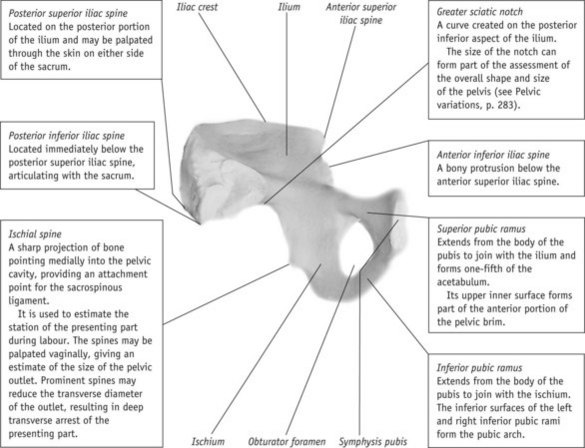
Figure 24.1 The female pelvis. A. Anterior view of pelvis. B. Inner surface of left innominate bone.
The innominate bones are each divided into three regions:
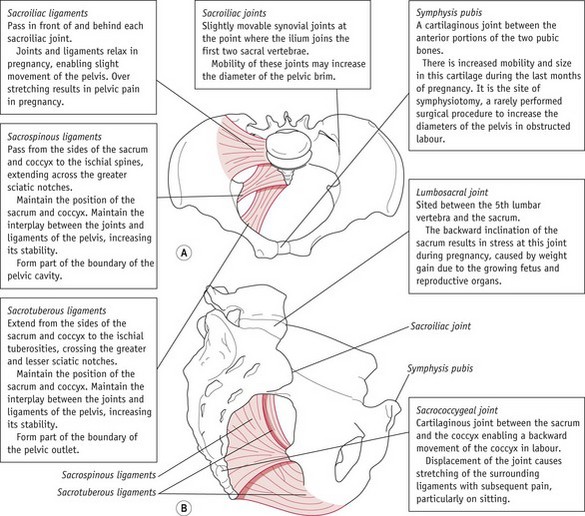
Joints and ligaments of the pelvis
The joints of the pelvis connect the innominate bones at the pubis anteriorly and to the sacrum posteriorly, and the sacrum to the coccyx (see Fig. 24.2). These joints are cartilaginous in type, consisting of plates of fibrocartilage. The pelvis also provides attachment points for ligaments, which are bands of tissue connecting two structures. In normal circumstances, ligaments do not possess the ability to stretch, and therefore prevent excessive movements within the joints, enhancing stability.
In pregnancy, the hormones relaxin, progesterone and oestrogen affect the joints and ligaments, enabling some movement of the joints to facilitate birth. Pelvic pain sometimes occurs during pregnancy, birth or post partum and is thought to be linked to overstretching of ligaments in the pelvis and lower spine (Rost et al 2004).
The true pelvis
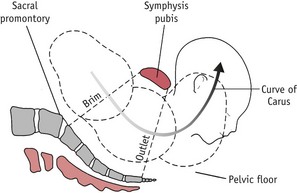
The true pelvis, through which a baby negotiates passage during labour and birth, is the most significant part of the pelvis. This is divided into three regions, known as the brim, cavity and outlet (see Fig. 24.3). As the presenting part descends into the pelvis, the baby negotiates each aspect of the true pelvis simultaneously. For example, in a cephalic presentation, as the baby’s head crowns, the presenting part negotiates the outlet, most of the baby’s head is in the cavity and the shoulders are at the brim.
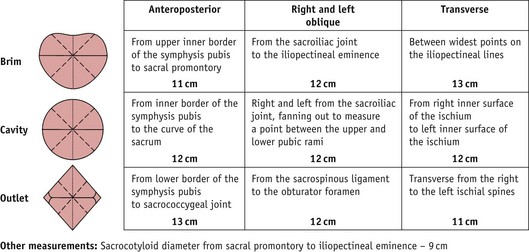
It is important to appreciate that the pelvis is three-dimensional. The pelvic measurements of the brim, cavity and outlet are viewed through a cross-section, whereas measurements incorporated in the pelvic conjugates are viewed through a sagittal section. These two measurements inform a pelvic assessment.
Pelvic measurements (Fig. 24.4)
The pelvic brim is the inlet to the true pelvis and is almost circular, except posteriorly, where the sacral promontory juts into the brim (see Fig. 24.5).
The landmarks of the pelvic brim describe the interplay between the fetus and the pelvis as the presenting part descends, and are a fundamental part of the assessment of descent and engagement of the presenting part. It is not the components of the brim that are important, it is the part that the brim plays as a whole in the assessment of progress during pregnancy and labour. This is the first test that the fetus has to pass as it descends through the pelvis. The midwife assesses engagement of the presenting part during abdominal and vaginal examinations (see Chs 35–37).
The pelvic cavity extends from the brim to the outlet of the pelvis. In the anteroposterior view the cavity is wedge shaped: shallow at the front and deep at the back. Viewed from above it is circular in shape in a gynaecoid pelvis and designed to facilitate the descent and rotation of the presenting part. The boundaries of the cavity are:
The pelvic outlet is diamond shaped and partly bound by ligaments. It can be described in two ways:
Pelvic conjugates
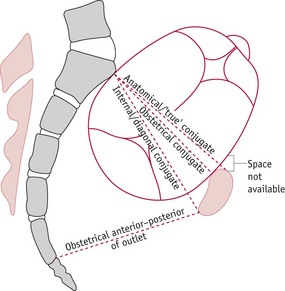
A conjugate is a measurement taken from one point in the pelvis to another. In midwifery there are the anatomical, obstetrical and internal (diagonal) conjugates (Fig. 24.6).
Internal or diagonal conjugate
Reflective activity 24.1
To appreciate the interplay between the regions of the pelvis you need to consider the three-dimensional structures of the regions of the brim, cavity and outlet and how they interrelate to form the anatomical dimensions.
Use a model of the pelvis to locate the structures identified in the text relating to the brim, cavity and outlet.
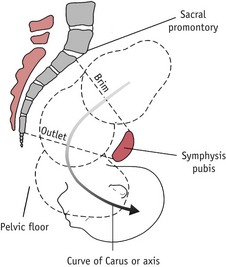
Angles and planes
These are mathematical concepts applied to the pelvis. When standing, the pelvis slopes into a position where the pubis is lower than the sacral promontory – described as an angle of 55° to the horizontal or to the floor. This slope continues through the cavity, reducing its angle to 15° at the outlet. The fetal head must negotiate the curve created by the changing angles within the pelvis as it enters the pelvic brim in a downward and backward direction. It emerges from the outlet in a downward and forward direction as the presenting part reaches the pelvic floor. The curve created in the pelvis is known as the curve of Carus.
The term plane describes the relationship between the pelvis and a flat surface, such as the floor, highlighting the tilt of the pelvis in a normal female skeleton. Hypothetical angles are then created in relation to the degree of tilt of a particular individual (see Figs 24.7 and 24.8), which provide a representation of the angles in relation to the planes of the pelvis. Figure 24.8 shows the axis (curve of Carus), an imaginary line through which a fetus rotates as it passes through the pelvis.
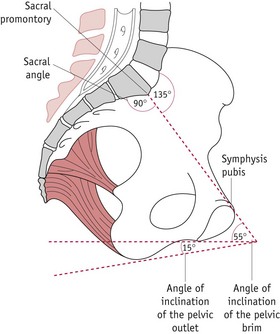
Figure 24.7 The pelvis, showing the degrees of inclination: inclination of the pelvic brim to the horizontal, 55°; inclination of pelvic outlet to the horizontal, 15°; angle of pelvic inclination, 135°; inclination of the sacrum, 90°.
In an abnormal pelvis, the plane of the pelvis may be significantly altered, affecting the axis of the birth canal and consequently the direction of the fetus through the pelvis. The midwife needs to consider the axis of the birth canal when women adopt alternative positions for childbirth during labour and delivery.
Reflective activity 24.2
Rotate Figure 24.2 to represent the woman in a variety of positions, i.e. standing, ‘all fours’ and squatting. Note the direction of the presenting part of the fetus during descent in all positions. What is the impact of these positions on labour?
The subpubic angle is between the two inferior pubic rami forming the pubic arch (Fig. 24.1). In a gynaecoid pelvis, this should be approximately 90°, enabling two finger widths to sit in the apex of the pubic arch during vaginal pelvic assessment.
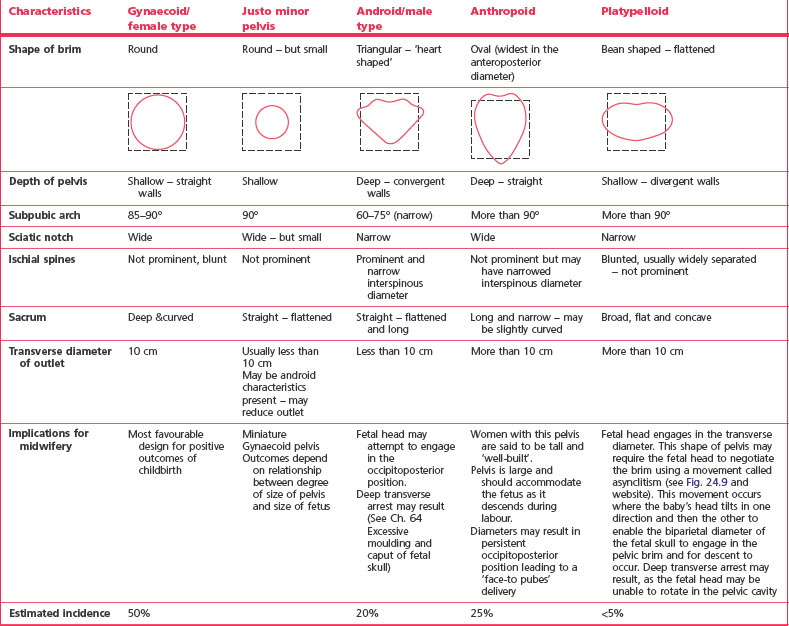
Pelvic variations
Although there are four recognized pelvic categories (Caldwell et al 1940) (Table 24.1), variations within these categories can occur. Some women may have mixed features, such as a gynaecoid posterior pelvis and android forepelvis. The most important factor is the true pelvic space available for the fetus to descend and emerge from the pelvis. The pelvic size and shape cannot be viewed in isolation from other factors, such as position and size of fetus and processes of labour.
Other factors that may influence the size and shape of the pelvis include:
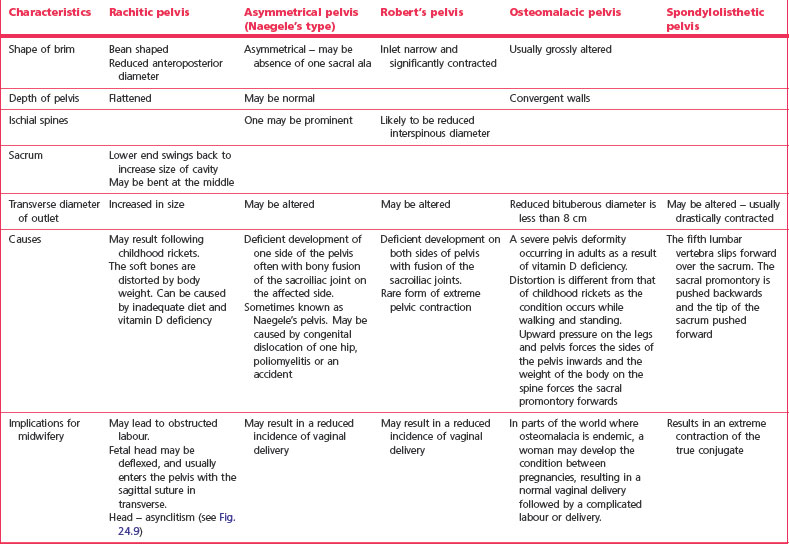
Other pelvic types identified
Any injury or disease of pelvic bones may significantly affect the dimensions of the pelvis, impacting on the outcome of labour and birth. Table 24.2 outlines the classification and characteristics of unusual pelves, each of which may have a mixture of characteristics, with the shape depending upon the degree and timing of damage. It is important that the midwife assesses women at risk of pelvic dysfunction as early as possible antenatally.
Pelvic assessment
Pelvic assessment enables estimation of whether the fetus will successfully pass through the pelvis during labour and delivery, by assessing the pelvic size and outlet. Although this can be undertaken at any time before or during pregnancy, the relationship of the pelvis to the fetal skull can only be assessed from 37 weeks’ gestation (antenatally or during labour). Pelvic assessment is no determinant of outcome but contributes to the overall assessment of pelvic adequacy.
Other factors must also be considered to enable a complete assessment to be made of the overall capacity of the woman’s true pelvis:
Female reproductive anatomy
The primary function of the female reproductive system is production and transmission of ova and provision of a nurturing environment for the fertilized ovum and developing fetus. It has the ability to accommodate the developing fetus, expel the baby and placenta at birth, and return to its near pre-pregnant state during the puerperium. The study of the female reproductive system is fundamental to the midwife’s understanding of gynaecology, pregnancy, birth and the impact birth has on the female reproductive anatomy. The structures identified with the female reproductive system include internal and external genitalia and the pelvis organs and structures (Table 24.3), particularly the bladder, urethra and rectum. In addition, uterine muscular support, blood supply, nerve supply and lymphatics are identified. This knowledge needs to be studied in conjunction with the pelvic floor muscle structure (see Ch. 40).
Table 24.3 Anatomical relations to the vagina
| View | Section of the vagina | Associated structures |
|---|---|---|
| Anteriorly | Upper half Lower half |
Bladder Urethra |
| Posteriorly | Upper third Middle third Lower third |
Pouch of Douglas Rectum Perineal body |
| Superiorly | Centrally Above lateral |
Cervix Fornices Ureters and uterine arteries |
| Inferiorly | Vaginal orifices and vestibule | |
| Laterally | Upper Middle Lower |
Parametrium Pubococcygeus muscles Perineal muscle Bulbocavernosus muscles |
Fetal development
During the first 6 weeks following fertilization, male and female gonads undergo identical forms of development. In female fetuses the ovaries descend a short distance from their position below the kidneys to sit in the pelvic cavity closely alongside the fallopian tubes. Their primary function of ovum production commences under the influence of female hormones during puberty (see Ch. 31).
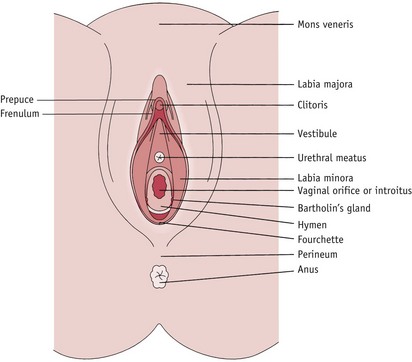
External genitalia
Knowledge of the anatomy of the female external genitalia (Fig. 24.10 and Box 24.1) provides a foundation for application to midwifery practice during the process of labour and birth, in relation to labial and perineal tears; episiotomy; tears to the urethral meatus or clitoris; fistulae and female genital mutilation.
Box 24.1
Female external genitalia
Labia majora
One of two thick folds of fatty tissue (labia majora) covered with skin, extending from the mons to the perineum. The inner surface contains sebaceous glands.
Labia minora
One of two small, smooth folds of skin (labia minora) between the labia majora, containing sweat and sebaceous glands. Anteriorly, the labia minora encircle the clitoris, forming the prepuce and a smaller, lower fold called the frenulum. They meet posteriorly to form the fourchette.
Clitoris
Highly sensitive erectile tissue about 2.5 cm long. Consists of two erectile bodies called the corpora cavernosa and a glans clitoris of spongy erectile tissue.
Vestibule
Extends from clitoris to the fourchette and contains urethral and vaginal orifices. Contains the vestibular glands known as Skene’s and Bartholin’s glands.
Urethral meatus
Situated between the clitoris anteriorly and vaginal orifice posteriorly and is the external opening of the urethra, connecting superiorly to the bladder.
Vaginal orifice or introitus
Located posteriorly to the urethral meatus, opening into the vagina above, with the ability to stretch to accommodate the emerging baby at birth.
Hymen
A thin membrane partially occluding the vaginal introitus – easily ruptured with the use of internal tampons, physical exercise and intercourse. Further rupture occurs during vaginal delivery, resulting in the remaining tissue forming tags – carunculae myrtiformes.
Bartholin’s glands
The ducts of the glands emerge on either side of the vaginal orifice on the inner surface of the labia minora. They secrete mucus to lubricate the vulva, and production increases during sexual arousal. They should not be palpable during vaginal examination unless obstructed or infected.
Any of the following structures may be damaged during the birthing process and must be assessed following birth:
Internal genitalia
Knowledge of female internal reproductive anatomy (Fig. 24.11) enables the understanding of:
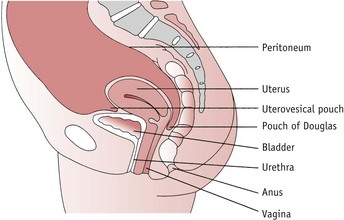
Vagina
The vagina is a fibromuscular tube directed upward and backward approximately parallel to the pelvic brim. It is important to note the angle of the vagina when conducting vaginal examinations and teaching women the correct insertion of pessaries, tampons and contraceptive diaphragms.
The vagina extends from the vulva to the cervix; the anterior wall is approximately 7.5 cm long and the posterior wall 10 cm. The walls of the vagina lie in apposition until it widens at the upper portion where the cervix projects into the vagina at right angles, forming four recesses (fornices). The anterior fornix is shallow and the lateral fornices are deeper. The posterior fornix is deepest, which facilitates pooling of semen during intercourse, increasing the opportunities for sperm to swim through the cervix.
There are no glands in the vagina: moisture is provided by secretions from the cervical glands and transudation of serous fluid from blood vessels. Vaginal secretions are acid (pH 4.5); providing an unfavourable environment for spermatozoa, and counteracted by the alkaline reaction of semen and cervical mucus. The vagina contains lactic acid produced by the action of lactobacilli (Döderlein’s bacilli) on glycogen in the squamous cells of the vaginal lining, causing vaginal acidity. Lactobacilli normally inhabit the vagina without pathology. The lactic acid produced helps destroy pathogenic bacteria that may enter the vagina. In prepubescent girls and postmenopausal women, the vagina acidity is around pH 7, creating a favourable environment for the growth of vaginal infections, such as Candida albicans.
Structure
The walls of the vagina have four layers:
Following childbirth, the vaginal walls must be examined for damage, and assessment made to establish a plan of care.
Function
The vagina is able to distend to facilitate the passage of the penis during intercourse, and the baby during childbirth.
Blood supply
is via the middle haemorrhoidal arteries, arising from a branch of the internal iliac arteries; drainage is through corresponding veins.
Uterus
The uterus is a muscular, vascular, pelvic organ, often described as shaped like an upturned pear. It is situated with the bladder anteriorly and the rectum posteriorly, and normally is in a position of anteversion (leaning forward towards the bladder) and anteflexion (curved forward on itself).
The uterus is divided into the body and the cervix. The narrow end of the uterus is inserted into the vagina and the upper body communicates with the fallopian tubes at the upper lateral surfaces (Fig. 24.12 and Box 24.2).
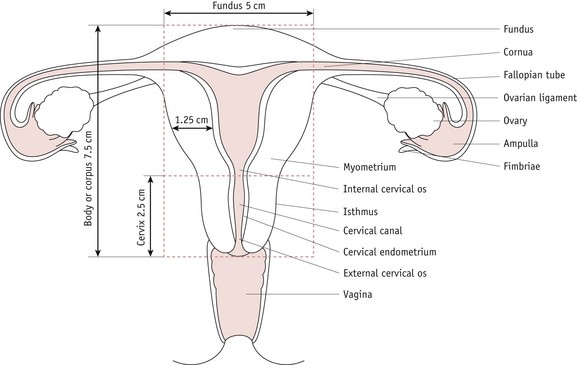
Figure 24.12 The non-pregnant uterus, fallopian tubes and ovaries. (See Box 24.2 for further information.)
Box 24.2
The non-pregnant uterus, fallopian tubes and ovaries
Body or corpus
The upper two-thirds of the uterus. The cavity of the body is triangular in shape. The structure is made up of the fundus, cornua (singular cornu) and the isthmus.
Cervix
The lowest third of the uterus – cylindrical in shape with its lower half projecting into the vagina at right angles.
Internal cervical os
At the top of the cervical canal, its walls are in close apposition in the newly parous woman. It dilates and thins, becoming part of the lower uterine segment during the first stage of labour.
External cervical os
Situated at the bottom of the cervical canal, its walls are in close apposition in the pre-pregnant state, remaining partially dilated in parous women.
Examination of the external os forms part of the assessment of progress during labour.
Cervical endometrium or arbor vitae
The cervical endometrium is arranged in deep folds to facilitate the passage of spermatozoa through the cervical canal. The upper two-thirds is made up of columnar epithelium containing compound racemose glands secreting alkaline mucus. The cervical mucus is thin at the time of ovulation to facilitate spermatozoa. At other times it is thick in consistency, acting as a plug that assists in the prevention of infection in the uterus. The lower third is composed of stratified squamous epithelium continuous with that of the vagina.
Fundus
The upper rounded part of the body of the uterus above the insertion of the two fallopian tubes. It may be palpated:
Fallopian tubes
Two tubes extending laterally from the uterus and opening into the peritoneal cavity. Each tube is approximately 10 cm long and 1 cm in diameter varying along its length. Hairs on the inner surface guide the ova towards the uterine cavity.
Scarring or obstruction caused by infection or trauma may lead to ectopic pregnancy and infertility. Tubes may be surgically ligated for sterilization purposes.
Ovarian ligament
This ligament suspends the ovary in a position close to the fimbriae of the fallopian tube to increase the probability of the ovum entering the fallopian tube.
Ovary
The female gonad that produces predetermined cells destined to become ova. Ovaries are endocrine organs producing oestrogen and progesterone and small amounts of the male hormone, androgen.
Fimbriae
Finger-like projections on the end of the fallopian tube that help to waft the ovum from the ovary to the fallopian tube.
Ampulla
Dilated distal portion of the fallopian tube where fertilization of the ovum usually occurs.
Structure
is the lining of the uterus which constantly changes throughout the woman’s reproductive lifecycle. It has the ability to shed during the menstrual cycle and be maintained and thickened during pregnancy.
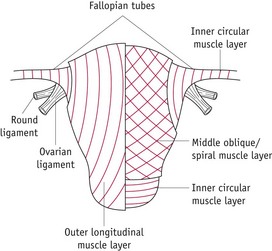
consists of plain muscle fibres and constitutes seven-eighths of the thickness of the uterine wall. In the non-pregnant state, the muscle layers are not clearly defined (Fig. 24.13).
In pregnancy, they become thicker and more defined as three layers of muscle:
is a layer of peritoneum draped over the uterus and fallopian tubes, continuous with the peritoneum covering the bladder, extending to the lateral walls of the pelvis (see Fig. 24.11). Folds in the peritoneum form:
Functions
Uterine ligaments
maintain the normal anteverted, anteflexed position of the uterus. Damage to these ligaments may occur as a direct result of childbirth, especially prolonged labour; chronic constipation and straining; poor lifting techniques; poor posture and obesity. The effect may not be seen until later in life at the menopause, where declining levels of oestrogen cause muscle and ligament atrophy and loss of function. The result of this may be uterine prolapse and associated stress incontinence and defecation difficulties (Fritel et al 2005).
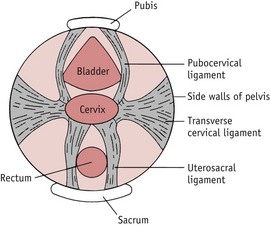
The uterine ligaments (Fig. 24.14) are:
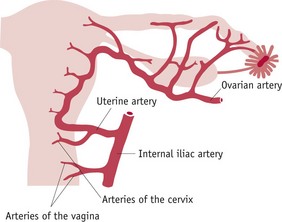
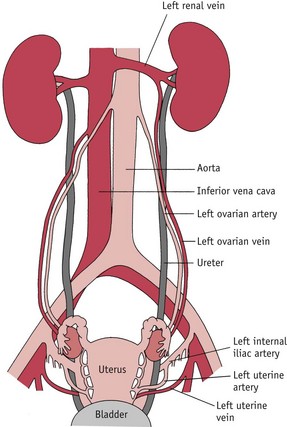
Blood supply
is via uterine and ovarian arteries; drainage is by corresponding veins (Figs 24.15 and 24.16). This provides a rich supply of blood vessels to facilitate growth of the uterus and placenta during pregnancy and supports the growth and development of the fetus. Blood vessels to the uterus are twisted in the non-pregnant state and have the ability to uncoil as the uterus expands during pregnancy.
Breaches of this system can occur during pregnancy, labour and through trauma to the genital tract. This may cause severe haemorrhage, increasing the incidence of mortality and morbidity for both mother and baby (Lewis 2007, MCHRC 2001).
The uterine artery arises from a branch of the internal iliac artery and enters the uterus at the level of the internal cervical os, turning at right angles following a spiral course along the lateral border of the uterus, joining with the ovarian artery, with a branch to the cervix and vagina. Uterine veins follow the arteries and drain into the corresponding internal iliac veins.
The ovarian arteries arise from the descending aorta and cross the urethra and internal iliac arteries before passing over the pelvic brim to enter the broad ligament just below the ovary. Branches of the ovarian artery supply the fallopian tubes and connect with the uterine artery. The right ovarian vein connects with the inferior vena cava and the left ovarian vein connects with the left renal vein.
Nerve supply
is both sympathetic and parasympathetic. The sympathetic nervous system to the pelvis is a continuation of the aortic plexus (sometimes called the presacral nerve), and lies in front of the fifth lumbar vertebra and the sacral promontory. It passes downwards, joining branches of the lumbar sympathetic chain lying on the floor of the pouch of Douglas. The parasympathetic nervous supply emerges from the sacral foramina to join the Lee–Frankenhäuser plexus. The nerves then pass to the uterus and other pelvic viscera (Waugh & Grant 2006).
Lymphatic drainage
The lymphatic vessels and nodes draining lymph away from the pelvic organs accompany the main arteries and veins, with nodes sited along the iliac vessels and the aorta. Drainage from the upper portion of the uterus is to the lumbar and hypogastric nodes, and from the lower portion to the hypogastric nodes.
Cervix
In women who have never been pregnant the cervix can be palpated as a firm structure similar in consistency to the tip of the nose and the cervical os is closed, whereas in a multigravid woman who is not pregnant the cervical os may remain partially dilated.
During pregnancy the cervix may appear to be blue owing to the abundant blood supply, and towards the end of pregnancy it becomes softer as it ‘ripens’ in preparation for labour.
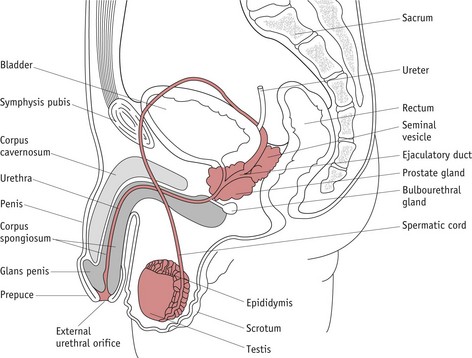
Male reproductive anatomy (Fig. 24.17)
The function of the male reproductive system is the production of spermatozoa and their transfer to the female during sexual intercourse for the creation of new human life. It could be argued that once successful fertilization of the ovum has occurred, the need for knowledge of the male reproductive system is of little importance to the midwife. However, there are a number of issues that could be considered, such as sexual intercourse in pregnancy, transmission of sexually transmitted diseases (see Ch. 57) and understanding of some of the causes of infertility (see Ch. 28).
Fetal development
In the fetus the male testes are located in the abdomen just below the kidneys, similar to the female. The gonads form distinct structures under genetic and hormonal influences (Johnson 2007). In the seventh or eighth month of pregnancy, male testes descend with the spermatic cord through the right and left inguinal canals and at birth should be located in the scrotum of the term infant (Snell 2000).
For more information on the male reproductive system, see the website.
Midwifery implications
Knowledge of anatomy of human reproduction can help identify women who might require different care, treatment and advice, enabling the midwife to plan the most appropriate care during pregnancy, labour and puerperium, and also identify problems which may occur in the fetus and neonate. Early contact with women can identify those who may require further investigations, or referral to the obstetrician for specialist care.
At the booking visit, the woman’s medical and family history must be explored, identifying potential problems which may have been caused by nutritional issues, such as rickets, osteomalacia or anorexia nervosa (Dimitri & Bishop 2007, Ekeus et al 2006). The midwife can identify whether the pelvis may have changed from its original shape through trauma, surgery or oesteoporosis (Leggon et al 2002, Phillips et al 2000) and identify normal changes in gait and in posture, as well as pelvic arthropathy, pelvic pain and symphysis pubis diastasis (Divekar & Keith 2004).
During labour, the midwife uses her understanding of pelvic anatomy to assess pelvic shape and size, using the woman’s history, clinical examination, abdominal palpation and vaginal examination, to provide information to help formulate a dynamic and appropriate plan of care for labour and birth. At this point, the midwife may be able to reduce the rate of prolonged labour, or identify dystocia early, and thus have a significant effect on morbidity.
During the postnatal period, the midwife assesses uterine involution and return to its pre-pregnant state. Any deviations from normal must be swiftly identified and appropriately referred. This includes problems caused by birth trauma, male and female circumcision, stress incontinence, contraceptive methods, sexually transmitted diseases (Ch. 57), and sexual function and dysfunction. During neonatal examination (Ch. 41) the midwife establishes the normality of neonate genitalia and educates the mother accordingly.
Conclusion
Knowledge of human reproduction provides the foundation on which to place everyday practice. This understanding of how human reproductive anatomy is constructed and functions enables a midwife to apply the concepts to both the normal physiological process of childbirth and the concepts of obstetrics. It enables midwifery practitioners to utilize a common language to discuss midwifery and obstetric practice issues with other healthcare professionals. This supports and enhances the midwife’s role as a health promoter and practitioner, interpreting complex health issues and relating them accurately and in appropriate terminology to women and their families.