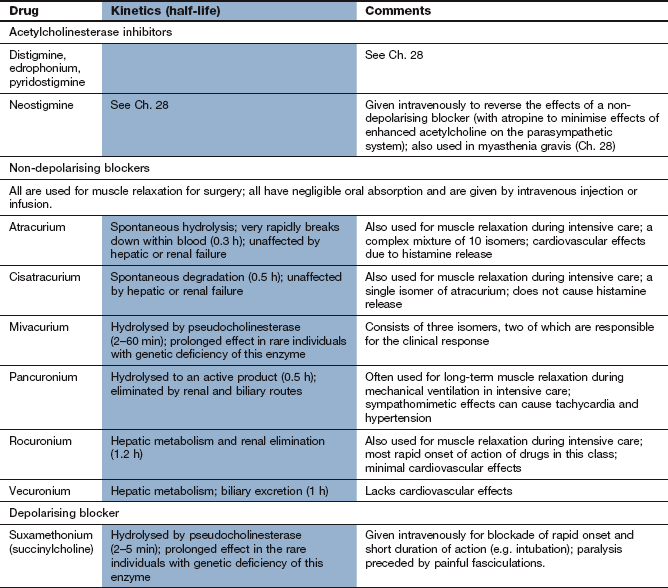
The neuromuscular junction and neuromuscular blockade
Neuromuscular transmission
The neuromuscular junction is a specialised synapse of a somatic neuron with the sarcolemma of skeletal muscle, termed the motor endplate (Fig. 27.1A). In mammals, depolarisation of the postsynaptic membrane at the motor endplate causes contraction of the muscle fibre in an all-or-nothing response. Greater contractility is achieved by the stimulation of more motor endplates.
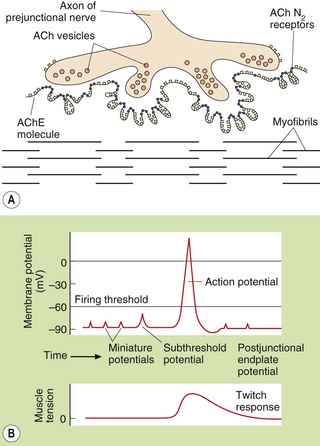
Fig. 27.1 Acetylcholine (ACh) at the neuromuscular junction. (A) The released ACh acts upon postsynaptic nicotinic N2 receptors on the motor endplate, opening cation channels and an influx of Na+ occurs, resulting in depolarisation. (B) At rest, insignificant amounts of ACh are released, and miniature endplate potentials generated are insufficient to reach the threshold potential to cause a propagated action potential. If sufficient ACh is released, an action potential is propagated, causing muscle contraction. Non-depolarising muscle relaxants prevent the generation of the action potential by blocking N2 receptors. AChE, acetylcholinesterase.
The neurotransmitter at the neuromuscular junction is acetylcholine (ACh), acting at postsynaptic nicotinic N2 receptors. The processes of synthesis and release of ACh are described in Chapter 4 in relation to the general properties of neurotransmitters in the nervous system. The presynaptic nerve terminal at the neuromuscular junction contains 300 000 or more vesicles, each of which may contain up to 5000 molecules of ACh (known as a quantum). In response to an action potential, up to 500 vesicles discharge their contents into the synapse over a very short period (0.5 ms). Each N2 receptor has two binding sites for ACh, and the Na+ channel in the centre of the receptor opens when both sites are occupied (Ch. 1). This allows an influx of Na + into the muscle cell and depolarisation of the motor endplate. If depolarisation is sufficient to reach the firing threshold potential for the cell then voltage-gated Na+ channels open, full depolarisation of the muscle cell is triggered and an action potential is generated and propagated along the postsynaptic membrane. Initiation of an action potential requires the release of 50–200 quanta of ACh, which will activate 10–15% of motor endplate N2 receptors (Fig. 27.1b).
The action potential generated in the skeletal muscle cell passes along the sarcolemma into the T tubules, where Ca2+ is released from the sarcoplasmic reticulum. The increased availability of intracellular Ca2+ brings about the processes that result in muscle contraction.
The action of ACh on N2 receptors is very short-lived (about 0.5 ms) because the synaptic cleft contains large amounts of the extremely potent enzyme acetylcholinesterase (AChE), which rapidly degrades ACh (Ch. 4). An esterase called pseudocholinesterase (butyrylcholinesterase, plasma cholinesterase) in plasma hydrolyses any ACh that escapes from the synaptic cleft; it acts more slowly than AChE. Pseudocholinesterase is important pharmacologically because of its ability to metabolise several drugs with ester bonds. Tissue esterases that break down ACh are also present in many cells, notably in the liver.
Although ACh is the neurotransmitter responsible for contraction of both skeletal muscle and most smooth muscles, the basic organisation and functioning of these neuroeffector systems are very different, as shown in Table 27.1.
Table 27.1
Comparison of skeletal and smooth muscle innervation
| Property | Skeletal muscle fibre | Smooth muscle fibre |
| Nerves supplying fibre | Single | Multiple |
| Junction | Highly organised motor endplate | Simple |
| Neurotransmitter | Acetylcholine | Acetylcholine |
| Receptor subtype | Nicotinic N2 | Muscarinic (mainly M3) |
| Receptor distribution | Only at motor endplate; only one motor endplate per muscle fibre | Widely on the muscle surface |
| Effects of stimulation | Single nerve contracts the whole muscle fibre (all-or-none response) | Each nerve contracts part of muscle fibre (graded response) |
| Effect of overdose with acetylcholinesterase inhibitor | Flaccid paralysis | Spasticity |
Drugs acting at the neuromuscular junction
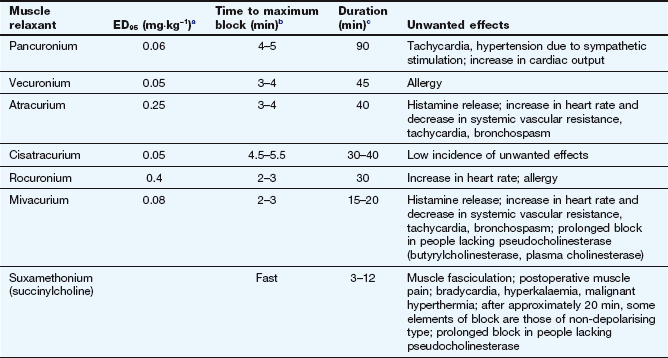
Acetylcholinesterase inhibitors
AChE inhibitors block the breakdown of ACh following its release in neuronal synapses and at neuroeffector junctions. The mechanisms of action of different types of AChE inhibitor are described in Chapter 4; they are non-selective and prolong the availability and actions of ACh at all its receptors (nicotinic N1 and N2 and muscarinic). Full details of AChE inhibitors in the treatment of myasthenia gravis are given in Chapter 28.
Inhibitors of acetylcholine release
Botulinum toxin from the anaerobic bacillus Clostridium botulinum decreases the release of ACh from vesicles. It binds selectively to cholinergic nerve terminals and, after internalisation via a cell membrane vesicle, is released into the cell cytoplasm. The toxin cleaves cytoplasmic proteins (SNARE proteins) on the cell membrane that are essential for docking and fusion of vesicles with the neuronal membrane, and this inhibits neurotransmitter release. This chemical denervation stimulates collateral axon growth which eventually results in the formation of a new neuromuscular junction. Botulinum toxin is extremely dangerous, as evidenced by the consequences of botulinum poisoning, but it also has clinical roles when injected locally. Two toxin serotypes, A and B, are used in clinical practice as botulinum toxin–haemagglutinin complex. Injection into skeletal muscles produces local muscle paralysis for many weeks until new nerve terminals develop. Botulinum toxin is used to treat involuntary movements such as blepharospasm (spasm of the eyelids) or torticollis (wry-neck) and to relieve spasticity (Ch. 24). It is also used by local injection to reduce excessive sweating, because it inhibits ACh release at sweat glands, and is occasionally injected into facial muscles for the prophylaxis of migraine (Ch. 26). Botulinum toxin is increasingly being used for cosmetic reasons to temporarily remove frown lines and wrinkles.
Antagonists/blockers at the neuromuscular junction
Skeletal muscle relaxation is achieved by drugs that specifically and reversibly block the actions of ACh on nicotinic N2 receptors at the neuromuscular junction; they do not affect autonomic nervous system function (i.e. the actions of ACh on nicotinic N1 receptors in ganglia or on muscarinic receptors at postganglionic nerve endings). Drugs that block the neuromuscular junction almost all resemble ACh in that they have a quaternary ammonium (N+) group that binds strongly to the anionic site of the nicotinic N2 receptor (Fig. 27.2).
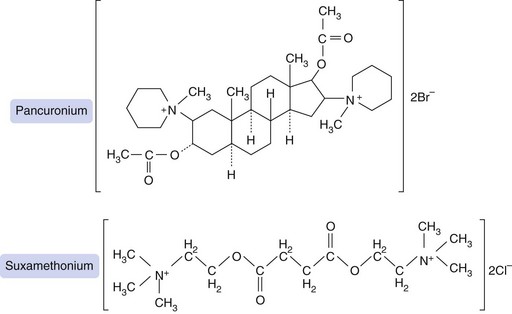
Fig. 27.2 Structures of pancuronium, a non-depolarising blocking drug, and suxamethonium (succinylcholine), a depolarising blocker. Suxamethonium resembles two molecules of acetylcholine, each with a quaternary ammonium (N+) group, linked back-to-back. Pancuronium was designed to have a similar spatial arrangement of quaternary nitrogens, but held rigidly in place by a steroid bridge that is resistant to pseudocholinesterase.
A neuromuscular blocker must occupy more than 75% of postsynaptic N2 receptors before it can start to produce neuromuscular blockade. The potency of a neuromuscular blocker is measured by the ED95, which is the dose required to produce 95% depression of muscular twitch (Table 27.2). About twice this dose is required for muscle relaxation adequate to permit tracheal intubation. The laryngeal muscles are more rapidly paralysed than other skeletal muscle groups, but the effect is often of shorter duration. This may reflect either the higher blood flow to this muscle, or the greater density of N2 receptors.
Table 27.2
Properties of some neuromuscular junction-blocking drugs
aED95 is the effective dose required to suppress muscle twitch by 95%.
bTime to maximum block following administration of the dose used for intubation (double the ED95).
cTime taken to recover to 25% of the original twitch height after an intubation dose (double the ED95).
Recovery of muscle action depends on the rate of clearance of the drug from the plasma. After a bolus injection of many neuromuscular blockers, this is largely a result of redistribution to tissues, rather than metabolism. Redistribution lowers the plasma concentration and consequently the concentration at the motor endplate. For those drugs which undergo rapid redistribution, the duration of neuromuscular blockade will be more prolonged after repeated boluses or infusions; this is because when equilibrium between plasma and tissue concentrations has been reached the duration of effect then becomes mainly dependent on metabolism.
Competitive N2 receptor antagonists (non-depolarising blockers)
Mechanism of action and effects: Competitive N2 receptor antagonists bind to the nicotinic N2 receptor at the neuromuscular junction without causing depolarisation of the postsynaptic membrane. This blocks the depolarising effect of ACh and leads to muscle relaxation. Whereas it takes two ACh molecules to activate the N2 receptor, only one molecule of a non-depolarising neuromuscular blocker at each receptor will prevent neurotransmission. Inhibition of ACh hydrolysis by an AChE inhibitor (usually neostigmine, see Ch. 28) will prolong the action of ACh and rapidly reverse competitive neuromuscular junction blockade. This principle is used at the end of an operation to aid recovery of the paralysed person.
Pharmacokinetics: Because of their high polarity, conferred by the quaternary ammonium (N+) group (Fig. 27.2), non-depolarising neuromuscular blockers are not absorbed from the gastrointestinal tract and are given by intravenous injection. They have a low apparent volume of distribution and do not cross the blood–brain barrier. Vecuronium is partially metabolised in the liver but largely excreted unchanged in the bile. Pancuronium and rocuronium are eliminated by a combination of metabolism and renal excretion of unchanged drug. Atracurium (a mixture of 10 isomers) and cisatracurium (a single isomer of atracurium) undergo non-enzymatic spontaneous degradation as well as hydrolysis by non-specific esterases in the plasma, which is an advantage in hepatic or renal impairment. Mivacurium, like suxamethonium (see below), is metabolised by pseudocholinesterase.
The speed of onset of action and duration of action of competitive blockers differ (Table 27.2). Rocuronium has the fastest onset of action, within 2 min, which can be useful during endotracheal intubation. With the exception of atracurium and cisatracurium, the duration of action of competitive antagonists at the neuromuscular junction (from about 30 min for vecuronium up to 75 min for pancuronium) is mainly determined by redistribution of the drug into the body tissues. This leads to prolonged action with repeated doses (see above). The duration of effect of atracurium and cisatracurium is about 40 min. This is slightly longer than predicted from their plasma half-lives and may be a consequence of high-affinity binding sites close to the ACh receptor acting as a reservoir for the drug.
Unwanted effects: See Table 27.2.
Depolarising neuromuscular-blocking drugs
Mechanism of action and effects: Suxamethonium is succinic acid with a choline molecule attached at each carboxylic acid group; it therefore resembles two ACh molecules joined back to back (Fig. 27.2). When two molecules of suxamethonium bind to the nicotinic N2 receptor it acts as an agonist and depolarises the motor endplate. However, suxamethonium is not hydrolysed by AChE and therefore produces more prolonged depolarisation than ACh. This probably leads to a conformational change in the receptor that allows the Na+ channel to close despite the continued presence of an agonist, a process of desensitisation. As a result, the muscle repolarises and, although it can respond to direct electrical stimulation, it can no longer be stimulated via the neuronal release of ACh. Indeed, if the amount of available synaptic ACh is enhanced (such as occurs with the use of an AChE inhibitor), it will intensify a partial depolarising blockade rather than reverse it. After about 20 min of depolarising blockade, suxamethonium exhibits the properties of a ‘dual block’, with the onset of a non-depolarising competitive type of blockade. At this stage, a partial blockade can be partially reversed by an AChE inhibitor.
Pharmacokinetics: Suxamethonium is a highly polar molecule, is not absorbed orally and must be given intravenously. It has a low volume of distribution and does not cross the blood–brain barrier. Suxamethonium has an onset of action within 1 min, but is rapidly hydrolysed by pseudocholinesterase, which results in a very short duration of action (about 3–12 min). An infusion is therefore necessary to produce a prolonged effect. A very prolonged paralysis occurs in about 1 in 2000–3000 individuals, who have a genetically determined deficiency of pseudocholinesterase (see Ch. 2). In this population, the action of suxamethonium is terminated after some 2–3 h by renal excretion.
 There is an initial depolarisation of the motor endplates prior to blockade, which results in muscle fasciculation.
There is an initial depolarisation of the motor endplates prior to blockade, which results in muscle fasciculation.
 Postoperative muscle pain is common, possibly due to muscle damage caused by fasciculation.
Postoperative muscle pain is common, possibly due to muscle damage caused by fasciculation.
 Prolonged neuromuscular blockade and apnoea occur if there is a low circulating concentration of pseudocholinesterase, through either a genetic deficiency or a decreased synthesis of the enzyme in severe liver disease.
Prolonged neuromuscular blockade and apnoea occur if there is a low circulating concentration of pseudocholinesterase, through either a genetic deficiency or a decreased synthesis of the enzyme in severe liver disease.
 The use of suxamethonium during anaesthesia has been linked with the development of a rare but potentially fatal disorder of muscles known as malignant hyperthermia, with a rapid rise in temperature, muscle rigidity, tachycardia and acidosis. Predisposition to this condition has an autosomal dominant inheritance and is associated with mutations in the ryanodine receptor RyR1. Treatment is with dantrolene (Ch. 24).
The use of suxamethonium during anaesthesia has been linked with the development of a rare but potentially fatal disorder of muscles known as malignant hyperthermia, with a rapid rise in temperature, muscle rigidity, tachycardia and acidosis. Predisposition to this condition has an autosomal dominant inheritance and is associated with mutations in the ryanodine receptor RyR1. Treatment is with dantrolene (Ch. 24).
 Stimulation of nicotinic N1 receptors at autonomic ganglia and muscarinic receptors produces bradycardia, especially with repeated doses.
Stimulation of nicotinic N1 receptors at autonomic ganglia and muscarinic receptors produces bradycardia, especially with repeated doses.
 Hyperkalaemia, probably due to persistent activation of of N2 receptors resulting in escape of intracellular K+ ions from skeletal muscle fibres. This is especially marked in the presence of prolonged immobilisation, major tissue trauma and severe burns.
Hyperkalaemia, probably due to persistent activation of of N2 receptors resulting in escape of intracellular K+ ions from skeletal muscle fibres. This is especially marked in the presence of prolonged immobilisation, major tissue trauma and severe burns.
Indications for neuromuscular-blocking drugs
The neuromuscular-blocking drugs are used in both surgical procedures and intensive care. Their administration forms part of the achievement of balanced anaesthesia described in Chapter 17.
Endotracheal intubation
Relaxation of the vocal cords allows easy passage of an endotracheal tube. A rapid onset of action is essential to minimise the risk of aspiration of gastric contents. This is the only current major use for suxamethonium. Because of frequent unwanted effects, suxamethonium is largely superseded by rapidly acting non-depolarising blockers such as rocuronium.
During surgical procedures
Neuromuscular blockade produces muscle relaxation for procedures such as abdominal incisions. Selective skeletal muscle relaxation reduces the concentrations of general anaesthetic needed for deep anaesthesia. It can be achieved by either a single injection of a drug or intravenous infusion for more prolonged surgery. At the end of the operation the effect of a non-depolarising blocker can be reversed within 1 min by intravenous injection of neostigmine. A muscarinic receptor blocker such as glycopyrrolate or atropine (Ch. 4) is given before neostigmine to prevent bradycardia or excessive salivation produced by stimulation of muscarinic receptors.
In intensive care
Neuromuscular blockade is used in addition to analgesia and sedation during mechanical ventilation, particularly if respiratory drive is suppressed (e.g. in adult respiratory distress syndrome), in status asthmaticus, for status epilepticus or tetanus and for people with raised intracranial pressure.
For a case-based question on the use of neuromuscular junction-blocking drugs in surgery, see the Self-assessment section of Ch. 17.
True/false questions
1. A skeletal muscle fibre is innervated by a single motor endplate.
2. The nicotinic receptors at skeletal muscle and autonomic ganglia are identical.
3. Suxamethonium is a competitive antagonist of nicotinic N2 receptors.
4. Vecuronium has no haemodynamic effects.
5. Malignant hyperthermia is a rare, genetically determined reaction to suxamethonium.
6. The duration of action of all non-depolarising neuromuscular junction-blocking drugs is limited by redistribution.
7. Suxamethonium is the only muscle relaxant used for tracheal intubation.
8. Cisatracurium is well absorbed orally.
9. Botulinum toxin acts postsynaptically to block depolarisation induced by acetylcholine.
10. Botulinum toxin can be used to treat excessive sweating.
One-best-answer (OBA) question
Which statement about neuromuscular junction-blocking drugs is the most accurate?
A Rocuronium crosses the blood–brain barrier and has direct effects on the central nervous system.
B Pancuronium is the neuromuscular-blocking drug of choice for a surgical procedure that will take less than 30 min.
C Suxamethonium is the only muscle relaxant that can be used for electroconvulsive therapy.
D About 50% of nicotinic N2 receptors must be occupied by a non-depolarising neuromuscular-blocking drug to produce complete block of an evoked twitch.
1. True. Contraction of a skeletal muscle fibre is an all-or-none response to nerve stimulation at the motor endplate.
2. False. The nicotinic N2 receptor at skeletal muscle is selectively blocked by non-depolarising and depolarising muscle relaxants, while the N1 receptor at autonomic ganglia is selectively blocked by ganglion-blocking drugs (which now have little clinical application).
3. False. Suxamethonium is a nicotinic N2 receptor agonist that causes persistent depolarisation then desensitisation of the receptor.
4. True. Unlike atracurium and mivacurium, vecuronium does not cause histamine release so it does not have significant haemodynamic effects.
5. True. Malignant hyperthermia in response to suxamethonium, halothane and some other drugs is associated with mutations in the ryanodine receptor RyR1, and is treated with dantrolene, a ryanodine receptor antagonist.
6. False. Atracurium and cisatracurium undergo spontaneous hydrolysis and mivacurium is hydrolysed by pseudocholinesterase.
7. False. Short-acting non-depolarising neuromuscular blockers such as rocuronium can also be used for intubation. The use of suxamethonium is declining because of the occurrence of malignant hyperthermia.
8. False. Because of the quaternary nature of their structures, neuromuscular junction-blocking drugs are not absorbed orally and do not cross the blood–brain barrier or placenta.
9. False. Botulinum toxin binds pre-synaptically to cause long-lasting block of ACh release.
10. True. Local injections of botulinum toxin can reduce activity of sweat glands, which are innervated by postsynaptic cholinergic fibres of the sympathetic nervous system.
OBA answer
A Incorrect. All non-depolarising neuromuscular-blocking drugs have a quaternary ammonium in their structure and will not cross the blood–brain barrier.
B Incorrect. Pancuronium is a long-acting blocking drug and is used for procedures taking longer than 90 min.
C Incorrect. Short-acting non-depolarising blocking drugs such as rocuronium or mivacurium are viable alternatives.
D Incorrect. More than 90% of receptors need to be occupied to produce a complete block of skeletal muscle contractility.
E Correct. Atracurium is one of the most potent neuromuscular-blocking drugs causing the release of histamine.
Bowman, WC. Neuromuscular block. Br J Pharmacol. 2006;147:S277–S286.
Denborough, M. Malignant hyperthermia. Lancet. 1998;352:1131–1136.
Fagerlund, MJ, Eriksson, LI. Current concepts in neuromuscular transmission. Br J Anaesth. 2009;103:108–114.
Moore, EW, Hunter, JM. The new neuromuscular blocking agents: do they offer any advantages? Br J Anaesth. 2001;87:912–925.
Münchau, A, Bhatia, KP. Uses of botulinum toxin injection in medicine today. BMJ. 2000;320:161–165.