Chapter 41 Physiology, assessment and care
At the end of this chapter, you will have:
Introduction
Providing the woman with support and guidance in her adjustment to motherhood is an important aspect of the midwife’s role. To achieve this, the midwife works with a range of agencies and professionals to support a seamless process from the antenatal period through to early parenthood.
As well as being a screening test, examination of the newborn enables maternal/paternal–infant interaction through understanding the baby’s unique development and behaviour.
The baby as an individual
Woman-centred care has been an important development in providing choice, continuity and control to women and their families. However, it is likely that the time and attention paid to the assessment and care of the baby, even on a day-to-day basis, has been a fraction of that paid to the woman. It is crucial that babies are viewed as individuals in their own right and that midwives allocate the same attention to their assessment and care. This requires in-depth knowledge of neonatal psychological and physiological development, and complex communication and educational skills.
The baby is recognized as a person (Children Act 1989) with individual needs that require the midwife to act as an advocate and act with duty of care for those needs. Rather than relying on verbal responses, the midwife communicates with the baby via sight, touch and hearing. This must be a focused activity in order to absorb all of the information provided by the baby’s responses and behaviour. Upon completion of the examination, the findings must be discussed with the parents so that the baby’s management and care can be planned as a partnership. Prior to the examination, the midwife must gain consent from the legal guardian. If an unmarried woman is unable to give consent, then it has to be gained from the woman’s next of kin. This should be discussed with the woman when she first attends for care, so that she can provide this information, which may be required in an emergency.
If consent is withheld, then further information, support of a peer, or medical advice may be sought. Consent needs to be obtained by the person providing the care – i.e. if the baby deviates from normal, the decision of how to proceed must be made in partnership with a senior neonatologist.
If the woman wishes the baby to be given oral (or no) vitamin K preparation, the midwife has a duty, under statute (NMC 2004), to ask the paediatrician to see the mother and ensure that the decision-making outcome is recorded in the baby’s notes. If invasive treatment is required, then consent needs to be obtained by the person implementing the invasive procedure, so that the parents can be given the information they need. If the parents feel that they have not been given adequate information, then consent may not be deemed valid (DH 2001).
If the parents refuse life-saving care for the baby, the midwife needs to work with the appropriate professionals (GP or senior neonatologist) to enable the parents to understand the severity of the situation. It is crucial to record what information has been given, and any discussions that take place.
The midwife should clearly document the decisions and justification of actions and omissions, providing a clear picture of the transitional events that occurred at birth and during the first 28 days of postnatal life.
Assessment of the newborn
This assessment is not a ‘one-off’ assessment but a complex, dynamic and continuous activity throughout the antenatal period, labour, at birth and in the neonatal period. Quick recognition and appropriate referral of the fetus/neonate with deviations from normal, results in an enhanced quality of life for that baby and family.
In order to achieve this, a formalized communication system between the baby and midwife is vital.
For a period of 9 months, the fetus has been in a safe, untouched and warm environment in which every need is catered for, free movement is allowed and psychological attachment to the mother is developed.
The long-term effects of the birth experience, and transition from this safe environment, are unknown, and it is imperative that birth attendants consider the baby and the environment he has recently left with equal empathy and care as that offered to the mother.
Applied physiology
The midwife’s knowledge of the transitional events that occur at birth, and the changes to the newborn’s physiology, can be applied to recognition of normal and abnormal events at birth and the difference between primary and secondary apnoea and their management. In this way, the midwife is able to provide thoughtful and reasoned practice and justify all actions.
Respiratory system
In this section, the embryological development of lungs, role of lung fluid, fetal breathing movements, and development and function of surfactant will be explored. The respiratory system consists of:
The transitional events that take place, in order for the baby to take the initial breath, change the lungs from passive organs filled with fluid to structures which play a vital role in aerobic metabolism.
In uterine life, the fetus obtains oxygen and excretes carbon dioxide via the placenta. Although the lungs are not used for gaseous exchange, the healthy fetus makes breathing movements 80% of the time in utero to exercise the muscles of respiration.
Development (see also Ch. 45)
It is important to understand the growth and development of the respiratory system from its initial development at embryonic stage through to prebirth. (See website for additional information.)
A term baby who is hypothermic may exhibit expiratory grunting – where the epiglottis closes prematurely – and does not exhale all carbon dioxide. If this is not treated promptly by increasing the baby’s temperature, respiratory acidosis will result, followed by metabolic acidosis and collapse.
Lung fluid
Lung fluid, a silky clear fluid which may be seen draining from the baby’s mouth at delivery, is different to surfactant. Its function appears to be mainly for cell proliferation and differentiation. At birth, the lungs must switch function from the secretion of fluid to absorption of gases. The catecholamine surge which occurs during labour is probably the final catalyst to complete this change (Milner & Vyas 1982). Some lung fluid is swallowed and then excreted via the fetal kidneys and into the amniotic fluid. At term, 10–25 mL/kg body weight of liquid remains, which is either expelled via the upper airways or absorbed via the lymphatic system of the lungs, a process commenced at the onset of labour and completed at birth (Taeusch et al 2004).
If delivered by elective lower section caesarean section (ELSCS), the burst of catecholamines provided by the onset of labour will not occur. The lungs will not have been compressed to expel lung fluid. The lung fluid is not absorbed and may be present following birth. Therefore, the midwife will need to observe the baby closely for signs and symptoms of transient tachypnoea of the newborn (TTN) (see Ch. 45).
Factors affecting lung maturity
Hormones – including steroids, insulin, prolactin and thyroxine – influence lung maturity and dictate how well the baby’s lung will function following birth.
Catecholamines are substances normally released in adults in response to stress and in the fetus may be identified around the onset of labour. These have a twofold action on the alveoli: increasing the lecithin:sphyngomyelin ratio to enhance synthesis of surfactant; and decreasing lung fluid production and increasing absorption of lung fluid during the labour process.
Fetal breathing movements
Fetal breathing movements occur from 11 weeks of gestation. As the fetus grows, the strength and frequency of breathing movements increases until they are present between 40–80% of the time at a rate of 30–70 breaths per minute (Davis & Bureau 1987).
Respiration in the neonate
Ribcage and respiratory musculature are immature and will continue to develop into adulthood (Harris 1988). The diaphragm and abdominal muscles are used for respiratory movement and it may be difficult to see movement of the chest when counting respiratory rate (more easily measured by observing the rise and fall of the baby’s abdomen).
For the first 2–3 months of life, the baby is an obligatory nose breather and is unable to breathe through his mouth, thus it is vital that the nose is kept clear at all times of any obstacles such as eye protection pads.
Breathing rate is a simple guide to wellbeing but needs to be assessed alongside the baby’s behaviour while validating normality. The respiratory rate is usually between 40 and 60 breaths per minute. Newborns are periodic rather than regular breathers and premature babies more so than full-term babies. They may have periods of even and uneven breathing with long gaps between breaths. A baby that has been very active or crying may have a respiratory rate above 70–80 per minute and during sleep the rate may be less than 40.
Tachypnoea (rate of >60) is a result of increased carbon dioxide and baroreceptors providing the information to the medulla; thus, an increased respiratory rate may reduce the respiratory acidosis (see Ch. 45).
Breathing movements should be symmetrical. Babies can generate spontaneous pressures above 70 cmH2O and develop a spontaneous pneumothorax; therefore, symmetrical movement of the chest confirms normality.
Babies mainly use the diaphragm to aid breathing, and so the diaphragm should also move symmetrically, confirming phrenic nerve integrity. Damage to the phrenic nerve can occur following shoulder dystocia and it is important to validate normality at an early stage to avoid later respiratory arrest.
Abnormal signs
Control of respiration
The control of the respiratory system is mainly autonomic, involving the cortex, brainstem, airways, aortic/carotid chemoreceptors and central control by the medulla. The development and maturity of the central nervous system influences control of respiration, as does temperature, drugs, hypoxia, acidosis and the sleep state of the infant.
At birth, the umbilical cord is clamped and cut; this causes major circulatory changes which divert the blood to the fetal lungs rather than to the placenta for oxygenation.
Cardiovascular system (CVS) in the embryo and fetus
The first functioning system in the embryo, the CVS, is composed of the heart and blood vessels and is a closed system that continuously circulates a given blood volume. Blood can be seen circulating in the body by the end of 3 weeks.
Fetal circulation (see Ch. 45)
The structure of the heart provides a circulatory process different from that needed to maintain cardiovascular function after birth. There is low systemic pressure and an increased pulmonic pressure, leading to very little blood flow to the lungs, which are non-functional in utero. The fetal brain requires the highest oxygen concentration and the fetal circulation is designed to provide the vital organs such as the brain, liver and tissues with the maximum concentration of vital materials.
Within the fetal system, oxygen content varies throughout the circulation and is lower than in the neonate or adult; with a concentration of fetal haemoglobin (18–20 g/dL), fetal blood has a high affinity for oxygen.
Changes at birth
At term, only 5–10% of the cardiac output perfuses the lungs to meet the needs of cellular nutrition, owing to pulmonary vascular resistance, the patent ductus arteriosus and low resistance of the placental component of the systemic circulation.
Following the birth and the taking of the first breath the right atrial pressure is lowered and the left atrial pressure is increased slightly, causing closure of the foramen ovale. Aeration of the lungs opens up the pulmonary capillary bed, lowering vascular resistance and increasing the pulmonary bed blood flow. The neonate can generate a pressure of up to 70 cmH2O during inspiration and 20–30 cmH2O on expiration (Strang 1977). This is thought to force fluid out of the lungs to overcome the high resistance and surface tension of the alveoli and to be necessary to establish lung volumes distributing gas through the lungs.
Oxygenation and the reduction of endogenous prostaglandins from the maternal circulation further reduces the vascular resistance and initiates the closure of the ductus arteriosus. As a result of pressure changes within the heart, the foramen ovale closes functionally at or soon after birth from compression of the two portions of the atrial septum. The ductus arteriosus is closed functionally between the fourth to seventh day, closing structurally later when fibrin is laid down – which can take several months to complete.
These physiological changes normally starts when the neonate takes the first breath. The neonatal brain must be functioning adequately in order for the baby to continue to breathe at a sufficient rate to allow homeostasis of oxygen and carbon dioxide within the body.
The vessels which in intrauterine life carried deoxygenated blood to the placenta, the umbilical and hypogastric arteries, and those which conveyed oxygenated blood from the placenta to the fetus, the umbilical vein and the ductus venosus, also close and later become ligaments.
These circulatory changes take place over a period of hours or even days. Respiratory and cardiac disorders accompanied by hypoxia and acidosis may delay, or even reverse, the circulatory changes in the heart and lungs.
Changes in the blood
At birth, the baby has a high haemoglobin concentration (about 17 g/dL), mostly fetal type, HbF, which is required in utero to increase the oxygen-carrying capacity of the blood. Since oxygenated blood from the placenta is soon mixed with deoxygenated blood from the lower part of the fetus, the overall oxygen saturation of fetal blood is therefore reduced.
After birth, the high number of red blood cells is not required, so haemolysis of excess red blood cells takes place. This may result in physiological jaundice of the newborn within 2–3 days of birth (see Ch. 46). The conversion from fetal to adult haemoglobin (HbA) starts in utero and is completed during the first year or two of life. By the age of 3 months, the haemoglobin has fallen to about 12 g/dL.
At birth, the prothrombin level is low because of lack of vitamin K, a cofactor required for the activation of several clotting proteins in the blood. A deficiency may result; for example, following ventouse birth the baby can develop a subgaleal haemorrhage (bleeding in the potential space between the skull galea aponeurosis). Vitamin K administration can rapidly correct such a clotting problem. By the fifth or sixth day, milk feeding is usually established and the bacteria necessary for the synthesis of vitamin K are present in the intestine.
Temperature control
Following birth, the baby must adjust to a lower and labile environmental temperature. The heat-regulating mechanism in the newborn is inefficient and the body temperature may drop unless great care is taken to avoid chilling. Heat is lost by radiation, convection, evaporation and conduction. These factors can be rectified if the baby is born into a warm environment of 26°C, dried carefully and wrapped warmly or provided with skin-to-skin contact with the mother (see Ch. 42).
Skin
The full-term newborn’s skin is well developed, opaque with few veins visible, has limited pigmentation and wrinkles around joints.
The layers of the skin include the epidermis, dermis, and subcutaneous layer. The epidermis is a thin, effective barrier preventing penetration and absorption of potential toxins and microorganisms and retaining water, heat, and other substances (see website).
The skin of full-term newborns is covered with a varying amount of vernix caseosa, a thick white, creamy substance. This forms between 17 and 20 weeks’ gestation and by 40 weeks is found primarily in creases such as the axilla, neck and groins, acting as protection during uterine life (Moore & Persaud 2007). Vernix is a perfectly balanced moisturizer and any surplus should be massaged gently into the baby’s skin after the birth.
Gastrointestinal system (see website)
Normal function of the gastrointestinal (GI) system should be established prior to artificially feeding the newborn baby. This can be achieved through reviewing the woman’s history and antenatal profile. Polyhydramnios, for example, may indicate disruption of the GI tract.
The midwife needs to understand glucose metabolism of the fetus and newborn in order to support the woman in her chosen method of infant feeding (de Rooy & Hawdon 2002) (see Ch. 43).
After birth, the maturation of the GI tract is stimulated by specific peptides: enteroglucagon stimulates intestinal mucosa to develop and motilin encourages gut motor activity.
Nutritive/non-nutritive sucking is the baby’s main pleasure and may be satisfied by breast- or bottle-feeding alone. Babies will find solace in sucking their fingers or thumbs or suckling at the breast. Mothers need to understand why the baby is frequently feeding, so that they are reassured and not concerned that they have insufficient milk to satisfy their baby.
The knee-to-abdomen position increases abdominal pressure and may cause vomiting of newly ingested food, therefore napkin changing should be avoided soon after a feed. The supporting gastric and intestinal musculature of the newborn is relatively deficient, shown by the reduced peristaltic movement and the tendency towards distension. The use of pethidine or morphine during labour may decrease peristalsis and in some cases increase regurgitation for several days following birth.
Meconium, a soft, greenish black viscid substance which has gradually accumulated in the intestine from about the 16th week of intrauterine life, consists of mucus, epithelial cells, swallowed amniotic fluid, fatty acids and bile pigments.
Renal system
The fetus passes urine into the amniotic fluid during pregnancy and oligohydramnios may indicate renal abnormalities. At term, the kidneys are relatively immature, especially the renal cortex. Glomerular filtration rate and ability to concentrate urine are limited. Relatively large amounts of fluid are required to excrete solids.
The baby should pass urine, which has a low specific gravity, within 24 hours of birth. Initially, urinary output is about 20–30 mL per day, rising to 100–200 mL daily by the end of the first week as fluid intake increases.
If the baby becomes dehydrated, excretion of solids such as urea and sodium chloride is impaired. Dehydration can be recognized by a sunken fontanelle, dry mouth and skin inelasticity, and, most importantly, more than 10% loss of birth weight. It is important to note that a baby who is dehydrated will continue to pass the normal amount of urine, thus a wet nappy does not validate normality.
Glucose metabolism
See website for fetal metabolism.
In utero, the fetus relies on the intravenous transfer of glucose and other nutrients via the umbilical vein for growth and development. Fetal metabolism is directed to anabolism under the influence of insulin, utilizing glycogen, fat and protein.
Metabolic adjustments after birth
After birth, normoglycaemia must be maintained to protect brain function and to adapt to the intermittent delivery of milk into the gut for nutritional needs. The normal term neonate is able to adapt physiologically to episodes of starvation by utilizing ketone bodies. This is reflected in a postnatal fall in blood glucose concentration, which may be wrongly viewed as pathological and managed accordingly (de Rooy & Hawdon 2002). Following birth, the breakdown of glucose continues under the influence of insulin, but about 8 hours after birth, the baby begins to switch to glucagon metabolism.
Musculoskeletal system
The musculoskeletal system provides stability and mobility for all physical activity and includes the bones, joints, and supporting and connecting tissue. This provides a means of protection for vital organs (brain, spinal cord), mineral storage (calcium, phosphorus) and production of red blood cells. In comparison with an adult or child’s skeleton, the newborn’s skeleton is flexible, the bones mainly consisting of cartilage, and joints are elastic, facilitating the passage through the birth canal.
Normal variations in shape, size, contour, or movement may be due to position in utero or genetic factors and should be distinguished from congenital anomalies and birth trauma. Early diagnosis of disorders and early intervention often prevent long-term deformity and the need for surgery.
Central nervous system
The development of the neurological system commences 18 days post conception (see website). After birth, the brain continues to grow rapidly within the first year of life, follows a more gradual growth rate until the age of 10, and then there is minimal growth to adolescence. Physiological and psychological wellbeing are vital to the development of full neurological potential.
Babies born at term can be active participants in their environment and are capable of social interaction. It has been shown that they are able to mimic the expression of their carers and are able to some extent to self-regulate themselves.
At birth, the baby’s autonomic system maintains homeostasis of all major organs, regulating temperature and cardiorespiratory function. The well newborn will have mature autonomic and motor systems which can be assessed by the ability to maintain stable cardiorespiratory function. If the baby is unwell or premature, handling will stress the autonomic system and the baby can become cyanosed and bradycardic (Roberton & Rennie 2001).
State of consciousness in the newborn is influenced by the reaction to stimuli, and understanding the baby’s level of consciousness ensures sensitive care and management in assisting in the adaptation to the environment and advance through stages of consciousness. Providing this information to the mother assists her in caring for her baby, may assist feeding, and utilizes the baby’s energy and available resources effectively (see Box 41.1).
Box 41.1
States of consciousness in the newborn (Brazelton & Nugent 1995)
Awake states
Babies are able to ‘tune out’ noxious stimuli and this occurs through the process of habituation. The baby stores the memory of the stimulus and with repeated episodes learns not to respond to it. Overstimulation of babies who are on system overload will cause them to suffer further stress, requiring appropriate care such as minimal handling and an environment with minimal noise and lights in order to support recovery.
The newborn baby has very poor motor development compared with other mammals but highly developed senses (sight, hearing, taste, smell); hence the importance of picking babies up, talking to them and stroking them to stimulate and evoke response. Maternal–infant interaction is facilitated by eye-to-eye contact with the mother. A 12-day-old baby is able to imitate the facial and manual gestures of adults and this may operate as a positive feedback mechanism to caregivers.
Protection against infection
In utero, the fetus is protected from infection by the intact amniotic sac and the barrier mechanism of the placenta, although certain microorganisms do cross the placenta and may infect the fetus (see Ch. 47). During the last trimester of pregnancy, there is a transplacental transfer of IgG from the mother to the fetus, providing protection against the infectious diseases to which the mother has antibodies. These antibodies provide baby passive immunity for about 6 months (Remington & Klein 2000).
The newborn baby has no immunity to the common organisms, and when exposed to them at birth for the first time, is highly susceptible to infection. Soon after birth, the baby becomes colonized by the mother’s set of microorganisms, facilitated by early and frequent contact. Clinical infection occurs when the number and virulence of the organisms overwhelm the poorly developed defence mechanisms of the baby. Breastfeeding encourages specific bacteria to multiply in the bowel and the acid conditions that result from this may help to prevent the overgrowth of potential pathogens, providing some protection from infection.
Care at birth
Preparation
The midwife is obliged to support the birth of any baby showing signs of life at any gestation – in all environments, including outside hospital. It is crucial that midwives are knowledgeable about the physiology of the baby born at different gestations, and how this changes their care and management needs.
Preparations should be made prior to the baby’s birth and these include identifying women whose babies are at increased risk or who will require specialist care following delivery. The midwife must be prepared to provide care for ‘high-risk’ and ‘low-risk’ women (see Box 41.2), though research indicates that the classification of risk factors remains a debatable area.
Box 41.2
Risk factors for specialist care (Levene & Tudehope 1993)
The development of complications during labour and birth is a major contributor to increased neonatal mortality and morbidity (MCHRC 2001). The midwife can identify that all is normal, detect any deviations and make appropriate referral or alter management of care accordingly.
This action plan begins antenatally to ensure that the woman is prepared and informed to self-manage her body and pregnancy so that she becomes confident and seeks appropriate support should deviations occur.
At birth, the transition to independent life involves a significant physiological shift. The midwife needs to have a good insight into changes of fetal physiology, in order to evaluate the care each individual newborn baby requires.
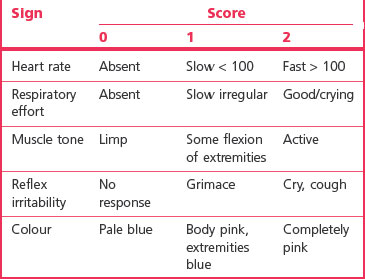
The Apgar score
The Apgar score, devised by Virginia Apgar in 1953 (Levene & Tudehope 1993), is a universally and commonly used quantitative measure of the neonate’s wellbeing at and around birth, though criticized for its simplicity. Five indicators are used to measure this: heart rate, respiratory effort, colour, muscle tone and response to stimuli (Table 41.1).
Recording the numerical score alone provides insufficient information concerning the neonatal condition. The important factor is that the neonate’s physiological condition and progress is recorded verbally and in writing until the neonate is in a good condition.
It is also advisable, if more than one practitioner is present at a delivery where resuscitation is undertaken, that the baby’s Apgar score is agreed between practitioners prior to the formal record being made. Disagreements can be discussed with the supervisor of midwives and senior neonatologist. It is important for the future management of the newborn’s wellbeing that an accurate assessment is given (UK Resuscitation Council 2006).
The heart and respiratory rate, the most important measures within this scoring system, will indicate the nature and timing of active resuscitation. An Apgar score of 8–9 indicates that the neonate is in good condition. The midwife should expect that most mature babies would obtain a score of about 9 as those above 38 weeks’ gestation will have a mature neurological system restricting blood flow to the extremities in order to supply the brain and other major organs with extra oxygenated blood. Therefore the baby will have acrocyanosis and this continues until after 24 hours because of poor peripheral circulation (see website).
Maternal–infant relationship
The relationship between mother and baby begins at birth. The experience of the pregnancy may act as a positive or negative foundation for this relationship. The mother’s reaction to her baby will vary greatly according to her culture, experience, expectations and environment and will be affected by her physical and emotional state. In some cultures, the mother will wish to have immediate and close contact with her baby from the moment of birth. Others will want the baby cleansed before holding. So that individual needs can be appropriately met, the midwife needs to discuss the mother’s wishes, expectations and fears prior to the labour.
‘Bonding’ is a term to be used with caution as it may imply an immediate and strong relationship at the moment of first sight. This may be very threatening and inhibiting for some mothers who will build up their relationship with their new baby in a slower and less obvious way, though the end result is as enduring and strong (see website).
Research illustrates mothers’ reactions to newborn infants. The mother’s first response is to touch her baby (easier if the baby is naked) with fingertips, progressing to a protective caressing movement. The mother will often then move the baby to a position to facilitate face-to-face eye contact. Throughout this time, she talks to the baby in a higher-pitched voice than usual (Klaus & Kennell 1976). Early research suggested the existence of a ‘sensitive time’ around the birth, at which the mother and baby should be encouraged to be together, and that women missing this time were at risk of neglecting or abusing their infants. However, Brazelton postulated that even should parent and child have to be separated, if the attendants ensure that the mother has photographs of her baby and is involved in the baby’s management and care, cuddling or even just touching her child, the relationship can be effectively preserved and nurtured (Brazelton 1983).
Warmth
The baby, accustomed to a constant intrauterine temperature of 37.8°C, is born into a much cooler atmosphere, ideally 26°C. At birth, the baby should be dried immediately to prevent evaporation and handed to the mother to keep warm, avoiding unnecessary exposure. Warm covers are placed over the baby, if necessary for skin-to-skin contact, and later the baby should be dressed, covered appropriately and placed in a preheated cot. Within an hour of birth, the baby’s axillary temperature is taken using a low-reading thermometer (see Ch. 42).
Identification
Two identification labels record name, date of birth and sex, using an indelible pen with clear and legible writing. These should be shown to the mother or partner and applied to the baby’s ankles or wrists in the mother’s presence. Should a label become detached, a replacement should be completed and placed on the baby using the same procedure. Ideally, the labels should not be removed until the baby is in his own home. During daily examination, these labels are checked by the midwife for cleanliness, comfort – neither too tight nor too loose for the baby’s wrist or ankle – and number (i.e. two).
Several maternity units have developed systems to ensure that babies are properly identified and secure, including recording footprints and handprints, and these should include the names of the mother and baby.
Ideally, a resuscitaire should be situated in the delivery room, because, should the baby need resuscitation, to remove him from his parents can add significantly to their distress. If the baby has to be separated from the mother, a relative must accompany the baby to enable feedback to be given to the mother as to what events took place and to validate that the baby returned to the mother is indeed her own baby.
Vitamin K
Following birth, free circulating vitamin K is low, decreasing during the first few days of life and gradually rising after 3–4 days. This may result in excessive bleeding if trauma occurs, for example during instrumental delivery.
It has been advised that all babies should be given vitamin K (DH) and parents should be provided with information on whether or not to give vitamin K and the route of administration as advised in the Drugs and Therapeutics Bulletin (www.dtb.org.uk/dtb/index.html).
Vitamin K deficiency bleeding (VKDB) (formerly known as haemorrhagic disease of the newborn) is a bleeding tendency which results from a lack of ability in the newborn to utilize vitamin K (see Ch. 44).
Oral use of vitamin K
Absorption from the gastrointestinal tract is erratic in the newborn and there is the possibility of regurgitation, inhalation and loss of vitamin K. Additional evidence is required before firm recommendations can be made concerning the optimal dose and form of the vitamin K.
Prophylaxis against late-onset haemolytic haemorrhagic disease of the newborn (HDN)
As three babies have been reported to have developed VKDB (late onset) after being given vitamin K at birth, it cannot yet be confirmed how best to prevent this.
The blood spot (Guthrie) screening test provides a simple method for assessing VKDN. Three minutes of pressure should be applied to the site after taking the blood sample, and a note made of the time taken for the bleeding to stop. Plasters damage the baby’s skin and should not be used unless absolutely necessary.
Examination of the newborn
The first question parents ask is whether or not their newborn baby is ‘normal’, as they examine him from head to toe in minute detail, equal to that of any dedicated professional. This is always an important adjunct to the midwife’s assessment and, prior to any examination, parents’ participation is welcomed and any concerns they have should be identified and discussed.
Three types of examination of the newborn are carried out:
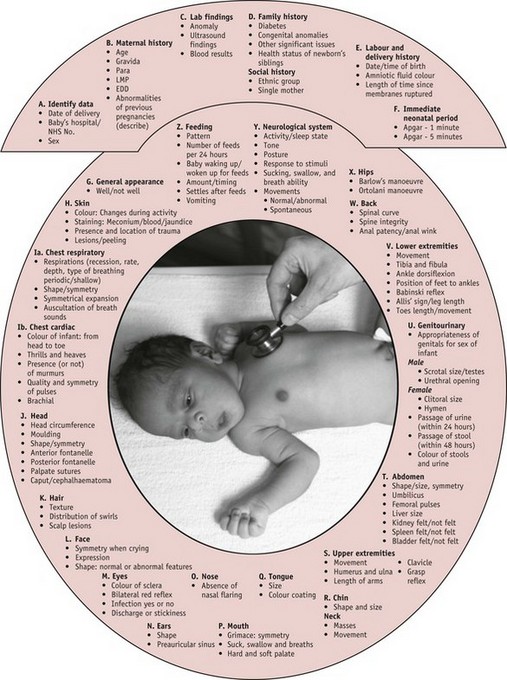
Each examination has a slightly different purpose, but all should follow a systematic process, and be undertaken with the principles set over the following pages, which will provide the midwife with the best means of assessment (see Fig. 41.1).
Initial post-birth examination
The midwife will undertake a thorough examination of the newborn soon after birth. This initial examination uses information elicited from intuitive knowledge gained from experience; the Apgar score; and physiological assessment using the senses: sound, vision and touch. It provides basic information, detects any obvious abnormalities or deviations from normal that require referral, and provides an opportunity for the midwife to support the parents in their role as carers for the new addition to their family.
Prior to this first examination, the baby should have at least 1 hour following birth to recover (NICE 2006). This allows mother and baby time to adapt to physiological changes and gives the baby time to adapt to the environment and, if breastfeeding, to feed successfully.
The holistic examination
This examination – including heart and lung sounds, full central nervous system examination, abdominal examination and examination of the neonate’s hips – is undertaken by an appropriately trained health professional. Some of these skills require postgraduate training at present. The main aim of the holistic examination is to validate normality and, where possible, detect abnormalities and communicate any action required to the parents.
Since 1994, increasingly midwives have undertaken this holistic examination rather than their medical colleagues, providing continuity of care as recommended by Changing childbirth (DH 1993), facilitating the midwife’s self-audit and with the potential for improving interprofessional partnerships (Hall 1999).
Midwives have a vital role to recognize and validate normality and refer when deviation from the norm is detected. Any possible problems should be ascertained at the outset, providing stabilization and minimizing any future harm prior to transfer in order to ensure future wellbeing.
The United Kingdom National Screening Committee (UKNSC) of the Newborn and Infant Physical Examination (NIPE) (UKNSC 2008) advocates the first holistic examination is undertaken within 72 hours of birth, allowing the postnatal transition of major organs, such as the heart, to take place prior to examination. This is done prior to discharge and transfer to the care of a health visitor and GP. It is expected that the midwife (NICE 2006) will care for the newborn from birth to 6 to 8 weeks. It is intended that the second holistic examination is combined into a single postnatal visit at 6 weeks to validate the woman’s wellbeing. In between those two examinations, the midwife will assess each baby, reviewing past and present individual history prior to deciding which criteria need assessment during physical examination and which can be validated through observation alone.
Examination of the newborn assessment tool
A clinical assessment tool (see website also) has been designed to assess the physiological and behavioural cues to assist the midwife to validate normality and recognize deviations (Michaelides 2010).
Using a tool enables the midwife to gather important information through assessment and analysis of the woman’s oral and recorded history. A systematic framework, beginning with examination of the heart while the baby is quiet, goes through to the most intrusive testing – the Moro reflex and measuring the head circumference – at the end. The latter is undertaken last as the baby will find it uncomfortable and will require comforting upon completion.
The tool consists of 26 criteria (Fig. 41.1 A–Z), the number of which that will be fully examined at each examination being dependent on the purpose of the examination, and the experience and training of the midwife.
Preparation
Preparation is vital to ensure a smooth and effective examination process. An area, to provide privacy and a controlled environment, needs to be set aside; an examining table with an overhead heater and light source can be utilized to examine babies at a height that will prevent practitioner back strain. It provides a safe environment for the baby (see Fig. 41.2) and a safe storage space for the required equipment (see Box 41.3). In the home environment, the midwife can use a changing mattress or table (or similar surface area) covered with a warm sheet/towel to examine the baby.
Communication
After the examination, the midwife must explain what has been examined and why. For women who are unable to speak English, link workers or translators are essential. The midwife must demonstrate an ability to communicate with the baby, an understanding of his ‘language’, to observe and note physiological and behavioural wellbeing.
Informed consent
The NIPE booklet Screening tests for you and your baby (see website), offered to mothers at booking, recommends midwives discuss the information with mothers at 36 weeks, and prior to the examination, enabling parents the time and information needed to give informed consent to the examination of their baby.
Daily examination
As part of the postnatal examination, the midwife will examine the baby, including checking the eyes, skin, umbilicus and napkin area, feeding patterns, and (if in hospital) the presence of two identification labels. This examination provides an opportunity to teach the mother what to look for in monitoring her baby’s wellbeing, and to learn skills in baby care.
Physical assessment of the newborn
The baby enters postnatal life from a quiet, dark, warm, wet environment, with boundaries provided by the uterus, entering a whole new world. While drying the baby or, in the case of waterbirth, when the baby reaches the surface, the midwife assesses adaptation to extrauterine life by undertaking the Apgar score at 1 and 5 minutes with a brief physical assessment to exclude gross structural abnormalities.
During the first hour of life, the baby is given to the mother or father and interaction begins. As the baby is alert in this first hour, the mother should be supported to give a first breastfeed. If artificially fed, the midwife needs to undertake a fuller assessment of the gastrointestinal system. The baby who breastfeeds will take in a small, but valuable, quantity of colostrum. A baby given formula is likely to take an amount of fluid which, if the GI tract is incomplete, such as in cleft palate or imperforate anus, may cause preventable damage.
Formal assessment of the newborn
Physical examination of the newborn baby should be performed systematically, examining each physiological system to ensure entirety (see Fig. 41.1), using the skills of observation, palpation and, where relevant, auscultation. Each system should be critically evaluated, normality validated and deviations recognized. Where deviations occur, the midwife needs to ascertain the severity in order to plan appropriate management and transfer to the care of the neonatologist as appropriate.
The midwife needs to explain that the assessment of wellbeing is a continual process and that each examination only validates normality for that moment in time. With continual observation, care and professional support through education and physical assessment, there is a growing reassurance.
History
During the antenatal period, a full record is taken of the family, previous medical and obstetric histories of the woman and partner. The present pregnancy, labour and prenatal period should be reviewed to identify any risk factors which may affect the baby.
When obtaining a history from women, it is important that the communication process is open and interactive. Women should be given the reasons for certain questions and how this affects the care provided (see website).
Laboratory results need to be assessed by the midwife for their relevance to the assessment of the newborn. For example, a group O positive mother with a baby who is jaundiced may trigger consideration of the possibility of ABO incompatibility.
Kell antibodies can attack the bone marrow, reduce red cell production and may result in the baby being anaemic at the time of birth. Anaemia in the newborn will render the baby hypoxic, requiring resuscitation at the time of birth and administration of fresh blood.
Sexually transmitted diseases, if not treated in the antenatal period, may affect the baby postnatally and thus the baby will need to be observed for signs of infection (see Ch. 47).
Health education is important though it is not always possible to reduce at-risk behaviour of women, and a non-judgemental and supportive approach is required in obtaining true and accurate information to facilitate appropriate care (see website).
Information such as the date of the first day of the last menstrual period (LMP) and the estimated date of conception (EDC) is crucial in the calculation of gestational age, an important aspect of management of care.
When undertaken correctly, fetal surveillance (see Ch. 36) can assist the midwife to have the relevant practitioners present at birth. The type of birth may affect the management of the baby – after a protracted labour, the baby may be traumatized and may require an initial superficial examination to validate wellbeing, followed by a full examination when signs of recovery are apparent. Minimal handling may assist the shocked newborn to recover. The examination should last no longer than 15 minutes.
Maternal concerns are an important guide to the focus of the examination as the majority of women will spend time examining, feeling, stroking and counting their baby’s fingers and toes. In the majority of cases, they themselves will recognize if their baby deviates from normal.
General appearance
A baby’s age and gestation will influence his general appearance. Type of birth, postnatal age, and the timing of the last feed affects his behaviour. A hungry baby will be difficult to examine as many of the assessments require a quiet, calm baby, able to tolerate handling for 10–15 minutes in order to complete the physical examination.
A baby who has had a difficult birth may be very irritable or be in a deep sleep (State 1 – see Box 41.1), and the midwife uses the baby’s behaviour to guide the examination. The physical examination can be delayed until the baby is able to tolerate handling and an interim observational examination undertaken.
Observation
A ‘hands-off’ approach is used when observing the baby. The baby of above 38 weeks’ gestation will display a flexed posture indicating good muscle tone (Fig. 41.3). General features are noted for dysmorphia.
Gestational assessment
Previously, weight defined term and preterm babies; a baby weighing below 2500 g was deemed to be premature. Further research (Battaglia & Lubchenco 1967) showed that gestational age and whether the baby’s growth is appropriate for that age is a greater predictor of outcome.
Assessment tools such as the Dubowitz scoring system (Dubowitz et al 1970) are used to assess the gestational age of the newborn using a neurological scale (see Ch. 44). This assessment is used with babies deemed to be less than 38 weeks’ gestation. The main assessment of gestational age can be carried out using approximate estimates of fetal development, i.e. the LMP, the estimated date of delivery (EDD), ultrasound and physical characteristics (see website).
Measurements
The UK WHO growth charts
These are based on measurements collected by the World Health Organization (WHO) (see website). Healthy breastfed babies whose mothers did not smoke and were not deprived were measured over time. Plotting the baby’s weight and head circumference enables the midwife to identify the ‘at risk’ and validate the normal baby in order to plan future care.
Weight
Scales need to be regularly maintained for accurate measurement and recording. Care should be taken to minimize the baby’s heat loss while weighing by placing him safely in the scales and ensuring that the surroundings are warm and free from draughts.
The weight can be plotted on the centile chart and babies who are small or large for gestational age identified and a plan of action developed, agreed and recorded in the baby notes. Babies below the 9th centile have reduced glycogen stores and may be more prone to hypothermia and hypoglycaemia so thermoregulation and feeding must be given extra attention.
The baby will lose 5–10% of body weight in the first week of life, then steadily gain at an average rate of 25–30 g per day until 6 months of age (Wilkinson 1997).
Note: A baby who has not reached his birth weight by day 10 needs to be reviewed to exclude signs of poor feeding or underlying urinary tract infection.
Dehydration is seen in babies who have yet to establish breastfeeding; identification is vital in order to prevent hypoglycaemia and hypernatraemia. Signs of dehydration include loss of skin turgor, dry mucous membranes, lethargy and a sunken fontanelle, and a weight loss of ≥10% is significant. Urine output is normally 1–3 mL per hour and this will continue regardless of the presence of dehydration; thus, a wet nappy does not indicate wellbeing.
Length
There is debate as to whether or not babies should be measured. Now, for accurate measurement, a supine stadiometer (Wilkinson 1997) newborn length instrument or a rollamat (Fig. 41.4) may be used. Both methods require the baby to be stretched, therefore two persons are required to undertake the measurement accurately.
Head circumference
This measurement is taken with a non-stretchable tape applied closely around the scalp, using the posterior fontanelle and the frontal and parietal eminences as markers. The largest estimate of three is taken. Immediately following birth, the measurement may be increased by oedema or caput, thus it needs to be repeated when any swelling has subsided.
Vital signs
The temperature is measured while the respiratory rate is counted. If the baby is cold (less than 36.5°C), the examination may be discontinued or the baby placed under the radiant heater for the rest of the assessment.
The respiratory rate is usually between 40 and 60 breaths per minute, although the baby’s behaviour prior to counting the respiratory rate needs to be taken into account. As periodic rather than regular breathers, the baby may have periods of even and very uneven breathing and long gaps between breaths. It is important to concentrate on a small area of the abdomen, and this makes counting a little easier.
Note: A baby that is otherwise well but has tachypnoea above 50 at rest, may be exhibiting a sign of respiratory acidosis, and must be referred to a senior paediatrician.
Skin
The skin protects the baby against infection and enables communication, and is sensitive to touch, pressure, temperature and pain. After birth, the baby is rubbed dry, and then touch should be gentle to minimize discomfort to the baby.
The epidermis of the skin of a newborn is thin and delicate and in postmature babies is dry and sometimes peeling (see website).
The best environment to observe the colour of the baby is in natural daylight, as artificial light can affect the depth of colour observed. Pink is the normal colour of newborns. A red/plethoric colour which, when the baby cries, becomes dusky/purple, may be due to an excessively high packed cell volume (PCV) and is deemed to be pathological as it may indicate polycythaemia (see website).
Pale skin or pallor is an indication of poor perfusion and anaemia. Infants of diabetic mothers tend to be pinker than average and ‘postmature’ infants are paler.
Asian and dark-skinned babies may have blue naevi scattered around any area of the body, which may be mistaken for bruises. Parents are sometimes concerned and can be reassured that this deep pigmentation of the skin will fade in a few months.
Petechiae, normally caused through traumatic delivery, for example a tight cord around the neck, should disappear within 24–48 hours. If this does not happen and they appear to multiply, this might be pathological and the baby needs to be referred for diagnosis.
Jaundice may occur physiologically after 48 hours because of extra red cell breakdown in combination with an immature liver which cannot metabolize all unconjugated bilirubin; the latter leaks under the skin and gives a jaundiced colour. The Kramer tool (see Ch. 46) enables estimation of jaundice.
Common variations of the skin include tiny milia on the nose (plugged sweat glands).
Erythema toxicum may be noted. These papular lesions with an erythematous base are found more on the trunk than on the extremities and fade away without treatment by 1 week of age. Occasionally their profusion is alarming.
Haemangiomata
The skin is observed daily for soreness, rashes and septic spots.
Dry skin
A normal skin barrier has cells that are packed tightly together. Applying olive oil for moisturizing or massaging baby skin has been used for years. However, oleic acid, a core component of vegetable oils, disrupts the structure of skin cells, weakening the skin barrier, and either avoiding oils completely (Lavender et al 2009) or using mineral based oils may be preferable.
It has been shown that exposing a skin barrier to an oleic acid solution (10%) causes the skin to commence breakdown. However, sunflower oil is the one oil that is free of oleic acid and can safely be used on baby’s skin to correct dryness (Wong 2004).
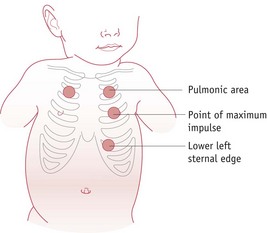
Cardiorespiratory system
The heart and lung assessments are interlinked in order to reduce handling and ascertain how both function, to distinguish between heart and lung physiology and pathology.
Observation
Colour
The infant’s colour is an important index of the function of the cardiorespiratory system.
Chest
The general appearance of the chest is noted, observing the neck and collarbone area. The chest and abdomen are examined whilst observing respirations.
Palpation
The chest is palpated gently as there may be breast enlargement due to maternal hormones and pressure can cause discomfort and pain.
Auscultation
Normal or abnormal breath sounds may be noticed by the practitioner prior to the use of the paediatric stethoscope to identify heart and breath sounds (see website). Done after a period of observation, this can enhance the examiner’s perception, knowledge of and communication with the baby. Warming the chest piece by applying friction to the stethoscope head reduces disturbance of the baby, facilitating auscultation.
Auscultation of breath sounds in the newborn is easier than in a child, as breath sounds are being established with the absence of crackles and wheezes (see Fig. 41.5).
The heart should be examined alongside other aspects such as femoral pulses. To determine whether the heart is on the right or left side, the examiner should observe precordial activity, rate, rhythm, quality of the heart sounds, and the presence or absence of murmurs.
It is difficult to examine the heart of a ‘fussy’ or crying baby. When the baby is peaceful, the rate, rhythm and presence of murmurs can be determined much more easily. The midwife could encourage the mother to pacify the baby by the use of her little finger or a dummy.
The heart rate is normally between 120 and 160 beats per minute, varying with gestational and chronological age and degree of activity.
Murmurs mean less in the newborn period than at any other time. A neonate may be found to have an extremely serious heart anomaly without any murmurs (Hall 1996). A closing ductus arteriosus may cause a murmur that, in retrospect, is only transient, but at the time is very loud, worrisome, and misleading. Gallop sounds may be an ominous finding, while the presence of a split ‘S2’ (i.e. lub dub dub) may be reassuring. If new to auscultation of heart sounds, it is difficult to ascertain SI and S2 (see website). Simultaneous palpation of the brachial pulse and auscultation of the lub dub makes identification of sounds easier.
The stethoscope aids assessment of the cardiovascular system. However, the best assessment is to observe or obtain an accurate history of the baby’s behaviour. A baby who has been active and suddenly becomes lethargic; appears to have less tone; is not interested in feeding; or is tachypnoeic on effort, needs urgent referral and admission by ambulance to the nearest acute neonatal unit.
Major congenital abnormalities can be duct dependent, therefore most cardiac conditions will be diagnosed in the community after discharge. It is important for the parents to understand normal behaviour of the newborn in order to seek advice if their baby deviates from this.
The cardiovascular assessment is not complete until the liver is palpated and deemed to be of normal size.
Congenital heart disease
Significant congenital heart disease (CHD) may be diagnosed at virtually any age. Some conditions are discovered in neonates; others rarely are identified during infancy. The profound haemodynamic transitions that occur at the time of birth make the clinical presentation of heart disease a challenge to practitioners to identify CHD. An understanding of the fetal circulation and transition to postnatal life can provide the clinician with the tools to anticipate and treat problems safely as they arise. For example, a baby who is suspected of having CHD and is cyanosed, is not given oxygen as this will encourage the ductus arteriosus to close faster.
While they cannot be prevented, there are many treatments for the defects and any related health problems. Babies in the UK have the physical examination within 72 hours following birth. While the ductus arteriosus is patent, it is difficult to identify the murmur. Research in Sweden and in the UK has identified the use of pulse oximetry as a test to be utilized to provide an improved means of identifying the at-risk newborns (de-Wahl Granelli et al 2009, Knowles et al 2005).
Pulse oximetry
Pulse oximetry is a non-invasive diagnostic test used for detecting the percentage of haemoglobin (Hb) that is saturated with oxygen. Oxygen saturation is a measure of how much oxygen the blood is carrying as a percentage of the maximum it could carry. A normal pulse reading is 98 to 100; a reading under 95 is too low and may indicate a baby at risk of CHD.
Morphological examination
Accurate assessment of the morphological system is essential for identifying the baby who will need more thorough examination, medical/support services or family counselling. External assessment of dysmorphic features offers clues to the presence of internal anomalies. This examination requires a systematic approach to assessment, including observation and palpation.
The head
Due to moulding, the shape of the head following birth can be round, bullet-shaped or an elongated oval, which may concern parents. They need to be reassured that the head will assume its natural shape, given time. This needs to be noted, as the measurement of the head circumference will differ from birth to that taken 4 or 5 days later. The average full-term head circumference, occipital–frontal diameter measurement, should be approximately 33–38 cm avoiding the ears.
The vault of the head is held in the midline while the size, shape and symmetry are assessed.
The scalp and face should be inspected for cuts, abrasions or bruises. Trauma sites such as fetal blood sample site should be identified and recorded.
The presence of caput succedaneum or cephalhaematoma should be noted (see Ch. 30).
The mobility and width of suture lines and the degree and direction of moulding of the skull bones is noted. Fontanelles are examined: large fontanelles may reflect a delay in ossification of bones and may be associated with hypothyroidism. The anterior fontanelle can provide valuable information on the wellbeing of the baby. In its normal state, it is flat and at the same level as the surrounding bones. A sunken fontanelle can be a symptom of dehydration, and a full and bulging fontanelle and wide sutures are characteristic of hydrocephalus.
The hair
The condition and amount of hair is also noted, as this can be affected by certain metabolic disturbances (e.g. hypothyroidism).
The face
This is examined for normal appearance and symmetry of eyes, ears and features during crying and rest.
The eyes
These are checked for congenital cataracts (UKNSC 2005), and any small haemorrhages within the conjunctiva or under the eyes are noted for size and severity. The eyes may be tested for the red reflex by means of an ophthalmoscope. On examination, the retina is seen as clear and red, the amount of red pigment being dependent on race.
Ophthalmia neonatorum is conjunctivitis that occurs in the newborn. Conjunctivitis is an inflammation of the conjunctiva, the surface or covering of the eye, due to infectious or non-infectious causes. It is identified by an inflamed conjunctiva and watery solution or pus secreted from the eye. Simple infective conjunctivitis is often caused by Staphylococcus aureus, streptococci or Escherichia coli. If infection is suspected, appropriate swabs for Chlamydia trachomatis and gonorrhoea must be taken to exclude these infections which are associated with corneal ulceration and blindness (UKNSC 2008).
The ears
Both are examined for symmetry and normal position on the baby. An imaginary line can be drawn from the inner canthus of the eye to the posterior fontanelle, and the helix of the ear should be above the line to validate normality. The pinna of the ear should be flexible and recoil easily. Accessory auricles, skin tags and sinuses should be noted as they may indicate further abnormalities such as renal (Roth et al 2008). The front and back of the ears should be examined closely for small spots or skin tags.
Hearing
Sensitivity to sounds should be noted. The ability to hear enables babies to communicate and learn about the world they live in. However, one baby will sleep through the loudest music and another will be startled by someone speaking softly. The best time to assess whether babies can hear or not is when they are fully awake. Hearing could be tested by observing the baby when a loud noise is made, but hearing can and should be tested fully at a later date.
Since March 2006, all babies in the UK have been offered a hearing screen test soon after birth. The screening for a hearing defect involves two painless tests – the otoacoustic emissions test (OAE) and the automated auditory brainstem response test (AABR).
Babies are sometimes referred due to the results being affected by the baby being unsettled at the time of the test or because fluid, such as vernix or liquor, was in the ear. The test can be repeated.
The mouth
This should be checked, commencing with the rooting and sucking reflexes, examining the gums for clefts and to ensure that there are no deciduous teeth present. Epstein’s pearls (small white inclusion cysts clustered about the midline at the juncture of the hard and soft palate) are a normal finding. Tongue-tie, in which the frenulum restricts the movement of the tongue, should be identified. The midwife should ensure that there are neither hard nor soft palatal clefts (Bannister 2001).
The palpation and visualization of both the hard and soft palates is imperative – it may be necessary to use a torch and tongue depressor. Midwives and doctors have been shown to have missed a cleft palate (Habel et al 2006).
To examine the mouth with a tongue depressor, the baby should be swaddled and the head gently held to avoid movement during the examination. The spatula is inserted and the tongue depressed, which enables the visualization of hard and soft palates. Wood carries bacteria and multiple spatulas in one box can become contaminated when accessing individual spatulas, thus encouraging cross-infection to the newborn; consequently, spatulas require sterilization prior to use.
The mouth should be examined at regular intervals to validate normality and exclude infection, for example Candida albicans.
The nose
This is examined for normal position and the presence of nares and possible choanal atresia which may or may not be easily identifiable.
Suctioning of babies is no longer advisable except in specific circumstances – for example, the presence of meconium or blood at birth. If a suction catheter is introduced into the nasal passages, the baby may become snuffly due to damaged epithelial lining and dissection of the mucous glands. Unless the baby has a problem with breathing, time will heal the damage and breathing should be normal within several days.
The neck
This is passively examined for rotation and for anterior and lateral flexion and extension.
When there is asymmetrical rotation or lateral flexion or when range of motion is limited, this is recognized as abnormal. The neck should also be examined for goitre and thyroglossal or brachial arch sinus tracks, and the spaces hidden by creases, for evidence of septic spots or irritated skin.
Sharing information with parents
If there are concerns that the baby is dysmorphic, it is important to communicate this sensitively to the parents prior to referral to a senior neonatologist, as a dysmorphic baby may be a clue to the presence of other congenital anomalies such as cardiac or gastrointestinal. One useful way to begin the discussion is to ask the parents whom the baby resembles. The parents may then feel they can disclose their concerns. Even if the baby does have a resemblance to other family members, it does not exclude genetic abnormalities and the baby should be referred to a neonatologist for follow-up. The words used to describe a dysmorphic baby need to accentuate the positive; words such as ‘distinctive facial features’ (Aase 1990) rather than ‘abnormal’ or ‘deformed’.
Musculoskeletal system
History
Prenatal history is vital to musculoskeletal assessment because the uterine environment affects the musculoskeletal development of the fetus. Any event or condition that changes the intrauterine environment can alter fetal growth, movement or position. Factors such as oligohydramnios, breech presentation, abnormal growth patterns and exposure to teratogenic agents may adversely affect the development and maturation of the musculoskeletal system in utero. The skeletal system is interlinked with the neurological system, therefore factors such as possible birth trauma need to be considered.
The birth history, such as duration of labour, signs of fetal distress, type of birth (vaginal or caesarean), has a bearing on conditions such as cerebral palsy and brachial palsy.
In multiple gestations, the birth order is worth noting because there is a higher incidence of congenital hip dysplasia in first-born children.
An accurate gestational age assessment is necessary for assessment of the infant’s posture and muscle tone.
Careful scrutiny and recording of the musculoskeletal system during the first newborn physical examination is imperative as this forms the basis for all future examinations.
Examination
A thorough and systematic physical examination of the skeletal system, including the skull, clavicles, upper limbs, legs, spine and the hips, should be done within the first 24 hours after delivery. Then, should an abnormality of the spine be noted, the senior neonatologist will undertake the hip examination, thereby limiting stress to the newborn. As with other systems, skeletal examinations are undertaken while watching the newborn or while examining other systems.
Evaluation of the musculoskeletal system includes an appraisal of:
Observation proceeds from the general to the specific and includes the ratio of extremity length to body length. General inspection includes observation for symmetry of movement as well as size, shape, general alignment, position and symmetry of different parts of the body.
Soft tissue and muscles should be observed for swelling, muscle wasting and symmetry. Asymmetry of length or circumference, constrictive bands, or length deformities of the extremities should not be present.
Palpation, along with inspection, is used on each extremity to identify component parts (for example, the two bones, radius and ulna, in the forearm), function and normal range of motion.
Upper extremities
Clavicles are inspected and palpated for size, contour and crepitus (grating that can be felt or heard on movement of ends of broken bone). A fractured clavicle, one of the most common birth injuries, should be suspected when there is a history of a difficult delivery, irregularity in contour, shortening, tenderness or crepitus on palpation. It can be very uncomfortable and painful.
Humerus length and contour should be noted. A fractured humerus should be suspected if there is a history of difficult delivery. A mass due to haematoma formation or signs of pain during palpation may also be noted.
Elbow, forearm, and wrist are examined for size, shape and number of bones as well as for range of joint motion.
Hands should be examined for shape, size and posture, and fingers for number, shape and length. Inspection of palm creases should also be included. Although a single simian crease across the palm is usually associated with Down syndrome, it is often found in normal babies.
The fingers are usually flexed in a fist with the thumb under the fingers, The nails, usually smooth and soft and extending to the fingertips, should be examined for size and shape. The mother should be advised how to cut the nails to avoid causing infection to the nail bed, which can cause septicaemia.
Whilst dressing or undressing the newborn. the midwife should note any apparent discomfort.
Abdomen
During fetal life, the fetus relies on the placenta for food and elimination of waste products. In order to sustain life after birth, the newborn baby must adapt to the intermittent intake of nutrients necessary for the body’s metabolic requirements of growth, replacement and energy production, followed by their digestion and utilization and the excretion of waste products. The baby is able to suck and swallow but the digestion process and glucose metabolism take time to adapt to postnatal life.
Physical assessment of the gastrointestinal system therefore commences with the mouth and completes on examination of the anus to confirm normality prior to the baby being able to undertake artificial feeding as this entails a comparatively large intake volume.
The shape of the abdomen should be rounded, soft, symmetrical and slightly protruding. A flat abdomen may signify decreased tone and may herald the presence of abdominal contents in the chest cavity through a diaphragmatic hernia or abnormalities of the abdominal musculature.
Abdominal skin in the term baby is smooth and opaque with a medium-thick texture. Post-term babies have thick, parchment-like skin with superficial or sometimes deep cracking in the creases of the skin, and no vessels seen over the trunk.
Diastasis recti (separation of the rectus muscles) is a common finding in the newborn. Another midline malformation is an umbilical hernia, which reduces spontaneously within 2 years. If it is large, it will require surgical treatment.
Midline defects such as omphalocele or gastroschisis may be seen at birth. As the fetus grows during the first trimester of pregnancy, the developing intestines extend into the umbilical cord and should return to the abdomen by the 11th week of fetal development. However, if the muscles in the abdominal wall fail to close properly, the intestines may partially return to the abdominal cavity. Immediate management is to avoid fluid loss and maintain a clean environment; therefore the baby’s body is placed in a special plastic bag, tied below the arms, or is wrapped in cling film from below the arms.
Umbilical cord is examined prior to cutting (Fig. 41.6) and applying the Hollister clamp, to exclude herniation of intestine into the cord itself and to visualize the presence of three vessels (Lissauer & Fanaroff 2008). Two vessels, one artery and a vein, sometimes indicate renal anomaly (Thummala et al 1988). The cord is a bluish white colour and gelatinous at birth. The quantity of Wharton’s jelly affects the thickness of cord. Large-for-gestational-age infants have thick, gelatinous cords. Babies with congenital syphilis may also have thick cords. A thin small cord is another indication of intrauterine growth restriction.
The cord darkens and shrivels as it dries, and separates by a process of dry gangrene, usually between the fifth and seventh day. It should be dry and without drainage of any type. Discharge of any colour before or after separation is not deemed normal; for example, clear discharge indicates a patent urachus or omphalomesenteric duct (Tappero & Honeyfield 2010).
The area around the cord is observed for any redness, which needs to be dealt with quickly to avoid serious septicaemia. The mother needs to understand the potential for infection from urine and faeces if the umbilical cord is placed inside the nappy, and the midwife can support the mother by showing her how to achieve this (Zupan et al 2004).
Cleaning the cord
A good handwashing technique is essential before attending to the cord, to avoid a spread of the highly dangerous Staphylococcus aureus. The umbilical cord is inspected daily by the midwife for signs of infection and separation. If the cord is soiled by a dirty nappy, it should be cleaned with water only and dried with cotton wool swabs.
Peristaltic movement
The observation of movement needs to be undertaken from the side of the abdomen and at eye level. The midwife should observe for patterns and shape of movement.
Normal abdominal movements are synchronous with chest movements. After 1 hour of life, intermittent peristaltic movement is visible. Continuous peristaltic movement can imply obstruction.
It is important for the midwife to auscultate numerous neonatal bowel sounds in order to confidently validate normality.
Palpation
Before palpating the abdomen, the midwife needs to check that the baby has not been fed a large amount prior to the examination, because such a baby will not be able to tolerate deep palpation. The midwife should stand at the side of the baby and, as with the rest of the examination, the hands must be warm and the nails short to enable palpation of the deep organs to take place without discomfort to the baby. The baby should be lying supine and be relaxed. Palpation should be light at first, progressing to deep palpation. The baby’s facial expression needs to be observed for signs of discomfort or pain; and to validate that the liver and spleen are not enlarged, the baby’s respirations need to be synchronized with the palpation. Flexing the baby’s knee at the hip can allow the abdominal muscles to relax and aid palpation.
Light palpation of the four quadrants assesses the texture and warmth of the skin; it also reveals tenderness and guarding. Deep palpation identifies the absence of masses.
The liver is a superficial organ and palpation needs to take that into consideration. The liver edge should not be more than 2 cm inferior to the right costal margin. Babies in heart failure, where the liver acts as a sponge for fluid, will have an enlarged liver which can be palpated more than 2 cm below the costal margin. Slight oedema can sometimes also be seen around the eyelids.
The spleen is a deep organ but, if enlarged, would become a superficial organ; thus, firm but light pressure is applied in order to confirm normality. A non-palpable spleen equates to normality.
The abdominal area overlying the kidneys is also balloted, applying firm even pressure. The kidney should not be felt (RCM 2009).
Vomiting
Most babies vomit at some time and mostly this is unimportant (Orenstein 1999). However, there are circumstances when the type of vomiting is important, the main one being green bile (Walker et al 2006). It cannot be assumed that this is meconium which was ingested at birth; and the baby should be examined by a senior neonatologist in order to exclude obstruction. Usually, the origin of blood is clear from the history, but if there is any doubt, the laboratory can perform an Apt test (blood mixed with sodium hydroxide), which distinguishes fetal from adult haemoglobin.
Possets are small, frequent vomits, particularly common in the first few days after birth, especially if the baby has swallowed any blood or meconium. ‘Posseting’ is also common when the milk flow is excessive. Most babies cope with these episodes quite well and either swallow the regurgitated contents or cough them out. The parents need to be informed how to manage these episodes. The baby should be left slightly on his side, while the posset is wiped away, and should not be lifted or patted on the back as both may cause overstimulation affecting the coordination of sucking, swallowing and breathing.
If the baby has inhaled a large amount of vomit, appropriate resuscitation needs to take place (Page & Jeffery 2000). Prior to any resuscitation involving mask ventilation, and when the baby has had a feed, the midwife needs to be prepared to pass a nasogastric tube to empty the contents of the stomach to avoid inhalation.
The groin
When lying quietly, the baby’s groin is flat, and if it is thin, visible pulsation of the femoral pulse may be noted. Any visible swelling on crying or on palpation must be referred urgently for diagnosis and management as this might indicate inguinal hernia or undescended testis – in the male or female – querying the sex of the baby.
Genitourinary
Male infant genitalia
Scrotum
All embryos are initially female. Under the influence of testosterone, the labia enlarge to become a scrotum, brownish in pigmentation, and should be fully rugated.
Testes
Normally, the testes of a full-term newborn are approximately 1.5–2 cm in length (Conner 2010). They should be palpated and have a consistency similar to that of a pea. If the scrotum appears discoloured and the testes feel solid, urgent referral is required.
The differential diagnosis for the presence of a solid scrotal mass includes testicular torsion, scrotal haematoma and testicular infarction (Diamond & Gosalbez 1998).
Hydrocele
The signs of a hydrocele include palpation of a cystic mass in the scrotal pouch. The whole scrotum appears swollen and firm – like a balloon filled with water – and it allows the passage of light from a torch (transillumination) (Diamond & Gosalbez 1998). Transillumination of the hydrocele excludes herniation of intestinal contents into the sac. Hydroceles are common and will disappear in time unless they are communicating types.
Undescended testes (UDT)
is a common finding and in most cases the aetiology is unknown. There is an increased risk of infertility and testicular cancer in men with a history of UDT. The testes are very sensitive to temperature and can sometimes be seen moving up the inguinal canal. If a testis is not readily identified, a finger sweep should be performed from the anterior iliac crest along the inguinal canal. It can take up to 3 years for UDT to descend; therefore the baby will be followed up until descent. A timeline and pathway of care is provided by the NIPE standards (UKNSC 2008).
Hypospadias
Congenital abnormalities rarely appear singly; therefore, if the baby is noted to have UDT, extra vigilance is required to assess whether the urethral opening is central on the glans. In hypospadias the opening is found on the undersurface and in epispadias it is above the surface. Observing the baby pass urine is a good method of validating normality.
The penis shape and length are noted. Chordee is a lack of ventral tissue on the penis, leading to it being curved ventrally. Surgery is required to correct the condition.
Female infant genitalia
In the female newborn, the labia majora cover the labia minora and the clitoris.
Before designating a sex to an apparently female infant, the labia majora must be parted and the clitoris observed to be an appropriate size. A discharge from the vagina will indicate that the hymen is perforated. If imperforate, the hymen appears like a tiny smooth bald head (Tappero & Honeyfield 2010). The discharge is usually creamy white at birth, occasionally being replaced after the second day by one appearing bloodstained (pseudomenses) as maternal hormones diminish.
Ambiguous genitalia
If there is doubt as to the sex of the baby, it is important that the concerns are discussed sensitively with the parents (Ahmed & Hughes 2002). Parents will often be very distressed and continually apply pressure to be told the sex of the baby. They will take on board any terminology used, so it is important to avoid the terms ‘he’ or ‘she’ or ‘it’. At the same time, the sex of the baby cannot be entered on the birth certificate until further investigations have been undertaken to confirm the sex. If the ‘wrong’ sex is registered, it is an extremely difficult and lengthy process to correct the mistake (Reiner 1999).
Anus and rectum
The anus and rectum should be checked for patency and position. The practice of using a clinical thermometer to ensure anal patency is now considered outmoded. The anal sphincter is assessed by gently touching the anus and eliciting the anal ‘wink’ – the contraction and retraction of the muscle proving the anus is patent.
Urinary output
is often less than 1 mL/kg/h during the first 12–18 hours after birth. Most healthy term babies urinate within the first 12 hours; however, a small number of healthy infants may not urinate until 24–36 hours after birth. If in doubt as to whether or not a baby has passed urine, place a piece of cotton wool at the end of the penis or urethra to elicit the passage of urine. Using bags should be avoided, as the adhesive can cause skin damage. Persistent oliguria beyond 36 hours should be evaluated in an otherwise healthy infant (Moghal & Embleton 2006).
The odour and colour of the urine are also noted. Occasionally, a red stain is found on the napkin due to urates colouring the urine.
Lower extremities
From observation, the position of the baby’s lower limbs will give a picture of the position adopted in utero. The majority of babies will lie with the legs folded on the abdomen, appearing externally rotated and bowed with everted feet. The baby delivered in a breech presentation often has flexed, abducted hips and extended knees. This positional adaptation of the lower limbs should not be confused with congenital malformations; however, a midwife who is in doubt should seek a second opinion from a peer or a neonatologist.
The midwife should examine the baby for normal appearance and for length, shape and movement of limbs, ensuring that the baby is able to move each limb fully and that the joints are functional. The legs are palpated to ascertain the presence of the femur, tibia and fibula. Femoral length can be observed by straightening both legs together and noting the length or by testing for the Allis sign as follows. Keeping the feet flat on the bed and the femurs aligned, flex both of the baby’s knees. With the tips of the big toes in the same horizontal plane, face the feet, bend so that the baby’s knees are at eye level and note the height of both knees. It will be apparent if one knee is higher than the other. This is a positive Allis sign and may indicate developmental hip displacement.
Ankles and feet
Examination includes observation of resting and active movement. Passive motion of the ankle in dorsiflexion and plantar flexion varies depending on the infant’s position in utero. For example, ankle and forefoot adduction, a positional deformity, can be differentiated from congenital equinovarus (clubfoot) malformation by passively positioning the foot in the midline and gently applying pressure to dorsiflex the foot to form a ‘square window’. A clubfoot or other structurally abnormal foot and ankle will not have a full range of motion, will resist dorsiflexion and will not be able to form a square window (Bridgens & Kiely 2010).
The feet should be examined for shape, size and posture, and to check that the baby is moving both feet and adopts a normal position when at rest. The toes are examined for number, position, spacing, the presence of webbing and whether the nails are a normal shape and appearance. The soles of the feet should be inspected as part of the gestational age assessment and should therefore each be opened fully. This part of the examination is undertaken when eliciting the Babinski reflex (see below).
Assessment of the back
Neural tube defects (NTD) are usually detected before birth as a result of maternal alpha-fetoprotein (AFP) measurement or ultrasound examination. Babies with NTD normally would have been born in an appropriate unit with the relevant staff, neonatologist and neonatal nurses, available at birth and afterwards. However, not all women choose antenatal screening and some may not have had antenatal care; thus, spinal neural defects could still present without warning.
On completing the examination of the lower limbs, the baby is lifted and held suspended with the examiner’s hand under the chest, the back is observed to view the curvature of the spine and the baby’s ability to lift the head. The spine should be straight, excluding scoliosis, kyphosis and lordosis.
The back continues to be observed with the baby lying prone. The spine is then examined from the base of the skull to the coccyx, noting any skin disruption, tufts of hair, soft or cystic masses, haemangioma, pilonidal dimple cysts or sinus tract. These deviations from normal may be signs of congenital spinal anomaly.
The position of the scapulae should also be noted while the infant is in the prone position to rule out Sprengel’s deformity, a winged or elevated scapula.
The entire length of the spine should be gently palpated to ensure that it is complete and that there is no sign of pain.
A baby born at home found to have a meningocele (herniation of meninges) requires urgent referral and transport to hospital. Before and during transport, the lesion – especially if ruptured – should be covered with a sterile, non-adherent dressing. If that is not available, gently place sterile gauze soaked in normal saline and wrap in cling film. Pressure on the affected area must be avoided, the baby must be nursed in the prone position and gently driven into hospital.
Hips
Developmental dysplasia of the hip (DDH) is the preferred term for the disease previously referred to as congenital dislocation of the hip (CDH). The new term takes into consideration that dislocation of the hip can develop after birth and although the hips can be deemed to be normal at birth, the baby can later have a positive screening for a dislocated or dislocatable hip joint.
The assessment of the baby’s hips is undertaken within the first 72 hours of birth to detect conditions that may need early treatment. The UKNSC has produced standards and competencies to ensure consistency throughout the UK for improved and early detection of abnormalities to enable non-invasive treatment and avoid surgical intervention. These standards detail how the examination should be undertaken and by whom (UKNSC 2008). The assessment of the hips should be undertaken on a firm surface and one hip at a time examined by a trained professional.
The pelvic girdle of the neonate is not fully ossified and does not have the same characteristics as the adult pelvic girdle; the acetabula are shallower than in the adult. The acetabulum is still developing and it is quite possible for the femoral head to be able to move outside the acetabulum (luxation or dislocation) or through an abnormality within the acetabulum (subluxation or partial dislocation).
Early detection is vital to avoid surgical intervention. Left untreated, the hip joint develops abnormally and surgical reduction is required. Early diagnosis enables the use of splints, allowing the hip joint to develop normally.
Examination
The ideal time to undertake examination of the hip (Fig. 41.7) is within the first 72 hours. Prior to the examination, the practitioner needs to recognize the importance of history in identifying the babies at risk. High-risk factors for DDH include (Keay & Morgan 1982):
The left hip is more frequently affected than the right.
Care that can prevent DDH includes postnatal application of mechanical forces associated with the baby able to fully abduct the hips, such as being allowed to lie in the prone position when awake and being carried in a sling with hips fully abducted – African babies whose mothers transport them in this way have a low incidence of DDH.
The hips should be examined at regular intervals for congenital dislocation, which may be identified by the use of one of two tests:
A distinctive ‘clunk’ is of significance. However, ‘clicks’, often felt while performing these tests, are not predictive of DDH but can be confusing for an inexperienced examiner.
Ideally, examination of the hips should be the final part of the examination as it is often disruptive and uncomfortable for the baby. The midwife can utilize methods to reduce discomfort, such as sucking the mother’s finger or, if bottle-feeding, the use of the pacifier.
Practitioners undertaking the examination of the hips need to have undertaken training during which they have been both taught and observed by an expert in the examination (STEPS 2004). Practice on the ‘Baby Hippy’ manikin is advised prior to examining a baby. An inexperienced practitioner can cause damage to the baby by failing to diagnose a false negative test, because of poor practice, or use of excessive force on a dislocated hip during abduction, causing damage to blood supply and ligaments.
Observation
The midwife should observe the baby and note any difficulties with abduction. For example, if the baby found the procedure of examining the femoral pulses distressing or the Allis sign was positive, there may be an indication that the right or left hip may be dislocated.
Ortolani and Barlow tests
The baby should be lying relaxed on a flat, firm surface in an environment warm and free from draughts. It is vital that the practitioner examines only one hip at a time with a full focus on undertaking the manoeuvre correctly.
Ortolani test
If the hip is dislocated, it will not be possible to abduct it and the neonate will keep the thigh at an angle less than expected. This angle is noted and recorded.
Barlow test
These two manoeuvres are then repeated with the other hip joint.
If any deviations from normal are noted, the examiner should refer the baby to a senior medical practitioner.
Additional investigations
X-rays are unhelpful in assessment as the femoral head is cartilaginous until 6 months of age. Ultrasound examination of the hips is undertaken as part of screening for DDH; however, its effectiveness is not recognized by all.
The Ortolani and Barlow manoeuvres remain the best screening method for DDH if undertaken by a competent practitioner.
The leaflet on developmental dysplasia of the hip, congenital talipes equinovarus (clubfoot) and lower limb deficiencies (STEPS 2004) should be given to parents of affected babies. This will inform them of facts relating to deviations from normal in the lower limbs and raise awareness that although the baby’s hips may be stable at the first examination, it is important to have the hips examined once again at 6 to 8 weeks to exclude the development of an abnormality.
Neurological examination
Assessment of neurological function is important in assessing successful transition from extrauterine life and environmental factors in the perinatal period that may have caused a pathological response of the central and peripheral nervous systems. Early identification of deviations from normal can significantly reduce mortality and improve the quality of life for the newborn and family.
The Apgar score and its running commentary may indicate a baby who requires focus on the neurological system. The type of delivery, such as in shoulder dystocia, can cause brachial plexus damage, facial and Erb’s palsy, paralysed vocal cords and damage to one or both of the phrenic nerves, all of which need to be excluded.
The examination of the neurological system is, in large part, undertaken by examining the other systems.
Physical examination
Probably the most reliable information that can be obtained quickly from a neurological evaluation is through discussing the baby’s behaviour with the mother and the baby’s response to handling during the preceding parts of the physical examination.
Level of consciousness
One of the most important areas of the examination is the neonate’s alertness and interaction with his mother, his overall behaviour and movement preceding and during the examination.
Cry
This is the baby’s main method of communication to alert carers to pain, hunger, discomfort or suffering. It is important that the carers understand the types of crying in order to give appropriate care. When listening to the sound of crying, note whether it is a clear tone, without hoarseness, or nasal tone. Equally, the type of pain and whether or not pain relief is required by the baby needs to be established. Change from an uncomfortable position, a soothing bath, massage, or sucking on a finger or breast might bring relief. It takes time and skill to interpret the different sounds, and conscious effort needs to be given to listening and observing babies in order to perfect this form of communication.
Head
The shape and size, fontanelle and suture size are examined as stated during the morphological examination. Cranial bruit may indicate an intracranial vascular malformation.
Face
Facial dysmorphism may indicate a genetic syndrome such as trisomy 18, and facial features are observed during crying for facial palsy.
Eye examination
Pupils should be equal and react to light and the red reflex should be present and completely round in shape.
Skin
Cutaneous birthmarks such as café-au-lait spots may indicate the presence of a genetic disorder such as neurofibromatosis.
Reflexes
It is now known that babies are aware of their in-utero environment and at birth are equipped for survival. They can hear, smell, taste, see up to a distance of 30 cm (Wilkinson 1997) and favour the colours black and white. The majority of reflexes are deemed to be primitive involving the brainstem and spinal cord.
The complete behavioural examination is quite dependent on infant–examiner interaction and thus the midwife should aim to examine the baby with gentleness and respect, communicating with him on both verbal and non-verbal levels.
Cranial nerves
The 12 pairs of cranial nerves are referred to by name or roman numerals. They originate from different parts of the brain and assessment of their function confirms normality and recognizes deviations from normal (see website).
Assessment of the autonomic nervous system
The autonomic nervous system is involved in a complex of reflex activities essential to sustain life and these are dependent on sensory input to the brain or spinal cord. Normal autonomic function in a baby at term is well developed and can be observed through the following reflex actions:
Identifying and managing pain and stress in the term newborn
Until the 1980s, it was thought that babies did not feel pain, therefore pain relief was rarely given.
Dummies laced with brandy and sugar were sometimes used to pacify a very distressed newborn; however, procedures which required pain relief in children or adults were undertaken on newborns without pain relief. Today, the physiology of pain pathways in babies is better understood, and it is now recognized that the baby’s spinal sensory nerve cells are more excitable than those of adults. Midwives, doctors and nurses rely on patients to report their pain and its severity. The baby is unable to speak, so practitioners need to be aware of evidence of pain and obtain experience of the normal behaviour of the baby. The inability to communicate in no way negates the possibility that the baby is experiencing pain and is in need of appropriate pain relief (Lago et al 2009). Time spent observing babies is invaluable, in trying to understand how to adapt the care provided in order to minimize stress and pain to the newborn.
The physiological response to painful stimulus in the baby is greater and lasts for a longer period of time than in the adult. Adults have a sophisticated nerve pathway which can narrowly pinpoint the area of painful stimulus. In the newborn, this pathway is still developing, which means the baby is unable to localize pain but can feel pain in response not only to painful stimuli but also to touch over a wide area of the body (Anand & Scalzo 2000). Damaged skin, either from a heel prick or from ventouse or other instrumental birth, will be very sensitive to touch.
Newborns feel pain (Anand 2001) and therefore procedures that can cause pain should be kept to a minimum. Handing the baby to his mother at birth instantly provides human contact. Being stroked gently and given the opportunity to suck at the breast will reduce the newborn’s pain and discomfort (Carbajal et al 2003). Bathing or washing the baby for whatever reason needs to be delayed until the baby has had time to recover and for his skin to heal prior to pressure being applied to broken or bruised skin. It is important to note that damage to the skin at birth or soon after can cause the damaged area to be oversupplied with sensory nerve terminals which will leave the area hypersensitive to touch for some weeks after the wound has heeled. This information needs to be shared with parents for them to have an insight into the baby’s behaviour when that area is handled.
Causes of pain
The effect of certain procedures needs to be considered in relation to the amount of pain caused to the baby, for example:
Signs of pain
One of the best indicators is vocal expression, heard in long-lasting crying. Facial expressions – brow bulge, eye squeeze, and nasolabial furrow – are also reliable indicators of pain (Stevens & Johnston 1993). Other behavioural signs of pain include pedalling movement of the legs, toes spread, legs tensed and pulled up, agitation of arms and a withdrawal reaction.
Sucrose administration
The majority of research regarding non-pharmacological analgesia, performed on babies at term undergoing a heel prick procedure, recommends that prior to this procedure, if possible, the baby should:
One study has shown that breastfeeding alone can reduce crying; however, a number of randomized controlled trials provide unequivocal evidence that babies cry less when given a combination of nutritive or non-nutritive sucking and sucrose (Carbajal et al 2003).
Many cultures recognize that the taste of sweetness reduces pain, as does massage, talking gently and obtaining eye contact with the baby.
Research on pain, undertaken on the blood spot screening and venepuncture procedures, recognizes these as being very painful for the newborn and for the parents observing a distressed newborn. There needs to be clear justification to undertake every heel-prick procedure.
Jitteriness versus seizures
Jitteriness, although not a type of seizure, is a movement disorder characterized by movements with qualities primarily of tremulousness and occasionally of clonus. It is important to distinguish jitteriness from seizures.
If the limb that is tremulous is pressed down against the mattress and the tremors stop, seizure is excluded; if movement continues, it is a positive sign of seizure. The midwife must call for help and stay with the baby to observe the progress and length of seizures; this is also important in order to provide support if the respiratory system is involved (Silverstein & Jensen 2007).
Assessment of feeding
The final and crucial part of the assessment to ascertain wellbeing is that of feeding. A baby who has been feeding well and who becomes tachypnoeic on feeding will require urgent further assessment.
Bad news
Prior to undertaking the examination of the newborn, it is important for practitioners to have had training in ‘giving bad news’, recognizing that what they might deem good news may not produce the same reaction in the parents. A girl rather than a boy is a disaster for some parents. The smallest of deformities, such as an extra digit, can cause major concerns for parents who wished for the ‘perfect’ baby. For major congenital abnormalities, it is important to know specialist centres in the area and the latest management and treatment in order to have some insight when the parents start asking questions about the wellbeing of their baby.
Consequently, it is important that the examination of the newborn is undertaken where privacy is guaranteed and the parents feel that they can ask questions and that they have the professionals’ full attention. If the midwife is not able to convey bad news, the examination should be delayed until the support of a senior colleague, with training and experience, is available.
Mother–baby attachment
Parent–infant interaction is believed to play a central role in the baby’s social, emotional and physiological development. The quality of the interaction between mother and baby can provide the baby with an environment for optimal development and growth. The foundation of this relationship is trust and affection. If there is failure to develop this relationship, the baby is at risk of delays in neurological developmental, child abuse, neglect and failure to thrive (Pridham et al 1999). Research has shown that educating the mother to understand her baby and his behaviour can have a positive effect on maternal–infant interaction (Anderson 1981).
Today in the UK, women stay in hospital less than 24 hours for a non-complicated birth, and therefore teaching opportunities are limited. Antenatal classes are an ideal opportunity to provide the necessary education that serves as a valuable health-promotion tool to effect positive parenting beginning at birth.
After the birth, mother and baby should be given a minimum of 1 hour of supported privacy together in the labour ward, and this should then be followed by keeping mother and baby together as much as possible during the early neonatal period when they are getting to know one another and mothering skills are developing. This is easily achieved if the birth takes place in the home but more difficult in the hospital setting. The Maternity Services Advisory Committee (MASC 1985) advocated that the baby’s cot remains beside the mother’s bed. Restricted contact between mother and baby in the early postnatal period is associated with less affectionate maternal behaviour and maternal feelings of incompetence and lack of confidence (Thomson & Westreich 1989). Maternal–infant attachment established from birth is strengthened by the woman getting to understand her baby, and because handling can aid this process, the mother is encouraged to care for her baby soon after birth. The use of strategies such as the shortened Brazelton Neonatal Behavioural Assessment Scale (see website) can assist parents to learn more about their baby’s capabilities (Nugent 2004). Unrestricted access allows the mother freedom to respond to her baby whenever he is awake. Although this aspect of initiating the relationship between mother and baby is important, the ability to enhance that relationship is dependent on the mother’s physiological wellbeing.
There must be communication between mother and baby in order for interaction to take place. Mother and baby need to respond to each other’s cues and the environment must be such as to facilitate that interaction. It is difficult for a woman who has had a difficult delivery to respond physically if she is unable to move and handle her baby. The midwife needs to provide the response to the cues given by the baby while allowing the mother to recover, and, in doing so, acts as a role model, educating the woman about the different cues, such as hunger, boredom, discomfort and pain, which the baby provides. A crying baby can overwhelm the woman’s psychological wellbeing at this vulnerable time following birth. The father, too, should be involved in his baby’s care and progress, otherwise he may feel neglected and become jealous of the close relationship developing between mother and baby.
Three stages have been described in the maternal– infant attachment process.
To reach this final stage, mother and baby grow to know and love each other as they interact. The baby may initiate interaction by crying. The mother responds by rocking the cot or picking the baby up and cuddling him. This is the expression of a mother’s instinct to tend and protect her child. The baby stops crying when he is picked up and becomes alert and responsive. The mother should be encouraged to talk and establish eye-to-eye contact. In turn, the baby gazes at his mother and responds; thus mother–baby interaction is synchronized and attachment develops.
At times, mother and baby have to be separated because of maternal illness or because the baby needs intensive or special care; most mothers are likely to overcome any adverse effects of this separation (Thomson & Westreich 1989). Some consider that the degree to which a mother perceives separation as having an adverse effect on her mothering ability may be related to the outcome (Richards 1978, Ross 1980) and also the contact between mother and baby while the baby is in hospital (Moore & Nelson 2003). Women of low socioeconomic status, with low social support, may be more adversely affected by restricted contact with their baby than their more affluent counterparts (Thomson & Westreich 1989). One study demonstrated this, highlighting the benefits of early and prolonged contact following birth to women and babies with low social support (Anisfeld & Lipper 1983).
Not uncommonly, some mothers are worried that they do not feel a maternal instinct or really love their baby during the early days of motherhood. They need reassurance that their feelings are quite normal and that, as they and their baby learn to know each other, love will follow.
Each society and culture has its behavioural norms about what is accepted as normal and appropriate maternal–infant interaction and it is important to acknowledge these differences.
Newborn behaviour
For the first 6 weeks of life, the baby does not distinguish night from day and spends 24 hours sleeping, waking, crying and feeding. Newborns have a very small stomach and require regular intake of food; they will, on the whole, feed every 3–4 hours. What parents find difficult is that the baby is awake at night and asleep during the day. Babies move from one sleep state to another, from quietly looking around, actively responding to sounds, to crying. Parents are sometimes concerned not to ‘spoil’ their babies and sometimes delay in answering their baby’s cries. Prior to 6 months of age, the neural processes are not mature enough to enable the baby to manipulate the carer; to think ‘if I cry I will get my mother to come to see to me’. If and when the baby cries, it is for a reason such as hunger, fear, discomfort, pain or boredom. Rather than spoiling the baby, if the mother/carer answers the cries immediately, the baby will develop securely, knowing his needs will be answered (Bell & Ainsworth 1972).
A baby’s primary needs are for food, fluid, sleep, warmth, security and love, and the method of expressing those needs is crying. This is a signal to the carer to communicate with the baby, recognize the cry and meet the need; parents and practitioners need time to understand and interpret. Parents need to be given this information to recognize the newborn baby’s needs and know what to do to help the baby calm down.
When responding to the baby’s cry, the mother/carer must be 10–12 inches in front of the baby, establish eye contact and at the same time find a way to control the baby’s flailing arms and legs while firmly and gently talking to him (Ludington-Hoe et al 2002). The baby can alternatively be held against the mother’s body and be talked to gently.
Another method of satisfying the baby is to provide non-nutritive sucking by giving him fingers or a dummy to suck or by putting the baby to the breast. Teaching the baby the difference between night and day is also helpful. That could be accomplished by placing the baby in an environment of light and normal sounds during the day, and at night making sure the environment is dark, or the lights dimmed and sounds are gentle. Parents need to understand that they will not always succeed immediately in stopping the baby from crying; however, a variety of methods should be tried until successful. Scientifically, it is recognized that crying in the newborn can cause pathological changes to the cardiorespiratory system (Anderson 1988); therefore, listening to the baby crying without taking action to stop the crying is no longer acceptable practice.
Placing the cot near the bed will make access to the baby easier at night-time. The baby will develop an organized pattern of sleep by the age of 16 weeks (Matsuoka et al 1991). At 6 weeks the baby should begin to smile, and at 3 months take note of his surroundings.
Sleep versus play time
Following any physical examination, the baby is dressed and given to a parent to hold. When the baby is placed in the cot, the position of the baby in the cot is informed by the ‘Back to sleep’ campaign to prevent sudden infant death syndrome (SIDS) (see Ch. 50). It is important to recognize that the baby is positioned on the back for sleep, but when the baby is awake, evidence recommends that he is able to play in the prone position for about 15 minutes a day. This can prevent conditions such as delays in motor skills, positional plagiocephaly (flattening of the occipital region of the head), positional torticollis (contracture of the sternocleidomastoid muscle) and shoulder retraction. None of these is life-threatening or should lead to abandoning the ‘back to sleep’ position (Fig. 41.8).
Postnatal care
Care of the newborn is based on the philosophy of a continuum of quality care that commences with antenatal and intrapartum care. This begins with getting to know the fetus both antenatally and during the intrapartum period, and that knowledge informs the management of care given to the baby from the moment of birth to 28 days.
Preparation of the parents for early detection of deviations from normal and management of the newborn is vital wherever the birth takes place. It is expected that preparation for parenthood has taken place in order to reduce the psychological stress to both the baby and family.
The UK is a multicultural society and in order for a partnership of care to be developed with parents, the cultural norms of the ethnic groups need to be understood. Many traditional practices need to be understood rather than feared. One of these practices, cup-feeding, utilized effectively today in neonatal units, was brought to the UK from Africa, where the survival of high-risk newborns was achieved by cup-feeding well before its introduction to the UK. The midwife needs to make links with women’s ethnic groups and religious leaders in order to learn and understand traditional practice so that safe care can be provided to the newborn by supporting and, where necessary, sensitively changing practice.
Follow-up of the baby
When the baby is deemed to be well and no longer requires midwifery care, the baby is transferred from the midwife to the health visitor, who usually visits the mother and baby at home. The health visitor discusses problems with the mother, gives advice on topics such as childcare and family planning, and encourages the mother to take her baby to the child health clinic or to her GP regularly. The baby’s development will be followed closely by initiating the vaccination programme and developmental assessments. The GP is responsible for general medical care but some babies with medical problems are also followed up by a neonatologist/paediatrician.
Hygiene
Because newborn infants have little resistance to microorganisms, they are highly susceptible to infection. An apparently mild infection can rapidly become a serious condition in the newborn, so every effort must be made to protect them from infection.
There are three main factors in avoiding infection:
Sources of infection
The infant may be infected in a number of ways:
Attendants
The nose, throat or skin of those dealing with the baby may harbour dangerous organisms (staphylococci and streptococci). This includes not only the midwife and doctor but also the parents themselves.
Hands and clothing
Facilities for washing the hands must be available after personal toilet and in the nursery and wards. Disposable hand towels are preferable for use. The hands must be washed before and after attending each baby. Antiseptic hand cream applied to the hands after washing is valuable. Long fingernails not only hinder many examination procedures but also can cause the baby discomfort and harbour infection.
Dust
The air and dust in maternity wards and nurseries contain many bacteria, one of which, Staphylococcus aureus, is most liable to cause infection. The ward and nursery should be adequately ventilated. Cleaning must be thorough and should minimize dust being scattered around the room. Floors are cleaned using vacuum cleaners with filters preventing bacteria passing out of the machine into the air. Damp dusting is advisable. Cots, trolleys and tables can be wiped over with dilute antiseptic and dried well.
Fomites
Infection may be spread by unsterilized instruments, bowls and dressings. Clothing and napkins may be the source. Before the era of pre-packed feeds and disposable bottles and teats in hospitals, inadequately sterilized bottles and teats were a source of infection. This may still be the case in some homes.
Cross-infection
Rooming-in, in which babies are nursed beside the mother’s bed, is the usual practice nowadays. This aids the bonding process and reduces the risk of cross-infection. Overcrowding in wards and nurseries should be avoided. Individual equipment for bathing and changing should be provided, disposable articles being used whenever possible. Any baby suspected of infection should be isolated from other babies.
The main routine care of the baby involves changing the napkins, washing or bathing, and feeding. Soiled linen and napkins should be handled, with gloved hands, as little as possible and placed in bags and closed while carried to the waste bin.
Bathing the baby
The issue of transmission of human immunodeficiency virus (HIV) through maternal vaginal secretions has encouraged the practice of the baby being given a bath soon after birth. Currently, there are no studies to support the reduction of HIV from this. Vernix is deemed to protect the skin, and may act as an antibacterial agent and promote healing from the trauma of birth. Bathing the baby removes this skin-protecting vernix. Work undertaken so far suggests the importance of the newborn’s condition and temperature being stabilized in the normal range for 2–4 hours prior to the bath being given, in order to avoid hypothermia (see Ch. 42).
Bath time offers parents a time to get to know their baby through tactile interaction.
In order to protect the skin pH, it is important that any cleansing agents that are used have a neutral pH and minimal dyes and perfumes, and that the baby’s skin is rinsed well to reduce the risk of allergic sensitization (Cetta et al 1991, NICE 2006, Crozier & Macdonald 2010).
Whilst the baby is being bathed, care must be taken to prevent abrasions of the skin which might allow entry of bacteria. Great care must also be taken with the eyes and cord, which are both sites of potential infection.
Chafing or intertrigo, caused by friction between two skin surfaces, is usually seen in the groin or axilla and in the folds of the neck. It indicates that the baby’s skin has not been adequately dried after being washed or bathed. The energetic removal of vernix caseosa may also be the cause. After a bath, a dabbing movement with a soft towel should dry the folds in the skin. Where chafing has occurred, drying and a very light dusting with an antiseptic powder will heal the lesion.
Dermatitis of the groin, buttocks and anus
Redness and excoriation may be produced around the groin, anus and buttocks. The development of this condition may be influenced by wetness of the skin (see website). When the skin is exposed to urine, the pH rises and changes from acid to alkaline, enabling penetration of microorganisms into the building blocks of the stratum corneum.
Treatment and care
Newborn screening tests
Various tests and examinations may be carried out in the early neonatal period to detect the presence of specific abnormal conditions. Early diagnosis and treatment may ameliorate the effects of many conditions. Thus, some inborn errors of metabolism may be managed with diet and/or drugs (see website).
Blood spot screening test
The UK National Screening Committee recommend that all babies in the UK are offered screening for phenylketonuria (PKU), congenital hypothyroidism (CHT), sickle cell disorders (SCD), cystic fibrosis (CF) and medium-chain acyl-CoA dehydrogenase deficiency (MCADD). The test is offered to all babies in the UK at the age of 5 to 8 days.
Phenylketonuria is an autosomal recessive genetic condition where babies are unable to metabolize phenylalanine (an amino acid found in proteins). It affects 1 in 10,000 babies in the UK. Babies who are not treated develop serious permanent mental disability. Once diagnosed, the baby should be started on a low protein diet by day 21 of age and this will effect a good quality of life.
Congenital hypothyroidism affects 1 in 4000 babies in the UK. Screening is done by measuring the level of thyroxine or thyroid-stimulating hormone (TSH) in the blood sample,. Further investigations of thyroid function will be required if the test result is abnormal. If the condition is confirmed, early treatment with levothyroxine (thyroxine) sodium by the age of 21 days will prevent mental handicap and promote normal growth (Kelnar et al 1995).
Sickle cell disorders affect 1 in 2500 babies in the UK and the aim of screening is to identify the babies who are affected in order to commence penicillin prophylaxis. This baby is at risk of infections and severe acute anaemia in the first few years of life if left untreated.
Deficiency of medium-chain acyl-CoA dehydrogenase causes the accumulation of medium-chain fatty acids and impairs ketone production.
Cystic fibrosis (CF) affects 1 in 2500 babies across the UK. It is an autosomal recessive inherited condition which mainly affects babies’ digestion and lung function. Diagnosis enables nutrition and growth to be improved and reduces chest infection.
Hearing tests
Recent technological advances have led to improved screening methods that can identify the majority of children with impaired hearing and it is recommended that babies should be screened before leaving hospital.
The test is non-invasive and involves the measurement of otoacoustic emissions (OAE) which are low-level inaudible sounds produced by the inner ear. The screening of newborns is part of the continuum of early childhood hearing tests which screen and diagnose to improve identification of hearing impairment in young children.
The value of such a test is that children with hearing impairments can be given extra help at an early age to develop speech since the critical period for language and speech development is generally regarded as the first 2 years of life.
Vaccinations at birth
Infants are known to be susceptible to infections in the first 2 months of life as the immune system of the newborn is immature and takes some time to develop. The UK Joint Committee for Vaccination and Immunisation (JCVI) recommends that parents give informed consent for their babies to be vaccinated against two of the most serious infections – tuberculosis (BCG) and hepatitis B – where it is necessary (DH 2009).
Vaccination is now offered in the early postnatal period to babies whose parents have emigrated from a country with high prevalence of tuberculosis or whose family members have previously been infected.
Hepatitis B vaccine is given within the first 12 hours following birth to babies whose mothers are chronic carriers of hepatitis B virus or who have had acute hepatitis B during pregnancy.
Record-keeping
Record-keeping is an important aspect of care given to the newborn. The examination needs to be recorded along with the underpinning rationale for present and future management (NICE 2006). This commences with completing the case notes and birth notification (within the first 36 hours), which must be sent to the appropriate medical officer. Important information such as whether or not the baby has fed or has passed urine and meconium needs to be documented in the notes, in order to form a baseline for further assessments.
To midwives, the hands-on care may be seen as more important than documentation, but medico-legal experts and the NMC advise that if contemporaneous records are not kept, then legally it did not happen (NMC 2009). Good record-keeping provides evidence of actions and omissions, protects the newborn by promoting high standards of clinical care, promotes team communication, gives an accurate account of treatment, and provides the ability to detect problems at an early stage (Walton & Bedford 2007).
A common core content record is available for every child and parent and for each professional engaged in delivery, to record the progress and care given, and this record is the UK Parent-held Child Health Record (PHCHR or ‘Red Book’).
The new WHO growth charts are included to document and support the decisions the practitioners make in regard to the care of the newborn.
Following the first holistic physical examination, the practitioner should complete the PHCHR and give it to parents to commence the documentation of the forthcoming journey.
Conclusion
The aim of this chapter has been to introduce the reader to physiology applied to the examination of the newborn and the care given to newborn babies and their families. For more detail, the reader is referred to the website for other resources and links, providing the in-depth knowledge required to undertake the examination of the newborn.